- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

The Effects of Drug Addiction on the Brain and Body
Signs of drug addiction, effects of drug addiction.
Drug addiction is a treatable, chronic medical disease that involves complex interactions between a person’s environment, brain circuits, genetics, and life experiences.
People with drug addictions continue to use drugs compulsively, despite the negative effects.
Substance abuse has many potential consequences, including overdose and death. Learn about the effects of drug addiction on the mind and body and treatment options that can help.
Verywell / Theresa Chiechi
Drug Abuse vs. Drug Addiction
While the terms “drug abuse” and “drug addiction” are often used interchangeably, they're different. Someone who abuses drugs uses a substance too much, too frequently, or in otherwise unhealthy ways. However, they ultimately have control over their substance use.
Someone with a drug addiction uses drugs in a way that affects many parts of their life and causes major disruptions. They can't stop using drugs, even if they want to.
The signs of drug abuse and addiction include changes in behavior, personality, and physical appearance. If you’re concerned about a loved one’s substance use, here are some of the red flags to watch out for:
- Changes in school or work performance
- Secretiveness
- Relationship problems
- Risk-taking behavior
- Legal problems
- Aggression
- Mood swings
- Changes in hobbies or friends
- Sudden weight loss or gain
- Unexplained odors on the body or clothing
Drug Addiction in Men and Women
Men and women are equally likely to develop drug addictions. However, men are more likely than women to use illicit drugs, die from a drug overdose, and visit an emergency room for addiction-related health reasons. Women are more susceptible to intense cravings and repeated relapses.
People can become addicted to any psychoactive ("mind-altering") substance. Common addictive substances include alcohol , tobacco ( nicotine ), stimulants, hallucinogens, and opioids .
Many of the effects of drug addiction are similar, no matter what substance someone uses. The following are some of the most common effects of drug addiction.
Effects of Drug Addiction on the Body
Drug addiction can lead to a variety of physical consequences ranging in seriousness from drowsiness to organ damage and death:
- Shallow breathing
- Elevated body temperature
- Rapid heart rate
- Increased blood pressure
- Impaired coordination and slurred speech
- Decreased or increased appetite
- Tooth decay
- Skin damage
- Sexual dysfunction
- Infertility
- Kidney damage
- Liver damage and cirrhosis
- Various forms of cancer
- Cardiovascular problems
- Lung problems
- Overdose and death
If left untreated drug addiction can lead to serious, life-altering effects on the body.
Dependence and withdrawal also affect the body:
- Physical dependence : Refers to the reliance on a substance to function day to day. People can become physically dependent on a substance fairly quickly. Dependence does not always mean someone is addicted, but the longer someone uses drugs, the more likely their dependency is to become an addiction.
- Withdrawal : When someone with a dependence stops using a drug, they can experience withdrawal symptoms like excessive sweating, tremors, panic, difficulty breathing, fatigue , irritability, and flu-like symptoms.
Overdose Deaths in the United States
According to the Centers for Disease Control and Prevention (CDC), over 100,000 people in the U.S. died from a drug overdose in 2021.
Effects of Drug Addiction on the Brain
All basic functions in the body are regulated by the brain. But, more than that, your brain is who you are. It controls how you interpret and respond to life experiences and the ways you behave as a result of undergoing those experiences.
Drugs alter important areas of the brain. When someone continues to use drugs, their health can deteriorate both psychologically and neurologically.
Some of the most common mental effects of drug addiction are:
- Cognitive decline
- Memory loss
- Mood changes and paranoia
- Poor self/impulse control
- Disruption to areas of the brain controlling basic functions (heart rate, breathing, sleep, etc.)
Effects of Drug Addiction on Behavior
Psychoactive substances affect the parts of the brain that involve reward, pleasure, and risk. They produce a sense of euphoria and well-being by flooding the brain with dopamine .
This leads people to compulsively use drugs in search of another euphoric “high.” The consequences of these neurological changes can be either temporary or permanent.
- Difficulty concentrating
- Irritability
- Angry outbursts
- Lack of inhibition
- Decreased pleasure/enjoyment in daily life (e.g., eating, socializing, and sex)
- Hallucinations
Help Someone With Drug Addiction
If you suspect that a loved one is experiencing drug addiction, address your concerns honestly, non-confrontationally, and without judgment. Focus on building trust and maintaining an open line of communication while setting healthy boundaries to keep yourself and others safe. If you need help, contact the SAMHSA National Helpline at 1-800-662-4357.
Effects of Drug Addiction on an Unborn Child
Drug addiction during pregnancy can cause serious negative outcomes for both mother and child, including:
- Preterm birth
- Maternal mortality
Drug addiction during pregnancy can lead to neonatal abstinence syndrome (NAS) . Essentially, the baby goes into withdrawal after birth. Symptoms of NAS differ depending on which drug has been used but can include:
- Excessive crying
- Sleeping and feeding issues
Children exposed to drugs before birth may go on to develop issues with behavior, attention, and thinking. It's unclear whether prenatal drug exposure continues to affect behavior and the brain beyond adolescence.
While there is no single “cure” for drug addiction, there are ways to treat it. Treatment can help you control your addiction and stay drug-free. The primary methods of treating drug addiction include:
- Psychotherapy : Psychotherapy, such as cognitive behavioral therapy (CBT) or family therapy , can help someone with a drug addiction develop healthier ways of thinking and behaving.
- Behavioral therapy : Common behavioral therapies for drug addiction include motivational enhancement therapy (MET) and contingency management (CM). These therapy approaches build coping skills and provide positive reinforcement.
- Medication : Certain prescribed medications help to ease withdrawal symptoms. Some examples are naltrexone (for alcohol), bupropion (for nicotine), and methadone (for opioids).
- Hospitalization : Some people with drug addiction might need to be hospitalized to detox from a substance before beginning long-term treatment.
- Support groups : Peer support and self-help groups, such as 12-step programs like Alcoholics Anonymous, can help people with drug addictions find support, resources, and accountability.
A combination of medication and behavioral therapy has been found to have the highest success rates in preventing relapse and promoting recovery. Forming an individualized treatment plan with your healthcare provider's help is likely to be the most effective approach.
Drug addiction is a complex, chronic medical disease that causes someone to compulsively use psychoactive substances despite the negative consequences.
Some effects of drug abuse and addiction include changes in appetite, mood, and sleep patterns. More serious health issues such as cognitive decline, major organ damage, overdose, and death are also risks. Addiction to drugs while pregnant can lead to serious outcomes for both mother and child.
Treatment for drug addiction may involve psychotherapy , medication, hospitalization, support groups, or a combination.
If you or someone you know is experiencing substance abuse or addiction, contact the Substance Abuse and Mental Health Services Administration (SAMHSA) National Helpline at 1-800-662-4357.
American Society of Addiction Medicine. Definition of addiction .
HelpGuide.org. Drug Abuse and Addiction .
Tennessee Department of Mental Health & Substance Abuse Services. Warning signs of drug abuse .
National Institute on Drug Abuse. Sex and gender differences in substance use .
Cleveland Clinic. Drug addiction .
National Institute on Drug Abuse. Drugs, Brains, and Behavior: The Science of Addiction Drugs and the Brain .
American Heart Association. Illegal Drugs and Heart Disease .
American Addiction Centers. Get the facts on substance abuse .
Szalavitz M, Rigg KK, Wakeman SE. Drug dependence is not addiction-and it matters . Ann Med . 2021;53(1):1989-1992. doi:10.1080/07853890.2021.1995623
Centers for Disease Control and Prevention. Drug overdose deaths in the U.S. top 100,000 annually .
American Psychological Association. Cognition is central to drug addiction .
National Institute on Drug Abuse. Understanding Drug Use and Addiction DrugFacts .
MedlinePlus. Neonatal abstinence syndrome .
National Institute on Drug Abuse. Treatment and recovery .
Grella CE, Stein JA. Remission from substance dependence: differences between individuals in a general population longitudinal survey who do and do not seek help . Drug and Alcohol Dependence. 2013;133(1):146-153. doi:10.1016/j.drugalcdep.2013.05.019
By Laura Dorwart Dr. Dorwart has a Ph.D. from UC San Diego and is a health journalist interested in mental health, pregnancy, and disability rights.

Violence in Families: Assessing Prevention and Treatment Programs (1998)
Chapter: 9 conclusions and recommendations, 9 conclusions and recommendations.
The problems of child maltreatment, domestic violence, and elder abuse have generated hundreds of separate interventions in social service, health, and law enforcement settings. This array of interventions has been driven by the urgency of the different types of family violence, client needs, and the responses of service providers, advocates, and communities. The interventions now constitute a broad range of institutional services that focus on the identification, treatment, prevention, and deterrence of family violence.
The array of interventions that is currently in place and the dozens of different types of programs and services associated with each intervention represent a valuable body of expertise and experience that is in need of systematic scientific study to inform and guide service design, treatment, prevention, and deterrence. The challenge for the research community, service providers, program sponsors, and policy makers is to develop frameworks to enhance critical analyses of current strategies, interventions, and programs and identify next steps in addressing emerging questions and cross-cutting issues. Many complexities now characterize family violence interventions and challenge the development of rigorous scientific evaluations. These complexities require careful consideration in the development of future research, service improvements, and collaborative efforts between researchers and service providers. Examples of these complexities are illustrative:
- The interventions now in place in communities across the nation focus services on discrete and isolated aspects of family violence. They address different aspects of child maltreatment, domestic violence, and elder abuse. Some
- interventions have an extensive history of experience, and others are at a very early stage of development.
- Many interventions have not been fully implemented because of limited funding or organizational barriers. Thus in many cases it is too early to expect that research can determine whether a particular intervention or strategy (such as deterrence or prevention) is effective because the intervention may not yet have sufficient strength to achieve its intended impact.
- The social and institutional settings of many interventions present important challenges to the design of systematic scientific evaluations. The actual strength or dosage of a particular program can be directly influenced by local or national events that stimulate changes in resources, budgets, and personnel factors that influence its operation in different service settings. Variations in service scope or intensity caused by local service practices and social settings are important sources of "noise" in cross-site research studies; they can directly affect evaluation studies in such key areas as definitions, eligibility criteria, and outcome measures.
- Emerging research on the experiences of family violence victims and offenders suggests that this is a complex population composed of different types of individuals and patterns of behavior. Evaluation studies thus need to consider the types of clients served by particular services, the characteristics of those who benefited from them, and the attributes of those who were resistant to change.
In this chapter the committee summarizes its overall conclusions and proposes policy and research recommendations. A key question for the committee was whether and when the research evidence is sufficient to guide a critical examination of particular interventions. In some areas, the body of research is sufficient to inform policy choices, program development, evaluation research, data collection, and theory-building; the committee makes recommendations for current policies and practices in these areas below. In other areas, although the research base is not yet mature enough to guide policy and program development, some interventions are ready for rigorous evaluation studies. For this second tier of interventions, the committee makes recommendations for the next generation of evaluation studies. The committee then identifies a set of four topics for basic research that reflect current insights into the nature of family violence and trends in family violence interventions. A final section makes some suggestions to increase the effectiveness of collaborations between researchers and service providers.
Conclusions
The committee's conclusions are derived from our analysis of the research literature and discussions with service providers in the workshops and site visits, rather than from specific research studies. This analysis takes a client-oriented
approach to family violence interventions, which means that we focus on how existing services in health, social services, and law enforcement settings affect the individuals who come in contact with them.
- The urgency of the need to respond to the problem of family violence and the paucity of research to guide service interventions have created an environment in which insights from small-scale studies are often adopted into policy and professional practice without sufficient independent replication or reflection on their possible shortcomings. Rigorous evaluations of family violence interventions are confined, for the most part, to small or innovative programs that provide an opportunity to develop a comparison or control study, rather than focusing on the major existing family violence interventions.
- This situation has fostered a series of trial-and-error experiences in which a promising intervention is later found to be problematic when employed with a broader and more varied population. Major treatment and prevention interventions, such as child maltreatment reporting systems, casework, protective orders, and health care for victims of domestic violence, battered women's shelters, and elder abuse interventions of all types, have not been the subjects of rigorous evaluation studies. The programmatic and policy emphasis on single interventions as panaceas to the complex problems of family violence, and the lack of sufficient opportunity for learning more about the service interactions, client characteristics, and contextual factors that could affect the impact of different approaches, constitute formidable challenges to the improvement of the knowledge base and prevention and treatment interventions in this filed.
- In all areas of family violence, after-the-fact services predominate over preventive interventions. For child maltreatment and elder abuse, case identification and investigative services are the primary form of intervention; services designed to prevent, treat, or deter family violence are relatively rare in social service, health, and criminal justice settings (with the notable exceptions of foster care and family preservation services). For domestic violence, interventions designed to treat victims and offenders and deter future incidents of violence are more common, but preventive services remain relatively underdeveloped.
- The current array of family violence interventions (especially in the areas of child maltreatment and elder abuse) is a loosely coupled network of individual programs and services that are highly reactive in nature, focused primarily on the detection of specific cases. It is a system largely driven by events, rather than one that is built on theory, research, and data collection. Interventions are oriented toward the identification of victims and the substantiation and documentation of their experiences, rather than the delivery of recommended services to reduce the incidence and consequences of family violence in the community overall. As a result, enormous resources are invested to develop evidence that certain victims or offenders need treatment, legal action, or other interventions, and comparatively limited funds are available for the treatment and support services themselves—a
- situation that results in lengthy waiting lists, discretionary decisionmaking processes in determining which cases are referred for further action, and extensive variation in a service system's ability to match clients with appropriate interventions.
- The duration and intensity of the mental health and social support services needed to influence behaviors that result from or contribute to family violence may be greater than initially estimated. Family violence treatment and preventive interventions that focus on single incidents and short periods of support services, especially in such areas as parenting skills, mental health, and batterer treatment, may be inadequate to deal with problems that are pervasive, multiple, and chronic. Many programs for victims involve short-term treatment services—less than 6 weeks. Services for offenders are also typically of short duration. Yet research suggests that short-term programs designed to alter violent behavior are often the least likely to succeed, because of the difficulties of changing behavior that has persisted for a period of years and has become part of an established pattern in relationships. Efforts to address fundamental sources of conflict, stress, and violence that occur repeatedly over time within the family environment may require extensive periods of support services to sustain the positive effects achieved in short-term interventions.
- The interactive nature of family violence interventions constitutes a major challenge to the evaluation of interventions because the presence or absence of policies and programs in one domain may directly affect the implementation and outcomes of interventions in another. Research suggests that the risk and protective factors for child maltreatment, domestic violence, and elder abuse interact across multiple levels. The uncoordinated but interactive system of services requires further attention and consideration in future evaluation studies. Such evaluations need to document the presence and absence of services that affect members of the same family unit but offer treatment for specific problems in separate institutions characterized by different service philosophies and resources.
- For example, factors such as court oversight or mandatory referrals may influence individual participation in treatment services and the outcomes associated with such participation. The culture and resources of one agency can influence the quality and timing of services offered by another. Yet little information is available regarding the extent or quality of interventions in a community. Clients who receive multiple interventions (especially children) are often not followed through different service settings. Limited information is available to distinguish key features of innovative interventions from those usually offered in a community; to describe the stages of implementation of specific family violence programs, interventions, or strategies; to explain rates of attrition in the client base; or to capture case characteristics that influence the ways in which clients are selected for specific treatment programs.
- The emergence of secondary prevention interventions specifically targeted to serve children, adults, and communities with characteristics that are
- thought to place them at greater risk of family violence than the general population, along with the increasing emphasis on the need for integration and coordination of services, has the potential to achieve significant benefits. However, the potential of these newer interventions to reduce the need for treatment or other support services over the lifetime of the client has not yet been proven for large populations.
- Secondary preventive interventions, such as those serving children exposed to domestic violence, have the potential to reduce future incidents of family violence and to reduce the existing need for services in such areas as recovery from trauma, substance abuse, juvenile crime, mental health and health care. However, evaluation studies are not yet available to determine the value of preventive interventions for large populations in terms of reduction of the need for treatment or other support services over a client's lifetime.
- The shortage of service resources and the emphasis on reactive, short-term treatment have directed comparatively little attention to interventions for people who have experienced or perpetrated violent behavior but who have not yet been reported or identified as offenders or victims. Efforts to achieve broader systemic collaboration, comprehensive service integration, and proactive interventions require attention to the appropriate balance among enforcement, treatment, and prevention interventions in addressing family violence at both state and national levels. Such efforts also need to be responsive to the particular requirements of diverse ethnic communities with special needs or unique resources that can be mobilized in the development of preventive interventions. Because they extend to a larger population than those currently served by treatment centers, secondary prevention efforts can be expensive; their benefits may not become apparent until many years after the intervention occurs.
- Policy leadership is needed to help integrate family violence treatment, enforcement and support actions, and preventive interventions and also to foster the development of evaluations of comprehensive and cross-problem interventions that have the capacity to consider outcomes beyond reports of future violent behavior.
- Creative research methodologies are also needed to examine the separate and combined effects of cross-problem service strategies (such as the treatment of substance abuse and family violence), follow individuals and families through multiple service interventions and agency settings, and examine factors that may play important mediating roles in determining whether violence will occur or continue (such as the use of social networks and support services and the threat of legal sanctions).
- Most evaluations seek to document whether violent behavior decreased as a result of the intervention, an approach that often inhibits attention to other factors that may play important mediating roles in determining whether violence will occur. The individual victim or offender is the focus of most interventions and
- the unit of analysis in evaluation studies, rather than the family or the community in which the violence occurred.
Integrated approaches have the potential to illuminate the sequences and ways in which different experiences with violence in the family do and do not overlap with each other and with other kinds of violence. This research approach requires time to mature; at present, it is not strong enough to determine the strengths or limitations of strategies that integrate different forms of family violence compared with approaches that focus on specific forms of family violence. Service integration efforts focused on single forms of family violence may have the potential to achieve greater impact than services that disregard the interactive nature of this complex behavior, but this hypothesis also remains unproven.
Recommendations For Current Policies And Practices
It is premature to offer policy recommendations for most family violence interventions in the absence of a research base that consists of well-designed evaluations. However, the committee has identified two areas (home visitation and family preservation services) in which a rigorous set of studies offers important guidance to policy makers and service providers. In four other areas (reporting practices, batterer treatment programs, record keeping, and collaborative law enforcement approaches) the committee has drawn on its judgment and deliberations to encourage policy makers and service providers to take actions that are consistent with the state of the current research base.
These six interventions were selected for particular attention because (1) they are the focus of current policy attention, service evaluation, and program design; (2) a sufficient length of time has elapsed since the introduction of the intervention to allow for appropriate experience with key program components and measurement of outcomes; (3) the intervention has been widely adopted or is under consideration by a large number of communities to warrant its careful analysis; and (4) the intervention has been described and characterized in the research literature (through program summaries or case studies).
Reporting Practices
All 50 states have adopted laws requiring health professionals and other service providers to report suspected child abuse and neglect. Although state laws vary in terms of the types of endangerment and evidentiary standards that warrant a report to child protection authorities, each state has adopted a procedure that requires designated professionals—or, in some states, all adults—to file a report if they believe that a child is a victim of abuse or neglect. Mandatory reporting is thought to enhance early case detection and to increase the likelihood that services will be provided to children in need.
For domestic violence, mandatory reporting requirements for professional groups like health care providers have been adopted by the state of California and are under consideration in several other states. Mandatory reports are seen as a method by which offenders who abuse multiple partners can be identified through the health care community for law enforcement purposes. Early detection is assumed to lead to remedies and interventions that will prevent further abuse by holding the abuser accountable and helping to mitigate the consequences of family violence.
Critics have argued that mandatory reporting requirements may damage the confidentiality of the therapeutic relationship between health professionals and their clients, disregard the knowledge and preferences of the victim regarding appropriate action, potentially increase the danger to victims when sufficient protection and support are not available, and ultimately discourage individuals who wish to seek physical or psychological treatment from contacting and disclosing abuse to health professionals. In many regions, victim support services are not available or the case requires extensive legal documentation to justify treatment for victims, offenders, and families.
For elder abuse, 42 states have mandatory reporting systems. Several states have opted for voluntary systems after conducting studies that considered the advantages and disadvantages of voluntary and mandatory reporting systems, on the grounds that mandatory reports do not achieve significant increases in the detection of elder abuse cases.
In reviewing the research base associated with the relationship between reporting systems and the treatment and prevention of family violence, the committee has observed that no existing evaluation studies can demonstrate the value of mandatory reporting systems compared with voluntary reporting procedures in addressing child maltreatment or domestic violence. For elder abuse, studies suggest that a high level of public and professional awareness and the availability of comprehensive services to identify, treat, and prevent violence is preferable to reporting requirements in improving rates of case detection.
The absence of a research base to support mandatory reporting systems raises questions as to whether they should be recommended for all areas of family violence. The impact of mandatory reporting systems in the area of child maltreatment and elder abuse remains unexamined. The committee therefore suggests that it is important for the states to proceed cautiously at this time and to delay adopting a mandatory reporting system in the area of domestic violence, until the positive and negative impacts of such a system have been rigorously examined in states in which domestic violence reports are now required by law.
Recommendation 1: The committee recommends that states initiate evaluations of their current reporting laws addressing family violence to examine whether and how early case detection leads to improved outcomes for the victims or families and promote changes based on sound research. In
particular, the committee recommends that states refrain from enacting mandatory reporting laws for domestic violence until such systems have been tested and evaluated by research.
In dealing with family violence that involves adults, federal and state government agencies should reconsider the nature and role of compulsory reporting policies. In the committee's view, mandatory reporting systems have some disadvantages in cases involving domestic violence, especially if the victim objects to such reports, if comprehensive community protections and services are not available, and if the victim is able to gain access to therapeutic treatment or support services in the absence of a reporting system.
The dependent status of young children and some elders provides a stronger argument in favor of retaining mandatory reporting requirements where they do exist. However, the effectiveness of reporting requirements depends on the availability of resources and service personnel who can investigate reports and refer cases for appropriate treatment, as well as clear guidelines for processing reports and determining which cases qualify for services. Greater discretion may be advised when the child and family are able to receive therapeutic treatment from health care or other service providers and when community resources are not available to respond appropriately to their cases. The treatment of adolescents especially requires major consideration of the pros and cons of mandatory reporting requirements. Adolescent victims are still in a vulnerable stage of development: they may or may not have the capacity to make informed decisions regarding the extent to which they wish to invoke legal protections in dealing with incidents of family violence in their homes.
Batterer Treatment Programs
Four key questions characterize current policy and research discussions about the efficacy of batterer treatment, one of the most challenging problems in the design of family violence interventions: Is treatment preferable to incarceration, supervised probation, or other forms of court oversight for batterers? Does participation in treatment change offenders' attitudes and behavior and reduce recidivism? Does the effectiveness of treatment depend on its intensity, duration, or the voluntary or compulsory nature of the program? Is treatment what creates change, or is change in behavior reduced by multiple interventions, such as arrest, court monitoring of client participation in treatment services, and victim support services?
Descriptive research studies suggest that there are multiple profiles of batterers, and therefore one generic approach is not appropriate for all offenders. Treatment programs may be helpful in changing abusive behavior when they are part of an overall strategy designed to recognize and reduce violence in a relationship, when the batterer is prepared to learn how to control aggressive impulses, and
when the treatment plan emphasizes victim safety and provides for frequent interactions with treatment staff.
Research on the effectiveness of treatment programs suggests that the majority of subjects who complete court-ordered treatment programs do learn basic cognitive and behavioral principles taught in their course. However, such learning requires appropriate program content and client participation in the program for a sufficient time to complete the necessary training. Very few studies have examined matched groups of violent offenders who are assigned to treatment and control groups or comparison groups (such as incarceration or work-release). As a result, the comparative efficacy of treatment is unknown in reducing future violence. Differing client populations and differing forms of court oversight are particularly problematic factors that inhibit the design of rigorous evaluation studies in this field.
The absence of strong theory and common measures to guide the development of family violence treatment regimens, the heterogeneity of offenders (including patterns of offending and readiness to change) who are the subjects of protective orders or treatment, and low rates of attendance, completion, and enforcement are persistent problems that affect both the evaluation of the interventions and efforts to reduce the violence. A few studies suggest that court oversight does appear to increase completion rates, which have been linked to enhanced victim safety in the area of domestic violence, but increased completion rates have not yet led to a discernible effect on recidivism rates in general.
Further evaluations are needed to examine the outcomes associated with different approaches and programmatic themes (such as cognitive-behavioral principles: issues of power, control, and gender; personal accountability). Completion rates have been used as an interim outcome to measure the success of batterer treatment programs; further studies are needed to determine if completers can be identified readily, if program completion by itself is a critical factor in reducing recidivism, and if participation in a treatment program changes the nature, timing, and severity of future violent behavior.
The current research base is inadequate to identify the conditions under which mandated referrals to batterer treatment programs offer a clear advantage over incarceration or untreated probation supervision in reducing recidivism for the general population of male offenders. Court officials should monitor closely the attendance, participation, and completion rates of offenders who are referred to batterer treatment programs in lieu of more punitive sentences. Treatment staff should inform law enforcement officials of any significant behavior by the offender that might represent a threat to the victim. Mandated treatment referrals may be effective for certain types of batterers, especially if they increase completion rates. The research is inconclusive, however, as to which types of individuals should be referred for treatment rather than more punitive sanctions. In selecting individuals for treatment, attention should be given to client history
(first-time offenders are more likely to benefit), motivation for treatment, and likelihood of completion.
Mandated treatment referrals for batterers do appear to provide benefits to victims, such as intensive surveillance of offenders, an interlude to allow planning for safety and victim support, and greater community awareness of the batterer's behavior. These outcomes may interact to deter and reduce domestic violence in the community, even if a treatment program does not alter the behavior of a particular batterer. Treatment programs that include frequent interactions between staff and victims also provide a means by which staff can help educate victims about danger signals and support them in efforts to obtain greater protection and legal safeguards, if necessary.
Recommendation 2: In the absence of research that demonstrates that a specific model of treatment can reduce violent behavior for many domestic violence offenders, courts need to put in place early warning systems to detect failure to comply with or complete treatment and signs of new abuse or retaliation against victims, as well as to address unintended or inadvertent results that may arise from the referral to or experience with treatment.
Further research evaluation studies are needed to review the outcomes for both offenders and victims associated with program content and levels of intensity in different treatment models. This research will help indicate whether treatment really helps and what mix of services are more helpful than others. Improved research may also help distinguish those victims and offenders for whom particular treatments are most beneficial.
Record Keeping
Since experience with family violence appears to be associated with a wide range of health problems and social service needs, service providers are recognizing the importance of documenting abuse histories in their client case records. The documentation in health and social service records of abuse histories that are self-reported by victims and offenders can help service providers and researchers to determine if appropriate referrals and services have been made and the outcomes associated with their use. The exchange of case records among service providers is essential to the development of comprehensive treatment programs, continuity of care, and appropriate follow-up for individuals and families who appear in a variety of service settings. Such exchanges can help establish greater accountability by service systems for responding to the needs of identifiable victims and offenders; health and social service records can also provide appropriate evidence for legal actions, in both civil and criminal courts and child custody cases.
Research evaluations of service interventions often require the use of anonymous case records. The documentation of family violence in such records will
enhance efforts to improve the quality of evaluations and to understand more about patterns of behavior associated with violent behaviors and victimization experiences. Although documentation of abuse histories can improve evaluations and lead to integrated service responses, such procedures require safeguards so that individuals are not stigmatized or denied therapeutic services on the basis of their case histories. Insurance discrimination, in particular, which may preclude health care coverage if abuse is judged to be a preexisting condition, requires attention to ensure that professional services are not diminished as a result of voluntary disclosures. Creative strategies are needed to support integrated service system reviews of medical, legal, and social service case records in order to enhance the quality and accountability of service responses. Such reviews will need to meet the expectations of privacy and confidentiality of both individual victims and the community, especially in cases in which maltreatment reports are subsequently regarded as unfounded.
Documentation of abuse histories that are voluntarily disclosed by victims or offenders to health care professionals and social service providers must be distinguished from screening efforts designed to trigger such disclosures. The committee recommends screening as a strong candidate for future evaluation studies (see discussion in the next section).
Recommendation 3: The committee recommends that health and social service providers develop safeguards to strengthen their documentation of abuse and histories of family violence in both individual and group records, regardless of whether the abuse is reported to authorities.
The documentation of histories of family violence in health records should be designed to record voluntary disclosures by both victims and offenders and to enhance early and coordinated interventions that can provide a therapeutic response to experiences with abuse or neglect. Safeguards are required, however, to ensure that such documentation does not lead to stigmatization, encourage discriminatory practices, or violate assurances of privacy and confidentiality, especially when individual histories become part of patient group records for health care providers and employers.
Collaborative Law Enforcement Strategies
In the committee's view, collaborative law enforcement strategies that create a web of social control for offenders are an idea worth testing to determine if such efforts can achieve a significant deterrent effect in addressing domestic violence. Collaborative strategies include such efforts as victim support and offender tracking systems designed to increase the likelihood that domestic violence cases will be prosecuted when an arrest has been made, that sanctions and treatment services will be imposed when evidence exists to confirm the charges brought against the offender, and that penalties will be invoked for failure to comply with treatment
conditions. The attraction of collaborative strategies is based on their potential ability to establish multiple interactions with offenders across a large domain of interactions that reinforce social standards in the community and establish penalties for violations of those standards. Creating the deterrent effect, however, requires extensive coordination and reciprocity between victim support and offender monitoring efforts involving diverse sectors of the law enforcement community. These efforts may be difficult to implement and evaluate. Further studies are needed to determine the extent to which improved collaboration among police officers, prosecutors, and judges will lead to improved coordination and stronger sanctions for offenders and a reduction in domestic violence.
The absence of empirical research findings of the results of a collaborative law enforcement approach in addressing domestic violence makes it difficult to compare the costs and benefits of increased agency coordination with those achieved by a single law enforcement strategy (such as arrest) in dealing with different populations of offenders and victims. Even though relatively few cases of arrest are made for any form of family violence, arrest is the most common and most studied form of law enforcement intervention in this area. Research studies conducted in the 1980s on arrest policies in domestic violence cases are the strongest experimental evaluations to date of the role of deterrence in family violence interventions. These experiments indicate that arrest may be effective for some, but not most, batterers in reducing subsequent violence by the offender. Some research studies suggest that arrest may be a deterrent for employed and married individuals (those who have a stake in social conformity) and may lead to an escalation of violence among those who do not, but this observation has not been tested in studies that could specifically examine the impact of arrest in groups that differ in social and economic status. The differing effects (in terms of a reduction of future violence) of arrest for employed/unemployed and married/unmarried individuals raise difficult questions about the reliance of law enforcement officers on arrest as the sole or central component of their response to domestic violence incidents in communities where domestic violence cases are not routinely prosecuted, where sanctions are not imposed by the courts, or where victim support programs are not readily available.
The implementation of proarrest policies and practices that would discriminate according to the risk status of specific groups is challenged by requirements for equal protection under the law. Law enforcement officials cannot tailor arrest policies to the marital or employment status of the suspect or other characteristics that may interact with deterrence efforts. Specialized training efforts may help alleviate the tendency of police officers to arrest both suspect and victim, however, and may alert law enforcement personnel to the need to review both criminal and civil records in determining whether an arrest is advisable in response to a domestic violence case.
Two additional observations merit consideration in examining the deterrent effects of arrest. First, in the research studies conducted thus far, the implementation
of legal sanctions was minimal. Most offenders in the replication studies were not prosecuted once arrested, and limited legal sanctions were imposed on those cases that did receive a hearing. Some researchers concluded that stronger evidence of effectiveness might be obtained from proarrest policies if they are implemented as part of a law enforcement strategy that expands the use of punitive sanctions for offenders—including conviction, sentencing, and intensive supervised probation.
Second is the issue of reciprocity between formal sanctions against the offender and informal support actions for the victims of domestic violence. The effects of proarrest policies may depend on the extent to which victims have access to shelter services and other forms of support, demonstrating the interactive dimensions of community interventions. A mandatory arrest policy, by itself, may be an insufficient deterrent strategy for domestic violence, but its effectiveness may be enhanced by other interventions that represent coordinated law enforcement efforts to deter domestic violence—including the use of protective orders, victim advocates, and special prosecution units. Coordinated efforts may help reduce or prevent domestic violence if they represent a collaborative strategy among police, prosecutors, and judges that improves the certainty of the use of sanctions against batterers.
Recommendation 4: Collaborative strategies among caseworkers, police, prosecutors, and judges are recommended as law enforcement interventions that have the potential to improve the batterer's compliance with treatment as well as the certainty of the use of sanctions in addressing domestic violence.
The impact of single interventions (such as mandatory arrest policies) is difficult to discern in the research literature. Such practices by themselves can neither be recommended nor rejected as effective measures in addressing domestic violence on the basis of existing research studies.
Home Visitation and Family Support Services
Home visitation and family support programs constitute one of the most promising areas of child maltreatment prevention. Studies in this area have experimented with different levels of treatment intensity, duration, and staff expertise. For home visitation, the findings generally support the principle that early intervention with mothers who are at risk of child maltreatment makes a difference in child outcomes. Such interventions may be difficult to implement and maintain over time, however, and their effectiveness depends on the willingness of the parents to participate. Selection criteria for home visitation should be based on a combination of social setting and individual risk factors.
In their current form, home visitation programs have multiple goals, only one of which is the prevention of child abuse and neglect. Home visitation and family
support programs have traditionally been designed to improve parent-child relations with regard to family functioning, child health and safety, nutrition and hygiene, and parenting practices. American home visiting programs are derived from the British system, which relies on public health nurses and is offered on a universal basis to all parents with young children. Resource constraints, however, have produced a broad array of variations in this model; most programs in the United States are now directed toward at-risk families who have been reported to social services or health agencies because of prenatal health risks or risks for child maltreatment. Comprehensive programs provide a variety of services, including in-home parent education and prenatal and early infant health care, screening, referral to and, in some cases, transportation to social and health services. Positive effects include improved childrearing practices, increased social supports, utilization of community services, higher birthweights, and longer gestation periods.
Researchers have identified improvements in cognitive and parenting skills and knowledge as evidence of reduced risk for child maltreatment; they have also documented lower rates of reported child maltreatment and number of visits to emergency services for home-visited families. The benefits of home visitation appear most promising for young, first-time mothers who delay additional pregnancies and thus reduce the social and financial stresses that burden households with large numbers of young children. Other benefits include improved child care for infants and toddlers and an increase in knowledge about the availability of community services for older children. The intervention has not been demonstrated to have benefits for children whose parents abuse drugs or alcohol or those who are not prepared to engage in help-seeking behaviors. The extent to which home visitation benefits families with older children, or families who are already involved in abusive or neglectful behaviors, remains uncertain.
Recommendation 5: As part of a comprehensive prevention strategy for child maltreatment, the committee recommends that home visitation programs should be particularly encouraged for first-time parents living in social settings with high rates of child maltreatment reports.
The positive impact of well-designed home visitation interventions has been demonstrated in several evaluation studies that focus on the role of mothers in child health, development, and discipline. The committee recommends their use in a strategy designed to prevent child maltreatment. Home visitation programs do require additional evaluation research, however, to determine the factors that may influence their effectiveness. Such factors include (1) the conditions under which home visitation should be provided as part of a continuum of family support programs, (2) the types of parenting behaviors that are most and least amenable to change as a result of home visitation, (3) the duration and intensity of services (including amounts and types of training for home visitors) that are necessary to achieve positive outcomes for high-risk families, (4) the experience
of fathers in general and of families in diverse ethnic communities in particular with home visitation interventions, and (5) the need for follow-up services once the period of home visitation has ended.
Intensive Family Preservation Services
Intensive family preservation services represent crisis-oriented, short-term, intensive case management and family support programs that have been introduced in various communities to improve family functioning and to prevent the removal of children from the home. The overall goal of the intervention is to provide flexible forms of family support to assist with the resolution of circumstances that stimulated the child placement proposal, thus keeping the family intact and reducing foster care placements.
Eight of ten evaluation studies of selected intensive family preservation service programs (including five randomized trials and five quasi-experimental studies) suggest that, although these services may delay child placement for families in the short term, they do not show an ability to resolve the underlying family dysfunction that precipitated the crisis or to improve child well-being or family functioning in most families. However, the evaluations have shortcomings, such as poorly defined assessment of child placement risk, inadequate descriptions of the interventions provided, and nonblinded determination of the assignment of clients to treatment and control groups.
Intensive family preservation services may provide important benefits to the child, family, and community in the form of emergency assistance, improved family functioning, better housing and environmental conditions, and increased collaboration among discrete service systems. Intensive family preservation services may also result in child endangerment, however, when a child remains in a family environment that threatens the health or physical safety of the child or other family members.
Recommendation 6: Intensive family preservation services represent an important part of the continuum of family support services, but they should not be required in every situation in which a child is recommended for out-of-home placement.
Measures of health, safety, and well-being should be included in evaluations of intensive family preservation services to determine their impact on children's outcomes as well as placement rates and levels of family functioning, including evidence of recurrence of abuse of the child or other family members. There is a need for enhanced screening instruments that can identify the families who are most likely to benefit from intensive short-term services focused on the resolution of crises that affect family stability and functioning.
The value of appropriate post-reunification (or placement) services to the child and family to enhance coping and the ability to make a successful transition
toward long-term adjustment also remains uncertain. The impact of post-reunification or post-placement services needs to be considered in terms of their relative effects on child and family functioning compared with the use of intensive family preservation services prior to child removal. In some situations, one or the other type of services might be recommended; in other cases, they might be used in some combination to achieve positive outcomes.
Recommendations For The Next Generation Of Evaluations
Determining which interventions should be selected for rigorous and in-depth evaluations in the future will acquire increased importance as the array of family violence interventions expands in social services, law, and health care settings. For this reason, clear criteria and guiding principles are necessary to guide sponsoring agencies in their efforts to determine which types of interventions are suitable for evaluation research. Recognizing that all promising interventions cannot be evaluated, public and private agencies need to consider how to invest research resources in areas that show programmatic potential as well as an adequate research foundation. Future allocations of research investments may require agencies to reorganize or to develop new programmatic and research units that can inform the process of selecting interventions for future evaluation efforts, determine the scope of adequate funding levels, and identify areas in which program integration or diversity may contribute to a knowledge base that can inform policy, practice, and research. Such agencies may also consider how to sustain an ongoing dialogue among research sponsors, research scientists, and service providers to inform these selection efforts and to disseminate evaluation results once they are available.
In the interim, the committee offers several guiding principles to help inform the evaluation selection process.
- meet the preconditions for experimentation that are described in the other principles outlined below.
With these principles in mind, the committee has identified a set of interventions that are the focus of current policy attention and service innovation efforts but have not received significant attention from research. In the committee's judgment, each of these nine interventions has reached a level of maturation and preliminary description in the research literature to justify their selection as strong candidates for future evaluation studies.
Training for Service Providers and Law Enforcement Officials
Training in basic educational programs and continuing education on all aspects
of family violence has expanded for professionals in the health care, legal, and social service systems. Such efforts can be expected to enhance skills in identifying individual experiences with family violence, but improvements in training may improve other outcomes as well, including the patterns and timing of service interventions, the nature of interactions with victims of family violence, linkage of service referrals, the quality of investigation and documentation for reported cases, and, ultimately, improved health and safety outcomes for victims and communities.
Training programs alone may be insufficient to change professional behavior and service interventions unless they are accompanied by financial and human resources that emphasize the role of psychosocial issues and support the delivery of appropriate treatment, prevention, and referral services in different institutional and community settings. Evaluations of their effectiveness therefore need to consider the institutional culture and resource base that influence the implementation of the training program and the abilities of service providers to apply their knowledge and skills in meeting the needs of their clients.
Evaluation research is needed to assess the impact of training programs on counseling and referral practices and service delivery in health care, social service, and law enforcement settings. This research should include examination of the effects of training on the health and mental health status of those who receive services, including short- and long-term outcomes such as empowerment, freedom from violence, recovery from trauma, and rebuilding of life. Evaluations should also examine the role of training programs as catalysts for innovative and collaborative services. They should consider the extent to which training programs influence the behavior of agency personnel, including the interaction of service providers with professionals from other institutional settings, their participation in comprehensive community service programs, and the exposure of personal experiences in institutions charged with providing interventions for abuse.
Universal Screening in Health Care Settings
The significant role of health care and social service professionals in screening for victimization by all forms of family violence deserves critical analysis and rigorous evaluation. Early detection of child maltreatment, spousal violence, and elder abuse is believed to lead to an infusion of treatment and preventive services that can reduce exposure to harm, mitigate the negative consequences of abuse and neglect, improve health outcomes, and reduce the need for future health services. Screening programs can also enhance primary prevention efforts by providing information, education, and awareness of resources in the community. The benefits associated with early detection need to be balanced against risks presented by false positives and false negatives associated with large-scale screening efforts and programs characterized by inadequate staff training and responses.
Such efforts also need to consider whether appropriate treatment, protection, and support services are available for victims or offenders once they have been detected.
The use of enhanced screening instruments also requires attention to the need for services that can respond effectively to the large caseloads generated by expanded detection activities. The child protective services literature suggests that increased reporting can diminish the capacity of agencies to respond effectively if additional resources are not available to support enhanced services as well as screening.
The use of screening instruments in health care and social service settings for batterer identification and treatment is more problematic, given the lack of knowledge about factors that enhance or discourage their violent behavior. Screening only victims may be insufficient to provide a full picture of family violence; however, screening batterers may increase the danger for their victims, especially if batterer treatment interventions are not available or are not reliable in providing effective treatment and if support services are not available for victims once a perpetrator is identified. Screening adults for histories of childhood abuse, which may help prevent future victimization of the patient or others, may also be problematic without adequate training or mental health services to deal with the possible resurgence of trauma.
Evaluation studies of family violence screening efforts could build on the lessons derived from screening research in other health care areas (such as HIV detection, lead exposure, sickle cell, and others). This research could provide data that would support or contradict the theory that early identification is a useful secondary prevention intervention, especially in areas in which appropriate services may not be available or reliable. The cost issues associated with universal screening need to be considered in terms of their implications for savings in possible cost reductions from consequent conditions (such as the health consequences of HIV infection, sexually transmitted diseases, unplanned pregnancy, substance abuse, post-traumatic stress disorder, depression, and the exacerbation of other medical conditions) that may occur in other health care areas. Finally, the risks associated with screening (such as the establishment of a preexisting condition that may influence insurance eligibility) require consideration; such issues are already being addressed by some advocacy groups, insurance corporations, and regulatory bodies in the health care area.
Mental Health and Counseling Services
Little is known at present regarding the comparative effectiveness of different forms of therapeutic services for victims of family violence. Findings from recent studies of child physical and sexual abuse suggest that certain approaches (specifically cognitive-behavioral programs) are associated with more positive outcomes for parents, such as reducing aggressive/coercive behavior, compared
with family therapy and routine community mental health services. No treatment outcome studies have been conducted in the area of child neglect. Interventions in this field generally draw on approaches for dealing with other childhood and adolescent problems with similar symptom profiles.
For domestic violence, research evaluations are in the early stages of design and empirical data are not yet available to guide analyses of the effectiveness of different approaches. Major challenges include the absence of agreement regarding key psychosocial outcomes of interest in assessing the effectiveness of interventions, variations in the use of treatment protocols designed for post-traumatic stress for individuals who may still be experiencing traumatic situations, tensions between protocol-driven models of treatment (which are easier to evaluate) and those that are driven by the needs of the client or the context in which the violence occurred, the co-occurrence of trauma and other problems (such as prior victimization, depression, substance abuse, and anxiety disorders) that may have preceded the violence but require mental health services, and the difficulty of involving victims in follow-up studies after the completion of treatment. Variations in the context in which mental health services are provided for victims of domestic violence (such as isolated services, managed care programs, and services that are incorporated into an array of social support programs, including housing and job counseling) also require attention. Topics of special interest include contextual issues, such as the general lack of access to quality mental health services for women without sufficient independent income, and the danger of psychiatric diagnoses being used against battered women in child custody cases.
Collaborative efforts are needed to provide opportunities for the exchange of methodology, research measures, and designs to foster the development of controlled studies that can compare the results of innovative treatment approaches with routine counseling programs in community services.
Comprehensive Community Initiatives
Evaluations of batterer treatment programs, protective orders, and arrest policies suggest that the role of these individual interventions may be enhanced if they are part of a broad-based strategy to address family violence. The development of comprehensive, community-based interventions has become extremely widespread in the 1990s; examples include domestic violence coordinating councils, child advocacy centers, and elder abuse task forces. A few communities (most notably Duluth, Minnesota, and Quincy, Massachusetts) have developed systemwide strategies to coordinate their law enforcement and other service responses to domestic violence.
Comprehensive community-based interventions must confront difficult challenges, both in the design and implementation of such services, and in the selection of appropriate measures to assess their effectiveness. Many evaluations of comprehensive community-based interventions have focused primarily on the
design and implementation process, to determine whether an individual program had incorporated sufficient range and diversity among formal and informal networks so that it can achieve a significant impact in the community. This type of process evaluation does not necessarily require new methods of assessment or analysis, although it can benefit from recent developments in the evaluation literature, such as the empowerment evaluations discussed in Chapter 3 .
In contrast, the evaluation challenges that emerge from large-scale community-based efforts are formidable. First, it may be difficult to determine when an intervention has reached an appropriate stage of implementation to warrant a rigorous assessment of its effects. Second, the implementation of a community-wide intervention may be accompanied by a widespread social movement against family violence, so that it becomes difficult to distinguish the effects of the intervention itself from the impact of changing cultural and social norms that influence behavior. In some cases, the effects attributed to the intervention may appear weak, because they are overwhelmed by the impact of the social movement itself. Third, the selection of an appropriate comparison or control group for community-wide interventions presents formidable problems in terms of matching social and structural characteristics and compensating for community-to-community variation in record keeping.
These challenges require close attention to the emerging knowledge associated with the evaluation of comprehensive community-wide interventions in areas unrelated to family violence, so that important design, theory, and measurement insights can be applied to the special needs of programs focused on child maltreatment, domestic violence, and elder abuse. Although no single model of service integration, comprehensive services, or community change can be endorsed at this time, a range of interesting community service designs has emerged that have achieved widespread popularity and support at the local level. Because their primary focus is often on prevention, rather than treatment, comprehensive community interventions have the potential to achieve change across multiple levels of interactions affecting individuals, families, communities, and social norms and thus reduce the scope and severity of family violence as well as contribute to remedies to other important social problems.
A growing research literature has appeared in other fields, particularly in the area of substance abuse and community development, that identifies the conceptual frameworks, data collection, and methodological issues that need to be considered in designing evaluation studies for community-based and systemwide interventions. As an example, the Center for Substance Abuse Prevention in the federal Substance Abuse and Mental Health Services Administration has funded a series of studies designed to improve methodologies for the evaluation of community-based substance abuse prevention programs that offer important building blocks for the field of family violence interventions.
Developing effective evaluation strategies for comprehensive and systemwide programs is one of the most challenging issues for the research community
in this field. No evaluations have been conducted to date to examine the relative advantages of comprehensive and systemwide community initiatives compared with traditional services. Evaluations need to consider the mix of components in comprehensive interventions that determine their effectiveness and successful implementation; the comparative strengths and limitations of inter- and intra-agency interventions; community factors, such as political leadership, historical tensions, diversity of ethnic/cultural composition, and resource allocation strategies; and the impact of comprehensive interventions on the capacity of service agencies to provide traditional care and effective responses to reports of family violence.
Shelter Programs and Other Domestic Violence Services
Over time, most battered women's shelters have expanded their services to encompass far more than the provision of refuge. Today, many shelters have support groups for women residents, support groups for child residents, emergency and transitional housing, and legal and welfare advocacy. Nonresidential services also have expanded, so that any battered woman in the community is able to attend a support group or request advocacy services. Many agencies now offer educational groups for men who batter, as well as programs dealing with dating violence. Some communities have never opened a shelter yet are able to offer support groups, advocacy, crisis intervention, and safe homes (neighbors sheltering a neighbor, for example) to help battered women and their families in times of crisis. In addition to providing services for victims, the battered women service organizations also define their goal as transforming the conditions and norms that support violence against women. Thus these organizations work as agents of social change in their communities to improve the community-wide response to battered women and their children.
Shelter services and battered women's support organizations are ready for evaluations that can identify program outcomes and compare the effectiveness of different service interventions. Research studies are also needed that can describe the multiple goals and theories that shape the program objectives of these interventions, provide detailed histories of the ways in which different service systems have been implemented, and examine the characteristics of the women who do or do not use or benefit from them.
Protective Orders
Protective orders can be an important part of the prevention strategy for domestic violence and help document the record of assaults and threatening actions. The low priority traditionally assigned to the handling of protective orders, which are usually treated as civil matters in police agencies, requires attention, as do the procedural requirements of the legal system. Courts have
accepted alternative forms of due process, including public notice, notice by mail, and other forms of notification that do not require personal contact. Efforts are needed now to compare the effectiveness of short-term (30-day) restraining orders with a longer (1-year) protective order in reducing violent behavior by offenders and securing access to legal and support services for the complainants.
In-depth case studies and interviews with victims who have had police and court contacts because of domestic violence are needed to highlight individual, social, and institutional factors that facilitate or inhibit victim use of and perpetrator compliance with protective orders in different community settings. Such studies could (1) reveal patterns of help-seeking contacts and services that affect the use of protective orders and compliance with their requirements, (2) highlight the forms of sanctions that are appropriate to ensure compliance and to deter future violent behavior, (3) explore the extent to which the effects of protective orders are enhanced in reducing violence if victim advocates, shelter services, or other social support resources are available and are used by the victim in redefining the terms of her relationship with her partner, and (4) examine the extent to which protective orders can mitigate the consequences of violence for children who may have been assaulted or who may have witnessed an assault against their mother.
Child Fatality Review Panels
The emergence of child fatality review teams in 21 states since 1978 represents an innovative effort in many communities to address systemwide implications of severe violence against children and infants. Child fatality review teams involve a multiagency effort to compile and integrate information about child deaths and to review and evaluate the record of caseworkers and agencies in providing services to these children when a report of abuse or neglect had been made prior to a child's death. These review teams can provide an opportunity to examine the quality of a community's total approach to child abuse and neglect prevention and treatment.
The experience of child fatality review teams in identifying systemic features that enhance or weaken agency efforts to protect children needs to be evaluated and made accessible to individual service providers in health, legal, and social service agencies. Key research issues include: the effect of review team actions on the protection of family members of children who have died as a result of child maltreatment; the impact of child fatality review reports on the prosecution of offenders; the influence of review team efforts on the routine investigation, treatment, and prevention activities of participating agencies; the impact of review teams on other community child protection and domestic violence prevention efforts; and the identification of early warning signals that emerge in child homicide investigations that represent opportunities for preventive interventions.
Child Witness to Violence Programs
Child witness programs represent an important development in the evolution of comprehensive approaches to family violence, but they have not yet been evaluated. Evaluation studies of these programs should examine the experience with symptomatology among children who witness family violence, to determine whether and for whom early intervention influences the course of development of social and mental health consequences, such as depression, anxiety, emotional detachment, aggression and violence, and post-traumatic stress symptoms. Such studies could also compare variations in the developmental histories of children who witness violence with those of children who are injured or otherwise are directly victimized by their parents or who witness violence in their communities. Evaluation studies should consider the recommended forms of treatment for these children, the standards of eligibility that determine their placement in treatment programs, and the impact of institutional setting (hospital, shelter, or social service agency) and reimbursement plans on the quality of the treatment.
Elder Abuse Services
Only seven program evaluation studies have been published on elder abuse interventions, none of which includes random groups and most of which involve small sample sizes. Three major issues challenge effective interventions in this area: the degree of dependence between perpetrators and victims, restricted social services budgets, general public distrust of social welfare programs, and the relationship between judgments about competence and the application of the principles of self-determination and privacy to the problem of elder abuse.
Evaluation studies should consider the different types and multiple dimensions of elder abuse in the development of effective interventions. The benefits of specific programs need to be compared with integrated service systems that are designed to foster the well-being of the elderly population without regard to special circumstances. Evaluation research should be integrated into community service programs and agency efforts on behalf of elderly persons to foster studies that involve the use of comparison and control groups, common measures, and the assessment of outcomes associated with different forms of service interventions.
Topics For Basic Research
The committee identified four basic research topics that require further development to inform policy and practice. These topics raise fundamental questions about the approaches that should be used in designing treatment, prevention, and enforcement strategies. As such, they highlight important dimensions of family violence that should be addressed in a research agenda for the field.
birth, infancy, and adolescence. Other issues linked to family formation include the use of corporal punishment in child discipline, gender roles, privacy, and strategies for resolving conflict among adults or siblings.
A third approach would be studies to discern the protective factors inside and outside families that enable some children who are exposed to violence to not only survive but also to develop coping mechanisms that serve them well later in life. This analysis would have widespread implications for assessing the impact of biological and experiential factors in specific domains, such as fear, anxiety, self-blame, identity formation, helplessness, and help-seeking behaviors. Such research could also identify abuse-related coping strategies (such as excessive distrust of or overdependence on others) that may contribute to other problems that emerge in the course of adolescent and adult development.
first-time parents, victims and offenders who have substance abuse histories, etc.)
Forging Partnerships Between Research And Practice
Although it is premature to expect research to offer definitive answers about the relative effectiveness of the array of current service and enforcement strategies, the committee sees valuable opportunities that now exist to accelerate the rate by which service providers can identify the types of individuals, families, and communities that may benefit from certain types or combinations of service and enforcement interventions. Major challenges must be addressed, however, to improve the overall quality of the evaluations of family violence interventions and to provide a research base that can inform policy and practice. These challenges include issues of study design and methodology as well as logistical concerns that must be resolved in order to conduct research in open service systems where the research investigator is not able to control factors that may weaken the study design and influence its outcome. The resolution of these challenges will require collaborative partnerships between researchers, service providers, and policy makers to generate common approaches and data sources.
The integration of research and practice in the field of family violence, as in many other areas of human services, has occurred on a haphazard basis. As a result, program sponsors, service providers, clients, victims, researchers, and community representatives have not been able to learn in a systematic manner from the diverse experiences of both large and small programs. Mayors, judges, police officers, caseworkers, child and victim advocates, health professionals, and others must make life-or-death decisions each day in the face of tremendous
uncertainty, often relying on conflicting reports, anecdotal data, and inconsistent information in judging the effectiveness of specific interventions.
The development of creative partnerships between the research and practice communities would greatly improve the targeting of limited resources to specific clients who can benefit most from a particular type of intervention. Yet significant barriers inhibit the development of such partnerships, including disagreements about the nature and origins of family violence, broad variations in the conceptual frameworks that guide service delivery, differences over the relative merits of service and research, a lack of faith in the ability of research to inform and improve services, a lack of trust in the ability of service providers to inform the design of research experiments and the formation of theoretical frameworks, and concerns about fairness and safety in including victims and offenders in experimental treatment groups. These fundamental differences obscure identification of outcomes of interest in the development of evaluation studies, which are further complicated by limitations in study design and access to appropriate subjects that are necessary for the conduct of research.
Even if greater levels of trust fostered more interaction between the research community and service providers, collaborative efforts would be challenged by factors such as the lack of funding for empirical studies, the availability of limited resources to support studies over appropriate time frames, and the social and economic characteristics of some of the populations served by family violence interventions that make them difficult to follow over extended periods of time (chaotic households, high mobility of the client population, concerns for safety, lack of telephones and permanent residences, etc.).
Service providers and program sponsors have often been skeptical of efforts to evaluate the impact of a selected intervention, knowing that critical or premature assessments could jeopardize the program's future and restrict future opportunities for service delivery. Service providers have also been less than enthusiastic in seeking program evaluations, knowing that the programs to be evaluated have been underfunded and are understaffed and present a less than ideal situation; in their view, the assessment may diminish future resources and affect the development of a particular strategy or programmatic approach. The tremendous demand for services and the limited availability of staff resources create a pressured environment in which the staff time involved in filling out forms for research purposes is seen as being sacrificed from time that might be used to serve people in need. In some cases, research funds support demonstration programs that are highly valued by a community, yet few resources are available to support them once the research phase has been completed.
Researchers and service providers need to resolve the programmatic tensions that have sometimes surfaced in contentious debates over the type of services that should be put into place in addressing problems of family violence. The mistrust and skepticism present major challenges that need to resolved before the technical challenges to effective evaluations can be addressed. A reformulation of the
research process is needed so that, while building a long-term capacity to focus on complex issues and conduct rigorous studies, researchers can also provide useful information to service providers.
The committee has identified three major principles to help integrate research and practice in the field of family violence interventions:
- Evaluation should be an integral part of any major intervention, particularly those that are designed to be replicated in multiple communities. Interventions have often been put into place without a research base to support them or rigorous evaluation efforts to guide their development. Evaluation research based on theoretical models is needed to link program goals and operational objectives with multiple program components and outcomes. Intensive marketing and praise for a particular intervention or program should no longer be a substitute for empirical data in determining the effectiveness of programs that are intended to be replicated in multiple sites.
- Coordinating policy, program, and research agendas will improve family violence interventions. Evaluation research will help program sponsors and managers clarify program goals and experience and identify areas in need of attention because of the difficulties of implementation, the use of resources, and changes in the client base. Research and data-based analysis can guide ongoing program and policy efforts if evaluation studies are integrated into the design and development of interventions. The knowledge base can be improved by (1) framing key hypotheses that can be tested by existing or new services, (2) building statistical models to explore the system-wide effects of selected interventions and compare these effects with the consequences of collaborative and comprehensive approaches, (3) using common definitions and measures to facilitate comparisons across individual studies, (4) using appropriate comparison and control groups in evaluation studies, including random assignment, when possible, (5) developing culturally sensitive research designs and measures, (6) identifying relevant outcomes in the assessment of selected interventions, and (7) developing alternative designs when traditional design methodology cannot be used for legal, ethical, or practical reasons.
- Surmounting existing barriers to collaboration between research and practice communities requires policy incentives and leadership to foster partnership efforts. Many interventions are not evaluated because of limited funds, because the individuals involved in service delivery consider research to be peripheral to the needs of their clients, because the researchers are disinterested in studying the complexity of service delivery systems and the impact of violence in clients' lives, or because research methods are not yet available to assess outcomes that result from the complex interaction of multiple systems. This situation will continue until program sponsors and policy officials exercise leadership to build partnerships between the research and practice communities and to provide funds for rigorous evaluations in the development of service and law enforcement
- interventions. Additional steps are required to foster a more constructive dialogue and partnership between the research and practice communities.
Partnership efforts are also needed to focus research attention on the particular implementation of an individual program rather than the strategy behind the program design. Promising intervention strategies may be discarded prematurely because of special circumstances that obstructed full implementation of the program. Conversely, programs that offer only limited effectiveness may appear to be successful on the basis of evaluation studies that did not consider the significant points of vulnerability and limitations in the service design or offer a comparative analysis with the benefits to be derived from routine services.
The establishment and documentation of a series of consensus conferences on relevant outcomes, and appropriate measurement tools, will strengthen and enhance evaluations of family violence interventions and lead to improvements in the design of programs, interventions, and strategies. May opportunities currently exist for research to inform the design and assessment of treatment and prevention interventions. In addition, service providers can help guide researchers in the identification of appropriate domains in which program effects may occur but are currently not being examined. Ongoing dialogues can guide the identification and development of instruments and methods that can capture the density and distribution of relevant effects that are not well understood. The organization of a series of consensus conferences by sponsors in public and private agencies that are concerned with the future quality of family violence interventions would be an important contribution to the development of this field.
Reports of mistreated children, domestic violence, and abuse of elderly persons continue to strain the capacity of police, courts, social services agencies, and medical centers. At the same time, myriad treatment and prevention programs are providing services to victims and offenders. Although limited research knowledge exists regarding the effectiveness of these programs, such information is often scattered, inaccessible, and difficult to obtain.
Violence in Families takes the first hard look at the successes and failures of family violence interventions. It offers recommendations to guide services, programs, policy, and research on victim support and assistance, treatments and penalties for offenders, and law enforcement. Included is an analysis of more than 100 evaluation studies on the outcomes of different kinds of programs and services.
Violence in Families provides the most comprehensive review on the topic to date. It explores the scope and complexity of family violence, including identification of the multiple types of victims and offenders, who require different approaches to intervention. The book outlines new strategies that offer promising approaches for service providers and researchers and for improving the evaluation of prevention and treatment services. Violence in Families discusses issues that underlie all types of family violence, such as the tension between family support and the protection of children, risk factors that contribute to violent behavior in families, and the balance between family privacy and community interventions.
The core of the book is a research-based review of interventions used in three institutional sectors—social services, health, and law enforcement settings—and how to measure their effectiveness in combating maltreatment of children, domestic violence, and abuse of the elderly. Among the questions explored by the committee: Does the child protective services system work? Does the threat of arrest deter batterers? The volume discusses the strength of the evidence and highlights emerging links among interventions in different institutional settings.
Thorough, readable, and well organized, Violence in Families synthesizes what is known and outlines what needs to be discovered. This volume will be of great interest to policymakers, social services providers, health care professionals, police and court officials, victim advocates, researchers, and concerned individuals.
READ FREE ONLINE
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Drugs, Brains, and Behavior: The Science of Addiction Drug Misuse and Addiction
What is drug addiction.
Addiction is defined as a chronic, relapsing disorder characterized by compulsive drug seeking and use despite adverse consequences. † It is considered a brain disorder, because it involves functional changes to brain circuits involved in reward, stress, and self-control. Those changes may last a long time after a person has stopped taking drugs. 11
Addiction is a lot like other diseases, such as heart disease. Both disrupt the normal, healthy functioning of an organ in the body, both have serious harmful effects, and both are, in many cases, preventable and treatable. If left untreated, they can last a lifetime and may lead to death.
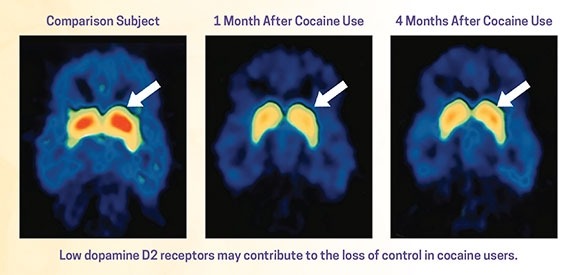
Why do people take drugs?
In general, people take drugs for a few reasons:
- To feel good. Drugs can produce intense feelings of pleasure. This initial euphoria is followed by other effects, which differ with the type of drug used. For example, with stimulants such as cocaine, the high is followed by feelings of power, self-confidence, and increased energy. In contrast, the euphoria caused by opioids such as heroin is followed by feelings of relaxation and satisfaction.
- To feel better. Some people who suffer from social anxiety, stress, and depression start using drugs to try to feel less anxious. Stress can play a major role in starting and continuing drug use as well as relapse (return to drug use) in patients recovering from addiction.
- To do better. Some people feel pressure to improve their focus in school or at work or their abilities in sports. This can play a role in trying or continuing to use drugs, such as prescription stimulants or cocaine.
- Curiosity and social pressure. In this respect, teens are particularly at risk because peer pressure can be very strong. Adolescence is a developmental period during which the presence of risk factors, such as peers who use drugs, may lead to substance use.
If taking drugs makes people feel good or better, what's the problem?

When they first use a drug, people may perceive what seem to be positive effects. They also may believe they can control their use. But drugs can quickly take over a person's life. Over time, if drug use continues, other pleasurable activities become less pleasurable, and the person has to take the drug just to feel “normal.” They have a hard time controlling their need to take drugs even though it causes many problems for themselves and their loved ones. Some people may start to feel the need to take more of a drug or take it more often, even in the early stages of their drug use. These are the signs of an addiction.
Even relatively moderate drug use poses dangers. Consider how a social drinker can become intoxicated, get behind the wheel of a car, and quickly turn a pleasurable activity into a tragedy that affects many lives. Occasional drug use, such as misusing an opioid to get high, can have similarly disastrous effects, including impaired driving and overdose.
Do people choose to keep using drugs?
The initial decision to take drugs is typically voluntary. But with continued use, a person's ability to exert self-control can become seriously impaired. This impairment in self-control is the hallmark of addiction.
Brain imaging studies of people with addiction show physical changes in areas of the brain that are critical to judgment, decision-making, learning and memory, and behavior control. 12 These changes help explain the compulsive nature of addiction.
Why do some people become addicted to drugs, while others do not?
As with other diseases and disorders, the likelihood of developing an addiction differs from person to person, and no single factor determines whether a person will become addicted to drugs. In general, the more risk factors a person has, the greater the chance that taking drugs will lead to drug use and addiction. Protective factors, on the other hand, reduce a person's risk. Risk and protective factors may be either environmental or biological.
What biological factors increase risk of addiction?
Biological factors that can affect a person's risk of addiction include their genes, stage of development, and even gender or ethnicity. Scientists estimate that genes, including the effects environmental factors have on a person's gene expression, called epigenetics, account for between 40 and 60 percent of a person's risk of addiction. 27 Also, teens and people with mental disorders are at greater risk of drug use and addiction than others. 28
What environmental factors increase the risk of addiction?
Environmental factors are those related to the family, school, and neighborhood. Factors that can increase a person's risk include the following:
- Home and Family. The home environment, especially during childhood, is a very important factor. Parents or older family members who use drugs or misuse alcohol, or who break the law, can increase children's risk of future drug problems. 29
- Peer and School. Friends and other peers can have an increasingly strong influence during the teen years. Teens who use drugs can sway even those without risk factors to try drugs for the first time. Struggling in school or having poor social skills can put a child at further risk for using or becoming addicted to drugs. 30
What other factors increase the risk of addiction?
- Early use. Although taking drugs at any age can lead to addiction, research shows that the earlier people begin to use drugs, the more likely they are to develop serious problems. 31 This may be due to the harmful effect that drugs can have on the developing brain. 32 It also may result from a mix of early social and biological risk factors, including lack of a stable home or family, exposure to physical or sexual abuse, genes, or mental illness. Still, the fact remains that early use is a strong indicator of problems ahead, including addiction.
- How the drug is taken. Smoking a drug or injecting it into a vein increases its addictive potential. 33,34 Both smoked and injected drugs enter the brain within seconds, producing a powerful rush of pleasure. However, this intense high can fade within a few minutes. Scientists believe this powerful contrast drives some people to repeatedly use drugs to recapture the fleeting pleasurable state.
Images of Brain Development in Healthy Children and Teens (Ages 5-20)
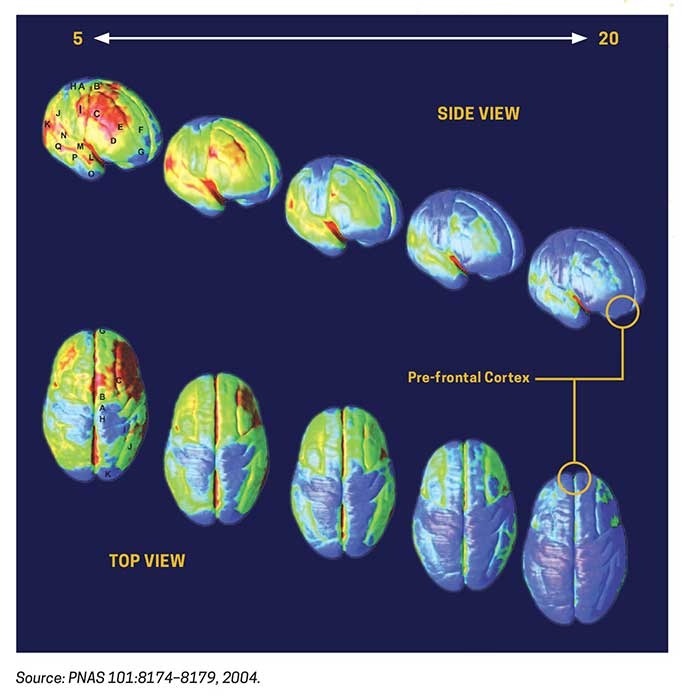
The brain continues to develop into adulthood and undergoes dramatic changes during adolescence.
One of the brain areas still maturing during adolescence is the prefrontal cortex—the part of the brain that allows people to assess situations, make sound decisions, and keep emotions and desires under control. The fact that this critical part of a teen’s brain is still a work in progress puts them at increased risk for trying drugs or continuing to take them. Introducing drugs during this period of development may cause brain changes that have profound and long-lasting consequences.
† The term addiction as used in this booklet is equivalent to a severe substance use disorder as defined by the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5, 2013).
- First Online: 24 June 2017
Cite this chapter

- John Joshua 2
556 Accesses
The use of illicit drugs and the quality of life is intended to provide a rational for a change in some of the present drug policies. After all, the use and the abuse of drugs is largely a health issue and cannot be solved without adequately considering the causes of drug abuse, including the medical, psychiatric, psychological, and sociological factors. Criminal law can only be part of the solution; it has to effectively work with psychologically and medically trained personnel. To use solely the criminal law in regard to drug abuse may treat the symptoms, but it is not a cure. It has been argued that the legalization of the use of illegal drugs but within a regulated market might be more suitable.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Johnson, C. M., & Meier, K. J. (1990). The wages of sin: Taxing America’s legal vices. Western Political Quarterly, 43 (3), 577–595.
Article Google Scholar
Download references
Author information
Authors and affiliations.
Deakin University, Melbourne, Victoria, Australia
John Joshua
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to John Joshua .
Rights and permissions
Reprints and permissions
Copyright information
© 2017 The Author(s)
About this chapter
Joshua, J. (2017). Conclusion. In: The Economics of Addictive Behaviours Volume III. Palgrave Macmillan, Cham. https://doi.org/10.1007/978-3-319-59138-4_8
Download citation
DOI : https://doi.org/10.1007/978-3-319-59138-4_8
Published : 24 June 2017
Publisher Name : Palgrave Macmillan, Cham
Print ISBN : 978-3-319-59137-7
Online ISBN : 978-3-319-59138-4
eBook Packages : Economics and Finance Economics and Finance (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

- Report Highlights
- EU-Summaries

- About the publications
Psychoactive Drugs Tobacco, Alcohol, and Illicit Substances
- Level 1: Summary
- Level 2: Details
- Level 3: Source
- 7. Conclusions
Drug use and addiction cause a lot of disease and disability in the world. Recent advances in neuroscience may help improve policies to reduce the harm that the use of tobacco, alcohol , and other psychoactive drugs impose on society.
Effective action should take into account the following:
- Since the effects of drugs on health vary greatly depending on the type of drug and on the way it is used, the public health response to drug use should be proportional to the health-related harm it causes.
- Use of psychoactive substances is to be expected because of their pleasurable effects as well as social influences. The greater the frequency and amount of drug used, the higher the risk of becoming dependent.
- Effective public health policies and programmes that address not only drug dependence but also other forms of harmful drug use could lead to a significant reduction in the overall health burden of drug use.
- The risk of becoming dependent on drugs is determined by a combination of biological, genetic , psychological, social, cultural, and environmental factors. Currently, it is impossible to predict who will become drug dependent.
- Drug dependence is a medical disorder, not a lack of willpower or strength of character.
- Drug dependence and mental illnesses often affect the same individuals. Therefore, it would be useful to integrate research, assessments, and treatments for both types of disorders.
- The cost-effective treatment and management of drug dependence can save lives, improve health, and reduce costs to society. Beyond stopping drug use, effective treatment requires changes in the behaviour of users and often the use of substitute drugs.
- Treatment must be accessible to all in need and the health care sector should provide the most cost-effective treatments.
- Prejudice and discrimination against drug dependent people is one of the main barriers to their treatment. Everyone has the same rights to health care, education, work opportunities and integration into society.
- Investment in brain research on drug dependence must continue and expand to cover social science, prevention, treatment and policy research. The results of research should be used to devise evidence-based policies to reducing the burden from drug use.
Recent advances in the treatment of drug dependence raise difficult ethical issues that must be addressed by scientific and policy communities as a priority. More...
- 1. What are psychoactive drugs and how much are they used?
- 2. How do psychoactive drugs affect health?
- 3. How does drug addiction affect the functioning of the brain?
- 4. How does drug addiction develop?
- 5. Why do drug addiction and mental illness often coexist?
- 6. How can addiction to psychoactive drugs be prevented and treated?
- Accidental poisoning
- Acrylamide in food
- Acupuncture
- Agriculture
- Aids Epidemic
- Air Pollution Europe
- Air quality in Europe
- Allergenic fragrances
- Aluminium exposure
- Animal testing
- Antibiotic resistance
- Antibiotics Research
- Antimicrobial resistance
- Aquatic environment
- Arctic Climate Change
- Artificial Light
- Artificial Light and Health
- Aspartame Reevaluation
- Aspirin & Cancer
- Benzodiazepines
- Biodiversity
- Biological Diversity
- Biosecurity
- Bisphenol A
- CO 2 Capture & Storage
- Cancer rates and mortality, types and causes
- Chemical Mixtures
- Children & Screens
- Chlorine Sodium Hypochlorite
- Chlorpyrifos pesticide
- Chronic Diseases on Labour Practices
- Circular Economy
- Climate Change
- Climate Change Mitigation
- Climate impact of shale gas
- Climate impacts adaptation
- Dental Amalgams
- Dental Fillings
- Desertification
- Diet & Nutrition
- Ecosystem Change
- Effects of cannabis
- Electromagnetic Fields
- Electronic Cigarettes
- Endocrine Disruptors
- Endocrine disrupting properties of pesticides
- Endocrine disruptors risks
- Energy Saving Lamps
- Energy Technologies
- Epidemic diseases
- Estrogen-progestogen cancer risk
- Europe Green Deal
- Evaluation of endocrine disruptors
- Exposure to chemical mixtures
- Fisheries and aquaculture
- Fluorinated gases
- Food & Agriculture
- Food Wastage
- Forests & Energy
- Forests & agriculture land use
- Fukushima Consequences
- Fukushima accident
- Genetically Modified Crops
- Geothermal Energy
- Global Biodiversity Outlook 4
- Global Public Health Threats
- Global Warming
- Gluten intolerance
- Glyphosate and cancer
- Hazardous chemicals
- Health Effects of Electromagnetic Fields
- Health Environment Management
- Illicit drugs in Europe
- Impacts of a 4°C global warming
- India Millennium Development Goals
- Indonesian forests
- Indoor Air Quality
- Land Degradation and Desertification
- Lyme Disease
- Marine Litter
- Marine litter
- Mercury from dental amalgam
- Mercury in CFL
- Metal-on-Metal hip implants
- Methylene glycol
- Mineral extraction risks
- Multiple vaccinations
- Nano-silica
- Nanomaterials
- Nanotechnologies
- Neonicotinoids
- Nitrogen Dioxide
- Non-human primates
- Organic Food
- Ozone layer depletion
- Parabens used in cosmetics
- Particulate Matter
- Perfluorooctanoic acid (PFOA)
- Personal Music Players & Hearing
- Pesticides occupational risks
- Pharmaceuticals environment
- Phosphate resources
- Phthalates Comparison
- Phthalates in school supplies
- Poly brominated flame retardant decaBDE
- Power lines
- Psychoactive Drugs
- Radiological nuclear emergency
- Respiratory Diseases
- Safety of Cosmetics
- Safety of sunscreens
- Sand Extraction
- Security Scanners
- Silver Nanoparticles
- Single-use plastics
- Soils degradation
- Solar Energy
- State of the European Environment
- Static Fields
- Substitution of harmful chemicals
- Sulfaxoflor Pesticide
- Sunbeds & UV radiation
- Sustainable oceans
- Synthetic Biology
- Thorium nuclear fuel
- Tidal Energy
- Titanium dioxide nanoparticles
- Tooth Whiteners
- Transgenic salmon
- Tuberculosis
- Wastewater management
- Water Disinfectants
- Water Resources
- Water Resources Assessments
- Water resources
- Wind Resources
- X-Ray Full-Body Scanners

Get involved!
This summary is free and ad-free, as is all of our content. You can help us remain free and independant as well as to develop new ways to communicate science by becoming a Patron!
- Terms & Conditions

- Search Menu
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Urban Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Papyrology
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Acquisition
- Language Evolution
- Language Reference
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Religion
- Music and Media
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Science
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Lifestyle, Home, and Garden
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Clinical Neuroscience
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Strategy
- Business Ethics
- Business History
- Business and Government
- Business and Technology
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic Systems
- Economic History
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Behaviour
- Political Economy
- Political Institutions
- Political Theory
- Politics and Law
- Public Administration
- Public Policy
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Developmental and Physical Disabilities Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

- < Previous chapter

12 Conclusion
- Published: February 2015
- Cite Icon Cite
- Permissions Icon Permissions
The main conclusions from the chapters are drawn. Substance use and gambling indeed permeate our daily lives, and the current way these behaviours are handled is neither integrated nor effective in optimizing well-being. As a consequence, these behaviours incur considerable health and social harm in current societies, leading to huge economic costs. Substance use and gambling should be seen as a continuum, with addiction just being one way to frame one end of this continuum, heavy use. If seen this way, it becomes clear that shifts in the distribution of behaviours can be very effective in reducing social and health harm. Policies should not just be focused on particular behaviours, but on the optimal mix of distributions which could reduce the maximum harm.
Signed in as
Institutional accounts.
- Google Scholar Indexing
- GoogleCrawler [DO NOT DELETE]
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
- Add your ORCID iD
Institutional access
Sign in with a library card.
- Sign in with username/password
- Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Sign in through your institution
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Cliff Schaffer's Home Page
Contents | Feedback | Search | DRCNet Home Page | Join DRCNet
DRCNet Library | Schaffer Library | Major Studies | Dealing With Drug Abuse
Essay on Drug Abuse
Here we have shared the Essay on Drug Abuse in detail so you can use it in your exam or assignment of 150, 250, 400, 500, or 1000 words.
You can use this Essay on Drug Abuse in any assignment or project whether you are in school (class 10th or 12th), college, or preparing for answer writing in competitive exams.
Topics covered in this article.
Essay on Drug Abuse in 150 words
Essay on drug abuse in 250-300 words, essay on drug abuse in 500-1000 words.
Drug abuse is a global issue that poses serious risks to individuals and society. It involves the harmful and excessive use of drugs, leading to physical and mental health problems. Drug abuse can result in addiction, organ damage, cognitive impairment, and social and economic difficulties. Prevention efforts should focus on education, raising awareness about the dangers of drug abuse, and promoting healthy lifestyles. Access to quality healthcare and addiction treatment services is crucial for recovery. Strengthening law enforcement measures against drug trafficking is necessary to address the supply side of the problem. Creating supportive environments and opportunities for positive engagement can help prevent drug abuse. By taking collective action, we can combat drug abuse and build healthier communities.
Drug abuse is a growing global concern that poses significant risks to individuals, families, and communities. It refers to the excessive and harmful use of drugs, both legal and illegal, that have negative effects on physical and mental health.
Drug abuse has severe consequences for individuals and society. Physically, drug abuse can lead to addiction, damage vital organs, and increase the risk of overdose. Mentally, it can cause cognitive impairment, and psychological disorders, and deteriorate overall well-being. Additionally, drug abuse often leads to social and economic problems, such as strained relationships, loss of employment, and criminal activities.
Preventing drug abuse requires a multi-faceted approach. Education and awareness programs play a crucial role in informing individuals about the dangers of drug abuse and promoting healthy lifestyle choices. Access to quality healthcare and addiction treatment services is vital to help individuals recover from substance abuse. Strengthening law enforcement efforts to curb drug trafficking and promoting international cooperation is also essential to address the supply side of the issue.
Community support and a nurturing environment are critical in preventing drug abuse. Creating opportunities for individuals, especially young people, to engage in positive activities and providing social support systems can serve as protective factors against drug abuse.
In conclusion, drug abuse is a significant societal problem with detrimental effects on individuals and communities. It requires a comprehensive approach involving education, prevention, treatment, and enforcement. By addressing the root causes, raising awareness, and providing support to those affected, we can combat drug abuse and create a healthier and safer society for all.
Title: Drug Abuse – A Global Crisis Demanding Urgent Action
Introduction :
Drug abuse is a pressing global issue that poses significant risks to individuals, families, and communities. It refers to the excessive and harmful use of drugs, both legal and illegal, that have detrimental effects on physical and mental health. This essay explores the causes and consequences of drug abuse, the social and economic impact, prevention and treatment strategies, and the importance of raising awareness and fostering supportive communities in addressing this crisis.
Causes and Factors Contributing to Drug Abuse
Several factors contribute to drug abuse. Genetic predisposition, peer pressure, stress, trauma, and environmental influences play a role in initiating substance use. The availability and accessibility of drugs, as well as societal norms and cultural acceptance, also influence drug abuse patterns. Additionally, underlying mental health issues and co-occurring disorders can drive individuals to self-medicate with drugs.
Consequences of Drug Abuse
Drug abuse has devastating consequences on individuals and society. Physically, drug abuse can lead to addiction, tolerance, and withdrawal symptoms. Substance abuse affects vital organs, impairs cognitive function, and increases the risk of accidents and injuries. Mental health disorders, such as depression, anxiety, and psychosis, are often associated with drug abuse. Substance abuse also takes a toll on relationships, leading to strained family dynamics, social isolation, and financial instability. The social and economic costs of drug abuse include increased healthcare expenses, decreased productivity, and the burden on criminal justice systems.
Prevention and Education
Preventing drug abuse requires a comprehensive and multi-faceted approach. Education and awareness programs are essential in schools, communities, and the media to inform individuals about the risks and consequences of drug abuse. Promoting healthy coping mechanisms, stress management skills, and decision-making abilities can empower individuals to resist peer pressure and make informed choices. Early intervention programs that identify at-risk individuals and provide support and resources are crucial in preventing substance abuse.
Treatment and Recovery
Access to quality healthcare and evidence-based addiction treatment is vital in addressing drug abuse. Treatment options include detoxification, counseling, behavioral therapies, and medication-assisted treatments. Rehabilitation centers, support groups, and outpatient programs provide a continuum of care for individuals seeking recovery. Holistic approaches, such as addressing co-occurring mental health disorders and promoting healthy lifestyles, contribute to successful long-term recovery. Support from family, friends, and communities plays a significant role in sustaining recovery and preventing relapse.
Law Enforcement and Drug Policies
Effective law enforcement efforts are necessary to disrupt drug trafficking and dismantle illicit drug networks. International cooperation and collaboration are crucial in combating the global drug trade. Additionally, drug policies should focus on a balanced approach that combines law enforcement with prevention, treatment, and harm reduction strategies. Shifting the emphasis from punitive measures toward prevention and rehabilitation can lead to more effective outcomes.
Creating Supportive Communities:
Fostering supportive communities is vital in addressing drug abuse. Communities should provide resources, social support networks, and opportunities for positive engagement. This includes promoting healthy recreational activities, providing vocational training, and creating safe spaces for individuals in recovery. Reducing the stigma associated with drug abuse and encouraging empathy and understanding are crucial to building a compassionate and supportive environment.
Conclusion :
Drug abuse remains a complex and multifaceted issue with far-reaching consequences. By addressing the causes, raising awareness, implementing preventive measures, providing quality treatment and support services, and fostering supportive communities, we can combat drug abuse and alleviate its impact. It requires collaboration and a collective effort from individuals, communities, governments, and organizations to build a society that is resilient against the scourge of drug abuse. Through education, prevention, treatment, and compassion, we can pave the way toward a healthier and drug-free future.
Related Posts

Essential Elements of Valid Contract (Explained With Examples)

What is World Population? Main Causes, Effects, Top 20 Countries
- Study Protocol
- Open access
- Published: 16 May 2024
Developing practical strategies to reduce addiction-related stigma and discrimination in public addiction treatment centers: a mixed-methods study protocol
- Maryam Khazaee-Pool ORCID: orcid.org/0000-0002-2587-3460 1 ,
- Seyed Abolhassan Naghibi 1 ,
- Tahereh Pashaei 2 &
- Koen Ponnet 3
Addiction Science & Clinical Practice volume 19 , Article number: 40 ( 2024 ) Cite this article
68 Accesses
Metrics details
People with substance use disorders (SUDs) have restricted engagement with health-care facilities and describe repeated experiences of stigma, discrimination, and mistreatment when receiving care at health-care and public addiction treatment centers (PATCs). The purpose of the current study is to design practical cultural-based strategies to reduce addiction-related stigma and discrimination at PATCs.
Methods/design
The present study will use a mixed-methods design with an explanatory sequential approach. Phase 1 of the study will combine a cluster sampling technique combined with a cross-sectional survey of Patients with Substance Use Disorders (SUDs) in Mazandaran, Iran. A total of three hundred and sixty individuals with SUDs will be selected to assess their experiences of stigma and factors predicting stigma. Phase 2 will involve qualitative study aimed at exploring participants’ perceptions regarding the aspects and determinants of their stigma experience. The participants will include two groups: people with SUDs and staff/health-care providers at PATCs. Participants for Phase 2 will be purposively sampled from those involved in Phase 1.Qualitative data will be collected using in-depth semi-structured interviews and focus group discussions and analyzed using content analysis with a conventional approach. Phase 3 will focus on the development of new strategies to reduce the experiences of stigma among people with SUDs at PATCs. These strategies will be formulated based on the findings derived from the qualitative and quantitative data obtained in Phases 1 and 2, a comprehensive review of the literature, and expert opinions gathered using the nominal group technique.
This is one of the few studies conducted within the domain of stigma pertaining to individuals who use drugs within the context of Iranian culture employing a mixed-methods approach, this study aims to develop culturally sensitive strategies to reduce such problems from the perspective of Iranian people who use drugs. It is anticipated that the study will yield evidence-based insights and provide practical strategies to reduce the stigma and discrimination experienced by people who use drugs at PATCs. Such outcomes are important for informing policymaking and designing healthcare interventions tailored to the needs of individuals grappling with substance dependency.
Introduction
Substance use disorders (SUDs) represent complex illnesses that disrupt brain activity and function resulting in significant personal and societal repercussions [ 1 , 2 , 3 , 4 ]. Recognizing the detrimental impact of SUD-related stigma, The National Institute on Drug Abuse has prioritized efforts to understand and diminish this stigma [ 5 ]. Research on mental illness stigma has consistently revealed its association with adverse outcomes, including exacerbated symptoms and impaired social functioning [ 6 ]. With the increasing prevalence of SUDs within the general population [ 1 , 2 , 3 , 4 , 7 ] and the necessity to inform policymakers and allocate legislative resources effectively [ 8 , 9 ], it becomes crucial to raise awareness about the stigma surrounding SUDs in society. Studies investigating SUD-related stigma have documented various forms of prejudice and discrimination experienced by people who use drugs, particularly from healthcare providers, which are correlated with detrimental health outcomes, including mental health disorders and compromised physical health [ 10 , 11 , 12 , 13 , 14 ].
Part of the stigmatization faced by healthcare providers stems from the inaction of public health leaders [ 15 ], while another part arises from the lack of training among healthcare workers in SUD treatment [ 16 , 17 ], both of which contribute to inadequate implementation of effective remedies. Numerous studies have demonstrated the persistent and entrenched nature of stigma, often rooted in the misconception that drug addiction reflects a personal choice, indicating a lack of self-control and moral failure. Stigma and discrimination levels are notably high both within the general population and among professions that interact with individuals with SUDs, such as the healthcare industry. Some studies have demonstrated that stigma and prejudice harm SUD patients’ health and cause delays in the delivery of high-quality care in venues for public addiction treatment. Individuals with SUDs frequently encounter stigma and discrimination across all levels of care at public addiction treatment centers (PATCs) [ 17 , 18 , 19 , 20 , 21 , 22 ].
The World Health Organization is working with several countries to train medical professionals in screening, brief intervention, and referral to treatment (SBIRT) [ 23 , 24 , 25 , 26 , 27 ]. SBIRT is a treatment strategy that encourages all medical professionals to identify patients who are taking drugs at statistically dangerous levels, provide brief interventions to promote drug use reduction, and then refer patients who meet criteria for drug use or addiction for more intensive treatments. According to some studies, screening and brief interventions (SBI) have the greatest effect on reducing the use of psychoactive substances [ 20 , 23 , 26 , and 28 ]. SBI is a simple, quick advisory intervention that stresses several types of specific behavior. It may be used by professionals in a variety of situations [ 29 ].
Unfortunately, societal acceptability of evidence-based initiatives does not always come easily [ 30 ]. The allocation of healthcare interventions is influenced by various factors, including the novelty of characteristics, healthcare worker attitudes, and the stigma associated with a health condition. Research has consistently demonstrated that negative attitudes among healthcare professionals can impede the adoption of innovative practices, the quality of services provided, and clients’ adherence to preventive and therapeutic measures [ 31 , 32 , 33 , 34 , 35 , 36 ]. Therefore, education and training programs should prioritize the modification of attitudes and beliefs among healthcare providers to promote the uptake of SBI for drug addiction [ 37 , 38 ].
Research in health has linked stigma from service providers at care or treatment centers with poor utilization of preventive programs and reduced accessibility for stigmatized individuals to access effective interventions [ 39 , 40 ]. Efforts to mitigate stigmatization are underway, particularly for individuals living with mental health conditions [ 40 , 41 ]. Studies have identified three main approaches: (i) providing educational interventions to dispel misconceptions about mental illnesses, (ii) facilitating interactions between individuals with mental illnesses and the community to challenge community attitudes, and (iii) exposing stigmatizing beliefs and behaviors in the hope of eliciting public condemnation and reducing their acceptance [ 41 , 42 , 43 ]. Although anti-stigma strategies are sometimes inaccessible or unproven, the aforementioned techniques aim to change community perceptions of people facing such circumstances [ 39 , 41 ].
To reduce the stigma associated with mental illness, several national and international strategies have been developed, and the range of programs continues to expand. However, stigma and discrimination against individuals with SUDs remain poorly understood [ 44 , 45 ]. Moreover, there has been limited research investigating the creation and execution of practices or interventions aimed at reducing SUD-related stigma and discrimination among people who use drugs by PHC professionals [ 46 , 47 , 48 , 49 , 50 ]. When developing anti-stigma strategies, it is essential to consider the cultural norms and different behaviors of specific groups, including healthcare professionals, youth, police, and policymakers [ 14 , 38 , 40 , 45 , 49 ].
For many years, stigma related to SUDs has posed challenges in Iran [ 51 , 52 , 53 ]. One of the most significant obstacles to improving the well-being and health of individuals with SUDs is the stigmatization and discrimination they face within the healthcare system [ 52 , 54 ]. This results in disparities in healthcare facilities, including limited availability, accessibility, and quality of services for individuals with SUDs [ 54 ]. Stigmatization negatively impacts help-seeking behavior from official healthcare facilities, leading to poorer outcomes and perpetuating the misconception that SUDs are untreatable. individuals with SUDs may be more prone to engaging in unhealthy behaviors, refusing treatment, non-compliance with prescription instructions, weakened immune systems, and experiencing adverse consequences [ 55 ].
Comprehensive plans for the promotion, prevention, treatment, and recovery of individuals with substance use disorders (SUDs) should consider numerous socioeconomic variables. Adopting a “health-in-all policies” approach is crucial in addressing these challenges. Strategies to increase access to treatment and reduce stigma and discrimination towards individuals with SUDs may involve integrating SUD care and fostering collaboration between primary care clinicians and other healthcare providers [ 22 , 38 , 39 , 40 , 53 ]. International efforts to combat addiction-related stigma have emphasized the importance of lowering barriers to a variety of health treatments for individuals with SUDs. Despite this emphasis and the widespread consensus that reducing stigma associated with SUDs is important, progress in this area has been slow [ 40 , 49 , 56 , 57 , 58 ]. While strategies to reduce SUD-related stigma have gained traction in Western industrial nations in recent years [ 59 , 60 ]. They remain largely absent from national and government policies, information, and healthcare plans in many parts of the world [ 40 , 42 , 44 , 53 , 58 , 61 ].
Longitudinal data on behavior changes in response to stigma and discrimination related to SUDs in Iran are lacking, making it challenging to develop effective strategies to reduce such stigma, especially in PATCs. The most widely recognized solutions are those that are acceptable, suitable, and adaptable across cultural contexts. Further research and needs assessments are required to identify additional strategies for addressing addiction-related stigma [ 42 , 47 , 56 ]. To address the stigma associated with addiction, it is necessary to study the effectiveness and feasibility of stigma-reducing interventions [ 55 , 58 , 62 ].
In Iran, as in many other countries, there is a lack of comprehensive strategies aimed at reducing stigma related to SUDs. Additionally, there is a dearth of studies providing practical strategies, both quantitative and qualitative, to address addiction-related stigma and discrimination specifically within PATCs for individuals with SUDs in Iran. Mixed-method analyses focusing on this issue are also lacking. While there have been some studies conducted in Iran to explore stigma toward individuals with SUDs, none have offered strategies or methods to mitigate stigma within public treatment settings. Although limited, existing data from small-scale qualitative studies in Iranian healthcare settings indicate the prevalence of discriminatory attitudes toward people with SUDs, manifesting as care refusal, substandard care, excessive precautions, physical distancing, humiliation, and blame [ 30 , 51 , 52 , 55 , 62 , 63 , 64 ].
Iran’s unique cultural characteristics [ 65 ] including demographic factors [ 66 ], cultural norms [ 67 ], ethnic identity [ 68 ], social customs, traditions, peer relationships, and poverty [ 69 ] shape the societal landscape and perceptions surrounding behaviors, including those related to SUDs. Consequently, addressing addiction-related stigma and its impact on individuals who use drugs in Iran requires sensitivity to these cultural nuances [ 64 , 70 ]. In Iran, SUDs are not solely viewed as medical issues but also as a socio-cultural problem. This perspective can lead to delays in treatment and pose significant challenges for patients and their families. Consequently, reducing stigma and discrimination associated with the rising prevalence of addiction among Iranians has been identified as a pressing priority within the healthcare system [ 70 ].
In Iranian society, plays a significant role in shaping perceptions and experiences of SUD across various demographic groups, including differences related to age, gender, socioeconomic status, and education level [ 64 ]. Research in Iran has extensively explored how cultural influences manifest in SUDs, examining factors such as demographic characteristics, regional prevalence patterns, gender dynamics, religious beliefs, and the stigma associated with drug use. These studies highlight the complex interplay between cultural norms, individual behaviors, and societal attitudes toward SUDs within the Iranian context [ 66 , 67 , 68 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 ].
Of course, the stigma surrounding drug addiction in Iran exhibits variations based on factors such as gender, the specific type of drug used, and residential location [ 81 , 82 ]. Interestingly, a study examining literary works in Iran reveals a historical acceptance of opium as a medicinal remedy by prominent Iranian poets. Opium has been portrayed positively, with references to its purported benefits such as regulating blood pressure and relieving pain [ 83 ]. This cultural perspective reflects a nuanced view of drug consumption in Iranian society, indicating that stigma surrounding certain drugs may not be uniform. Rather, stigma appears to evolve dynamically within social contexts, presenting new challenges that may differ from those associated with more entrenched forms of stigma.
Although previous qualitative studies have provided valuable insights into the experiences of individuals with SUD interacting with healthcare professionals, our understanding of SUD-related stigma within the Iranian healthcare system remains limited. A comprehensive, multiphase study employing a mixed-methods approach is needed to systematically assess the experiences of Iranian people who use drugs regarding stigma and to develop evidence-based guidelines and strategies for reducing stigma and discrimination against individuals with SUDs at PATCs. The importance and the impact of stigma and discrimination related to SUDs within Iranian culture as well as the influence of cultural differences on patients’ healthcare-seeking attitudes and the support services provided by the healthcare system, form the foundation of this mixed-method study. Given these considerations, it is imperative to address cultural factors associated with substance use disorders and the stigma stemming from substance consumption in Iranian society. This is because the cultural, economic, and social variations across different societies warrant an examination of human experiences within each unique cultural context. Therefore, the aim of this study is to explore comprehensive and culturally sensitive strategies in order to reduce addiction-related stigma and discrimination at PATCs.
The study aims
This mixed-methods study aims to identify strategies to reduce stigma and discrimination against Iranian people who use drugs at PATCs. The specific objectives of the study can be categorized into three phases as follows:
To measure the perceived stigma score among people with substance use disorders (SUDs) who were referred to PATCs in Mazandaran, Iran.
To evaluate professionals’ attitudes towards people with SUDs receiving treatment at PATCs in Mazandaran, Iran.
To measure the social distance score towards people with substance use disorders seeking treatment at PATCs in Mazandaran, Iran.
To examine the relationship between socio-demographic characteristics and perceived stigma among individuals with substance use disorders.
To investigate the relationship between perceived stigma, social distance, and professionals’ attitudes toward people with SUDs.
To explore the perspectives and experiences of people who use drugs concerning the various aspects and determinants of stigma and discrimination stemming from the community, healthcare centers, or PATCs due to drug use.
To examine healthcare providers’ perspectives on stigma against individuals who use drugs.
To develop evidence-based cultural strategies aimed at diminishing stigma and discrimination at PATCs against Iranian people who use drugs faced health challenges.
Study design
This study will employ a mixed-methods technique with an explanatory sequential approach for data collection and analysis. Grounded in pragmatic principles and logic, the mixed-methods paradigm combines quantitative and qualitative methodologies to provide a comprehensive understanding of the research questions. In this methodology, the researcher first gathers quantitative data to identify patterns or trends requiring further exploration. Subsequently, qualitative data are collected from individuals who can offer insights to enhance the understanding and interpretation of the quantitative findings [ 84 ]. According to this paradigm, merging qualitative and quantitative methods results in a deeper comprehension of the issue [ 85 , 86 ].
This study will be conducted in three phases. The first phase will be a quantitative study, during which, quantitative data will be gathered. The second phase of this project will be a more detailed exploratory qualitative study of participants’ experiences regarding SUD-related stigma toward and discrimination against people who use drugs at PATCs. At the end of the second phase, the qualitative and quantitative findings will be integrated. The third phase of the study will involve the development of evidence-based and culturally sensitive strategies based on a literature review, the results of Phases 1 and 2, and experts’ opinions using the nominal group technique (NGT) (Fig. 1 ). Full explanations of each part of the study are provided below.
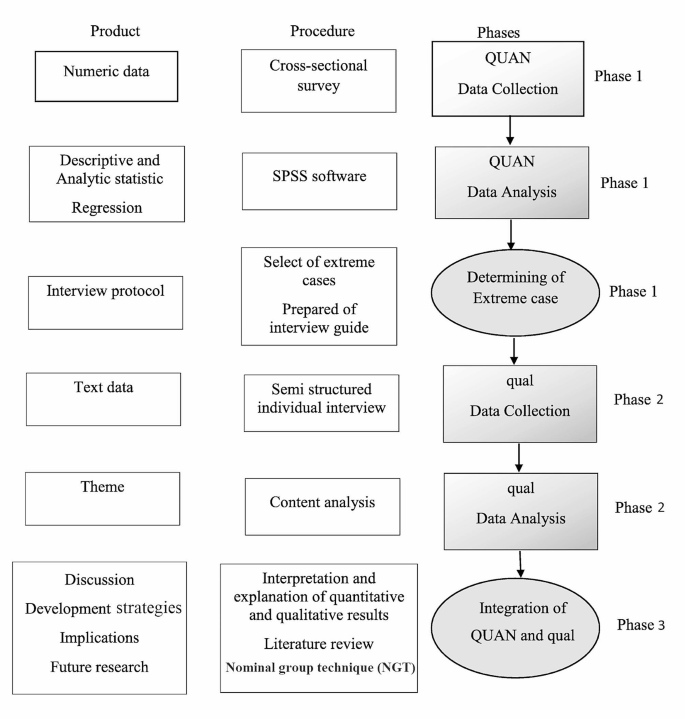
Study visual diagram
Phase 1: quantitative study
The quantitative phase will be a descriptive-analytic cross-sectional study conducted among Iranian people with SUDs living in Mazandaran, Iran. In this phase, we will assess perceived stigma experiences and their relationship with social distance, perceived dangerousness, experts’ discrimination or acceptance, and sociodemographic characteristics among the participants. The target population will consist of people who are referred to PATCs in Mazandaran, Iran. The Perceived Stigma of Addiction Scale (PSAS), Health Professionals’ Attitude Towards Substance Abusers Scale (HPA-SAS), and Social Distance Scale (SDS) will be used. These scales will be validated for use among Iranian people.
Sample size and sampling method
There is no shortage of research on stigma toward and discrimination against people with SUDs at PATCs and other health-care settings in Iran. Therefore, the sample size is calculated based on Matsumoto’s study [ 87 ]. Following Matsumoto et al. [ 87 ], the calculated sample size is 240, based on the largest standard deviation related to the sub dimension of stigma (SD = 12.39), with a precision (d) of 0.05 around the mean (m = 35.01), and α = 0.05. In most cases, the design effect’s numerical value is about 1.5–2. In this study, we will apply 1.5, and the final sample size will be increased to 360 substance users, based on cluster sampling.
For this project, fifteen PATCs in Mazandaran will be selected. A cluster sampling method will be employed, with each cluster comprising a comparable number of respondents. Mazandaran will be divided into three areas (west, central, and east). All PATCs within these areas will be enumerated, and five PATCs will be randomly chosen from each area. Individuals with SUDs who are referred to the PATCs will be invited to participate in the project.
The participants will be offered comprehensive explanations of the goals and methods of the research. The sociodemographic questions, the PSAS, HPA-SAS, and SDS will be administered in a “quiet setting” [questionnaire will be presented while maintaining patient privacy] by a research group member and then collected in person. The investigator will fill out the scales to ensure that the same data collection method is used for all individuals. Informed consent will be obtained from the individuals prior to the data collection.
Inclusion criteria
Individuals will be eligible for the current project if they are adults (aged 20 years or older), reside in Mazandaran province, have a history of any kind of substance use, and have no severe mental difficulties that prevent them from answering the items in the questionnaires.
Exclusion criteria
The exclusion criteria for participants will be: having a mental disability, having psychiatry history like active bipolar disease, depression with psychosis, or schizophrenia, being deaf or mute, showing unwillingness to continue participating in the study, and not fully completing the questionnaires.
Questionnaires and data collection
Quantitative data will be collected utilizing sociodemographic variables and the PSAS, HPA-SAS, and SDS scales. The sociodemographic section will include questions on age, gender, occupation, duration of employment, and education. The PSAS comprises eight items to measure the perceived stigma towards individuals with substance use disorders. Initially developed and validated among patients undergoing treatment for substance use–related issues in the United States [ 88 ]. he items were adapted from a study conducted by Link and colleagues on perceived discrimination-devaluation processes, Content validity was established through review by stigma professionals in the substance use field the PSAS was related to adopted shame, self-concealment, adopted stigma, and depression [ 89 ]. The PSAS employs a four-point Likert scale ranging from “strongly disagree” to “strongly agree” for participants to rate their agreement or disagreement with each item. Scores range from 8 to 32, with higher scores indicating greater perceived stigma. The PSAS has demonstrated good reliability, with a Cronbach’s alpha of 0.71 and a reliability coefficient of 0.79 based on the test-retest method in American society [ 88 ]. In an Iranian study, the reliability of the PSAS was found to be 0.85, with a test-retest correlation coefficient of 0.81 [ 90 ].
The HPA-SAS consists of 10 items, with questions addressing the attitudes and/or views of health professionals toward people with SUD, their knowledge of addiction, and their training in substance use. The constructs of attitudes will focus on discrimination and acceptance towards people who use drugs. The HPA-SAS was developed utilizing a Likert scale format, with each item offering four response options: (1) strongly disagree (2), disagree (3), agree, and (4) strongly agree, resulting in total scores ranging from 10 to 40. The validity and reliability of the HPA-SAS were established through research conducted by a team of psychological counseling and medical care professionals. The overall Cronbach’s alpha of the original HPA-SAS has been reported as 0.79 [ 91 ]. In this study, the validity and reliability of the questionnaire were assessed prior to data collection with a sample of Iranian people who use drugs. The overall Cronbach’s alpha of the HPA-SAS was found to be 0.76, and the test–retest correlation coefficient of this scale was 0.74.
The seven-item SDS, which was created by Bogardus et al. (1925) [ 92 ] and then modified by Link et al. (1987) [ 89 ], measures the social distance that interviewees wish to keep toward a person with a particular condition (diverse social, ethnic, or racial backgrounds). This scale focuses on respondents’ willingness to engage in a relationship with someone who is dependent on illegal substances. In particular, it measures people’s willingness to take part in a variety of social contacts with a particular group. The SDS consists of seven items presented as multiple-choice questions, which assess social distance by probing the respondent’s willingness to engage in various social interactions with stigmatized individuals: These interactions include scenarios such as being a sub-lessee, neighbor, co-worker, spouse of a family member, caretaker of one’s child, and member of the same social group. Participants will be asked to rate their level of willingness or unwillingness for each item using a four-point Likert scale with the following options: (0) definitely willing [ 1 ], willing [ 2 ], unwilling, and [ 3 ] definitely unwilling. The total score ranges from 0 to 21; scores higher than the mean identify higher social distance. The overall Cronbach’s alpha of the original SDS is 0.75 [ 89 ]. The Iranian version of the SDS has found to have a Cronbach’s alpha value of 0.92. The test–retest reliability coefficient for the SDS was 0.89, and the content validity coefficient was 0.75 [ 90 ].
Data analysis
The data from the first phase of the study will be analyzed using SPSS Statistics Version 26.0 for Windows (IBM Inc., Armonk, NY, USA). In the cross-sectional phase, descriptive statistics will be applied to describe the sociodemographic factors and perceived stigma of addiction, experts’ attitudes toward people with SUD, and social distance. Univariate analytical statistics will be used to test the correlation between the sociodemographic variables and perceived stigma, experts’ attitudes toward people with SUD, and social distance. Variables with a correlation of p < 0.1 in the univariate analysis will be included in the multivariable logistic model. All statistical tests will be two-tailed, and a p -value < 0.05 will be considered statistically significant. To ensure data quality during this phase of the study, measures such as double data entry and range checks for data values will be implemented.
Phase 2: qualitative study
In Phase 2, an exploratory qualitative study will be conducted utilizing a conventional content analysis method to explore the experiences of people who use drugs regarding stigma and discrimination stemming from the community, health-care centers, or PATCs as a result of drug use. Additionally, this phase will aim to gain insight into healthcare providers’ perspectives on stigma against people who use drugs in greater detail. Given the objectives of the project’s qualitative phase, employing this method will enable the investigator to gain a comprehensive understanding of the situation, facilitating the clarification of the impact of stigma and discrimination on Iranian people who use drugs at PATCs.
Participants and sampling method
A purposive sampling approach will be used in the second phase of the study. The target population will consist of two groups of people, namely, those who have experienced drug use and staff members at PATCs. The first group of participants (people who use drugs) will be selected from those willing to participate in the quantitative phase of the study and will be based on the mean total score of the stigma experience, which will be collected in Phase 1 of the study. People with 10% upper and lower stigma experience scores will be selected as extreme cases, and will be retained for the next phase. We will seek to interview people with either a stigma or discrimination experience in order to collect more comprehensive information about their stigma experiences and its related factors. Efforts will be made to have variety in terms of gender, level of education, religion, age, socioeconomic situation, and the use of different types of drugs.
The second group of participants will consist of health-care workers and providers at PATCs. This sample will include agents from (i) PATC management, (ii) clinical and medical teams, (iii) health-care program teams and (iv)others according to the setting (e.g., finance). Health-care workers will be enlisted using purposive sampling methods. Four of them will be contacted through education programs with a specific focus on staff involved in drug treatment. The retained persons will be invited to register, and a member of the research team will be in touch to schedule an interview. Health-care workers in specific treatment centers will also receive direct invitations from the investigation team.
Data analysis will commence after the first interview, focusing on elucidating the intricacies and interactions among key concepts and categories derived from the exploration of the primary data. Consequently, the selection of participants will persist until theoretical saturation is achieved, ensuring a comprehensive understanding of the relationships between the study concepts and components [ 93 ]. In the current study, sampling will continue until the investigator determines that no further data can be garnered through data analysis and coding, signifying theoretical saturation. However, it is recommended by experts that a minimum of 12 participants be interviewed for a qualitative study to ensure a robust and comprehensive analysis [ 94 ].

Data collection
Data will be collected by two methods: in-depth interviews with individuals with SUDs and focus group discussions with PATC staff members.
Semi-structured, in-depth interviews
Individual, in-depth, semi-structured interviews featuring open-ended questions will be employed to gather data. These interviews will focus on exploring participants’ perspectives and experiences related to stigma and discrimination against individuals with (SUDs within healthcare settings. The target group for this part of the study will consist of people who use drugs who have been referred to PATCs in Mazandaran, Iran. Before the qualitative phase of the study, the interview protocol questions will be prepared based on the results of the first phase of the study as well as the literature review. Interviews will be held in locations, such as clinics, where respondents will feel safe and relaxed. All individual in-depth interviews will be recorded using a digital tape recorder after the applicant’s permission. In addition to the audio recordings, the interviewer will take notes. If participants decline to be audio-recorded, only notes will be employed for data gathering. Furthermore, non-verbal cues, such as facial expressions, tone of voice, and the respondents’ state, will also be noted by the interviewer, together with the date and place of the interview.
All interviews will be conducted by the first author of this study, who is familiar with qualitative research methods and the topic, and who has conducted similar studies on addiction,. Participants will be encouraged to discuss their experiences related to strategies to reduce addiction-related stigma and discrimination in public addiction treatment centers. Further, they will be encouraged to discuss sociocultural and ecological components that might have had an effect on the level of using these strategies in this regard.
The interviews will be focused on the following three main questions:
How was the experience with stigma toward and discrimination in health-care settings?
What strategy and procedure have they applied to reduce and cope with stigma and discrimination in health-care settings?
How have the strategies and procedures affected their coping strategies in this regard?
Based on the responses to these questions, follow-up questions will be asked. After each question, participants will be invited to explain more thoroughly their answer, by probing questions such as “What do you mean?” or “can you explain this more”.
Interviews will be performed during a single meeting with each participant and is estimated to last between 40 and 60 min, although this can differ slightly based on the experiences of each participant. The investigator will start with explaining the significance of the study in order to gain their confidence. All interview questions will be reviewed after the first interview, and all interviews will be taped. Data collection will be continued until saturation is reached.
Focus group discussions
Following semi-structured interviews, the principal researcher (first author), who is an expert in qualitative studies, an expert in qualitative studies, will conduct focus group discussions with staff members at Patients with Substance Use Disorders Treatment Centers (PATCs), which comprise the second target group of this phase of the study. These focus group discussions aim to validate the emerging themes from the individual interviews and gain deeper insights into the identified themes. The focus group discussions will be guided by the two main research questions: (i) What is providers’ understanding of stigma towards and discrimination against persons with SUDs? and [ 2 ] What are the providers’ opinions regarding a response to stigma and discrimination? Furthermore, more detailed investigative questions will be incorporated, such as: What types of SUDs do your clients typically present with? Are there any other community-level factors that could influence experiences of stigma and discrimination against individuals with SUDs?
Immediately following data collection, the coding process will be initiated, and the data will be analyzed. The main themes will be identified using a conventional content analysis method of Graneheim and Lundman [ 95 ], in which themes and subthemes are identified to reveal participants’ perceptions and experiences toward stigma and discrimination against Iranian people who use drugs at PATCs. This process will employ inductive reasoning, which introduces concepts and categories via a detailed exploration of the data by the researcher.
In Graneheim and Lundman’s method, qualitative content analysis addresses the obvious content of an interview, along with explanations of content that can be construed or added from the interview but are not obviously detailed in the transcript [ 95 ]. Further, coding classifications are derived directly from the transcription data. Without laying on preset themes or prior theoretical opinions to categorize extracted codes from interviews, the conventional content analysis method is a suitable technique for advancing coding categorizations from the raw interview transcripts.
In this method, data analysis begins with a comprehensive reading of the entire text to ensure a thorough understanding. Subsequently, the text is examined word by word to extract codes, initially identifying specific words that may encapsulate the main concepts. These texts are derived from notes documenting the initial opinions of the interviewees and the preliminary analysis conducted. Codes that are indicative of more than one main thought are tagged and then categorized based on their dissimilarities and similarities. The greatest benefit of a conventional content analysis is attaining data directly from the study without imposing preplanned and defined categories, themes, or theories. However, one problem with this kind of analysis is that it interjects with other qualitative methods (i.e., grounded theory or phenomenology). While these approaches share similarities with initial analysis, they are emphasized for their relevance to theory advancement. Additionally, they hold significance for model development. To evaluate the trustworthiness of the results in this phase of the study, four criteria —reliability, portability, credibility, and verifiability— will be employed [ 96 ]. MAXQDA software will be used for data processing.
Phase three: integration of quantitative and qualitative data and the development of strategies
In this phase, cultural evidence-based strategies aimed at reducing stigma and discrimination associated with substance use of Iranian people at PATCs will be developed This will involve integrating insights from the literature review, the findings of the preceding study phases, and input from experts. The target group for this aspect of the study will comprise PATC experts residing in Mazandaran, Iran.
Upon completion of the second phase of the study, the quantitative and qualitative results will be merged to glean additional insights that will inform the design and implementation of appropriate strategies to mitigate stigma and discrimination against individuals with SUDs at PATCs. Three techniques can be employed to integrate the quantitative and qualitative findings: combining the data into a discussion, utilizing a matrix for combination, or employing a side-by-side display and transformation. n this study, the data will be combined into a discussion format. Some researchers often commence this approach with a section outlining the quantitative findings, followed by a section detailing the qualitative findings. Alternatively, researchers may present the quantitative findings while substantiating claims with quotes extracted from them. Another less common technique involves initially presenting the quantitative results and subsequently confirming and validating them with descriptive qualitative findings [ 97 , 98 ].
To develop strategies for reducing stigma and discrimination against people who use drugs at PATCs, the research team will start with formulating guidelines after a comprehensive review of the available literature. Systematic review and interventional studies will be conducted to find approaches. The search will encompass English-language databases (including Cochrane Library, APA PsycNET, MEDLINE, Web of Science, Embase, Scopus, ProQuest) as well as Persian databases (such as Magiran, Irandoc, SID, and Barakat). No restrictions will be imposed, particularly with regard to publication dates, to ensure comprehensive coverage of relevant studies. A uniform search strategy will be applied across all databases, utilizing the intersection of three fields via the Boolean AND operator. To define search terms, the Medical Subject Headings (MeSH) dictionary will be referenced. Upon identification of relevant documents, their quality will be assessed using the GRADE approach, followed by evidence analysis. Insights gleaned from the literature review will also be incorporated. Subsequently, the recommended strategies developed will be offered to Nominal Group Technique (NGT) experts.
NGT will be applied will be employed to devise and implement effective strategies aimed at diminishing stigma and discrimination against individuals with SUDs at PATCs. NGT is a structured, group-based method utilized to achieve consensus. Participants are encouraged to independently generate viewpoints based on predetermined and organized questions facilitated by a moderator [ 99 ]. To initiate the NGT process, primary strategies will be extracted from the findings of the first and second phases of the study, in addition to insights gathered from a literature review and examination of relevant rules and regulations A meeting will then be held with the experts who must meet the inclusion criteria of being residents of Mazandaran, Iran, possessing a minimum of one year of relevant work experience, having comprehensive familiarity with Iranian culture and customs, and being employed in a clinic associated with the treatment of people who use drugs. During this meeting, specialists will be invited to share their opinions on the developed strategies in relation to the key study questions, with all ideas and suggestions being meticulously recorded. Subsequently, these suggestions will be organized and prioritized to formulate consensus-driven strategies for effectively reducing stigma and discrimination against Iranian individuals with SUDs.
Ethical approval
The Ethics Committee of the Mazandaran University of Medical Sciences in Mazandaran, Sari, Iran, has approved the protocol for the present study [code number: IR.MAZUMS.REC.1401.192]. Informed written consent will be obtained from all participants during the quantitative and qualitative stages. Participants will be assured of the confidentiality of their data and identities. Additionally, they will be informed that they have the right to withdraw from the project at any phase of the intervention, and that their decision to refuse participation at any time will not impact or alter the quality of services provided to them.
The study is still ongoing, and no results have yet been generated. We will wait until the completion of our first data collection before disseminating any findings.
This article outlines the protocol for a mixed-method study aimed at identifying and formulating appropriate strategies to mitigate addiction-related stigma and discrimination at PATCs. The study will offer comprehensive insights into the stigma encountered by a cohort of Iranian people who use drugs and the factors influencing their experiences. The findings of this study will be utilized to develop and implement culturally tailored strategies geared towards reducing stigma and discrimination associated with substance use among Iranian people who use drugs attending PATCs.
While stigma and discrimination linked with drug addiction is a global concern, their nature and expression are contingent upon the religious, social, and cultural frameworks prevalent in various societies. Operating as a multilevel phenomenon, stigma arises when harm resulting from unfavorable status, labeling, or discrimination transpires within a power structure that perpetuates and reinforces social inequalities among those labeled [ 100 ]. Stigma toward substance use can profoundly impact an individual’s social and personal connections, often resulting in feelings of worthlessness. Such stigma may provoke negative responses and behaviors from various organizations and individuals towards the affected person [ 101 , 102 ]. These behaviors can impede access to treatment for individuals with substance use disorders. Moreover, they contribute to social, financial, and health discrimination within these communities, fostering the perception that individuals with SUDs are undeserving of the opportunity to address their condition [ 103 ].
Stigma significantly impacts the spectrum of care for individuals with SUDs, influencing aspects such as treatment seeking, preference, maintenance, and adherence, consequently leading to poorer health outcomes within this population or ever, stigma may exacerbate disparities in accessing medical and health services, as individuals with SUDs may be hesitant to pursue and adhere to health-oriented measures [ 104 ].
Studies evaluating the stigma experiences of persons with SUDs are mainly qualitative in nature [ 21 , 52 , 62 , 98 , 105 , 106 ]. The present study will be one of the few studies addressing addiction-related stigma in Iran that applies a mixed-methods technique to identify suitable strategies to reduce addiction-related stigma and discrimination at PATCs from the perspective of Iranian people who use drugs. It is expected that the current work, by using quantitative and qualitative methods, will offer valid data regarding suitable cultural strategies to reduce stigma against persons with SUDs at health-care and treatment centers.
The findings of the current study hold potential significance for healthcare specialists and policymakers shedding light on the pivotal role of cultural strategies in mitigating stigma against individuals with SUDs within healthcare and treatment settings employing a culturally sensitive approach Furthermore, the study aims to elucidate the needs of individuals with SUDs and provide insights into the factors influencing addiction-related stigma that require attention. Effective strategies emerging from this research may encompass interventions geared towards enhancing the health outcomes of Iranian people who use drugs and their families, as well as those from other nationalities and countries sharing similar cultural contexts with Iran. Additionally, the study’s findings are anticipated to inform stigma-reduction education and healthcare support initiatives tailored to the Iranian population, underpinned by a culture-based approach.
Potential strengths of the study
This study has several advantages. The results will potentially fill some of the gaps in research on people with SUDs who encounter stigma and discrimination at PATCs thus holding significant clinical implications. By employing a mixed-methods approach, this study facilitates the integration of diverse approaches and methodologies. The collection of both qualitative and quantitative data will provide a comprehensive understanding of. People who use drugs’ experiences of stigma and discrimination at PATCs. Moreover, the qualitative component of the study involves various participants directly or indirectly associated with this phenomenon, including individuals with SUDs and staff/clinicians. Conducting interviews with substance users and clinicians will enable a deeper understanding of how the phenomenon is perceived by those directly affected by stigma/discrimination, as well as by individuals closely involved in the patients’ daily lives and clinicians, who play a crucial role in both the phenomenon and its treatment.
Potential limitations of the study
The researchers acknowledge several limitations in the current study although the developed strategies will be evaluated upon achievement to ascertain their suitability and effectiveness, detailed descriptions will be necessary to design appropriate interventions and allow for generalization in similar contexts. One limitation is related to the sampling, which will be conducted in only one province in Iran. To mitigate this weakness, we will try to use maximum variation in the study phases. Another limitation is the possibility that the participants will not cooperate and drop out before the end of the study. Additionally, the scarcity of research and literature reviews regarding the stigma experienced by this population at PATCs poses a challenge. Furthermore, there is limited available data on how stigma varies among different subgroups, such as based on gender, race, religion, or socioeconomic status. These limitations will be considered during the interpretation of the study results and may influence the generalizability of findings to broader contexts.
The stigma and discrimination faced by individuals’ with SUDs experience persist not only in the community but also within PATCs, and medical settings. This Stigmatization adversely affects the accessibility and acceptability of care, as the lack of anonymity limits the willingness of this population to seek SUD treatment. The present study aims to provide comprehensive insights into the development of appropriate strategies to reduce addiction-related stigma and discrimination at PATCs. By incorporating evidence-based practice principles, insights from people who use drugs’ experiences, and input from PATC staff, these strategies can offer valuable guidance for healthcare professionals, policymakers, and managers seeking to enhance the quality of care for individuals with a history of drug use worldwide. Furthermore, the strategies developed may serve as a blueprint for adapting interventions for patients with SUDs in various settings, including other healthcare treatment centers, clinics, and within the broader public community.
Data availability
Not applicable.
Abbreviations
substance use disorder
public addiction treatment centers
Perceived Stigma of Addiction Scale
Professional’s Discrimination, Acceptance, Attitude, and Training toward Substance Abusers
Social Distance Scale
focus group discussions
screening, brief intervention and referral to treatment
in-depth interviews
nominal group technique
standard deviation
Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, et al. Epidemiology of DSM-5 alcohol use disorder: results from the national epidemiologic survey on Alcohol and related conditions III. JAMA Psychiatry. 2015;72(8):757–66.
Article PubMed PubMed Central Google Scholar
Grant BF, Saha TD, Ruan WJ, Goldstein RB, Chou SP, Jung J, et al. Epidemiology of DSM-5 drug use disorder: results from the national epidemiologic survey on Alcohol and related Conditions–III. JAMA Psychiatry. 2016;73(1):39–47.
Hasin DS, Kerridge BT, Saha TD, Huang B, Pickering R, Smith SM, et al. Prevalence and correlates of DSM-5 cannabis use disorder, 2012–2013: findings from the National Epidemiologic Survey on Alcohol and related Conditions–III. Am J Psychiatry. 2016;173(6):588–99.
Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H, Jung J, et al. Nonmedical prescription opioid use and DSM-5 nonmedical prescription opioid use disorder in the United States. J Clin Psychiatry. 2016;77(6):12855.
Article Google Scholar
Council WB. Strategic plan. New South Wales Aboriginal Land Council; 2013.
Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: a systematic review and meta-analysis. Soc Sci Med. 2010;71(12):2150–61.
Article PubMed Google Scholar
Hasin DS, Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H, et al. Prevalence of marijuana use disorders in the United States between 2001–2002 and 2012–2013. JAMA Psychiatry. 2015;72(12):1235–42.
Semple SJ, Grant I, Patterson TL. Utilization of drug treatment programs by methamphetamine users: the role of social stigma. Am J Addictions. 2005;14(4):367–80.
Link BG, Phelan JC. Conceptualizing stigma. Ann Rev Sociol. 2001;27(1):363–85.
Ahern J, Stuber J, Galea S. Stigma, discrimination and the health of illicit drug users. Drug Alcohol Depend. 2007;88(2–3):188–96.
Latkin C, Davey-Rothwell M, Yang J-y, Crawford N. The relationship between drug user stigma and depression among inner-city drug users in Baltimore, MD. J Urb Health. 2013;90:147–56.
Link BG, Struening EL, Rahav M, Phelan JC, Nuttbrock L. On stigma and its consequences: evidence from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. J Health Soc Behav. 1997:177–90.
Luoma JB, Kohlenberg BS, Hayes SC, Bunting K, Rye AK. Reducing self-stigma in substance abuse through acceptance and commitment therapy: Model, manual development, and pilot outcomes. Addict Res Theory. 2008;16(2):149–65.
Paquette CE, Syvertsen JL, Pollini RA. Stigma at every turn: health services experiences among people who inject drugs. Int J Drug Policy. 2018;57:104–10.
Formigoni MLO. A intervençäo breve na dependencia de drogas. A intervençäo breve na dependencia de drogas1992. p. 210-.
Palm J. Moral concerns-treatment staff and user perspectives on alcohol and drug problems. Kriminologiska institutionen; 2006.
Corrigan P. How stigma interferes with mental health care. Am Psychol. 2004;59(7):614.
Cheetham A, Picco L, Barnett A, Lubman DI, Nielsen S. The impact of stigma on people with opioid use disorder, opioid treatment, and policy. Subst Abuse Rehabilitation. 2022:1–12.
Madras BK, Ahmad NJ, Wen J, Sharfstein JS. Improving access to evidence-based medical treatment for opioid use disorder: strategies to address key barriers within the treatment system. NAM perspectives. 2020;2020.
Drabish K, Theeke LA. Health impact of stigma, discrimination, prejudice, and bias experienced by transgender people: a systematic review of quantitative studies. Issues Ment Health Nurs. 2022;43(2):111–8.
Garpenhag L, Dahlman D. Perceived healthcare stigma among patients in opioid substitution treatment: a qualitative study. Subst Abuse Treat Prev Policy. 2021;16(1):1–12.
Speerforck S, Schomerus G. Reducing substance use stigma in health care. The stigma of substance use disorders. 2022:232.
Babor TF, Del Boca F, Bray JW. Screening, brief intervention and referral to treatment: implications of SAMHSA’s SBIRT initiative for substance abuse policy and practice. Addiction. 2017;112:110–7.
Rahm AK, Boggs JM, Martin C, Price DW, Beck A, Backer TE, et al. Facilitators and barriers to implementing screening, brief intervention, and referral to treatment (SBIRT) in primary care in integrated health care settings. Substance Abuse. 2015;36(3):281–8.
Matheson C, Pflanz-Sinclair C, Almarzouqi A, Bond CM, Lee AJ, Batieha A, et al. A controlled trial of screening, brief intervention and referral for treatment (SBIRT) implementation in primary care in the United Arab Emirates. Prim Health care Res Dev. 2018;19(2):165–75.
Levy SJ, Williams JF, Ryan SA, Gonzalez PK, Patrick SW, Quigley J et al. Substance use screening, brief intervention, and referral to treatment. Pediatrics. 2016;138(1).
Aldridge A, Linford R, Bray J. Substance use outcomes of patients served by a large US implementation of screening, brief intervention and referral to treatment (SBIRT). Addiction. 2017;112:43–53.
Graham LJ, Davis AL, Cook PF, Weber M. Screening, brief intervention, and referral to treatment in a rural Ryan White Part C HIV clinic. AIDS Care. 2016;28(4):508–12.
Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, brief intervention, and referral to treatment (SBIRT): toward a public health approach to the management of substance abuse. Focus. 2011;9(1):130–48.
Al-Ansari B, Noroozi A, Thow A-M, Day CA, Mirzaie M, Conigrave KM. Alcohol treatment systems in muslim majority countries: Case study of alcohol treatment policy in Iran. Int J Drug Policy. 2020;80:102753.
Crisp A, Gelder M, Goddard E, Meltzer H. Stigmatization of people with mental illnesses: a follow-up study within the changing minds campaign of the Royal College of Psychiatrists. World Psychiatry. 2005;4(2):106.
PubMed PubMed Central Google Scholar
Allen B, Harocopos A, Chernick R. Substance use stigma, primary care, and the New York State prescription drug monitoring program. Behav Med. 2020;46(1):52–62.
Tran BX, Vu PB, Nguyen LH, Latkin SK, Nguyen CT, Phan HTT, et al. Drug addiction stigma in relation to methadone maintenance treatment by different service delivery models in Vietnam. BMC Public Health. 2016;16:1–9.
Bielenberg J, Swisher G, Lembke A, Haug NA. A systematic review of stigma interventions for providers who treat patients with substance use disorders. J Subst Abuse Treat. 2021;131:108486.
Article CAS PubMed Google Scholar
Chang J, Dubbin L, Shim J. Negotiating substance use stigma: the role of cultural health capital in provider–patient interactions. Sociol Health Illn. 2016;38(1):90–108.
Salamat S, Hegarty P, Patton R. Same clinic, different conceptions: drug users’ and healthcare professionals’ perceptions of how stigma may affect clinical care. J Appl Soc Psychol. 2019;49(8):534–45.
Van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Healthcare professionals’ regard towards working with patients with substance use disorders: comparison of primary care, general psychiatry and specialist addiction services. Drug Alcohol Depend. 2014;134:92–8.
Sapag JC, Sena BF, Bustamante IV, Bobbili SJ, Velasco PR, Mascayano F, et al. Stigma towards mental illness and substance use issues in primary health care: challenges and opportunities for Latin America. Glob Public Health. 2018;13(10):1468–80.
Corrigan P, Schomerus G, Shuman V, Kraus D, Perlick D, Harnish A, et al. Developing a research agenda for understanding the stigma of addictions part I: lessons from the mental health stigma literature. Am J Addictions. 2017;26(1):59–66.
McGinty E, Pescosolido B, Kennedy-Hendricks A, Barry CL. Communication strategies to counter stigma and improve mental illness and substance use disorder policy. Psychiatric Serv. 2018;69(2):136–46.
Corrigan PW, Rao D. On the self-stigma of mental illness: stages, disclosure, and strategies for change. Can J Psychiatry. 2012;57(8):464–9.
Wong EC, Collins RL, Cerully JL, Yu JW, Seelam R. Effects of contact-based mental illness stigma reduction programs: age, gender, and Asian, latino, and White American differences. Soc Psychiatry Psychiatr Epidemiol. 2018;53:299–308.
İnan FŞ, Günüşen N, Duman ZÇ, Ertem MY. The impact of mental health nursing module, clinical practice and an anti-stigma program on nursing students’ attitudes toward mental illness: a quasi-experimental study. J Prof Nurs. 2019;35(3):201–8.
Shim R, Rust G. Primary care, behavioral health, and public health: partners in reducing mental health stigma. American Public Health Association; 2013. pp. 774–6.
Bonnevie E, Kaynak Ö, Whipple CR, Kensinger WS, Stefanko M, McKeon C, et al. Life unites us: a novel approach to addressing opioid use disorder stigma. Health Educ J. 2022;81(3):312–24.
Khenti A, Mann R, Sapag JC, Bobbili SJ, Lentinello EK, Van Der Maas M, et al. Protocol: a cluster randomised control trial study exploring stigmatisation and recovery-based perspectives regarding mental illness and substance use problems among primary healthcare providers across Toronto, Ontario. BMJ open. 2017;7(11):e017044.
Mehta N, Clement S, Marcus E, Stona A-C, Bezborodovs N, Evans-Lacko S, et al. Evidence for effective interventions to reduce mental health-related stigma and discrimination in the medium and long term: systematic review. Br J Psychiatry. 2015;207(5):377–84.
Article CAS PubMed PubMed Central Google Scholar
Collins RL, Wong EC, Cerully JL, Schultz D, Eberhart NK. Interventions to reduce mental health stigma and discrimination: a literature review to guide evaluation of California’s mental health prevention and early intervention initiative. Rand Health Q. 2013;2(4).
Lancaster K, Seear K, Ritter A. Reducing stigma and discrimination for people experiencing problematic alcohol and other drug use. Brisbane: Queensland Mental Health Commission. 2017;118:1-118.
Girma E, Ketema B, Mulatu T, Kohrt BA, Wahid SS, Heim E, et al. Mental health stigma and discrimination in Ethiopia: evidence synthesis to inform stigma reduction interventions. Int J Mental Health Syst. 2022;16(1):1–18.
Khazaee-Pool M, Pashaei T, Nouri R, Taymoori P, Ponnet K. Understanding the relapse process: exploring Iranian women’s substance use experiences. Subst Abuse Treat Prev Policy. 2019;14(1):1–11.
Ghasemi E, Rajabi F, Negarandeh R, Vedadhir A, Majdzadeh R. HIV, migration, gender, and drug addiction: a qualitative study of intersectional stigma towards Afghan immigrants in Iran. Health Soc Care Commun. 2022;30(5):e1917–25.
Taghva A, Farsi Z, Javanmard Y, Atashi A, Hajebi A, Noorbala AA. Strategies to reduce the stigma toward people with mental disorders in Iran: stakeholders’ perspectives. BMC Psychiatry. 2017;17:1–12.
Farhoudian A, Baldacchino A, Clark N, Gerra G, Ekhtiari H, Dom G, et al. COVID-19 and substance use disorders: recommendations to a comprehensive healthcare response. An international society of addiction medicine practice and policy interest group position paper. Basic Clin Neurosci. 2020;11(2):133.
CAS PubMed PubMed Central Google Scholar
Mirzaei S, Yazdi-Feyzabadi V, Mehrolhassani MH, Nakhaee N, Oroomiei N. Setting the policy agenda for the treatment of substance use disorders in Iran. Harm Reduct J. 2022;19(1):1–10.
Article CAS Google Scholar
Biancarelli DL, Biello KB, Childs E, Drainoni M, Salhaney P, Edeza A, et al. Strategies used by people who inject drugs to avoid stigma in healthcare settings. Drug Alcohol Depend. 2019;198:80–6.
Earnshaw VA. Stigma and substance use disorders: a clinical, research, and advocacy agenda. Am Psychol. 2020;75(9):1300.
Moore KE, Johnson JE, Luoma JB, Taxman F, Pack R, Corrigan P, et al. A multi-level intervention to reduce the stigma of substance use and criminal involvement: a pilot feasibility trial protocol. Health Justice. 2023;11(1):1–13.
Bayat A-H, Mohammadi R, Moradi-Joo M, Bayani A, Ahounbar E, Higgs P, et al. HIV and drug related stigma and risk-taking behaviors among people who inject drugs: a systematic review and meta-analysis. J Addict Dis. 2020;38(1):71–83.
Broman MJ, Pasman E, Brown S, Lister JJ, Agius E, Resko SM. Social support is associated with reduced stigma and shame in a sample of rural and small urban adults in methadone treatment. Addict Res Theory. 2023;31(1):37–44.
Williams LD, Mackesy-Amiti ME, Latkin C, Boodram B. Drug use-related stigma, safer injection norms, and hepatitis C infection among a network-based sample of young people who inject drugs. Drug Alcohol Depend. 2021;221:108626.
Noroozi A, Conigrave KM, Mirrahimi B, Bastani P, Charkhgard N, Salehi M, et al. Factors influencing engagement and utilisation of opium tincture-assisted treatment for opioid use disorder: a qualitative study in Tehran, Iran. Drug Alcohol Rev. 2022;41(2):419–29.
Khazaee-Pool M, Moeeni M, Ponnet K, Fallahi A, Jahangiri L, Pashaei T. Perceived barriers to methadone maintenance treatment among Iranian opioid users. Int J Equity Health. 2018;17:1–10.
Razaghi E, Farhoudian A, Pilevari A, Noroozi A, Hooshyari Z, Radfar R et al. Identification of the socio-cultural barriers of drug addiction treatment in Iran. Heliyon. 2023;9(5).
Jafari S, Movaghar AR, Craib K, Baharlou S, Mathias R. Socio-cultural factors associated with the initiation of opium use in Darab, Iran. Int J Mental Health Addict. 2009;7:376–88.
Rasekh K, Allapanazadeh T. Social factors affecting on drugs abuse:(Slum dwellers in Shiraz-Iran). Sociol Stud Youth. 2012;3(7):25–42.
Google Scholar
Kazemi F, Motalebi SA, Mirzadeh M, Mohammadi F. Predisposing factors for substance abuse among elderly people referring to Qazvin addiction treatment centers, Iran (2017). J Inflamm Dis. 2018;22(5):26–35.
Shirinzadeh-Dastgiri S, Alamikhah M, Saed O, Kazemini T. Comparison of patterns of substance abuse disorders in urban and rural population. Zahedan J Res Med Sci. 2011;13(1).
Ghaemi F, Samsam Shariat S, Asef Vaziri K, Balouchi D. Relationship between Extravertion, Neuroticism, Forgiveness and Islamic Coping Strategies with Happiness in College Students of Ahvaz Universities in 1387. Knowl Res Appl Psychol. 2008;38:93–104.
Agahi Z, Zarrani F. Cultural contexts of substance abuse disorders in Iran: qualitative meta-synthesis. Clin Excellence. 2021;11(1):24–42.
Mirfardi A, Shahriari M. Ethnographic Study of Folk norms and recommendations encouraging drug Use (Case of Arab people of Ahvaz City). Sci Q Res Addict. 2017;11(43):105–26.
Ghanbari A, Rabiei K. Etiology of changes in pattern of narcotic consumption in Iran. Soci-cultu Sreategy. 2015;4(15):243–69.
Hajli A, Zakariaey MA, Hojati Kermani S. Iranians’ attitude towards drug abuse. J Social Probl Iran. 2010;1(2):81–111.
Mohammadi K, editor. Editor investigating the causes of changing the pattern of drug use from traditional (low risk) to industrial (high risk) in Iran (Lorestan and Isfahan provinces). Sil Inva Conf (University Jihad); 2011.
Moddabernia M, Mirhosseini S, Tabari R. Factors influencing addiction in people of 15 to 30 years of age: a qualitative study. J Guilan Univ Med Sci. 2013;22(87):70–7.
SediqSarvestani R, Qaderi S. Norms facilitating drug use (opium and the like) among ethnic subcultures in Iran. Discip Knowl. 2008;2(39):85–103.
Ezatpour EE-d, Rahmani K, Bidarpoor F. Investigation of drug use causes in young persons of Sanandaj using Respondent Driven Sampling. Shenakht J Psychol Psychiatry. 2018;5(3):12–21.
Ghaderi S, Mohseni Tabrizi A. A qualitative study in recognizing the norms facilitating the use of addictive substances among the ethnic subcultures of Iran Title. Study Soc Issues Iran. 2010;1(4):37–54.
Shahraki G, Sedaghat Z, Fararouei M. Family and social predictors of substance use disorder in Iran: a case-control study. Subst Abuse Treat Prev Policy. 2019;14:1–8.
Mirzakhani F, Khodadadi Sangdeh J, Nabipour AR. Marital factors affecting addiction among Iranian women: a qualitative study. J Subst Use. 2020;25(1):28–33.
Etesam F, Assarian F, Hosseini H, Ghoreishi FS. Stigma and its determinants among male drug dependents receiving methadone maintenance treatment. 2014.
Mokri A. Brief overview of the status of drug abuse in Iran. 2002.
Zarghami M. Iranian common attitude toward opium consumption. Iran J Psychiatry Behav Sci. 2015;9(2).
Creswell JW. Controversies in mixed methods research. Sage Handb Qualitative Res. 2011;4(1):269–84.
Johnson RB, Onwuegbuzie AJ. Mixed methods research: a research paradigm whose time has come. Educational Researcher. 2004;33(7):14–26.
Nejati B, Lin C-C, Imani V, Browall M, Lin C-Y, Broström A, et al. Validating patient and physician versions of the shared decision making questionnaire in oncology setting. Health Promotion Perspect. 2019;9(2):105.
Matsumoto A, Santelices C, Lincoln AK. Perceived stigma, discrimination and mental health among women in publicly funded substance abuse treatment. Stigma Health. 2021;6(2):151.
Luoma JB, O’Hair AK, Kohlenberg BS, Hayes SC, Fletcher L. The development and psychometric properties of a new measure of perceived stigma toward substance users. Subst Use Misuse. 2010;45(1–2):47–57.
Link BG, Cullen FT, Frank J, Wozniak JF. The social rejection of former mental patients: understanding why labels matter. Am J Sociol. 1987;92(6):1461–500.
Ranjbar Kermani F, Mazinani R, Fadaei F, Dolatshahi B, Rahgozar M. Psychometric properties of the Persian version of social distance and dangerousness scales to investigate stigma due to severe mental illness in Iran. Iran J Psychiatry Clin Psychol. 2015;21(3):254–61.
Gotay A. Health Professionals’ Attitude towards Substance Abusers: A Part of the Health Professionals’ Value and Belief System Which Prevails in Society. 2014.
BOGARDUS ES. Measuring social distance./. appl. Social; 1925.
Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18(1):59–82.
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–12.
Shenton AK. Strategies for ensuring trustworthiness in qualitative research projects. Educ Inform. 2004;22(2):63–75.
Creswell JW, Clark VLP. Designing and conducting mixed methods research. Sage; 2017.
Plano Clark VL, Garrett AL, Leslie-Pelecky DL. Applying three strategies for integrating quantitative and qualitative databases in a mixed methods study of a nontraditional graduate education program. Field Methods. 2010;22(2):154–74.
MacPhail A. Nominal group technique: a useful method for working with young people. Br Edu Res J. 2001;27(2):161–70.
Link BG, Phelan JC. Stigma and its public health implications. Lancet. 2006;367(9509):528–9.
Zissi A. Social stigma in mental illness: A review of concepts, methods and empirical evidence. Psychiatrike = Psychiatriki. 2021.
Bos AE, Pryor JB, Reeder GD, Stutterheim SE, Stigma. Advances in theory and research. Basic Appl Soc Psychol. 2013;35(1):1–9.
Strathdee S, Shoptaw S, Dyer T, Quan V, Aramrattana A. Substance Use Scientific Committee of the HIVPTN. Towards combination HIV prevention for injection drug users: addressing addictophobia, apathy and inattention. Curr Opin HIV AIDS. 2012;7(4):320–5.
Courtwright AM. Justice, stigma, and the new epidemiology of health disparities. Bioethics. 2009;23(2):90–6.
Yang LH, Wong LY, Grivel MM, Hasin DS. Stigma and substance use disorders: an international phenomenon. Curr Opin Psychiatry. 2017;30(5):378–88.
Mora-Ríos J, Ortega-Ortega M, Medina-Mora ME. Addiction-related stigma and discrimination: a qualitative study in treatment centers in Mexico City. Subst Use Misuse. 2017;52(5):594–603.
Download references
Acknowledgements
The authors are thankful for the support of the Mazandaran University of Medical Sciences.
No external funding sources were provided for this manuscript.
Author information
Authors and affiliations.
Department of Health Education and Promotion, School of Health, Health Sciences Research Center, Mazandaran University of Medical Sciences, Sari, Iran
Maryam Khazaee-Pool & Seyed Abolhassan Naghibi
Department of Health Promotion and Education, School of Health, Kermanshah University of Medical Sciences, Kermanshah, Iran
Tahereh Pashaei
Department of Communication Sciences, imec-mict-Ghent University, Ghent, Belgium
Koen Ponnet
You can also search for this author in PubMed Google Scholar
Contributions
MK designed the project, and will collect and analyze the data. Mk wrote the first draft of this manuscript. TP and SAN will participate in the analyses of data. MK and KP critically revised the final version of this article. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Maryam Khazaee-Pool or Tahereh Pashaei .
Ethics declarations
Ethics approval.
The study procedure was approved by the Medical Ethics Committee of Mazandaran University of Medical Sciences [Grant NO: 18008; Ethical code number: IR.MAZUMS.REC.1401.192].
Competing interests
The authors declare that they have no competing interests.
Informed consent statement
The authors have agreed on the content of the manuscript.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Khazaee-Pool, M., Naghibi, S.A., Pashaei, T. et al. Developing practical strategies to reduce addiction-related stigma and discrimination in public addiction treatment centers: a mixed-methods study protocol. Addict Sci Clin Pract 19 , 40 (2024). https://doi.org/10.1186/s13722-024-00472-8
Download citation
Received : 08 August 2023
Accepted : 06 May 2024
Published : 16 May 2024
DOI : https://doi.org/10.1186/s13722-024-00472-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Addiction-related stigma
- Addiction-related discrimination
- Addiction treatment centers
- Mixed-methods study
Addiction Science & Clinical Practice
ISSN: 1940-0640
- Submission enquiries: [email protected]
- General enquiries: [email protected]
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Managing Substance Use Disorders
- Health Equity
- Data Resources
- Additional HHS Resources
- Overdose Prevention Resources
- Management and Treatment of Pain
- Clinical Practice Guideline at a Glance
- Clinical Care and Treatment
- Health Care Provider Toolkits
- Electronic CDS Tools for Opioids
- Strategies and Partnerships
- Resources for Public Health Professionals
- Journal Articles
- MMWR Articles
- Guides and Meeting Reports
- Related Publications
- Overdose Data to Action
- Drug-Free Communities (DFC)
Treatment of Substance Use Disorders
- Millions of Americans have a substance use disorder (SUD), and it remains an important health issue in our country.
- In 2022, more than one in six Americans aged 12 or older reported experiencing a SUD.
- With effective treatment, recovery is possible for everyone. There is strength in getting help.

What is an SUD?
A substance use disorder (SUD) is a treatable, chronic disease characterized by a cluster of cognitive, behavioral, and physiological symptoms indicating that the individual continues using the substance despite significant substance-related problems. 1 In 2022, more than one in six Americans aged 12 or older reported experiencing a SUD. 2
SUDs can lead to significant problems in all aspects of a person's life. Patterns of symptoms resulting from substance use (drugs or alcohol) can help a doctor diagnose a person with a SUD or SUDs and connect them to appropriate treatment.
For certain drug types, some symptoms are less prominent, and in some cases, not all symptoms apply. For example, withdrawal symptoms are not specified for inhalant use.
SUDs can range in severity from mild to severe and can affect people of any race, gender, income level, or social class. A SUD can be applied to the following types of drugs: 1
- Hallucinogens
- Opioids (Prescription and Illegal)
- Sedatives, hypnotics, or anxiolytics
- Stimulants and Psychostimulants
- Tobacco (nicotine)
- Other (unknown) substance
Treatment and recovery options
Addiction is a disease, not a character flaw. People experiencing SUDs have trouble controlling their drug use even though they know drugs are harmful.
Overcoming an SUD is not as simple as resisting the temptation to take drugs. Recovery may involve medication to help with cravings and withdrawal as well as different forms of therapy. It may even require checking into a rehabilitation facility.
Addiction is a treatable disease
Like many other chronic conditions, treatment is available for substance use disorders. While no single treatment method is right for everyone, recovery is possible, and help is available for patients with SUDs.
Evidence-based guidelines can assist doctors with choosing the right treatment options. These guidelines help evaluate a patient's clinical needs and situation to match them with the right level of care, in the most appropriate available setting. For more information on evidence-based guidelines visit Addiction Medicine Primer .
Recovery options
There are safe and effective ways to recover from SUDs. Finding the right treatment option can be the key to a successful recovery journey.
Outpatient counseling
Helps people understand addiction, their triggers, and their reasons for using drugs. This form of treatment can be done at a doctor’s office or via telehealth appointment.
Inpatient rehabilitation
A full-time facility provides a supportive environment to help people recover without distractions or temptations.
Behavioral health care
Trained providers who help with mental health concerns.
Medications for opioid use disorder (MOUD)
Specific conditions like opioid use disorder may require medication as the first course of treatment. MOUD can help with cravings and withdrawal symptoms. 3 MOUD is effective in helping people reduce illegal opioid use, stay in treatment longer, and reduce the risk of opioid-involved overdose. 4
MOUD medications approved by the Food and Drug Administration (FDA):
- Buprenorphine
Research has demonstrated that MOUD is effective in helping people recover from their OUD. 5 6 7 It is important to find what works best each individual.
Resource
Reducing stigma is important, addiction can happen to anyone.
SUD is a treatable, chronic disease that can affect people of any race, gender, income level, or social class. No one driving factor leads to SUD. Some people may use drugs to help cope with stress and trauma or to help with mental health issues. Some may develop a SUD after taking opioids that are prescribed to them by doctors. In any case, using drugs over time may cause changes in a person's brain, leading to intense cravings and continued use. 8
Some may view acknowledging and receiving treatment for an SUD as a sign of personal failure and weakness. The associated shame felt by patients and families can make it difficult to seek treatment. Finding a doctor who is comfortable discussing SUDs can help ensure long-term recovery.
Find treatment services
Use these resources to find services that fit your needs:
Mental Health and Addiction Insurance Help (HHS)
Health Center Locator (HRSA)
Behavioral Health Treatment Services (SAMHSA)
Opioid Treatment Program Directory by State (SAMHSA)
Buprenorphine Providers Locator (SAMHSA)
Learn more about recovery
SAMHSA Behavioral Health Treatment Services Locator

Rx Awareness: Real Stories

Recovery is Possible: Know the Options
What You Need to Know About Treatment and Recovery

Opioid Therapy and Different Types of Pain

Addiction Medicine Toolkit
Medication-Assisted Treatment (MAT) | SAMHSA
Decisions in Recovery: Treatment for Opioid Use Disorder
Stigma Reduction
Addiction Treatment Locator, Assessment, and Standards (ATLAS) Platform

Linking People with Opioid Use Disorder to Medication Treatment
Working Together With Your Doctor to Manage Your Pain
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA, American Psychiatric Association, 2013.
- Substance Abuse and Mental Health Services Administration. (2023). Key substance use and mental health indicators in the United States: Results from the 2022 National Survey on Drug Use and Health (HHS Publication No. PEP23-07-01-006, NSDUH Series H-58). Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/report/2022-nsduh-annual-national-report
- SAMHSA. 2022, March 22. Medications, Counseling, and Related Conditions. Retrieved from https://www.samhsa.gov/medications-substance-use-disorders/medications-counseling-related-conditions
- TIP 63: Medications for Opioid Use Disorder - Full Document | SAMHSA
- Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev 2014;(6): CD002207. https://doi.org/10.1002/14651858.CD002207.pub4 PMID:24500948
- Mattick RP, Breen C, Kimber J, Davoli M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst Rev 2009;(3): CD002209. https://doi.org/10.1002/14651858.CD002209.pub2 PMID:19588333
- Fullerton CA, Kim M, Thomas CP, et al. Medication-assisted treatment with methadone: assessing the evidence. Psychiatr Serv 2014;65: 146–57. https://doi.org/10.1176/appi.ps.201300235 PMID:24248468
- https://nida.nih.gov/publications/drugs-brains-behavior-science-addiction/drug-misuse-addiction
Overdose Prevention
Overdose prevention is a CDC priority that impacts families and communities. Drug overdose is a leading cause of preventable death in the U.S.
For Everyone
Health care providers, public health.
- IPR Intranet
INSTITUTE FOR POLICY RESEARCH
Unraveling the drug crisis: providing timely data to break the cycle.
IPR’s Lori Ann Post is leading a drug data research center to combat overdose deaths
Get all our news
Subscribe to newsletter
The problem is that we're too late. Data were just released for 2021; it's 2024. It's as helpful to me today to combat drug overdose deaths to study the year 2021 as it is 1850. It's just a whole different ballgame out there.”
Lori Ann Post Demographer, epidemiologist, and IPR associate

Throughout its history, the U.S. has battled waves of widespread drug addiction. From painkiller addictions on Civil War battlefields to the 1980s era of crack cocaine, each crisis gives way to a new one.
Today, however, with new drugs constantly emerging, it's becoming harder to keep up with creating drug screenings and medicine to reverse overdoses. This lag leads to more overdose deaths, according to demographer, epidemiologist, and IPR associate Lori Ann Post.
Post emphasizes that we are not in a drug epidemic: We’re in a continuous, evolving drug crisis. Pandemics and epidemics have a clear beginning, middle, and end, she says, but the shape-shifting nature of the drug crisis leaves no end in sight.
The Ohio River Valley Corridor Regional Drug Data Research Center (ORVC-C) , led by Post, aims to keep history from repeating itself. The center aims to support prevention, harm reduction, treatment, public safety, and recovery services, and to create a drug data-sharing model for others. Currently, overdose death data lags two or three years behind.
“The problem is that we're too late. Data were just released for 2021; it's 2024,” Post said. “It's as helpful to me today to combat drug overdose deaths to study the year 2021 as it is 1850. It's just a whole different ballgame out there.”
“By the time we get the evidence we have, it's already too late and the problem has evolved, and it's a new variant of concern and has new treatment and needs,” she explained.
Approximately 107,622 drug overdose deaths were reported in 2021, up nearly 15% from 93,655 deaths in 2020. Over 75% of those deaths involved opioids. The COVID-19 pandemic is commonly blamed for the surge in overdose deaths, but Post said the rates were "skyrocketing" before the pandemic.
Since 1999, almost 645,000 people have died from overdoses involving opioids. This rise in opioid overdose deaths can be explained in waves, according to Post:
- The first wave started in the 1990s due to an increase in opioid prescriptions.
- The second wave began in 2010, marked by a sharp increase in overdose deaths involving heroin.
- The third wave began in 2013, with significant increases in overdose deaths involving synthetic opioids, particularly illicitly manufactured fentanyl.
- The fourth wave began around 2019 and is largely still driven by fentanyl with the addition of stimulants such as cocaine and methamphetamines.
Post explains that the fourth wave is further evolving into drug cocktails that are adulterated with animal tranquilizers . This wave is more dangerous than its predecessors, as these drug combinations are more lethal and reversal agents are limited to fentanyl overdoses.
The ORVC-C launched in October with $3.55 million in funding from the Bureau of Justice Assistance. It operates in the Ohio River Valley Corridor, encompassing Delaware, Illinois, Indiana, Maryland, Michigan, Ohio, Pennsylvania, Virginia, Washington, D.C., and West Virginia. These regions bear a lopsided burden of escalating rates of drug overdoses, individuals with substance use disorder, and drug/narcotic violations, Post says.
The Bureau of Justice Assistance has doubled the funding to create a second regional center extending the initial center to New England, New York, and New Jersey.
Within the center, Post established a Central Data Repository (CDR) and a Dissemination and Engagement Center (DEC). The CDR collects, analyzes, and shares comprehensive drug-related data from existing information collected by local, state, and national agencies. This covers labor, crime, public health indicators, and demographic data. The DEC fosters partnerships and produces educational materials to address needs as they arise.
Post says that the center processes data to provide actionable insights for policymakers, public health practitioners, law enforcement, and other stakeholders, while also ensuring accessibility for fellow researchers.
Streamlining the data collection process reduces administrative burdens. It also allows researchers to delve directly into addressing critical issues without unnecessary hurdles.
“The more people doing research on it, the better we're going to do,” she said. “The timelier the data is, the more relevant it is to solving drug use and preventing drug overdose deaths. That’s the whole point.”
Lori Ann Post is the Buehler Professor for Aging, director of the Buehler Center for Health Policy and Economics, and an IPR associate.
Photo credit: iStock
Published: May 10, 2024.
Related Research Stories

U.S. Employees Overestimate Racial Progress at Work

New IPR Research: April 2024

Harnessing the Power of Artificial Intelligence
These mothers lost children to opioid overdoses. On Mother's Day, they offer new approach.
Aimee Dunkle often ruminates about the call that could have saved her son's life.
A friend was with her 20-year-old son when he was in the grips of a heroin overdose in 2012, but the young man never called 911 for fear he'd be locked up for violating the terms of his drug diversion program. Ben suffered a catastrophic brain injury as a result of the delay in getting medical help. He died after eight days on life-support.
More than a decade later, as fatal opioid overdoses are skyrocketing across the U.S., Dunkle, 63, and other grieving family members have joined forces to call for compassionate treatment rather than criminalization of drug users like Ben's friend.
These types of punitive drug laws, Dunkle said, “cost my boy his life.”
Opioid crisis: Fueled by fentanyl, drug overdose deaths have quadrupled in past 2 decades
As more than 100,000 people died from overdose deaths for a second consecutive year, lawmakers proposed a slew of bills aimed at doling out harsher sentences – including murder charges – for people who sell or distribute drugs such as fentanyl, a synthetic opiate that's exponentially stronger than heroin. Families who have lost children to overdoses say such policies won't reduce deaths like those their relatives suffered. Instead, they'll push chronic health issues of addiction into prisons. They will perpetuate but not curtail the country’s decades-long war on drugs, the families said.
“We all want to see a reduction in overdose deaths, but punishment is not the answer,” Dr. Tamara Olt , a mother from Peoria, Illinois who lost her 16-year-old son Josh to an opioid overdose in 2012, said at a recent news briefing.
Olt serves as executive director of Broken No More, an organization founded by families and friends of people with substance use disorders. The organization held a virtual news conference in the lead-up to Mother's Day to share their support for drug policies informed by evidence-based public health practices, rather than punitive approaches.
In September, hundreds of grieving family members issued an open letter to lawmakers to call for “lifesaving health responses to the overdose crisis.” They pushed back on laws that establish murder charges for “drug-induced homicide” if someone sells or shares drugs that result in a fatal overdose and on mandatory minimum sentences and increased punishment for drug use. Instead, the letter urged lawmakers to find ways to decriminalize drugs and work on providing better access to needle exchanges and overdose-reversing medications like naloxone, and focus on evidence-based treatment options and broadening education on opioid use disorder.
States shift approach on fentanyl
Several states have changed the penalties for distributing or manufacturing fentanyl, according to an August analysis by the National Conference of State Legislatures . This includes new laws in Arkansas and Kansas that impose life imprisonment for manufacturing fentanyl that could appeal to a minor through shape or packaging. Tennessee also allows prosecutors to charge people with murder if they give fentanyl to a person who dies from an overdose.
While these laws have cropped up in Republican-led states that traditionally embraced tougher drug laws, advocates at the briefing this week warned that Democratic-leaning states are embracing similar approaches at the peril of people suffering from substance use disorder.
In 2021, Oregon became the first state to decriminalize illicit drugs. The policy, backed by the American Pharmacists Association, would allow people using illegal substances to retain their employment while involved in treatment. But following the recent explosion in synthetic opioid deaths, the blue state brought back criminal punishment for use and possession of narcotics in 2024 . The law never had a chance to work, Jeffrey Bratberg, clinical professor in the University of Rhode Island College of Pharmacy, told USA TODAY at the time the law was reversed.
Related: These two moms lost sons to opioids. Now they’re on opposite sides at the Supreme Court.
California, where Dunkle lives, has also shifted its drug policies, cracking down harder in recent years on people who perpetuate use. In her son Ben’s memory, in 2015, Dunkle founded the nonprofit Solace Foundation of Orange County, the first naloxone distribution program in her region of Southern California. Dunkle also began distributing fentanyl test strips and worked with a needle exchange until Santa Ana city officials shut it down in 2018.
After that, Dunkle said, "I took to the streets of Santa Ana with a backpack to hand out supplies and naloxone."
In the years she's been focused on these issues, she's seen a push for punitive measures fueled by other grieving families. She has thought long and hard about that. But she's seen that, all too often, the people who give someone a drug that causes a fatal overdose are also users. Fentanyl − a drug far more powerful than heroin that replaced it on streets in the U.S. in recent years − poses even greater danger to people with substance use disorders.
“They didn’t choose fentanyl,” she told USA TODAY. “Fentanyl was chosen for them.”
One instance of families pushing for harsher laws is a bill by California State Senator Tom Umberg, D-Orange County, whose legislation “Alexandra’s Law” requires educating people convicted of distributing opioids publicly within the court setting. The bill requires a judge to read a “fentanyl admonishment” to anyone convicted of a fentanyl-related drug offense, stating, "You are hereby advised that all illicit drugs and counterfeit pills are dangerous to human life and become even deadlier when they are, sometimes unknowingly, mixed with substances such as fentanyl and analogs of fentanyl." The bill is named after a 20-year-old Temecula, California woman, Alexandra Capelouto , who died from a fentanyl overdose. Several families who lost loved ones to fentanyl overdoses, including Capelouto's family, backed the bill.
The admonishment is similar to statements judges must read to people convicted of a DUI. The current draft language for "Alexandra's Law" says that if a convicted person sells or administers fentanyl in the future that results in someone’s death, they could be charged with murder. The bill is stuck in the state Legislature.
“While any purchase of drugs from the street or black market inherently carries a risk, what we are seeing today is the unprecedented poisoning of young Americans,” Umberg, a former prosecutor, said in a statement to USA TODAY. “There is no fear of addiction, or need to ask for help when a victim dies almost immediately of a substance they never assumed would kill them.”
Dunkle said such legislation doesn’t address the overdose problem in its entirety, especially for young people like the man who was with her son when he overdosed. Umberg, a lawmaker in Dunkle's county, said in his statement that he knew Dunkle and felt for her family and others who have lost loved ones to the opioid crisis.
However, he refuted the notion that California is prosecuting fentanyl users by applying harsher penalties, and putting them behind bars instead of offering treatment.
“To suggest so and equate it to the ‘War on Drugs’ is dangerously misleading and borderline irresponsible,” Umberg said. “This epidemic requires an ‘all in/every tool’ approach to the crisis,” including prevention, education, treatment and stopping repeat sellers. “Arresting and prosecuting fentanyl dealers alone is an insufficient response to meet this crisis,” he said.
Dunkle said she understands the anger that families feel. She felt it, too, after Ben’s death. But it changed a few weeks after his death. Her younger son, then 17, bumped into Ben's friend who had refused to call for help the day of the overdose. The friend looked terrible, her younger son said.
She wanted people to look for light out of the darkness, she said. Fentanyl overdoses happen quickly. People should feel assured that saving their friends is not just the right thing, it's something they can safely do without being punished.

An official website of the United States government, Department of Justice.
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Drug-Impaired Driving: The Contribution of Emerging and Undertested Drugs
Impaired driving is often with alcohol use and frequently leads to accidents, injuries, and fatalities. According to the National Highway Traffic Safety Administration, one person was killed every 39 minutes in an alcohol-related crash in 2021. [1] But alcohol is not the only concern; the use of illicit drugs, legalized drugs such as cannabis, and the abuse of prescription medications may also impair a driver’s abilities. In 2022, an estimated 13.6 million people drove under the influence of illicit drugs during the prior year. [2]
In 2007, the National Safety Council (NSC) introduced testing scope and cutoff standardization for impaired driving cases and traffic fatalities to improve testing consistency. Since 2013, it has recommended that forensic toxicology labs regularly test blood for 35 of the most often encountered drugs and metabolites. Referred to as Tier I drugs ( Figure 1 ), they are now included as a testing standard in many forensic toxicology labs. [3] Furthermore, these compounds can be detected and confirmed with commonly used analytical instrumentation.
Figure 1. List of Tier I and Tier II drugs. Tier II drugs can be both individually named drugs and classes of drugs (e.g., atypical antipsychotics).
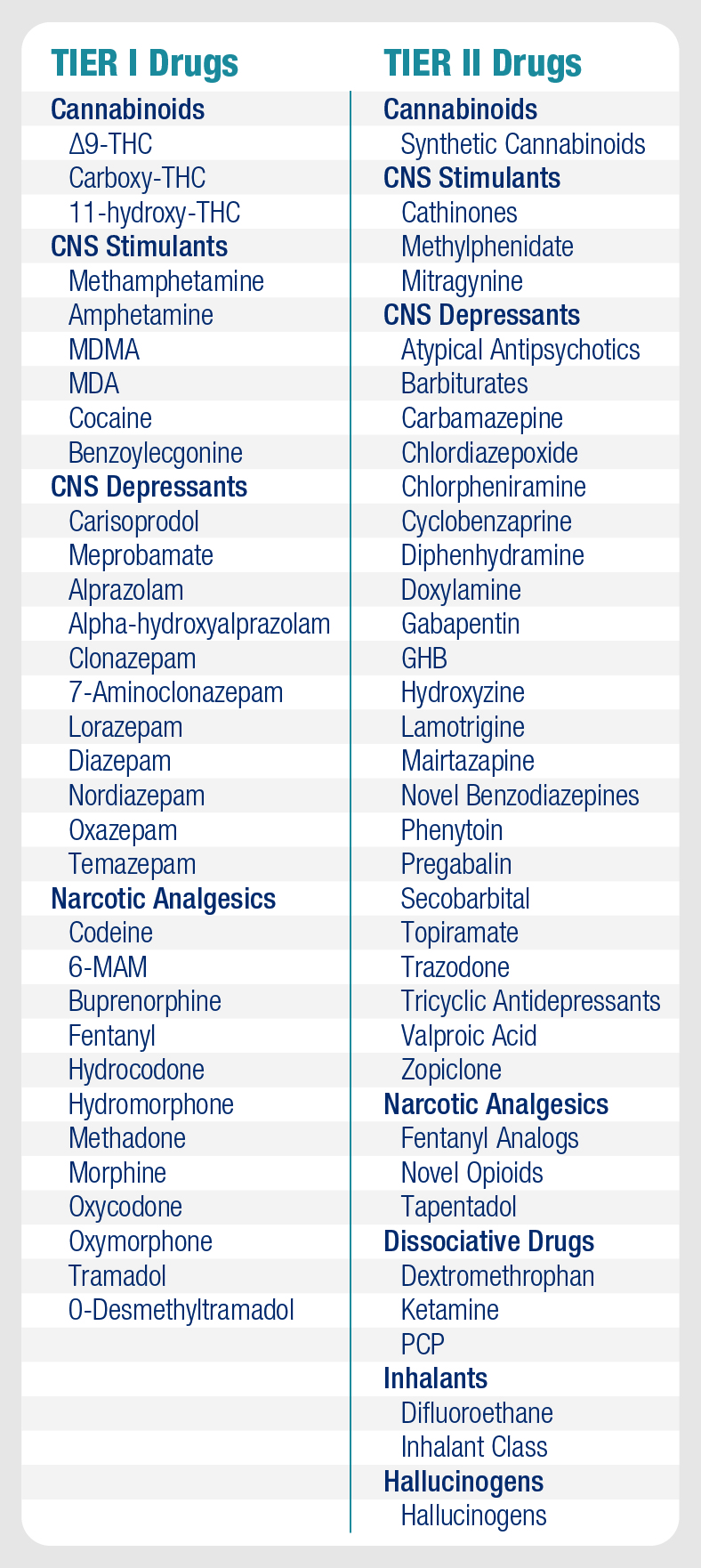
NSC also created a second drug category with significant impairment potential, termed Tier II drugs. These drugs include emerging novel psychoactive substances, prescription drugs, and traditional drugs of abuse with limited or regional prevalence, many of which require advanced instrumentation for detection. Most laboratories test for Tier I drugs, but only test for select Tier II drugs when they are regionally relevant. Therefore, the frequency and the types of Tier II substances contributing to drug-impaired driving cases and fatal crashes is not well understood.
NIJ-funded researchers from the Center for Forensic Science Research and Education examined blood samples from over 2,500 driving under the influence of drugs (DUID) cases. The goal was to create a detailed picture of both Tier I and Tier II drugs that contribute to impaired driving cases and compare results to the NSC’s recommended testing scopes. Researchers also analyzed drug presence at various blood alcohol concentrations to assess the operational impact of different testing thresholds and stop limit testing.
What is Stop Limit Testing?
If a sample meets or exceeds a pre-determined blood alcohol concentration threshold, some labs will not perform any additional drug tests. This cutoff is most commonly either 0.08% or 0.10%. [4] The legal blood alcohol limit in the U.S. across every state is 0.08%. Labs that adhere to this practice will not detect other drugs that may cause or contribute to driving impairment.
This stop limit testing can interfere with a comprehensive understanding of drug involvement in impaired driving. Why do so many labs use it?
- Toxicology labs have limited budgets and resources.
- Driving impairment can be explained by the blood alcohol concentration alone.
- A lack of enhanced penalties for drug use means there is no need to measure beyond the blood alcohol level.
- Agencies that use the laboratories’ services have requested this limit.
National Safety Council Recommendations Are Supported
Researchers estimated the frequency with which drugs contribute to the national DUID problem by testing 2,514 cases using a scope of 850 therapeutic, abused, and emerging drugs. They examined deidentified blood samples randomly selected from a pool of suspected impaired driving cases. The samples were collected from NMS Labs in Horsham, Pennsylvania, between 2017 –2020.
Of the 2,514 suspected DUID cases examined:
- The overall drug positivity (Tier I or Tier II drugs) was 79%, nearly double the 40% positive for alcohol ( Figure 2 ).
- A smaller portion of cases (23%) tested positive for both drugs and alcohol.
- Only 17% of the cases were positive for alcohol alone.
- Naturally occurring cannabinoids experienced a statistically significant increase in positivity over the four years.
Figure 2. The frequency of cases with (a) no drugs or ethanol detected (4%), (b) ethanol detected (40%), (c) drugs and ethanol detected (23%), and (d) drugs detected (79%).
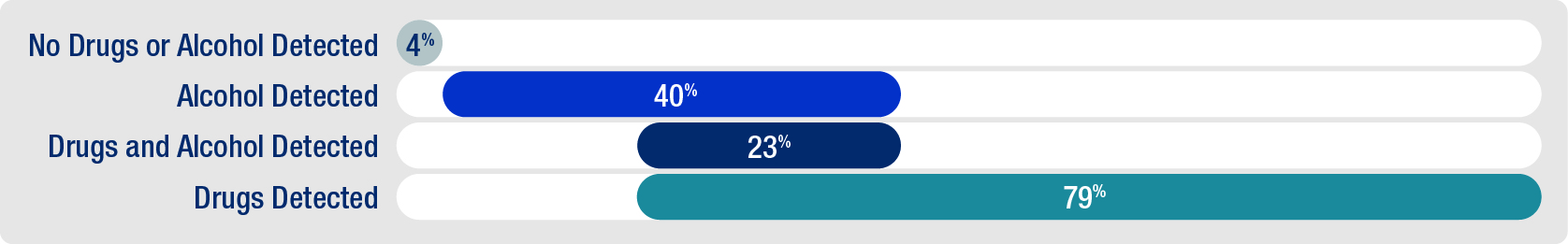
Alcohol use in combination with drugs spanning multiple categories was common, as was multiple drugs used in combination. THC (the primary psychoactive component of marijuana) was most often found with ethanol (n=359), and it was frequently found with amphetamine/methamphetamine (n=146).
Samples with a blood alcohol content of 0.08% or higher that were also positive for either Tier I or Tier II drugs occurred 19% of the time (n=478). Cases with blood alcohol content of 0.10% (the cutoff used most frequently by toxicology labs) were also positive for Tier I or Tier II drugs 17.3% of the time (n=434). This suggests that laboratories employing stop limit testing may miss many drug-positive cases.
“Limiting testing based on alcohol results precludes information of drug involvement in several cases and leads to underreporting of drug contributions to impaired driving,” said Mandi Moore, one of the researchers involved in the study.
The research supported NSC’s recommendations for Tier I and Tier II testing. Tier I drugs were found in 73% of suspected impaired driving cases while only 3% contained just Tier II drugs. This suggests that Tier I testing captures the vast majority of drug-involved DUID cases. However, some Tier II drugs (diphenhydramine, gabapentin, hydroxyzine, and two novel psychoactive substances) were found as often or more often than some Tier I drugs, potentially indicating their increased prevalence and a need to re-examine guidelines.
Study Limitations
The cases used in this analysis were exclusively from Pennsylvania. Therefore, they provide a geographically limited snapshot rather than a comprehensive characterization for the entire U.S. population. However, the sample size of over 2,500 cases was “suitable to meet the research goals outlined” by the researchers.
Because Tier II and novel psychoactive substances were found in relatively low frequencies, the researchers did not develop or validate additional confirmatory methods as they had previously planned.
Filling in the Big Picture Details
This work increases awareness of drugs that labs are less likely to test for and labs’ role in addressing the DUID problem. It also demonstrates how frequently DUID cases involve drugs other than alcohol. Although stop limit testing can be justified, data on both alcohol and drug use creates the clearest picture of DUID contributing factors. Current estimates of drug frequency in DUID cases are likely to be inaccurate and actual usage is likely to be higher than previously believed due to stop limit testing. Equipping labs with sufficient resources could encourage labs to eliminate stop limit testing.
About This Article
The work described in this article was supported by NIJ award number 2020-DQ-BX-0009 , awarded to the Frederic Rieders Family Renaissance Foundation.
This article is based on the grantee report “ Assessment of the Contribution to Drug Impaired Driving from Emerging and Undertested Drugs ” (pdf, 26 pages), by Amanda L.A. Mohr and Barry Logan, The Center for Forensic Science Research and Education (CFSRE) at the Frederic Rieders Family Renaissance Foundation.
[1] NHTSA.gov, accessed January 29,2024, https://www.nhtsa.gov/risky-driving .
[2] Select Illicit Drugs include the use of marijuana, cocaine (including crack), heroin, hallucinogens, inhalants, or methamphetamine. For more information, see "Table 8.35A" in 2022 NSDUH Detailed Tables, Substance Abuse and Mental Health Services Administration, https://www.samhsa.gov/data/sites/default/files/reports/rpt42728/NSDUHDetailedTabs2022/NSDUHDetailedTabs2022/NSDUHDetTabsSect8pe2022.htm#tab8.35a .
[3] ANSO/ASB Standard 120.
[4] Amanda D’Orazio, Amada Mohr, and Barry Logan, “Updates for Recommendations for Drug Testing in DUID & Traffic Fatality Investigations, Toxicology Laboratory Survey,” Willow Grove, PA: The Center for Forensic Science Research & Education at the Frederic Rieders Family Foundation, June 28, 2020, https://www.cfsre.org/images/content/research/toxicology/Survey_Report_Final.pdf .
Cite this Article
Read more about:, related publications.
- Assessment of the Contribution to Drug Impaired Driving from Emerging and Undertested Drugs
Related Awards

How We Can Exercise Away Addiction and Depression
There are multiple major benefits from becoming active..
Posted May 16, 2024 | Reviewed by Gary Drevitch
- What Is Depression?
- Find a therapist to overcome depression
- Exercise helps substance abusers kick habits.
- Brain chemicals are enhanced and new connections made with exercise.
- Depression levels plummet with exercise.
- Exercise is safe and effective, and especially helpful in long-term recovery from substance use disorders.
Exorcise addictive and depressive demons the way celebrities do — with exercise. You’ve probably heard how many famous people have chosen exercise to effectively prevent and even treat mental health problems like addictions and depression . This is because exercise helps support and normalize mood-stabilizing neurochemicals like dopamine and glutamate, as well as serotonin.
Brain Chemicals Generated by Exercise
One key neurochemical that may not trip off your tongue is brain-derived neurotrophic factor (BDNF). This is a protein in the brain and spinal cord that is vital for developing and maintaining the central nervous system (CNS). BDNF is especially concentrated in the hippocampus, cortex, and basal forebrain. This substance promotes the survival of nerve cells (neurons) by helping growth, maturation, and maintenance. It also helps control synaptic plasticity — the ability of brain connections to change and adapt over time — and consequently is important for learning and memory . Low levels of BDNF can cause difficulties in learning new things, as well as lead to depression and mood swings.
Strangely, exercise and using drugs of abuse act on similar parts of the brain. For example, each similarly activates the reward pathway, triggering the release of feel-good chemicals like serotonin and dopamine. This is another reason why people turn to drugs repeatedly. However, exercising itself may build up the amount of dopamine, regenerative proteins, and other synapses. As a result, these added connections increase the quantity of available dopamine and support other brain chemicals. The end result is feeling much better.
Eminem, Addiction, and Exercise
Intense physical exercise has received major attention as an effective way to reduce cravings and remain sober by celebrities like the rapper Eminem. In 2024, Em posted his annual updated AA pin on his social media account, where he reported being sober 16 years . He explained drugs had loomed large in his life after the release of his 1999 album, The Slim Shady LP . The singer didn’t think he had a problem; however, as his fame increased and drugs became more plentiful — especially on tour — Eminem realized he was battling addiction. Things were bad in 2000-2002 when he was taking Vicodin, Valium, and alcohol . The performer said he took “75 to 80 Valiums” a night.

Eminem battled his addiction using running and exercise. He also did push-ups and sit-ups, tried boxing, and attended recovery meetings. Eventually, he moved to the “Body Beast” workout, using free weights, the pullup bar, and the bench.
The Experts Explain It All
According to the scientist who showed exercise could help people addicted to cocaine, Panayotis K. Thanos , Director of Behavioral Neuropharmacology and Neuroimaging Laboratory, Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, “Our research has proven aerobic exercise has many benefits, but it has a profound effect on dopamine and the dopamine receptor.” Adds Thanos, “Aerobic exercise can decrease drug-seeking behaviors, cocaine preference, cocaine relapse , and cocaine stress-induced reinstatement.” Exercise also appears to have the same potential positive effects on cigarette smokers, opioid users, and others with drug use disorders.
Why People Resist Exercise as a Treatment for Drug Abuse or Depression
Why do people shun exercise as a possible answer to substance abuse or severe depression? I asked former Olympian and Olympic psychiatrist Dave Baron this question.
Baron said, “People don't see exercise as an intervention, but more of a lifestyle choice. The best available scientific data is overwhelmingly positive yet is not well-appreciated by the general public. In addition, exercise is not aggressively promoted, as the pharma industry does with medications.” Baron says too many people regard exercise like their gym class—an annoying and sweaty requirement they left back in high school.

Types of Problems Exercise Can Improve
Most data supports the role of exercise in the following:
Curbing cravings. After cutting down or off drugs, the brain sends alarm or anxiety signals caused by abstinence. These symptoms may be intense and may also drive relapse. Many people who successfully avoid drugs still may develop urges to use them again. Exercise is an excellent way to reduce the intensity of cravings, make them feel much less powerful, and help the recovering person control or reduce the frequency and intensity of these cravings.
Replacing triggers for abuse. It’s best for substance abusers to trade their old drug buddies in for some new exercise pals. Exercises like running in a group or club or training with a class and trainer, can become a positive routine—an important activity to perform and build up a person’s social network . This change of places, people, and things is important, as key recovery axioms include avoiding triggering people, places, or things and reminding the person of drugs used when abuse formerly was an active problem.
Improving sleep. If a person has a substance use disorder (SUD), often they take drugs to sleep. It is also true that recovering SUD patients suffer sleep problems as they struggle to avoid drugs or alcohol. Regular exercise helps individuals fall asleep faster and obtain a better quality of rest at night.

Helping the body and brain become stronger. Abused drugs have numerous harmful effects on the heart, lungs, liver, brain and immune functions. In contrast, exercise has the opposite effect. Exercise can also help recovering people think more clearly; often they report their mind starts working much better. Regular physical activity continues this positive process.
Improving self-image . Exercise can make people feel more self-control , which is very important for substance abusers who feel like they’ve lost control. Exercise also has positive anti-anxiety and antidepressant effects, making it easier to manage stressful situations and feelings.
What if Exercise Were a Medication?
With all the benefits described, I wondered if exercise might be treated differently if people compared the activity to taking a pill or other medication . Baron liked this idea and said, “If exercise were a medication in a double-blind FDA qualifying clinical trial, the trial would be stopped by the FDA, because exercise is so effective, and with virtually no side effects, that it would be unethical to not treat everyone with it.” Baron says that if exercise were a pill, it would be a blockbuster drug.
He continued, “Exercise has been shown effective in virtually every age range for virtually every form of psychopathology and as a primary and adjunctive treatment. It would be very difficult to find another treatment as effective and safe in maintaining mental and physical health, improving overall quality of life, and effectively treating psychopathology.”
Early research shows that aerobic exercise and resistance training may be most effective with addiction recovery. However, the evidence so far is insufficient to recommend one kind of physical activity over another. So if a person prefers yoga or mountain biking, either option may be helpful to combat addiction. Future studies should help us learn more and create programs tailored to individuals.
Considering Exercise and Depression
Major depressive disorder (MDD) is characterized by a depressed mood, loss of interest, and a reduced ability to experience pleasure in daily activities for at least two weeks. In 2020, the World Health Organization (WHO) estimated 264 million people worldwide were affected by depression , or 3.8% of the population. The WHO also estimates that depression is the world's leading cause of disability.
Individuals with this disorder face an increased risk of type 2 diabetes, cardiovascular disease, lower back pain, and an overall decline in life quality. It is also the leading cause of suicide deaths worldwide, with an estimated incidence of up to 800,000 suicides annually.
Physical exercise is not only an effective intervention for depression, but researchers also report that exercise may be a viable adjunct treatment in combination with antidepressants .
Clinical practice guidelines recommend psychotherapy and/or pharmacotherapy for MDD. But at least 30% of people with depression have treatment-resistant depression, which means medications and therapy don’t help. Consequently, there is an urgent need to explore non-pharmacological and patient-centered strategies that are safe, feasible, and easily integrated into adult daily routines. A recent major study published in 2024 showed exercise is an effective depression treatment.
In addition, exercise apparently is about as effective for reducing depression as cognitive behavioral therapy (CBT) or medications, although combining exercise with antidepressants may improve symptoms more than medication alone. The more intense the workout, the more effective at managing depression. But even low-intensity physical activity helps.
Current National Institute for Health and Care Excellence (NICE) guidance on treating depression in adults says the condition may respond to a variety of options, with group exercise recommended as cost-effective and easy to implement.
Commenting on the results of the study, Jonathan Roiser, professor of neuroscience and mental health at University College London, said, “The headline result is that all types of physical activity (especially aerobic exercise) cause a reduction in depressive symptoms ; a similar conclusion to many reviews over the past decade.”
Many people severely undervalue—or don’t even consider—that exercise decreases addictive cravings as well as depressive symptoms. People can exercise at home or in a gym or begin a walking or running program in their neighborhood or at a local mall after checking with their doctor.
To find a therapist, visit the Psychology Today Therapy Directory .
Perreault B, Hammond N, Thanos PK. Effects of Exercise on Testosterone and Implications of Drug Abuse: A Review. Clin Neuropharmacol. 2023 May-Jun 01;46(3):112-122. doi: 10.1097/WNF.0000000000000546. Epub 2023 Mar 7. PMID: 37191565.
Noetel M, Sanders T, Gallardo-Gómez D, Taylor P, Del Pozo Cruz B, van den Hoek D, Smith JJ, Mahoney J, Spathis J, Moresi M, Pagano R, Pagano L, Vasconcellos R, Arnott H, Varley B, Parker P, Biddle S, Lonsdale C. Effect of exercise for depression: systematic review and network meta-analysis of randomised controlled trials. BMJ. 2024 Feb 14;384:e075847. doi: 10.1136/bmj-2023-075847. PMID: 38355154; PMCID: PMC10870815.
Tyler J, Podaras M, Richardson B, Roeder N, Hammond N, Hamilton J, Blum K, Gold M, Baron DA, Thanos PK. High intensity interval training exercise increases dopamine D2 levels and modulates brain dopamine signaling. Front Public Health. 2023 Dec 19;11:1257629. doi: 10.3389/fpubh.2023.1257629. PMID: 38192549; PMCID: PMC10773799.
Claussen MC, Currie A, Koh Boon Yau E, Nishida M, Martínez V, Burger J, Creado S, Schorb A, Nicola RF, Pattojoshi A, Menon R, Glick I, Whitehead J, Edwards C, Baron D. First international consensus statement on sports psychiatry. Scand J Med Sci Sports. 2024 Apr;34(4):e14627. doi: 10.1111/sms.14627. PMID: 38610076.

Mark S. Gold, M.D., is a pioneering researcher, professor, and chairman of psychiatry at Yale, the University of Florida, and Washington University in St Louis. His theories have changed the field, stimulated additional research, and led to new understanding and treatments for opioid use disorders, cocaine use disorders, overeating, smoking, and depression.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
- Open access
- Published: 11 May 2024
How do we understand the value of drug checking as a component of harm reduction services? A qualitative exploration of client and provider perspectives
- Lissa Moran 1 ,
- Jeff Ondocsin 1 , 2 ,
- Simon Outram 1 ,
- Daniel Ciccarone 2 ,
- Daniel Werb 3 , 4 ,
- Nicole Holm 2 &
- Emily A. Arnold 1
Harm Reduction Journal volume 21 , Article number: 92 ( 2024 ) Cite this article
325 Accesses
Metrics details
Mortality related to opioid overdose in the U.S. has risen sharply in the past decade. In California, opioid overdose death rates more than tripled from 2018 to 2021, and deaths from synthetic opioids such as fentanyl increased more than seven times in those three years alone. Heightened attention to this crisis has attracted funding and programming opportunities for prevention and harm reduction interventions. Drug checking services offer people who use drugs the opportunity to test the chemical content of their own supply, but are not widely used in North America. We report on qualitative data from providers and clients of harm reduction and drug checking services, to explore how these services are used, experienced, and considered.
We conducted in-depth semi-structured key informant interviews across two samples of drug checking stakeholders: “clients” (individuals who use drugs and receive harm reduction services) and “providers” (subject matter experts and those providing clinical and harm reduction services to people who use drugs). Provider interviews were conducted via Zoom from June-November, 2022. Client interviews were conducted in person in San Francisco over a one-week period in November 2022. Data were analyzed following the tenets of thematic analysis.
We found that the value of drug checking includes but extends well beyond overdose prevention. Participants discussed ways that drug checking can fill a regulatory vacuum, serve as a tool of informal market regulation at the community level, and empower public health surveillance systems and clinical response. We present our findings within three key themes: (1) the role of drug checking in overdose prevention; (2) benefits to the overall agency, health, and wellbeing of people who use drugs; and (3) impacts of drug checking services at the community and systems levels.
This study contributes to growing evidence of the effectiveness of drug checking services in mitigating risks associated with substance use, including overdose, through enabling people who use and sell drugs to test their own supply. It further contributes to discussions around the utility of drug checking and harm reduction, in order to inform legislation and funding allocation.
The opioid crisis in the U.S. consists of multiple overlapping and inter-related waves of surging opioid exposure, dependency, overdose, and death rates. Each wave has emerged from different eras of an evolving drug market and multiple intersecting contextual factors such as trends in pharmaceutical manufacturing and prescription, socioeconomic inequities, and positive supply shocks of both licit and illicit opioids [ 1 , 2 , 3 ]. Though its history can be traced back to the 1980s and 1990s, the past decade has redefined the crisis [ 4 ].
By the time the U.S. Department of Health and Human Services (HHS) declared the opioid crisis a public health emergency in 2017 [ 5 ], a wave of unprecedented magnitude had been on the rise for nearly 4 years, marked by the rapid proliferation of fentanyl and synthetic analogues into the drug market [ 4 , 6 ]. Even as mortality from heroin and prescription opioids leveled off or decreased, opioid overdose and death rates rose precipitously [ 6 ]. From 2018 to 2021, the rates of opioid overdose deaths in the U.S. nearly doubled, and by 2021, roughly 9 out of every 10 opioid overdoses in the country (88%) were fentanyl-related [ 7 ].
In California, home to the highest number of opioid-related deaths in the U.S. [ 8 ], the opioid overdose death rate curve from 2011 to 2021 tells a harrowing story. The third wave was later to arrive in California than the national average, but its onset was rapid and dramatic. Opioid overdose death rates more than tripled from 2018 to 2021, and synthetic opioid (e.g., fentanyl) deaths increased 7.2 times, responsible for 37% of opioid overdose deaths in 2018, and 86% just three years later [ 9 ].
In response, the California Department of Public Health has committed to the expansion and promotion of policies, programs, and services to combat the overdose epidemic, with a special focus on harm reduction and drug checking strategies [ 10 ].
Drug checking services
Drug checking services (DCS) have garnered particular interest as an expansion of harm reduction strategies, as they offer the opportunity for people who use drugs to test the chemical content of their own supply [ 11 , 12 ]. In doing so, people who use drugs may be afforded the possibility of changing their use behavior to remove or reduce the likelihood of harm [ 13 , 14 ]. Multiple DCS have been operating in Europe for years—particularly in venues known for high rates of recreational drug use like music festivals [ 14 , 15 ]—but are less common in North America. In the U.S. and Canada, DCS have emerged primarily in response to the needs of marginalized people who use opioids, and operate predominantly within the context of frontline services [ 16 , 17 , 18 ].
Though not mainstream or broadly implemented, studies from North America indicate that DCS are generally acceptable among people who use drugs [ 19 , 20 ], and report that both service users and providers have expressed desire for better access to DCS, legal protections for those providing and using drug checking, and advanced technologies that provide information on drug concentrations—not just drugs present—at the point of care [ 21 , 22 , 23 , 24 ]. Several studies explore the potential impact of drug checking when used at various points along the supply chain [ 25 , 26 ], with findings that suggest feasibility, acceptability, and uptake of DCS among drug sellers [ 27 ], noting particular importance to drug sellers who are embedded in their community and hold long-term trusted relationships with customers [ 28 , 29 ].
Arguably the most common and well-known drug checking modality in North America are fentanyl testing strips (FTS), or lateral flow assays, which were originally designed for the clinical use of detecting fentanyl in urine samples, but have been publicly available for several years for modified use with drug samples [ 30 , 31 , 32 , 33 ]. FTS have been a powerful tool to combat accidental fentanyl exposure: they are small, portable, relatively accessible, and detect fentanyl in minute concentrations that could still be enough to trigger an overdose in an opiate-naïve individual [ 31 , 34 ]. They have been found to be particularly useful for outreach and street use [ 13 , 25 , 35 ]. That said, FTS are not useful in the same way for those who intend to use fentanyl, where the overdose risk is not in the presence of fentanyl, but in the concentration and presence of additional adulterants like sedatives [ 36 ].
Drug checking technology has advanced, and continues to advance, such that a greater amount can be known about the chemical components of a drug sample in a shorter period of time, in a broader array of environments [ 37 ]. Multiple drug checking modalities can inform people who use drugs about the presence of unexpected adulterants, such as benzodiazepines and xylazine, among others. Technologies that offer the greatest specificity and sensitivity include Gas Chromatography Mass Spectrometry and High-Performance Liquid Chromatography, which can detect the presence and concentrations of a wide array of chemicals present in even small amounts in a sample, but must be used in a laboratory setting by a trained technician [ 37 ]. More flexible technologies have emerged, like Fourier-Transform Infrared Spectroscopy (FTIR) [ 38 ], which is semi-portable, and returns information on the main chemical components of a drug sample (above 5% concentration) in a matter of minutes [ 31 ]. Paper spray mass spectrometry is more expensive than FTIR but is just as fast, and provides quantitative results [ 39 ]. Today, multi-technology-based drug checking services are available in some areas as standalone programs, or as added components to existing harm reduction centers [ 30 , 40 ].
These innovations continue to advance amidst complex and evolving social, legal, political, and funding conditions [ 11 , 21 , 41 , 42 ]. Legally, drug checking can be complicated as a public service, requiring the handling and, often, exchange of illicit drug material, of which possession and distribution is often criminalized [ 21 ]. Harm reduction initiatives more broadly—DCS, syringe access services, naloxone distribution, HIV/HCV testing, wound care, supervised consumption sites, and medications for opioid use disorder (MOUD), among others—can at times be unpopular socially and politically, as stigma associated with addiction and drug use combined with concerns about the goals and practices of harm reduction can generate powerful community pushback [ 41 , 42 , 43 , 44 , 45 , 46 , 47 ]. Legislators and policymakers at local, state, and federal levels who rely on constituent support may therefore shy away from supporting various harm reduction strategies, despite endorsement from public health officials and robust evidence showing that harm reduction improves the health, survival, and recovery potential for people who use drugs, without compromising community safety [ 48 , 49 ]. At the same time, California was one of several states to bring lawsuits against opioid manufacturers, distributors, and pharmacy chains, alleging that they played an active and/or negligent role in the genesis and exacerbation of the opioid crisis [ 50 ]. Of the $43.3 billion in settlement funds that have been awarded thus far, California may receive nearly $4 billion [ 51 ]. These funds are specifically earmarked for activities that are to include “prevention, intervention, harm reduction, treatment and recovery services.” [ 52 ].
As the opioid crisis reaches an unprecedented magnitude and strategies to address it are at once both a priority and a topic of controversy, we aimed to explore the value of drug checking services and their role within harm reduction more broadly. In this study, we report on qualitative data from providers and clients of harm reduction and drug checking services, to explore how these services are used, experienced, and considered. We aim to contribute to an existing qualitative evidence base exploring the value and utility of drug checking services, particularly as data are leveraged to inform political narratives, legislation, and funding allocation.
For this study, we conducted in-depth semi-structured key informant interviews across two samples: a “provider” sample and a “client” sample. The “provider” sample consisted of individuals providing clinical and harm reduction services to people who use drugs, as well as drug checking subject matter experts such as researchers and program heads. The “client” sample consisted of individuals who use drugs and were receiving harm reduction services at an agency where multiple forms of drug checking were included in the services provided.
From June to November 2022, two authors (DC & LM) conducted in-depth semi-structured key informant interviews with 11 providers—8 working in the U.S., 2 working in Canada, and one working in both countries. Included in the sample were 2 clinical providers, 4 researchers, and 5 harm reduction service providers [Table 1 ].
We employed purposive sampling of known providers first, then snowball sampling, contacting additional potential participants at informants’ recommendation. All potential participants were contacted via email and invited to participate. If the participant agreed, an appointment was made for the interview to take place over Zoom. Interviews lasted between approximately 45 and 60 min, and solicited provider perspectives on the state of the drug market in their area, the perceived needs of and challenges faced by their local client population, and their attitudes and experiences with drug checking methods and programs and integrating such programs into existing services. Verbal consent was collected at the outset of the interviews, which were then recorded. Audio from the recordings was isolated and transcribed using a secure third-party professional transcription service. All transcripts were deidentified and researchers created unique anonymous ID numbers for each participant. Participating providers were offered an honorarium of $100 in the form of a gift card. The study protocol was reviewed by the University of California San Francisco Institutional Review Board (IRB #22-36262).
Client participant ( n = 13) recruitment and data collection took place over a one-week period in November 2022 [Table 2 ].
We employed a non-random convenience sample, recruiting from four harm reduction programs in San Francisco, where clients were approached either by interviewers (NH & JO) or program staff who had been instructed on eligibility requirements. Eligible participants were at least 18 years of age, and currently using fentanyl, heroin, or methamphetamine. Clients were excluded from eligibility if they were intoxicated or otherwise unable to provide informed consent. Given that current drug use was an eligibility requirement, we assessed “intoxicated” as an inability to respond to simple questions, providing responses that are incoherent or unintelligible, or if the participant indicates that they are too high to continue. Potential participants who were eligible and interested were then formally verbally consented and interviewed on-site. Client interviews explored participants’ history of drug use and experiences with harm reduction services, as well as their awareness of, attitudes about, and experiences with various drug checking modalities. Interviews lasted approximately 30–60 min and were recorded, then submitted to the same external third-party transcription service being used for provider interviews. Participants were provided a $25 cash incentive as a token of appreciation for their time and expertise, and were provided unique ID numbers to anonymize their data. This study protocol, distinct from the protocol covering provider interviews, was reviewed and approved as well by the UCSF IRB (#22-36640).
Client interview transcripts were uploaded to Dedoose, a qualitative analytic program [ 53 ]. Four analysts (EA, LM, SO, and JO), two of whom were involved in data collection (LM & JO), read transcribed interviews from both client and provider data sets and drafted summaries which were then systematically reviewed as a team. Following the tenets of thematic analysis and adopting the framework developed by Miles and Huberman (1994) [ 54 ], the team collaboratively identified cross-cutting themes from interview summaries, covering areas of concordance, discordance, and particular importance, as well as exemplar and negative cases. Once major themes and sub-themes were identified and articulated, authors drafted analytic memos which consolidated and explored in detail each major theme.
Following publication of an article focused on findings from the provider data set [ 55 ], further analysis of the client data set included the development of a formal coding scheme (SO), based on a priori codes extracted from the interview guide, as well as codes reflecting themes and sub-themes identified in the summarizing process and further refined via ongoing weekly analytic meetings. Coding was led by the primary qualitative analyst [SO] with secondary coding by client interviewer and author [JO]. The application of codes was discussed regularly among all team members, focusing on discrepancies between primary and secondary coders, insights developed, and the potential emergent themes. Discrepancies occurred approximately 10% of the time, and these were resolved through group consensus in accordance with established qualitative research methods [ 56 ].
Through key informant interviews, we captured diverse perspectives on how existing and emerging drug checking services are being used, and their potential for future impact within the harm reduction suite of services.
We present our findings within three key themes: (1) the role of drug checking in overdose prevention; (2) benefits to the overall agency, health, and wellbeing of people who use drugs; and (3) impacts of drug checking services at the community and systems levels.
The role of drug checking in overdose prevention
Service providers and clients expressed varying opinions on the extent to which information from drug checking services would prevent overdose and, indeed, whether overdose prevention is the appropriate metric by which drug checking’s impact should be measured. Clients reported diverse experiences and perspectives on how they use (or don’t use) drug checking, and expectations for their own future use.
Fentanyl test strips
Almost all client participants reported having had some experience with fentanyl testing strips (FTS), either using them personally or seeing others use them. Attitudes about FTS varied. Some expressed concern that they are difficult to use correctly or that they have heard they may be unreliable (prone to false positives or negatives):
We were using them constantly when they were telling us that all the drugs had fentanyl in them. But then we found out that if you don’t put enough water on speed, that it can come up positive because of some chemical. [Client, 40, female].
Others reported relying on them heavily and using them often:
I’ve just got to have that insurance that there’s no fentanyl in [my drugs]. … I have a drawer. Like that? That’s all full of test strips. Usually every time I come to a needle exchange, if they have them, I grab as many as I can and just put them in the drawer. [Client, 43, male].
Spectrometry
Although many had not heard of spectrometry, spectroscopy, or anything beyond FTS, once it was described what a range of drug checking services could look like, clients were interested and excited about the possibilities. Some expressed interest in using mobile or site-based spectroscopy, but were concerned about their safety, one expressing worry about “ judgment from the community ” or bystanders taking videos and calling the police, another wondering if they would be an “ easy target ” for law enforcement harassment. Those who reported having used FTIR as part of their harm reduction visits, however, had positive things to say:
Interviewer: And how do you feel about that testing service at the van? Participant: I think it’s remarkably great. Interviewer: yeah? Participant: Yeah. They answered my questions, exactly what I wanted to know. [Client, 66, male]
Some participants described high percentages of testing experiences coming back with a positive or unexpected result, like a client who said that he’d used the FTIR mobile service four times with meth from four different suppliers, and “ only one came back pure .”
Using drug checking results
What participants reported doing with the results of checking their drugs varied as well. Some participants spoke about specific situations where drug checking prompted them to avoid buying contaminated drugs.
Actually I just used [drug checking] yesterday. Luckily, I didn’t buy the heroin I was going to, because it tested for fentanyl . [Client, 32, male]
Other community members expressed disinterest in checking drugs, often citing a lack of realistic options for using test results in a way that made sense for them. One participant stated directly that they didn’t want to test because they didn’t want to have to not use drugs if they got a result they didn’t like:
What if it comes up with fentanyl in it? Then I bought it but I can’t do it? They’re not going to take it back, the people I bought it from. I mean even if I get them to write me a receipt, you know? [Client, 49, male]
Another client said that she was interested in drug checking generally, but wouldn’t bother if she only had a little bit and was relying on it to keep her from getting sick:
If I was trying to [check my drugs], I would do it when I had enough to do that, you know. Because if I was dope sick and I only had two hits of fentanyl, I probably would not [test]. [Client, 24, female]
Data from service provider interviews echoed these dynamics. We heard from provider participants that, broadly, drug checking services prevent overdose directly some of the time, but not all the time, by way of individual behavior change on a case-by-case basis. One provider—a clinician with a lengthy career in addiction medicine and harm reduction—echoed doubts about how common it would be for a patient to make use choices based on drug checking results, broadening the focus to personal harm reduction behavior change rather than abstinence behavior alone:
And then the question is, what do you do about it? I’ve had a patient who is, like, yeah, I tested it. It was positive for fentanyl. I go, well, what did you do? Well, we just used anyway because it’s all we had. And we had, like, the Narcan out, and I – I just felt really sleepy afterwards. … So I guess that’s the other question – if you do drug testing and it isn’t what you expect, like, you can’t take it back to the dealer and say, hey, this isn’t – I want a refund; right? So what do you do with that information? And if, you know, if you’re in withdrawal and you really need to use that drug, like, what kind of safeguards are you going to take if you decide, yeah, I’m going to go ahead and use this; right? [Clinician, U.S.]
Other service providers similarly drew a distinction between drug checking sparking behavior change that prevents overdose versus behavior change that reduces the risk of death from overdose, situating drug checking services as a set of tools that dovetail with existing personal harm reduction strategies.
The reality is, you know, people still are using their drugs. Now, a large proportion of people who use our service say that they’ll do something differently after, you know, accessing our service, so they maybe will do a test dose first, or start, like, start with a smaller dose, or use with a friend, or use at an SCS [supervised consumption site]. [Direct service provider, Canada].
Overdose prevention versus overdose rates
Interestingly, many service providers when asked for their perspective on the role of drug checking services in overdose prevention expressed concern about a gulf between the overdose prevention they observe at the service level versus what they see represented in population-level data.
Will drug checking save a life? Absolutely. Yes, for sure. Will it, at a population level, drop overdose rates? I don’t know the answer to that. [Researcher, U.S.]
Participants offered multiple explanations for this. One described challenges inherent in proving prevention, while another explained how population overdose rates can obscure the impact of drug checking programs when they operate within a rapidly-changing drug supply:
It will be very hard to prove within these prevention paradoxes. I think prevention is one of those things that is so important, but within our scientific frameworks … preventable events are so rare and on the grand scheme of things, they’re really hard to prove. … But will [DCS] save lives? Yeah. [Clinician, U.S.] The numbers aren’t showing [an overall decrease in overdose], right, because at the same time, even though we’re offering this service, the supply is just getting worse and worse, so overdose rates are rising. [Direct service provider, Canada].
Not every participant who commented on this gulf found it to be wide or troubling, but instead remarked on it as a neutral distance between two related but distinct constructs, one of which is a measure of what outcomes drug checking information could yield, and the other of which is a fundamental right to that information.
It’s really a great question if we’re going to see things pan out in the numbers. I certainly hope so and I certainly think so, but I think that we just have the right to know what we’re putting into our bodies, regardless of what outcome measures are. We deserve to know what’s in our drugs . [Direct service provider, U.S.]
Similarly, a direct service provider offered a structural perspective on overdose prevention, decoupling the value of drug checking services from overdose outcomes, prioritizing instead the intrinsic value of equipping people with critical information about what they are putting in their body and the importance of empowering people to make decisions with as much information as possible.
I don’t really know if [drug checking] is going to decrease the rate of overdose. In my mind, the problems that contribute to overdose are prohibition, law enforcement harassment, and everything that surrounds that that creates a shitty drug supply and then prevents people from investigating it. But what [drug checking] does do, again, is this piece around like, people should know that they can find out there’s more in their drug. … I think that it just enables people to make better educated decisions around their substance use and to understand their bodies better . [Direct service provider, U.S.]
Benefits to the overall agency, health, and wellbeing of people who use drugs
Drug checking services offer users the tools to independently identify risks in the drug supply and make decisions about what to do with that information in the short and long term. Many of the service providers interviewed for this study, when asked how drug checking would impact overdose rates, gave some version of a reframed response, repositioning the focus from the drug use decisions themselves to the importance of information in fortifying the overall agency, health, and wellbeing of people who use drugs.
The provider quoted in the above section went on to reflect on the intrinsic value of giving people information, arguing that it contributes to essential experiences of bodily autonomy and health equity:
What’s really important to me as well is just sort of building this momentum around people feeling entitled to bodily autonomy and seeing that [drug checking] is a part of [that], and having folks know that, yeah, they fucking deserve to have this information. They are entitled to know what is in their stuff. And so, that’s not the only piece to health equity and justice around substances and substance use, but I think that it’s a significant piece. [Direct service provider, U.S.]
Knowledge of what is in their drugs can also confirm users’ internal experience. One provider, who had piloted an early drug checking intervention in a major metropolitan area in the U.S., believed that drug checking for people who use drugs offers confirmation of the embodied experience of their substance use, which in this provider’s experience was often regarded with skepticism by health workers:
I think that people are able to connect experiences that they’re feeling in their body with real information. And I think that actually validates the really organic knowledge and experiential knowledge of drug users as the true experts about drugs. You know, when we were doing our project in [city] and fentanyl was not everywhere [yet]—almost 100% of the time, if someone brought us a sample and said, “I think this has fentanyl in it,” it was true. … It validates experience where people’s experiential knowledge is not really validated by an educational system. It’s always this kind of thing where public health people are telling drug users what’s true. And drug checking sort of validates that drug users actually know what’s true, and we’re just using science to confirm it.” [Direct service provider, U.S.]
Client interviews echoed this theme. Several clients recounted experiences that illustrated how navigating the drug market is becoming increasingly difficult, and that drug checking provides an important tool that they can pair with their own instincts and expertise as they try to keep themselves safe.
I can look at it and I can be like, “Wait a minute, we might want to test that.” Because speed and fentanyl are different. They actually look different than the other one, so when I start seeing traces of fentanyl being in the speed, I go, “We need to check that before we do any of it.” And, hey, sometimes I’m wrong. [Client, 43, male] The [meth] that was in the medicine bottle [tested positive for fentanyl], yeah. But I kind of knew it was going to because I packed a bowl right before and if it’s dirty … yeah, the color starts changing wrong right away. [Client, 43, male] I like that [drug checking] gives us some certainty of what’s in the drug … like with the heroin, there was stuff in that that just did not feel good. I’d love to know what they were cutting that stuff with. We used to joke it was shoe polish because it was so dark and dirty, but it’s really important what you put in your body . [Client, 48, female]
Our client data further provide evidence that people who use drugs are making health-related decisions for themselves and care about their own health and wellbeing. Woven throughout community member interviews were examples of health-seeking decision-making in users’ everyday lives, demonstrating agency in considering health behaviors and expressing both implicitly and explicitly a desire to care for themselves. Examples of these pro-health micro-decisions include choosing not to smoke out of foil (it’s “ not healthy to smoke out of ” and “ it’s going to give us Alzheimer’s or something ”) or reducing smoking marijuana due to a “ sensitive ” respiratory system. One informant laid out explicitly their hopes for their future, shaped too by an acute awareness of the risks of the current drug market:
I don’t want to be a statistic out here. I want to go back to regular life and experience all the rest of the highs that there still are out there before I die. I want to jump out of an airplane, or take a balloon ride, or ride more rollercoasters. … I don’t want to limit myself to one freaking high. … it’s not worth it anymore at all. … You’d never OD on meth before. Meth and weed were two things you just didn’t overdose on. If you did too much, you passed out and you slept it off and that was it. Now, no matter what drugs you’re doing, every time you use, it’s a 50–50 chance that you could die. [Client, 49, female]
These excerpts from client interviews highlight the demand among potential DCS users for strategies that contribute to their agency, health, and wellbeing, even within the context of continued drug use in the short- or long-term.
Impacts of drug checking services at community and systems levels
In addition to use at the individual level, participants talked extensively about the ways that they experience and imagine DCS having an impact at community and systems levels. They described the ways that drug checking could facilitate upstream regulation of the drug market, how the information and transparency made possible by checking drugs can fill a policy and regulatory vacuum, and how drug checking can empower public health surveillance systems and clinical response.
Community level regulation of the drug market
Multiple informants, both service providers and clients, reflected on the use—or potential use—of drug checking as a grassroots tool to regulate the drug market.
Participants talked about using, or thinking one could use, DCS as a vetting tool for sellers or suppliers.
And if people could get their shit tested, almost every time if not every time, not only would it help them to be safer by them regulating themselves and knowing what’s in their stuff … But I feel like if they knew exactly what was in it, they could go tell their guys that they got it from, “Look, man, I’m not buying that shit anymore if it’s like that. If that shit -- if this or that’s in it or whatever. Or if you don’t, whatever, I’m not buying it from you. I’m buying it from someone else.” And that might even make them be… It’ll hold them more accountable. [Client, 32, male]
This use was so important to one participant that they expressed interest in their samples being sent for more extensive in-lab spectrometry testing that could give them greater detail about the compounds and amounts in their sample:
Hey, [a full spectrometry report] may take a week, but at least in that week, I find out if I should go back to that person or not. [Client, 43, male]
Client participants frequently referred to DCS as a tool to “keep [suppliers] honest”; that is, as informal regulatory pressure on currently unregulated illegal drug markets. Some reported that they spread the word if drugs from a supplier come up contaminated or low-grade. One participant, who uses fentanyl, reported using FTS to ensure that what they are about to buy is, indeed, fentanyl:
I keep them [FTS] around. … Then I say, “Can I test it?” and I test it in front of them. And like some of it’s turned up negative. And so I totally outed them out on the block with it. It pisses them off – it kind of keeps them honest. … When you got a bunch of test strips, I can go down the line and keep, yeah, at least trying to keep them honest, you know. I got a pile of those things right now. That’s actually what I use them for. [Client, 40, male]
Of particular value, according to our participants, was the idea that spectrometry would provide formal documentation of drugs’ contents. Analytical evidence that something was either dangerously contaminated or not what the seller claimed it to be can shift the balance of power in the transactional dynamic, placing upstream pressure on suppliers to better monitor what they are contributing to the market.
If you could get results that are on paper or on a text or on a whatever, then you could bring it to them that, “Look, dude. I’m not fucking around. You need to make this shit right or I’m not buying it anymore.” That would be a game-changer . [Client, 32, male]
From the service provider standpoint, one participant, a drug checking technician and program manager with a longstanding history in their city’s drug scene, identified similar opportunities for DCS to impact the drug market, were it made easily accessible to those at multiple points in the drug supply chain in addition to consumers.
It’s not just people who are consuming the drugs that can use the service. It’s also people who are selling them. And so, oftentimes people who are not essentially the first or second hands that are creating the substance and then moving it down the chain towards the end consumer, they don’t know what is in their product. For folks who are selling drugs, if they’re able to come and get an ingredient list, they can then kind of know what to say to folks who are buying. [Direct service provider, U.S.]
This was not discussed as just a hypothetical. One informant who sells drugs validated this use as feasible and valuable:
I want to make sure what I’m buying is what it is. … I do sell it myself, so [spectrometry]’s a good service because that’s what I want to know is the chemical balance as to how much it is and how much it isn’t and whether it’s good every time. [Client, 66, male]
Filling a policy and regulatory vacuum
In the absence of a government or regulatory body that will monitor and report on the verified contents of illicit drugs, our data suggest that drug checking services, and spectrometry in particular, may be filling a policy and regulatory vacuum.
Clients likened the idea of having access to a list of drugs present in a sample to knowing ingredients of something that they would eat.
I mean we know what’s in our food, right? The packaging is all labeled and the ingredients are listed. It’s just too important, especially with drugs. Especially because we don’t know who’s making them. We don’t know exactly where they’re coming from. And every single one is different. Every week is different. Even if you buy it from the same person all the time, they’re always having something different. Maybe you’ll have the same thing twice or three times but that’s it. [Client, 48, female]
Providers, meanwhile, explicitly framed the value of drug checking within the context of an unmet regulatory need. One service provider qualified many of their statements about drug checking services with “until prohibition goes away,” situating DCS as being necessary only in a regulatory vacuum. Another spoke more directly to the relationship between drug checking and regulation:
And with drugs, because of prohibition, we just have this unknown, unregulated supply, and people are – what they’re putting in their bodies and what they’re purchasing is obscured, right? And so, drug checking is like a series of sort of imperfect tools to help consumers of drugs regain a little bit of control in the form of information around what it is that they are using. …. And there’s a very good argument that, if we had some kind of safe, regulated supply, we wouldn’t need drug checking at all, which is true . [Direct service provider, U.S.]
Empowering public health surveillance systems and clinical response
Data from our interviews suggest that drug checking technologies and programming may also contribute meaningfully at a structural level, to public health surveillance systems and clinical response. Aggregated sample results provide real-time data about what drug compositions are trending across regions, and what the clinical implications may be for providers treating clients who use drugs [ 57 ]. One drug checking program team posted results to their website in the hopes of informing local clinicians and public health policy makers about what was circulating in the drug supply. This program manager talked about making results available “at the societal level”:
And then at the kind of societal level what we do … [is] every other week we take all of the results from the samples that we’ve checked, and we combine them, and then we put out a report and update our website about, like, what’s circulating in the drug supply. So we talk about, you know, trends in the drug supply over that period, and new drugs that have been introduced, and what those drugs could mean, that type of thing. So service doesn’t only benefit individuals, but it also benefits the larger community by being able to say, okay, this is what we’re seeing. If you can’t access the service, you still at least know, you know, what is circulating. [Direct service provider, Canada]
Community members expressed an awareness of this function. One participant cited drug checking’s role in a larger tracking network as one of the things they value most about the service:
I liked a lot about [drug checking]. One, that it was available in the first place. Two, that it was not just doing its own thing. It was part of a larger network that was keeping track of what drugs were popping up on the streets and what their makeup was. I really like that that’s happening. [Client, 30, male]
At the point-of-service level, provider informants discussed significant benefits that drug checking could provide to clinicians and other medical professionals who work closely with people who use drugs. This informant posited specifically that having more detailed knowledge about what was circulating in the drug supply could help clinicians better formulate strategies for managing opioid use disorder and transitioning patients onto MOUD:
Understanding what’s actually in the supply… allows clinicians to tailor the care that they are providing to people who use drugs. So, you know, if they know that the average amount of fentanyl in a fentanyl sample is this and they want to transition someone off the unregulated drug supply onto, like, a pharmaceutical alternative, well, what pharmaceutical alternative is actually suitable based on what they’ve been using? [Direct service provider, Canada]
This is especially critical given the significant difficulties that have been recently reported when transitioning people using fentanyl to appropriate longitudinal services [ 58 ]. A provider we interviewed who runs a mail-based drug checking service in the U.S. reported that developing a more thorough knowledge of the drug supply outside of the current surveillance panoply may provide important clinical toxicology assistance to help physicians connect health outcomes to specific substances or components of the drug supply, and more quickly provide tailored treatment:
There’s one other really big one for me, which is that it allows us to link specific physiological harms with specific chemicals. So, we’re not just talking about dope anymore. We’re talking about this component of dope causing this specific reaction. What we have been able to do is, we’ll get calls from our central hospital on campus, and they’ll say, “We have this patient with an idiosyncratic presentation. Boom, boom, boom, boom, boom, boom. Here it is. We think it might be… You know, they’ve been injecting this, this, and this. We have some of their samples. Can we get them tested?” Or if they don’t have the samples, they’re like, “This is what the symptoms are. This is where they’re from. What are you seeing about the drug supply in their area?” And I can be like, “Well, yeah, there’s been a spike in levamisole in that area or xylazine,” you know, whatever it is. And then they can get to treatment quicker because the physicians have a more specific knowledge about the ideology of the harm that they’re observing in clinic. [Researcher, U.S.]
Negative cases
While the vast majority of participant responses reflected positive experiences with or attitudes about DCS, some participants additionally expressed ambivalence or concern. Many of these perspectives are embedded within the themes reported above, but deserve reiteration: service users expressed concerns about the accuracy of drug checking technologies, their privacy and safety relative to community stigma and law enforcement, and anxiety about having to make hard choices about drug use in the face of an unexpected result. Service providers expressed concern about the “then what” of drug checking, citing constrained choices and limits to what could be realistically expected in terms of behavior change without other supports in place. Some further lamented the challenges of translating the benefits of what they were seeing in practice to what is visible to a broader audience.
Not included in the above findings, but important to note, are two additional concerns that arose in interviews. First, service users and providers cautioned that the street drug supply changes so quickly that new compounds may be showing up on the street before they are identified in spectrometry libraries, potentially limiting their ability to accurately identify contaminants. Finally, one provider, a clinician with a longstanding career in addiction medicine and harm reduction, closed their interview with a somber caution against decontextualizing drug checking from a broader commitment to multi-method harm reduction, health equity, and social justice.
[I worry that] we’re just throwing yet another technology at a much bigger problem. My fear is that people will say, oh, now we have drug checking, so now we can stop trying to dismantle, you know, structures of racism and oppression in society, right? We can stop looking for homes for people because we have this technology that’s going to prevent people from dying. … It doesn’t work that way. [Clinician, U.S.]
While the magnitude of the opioid crisis is often communicated in terms of overdose and death rates, the harms associated with opioid use—intentional or unintentional—in an unregulated drug market extend far beyond those data points alone, and so too must the strategies leveed to combat them. Our findings demonstrate that drug checking services offer diverse benefits at the individual, community, public health, and health systems levels.
Overdose prevention and beyond
If the question is, do and will these technologies contribute to overdose prevention , our findings suggest that the answer is yes, with some important caveats. The first being that, according to our participants, they do not prevent overdose all the time. Our findings reflect that individuals make complex and highly contextualized decisions regarding their use behavior each time they use drugs. Information about the chemical composition of a drug sample sometimes leads to decisions to abstain, but more often leads to decisions to engage in other types of harm reduction behaviors—like using with a friend rather than alone, making sure to have naloxone on hand, using at a supervised consumption site, alerting others to a bad batch, using a tester first, or avoiding a certain supplier in the future. Sometimes it leads to no observable behavior change at all.
Further, DCS have not been scaled up to meet the needs of everyone at risk for overdose; until it is, it is premature to discuss population-level prevention. This study does not purport DCS to be in and of themselves sufficient to prevent overdose, but they are clearly part of a continuum of services that can prevent overdose mortality.
Many participants took care to note as well that the needs of people who use drugs are not solely to avoid overdose; people navigating drug use are whole people, and the stigmatization and criminalization of drug use regulates their access to a multitude of essential needs and liberties, like health care, housing, employment, agency, and a host of social and legal protections. Access to information that contributes to agency and autonomy, and enables more informed decision-making, is an essential service regardless of other outcomes.
Of course, among harm reductionists and researchers acquainted with the diverse and dynamic ways that harm reduction functions within communities, this is not news. Our findings reflect and reinforce much of the existing evidence from studies aiming to understand the role of drug checking within the larger constellation of harm reduction and, indeed, the role of harm reduction itself.
One recent qualitative study in particular reported themes with striking similarities to the prevailing themes from our interviews. Wallace et al. [ 59 ] explored the potential impacts of community drug checking on prospective service users, finding drug checking to “increase quality control in an unregulated market,” “improve the health and wellbeing of people who use substances,” and “mediate policies around substance use.”
Our findings further add to existing evidence that links drug checking with consumer empowerment within an opaque drug market [ 25 , 26 , 29 ] and underlines the reciprocal relationship between individual agency and the adoption of harm reduction strategies [ 46 , 60 , 61 ].
Of note is the shifting context in which many existing drug checking studies, including ours, are situated. In some areas, fentanyl appears most often as an unwanted adulterant in another drug—be it a non-opioid or a less potent opioid like heroin—and DCS are used primarily for fentanyl avoidance [ 13 , 19 ]. Increasingly, however, pockets of consumers are preferring fentanyl, as seen in our San Francisco client sample and within populations reflected in recent drug checking studies. Our data echo the broader finding that drug checking technologies are likely to be used differently by fentanyl-seeking opioid users versus fentanyl-avoiding opioid users, and differently still among those using stimulants, psychedelics, or other non-opioid drugs [ 22 , 62 ].
On the subject of behavior change—whether and how drug checking can be understood to prompt changes in drug use behavior—our findings align with existing evidence showing that drug checking is at times followed by contaminated drug disposal, and at times followed by the employment of personal harm reduction techniques such as spreading information within the community [ 30 , 63 ], and reduction in polysubstance use or dosage [ 13 , 14 , 15 , 64 ]. Lacking as we do a robust methodological-empirical foundation to assess this type of causality, whether and to what extent drug checking in various contexts leads to less use or more safe use among different populations cannot be stated concretely [ 16 , 65 , 66 ]. Whether individuals change their use behavior based on drug checking results is highly informed by such matters as how limited their access to drugs is, realistic options for modified use, and their perceived relative risks of knowingly ingesting a potentially dangerous compound or compounds versus not.
The tension at the center of harm reduction policy
The role of harm reduction services within communities have long reflected a central tension: in contrast with abstinence and criminalization models, harm reduction is often socially and politically criticized as enabling drug use and making neighborhoods less safe [ 67 , 68 , 69 ], while research consistently finds harm reduction to yield positive outcomes for both service users and surrounding communities [ 70 , 71 ]. In addition to improving the health and wellbeing of people using drugs, evidence suggests that those accessing harm reduction services are more likely to ultimately seek treatment and pursue recovery [ 49 , 70 , 72 , 73 ]. Concerns about public safety, too, while in many cases expressed in good faith, have been shown to be largely misplaced: multiple studies show harm reduction programs to have no significant impact on nearby violent or property-related crime, with some findings suggesting improved indicators of public order and safety [ 48 , 49 , 74 , 75 ]. Harm reduction strategies have additionally been found to be cost-effective in the short term and cost-saving to public monies in the medium- and long-term [ 76 ]. Nonetheless, public perception of harm reduction has historically been interwoven with deeply entrenched cultural stigmas related to race and ethnicity, socioeconomics, and an imprecise moralism that positions access to health and protection as a privilege that should be earned or denied based on behavior [ 67 , 69 , 71 ].
This tension plays out most concretely in the public policy space. Even as the opioid crisis dominates public health discourse and funding is earmarked for research and programming to combat it [ 77 ], harm reduction programs on the ground are under siege. At the federal level, the House Appropriations bill for the Fiscal Year 2024 HHS budget dramatically cuts funding to HIV/AIDS programs—a budget umbrella under which many harm reduction, substance use support and treatment programs are funded [ 78 , 79 ]. In California, a $15.2 million state grant supporting syringe access services has dried up amidst an overdose crisis at its peak, with no plans for replacement [ 80 ]. In 2022, a landmark bill (SB58) that would have authorized overdose prevention programs with supervised consumption in Los Angeles, Oakland, and San Francisco was vetoed by the Governor, despite broad support and robust evidence behind it [ 81 ]. Funds for such safe consumption sites have further been excluded from receiving opioid settlement funds in San Francisco [ 82 ], and in September of 2023, a bill was put forth by the San Francisco Mayor’s office to require drug screening and mandatory treatment for anyone receiving public services [ 83 ]. This, despite the expressly articulated commitment to and acknowledged necessity of harm reduction services—services explicitly aimed at helping people who use drugs to be more safe rather than abstaining from use—highlighted in policy language across multiple levels of government and legislature [ 10 , 84 , 85 , 86 , 87 ].
It is worth noting that one of the harm reduction sites where several of this study’s client participants were receiving services was defunded shortly after we completed data collection, and since then, overdose death rates in the city have climbed [ 88 ] and public order in that area has reportedly deteriorated [ 89 ].
The framing of effectiveness is crucial in this policy environment
In light of these tensions, we offer the findings of this study as a contribution to an evidence base that may play an increasingly central role in California’s—and the nation’s—opioid crisis response. The allowable expenditures for opioid settlement funds list “evidence-informed programs to reduce the harms associated with intravenous drug use” as a focus area [ 51 ] and California’s Overdose Prevention Initiative describes its approach as being “data-driven.” [ 10 ] The proposed HHS FY2024 budget, in addition to cutting much of the funding that covers harm reduction programming, proposes the rejection of “controversial programs” while maintaining funding for “an effective opioid response.” [ 78 ] As California faces a $68 billion budget deficit [ 90 ] and supplementary federal and settlement funds are to be apportioned based on strategy effectiveness and the body of scientific evidence, the role of research comes into sharper focus. It is the strength or weakness of the evidence base—of the complexity of the research inquiry and integrity of the data—that may ultimately frame which initiatives are eligible for support.
When asked about the place and promise of drug checking within the broader constellation of harm reduction services, it was drug users’ humanity and right to health, more so than the public health implications, that grounded many of our participants’ responses. Their responses implicated, too, the underlying operating principle that, ultimately, people make choices that make sense for them. Whether by the hand of addiction or desire, constrained options or access, or every individual’s complex hierarchy of relative dangers and needs, people’s choices are reflections of their full humanity. Approaches to stemming the tide of this crisis cannot be effective unless they are built on respect for the individuals living it, and focused on understanding their needs.
We encourage continued research and reporting on drug checking services and emerging technologies, with an emphasis on exploring effectiveness within a broad scope, reflective of the impacts of these services on whole lives and systems.
Limitations
Many of the community members we interviewed had not heard of spectrometry or spectroscopy, and the interview represented the first time they were introduced to the technology as a concept and the first time they considered whether and how they could see themselves using it in their own lives. This limits the range of our findings among the client sample, given that much of our qualitative data speaks to hypothetical future use rather than past or current use of emerging technologies. The absence of data on client use should not be interpreted to mean that participants chose not to use DCS.
Additionally, the sampling frame for clients was limited to one setting, while providers were sampled from across North America, and the small sample size for both groups may have limited saturation. Finally, providers did not reflect all North American regions where drug checking has been implemented, nor all DCS models, limiting the generalizability of findings.
Our manuscript contributes to growing evidence of the effectiveness of drug checking services in mitigating a range of risks associated with substance use, including overdose, and offer diverse benefits at the individual, community, public health, and health systems levels. For that reason, policymakers should consider allocating resources towards its implementation and scale-up in settings impacted by overdose mortality.
Data availability
Due to ethical restrictions, the data generated and analyzed during the current study are not available to those outside the study team. Data and materials are of a sensitive nature, and participants did not consent to transcripts of their interviews being publicly available. Portions of interviews about which editors have questions or concerns may be provided upon request after any details that may risk the confidentiality of the participants beyond de-identification have been removed. Researchers who meet the criteria for access to confidential data may send requests for the interview transcripts to the Human Research Protection Program (HRPP)/IRB at the University of California, San Francisco at 415-476-1814 or [email protected].
Abbreviations
Fourier–Transform Infrared Spectroscopy
Fentanyl testing strips
US Department of Health and Human Services
Medications for opioid use disorder
Volkow ND, Blanco C. The changing Opioid Crisis: development, challenges and opportunities. Mol Psychiatry. 2021;26(1):218–33.
Article PubMed Google Scholar
Ciccarone D. Fentanyl in the US heroin supply: a rapidly changing risk environment. Int J Drug Policy. 2017;46:107–11.
Article PubMed PubMed Central Google Scholar
Dasgupta N, Beletsky L, Ciccarone D. Opioid Crisis: no Easy fix to its Social and Economic determinants. Am J Public Health. 2018;108(2):182–6.
Ciccarone D. The rise of Illicit fentanyls, stimulants and the Fourth Wave of the Opioid Overdose Crisis. Curr Opin Psychiatry. 2021;34(4):344–50.
U.S. Department of Health and Human Services (HHS). List of Public Health Emergency Declarations [Internet]. Administration for Strategic Preparedness & Response. [cited 2023 Oct 11]. https://aspr.hhs.gov:443/legal/PHE/Pages/default.aspx .
Center for Disease Control and Prevention (CDC). Understanding the Opioid Overdose Epidemic [Internet]. 2023. https://www.cdc.gov/opioids/basics/epidemic.html .
Center for Disease Control and Prevention (CDC). Data brief - Overdose deaths in the United States [Internet]. https://www.cdc.gov/nchs/data/databriefs/db457-tables.pdf#4 .
Center for Disease Control and Prevention, National Center for Health Statistics. Drug Overdose Mortality by State [Internet]. 2022. https://www.cdc.gov/nchs/pressroom/sosmap/drug_poisoning_mortality/drug_poisoning.htm .
California Department of Public Health (CDPH) - Substance and Addiction Prevention Branch (SAPB). CDPH Center for Health Statistics and Informatics Vital Statistics - Multiple Cause of Death and California Comprehensive Death Files [Internet]. California Overdose Surveillance Dashboard. [cited 2023 Nov 6]. https://skylab.cdph.ca.gov/ODdash/?tab=CA .
California Department of Public Health (CDPH). Substance and Addiction Prevention Branch. California’s Approach to the Overdose Epidemic [Internet]. [cited 2023 Oct 11]. https://www.cdph.ca.gov/Programs/CCDPHP/sapb/Pages/CA-Approach.aspx .
Barratt MJ, Measham F. What is drug checking. Anyway? Drugs Habits Soc Policy. 2022;23(3):176–87.
Article Google Scholar
Brunt T. Drug checking as a harm reduction tool for recreational drug users: opportunities and challenges. Background paper commissioned by the EMCDDA for Health and social responses to drug problems: a European guide [Internet]. 2017 Oct 30 [cited 2023 Oct 11]; https://apo.org.au/node/219011 .
Peiper NC, Clarke SD, Vincent LB, Ciccarone D, Kral AH, Zibbell JE. Fentanyl test strips as an opioid overdose prevention strategy: findings from a syringe services program in the Southeastern United States. Int J Drug Policy. 2019;63:122–8.
Measham F, Turnbull G. Intentions, actions and outcomes: a follow up survey on harm reduction practices after using an English festival drug checking service. Int J Drug Policy. 2021;95:103270.
Measham F, Simmons H. Who uses drug checking services? Assessing uptake and outcomes at English festivals in 2018. Drugs Habits Soc Policy. 2022;23(3):188–99.
Maghsoudi N, Tanguay J, Scarfone K, Rammohan I, Ziegler C, Werb D, et al. Drug checking services for people who use drugs: a systematic review. Addict Abingdon Engl. 2022;117(3):532–44.
Maghsoudi N, McDonald K, Stefan C, Beriault DR, Mason K, Barnaby L, et al. Evaluating networked drug checking services in Toronto, Ontario: study protocol and rationale. Harm Reduct J. 2020;17(1):9.
Article CAS PubMed PubMed Central Google Scholar
Johns Hopkins Bloomberg School of Public Health and Bloomberg American Health Initiative. Fentanyl Overdose Reduction Checking Analysis Study (FORECAST). Baltimore, MD; 2018.
Krieger MS, Yedinak JL, Buxton JA, Lysyshyn M, Bernstein E, Rich JD, et al. High willingness to use rapid fentanyl test strips among young adults who use drugs. Harm Reduct J. 2018;15(1):7.
Rammohan I, Bouck Z, Fusigboye S, Bowles J, McDonald K, Maghsoudi N, et al. Drug checking use and interest among people who inject drugs in Toronto, Canada. Int J Drug Policy. 2022;107:103781.
Davis CS, Lieberman AJ, O’Kelley-Bangsberg M. Legality of drug checking equipment in the United States: a systematic legal analysis. Drug Alcohol Depend. 2022;234:109425.
Swartz JA, Lieberman M, Jimenez AD, Mackesy-Amiti ME, Whitehead HD, Hayes KL, et al. Current attitudes toward drug checking services and a comparison of expected with actual drugs present in street drug samples collected from opioid users. Harm Reduct J. 2023;20(1):87.
Reagan-Udall Foundation for the FDA. Fentanyl Drug Checking and Screening: Roundtable on Clinical Perspectives [Internet]. 2021. https://reaganudall.org/sites/default/files/2022-06/FTS_Clinician%20Roundtable_Final_Complete%206.30.pdf .
Reagan-Udall Foundation for the FDA. Fentanyl Drug Checking and Screening: Roundtable on Community Perspectives [Internet]. 2021. https://reaganudall.org/sites/default/files/2022-06/FTS_Community%20Roundtable_Final_Complete%206.30.pdf .
Weicker NP, Owczarzak J, Urquhart G, Park JN, Rouhani S, Ling R, et al. Agency in the fentanyl era: exploring the utility of fentanyl test strips in an opaque drug market. Int J Drug Policy. 2020;84:102900.
Bardwell G, Boyd J, Arredondo J, McNeil R, Kerr T. Trusting the source: the potential role of drug dealers in reducing drug-related harms via drug checking. Drug Alcohol Depend. 2019;198:1–6.
Long V, Arredondo J, Ti L, Grant C, DeBeck K, Milloy MJ, et al. Factors associated with drug checking service utilization among people who use drugs in a Canadian setting. Harm Reduct J. 2020;17(1):100.
Carroll JJ, Rich JD, Green TC. The protective effect of trusted dealers against opioid overdose in the U.S. Int J Drug Policy. 2020;78:102695.
Betsos A, Valleriani J, Boyd J, Bardwell G, Kerr T, McNeil R. I couldn’t live with killing one of my friends or anybody: a rapid ethnographic study of drug sellers’ use of drug checking. Int J Drug Policy. 2021;87:102845.
Wallace B, Hills R, Rothwell J, Kumar D, Garber I, van Roode T, et al. Implementing an integrated multi-technology platform for drug checking: Social, scientific, and technological considerations. Drug Test Anal. 2021;13(4):734–46.
Article CAS PubMed Google Scholar
McCrae K, Tobias S, Grant C, Lysyshyn M, Laing R, Wood E, et al. Assessing the limit of detection of Fourier-transform infrared spectroscopy and immunoassay strips for fentanyl in a real-world setting. Drug Alcohol Rev. 2020;39(1):98–102.
Center for Disease Control and Prevention (CDC). Fentanyl Test Strips: A Harm Reduction Strategy [Internet]. 2023 [cited 2023 Oct 11]. https://www.cdc.gov/stopoverdose/fentanyl/fentanyl-test-strips.html .
Miller A. More states allow fentanyl test strips as a tool to prevent overdoses [Internet]. CNN. 2022 [cited 2023 Oct 12]. https://www.cnn.com/2022/05/04/health/fentanyl-test-strips-khn/index.html .
Green TC, Park JN, Gilbert M, McKenzie M, Struth E, Lucas R, et al. An assessment of the limits of detection, sensitivity and specificity of three devices for public health-based drug checking of fentanyl in street-acquired samples. Int J Drug Policy. 2020;77:102661.
Park JN, Frankel S, Morris M, Dieni O, Fahey-Morrison L, Luta M, et al. Evaluation of fentanyl test strip distribution in two Mid-atlantic syringe services programs. Int J Drug Policy. 2021;94:103196.
Laing MK, Ti L, Marmel A, Tobias S, Shapiro AM, Laing R, et al. An outbreak of novel psychoactive substance benzodiazepines in the unregulated drug supply: preliminary results from a community drug checking program using point-of-care and confirmatory methods. Int J Drug Policy. 2021;93:103169.
Harper L, Powell J, Pijl EM. An overview of forensic drug testing methods and their suitability for harm reduction point-of-care services. Harm Reduct J. 2017;14(1):52.
Tupper KW, McCrae K, Garber I, Lysyshyn M, Wood E. Initial results of a drug checking pilot program to detect fentanyl adulteration in a Canadian setting. Drug Alcohol Depend. 2018;190:242–5.
Borden SA, Saatchi A, Vandergrift GW, Palaty J, Lysyshyn M, Gill CG. A new quantitative drug checking technology for harm reduction: pilot study in Vancouver, Canada using paper spray mass spectrometry. Drug Alcohol Rev. 2022;41(2):410–8.
Gozdzialski L, Wallace B, Hore D. Point-of-care community drug checking technologies: an insider look at the scientific principles and practical considerations. Harm Reduct J. 2023;20:39.
Barry CL. Fentanyl and the evolving opioid epidemic: what strategies should Policy makers consider? Psychiatr Serv Wash DC. 2018;69(1):100–3.
Tsai AC, Kiang MV, Barnett ML, Beletsky L, Keyes KM, McGinty EE, et al. Stigma as a fundamental hindrance to the United States opioid overdose crisis response. PLOS Med. 2019;16(11):e1002969.
Khan GK, Harvey L, Johnson S, Long P, Kimmel S, Pierre C, et al. Integration of a community-based harm reduction program into a safety net hospital: a qualitative study. Harm Reduct J. 2022;19:35.
Kulesza M, Teachman BA, Werntz AJ, Gasser ML, Lindgren KP. Correlates of public support toward federal funding for harm reduction strategies. Subst Abuse Treat Prev Policy. 2015;10:25.
Socia KM, Stone R, Palacios WR, Cluverius J. Focus on prevention: the public is more supportive of overdose prevention sites than they are of safe injection facilities. Criminol Public Policy. 2021;20(4):729–54.
Vearrier L. The value of harm reduction for injection drug use: a clinical and public health ethics analysis. Dis–Mon DM. 2019;65(5):119–41.
Csák R, Shirley-Beavan S, McHenry AE, Daniels C, Burke-Shyne N. Harm reduction must be recognised an essential public health intervention during crises. Harm Reduct J. 2021;18:128.
Levengood TW, Yoon GH, Davoust MJ, Ogden SN, Marshall BDL, Cahill SR, et al. Supervised Injection facilities as Harm reduction: a systematic review. Am J Prev Med. 2021;61(5):738–49.
Kennedy MC, Karamouzian M, Kerr T. Public Health and Public Order Outcomes Associated with supervised drug Consumption facilities: a systematic review. Curr HIV/AIDS Rep. 2017;14(5):161–83.
Plaintiff’s Executive Committee. National Opioids Settlement [Internet]. [cited 2023 Oct 11]. https://nationalopioidsettlement.com/ .
California Department of Heathcare Services (DHCS). California’s Opioid Settlements [Internet]. https://www.dhcs.ca.gov/provgovpart/Pages/California-Opioid-Settlements.aspx .
California Department of Heathcare Services (DHCS). Janssen & Distributors Settlement Funds Allowable Expenditures [Internet]. https://www.dhcs.ca.gov/Documents/CSD/CA-OSF-Allowable-Expenses.pdf .
SocioCultural R, Consultants LLC. Dedoose 9.0.17, web application for managing, analyzing, and presenting qualitative and mixed method research data. Los Angeles, CA; 2021.
Miles M, Huberman A. Qualitative data analysis: an expanded sourcebook. 2nd ed. Sage; 1994.
Ondocsin J, Ciccarone D, Moran L, Outram S, Werb D, Thomas L, et al. Insights from drug checking programs: Practicing Bootstrap Public Health whilst Tailoring to local drug user needs. Int J Environ Res Public Health. 2023;20(11):5999.
Saldaña J. The coding manual for qualitative researchers. London: Sage; 2009.
Google Scholar
Ciccarone D, Ondocsin J, Mars S. Heroin uncertainties: exploring users’ perceptions of fentanyl-adulterated and -substituted ‘heroin’. Int J Drug Policy. 2017;46:146–55.
Duber HC, Barata IA, Cioè-Peña E, Liang SY, Ketcham E, Macias-Konstantopoulos W, et al. Identification, management, and transition of care for patients with opioid Use Disorder in the Emergency Department. Ann Emerg Med. 2018;72(4):420–31.
Wallace B, van Roode T, Pagan F, Hore D, Pauly B. The potential impacts of community drug checking within the overdose crisis: qualitative study exploring the perspective of prospective service users. BMC Public Health. 2021;21(1):1156.
Boucher LM, Marshall Z, Martin A, Larose-Hébert K, Flynn JV, Lalonde C, et al. Expanding conceptualizations of harm reduction: results from a qualitative community-based participatory research study with people who inject drugs. Harm Reduct J. 2017;14(1):18.
Gowan T, Whetstone S, Andic T. Addiction, agency, and the politics of self-control: doing harm reduction in a heroin users’ group. Soc Sci Med 1982. 2012;74(8):1251–60.
Beaulieu T, Wood E, Tobias S, Lysyshyn M, Patel P, Matthews J, et al. Is expected substance type associated with timing of drug checking service utilization? A cross-sectional study. Harm Reduct J. 2021;18(1):66.
Ivers JH, Killeen N, Keenan E. Drug use, harm-reduction practices and attitudes toward the utilisation of drug safety testing services in an Irish cohort of festival-goers. Ir J Med Sci 1971 -. 2022;191(4):1701–10.
Mars SG, Ondocsin J, Ciccarone D. Toots, tastes and tester shots: user accounts of drug sampling methods for gauging heroin potency. Harm Reduct J. 2018;15(1):26.
Tilhou AS, Zaborek J, Baltes A, Salisbury-Afshar E, Malicki J, Brown R. Differences in drug use behaviors that impact overdose risk among individuals who do and do not use fentanyl test strips for drug checking. Harm Reduct J. 2023;20(1):41.
Aarhus Universitet. Literature Review of Drug Checking in Nightlife – Methods, Services, and Effects [Internet], Aarhus. Denmark: Center for Rusmiddelforskning, Psykologisk Institut; 2019. https://www.sst.dk/-/media/Udgivelser/2019/Engelsk-version-Litteraturgennemgang-om-stoftest-i-nattelivet.ashx .
Des Jarlais DC. Harm reduction in the USA: the research perspective and an archive to David Purchase. Harm Reduct J. 2017;14(1):51.
Jackson LA, Dechman M, Mathias H, Gahagan J, Morrison K. Safety and danger: perceptions of the implementation of harm reduction programs in two communities in Nova Scotia, Canada. Health Soc Care Community. 2022;30(1):360–71.
Keane H. Critiques of harm reduction, morality and the promise of human rights. Int J Drug Policy. 2003;14(3):227–32.
Armbrecht E, Guzauskas G, Hansen R, Pandey R, Fazioli K, Chapman R. Supervised injection facilities and other supervised consumption sites: effectiveness and value; final evidence report [Internet]. Institute for Clinical and Economic Review; 2021 Jan. https://icer.org/wp-content/uploads/2020/10/ICER_SIF_Final-Evidence-Report_010821.pdf .
Klein A. Harm reduction works: evidence and inclusion in Drug Policy and Advocacy. Health Care Anal HCA J Health Philos Policy. 2020;28(4):404–14.
DeBeck K, Kerr T, Bird L, Zhang R, Marsh D, Tyndall M, et al. Injection drug use cessation and use of North America’s first medically supervised safer injecting facility. Drug Alcohol Depend. 2011;113(2–3):172–6.
Hagan H, McGough JP, Thiede H, Hopkins S, Duchin J, Alexander ER. Reduced injection frequency and increased entry and retention in drug treatment associated with needle-exchange participation in Seattle drug injectors. J Subst Abuse Treat. 2000;19(3):247–52.
Fixler AL, Jacobs LA, Jones DB, Arnold A, Underwood EE. There Goes the Neighborhood? The Public Safety Enhancing Effects of a Mobile Harm Reduction Intervention [Internet]. medRxiv; 2023 [cited 2023 Nov 1]. p. 2023.05.30.23290739. https://www.medrxiv.org/content/ https://doi.org/10.1101/2023.05.30.23290739v1 .
Chalfin A, Del Pozo B, Mitre-Becerril D. Overdose Prevention Centers, Crime, and disorder in New York City. JAMA Netw Open. 2023;6(11):e2342228.
Wilson DP, Donald B, Shattock AJ, Wilson D, Fraser-Hurt N. The cost-effectiveness of harm reduction. Int J Drug Policy. 2015;26:S5–11.
Weiss M, Zoorob M. Political frames of public health crises: discussing the opioid epidemic in the US Congress. Soc Sci Med. 2021;281:114087.
Committee Releases FY, Labor. Health and Human Services, Education, and Related Agencies Appropriations Bill [Internet]. House Committee on Appropriations - Republicans. 2023 [cited 2023 Oct 11]. https://appropriations.house.gov/news/press-releases/committee-releases-fy24-labor-health-and-human-services-education-and-related .
San Francisco AIDS, Foundation. Devastating cuts proposed to Federal HIV budget [Internet]. San Francisco AIDS Foundation. 2023 [cited 2023 Oct 11]. https://www.sfaf.org/collections/breaking-news/devastating-cuts-proposed-to-federal-hiv-budget/ .
Emily Alpert Reyes. Amid an overdose crisis, a California grant that helped syringe programs is drying up. Los Angeles Times [Internet]. 2023 Feb 19 [cited 2023 Oct 11]; https://www.latimes.com/california/story/2023-02-19/overdose-california-grant-syringe-programs .
Healthright 360. Outrage at Governor Newsom’s decision to veto SB 57, landmark overdose prevention bill | News | HealthRIGHT 360 [Internet]. [cited 2023 Oct 11]. https://www.healthright360.org/news/outrage-governor-newsom%E2%80%99s-decision-veto-sb-57-landmark-overdose-prevention-bill# .
Sjostedt D. SF Can’t Use Opioid Settlement on Drug Sites, Attorney Says. The San Francisco Standard [Internet]. 2023 Jan 21 [cited 2023 Oct 11]; https://sfstandard.com/2023/01/20/san-francisco-cant-use-opioid-settlement-funds-for-drug-sites-attorney-says/ .
City and County of San Francisco - News. Mayor London Breed Announces New Initiative to Require Screening and Treatment for Substance Use Disorder in Order to Receive County-Funded Cash Assistance | San Francisco [Internet]. [cited 2023 Oct 11]. https://sf.gov/news/mayor-london-breed-announces-new-initiative-require-screening-and-treatment-substance-use .
Executive Office of the President, Office of National Drug Control Policy. The Biden-Harris Administration’s Statement of Drug Policy Priorities for Year One [Internet]. Washington, DC; https://www.whitehouse.gov/wp-content/uploads/2021/03/BidenHarris-Statement-of-Drug-Policy-Priorities-April-1.pdf .
U.S. Department of Health and Human Services (HHS). Harm Reduction [Internet]. Overdose Prevention Strategy. 2021 [cited 2023 Oct 11]. https://www.hhs.gov/overdose-prevention/harm-reduction .
California Department of Public Health (CDPH). Substance and Addiction Prevention Branch. OPI Landing Page [Internet]. Overdose Prevention Initiative (OPI). [cited 2023 Oct 11]. https://www.cdph.ca.gov/Programs/CCDPHP/sapb/Pages/OPI-landing.aspx .
Center for Disease Control and Prevention (CDC). Opioid Rapid Response Program (ORRP) | Opioids | CDC [Internet]. 2022 [cited 2023 Oct 11]. https://www.cdc.gov/opioids/opioid-rapid-response-program.html .
Thadani T, Jung Y. After Mayor Breed’s Tenderloin Center closed, S.F. overdose deaths jumped. Here’s what the data shows. San Francisco Chronicle [Internet]. [cited 2023 Dec 20]; https://www.sfchronicle.com/sf/article/sf-mayor-breed-overdose-tenderloin-center-fentanyl-17846320.php .
Quintana S. Closure of SF’s Controversial Tenderloin Linkage Center Creates New Issue for the City [Internet]. NBC Bay Area. 2022. https://www.nbcbayarea.com/news/local/san-francisco/tenderloin-linkage-center-closure/3101390/ .
Petek G. The 2024-25 Budget: California’s Fiscal Outlook [Internet]. Legislative Analyst’s Office; 2023 Dec. https://lao.ca.gov/reports/2023/4819/2024-25-Fiscal-Outlook-120723.pdf .
Download references
Acknowledgements
This study would not have been possible without the client participants who so generously shared insights about their lives and how they access harm reduction services, and our provider key informants and their work on behalf of people who use drugs. The authors would also like to thank the staff of the Northern California HIV/AIDS Policy Research Center who supported the project during its inception, data collection, and writing.
This research was funded by the California HIV/AIDS Research Program (CHRP) to the Northern California HIV/AIDS Policy Research Center (PI Arnold), H21PC3238. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Author information
Authors and affiliations.
Center for AIDS Prevention Studies, Department of Medicine, University of California, San Francisco, CA, 94143, USA
Lissa Moran, Jeff Ondocsin, Simon Outram & Emily A. Arnold
Family & Community Medicine, Department of Medicine, University of California, San Francisco, CA, 94143, USA
Jeff Ondocsin, Daniel Ciccarone & Nicole Holm
Centre on Drug Policy Evaluation, St. Michael’s Hospital, Toronto, ON, M5B 1W8, Canada
Daniel Werb
Division of Infectious Diseases & Global Public Health, UC San Diego School of Medicine, University of California, San Diego, CA, 92093, USA
You can also search for this author in PubMed Google Scholar
Contributions
E.A.A. and D.C. conceptualized and designed the study; J.O., L.M., D.C., and N.H. were responsible for data collection, each conducting in-depth key informant interviews. L.M., J.O., S.O., and E.A.A. analyzed the data. L.M. led the writing of the original manuscript draft with significant contributions from J.O., S.O., and E.A.A. L.M., J.O., D.C., S.O., D.W., N.H., and E.A.A. were directly involved in iterative review and revision. E.A.A. provided supervision, project administration, and funding acquisition. All authors have read and agreed to the submitted version of the manuscript.
Corresponding author
Correspondence to Lissa Moran .
Ethics declarations
Ethics approval and consent to participate.
The study was conducted in accordance with the Declaration of Helsinki and informed consent was obtained from all subjects involved in the study. The study protocol and consent procedures were reviewed and approved by the UCSF IRB (#22-36640) on 12 September 2022.
Consent for publication
Not applicable.
Competing interests
D.W. is a founder of DoseCheck, a commercial entity that is developing a mobile drug checking technology. D.C. reports the following relevant financial relationships during the past 12 months: (1) he is a scientific advisor to Celero Systems; and (2) he has been retained as an expert witness in ongoing prescription opioid litigation by Motley Rice, LLP. The remaining authors have no relevant financial or non-financial interests to disclose. The remaining authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Moran, L., Ondocsin, J., Outram, S. et al. How do we understand the value of drug checking as a component of harm reduction services? A qualitative exploration of client and provider perspectives. Harm Reduct J 21 , 92 (2024). https://doi.org/10.1186/s12954-024-01014-w
Download citation
Received : 23 January 2024
Accepted : 02 May 2024
Published : 11 May 2024
DOI : https://doi.org/10.1186/s12954-024-01014-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Drug checking
- Harm reduction
- Substance use
- Qualitative
- North america
Harm Reduction Journal
ISSN: 1477-7517
- Submission enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Indian J Med Res
- v.137(6); 2013 Jun
Adolescent drug abuse - Awareness & prevention
Bharath chakravarthy.
The Center of Trauma & Injury Prevention Research- University of California, Irvine- Department of Emergency Medicine, University of California, Irvine School of Medicine, California, USA
Shahram Lotfipour
The abuse of alcohol and illicit and prescription drugs continues to be a major health problem internationally. The United Nations Office on Drugs and Crime (UNODC) reports that approximately 5 per cent of the world's population used an illicit drug in 2010 and 27 million people, or 0.6 per cent of the worlds adult population, can be classified as problem drug users. It is estimated that alcohol abuse results in 2.5 million deaths per year and that heroin, cocaine and other drugs are responsible for 0.1 to 0.2 million deaths per year. In addition to causing death, substance abuse is also responsible for significant morbidity and the treatment of drug addiction creates a tremendous burden on society. UNODC estimates that worldwide costs related to treating drug abuse total $200-$250 billion, or 0.3-0.4 per cent of global GDP; additionally, it is estimated that only 20 per cent of drug users received treatment for their dependence in 2010 1 .
Existing studies have found a high correlation between adolescent abuse and becoming a problem drug user in adulthood 2 ; therefore, it can be inferred that many problem drug users start abusing drugs at an early age. Additionally, accidental and intentional fatalities that are associated with drug and alcohol use represent one of the leading preventable causes of death for the 15 to 24-year-old population. Alcohol and other drug use in the adolescent population carries a high risk for school underachievement, delinquency, teenage pregnancy, and depression 2 .
Preventative science postulates that negative health outcomes, including those resulting from substance abuse, can be prevented by reducing risk factors and enhancing protective factors 3 . The general framework used in this article is based on research presented by the National Institute of Drug Abuse (NIDA) and emphasizes the strategy of targeting modifiable risk factors and enhancing protective factors through family, school and community prevention programmes.
Identify risk factors
Prevention of substance abuse among adolescents requires awareness of characteristics that place youth at risk and targeting risk factors that are modifiable. Many studies have attempted to identify risk factors associated with adolescent drug and alcohol usage.
In its 2010 report titled “Preventing Drug Use Among Children and Adolescents”, NIDA lists several factors that can enhance or mitigate adolescent risk for initiating or continuing to abuse drugs. These factors include exposure to drugs, socio-economic status, quality of parenting, peer group influence and biological/inherent predisposition towards drug addiction 4 . A retrospective study by Dube et al 5 measured correlations between the number of adverse childhood experiences (ACEs) and future substance abuse behaviour. Adverse childhood events included abuse (physical, emotional or sexual), neglect (physical or emotional); growing up with household substance abuse, criminality of household members, mental illness among household members, and parental discord and illicit drug use. The study specifically compared the number of ACEs resulting in a greater likelihood of drug use initiation under 14 yr of age and also compared the number of ACEs associated with increased risk of developing addiction. The study demonstrated that each additional ACE increased the likelihood for drug use under 14 yr of age by two to fourfold and raised the risk of later addiction by five times. People with five or more ACEs were seven to ten times more likely to report illicit drug use than those with none 5 .
Hawkins et al 3 also reviewed many studies that attempted to identify risk factors for adolescent drug abuse. They discussed specific risk factors occurring at the societal/community level and at the individual level. Of the societal risk factors, the following were identified: laws and norms favourable toward behaviour (including lower minimum drinking ages) and availability. Interestingly, socio-economic status did not seem to correlate with increased risk of drug abuse among adolescents; it was only in cases of extreme poverty in conjunction with childhood behavioural problems where increased risk was observed. The personal characteristics that positively correlated with drug and alcohol abuse are numerous and include low harm avoidance, poor impulse control, parents with a history of alcoholism and drug abuse, high levels of family conflict, lack of and/or inconsistent parental discipline, a history of academic failure and a history of antisocial and aggressive behaviour 3 .
Being aware of these risk factors can assist families, health professionals, schools and other community workers with identifying at risk youth and aid in reducing or eliminating risk factors through prevention and treatment programmes.
Prevention programmes
Botvin et al 6 cited several key factors required in prevention programmes to make them effective. These factors include a need to address multiple risk and protective factors, provide developmentally appropriate information relative to the target age group, include material to help young people recognize and resist pressures to engage in drug use, include comprehensive personal and social skills training to build resistance, deliver information through interactive methods and cultural sensitivity that includes relevant language and audiovisual content familiar to the target audience 6 . Successful prevention programmes should incorporate all of these characteristics and can then be provided through the family, school, community or healthcare community.
The 2010 NIDA Report 4 emphasizes both the role of family and community prevention programmes as vital to deterring child and adolescent substance abuse. Their findings are summarized below:
Family prevention programmes: The NIDA Report emphasizes strengthening protective factors through the family, including increasing family bonding and using appropriate discipline. The following family characteristics place children at a higher risk for substance abuse: parent with a history of alcoholism and drug abuse, high levels of family conflict, lack of and/or inconsistent parental discipline. It follows that eliminating these risk factors can reduce the risk of a child/adolescent abusing drugs and alcohol. Once these risk factors are identified, families may benefit from formal prevention programmes that can focus on enhancing family bonding, parenting skills (including communication, rule-setting, appropriate disciplinary actions) and changing parental behaviours that may place a child at risk for later abuse 4 .
One example of a family prevention/treatment programme is multi-dimensional family therapy (MDFT). This is a comprehensive family-based outpatient or partial hospitalization (day treatment) programme for substance-abusing adolescents and those at high risk for continued substance abuse and other problem behaviours. MDFT focuses on helping youth develop more effective coping and problem-solving skills for better decision-making and helps the family improve interpersonal functioning as a protective factor against substance abuse and related problems. Liddle et al 7 compared multi-dimensional family therapy with individual cognitive behavioural therapy (CBT) and found that although both treatments were promising, MDFT was more efficacious in treating substance use problem severity, in addition to creating more long lasting effects than standard CBT.
Community and school prevention programmes: In addition to family programmes, NIDA emphasizes school and community programmes as being beneficial in substance abuse prevention. The Report also suggests introducing programmes at an early-age (pre-school/first grade) to address risk factors for later substance abuse, such as early aggression, poor social skills and academic difficulty.
One of the many examples of school prevention programmes cited in the NIDA Report 4 is Reconnecting Youth (RY); a school-based prevention programme for high school students with poor school achievement and a potential for not completing their education. Participants may also show signs of multiple problem behaviours, such as substance abuse, depression, aggression, or suicidal behaviours. Students are screened for eligibility and then invited to participate in the programme. The programme goals are to increase school performance, reduce drug use, and learn skills to manage mood and emotions. RY blends small group work (10-12 students per class) to foster positive peer bonding, with social skills training in a daily, semester-long class. Early experiments have shown that participation in RY improved school performance (20% improvement in grade point averages), decreased school dropout, reduced hard drug use (by 60%), and decreased drug use control problems, such as progression to heavier drug use 8 , 9 .
Role of healthcare providers in prevention: It is believed that less than 30 per cent of primary care providers perform any screening for substance abuse and as many as 69 per cent do not offer any type of counselling 10 . Hallfors et al 11 cited the following barriers affecting the screening and prevention services in primary care: lack of tested screening tools, lack of knowledge, skills and confidence, financial disincentives (third party services for covering prescription abuse vary widely); and lack of follow up services and resource limitations.
Efforts from paediatricians and primary care providers to overcome these barriers can assist in identifying substance abusers and eventually lead to their treatment.
The abuse of alcohol and drugs has resulted in significant morbidity and mortality among adolescents worldwide. Many of these youth will lose their lives to drugs and alcohol and a significant number are likely to grow up to become problem drug users. Although, the substance abuse problem is complex and large in magnitude, there is a substantial amount of evidence-based research available to physicians, community leaders and schools to implement interventions that can decrease adolescent substance abuse rates. Because this issue is not peculiar to any one community or culture, we recognize that individual interventions may not be universally effective. Therefore, we emphasize the NIDA strategy of targeting modifiable risk factors and enhancing protective factors through family, school and community prevention programmes, as a generalized framework for healthcare and community activists to use when researching programmes and strategies best suited for their own community.
This editorial is published on the occasion of International Day Against Drug Abuse and Illicit Trafficking - June 26, 2013.

IMAGES
VIDEO
COMMENTS
Factors such as peer pressure, physical and sexual abuse, early exposure to drugs, stress, and parental guidance can greatly affect a person's likelihood of drug use and addiction. Development. Genetic and environmental factors interact with critical developmental stages in a person's life to affect addiction risk. Although taking drugs at ...
Recently, DoD made changes to its drug testing program to expand the panel of tested substances to include hydrocodone and benzodiazepines, two of the most widely abused prescription medications. DoD should continue to revise the panel of tested substances as feasible to include the detection of emerging drugs of abuse, such as Spice and bath ...
Effects of Drug Addiction on Behavior. Psychoactive substances affect the parts of the brain that involve reward, pleasure, and risk. They produce a sense of euphoria and well-being by flooding the brain with dopamine. This leads people to compulsively use drugs in search of another euphoric "high.".
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol.When considering other substances, the report estimated that 4.4 million individuals ...
The intervention has not been demonstrated to have benefits for children whose parents abuse drugs or alcohol or those who are not prepared to engage in help-seeking behaviors. The extent to which home visitation benefits families with older children, or families who are already involved in abusive or neglectful behaviors, remains uncertain.
Conclusions. Substance use in adolescence is heterogeneous, ranging from normative to pathological, and can lead to significant acute and long-term morbidity and mortality. ... with 15% of youth meeting diagnostic criteria for alcohol abuse and 16% for drug abuse by age 18 (Swendsen et al. 2012). Tobacco, alcohol, and marijuana are typically ...
Addiction is defined as a chronic, relapsing disorder characterized by compulsive drug seeking and use despite adverse consequences.†. It is considered a brain disorder, because it involves functional changes to brain circuits involved in reward, stress, and self-control. Those changes may last a long time after a person has stopped taking ...
Substance addiction, therefore, is a complex disease whose onset, persistence, and treatment are likely influenced by interactions between genetic, environmental, and pharmacological factors. Substance addiction is a chronic relapsing disorder. Individuals abuse substances for different reasons. There may be personal and mitigating circumstances.
Conclusion. Cannabis production as well as global cannabis seizures rose over the last decade and are now back to the levels of the late 1980s. UNODC's Drug Abuse Trend Index showed an ongoing increase of cannabis use over the last decade and even some acceleration over the 2000-2002 period. Cannabis
Abstract. The use of illicit drugs and the quality of life is intended to provide a rational for a change in some of the present drug policies. After all, the use and the abuse of drugs is largely a health issue and cannot be solved without adequately considering the causes of drug abuse, including the medical, psychiatric, psychological, and ...
Conclusions. Because substance abuse and delinquency are inextricably interrelated, identifying substance-abusing youth in the juvenile justice system is an important first step for intervening in both their substance abuse and their delinquent behavior. Drug identification strategies, followed by effective interventions, help prevent further ...
Tobacco, Alcohol, and Illicit Substances. 7. Conclusions. Drug use and addiction cause a lot of disease and disability in the world. Recent advances in neuroscience may help improve policies to reduce the harm that the use of tobacco, alcohol, and other psychoactive drugs impose on society. Effective action should take into account the following:
The main conclusions from the chapters are drawn. Substance use and gambling indeed permeate our daily lives, and the current way these behaviour ... 6 Drug and alcohol policy for European youth: ... (National Institute of Alcohol Abuse and Alcoholism, 2011; Patra et al., 2011), or the effects of any psychoactive substances on traffic and other ...
Substance abuse during adolescence. The use of substances by youth is described primarily as intermittent or intensive (binge) drinking and characterized by experimentation and expediency (Degenhardt et al., Citation 2016; Morojele & Ramsoomar, Citation 2016; Romo-Avilés et al., Citation 2016).Intermittent or intensive substance use is linked to the adolescent's need for activities that ...
Summary of Findings, Conclusions, and Recommendations. by Patricia M. Wald and Peter Barton Hutt. The Present Problem and Efforts to Control It. A More Promising Approach to Drug Abuse. The Drug Abuse Council. This report, which summarizes the results of the Drug Abuse Survey Project, is based upon extensive reading and numerous interviews with ...
In conclusion, drug abuse rate among adolescents is still increasing hence prevention and control should be emphasized in our country. Awareness and lectures should be given continually to the ...
Conclusion. Drug abuse has many damaging consequences not only for the individual, but also for the society as a whole. Underneath the pleura of social problems is a phenomenally complex mechanism involving tolerance, dependence, and addiction. Multiple brain areas are implicated in many functions such as reward, motivation, learning ...
In conclusion, drug abuse is a significant societal problem with detrimental effects on individuals and communities. It requires a comprehensive approach involving education, prevention, treatment, and enforcement. By addressing the root causes, raising awareness, and providing support to those affected, we can combat drug abuse and create a ...
Substance use disorders (SUDs) represent complex illnesses that disrupt brain activity and function resulting in significant personal and societal repercussions [1,2,3,4].Recognizing the detrimental impact of SUD-related stigma, The National Institute on Drug Abuse has prioritized efforts to understand and diminish this stigma [].Research on mental illness stigma has consistently revealed its ...
Patterns of symptoms resulting from substance use (drugs or alcohol) can help a doctor diagnose a person with a SUD or SUDs and connect them to appropriate treatment. For certain drug types, some symptoms are less prominent, and in some cases, not all symptoms apply. ... Substance Abuse and Mental Health Services Administration. (2023). Key ...
Throughout its history, the U.S. has battled waves of widespread drug addiction. From painkiller addictions on Civil War battlefields to the 1980s era of crack cocaine, each crisis gives way to a new one. Today, however, with new drugs constantly emerging, it's becoming harder to keep up with creating drug screenings and medicine to reverse overdoses.
These types of punitive drug laws, Dunkle said, "cost my boy his life." Opioid crisis:Fueled by fentanyl, drug overdose deaths have quadrupled in past 2 decades As more than 100,000 people ...
Impaired driving is often with alcohol use and frequently leads to accidents, injuries, and fatalities. According to the National Highway Traffic Safety Administration, one person was killed every 39 minutes in an alcohol-related crash in 2021.[1] But alcohol is not the only concern; the use of illicit drugs, legalized drugs such as cannabis, and the abuse of prescription medications may also ...
Drug abuse is a serious problem that adversely affects the health of consumers and can have irreversible consequences (Bryan, 2019; Fuchshuber et al., 2018). Abuse of alcohol and other drugs contributes to both morbidity and mortality. It is important to look at what drives people to abuse drugs and develop addiction. ... Conclusions. From ...
Strangely, exercise and using drugs of abuse act on similar parts of the brain. For example, each similarly activates the reward pathway, triggering the release of feel-good chemicals like ...
Drug Abuse. Drug abuse has an effect on all aspects of life; overall health and wellness‚ family life‚ and the community. With there being so many different kinds of drugs the effects are endless. The effect of drug abuse does not discriminate or focus on any one person. Drug abuse can be found in any area of the world and the overall ...
Conclusion. This study contributes to growing evidence of the effectiveness of drug checking services in mitigating risks associated with substance use, including overdose, through enabling people who use and sell drugs to test their own supply. ... frequency and increased entry and retention in drug treatment associated with needle-exchange ...
Conclusion. The abuse of alcohol and drugs has resulted in significant morbidity and mortality among adolescents worldwide. Many of these youth will lose their lives to drugs and alcohol and a significant number are likely to grow up to become problem drug users. Although, the substance abuse problem is complex and large in magnitude, there is ...