An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Diabetes Res
- v.2022; 2022


Prevention and Management of Diabetes-Related Foot Ulcers through Informal Caregiver Involvement: A Systematic Review
Joseph ngmenesegre suglo.
1 Florence Nightingale Faculty of Nursing, Midwifery and Palliative Care, Kings College London, UK
2 Department of Nursing, Presbyterian University College Ghana, Ghana
Kirsty Winkley
Jackie sturt, associated data.
All data generated or analyzed during this study are included in this article and its supplementary information files.
The literature remains unclear whether involving informal caregivers in diabetes self-care could lead to improved diabetic foot outcomes for persons at risk and/or with foot ulcer. In this review, we synthesized evidence of the impact of interventions involving informal caregivers in the prevention and/or management of diabetes-related foot ulcers.
A systematic review based on PRISMA, and Synthesis Without Meta-analysis (SWiM) guidelines was conducted. MEDLINE (Ovid), Embase (Ovid), PsycINFO, CINAHL, and Cochrane Central Register of Controlled Trial of the Cochrane Library databases were searched from inception to February 2021. The following MESH terms were used: diabetic foot, foot ulcer, foot disease, diabetes mellitus, caregiver, family caregiver ,and family. Experimental studies involving persons with diabetes, with or at risk of foot ulcers and their caregivers were included. Data were extracted from included studies and narrative synthesis of findings undertaken.
Following the search of databases, 9275 articles were screened and 10 met the inclusion criteria. Studies were RCTs ( n = 5), non-RCTs ( n = 1), and prepoststudies ( n = 4). Informal caregivers through the intervention programmes were engaged in diverse roles that resulted in improved foot ulcer prevention and/or management outcomes such as improved foot care behaviors, increased diabetes knowledge, decreased HbA1c (mmol/mol or %), improved wound healing, and decreased limb amputations rates. Engaging both caregivers and the person with diabetes in education and hands-on skills training on wound care and foot checks were distinctive characteristics of interventions that consistently produced improved foot self-care behavior and clinically significant improvement in wound healing.
Informal caregivers play diverse and significant roles that seem to strengthen interventions and resulted in improved diabetes-related foot ulcer prevention and/or management outcomes. However, there are multiple intervention types and delivery strategies, and these may need to be considered by researchers and practitioners when planning programs for diabetes-related foot ulcers.
1. Introduction
Diabetes mellitus is among the top four noncommunicable diseases (NCD) targeted for action under the Sustainable Development Goals by the United Nations in 2015. Thus, all member countries are required to reduce premature death due to NCD by a third before 2030 [ 1 ]. Over 460 million people had diabetes in 2019, and this number has been estimated to rise to 578 million and 700 million by 2030 and 2045, respectively [ 2 ]. This high prevalence of diabetes and its complications puts pressure on global health expenditure. For instance, in 2017, the global health expenditure was estimated at over 7 billion USD with around 4 million diabetes related deaths [ 3 ].
One of the commonest and most debilitating complications of diabetes is diabetic foot ulcer (DFU) [ 4 ]. People with diabetes have a lifetime risk of up to 25% of developing DFU, and this greatly increases their chances of lower limb amputations [ 5 ]. This has made DFU the leading cause of nontraumatic amputations [ 5 ], and morbidity and mortality related to DFU are almost 50% over a five-year period [ 6 ].
The burden and debilitating effects of DFU reflect the need for strategic interventions to prevent and/or manage DFUs. Patient education, specialist care, clear referral pathways, use of multidisciplinary/professional teams, and other stringent interventions have significantly reduced foot ulcers and lower limb amputation (LLA) in developed countries over the past two decades [ 7 – 9 ]. For instance, to manage and/or prevent foot complications, the National Institute for Health and Care Excellence (NICE) recommends the use of health professional led multidisciplinary foot care service teams. The guideline stipulates that those persons with diabetes should be assessed for their risk of foot problems when diabetes is diagnosed and at least annually thereafter. Appropriate management and/or prevention services are then put in place based on the risk stratification of the patient [ 10 ]. Similarly, the International Working Group on the Diabetic Foot (IWGDF) in its evidence-based guidelines suggested that all preulcerative signs on the foot of persons with diabetes must be treated. The IWGDF further recommended that recurrent foot ulcers should be prevented through the provision of integrated foot care. This integrated foot care includes professional foot care, adequate footwear, and structured education about foot care [ 11 ].
Apparently, prevention of DFU requires persons with diabetes to engage in appropriate self-care behaviors relating to wearing off-loading footwear, exercise, diet, blood glucose monitoring, medication, and foot care [ 10 – 12 ]. Nevertheless, self-care behavior in the management of chronic conditions like diabetes is a complex phenomenon and impacted by multiple factors including but not limited to issues pertaining to problem solving skills, self-efficacy, and environment [ 13 – 15 ]. Thus, the social environment consisting of family members, friends, and significant others of persons with diabetes stands as one of the factors that can significantly influence individual's ability to manage diabetes-related foot ulcers (DFUs) at home [ 16 – 18 ]. Consequently, it has been suggested that diabetes self-management interventions should demonstrate active patient engagement and involvement of the caregivers of people with diabetes [ 18 – 20 ]. Involving informal caregivers (ICG) in caring for DFU is particularly important to achieving treatment goals especially in settings where family ties are strong [ 21 ], and it is also a cost-effective strategy [ 20 , 22 ]. ICG refers to persons providing unpaid services to the patient and may include parents, children, spouse, friends, other relatives, or nonkin. They are sometimes called ‘family caregivers,, or ‘caregivers' [ 23 ]. Though mostly not formally trained, they feel they have a moral and social obligation to care for the sick at home [ 20 ].
The presence of ICG at home can play the role of negotiating and monitoring how well patients are following self-management plans [ 20 ], detecting any improvement or deterioration in patients' health situation while providing care and calling for medical assistance when needed [ 24 ]. The social support offered by ICGs also creates a feeling of acceptance and high level life satisfaction among persons with diabetes-related foot problems [ 25 ]. However, it has been identified that majority of ICG fear making mistakes and found tasks such as wound dressing to be emotionally challenging and indicated that they needed training to be effective at home [ 26 ]. Despite some of the known evidence of the active role ICGs can play in DFU care, a systematic review indicated that from 1995 to 2013, only 1% of publications in the literature mentioned ICGs as members of the wound care team [ 27 ]. It was identified in another study that 11% of ICGs are actively involved in the management of DFU and that interventions should be planned to include patients and their ICGs [ 19 ]. To effectively engage ICGs in DFU interventions, there is the need to synthesize the evidence to ascertain the impact of ICGs on the prevention and/or management of DFUs. Therefore, this review is aimed at the following:
- Determine how informal caregivers' engagement in interventions can aid in the prevention and management of diabetes-related foot ulcers in adults
- Understand the types of interventions participated in by informal caregivers to prevent and/or manage diabetes-related foot ulcers
2. Materials and Methods
This review was guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [ 28 ] together with recommendations from the Synthesis Without Meta-analysis (SWiM) in systematic review guidelines [ 29 ]. The protocol was duly registered with the International Prospective Register of Systematic Reviews, PROSPERO, with registration number: CRD42021231768.
2.1. Eligibility Criteria
The review was based on predefined criteria for inclusion and exclusion of studies as indicated in Table 1 .
Eligibility criteria for studies.
2.2. Searching and Selection of Studies
The search for studies was conducted in five databases without recourse to publication date, country, or language. Using both subject headings and key words, a search strategy (see supplementary file 1 ) was constructed and optimized for each of the following databases from inception to February 2021: MEDLINE (Ovid), Embase (Ovid), PsycINFO, Cumulative Index of Nursing and Allied Health Literature (CINAHL), and Cochrane Central Register of Controlled Trial of the Cochrane Library. Additionally, the reference list of included studies and relevant systematic reviews were screened for studies that might have been missed by the searched strategy. All searched outcomes were imported into Covidence systematic review manager, and duplicates were automatically detected and removed. Titles and abstracts of the studies were then screened and studies not relevant to the aim of this review excluded. The full text of potentially eligible studies was read in full by two authors, and disagreements were discussed to reach consensus.
2.3. Quality Assessment and Data Extraction
The Cochrane Collaboration risk of bias for RCTs [ 30 ] and risk of bias in nonrandomized studies of interventions (ROBINS-I) [ 31 ] tools were used in assessing the studies. Certainty of the evidence was ranked using the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) guidelines for no single or no pooled estimate of effect [ 32 ]. Rating was done using the GRADEpro GDT software ( https://gdt.gradepro.org/app/#organizations ).
Data extraction used a modified template in covidence which was first piloted with one study. Also, the Template for Intervention Description and Replication (TIDieR) checklist [ 33 ] was used to guide the extraction of the necessary components of various interventions in studies. Key data extracted from studies included study reference, objective, setting, sample for intervention and control groups, participants characteristics, postintervention follow-up time, intervention description, and relevant outcomes.
2.4. Data Synthesis
A narrative synthesis of findings guided by the SWiM guidelines [ 29 ] was undertaken due to high heterogeneity in included studies in their intervention types, duration, data collection time points, and settings which made meta-analysis inappropriate. Therefore, data was synthesized based on direction of effect. Based on the objectives of this review, the first stage of synthesis was done to determine how ICG interventions aided outcomes pertaining to the prevention and management of DFU, and the second stage evaluated the various types of ICG interventions utilized to prevent or manage DFU. Studies were grouped based on the outcomes reported, and these outcomes were subsequently grouped into DFU prevention outcomes and DFU management outcomes. The prevention outcomes included HbA1c, diabetes knowledge, and foot self-care behavior/practices, while the DFU management outcomes measured among persons with current DFU included wound healing and limb amputation. To facilitate description of the ICG interventions, study intervention types were coded as educational, behavioral, psychological, and mixed (psychobehavioral/educational) [ 34 , 35 ]. Educational interventions were programs implemented by the health professional that focused on providing participants with information to enhance their knowledge of foot and diabetes self-management. Behavioral interventions focus on skills training, change in skills and lifestyle, aimed at improving self-management behaviors. Interventions were classed as psychological if their major aim were to address negative mood states, social support, and coping skills. Finally, interventions were described as mixed if they used two or more of the above categories of interventions.
3. Results of Review
3.1. search results.
The primary search of databases identified seven eligible papers and several relevant systematic reviews. The reference list of systematic reviews was checked, and further three eligible papers were identified from three systematic reviews [ 36 – 38 ]. This resulted in ten primary studies being included in this review. The searching and selection of studies and reasons for excluding studies after full-text retrieval are presented in Figure 1 , PRISMA flow diagram.

PRISMA flow diagram for study identification and selection process.
3.2. Characteristics of Included Studies
The review included 10 studies. Three of the studies came from the USA [ 39 – 41 ], two from China [ 42 , 43 ], two from Indonesia [ 44 , 45 ] and one each from Iran [ 46 ], Ireland [ 47 ], and India [ 48 ]. The total number of participants with diabetes was 5532. Only five studies [ 39 , 41 , 43 – 45 ] reported the characteristics and number of caregivers involved which was 359. Majority of caregivers were female (73.6%), and family relationship was mostly spouse or partner (53.6%), son/daughter (28.3%), or other family members (14.7%). Parents and siblings were the least likely to be involved as caregivers, 1.5% and 1.9%, respectively. Table 2 presents the characteristics of studies.
Characteristics of studies.
I: intervention group; C: controlled group; SD: standard deviation; RCT: randomized controlled trial; non-RCT: nonrandomized controlled trial; LLA: lower limb amputation; PEDIS: Perfusion, Extent, Depth, Infection and Sensation; MS: mean square between subjects; %: percentage; HbA1c: glycated hemoglobin; vs.: versus; DSME: diabetes self-management education; ADA: American Diabetes Association.
3.3. Risk of Bias and GRADE Assessment
The risk of bias assessment of studies indicating authors judgement with supporting reasons are presented as supplementary files 2 and 3 for RCTs and non-randomized studies, respectively. All the RCTs had high risk of bias for nonblinding of participants and personnel since it was not possible to blind these people. Apart from one study [ 47 ], it was unclear if outcome assessors were blinded or not. Non-RCT studies were all rated moderate for bias due to confounding, and they all also had an overall moderate risk of bias. GRADE assessment for each outcome followed the criteria for evidence ranking in the absence of single estimate of effect [ 32 ]. Most outcomes were graded as moderate (see Table 3 ) due to serious risk of bias, serious inconsistency, but not serious indirectness and imprecision.
Diabetes-related foot ulcer prevention outcomes.
Key: DFSCBS: Diabetes Foot Self-care Behaviour Scale; SDSCA: Summary of Diabetes Self-care Activities scale; DFUAS: Diabetes Foot Ulcer Assessment Scale; PEDIS: Perfusion, Extent, Depth, Infection and Sensation; SKILLD: Spoken Knowledge in Low Literacy patients with Diabetes; DKQ: Diabetes Knowledge Questionnaire; DFCS: Diabetes Foot Care Scale.
3.4. Outcomes and Measures
The first objective of this review was to determine how ICG interventions aided the prevention and management of DFUs. The outcomes reported by studies consisted of DFU prevention and DFU management outcomes as presented in Tables Tables3 3 and and4, 4 , respectively. Prevention outcomes reported by almost all studies included foot self-care behaviors/practices of participants, diabetes knowledge, and HbA1c [ 39 – 44 , 46 – 48 ]. Wound healing and limb amputations/surgical interventions were the DFU management outcomes indicated by four studies [ 42 , 44 , 45 , 48 ].
Diabetes-related foot ulcer management outcomes.
Key: DFSCBS: Diabetes Foot Sel-care Behaviour Scale; SDSCA: Summary of Diabetes Self-care Activities scale; DFUAS: Diabetes Foot Ulcer Assessment Scale; PEDIS: Perfusion, Extent, Depth, Infection and Sensation; SKILLD: Spoken Knowledge in Low Literacy patients with Diabetes; DKQ: Diabetes Knowledge Questionnaire; DFCS: Diabetes Foot Care Scale.
Seven studies assessed the foot self-care behavior and practices of participants, and six of them indicated improvement in foot care behavior of participants at follow-up [ 39 – 43 , 46 ]. Five studies further indicated that the change in foot care practice was significant in the ICG intervention groups [ 40 – 43 , 46 ]. The foot care activities engaged in by ICGs included assisting persons with diabetes in nail trimming, daily foot inspection, footwear inspection, checking of water temperature before patients washed their feet, checking of protective foot sensitivity using monofilaments, and collaborative problem solving. The assessment of participants' foot care behavior differed across studies. In majority of the outcome measure instruments, foot care questions were few, and only a part of a generic tool used in assessing participants' diabetes self-management activities [ 39 – 41 , 46 , 47 ]. However, two studies used diabetes foot self-care behavior scale (DFSCBS) and diabetes foot care scale (DFCS) that were specifically designed for assessing foot care practices [ 42 , 43 ]. Both the generic diabetes self-management tools (summary of diabetes self-care activities scale (SDSCA)) and specifically devised foot care measure (DFCS) both recorded improved foot care practices among participants.
Study participants' knowledge on diabetes was assessed by three studies, and all of them reported significant improvement at postintervention follow-ups [ 40 ]–[ 42 ]. A supportive family member or friend was included in these interventions to encourage shared learning and to enhance the abilities of the ICG to know how to be helpful to the person with diabetes. Diabetes knowledge was assessed using either the Spoken Knowledge in Low Literacy patients with Diabetes (SKILLD) [ 40 , 41 ] or Diabetes Knowledge Questionnaire (DKQ) [ 42 ]. Both outcome measure instruments suggested that interventions were effective in improving diabetes knowledge among participants [ 40 – 42 ].
Finally, under DFU prevention outcome, all ten included studies except one [ 43 ] investigated participants HbA1c at various time points' postintervention. Even though all nine studies reported reduction in HbA1c, almost equal number of studies, four and five reported insignificant and significant improvement, respectively, at postintervention follow-up. Measuring HbA1c at 3, 6, 12, or 18 months postintervention could still result in either significant or insignificant improvement in HbA1c results. The ICGs and persons with diabetes in the intervention groups were offered education on physical activity (exercise), blood glucose monitoring, healthy eating habits, and medication regimens. ICGs acted as support persons and helped in dietary planning and setting of diabetes management goals.
DFU management outcomes were assessed among participants who already had DFU problems. Healing of diabetic wounds was objectively assessed in three studies [ 44 , 45 , 48 ], and all of them reported clinically significant improvement in wound size. Limb amputations/surgical interventions prevalence was also recorded by two studies [ 42 , 48 ]. These studies observed that even though the difference was not significant, amputations were lower in the study intervention group compared to study control group [ 42 ]. To actively support the management of DFU, ICGs in the intervention programs together with the person with DFU were trained on wound care. Family caregivers were taught their roles and effective involvement in DFU care, problem solving skills, and diet planning [ 42 , 44 , 45 , 48 ].
3.5. Intervention Types
Various intervention types as operationally defined earlier were implemented to prevent and/or manage DFU. They included six psychobehavioral/educational type intervention [ 39 – 41 , 44 – 46 ], two behavioral [ 42 , 48 ] and one each of psychological [ 47 ] and educational interventions [ 43 ]. These interventions were delivered over several sessions with a mean of 15 (range 3 to 24) over a mean duration of 20 weeks (range 3 to 104) (see supplementary file 4 for coded intervention types and delivery methods).
The study intervention types implemented produced similar results on the outcomes measured. Apart from psychological intervention [ 47 ], all other intervention types reported improved diabetes knowledge and foot care behavior. These interventions were delivered through a mixture of didactic and interactive teaching methods, through face-to-face or phone calls. A mixed format of intervention delivery which involves a combined use of face-to-face, phone calls, videotapes and information booklets was utilized in behavioral or mixed psychobehavioral/educational interventions and resulted in significant improvement in foot self-care practices among participants [ 40 – 42 , 45 , 46 ]. ICGs and persons with diabetes were taught together in all interventions to promote shared learning and agreed self-care goals.
Behavioral interventions in China and India resulted in both improved foot care practices and lower prevalence of amputations [ 42 , 48 ]. In these behavioral interventions, participants with diabetes and their caregivers were provided with skills training on various foot care activities and study participants tasked to report to clinic with any sign of foot disease for treatment. This intervention type even at long-term follow-up still recorded significant results at 12 months and 18 months, respectively, for Liang et al. [ 42 ] and Viswanathan et al. [ 48 ].
Also, behavioral [ 48 ] and mixed behavioral/educational interventions [ 44 , 45 ] produced clinically significant reduction in diabetic wound size and healing time. Persons with diabetes and their ICGs in these interventions were engaged in participatory diabetes education, hands-on workshop on wound care, problem solving skills, and establishment of family roles in DFU care. Thus, an interactive and mixed method of teaching was utilized to achieve wound healing results. In these participatory teaching methods, diabetes self-management activities were discussed, and concerns of both the person with diabetes and their ICG were addressed before setting diabetes management goals [ 39 – 41 , 46 ].
4. Discussion
4.1. main findings.
This review is the first systematic review focusing solely on DFU and ICGs. It identified that trials of ICG interventions resulted in improved DFU prevention and management outcomes, possibly through the diverse roles played by ICGs. Thus, designing of interventions to engage family caregivers strengthened the programs, and this is evidenced in the improved foot self-care practices, improved diabetes knowledge, and better DFU management outcomes in the ICG intervention groups. Caregivers actively participated in the prevention of DFU through their diverse activities ranging from working collaboratively with the person with diabetes in feet inspection, checking of feet sensation, diet/meal planning, and setting of diabetes self-management goals. The management of DFUs was facilitated by ICGs through their engagement in wound care and participatory problem-solving activities. ICG participation in interventions characterized by hands-on skills training on wound and/or foot care, combined used of interactive, face-to-face and phone calls intervention delivery resulted in improved foot self-care behaviors and wound healing.
4.2. Findings Compared to Wider Evidence
The impacts of ICG interventions identified in this review are not dissimilar to other previous systematic reviews indicating that involvement of family caregivers in interventions improved clinical outcomes for persons with cancer, stroke, and other debilitating chronic conditions [ 21 , 49 – 52 ]. For instance, an evidence synthesis involving stroke survivors indicated that family-oriented interventions were effective in reducing poststroke depression and improving the quality of life of both patients and caregivers [ 53 ]. Similar significant improved health outcomes were detected among persons with cancer and their family caregivers [ 51 , 54 ]. Generally, the involvement of ICGs in the management of community-based adult is widely recommended as superior to patient-only interventions [ 55 – 57 ]. This probably is based on the assertion that family health and function influence the health status and functioning of individual family members, and a joint family and patient intervention could produce better health outcome for both. In the context of diabetes, our review findings resonates with previous systematic reviews suggesting that involvement of caregivers and social support significantly improves self-management behaviors and health outcomes of persons with diabetes [ 36 , 58 ]. Our review reiterates the significance of ICG and the patient's social environment in the diabetes self-management continuum, and this could be applied in the prevention and management of diabetes-related foot ulcer. A review of reviews suggested that ICGs were often included in interventions and acted as a surrogate for the health care provider and the health care system. Family members were used as substitutes for professionals to deliver needed care, monitor, or encourage the patient to achieve desired health outcomes. These interventions were planned to strengthen family's ability to work together with the person with the chronic condition in solving challenging situations [ 21 ]. This consolidates our findings suggesting that ICGs were involved in setting diabetes management goals, diet planning, and other activities that strengthened the interventions and resulted in improved clinical outcomes. The skills and competence of these ICGs in our review were probably enhanced through the workshops and interactive sessions of the interventions. The need to train and engage ICGs in wound care process was further suggested in a national survey conducted in the United States. The survey reported that over a third of caregivers were providing wound care at home but indicated they were afraid of making mistakes and needed some skill training [ 59 ]. Therefore, the design of foot care programs could make family caregivers more confident in their support roles by incorporating easy-to-follow training for them. Nevertheless, even though none of the included studies critiqued or assessed how interventions affected ICG themselves, it is important that such programs prevent patient-caregiver conflicts by maintaining patient autonomy and reducing diabetes distress [ 20 ]. This might be necessary in maximizing the impact and sustainability of such ICG interventions.
This narrative synthesis further described the various types of interventions participated in by ICGs. Both persons with diabetes and their ICGs participated in interventions that were focused on providing problem-solving skills, foot care skills, and general diabetes information using diverse intervention delivery strategies. This seems to be consistent with previous study findings that education combined with specific behavioral change strategies produced improved health outcomes for persons with chronic conditions [ 35 , 60 , 61 ]. Our findings suggest that interventions that taught both patient and carer how to examine feet and provide foot-related care and wound care improved outcomes. Nevertheless, this does not corroborate with previous systematic reviews and meta-analysis suggesting that foot care education alone has no significant effect and that there is no advantage of combining different educational approaches in preventing/reducing DFU [ 62 ]. Another Cochrane review indicated that even though foot care knowledge and self-reported patient behavior seem to be positively influenced by education in the short term, there is insufficient robust evidence that patient education alone is effective in achieving clinically relevant reductions in ulcer and amputation incidence [ 9 ]. The differences in findings and the results of these systematic reviews [ 9 , 62 ] must be viewed with caution as they reviewed educational intervention studies that focused primarily on the patient alone. However, this also suggest the need for future reviews to examine whether educational interventions engaging both patient and their ICG resulted in better DFU clinical outcomes compared with interventions targeting patients alone. This will reaffirm how and whether it is more beneficial to engage both persons with diabetes and their ICG when planning DFU programs.
4.3. Strengths and Limitations
This review is the first of its kind focusing solely on ICGs and DFU. It uses transparent and rigorous methods, following the PRISMA and SWiM guidelines, and this allows for reproducibility of this study. A limitation of this review is that, despite a comprehensive search strategy, eligible studies were identified from only six countries across the globe. This makes it unclear to what extend findings may be applicable to other dissimilar contexts. This indicates the dearth of literature in the field, and given the potential devastating impact of DFUs, more research is needed in other contexts and the findings integrated into appropriate health system response. Most outcomes on the GRADE evidence rating were ranked moderate due to risk of bias especially with baseline confounders in the quasiexperimental studies. Hence, subsequent studies should adapt a well-designed RCT approach to be able establish the exact impact of ICG interventions.
4.4. Recommendations for Practice, Research, and Policy
Based on the evidence of the roles ICGs play in diabetes-related foot ulcer prevention, health care practitioners ought to recognize carers as active members in DFU prevention and/or management strategies. This implies involving them in planning and determining diabetes management goals, establishing their specific roles and how they can be effectively involved in foot disease prevention and management. As part of diabetes self-management education and support (DSME/S), practitioners should take pragmatic efforts to enhance the knowledge, skills, and confidence of ICGs by organizing easy to do skills training and education for both carers and patients. Also, ICG involvement holds advantages in high and low resource settings and policymakers could optimize their health expenditure by supporting the involvement of this unpaid caring work by upskilling ICGs. There is evidence that involving both ICGs and patients in the management of chronic conditions is cost-effective and interventions produces long-lasting effects [ 20 , 22 ]. Foot specialist services and other foot care resources are mostly either not available or not affordable to persons especially in developing countries. Involving ICGs could be an innovative health care intervention to prevent foot disease. It is therefore imperative that these interventions need evaluating in lower resource settings where the involvement of knowledgeable, skilled and confident ICGs could reap significant benefits to their family and community in the absence of access to high quality healthcare for people with and/or at risk of diabetic foot disease.
Data Availability
This study is part of the first author's PhD thesis at King's College London funded by the Centre for Doctoral Studies under the Africa International Postgraduate Research Scholarship.
Conflicts of Interest
The authors declare that they have no competing interests.
Supplementary Materials
Supplementary 1.
Supplementary file 1: search strategy.
Supplementary 2
Supplementary file 2: risk of bias for RCTs.
Supplementary 3
Supplementary file 3: Risk of bias for non-RCTs.
Supplementary 4
Supplementary file 4: description of interventions.
Supplementary 5
Supplementary file 5: coded intervention elements.
Supplementary 6
PRISMA checklist.
- Open access
- Published: 06 August 2022
A qualitative study of barriers to care-seeking for diabetic foot ulceration across multiple levels of the healthcare system
- Tze-Woei Tan ORCID: orcid.org/0000-0002-6658-9482 1 , 2 ,
- Rebecca M. Crocker 3 ,
- Kelly N. B. Palmer 3 ,
- Chris Gomez 4 ,
- David G. Armstrong 1 , 2 &
- David G. Marrero 3
Journal of Foot and Ankle Research volume 15 , Article number: 56 ( 2022 ) Cite this article
6224 Accesses
12 Citations
5 Altmetric
Metrics details
Introduction
The mechanisms for the observed disparities in diabetes-related amputation are poorly understood and could be related to access for diabetic foot ulceration (DFU) care. This qualitative study aimed to understand patients’ personal experiences navigating the healthcare system and the barriers they faced.
Fifteen semi-structured interviews were conducted over the phone between June 2020 to February 2021. Participants with DFUs were recruited from a tertiary referral center in Southern Arizona. The interviews were audio-recorded and analyzed according to the NIMHD Research Framework, focusing on the health care system domain.
Among the 15 participants included in the study, the mean age was 52.4 years (66.7% male), 66.7% was from minority racial groups, and 73.3% was Medicaid or Indian Health Service beneficiaries. Participants frequently reported barriers at various levels of the healthcare system.
On the individual level, themes that arose included health literacy and inadequate insurance coverage resulting in financial strain. On the interpersonal level, participants complained of fragmented relationships with providers and experienced challenges in making follow-up appointments. On the community level, participants reported struggles with medical equipment.
On the societal level, participants also noted insufficient preventative foot care and education before DFU onset, and many respondents experienced initial misdiagnoses and delays in receiving care.
Conclusions
Patients with DFUs face significant barriers in accessing medical care at many levels in the healthcare system and beyond. These data highlight opportunities to address the effects of diabetic foot complications and the inequitable burden of inadequately managed diabetic foot care.
Peer Review reports
Diabetic foot ulceration (DFU) is a common and often catastrophic complication for people with diabetes. In the United States, people with diabetes have an up to 34% lifetime risk of developing a foot ulcer [ 1 , 2 ], a medical complication that increases their five-year mortality rate by 2.5 times [ 3 , 4 ]. Moreover, foot ulceration is a causal factor for up to 85% of diabetic patients who subsequently undergo lower extremity amputation [ 1 , 5 ]. As compared to the overall United States population, people with diabetes are more likely to undergo lower extremity amputation and repeat amputations [ 1 , 6 ]. The annual medical cost associated with DFU care in the United States is an additional $9–13 billion on top of other costs associated with diabetes [ 7 ].
Moreover, DFUs and subsequent amputations are unevenly patterned along lines of racial and ethnic minority status, low socio-economic status, low insurance coverage rates, and geographic isolation. African American, Hispanic, and Native American adults with diabetes have higher prevalence of DFUs and amputation than their White counterparts [ 8 , 9 , 10 ]. Across the board, patients in the lowest income quartiles experience higher odds of amputation and death due to peripheral artery disease [ 11 , 12 ]. In addition, those with suboptimal or no medical insurance are at an elevated risk of major amputation [ 13 ]. This illuminates a glaring and yet unabated public health problem, especially among minority and low-income populations [ 8 , 9 , 12 , 13 , 14 , 15 , 16 ].
The mechanisms of these observed disparities in DFU incidence and progression are poorly understood [ 9 , 11 , 17 , 18 ]. There is evidence, however, indicating that access to affordable and quality medical care, preventive services, and limb salvage care is an important contributing factor to disparities in amputation rates [ 19 , 20 , 21 ]. This qualitative study aimed to understand patients’ personal experiences with DFUs in a safety net health system, including their processes of navigating the healthcare system and the barriers they faced. The themes elicited in the study concerning multiple barriers at varying levels of the healthcare system will help to improve health care delivery in a population experiencing elevated risks of diabetes-related ulceration and amputation.
This qualitative study was designed to better understand the various challenges faced by patients with a history of DFUs and lower extremity amputations as they managed their conditions and sought medical care. Semi-structured interviews were conducted between June 2020 to February 2021 and the results were analyzed according to the “Health Care System” domain of the National Institute on Minority Health and Health Disparities Research Framework [ 22 ]. The University of Arizona Institutional Review Board approved the study in July 2019 (Protocol Number 1906749805).
Participants
Patients were selected from the Southwestern Academic Limb Salvage Alliance (SALSA), a multidisciplinary limb salvage care team located in Tucson, Arizona, to participate in semi-structured interviews. SALSA treats over 5,000 patient visits annually for diabetic foot problems, of which 40% are from racial and ethnic minority groups. It is the primary referral center for limb salvage and care for minorities and patients with low socioeconomic status in suburban and rural Arizona. Participants were identified and approached for participation during scheduled clinic appointments or by follow-up phone calls by our research team. We purposely sampled participants, using criterion sampling, to reflect the diverse range of race/ethnicity, gender, history of DFU, foot infection, minor amputation (below the ankle), and major amputation (ankle or above) treated by SALSA [ 23 ].
Interview guide and data collection
The research team jointly developed a semi-structured interview guide to encourage patient perspectives regarding their living experiences with foot ulceration and how they sought care for DFUs. Interviews were conducted in the patients’ preferred language (English or Spanish). Three research team members experienced in qualitative interviews (R.M.C., K.N.B.P., and D.G.M.) completed 15 interviews over the phone, lasting 40–60 min each. Interviews were recorded with consent using the “Tape A Call” mobile application ( www.tapeacall.com ) or via the University of Arizona Health Sciences Zoom Platform. The interviews were conducted in phases to allow for simultaneous analysis and redirection of subsequent data collection.
The research team used the Dedoose software version 9.0.17 (SocioCultural Research Consultants, LLC, Los Angeles, CA) to assist in data storage, coding, and data analysis. Audio files of the interviews were transcribed into the language spoken. After a quality assurance check, the transcriptions were uploaded into the software. The transcripts were independently reviewed and coded by three members of the research team (R.M.C., K.N.B.P., and T-W.T.). Data for this article were analyzed according to the NIMHD Research Framework (2017) that includes a multilevel approach including individual, interpersonal, community, and societal-level factors. While this model includes several domains, for the purposes of this paper we are focusing only on the Health Care System domain. This framework has been used in health disparities research to conceptualize and evaluate a wide array of determinants that promote or worsen health disparities [ 24 ]. Team members met regularly to compare coding results and resolve discrepancies by discussion and consensus.
The study sample included 15 participants (Table 1 ). The mean age was 54.2 years. Eleven participants (73.3%) were Medicaid or Indian Health Program beneficiaries and 80% of participants were either unemployed or had retired. All participants had history of at least one DFU, 12 had a history of foot infection, eight underwent minor amputations, and one had a major amputation. Four patients underwent at least one open surgery or endovascular procedure due to peripheral artery disease. During the interviews, participants frequently reported barriers at various levels of the health care system (Table 2 , Fig. 1 ).

Patient reported barriers at all levels influence of the health care system domain
Individual Level of Influence
Health literacy.
While most participants were aware of the risks of foot infection and amputation, there were significant gaps in their health literacy that compromised their ability to make informed decisions about when and how to seek medical care. Most notably, although all participants had a history of DFUs, many were unfamiliar with the term “ulcer” and expressed confusion when interviewers asked questions using that term. This finding, which reflects poor communication by providers and medical staff, resulted in most participants using alternate terms such as “blister,” “callous,” “cut,” “infection,” and “injury” to describe their foot abnormalities. This confusion in terminology was critical, as many patients described not initially seeking medical care because they interpreted their foot abnormality to be a common, everyday problem rather than one warranting medical attention. As one participant described: “Nobody ever really said what I’m looking for just anything that is not normal, I guess. But like I said, I have never heard of a diabetic foot ulcer.” (57-year-old Hispanic male, history of DFU).
In addition, participants described gaps in their health literacy related to the specifics of foot ulcer progression and the appropriate management strategies to prevent amputation. Most participants did not have a solid understanding of warning signs for when medical care should be secured for foot problems or what type of medical care should be sought. One frustrated participant stated: “If I had gotten better, like a different type of information that they could’ve given me, that might’ve helped me improve this ulcer to be going away. From what I have been given, you know, it’s just hard. I don’t know if it’s my foot itself or if it’s the medication. I don’t know. I don’t know if I am a unique case, I know there are people out there that have one foot. And they are able to get, probably, their ulcer better” (29-year-old Native female, history of DFU and recurrent foot infection).
Insurance coverage
While all participants had medical care coverage under Medicaid, Medicare, Indian Health Services or commercial insurance, the majority described significant medical expenses and financial strain related to their diabetes care in general, and in many cases to DFU care in particular. Most of the participants reported multiple recurring expenses such as medications (particularly insulin), co-payments for specialist visits and procedures, and the need for extensive travel, a financial strain that was frequently exacerbated by temporary or permanent loss of employment and under-employment. One participant said that following his second toe amputation: “I was in the hospital for 15 days, 13 days. They are charging me a copay, but I don’t have money to pay it. I am currently not working. I have social security and they don’t give me very much and it’s not enough to cover the copay.” (67-year-old Hispanic male, commercial insurance). In addition, many described substantial out-of-pocket payments for ancillary supplies, such as diabetic footwear and wound dressings due to inadequate insurance coverage, which often resulted in participants being unable to secure the supplies and care they needed for optimal DFU management. For example, a participant explained: “They want me to get diabetic shoes and the orthotic but at the time I didn’t have Medicaid … and with the deductible, they wanted $1,000 for the pair of shoes and the orthotic and I couldn’t afford it.” (45-year-old White female, Medicaid).
Interpersonal Level of Influence
Patient–clinician relationships.
Participants reported a wide array of levels of satisfaction with their medical providers, from long-standing personal and medically supportive relationships to negative experiences of not being listened to or being bounced from provider to provider. A predominant theme involved fragmented relationships with healthcare providers due to multiple factors including patients’ changes in residence, transitions in insurance status, providers leaving the area or switching practices, providers’ medical and holiday leave, and the COVID-19 pandemic. Given the complexity of managing their diabetes and related complications, these interruptions to patient-clinician relationships posed considerable barriers to effective disease management.
In addition, participants mentioned challenges in making timely appointments, and in getting time with their primary care physicians after major clinical events such as hospitalizations. One patient explained: “I had a lot of problems getting in contact with that doctor (primary care doctor). And after, I think it was the first four months after the amputation, and I just kept on trying to contact her… and I would try to call her, and she never returned my calls.” (47-year-old Hispanic male, history of multiple DFUs, foot infection, and toe amputation).
Similar challenges existed around establishing trusting relationships with the nurses that conducted home wound care following DFUs and amputations. This was due in large part to turnover in nursing staff or the rotation of nurses who conducted their home visits. A participant explained: “They [the companies] make a big deal about bringing the nurse in and have them trained on me and then two weeks later, I get a new nurse and redo it.” (45-year-old White female, underwent more than 20 procedures for DFUs).
Lastly, participants reported that the COVID-19 pandemic further intensified this lack of provider continuity due to limited in-person visits. For example, one participant described his struggles to connect with a new endocrinologist during the pandemic, stating: “I see him once and a current situation came up, so I haven’t been able to see him since then. [Due to the pandemic] it has been phone interviews, so, I haven’t really developed any significant rapport with my current endocrinologist.” (41-year-old White male, history of recurrent DFUs and toe amputations).
Community Level of Influence
Availability of services.
Participants commonly reported struggles with getting the medical equipment needed to prevent and manage their DFUs in a timely fashion, including offloading braces, dressing supplies, and therapeutic shoes and insoles. A few noted that the wound supplies provided by the hospital, clinic, or home healthcare companies ran out before their wounds had healed. One participant described maintaining medical supplies as his biggest challenge, saying: “The nurses themselves have been wonderful but their companies have been mainly touch-and-go with maintaining the supplies being delivered at an appropriate time” (41-year-old White male, Medicaid). Despite having prescriptions from physicians and insurance coverage, many participants also faced long waits for securing specialized diabetic shoes from medical supply companies, resulting in delayed or interrupted care. One participant described: "The insoles that I went in for, that they prescribed for me, it took me a long time to get them. Probably like three months after … and then when I got them, they, they were very flimsy, they didn’t last. It took me awhile to get another pair, a better design of the ones that they had” (47-year-old Hispanic male, self-employed, commercial health insurance).
Participants living in rural areas outside of Tucson cited additional challenges in managing their DFUs due to the time, expense, and distance involved in securing the elaborate routines of specialist appointments, routines, medications, and wound care necessary to effectively manage their DFUs. One participant described: “It was a difficulty because I am on the reservation and sometimes the medical things that I would need, like I said, insulin, the IV antibiotics, they wouldn't be able to come out here and do it. If I had lived in a city, then the people would come and get it done.” (38-year-old Native male, Medicare, rural Arizona).
Societal Level of Influence
Quality of care.
Many participants noted insufficient preventative foot care and education prior to DFU onset. Some reported that they did not learn about ulcer prevention until they developed DFUs. For example, one participant stated: “I don’t really remember (doctors) saying anything on ways to prevent other ulcers.” (38-year-old Native male, Medicaid and Indian Health Services). Some participants similarly reported that they did not receive routine foot examinations prior to developing their first DFU, even though they had regularly scheduled primary care appointments. One explained: “Well, early on they didn’t look at my feet. Before I got the ulcer, they didn’t look at them. They would just instruct me to check my blood sugar. But then after the ulcer and when they cut off my toe, that’s when they started to check my feet.” (67-year-old Hispanic male, commercial insurance).
Other barriers presented themselves while seeking adequate medical care for their new ulcers. Participants initially sought care from a variety of different venues— primary care doctors, podiatrists, specialists, emergency rooms, and urgent care clinics— as determined by how serious they interpreted their foot problems and insurance status and access issues. Some participants had the experience of being sent to multiple facilities in search of appropriate care, and those living in rural areas faced travel to different cities or towns. For example, a participant recalled that: “I went to the ER down here in XXX (a community hospital) and that was Friday (was discharged home) and then I saw my doctor on Monday and he sent me to XXX (a tertiary hospital) in Tucson.” (41-year-old White male, history of multiple DFUs and two toe amputations).
Many respondents experienced initial misdiagnoses and delays in receiving care. This included a few participants who presented for diabetic foot complications to acute care facilities, such as urgent care clincs and emergency rooms, and were sent home without an appropriate diagnosis, treatment, and follow-up. One woman recalled her frustrating journey that led to amputation:
‘I called my doctor…. She told me I want you to see an infectious disease doctor and have them put you on an IV antibiotic …. So, I get to the infectious disease doctor, and he says, ‘I’m not going to put you on antibiotic, it isn’t infected.’ So, that’s how I ended up with an amputation because he did not put me on any antibiotic. So, I went into the hospital, and they assigned me an infectious disease doctor and she came in, I’ll never forget this, and she started talking to me like I was stupid, and she goes, ‘You know you’re diabetic, you should’ve gone to a doctor right away ...’ And I said, ‘… hold on a second here, I am a very intelligent person and yes, I did, I went to my own doctor who made an appointment for me to see an infectious disease doctor.” (71-year-old White female, history of multiple DFUs and toe amputations)
Over the past two decades, substantial advances in diabetes therapy have greatly extended health and reduced morbidity. However, as evidenced in this article, significant obstacles to effective DFU treatment and management remain at multiple levels of the healthcare system. Some of these obstacles can be mitigated with more thoughtful education and alignment of access points to receive adequate health care. In this context we offer observations from our study to help address these deficits, particularly as they relate to decreasing notable health disparities.
An important individual level barrier is deficits in health literacy surrounding appropriate terminology to describe diabetic foot complications and how to make informed medical decisions about when to seek medical intervention [ 25 ]. Our findings suggest that a more aggressive and tailored education approach that guides patients to act quickly in seeking medical care and for rapid wound examination is warranted. Part of this education needs to emphasize that diabetes increases the infection and amputation risks of these seemingly “minor” foot injuries. Burdensome expenses related to DFU care posed a second individual level barrier, suggesting the need for continued advocacy for full coverage of DFU care among safety net insurance providers [ 26 , 27 ].
On the interpersonal level, our data illustrate that disruptions to the patient-clinician relationship damages rapport with patients and hinders optimal DFU care. Study participants frequently reported difficulties in accessing appropriate health care providers and disruptions to the patient-physician relationship due to the turnover of providers, changes to region and insurance status, and other factors. This gap calls for developing solutions to address medical provider shortages and to “fill in” health care assessment in a timely manner. One potential approach is to expand the use of trained community health workers who can help triage persons with differing levels of foot ulcers to available health care providers who work outside of the patient’s known environment [ 28 , 29 ].
On the community level, despite having appropriate prescriptions and insurance coverage, participants described significant challenges receiving medical equipment, which was often perceived to be due to shortcomings at the medical supply companies. Since most persons with diabetes see their pharmacist more frequently than any other member of their health care team, developing collaborations between pharmacies, providers, or healthcare system in which pharmacists take on the role of providing medical equipment such as wound care supplies or diabetic shoes, may be an effective approach. Pharmacist supported diabetes care has been shown to be well received by minority patients and to result in improved diabetes outcomes [ 30 , 31 ].
Finally, on the societal level, there is a need to improve preventive care for DFUs on the primary care physician level, a crucial strategy for limb salvage. The American Diabetes Association recommends that all patients with diabetes have their feet inspected at each doctor visit and have a comprehensive foot evaluation at least annually to identify risk factors for DFUs [ 32 ]. Greater focus needs to be placed on educating medical providers and patients, and on the importance of preventive foot care including self-foot inspection, foot examination by a medical professional, and the use of appropriate footwear. In addition, given that sample participants commonly reported receiving misdiagnoses and delays after seeking medical care for DFUs, a standardized protocol and care pathway for when, where, and how patients should seek initial DFU care and how the DFUs should be treated are imperative. Because delays occur both before and after seeking care, a focus must be made to educate both patients and providers about the standard protocol [ 33 ].
There are limitations to this study which should be considered when interpreting the results. Given the relatively modest sample size, we were not able to analyze the data for gender or age effects or by duration of diabetes. Nonetheless, this hard to reach patient sample representing a diverse population did offer very similar stories about the experiences and health disparities they faced in dealing with DFUs.
Diabetic foot ulceration remains a common and life-altering disease complication and one that disproportionately burdens people of racial and ethnic minority status, low socio-economic status, low insurance coverage, and those residing in rural areas. Our study examined the lived experience of a sample of persons with diabetes that face significant barriers at all levels of the healthcare system. Their stories highlight the importance of selecting multiple points of entry to make significant improvements in peoples’ health literacy, relationships with providers, and access to quality and effective medical care, services, and medical supplies. Moreover, this approach should creatively incorporate multiple possible modes of service delivery, including the integration of community health workers and pharmacists. While there are considerable challenges to achieving this goal, concerted efforts are needed to reduce DFUs’ devastating effects on mortality and morbidity and the inequitable burden of poorly managed diabetes foot care among highly affected populations.
Availability of data and materials
The de-identified qualitative data that support the findings of this study are available from corresponding author upon reasonable request.
Armstrong DG, Boulton AJM, Bus SA. Diabetic Foot Ulcers and Their Recurrence. N Engl J Med. 2017;376(24):2367–75.
Article Google Scholar
Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA. 2005;293(2):217–28.
Article CAS Google Scholar
Hoffstad O, Mitra N, Walsh J, Margolis DJ. Diabetes, lower-extremity amputation, and death. Diabetes Care. 2015;38(10):1852–7.
Walsh JW, Hoffstad OJ, Sullivan MO, Margolis DJ. Association of diabetic foot ulcer and death in a population-based cohort from the United Kingdom. Diabet Med. 2016;33(11):1493–8.
Mayfield JA, Reiber GE, Sanders LJ, Janisse D, Pogach LM. Preventive foot care in people with diabetes. Diabetes Care. 1998;21(12):2161–77.
Ratliff HT, Shibuya N, Jupiter DC. Minor vs. major leg amputation in adults with diabetes: Six-month readmissions, reamputations, and complications. J Diabetes Complications. 2021;35(5):107886.
Rice JB, Desai U, Cummings AK, Birnbaum HG, Skornicki M, Parsons NB. Burden of diabetic foot ulcers for medicare and private insurers. Diabetes Care. 2014;37(3):651–8.
Tan TW, Armstrong DG, Concha-Moore KC, et al. Association between race/ethnicity and the risk of amputation of lower extremities among medicare beneficiaries with diabetic foot ulcers and diabetic foot infections. BMJ Open Diabetes Res Care. 2020;8(1):e001328.
Tan TW, Shih CD, Concha-Moore KC, et al. Disparities in outcomes of patients admitted with diabetic foot infections. PLoS One. 2019;14(2):e0211481.
Margolis DJ, Malay DS, Hoffstad OJ, et al. Incidence of diabetic foot ulcer and lower extremity amputation among Medicare beneficiaries, 2006 to 2008: Data Points #2. In: Data Points Publication Series. Rockville (MD) 2011.
Skrepnek GH, Mills JL, Armstrong DG. A Diabetic Emergency One Million Feet Long: Disparities and Burdens of Illness among Diabetic Foot Ulcer Cases within Emergency Departments in the United States, 2006–2010. PLoS One. 2015;10(8):e0134914.
Arya S, Binney Z, Khakharia A, et al. Race and Socioeconomic Status Independently Affect Risk of Major Amputation in Peripheral Artery Disease. J Am Heart Assoc. 2018;7(2):e007425.
Eslami MH, Zayaruzny M, Fitzgerald GA. The adverse effects of race, insurance status, and low income on the rate of amputation in patients presenting with lower extremity ischemia. J Vasc Surg. 2007;45(1):55–9.
Lefebvre KM, Chevan J. The persistence of gender and racial disparities in vascular lower extremity amputation: an examination of HCUP-NIS data (2002–2011). Vasc Med. 2015;20(1):51–9.
Lefebvre KM, Lavery LA. Disparities in amputations in minorities. Clin Orthop Relat Res. 2011;469(7):1941–50.
Lefebvre KM, Metraux S. Disparities in level of amputation among minorities: implications for improved preventative care. J Natl Med Assoc. 2009;101(7):649–55.
PubMed Google Scholar
Skrepnek GH, Mills JL, Lavery LA, Armstrong DG. Health Care Service and Outcomes Among an Estimated 6.7 Million Ambulatory Care Diabetic Foot Cases in the U.S. Diabetes Care. 2017;40(7):936–42.
Isa D, Pace D. Is ethnicity an appropriate measure of health care marginalization? A systematic review and meta-analysis of the outcomes of diabetic foot ulceration in Aboriginal populations. Can J Surg. 2021;64(5):E476–83.
Carr D, Kappagoda M, Boseman L, Cloud LK, Croom B. Advancing Diabetes-Related Equity Through Diabetes Self-Management Education and Training: Existing Coverage Requirements and Considerations for Increased Participation. J Public Health Manag Pract. 2020;26 Suppl 2, Advancing Legal Epidemiology:S37-S44.
Sutherland BL, Pecanac K, Bartels CM, Brennan MB. Expect delays: poor connections between rural and urban health systems challenge multidisciplinary care for rural Americans with diabetic foot ulcers. J Foot Ankle Res. 2020;13(1):32.
Stevens CD, Schriger DL, Raffetto B, Davis AC, Zingmond D, Roby DH. Geographic clustering of diabetic lower-extremity amputations in low-income regions of California. Health Aff (Millwood). 2014;33(8):1383–90.
NIMHD Research Framework. National Institute on Minority Helath and Health Disparities Web site. https://www.nimhd.nih.gov/about/overview/research-framework/ . Published 2017. Accessed 22 Jan 2022.
Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful Sampling for Qualitative Data Collection and Analysis in Mixed Method Implementation Research. Adm Policy Ment Health. 2015;42(5):533–44.
Alvidrez J, Castille D, Laude-Sharp M, Rosario A, Tabor D. The National Institute on Minority Health and Health Disparities Research Framework. Am J Public Health. 2019;109(S1):S16–20.
Crocker RT, T-W. Palmer, KNB. Marrero, DG. . The Patient’s Perspective of Diabetic Foot Ulceration: A Phenomenological Exploration of Causes, Detection, and Care-Seeking. J Adv Nurs. 2022;78(8):2482–94.
Fayfman M, Schechter MC, Amobi CN, et al. Barriers to diabetic foot care in a disadvantaged population: a qualitative assessment. J Diabetes Complications. 2020;34(12):107688.
Schaper NC, Apelqvist J, Bakker K. Reducing lower leg amputations in diabetes: a challenge for patients, healthcare providers and the healthcare system. Diabetologia. 2012;55(7):1869–72.
Collinsworth AW, Vulimiri M, Schmidt KL, Snead CA. Effectiveness of a community health worker-led diabetes self-management education program and implications for CHW involvement in care coordination strategies. Diabetes Educ. 2013;39(6):792–9.
Rosenthal EL, Wiggins N, Ingram M, Mayfield-Johnson S, De Zapien JG. Community health workers then and now: an overview of national studies aimed at defining the field. J Ambul Care Manage. 2011;34(3):247–59.
Smith M. Pharmacists’ role in improving diabetes medication management. J Diabetes Sci Technol. 2009;3(1):175–9.
Nabulsi NA, Yan CH, Tilton JJ, Gerber BS, Sharp LK. Clinical pharmacists in diabetes management: What do minority patients with uncontrolled diabetes have to say? J Am Pharm Assoc (2003). 2020;60(5):708–15.
American Diabetes A. 10 Microvascular Complications and Foot Care: Standards of Medical Care in Diabetes-2018. Diabetes Care. 2018;41(Suppl 1):S105–18.
Sanders AP, Stoeldraaijers LG, Pero MW, Hermkes PJ, Carolina RC, Elders PJ. Patient and professional delay in the referral trajectory of patients with diabetic foot ulcers. Diabetes Res Clin Pract. 2013;102(2):105–11.
Download references
Acknowledgements
Our team acknowledge the participants of the study.
The project is supported by a National Institute of Diabetes and Kidney Disease K23 Mentored Patient-Oriented Research Career Development Award (1K23DK122126) and a Society of Vascular Surgery Foundation Mentored Research Career Development Award Program (T-W.T) and a National Institute of Diabetes and Kidney Disease R01 (1R01124789) Award (D.G.A).
Author information
Authors and affiliations.
Southwestern Academic Limb Salvage Alliance (SALSA), Los Angeles, Tucson, USA
Tze-Woei Tan & David G. Armstrong
Division of Vascular Surgery and Endovascular Therapy, Keck School of Medicine, University of Southern California, 1520 San Pablo Street, Ste 4300, Los Angeles, CA, 90033, USA
Center for Health Disparities Research (CHDR), University of Arizona Health Sciences, Tucson, AZ, USA
Rebecca M. Crocker, Kelly N. B. Palmer & David G. Marrero
University of Arizona College of Medicine, Tucson, AZ, USA
Chris Gomez
You can also search for this author in PubMed Google Scholar
Contributions
Tze-Woei Tan: Conceptualization, Methology, Validation, Formal Analysis, Writing – Original Draft, Writing – Review & Editing, Supervision, Project Administration, Funding Acquisition. Rebecca M. Crocker: Conceptualization, Methology, Validation, Formal Analysis, Writing – Original Draft, Writing – Review & Editing. Kelly N.B. Palmer: Conceptualization, Methology, Validation, Formal Analysis, Writing – Review & Editing. Chris Gomez: Methology, Validation, Formal Analysis, Writing – Original Draft, Writing – Review & Editing. David G. Armstrong: Conceptualization, Methology, Writing – Review & Editing. David G. Marrero: Conceptualization, Methology, Validation, Formal Analysis, Writing – Original Draft, Writing – Review & Editing. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Tze-Woei Tan .
Ethics declarations
Ethics approval and consent to participate.
The University of Arizona Institutional Review Board approved the study in July 2019 (Protocol Number 1906749805). All participants provided written informed consent prior to participation.
Consent for publication
Not applicable.
Competing interests
The authors haves no related conflicts of interest to declare.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Tan, TW., Crocker, R.M., Palmer, K.N.B. et al. A qualitative study of barriers to care-seeking for diabetic foot ulceration across multiple levels of the healthcare system. J Foot Ankle Res 15 , 56 (2022). https://doi.org/10.1186/s13047-022-00561-4
Download citation
Received : 24 May 2022
Accepted : 22 July 2022
Published : 06 August 2022
DOI : https://doi.org/10.1186/s13047-022-00561-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Diabetic foot complications
- Foot ulceration
- Barriers in assessing medical care
- Health care system barriers
- Qualitative
Journal of Foot and Ankle Research
ISSN: 1757-1146
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Frontiers in Endocrinology
- Clinical Diabetes
- Research Topics
Improving Outcomes in Diabetic Foot Care - A Worldwide Perspective
Total Downloads
Total Views and Downloads
About this Research Topic
Enhanced population longevity, decrease in physical activity and the obesity pandemic have resulted in an increase in incidence of type 2 diabetes in all WHO health care areas. The prevalence of the condition has been further increased by an increase in life expectancy of those living with both type 1 and ...
Keywords : Diabetic Foot, Diabetic Foot Ulcers, Diabetic Foot Infections, Diabetic Foot Osteomyelitis, Lower limb amputation, Peripheral arterial disease, Diabetes peripheral neuropathy, Charcot Foot, Diabetic Foot Prevention, Therapeutic Shoes, Wound healing
Important Note : All contributions to this Research Topic must be within the scope of the section and journal to which they are submitted, as defined in their mission statements. Frontiers reserves the right to guide an out-of-scope manuscript to a more suitable section or journal at any stage of peer review.
Topic Editors
Topic coordinators, recent articles, submission deadlines.
Submission closed.
Participating Journals
Total views.
- Demographics
No records found
total views article views downloads topic views
Top countries
Top referring sites, about frontiers research topics.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.

Research advances in hydrogel-based wound dressings for diabetic foot ulcer treatment: a review
- Published: 05 May 2024
- Volume 59 , pages 8059–8084, ( 2024 )
Cite this article

- Jie Zhao ORCID: orcid.org/0000-0001-9006-0004 1 , 2 ,
- Jie Liu 3 ,
- Yuxin Hu 1 , 2 ,
- Wanxuan Hu 4 ,
- Juan Wei 5 ,
- Haisheng Qian 6 &
- Yexiang Sun 4
141 Accesses
Explore all metrics
Diabetic foot ulcers (DFUs) are one of the most challenging and prevalent refractory wounds associated with diabetes mellitus. It is characterized with long courses, high recurrence and disability rates. Hydrogel-based wound dressings have been demonstrated an effective and promising strategy for treating diabetic wounds. However, the complexity of the pathogenesis and microenvironment in diabetic wounds have restricted both the experts in functional hydrogels and clinicians. The former had no inspiration for clinical demands in the design process, and the latter was confused about clinical use because they knew little about the tremendous potential of the functional hydrogels. Here, important targets for DFUs treatment were listed, and effective products underlying the molecular pathogenesis were suggested for the designer. Then, the application of hydrogels into DFUs were classified in accordance with their functional targets and active ingredients. Hence, it is very convenient for clinicians to make a perfect option for different wounds. Finally, research gaps and future prospects for wound-healing hydrogels were presented. We envision that this review can inspire creativity and innovation in the development of hydrogel-based wound dressings for diabetic foot ulcer treatment.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others

Injectable carrier hydrogel for diabetic foot ulcer wound repair

Research advances in smart responsive-hydrogel dressings with potential clinical diabetic wound healing properties

Advanced polymer hydrogels that promote diabetic ulcer healing: mechanisms, classifications, and medical applications
Availability of data and materials.
Not applicable.
American Diabetes A (2020) 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2020. Diabetes Care 43(Suppl 1):S14–S31. https://doi.org/10.2337/dc20-S002
Article Google Scholar
Sun H, Saeedi P, Karuranga S et al (2022) IDF diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract 183:109119. https://doi.org/10.1016/j.diabres.2021.109119
Article PubMed Google Scholar
Armstrong DG, Swerdlow MA, Armstrong AA et al (2020) Five year mortality and direct costs of care for people with diabetic foot complications are comparable to cancer. J Foot Ankle Res 13(1):16. https://doi.org/10.1186/s13047-020-00383-2
Article PubMed PubMed Central Google Scholar
Armstrong DG, Boulton AJM, Bus SA (2017) Diabetic foot ulcers and their recurrence. N Engl J Med 376(24):2367–2375. https://doi.org/10.1056/NEJMra1615439
Reardon R, Simring D, Kim B et al (2020) The diabetic foot ulcer. Aust J Gen Pract 49(5):250–255. https://doi.org/10.31128/AJGP-11-19-5161
Huang ZH, Li SQ, Kou Y et al (2019) Risk factors for the recurrence of diabetic foot ulcers among diabetic patients: a meta-analysis. Int Wound J 16(6):1373–1382. https://doi.org/10.1111/iwj.13200
Chamberlain RC, Fleetwood K, Wild SH et al (2022) Foot ulcer and risk of lower limb amputation or death in people with diabetes: a national population-based retrospective cohort study. Diabetes Care 45(1):83–91. https://doi.org/10.2337/dc21-1596
Bandyk DF (2018) The diabetic foot: pathophysiology, evaluation, and treatment. Semin Vasc Surg 31(2–4):43–48. https://doi.org/10.1053/j.semvascsurg.2019.02.001
Francia P, Gualdani E, Policardo L et al (2022) Mortality risk associated with diabetic foot complications in people with or without history of diabetic foot hospitalizations. J Clin Med 11(9):2454. https://doi.org/10.3390/jcm11092454
Dogruel H, Aydemir M, Balci MK (2022) Management of diabetic foot ulcers and the challenging points: an endocrine view. World J Diabetes 13(1):27–36. https://doi.org/10.4239/wjd.v13.i1.27
Schaper NC, van Netten JJ, Apelqvist J et al (2020) Practical Guidelines on the prevention and management of diabetic foot disease (IWGDF 2019 update). Diabetes Metab Res Rev 36(Suppl 1):e3266. https://doi.org/10.1002/dmrr.3266
Falanga V (2005) Wound healing and its impairment in the diabetic foot. Lancet 366(9498):1736–1743. https://doi.org/10.1016/S0140-6736(05)67700-8
Ryall C, Duarah S, Chen S et al (2022) Advancements in skin delivery of natural bioactive products for wound management: a brief review of two decades. Pharmaceutics 14(5):1072. https://doi.org/10.3390/pharmaceutics14051072
Article CAS PubMed PubMed Central Google Scholar
Ongarora BG (2022) Recent technological advances in the management of chronic wounds: a literature review. Health Sci Rep 5(3):e641. https://doi.org/10.1002/hsr2.641
Hunt TK, Hopf HW (1997) Wound healing and wound infection. What surgeons and anesthesiologists can do. Surg Clin North Am 77(3):587–606. https://doi.org/10.1016/s0039-6109(05)70570-3
Article CAS PubMed Google Scholar
Stadelmann WK, Digenis AG, Tobin GR (1998) Physiology and healing dynamics of chronic cutaneous wounds. Am J Surg 176(2A Suppl):26S-38S. https://doi.org/10.1016/s0002-9610(98)00183-4
Undas A, Wiek I, Stepien E et al (2008) Hyperglycemia is associated with enhanced thrombin formation, platelet activation, and fibrin clot resistance to lysis in patients with acute coronary syndrome. Diabetes Care 31(8):1590–1595. https://doi.org/10.2337/dc08-0282
Al SH (2022) Macrophage phenotypes in normal and diabetic wound healing and therapeutic interventions. Cells 11(15):2430. https://doi.org/10.3390/cells11152430
Article CAS Google Scholar
Peng Y, Xiong RP, Zhang ZH et al (2021) Ski promotes proliferation and inhibits apoptosis in fibroblasts under high-glucose conditions via the FoxO1 pathway. Cell Prolif 54(2):e12971. https://doi.org/10.1111/cpr.12971
Hu SC, Lan CE (2016) High-glucose environment disturbs the physiologic functions of keratinocytes: focusing on diabetic wound healing. J Dermatol Sci 84(2):121–127. https://doi.org/10.1016/j.jdermsci.2016.07.008
Wei F, Wang A, Wang Q et al (2020) Plasma endothelial cells-derived extracellular vesicles promote wound healing in diabetes through YAP and the PI3K/Akt/mTOR pathway. Aging (Albany NY) 12(12):12002–12018. https://doi.org/10.18632/aging.103366
Nie X, Zhang H, Shi X et al (2020) Asiaticoside nitric oxide gel accelerates diabetic cutaneous ulcers healing by activating Wnt/beta-catenin signaling pathway. Int Immunopharmacol 79:106109. https://doi.org/10.1016/j.intimp.2019.106109
Geng K, Ma X, Jiang Z et al (2023) WDR74 facilitates TGF-beta/Smad pathway activation to promote M2 macrophage polarization and diabetic foot ulcer wound healing in mice. Cell Biol Toxicol 39(4):1577–1591. https://doi.org/10.1007/s10565-022-09748-8
Yang Y, Zhang B, Yang Y et al (2022) FOXM1 accelerates wound healing in diabetic foot ulcer by inducing M2 macrophage polarization through a mechanism involving SEMA3C/NRP2/Hedgehog signaling. Diabetes Res Clin Pract 184:109121. https://doi.org/10.1016/j.diabres.2021.109121
Luanraksa S, Jindatanmanusan P, Boonsiri T et al (2018) An MMP/TIMP ratio scoring system as a potential predictive marker of diabetic foot ulcer healing. J Wound Care 27(12):849–855. https://doi.org/10.12968/jowc.2018.27.12.849
Zubair M, Ahmad J (2019) Role of growth factors and cytokines in diabetic foot ulcer healing: a detailed review. Rev Endocr Metab Disord 20(2):207–217. https://doi.org/10.1007/s11154-019-09492-1
Yang H-L, Tsai Y-C, Korivi M et al (2017) Lucidone promotes the cutaneous wound healing process via activation of the PI3K/AKT. Wnt/β-catenin and NF-κB signaling pathways 1864(1):151–168
CAS Google Scholar
Zhao Y, Liu M, Zhang Y et al (2015) Expression changes of Wnt/β-catenin signaling pathway in diabetic ulcer. Chin J Pathophysiol 31(11):2033–2038. https://doi.org/10.3969/j.issn.1000-4718.2015.11.018
Lee EG, Luckett-Chastain LR, Calhoun KN et al (2019) Interleukin 6 function in the skin and isolated keratinocytes is modulated by hyperglycemia. J Immunol Res 3:5087847. https://doi.org/10.1155/2019/5087847
Amin KN, Umapathy D, Anandharaj A et al (2020) miR-23c regulates wound healing by targeting stromal cell-derived factor-1alpha (SDF-1alpha/CXCL12) among patients with diabetic foot ulcer. Microvasc Res 127:103924. https://doi.org/10.1016/j.mvr.2019.103924
Liu L, Chen R, Jia Z et al (2022) Downregulation of hsa-miR-203 in peripheral blood and wound margin tissue by negative pressure wound therapy contributes to wound healing of diabetic foot ulcers. Microvasc Res 139:104275. https://doi.org/10.1016/j.mvr.2021.104275
Pichu S, Sathiyamoorthy J, Vimalraj S et al (2017) Impact of lysyl oxidase (G473A) polymorphism on diabetic foot ulcers. Int J Biol Macromol 103:242–247. https://doi.org/10.1016/j.ijbiomac.2017.05.050
Xu Y, Chen H, Fang Y et al (2022) Hydrogel combined with phototherapy in wound healing. Adv Healthc Mater 11(16):e2200494. https://doi.org/10.1002/adhm.202200494
Stan D, Tanase C, Avram M et al (2021) Wound healing applications of creams and “smart” hydrogels. Exp Dermatol 30(9):1218–1232. https://doi.org/10.1111/exd.14396
Gjorevski N, Sachs N, Manfrin A et al (2016) Designer matrices for intestinal stem cell and organoid culture. Nature 539(7630):560–564. https://doi.org/10.1038/nature20168
Zhang W, Zhang Y, Zhang Y et al (2021) Adhesive and tough hydrogels: from structural design to applications. J Mater Chem B 9(30):5954–5966. https://doi.org/10.1039/d1tb01166a
Fuchs S, Shariati K, Ma M (2020) Specialty Tough Hydrogels and Their Biomedical Applications. Adv Healthc Mater 9(2):e1901396. https://doi.org/10.1002/adhm.201901396
Vasile C, Pamfil D, Stoleru E et al (2020) New developments in medical applications of hybrid hydrogels containing natural polymers. Molecules 25(7):1539. https://doi.org/10.3390/molecules25071539
Hotz N, Wilcke L, Weber W (2013) Design, synthesis, and application of stimulus-sensing biohybrid hydrogels. Macromol Rapid Commun 34(20):1594–1610. https://doi.org/10.1002/marc.201300468
Malone-Povolny MJ, Maloney SE, Schoenfisch MH (2019) Nitric Oxide Therapy for Diabetic Wound Healing. Adv Healthc Mater 8(12):e1801210. https://doi.org/10.1002/adhm.201801210
Guo S, Dipietro LA (2010) Factors affecting wound healing. J Dent Res 89(3):219–229. https://doi.org/10.1177/0022034509359125
Bjarnsholt T, Kirketerp-Moller K, Jensen PO et al (2008) Why chronic wounds will not heal: a novel hypothesis. Wound Repair Regen 16(1):2–10. https://doi.org/10.1111/j.1524-475X.2007.00283.x
Satitsri S, Muanprasat C (2020) Chitin and chitosan derivatives as biomaterial resources for biological and biomedical applications. Molecules 25(24):5961. https://doi.org/10.3390/molecules25245961
Webber MJ, Pashuck ET (2021) (Macro)molecular self-assembly for hydrogel drug delivery. Adv Drug Deliv Rev 172:275–295. https://doi.org/10.1016/j.addr.2021.01.006
Waters DJ, Engberg K, Parke-Houben R et al (2010) Morphology of photopolymerized end-linked poly(ethylene glycol) hydrogels by small angle X-ray Scattering. Macromolecules 43(16):6861–6870. https://doi.org/10.1021/ma101070s
Ferreira PG, Ferreira VF, da Silva FC et al (2022) Chitosans and nanochitosans: recent advances in skin protection, regeneration, and repair. Pharmaceutics 14(6):1307. https://doi.org/10.3390/pharmaceutics14061307
Ganan M, Carrascosa AV, Martinez-Rodriguez AJ (2009) Antimicrobial activity of chitosan against Campylobacter spp. and other microorganisms and its mechanism of action. J Food Prot 72(8):1735–1738. https://doi.org/10.4315/0362-028x-72.8.1735
Matica MA, Aachmann FL, Tondervik A et al (2019) Chitosan as a wound dressing starting material: antimicrobial properties and mode of action. Int J Mol Sci 20(23):5889. https://doi.org/10.3390/ijms20235889
Raafat D, von Bargen K, Haas A et al (2008) Insights into the mode of action of chitosan as an antibacterial compound. Appl Environ Microbiol 74(12):3764–3773. https://doi.org/10.1128/AEM.00453-08
Lopez-Moya F, Suarez-Fernandez M, Lopez-Llorca LV (2019) Molecular mechanisms of chitosan interactions with fungi and plants. Int J Mol Sci 20(2):332. https://doi.org/10.3390/ijms20020332
Tan H, Ma R, Lin C et al (2013) Quaternized chitosan as an antimicrobial agent: antimicrobial activity, mechanism of action and biomedical applications in orthopedics. Int J Mol Sci 14(1):1854–1869. https://doi.org/10.3390/ijms14011854
Vishu Kumar AB, Varadaraj MC, Gowda LR et al (2005) Characterization of chito-oligosaccharides prepared by chitosanolysis with the aid of papain and Pronase, and their bactericidal action against Bacillus cereus and Escherichia coli. Biochem J 391(Pt 2):167–175. https://doi.org/10.1042/BJ20050093
Hu C, Long L, Cao J et al (2021) Dual-crosslinked mussel-inspired smart hydrogels with enhanced antibacterial and angiogenic properties for chronic infected diabetic wound treatment via pH-responsive quick cargo release. Chem Eng J 411:128564
He J, Li Z, Wang J et al (2023) Photothermal antibacterial antioxidant conductive self-healing hydrogel with nitric oxide release accelerates diabetic wound healing. Compos Part B Eng 266:110985
Kasparova P, Zmuda M, Vankova E et al (2021) Low-molecular weight chitosan enhances antibacterial effect of antibiotics and permeabilizes cytoplasmic membrane of Staphylococcus epidermidis biofilm cells. Folia Microbiol (Praha) 66(6):983–996. https://doi.org/10.1007/s12223-021-00898-6
Jing YJ, Hao YJ, Qu H et al (2007) Studies on the antibacterial activities and mechanisms of chitosan obtained from cuticles of housefly larvae. Acta Biol Hung 58(1):75–86. https://doi.org/10.1556/ABiol.57.2007.1.7
Younes I, Sellimi S, Rinaudo M et al (2014) Influence of acetylation degree and molecular weight of homogeneous chitosans on antibacterial and antifungal activities. Int J Food Microbiol 185:57–63. https://doi.org/10.1016/j.ijfoodmicro.2014.04.029
Mellegard H, Strand SP, Christensen BE et al (2011) Antibacterial activity of chemically defined chitosans: influence of molecular weight, degree of acetylation and test organism. Int J Food Microbiol 148(1):48–54. https://doi.org/10.1016/j.ijfoodmicro.2011.04.023
Younes I, Rinaudo M (2015) Chitin and chitosan preparation from marine sources. Structure, properties and applications. Mar Drugs 13(3):1133–1174. https://doi.org/10.3390/md13031133
Cele ZED, Somboro AM, Amoako DG et al (2020) Fluorinated Quaternary Chitosan Derivatives: Synthesis, Characterization, Antibacterial Activity, and Killing Kinetics. ACS Omega 5(46):29657–29666. https://doi.org/10.1021/acsomega.0c01355
Hoque J, Adhikary U, Yadav V et al (2016) Chitosan derivatives active against multidrug-resistant bacteria and pathogenic fungi: in vivo evaluation as topical antimicrobials. Mol Pharm 13(10):3578–3589. https://doi.org/10.1021/acs.molpharmaceut.6b00764
Wahid F, Hu XH, Chu LQ et al (2019) Development of bacterial cellulose/chitosan based semi-interpenetrating hydrogels with improved mechanical and antibacterial properties. Int J Biol Macromol 122:380–387. https://doi.org/10.1016/j.ijbiomac.2018.10.105
Omidi S, Kakanejadifard A (2019) Modification of chitosan and chitosan nanoparticle by long chain pyridinium compounds: Synthesis, characterization, antibacterial, and antioxidant activities. Carbohydr Polym 208:477–485. https://doi.org/10.1016/j.carbpol.2018.12.097
Zhao X, Wu H, Guo B et al (2017) Antibacterial anti-oxidant electroactive injectable hydrogel as self-healing wound dressing with hemostasis and adhesiveness for cutaneous wound healing. Biomaterials 122:34–47. https://doi.org/10.1016/j.biomaterials.2017.01.011
Wang M, Yue L, Niazi S et al (2022) Synthesis and characterization of cinnamic acid conjugated N-(2-hydroxy)-propyl-3-trimethylammonium chitosan chloride derivatives: A hybrid flocculant with antibacterial activity. Int J Biol Macromol 206:886–895. https://doi.org/10.1016/j.ijbiomac.2022.03.075
Sivanesan I, Muthu M, Gopal J et al (2021) Nanochitosan: commemorating the metamorphosis of an exoskeletal waste to a versatile nutraceutical. Nanomater (Basel) 11(3):821. https://doi.org/10.3390/nano11030821
Duan S, Wang R (2013) Bimetallic nanostructures with magnetic and noble metals and their physicochemical applications. Prog Nat Sci Mater Int 23(2):113–126. https://doi.org/10.1016/j.pnsc.2013.02.001
Guo Z, Chen Y, Wang Y et al (2020) Advances and challenges in metallic nanomaterial synthesis and antibacterial applications. J Mater Chem B 8(22):4764–4777. https://doi.org/10.1039/d0tb00099j
Hamdan S, Pastar I, Drakulich S et al (2017) Nanotechnology-driven therapeutic interventions in wound healing: potential uses and applications. ACS Cent Sci 3(3):163–175. https://doi.org/10.1021/acscentsci.6b00371
Kedziora A, Speruda M, Krzyzewska E et al (2018) Similarities and differences between silver ions and silver in nanoforms as antibacterial agents. Int J Mol Sci 19(2):444. https://doi.org/10.3390/ijms19020444
Choudhury H, Pandey M, Lim YQ et al (2020) Silver nanoparticles: Advanced and promising technology in diabetic wound therapy. Mater Sci Eng C Mater Biol Appl 112:110925. https://doi.org/10.1016/j.msec.2020.110925
Burdusel AC, Gherasim O, Grumezescu AM et al (2018) Biomedical applications of silver nanoparticles: an up-to-date overview. Nanomater (Basel) 8(9):681. https://doi.org/10.3390/nano8090681
Das S, Baker AB (2016) Biomaterials and nanotherapeutics for enhancing skin wound healing. Front Bioeng Biotechnol 4:82. https://doi.org/10.3389/fbioe.2016.00082
Bruna T, Maldonado-Bravo F, Jara P et al (2021) Silver nanoparticles and their antibacterial applications. Int J Mol Sci 22(13):7202. https://doi.org/10.3390/ijms22137202
Zhao Y, Li Z, Song S et al (2019) Skin-Inspired Antibacterial Conductive Hydrogels for Epidermal Sensors and Diabetic Foot Wound Dressings. Adv Funct Mater 29(31):1901474. https://doi.org/10.1002/adfm.201901474
Wang P, Jiang S, Li Y et al (2021) Virus-like mesoporous silica-coated plasmonic Ag nanocube with strong bacteria adhesion for diabetic wound ulcer healing. Nanomedicine 34:102381. https://doi.org/10.1016/j.nano.2021.102381
Pham TN, Jiang YS, Su CF et al (2020) In situ formation of silver nanoparticles-contained gelatin-PEG-dopamine hydrogels via enzymatic cross-linking reaction for improved antibacterial activities. Int J Biol Macromol 146:1050–1059. https://doi.org/10.1016/j.ijbiomac.2019.09.230
Laurenti M, Cauda V (2017) ZnO nanostructures for tissue engineering applications. Nanomater (Basel) 7(11):374. https://doi.org/10.3390/nano7110374
Jamnongkan T, Sukumaran SK, Sugimoto M et al (2015) Towards novel wound dressings: antibacterial properties of zinc oxide nanoparticles and electrospun fiber mats of zinc oxide nanoparticle/poly (vinyl alcohol) hybrids. J Polym Eng 35(6):575–586
Ottone C, Rivera VF, Fontana M et al (2014) Ultralong and mesoporous ZnO and γ-Al2O3 oriented nanowires obtained by template-assisted hydrothermal approach. J Mater Sci Technol 30(12):1167–1173
Dumontel B, Canta M, Engelke H et al (2017) Enhanced biostability and cellular uptake of zinc oxide nanocrystals shielded with a phospholipid bilayer. J Mater Chem B 5(44):8799–8813. https://doi.org/10.1039/c7tb02229h
Ahmed S, Chaudhry SA et al (2017) A review on biogenic synthesis of ZnO nanoparticles using plant extracts and microbes: a prospect towards green chemistry. J Photochem Photobiol B 166:272–284. https://doi.org/10.1016/j.jphotobiol.2016.12.011
Hajipour MJ, Fromm KM, Ashkarran AA et al (2012) Antibacterial properties of nanoparticles. Trends Biotechnol 30(10):499–511. https://doi.org/10.1016/j.tibtech.2012.06.004
Chupani L, Zuskova E, Niksirat H et al (2017) Effects of chronic dietary exposure of zinc oxide nanoparticles on the serum protein profile of juvenile common carp ( Cyprinus carpio L.). Sci Total Environ 579:1504–1511. https://doi.org/10.1016/j.scitotenv.2016.11.154
Blecher K, Nasir A, Friedman A (2011) The growing role of nanotechnology in combating infectious disease. Virulence 2(5):395–401. https://doi.org/10.4161/viru.2.5.17035
Huh AJ, Kwon YJ (2011) “Nanoantibiotics”: a new paradigm for treating infectious diseases using nanomaterials in the antibiotics resistant era. J Control Release 156(2):128–145. https://doi.org/10.1016/j.jconrel.2011.07.002
Steffy K, Shanthi G, Maroky AS et al (2018) Enhanced antibacterial effects of green synthesized ZnO NPs using Aristolochia indica against multi-drug resistant bacterial pathogens from Diabetic Foot Ulcer. J Infect Public Health 11(4):463–471. https://doi.org/10.1016/j.jiph.2017.10.006
Vinotha V, Iswarya A, Thaya R et al (2019) Synthesis of ZnO nanoparticles using insulin-rich leaf extract: anti-diabetic, antibiofilm and anti-oxidant properties. J Photochem Photobiol B 197:111541. https://doi.org/10.1016/j.jphotobiol.2019.111541
Tavakoli S, Mokhtari H, Kharaziha M et al (2020) A multifunctional nanocomposite spray dressing of Kappa-carrageenan-polydopamine modified ZnO/L-glutamic acid for diabetic wounds. Mater Sci Eng C Mater Biol Appl 111:110837. https://doi.org/10.1016/j.msec.2020.110837
Soenen SJ, Parak WJ, Rejman J et al (2015) (Intra)cellular stability of inorganic nanoparticles: effects on cytotoxicity, particle functionality, and biomedical applications. Chem Rev 115(5):2109–2135. https://doi.org/10.1021/cr400714j
Wynn TA, Barron L (2010) Macrophages: master regulators of inflammation and fibrosis. Semin Liver Dis 30(3):245–257. https://doi.org/10.1055/s-0030-1255354
Bratton DL, Henson PM (2011) Neutrophil clearance: when the party is over, clean-up begins. Trends Immunol 32(8):350–357. https://doi.org/10.1016/j.it.2011.04.009
Krzyszczyk P, Schloss R, Palmer A et al (2018) The role of macrophages in acute and chronic wound healing and interventions to promote pro-wound healing phenotypes. Front Physiol 9:419. https://doi.org/10.3389/fphys.2018.00419
Shen T, Dai K, Yu Y et al (2020) Sulfated chitosan rescues dysfunctional macrophages and accelerates wound healing in diabetic mice. Acta Biomater 117:192–203. https://doi.org/10.1016/j.actbio.2020.09.035
Yang H, Song L, Sun B et al (2021) Modulation of macrophages by a paeoniflorin-loaded hyaluronic acid-based hydrogel promotes diabetic wound healing. Mater Today Bio 12:100139. https://doi.org/10.1016/j.mtbio.2021.100139
Xia H, Dong Z, Tang Q et al (2023) Glycopeptide-based multifunctional hydrogels promote diabetic wound healing through ph regulation of microenvironment. Adv Funct Mater. https://doi.org/10.1002/adfm.202215116
Wong SL, Demers M, Martinod K et al (2015) Diabetes primes neutrophils to undergo NETosis, which impairs wound healing. Nat Med 21(7):815–819. https://doi.org/10.1038/nm.3887
Yuan Y, Fan D, Shen S et al (2022) An M2 macrophage-polarized anti-inflammatory hydrogel combined with mild heat stimulation for regulating chronic inflammation and impaired angiogenesis of diabetic wounds. Chem Eng J 433:133859
Soehnlein O, Steffens S, Hidalgo A et al (2017) Neutrophils as protagonists and targets in chronic inflammation. Nat Rev Immunol 17(4):248–261. https://doi.org/10.1038/nri.2017.10
Karima M, Kantarci A, Ohira T et al (2005) Enhanced superoxide release and elevated protein kinase C activity in neutrophils from diabetic patients: association with periodontitis. J Leukoc Biol 78(4):862–870. https://doi.org/10.1189/jlb.1004583
Kaur T, Dumoga S, Koul V et al (2020) Modulating neutrophil extracellular traps for wound healing. Biomater Sci 8(11):3212–3223. https://doi.org/10.1039/d0bm00355g
Hyun SW, Kim J, Jo K et al (2018) Aster koraiensis extract improves impaired skin wound healing during hyperglycemia. Integr Med Res 7(4):351–357. https://doi.org/10.1016/j.imr.2018.09.001
Li N, Yang L, Pan C et al (2020) Naturally-occurring bacterial cellulose-hyperbranched cationic polysaccharide derivative/MMP-9 siRNA composite dressing for wound healing enhancement in diabetic rats. Acta Biomater 102:298–314. https://doi.org/10.1016/j.actbio.2019.11.005
Zhou W, Duan Z, Zhao J et al (2022) Glucose and MMP-9 dual-responsive hydrogel with temperature sensitive self-adaptive shape and controlled drug release accelerates diabetic wound healing. Bioact Mater 17:1–17. https://doi.org/10.1016/j.bioactmat.2022.01.004
Walton DM, Minton SD, Cook AD (2019) The potential of transdermal nitric oxide treatment for diabetic peripheral neuropathy and diabetic foot ulcers. Diabetes Metab Syndr 13(5):3053–3056. https://doi.org/10.1016/j.dsx.2018.07.003
Ahmed R, Augustine R, Chaudhry M et al (2022) Nitric oxide-releasing biomaterials for promoting wound healing in impaired diabetic wounds: state of the art and recent trends. Biomed Pharmacother 149:112707. https://doi.org/10.1016/j.biopha.2022.112707
Suschek CV, Feibel D, von Kohout M et al (2022) Enhancement of nitric oxide bioavailability by modulation of cutaneous nitric oxide stores. Biomedicines 10(9):2124. https://doi.org/10.3390/biomedicines10092124
Nathan CF, Hibbs JB Jr (1991) Role of nitric oxide synthesis in macrophage antimicrobial activity. Curr Opin Immunol 3(1):65–70. https://doi.org/10.1016/0952-7915(91)90079-g
Bredt DS, Snyder SH (1990) Isolation of nitric oxide synthetase, a calmodulin-requiring enzyme. Proc Natl Acad Sci U S A 87(2):682–685. https://doi.org/10.1073/pnas.87.2.682
Coneski PN, Schoenfisch MH (2012) Nitric oxide release: part III. Meas report Chem Soc Rev 41(10):3753–3758. https://doi.org/10.1039/c2cs15271a
Neufeld BH, Reynolds MM (2016) Critical nitric oxide concentration for Pseudomonas aeruginosa biofilm reduction on polyurethane substrates. Biointerphases 11(3):031012. https://doi.org/10.1116/1.4962266
Kreuger MR, Tames DR, Mariano M (1998) Expression of NO-synthase in cells of foreign-body and BCG-induced granulomata in mice: influence of L-NAME on the evolution of the lesion. Immunology 95(2):278–282. https://doi.org/10.1046/j.1365-2567.1998.00542.x
Krischel V, Bruch-Gerharz D, Suschek C et al (1998) Biphasic effect of exogenous nitric oxide on proliferation and differentiation in skin derived keratinocytes but not fibroblasts. J Invest Dermatol 111(2):286–291. https://doi.org/10.1046/j.1523-1747.1998.00268.x
Howdieshell TR, Webb WL, Sathyanarayana MD et al (2003) Inhibition of inducible nitric oxide synthase results in reductions in wound vascular endothelial growth factor expression, granulation tissue formation, and local perfusion. Surgery 133(5):528–537. https://doi.org/10.1067/msy.2003.128
Zhao Y, Luo L, Huang L et al (2022) In situ hydrogel capturing nitric oxide microbubbles accelerates the healing of diabetic foot. J Control Release 350:93–106. https://doi.org/10.1016/j.jconrel.2022.08.018
Tu C, Lu H, Zhou T et al (2022) Promoting the healing of infected diabetic wound by an anti-bacterial and nano-enzyme-containing hydrogel with inflammation-suppressing, ROS-scavenging, oxygen and nitric oxide-generating properties. Biomaterials 286:121597. https://doi.org/10.1016/j.biomaterials
Ando A, Miyamoto M, Saito N et al (2021) Small fibre neuropathy is associated with impaired vascular endothelial function in patients with type 2 diabetes. Front Endocrinol (Lausanne) 12:653277. https://doi.org/10.3389/fendo.2021.653277
Li L, Yang Y, Bai J et al (2022) Impaired vascular endothelial function is associated with peripheral neuropathy in patients with type 2 diabetes. Diabetes Metab Syndr Obes 15:1437–1449. https://doi.org/10.2147/DMSO.S352316
den Dekker A, Davis FM, Kunkel SL et al (2019) Targeting epigenetic mechanisms in diabetic wound healing. Transl Res 204:39–50. https://doi.org/10.1016/j.trsl.2018.10.001
Veves A, Akbari CM, Primavera J et al (1998) Endothelial dysfunction and the expression of endothelial nitric oxide synthetase in diabetic neuropathy, vascular disease, and foot ulceration. Diabetes 47(3):457–463. https://doi.org/10.2337/diabetes.47.3.457
DiPietro LA (2016) Angiogenesis and wound repair: when enough is enough. J Leukoc Biol 100(5):979–984. https://doi.org/10.1189/jlb.4MR0316-102R
Guan Y, Niu H, Liu Z et al (2021) Sustained oxygenation accelerates diabetic wound healing by promoting epithelialization and angiogenesis and decreasing inflammation. Sci Adv 7(35):eabj0153. https://doi.org/10.1126/sciadv.abj0153
Jee JP, Pangeni R, Jha SK et al (2019) Preparation and in vivo evaluation of a topical hydrogel system incorporating highly skin-permeable growth factors, quercetin, and oxygen carriers for enhanced diabetic wound-healing therapy. Int J Nanomedicine 14:5449–5475. https://doi.org/10.2147/IJN.S213883
Zhu S, Zhao B, Li M et al (2023) Microenvironment responsive nanocomposite hydrogel with NIR photothermal therapy, vascularization and anti-inflammation for diabetic infected wound healing. Bioact Mater 26:306–320
CAS PubMed PubMed Central Google Scholar
Chen B, Zhang H, Qiu J et al (2022) Mechanical force induced self-assembly of chinese herbal hydrogel with synergistic effects of antibacterial activity and immune regulation for wound healing. Small 18(21):e2201766. https://doi.org/10.1002/smll.202201766
Ning S, Zang J, Zhang B et al (2022) Botanical drugs in traditional chinese medicine with wound healing properties. Front Pharmacol 13:885484. https://doi.org/10.3389/fphar.2022.885484
Li J, Luo J, Chai Y et al (2021) Hypoglycemic effect of Taraxacum officinale root extract and its synergism with Radix Astragali extract. Food Sci Nutr 9(4):2075–2085. https://doi.org/10.1002/fsn3.2176
Luo X, Huang P, Yuan B et al (2016) Astragaloside IV enhances diabetic wound healing involving upregulation of alternatively activated macrophages. Int Immunopharmacol 35:22–28. https://doi.org/10.1016/j.intimp.2016.03.020
Zhao B, Zhang X, Han W et al (2017) Wound healing effect of an Astragalus membranaceus polysaccharide and its mechanism. Mol Med Rep 15(6):4077–4083. https://doi.org/10.3892/mmr.2017.6488
Peng LH, Chen X, Chen L et al (2012) Topical astragaloside IV-releasing hydrogel improves healing of skin wounds in vivo. Biol Pharm Bull 35(6):881–888. https://doi.org/10.1248/bpb.35.881
He X, Wang X, Fang J et al (2017) Bletilla striata: Medicinal uses, phytochemistry and pharmacological activities. J Ethnopharmacol 195:20–38. https://doi.org/10.1016/j.jep.2016.11.026
Zhao Y, Wang Q, Yan S et al (2021) Bletilla striata polysaccharide promotes diabetic wound healing through inhibition of the NLRP3 inflammasome. Front Pharmacol 12:659215. https://doi.org/10.3389/fphar.2021.659215
Zhang P, He L, Zhang J et al (2020) Preparation of novel berberine nano-colloids for improving wound healing of diabetic rats by acting Sirt1/NF-kappaB pathway. Colloids Surf B Biointerfaces 187:110647. https://doi.org/10.1016/j.colsurfb.2019.110647
Xu N, Wang L, Guan J et al (2018) Wound healing effects of a Curcuma zedoaria polysaccharide with platelet-rich plasma exosomes assembled on chitosan/silk hydrogel sponge in a diabetic rat model. Int J Biol Macromol 117:102–107. https://doi.org/10.1016/j.ijbiomac.2018.05.066
Xia S, Weng T, Jin R et al (2022) Curcumin-incorporated 3D bioprinting gelatin methacryloyl hydrogel reduces reactive oxygen species-induced adipose-derived stem cell apoptosis and improves implanting survival in diabetic wounds. Burns Trauma 10:tkac001. https://doi.org/10.1093/burnst/tkac001
Rodriguez-Acosta H, Tapia-Rivera JM, Guerrero-Guzman A et al (2022) Chronic wound healing by controlled release of chitosan hydrogels loaded with silver nanoparticles and calendula extract. J Tissue Viability 31(1):173–179. https://doi.org/10.1016/j.jtv.2021.10.004
Gao SQ, Chang C, Li JJ et al (2018) Co-delivery of deferoxamine and hydroxysafflor yellow A to accelerate diabetic wound healing via enhanced angiogenesis. Drug Deliv 25(1):1779–1789. https://doi.org/10.1080/10717544.2018.1513608
Liu J, Qu M, Wang C et al (2022) A dual-cross-linked hydrogel patch for promoting diabetic wound healing. Small 18(17):e2106172. https://doi.org/10.1002/smll.202106172
Wang T, Liao Q, Wu Y et al (2020) A composite hydrogel loading natural polysaccharides derived from Periplaneta americana herbal residue for diabetic wound healing. Int J Biol Macromol 164:3846–3857. https://doi.org/10.1016/j.ijbiomac.2020.08.156
Shukla R, Kashaw SK, Jain AP et al (2016) Fabrication of Apigenin loaded gellan gum-chitosan hydrogels (GGCH-HGs) for effective diabetic wound healing. Int J Biol Macromol 91:1110–1119. https://doi.org/10.1016/j.ijbiomac.2016.06.075
Gan J, Liu C, Li H et al (2019) Accelerated wound healing in diabetes by reprogramming the macrophages with particle-induced clustering of the mannose receptors. Biomaterials 219:119340. https://doi.org/10.1016/j.biomaterials.2019.119340
Veerasubramanian PK, Thangavel P, Kannan R et al (2018) An investigation of konjac glucomannan-keratin hydrogel scaffold loaded with Avena sativa extracts for diabetic wound healing. Colloids Surf B Biointerfaces 165:92–102. https://doi.org/10.1016/j.colsurfb.2018.02.022
Gharaboghaz MNZ, Farahpour MR, Saghaie S (2020) Topical co-administration of Teucrium polium hydroethanolic extract and Aloe vera gel triggered wound healing by accelerating cell proliferation in diabetic mouse model. Biomed Pharmacother 127:110189. https://doi.org/10.1016/j.biopha.2020.110189
Ponrasu T, Veerasubramanian PK, Kannan R et al (2018) Morin incorporated polysaccharide-protein (psyllium-keratin) hydrogel scaffolds accelerate diabetic wound healing in Wistar rats. RSC Adv 8(5):2305–2314. https://doi.org/10.1039/c7ra10334d
Tottoli EM, Dorati R, Genta I et al (2020) Skin wound healing process and new emerging technologies for skin wound care and regeneration. Pharmaceutics 12(8):735. https://doi.org/10.3390/pharmaceutics12080735
Zhao L, Niu L, Liang H et al (2017) pH and glucose dual-responsive injectable hydrogels with insulin and fibroblasts as bioactive dressings for diabetic wound healing. ACS Appl Mater Interfaces 9(43):37563–37574. https://doi.org/10.1021/acsami.7b09395
Zhu Y, Zhang J, Song J et al (2019) A multifunctional pro-healing zwitterionic hydrogel for simultaneous optical monitoring of pH and glucose in diabetic wound treatment. Adv Funct Mater 30(6):1905493. https://doi.org/10.1002/adfm.201905493
Dong M, Mao Y, Zhao Z et al (2022) Novel fabrication of antibiotic containing multifunctional silk fibroin injectable hydrogel dressing to enhance bactericidal action and wound healing efficiency on burn wound: in vitro and in vivo evaluations. Int Wound J 19(3):679–691. https://doi.org/10.1111/iwj.13665
Shi M, Zhang H, Song T et al (2019) Sustainable dual release of antibiotic and growth factor from pH-responsive uniform alginate composite microparticles to enhance wound healing. ACS Appl Mater Interfaces 11(25):22730–22744. https://doi.org/10.1021/acsami.9b04750
Liang Y, Zhao X, Hu T et al (2019) Mussel-inspired, antibacterial, conductive, antioxidant, injectable composite hydrogel wound dressing to promote the regeneration of infected skin. J Colloid Interface Sci 556:514–528. https://doi.org/10.1016/j.jcis.2019.08.083
Galkowska H, Wojewodzka U, Olszewski WL (2006) Chemokines, cytokines, and growth factors in keratinocytes and dermal endothelial cells in the margin of chronic diabetic foot ulcers. Wound Repair Regen 14(5):558–565. https://doi.org/10.1111/j.1743-6109.2006.00155.x
Zarei F, Negahdari B, Eatemadi A (2018) Diabetic ulcer regeneration: stem cells, biomaterials, growth factors. Artif Cells Nanomed Biotechnol 46(1):26–32. https://doi.org/10.1080/21691401.2017.1304407
Xiong Y, Chen L, Liu P et al (2022) All-in-One: multifunctional hydrogel accelerates oxidative diabetic wound healing through timed-release of exosome and fibroblast growth factor. Small 18(1):e2104229. https://doi.org/10.1002/smll.202104229
Jeong S, Kim B, Park M et al (2020) Improved diabetic wound healing by EGF encapsulation in gelatin-alginate coacervates. Pharmaceutics 12(4):334. https://doi.org/10.3390/pharmaceutics12040334
Huang L, Shi Y, Li M et al (2021) Plasma exosomes loaded ph-responsive carboxymethylcellulose hydrogel promotes wound repair by activating the vascular endothelial growth factor signaling pathway in type 1 diabetic mice. J Biomed Nanotechnol 17(10):2021–2033. https://doi.org/10.1166/jbn.2021.3165
Banerjee A, Koul V, Bhattacharyya J (2021) Fabrication of in situ layered hydrogel scaffold for the co-delivery of PGDF-BB/Chlorhexidine to regulate proinflammatory cytokines, growth factors, and MMP-9 in a diabetic skin defect albino rat model. Biomacromol 22(5):1885–1900. https://doi.org/10.1021/acs.biomac.0c01709
Yang X, Yang R, Chen M et al (2020) KGF-2 and FGF-21 poloxamer 407 hydrogel coordinates inflammation and proliferation homeostasis to enhance wound repair of scalded skin in diabetic rats. BMJ Open Diabetes Res Care 8(1):e001009. https://doi.org/10.1136/bmjdrc-2019-001009
Lan B, Zhang L, Yang L et al (2021) Sustained delivery of MMP-9 siRNA via thermosensitive hydrogel accelerates diabetic wound healing. J Nanobiotechnology 19(1):130. https://doi.org/10.1186/s12951-021-00869-6
da Silva LP, Santos TC, Rodrigues DB et al (2017) Stem cell-containing hyaluronic acid-based spongy hydrogels for integrated diabetic wound healing. J Invest Dermatol 137(7):1541–1551. https://doi.org/10.1016/j.jid.2017.02.976
Wang H, Sun D, Lin W et al (2023) One-step fabrication of cell sheet-laden hydrogel for accelerated wound healing. Bioact Mater 28:420–431. https://doi.org/10.1016/j.bioactmat.2023.06.005
Wu X, Zhu H, Che J et al (2023) Stem cell niche-inspired microcarriers with ADSCs encapsulation for diabetic wound treatment. Bioact Mater 26:159–168. https://doi.org/10.1016/j.bioactmat.2023.02.031
Shang L, Yu Y, Jiang Y et al (2023) Ultrasound-augmented multienzyme-like nanozyme hydrogel spray for promoting diabetic wound healing. ACS Nano 17(16):15962–15977. https://doi.org/10.1021/acsnano.3c04134
Qi X, Cai E, Xiang Y et al (2023) An immunomodulatory hydrogel by hyperthermia-assisted self-cascade glucose depletion and ROS scavenging for diabetic foot ulcer wound therapeutics. Adv Mater 35(48):e2306632. https://doi.org/10.1002/adma.202306632
Wenlong Li, Haoxiang C, Jingfeng C et al (2023) Poly(pentahydropyrimidine)-based hybrid hydrogel with synergistic antibacterial and pro-angiogenic ability for the therapy of diabetic foot ulcers. Adv Funct Mater 33:2303147. https://doi.org/10.1002/adfm.202303147
Yang JM, Yang JH, Huang HT (2014) Chitosan/polyanion surface modification of styrene-butadiene-styrene block copolymer membrane for wound dressing. Mater Sci Eng C Mater Biol Appl 34:140–148. https://doi.org/10.1016/j.msec.2013.09.001
Cidreira ACM, de Castro KC, Hatami T et al (2021) Cellulose nanocrystals-based materials as hemostatic agents for wound dressings: a review. Biomed Microdevices 23(4):43. https://doi.org/10.1007/s10544-021-00581-0
Varaprasad K, Jayaramudu T, Kanikireddy V et al (2020) Alginate-based composite materials for wound dressing application: A mini review. Carbohydr Polym 236:116025. https://doi.org/10.1016/j.carbpol.2020.116025
Fletcher J (2003) The benefits of using hydrocolloids. Nurs Times 99(21):57
PubMed Google Scholar
Graca MFP, Miguel SP, Cabral CSD et al (2020) Hyaluronic acid-Based wound dressings: a review. Carbohydr Polym 241:116364. https://doi.org/10.1016/j.carbpol.2020.116364
Chen Y, Wang X, Tao S et al (2023) Research advances in smart responsive-hydrogel dressings with potential clinical diabetic wound healing properties. Mil Med Res 10(1):37. https://doi.org/10.1186/s40779-023-00473-9
Qi X, Xiang Y, Cai E et al (2023) Inorganic–organic hybrid nanomaterials for photothermal antibacterial therapy. Coord Chem Rev 496:215426. https://doi.org/10.1016/j.ccr.2023.215426
Gao L, Li C, Huang W et al (2020) MXene/polymer membranes: synthesis, properties, and emerging applications. Chem Mater 32(5):1703–1747. https://doi.org/10.1021/acs.chemmater.9b04408
Nunan R, Harding KG, Martin P (2014) Clinical challenges of chronic wounds: searching for an optimal animal model to recapitulate their complexity. Dis Model Mech 7(11):1205–1213. https://doi.org/10.1242/dmm.016782
Download references
Acknowledgements
This study was sponsored by the National Natural Science Fund (NO:81903994), Youth Development of the First Affiliated Hospital of Anhui Medical University (NO:2793), the Key projects of the clinical research of the First Affiliated Hospital of Anhui Medical University (NO: LCYJ2021ZD005), the Peak Discipline Construction Project of School of Public Health, Anhui Medical University (2021, 2022), Anhui Medical University College Students Innovation and Entrepreneurship Project (Provincial Project, 2022).
Author information
Authors and affiliations.
Department of Chinese Medicine, The First Affiliated Hospital of Anhui Medical University, No. 218, Jixi Road, Shushan District, Hefei, 230032, Anhui, People’s Republic of China
Jie Zhao & Yuxin Hu
Department of Chinese Integrative Medicine, Anhui Medical University, No. 80, Meishan Road, Shushan District, Hefei, 230032, Anhui, People’s Republic of China
Institute for Medical Virology, Goethe University Frankfurt Am Main, 60596, Frankfurt, Germany
Department of Burns, The First Affiliated Hospital of Anhui Medical University, Hefei, 230022, Anhui, People’s Republic of China
Wanxuan Hu & Yexiang Sun
School of Public Health, Anhui Medical University, Hefei, 230032, Anhui, People’s Republic of China
Anhui Engineering Research Center for Medical Micro-Nano Devices, School of Biomedical Engineering, Anhui Provincial Institute of Translational Medicine, Anhui Medical University, Hefei, 230011, People’s Republic of China
Haisheng Qian
You can also search for this author in PubMed Google Scholar
Contributions
The authors’ responsibilities were as follows: Jie zhao completed the collection and analysis of relevant literature and the preparation of the first draft of the thesis; Jie liu participated in graphics. Yuxin Hu and Wanxuan Hu participated in the analysis and collation of the literature. Juan Wei, Haisheng Qian and Yexiang Sun are the project creators and principals, and Yexiang Sun critically revised the manuscript for intellectual content, guiding the paper writing. All authors read and agreed to the final text.
Corresponding authors
Correspondence to Jie Zhao , Juan Wei , Haisheng Qian or Yexiang Sun .
Ethics declarations
Competing interest.
The authors report no declarations of interest.
Ethics approval and consent to participate
Consent for publication, additional information.
Handling Editor: Annela M. Seddon.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Zhao, J., Liu, J., Hu, Y. et al. Research advances in hydrogel-based wound dressings for diabetic foot ulcer treatment: a review. J Mater Sci 59 , 8059–8084 (2024). https://doi.org/10.1007/s10853-024-09493-9
Download citation
Received : 04 December 2023
Accepted : 08 February 2024
Published : 05 May 2024
Issue Date : May 2024
DOI : https://doi.org/10.1007/s10853-024-09493-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Advertisement
- Find a journal
- Publish with us
- Track your research
- Research article
- Open access
- Published: 20 March 2020
Diabetic foot care: knowledge and practice
- Aydin Pourkazemi 1 ,
- Atefeh Ghanbari ORCID: orcid.org/0000-0002-7949-5717 2 ,
- Monireh Khojamli 1 ,
- Heydarali Balo 1 ,
- Hossein Hemmati 1 ,
- Zakiyeh Jafaryparvar 1 &
- Behrang Motamed 3
BMC Endocrine Disorders volume 20 , Article number: 40 ( 2020 ) Cite this article
35k Accesses
50 Citations
1 Altmetric
Metrics details
Diabetic foot ulcers (DFUs) are common problems in diabetes. One of the most important factors affecting the quality of diabetes care is knowledge and practice. The current study aimed at determining the knowledge and practice of patients with diabetes regarding the prevention and care of DFUs.
The current analytical, cross sectional study was conducted in Guilan Province (north of Iran) on 375 patients registered in the medical records as type 2 diabetes mellitus. Demographic characteristics, knowledge, and practice of participants were recorded in a questionnaire during face-to-face interviews conducted by the researcher. Descriptive and inferential statistics were performed using SPSS version18.
The mean score of knowledge was 8.63 ± 2.5 out of 15, indicating that the majority of participants had a poor knowledge (84.8%). The mean practice score was 7.6 ± 2.5 out of 15, indicating that a half of them had poor performance (49.6%). There was a significant and direct correlation between knowledge and practice. Knowledge level, place of residence, marital status, and history of admission due to diabetic foot were predictors of practice score.
Conclusions
According to the low level of knowledge and practice in patients with diabetes regarding the prevention and care of DFUs, and considering the significant relationship of some demographics of patients with knowledge and practice scores, a targeted educational program is needed to promote knowledge of patients with diabetes.
Peer Review reports
What is already known about this subject?
Diabetes accounted for 1.3 million deaths (2.4% of all death). The prevalence of diabetes varies among countries in Eastern Mediterranean Region (EMR).
Prevalence of diabetes mellitus in Iran ranged 20 to 30% in different provinces with higher frequency among females from 1990 to 2013.
Among people living with diabetes mellitus, 20% are at risk for foot ulceration as a result of neuropathy.
Diabetic foot ulcers (DFUs) are one of most common diabetes complications with 0–4% prevalence.
Good knowledge and practice regarding DFU reduces the risk of diabetic foot complications and ultimately amputation.
What are the new findings?
- In the current study, 84.8% of the participants had poor knowledge and only 8.8% had good practice. There was a direct and significant correlation between knowledge and practice.
The lowest knowledge scores belonged to the use of talcum powder or other powders and not using lotions between the toes.
The strongest variables related to practice were knowledge, place of residence, marital status, and history of admission due to diabetic foot, indicating that these four variables were the predictors of practice score.
How might this impact on clinical practice in the foreseeable future?
Patients’ knowledge about foot ulcer prevention should be promoted based on guidelines both in community and hospitals.
Adherence to guidelines prevents DFU; targeted interventions directed toward patients/health care providers can lead to reduced DFU complications.
Diabetes mellitus is a group of common metabolic disease characterized by hyperglycemia. Due to multiple and prolonged complications, diabetes affects almost all systems of the body [ 1 ]. Diabetes caused 1.3 million deaths (2.4% of all death) and 56 million disability adjusted life years (DALYs) in 2013. The diabetes DALY rate increased from 589.9 per 100,000 in 1990 to 883.5 per 100,000 populations in 2013. Total DALYs from diabetes increased by 148.6% during 1990–2013; population growth accounted for a 62.9% increase, and aging and increase in age-specific DALY rates accounted for 31.8 and 53.9%, respectively [ 2 ]. The prevalence of diabetes varies among countries in EMR. In Saudi Arabia, the prevalence of diabetes was reported 13.4% Saudis aged 15 years or older [ 3 ] and in Pakistan 12.1% for males and 9.8% for females aged ≥25 years [ 2 ]. A systematic review on the prevalence of type 2 diabetes in Iran showed a range of 3 to 20% in different provinces [ 4 ].
Of people living with diabetes, 20% are at high risk of foot ulceration as a result of neuropathy [ 5 ]. Diabetic foot ulcers (DFU S ) comprise 12–15% of total estimated cost of diabetes in the developed countries, increasing to 40% in the developing countries [ 6 ]. DFUs are one of the most common diabetes complications with 4 to 10% prevalence in the affected population [ 7 ]. The overall incidence of DFU is 5.8–6.0% in some particular diabetic in the U. S, while it is 2.1–2.2% in smaller populations in Europe [ 8 ]. Treating foot ulcers can be expensive and it is evident that about 49–85% of all DFU S can be prevented by raising awareness and taking proper measures [ 7 ]..
Among the complications of diabetes, DFU S affects the patient’s quality of life in case of amputation. However, it is possible to prevent amputation using educational and care strategies [ 9 ]. Data show that 25% of patients with diabetes develop a foot ulcer in their lifetime and that the cost of treating a DFU S is more than twice that of any other chronic ulcer [ 10 ]. Diabetic foot amputation remains an unpleasant impact on patients’ life more than other complications [ 11 , 12 ]. Delays in referral of serious foot problems are of particular concern [ 5 ]. Ndosi et al., reported that 15.1% of patients died within the year of presentation, the ulcer had healed in 45.5%, but recurred in (9.6%). Participants with a single ulcer on their index foot had a higher incidence of healing than those with multiple ulcers (hazard ratio 1.90, 95% CI 1.18 to 3.06) [ 13 ].
Understanding the level of knowledge and practice in patients with diabetes is important in planning for the better control of diabetes and its complications. A study by Ahmad and Ahmad on 124 patients with diabetes in North India reported that 60.5 and 79.0% got lower scores in knowledge and practice toward diabetes, respectively [ 14 ]. Jackson IL et al., reported that 79.5% of patients with diabetes in Nigeria had more than 70% of overall knowledge about self-care [ 15 ]. The results of a study in Malaysia showed that the most patients (58%) had poor knowledge and 61.8% of them had poor practice of foot care [ 16 ].
Among diabetes complications, the foot ulcers are considered as the most preventable ones. Risk factors of DFU S are correlated with poor practices and knowledge. Good knowledge and practice toward diabetic foot care reduces the risk of diabetic foot complications and ultimately amputation [ 7 ]. According to American Diabetes Association, annual assessments of knowledge, skills and behaviors are necessary for patients with diabetes [ 15 ].. The current study was conducted to assess patients’ knowledge and practice toward diabetic foot care. No similar study is conducted in Rasht City (the capital of Guilan Province, Northern Iran) thus far; therefore, the present study aimed at evaluating the level of practice and knowledge toward foot care in patients with type 2 diabetes mellitus. Health system can prevent DFU and amputation by applying a strategy to raise knowledge in patients.
Study design and subjects
The current analytical, cross sectional study was conducted at a clinic in Razi Hospital, affiliated to Guilan University of Medical Sciences, which is the only endocrine disease referral center across the province. Data were gathered from May to July 2017 and the subjects were selected by consecutive sampling. To Diagnostic and classify the patients, the American Diabetic Association, the diagnostic criteria were utilized [ 17 ]. Patients with diabetes receive care, education, treatment, and other services at this center. The center also delivers healthcare services to outpatients and inpatients, as well as routine training. The research project was approved by the Deputy of Research, Guilan University of Medical Sciences. Participation in the study was voluntarily and the subjects were informed about their right to withdraw from the study at any stage. The participant’s privacy was respected, and data were kept confidential and utilized for study purposes only. Participants were asked to read and sign an informed consent form. Inclusion criteria were: receiving the diagnosis of type 2 diabetes mellitus, age 18 years or above, taking anti-diabetic medications for at least 1 month prior to the study, having clinical records at the center, and willing to participate in the study. The exclusion criteria were: critically ill patients with diabetes, pregnant or newly diagnosed (less than 1 month) patients, receiving any other treatment or therapy, and having major psychiatric problems. A structured datasheet was used to collect demographic and clinical information of the patients using paper-based and digital records archives. Some information was also collected by a medical student through face-to-face interviews. A paper-based questionnaire was distributed among both outpatients and inpatients. Wagner DFU classification system was used to classify the patients based on ulcers. In this hospital, we assessed peripheral neuropathy, retinopathy and peripheral vascular disease (PVD), respectively by using monofilament testing, optometrist or ophthalmologist reports and the clinical diagnosis documented by the surgeon or, if available, images taken through arterial Doppler or angiography. Macro vascular disease was defined as any macro vascular complications other than PVD including prior myocardial infarction, angioplasty, coronary artery bypass grafting, ischemic heart disease, or stroke [ 18 ].
In the current study, having one or two more complications was considered a positive condition. The sample size was determined 375 considering 95% confidence interval with d = 0.05 and P = 0.58. A total of 375 out of 395 distributed questionnaires were completed and returned; the response rate was 94.4%.
A three-section questionnaire was used in the current study. First section included demographic characteristics such as age, gender, and duration of diabetes mellitus, place of residence, occupation, and level of education, marital status, and body mass index. Second part consisted of 15 questions about knowledge scored based on nominal (yes/no/I don’t know) scale, and third part with 15 questions focusing on practice was scored based on “yes/no” scale. The questionnaire was used to measure the level of knowledge and practice of subjects toward diabetic foot care. Patients’ demographic data were collected to analyze factors associated with knowledge and practice toward diabetic foot care. Each correct answer was given 1 point; however, wrong answers or choosing “I don’t know” option was given 0 point. The total score for each part ranged 0 to 15. Good or poor level of knowledge was determined based on the 75% of the maximum score of the questionnaire; therefore, the scores higher than 11.25 were considered good and those lower than 11.25 were considered poor. Examples of the questions included “Do you care about your diabetes?”; “Do you wash your feet every day?”; “Do you check the water temperature before using it?” and “Do you dry your feet after washing?”
The questionnaire was translated into the Persian language. Following the translations conducted by an Iranian professor of English literature, a native bilingual English speaker translated it back into English. Content validity was determined by gathering the views of 15 medical and nursing professionals after reviewing the questionnaire. Content validity ratio (CVR) and content validity index (CVI) of the questionnaire were assessed. Mean scores of CVI and CVR were higher than 0.80. Cronbach’s α coefficients were computed to evaluate reliability of knowledge and practice, which were 0.80 and 0.85, respectively.
Statistical analysis
After collecting data, descriptive statistics (frequency, mean, and standard deviation) were employed to summarize patients’ socio-demographic data and Chi-square test to investigate association between predictors (factors) and knowledge and practice level. In order to assess the differences between groups, the Wilcoxon, Mann-Whitney, and Kruskal-Willis tests were used for continuous variables. Factors related to knowledge and practice was estimated by multiple regressions. In this research, wrong answers and “I don’t know” merged as poor awareness. In order to assess the relationship between individual variables with knowledge and practice, we had to integrate these two items in order to have a better analysis. Variables with a P -value of < 0.1 were included in the multi-variate models. P -value < 0.05 was considered as the level of significance. All analyses were performed using SPSS version 18.
The mean (± SD) age of the 375 participants was 55.4 (±12.9) years, and 56.4% were female. Majority of patients had diabetes for less than 10 years (54.1%), were female (56.5%), urban residents (62.1%), illiterate or had elementary education (73.1%), did not have normal BMI (69.8%), and (10.6%) patients had 2 and more complications (Table 1 ). In terms of knowledge, only 57 participants (15.2%) had good knowledge, most of them (84.8%) had poor knowledge, and the mean score of patients’ knowledge was 8.63 ± 2.65. The highest percentage of correct answers was found with the knowledge about “The need for meeting or consulting a physician, if there were signs of wounding” (88.8%), followed by “Not walking without shoes” (83.5%) and “Washing and changing socks” (9.81%). The lowest knowledge was about “The use of talcum powder or other powders between the toes” (3.5%), followed by “Not using lotion between the toes” (22.24%), and “The proper method of trimming the toenails” (23.2%).
In terms of practice, only 33 patients (8.8%) had a good practice; most of them (91.2%) had a poor practice (Table 2 ), and the mean score of patients’ practice was 7.6 (± 2.5). The participants reported their best practice toward “Importance of diabetes control” (80.5%), followed by “Meeting or consulting a physician, in case of signs of DFU” (79.2%). The poorest practice was toward “The use of talcum powder between the toes” (2.7%), followed by “Proper method of trimming the toenails” (25.9%), and “Keeping the foot skin soft” (30.9%).
There was a direct and significant correlation between knowledge and practice ( P < 0.0001, r < 0.8) (Fig. 1 ). There was a significant relationship between knowledge score and gender, duration of diabetes, occupation, level of education, place of residence, having DFU, hospital stay history, and amputation history.

Correlation Between Khowledge and Practice
The study results showed that patients with more than 10 years history of diabetes, history of DFU, history of hospital stay or experience of lower limb amputation due to DFU, female gender, and the ones with complications had higher knowledge ( P < 0.05).
There was a significant correlation between practice score and gender, duration of diabetes, occupation, level of education, and place of residence (P < 0.05) (Table 3 ).
Also, based on multiple regression, the strongest variables related to practice were knowledge score ( P < 0.0001), place of residence ( P < 0.03), marital status ( P = 0.008), and DFU ( P = 0.02), indicating that these four variables were the predictors of foot care practices in the current study (Table 4 ).
In the current study, majority of patients with diabetes had lower levels of education. Studies report that level of knowledge depends on the level of education [ 14 , 19 ]. Understanding this variable is highly important in designing strategies to prevent diabetes.
In the current study, most patients had lower scores of knowledge and practice toward foot care, and the mean practice score was lower than the mean knowledge score, which was similar to the findings of Muhammad-Lutfi’s and Kim’s studies [ 16 , 20 ]. A study conducted on patients with diabetes in Western Nepal reported poor KAP (knowledge, attitude and practices) score; they indicated that the plausible factors could be lack of knowledge, lack of information, and literacy level of the studied population [ 21 ]. Another study on young Saudi females with diabetes also reported poor KAP scores [ 19 ]. Some studies reported that patients with diabetes had good level of knowledge about diabetes [ 7 , 16 , 22 , 23 ]. The differences in knowledge about foot care among patients with diabetes across the studies could be due to different trainings on diabetes care provided by the health care professionals in different settings [ 23 ] and also the literacy level of the studied subjects.
Several studies reported poor foot care practices among patients with diabetes. Kheir et al., reported poor practices toward regular inspection of feet among patients in Qatar [ 24 ]. Hamidah et al., from Malaysia observed that 28.4% of patients newly diagnosed with diabetes practiced good habits towards foot care [ 25 ]. Desalu et al., from Nigeria observed that only 10.2% of patients with diabetes had good foot care practices [ 26 ]. It was difficult to compare the results of the current study with those of other studies since the nature of the study populations and the applied measurements were different.
In the current study, there was a direct and significant correlation between knowledge and practice scores; therefore, with an increase in the knowledge score, the practice score also increased. Other studies also showed that patients who receive trainings on foot care checked their feet regularly [ 20 ]. Patients who are advised to take care of their feet and the ones whose feet are regularly checked by physicians have better practices toward foot care [ 27 ].
In the current study, the lowest knowledge scores were regarding the application of talcum powder or other powders and not using lotions between the toes, and the proper way of trimming the toenails; while the lowest practice scores were related to the application of talcum powder between the toes, the proper way of trimming the toenails; keeping the foot skin soft, and avoid dryness.
It should also be noted that due to wet climate in the North of Iran, use of lotion between the toes is not common. Nevertheless, it also needs training. Patients with diabetes need to keep between their toes dry using talcum powder and avoid the application of lotion since it is important as a hygienic measure for feet in preventing fungal infection [ 28 ]. Patients should also use skin moisturizers daily to keep the skin of their feet soft and should trim their toenails straight across (not rounded) to prevent damage to their toes [ 29 ].
In the current study, gender, duration of disease, occupation, place of residence, level of education, having DFU, and a history of hospitalization, amputation, and complication had significant relationships with knowledge. Also, gender, duration of disease, place of residence, occupation, and level of education had significant relationships with practice. It was found that knowledge level was higher in females, patients with a diabetes history of more than 10 years, and the ones underwent amputation due to DFU compared to the others; in addition, females, patients with a diabetes history of more than 10 years, and urban residents had better performance. The current study results showed that males were usually reluctant to disclose their health problems and seek professional care. Also, males presented greater deficit in self-care compared to females [ 30 ].
In the study by Muhammad-Lotfi, age, gender, level of education, and duration of diabetes had no significant relationship with knowledge and practice. This finding was in agreement with that of the current study [ 16 ], but another study indicated a significant relationship between the level of education and knowledge [ 31 ].
People with higher education are expected to be more likely to read and receive information about their illness and foot care and understand the information provided by medical staff in health care settings.
But in the current study, there was no significant relationship between the level of education and knowledge or practice, which could be due to the poor and inadequate resources of information about diabetes at the community level, since both educated and uneducated groups had inadequate information. It may also be due to the fact that in spite of possessing knowledge, due to the lack of time, heavy work load, and lack of adequate insurance coverage, patients could not take good care of their feet in practice, which requires more studies to root out the causes.
Nevertheless, the attitude of patients toward self-care in addition to sufficient knowledge was not studied in the current study. As observed in the present study, patients with a history of DFU or hospital stay, and even amputation and complication had higher knowledge level. It could be due to the fact that while completing the questionnaire, the current knowledge level of the subjects was questioned, which indicated that training medical centers can raise the level of knowledge in patients with DFU. In many Iranian state hospitals, diabetic training programs are not well organized, and the existing programs are weak. It is believed that knowledge about diabetes in the general population as well as patients with diabetes in Iran is not enough and there is a dire need for a good program for diabetes [ 32 ].
The collected data indicated that patients with diabetes had poor practice and knowledge about foot care. This is basically due to lack of proper communication between patients and medical team and inadequate education. Based on nurses’ opinion, recommendations and guidelines play an effective role in prevention, treatment, and reduction of complication among patients with DFU. Therefore, adaptation, implementation, and evaluation of the educational programs were recommended [ 33 ].
Thus, patients should be trained for foot ulcer prevention based on clinical practice guidelines for diabetes mellitus both in the community and hospitals. The results of the current study encouraged a positive outlook: A diabetes educator should give necessary advices to patients during every visit, in order to improve their perception about disease, diet, and lifestyle changes and help them control their glycemic level and overcome the complications of diabetes.
According to the principle of “prevention is better than cure” and considering the predictive factors in the current study including poor knowledge, urban residency, being single, and lack of DFU, more attention should be paid to patients possessing risk factors .
Knowledge and practice toward foot care were poor in most patients with diabetes. There was a significant relationship between some demographic characteristics of patients and knowledge and practice toward foot care. The level of knowledge, place of residence, marital status, and history of hospital stay due to DFU were the predictors of practice in patients with diabetes.
The strength of the current study was that it was the first, study to discuss this important issue in Guilan Province. The study also had some limitations; first, since the work had a cross sectional design, the direction of relationships and causal relationships cannot be determined. Second, the result of the study should be interpreted with caution, since they were obtained from a single center; a clinic-based study. Hospital-based studies cannot provide a true picture of knowledge and practice in the community. The current study sample did not represent the whole Iranian population consisting of several ethnicities. In this research, responses of the wrong answers and “I don’t know” have been grouped together, in order to achieve better analysis. Perhaps with increasing sample size, we could solve this problem in future studies.
Adequate knowledge and good practices are important to effectively control diabetes mellitus. Patients require continuous support of family members and community in order to modify their lifestyle and behaviors and make sustainable changes in order to better control their diabetes disease. Also, education about diabetes mellitus and its risk factors should be provided through mass media in order to effectively control it in the community.
Availability of data and materials
The datasets used and /or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Content validity index
Content validity ratio
Diabetic foot ulcers
Eastern Mediterranean Region
World health organization
Janmohammadi N, Moazzezi Z, Ghobadi P, et al. Evaluation of the risk factors of diabetic foot ulcer and its treatment in diabetic patients, Babol, North of Iran. Iranian J Endocrinol Metab. 2010;11(2):121–5. https://doi.org/10.1155/2018/7631659 .
Article Google Scholar
Moradi-Lakeh M, Forouzanfar MH, El Bcheraoui C, et al. High fasting plasma glucose, diabetes, and its risk factors in the eastern mediterranean region, 1990–2013: findings From the Global Burden of Disease Study 2013. Diabetes Care. 2017;40(1):22–9. https://doi.org/10.2337/dc16-1075 Epub 2016 Oct 26.
Article PubMed Google Scholar
Bcheraoui C, Basulaiman M, Tuffaha M, et al. Status of the diabetes epidemic in the kingdom of Saudi Arabia, 2013. Int J Public Health. 2014;59:1011–21.
Haghdoost AA, Rezazadeh-Kermani M, Sadghirad B, Baradaran HR. Prevalence of type 2 diabetes in the Islamic Republic of Iran: systematic review and meta-analysis. East Mediterr Health J. 2009;15:591–9.
Article CAS Google Scholar
Paisey R, Abbott A, Levenson R, et al. Diabetes-related major lower limb amputation incidence is strongly related to diabetic foot service provision and improves with enhancement of services: peer review of the south-west of England. Diabet Med. 2018;35(1):53–62. https://doi.org/10.1111/dme.13512 Epub 2017 Oct 11.
Article CAS PubMed Google Scholar
Solan YM, Kheir HM, Mahfouz MS, et al. Diabetic Foot Care: Knowledge and Practice. J Endocrinol Metab. 2017;6(6):172–7. https://doi.org/10.14740/jem388e .
Haq NU, Durrani P, Nasim A, et al. Assessment of Knowledge and Practice of Diabetes Mellitus Patients Regarding Foot Care in Tertiary Care Hospitals in Quetta, Pakistan. Specialty J Med Res Health Sci. 2017;2(4):35–43.
Google Scholar
Jeffcoate WJ, Boyko EJ, Vileikyte L, et al. Current Challenges and Opportunities in the Prevention and Management of Diabetic Foot Ulcers. Diabetes Care. 2018;41:645–52. https://doi.org/10.2337/dc17-1836 .
Morey-Vargas OL, Smith SA. Be Smart: Strategies for foot care and prevention of foot complications in patients with diabetes. Prosthet Orthot Int. 2015;39(1):48–60.
Hurlow JL, Hamphreys GI, Bowling FL, et al. Diabetic foot infection: a critical complication. Int Wound J. 2018:1–8. https://doi.org/10.1177/0309364614535622 .
Clarke P, Gray A, Holman R. Estimating utility values for health states of type 2 diabetic patients using the EQ-5D (UKPDS 62). Med Decis Mak. 2002;22(4):340–9. https://doi.org/10.1177/0272989X0202200412 .
Laiteerapong N, Karter AJ, Liu JY, et al. Correlates of quality of life in older adults with diabetes. Diabetes Care. 2011;34(8):1749–53. https://doi.org/10.2337/dc10-2424 Epub 2011 Jun 2.
Article PubMed PubMed Central Google Scholar
Ndosi M, Wright-Hughes A, Brown S, et al. Prognosis of the infected diabetic foot ulcer: a 12-month prospective observational study. Diabet Med. 2018;35(1):78–88. https://doi.org/10.1111/dme.13537 Epub 2017 Nov 20.
Ahmad S, Ahmad MT. Assessment of knowledge, attitude and practice among diabetic patients attending a health care facility in North India. Indian J Basic Appl Med Res. 2015;4(3):501–9.
Jackson IL, Adibe MO, Okonta MJ, et al. Knowledge of self-care among type 2 diabetes patients in two states of Nigeria. Pharmacy Pract. 2014;12(3) PMID:25243026,PMCID:PMC4161403.
Muhammad-Lutfi A, Zaraihah M, Anuar-Ramdhan I. Knowledge and practice of diabetic foot care in an in-patient setting at a tertiary medical center. Malays Orthop J. 2014;8(3):22. https://doi.org/10.5704/MOJ.1411.005 .
Article CAS PubMed PubMed Central Google Scholar
American Diabetes Association. Classification and diagnosis of diabetes: standards of medical Care in Diabetes 2019. Diabetes Care. 2019;42(Suppl. 1):S13–28. https://doi.org/10.2337/dc19-S002 .
Jeyaraman K, Berhane T, Hamilton M, et al. Mortality in patients with diabetic foot ulcer: A retrospective study of 513 cases from a single Centre in the Northern Territory of Australia. BMC Endocr Disord. 2019;19:1. https://doi.org/10.1186/s12902-018-0327-2 .
Saadia Z, Rushdi S, Alsheha M, et al. A study of knowledge attitude and practices of Saudi women towards diabetes mellitus. A (KAP) study in Al-Qassim region. Internet J Health. 2010;11(2). https://doi.org/10.4236/jdm.2015.52014 .
Kim A, Hongsranagon P. Preventive behaviors regarding foot ulcers in diabetes type II patients at BMA health center no. 48, Bangkok, Thailand. J Health Res. 2008;22(suppl):21–8.
Gautam A, Bhatta DN, Aryal UR. Diabetes related health knowledge, attitude and practice among diabetic patients in Nepal. BMC Endocr Disord. 2015;15(1):25. https://doi.org/10.1186/s12902-015-0021-6 .
Saleh F, Mumu SJ, Ara F, et al. Knowledge and self-care practices regarding diabetes among newly diagnosed type 2 diabetics in Bangladesh: a cross-sectional study. BMC Public Health. 2012;12(1):1112. https://doi.org/10.1186/1471-2458-12-1112 .
Gul N. Knowledge, attitudes and practices of type 2 diabetic patients. J Ayub Med Coll Abbottabad. 2010;22(3):128–31 PMID: 22338437.
PubMed Google Scholar
Kheir N, Greer W, Yousif A, et al. Knowledge, attitude and practices of Qatari patients with type 2 diabetes mellitus. Int J Pharm Prac. 2011;19(3):185–91. https://doi.org/10.1111/j.2042-7174.2011.00118.x .
Hamidah H, Santhna L, Ruth RP, et al. Foot care strategy for the newly diagnosed DM Type 2 patients with low educational and socio-economic background: a step towards future. Clin Ter. 2012;163(6):473–8.
CAS PubMed Google Scholar
Desalu O, Salawu F, Jimoh A, et al. Diabetic foot care: self-reported knowledge and practice among patients attending three tertiary hospital in Nigeria. Ghana Med J. 2011;45(2):60–5 PMID: 21857723.
Bell RA, Arcury TA, Snively BM, et al. Diabetes foot self-care practices in a rural, triethnic population. Diabetes Educ. 2005;31(1):75–83. https://doi.org/10.1177/0145721704272859 .
Aalami HB, Aalami HA, Siavashi B. Diabetic foot ulcer management review of literature. Iran J Surgery. 2009;16(4):1–7. https://doi.org/10.17795/jssc23312 .
Hasnain S, Sheikh NH. Knowledge and practices regarding foot care in diabetic patients visiting diabetic clinic in Jinnah hospital, Lahore. J Pak Med Assoc. 2009;59(10):687 PMID: 19813683.
Rossaneis MA, Haddad MD, Mathias T, et al. Differences in foot self-care and lifestyle between men and women with diabetes mellitus. Rev Lat Am Enfermagem. 2016;24:e2761. https://doi.org/10.1590/1518-8345.1203.2761 .
Chiwanga FS, Njelekela MA. Diabetic foot: prevalence, knowledge, and foot self-care practices among diabetic patients in Dar es Salaam, Tanzania–a cross-sectional study. J Foot Ankle Res. 2015;8(1):20. https://doi.org/10.1186/s13047-015-0080-y .
Delavari A, Alikhani S, Nili S, et al. Quality of care of diabetes mellitus type II patients in Iran. AIM . 2009;12(5):492–5 PMID: 19722773.
Ghanbari A, Rahmatpour P,Jafaraghaee et al .Quality assessment of Diabetic Foot ulcer clinical practice guildeline. J Evid Based Med .2018; 11(3):200–207. doi: https://doi.org/10.1111/jebm.12304 .
Download references
Acknowledgements
The authors wish to thank all the individuals who helped throughout the study, especially Razi Clinical Research Development Center.
The study was funded by the Deputy for Research; Guilan University of Medical Sciences. The funder had no role in the study design, data analysis and interpretation, and writing of the manuscript.
Author information
Authors and affiliations.
Razi Clinical Research Development unit, Guilan university of medical sciences, Rasht, Iran
Aydin Pourkazemi, Monireh Khojamli, Heydarali Balo, Hossein Hemmati & Zakiyeh Jafaryparvar
Social Determinants of Health Research center, nursing and midwifery school, Guilan University of medical sciences, Rasht, Iran
Atefeh Ghanbari
Department of internal medicine , Razi Hospital ,School of Medicine, Guilan university of Medical Sciences, Rasht, Iran
Behrang Motamed
You can also search for this author in PubMed Google Scholar
Contributions
PA, KM, and GA: the study design; PA,KM and MB: data collection; PA, KM, GA, HH, and BH: data analysis; PA, GA, KM, BH, HH, MB and JZ: data interpretation and drafting of the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Correspondence to Atefeh Ghanbari .
Ethics declarations
Ethics approval and consent to participate.
Written informed consent was obtained from participations and verbal consent from illiterate participants following a detailed explanation of the study objectives. The study was conducted in accordance with the ethical principles and its protocol was approved by the Ethics Committee of Guilan University of Medical Sciences (ethical code: IR.GUMS.REC.1396.8).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Pourkazemi, A., Ghanbari, A., Khojamli, M. et al. Diabetic foot care: knowledge and practice. BMC Endocr Disord 20 , 40 (2020). https://doi.org/10.1186/s12902-020-0512-y
Download citation
Received : 07 January 2019
Accepted : 25 February 2020
Published : 20 March 2020
DOI : https://doi.org/10.1186/s12902-020-0512-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Diabetic foot
- Diabetes mellitus
BMC Endocrine Disorders
ISSN: 1472-6823
- General enquiries: [email protected]
- How it works

Useful Links
How much will your dissertation cost?
Have an expert academic write your dissertation paper!
Dissertation Services
Get unlimited topic ideas and a dissertation plan for just £45.00
Order topics and plan
Get 1 free topic in your area of study with aim and justification
Yes I want the free topic
Latest List of Best Diabetes Dissertation Topics
Published by Owen Ingram at January 2nd, 2023 , Revised On May 17, 2024
The prevalence of diabetes among the world’s population has been increasing steadily over the last few decades, thanks to the growing consumption of fast food and an increasingly comfortable lifestyle. With the field of diabetes evolving rapidly, it is essential to base your dissertation on a trending diabetes dissertation topic that fills a gap in research.
Finding a perfect research topic is one of the most challenging aspects of dissertation writing in any discipline . Several resources are available to students on the internet to help them conduct research and brainstorm to develop their topic selection, but this can take a significant amount of time. So, we decided to provide a list of well-researched, unique and intriguing diabetes research topics and ideas to help you get started.
Other Subject Links:
- Evidence-based Practice Nursing Dissertation Topics
- Child Health Nursing Dissertation Topics
- Adult Nursing Dissertation Topics
- Critical Care Nursing Dissertation Topics
- Palliative Care Nursing Dissertation Topics
- Mental Health Nursing Dissertation Topics
- Nursing Dissertation Topics
- Coronavirus (COVID-19) Nursing Dissertation Topics
List of Diabetes Dissertation Topics
- Why do people recently diagnosed with diabetes have such difficulty accepting reality and controlling their health?
- What are the reactions of children who have recently been diagnosed with diabetes? What can be done to improve their grasp of how to treat the disease?
- In long-term research, people getting intensive therapy for the condition had a worse quality of life. What role should health professionals have in mitigating this effect?
- Why do so many individuals experience severe depression the months after their diagnosis despite displaying no other signs of deteriorating health?
- Discuss some of the advantages of a low-carbohydrate, high-fat diet for people with diabetes
- Discuss the notion of diabetes in paediatrics and why it is necessary to do this research regularly.
- Explain the current threat and difficulty of childhood obesity and diabetes, stressing some areas where parents are failing in their position as guardians to avoid the situation
- Explain some of the difficulties that persons with diabetes have, particularly when obtaining the necessary information and medical treatment
- Explain some of the most frequent problems that people with diabetes face, as well as how they affect the prevalence of the disease. Put out steps that can be implemented to help the problem.
- Discuss the diabetes problem among Asian American teens
- Even though it is a worldwide disease, particular ethnic groups are more likely to be diagnosed as a function of nutrition and culture. What can be done to improve their health literacy?
- Explain how self-management may be beneficial in coping with diabetes, particularly for people unable to get prompt treatment for their illness
- Discuss the possibility of better management for those with diabetes who are hospitalised
- What current therapies have had the most influence on reducing the number of short-term problems in patients’ bodies?
- How have various types of steroids altered the way the body responds in people with hypoglycemia more frequently than usual?
- What effects do type 1, and type 2 diabetes have on the kidneys? How do the most widely used monitoring approaches influence this?
- Is it true that people from specific ethnic groups are more likely to acquire heart disease or eye illness due to their diabetes diagnosis?
- How has the new a1c test helped to reduce the detrimental consequences of diabetes on the body by detecting the condition early?
- Explain the difficulty of uncontrolled diabetes and how it can eventually harm the kidneys and the heart
- Discuss how the diabetic genetic strain may be handed down from generation to generation
- What difficulties do diabetic people have while attempting to check their glucose levels and keep a balanced food plan?
- How have some individuals with type 1 or type 2 diabetes managed to live better lives than others with the disease?
- Is it true that eating too much sugar causes diabetes, cavities, acne, hyperactivity, and weight gain?
- What effect does insulin treatment have on type 2 diabetes?
- How does diabetes contribute to depression?
- What impact does snap participation have on diabetes rates?
- Why has the number of persons who perform blood glucose self-tests decreased? Could other variables, such as social or environmental, have contributed to this decrease?
- Why do patients in the United States struggle to obtain the treatment they require to monitor and maintain appropriate glucose levels? Is this due to increased healthcare costs?
- Nutrition is critical to a healthy lifestyle, yet many diabetic patients are unaware of what they should consume. Discuss
- Why have injuries and diabetes been designated as national health priorities?
- What factors contribute to the growing prevalence of type II diabetes in adolescents?
- Does socioeconomic status influence the prevalence of diabetes?
- Alzheimer’s disease and type 2 diabetes: a critical assessment of the shared pathological traits
- What are the effects and consequences of diabetes on peripheral blood vessels?
- What is the link between genetic predisposition, obesity, and type 2 diabetes development?
- Diabetes modifies the activation and repression of pro- and anti-inflammatory signalling pathways in the vascular system.
- Understanding autoimmune diabetes through the tri-molecular complex prism
- Does economic status influence the regional variation of diabetes caused by malnutrition?
- What evidence is there for using traditional Chinese medicine and natural products to treat depression in people who also have diabetes?
- Why was the qualitative method used to evaluate diabetes programs?
- Investigate the most common symptoms of undiagnosed diabetes
- How can artificial intelligence help diabetes patients?
- What effect does the palaeolithic diet have on type 2 diabetes?
- What are the most common causes of diabetes and what are the treatments?
- What causes diabetes mellitus, and how does it affect the United Kingdom?
- The impact of sociodemographic factors on the development of type II diabetes
- An examination of the link between gut microbiome and diabetes risk
- The effectiveness of lifestyle interventions in preventing type II diabetes
- The role of maternal diabetes in offspring’s risk of developing diabetes
- Artificial intelligence in diabetes diagnosis and management
- Continuous glucose monitoring
- Telehealth interventions for improving diabetes self-management
- The role of wearable technology in diabetes management
- Personalised medicine approaches for diabetes treatment
- The impact of diabetes on mental health and well-being
- The link between diabetes and cognitive decline
- The potential of stem cell therapy for diabetes treatment
- Advances in closed-loop insulin delivery systems
- The use of glucagon-like peptide-1 (GLP-1) receptor agonists in diabetes treatment
- Investigating the efficacy of new oral medications for type II diabetes
- The role of bariatric surgery in the management of type II diabetes
- Improving patient adherence to diabetes treatment regimens
- The role of social support in diabetes management
- Developing culturally sensitive diabetes education programs
- The role of dietary patterns in diabetes prevention and management
- Low-carbohydrate vs. Mediterranean diet for diabetes: A comparative study
- The use of artificial sweeteners in diabetes management: Benefits and risks
- The impact of the gut microbiome on dietary interventions for diabetes
- The role of exercise in improving glycemic control
- Developing effective exercise programs for individuals with diabetes
- The impact of physical activity on diabetic complications
- Promoting physical activity adherence in people with diabetes
- The use of exercise gamification to increase physical activity in diabetes
- The potential of CRISPR gene editing for diabetes treatment
- The role of the microbiome in the development and treatment of diabetes
- An analysis of the artificial Pancreas systems
- The use of big data analytics in diabetes research
- The impact of environmental factors on diabetes risk
- Cost-effectiveness of different diabetes treatment strategies
- Developing effective diabetes prevention programs for communities
- The role of government policies in addressing the diabetes epidemic
- Improving access to diabetes care in underserved populations
- The impact of social determinants of health on diabetes risk
- Management of diabetes in children and adolescents
- The unique challenges of diabetes management in older adults
- Diabetes in ethnic minorities: Disparities in prevalence and care
- The impact of diabetes on LGBTQ+ populations
Hire an Expert Writer
Orders completed by our expert writers are
- Formally drafted in an academic style
- Free Amendments and 100% Plagiarism Free – or your money back!
- 100% Confidential and Timely Delivery!
- Free anti-plagiarism report
- Appreciated by thousands of clients. Check client reviews
You can contact our 24/7 customer service for a bespoke list of customised diabetes dissertation topics , proposals, or essays written by our experienced writers . Each of our professionals is accredited and well-trained to provide excellent content on a wide range of topics. Getting a good grade on your dissertation course is our priority, and we make sure that happens. Find out more here .
Free Dissertation Topic
Phone Number
Academic Level Select Academic Level Undergraduate Graduate PHD
Academic Subject
Area of Research
Frequently Asked Questions
How to find diabetes dissertation topics.
To find diabetes dissertation topics:
- Study recent research in diabetes.
- Focus on emerging trends.
- Explore prevention, treatment, tech, etc.
- Consider cultural or demographic aspects.
- Consult experts or professors.
- Select a niche that resonates with you.
You May Also Like
Need interesting and manageable management dissertation topics or thesis? Here are the trending management dissertation titles so you can choose the most suitable one.
Need interesting and manageable history dissertation topics or thesis? Here are the trending history dissertation titles so you can choose the most suitable one.
When you choose business management as your field of study, you are undoubtedly not a typical student. A degree in business administration is intended for those wishing to start their own business or expand an existing one.
USEFUL LINKS
LEARNING RESOURCES

COMPANY DETAILS

- How It Works
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Risk Factors
- Providing Care
- Living with Diabetes
- Clinical Guidance
- DSMES for Health Care Providers
- Prevent Type 2 Diabetes: Talking to Your Patients About Lifestyle Change
- Employers and Insurers
- Community-based Organizations (CBOs)
- Toolkits for Diabetes Educators and Community Health Workers
- National Diabetes Statistics Report
- Reports and Publications
- Current Research Projects
- National Diabetes Prevention Program
- State, Local, and National Partner Diabetes Programs for Public Health
- Diabetes Self-Management Education and Support (DSMES) Toolkit
Your Feet and Diabetes
- Nerve damage from diabetes puts you at risk for foot ulcers.
- Check your feet every day, even if they feel fine.
- That way you can catch problems early and get them treated right away.

Nerve damage
About half of all people with diabetes have some kind of nerve damage . Nerves in your feet and legs are most often affected. Nerve damage can cause you to lose feeling in your feet.
Some people with nerve damage have numbness, tingling, or pain. Others have no symptoms. Nerve damage can also lower your ability to feel pain, heat, or cold.
Pain is the body’s way of telling you something’s wrong so you can take care of yourself. If you don’t feel pain in your feet, you may not notice a cut, blister, sore, or other problem. Small problems can become serious if they aren’t treated early.
Could you have nerve damage?

Know the risks
Anyone with diabetes can develop nerve damage, but these factors increase your risk:
- Blood sugar levels that are hard to manage.
- Having diabetes for a long time, especially if your blood sugar is often higher than your target levels.
- Having overweight.
- Being older than 40 years.
- Having high blood pressure.
- Having high cholesterol.
Nerve damage and poor blood flow—another diabetes complication—put you at risk for developing a foot ulcer (a sore or wound). With diabetes, a foot ulcer could get infected and not heal well. If an infection doesn't get better with treatment, your toe, foot, or leg may need to be amputated (removed by surgery). This is done to prevent the infection from spreading and to save your life.
Check your feet daily
When you check your feet every day, you can catch problems early and get them treated right away. Early treatment greatly lowers your risk of amputation.
Prevent or delay nerve damage
Keep your blood sugar in your target range as much as possible. This is one of the most important things you can do to prevent nerve damage or stop it from getting worse. Other good diabetes management habits can help, too:
- Don't smoke . Smoking reduces blood flow to the feet.
- Follow a healthy eating plan .
- Get physically active —10 to 20 minutes a day is better than an hour once a week. And both are better than none!
- Take medicines as prescribed by your doctor.
Tips for healthy feet
Check your feet every day for cuts, redness, swelling, sores, blisters, corns, calluses, or other change to the skin or nails. Use a mirror if you can't see the bottom of your feet, or ask a family member to help.
Wash your feet every day in warm (not hot) water. Don't soak your feet. Dry your feet completely and apply lotion to the top and bottom. Don't put lotion between your toes; that could lead to infection.
Never go barefoot. Always wear shoes and socks or slippers, even inside, to avoid injury. Check that there aren't any pebbles or other objects inside your shoes. Make sure that the lining is smooth.
Wear shoes that fit well . For the best fit, try on new shoes at the end of the day when your feet tend to be largest. Break in your new shoes slowly. Wear them for an hour or two a day at first until they're completely comfortable. Always wear socks with your shoes.
Trim your toenails straight across and gently smooth any sharp edges with a nail file. Have your foot doctor (podiatrist) trim your toenails if you can't see or reach your feet.
Don't remove corns or calluses yourself. Also, don't use over-the-counter products to remove them. They could burn your skin.
Get your feet checked at every visit with your primary care provider. Also, visit your foot doctor every year (more often if you have nerve damage) for a complete exam. A complete exam will include checking for feeling and blood flow in your feet.
Keep the blood flowing. Put your feet up when you're sitting. Wiggle your toes for a few minutes several times throughout the day.
Choose feet-friendly activities like walking, riding a bike, or swimming. Check with your doctor about which activities are best for you and any you should avoid.
Be sure to ask your doctor what else you can do to keep your feet healthy.
When to see your doctor
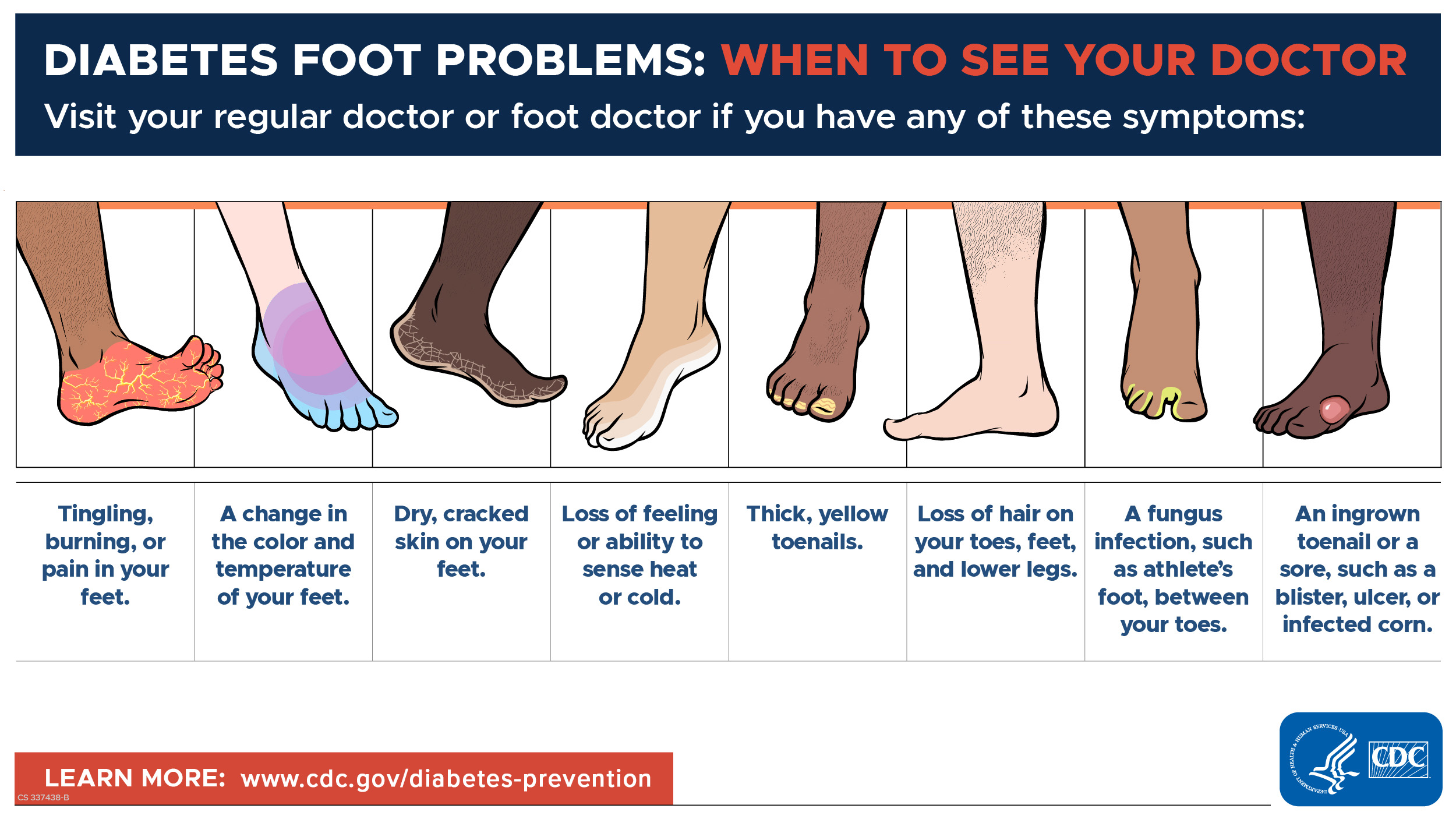
If you have any of these symptoms, don't wait for your next appointment. See your regular doctor or foot doctor right away:
- Pain in your legs or cramping in your buttocks, thighs, or calves during physical activity.
- Tingling, burning, or pain in your feet.
- Loss of sense of touch or ability to feel heat or cold very well.
- A change in the shape of your feet over time.
- Loss of hair on your toes, feet, and lower legs.
- Dry, cracked skin on your feet.
- A change in the color and temperature of your feet.
- Thickened, yellow toenails.
- Fungus infections such as athlete's foot between your toes.
- A blister, sore, ulcer, infected corn, or ingrown toenail.
Most people with diabetes can prevent serious foot complications. Regular care at home and going to all doctor's appointments are your best bet. Doing both will help you prevent foot problems (and stop small problems from becoming serious ones).
Diabetes is a chronic disease that affects how your body turns food into energy. About 1 in 10 Americans has diabetes.
For Everyone
Health care providers, public health.

COMMENTS
1. INTRODUCTION. Diabetic foot ulceration (DFU) is among the most common and debilitating complications of diabetes, with a lifetime incidence of up to 25% in people with this condition. 1 DFU represents a major health problem in this population because of its deleterious impact on physical and psychosocial functioning 2 and increased risks of DFU recurrence, 3 amputation, 1 and mortality. 4 ...
2.2 Diabetic foot ulcer and risk factors Diabetic foot ulcers is defined as the manifestation of infection, ulceration and any damage of deep tissues in connection to neurological problems or any level of peripheral arterial disease (PAD) around the foot of a diabetic person (Yazdanpanah et al., 2018). Foot ulcerations starts
Results. Following the search of databases, 9275 articles were screened and 10 met the inclusion criteria. Studies were RCTs (n = 5), non-RCTs (n = 1), and prepoststudies (n = 4).Informal caregivers through the intervention programmes were engaged in diverse roles that resulted in improved foot ulcer prevention and/or management outcomes such as improved foot care behaviors, increased diabetes ...
Diabetic foot ulceration (DFU) is a common and often catastrophic complication for people with diabetes. In the United States, people with diabetes have an up to 34% lifetime risk of developing a foot ulcer [1, 2], a medical complication that increases their five-year mortality rate by 2.5 times [3, 4].Moreover, foot ulceration is a causal factor for up to 85% of diabetic patients who ...
This thesis aimed to review what kind of nursing interventions are needed to prevent diabetic foot ulcers in adult inpatients. The importance of this study was to get accurate data, updat-ed facts and a better understanding of previous and existing studies since there were little awareness and knowledge about diabetic foot ulcers and its ...
Diabetic foot ulcers (DFUs) are one of the most severe and costly complications of diabetes, affecting nearly 40-60 million people; 12%-25% of patients with diabetes may develop diabetic foot ulcers [[2], [3], [4]]. DFUs impose a heavy economic burden on society, even within the country [5, 6].
protocol for staff nurses to implement into routine practice when caring for diabetic. patients was evidence that provided the best clinical outcomes. Keogh (2014) reported that the National Confidential Enquiry into Patient. Outcome and Death (NCEPOD) performed a study that involved 519 cases of lower limb.
society.( Working Group on the Diabetic Foot, 2019.) The aim of the thesis is to find out how nurse's role is described in prevention of diabetic foot ulcers through reviewing of existing literature. The purpose of the thesis is to offer in-formation and knowledge related to prevention of diabetic foot ulcers to nursing students
reported among 42.6% (P=0.313). It was affected by the presence of diabetic. foot ulcer and co-morbidity (P=0.04, and P=0.002 respectiv ely). Conclusion: A. low percentage of populations are aware ...
Keywords: Diabetic Foot, Diabetic Foot Ulcers, Diabetic Foot Infections, Diabetic Foot Osteomyelitis, Lower limb amputation, Peripheral arterial disease, Diabetes peripheral neuropathy, Charcot Foot, Diabetic Foot Prevention, Therapeutic Shoes, Wound healing . Important Note: All contributions to this Research Topic must be within the scope of the section and journal to which they are ...
THESIS SUMMARY Background: Diabetic foot ulcers are often described as painless due to peripheral neuropathy. The literature reveals that pain poses a significant problem than expected and severely affects the patient's quality of life and functional status. There has been no research conducted in Malaysia on this
Diabetic foot ulcers (DFUs) are one of the most challenging and prevalent refractory wounds associated with diabetes mellitus. It is characterized with long courses, high recurrence and disability rates. Hydrogel-based wound dressings have been demonstrated an effective and promising strategy for treating diabetic wounds. However, the complexity of the pathogenesis and microenvironment in ...
Diabetic foot ulcers (DFUs) are common problems in diabetes. One of the most important factors affecting the quality of diabetes care is knowledge and practice. The current study aimed at determining the knowledge and practice of patients with diabetes regarding the prevention and care of DFUs. The current analytical, cross sectional study was conducted in Guilan Province (north of Iran) on ...
In the world about 1/2 billion people are living with diabetes and the number is on a rise by 25% in 2030 and expected to hit 51% in 2045 (International Diabetes Federation 2019.) Diabetes has many types, but in this thesis will discuss the three main types, type 1 (DT1), type 2 (DT2), and Gestational diabetes (GDM).
Diabetes distress, self-efficacy, and social support should be assessed and monitored, in addition ... me to truly take ownership of my thesis and for giving me the freedom to design and execute my own study. I appreciate all the support you provided me along the way from navigating an IRB ... foot care, and medication management (Estes, 2016). ...
Diabetic Foot Thesis Topics - Free download as PDF File (.pdf), Text File (.txt) or read online for free. Scribd is the world's largest social reading and publishing site.
Diabetic foot ulcers (DFUs) account for 12-15% of the overall projected cost of diabetes in prosperous countries, compared to 40% in developing nations (3). ... Knowledge and Self-Care Practices ...
AND PRACTICE OF DIABETIC FOOT CARE IN PATIENTS WITH DIABETIC FOOT ULCER A Dissertation submitted to THE TAMIL NADU Dr. M.G.R. MEDICAL UNIVERSITY, CHENNAI- 600 032 In partial fulfillment of the award of the degree of MASTER OF PHARMACY IN Branch-VII -PHARMACY PRACTICE Submitted by Name: JANAANI V REG. No: 261740206 Under the Guidance of
Evidence-based Practice Nursing Dissertation Topics. Child Health Nursing Dissertation Topics. Adult Nursing Dissertation Topics. Critical Care Nursing Dissertation Topics. Palliative Care Nursing Dissertation Topics. Mental Health Nursing Dissertation Topics. Nursing Dissertation Topics. Coronavirus (COVID-19) Nursing Dissertation Topics.
The purpose of this thesis is to describe the nursing interventions used in the prevention of foot ulcer in elderly diabetic patients. The research question was what the nursing interven-tions are used in the prevention of foot ulcers in elderly diabetic patients. The search for data was conducted in January 2018.
Staphylococcus aureus or β - hemolytic streptococci, pathogens that. colonize the skin of diabetic patients are the causative agents of acute. infections in antibiotic-naive patients, and are nearly always the cause of. cellulitis in non-ulcerated skin. Staphylococcus aureus is the most commonly recovered pathogen in.
For individuals with T2DM, DSM is a fundamental aspect of diabetes care. DSM is the most widely accepted and efficacious method of promoting healthy lifestyle change for people with T2DM (American Diabetes Association, 2018). DSM is often based upon the AADE7 Self-Care Behaviors™, a product of the American Association of Diabetes Educators (AADE)
Medicare covers a foot exam once a year and some treatments for foot injuries or diseases. Medicaid covers foot care in some states. Check with your state Medicaid agency to find out what foot care services are covered in your plan. Federally qualified community health centers provide low-cost primary care services in both urban and rural areas.
comprehensive management and treatment of diabetic foot at early stages is crucial. (Zielinski, Paola, & Martínez, 2018.) The complications of diabetes include decrease in visual acuity, neuropathy, and amputation of a limb due to diabetic foot, and they affect the patient's quality of life (WHO 2016, according to Figueiredo et al. 2017).
Nerve damage and poor blood flow—another diabetes complication—put you at risk for developing a foot ulcer (a sore or wound). With diabetes, a foot ulcer could get infected and not heal well. If an infection doesn't get better with treatment, your toe, foot, or leg may need to be amputated (removed by surgery).