Section 8 of the AMCAS® Application: Essays
New section.
Here you will upload your Personal Comments essay.
- AMCAS® Sign In
Every applicant is required to submit a Personal Comments essay. The available space for this essay is 5,300 characters (spaces are counted as characters), or approximately one page. You will receive an error message if you exceed the available space. Click the "What information should I consider including in my personal comments?" link in the application or see Section 8 of the AMCAS Applicant Guide for suggestions of things to think about when writing this essay.
- If you're applying to an MD-PhD program, you must complete two additional essays: the MD-PhD Essay and the Significant Research Experience Essay.
- To avoid formatting issues, we recommend that you type your essay directly into the AMCAS ® application rather than copying and pasting your essay from other software.
- Alternately, you can draft your essay(s) in text-only word processing software, such as Microsoft Notepad or Mac TextEdit, then copy and paste your essay(s) into the application. Copying formatted text into the application may result in formatting issues that you will not be able to edit after your application is submitted.
- Proofread carefully! There is no “spellchecker” in the AMCAS application, and no changes will be permitted to this section after you have submitted your application.
Send us a message .
Monday-Friday, 9 a.m.-7 p.m. ET Closed Wednesday, 3-5 p.m. ET
The 2025 AMCAS application is now open . If you wish to start medical school in Fall 2025, please complete and submit the 2025 AMCAS application.
As of June 6 AMCAS is:
Marking transcripts as "Received" that were delivered on or before:
Paper (mailed) – June 5
Parchment – June 5
National Student Clearinghouse – June 6
Processing applications that reached "Ready for Review" on May 28.
Processing Academic Change Requests submitted on June 4.
Outline of the current AMCAS application process, policies, and procedures.
This resource is designed to help you prepare your materials for the AMCAS ® application but does not replace the online application.
The application processing fee is $175 and includes one medical school designation. Additional school designations are $46 each. Tax, where applicable, will be calculated at checkout.
If approved for the Fee Assistance Program, you will receive a waiver for all AMCAS fees for one (1) application submission with up to 20 medical school designations ($1,030 value). Benefits are not retroactive.
- Harvard Medical School

HMS Theses and Dissertations
- Communities & Collections
- By Issue Date
- FAS Department
- Quick submit
- Waiver Generator
- Lin, Yan (2)
- Aboelsaad, Iman Ahmed Fathalla (1)
- Acar, Utkucan (1)
- Acharya, Shree (1)
- Afari, Henrietta (1)
- Afinogenova, Yuliya (1)
- Agrawal, Vishesh (1)
- Ajari, Ogheneochuko Winifred (1)
- Akabane, Andressa Lumi (1)
- Akinwunmi, Babatunde Olayode (1)
- ... View More
- Medicine (90)
- Immunology (77)
- Neurosciences (17)
- Oncology (16)
- Education (14)
- Health sciences (14)
- Bioinformatics (10)
- Biology (10)
- Epidemiology (7)
- Genetics (6)
- Scholarly Project (2)
- Honors in a Special Field (1)
- Master of Medical Sciences in Biomedical Informatics (1)
- Master’s Program in Clinical Investigation (1)
- DASH Stories
- Accessibility
- COVID-related Research
- Terms of Use
- Privacy Policy
- By Collections
- By Departments
Recent Submissions
Synthetic genetic circuits for cancer immunotherapy , modeling t cell- b cell interaction in rheumatoid arthritis in a 3d organoid system , the role of gasdermin d in escherichia coli k1 bacterial brain infections .
- Home
Submission Guidelines for Morningside Dissertations and Theses
Benefits to umass chan students of archiving your thesis/dissertation in the escholarship@umasschan repository, requirements prior to submission, before you begin the online submission process, how to submit, what happens next, public access, embargoes, licenses, and subsequent publishing, digital object identifiers (dois), sharing research data publicly, publication and post-publication edits, repository citation and download metrics, removal of content.
- Immediate exposure through Google and other search engines to maximize readership and impact (citations) of your scholarship
- Download statistics are available
- Permanent link, DOI and citation for inclusion on your CV
- Students must follow the graduate school's preparation guidelines for doctoral dissertations and master's theses to ensure that formatting is correct, no required pages are missing, and their thesis/dissertation is properly converted to PDF format. Please make your document is as accessible to users with disabilities as possible. This ensures ease of use and the broadest possible readership for your work. See our accessibility guidelines for authors .
- The student should ensure that their thesis/dissertation is free of errors. Once the graduate school has posted the thesis/dissertation on eScholarship@UMassChan, corrections cannot be made unless the student submits an official request to the Dean of the graduate school.
- The Dissertation Defense Outcome (BBS08) form or the Master's Thesis Outcome (MSCI08) form must be completed and submitted before beginning the electronic submission process in eScholarship@UMassChan.
- Students and their thesis advisor should discuss and reach a mutual agreement regarding which embargo option and which license are appropriate. See Public access, embargoes, licenses, and subsequent publishing for guidelines and a full explanation of options.
- The GSBS19 eScholarship Permission Form must be filled out and signed electronically by the student and the student’s advisor(s). This form certifies that the manuscript is complete and has been approved by the student’s advisory committee, and designates the student’s selections for embargo and re-use rights. Preview GSBS19 form
- Students are required to register for an ORCID and enter their ORCID ID on the GSBS19 eScholarship Permission Form. ORCIDs are unique author identifiers for researchers that are becoming integrated into research workflows. Your ORCID iD ensures you get credit for your work throughout your career and is increasingly a requirement for publication and funding. Registration is free and takes 30 seconds.
Before you begin the online submission process, please be sure you have the following items ready:
- Full text of your final, approved thesis/dissertation in PDF format
- Name of Thesis Advisor(s)
- Your GSBS19 eScholarship Permission Form must first be completed and electronically signed by you and your thesis advisor(s)
- Supplemental files to be displayed on the web page with your thesis/dissertation (e.g. data sets, video clips, sound files), if applicable
- Log into eScholarship@UMassChan using your UMass Chan email address and password
- Click the "Submissions" link in the left sidebar under "My Account"
- Click on "start a new submission"
- Select this collection: UMass Chan Student Research and Publications > Morningside Graduate School of Biomedical Sciences > Morningside GSBS Dissertations and Theses
- Fill in submission form and submit
- NOTE: The Upload File(s) step on the submission form includes an Embargo field. Select a date based on the embargo option you and your advisor chose on your eScholarship permission form. For example, for a 1-year embargo, select a date one year from the submission date. Skip this field if you are not requesting an embargo.
- After reviewing the submission, the graduate school or the library will contact the student for any revisions necessary.
- The library will post the thesis/dissertation in eScholarship@UMassChan within 1-2 weeks of acceptance, with or without an embargo and Creative Commons license as specified on the permission form.
- The student will receive an email with a persistent link to the submission when it is posted.
Students retain ownership of the copyright for the content of their thesis or dissertation, including the right to use all or part of the content in future works. Students are free to register the copyright to their work with the U.S. Copyright Office.
Students are solely responsible for obtaining the rights to use any third-party copyrighted materials, allowing electronic distribution, prior to submission.
The full text of theses and dissertations from the graduate school are made publicly available in UMass Chan Medical School’s repository, Scholarship@UMassChan, unless the student has elected to postpone online access to the full text for a specified time (this is known as an embargo). Students may choose from the following embargo options: no embargo; 6 months; 1 year; 2 years and indicate their choice on the GSBS19 eScholarship Permission Form.
There is a record of each embargoed thesis/dissertation in eScholarship@UMassChan that displays the author name, title, abstract, publication year, GSBS program, advisor, and department affiliations. The record also shows when the embargo will expire. Only the administrators of eScholarship@UMassChan can access the full text of the thesis/dissertation before the embargo expiration date.
Possible reasons to consider an embargo:
- The student is applying for a patent on an invention or procedure documented in the thesis/dissertation and does not wish to make the contents public until the patent application has been filed
- The thesis/dissertation contains sensitive and/or classified information
- Immediate release of the thesis/dissertation may impact an existing or potential publishing agreement
Students often wonder if including unpublished data in a thesis or dissertation precludes later publication in peer-reviewed journals. As publisher policies on previous or duplicate publication vary, it is best to check with the publisher in question. Many publishers include this information on their websites. For example, Nature will consider submissions of material previously published in a thesis or dissertation. The MIT Libraries have compiled a helpful chart summarizing the policies of some publishers. UMass Chan students have the option of utilizing the embargo feature so that the full text of their dissertation is not publicly available while they are in the process of submitting manuscripts for publication in journals.
If students do not request an embargo, or following the expiration of an embargo, the thesis/dissertation will be made publicly available in eScholarship@UMassChan and marked with “All Rights Reserved” or a Creative Commons license as specified by the student.
Creative Commons (CC) licenses are popular tools to facilitate knowledge sharing and creative innovation that copyright holders can apply to their works to indicate how they would like their materials to be used. Those who want to make their work available to the public for limited kinds of uses while preserving their copyright may want to consider using CC licenses. Students have three options to choose from and should select the option that best meets their goals:
- Creative Commons Attribution (CC BY) : This license lets others distribute, remix, tweak, and build upon your work, even commercially, as long as they credit you for the original creation. This is the most accommodating of licenses offered. Recommended for maximum dissemination and use of licensed materials.
- Creative Commons Attribution-NonCommercial (CC BY-NC) : This license lets others remix, tweak, and build upon your work non-commercially, and although their new works must also acknowledge you and be non-commercial, they don’t have to license their derivative works on the same terms.
- Copyright is held by the author, with all rights reserved: This phrase indicates that the student, as the copyright holder, reserves, or holds for their own use, all the rights provided by copyright law, and that nothing may be done with a copyrighted work without their explicit permission.
Students and their thesis advisors should discuss and reach a mutual agreement regarding which embargo option and which Creative Commons license are appropriate. Conflicts between the wishes of the student and the advisor should be resolved before the student completes the GSBS19 eScholarship Permission Form .
Students can direct questions about public access, copyright, embargoes, and subsequent publication to the library .
Students are required to register for an ORCID and enter their ORCID ID on the GSBS19 eScholarship Permission Form. ORCIDs are unique author identifiers for researchers that are becoming integrated into research workflows. Your ORCID iD ensures you get credit for your work throughout your career and is increasingly a requirement for publication and funding. Registration is free and takes 30 seconds.
Theses and dissertations deposited in eScholarship@UMassChan are assigned a DOI (Digital Object Identifier). DOIs are permanent unique identifiers assigned to publications, data, and other scholarly products that make it easier for them to be discovered, cited, and credited.
Students have many options for publicly sharing research data, including government-sponsored repositories such as GenBank or GEO, disciplinary repositories, third-party repositories, and established campus resources such as LabArchives and UMass Chan's institutional repository, eScholarship@UMassChan .
In thesis and dissertation manuscripts, students can include links to research data that has been permanently shared publicly, whether through deposit to a repository or published with a DOI through LabArchives. DOIs are permanent unique identifiers assigned to publications, data, and other scholarly products that make it easier for data to be discovered, cited, and credited. It is recommended that students use a DOI, if available, to link to research data from within their theses and dissertations. Both LabArchives and eScholarship@UMassChan have the ability to assign DOIs to datasets stored and shared with the software.
Students also have the option to upload research data as supplemental files when they are submitting their thesis or dissertation to eScholarship@UMassChan. Data files are displayed on the web page with the thesis or dissertation and download statistics are available.
In all cases, students should make sure that permanent, public data sharing is appropriate. Data should be documented so that it is easier to understand. Good data management practices should be followed, including using standard data and file formats, good null values, and basic quality control (see Ten Simple Rules for the Care and Feeding of Scientific Data ).
Theses and dissertations are published exactly as they are submitted. They are not edited, typeset, or retyped by the graduate school or the library. Therefore, the document’s appearance when it is accessed or printed is entirely the responsibility of the student. The student must assume responsibility for: preparing the document according to the graduate school guidelines for preparation of theses and dissertations; converting the document into Adobe PDF format; checking the document for appearance; and submitting the final, approved PDF document to eScholarship@UMassChan.
Once the graduate school has posted the thesis/dissertation on eScholarship@UMassChan, corrections or retractions cannot be made unless the student submits an official request to the Dean of the graduate school. Since this is the version of record, the full-text cannot simply be swapped out. Changes can be made to the metadata (descriptive information about the thesis/dissertation) but not to the full text. Upon graduate school approval, students will be allowed to upload another version which will display as an additional file, or to submit revised supplemental data as an additional file. The record will be amended to describe the actions/correction.
As the thesis/dissertation is the student’s intellectual property, only the student can initiate a cancellation or an extension of an approved embargo, or a change to a Creative Commons license, by submitting an official request to the Dean of the graduate school. The request should include the reason for the requested change and the desired length of time to extend the embargo.
Posting your thesis/dissertation in eScholarship@UMassChan provides a permanent link and DOI that you can include on a resume or CV. A citation can be exported from the main page of each thesis/dissertation for EndNote, RefWorks, and other formats. Theses and dissertations are available immediately in Google, Google Scholar, and other search engines to maximize readership and impact of your scholarship. The number of full text downloads is updated daily. The download count is available from the thesis/dissertation main page by clicking "Show Statistical Information".
Binding of theses or dissertations is no longer a UMass Chan requirement by the graduate school or the library. The electronic versions will be the version of record. If the student’s department/committee chair requires a print copy, or the student wants print copies, binding arrangements and fees are the sole responsibility of the student. Interested students can consult the graduate school for a recommendation for a local bindery. If you have further questions, please contact the graduate school at [email protected] .
The full text of a work will generally be removed from eScholarship@UMassChan only for reasons such as unethical/ unsound science, plagiarism, copyright infringement, IRB non-compliance and/or violation of the Licensing Agreement. Removal requests should be sent to the GSBS Dean and should include the reason for removal. If the work is removed, a record describing the original version of the paper will always remain on the site at the same URL.
Export search results
The export option will allow you to export the current search results of the entered query to a file. Different formats are available for download. To export the items, click on the button corresponding with the preferred download format.
By default, clicking on the export buttons will result in a download of the allowed maximum amount of items.
To select a subset of the search results, click "Selective Export" button and make a selection of the items you want to export. The amount of items that can be exported at once is similarly restricted as the full export.
After making a selection, click one of the export format buttons. The amount of items that will be exported is indicated in the bubble next to export format.
10 Successful Medical School Essays
Sponsored by.

-- Accepted to: Harvard Medical School GPA: 4.0 MCAT: 522
Sponsored by A ccepted.com : Great stats don’t assure acceptance to elite medical schools. The personal statement, most meaningful activities, activity descriptions, secondaries and interviews can determine acceptance or rejection. Since 1994, Accepted.com has guided medical applicants just like you to present compelling medical school applications. Get Accepted !
I started writing in 8th grade when a friend showed me her poetry about self-discovery and finding a voice. I was captivated by the way she used language to bring her experiences to life. We began writing together in our free time, trying to better understand ourselves by putting a pen to paper and attempting to paint a picture with words. I felt my style shift over time as I grappled with challenges that seemed to defy language. My poems became unstructured narratives, where I would use stories of events happening around me to convey my thoughts and emotions. In one of my earliest pieces, I wrote about a local boy’s suicide to try to better understand my visceral response. I discussed my frustration with the teenage social hierarchy, reflecting upon my social interactions while exploring the harms of peer pressure.
In college, as I continued to experiment with this narrative form, I discovered medical narratives. I have read everything from Manheimer’s Bellevue to Gawande’s Checklist and from Nuland’s observations about the way we die, to Kalanithi’s struggle with his own decline. I even experimented with this approach recently, writing a piece about my grandfather’s emphysema. Writing allowed me to move beyond the content of our relationship and attempt to investigate the ways time and youth distort our memories of the ones we love. I have augmented these narrative excursions with a clinical bioethics internship. In working with an interdisciplinary team of ethics consultants, I have learned by doing by participating in care team meetings, synthesizing discussions and paths forward in patient charts, and contributing to an ongoing legislative debate addressing the challenges of end of life care. I have also seen the ways ineffective intra-team communication and inter-personal conflicts of beliefs can compromise patient care.
Writing allowed me to move beyond the content of our relationship and attempt to investigate the ways time and youth distort our memories of the ones we love.
By assessing these difficult situations from all relevant perspectives and working to integrate the knowledge I’ve gained from exploring narratives, I have begun to reflect upon the impact the humanities can have on medical care. In a world that has become increasingly data driven, where patients can so easily devolve into lists of numbers and be forced into algorithmic boxes in search of an exact diagnosis, my synergistic narrative and bioethical backgrounds have taught me the importance of considering the many dimensions of the human condition. I am driven to become a physician who deeply considers a patient’s goal of care and goals of life. I want to learn to build and lead patient care teams that are oriented toward fulfilling these goals, creating an environment where family and clinician conflict can be addressed efficiently and respectfully. Above all, I look forward to using these approaches to keep the person beneath my patients in focus at each stage of my medical training, as I begin the task of translating complex basic science into excellent clinical care.
In her essay for medical school, Morgan pitches herself as a future physician with an interdisciplinary approach, given her appreciation of how the humanities can enable her to better understand her patients. Her narrative takes the form of an origin story, showing how a childhood interest in poetry grew into a larger mindset to keep a patient’s humanity at the center of her approach to clinical care.
This narrative distinguishes Morgan as a candidate for medical school effectively, as she provides specific examples of how her passions intersect with medicine. She first discusses how she used poetry to process her emotional response to a local boy’s suicide and ties in concern about teenage mental health. Then, she discusses more philosophical questions she encountered through reading medical narratives, which demonstrates her direct interest in applying writing and the humanities to medicine. By making the connection from this larger theme to her own reflections on her grandfather, Morgan provides a personal insight that will give an admissions officer a window into her character. This demonstrates her empathy for her future patients and commitment to their care.
Her narrative takes the form of an origin story, showing how a childhood interest in poetry grew into a larger mindset to keep a patient's humanity at the center of her approach to clinical care.
Furthermore, it is important to note that Morgan’s essay does not repeat anything in-depth that would otherwise be on her resume. She makes a reference to her work in care team meetings through a clinical bioethics internship, but does not focus on this because there are other places on her application where this internship can be discussed. Instead, she offers a more reflection-based perspective on the internship that goes more in-depth than a resume or CV could. This enables her to explain the reasons for interdisciplinary approach to medicine with tangible examples that range from personal to professional experiences — an approach that presents her as a well-rounded candidate for medical school.
Disclaimer: With exception of the removal of identifying details, essays are reproduced as originally submitted in applications; any errors in submissions are maintained to preserve the integrity of the piece. The Crimson's news and opinion teams—including writers, editors, photographers, and designers—were not involved in the production of this article.
-- Accepted To: A medical school in New Jersey with a 3% acceptance rate. GPA: 3.80 MCAT: 502 and 504
Sponsored by E fiie Consulting Group : “ EFIIE ” boasts 100% match rate for all premedical and predental registered students. Not all students are accepted unto their pre-health student roster. Considered the most elite in the industry and assists from start to end – premed to residency. EFIIE is a one-stop-full-service education firm.
"To know even one life has breathed easier because you have lived. This is to have succeeded." – Ralph Waldo Emerson.
The tribulations I've overcome in my life have manifested in the compassion, curiosity, and courage that is embedded in my personality. Even a horrific mishap in my life has not changed my core beliefs and has only added fuel to my intense desire to become a doctor. My extensive service at an animal hospital, a harrowing personal experience, and volunteering as an EMT have increased my appreciation and admiration for the medical field.
At thirteen, I accompanied my father to the Park Home Animal Hospital with our eleven-year-old dog, Brendan. He was experiencing severe pain due to an osteosarcoma, which ultimately led to the difficult decision to put him to sleep. That experience brought to light many questions regarding the idea of what constitutes a "quality of life" for an animal and what importance "dignity" plays to an animal and how that differs from owner to owner and pet to pet. Noting my curiosity and my relative maturity in the matter, the owner of the animal hospital invited me to shadow the professional staff. Ten years later, I am still part of the team, having made the transition from volunteer to veterinarian technician. Saving a life, relieving pain, sharing in the euphoria of animal and owner reuniting after a procedure, to understanding the emotions of losing a loved one – my life was forever altered from the moment I stepped into that animal hospital.
As my appreciation for medical professionals continued to grow, a horrible accident created an indelible moment in my life. It was a warm summer day as I jumped onto a small boat captained by my grandfather. He was on his way to refill the boat's gas tank at the local marina, and as he pulled into the dock, I proceeded to make a dire mistake. As the line was thrown from the dock, I attempted to cleat the bowline prematurely, and some of the most intense pain I've ever felt in my life ensued.
Saving a life, relieving pain, sharing in the euphoria of animal and owner reuniting after a procedure, to understanding the emotions of losing a loved one – my life was forever altered from the moment I stepped into that animal hospital.
"Call 911!" I screamed, half-dazed as I witnessed blood gushing out of my open wounds, splashing onto the white fiberglass deck of the boat, forming a small puddle beneath my feet. I was instructed to raise my hand to reduce the bleeding, while someone wrapped an icy towel around the wound. The EMTs arrived shortly after and quickly drove me to an open field a short distance away, where a helicopter seemed to instantaneously appear.
The medevac landed on the roof of Stony Brook Hospital before I was expeditiously wheeled into the operating room for a seven-hour surgery to reattach my severed fingers. The distal phalanges of my 3rd and 4th fingers on my left hand had been torn off by the rope tightening on the cleat. I distinctly remember the chill from the cold metal table, the bright lights of the OR, and multiple doctors and nurses scurrying around. The skill and knowledge required to execute multiple skin graft surgeries were impressive and eye-opening. My shortened fingers often raise questions by others; however, they do not impair my self-confidence or physical abilities. The positive outcome of this trial was the realization of my intense desire to become a medical professional.
Despite being the patient, I was extremely impressed with the dedication, competence, and cohesiveness of the medical team. I felt proud to be a critical member of such a skilled group. To this day, I still cannot explain the dichotomy of experiencing being the patient, and concurrently one on the professional team, committed to saving the patient. Certainly, this experience was a defining part of my life and one of the key contributors to why I became an EMT and a volunteer member of the Sample Volunteer Ambulance Corps. The startling ring of the pager, whether it is to respond to an inebriated alcoholic who is emotionally distraught or to help bring breath to a pulseless person who has been pulled from the family swimming pool, I am committed to EMS. All of these events engender the same call to action and must be reacted to with the same seriousness, intensity, and magnanimity. It may be some routine matter or a dire emergency; this is a role filled with uncertainty and ambiguity, but that is how I choose to spend my days. My motives to become a physician are deeply seeded. They permeate my personality and emanate from my desire to respond to the needs of others. Through a traumatic personal event and my experiences as both a professional and volunteer, I have witnessed firsthand the power to heal the wounded and offer hope. Each person defines success in different ways. To know even one life has been improved by my actions affords me immense gratification and meaning. That is success to me and why I want to be a doctor.
This review is provided by EFIIE Consulting Group’s Pre-Health Senior Consultant Jude Chan
This student was a joy to work with — she was also the lowest MCAT profile I ever accepted onto my roster. At 504 on the second attempt (502 on her first) it would seem impossible and unlikely to most that she would be accepted into an allopathic medical school. Even for an osteopathic medical school this score could be too low. Additionally, the student’s GPA was considered competitive at 3.80, but it was from a lower ranked, less known college, so naturally most advisors would tell this student to go on and complete a master’s or postbaccalaureate program to show that she could manage upper level science classes. Further, she needed to retake the MCAT a third time.
However, I saw many other facets to this student’s history and life that spoke volumes about the type of student she was, and this was the positioning strategy I used for her file. Students who read her personal statement should know that acceptance is contingent on so much more than just an essay and MCAT score or GPA. Although many students have greater MCAT scores than 504 and higher GPAs than 3.80, I have helped students with lower scores and still maintained our 100% match rate. You are competing with thousands of candidates. Not every student out there requires our services and we are actually grateful that we can focus on a limited amount out of the tens of thousands that do. We are also here for the students who wish to focus on learning well the organic chemistry courses and physics courses and who want to focus on their research and shadowing opportunities rather than waste time deciphering the next step in this complex process. We tailor a pathway for each student dependent on their health care career goals, and our partnerships with non-profit organizations, hospitals, physicians and research labs allow our students to focus on what matters most — the building up of their basic science knowledge and their exposure to patients and patient care.
Students who read her personal statement should know that acceptance is contingent on so much more than just an essay and MCAT score or GPA.
Even students who believe that their struggle somehow disqualifies them from their dream career in health care can be redeemed if they are willing to work for it, just like this student with 502 and 504 MCAT scores. After our first consult, I saw a way to position her to still be accepted into an MD school in the US — I would not have recommended she register to our roster if I did not believe we could make a difference. Our rosters have a waitlist each semester, and it is in our best interest to be transparent with our students and protect our 100% record — something I consider a win-win. It is unethical to ever guarantee acceptance in admissions as we simply do not control these decisions. However, we respect it, play by the rules, and help our students stay one step ahead by creating an applicant profile that would be hard for the schools to ignore.
This may be the doctor I go to one day. Or the nurse or dentist my children or my grandchildren goes to one day. That is why it is much more than gaining acceptance — it is about properly matching the student to the best options for their education. Gaining an acceptance and being incapable of getting through the next 4 or 8 years (for my MD/PhD-MSTP students) is nonsensical.
-- Accepted To: Imperial College London UCAT Score: 2740 BMAT Score: 3.9, 5.4, 3.5A
My motivation to study Medicine stems from wishing to be a cog in the remarkable machine that is universal healthcare: a system which I saw first-hand when observing surgery in both the UK and Sri Lanka. Despite the differences in sanitation and technology, the universality of compassion became evident. When volunteering at OSCE training days, I spoke to many medical students, who emphasised the importance of a genuine interest in the sciences when studying Medicine. As such, I have kept myself informed of promising developments, such as the use of monoclonal antibodies in cancer therapy. After learning about the role of HeLa cells in the development of the polio vaccine in Biology, I read 'The Immortal Life of Henrietta Lacks' to find out more. Furthermore, I read that surface protein CD4 can be added to HeLa cells, allowing them to be infected with HIV, opening the possibility of these cells being used in HIV research to produce more life-changing drugs, such as pre-exposure prophylaxis (PreP). Following my BioGrad laboratory experience in HIV testing, and time collating data for research into inflammatory markers in lung cancer, I am also interested in pursuing a career in medical research. However, during a consultation between an ENT surgeon and a thyroid cancer patient, I learnt that practising medicine needs more than a scientific aptitude. As the surgeon explained that the cancer had metastasised to her liver, I watched him empathetically tailor his language for the patient - he avoided medical jargon and instead gave her time to come to terms with this. I have been developing my communication skills by volunteering weekly at care homes for 3 years, which has improved my ability to read body language and structure conversations to engage with the residents, most of whom have dementia.
However, during a consultation between an ENT surgeon and a thyroid cancer patient, I learnt that practising medicine needs more than a scientific aptitude.
Jude’s essay provides a very matter-of-fact account of their experience as a pre-medical student. However, they deepen this narrative by merging two distinct cultures through some common ground: a universality of compassion. Using clear, concise language and a logical succession of events — much like a doctor must follow when speaking to patients — Jude shows their motivation to go into the medical field.
From their OSCE training days to their school’s Science society, Jude connects their analytical perspective — learning about HeLa cells — to something that is relatable and human, such as a poor farmer’s notable contribution to science. This approach provides a gateway into their moral compass without having to explicitly state it, highlighting their fervent desire to learn how to interact and communicate with others when in a position of authority.
Using clear, concise language and a logical succession of events — much like a doctor must follow when speaking to patients — Jude shows their motivation to go into the medical field.
Jude’s closing paragraph reminds the reader of the similarities between two countries like the UK and Sri Lanka, and the importance of having a universal healthcare system that centers around the just and “world-class” treatment of patients. Overall, this essay showcases Jude’s personal initiative to continue to learn more and do better for the people they serve.
While the essay could have benefited from better transitions to weave Jude’s experiences into a personal story, its strong grounding in Jude’s motivation makes for a compelling application essay.
-- Accepted to: Weill Cornell Medical College GPA: 3.98 MCAT: 521
Sponsored by E fie Consulting Group : “ EFIIE ” boasts 100% match rate for all premedical and predental registered students. Not all students are accepted unto their pre-health student roster. Considered the most elite in the industry and assists from start to end – premed to residency. EFIIE is a one-stop-full-service education firm.
Following the physician’s unexpected request, we waited outside, anxiously waiting to hear the latest update on my father’s condition. It was early on in my father’s cancer progression – a change that had shaken our entire way of life overnight. During those 18 months, while my mother spent countless nights at the hospital, I took on the responsibility of caring for my brother. My social life became of minimal concern, and the majority of my studying for upcoming 12th- grade exams was done at the hospital. We were allowed back into the room as the physician walked out, and my parents updated us on the situation. Though we were a tight-knit family and my father wanted us to be present throughout his treatment, what this physician did was give my father a choice. Without making assumptions about who my father wanted in the room, he empowered him to make that choice independently in private. It was this respect directed towards my father, the subsequent efforts at caring for him, and the personal relationship of understanding they formed, that made the largest impact on him. Though my decision to pursue medicine came more than a year later, I deeply valued what these physicians were doing for my father, and I aspired to make a similar impact on people in the future.
It was during this period that I became curious about the human body, as we began to learn physiology in more depth at school. In previous years, the problem-based approach I could take while learning math and chemistry were primarily what sparked my interest. However, I became intrigued by how molecular interactions translated into large-scale organ function, and how these organ systems integrated together to generate the extraordinary physiological functions we tend to under-appreciate. I began my undergraduate studies with the goal of pursuing these interests, whilst leaning towards a career in medicine. While I was surprised to find that there were upwards of 40 programs within the life sciences that I could pursue, it broadened my perspective and challenged me to explore my options within science and healthcare. I chose to study pathobiology and explore my interests through hospital volunteering and research at the end of my first year.
Though my decision to pursue medicine came more than a year later, I deeply valued what these physicians were doing for my father, and I aspired to make a similar impact on people in the future.
While conducting research at St. Michael’s Hospital, I began to understand methods of data collection and analysis, and the thought process of scientific inquiry. I became acquainted with the scientific literature, and the experience transformed how I thought about the concepts I was learning in lecture. However, what stood out to me that summer was the time spent shadowing my supervisor in the neurosurgery clinic. It was where I began to fully understand what life would be like as a physician, and where the career began to truly appeal to me. What appealed to me most was the patient-oriented collaboration and discussions between my supervisor and his fellow; the physician-patient relationship that went far beyond diagnoses and treatments; and the problem solving that I experienced first-hand while being questioned on disease cases.
The day spent shadowing in the clinic was also the first time I developed a relationship with a patient. We were instructed to administer the Montreal cognitive assessment (MoCA) test to patients as they awaited the neurosurgeon. My task was to convey the instructions as clearly as possible and score each section. I did this as best I could, adapting my explanation to each patient, and paying close attention to their responses to ensure I was understood. The last patient was a challenging case, given a language barrier combined with his severe hydrocephalus. It was an emotional time for his family, seeing their father/husband struggle to complete simple tasks and subsequently give up. I encouraged him to continue trying. But I also knew my words would not remedy the condition underlying his struggles. All I could do was make attempts at lightening the atmosphere as I got to know him and his family better. Hours later, as I saw his remarkable improvement following a lumbar puncture, and the joy on his and his family’s faces at his renewed ability to walk independently, I got a glimpse of how rewarding it would be to have the ability and privilege to care for such patients. By this point, I knew I wanted to commit to a life in medicine. Two years of weekly hospital volunteering have allowed me to make a small difference in patients’ lives by keeping them company through difficult times, and listening to their concerns while striving to help in the limited way that I could. I want to have the ability to provide care and treatment on a daily basis as a physician. Moreover, my hope is that the breadth of medicine will provide me with the opportunity to make an impact on a larger scale. Whilst attending conferences on neuroscience and surgical technology, I became aware of the potential to make a difference through healthcare, and I look forward to developing the skills necessary to do so through a Master’s in Global Health. Whether through research, health innovation, or public health, I hope not only to care for patients with the same compassion with which physicians cared for my father, but to add to the daily impact I can have by tackling large-scale issues in health.
Taylor’s essay offers both a straightforward, in-depth narrative and a deep analysis of his experiences, which effectively reveals his passion and willingness to learn in the medical field. The anecdote of Taylor’s father gives the reader insight into an original instance of learning through experience and clearly articulates Taylor’s motivations for becoming a compassionate and respectful physician.
Taylor strikes an impeccable balance between discussing his accomplishments and his character. All of his life experiences — and the difficult challenges he overcame — introduce the reader to an important aspect of Taylor’s personality: his compassion, care for his family, and power of observation in reflecting on the decisions his father’s doctor makes. His description of his time volunteering at St. Michael’s Hospital is indicative of Taylor’s curiosity about medical research, but also of his recognition of the importance of the patient-physician relationship. Moreover, he shows how his volunteer work enabled him to see how medicine goes “beyond diagnoses and treatments” — an observation that also speaks to his compassion.
His description of his time volunteering at St. Michael's Hospital is indicative of Taylor's curiosity about medical research, but also of his recognition of the importance of the patient-physician relationship.
Finally, Taylor also tells the reader about his ambition and purpose, which is important when thinking about applying to medical school. He discusses his hope of tackling larger scale problems through any means possible in medicine. This notion of using self interest to better the world is imperative to a successful college essay, and it is nicely done here.
-- Accepted to: Washington University
Sponsored by A dmitRx : We are a group of Chicago-based medical students who realize how challenging medical school admissions can be, so we want to provide our future classmates with resources we wish we had. Our mission at AdmitRx is to provide pre-medical students with affordable, personalized, high-quality guidance towards becoming an admitted medical student.
Running has always been one of my greatest passions whether it be with friends or alone with my thoughts. My dad has always been my biggest role model and was the first to introduce me to the world of running. We entered races around the country, and one day he invited me on a run that changed my life forever. The St. Jude Run is an annual event that raises millions of dollars for St. Jude Children’s Research Hospital. My dad has led or our local team for as long as I can remember, and I had the privilege to join when I was 16. From the first step I knew this was the environment for me – people from all walks of life united with one goal of ending childhood cancer. I had an interest in medicine before the run, and with these experiences I began to consider oncology as a career. When this came up in conversations, I would invariably be faced with the question “Do you really think you could get used to working with dying kids?” My 16-year-old self responded with something noble but naïve like “It’s important work, so I’ll have to handle it”. I was 16 years young with my plan to become an oncologist at St. Jude.
As I transitioned into college my plans for oncology were alive and well. I began working in a biochemistry lab researching new anti-cancer drugs. It was a small start, but I was overjoyed to be a part of the process. I applied to work at a number of places for the summer, but the Pediatric Oncology Education program (POE) at St. Jude was my goal. One afternoon, I had just returned from class and there it was: an email listed as ‘POE Offer’. I was ecstatic and accepted the offer immediately. Finally, I could get a glimpse at what my future holds. My future PI, Dr. Q, specialized in solid tumor translational research and I couldn’t wait to get started.
I was 16 years young with my plan to become an oncologist at St. Jude.
Summer finally came, I moved to Memphis, and I was welcomed by the X lab. I loved translational research because the results are just around the corner from helping patients. We began a pre-clinical trial of a new chemotherapy regimen and the results were looking terrific. I was also able to accompany Dr. Q whenever she saw patients in the solid tumor division. Things started simple with rounds each morning before focusing on the higher risk cases. I was fortunate enough to get to know some of the patients quite well, and I could sometimes help them pass the time with a game or two on a slow afternoon between treatments. These experiences shined a very human light on a field I had previously seen only through a microscope in a lab.
I arrived one morning as usual, but Dr. Q pulled me aside before rounds. She said one of the patients we had been seeing passed away in the night. I held my composure in the moment, but I felt as though an anvil was crushing down on me. It was tragic but I knew loss was part of the job, so I told myself to push forward. A few days later, I had mostly come to terms with what happened, but then the anvil came crashing back down with the passing of another patient. I could scarcely hold back the tears this time. That moment, it didn’t matter how many miraculous successes were happening a few doors down. Nothing overshadowed the loss, and there was no way I could ‘get used to it’ as my younger self had hoped.
I was still carrying the weight of what had happened and it was showing, so I asked Dr. Q for help. How do you keep smiling each day? How do you get used to it? The questions in my head went on. What I heard next changed my perspective forever. She said you keep smiling because no matter what happened, you’re still hope for the next patient. It’s not about getting used to it. You never get used to it and you shouldn’t. Beating cancer takes lifetimes, and you can’t look passed a life’s worth of hardships. I realized that moving passed the loss of patients would never suffice, but I need to move forward with them. Through the successes and shortcomings, we constantly make progress. I like to imagine that in all our future endeavors, it is the hands of those who have gone before us that guide the way. That is why I want to attend medical school and become a physician. We may never end the sting of loss, but physicians are the bridge between the past and the future. No where else is there the chance to learn from tragedy and use that to shape a better future. If I can learn something from one loss, keep moving forward, and use that knowledge to help even a single person – save one life, bring a moment of joy, avoid a moment of pain—then that is how I want to spend my life.
The change wasn’t overnight. The next loss still brought pain, but I took solace in moving forward so that we might learn something to give hope to a future patient. I returned to campus in a new lab doing cancer research, and my passion for medicine continues to flourish. I still think about all the people I encountered at St. Jude, especially those we lost. It might be a stretch, but during the long hours at the lab bench I still picture their hands moving through mine each step of the way. I could never have foreseen where the first steps of the St. Jude Run would bring me. I’m not sure where the road to becoming a physician may lead, but with helping hands guiding the way, I won’t be running it alone.
This essay, a description of the applicant’s intellectual challenges, displays the hardships of tending to cancer patients as a milestone of experience and realization of what it takes to be a physician. The writer explores deeper ideas beyond medicine, such as dealing with patient deaths in a way to progress and improve as a professional. In this way, the applicant gives the reader some insight into the applicant’s mindset, and their ability to think beyond the surface for ways to become better at what they do.
However, the essay fails to zero in on the applicant’s character, instead elaborating on life events that weakly illustrate the applicant’s growth as a physician. The writer’s mantra (“keep moving forward”) is feebly projected, and seems unoriginal due to the lack of a personalized connection between the experience at St. Jude and how that led to the applicant’s growth and mindset changes.
The writer explores deeper ideas beyond medicine, such as dealing with patient deaths in a way to progress and improve as a professional.
The writer, by only focusing on grief brought from patient deaths at St. Jude, misses out on the opportunity to further describe his or her experience at the hospital and portray an original, well-rounded image of his or her strengths, weaknesses, and work ethic.
The applicant ends the essay by attempting to highlight the things they learned at St. Jude, but fails to organize the ideas into a cohesive, comprehensible section. These ideas are also too abstract, and are vague indicators of the applicant’s character that are difficult to grasp.
-- Accepted to: New York University School of Medicine
Sponsored by MedEdits : MedEdits Medical Admissions has been helping applicants get into medical schools like Harvard for more than ten years. Structured like an academic medical department, MedEdits has experts in admissions, writing, editing, medicine, and interview prep working with you collaboratively so you can earn the best admissions results possible.
“Is this the movie you were talking about Alice?” I said as I showed her the movie poster on my iPhone. “Oh my God, I haven’t seen that poster in over 70 years,” she said with her arms trembling in front of her. Immediately, I sat up straight and started to question further. We were talking for about 40 minutes, and the most exciting thing she brought up in that time was the new flavor of pudding she had for lunch. All of sudden, she’s back in 1940 talking about what it was like to see this movie after school for only 5¢ a ticket! After an engaging discussion about life in the 40’s, I knew I had to indulge her. Armed with a plethora of movie streaming sights, I went to work scouring the web. No luck. The movie, “My Son My Son,” was apparently not in high demand amongst torrenting teens. I had to entreat my older brother for his Amazon Prime account to get a working stream. However, breaking up the monotony and isolation felt at the nursing home with a simple movie was worth the pandering.
While I was glad to help a resident have some fun, I was partly motivated by how much Alice reminded me of my own grandfather. In accordance with custom, my grandfather was to stay in our house once my grandmother passed away. More specifically, he stayed in my room and my bed. Just like grandma’s passing, my sudden roommate was a rough transition. In 8th grade at the time, I considered myself to be a generally good guy. Maybe even good enough to be a doctor one day. I volunteered at the hospital, shadowed regularly, and had a genuine interest for science. However, my interest in medicine was mostly restricted to academia. To be honest, I never had a sustained exposure to the palliative side of medicine until the arrival of my new roommate.
The two years I slept on that creaky wooden bed with him was the first time my metal was tested. Sharing that room, I was the one to take care of him. I was the one to rub ointment on his back, to feed him when I came back from school, and to empty out his spittoon when it got full. It was far from glamorous, and frustrating most of the time. With 75 years separating us, and senile dementia setting in, he would often forget who I was or where he was. Having to remind him that I was his grandson threatened to erode at my resolve. Assured by my Syrian Orthodox faith, I even prayed about it; asking God for comfort and firmness on my end. Over time, I grew slow to speak and eager to listen as he started to ramble more and more about bits and pieces of the past. If I was lucky, I would be able to stich together a narrative that may or may have not been true. In any case, my patience started to bud beyond my age group.
Having to remind him that I was his grandson threatened to erode at my resolve.
Although I grew more patient with his disease, my curiosity never really quelled. Conversely, it developed further alongside my rapidly growing interest in the clinical side of medicine. Naturally, I became drawn to a neurology lab in college where I got to study pathologies ranging from atrophy associated with schizophrenia, and necrotic lesions post stroke. However, unlike my intro biology courses, my work at the neurology lab was rooted beyond the academics. Instead, I found myself driven by real people who could potentially benefit from our research. In particular, my shadowing experience with Dr. Dominger in the Veteran’s home made the patient more relevant in our research as I got to encounter geriatric patients with age related diseases, such as Alzhimer’s and Parkinson’s. Furthermore, I had the privilege of of talking to the families of a few of these patients to get an idea of the impact that these diseases had on the family structure. For me, the scut work in the lab meant a lot more with these families in mind than the tritium tracer we were using in the lab.
Despite my achievements in the lab and the classroom, my time with my grandfather still holds a special place in my life story. The more I think about him, the more confident I am in my decision to pursue a career where caring for people is just as important, if not more important, than excelling at academics. Although it was a lot of work, the years spent with him was critical in expanding my horizons both in my personal life and in the context of medicine. While I grew to be more patient around others, I also grew to appreciate medicine beyond the science. This more holistic understanding of medicine had a synergistic effect in my work as I gained a purpose behind the extra hours in the lab, sleepless nights in the library, and longer hours volunteering. I had a reason for what I was doing that may one day help me have long conversations with my own grandchildren about the price of popcorn in the 2000’s.
The most important thing to highlight in Avery’s essay is how he is able to create a duality between his interest in not only the clinical, more academic-based side of medicine, but also the field’s personal side.
He draws personal connections between working with Alice — a patient in a hospital or nursing home — and caring intensely for his grandfather. These two experiences build up the “synergistic” relationship between caring for people and studying the science behind medicine. In this way, he is able to clearly state his passions for medicine and explain his exact motives for entering the field. Furthermore, in his discussion of her grandfather, he effectively employs imagery (“rub ointment on his back,” “feed him when I came back from school,” etc.) to describe the actual work that he does, calling it initially as “far from glamorous, and frustrating most of the time.” By first mentioning his initial impression, then transitioning into how he grew to appreciate the experience, Avery is able to demonstrate a strength of character, sense of enormous responsibility and capability, and open-minded attitude.
He draws personal connections between working with Alice — a patient in a hospital or nursing home — and caring intensely for his grandfather.
Later in the essay, Avery is also able to relate his time caring for his grandfather to his work with Alzheimer’s and Parkinson’s patients, showcasing the social impact of his work, as the reader is likely already familiar with the biological impact of the work. This takes Avery’s essay full circle, bringing it back to how a discussion with an elderly patient about the movies reminds him of why he chose to pursue medicine.
That said, the essay does feel rushed near the end, as the writer was likely trying to remain within the word count. There could be a more developed transition before Avery introduces the last sentence about “conversations with my own grandchildren,” especially as a strong essay ending is always recommended.
-- Accepted To: Saint Louis University Medical School Direct Admission Medical Program
Sponsored by Atlas Admissions : Atlas Admissions provides expert medical school admissions consulting and test preparation services. Their experienced, physician-driven team consistently delivers top results by designing comprehensive, personalized strategies to optimize applications. Atlas Admissions is based in Boston, MA and is trusted by clients worldwide.
The tension in the office was tangible. The entire team sat silently sifting through papers as Dr. L introduced Adam, a 60-year-old morbidly obese man recently admitted for a large open wound along his chest. As Dr. L reviewed the details of the case, his prognosis became even bleaker: hypertension, diabetes, chronic kidney disease, cardiomyopathy, hyperlipidemia; the list went on and on. As the humdrum of the side-conversations came to a halt, and the shuffle of papers softened, the reality of Adam’s situation became apparent. Adam had a few months to live at best, a few days at worst. To make matters worse, Adam’s insurance would not cover his treatment costs. With no job, family, or friends, he was dying poor and alone.
I followed Dr. L out of the conference room, unsure what would happen next. “Well,” she muttered hesitantly, “We need to make sure that Adam is on the same page as us.” It’s one thing to hear bad news, and another to hear it utterly alone. Dr. L frantically reviewed all of Adam’s paperwork desperately looking for someone to console him, someone to be at his side. As she began to make calls, I saw that being a physician calls for more than good grades and an aptitude for science: it requires maturity, sacrifice, and most of all, empathy. That empathy is exactly what I saw in Dr. L as she went out of her way to comfort a patient she met hardly 20 minutes prior.
Since high school, I’ve been fascinated by technology’s potential to improve healthcare. As a volunteer in [the] Student Ambassador program, I was fortunate enough to watch an open-heart surgery. Intrigued by the confluence of technology and medicine, I chose to study biomedical engineering. At [school], I wanted to help expand this interface, so I became involved with research through Dr. P’s lab by studying the applications of electrospun scaffolds for dermal wound healing. While still in the preliminary stages of research, I learned about the Disability Service Club (DSC) and decided to try something new by volunteering at a bowling outing.
As she began to make calls, I saw that being a physician calls for more than good grades and an aptitude for science: it requires maturity, sacrifice, and most of all, empathy.
The DSC promotes awareness of cognitive disabilities in the community and seeks to alleviate difficulties for the disabled. During one outing, I collaborated with Arc, a local organization with a similar mission. Walking in, I was told that my role was to support the participants by providing encouragement. I decided to help a relatively quiet group of individuals assisted by only one volunteer, Mary. Mary informed me that many individuals with whom I was working were diagnosed with ASD. Suddenly, she started cheering, as one of the members of the group bowled a strike. The group went wild. Everyone was dancing, singing, and rejoicing. Then I noticed one gentleman sitting at our table, solemn-faced. I tried to start a conversation with him, but he remained unresponsive. I sat with him for the rest of the game, trying my hardest to think of questions that would elicit more than a monosyllabic response, but to no avail. As the game ended, I stood up to say bye when he mumbled, “Thanks for talking.” Then he quickly turned his head away. I walked away beaming. Although I was unable to draw out a smile or even sustain a conversation, at the end of the day, the fact that this gentleman appreciated my mere effort completely overshadowed the awkwardness of our time together. Later that day, I realized that as much as I enjoyed the thrill of research and its applications, helping other people was what I was most passionate about.
When it finally came time to tell Adam about his deteriorating condition, I was not sure how he would react. Dr. L gently greeted him and slowly let reality take its toll. He stoically turned towards Dr. L and groaned, “I don’t really care. Just leave me alone.” Dr. L gave him a concerned nod and gradually left the room. We walked to the next room where we met with a pastor from Adam’s church.
“Adam’s always been like that,” remarked the pastor, “he’s never been one to express emotion.” We sat with his pastor for over an hour discussing how we could console Adam. It turned out that Adam was part of a motorcycle club, but recently quit because of his health. So, Dr. L arranged for motorcycle pictures and other small bike trinkets to be brought to his room as a reminder of better times.
Dr. L’s simple gesture reminded me of why I want to pursue medicine. There is something sacred, empowering, about providing support when people need it the most; whether it be simple as starting a conversation, or providing support during the most trying of times. My time spent conducting research kindled my interest in the science of medicine, and my service as a volunteer allowed me to realize how much I valued human interaction. Science and technology form the foundation of medicine, but to me, empathy is the essence. It is my combined interest in science and service that inspires me to pursue medicine. It is that combined interest that makes me aspire to be a physician.
Parker’s essay focuses on one central narrative with a governing theme of compassionate and attentive care for patients, which is the key motivator for her application to medical school. Parker’s story focuses on her volunteer experience shadowing of Dr. L who went the extra mile for Adam, which sets Dr. L up as a role model for Parker as she enters the medical field. This effectively demonstrates to the reader what kind of doctor Parker wants to be in the future.
Parker’s narrative has a clear beginning, middle, and end, making it easy for the reader to follow. She intersperses the main narrative about Adam with experiences she has with other patients and reflects upon her values as she contemplates pursuing medicine as a career. Her anecdote about bowling with the patients diagnosed with ASD is another instance where she uses a story to tell the reader why she values helping people through medicine and attentive patient care, especially as she focuses on the impact her work made on one man at the event.
Parker's story focuses on her volunteer experience shadowing of Dr. L who went the extra mile for Adam, which sets Dr. L up as a role model for Parker as she enters the medical field.
All throughout the essay, the writing is engaging and Parker incorporates excellent imagery, which goes well with her varied sentence structure. The essay is also strong because it comes back full circle at its conclusion, tying the overall narrative back to the story of Dr. L and Adam, which speaks to Parker’s motives for going to medical school.
-- Accepted To: Emory School of Medicine
Growing up, I enjoyed visiting my grandparents. My grandfather was an established doctor, helping the sick and elderly in rural Taiwan until two weeks before he died at 91 years old. His clinic was located on the first floor of the residency with an exam room, treatment room, X-ray room, and small pharmacy. Curious about his work, I would follow him to see his patients. Grandpa often asked me if I want to be a doctor just like him. I always smiled, but was more interested in how to beat the latest Pokémon game. I was in 8th grade when my grandfather passed away. I flew back to Taiwan to attend his funeral. It was a gloomy day and the only street in the small village became a mourning place for the villagers. Flowers filled the streets and people came to pay their respects. An old man told me a story: 60 years ago, a village woman was in a difficult labor. My grandfather rushed into the house and delivered a baby boy. That boy was the old man and he was forever grateful. Stories of grandpa saving lives and bringing happiness to families were told during the ceremony. At that moment, I realized why my grandfather worked so tirelessly up until his death as a physician. He did it for the reward of knowing that he kept a family together and saved a life. The ability for a doctor to heal and bring happiness is the reason why I want to study medicine. Medical school is the first step on a lifelong journey of learning, but I feel that my journey leading up to now has taught me some things of what it means to be an effective physician.
With a newfound purpose, I began volunteering and shadowing at my local hospital. One situation stood out when I was a volunteer in the cardiac stress lab. As I attached EKG leads onto a patient, suddenly the patient collapsed and started gasping for air. His face turned pale, then slightly blue. The charge nurse triggered “Code Blue” and started CPR. A team of doctors and nurses came, rushing in with a defibrillator to treat and stabilize the patient. What I noticed was that medicine was not only about one individual acting as a superhero to save a life, but that it takes a team of individuals with an effective leader, working together to deliver the best care. I want to be a leader as well as part of a team that can make a difference in a person’s life. I have refined these lessons about teamwork and leadership to my activities. In high school I was an 8 time varsity letter winner for swimming and tennis and captain of both of those teams. In college I have participated in many activities, but notably serving as assistant principle cellist in my school symphony as well as being a co-founding member of a quartet. From both my athletic experiences and my music experiences I learned what it was like to not only assert my position as a leader and to effectively communicate my views, but equally as important I learned how to compromise and listen to the opinions of others. Many physicians that I have observed show a unique blend of confidence and humility.
What I noticed was that medicine was not only about one individual acting as a superhero to save a life, but that it takes a team of individuals with an effective leader, working together to deliver the best care.
College opened me up to new perspectives on what makes a complete physician. A concept that was preached in the Guaranteed Professional Program Admissions in Medicine (GPPA) was that medicine is both an art and a science. The art of medicine deals with a variety of aspects including patient relationships as well as ethics. Besides my strong affinity for the sciences and mathematics, I always have had interest in history. I took courses in both German literature and history, which influenced me to take a class focusing on Nazi neuroscientists. It was the ideology of seeing the disabled and different races as test subjects rather than people that led to devastating lapses in medical ethics. The most surprising fact for me was that doctors who were respected and leaders in their field disregarded the humanity of patient and rather focused on getting results from their research. Speaking with Dr. Zeidman, the professor for this course, influenced me to start my research which deals with the ethical qualms of using data derived from unethical Nazi experimentation such as the brains derived from the adult and child euthanasia programs. Today, science is so result driven, it is important to keep in mind the ethics behind research and clinical practice. Also the development of personalized genomic medicine brings into question about potential privacy violations and on the extreme end discrimination. The study of ethics no matter the time period is paramount in the medical field. The end goal should always be to put the patient first.
Teaching experiences in college inspired me to become a physician educator if I become a doctor. Post-MCAT, I was offered a job by Next Step Test Prep as a tutor to help students one on one for the MCAT. I had a student who stated he was doing well during practice, but couldn’t get the correct answer during practice tests. Working with the student, I pointed out his lack of understanding concepts and this realization helped him and improves his MCAT score. Having the ability to educate the next generation of doctors is not only necessary, but also a rewarding experience.
My experiences volunteering and shadowing doctors in the hospital as well as my understanding of what it means to be a complete physician will make me a good candidate as a medical school student. It is my goal to provide the best care to patients and to put a smile on a family’s face just as my grandfather once had. Achieving this goal does not take a special miracle, but rather hard work, dedication, and an understanding of what it means to be an effective physician.
Through reflecting on various stages of life, Quinn expresses how they found purpose in pursuing medicine. Starting as a child more interested in Pokemon than their grandfather’s patients, Quinn exhibits personal growth through recognizing the importance of their grandfather’s work saving lives and eventually gaining the maturity to work towards this goal as part of a team.
This essay opens with abundant imagery — of the grandfather’s clinic, flowers filling the streets, and the village woman’s difficult labor — which grounds Quinn’s story in their family roots. Yet, the transition from shadowing in hospitals to pursuing leadership positions in high schools is jarring, and the list of athletic and musical accomplishments reads like a laundry list of accomplishments until Quinn neatly wraps them up as evidence of leadership and teamwork skills. Similarly, the section about tutoring, while intended to demonstrate Quinn’s desire to educate future physicians, lacks the emotional resonance necessary to elevate it from another line lifted from their resume.
This essay opens with abundant imagery — of the grandfather's clinic, flowers filling the streets, and the village woman's difficult labor — which grounds Quinn's story in their family roots.
The strongest point of Quinn’s essay is the focus on their unique arts and humanities background. This equips them with a unique perspective necessary to consider issues in medicine in a new light. Through detailing how history and literature coursework informed their unique research, Quinn sets their application apart from the multitude of STEM-focused narratives. Closing the essay with the desire to help others just as their grandfather had, Quinn ties the narrative back to their personal roots.
-- Accepted To: Edinburgh University UCAT Score: 2810 BMAT Score: 4.6, 4.2, 3.5A
Exposure to the medical career from an early age by my father, who would explain diseases of the human body, sparked my interest for Medicine and drove me to seek out work experience. I witnessed the contrast between use of bone saws and drills to gain access to the brain, with subsequent use of delicate instruments and microscopes in neurosurgery. The surgeon's care to remove the tumour, ensuring minimal damage to surrounding healthy brain and his commitment to achieve the best outcome for the patient was inspiring. The chance to have such a positive impact on a patient has motivated me to seek out a career in Medicine.
Whilst shadowing a surgical team in Texas, carrying out laparoscopic bariatric procedures, I appreciated the surgeon's dedication to continual professional development and research. I was inspired to carry out an Extended Project Qualification on whether bariatric surgery should be funded by the NHS. By researching current literature beyond my school curriculum, I learnt to assess papers for bias and use reliable sources to make a conclusion on a difficult ethical situation. I know that doctors are required to carry out research and make ethical decisions and so, I want to continue developing these skills during my time at medical school.
The chance to have such a positive impact on a patient has motivated me to seek out a career in Medicine.
Attending an Oncology multi-disciplinary team meeting showed me the importance of teamwork in medicine. I saw each team member, with specific areas of expertise, contributing to the discussion and actively listening, and together they formed a holistic plan of action for patients. During my Young Enterprise Award, I facilitated a brainstorm where everyone pitched a product idea. Each member offered a different perspective on the idea and then voted on a product to carry forward in the competition. As a result, we came runners up in the Regional Finals. Furthermore, I started developing my leadership skills, which I improved by doing Duke of Edinburgh Silver and attending a St. John Ambulance Leadership course. In one workshop, similar to the bariatric surgeon I shadowed, I communicated instructions and delegated roles to my team to successfully solve a puzzle. These experiences highlighted the crucial need for teamwork and leadership as a doctor.
Observing a GP, I identified the importance of compassion and empathy. During a consultation with a severely depressed patient, the GP came to the patient's eye level and used a calm, non-judgmental tone of voice, easing her anxieties and allowing her to disclose more information. While volunteering at a care home weekly for two years, I adapted my communication for a resident suffering with dementia who was disconnected from others. I would take her to a quiet environment, speak slowly and in a non-threatening manner, as such, she became talkative, engaged and happier. I recognised that communication and compassion allows doctors to build rapport, gain patients' trust and improve compliance. For two weeks, I shadowed a surgeon performing multiple craniotomies a day. I appreciated the challenges facing doctors including time and stress management needed to deliver high quality care. Organisation, by prioritising patients based on urgency and creating a timetable on the ward round, was key to running the theatre effectively. Similarly, I create to-do-lists and prioritise my academics and extra-curricular activities to maintain a good work-life balance: I am currently preparing for my Grade 8 in Singing, alongside my A-level exams. I also play tennis for the 1st team to relax and enable me to refocus. I wish to continue my hobbies at university, as ways to manage stress.
Through my work experiences and voluntary work, I have gained a realistic understanding of Medicine and its challenges. I have begun to display the necessary skills that I witnessed, such as empathy, leadership and teamwork. The combination of these skills with my fascination for the human body drives me to pursue a place at medical school and a career as a doctor.
This essay traces Alex's personal exploration of medicine through different stages of life, taking a fairly traditional path to the medical school application essay. From witnessing medical procedures to eventually pursuing leadership positions, this tale of personal progress argues that Alex's life has prepared him to become a doctor.
Alex details how experiences conducting research and working with medical teams have confirmed his interest in medicine. Although the breadth of experiences speaks to the applicant’s interest in medicine, the essay verges on being a regurgitation of the Alex's resume, which does not provide the admissions officer with any new insights or information and ultimately takes away from the essay as a whole. As such, the writing’s lack of voice or unique perspective puts the applicant at risk of sounding middle-of-the-road.
From witnessing medical procedures to eventually pursuing leadership positions, this tale of personal progress argues that Alex's life has prepared him to become a doctor.
The essay’s organization, however, is one of its strengths — each paragraph provides an example of personal growth through a new experience in medicine. Further, Alex demonstrates his compassion and diligence through detailed stories, which give a reader a glimpse into his values. Through recognizing important skills necessary to be a doctor, Alex demonstrates that he has the mature perspective necessary to embark upon this journey.
What this essay lacks in a unique voice, it makes up for in professionalism and organization. Alex's earnest desire to attend medical school is what makes this essay shine.
-- Accepted To: University of Toronto MCAT Scores: Chemical and Physical Foundations of Biological Systems - 128, Critical Analysis and Reading Skills - 127, Biological and Biochemical Foundations of Living Systems - 127, Psychological, Social, and Biological Foundations of Behavior - 130, Total - 512
Moment of brilliance.
Revelation.
These are all words one would use to describe their motivation by a higher calling to achieve something great. Such an experience is often cited as the reason for students to become physicians; I was not one of these students. Instead of waiting for an event like this, I chose to get involved in the activities that I found most invigorating. Slowly but surely, my interests, hobbies, and experiences inspired me to pursue medicine.
As a medical student, one must possess a solid academic foundation to facilitate an understanding of physical health and illness. Since high school, I found science courses the most appealing and tended to devote most of my time to their exploration. I also enjoyed learning about the music, food, literature, and language of other cultures through Latin and French class. I chose the Medical Sciences program because it allowed for flexibility in course selection. I have studied several scientific disciplines in depth like physiology and pathology while taking classes in sociology, psychology, and classical studies. Such a diverse academic portfolio has strengthened my ability to consider multiple viewpoints and attack problems from several angles. I hope to relate to patients from all walks of life as a physician and offer them personalized treatment.
I was motivated to travel as much as possible by learning about other cultures in school. Exposing myself to different environments offered me perspective on universal traits that render us human. I want to pursue medicine because I believe that this principle of commonality relates to medical practice in providing objective and compassionate care for all. Combined with my love for travel, this realization took me to Nepal with Volunteer Abroad (VA) to build a school for a local orphanage (4). The project’s demands required a group of us to work closely as a team to accomplish the task. Rooted in different backgrounds, we often had conflicting perspectives; even a simple task such as bricklaying could stir up an argument because each person had their own approach. However, we discussed why we came to Nepal and reached the conclusion that all we wanted was to build a place of education for the children. Our unifying goal allowed us to reach compromises and truly appreciate the value of teamwork. These skills are vital in a clinical setting, where physicians and other health care professionals need to collaborate as a multidisciplinary team to tackle patients’ physical, emotional, social, and psychological problems.
I hope to relate to patients from all walks of life as a physician and offer them personalized treatment.
The insight I gained from my Nepal excursion encouraged me to undertake and develop the role of VA campus representative (4). Unfortunately, many students are not equipped with the resources to volunteer abroad; I raised awareness about local initiatives so everyone had a chance to do their part. I tried to avoid pushing solely for international volunteerism for this reason and also because it can undermine the work of local skilled workers and foster dependency. Nevertheless, I took on this position with VA because I felt that the potential benefits were more significant than the disadvantages. Likewise, doctors must constantly weigh out the pros and cons of a situation to help a patient make the best choice. I tried to dispel fears of traveling abroad by sharing first-hand experiences so that students could make an informed decision. When people approached me regarding unfamiliar placements, I researched their questions and provided them with both answers and a sense of security. I found great fulfillment in addressing the concerns of individuals, and I believe that similar processes could prove invaluable in the practice of medicine.
As part of the Sickkids Summer Research Program, I began to appreciate the value of experimental investigation and evidence-based medicine (23). Responsible for initiating an infant nutrition study at a downtown clinic, I was required to explain the project’s implications and daily protocol to physicians, nurses and phlebotomists. I took anthropometric measurements and blood pressure of children aged 1-10 and asked parents about their and their child’s diet, television habits, physical exercise regimen, and sunlight exposure. On a few occasions, I analyzed and presented a small set of data to my superiors through oral presentations and written documents.
With continuous medical developments, physicians must participate in lifelong learning. More importantly, they can engage in research to further improve the lives of their patients. I encountered a young mother one day at the clinic struggling to complete the study’s questionnaires. After I asked her some questions, she began to open up to me as her anxiety subsided; she then told me that her child suffered from low iron. By talking with the physician and reading a few articles, I recommended a few supplements and iron-rich foods to help her child. This experience in particular helped me realize that I enjoy clinical research and strive to address the concerns of people with whom I interact.
Research is often impeded by a lack of government and private funding. My clinical placement motivated me to become more adept in budgeting, culminating in my role as founding Co-President of the UWO Commerce Club (ICCC) (9). Together, fellow club executives and I worked diligently to get the club ratified, a process that made me aware of the bureaucratic challenges facing new organizations. Although we had a small budget, we found ways of minimizing expenditure on advertising so that we were able to host more speakers who lectured about entrepreneurship and overcoming challenges. Considering the limited space available in hospitals and the rising cost of health care, physicians, too, are often forced to prioritize and manage the needs of their patients.
No one needs a grand revelation to pursue medicine. Although passion is vital, it is irrelevant whether this comes suddenly from a life-altering event or builds up progressively through experience. I enjoyed working in Nepal, managing resources, and being a part of clinical and research teams; medicine will allow me to combine all of these aspects into one wholesome career.
I know with certainty that this is the profession for me.
Jimmy opens this essay hinting that his essay will follow a well-worn path, describing the “big moment” that made him realize why he needed to become a physician. But Jimmy quickly turns the reader’s expectation on its head by stating that he did not have one of those moments. By doing this, Jimmy commands attention and has the reader waiting for an explanation. He soon provides the explanation that doubles as the “thesis” of his essay: Jimmy thinks passion can be built progressively, and Jimmy’s life progression has led him to the medical field.
Jimmy did not make the decision to pursue a career in medicine lightly. Instead he displays through anecdotes that his separate passions — helping others, exploring different walks of life, personal responsibility, and learning constantly, among others — helped Jimmy realize that being a physician was the career for him. By talking readers through his thought process, it is made clear that Jimmy is a critical thinker who can balance multiple different perspectives simultaneously. The ability to evaluate multiple options and make an informed, well-reasoned decision is one that bodes well for Jimmy’s medical career.
While in some cases this essay does a lot of “telling,” the comprehensive and decisive walkthrough indicates what Jimmy’s idea of a doctor is. To him, a doctor is someone who is genuinely interested in his work, someone who can empathize and related to his patients, someone who can make important decisions with a clear head, and someone who is always trying to learn more. Just like his decision to work at the VA, Jimmy has broken down the “problem” (what his career should be) and reached a sound conclusion.
By talking readers through his thought process, it is made clear that Jimmy is a critical thinker who can balance multiple different perspectives simultaneously.
Additionally, this essay communicates Jimmy’s care for others. While it is not always advisable to list one’s volunteer efforts, each activity Jimmy lists has a direct application to his essay. Further, the sheer amount of philanthropic work that Jimmy does speaks for itself: Jimmy would not have worked at VA, spent a summer with Sickkids, or founded the UWO finance club if he were not passionate about helping others through medicine. Like the VA story, the details of Jimmy’s participation in Sickkids and the UWO continue to show how he has thought about and embodied the principles that a physician needs to be successful.
Jimmy’s essay both breaks common tropes and lives up to them. By framing his “list” of activities with his passion-happens-slowly mindset, Jimmy injects purpose and interest into what could have been a boring and braggadocious essay if it were written differently. Overall, this essay lets the reader know that Jimmy is seriously dedicated to becoming a physician, and both his thoughts and his actions inspire confidence that he will give medical school his all.
The Crimson's news and opinion teams—including writers, editors, photographers, and designers—were not involved in the production of this content.

Medical Student Research
Medical research informs everything we do in medicine. Basic research helps us understand how the human body works at the molecular and cellular levels. Applied research in the lab gives rise to potential new diagnostic and therapeutic modalities. Clinical research tells us what medical interventions work and do not work in humans. Health services research helps us understand the best way to deliver medical care, including ongoing issues with health disparities. Quality improvement research helps make our care better. Epidemiologic research, population health research, and health policy research guide us in the realm of public health. And finally, medical education research helps us understand the best way to teach the next generation of doctors. Translational research and dissemination and implementation science bring these different research approaches together to bridges the gap from bench to bedside..
Given the importance of research within the medical profession, Case Western Reserve University School of Medicine requires a mentored research project and associated written MD Thesis to graduate. All areas of exploration on the biomedical research spectrum, detailed above, are open for these projects. The Office of Medical Student Research is committed to helping you have a productive and positive experience, whatever your previous research background. We have numerous resources available, including a needs assessment delivered to all incoming medical students, in-person workshops, online learning modules, an easy-to-use website that links faculty research mentors and interested students together, and a dedicated faculty and staff team give you individualized support through the research process.
Being involved in research during medical school will help you in your career at every stage, including residency, fellowship, and beyond. Understanding medical research—what it is, how it is done, what it shows us and its limitations—allows you to practice both the science and art of medicine after graduation and beyond, whether you are doing the research yourself in an academic setting or serving patients or communities. Research can also be personally rewarding, opening doors to travel, collaboration, and lifelong learning.
If you are a CWRU faculty member interested in being a medical student research mentor, please click on the ‘Submit a Project’ link and take a few minutes to enter one or more projects that would be applicable to medical students. If you have many projects, enter your research interests and contact information and indicate that students should contact you. As of 2023, the large majority of required medical student research occurs over 12 weeks of summer. Many students continue the same project or join another one beyond this required experience. You can submit projects that are appropriate for either timeline.
If you are a current CWRU medical student, please click on the ‘Search for Project’ link to search the database for potential research mentors and projects. This requires CWRU single sign-on.
We also keep a partial list of potential student research opportunities external to CWRU, of which we are aware. Click on the ‘External Research Opportunities’ link to explore these.
If you need help or want more information, please email [email protected].
Rosa K Hand, PhD, RDN, LD, FAND
Associate Professor, Nutrition Director, Medical Student Research & Scholarship
Sharon Callahan Administrative Director, Medical Student Research & Scholarship
Edinburgh Research Archive

- ERA Home
- Edinburgh Medical School
Edinburgh Medical School thesis and dissertation collection
By Issue Date Authors Titles Subjects Publication Type Sponsor Supervisors
Search within this Collection:
Edinburgh Medical School is one of two schools at the College of Medicine and Veterinary Medicine at the University of Edinburgh. The Edinburgh Medical School integrates research and teaching across our three Deaneries: Biomedical Sciences, Clinical Sciences and Molecular,Genetic and Population Health Sciences.
Recent Submissions
Investigating the role of pabpc5 in mouse physiology , community use of digital auscultation to improve diagnosis of childhood pneumonia in sylhet, bangladesh , investigating mechanisms of demyelination , preterm birth and the early-life respiratory microbiota: implications for host epigenetics and respiratory health , single-synapse resolution molecular mapping reveals both widespread and highly targeted experience-dependent synaptic plasticity in the mammalian brain , impact of primary renal epithelial senescence induction in the murine kidney , anatomic, histologic and histomorphometric analysis of the acetabular labrum and its enthesis , investigating disease progression of cutaneous squamous cell carcinoma , identification of methylation qtls in breast cancer characterises the influence of germline snp variation on the abnormal tumour methylome , investigating the sex-specific role of perivascular adipose tissue (pvat) on vascular function in obesity , integrated analysis of patient gene expression data for precision medicine applications in breast and pancreatic cancer , investigating chromosome cohesion loss in mammalian oocytes , quality palliative care in humanitarian crises in low- and middle-income country context , understanding and stratifying brain health through blood-based omics data , role of the nuclear basket in regulating the senescence-associated secretory phenotype , identifying mistranslating mrnas in mouse models of autism , development of attachment in infants born preterm , investigating the motor neuron translatome in spinal muscular atrophy and normal postnatal development , impact of prenatal stress and chronic stress in adult rats on the brain, behaviour and gut microbiome , investigating colonic macrophage heterogeneity in steady-state, inflammation, and resolution .
Secondary Medical School Application Essays: How to Shine
Emphasizing fit and showing authenticity help medical school secondary essays stand out, experts say.
Tips for Secondary Med School Essays

Getty Images | iStockphoto
One of best pieces of advice when writing an application essay is to be authentic.
Key Takeaways
- Secondary medical school essays should highlight why an applicant is a good fit.
- Applicants should submit the essays early without compromising quality.
- It's important to be authentic in essay responses.
After receiving primary applications, most medical schools ask applicants to complete a secondary application, which typically includes additional essay questions. While primary essay prompts ask why you're pursuing medicine, medical school secondary essays focus on you and how you fit with a specific school.
Secondary essay prompts vary by school, but they're generally designed to help med schools learn about you at a deeper level. They may ask you to reflect on what makes you who you are, a time when you worked with a population different than yourself, an occasion where you asked for help or a time when you worked in a team. They may ask how you spent a gap year before applying to medical school or what you did after your undergraduate degree.
"What we are trying to figure out is if this is a candidate that can fulfill the premedical competencies and whether they are mission-aligned," says Dr. Wendy Jackson, associate dean for admissions at the University of Kentucky College of Medicine . “Can they help fulfill the needs that our institution is trying to deliver?”
A lot rides on these essays, but keeping a few best practices in mind can make the process less daunting.
Emphasize Fit
The first thing medical schools look for is whether an applicant will be a good fit for the school’s mission, Jackson says.
“I would challenge someone who is completing a secondary application to understand the mission of the school and envision how they are going to contribute to that,” she says. “The vast majority of schools are going to ask why you chose their institution, so you need to be prepared to answer that.”
Some secondary essay questions are optional, but experts recommend answering them even though they're extra work. For example, the Vanderbilt University School of Medicine in Tennessee asks applicants what makes them interested in the school.
“We just want to see if they’re a good fit for us and that they’ve done a little bit of homework about Vanderbilt," says Jennifer Kimble, director of admissions at Vanderbilt's medical school. "We want to make sure that the students we admit are going to be happy with their Vanderbilt experience.”
Avoid focusing on what you’re going to gain from the school – schools are really asking how you'll be an asset to the program.
"It’s almost like if you’re trying to date someone and you tell them, ‘Here’s what I’m going to get from this relationship,’ without saying, ‘We’re better off together,’” says Shirag Shemmassian, founder of Shemmassian Academic Consulting. “You have to sell the idea that you’re bettering one another and how you’re better together than apart. I think students often miss that latter component."
Don't Procrastinate
The medical school application process is often compared to a marathon, but the final steps may feel like a sprint. Applicants typically receive secondary application requests in late June, and in some cases schools want those back within a matter of weeks. Others set deadlines months down the road.
Either way, because of rolling admissions , it's best to send essays in as early as possible without compromising quality, Shemmassian says.
The earlier an applicant submits materials, the less competition they typically face, experts say. For example, Vanderbilt receives nearly 7,000 applications per year. Of those, roughly 600 applicants will be asked to interview and around 260 will be offered admission for 96 spots.
"At the beginning of the cycle, our calendar is wide open and we’re very open to who we bring in for an interview," Kimble says. "Down the road when we only have 30 seats left, it’s highly selective who those candidates are that get those coveted 30 interview spots that are left over."
Prewrite Essays
Applicants won't know the specific language of secondary essay prompts until schools send them, but in many cases, essay prompts are similar year to year and the previous year's prompts are often published on a school's admissions website, experts say. Some schools may change or tweak questions, but you can generally get a head start by prewriting essays based on previous prompts.
"As the new ones come out, you can modify as needed," Shemmassian says. "I would say that about 70% to 80% of prompts will remain the same or similar. If they change, you can usually adapt an essay you’ve written for another school."
Secondary essays vary in length and number. Vanderbilt requires applicants to submit an 800-word essay and two 600-word essays. Some schools may require close to 10 secondary essays. Shemmassian says this is significantly more writing than applicants are used to, so budgeting time is crucial.
But applicants should take care when prewriting essays and make sure each is tailored to the specific school with the correct school name, experts say. Jackson says she's read plenty of essays where applicants included the wrong school name and it cost them.
“You may think you can save time by cutting and pasting or taking half of a previously written essay response and making a modification,” Jackson says. “Be careful, because the questions vary from institution to institution.”
Experts say applicants often neglect to fully read prompts in their haste to complete answers. Though there's a time crunch, it's vital to thoroughly read the prompt and answer the question fully without grammatical or spelling errors.
“That seems kind of silly, but I think we can get going down a road when we’re writing and feel like we’ve completed and written something well but look back and never really have a response to the true question being asked," Jackson says.
Be Authentic
Medical school applicants tend to put a lot of pressure on themselves to write something that schools haven't read before, Kimble says. Given that med schools sift through thousands of applicants a year, "we’ve read all sorts of scenarios in life, so take that pressure and put it on the shelf," she says. "That’s not a concern for us. We aren’t looking for something that’s totally innovative."
Experts say schools are mostly looking for authenticity and an organic, genuine tone. The tone "can make or break an applicant," Jackson says.
It may be tempting, especially given time constraints, to rely on outside help – such as ChatGPT or other AI-powered software – to write essays. While some professors and admissions officers have embraced AI to help automate certain processes, Kimble says she strongly discourages med school applicants from using AI to help with secondary essays.
"We had an (application) that you could clearly see was not written by a human voice," she says. "It sounded very computer generated, so we ended up passing on the candidate just because we want to hear their story in their own words."
A Secondary Essay Example
Shemmassian compiles more than 1,000 sample secondary essays each year, using prompts from more than 150 medical schools in various states, and offers them to paying clients. The excerpted example below, created by Shemmassian's team and used with their permission, shows what he considers to be a successful diversity-themed essay in response to a Yale University School of Medicine prompt that asks applicants to reflect on how their background and experiences contribute to the school's focus on diversity and how it will inform their future role as a doctor.
As a child, one of my favorite times of the year was the summer, when I would travel to Yemen… at least until I turned twelve. Suddenly, the traditional and, in my Yemeni American view, restrictive laws for women, applied to me. Perhaps the most representative of these laws was having to cover my hair with a scarf-like garment. Staying true to my values, I decided against returning to Yemen, thereby losing a vital connection to my culture. However, this estrangement did not inhibit my growth.
The 500-word response continues with how the applicant met a Yemeni student who grew up in France and was barred from wearing a headscarf due to a school uniform policy. Where the applicant saw the headscarf as restrictive, the other student saw it as a connection to her roots. The applicant describes how although the same object held different meanings to two people from the same background, she used that to appreciate different perspectives and to advocate for a woman's right to express herself.
Later that year, I applied this lesson in perspective to my work as a clinical coordinator, when a patient walked into the office and handed me a piece of paper explaining she only spoke Arabic...By thinking critically while vernacularly translating the doctor’s advice, I was directly involved in the process of her medical care. Because of my experience in exploring the multi-cultural barriers I faced alongside the Yemeni French student who cherished her headscarf, I spent time talking to this Yemeni patient about the barriers she had faced in receiving care.
This experience motivated me to help overcome cultural healthcare barriers and disparities, showcasing my devotion to equitable treatment by creating a new protocol within the clinic where I work. Now, when scheduling patients over the phone, we ask if they have any language preferences, and we have a series of scripts we can use during each patient’s treatment.
The applicant then drives home why she believes she's a good fit for the school.
My background and experiences will contribute to Yale School of Medicine’s diversity and inform my future role as a physician by creating a student organization that holds informational workshops, utilizing my unique experiences to connect with Yale’s diverse patient population, and working to address healthcare disparities as a future physician. I envision these informational workshops would operate in the Haven Free Clinic patient waiting rooms to empower all patients, regardless of their background.
This essay is successful because it does more than tell essay readers about the applicant's background, Shemmassian says. It shows how the applicant grew "into a more compassionate and culturally humble future physician who will help patients overcome health care barriers."
"Strong diversity essays will always show admissions committees how a unique trait or life experience will help them become a better physician," he says. "This essay is especially successful because the applicant connects their experiences and what they’ve learned because of them to the Yale School of Medicine itself. This is an applicant who is already thinking deeply about not just what they can get out of medical school but how they can contribute to the values and mission of the school they attend."
Searching for a medical school? Get our complete rankings of Best Medical Schools.
Medical School Application Mistakes

Tags: medical school , doctors , graduate schools , education , students
You May Also Like
15 b-schools with low acceptance rates.
Ilana Kowarski and Cole Claybourn June 5, 2024

Advice About Online J.D. Programs
Gabriel Kuris June 3, 2024

Questions to Ask Ahead of Law School
Cole Claybourn May 31, 2024

Ways Women Can Thrive in B-School
Anayat Durrani May 29, 2024

Study Away or Abroad in Law School
Gabriel Kuris May 28, 2024

A Guide to Executive MBA Degrees
Ilana Kowarski and Cole Claybourn May 24, 2024

How to Choose a Civil Rights Law School
Anayat Durrani May 22, 2024

Avoid Procrastinating in Medical School
Kathleen Franco, M.D., M.S. May 21, 2024

Good Law School Recommendation Letters
Gabriel Kuris May 20, 2024

Get Accepted to Multiple Top B-schools
Anayat Durrani May 16, 2024

- History, Facts & Figures
- YSM Dean & Deputy Deans
- YSM Administration
- Department Chairs
- YSM Executive Group
- YSM Board of Permanent Officers
- FAC Documents
- Current FAC Members
- Appointments & Promotions Committees
- Ad Hoc Committees and Working Groups
- Chair Searches
- Leadership Searches
- Organization Charts
- Faculty Demographic Data
- Professionalism Reporting Data
- 2022 Diversity Engagement Survey
- State of the School Archive
- Faculty Climate Survey: YSM Results
- Strategic Planning
- Mission Statement & Process
- Beyond Sterling Hall
- COVID-19 Series Workshops
- Previous Workshops
- Departments & Centers
- Find People
- Biomedical Data Science
- Health Equity
- Inflammation
- Neuroscience
- Global Health
- Diabetes and Metabolism
- Policies & Procedures
- Media Relations
- A to Z YSM Lab Websites
- A-Z Faculty List
- A-Z Staff List
- A to Z Abbreviations
- Dept. Diversity Vice Chairs & Champions
- Dean’s Advisory Council on Lesbian, Gay, Bisexual, Transgender, Queer and Intersex Affairs Website
- Minority Organization for Retention and Expansion Website
- Office for Women in Medicine and Science
- Committee on the Status of Women in Medicine Website
- Director of Scientist Diversity and Inclusion
- Diversity Supplements
- Frequently Asked Questions
- Recruitment
- By Department & Program
- News & Events
- Executive Committee
- Aperture: Women in Medicine
- Self-Reflection
- Portraits of Strength
- Mindful: Mental Health Through Art
- Event Photo Galleries
- Additional Support
- MD-PhD Program
- PA Online Program
- Joint MD Programs
- How to Apply
- Advanced Health Sciences Research
- Clinical Informatics & Data Science
- Clinical Investigation
- Medical Education
- Visiting Student Programs
- Special Programs & Student Opportunities
- Residency & Fellowship Programs
- Center for Med Ed
- Organizational Chart
- Leadership & Staff
- Committee Procedural Info (Login Required)
- Faculty Affairs Department Teams
- Recent Appointments & Promotions
- Academic Clinician Track
- Clinician Educator-Scholar Track
- Clinican-Scientist Track
- Investigator Track
- Traditional Track
- Research Ranks
- Instructor/Lecturer
- Social Work Ranks
- Voluntary Ranks
- Adjunct Ranks
- Other Appt Types
- Appointments
- Reappointments
- Transfer of Track
- Term Extensions
- Timeline for A&P Processes
- Interfolio Faculty Search
- Interfolio A&P Processes
- Yale CV Part 1 (CV1)
- Yale CV Part 2 (CV2)
- Samples of Scholarship
- Teaching Evaluations
- Letters of Evaluation
- Dept A&P Narrative
- A&P Voting
- Faculty Affairs Staff Pages
- OAPD Faculty Workshops
- Leadership & Development Seminars
- List of Faculty Mentors
- Incoming Faculty Orientation
- Faculty Onboarding
- Past YSM Award Recipients
- Past PA Award Recipients
- Past YM Award Recipients
- International Award Recipients
- Nominations Calendar
- OAPD Newsletter
- Fostering a Shared Vision of Professionalism
- Academic Integrity
- Addressing Professionalism Concerns
- Consultation Support for Chairs & Section Chiefs
- Policies & Codes of Conduct
- First Fridays
- Fund for Physician-Scientist Mentorship
- Grant Library
- Grant Writing Course
- Mock Study Section
- Research Paper Writing
- Establishing a Thriving Research Program
- Funding Opportunities
- Join Our Voluntary Faculty
- Child Mental Health: Fostering Wellness in Children
- Faculty Resources
- Research by Keyword
- Research by Department
- Research by Global Location
- Translational Research
- Research Cores & Services
- Program for the Promotion of Interdisciplinary Team Science (POINTS)
- CEnR Steering Committee
- Experiential Learning Subcommittee
- Goals & Objectives
- Issues List
- Print Magazine PDFs
- Print Newsletter PDFs
- YSM Events Newsletter
- Social Media
- Patient Care
INFORMATION FOR
- Residents & Fellows
- Researchers
Now online, decades of medical student theses available for download
- Features Alumni brave fires and floods in catastrophic season Strange bedfellows, great science How West Campus is fulfilling its dream A meeting of proteomics and ancient art Biomedical engineering meets radiology meets genetics A fab lab collab A catastrophe in the brain Melanoma, hooves, and the uterus Putting the precise in precision medicine A new tool against cancer Old specimens yield new clues to disease Bonding through hiking
- News Deans named to replace Carolyn Slayman Navigating power structures in medicine New drugs to fight resistant bacteria Playing sports with a defibrillator Evolutionary trade-off: having kids will break your heart Questions about early detection Now online, decades of medical student theses available for download Haitian Doctors Study Latest Practices in Group Care at Yale Crowdsourcing ways to reduce America's drug overdose crisis Plenty of “Me Too” stories exist in medicine How Peter Schulam came to lead a center for innovative thinking Art in medicine: observation without interpretation School of Medicine and CBIT host health Hackathon A voice for the voiceless: programs at Yale aim to stop child abuse
- People M.D./Ph.D. student wins Soros Fellowship A diagnosis of the health care system
- Dialogue Your editor bids farewell Second Opinion Cultural heritage to the microbiome: research at West Campus Life on Ice: A History of New Uses for Cold Blood
In the spring of 1952, Jocelyn Malkin, M.D. ’52, completed her student thesis on laryngeal cancer. Using punch cards, Malkin encoded clinical characteristics of 235 patients suffering from the malignancy, including race, religion, family history, and “excessive voice use.” She then threaded the cards onto a sorter shaped like an ice pick, looking for clear-cut risk factors. One stood out starkly: tobacco use.
After seeing her own thesis results, Malkin recalls, she “nagged” her husband to quit his cigarette habit. Later, as a psychoanalytic institute leader in Washington, D.C., she refused to allow light-ups in meetings.
“Everybody smoked—it was considered very, very cool,” she says. “I was very unpopular because I made a fuss about it.” Thanks to her thesis, Malkin was far ahead of her time. Not until 1957 did the U.S. Surgeon General issue its first report on the health consequences of smoking. Tobacco use is now known to be the most important laryngeal-cancer risk factor.
Malkin’s historic typewritten thesis is freely available online, along with hundreds of other newly digitized Yale medical student theses. Although hard copies of most recent and many older theses are available to peruse in the medical library, digitization and open access means a much larger audience.
“What we’re doing now just opens them up to the world,” says Melissa Grafe, Ph.D., the John R. Bumstead Librarian for Medical History at the Cushing/Whitney Medical Library.
The world has responded. Over 80,000 downloads of Yale medical student theses have taken place by readers in 187 countries, over half at educational or governmental facilities. The theses are available at both the Medical Heritage Library, an online consortium of major medical libraries that digitizes materials and makes them freely available via Internet Archive, and from Yale’s in-house repository, Eli Scholar.
With the first evidence of a thesis requirement appearing in an 1839 catalog, the Yale School of Medicine is perhaps the longest-lived such directive of its kind. Many theses go on to be edited and published in medical journals, but many others have long languished on shelves, largely unread.
Digitization has been underway since 2002, when the medical library and the YSM Office of Student Research placed some of that year’s theses online as part of the Yale Medicine Thesis Digital Library project. Four years later, submitting a digital copy became mandatory of all students. Living alumni were first invited to participate in 2012, and the project has rolled along since then via outreach at alumni events.
But in 2017, a grant to Yale University Library by the Arcadia Fund, one intended to preserve at-risk cultural materials, made it possible to digitize many more.
On July 12, 2017, John Gallagher, director of the Medical Library, with the assistance of Deborah Jagielow, director of Alumni Affairs, emailed some 3,000 alumni from the Class of 2009 and before, inviting them to participate. Within five hours, close to 400 replies had come in granting permission. Eventually, nearly 1,200 alumni agreed to allow digitization, including the families of four who had died.
Grafe and her colleagues then packed up 51 boxes of hard-copy theses and mailed them to Princeton, New Jersey, where, over October, November, and December, the Internet Archive scanned them in (and then mailed them back). Yale library staff then embarked on a quality-control check, making sure all the scans were legible and the data attached to each thesis were accurate.
“Even though it was a short timeline, it was a careful process,” Grafe says. “We wanted to make sure that the alumni who entrusted us with digitizing their material were happy with what they saw [and] received something they could share.”
Topics trend over time, she adds.
“In the late 80s and early 90s, I saw a batch of theses having to do with HIV and AIDS, and in recent years there’s been some global health emphasis,” she says. By contrast, in the 1960s and 70s, patient care and community health were popular.
A quick browse turns up theses on West Nile myeloencephalitis (1955), fetal electrocardiography (1957), cross-cultural psychiatry (1966), concentration camp survivors’ guilt (1971), health care for migrant farmworkers (1975), athletics in hemophilia (1980), detective fiction (1980), children’s fear of needles (1982), childbirth in literature (1987), professional courtesy (1996), and spirituality in HIV care (2001).
There are also many 19th-century theses in elaborate copperplate handwriting, including “On Diabetes Mellitus,” “On Gonorrhea,” and “On The Therapeutic Application of Ice.”
Everything is faithfully preserved as a PDF, including linen-bound covers, blank pages, and librarians’ penciled notations on title pages. Malkin’s includes a copy of the cards she used, notched with their telltale punch-outs. So far, it has been downloaded 50 times.
The digitization project is ongoing. Though theses written prior to 1923 are in the public domain, the library continues to seek permission from alumni or living relatives for any written after that. Interested alumni can fill out an online form .
- Open access
- Published: 27 May 2024
Associations between medical students’ stress, academic burnout and moral courage efficacy
- Galit Neufeld-Kroszynski ORCID: orcid.org/0000-0001-9093-1308 1 na1 ,
- Keren Michael ORCID: orcid.org/0000-0003-2662-6362 2 na1 &
- Orit Karnieli-Miller ORCID: orcid.org/0000-0002-5790-0697 1
BMC Psychology volume 12 , Article number: 296 ( 2024 ) Cite this article
267 Accesses
Metrics details
Medical students, especially during the clinical years, are often exposed to breaches of safety and professionalism. These contradict personal and professional values exposing them to moral distress and to the dilemma of whether and how to act. Acting requires moral courage, i.e., overcoming fear to maintain one’s core values and professional obligations. It includes speaking up and “doing the right thing” despite stressors and risks (e.g., humiliation). Acting morally courageously is difficult, and ways to enhance it are needed. Though moral courage efficacy, i.e., individuals’ belief in their capability to act morally, might play a significant role, there is little empirical research on the factors contributing to students’ moral courage efficacy. Therefore, this study examined the associations between perceived stress, academic burnout, and moral courage efficacy.
A cross-sectional study among 239 medical students who completed self-reported questionnaires measuring perceived stress, academic burnout (‘exhaustion,’ ‘cynicism,’ ‘reduced professional efficacy’), and moral courage efficacy (toward others’ actions and toward self-actions). Data analysis via Pearson’s correlations, regression-based PROCESS macro, and independent t -tests for group differences.
The burnout dimension of ‘reduced professional efficacy’ mediated the association between perceived stress and moral courage efficacy toward others’ actions. The burnout dimensions ‘exhaustion’ and ‘reduced professional efficacy’ mediated the association between perceived stress and moral courage efficacy toward self-actions.
Conclusions
The results emphasize the importance of promoting medical students’ well-being—in terms of stress and burnout—to enhance their moral courage efficacy. Medical education interventions should focus on improving medical students’ professional efficacy since it affects both their moral courage efficacy toward others and their self-actions. This can help create a safer and more appropriate medical culture.
Peer Review reports
Introduction
In medical school, and especially during clinical years, medical students (MS) are often exposed to physicians’ inappropriate behaviors and various breaches of professionalism or safety [ 1 , 2 , 3 ]. These can include lack of respect or sensitivity toward patients and other healthcare staff, deliberate lies and deceptions, breaching confidentiality, inadequate hand hygiene, or breach of a sterile field [ 4 , 5 ]. Furthermore, MS find themselves performing and/or participating in these inappropriate behaviors. For example, a study found that 80% of 3 rd– 4th year MS reported having done something they believed was unethical or having misled a patient [ 6 ]. Another study showed that 47.1–61.3% of females and 48.8–56.6% of male MS reported violating a patient’s dignity, participating in safety breaches, or examining/performing a procedure on a patient without valid consent, following a clinical teacher’s request, as a learning exercise [ 5 ]. These behaviors contradict professional values and MS’ own personal and moral values, exposing them to a dilemma in which they must choose if and how to act.
Taking action requires moral courage, i.e., taking an active stand or acting in the face of wrongdoing or moral injustice jeopardizing mental well-being [ 7 , 8 , 9 , 10 ]. Moral courage includes speaking up and “doing the right thing” despite risks, such as shame, retaliation, threat to reputation, or even loss of employment [ 8 ]. Moral courage is expressed in two main situations: when addressing others’ wrongdoing (e.g., identifying and disclosing a past/present medical error by colleagues/physicians); or when admitting one’s own wrongdoing (e.g., disclosing an error or lack of knowledge) [ 11 ].
Due to its “calling out” nature, acting on moral courage is difficult. A hierarchy and unsafe learning environment inhibits the ability for assertive expression of concern [ 12 , 13 , 14 ]. This leads to concerning findings indicating that only 38% of MS reported that they would approach someone performing an unsafe behavior [ 12 ], and about half claimed that they would report an error they had observed [ 15 ].
Various reasons were suggested to explain why MS, interns, residents, or nurses, hesitate to act in a morally courageous way, including difficulty questioning the decisions or actions of those with more authority [ 12 ], and fear of negative social consequences, such as being disgraced, excluded, attacked, punished, or poorly evaluated [ 13 ]. Other reasons were the wish to fit into the team [ 6 ] and being a young professional experiencing “lack of knowledge” or “unfamiliarity” with clinical subtleties [ 16 ].
Nevertheless, failing to act on moral courage might lead to negative consequences, including moral distress [ 17 ]. Moral distress is a psychological disequilibrium that occurs when knowing the ethically right course of action but not acting upon it [ 18 ]. Moral distress is a known phenomenon among MS [ 19 ], e.g., 90% of MS at a New York City medical school reported moral distress when carrying for older patients [ 20 ]. MS’ moral distress was associated with thoughts of dropping out of medical school, choosing a nonclinical specialty, and increased burnout [ 20 ].
These consequences of moral distress and challenges to acting in a morally courageous way require further exploration of MS’ moral courage in general and their moral courage efficacy specifically. Bandura coined the term self-efficacy, focused on one’s perception of how well s/he can execute the action required to deal successfully with future situations and to achieve desired outcomes [ 21 ]. Self-efficacy plays a significant role in human behavior since individuals are more likely to engage in activities they believe they can handle [ 21 ]. Therefore, self-efficacy regarding a particular skill is a major motivating factor in the acquisition, development, and application of that skill [ 22 ]. For example, individuals’ perception regarding their ability to deal positively with ethical issues [ 23 ], their beliefs that they can handle effectively what is required to achieve moral performance [ 24 ], and to practically act as moral agents [ 25 ], can become a key psychological determinant of moral motivation and action [ 26 ]. Due to self-efficacy’s importance there is a need to learn about moral courage efficacy, i.e., individuals’ belief in their ability to exhibit moral courage through sharing their concerns regarding others and their own wrongdoing. Moral courage efficacy was suggested as important to moral courage in the field of business [ 27 ], but not empirically explored in medicine. Thus, there is no known prevalence of moral courage efficacy toward others and toward one’s own wrongdoing in medicine in general and for MS in particular. Furthermore, the potential contributing factors to moral courage efficacy, such as stress and burnout, require further exploration.
The associations between stress, burnout, and moral courage efficacy
Stress occurs when people view environmental demands as exceeding their ability to cope with them [ 28 ]. MS experience high levels of stress during their studies [ 29 ], due to excessive workload, time management difficulties, work–life balance conflicts, health concerns, and financial worries [ 30 ]. Studies show that high levels of stress were associated with decreased empathy [ 31 ], increased academic burnout, academic dishonesty, poor academic performance [ 32 ], and thoughts about dropping out of medical school [ 33 ]. As stress may impact one’s perceived efficacy [ 34 ], this study examined whether stress can inhibit individuals’ moral courage efficacy to address others’ and their own wrongdoing.
An aspect related to a poor mental state that may mediate the association between stress and MS’ moral courage efficacy is burnout. Burnout includes emotional exhaustion, cynicism toward one’s occupation value, and doubting performance ability [ 35 ]. Burnout is usually work-related and is common in the helping professions [ 60 ]. For students, this concept relates to academic burnout [ 36 ], which includes exhaustion due to study demands, a cynical and detached attitude to studying, and low/reduced professional efficacy, i.e. feeling incompetent as learners [ 37 ].
Burnout has various negative implications for MS’ well-being and professional development. Burnout is associated with psychiatric disorders and thoughts of dropping out of medical school [ 33 ]. Furthermore, MS’ burnout is associated with increased involvement in unprofessional behavior, eroding professional development, diminishing qualities such as honesty, integrity, altruism, and self-regulation [ 38 ], reducing empathy [ 31 , 39 ] and unwillingness to provide care for the medically underserved [ 40 ]. Thus, burnout may also impact MS’ views on their responsibility and perceived ability to promote high-quality care and advocate for patients [ 41 ], possibly leading them to feel reluctant and incapable to act with moral courage [ 42 ]. Earlier studies exploring stress and its various outcomes, found that burnout, and specifically exhaustion, can become a crucial mediator for various harmful outcomes [ 43 ]. Although stress is impactful to creating discomfort, the decision and ability to intervene requires one’s own drive and power. When one is feeling stress, leading to burnout their depleted energy reserves and diminished sense of professional worth likely undermine their perceived power (due to exhaustion) or will (due to cynicism) to uphold professional ethical standards and intervene to advocate for patient care in challenging circumstances, such as the need to speak up in front of authority members. Furthermore, burnout may facilitate a cognitive distancing from professional values and responsibilities, allowing for moral disengagement and reducing the likelihood of morally courageous actions. This mediation role requires further exploration.
This study examined associations between perceived stress, academic burnout, and moral courage efficacy. In addition to the mere associations among the variables, it will be examined whether there is a mediation effect (perceived stress → academic burnout → moral courage efficacy) to gain more insight into possible mechanisms of the development of moral courage efficacy and of protective factors. Understanding these mechanisms has educational benefit for guiding interventions to enhance MS’ moral courage efficacy.
H1: Perceived stress and academic burnout dimensions will be negatively associated with moral courage efficacy dimensions.
H2: Perceived stress will be positively associated with academic burnout dimensions.
H3: Academic burnout dimensions will mediate the association between perceived stress and moral courage efficacy dimensions.
Materials and methods
Sample and procedure.
A quantitative cross-sectional study among 239 MS. Most participants were female (60%), aged 29 or less (90%), and unmarried (75%). About two thirds (64.3%) were at the pre-clinical stage of medical school and about a third (35.7%) at the clinical stage. In December 2019, the research team approached MS through email and social media to participate in the study and complete an online questionnaire. This was a part of a national study focused on MS’ burnout [ 44 ]. The 239 participants were recruited by a convenience sampling. Data were collected online through Qualtrics platform, via anonymous self-reported questionnaires. The University Ethics Committee approved the study, and all participants signed an informed consent form.
Moral courage efficacy —This 8-item instrument, developed for this study, is based on the literature on moral courage, professionalism, and speaking-up, including qualitative and quantitative studies [ 7 , 13 , 45 , 46 , 47 ], and discussions with MS and medical educators. The main developing team included a Ph.D. medical educator expert in communication in healthcare and professionalism; an M.D. psychiatrist expert in decision making, professionalism, and philosophy; a Ph.D. graduate who analyzed MS’ narratives focused on moral dilemmas and moral courage during professionalism breaches; and a Ph.D. candidate focused on assertiveness in medicine [ 14 ]. This allowed the identification of different types of situations MS face that may require moral courage.
As guided by instructions for measuring self-efficacy, which encourage using specific statements that relate to the specific situation and skill required [ 48 ], the instrument measures MS’ perception of their own ability, i.e., self-efficacy, to act based on their moral beliefs when exposed to safety and professionalism breaches or challenges. Due to our qualitative findings indicating that students change their interpretation of the problematic event based on their decision to act in a morally courageous way and that some are exposed to specific professionalism violations while others are not when designing the questionnaire, we decided to make the cases not explicit to specific types of professionalism breaches – e.g., not focused on talking above a patient’s head [ 1 ], but rather general the type of behavior e.g., “behaves immorally”. This decreases the personal interpretation if one behavior is acceptable by this individual; and also decreases the possibility of not answering the question if the individual student has never seen that specific behavior. Furthermore, to avoid “gray areas” in moral issues, we wrote the statements in a manner where there is no doubt whether there is a moral problem (“problematic situation”) [ 47 ], and thus the focus was only on one’s feeling of being capable of speaking up about their concern, i.e., act in a moral courage efficacy (see Table 1 ).
The instrument’s initial development consisted of 14 items addressing various populations, including senior MDs. The 14-item tool included questions regarding the willingness to recommend a second opinion or to convey one’s medical mistake to patients and their families. These actions are less relevant to MS. Thus, we extracted the questionnaire to a parsimonious instrument of 8 items.
The 8 items were divided into two dimensions: others and the self. This division is supported by the literature on moral courage that distinguishes between courage regarding others- vs. self-behavior. Hence, the questionnaire was designed to assess one’s perceived ability to act/speak up in these two dimensions: (a) situations of moral courage efficacy relating to others’ behavior (e.g., “ capable of telling a senior physician if I have detected a mistake s/he might have made ”); (b) situations of moral courage efficacy relating to self (e.g., “ capable of disclosing my mistakes to a senior physician ”). This two-dimension division is important and was absent in former measurements of moral courage. It was also replicated in another study we conducted among MS [ 49 ]. Furthermore, factor analysis with Oblimin rotation supported this two-factor structure (Table 1 ). All items had a high factor loading on the relevant factor (it should be mentioned that item 4 was loaded 0.59 on the relevant factor and 0.32 on the non-relevant factor).
All items are rated on a 5-point Likert scale (0 = to a small extent; 4 = to a very great extent) and are calculated by averaging the answers on the dimension, with higher scores representing higher moral courage efficacy. Internal reliability was α = 0.80 for the “others” dimension and α = 0.84 for the “self” dimension.
Perceived stress —This single-item questionnaire (“How would you rate the level of stress you’ve been experiencing in the last few days?” ) evaluates MS’ perceived stress currently in their life on an 11-point Likert scale (0 = no stress; 10 = extreme stress), with higher scores representing higher perceived stress. It is based on a similar question evaluating MS’ perceived emotional stress [ 29 ]. Even though a multi-item measure might be more stable, previous studies indicated that using a single item is a practical, reliable alternative, with high construct validity in the context of felt/perceived stress, self-esteem, health status, etc [ 43 , 50 , 51 ].
Academic burnout —This 15-item instrument is a translated version [ 44 ] of the MBI-SS (MBI–Student Survey) [ 37 ], a common instrument used to measure burnout in the academic context, e.g. MS [ 52 , 53 ]. It measures students’ feelings of burnout regarding their studies on three dimensions: (a) ‘exhaustion’ (5 items; e.g., “ Studying or attending a class is a real strain for me ”), (b) ‘cynicism’ (4 items; e.g., “ I doubt the significance of my studies ”), (c) lack of personal academic efficacy (‘reduced professional efficacy’) (6 items; “ I feel [un]stimulated when I achieve my study goals ”). Each item is rated on a 7-point Likert scale (0 = never; 6 = always) and is calculated by summing the answers on the dimension (after re-coding all professional efficacy items), with higher scores representing more frequent feelings of burnout. Internal reliability was α = 0.80 for ‘exhaustion’, α = 0.80 for ‘cynicism’, and α = 0.84 for ‘reduced professional efficacy’.
Statistical analyses
IBM-SPSS (version 25) was used to analyze the data. Pearson’s correlations examined all possible bivariate associations between the study variables. PROCESS macro examined the mediation effects (via model#4). The significance of the mediation effects was examined by calculating 5,000 samples to estimate the 95% percentile bootstrap confidence intervals (CIs) of indirect effects of the predictor on the outcome through the mediator [ 54 ]. T -tests for independent samples examined differences between the study variables in the pre-clinic and clinic stages. The defined significance level was set generally to 5% ( p < 0.05).
This study focused on understanding moral courage efficacy, i.e., MS’ perceived ability to speak up and act while exposed to others’ and their own wrongdoing. The sample’s frequencies demonstrate that only 10% of the MS reported that their moral courage efficacy toward the others was “very high to high,” and 54% reported this toward the self. Mean scores demonstrate that regarding the others, MS showed relatively low/moderate levels of moral courage and higher levels regarding the self. As for the variables tested to be associated with moral courage efficacy, MS showed relatively high perceived stress and low-to-moderate academic burnout (see Table 2 for the variables’ psychometric characteristics).
Table 2 also shows the correlations among the study variables. According to Cohen’s (1988) [ 55 ] interpretation of the strength in bivariate associations (Pearson correlation), the effect size is low when r value varies around 0.1, medium when it is around 0.3, and large when it is more than 0.5. Hence, regarding the associations between the two dimensions of moral courage efficacy: we found a moderate positive correlation between the efficacy toward others and the efficacy toward the self. Regarding the associations among the three academic burnout dimensions: we found a strong positive correlation between ‘exhaustion’ and ‘cynicism,’ a weak positive correlation between ‘exhaustion’ and ‘reduced professional efficacy,’ and a moderate positive correlation between ‘cynicism,’ and ‘reduced professional efficacy.’
As for the associations concerning H1, Table 2 indicates that one academic burnout dimension, i.e., ‘reduced professional efficacy,’ had a weak negative correlation with moral courage efficacy toward the others, thus high burnout was associated with lower perceived moral courage efficacy toward others. Additionally, perceived stress and all three burnout dimensions had weak negative correlations with moral courage efficacy toward the self—partially supporting H1.
As for the associations concerning H2, Table 2 indicates that perceived stress had a strong positive correlation with ‘exhaustion,’ a moderate positive correlation with ‘cynicism,’ and a weak positive correlation with ‘reduced professional efficacy’—supporting H2.
Based on these correlations, we conducted regression-based models to examine the unique and complex relationships among the study variable, including their various dimensions, while focusing on the examination of whether academic burnout mediates the association between perceived stress and moral courage efficacy (see Tables 3 and 4 ; and Figs. 1 and 2 ).
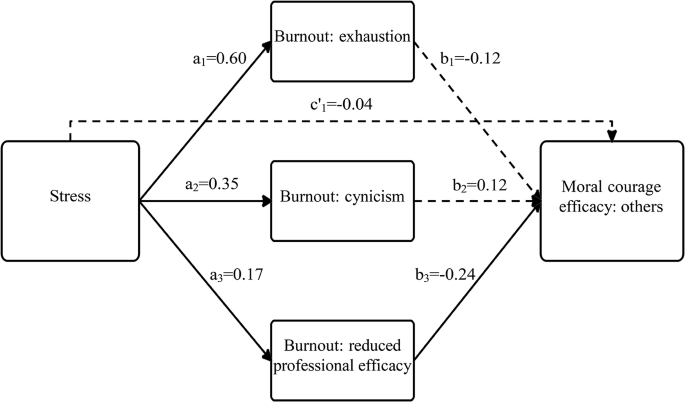
A model presenting the association between perceived stress and moral courage efficacy toward others, mediated by academic burnout. Note full arrows contain significant β coefficient values (fractured arrows mean nonsignificance
Focusing on moral courage efficacy toward others
Table 3 and Fig. 1 indicate that perceived stress was positively associated with all three academic burnout dimensions: ‘exhaustion’ (path a 1 ), ‘cynicism’ (path a 2 ), and ‘reduced professional efficacy’ (path a 3 ). These paths support H2. In turn, ‘reduced professional efficacy’ was negatively associated with moral courage efficacy toward the others (path b 3 ), supporting H1. The CIs of the indirect effect (paths a 3 b 3 ) did not contain zero; therefore, perceived stress had a significant indirect effect on moral courage efficacy toward the others, through the burnout dimension ‘reduced professional efficacy.’ This path supports H3.
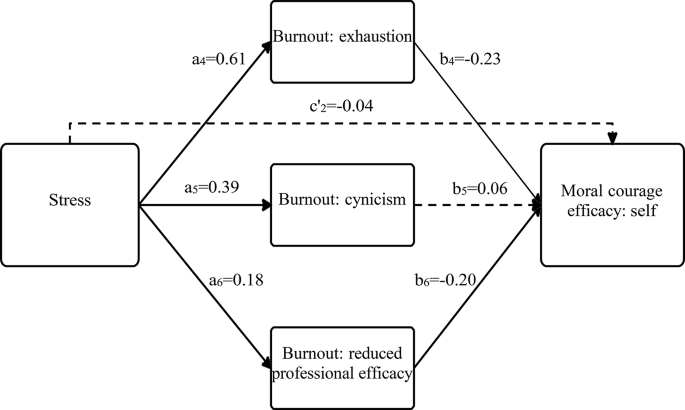
A model presenting the association between perceived stress and moral courage efficacy towards self, mediated by academic burnout. Note full arrows contain significant β coefficient values (fractured arrows mean non-significance
Focusing on moral courage efficacy toward the self
Table 4 and Fig. 2 also indicate that perceived stress was positively associated with all three academic burnout dimensions: ‘exhaustion’ (path a 4 ), ‘cynicism’ (path a 5 ), and ‘reduced professional efficacy’ (path a 6 ). These paths support H2. In turn, ‘exhaustion’ and ‘reduced professional efficacy’ were negatively associated with moral courage efficacy toward the self (paths b 4 , b 6 respectively). These paths support H1 The CIs of the indirect effects (paths a 4 b 4 , a 6 b 6 ) did not contain zero; therefore, perceived stress had a significant indirect effect on moral courage efficacy toward the self, through the burnout dimensions ‘exhaustion’ and ‘reduced professional efficacy.’ These paths support H3. It should be noted that in this analysis, the initially significant association between perceived stress and moral courage efficacy toward the self (path c 2, representing H1) became insignificant in the existence of academic burnout dimensions (path c’ 2 ). These results demonstrate complete mediation and also support H3.
In addition to examining the complex relationships between stress, academic burnout, and moral courage efficacy among MS, we tested the differences between MS in the pre-clinical and clinical school stages in all study variables. The results indicate non-significant differences in moral courage efficacy. However, medical-school-stage differences were found in stress [t(197.4)=-4.36, p < 0.001] and in one academic burnout dimension [t(233)=-2.40, p < 0.01]. In that way, MS at the clinical stage reported higher levels of perceived stress ( M = 7.32; SD = 2.17) and exhaustion ( M = 19.67; SD = 6.58) than MS in the pre-clinical stage ( M = 5.94; SD = 2.59 and M = 17.48; SD = 6.78, respectively).
This study examined the associations between perceived stress, academic burnout, and moral courage efficacy to understand MS’ perceived ability to speak up and act while exposed to others’ and their own wrongdoing. The findings show that one dimension of burnout, that of ‘reduced professional efficacy,’ mediated the associations between perceived stress and moral courage efficacy toward both others and self. ‘Exhaustion’ mediated the association between perceived stress and moral courage efficacy only toward the self.
Before discussing the meanings of the associations, this study was an opportunity to explore moral courage efficacy occurrence. The findings indicated fairly low/moderate mean scores of perceived ability to speak up and act while confronted with others’ wrongdoing and moderate/high scores of perceived ability while confronted with one’s own wrongdoing. This implies that students do not feel capable enough to share their concerns regarding others’ possible errors and feel more able, but still not enough, to share their own flaws and needs for guidance. These findings require attention, from both patient safety and learning perspectives.
Regarding patient safety, feeling unable to act while confronted with others or self- wrongdoing means that some errors may occur and not be addressed. This is in line with former findings that showed that less than 50% of MS would actually approach someone performing an unsafe behavior [ 12 ], or report an error they had observed [ 15 ]. These numbers are likely to improve in postgraduates as studies showed that between 64 and 79% of interns and residents reported they would likely speak up to an attending when exposed to a safety threat [ 56 , 57 ].
Regarding learning, our MS’ scores must improve for various reasons. First, moderate scores may indicate a psychologically unsafe learning environment, which prevents or discourages sharing uncertainties, especially about others’ behavior, and creates difficulty for students to share their own concerns, limitations, mistakes, and hesitations when feeling incapable or unqualified for a task [ 58 ]. Second, limited sharing of errors may be problematic because by not disclosing their error, students miss the chance to learn from it; [ 59 ] they lose the opportunity for reflective guidance to explore what worked well, what did not, and how to improve [ 59 , 60 ]. Third, if they do not discuss others’ errors or their own, they may deny themselves the necessary support to learn the all-important skills of how to deal with the emotional turmoil and challenges of errors, and how to share the error with a patient or family member [ 61 ]. Furthermore, if MS feel incapable of sharing their concern about a senior’s possible mistake, they miss other learning opportunities—e.g., the senior’s reasoning and clinical judgment may show that a mistake was not made. In this case, the student would miss being shown why they were wrong and what they did do well. Thus, identifying what can enhance moral courage efficacy and practice is needed. The fact that there are no significant differences between pre-clinical and clinical years students in their perceived ability to apply moral courage, may indicate that there is a cultural barrier in perceiving the idea of sharing weakness or of revealing others’ mistakes as unacceptable. Thus, the socialization, in the medical school environment, both in pre-clinical and clinical years, perhaps lacks the encouragement to speak up and provision of safe space.
This study examined the associations between perceived stress, academic burnout, and moral courage efficacy among MS. The findings indicate that, like earlier studies, stress is not directly connected to speaking up [ 62 ] or moral courage. It rather contributes to it indirectly, through the impact of burnout. Beyond the well-established role of stress in explaining burnout [ 63 , 64 ], we identified a negative consequence of burnout—hindering moral courage efficacy. This may help explain the path in which previous studies found burnout to impair MS’ quality of life, how it leads to dropout, and to more medical errors [ 65 ]. When individuals experience the burnout dimension of ‘reduced professional efficacy,’ they may feel less confident and fit, leading them to feel more disempowered to take the risk (required in courage) and share their concerns and hesitations about others’ mistakes and their own challenges. This fits earlier studies indicating that being a young professional experiencing “lack of knowledge” or “unfamiliarity” with clinical subtleties is a barrier to moral courage [ 11 ]. This may have various negative implications, of limited moral courage efficacy, as seen here, as well as paying less attention and not fully addressing their learning needs, leading to a vicious cycle of “feeding” the misfit feeling, potentially increasing their moral distress. Furthermore, those who feel they know less and, therefore, need more support to fill the gap in knowledge and skills, are less inclined to ask for help.
Beside the negative associations between ‘reduced professional efficacy’ and both dimensions of moral courage efficacy (toward others and the self), another dimension of academic burnout—‘exhaustion’—was negatively associated with moral courage efficacy toward the self. This is worrying because when learners are exhausted, their attention is reduced and they are at greater risk of error, as proven in an earlier study [ 65 ]. The current study adds to this information another worry, showing that MS are less willing to share their hesitations about themselves or the mistakes they already made, thus perhaps not preventing the error or fixing it. MS might create an unspoken contract with senior physicians about not exposing each other’s mistakes, with various possible negative implications. Some MS’ tendency to defend physicians’ mistakes was identified elsewhere [ 66 ].
The findings concerning medical-school-stage differences demonstrated that MS in the clinical stage had higher perceived stress and exhaustion levels than MS in the pre-clinical stage. These results support previous studies indicating stress, academic burnout, and more challenging characteristics among more senior students, including a decline in ideals, altruistic attitudes, and empathy during medical school studies; or more exhaustion, cynicism, and higher levels of detached emotions and depression through the years of medical school [ 67 , 68 , 69 ]. These higher levels of stress and exhaustion, can be explained by the senior students’ exposure to the rounds in the hospitals, which requires ongoing learning, more pressure, and a sense of overload in their academic life.
Limitations and future studies
Despite the importance of the findings, the study has several limitations. First, the participants were from one university, and recruited via convenience sampling, including only MS who voluntarily completed the questionnaires, undermining generalizability. To address this limitation, future research should aim to include a more diverse and representative sample of medical students from multiple universities and geographical regions. This would enhance the external validity and applicability of the findings across different educational and cultural contexts. Second, future studies are recommended to follow up on medical students’ stress, academic burnout, and moral courage efficacy over time. Exploring the development of professional efficacy and the barriers to exposing one’s and others’ weaknesses and flaws within the medical environment can help improve the medical culture into a safer space. Third, an intriguing avenue for future research is the exploration of the construct of ‘moral courage efficacy’ within different cohorts of healthcare students throughout their undergraduate and postgraduate years to learn about their moral courage efficacy development as well as and to verify the association between the findings from this newly developed scale and actual moral courage behavior. Additionally, experimental designs, such as interventions to reduce stress and burnout among medical students, could be employed to observe the impact on moral courage efficacy.
Conclusions and implications
This study is a first step in understanding moral courage efficacy and what contributes to it. The study emphasizes the importance of promoting MS’ well-being—in terms of stress and burnout—to enhance their moral courage efficacy. The findings show that the ‘reduced professional efficacy’ mediated the association between perceived stress and moral courage efficacy, toward both the others and self. This has potential implications for safety, learning, and well-being. To encourage MS to develop moral courage efficacy that will potentially increase their morally courageous behavior, we must find ways to reduce their stress and burnout levels. As the learning and work environments are a major cause of burnout [ 38 ], it would be helpful to focus on creating safe spaces where they can share others- and self-related concerns [ 70 ]. The first step is a learning environment promoting students’ overall health and well-being [ 71 ]. Useful additions are processes that support MS while dealing with education- and training-related stresses, improving their academic-professional efficacy, and constructively helping them handle challenging situations through empathic feedback [ 70 ]. This can lead them to a stronger belief in their ability to share safety and professionalism issues, thus enhancing their learning and patient care.
Data availability
No datasets were generated or analysed during the current study.
Karnieli-Miller O, Vu TR, Holtman MC, Clyman SG, Inui TS. Medical students’ professionalism narratives: a window on the informal and hidden curriculum. Acad Med. 2010;85(1):124–33. https://doi.org/10.1097/ACM.0b013e3181c42896 .
Article PubMed Google Scholar
Gaufberg EH, Batalden M, Sands R, Bell SK. The hidden curriculum: what can we learn from third-year medical student narrative reflections? Acad Med. 2010;85(11):1709–16. https://doi.org/10.1097/ACM.0b013e3181f57899 .
Monrouxe LV, Rees CE, Endacott R, Ternan E. Even now it makes me angry: Health care students’ professionalism dilemma narratives. Med Educ. 2014;48(5):502–17. https://doi.org/10.1111/medu.12377 .
Karnieli-Miller O, Taylor AC, Cottingham AH, Inui TS, Vu TR, Frankel RM. Exploring the meaning of respect in medical student education: an analysis of student narratives. J Gen Intern Med. 2010;25(12):1309–14. https://doi.org/10.1007/s11606-010-1471-1 .
Article PubMed PubMed Central Google Scholar
Monrouxe LV, Rees CE, Dennis I, Wells SE. Professionalism dilemmas, moral distress and the healthcare student: insights from two online UK-wide questionnaire studies. BMJ Open. 2015;5(5):e007518. https://doi.org/10.1136/bmjopen-2014-007518 .
Feudtner C, Christakis DA, Christakis NA. Do clinical clerks suffer ethical erosion? Students’ perceptions of their ethical environment and personal development. Acad Med. 1994;69(8):670–9. https://doi.org/10.1097/00001888-199408000-00017 .
Osswald S, Greitemeyer T, Fischer P, Frey D. What is moral courage? Definition, explication, and classification of a complex construct. In: Pury LS, Lopez SJ, editors. The psychology of courage: Modern Research on an ancient Virtue. American Psychological Association; 2010. pp. 149–64. https://doi.org/10.1037/12168-008 .
Murray CJS. Moral courage in healthcare: acting ethically even in the presence of risk. Online J Issues Nurs. 2010;15(3):Manuscript2. https://doi.org/10.3912/OJIN.Vol15No03Man02 .
Article Google Scholar
Kidder RM, Bracy M. Moral Courage A White Paper .; 2001.
Lachman VD. Ethical challenges in Health Care: developing your Moral Compass. Springer Publishing Company; 2009. http://ovidsp.ovid.com/ovidweb.cgi?T=JS . &PAGE=reference&D=psyc6&NEWS=N&AN=2009-11697-000.
Lachman VD. Moral courage: a virtue in need of development? Medsurg Nurs. 2007;16(2):131–3. http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L47004201 .
PubMed Google Scholar
Doyle P, Vandenkerkhof EG, Edge DS, Ginsburg L, Goldstein DH. Self-reported patient safety competence among Canadian medical students and postgraduate trainees: a cross-sectional survey. BMJ Qual Saf. 2015;24:135–41. https://doi.org/10.1136/bmjqs .
Martinez W, Bell SK, Etchegaray JM, Lehmann LS. Measuring moral courage for interns and residents: scale development and initial psychometrics. Acad Med. 2016;91(10):1431–8. https://doi.org/10.1097/ACM.0000000000001288 .
Gutgeld-Dror M, Laor N, Karnieli-Miller O. Assertiveness in physicians’ interpersonal professional encounters: a scoping review. Med Educ Published Online 2023:1–13. https://doi.org/10.1111/medu.15222 .
Madigosky WS, Headrick LA, Nelson K, Cox KR, Anderson T. Changing and sustaining medical students’ knowledge, skills, and attitudes about patient safety and medical fallibility. Acad Med. 2006;81(1):94–101.
Weinzimmer S, Miller SM, Zimmerman JL, Hooker J, Isidro S, Bruce CR. Critical care nurses’ moral distress in end-of-life decision making. J Nurs Educ Pract. 2014;4(6):6–12. https://doi.org/10.5430/jnep.v4n6p6 .
Savel RH, Munro CL. Moral distress, moral courage. Am J Crit Care. 2015;24(4):276–8. https://doi.org/10.1037/a0022283 .
Elpern EH, Covert B, Kleinpell R. Moral distress of staff nurses in a medical intensive care unit. Am J Crit Care. 2005;14(6):523–30. https://doi.org/10.4037/ajcc2005.14.6.523 .
Camp M, Sadler J. Moral distress in medical student reflective writing. AJOB Empir Bioeth. 2019;10(1):70–8. https://doi.org/10.1080/23294515.2019.1570385 .
Perni S, Pollack LR, Gonzalez WC, Dzeng E, Baldwin MR. Moral distress and burnout in caring for older adults during medical school training. BMC Med Educ. 2020;20(1):1–10. https://doi.org/10.1186/s12909-020-1980-5 .
Bandura A. Self-Efficacy: the Exercise of Control. W.H. Freeman; 1997.
Artino AR. Academic self-efficacy: from educational theory to instructional practice. Perspect Med Educ. 2012;1(2):76–85. https://doi.org/10.1007/s40037-012-0012-5 .
May DR, Luth MT, Schwoerer CE. The influence of business ethics education on moral efficacy, moral meaningfulness, and moral courage: a quasi-experimental study. J Bus Ethics. 2014;124(1):67–80. https://doi.org/10.1007/s10551-013-1860-6 .
Hannah ST, Avolio BJ. Moral potency: building the capacity for character-based leadership. Consult Psychol J. 2010;62(4):291–310. https://doi.org/10.1037/a0022283 .
Schaubroeck JM, Hannah ST, Avolio BJ, et al. Embedding ethical leadership within and across organization levels. Acad Manag J. 2012;55(5):1053–78. https://doi.org/10.5465/amj.2011.0064 .
Hannah ST, Avolio BJ, May DR. Moral maturation and moral conation: a capacity approach to explaining moral thought and action. Acad Manag Rev. 2011;36(4):663–85. https://doi.org/10.5465/amr.2010.0128 .
Sekerka LE, Bagozzi RP. Moral courage in the workplace: moving to and from the desire and decision to act. Bus Ethics Eur Rev. 2007;16(2):132–49.
Lazarus RS. Stress and emotion: a New Synthesis. Springer Publishing Company; 1999.
Backović DV, Živojinović JI, Maksimović J, Maksimović M. Gender differences in academic stress and burnout among medical students in final years of education. Psychiatr Danub. 2012;24(2):175–81.
Hill MR, Goicochea S, Merlo LJ. In their own words: stressors facing medical students in the millennial generation. Med Educ Online. 2018;23(1):1530558. https://doi.org/10.1080/10872981.2018.1530558 .
Neumann M, Edelhäuser F, Tauschel D, et al. Empathy decline and its reasons: a systematic review of studies with medical students and residents. Acad Med. 2011;86(8):996–1009. https://doi.org/10.1097/ACM.0b013e318221e615 .
Dyrbye LN, Thomas MR, Shanafelt TD. Medical student distress: causes, consequences, and proposed solutions. Mayo Clin Proc. 2005;80(12):1613–22. https://doi.org/10.4065/80.12.1613 .
Dyrbye LN, Thomas MR, Power DV, et al. Burnout and serious thoughts of dropping out of medical school: a multi-institutional study. Acad Med. 2010;85(1):94–102. https://doi.org/10.1097/ACM.0b013e3181c46aad .
Bresó E, Schaufeli WB, Salanova M. Can a self-efficacy-based intervention decrease burnout, increase engagement, and enhance performance? A quasi-experimental study. Published online 2010. https://doi.org/10.1007/s10734-010-9334-6 .
Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. 2016;15(2):103–11. https://doi.org/10.1002/wps.20311 .
Galán F, Sanmartín A, Polo J, Giner L. Burnout risk in medical students in Spain using the Maslach Burnout Inventory-Student Survey. Int Arch Occup Environ Health. 2011;84(4):453–9. https://doi.org/10.1007/s00420-011-0623-x .
Schaufeli WB, Martinez IM, Pinto AM, Salanova M, Bakker AB. Burnout and engagement in university students: a cross-national study. J Cross Cult Psychol. 2002;33(5):464–81. https://doi.org/10.1177/0022022102033005003 .
Dyrbye LN, Shanafelt T. A narrative review on burnout experienced by medical students and residents. Med Educ. 2016;50(1):132–49. https://doi.org/10.1111/medu.12927 .
Shin HS, Park H, Lee YM. The relationship between medical students’ empathy and burnout levels by gender and study years. Patient Educ Couns. 2022;105(2):432–9. https://doi.org/10.1016/j.pec.2021.05.036 .
Dyrbye LN, Massie FSJ, Eacker A, et al. Relationship between burnout and professional conduct and attitudes among US medical students. JAMA - J Am Med Assoc. 2010;304(11):1173–80. https://doi.org/10.1001/jama.2010.1318 .
Taormina RJ, Law CM. Approaches to preventing burnout: the effects of personal stress management and organizational socialization. J Nurs Manag. 2000;8(2):89–99. https://doi.org/10.1046/j.1365-2834.2000.00156.x .
Locati F, De Carli P, Tarasconi E, Lang M, Parolin L. Beyond the mask of deference: exploring the relationship between ruptures and transference in a single-case study. Res Psychother Psychopathol Process Outcome. 2016;19(2):89–101. https://doi.org/10.4081/ripppo.2016.212 .
Koeske GF, Daimon R. Student burnout as a mediator of the stress-outcome relationship. Res High Educ. 1991;32:415–431.
Gilbey P, Moffat M, Sharabi-Nov A, et al. Burnout in Israeli medical students: a national survey. BMC Med Educ. 2023;23:55–66. https://doi.org/10.1186/s12909-023-04037-2 .
Konings KJP, Gastmans C, Numminen OH, et al. Measuring nurses’ moral courage: an explorative study. Nurs Ethics. 2022;29(1):114–30. https://doi.org/10.1177/09697330211003211 .
Neufeld-Kroszynski G. Medical students’ professional identity formation: a prospective and retrospective study of students’ perspectives. Published online 2021.
Hauhio N, Leino-Kilpi H, Katajisto J, Numminen O. Nurses’ self-assessed moral courage and related socio-demographic factors. https://doi.org/10.1177/0969733021999763 .
Egbert N, Reed PR. Self-efficacy. In: Kim DK, Dearing JW, editors. Health Communication Research Measures. Peter Lang Publishing; 2016. pp. 203–12.
Farajev N, Michael K, Karnieli-Miller, O. The associations between environmental professionalism, empathy attitudes, communication self-efficacy, and moral courage efficacy among medical students. Unpublished.
Ben-Zur H, Michael K. Positivity and growth following stressful life events: associations with psychosocial, health, and economic resources. Int J Stress Manag. 2020;27(2):126–34. https://doi.org/10.1037/str0000142 .
Keech JJ, Hagger MS, O’Callaghan FV, Hamilton K. The influence of university students’ stress mindsets on health and performance outcomes. Ann Behav Med. 2018;52(12):1046–59. https://doi.org/10.1093/abm/kay008 .
Obregon M, Luo J, Shelton J, Blevins T, MacDowell M. Assessment of burnout in medical students using the Maslach Burnout Inventory-Student Survey: a cross-sectional data analysis. BMC Med Educ. 2020;20(1). https://doi.org/10.1186/s12909-020-02274-3 .
Erschens R, Keifenheim KE, Herrmann-Werner A, et al. Professional burnout among medical students: systematic literature review and meta-analysis. Med Teach. 2019;41(2):172–83. https://doi.org/10.1080/0142159X.2018.1457213 .
Hayes AF. Introduction to Mediation, Moderation, and conditional process analysis: a regression-based Approach. 2nd ed. Guilford; 2018.
Cohen J. Statistical Power Analysis for the behavioral sciences. Routledge; 2013. https://doi.org/10.4324/9780203771587 .
Martinez W, Lehmann LS, Thomas EJ, et al. Speaking up about traditional and professionalism-related patient safety threats: a national survey of interns and residents. BMJ Qual Saf. 2017;26(11):869–80. https://doi.org/10.1136/bmjqs-2016-006284 .
Kesselheim JC, Shelburne JT, Bell SK, et al. Pediatric trainees’ speaking up about unprofessional behavior and traditional patient safety threats. Acad Pediatr. 2021;21(2):352–7.
Edmondson AC. The Fearless Organization: creating Psychological Safety in the Workplace for Learning, Innovation, and growth. Wiley; 2018.
Plews-Ogan M, May N, Owens J, Ardelt M, Shapiro J, Bell SK. Wisdom in medicine: what helps physicians after a medical error? Acad Med. 2016;91(2):233–41. https://doi.org/10.1097/ACM.0000000000000886 .
Karnieli-Miller O. Reflective practice in the teaching of communication skills. Patient Educ Couns. 2020;103(10):2166–72. https://doi.org/10.1016/j.pec.2020.06.021 .
Klasen JM, Driessen E, Teunissen PW, Lingard LA. Whatever you cut, I can fix it: clinical supervisors’ interview accounts of allowing trainee failure while guarding patient safety. BMJ Qual Saf. 2020;29(9):727–34. https://doi.org/10.1136/BMJQS-2019-009808 .
Lyndon A, Sexton JB, Simpson KR, Rosenstein A, Lee KA, Wachter RM. Predictors of likelihood of speaking up about safety concerns in labour and delivery. BMJ Qual Saf. 2012;21(9):791–9. https://doi.org/10.1136/bmjqs-2010-050211 .
Ben-zur H. Burnout, social support, and coping at work among social workers, psychologists, and nurses: the role of challenge/control appraisals. Soc Work Health Care. 2007;45(4):63–82. https://doi.org/10.1300/J010v45n04 .
Haghighi M, Gerber M. Does mental toughness buffer the relationship between perceived stress, depression, burnout, anxiety, and sleep? Int J Stress Manag. 2019;26(3):297–305. https://doi.org/10.1037/str0000106 .
Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251(6):995–1000. https://doi.org/10.1097/SLA.0b013e3181bfdab3 .
Fischer MA, Mazor KM, Baril J, Alper E, DeMarco D, Pugnaire M. Learning from mistakes factors that influence how students and residents learn from medical errors. J Gen Intern Med. 2006;21(5):419–23.
Hojat M, Vergare MJ, Maxwell K, et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84(9):1182–91. https://doi.org/10.1097/ACM.0b013e3181b17e55 .
Chen D, Lew R, Hershman W, Orlander J. A cross-sectional measurement of medical student empathy. J Gen Intern Med. 2007;22(10):1434–8. https://doi.org/10.1007/s11606-007-0298-x .
Spencer J. Decline in empathy in medical education: how can we stop the rot? Med Educ. 2004;38(9):916–8. https://doi.org/10.1111/j.1365-2929.2004.01965.x .
Karnieli-Miller O. Caring for the health and well-being of our learners in medicine as critical actions toward high-quality care. Isr J Health Policy Res. 2022;11(1):10. https://doi.org/10.1186/S13584-022-00517-W .
Dyrbye LN, Thomas MR, Harper W, et al. The learning environment and medical student burnout: a multicentre study. Med Educ. 2009;43(3):274–82. https://doi.org/10.1111/j.1365-2923.2008.03282.x .
Download references
Acknowledgements
The authors wish to thank Dr. Lior Rozental in helping in recruiting students to the study. This study was done as part of Orit Karnieli-Miller’s Endowed chair of the Dr. Sol Amsterdam, Dr. David P. Schumann in Medical Education, Tel Aviv University. This study is written in the blessed memory of Oshrit Bar-El, devoted to enhancing Moral Courage.
The manuscript was partially supported by a grant by the by the Israel Science Foundation (grant no. 1599/21).
Author information
Galit Neufeld-Kroszynski and Keren Michael contributed equally to this work.
Authors and Affiliations
Department of Medical Education, Faculty of Medical & Health Sciences, Tel Aviv University, Tel Aviv, 69778, Israel
Galit Neufeld-Kroszynski & Orit Karnieli-Miller
Department of Human Services, Max Stern Yezreel Valley College, Yezreel Valley, Israel
Keren Michael
You can also search for this author in PubMed Google Scholar
Contributions
GNK: conception and design, interpretation of data, drafting and revision of the manuscript, and final approval of the version to be published; KM: analysis and interpretation of data, drafting and revision of the manuscript, and final approval of the version to be published; OKM: conception and design, interpretation of data, drafting and revision of the manuscript, and final approval of the version to be published.
Corresponding author
Correspondence to Orit Karnieli-Miller .
Ethics declarations
Ethics approval and consent to participate.
This study was conducted in accordance with the principles outlined in the Declaration of Helsinki and received ethical approval by the Ethics Committee of Tel-Aviv University on 31/10/2019. Informed written consent was obtained from all participants before their participation in this study.
Consent for publication
Not applicable.
Previous presentations
Study findings were presented at the Academy for Professionalism in Healthcare Conference, June 2nd, 2022, virtual; and the 7th International Conference on Public Health, August 8th, 2021, virtual.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Neufeld-Kroszynski, G., Michael, K. & Karnieli-Miller, O. Associations between medical students’ stress, academic burnout and moral courage efficacy. BMC Psychol 12 , 296 (2024). https://doi.org/10.1186/s40359-024-01787-6
Download citation
Received : 03 December 2023
Accepted : 13 May 2024
Published : 27 May 2024
DOI : https://doi.org/10.1186/s40359-024-01787-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Moral courage
- Self-efficacy
- Medical students
- Professionalism
- Patient safety
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
Indigenous Medicine Blanket Ceremony Honors Traditions and Celebrates Students
Published date.
Story by: Joyce Pritchett / [email protected]
Media Contacts
Media contact: Stephanie Healey / [email protected]
Photos by: Erik Jepsen/ UC San Diego Communications
Article Content
Blankets are intertwined in the stories of our lives. Blankets can represent, life, death and survival. Blankets can tell stories and transcend generations.
As the University of California San Diego School of Medicine wraps up the academic year, first year Native American medical students were recognized, honored and blessed as they celebrated the completion of their first year of medical school with a traditional blanket ceremony. Blanket ceremonies are a pan-Indigenous practice that celebrate individuals going through life-changing events.
In addition to faculty, staff and leaders from UC San Diego School of Medicine, tribal community leaders were on hand to recognize the achievements of the students, many of whom are part of the school’s Program in Medical Education-Transforming Indigenous Doctor Education (PRIME-TIDE). The University of California system-wide PRIME initiative is c ommitted to training physicians to meet the needs of under-resourced communities in California. The PRIME-TIDE program is focused specifically on preparing medical students for careers focused on providing healthcare to Native populations.
Stanley Rodriguez, Ed.D., who is from the Santa Ysabel Band of the Iipay Nation, and a tribal councilman for the Nation spoke at the event.
“People believe in you, we all believe in you.”
At the event Rodriguez, who is also d irector of Kumeyaay Community College, shared his personal medical journey with the students, friends, family, faculty and staff members who were in attendance. He reminded the students about the importance of carrying on traditions and honoring the legacy of their ancestors.
First-year medical students who received blankets include (from left) Averi Wilhelms, Sarah Gierok, Dane Winter, Rachel Maguire, Jessica Ross, Marissa Stinnett and Steven Jump.
Each of the seven Native American students who are wrapping up their first year of medical school were presented with a Blanket of Knowledge. Created by Eighth Generation, a Seattle-based art and lifestyle brand owned by the Snoqualmie Tribe, each blanket was designed by a Native American artist. According to the designer of this blanket, the design is based on the ancient Northwest Coast art practice of Chilkat weaving, one of the most complex weaving techniques in the world. The intricacy of the circular and curved shapes and patterns on the blanket give the perception of movement when draped over the shoulders.
While presenting the blankets, second-year PRIME-TIDE student Katie Mostoller spoke of the significance of the blankets.
“The blankets represent relationships, honor, respect, achievement. Your community is here to celebrate you.”
Mostoller explained that being a Native American medical student is particularly significant because the students’ success in an integrated world means that they are learning how to take the old practices learned from their ancestors and bringing them together into a new context to help foster health and wellbeing within the Native community.
Native American students who had previously been presented blankets were also honored and celebrated at the event. Those students received jackets to acknowledge their continued focus and success within their medical education journey. After the presentation of jackets, each of the students spoke about their respective mentors and community partners, presenting them with gifts to acknowledge the continuing relationships and respect for those who have supported the students thus far.
The event included performances by the Soaring Eagles, a group established in 2008 which is dedicated to educating American Indian families about the tradition of Native American Powwow dance. Additionally, the Kumeyaay Bird Singers accompanied the dancers throughout the evening. The event concluded with a traditional Round Dance, which symbolizes unity and wholeness. Everyone in attendance was encouraged to join the circle and celebrate the students’ achievements and potential.
Share This:
You may also like, using oceanography to understand fronts and cyclones on jupiter, chasing down a cellular ‘short circuit’, uc san diego health first in region to provide novel therapy for melanoma, uc san diego startup incubator helps company expand wireless reach, stay in the know.
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.
You have been successfully subscribed to the UC San Diego Today Newsletter.
Campus & Community
Arts & culture, visual storytelling.
- Media Resources & Contacts
Signup to get the latest UC San Diego newsletters delivered to your inbox.
Award-winning publication highlighting the distinction, prestige and global impact of UC San Diego.
Popular Searches: Covid-19 Ukraine Campus & Community Arts & Culture Voices
Does Med School Have a DEI Problem?
As medicine becomes more politicized, a debate is raging over what it means for patient care.

Listen to this article
Produced by ElevenLabs and News Over Audio (NOA) using AI narration.
“People will die if doctors misdiagnose patients.” This is true as far as it goes. But the recent news that prompted Elon Musk to share this observation on X was not precisely about medical errors. It was about what he might call the “ woke mind virus .” A story by Aaron Sibarium in The Washington Free Beacon had revealed complaints that UCLA’s medical school was admitting applicants partly based on race—a practice that has long been outlawed in California public schools. And this process wasn’t just discriminatory, the story argued; it was potentially disastrous for the public.
The Free Beacon noted that the med school’s U.S. News & World Report ranking had dropped from 6 to 18 since 2020, and the story shared leaked data showing students’ poor performance on their shelf exams . (These evaluations are used as preparation for the national licensing exams that every M.D. recipient must pass before they can practice medicine in the United States.) According to Sibarium, almost one-quarter of the class of 2025 had failed at least three shelf exams, while more than half of students in their internal-medicine, family-medicine, emergency-medicine, or pediatrics rotations had failed tests in those subjects at one point during the 2022–23 academic year—and those struggles led many trainees to postpone taking their national licensing exams. “I don’t know how some of these students are going to be junior doctors,” one unnamed UCLA professor told him. “Faculty are seeing a shocking decline in knowledge of medical students.”
Steven Dubinett, the dean of UCLA med school, denied the story’s allegations. He told me that the admissions committee does not give advantages to any applicants based on race, and he called it “malign and totally not true” to say that his students have been struggling. Dubinett believes that anti-DEI sentiment both within and outside the school is to blame for stirring up this controversy: People “think diversity, equity, and inclusion is in some way against them. And nothing could be further from the truth,” he said. But the stakes are high for prospective doctors and patients alike. The Free Beacon ’s claims call attention to a heated fight among medical educators over how much admissions criteria and test scores actually matter, and whether they have any bearing on what it means to be a good physician.
Read: When medical schools become less diverse
Sibarium asserts that both UCLA’s fall in the rankings and its decline in test performance can be blamed, in part, on race-based admissions. The latter metric “coincided with a steep drop in the number of Asian matriculants,” the story said, and was associated with a change in the med school’s admissions standards. Dubinett told me that the decline in shelf-exam performance was “modest.” He also pointed to data shared with the UCLA community by the school after the publication of the Free Beacon story, which show that every test-taker had passed surgery, neurology, and emergency medicine during a recent set of exams from 2023–24. The data also show that, for most other specialties, the passing rates were close to the expected benchmark of 95 percent. Moreover, 99 percent of UCLA’s med students had passed the second of three tests required to obtain a medical license on their first try as of 2022–23, and scores have remained above the national average over the past three years.
Meanwhile, the Free Beacon offers little more than speculation about how UCLA’s shifting racial demographics might be linked to academic problems at the school. Nationwide, Black and Hispanic medical students do matriculate with slightly lower grades and scores on the standardized Medical College Admission Test than white and Asian matriculants, according to statistics compiled by the Association of American Medical Colleges. Yet data from UCLA and the AAMC show that the average MCAT scores of UCLA’s accepted medical students have not declined in recent years. As for grades, the average GPA among UCLA’s accepted applicants is 3.8—up from 3.7 in 2019. Dubinett told me that the school sets a minimum threshold for MCAT scores and GPAs that is designed to produce a high graduation rate. “There’s a cutoff based on national data—it’s not made up in our back room,” he said. “We've got nearly 14,000 students applying for 173 spots. Are you going to tell me that we’re getting people who are unqualified?”
So what did happen in 2022 to suddenly make so many students perform poorly on their shelf exams? The Free Beacon acknowledges that the med school began a major update to its curriculum in 2020. Following a national trend , UCLA significantly cut back the initial amount of time spent on classroom teaching so that clinical rotations could begin a year earlier. Med schools have been trying to expose their students to real-world experiences sooner, on the principle that book-learned facts are less worthwhile without on-the-job training. Yet shelf exams still require memorizing a hefty dose of facts, which can only be more difficult given less time to study. Dubinett chalks up the initial drop in scores to having students take the tests earlier in their education. Five other medical schools, he notes, also reported a decline in shelf-exam performance under a compressed curriculum.
From the May 1966 issue: “Our Backward Medical Schools”
Whether med schools’ broader shift away from traditional coursework has been producing better doctors overall is a separate question. A new curriculum that led to lower standardized-test scores in the short term might be associated, in the long run, with either better or worse clinical care. But no one really knows which is the case. There is still no reliable way to track educational quality. The influential—but controversial — U.S. News med-school rankings, for instance, don’t directly evaluate how good a program is at preparing future doctors. The benefits (or costs) of switching up criteria for admission into med school are just as mysterious. One study counted as many as 87 different personal qualities that are considered useful in the practice of medicine. Which qualities matter most is anyone’s guess.
At UCLA, dry—yet still important—scientific material has been compressed in favor of hands-on experience. The school has also committed to instilling its student body with a social consciousness . In prior coverage for the Free Beacon , Sibarium has described the mandatory Structural Racism and Health Equity course for first-years, which, according to a 2023–24 syllabus obtained by the Free Beacon , intends to help students “develop a structurally competent, anti-racist lens for viewing and treating health and illness,” and encourages them to become “physician-advocates within and outside of the clinical setting.” The Free Beacon called attention to pro-Palestinian, anti-capitalist, and fat-activist messaging included in the course this academic year. That story quotes a former dean of Harvard Medical School, Jeffrey Flier, who described the course as “truly shocking” and said that it is based on a “socialist/Marxist ideology that is totally inappropriate.” (Dubinett told me that the entire first-year curriculum is being evaluated.) Other academics have expressed concern about how a similar approach to teaching students, adopted on a larger scale, might be changing medicine. Schools’ focus on racism and inequality “is coming at the expense of rigorous training in medical science. The prospect of this ‘new,’ politicized medical education should worry all Americans,” Stanley Goldfarb, a former associate dean at the University of Pennsylvania medical school, wrote in a 2019 op-ed in The Wall Street Journal . In a follow-up from 2022 , he warned of a “woke takeover of healthcare.”
Read: The French are in a panic over le Wokisme
What, exactly, makes a med school “woke”? Any physician can see that unevenly distributed wealth and opportunity play a role in people’s health, and that many illnesses disproportionately fall along racial lines. Doctors who learn about these topics while in school may be more cognizant of them in the clinic. Indeed, after Goldfarb’s first essay was published in the Journal , some physicians started sharing stories that could be taken to support this argument: Posting under the hashtag #GoldfarbChallenge, they described how trying to help patients navigate dire living situations is as much a part of the job as recalling the nuances of biochemistry.
Acknowledging inequality is not an entirely new phenomenon in medicine. Schools were already teaching classes on cultural competence and health disparities when I was a student at the University of Rochester a decade ago. What is different is the open endorsement of political activism—almost always from a left-wing perspective. I certainly attended my share of lectures on how to care for patients from different backgrounds, but I don’t recall witnessing any lecturers leading classroom chants of “ Free, Free Palestine ,” as allegedly occurred during UCLA’s first-year course this spring. Since I graduated, the AAMC has published a voluntary set of “ Diversity, Equity, and Inclusion Competencies ” that encourage trainees to “influence decision-makers and other vested groups” by advocating for “public policy that promotes social justice and addresses social determinants of health.” The guidance lists “colonization, White supremacy, acculturation, assimilation” as “systems of oppression” whose impact must be remedied. This new pedagogical approach comes at a time when U.S. physician groups have taken vocal stances on controversial issues such as gun violence , transgender rights , and mask mandates .
I suspect this left turn in medicine was born of a feeling of impotence, rather than a Marxist conspiracy. Doctors have always been better at altering people’s physiology than fixing the social and economic circumstances of their patients. Perhaps medical schools now figure that health outcomes will improve if physicians become more involved in progressive politics. But whatever the intention, this approach will alienate a lot of patients. In recent months, some doctors have been disciplined for voicing pro-Palestine or pro-Israel stances—presumably on behalf of potential patients who might be offended by their politics. Maybe the same caution should apply to med-school lectures given at UCLA.
The push for improved student-body diversity has also grown in prominence. For most of the 20th century , schools encouraged applicants to fit the typical pre-med profile of a diligent lab rat. Over the past few decades, that attitude has changed. Now admissions offices are more comfortable with the idea that students who haven’t focused on the hard sciences or don’t have perfect academic records can still become successful—or might be even better—physicians.
I credit this shift for my own admission to medical school. I was a socially minded liberal-arts student who decided to study linguistics after a calamitous run-in with organic chemistry. By the time I applied, some schools had decided that MCAT scores were not the ultimate determinant of who will make a good doctor. My university was so interested in attracting the sorts of kids who might enrich the campus through what it now calls “the diversity of their educational and experiential backgrounds” that it allowed me to skip the exam altogether. I did end up having academic struggles, and passed anatomy by the skin of my teeth (having failed to correctly answer how many teeth humans have, among other questions). Now I’m a medical-school professor myself. It takes all kinds.
To this day, would-be doctors are expected to master an incredible amount of minutiae, but it is only through clinical practice that they figure out which facts matter most. Nothing is as clarifying as seeing patients live or die because of what you know—or, just as often, how well you communicate it. The Free Beacon article relayed an anecdote by a faculty member describing how a student “could not identify a major artery” in the operating room when asked. Being told to pick out an artery on the spot and failing at that task is, frankly, a rite of passage for medical students. But I’ve seen more people hurt by doctors who didn’t know how to speak Spanish or build rapport than by doctors who forgot the name of a blood vessel. If we keep arguing over what health-care professionals must know, it’s because the answers are as varied as our patients.
- (888) 381-9509
- [email protected]
- Book a Meeting
- student login
- Student Login
- Our Services
- Our Story How it started
- Our Team Meet Our Advisors & Tutors
- Our Services How we can help you
- Our Difference Learn why we stand out
- Success Stories & Testimonials Hear the stories
- For Parents Learn why you should trust us
- Organizational Partners Provide value to your students
- Institutional Partners Enhance your student offering
- In the News Read Our Stories
- Frequently Asked Questions Find answers
- MCAT Tutoring One-on-One Personalized Help
- MCAT Go An Audio Learning Experience
- MCAT Practice Exams Boost Your Score
- MCAT Prep App Videos, Flashcards & Q-Bank
- MCAT CARS Mastery Top-Rated CARS Video Course
- Pre-Med Coach 9th & 10th Grade Roadmap Planning
- College Admissions 11th & 12th Grade Pre-Med Consulting
- Direct Medical (BS/MD & BA/MD) Application Consulting
- Interview Preparation BS/MD Candidates
- Pre-Med Coach Pre-Application Development
- Application Advising Med School Admissions Support
- Personal Statement Editing Refine Your Narrative
- AMCAS Editing Application Editing
- Secondary Editing Secondary Application Editing
- Interview preparation Realistic Practice
- CASPer Preparation Simulation & Coaching
- Ontario Application Support OMSAS Application
- Residency Advising Complete Match Support
- Residency Interview Preparation
- ERAS Personal Statement Refine Your Story
- USMLE STEP 1 Maximize your scores
- USMLE STEP 2 Shine on your boards
- USMLE STEP 3 Conquer your final hurdle
- COMLEX LEVEL 1 and 2 Score higher
- Travel with Us Hands-On Clinical & Research
- Virtual Shadowing Explore Medical Specialties
- Under the Stethoscope Admissions Video Course
- Research Roadmap Master Clinical Research
- MSC Score Calculate Your Chances
- Guidebooks Comprehensive Guides
- Med School Explorer Find Your School
- MCAT Review Videos, Questions, Notes
The Only 3 Medical School Personal Statement Examples You Need to Read
Posted in: Applying to Medical School

Table of Contents
The personal statement is one of the most important parts of the med school application process because t his mini-essay is a critical opportunity for you to stand out from other prospective medical students by demonstrating your passion and personality, not just your grades.
Admissions committees receive hundreds or more AMCAS medical school applications , so yours should be unique and captivating. Your medical school personal statement shows admissions officers who you are beyond your high school or pre-med GPA , extracurriculars , and MCAT score .
The best personal statements are… well, personal . This is your chance to share what life experiences have compelled you toward a career in healthcare or the medical field , and how those experiences shape the picture of your ideal future.
MedSchoolCoach has crucial advice for writing your personal statement .
Read these examples of personal statements for prospective med students.
Writing a great medical school personal statement is a lot easier with the right support. We’ve helped numerous med school applicants craft top-notch personal statements and can do the same for you.
But first: 7 steps to writing an engaging personal statement.
Before you read these excellent examples, you need to understand the process of writing a personal statement.
Include these in your medical school personal statement:
- Why you’re passionate about becoming a doctor
- Your qualities that will make you a great physician
- Personal stories that demonstrate those qualities
- Specific examples of the communities you want to serve as a member of the medical field
What are the most important things to remember when writing a medical school personal statement ?
- Begin the writing process early: Give yourself plenty of time for brainstorming and to revisit your first draft, revising it based on input from family members and undergrad professors. Consult the application timeline for your target enrollment season.
- Choose a central theme: An unfocused essay will leave readers confused and uninterested. Give your statement a clear thesis in the first paragraph that guides its formation.
- Start with a hook: Grab the reader’s attention immediately with your statement’s first sentence. Instead of opening with a conventional introduction, be creative! Begin with something unexpected.
- Be the you of today, not the you of the future: Forecasting your future as a physician can come across as empty promises. Don’t get caught up in your ambitions; instead, be honest about your current situation and interest in the field of medicine.
- Demonstrate your passion: It’s not enough to simply state your interest in becoming a doctor; you have to prove it through personal stories. Show how your perspectives have been shaped by formative experiences and how those will make you an effective physician.
- Show, don’t tell : Avoid cliches that admissions committees have heard hundreds of times, like “I want to help people.” Make your writing come alive with dynamic, persuasive storytelling that recounts your personal experiences.
- Tie everything together: Conclude by wrapping up your main points. Reiterate your passion for the medical profession, your defining personal qualities, and why you’ll make a good doctor.
You can read more about our recommended method in our step-by-step guide , but those are the major points.

Example 1 — From the Stretcher to the Spotlight: My Journey to Becoming an Emergency Medicine Physician
Another siren shrieks as the emergency room doors slide open and a team of EMTs pushes a blood-soaked stretcher through the entrance. It’s the fifth ambulance to arrive tonight — and only my first clinical shadowing experience in an emergency medicine department since my premed education began.
But it wasn’t my first time in an emergency room, and I knew I was meant to be here again.
In those crucial moments on the ER floor, many of my peers learned that they stumble in high-pressure environments. A few weeks of gunshot wounds, drug overdoses, broken bones, and deep lacerations in the busiest trauma bay in the region were enough to alter their career path.
They will be better practitioners somewhere predictable, like a pediatrician in a private practice where they choose their schedules, clients, and staff.
Every healthcare provider has their specialties, and mine are on full display in those crucial moments of lifesaving care. Why am I pursuing a career in Emergency Medicine? Because I’ve seen firsthand the miracles that Emergency Medicine physicians perform.
12 years ago, I was in an emergency room… but I was the one on the stretcher.
A forest-green Saturn coupe rolled into my parent’s driveway. The driver, my best friend Kevin, had just passed his driving test and was itching to take a late-night run to the other side of town. I had ridden with Kevin and his father many times before when he held his learner’s permit. But this time, we didn’t have an adult with us, and the joyride ended differently: with a 40-mph passenger-side collision, T-boned by a drunk driver.
I distinctly recall the sensation of being lifted out of the crumpled car by a paramedic and laid onto a stretcher. A quick drive later, I was in the care of Dr. Smith, the ER resident on call that night. Without missing a beat, he assessed my condition and provided the care I needed. When my mom thanked him for saving my life, he simply responded, “It’s what he needed.”
Now I’m watching other doctors and nurses provide this life-saving care as I observe as a premed student. I see the way the staff works together like a well-oiled machine, and it reminds me of my time in high-school theater.
Everyone has a role to play, however big or small, to make the show a success. All contributions are essential to a winning performance — even the technicians working behind the scenes. That’s what true teamwork is, and I see that same dynamic in the emergency department.
Some actors freeze during performances, overcome by stage fright. Other students are too anxious to even set foot in front of an audience; they remain backstage assisting with split-second costume changes.
Not me. I felt energized under the spotlight, deftly improvising to help my co-stars when they would forget their lines. Admittedly, I wasn’t the best actor or singer in the cast, but I provided something essential: assurance under pressure. Everyone knew me as dependable, always in their corner when something went awry. I had a reputation for remaining calm and thinking on my feet.
My ability to stay unruffled under pressure was first discovered on stage, but I can use it on a very different platform providing patient care. Now, when other people freeze under the intensity of serving public health on the front lines, I can step in and provide my calm, collected guidance to see them through.
As an ER doctor, I will have to provide that stability when a nurse gets flustered by a quarrelsome patient or shaken from an irreparably injured infant. When you’re an Emergency Medicine physician, you’re not following a script. It takes an aptitude of thinking on your toes to face the fast pace and unpredictable challenges of an emergency center.
During my time shadowing, I saw experienced physicians put those assured, gentle communication skills to use. A 13-year-old boy was admitted for a knife wound he’d received on the streets. He only spoke Spanish, but it was clear he mistrusted doctors and was alarmed by the situation. In mere minutes, one of the doctors calmed the patient so he could receive care he needed.
Let me be clear: I haven’t simply gravitated toward Emergency Medicine because I liked it most. It’s not the adrenaline or the pride that compel me. I owe Emergency Medicine my life, and I want to use my life to extend the lives of other people. Every person brought into the trauma bay could be another me , no matter what they look like.
People are more than their injury, health record, or circumstances. They are not just a task to complete or a challenge to conquer.
My childhood injury gave me an appreciation for the work of ER doctors and a compassion for patients, to foster well-being when people are most broken and vulnerable. I already have the dedication to the work and the heart for patients; I just need the medical knowledge and procedural skills to perform life-saving interventions. My ability to remain calm, think on my toes, be part of a team, and work decisively without making mistakes or overlooking critical issues will serve me well as an Emergency Medicine physician.
Some ER physicians I spoke with liked to think that they’re “a different breed” than other medical professionals — but I don’t see it that way. We’re just performing a different role than the rest of the cast.
Breaking It Down
Let’s look at what qualities make this a great personal statement for med school.
- Engaging opening: The writer painted a vivid scene that immediately puts the reader in their shoes and leaves them wanting more.
- Personal examples: The writer demonstrated his ability to stay calm, work as a team, and problem-solve through theater experience, which he also uses as a comparison. And, he explained his passion for Emergency Medical care from his childhood accident.
- Organized: The writer transitions fluidly between body paragraphs, connecting stories and ideas by emphasizing parallels and hopping back and forth between time.
- Ample length: Makes full use of the AACOMAS and AMCAS application personal statement’s character limit of 5,300 characters (including spaces), which is about 850-950 words.
Unsure what traits and clinical or research experience your preferred medical school values ? You can research their admissions requirements and mission statement using the MSAR .
Example 2 — Early Clinical Work For Empathetic Patient Care
The applicant who wrote this personal statement was accepted into University of South Florida Morsani College of Medicine, University of Central Florida College of Medicine, and Tufts University School of Medicine.
As I walked briskly down the hall to keep up during our daily rounds in the ICU, I heard the steady beeping of Michelle’s cardiac monitor and saw a ruby ornament twinkling on the small Christmas tree beside her. She was always alone, but someone had decorated her room for the holidays.
It warmed my heart that I wasn’t the only one who saw her as more than a patient in a coma. I continually felt guilty that I couldn’t spend more time with her; her usual companions were ventilators, IV bags, and catheters, not to mention the golf ball-sized tumors along her spine. Every day, I thought about running to Michelle’s bedside to do anything I could for her.
Thus, I was taken aback when my advisor, who was visiting me that day, asked me if I was okay. It never crossed my mind that at age 17, my peers might not be able to handle the tragedies that healthcare workers consistently face. These situations were difficult, but they invoked humanity and compassion from me. I knew I wanted to pursue medicine. And I knew I could do it.
From my senior year of high school to my senior year of college, I continued to explore my passion for patient interaction.
At the Stepp Lab, I was charged with contacting potential study participants for a study focusing on speech symptoms in individuals with Parkinson’s Disease. The study would help future patients, but I couldn’t help but think: “What are we doing for these patients in return?” I worried that the heart and soul behind the research would get lost in the mix of acoustic data and participant ID numbers.
But my fears were put to rest by Richard, the self-proclaimed “Parkinson’s Song & Dance Man,” who recorded himself singing show tunes as part of his therapy. Knowing that he was legally blind and unable to read caller ID, I was always thrilled when he recognized my voice. The spirit in his voice indicated that my interest in him and his journey with Parkinson’s was meaningful. Talking with him inspired me to dive deeper, which led to an appreciative understanding of his time as a sergeant in the U.S. military.
It was an important reminder: my interest and care are just as important as an effective prescribed treatment plan.
Following graduation, I began my work as a medical assistant for a dermatologist. My experience with a patient, Joann, validated my ability to provide excellent hands-on patient care. Other physicians prescribed her painkillers to relieve the excruciating pain from the shingles rash, which presented as a fiery trail of blisters wrapped around her torso. But these painkillers offered no relief and made her so drowsy that she fell one night on the way to the bathroom.
Joann was tired, suffering, and beaten down. The lidocaine patches we initially prescribed would be a much safer option, but I refused for her to pay $250, as she was on the brink of losing her job. When she returned to the office a week later, she held my hand and cried tears of joy because I found her affordable patches, which helped her pain without the systemic effects.
The joy that pierced through the weariness in her eyes immediately confirmed that direct patient care like this was what I was meant to do. As I passed her a tissue, I felt ecstatic that I could make such a difference, and I sought to do more.
Since graduation, I have been volunteering at Open Door, a small pantry that serves a primarily Hispanic community of lower socioeconomic families. It is gut-wrenching to explain that we cannot give them certain items when our stock is low. After all, the fresh fruits and vegetables I serve are fundamental to their culturally-inspired meals.
For the first time, I found myself serving anguish rather than a helping hand. Usually, uplifting moments strengthen one’s desire to become a physician, but in this case, it was my ability to handle the low points that reignited my passion for aiding others.
After running out of produce one day, I was confused as to why a woman thanked me. Through translation by a fellow volunteer, I learned it was because of my positivity. She taught me that the way I approach unfavorable situations affects another’s perception and that my spirited attitude breaks through language barriers.
This volunteer work served as a wake-up call to the unacceptable fact that U.S. citizens’ health suffers due to lack of access to healthy foods. If someone cannot afford healthy foods, they may not have access to healthcare. In the future, I want to partner with other food banks to offer free services like blood pressure readings. I have always wanted to help people, but I now have a particular interest in bringing help to people who cannot afford it.
While the foundation of medicine is scientific knowledge, the foundation of healthcare is the word “care” itself. I never found out what happened to Michelle and her Christmas tree, but I still wonder about her to this day, and she has strengthened my passion to serve others. A sense of excitement and comfort stems from knowing that I will be there for people on their worst days, since I have already seen the impact my support has had.
In my mind, becoming a physician is not a choice but a natural next step to continue bringing humanity and compassion to those around me.
How did this personal statement grab and sustain attention so well?
- Personalization: Everything about this statement helps you to understand the writer, from their personal experiences to their hope for how their future career will look.
- Showing, not telling: From the first sentence, the reader is hooked. This prospective medical student has plenty of great “on paper” experience (early shadowing, clinical experience, etc.), but they showed this with storytelling, not by repeating their CV.
- Empathy: An admissions committee reading this personal statement would know beyond a shadow of a doubt that this student cares deeply about their patients. They remember first names, individual details, and the emotions that each patient made them feel.
- A clear path forward: The writer doesn’t just want to work in the medical field — they have a passion for exactly how they want to impact the communities they serve. Outside of strictly medical work, they care about the way finances can limit access to healthcare and the struggle to find healthy food in food deserts around the US .
Read Next: How Hard Is It to Get Into Medical School?
Example 3 — Beyond the Diagnosis: The Importance of Individualized Care in Medicine
The applicant who wrote this personal statement was accepted into Touro College of Osteopathic Medicine and Nova Southeastern University College Of Osteopathic Medicine.
Dr. Haywood sighs and shakes her head upon opening the chart. “I was worried about her A1C. It’s up again. Hypertension, too. Alright, let’s go.”
As we enter the patient’s room, I’m expecting the news about her blood sugar and pressure to fill the room. Instead, Dr. Haywood says, “Roseline! How are you doing? How’s your girl, doing well?”
Dr. Haywood continues to ask questions, genuinely interested in Roseline’s experience as a new mother. If not for the parchment-lined examination chair and anatomy posters plastered to the wall, this exchange could be happening in a grocery store. What about her A1C? Her blood pressure? Potential Type II diabetes?
As I continue to listen, Dr. Haywood discovers that Roseline’s mother moved in with her, cooking Haitian meals I recognize as high on the glycemic index. Dr. Haywood effortlessly evolves their conversation to focus on these. Being Haitian herself, she knows some traditional dishes are healthier than others and advises Roseline to avoid those that might exacerbate her high blood sugar and blood pressure. Dr. Haywood also suggests Roseline incorporate exercise by bringing her baby on a walk through her neighborhood.
During my shadowing experience, I observed one of the core components of being a physician through several encounters like this one. By establishing a relationship with her patient where Roseline was comfortable sharing the details of new motherhood, Dr. Haywood was able to individualize her approach to lowering the patient’s A1C and hypertension. Inspired by her ability to treat the whole person , I began to adopt a similar practice as a tutor for elementary kids in underserved areas of D.C.
Shaniyah did not like Zoom, or math for that matter. When I first met her as a prospective tutee online, she preferred to keep her microphone muted and would claim she was finished with her math homework after barely attempting the first problem. Realizing that basing our sessions solely on math would be fruitless, I adapted my tutoring style to incorporate some of the things for which she had a natural affinity.
The first step was acknowledging the difficulties a virtual environment posed to effective communication, particularly the ease at which distractions might take over. After sharing this with Shaniyah, she immediately disclosed her struggles to share her work with me. With this information, I found an online platform that allowed us to visualize each other’s work.
This obstacle in communication overcome, Shaniyah felt more comfortable sharing details about herself that I utilized as her tutor. Her love of soccer gave me the idea to use the concept of goal scoring to help with addition, and soon Shaniyah’s math skills and enthusiasm began to improve. As our relationship grew, so did her successes, and I suspect the feelings I experienced as her tutor are the same as a physician’s when their patient responds well to prescribed treatment.
I believe this skill, caring for someone as a whole person , that I have learned and practiced through shadowing and tutoring is the central tenet of medicine that allows a doctor to successfully treat their patients.
Inspired by talking with patients who had received life-altering organ transplants during my shadowing experience, I created a club called D.C. Donors for Georgetown University students to encourage their peers to register as organ donors or donate blood. This experience taught me that to truly serve a person, you must involve your whole person, too.
In starting this club to help those in need of transplants, I had to dedicate my time and effort beyond just my physical interactions with these patients. For instance, this involved reaching out to D.C.’s organ procurement organization to inquire about a potential partnership with my club, to which they agreed. In addition, I organized tabling events on campus, which required significant planning and communication with both club members and my university.
Though exciting, starting a club was also a difficult process, especially given the limitations the pandemic imposed on in-person meetings and events. To adapt, I had to plan more engaging meetings, designing virtual activities to make members more comfortable contributing their ideas. In addition, planning a blood drive required extensive communication with my university to ensure the safety of the staff and participants during the pandemic.
Ultimately, I believe these behind-the-scenes actions were instrumental in addressing the need for organ and blood donors in the D.C. area.
From these experiences, I have grown to believe that good medicine not only necessitates the physician cares for her patient as a whole, but also that she fully commits her whole person to the care of the patient. Tutoring and starting D.C. Donors not only allowed me to develop these skills but also to experience such fulfilling emotions: the pride I had in Shaniyah when her math improved, the gratefulness I felt when she confided in me, the steadfast commitment I expressed to transplant patients, and the joy I had in collaborating with other passionate club members.
I envision a career as a physician to demand these skills of me and more, and I have confirmed my desire to become one after feeling so enriched by practicing them.
Here’s what makes this personal statement such a good example of what works:
- Desirable qualities: The student clearly demonstrates qualities any school would want in an applicant: teachability, adaptability, leadership, organization, and empathy, to name a few. This again uses the “show, don’t tell” method, allowing the readers to understand the student without hand-holding.
- Personalized storytelling: Many in the healthcare profession will connect with experiences like the ones expressed here, such as addressing patient concerns relationally or the lack of blood donors during the recent pandemic. The writer automatically makes a personal link between themselves and the admissions committees reading this statement.
- Extensive (but not too long): Without feeling too wordy, this personal statement uses nearly all of the 5,300 characters allowed on the AMCAS application. There’s no fluff left in the final draft, only what matters.
Avoid These Common Mistakes
You can learn a lot from those personal statements. They avoid the most common mistakes that med school applicants make when writing the medical school personal statement.
Here are some things you should avoid in your personal statement if you want to be a doctor:
- Name-dropping: Admissions counselors won’t be impressed when you brag about your highly regarded family members, associates, or mentors. You need to stand on your own feet — not someone else’s.
- Dishonesty: Lies and exaggerations can torpedo your application. And they’re bad habits for anyone entering the medical field. Don’t do it.
- Unedited AI content: Artificial intelligence can help you edit and improve your writing, but don’t let it do the work for you. Your statement needs to be authentic, which means in your voice! A chatbot can’t feel or adequately convey your own empathy, compassion, trauma, drive, or personality.
- Grammatical errors and typos: Have someone reliable proofread your essay and scour it for typos, misspellings, and punctuation errors. Even free grammar-checking apps can catch mistakes!
- Telling without showing: I’ll reiterate how important it is to prove your self-descriptive statements with real-life examples. Telling without showing won’t persuade readers.
- Too many examples: Have 3-4 solid personal stories at most; only include a few that are crucial for providing your points. The more experiences you share, the less impact they’ll make.
- Fluff and filler: Cut all fluff, filler words, and irrelevant points. There are many other places you can include information in your application, such as secondary essays on your clinical experience, volunteer work, and research projects .
You can find more valuable do’s and don’ts in our in-depth guide to writing your best personal statement .
Need extra help? We’ve got you covered.
Schedule a meeting with medschoolcoach for expert support on writing and editing your personal statement. we’re here to help you impress medical school admissions committees .

Renee Marinelli, MD
Dr. Marinelli has practiced family medicine, served on the University of California Admissions Committee, and has helped hundreds of students get into medical school. She spearheads a team of physician advisors who guide MedSchoolCoach students.
See How We Can Help
Search for:, recent posts, medschoolcoach, recent blog posts.

Can You Negotiate a Medical School Scholarship?
When you receive a medical school acceptance, you are elated, and rightfully so! You've worked a tremendous amount to get[...]
March 7, 2018

What an Admissions Committee Member Looks for During an Interview
We sat down with Dr. Harvey Katzen, a clinical oncologist and former admissions committee member at George Washington University School[...]
August 19, 2016

What Are DO Schools? [Admissions, Top Schools, + Full List]
Table of Contents Over the last decade, the number of enrolled osteopathic medical students has risen by 77% in the[...]
September 30, 2023

The Pre-Med Journey: What it Takes to Get into Medical School
Thinking about applying to medical school? Discover what high school students need to know about obtaining a career in medicine.

Successfully Planning for the USMLE Step 1 and 2 CK
Get ready for the USMLE Step 1 and Step 2 with this free guide to study planning and resource utilization.
100 MCAT Study Tips
Taking the MCAT? These 100 tips and tricks will help you ace the MCAT.
Call us at (888) 381-9509
Call Us Now
Or, Schedule a Meeting Below

Happy April Fool’s Day from MedSchoolCoach!
While mastering sleep-learning is still a dream, mcat go helps you study for the mcat while you are awake. listen to mcat go for free (a $99 value) by entering your email below to receive an exclusive discount code. this ain’t no joke..
Recent high school grads win scholarships for essays about teen mental health and policing
NORTH KANSAS CITY, Mo. (KCTV) - Two area high schoolers got a special honor on Wednesday from Crimestoppers and the KC Metro Chiefs and Sheriff’s Association.
Two graduating seniors, one from each side of the state line, were awarded a $2,000 scholarship for their winning essays on how the pandemic impacted mental health and in teens, how that contributed to teen violence, and what law enforcement can do to address that.
You may know Crimestoppers as the organization that runs the TIPS Hotline, trying to help police solve violent crimes, but they also have a mission of giving back with things like the scholarships. The teens’ essays both talked about their own challenges handling isolation during the pandemic.
“We wanted to ask that question because we needed to hear straight from them what they went through, and it was insightful to know what they went through,” said Det. Christina Ludwig, the Greater Kansas City Crimestoppers Program coordinator.
The teens wrote about the value of Crisis Intervention Teams trained in mental health response, community policing, and youth outreach.
Da’Vontae Rochester graduated from Lincoln Preparatory Academy in the Kansas City Public Schools. She did a ride-along with CIT officers and said it gave her a new perspective. She advocates for more activities like that.
“Hands-on programs with the teens and officers to just kind of give teens a look on how police interact with each other,” Rochester suggested as a way of addressing teen violence.
Graycie Brockman graduated from Leavenworth High School. Her essay included takeaways from research on the value of community policing.
“Doing things within the community that the youth can be a part of, and the officers can be a part of, I think is a really important piece that I focused on,” Brockman said.
The scholarship money will go directly to the college or trade school of their choice.
Rochester plans to major in psychology to become a criminal psychologist. Brockman wants to pursue a career in the medical field.
Copyright 2024 KCTV. All rights reserved.

Kansas City 8th grader runs 4th-fastest mile in the nation

More than 10,000 human remains found on suspected serial killer’s farm

Victim in critical condition, 5 suspects in custody following fight over video game in Overland Park

As teen continues to recover in Raytown child abuse case, his aunt speaks out

Chiefs cancel practice after medical emergency involving player
Latest news.

Report: Chiefs’ BJ Thompson ‘still unconscious,’ remains in stable condition following cardiac arrest

Illinois basketball player seeks to admit mistaken-identity evidence in Lawrence rape case

Kansas City Pride Fest, parade march forward despite stage theft

Judge raises bond for suspect tied to Hereford House food contamination

- Medical School Application
Medical School Personal Statement Examples That Got 6 Acceptances
Featured Admissions Expert: Dr. Monica Taneja, MD
These 30 exemplary medical school personal statement examples come from our students who enrolled in one of our application review programs. Most of these examples led to multiple acceptance for our students. For instance, the first example got our student accepted into SIX medical schools. Here's what you'll find in this article: We'll first go over 30 medical school personal statement samples, then we'll provide you a step-by-step guide for composing your own outstanding statement from scratch. If you follow this strategy, you're going to have a stellar statement whether you apply to the most competitive or the easiest medical schools to get into .
>> Want us to help you get accepted? Schedule a free strategy call here . <<
Listen to the blog!
Article Contents 36 min read
Stellar medical school personal statement examples that got multiple acceptances, medical school personal statement example #1.
I made my way to Hillary’s house after hearing about her alcoholic father’s incarceration. Seeing her tearfulness and at a loss for words, I took her hand and held it, hoping to make things more bearable. She squeezed back gently in reply, “thank you.” My silent gesture seemed to confer a soundless message of comfort, encouragement and support.
Through mentoring, I have developed meaningful relationships with individuals of all ages, including seven-year-old Hillary. Many of my mentees come from disadvantaged backgrounds; working with them has challenged me to become more understanding and compassionate. Although Hillary was not able to control her father’s alcoholism and I had no immediate solution to her problems, I felt truly fortunate to be able to comfort her with my presence. Though not always tangible, my small victories, such as the support I offered Hillary, hold great personal meaning. Similarly, medicine encompasses more than an understanding of tangible entities such as the science of disease and treatment—to be an excellent physician requires empathy, dedication, curiosity and love of problem solving. These are skills I have developed through my experiences both teaching and shadowing inspiring physicians.
Medicine encompasses more than hard science. My experience as a teaching assistant nurtured my passion for medicine; I found that helping students required more than knowledge of organic chemistry. Rather, I was only able to address their difficulties when I sought out their underlying fears and feelings. One student, Azra, struggled despite regularly attending office hours. She approached me, asking for help. As we worked together, I noticed that her frustration stemmed from how intimidated she was by problems. I helped her by listening to her as a fellow student and normalizing her struggles. “I remember doing badly on my first organic chem test, despite studying really hard,” I said to Azra while working on a problem. “Really? You’re a TA, shouldn’t you be perfect?” I looked up and explained that I had improved my grades through hard work. I could tell she instantly felt more hopeful, she said, “If you could do it, then I can too!” When she passed, receiving a B+;I felt as if I had passed too. That B+ meant so much: it was a tangible result of Azra’s hard work, but it was also symbol of our dedication to one another and the bond we forged working together.
My passion for teaching others and sharing knowledge emanates from my curiosity and love for learning. My shadowing experiences in particular have stimulated my curiosity and desire to learn more about the world around me. How does platelet rich plasma stimulate tissue growth? How does diabetes affect the proximal convoluted tubule? My questions never stopped. I wanted to know everything and it felt very satisfying to apply my knowledge to clinical problems.
Shadowing physicians further taught me that medicine not only fuels my curiosity; it also challenges my problem solving skills. I enjoy the connections found in medicine, how things learned in one area can aid in coming up with a solution in another. For instance, while shadowing Dr. Steel I was asked, “What causes varicose veins and what are the complications?” I thought to myself, what could it be? I knew that veins have valves and thought back to my shadowing experience with Dr. Smith in the operating room. She had amputated a patient’s foot due to ulcers obstructing the venous circulation. I replied, “veins have valves and valve problems could lead to ulcers.” Dr. Steel smiled, “you’re right, but it doesn’t end there!” Medicine is not disconnected; it is not about interventional cardiology or orthopedic surgery. In fact, medicine is intertwined and collaborative. The ability to gather knowledge from many specialties and put seemingly distinct concepts together to form a coherent picture truly attracts me to medicine.
It is hard to separate science from medicine; in fact, medicine is science. However, medicine is also about people—their feelings, struggles and concerns. Humans are not pre-programmed robots that all face the same problems. Humans deserve sensitive and understanding physicians. Humans deserve doctors who are infinitely curious, constantly questioning new advents in medicine. They deserve someone who loves the challenge of problem solving and coming up with innovative individualized solutions. I want to be that physician. I want to be able to approach each case as a unique entity and incorporate my strengths into providing personalized care for my patients. Until that time, I may be found Friday mornings in the operating room, peering over shoulders, dreaming about the day I get to hold the drill.
Let's take a step back to consider what this medical school personal statement example does, not just what it says. It begins with an engaging hook in the first paragraph and ends with a compelling conclusion. The introduction draws you in, making the essay almost impossible to put down, while the conclusion paints a picture of someone who is both passionate and dedicated to the profession. In between the introduction and conclusion, this student makes excellent use of personal narrative. The anecdotes chosen demonstrate this individual's response to the common question, " Why do you want to be a doctor ?" while simultaneously making them come across as compassionate, curious, and reflective. The essay articulates a number of key qualities and competencies, which go far beyond the common trope, I want to be a doctor because I want to help people.
This person is clearly a talented writer, but this was the result of several rounds of edits with one of our medical school admissions consulting team members and a lot of hard work on the student's part. If your essay is not quite there yet, or if you're just getting started, don't sweat it. Do take note that writing a good personal essay takes advanced planning and significant effort.
I was one of those kids who always wanted to be doctor. I didn’t understand the responsibilities and heartbreaks, the difficult decisions, and the years of study and training that go with the title, but I did understand that the person in the white coat stood for knowledge, professionalism, and compassion. As a child, visits to the pediatrician were important events. I’d attend to my hair and clothes, and travel to the appointment in anticipation. I loved the interaction with my doctor. I loved that whoever I was in the larger world, I could enter the safe space of the doctor’s office, and for a moment my concerns were heard and evaluated. I listened as my mother communicated with the doctor. I’d be asked questions, respectfully examined, treatments and options would be weighed, and we would be on our way. My mother had been supported in her efforts to raise a well child, and I’d had a meaningful interaction with an adult who cared for my body and development. I understood medicine as an act of service, which aligned with my values, and became a dream.
I was hospitalized for several months as a teenager and was inspired by the experience, despite the illness. In the time of diagnosis, treatment and recovery, I met truly sick children. Children who were much more ill than me. Children who wouldn’t recover. We shared a four-bed room, and we shared our medical stories. Because of the old hospital building, there was little privacy in our room, and we couldn’t help but listen-in during rounds, learning the medical details, becoming “experts” in our four distinct cases. I had more mobility than some of the patients, and when the medical team and family members were unavailable, I’d run simple errands for my roommates, liaise informally with staff, and attend to needs. To bring physical relief, a cold compress, a warmed blanket, a message to a nurse, filled me with such an intense joy and sense of purpose that I applied for a volunteer position at the hospital even before my release.
I have since been volunteering in emergency departments, out-patient clinics, and long term care facilities. While the depth of human suffering is at times shocking and the iterations of illness astounding, it is in the long-term care facility that I had the most meaningful experiences by virtue of my responsibilities and the nature of the patients’ illnesses. Charles was 55 when he died. He had early onset Parkinson’s Disease with dementia that revealed itself with a small tremor when he was in his late twenties. Charles had a wife and three daughters who visited regularly, but whom he didn’t often remember. Over four years as a volunteer, my role with the family was to fill in the spaces left by Charles’ periodic inability to project his voice as well as his growing cognitive lapses. I would tell the family of his activities between their visits, and I would remind him of their visits and their news. This was a hard experience for me. I watched as 3 daughters, around my own age, incrementally lost their father. I became angry, and then I grew even more determined.
In the summer of third year of my Health Sciences degree, I was chosen to participate in an undergraduate research fellowship in biomedical research at my university. As part of this experience, I worked alongside graduate students, postdoctoral fellows, medical students, physicians, and faculty in Alzheimer’s research into biomarkers that might predict future disease. We collaborated in teams, and by way of the principal investigator’s careful leadership, I learned wherever one falls in terms of rank, each contribution is vital to the outcome. None of the work is in isolation. For instance, I was closely mentored by Will, a graduate student who had been in my role the previous summer. He, in turn, collaborated with post docs and medical students, turning to faculty when roadblocks were met. While one person’s knowledge and skill may be deeper than another’s, individual efforts make up the whole. Working in this team, aside from developing research skills, I realized that practicing medicine is not an individual pursuit, but a collaborative commitment to excellence in scholarship and leadership, which all begins with mentorship.
Building on this experience with teamwork in the lab, I participated in a global health initiative in Nepal for four months, where I worked alongside nurses, doctors, and translators. I worked in mobile rural health camps that offered tuberculosis care, monitored the health and development of babies and children under 5, and tended to minor injuries. We worked 11-hour days helping hundreds of people in the 3 days we spent in each location. Patients would already be in line before we woke each morning. I spent each day recording basic demographic information, blood pressure, pulse, temperature, weight, height, as well as random blood sugar levels, for each patient, before they lined up to see a doctor. Each day was exhausting and satisfying. We helped so many people. But this satisfaction was quickly displaced by a developing understanding of issues in health equity.
My desire to be doctor as a young person was not misguided, but simply naïve. I’ve since learned the role of empathy and compassion through my experiences as a patient and volunteer. I’ve broadened my contextual understanding of medicine in the lab and in Nepal. My purpose hasn’t changed, but what has developed is my understanding that to be a physician is to help people live healthy, dignified lives by practicing both medicine and social justice.
28 More Medical School Personal Statement Examples That Got Accepted
What my sister went through pushed me to strengthen my knowledge in medical education, patient care, and research. These events have influenced who I am today and helped me determine my own passions. I aspire to be a doctor because I want to make miracles, like my sister, happen. Life is something to cherish; it would not be the same if I did not have one of my four sisters to spend it with. As all stories have endings, I hope that mine ends with me fulfilling my dream of being a doctor, which has been the sole focus of my life to this point. I would love nothing more than to dedicate myself to such a rewarding career, where I achieve what those doctors did for my family. Their expertise allowed my sister to get all the care she needed for her heart, eyes, lungs, and overall growth. Those physicians gave me more than just my little sister, they gave me the determination and focus needed to succeed in the medical field, and for that, I am forever grateful. ","label":"Medical School Personal Statement Example #3","title":"Medical School Personal Statement Example #3"}]" code="tab4" template="BlogArticle">
I came to America, leaving my parents and friends behind, to grasp my chance at a better future. I believe this chance is now in front of me. Medicine is the only path I truly desire because it satisfies my curiosity about the human body and it allows me to directly interact with patients. I do not want to miss this chance to further hone my skills and knowledge, in order to provide better care for my patients. ","label":"Medical School Personal Statement #4","title":"Medical School Personal Statement #4"}]" code="tab5" template="BlogArticle">
The time I have spent in various medical settings has confirmed my love for the field. Regardless of the environment, I am drawn to patients and their stories, like that scared young boy at AMC. I am aware that medicine is a constantly changing landscape; however, one thing that has remained steadfast over the years is putting the patient first, and I plan on doing this as a physician. All of my experiences have taught me a great deal about patient interaction and global health, however, I am left wanting more. I crave more knowledge to help patients and become more useful in the healthcare sector. I am certain medical school is the path that will help me reach my goal. One day, I hope to use my experiences to become an amazing doctor like the doctors that treated my sister, so I can help other children like her. ","label":"Medical School Personal Statement Example #5","title":"Medical School Personal Statement Example #5"}]" code="tab6" template="BlogArticle">
My interest in the field of medicine has developed overtime, with a common theme surrounding the importance of personal health and wellness. Through my journey in sports, travelling, and meeting some incredible individuals such as Michael, I have shifted my focus from thinking solely about the physical well-being, to understanding the importance of mental, spiritual, and social health as well. Being part of a profession that emphasizes continuous education, and application of knowledge to help people is very rewarding, and I will bring compassion, a hard work ethic and an attitude that is always focused on bettering patient outcomes. ","label":"Medical School Personal Statement Example # 7","title":"Medical School Personal Statement Example # 7"}]" code="tab8" template="BlogArticle">
Medicine embodies a hard science, but it is ultimately a profession that treats people. I have seen firsthand that medicine is not a \u201cone-treatment-fits-all\u201d practice, as an effective physician takes a holistic approach. This is the type of physician I aspire to be: one who refuses to shy away from the humanity of patients and their social context, and one who uses research and innovation to improve the human condition. So, when I rethink \u201cwhy medicine?\u201d, I know it\u2019s for me \u2013 because it is a holistic discipline, because it demands all of me, because I am ready to absorb the fascinating knowledge and science that dictates human life, and engage with humanity in a way no other profession allows for. Until the day that I dawn the coveted white coat, you can find me in inpatient units, comforting the many John\u2019s to come, or perhaps at the back of an operating room observing a mitral valve repair \u2013 dreaming of the day the puck is in my zone. ","label":"Medical School Personal Statement Example #8","title":"Medical School Personal Statement Example #8"}]" code="tab9" template="BlogArticle">
When I signed up to be a live DJ, I didn't know that the oral skills I practiced on-air would influence all aspects of my life, let alone lead me to consider a career in the art of healing. I see now, though, the importance of these key events in my life that have allowed me to develop excellent communication skills--whether that be empathic listening, reading and giving non-verbal cues, or verbal communication. I realize I have always been on a path towards medicine. Ultimately, I aim to continue to strengthen my skills as I establish my role as a medical student and leader: trusting my choices, effectively communicating, and taking action for people in need. ","label":"Medical School Personal Statement Example #9","title":"Medical School Personal Statement Example #9"}]" code="tab10" template="BlogArticle">
\u201cWhy didn\u2019t I pursue medicine sooner?\u201d Is the question that now occupies my mind. Leila made me aware of the unprofessional treatment delivered by some doctors. My subsequent activities confirmed my desire to become a doctor who cares deeply for his patients and provides the highest quality care. My passion for research fuels my scientific curiosity. I will continue to advocate for patient equality and fairness. Combining these qualities will allow me to succeed as a physician. ","label":"Medical School Personal Statement Example #10","title":"Medical School Personal Statement Example #10"}]" code="tab11" template="BlogArticle">
Medical school personal statement example: #11
Medical school personal statement example: #12, medical school personal statement example: #13, medical school personal statement example: #14, medical school personal statement example: #15, medical school personal statement example: #16, medical school personal statement example: #17, medical school personal statement example: #18, medical school personal statement example: #19, medical school personal statement example: #20, medical school personal statement example: #21, medical school personal statement example: #22, medical school personal statement example: #23, medical school personal statement example: #24, medical school personal statement example: #25, medical school personal statement example: #26, medical school personal statement example: #27, medical school personal statement example: #28, medical school personal statement example: #29, medical school personal statement example: #30.
Please note that all personal statements are the property of the students who wrote them, re-printed with permission. Names and identifying characteristics have been changed. Plagiarism detection software is used when evaluating personal statements. Plagiarism is grounds for disqualification from the application. ","label":"NOTE","title":"NOTE"}]" code="tab2" template="BlogArticle">
As one of the most important medical school requirements , the personal statement tells your story of why you decided to pursue the medical profession. Keep in mind that personal statements are one of the key factors that affect medical school acceptance rates . This is why it's important to write a stellar essay!
“Personal statements are often emphasized in your application to medical school as this singular crucial factor that distinguishes you from every other applicant. Demonstrating the uniqueness of my qualities is precisely how I found myself getting multiple interviews and offers into medical school.” – Dr. Vincent Adeyemi, MD
But this is easier said than done. In fact, medical school personal statements remain one of the most challenging parts of students' journeys to medical school. Here's our student Melissa sharing her experience of working on her personal statement:
"I struggled making my personal statement personal... I couldn't incorporate my feelings, motives and life stories that inspired me to pursue medicine into my personal statement" -Melissa, BeMo Student
Our student Rishi, who is now a student at the Carver College of Medicine , learned about the importance of the medical school personal statement the hard way:
"If you're a reapplicant like me, you know we all dread it but you have to get ready to answer what has changed about your application that we should accept you this time. I had an existing personal statement that did not get me in the first time so there was definitely work to be done." - Rishi, BeMo Student
The importance of the medical school personal statement can actually increase if you are applying to medical school with any red flags or setbacks, as our student Kannan did:
"I got 511 on my second MCAT try... My goal was anything over median of 510 so anything over that was honestly good with me because it's just about [creating] a good personal statement at that point... I read online about how important the personal statement [is]... making sure [it's] really polished and so that's when I decided to get some professional help." - Kannan, BeMo Student
As you can see from these testimonials, your medical school personal statement can really make a difference. So we are here to help you get started writing your own personal statement. Let's approach this step-by-step. Below you will see how we will outline the steps to creating your very best personal statement. And don't forget that if you need to see more examples, you can also check out our AMCAS personal statement examples, AACOMAS personal statement examples and TMDSAS personal statement examples to further inspire you!
Here's a quick run-down of what we'll cover in the article:
Now let's dive in deeper!
#1 Understanding the Qualities of a Strong Med School Personal Statement
Before discussing how to write a strong medical school personal statement, we first need to understand the qualities of a strong essay. Similar to crafting strong medical school secondary essays , writing a strong personal statement is a challenging, yet extremely important, part of your MD or MD-PhD programs applications. Your AMCAS Work and Activities section may show the reader what you have done, but the personal statement explains why. This is how Dr. Neel Mistry, MD and our admissions expert, prepared for his medical school personal statement writing:
"The personal statement is an opportunity for you to shine and really impress the committee to invite you for an interview. The personal statement is your chance to be reflective and go beyond what is stated on your CV and [activities]. In order to stand out, it is important to answer the main questions [of medical school personal statements] well: a bit about yourself and what led you to medicine, why you would make an ideal medical student and future physician, what attracts you to [medicine], and what sets you apart from the other candidates. The key here is answering the last two questions well. Most candidates simply highlight what they have done, but do not reflect on it or mention how what they have done has prepared them for a future medical career." - Dr. Neel Mistry, MD
“my essay also focused on volunteering in the local health clinic during the many summer breaks. volunteering was more than just another activity to tick off my bucket list for my medical school … i volunteered because i wanted to view medical practice through the lenses of already qualified doctors, not because i needed a reason to be a doctor. i understood that the admissions committee would be more interested in how i was motivated.” – dr. vincent adeyemi, md.
A personal statement should be deeply personal, giving the admissions committee insight into your passions and your ultimate decision to pursue a career in medicine. A compelling and introspective personal statement can make the difference between getting an interview and facing medical school rejection . Review our blogs to find out how to prepare for med school interviews and learn the most common medical school interview questions .
As you contemplate the task in front of you, you may be wondering what composing an essay has to do with entering the field of medicine. Many of our students were surprised to learn that medical school personal statements are so valued by med schools. The two things are more closely related than you think. A compelling personal statement demonstrates your written communication skills and highlights your accomplishments, passions, and aspirations. The ability to communicate a complex idea in a short space is an important skill as a physician. You should demonstrate your communication skills by writing a concise and meaningful statement that illustrates your best attributes. Leaving a lasting impression on your reader is what will lead to interview invitations.
A quick note: if you are applying to schools that do not require the formal medical school personal statement, such as medical schools in Canada , you should still learn how to write such essays. Many medical schools in Ontario , for example, ask for short essays for supplementary questionnaires. These are very similar to the personal statement. Knowing how to brainstorm, write, and format your answers is key to your success!!!
You want to give yourself as much time as possible to write your statement. Do not think you can do this in an evening or even in a week. Some statements take months. My best statement took almost a year to get right. Allow yourself time and start early to avoid added stress. Think of the ideas you want to include and brainstorm possible ways to highlight these ideas. Ask your friends for ideas or even brainstorm your ideas with people you trust. Get some feedback early to make sure you are headed in the right direction.
“I wrote scores of essays at my desk in those few weeks leading up to application submission. I needed it to be perfect. Do not let anyone tell you to settle. There was no moment when I had this shining light from the sky filtering into my room to motivate me. The ultimate trick is to keep writing. It is impossible to get that perfect essay on the first try, and you may not even get it on your fifteenth attempt, but the goal is to keep at it, keep making those edits, and never back down.” – Dr. Vincent Adeyemi, MD
All personal statements for medical school, often start by explaining why medicine is awesome; the admission committee already knows that. You should explain why you want a career in medicine. What is it about the practice of medicine that resonates with who you are? Naturally, this takes a lot of reflection around who you are. Here are some additional questions you can consider as you go about brainstorming for your essay:
- What motivates you to learn more about medicine?
- What is something you want them to know about you that isn't in your application?
- Where were you born, how did you grow up, and what type of childhood did you have growing up (perhaps including interesting stories about your siblings, parents, grandparents)?
- What kinds of early exposure to the medical field left an impression on you as a child?
- Did you become familiar with and interested in the field of medicine at an early stage of your life? If so, why?
- What are your key strengths, and how have you developed these?
- What steps did you take to familiarize yourself with the medical profession?
- Did you shadow a physician? Did you volunteer or work in a clinical setting? Did you get involved in medical research?
- What challenges have you faced? Have these made an impact on what you chose to study?
- What are your favorite activities?
- What kinds of extracurriculars for medical school or volunteer work have you done, and how have these shaped who you are, your priorities, and or your perspectives on a career in medicine?
- What was your "Aha!" moment?
- When did your desire to become a doctor solidify?
- How did you make the decision to apply to medical school?
You shouldn't try to answer all of these in your essay. Try only a few main points that will carry over into the final draft. Use these to brainstorm and gather ideas. Start developing your narrative by prioritizing the most impactful responses to these prompts and the ideas that are most relevant to your own experiences and goals. The perfect personal statement not only shows the admissions committee that you have refined communication skills, but also conveys maturity and professionalism. It should also display your motivation and suitability for medical practice. Here's how our student Alison, who was a non-traditional applicant with a serious red flag in her application, used her brainstorming sessions with our admissions experts to get a theme going in her medical school personal statement and her overall application package:
"I think it was during my brainstorming session that we really started talking about... what the theme [was] going to be for my application. And I think that was really helpful in and of itself. Just [reflecting] 'Hey, what's your focus going to be like? How are we going to write this? What's the style going to be?' Just to create an element of consistency throughout..." Alison, BeMo Student, current student at Dell Medical School
After brainstorming, you should be able to clearly see a few key ideas, skills, qualities, and intersections that you want to write about. Once you've isolated the elements you want to explore in your essay (usually 2-4 key ideas), you can begin building your outline. In terms of structure, this should follow the standard academic format, with an introduction, body paragraphs, and a conclusion.
As you begin thinking about what to include in your personal essay, remember that you are writing for a specific audience with specific expectations. Your evaluator will be familiar with the key qualities desired by medical schools, as informed by the standards of the profession. But keep in mind that they too are human, and they respond well to well-crafted, engaging essays that tell a story. Here's what our student Alison had to share about keeping your audience in mind when writing your personal statement:
"Make it easy for the reader to be able to work [their] way through [your personal statement]. Because, at the end of the day, I think one thing that helped me a lot was being able to think about who was going to be reading this application and it's going to be these people that are sitting around a desk or sitting at a table and [go] through massive numbers of applications every single day. And the easier and more digestible that you can make it for them, gives you a little bit of a win." - Alison, BeMo student, current student at Dell Medical School
The admissions committee will be examining your essay through the lens of their particular school's mission, values, and priorities. You should think about your experiences with reference to the AAMC Core Competencies and to each school's mission statement so that you're working toward your narrative with the institution and broader discipline in mind.
The AAMC Core Competencies are the key characteristics and skills sought by U.S. medical schools. These are separated into three general categories:
You are not expected to have mastered all of these competencies at this stage of your education. Display those that are relevant to your experiences will help demonstrate your commitment to the medical profession.
Review the school's mission statement: Educational institutions put a lot of time and care into drafting their school's vision. The mission statement will articulate the overall values and priorities of each university, giving you insight into what they might seek in candidates, and thus what you should try to display in your personal statement. Echoing the values of the university helps illustrate that you are a good fit for their intellectual culture. The mission statement may help you identify other priorities of the university, for example, whether they prioritize research-based or experiential-based education. All this research into your chosen medical schools will help you tremendously not only when you write you personal statement, but also the rest of your medical school application components, including your medical school letter of intent if you ever need to write one later.
Just like the personal statement is, in essence, a prompt without a prompt. They give you free rein to write your own prompt to tell your story. This is often difficult for students as they find it hard to get started without having a true direction. Below is a list of ideas to get your creative juices flowing. Use these prompts as a starting point for your essay. Also, they are a great way of addressing why you want to be a doctor without saying something generic.
- The moment your passion for medicine crystallized
- The events that led you toward this path
- Specific instances in which you experienced opportunities
- Challenges that helped shape your worldview
- Your compassion, resilience, or enthusiastic collaboration
- Demonstrate your commitment to others
- Your dependability
- Your leadership skills
- Your ability to problem-solve or to resolve a conflict
These are personal, impactful experiences that only you have had. Focus on the personal, and connect that to the values of your future profession. Do that and you will avoid writing the same essay as everyone else. Dr. Monica Taneja, MD and our admissions expert, shares her tip that got her accepted to the University of Maryland School of Medicine :
"I focused on my journey to medicine and opportunities that I sought out along the way. Everyone’s path and validation is unique, so walking the reader through your growth to the point of application will naturally be different, but that's what I wanted to share in my personal statement." - Dr. Monica Taneja, MD
“the essay is not about what you have been through; it's about who it made you into.” – dr. vincent adeyemi, md.
Admissions committees don't want your resumé in narrative form. The most boring essays are those of applicants listing their accomplishments. Remember, all that stuff is already in the activities section of the application. This is where you should discuss interesting or important life events that shaped you and your interest in medicine (a service trip to rural Guatemala, a death in the family, a personal experience as a patient). One suggestion is to have an overarching theme to your essay to tie everything together, starting with an anecdote. Alternatively, you can use one big metaphor or analogy through the essay. Dr. Jaime Cazes, MD and experienced admissions committee member of the University of Toronto Faculty of Medicine, encourages you to be creative when it comes to the theme of your personal statement:
"It is very easy to make the “cookie cutter” personal statement. To a reviewer who is reading tens of these at a time it can become quite boring. What I did was [tell] a story. Like any good novel, the stories' first lines are meant to hook the reader. This can be about anything if you can bring it back and relate it to your application. It could be about the time your friend was smashed up against the boards in hockey and you, with your limited first aid experience helped to treat him. It is important that the story be REAL." - Dr. Jaime Cazes, MD, University of Toronto Faculty of Medicine
Your personal statement must be well-organized, showing a clear, logical progression, as well as connections between ideas. It is generally best to use a chronological progression since this mirrors your progression into a mature adult and gives you the opportunity to illustrate how you learned from early mistakes later on. Carry the theme throughout the statement to achieve continuity and cohesion. Use the theme to links ideas from each paragraph to the next and to unite your piece.
Medical School Personal Statement Structure
When working toward the initial draft of your essay, it is important to keep the following in mind: The essay should read like a chronological narrative and have good structure and flow. Just like any academic essay, it will need an introduction, body content, and a conclusion. If you're wondering whether a medical school advisor can help you with your medical school application, check out our blog for the answer.
Check out our video to learn how to create a killer introduction to your medical school personal statement:
Introduction
The introductory paragraph and, even more importantly, the introductory sentence of your essay, will most certainly make or break your overall statement. Ensure that you have a creative and captivating opening sentence that draws the reader in. This is your first and only chance to make a first impression and really capture the attention of the committee. Starting with an event or an Aha! moment that inspired your decision to pursue a medical profession is one way to grab their attention. The kinds of things that inspire or motivate you can say a lot about who you are as a person.
The broader introductory paragraph itself should serve several functions. First, it must draw your reader in with an eye-catching first line and an engaging hook or anecdote. It should point toward the qualities that most effectively demonstrate your desire and suitability for becoming a physician (you will discuss these qualities further in the body paragraphs). The thesis of the introduction is that you have certain skills, experiences, and characteristics and that these skills, experiences, and characteristics will lead you to thrive in the field of medicine. Finally, it must also serve as a roadmap to the reader, allowing them to understand where the remainder of the story is headed.
That is a lot of work for a single paragraph to do. To better help you envision what this looks like in practice, here is a sample introduction that hits these main points.
I was convinced I was going to grow up to be a professional chef. This was not just another far-fetched idealistic childhood dream that many of us had growing up. There was a sense of certainty about this dream that motivated me to devote countless hours to its practice. It was mostly the wonder that it brought to others and the way they were left in awe after they tried a dish that I recall enjoying the most creating as a young chef. But, when I was 13, my grandfather was diagnosed with stage four lung cancer, and I realized that sometimes cooking is not enough, as I quickly learned about the vital role physicians play in the life of everyday people like my family and myself. Although my grandfather ended up passing away from his illness, the impact that the healthcare team had on him, my family, and I will always serve as the initial starting point of my fascination with the medical profession. Since that time, I have spent years learning more about the human sciences through my undergraduate studies and research, have developed a deeper understanding of the demands and challenges of the medical profession through my various volunteer and extra-curricular experiences, and although it has been difficult along the way, I have continued to forge a more intimate fascination with the medical field that has motivated me to apply to medical school at this juncture of my life. ","label":"Sample Introduction","title":"Sample Introduction"}]" code="tab3" template="BlogArticle">
In the body of your essay, you essentially want to elaborate on the ideas that you have introduced in your opening paragraph by drawing on your personal experiences to provide evidence. Major points from the above sample introduction could be: dedication and resilience (practicing cooking for hours, and devoting years to undergraduate studies in human sciences), passion and emotional connection (being able to create something that inspired awe in others, and personally connecting with the work of the grandfather's healthcare team), motivation and drive (being inspired by the role physicians play in their patients' lives, participating in volunteer work and extracurriculars, and an enduring fascination with the field of medicine). Depending on the details, a selection of volunteer and extra-curricular experiences might also be discussed in more detail, in order to emphasize other traits like collaboration, teamwork, perseverance, or a sense of social responsibility – all key characteristics sought by medical schools. Just like an academic essay, you will devote one paragraph to each major point, explaining this in detail, supporting your claims with experiences from your life, and reflecting on the meaning of each plot point in your personal narrative, with reference to why you want to pursue a medical career.
Your final statement should not be a simple summary of the things you have discussed. It should be insightful, captivating, and leave the reader with a lasting impression. Although you want to re-emphasize the major ideas of your essay, you should try to be creative and captivating, much like your opening paragraph. Sometimes if you can link your opening idea to your last paragraph it will really tie the whole essay together. The conclusion is just as important as the introduction. It is your last chance to express your medical aspirations. You want to impress the reader while also leaving them wanting more. In this case, more would mean getting an interview so they can learn more about who you are! Leave them thinking I have got to meet this person.
The narrative you construct should display some of your most tightly held values, principles, or ethical positions, along with key accomplishments and activities. If you see yourself as someone who is committed to community service, and you have a track record of such service, your story should feature this and provide insight into why you care about your community and what you learned from your experiences. Saying that you value community service when you've never volunteered a day in your life is pointless. Stating that your family is one where we support each other through challenge and loss (if this is indeed true), is excellent because it lays the groundwork for telling a story while showing that you are orientated towards close relationships. You would then go on to offer a brief anecdote that supports this. You are showing how you live such principles, rather than just telling your reader that you have such principles:
"Remember to use specific personal examples throughout your statement to make it more impactful and memorable for the readers. Often, painting a picture in the reader’s mind in the form of a story helps with this." - Dr. Neel Mistry, MD
A lot of students make the mistake of verbalizing their personal attributes with a bunch of adjectives, such as, "This experience taught me to be a self-reliant leader, with excellent communication skills, and empathy for others..." In reality, this does nothing to convey these qualities. It's a mistake to simply list your skills or characteristics without showing the reader an example of a time you used them to solve a problem. If you simply list your skills or characteristics (telling), without demonstrating the ways you have applied them (showing), you risk coming across as arrogant. The person reading the essay may not believe you, as you've not really given them a way to see such values in your actions. It is better to construct a narrative to show the reader that you possess the traits that medical schools are looking for, rather than explicitly stating that you are an empathetic individual or capable of deep self-reflection. Instead of listing adjectives, tell your personal story and allow the admissions committee to paint the picture for themselves. This step is very challenging for many students, but it's one of the most important strategies used in successful essays. Writing this way will absolutely make your statement stand out from the rest.
While it may be tempting to write in a high academic tone, using terminology or jargon that is often complex or discipline-specific, requiring a specialized vocabulary for comprehension. You should actually aim to write for a non-specialist audience. Remember, in the world of medicine, describing a complex, clinical condition to a patient requires using specific but clear words. This is why your personal statement should show that you can do the same thing. Using large words in unwieldy ways makes you sound like you are compensating for poor communication skills. Use words that you believe most people understand. Read your personal statement back to a 14-year-old, and then again to someone for whom English is not their first language, to see if you're on the right path.
Ultimately, fancy words do not make you a good communicator; listening and ensuring reader comprehension makes you a good communicator. Instead of using complex terminology to tell the admissions committee that you have strong communication skills, show them your communication skills through clear, accessible prose, written with non-specialists in mind. A common refrain among writing instructors is, never use a $10 word where a $2 word will suffice. If you can say it in plain, accessible language, then this is what you should do.
Display Professionalism
Professionalism may seem like a difficult quality to display when only composing a personal statement. After all, the reader can't see your mannerisms, your personal style, or any of those little qualities that allow someone to appear professional. Professionalism is about respect for the experience of others on your team or in your workplace. It is displayed when you are able to step back from your own individual position and think about what is best for your colleagues and peers, considering their needs alongside your own. If a story is relevant to why you want to be a physician and demonstrates an example of how you were professional in a workplace setting, then it is appropriate to include in your essay.
One easy way to destroy a sense of professionalism is to act in a judgmental way towards others, particularly if you perceived and ultimately resolved an error on someone else's part. Sometimes students blame another medical professional for something that went wrong with a patient.
They might say something to the effect of, "The nurse kept brushing off the patient's concerns, refusing to ask the attending to increase her pain medications. Luckily, being the empathetic individual that I am, I took the time to listen to sit with the patient, eventually bringing her concerns to the attending physician, who thanked me for letting him know."
There are a couple of things wrong with this example. It seems like this person is putting down someone else in an attempt to make themselves look better. They come across as un-empathetic and judgmental of the nurse. Maybe she was having a busy day, or maybe the attending had just seen the patient for this issue and the patient didn't really need re-assessment. Reading this kind of account in a personal statement makes the reader question the maturity of the applicant and their ability to move past blaming others and resolve problems in a meaningful way. Instead of allocating blame, identify what the problem was for the patient and then focus on what you did to resolve it and reflect on what you learned from the whole experience.
One last note on professionalism: Being professional does not mean being overly stoic, hiding your emotions, or cultivating a bland personality. A lot of students are afraid to talk about how a situation made them feel in their personal statement. They worry that discussing feelings is inappropriate and will appear unprofessional. Unfortunately for these students, emotional intelligence is hugely important to the practice of medicine. In order to be a good doctor, one must be aware of their own emotions as well as those of their patients. Good doctors are able to quickly identify their own emotions and understand how their emotional reactions may inform their actions, and the ability to deliver appropriate care, in a given situation. Someone who is incapable of identifying their emotions is also incapable of managing them effectively and will likely struggle to identify the emotions of others. So, when writing your personal statement, think about how each experience made you feel, and what you learned from those feelings and that experience.
How to Write About Discrepancies and Common Mistakes to Avoid
Part of your essay's body can include a discussion of any discrepancies or gaps in your education, or disruptions in your academic performance. If you had to take time off, or if you had a term or course with low grades, or if you had any other extenuating circumstances that impacted your education, you can take time to address these here. It is very important to address these strategically. Do not approach this section as space to plead your case. Offer a brief summary of the situation, and then emphasize what you learned from such hardships. Always focus on the positive, illustrating how such difficulties made you stronger, more resilient, or more compassionate. Connect your experiences to the qualities desired by medical schools. Here's how I student Alison address an academic discrepancy in her application:
I had an academic dishonesty during undergrad, which, at the time, ended up being this big misunderstanding. But I was going to appeal this and get it off my record. I was supposed to start nursing school two weeks after this whole ordeal had gone down and, at our university, if you try to appeal your academic dishonesty then you'd have to take an incomplete in that class and I needed this class in order to start nursing school. So I wasn't able to [appeal]. So when I talked with the people at the nursing school they were like ‘it's no big deal, it's fine’. [But] it came back and it haunted me very much. When I was applying [to medical school] I started looking online [to see] how big of a deal is it to have this ‘red flag’ on my application. I started reading all of these horror stories on Student Doctor Network and all of these other forums about how if you have an academic dishonesty you shouldn't even bother applying, that you'll never get in. Schools will blacklist you and I was [wondering] what am I going do. [My advisor suggested I use the essay to talk about my discrepancy].
First off, if anyone out there has an academic violation don't read student doctor network. don't listen to anybody. you absolutely are still a potential medical student and schools are not going to blacklist you just because of one mistake that you made. that's all lies. don't listen to them. i don't even think it came up a single time during any of my interviews. i think a lot of that came back to how i wrote that essay and the biggest advice that i can give that i got from the [bemo] team is explain what happened… just give the facts. be very objective about it. in the last two thirds [of the essay] you want to focus on what you learned from it and how it made you a better person and how it's going to make you a better physician.” – alison, bemo student, current student at dell medical school.
We hope many of you find a peace of mind when you read Alison's story. Because it shows that with the right approach to your medical school personal statement, you can overcome even red flags or setbacks that made you dread the application process. Use your personal statement to emphasize your ability to persevere through it all but do so in a positive way. Most of all, if you feel like you have to explain yourself, take accountability for the situation. State that it is unfortunate and then redirect it to what you learned and how it will make you a better doctor. Always focus on being positive and do not lament on the negative situation too much.
Additional Mistakes to Avoid in Personal Statements:
Check out this video on the top 5 errors to avoid in your personal statement!
Step 3: Writing Your First Draft
As you can see, there is a LOT of planning and consideration to be done before actually starting your first draft. Properly brainstorming, outlining, and considering the content and style of your essay prior to beginning the essay will make the writing process much smoother than it would be you to try to jump right to the draft-writing stage. Now, you're not just staring at a blank page wondering what you could possibly write to impress the admissions committee. Instead, you've researched what the school desires from its students and what the medical profession prioritizes in terms of personal characteristics, you've sketched out some key moments from your life that exemplify those traits, and you have a detailed outline that just needs filling in.
As you're getting started, focus on getting content on the page, filling in your outline and getting your ideas arranged on the page. Your essay will go through multiple drafts and re-writes, so the first step is to free write and start articulating connections between your experiences and the characteristics you're highlighting. You can worry about flow, transitions, and perfect grammar in later drafts. The first draft is always a working draft, written with the understanding that its purpose is to act as a starting point, not an ending point. Once you've completed a draft, you can begin the revising process. The next section will break down what to do once you have your first draft completed.
You can also begin looking at things like style, voice, transitions, and overall theme. The best way to do this is to read your essay aloud. This may sound strange, but it is one of the single most impactful bits of writing advice a student can receive. When we're reading in our heads (and particularly when we're reading our own words), it is easy to skip over parts that may be awkwardly worded, or where the grammar is off. As our brains process information differently, depending on whether we're taking in visual or auditory information, this can also help you understand where the connections between ideas aren't as evident as you would like. Reading the essay aloud will help you begin internalizing the narrative you've crafted, so that you can come to more easily express this both formally in writing and informally in conversation (for example, in an interview).
#1 Did You Distinguish Yourself From Others?
Does your narrative sound unique? Is it different than your peers or did you write in a generic manner? Our admissions expert Dr. Monica Taneja, MD, shares how she got the attention of the admissions committee with her personal statement:
"I also found it helpful to give schools a 'punch-line'. As in I wanted them to remember 1-2 things about me that are my differentiators and I reiterated those throughout [the personal statement]." - Dr. Monica Taneja, MD
Use your narrative to provide a compelling picture of who you are as a person, as a learner, as an advocate, and as a future medical professional. What can you offer? Remember, you will be getting a lot out of your med school experience, but the school will be getting a lot out of you, as well. You will be contributing your research efforts to your department, you will be participating in the academic community, and as you go on to become a successful medical professional you will impact the perception of your school's prestige. This is a mutually beneficial relationship, so use this opportunity to highlight what you bring to the table, and what you will contribute as a student at their institution. Let them know what it is about you that is an attribute to their program. Make them see you as a stand out from the crowd.
#2 Does My Essay Flow and is it Comprehensible?
Personal statements are a blessing and a curse for admission committees. They give them a better glimpse of who the applicant is than simple scores. Also, they are long and time-consuming to read. And often, they sound exactly alike. On occasion, a personal statement really makes an applicant shine. After reading page after page of redundant, cookie-cutter essays, an essay comes along with fluid prose and a compelling narrative, the reader snaps out of that feeling of monotony and gladly extends their enthusiastic attention.
Frankly, if the statement is pleasant to read, it will get read with more attention and appreciation. Flow is easier to craft through narrative, which is why you should root the statement in a story that demonstrates characteristics desirable to medical schools. Fluidity takes time to build, though, so your statement should be etched out through many drafts and should also be based on an outline. You need to brainstorm, then outline, then draft and re-draft, and then bring in editors and listeners for feedback (Note: You need someone to proofread your work. Bestselling authors have editors. Top scholars have editors. I need an editor. You need an editor. Everyone needs an editor). Then, check and double-check and fix anything that needs fixing. Then check again. Then submit. You want this to be a statement that captures the reader's interest by creating a fluid, comprehensible piece that leads the reader to not only read each paragraph but want to continue to the next sentence.
#3 Did You Check Your Grammar?
If you give yourself more than one night to write your statement, the chances of grammatical errors will decrease considerably. If you are pressed for time, upload your file into an online grammar website. Use the grammar checker on your word processor, but know that this, in itself, isn't enough. Use the eyes and ears of other people to check and double-check your grammar, punctuation, and syntax. Read your statement out loud to yourself and you will almost certainly find an error (and likely several errors). Use fresh eyes to review the statement several times before you actually submit it, by walking away from it for a day or so and then re-reading it. Start your essay early, so that you actually have time to do this. This step can make or break your essay. Do not waste all the effort you have put into writing, to only be discarded by the committee for using incorrect grammar and syntax.
#4 Did You Gather Feedback From Other People?
The most important tip in writing a strong application essay is this getting someone else to read your work. While the tips above are all very useful for writing a strong draft, nothing will benefit you more than getting an outside appraisal of your work. For example, it's very easy to overlook your own spelling or grammatical errors. You know your own story and you may think that your narrative and it's meaning make sense to your reader. You won't know that for sure without having someone else actually read it. This may sound obvious, but it's still an absolute necessity.
“It was very helpful for two of my mentors to review my statements before submitting my application. Ensure you trust the judgement and skills of the person to whom you would be giving your personal statement for review.” – Dr. Vincent Adeyemi, MD
Have someone you trust to read the essay and ask them what they thought of it. What was their impression of you after reading it? Did it make sense? Was it confusing? Do they have any questions? What was the tone of the essay? Do they see the connections you're trying to make? What were their takeaways from your essay, and do these align with your intended takeaways for your reader? Ideally, this person should have some knowledge of the application process or the medical profession, so that they can say whether you were successful in demonstrating that you are a suitable candidate for medical school. However, any external reader is better than no external reader at all.
Avoid having people too close to you read your work. They may refrain from being too critical in an effort to spare your feelings. This is the time to get brutal, honest feedback. If you know someone who is an editor but do not feel that they can be objective, try and find someone else.
Want more examples? Check out our video below:
FAQs and Final Notes
Your personal statement should tell your story and highlight specific experiences or aspects of your journey that have led you to medicine. If your first exposure or interest in the medical field was sparked from your own medical struggles, then you can certainly include this in your statement. What is most important is that you write about what factors or experiences attributed to you deciding that medicine is the right career path for you.
Sometimes students shy away from including their own personal struggles and describing how they felt during difficult times but this is a great way for admissions committees to gain perspective into who you are as a person and where your motivations lie. Remember, this is your story, not someone else's, so your statement should revolve around you. If you choose to discuss a personal hardship, what's most important is that you don't cast yourself as the victim and that you discuss what the experience taught you. Also, medical schools are not allowed to discriminate against students for discussing medical issues, so it is not looked at as a red flag unless you are talking about an issue inappropriately. For example, making yourself appear as the victim or not taking responsibility.
All US medical schools require the completion of a personal statement with your AMCAS, TMDSAS or AACOMAS applications.
Medical schools in Canada on the other hand, do not require or accept personal statements. In lieu of the personal statement, a few of these schools may require you to address a prompt in the form of an essay, or allow you to submit an explanation essay to describe any extenuating circumstances, but this is not the same as the US personal statement. For example, when applying through OMSAS , the University of Toronto medical school requires applicants to complete four short, 250 words or less, personal essays.
Many students struggle with whether or not they should address an unfavorable grade in their personal statement. What one student does isn't necessarily the right decision for you.
To help you decide, think about whether or not that bad grade might reflect on your poorly. If you think it will, then it's best to address the academic misstep head-on instead of having admissions committees dwell on possible areas of concern. If you're addressing a poor evaluation, ensure that you take responsibility for your grade, discuss what you learned and how your performance will be improved in the future - then move on. It's important that you don't play the victim and you must always reflect on what lessons you've learned moving forward.
Of course not, just because you didn't wake up one morning and notice a lightbulb flashing the words medicine, doesn't mean that your experiences and journey to medicine are inferior to those who did. Students arrive to medicine in all sorts of ways, some change career paths later in life, some always knew they wanted to pursue medicine, and others slowly became interested in medicine through their life interactions and experiences. Your personal statement should address your own unique story to how you first became interested in medicine and when and how that interest turned to a concrete desire.
While your entire statement is important, the opening sentence can often make or break your statement. This is because admission committee members are reviewing hundreds, if not thousands of personal statements. If your opening sentence is not eye-catching, interesting, and memorable, you risk your statement blending in with the large pile of other statements. Have a look at our video above for tips and strategies for creating a fantastic opening sentence.
Having your statement reviewed by family and friends can be a good place to start, but unfortunately, it's near-impossible for them to provide you with unbiased feedback. Often, friends and family members are going to support us and rave about our achievements. Even if they may truly think your statement needs work, they may feel uncomfortable giving you their honest feedback at the risk of hurting your feelings.
In addition, family and friends don't know exactly what admission committee members are looking for in a personal statement, nor do they have years of experience reviewing personal statements and helping students put the best version of themselves forward. For these reasons, many students choose to seek the help of a professional medical school advisor to make sure they have the absolute best chances of acceptance to medical school the first time around.
If you have enough time set aside to write your statement without juggling multiple other commitments, it normally takes at least four weeks to write your statement. If you are working, in school, or volunteering and have other commitments, be prepared to spend 6-8 weeks.
Your conclusion should have a summary of the main points you have made in your essay, but it should not just be a summary. You should also end with something that makes the reader want to learn more about you (i.e. call you for an interview). A good way to do this is to include a call-back to your opening anecdote: how have you grown or matured since then? How are you more prepared now to begin medical school?
The goal is to show as many of them as you can in the WHOLE application: this includes your personal statement, sketch, reference letters, secondary essays, and even your GPA and MCAT (which show critical thinking and reasoning already). So, it’s not an issue to focus on only a few select experiences and competencies in the personal statement.
Yes, you can. However, if you used an experience as a most meaningful entry, pick something else to talk about in your essay. Remember, you want to highlight as many core competencies across your whole application). Or, if you do pick the same experience: pick a different specific encounter or project with a different lesson learned.
Once your essay is in good shape, it's best to submit to ensure your application is reviewed as soon as possible. Remember, with rolling admissions, as more time passes before you submit your application, your chances of acceptance decreases. Nerves are normal and wanting to tinker is also normal, but over-analyzing and constant adjustments can actually weaken your essay.
So, if you're thinking about making more changes, it's important to really reflect and think about WHY you want to change something and if it will actually make the essay stronger. If not your changes won't actually make the essay stronger or if it's a very minor change you're thinking of making, then you should likely leave it as is.
The reality is, medical school admission is an extremely competitive process. In order to have the best chance of success, every part of your application must be stellar. Also, every year some students get in whose GPAs or MCAT scores are below the median. How? Simply because they must have stood out in other parts of the application, such as the personal statement.
The ones that honestly made the most impact on you. You'll need to reflect on your whole life and think about which experiences helped you grow and pushed you to pursue medicine. Ideally, experiences that show commitment and progression are better than one-off or short-term activities, as they usually contribute more to growth.
Final Notes
This Ultimate Guide has demonstrated all the work that needs to be done to compose a successful, engaging personal statement for your medical school application. While it would be wonderful if there was an easy way to write your personal statement in a day, the reality is that this kind of composition takes a lot of work. As daunting as this may seem, this guide lays out a clear path. In summary, the following 5 steps are the basis of what you should take away from this guide. These 5 steps are your guide and sort of cheat sheet to writing your best personal statement.
5 Main Takeaways For Personal Statement Writing:
- Brainstorming
- Content and Theme
- Multiple Drafts
- Revision With Attention to Grammar
While a strong personal statement alone will not guarantee admission to medical school, it could absolutely squeeze you onto a medical school waitlist , off the waitlist, and onto the offer list, or give someone on the admissions committee a reason to go to battle for your candidacy. Use this as an opportunity to highlight the incredible skills you've worked and studied to refine, the remarkable life experiences you've had, and the key qualities you possess in your own unique way. Show the admissions committee that you are someone they want to meet. Remember, in this context, wanting to meet you means wanting to bring you in for an interview!
Dr. Lauren Prufer is an admissions expert at BeMo. Dr. Prufer is also a medical resident at McMaster University. Her medical degree is from the Schulich School of Medicine and Dentistry. During her time in medical school, she developed a passion for sharing her knowledge with others through medical writing, research, and peer mentoring.
To your success,
Your friends at BeMo
BeMo Academic Consulting
Want more free tips? Subscribe to our channels for more free and useful content!
Apple Podcasts
Like our blog? Write for us ! >>
Have a question ask our admissions experts below and we'll answer your questions.
Jack Weaver
I have been reading posts regarding this topic and this post is one of the most interesting and informative one I have read. Thank you for this!
Hello Jack! Thank you very much for your comment. We glad you find this helpful!
Get Started Now
Talk to one of our admissions experts
Our site uses cookies. By using our website, you agree with our cookie policy .
FREE Training Webinar: How To Make Your Med School Application Stand Out
(and avoid the top 5 reasons that get 90% of applicants rejected).
Time Sensitive. Limited Spots Available:
We guarantee your acceptance to med school or you don't pay.
Swipe up to see a great offer!

IMAGES
VIDEO
COMMENTS
Formal MD Thesis Requirement. All students at Yale School of Medicine engage in research and are required to write an MD thesis during medical school. The only exceptions are students who have earned a PhD degree in the health sciences before matriculation and students enrolled in Yale's MD/PhD program. The YSM MD Thesis is under the ...
August - Students must attend the HST Research Assistantship (RA) and Thesis meeting and turn in an I-9 form to MIT. December - Identify lab, complete RA paperwork. Includes filling out RA form, and completing online paperwork (W4, M4, direct deposit). Beginning in January - Turn in RA form to Laurie Ward, MIT (this can be delayed, but RA ...
dissertation-style thesis ("MD thesis") reporting original, health-related research conducted under the supervision of YSM faculty member during medical school. Presentation of a thesis has been one of the requirements for the degree of Doctor of Medicine at Yale for over 180 years. Initially, case reports and
link in the application or see Section 8 of the AMCAS Applicant Guide for suggestions of things to think about when writing this essay. If you're applying to an MD-PhD program, you must complete two additional essays: the MD-PhD Essay and the Significant Research Experience Essay. To avoid formatting issues, we recommend that you type your ...
Harvard Medical School; HMS Theses and Dissertations; JavaScript is disabled for your browser. Some features of this site may not work without it. Search DASH. This Collection. Browse. ... Master of Medical Sciences in Biomedical Informatics (1) Master's Program in Clinical Investigation (1) Date Issued. 2015 (113) 2016 (77) 2023 (74) 2018 ...
Distinct work Your thesis should be distinct from any prior or concurrent graduate-level thesis. Work submitted to fulfill program requirements for another graduate degree (e.g., masters or doctorate) at Harvard or any other university is NOT eligible. ... Harvard Medical School Tosteson Medical Education Center, Suite 347 260 Longwood Avenue ...
Electronic Theses & Dissertations. Harvard Medical School & Harvard T.H. Chan School of Public Health students can now use ProQuest ETD to make their electronic theses and dissertations accessible to the research community: Submitted works will join almost 5 million others freely available through ProQuest Dissertations & Theses Global.
Chapter 20 Supervising Medical Research and Being Supervised; Chapter 21 Funding Medical Research; Chapter 22 The Purpose and Practice of Medical Research Meetings; Chapter 23 How to Present a Medical Research Paper; Chapter 24 How to Write a Medical Research Paper and Get It Accepted for Publication; Chapter 25 How to Write a Medical Thesis
Requirements prior to submission. Students must follow the graduate school's preparation guidelines for doctoral dissertations and master's theses to ensure that formatting is correct, no required pages are missing, and their thesis/dissertation is properly converted to PDF format. Please make your document is as accessible to users with ...
M.D.-Ph.D. applicants are usually expected to write more admissions essays than traditional medical school applicants. Pursuing an M.D.-Ph.D. degree, which combines the rigors of medical school ...
eScholarship@UMassChan. eScholarship@UMassChan is a digital repository for UMass Chan Medical School's research and scholarship, including journal articles, theses, datasets and more. We welcome submissions from our faculty, staff, and students. eScholarship@UMassChan is a service of the Lamar Soutter Library, Worcester, MA, USA.
The Crimson dissects ten successful medical school essays. sponsored by sponsored by sponsored by sponsored by sponsored by Morgan -- Accepted to: Harvard Medical School GPA: 4.0 MCAT: 522 ...
Given the importance of research within the medical profession, Case Western Reserve University School of Medicine requires a mentored research project and associated written MD Thesis to graduate. All areas of exploration on the biomedical research spectrum, detailed above, are open for these projects.
Thesis Advisors must: Hold a faculty appointment at a Harvard University school at the rank of Assistant Professor or above. Have a research program that uses computational methods in biomedical applications. Students may be co-advised by up to two advisors, with approval from the Program. The Thesis Advisor is expected to meet with students ...
Anatomic, histologic and histomorphometric analysis of the acetabular labrum and its enthesis . Alomiery, Abdulaziz Ahmad A. (The University of Edinburgh, 2024-06-03) The acetabular labrum is a fibrocartilaginous tissue attached to the acetabular rim of the hip joint. It plays a vital role in maintaining both static and dynamic hip joint ...
Secondary medical school essays should highlight why an applicant is a good fit. Applicants should submit the essays early without compromising quality. It's important to be authentic in essay ...
MD with Thesis Program . The M.D. with Thesis Program offers a unique opportunity to NJMS medical students to conduct original research of excellent quality during their Medical School training. The student is expected to devote one year exclusively to independent research that is Laboratory, Clinical or Population based.
This is precisely why we included the numerous sample medical school personal statement essays at the end of this guide. We also don't believe that reviewing your CV or thinking through your personal experiences to identify the "most unique" topic ideas is a valuable approach to brainstorming your personal statement. This "resume-first ...
Pursuing a dual degree path can help medical students grow their expertise and open up additional career paths. Dual degree programs have grown in popularity in recent years. According to the Association of American Medical Colleges, roughly 10% of medical school graduates pursued a dual degree in 2023. Master's degree tracks usually add ...
The theses are available at both the Medical Heritage Library, an online consortium of major medical libraries that digitizes materials and makes them freely available via Internet Archive, and from Yale's in-house repository, Eli Scholar. With the first evidence of a thesis requirement appearing in an 1839 catalog, the Yale School of ...
In medical school, and especially during clinical years, medical students (MS) are often exposed to physicians' inappropriate behaviors and various breaches of professionalism or safety [1,2,3].These can include lack of respect or sensitivity toward patients and other healthcare staff, deliberate lies and deceptions, breaching confidentiality, inadequate hand hygiene, or breach of a sterile ...
Each of the seven Native American students who are wrapping up their first year of medical school were presented with a Blanket of Knowledge. Created by Eighth Generation, a Seattle-based art and lifestyle brand owned by the Snoqualmie Tribe, each blanket was designed by a Native American artist. According to the designer of this blanket, the ...
As for grades, the average GPA among UCLA's accepted applicants is 3.8—up from 3.7 in 2019. Dubinett told me that the school sets a minimum threshold for MCAT scores and GPAs that is designed ...
Example 3 — Beyond the Diagnosis: The Importance of Individualized Care in Medicine. The applicant who wrote this personal statement was accepted into Touro College of Osteopathic Medicine and Nova Southeastern University College Of Osteopathic Medicine. Dr. Haywood sighs and shakes her head upon opening the chart.
Recent high school grads win scholarships for essays about teen mental health and policing. NORTH KANSAS CITY, Mo. (KCTV) - Two area high schoolers got a special honor on Wednesday from ...
Similar to crafting strong medical school secondary essays, writing a strong personal statement is a challenging, yet extremely important, part of your MD or MD-PhD programs applications. Your AMCAS Work and Activities section may show the reader what you have done, but the personal statement explains why. This is how Dr. Neel Mistry, MD and ...