- Open access
- Published: 26 November 2021

Women’s Perceptions and Experiences of Breastfeeding: a scoping review of the literature
- Bridget Beggs 1 ,
- Liza Koshy 1 &
- Elena Neiterman 1
BMC Public Health volume 21 , Article number: 2169 ( 2021 ) Cite this article
12k Accesses
23 Citations
4 Altmetric
Metrics details
Despite public health efforts to promote breastfeeding, global rates of breastfeeding continue to trail behind the goals identified by the World Health Organization. While the literature exploring breastfeeding beliefs and practices is growing, it offers various and sometimes conflicting explanations regarding women’s attitudes towards and experiences of breastfeeding. This research explores existing empirical literature regarding women’s perceptions about and experiences with breastfeeding. The overall goal of this research is to identify what barriers mothers face when attempting to breastfeed and what supports they need to guide their breastfeeding choices.
This paper uses a scoping review methodology developed by Arksey and O’Malley. PubMed, CINAHL, Sociological Abstracts, and PsychInfo databases were searched utilizing a predetermined string of keywords. After removing duplicates, papers published in 2010–2020 in English were screened for eligibility. A literature extraction tool and thematic analysis were used to code and analyze the data.
In total, 59 papers were included in the review. Thematic analysis showed that mothers tend to assume that breastfeeding will be easy and find it difficult to cope with breastfeeding challenges. A lack of partner support and social networks, as well as advice from health care professionals, play critical roles in women’s decision to breastfeed.
While breastfeeding mothers are generally aware of the benefits of breastfeeding, they experience barriers at individual, interpersonal, and organizational levels. It is important to acknowledge that breastfeeding is associated with challenges and provide adequate supports for mothers so that their experiences can be improved, and breastfeeding rates can reach those identified by the World Health Organization.
Peer Review reports
Public health efforts to educate parents about the importance of breastfeeding can be dated back to the early twentieth century [ 1 ]. The World Health Organization is aiming to have at least half of all the mothers worldwide exclusively breastfeeding their infants in the first 6 months of life by the year 2025 [ 2 ], but it is unlikely that this goal will be achieved. Only 38% of the global infant population is exclusively breastfed between 0 and 6 months of life [ 2 ], even though breastfeeding initiation rates have shown steady growth globally [ 3 ]. The literature suggests that while many mothers intend to breastfeed and even make an attempt at initiation, they do not always maintain exclusive breastfeeding for the first 6 months of life [ 4 , 5 ]. The literature identifies various barriers, including return to paid employment [ 6 , 7 ], lack of support from health care providers and significant others [ 8 , 9 ], and physical challenges [ 9 ] as potential factors that can explain premature cessation of breastfeeding.
From a public health perspective, the health benefits of breastfeeding are paramount for both mother and infant [ 10 , 11 ]. Globally, new mothers following breastfeeding recommendations could prevent 974,956 cases of childhood obesity, 27,069 cases of mortality from breast cancer, and 13,644 deaths from ovarian cancer per year [ 11 ]. Global economic loss due to cognitive deficiencies resulting from cessation of breastfeeding has been calculated to be approximately USD $285.39 billion dollars annually [ 11 ]. Evidently, increasing exclusive breastfeeding rates is an important task for improving population health outcomes. While public health campaigns targeting pregnant women and new mothers have been successful in promoting breastfeeding, they also have been perceived as too aggressive [ 12 ] and failing to consider various structural and personal barriers that may impact women’s ability to breastfeed [ 1 ]. In some cases, public health messaging itself has been identified as a barrier due to its rigid nature and its lack of flexibility in guidelines [ 13 ]. Hence, while the literature on women’s perceptions regarding breastfeeding and their experiences with breastfeeding has been growing [ 14 , 15 , 16 ], it offers various, and sometimes contradictory, explanations on how and why women initiate and maintain breastfeeding and what role public health messaging plays in women’s decision to breastfeed.
The complex array of the barriers shaping women’s experiences of breastfeeding can be broadly categorized utilizing the socioecological model, which suggests that individuals’ health is a result of the interplay between micro (individual), meso (institutional), and macro (social) factors [ 17 ]. Although previous studies have explored barriers and supports to breastfeeding, the majority of articles focus on specific geographic areas (e.g. United States or United Kingdom), workplaces, or communities. In addition, very few articles focus on the analysis of the interplay between various micro, meso, and macro-level factors in shaping women’s experiences of breastfeeding. Synthesizing the growing literature on the experiences of breastfeeding and the factors shaping these experiences, offers researchers and public health professionals an opportunity to examine how various personal and institutional factors shape mothers’ breastfeeding decision-making. This knowledge is needed to identify what can be done to improve breastfeeding rates and make breastfeeding a more positive and meaningful experience for new mothers.
The aim of this scoping review is to synthesize evidence gathered from empirical literature on women’s perceptions about and experiences of breastfeeding. Specifically, the following questions are examined:
What does empirical literature report on women’s perceptions on breastfeeding?
What barriers do women face when they attempt to initiate or maintain breastfeeding?
What supports do women need in order to initiate and/or maintain breastfeeding?
Focusing on women’s experiences, this paper aims to contribute to our understanding of women’s decision-making and behaviours pertaining to breastfeeding. The overarching aim of this review is to translate these findings into actionable strategies that can streamline public health messaging and improve breastfeeding education and supports offered by health care providers working with new mothers.
This research utilized Arksey & O’Malley’s [ 18 ] framework to guide the scoping review process. The scoping review methodology was chosen to explore a breadth of literature on women’s perceptions about and experiences of breastfeeding. A broad research question, “What does empirical literature tell us about women’s experiences of breastfeeding?” was set to guide the literature search process.
Search methods
The review was undertaken in five steps: (1) identifying the research question, (2) identifying relevant literature, (3) iterative selection of data, (4) charting data, and (5) collating, summarizing, and reporting results. The inclusion criteria were set to empirical articles published between 2010 and 2020 in peer-reviewed journals with a specific focus on women’s self-reported experiences of breastfeeding, as well as how others see women’s experiences of breastfeeding. The focus on women’s perceptions of breastfeeding was used to capture the papers that specifically addressed their experiences and the barriers that they may encounter while breastfeeding. Only articles written in English were included in the review. The keywords utilized in the search strategy were developed in collaboration with a librarian (Table 1 ). PubMed, CINAHL, Sociological Abstracts, and PsychInfo databases were searched for the empirical literature, yielding a total of 2885 results.
Search outcome
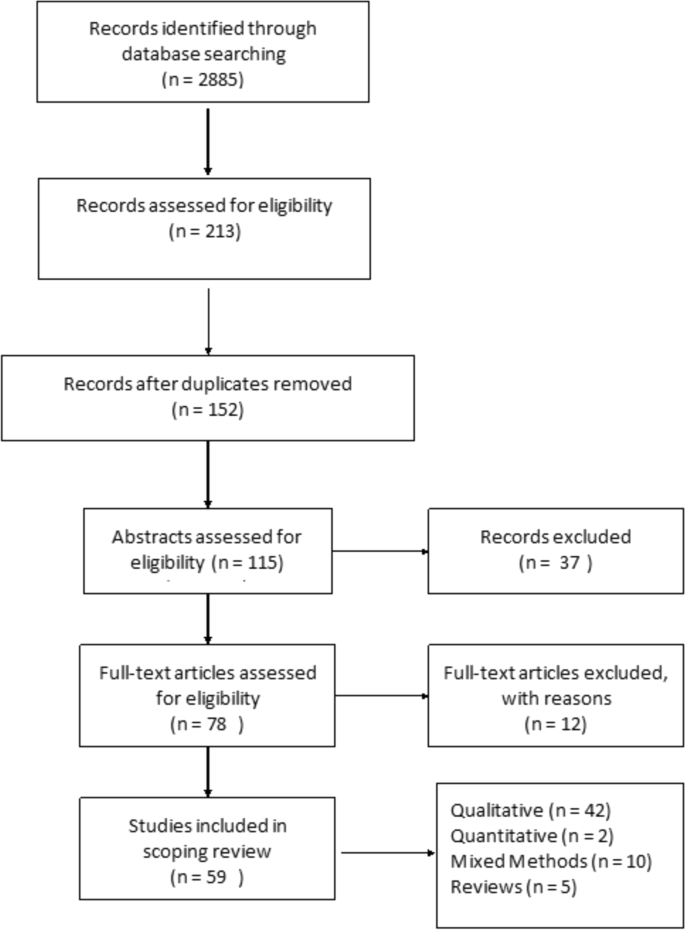
The articles deemed to fit the inclusion criteria ( n = 213) were imported into RefWorks, an online reference manager tool and further screened for eligibility (Fig. 1 ). After the removal of 61 duplicates and title/abstract screening, 152 articles were kept for full-text review. Two independent reviewers assessed the papers to evaluate if they met the inclusion criteria of having an explicit analytic focus on women’s experiences of breastfeeding.
Prisma Flow Diagram
Quality appraisal
Consistent with scoping review methodology [ 18 ], the quality of the papers included in the review was not assessed.
Data abstraction
A literature extraction tool was created in MS Excel 2016. The data extracted from each paper included: (a) authors names, (b) title of the paper, (c) year of publication, (d) study objectives, (e) method used, (f) participant demographics, (g) country where the study was conducted, and (h) key findings from the paper.
Thematic analysis was utilized to identify key topics covered by the literature. Two reviewers independently read five papers to inductively generate key themes. This process was repeated until the two reviewers reached a consensus on the coding scheme, which was subsequently applied to the remainder of the articles. Key themes were added to the literature extraction tool and each paper was assigned a key theme and sub-themes, if relevant. The themes derived from the analysis were reviewed once again by all three authors when all the papers were coded. In the results section below, the synthesized literature is summarized alongside the key themes identified during the analysis.
In total, 59 peer-reviewed articles were included in the review. Since the review focused on women’s experiences of breastfeeding, as would be expected based on the search criteria, the majority of articles ( n = 42) included in the sample were qualitative studies, with ten utilizing a mixed method approach (Fig. 2 ). Figure 3 summarizes the distribution of articles by year of publication and Fig. 4 summarizes the geographic location of the study.
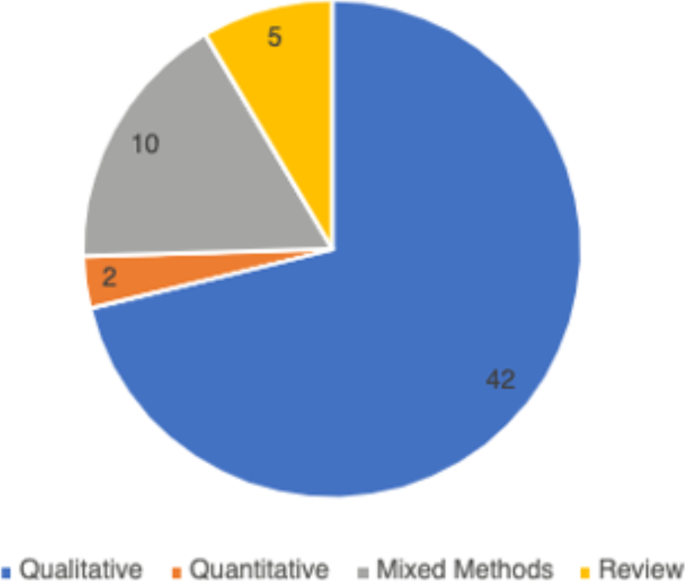
Types of Articles

Years of Publication
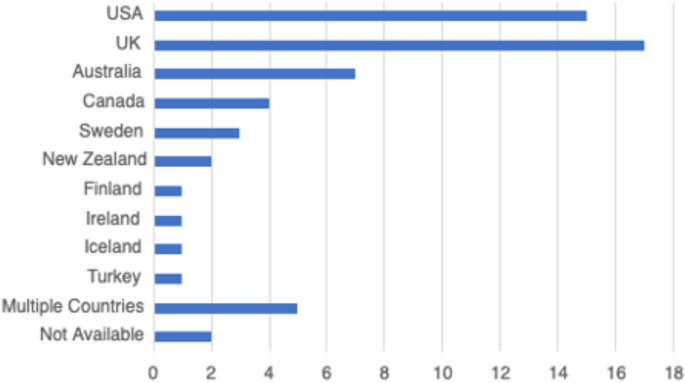
Countries of Focus Examined in Literature Review
Perceptions about breastfeeding
Women’s perceptions about breastfeeding were covered in 83% ( n = 49) of the papers. Most articles ( n = 31) suggested that women perceived breastfeeding as a positive experience and believed that breastfeeding had many benefits [ 19 , 20 ]. The phrases “breast is best” and “breastmilk is best” were repeatedly used by the participants of studies included in the reviewed literature [ 21 ]. Breastfeeding was seen as improving the emotional bond between the mother and the child [ 20 , 22 , 23 ], strengthening the child’s immune system [ 24 , 25 ], and providing a booster to the mother’s sense of self [ 1 , 26 ]. Convenience of breastfeeding (e.g., its availability and low cost) [ 19 , 27 ] and the role of breastfeeding in weight loss during the postpartum period were mentioned in the literature as other factors that positively shape mothers’ perceptions about breastfeeding [ 28 , 29 ].
The literature suggested that women’s perceptions of breastfeeding and feeding choices were also shaped by the advice of healthcare providers [ 30 , 31 ]. Paradoxically, messages about the importance and relative simplicity of breastfeeding may also contribute to misalignment between women’s expectations and the actual experiences of breastfeeding [ 32 ]. For instance, studies published in Canada and Sweden reported that women expected breastfeeding to occur “naturally”, to be easy and enjoyable [ 23 ]. Consequently, some women felt unprepared for the challenges associated with initiation or maintenance of breastfeeding [ 31 , 33 ]. The literature pointed out that mothers may feel overwhelmed by the frequency of infant feedings [ 26 ] and the amount as well as intensity of physical difficulties associated with breastfeeding initiation [ 33 ]. Researchers suggested that since many women see breastfeeding as a sign of being a “good” mother, their inability to breastfeed may trigger feelings of personal failure [ 22 , 34 ].
Women’s personal experiences with and perceptions about breastfeeding were also influenced by the cultural pressure to breastfeed. Welsh mothers interviewed in the UK, for instance, revealed that they were faced with judgement and disapproval when people around them discovered they opted out of breastfeeding [ 35 ]. Women recalled the experiences of being questioned by others, including strangers, when they were bottle feeding their infants [ 9 , 35 , 36 ].
Barriers to breastfeeding
The vast majority ( n = 50) of the reviewed literature identified various barriers for successful breastfeeding. A sizeable proportion of literature (41%, n = 24) explored women’s experiences with the physical aspects of breastfeeding [ 23 , 33 ]. In particular, problems with latching and the pain associated with breastfeeding were commonly cited as barriers for women to initiate breastfeeding [ 23 , 28 , 37 ]. Inadequate milk supply, both actual and perceived, was mentioned as another barrier for initiation and maintenance of breastfeeding [ 33 , 37 ]. Breastfeeding mothers were sometimes unable to determine how much milk their infants consumed (as opposed to seeing how much milk the infant had when bottle feeding), which caused them to feel anxious and uncertain about scheduling infant feedings [ 28 , 37 ]. Women’s inability to overcome these barriers was linked by some researchers to low self-efficacy among mothers, as well as feeling overwhelmed or suffering from postpartum depression [ 38 , 39 ].
In addition to personal and physical challenges experienced by mothers who were planning to breastfeed, the literature also highlighted the importance of social environment as a potential barrier to breastfeeding. Mothers’ personal networks were identified as a key factor in shaping their breastfeeding behaviours in 43 (73%) articles included in this review. In a study published in the UK, lack of role models – mothers, other female relatives, and friends who breastfeed – was cited as one of the potential barriers for breastfeeding [ 36 ]. Some family members and friends also actively discouraged breastfeeding, while openly questioning the benefits of this practice over bottle feeding [ 1 , 17 , 40 ]. Breastfeeding during family gatherings or in the presence of others was also reported as a challenge for some women from ethnic minority groups in the United Kingdom and for Black women in the United States [ 41 , 42 ].
The literature reported occasional instances where breastfeeding-related decisions created conflict in women’s relationships with significant others [ 26 ]. Some women noted they were pressured by their loved one to cease breastfeeding [ 22 ], especially when women continued to breastfeed 6 months postpartum [ 43 ]. Overall, the literature suggested that partners play a central role in women’s breastfeeding practices [ 8 ], although there was no consistency in the reviewed papers regarding the partners’ expressed level of support for breastfeeding.
Knowledge, especially practical knowledge about breastfeeding, was mentioned as a barrier in 17% ( n = 10) of the papers included in this review. While health care providers were perceived as a primary source of information on breastfeeding, some studies reported that mothers felt the information provided was not useful and occasionally contained conflicting advice [ 1 , 17 ]. This finding was reported across various jurisdictions, including the United States, Sweden, the United Kingdom and Netherlands, where mothers reported they had no support at all from their health care providers which made it challenging to address breastfeeding problems [ 26 , 38 , 44 ].
Breastfeeding in public emerged as a key barrier from the reviewed literature and was cited in 56% ( n = 33) of the papers. Examining the experiences of breastfeeding mothers in the United States, Spencer, Wambach, & Domain [ 45 ] suggested that some participants reported feeling “erased” from conversations while breastfeeding in public, rendering their bodies symbolically invisible. Lack of designated public spaces for breastfeeding forced many women to alter their feeding in public and to retreat to a private or a more secluded space, such as one’s personal car [ 25 ]. The oversexualization of women’s breasts was repeatedly noted as a core reason for the United States women’s negative experiences and feelings of self-consciousness about breastfeeding in front of others [ 45 ]. Studies reported women’s accounts of feeling the disapproval or disgust of others when breastfeeding in public [ 46 , 47 ], and some reported that women opted out of breastfeeding in public because they did not want to make those around them feel uncomfortable [ 25 , 40 , 48 ].
Finally, return to paid employment was noted in the literature as a significant challenge for continuation of breastfeeding [ 48 ]. Lack of supportive workplace environments [ 39 ] or inability to express milk were cited by women as barriers for continuing breastfeeding in the United States and New Zealand [ 39 , 49 ].
Supports needed to maintain breastfeeding
Due to the central role family members played in women’s experiences of breastfeeding, support from partners as well as female relatives was cited in the literature as key factors shaping women’s breastfeeding decisions [ 1 , 9 , 48 ]. In the articles published in Canada, Australia, and the United Kingdom, supportive family members allowed women to share the responsibility of feeding and other childcare activities, which reduced the pressures associated with being a new mother [ 19 , 20 ]. Similarly, encouragement, breastfeeding advice, and validation from healthcare professionals were identified as positively impacting women’s experiences with breastfeeding [ 1 , 22 , 28 ].
Community resources, such as peer support groups, helplines, and in-home breastfeeding support provided mothers with the opportunity to access help when they need it, and hence were reported to be facilitators for breastfeeding [ 19 , 22 , 33 , 44 ]. An increase in the usage of social media platforms, such as Facebook, among breastfeeding mothers for peer support were reported in some studies [ 47 ]. Public health breastfeeding clinics, lactation specialists, antenatal and prenatal classes, as well as education groups for mothers were identified as central support structures for the initiation and maintenance of breastfeeding [ 23 , 24 , 28 , 33 , 39 , 50 ]. Based on the analysis of the reviewed literature, however, access to these services varied greatly geographically and by socio-economic status [ 33 , 51 ]. It is also important to note that local and cultural context played a significant role in shaping women’s perceptions of breastfeeding. For example, a study that explored women’s breastfeeding experiences in Iceland highlighted the importance of breastfeeding in Icelandic society [ 52 ]. Women are expected to breastfeed and the decision to forgo breastfeeding is met with disproval [ 52 ]. Cultural beliefs regarding breastfeeding were also deemed important in the study of Szafrankska and Gallagher (2016), who noted that Polish women living in Ireland had a much higher rate of initiating breastfeeding compared to Irish women [ 53 ]. They attributed these differences to familial and societal expectations regarding breastfeeding in Poland [ 53 ].
Overall, the reviewed literature suggested that women faced socio-cultural pressure to breastfeed their infants [ 36 , 40 , 54 ]. Women reported initiating breastfeeding due to recognition of the many benefits it brings to the health of the child, even when they were reluctant to do it for personal reasons [ 8 ]. This hints at the success of public health education campaigns on the benefits of breastfeeding, which situates breastfeeding as a new cultural norm [ 24 ].
This scoping review examined the existing empirical literature on women’s perceptions about and experiences of breastfeeding to identify how public health messaging can be tailored to improve breastfeeding rates. The literature suggests that, overall, mothers are aware of the positive impacts of breastfeeding and have strong motivation to breastfeed [ 37 ]. However, women who chose to breastfeed also experience many barriers related to their social interactions with significant others and their unique socio-cultural contexts [ 25 ]. These different factors, summarized in Fig. 5 , should be considered in developing public health activities that promote breastfeeding. Breastfeeding experiences for women were very similar across the United Kingdom, United States, Canada, and Australia based on the studies included in this review. Likewise, barriers and supports to breastfeeding identified by women across the countries situated in the global north were quite similar. However, local policy context also impacted women’s experiences of breastfeeding. For example, maintaining breastfeeding while returning to paid employment has been identified as a challenge for mothers in the United States [ 39 , 45 ], a country with relatively short paid parental leave. Still, challenges with balancing breastfeeding while returning to paid employment were also noticed among women in New Zealand, despite a more generous maternity leave [ 49 ]. This suggests that while local and institutional policies might shape women’s experiences of breastfeeding, interpersonal and personal factors can also play a central role in how long they breastfeed their infants. Evidently, the importance of significant others, such as family members or friends, in providing support to breastfeeding mothers was cited as a key facilitator for breastfeeding across multiple geographic locations [ 29 , 34 , 48 ]. In addition, cultural beliefs and practices were also cited as an important component in either promoting breastfeeding or deterring women’s desire to initiate or maintain breastfeeding [ 15 , 29 , 37 ]. Societal support for breastfeeding and cultural practices can therefore partly explain the variation in breastfeeding rates across different countries [ 15 , 21 ]. Figure 5 summarizes the key barriers identified in the literature that inhibit women’s ability to breastfeed.
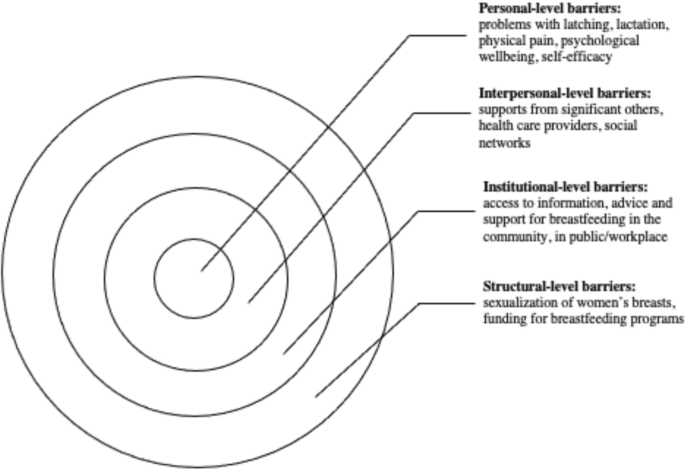
Barriers to Breastfeeding
At the individual level, women might experience challenges with breastfeeding stemming from various physiological and psychological problems, such as issues with latching, perceived or actual lack of breastmilk, and physical pain associated with breastfeeding. The onset of postpartum depression or other psychological problems may also impact women’s ability to breastfeed [ 54 ]. Given that many women assume that breastfeeding will happen “naturally” [ 15 , 40 ] these challenges can deter women from initiating or continuing breastfeeding. In light of these personal challenges, it is important to consider the potential challenges associated with breastfeeding that are conveyed to new mothers through the simplified message “breast is best” [ 21 ]. While breastfeeding may come easy to some women, most papers included in this review pointed to various challenges associated with initiating or maintaining breastfeeding [ 19 , 33 ]. By modifying public health messaging regarding breastfeeding to acknowledge that breastfeeding may pose a challenge and offering supports to new mothers, it might be possible to alleviate some of the guilt mothers experience when they are unable to breastfeed.
Barriers that can be experienced at the interpersonal level concern women’s communication with others regarding their breastfeeding choices and practices. The reviewed literature shows a strong impact of women’s social networks on their decision to breastfeed [ 24 , 33 ]. In particular, significant others – partners, mothers, siblings and close friends – seem to have a considerable influence over mothers’ decision to breastfeed [ 42 , 53 , 55 ]. Hence, public health messaging should target not only mothers, but also their significant others in developing breastfeeding campaigns. Social media may also be a potential medium for sharing supports and information regarding breastfeeding with new mothers and their significant others.
There is also a strong need for breastfeeding supports at the institutional and community levels. Access to lactation consultants, sound and practical advice from health care providers, and availability of physical spaces in the community and (for women who return to paid employment) in the workplace can provide more opportunities for mothers who want to breastfeed [ 18 , 33 , 44 ]. The findings from this review show, however, that access to these supports and resources vary greatly, and often the women who need them the most lack access to them [ 56 ].
While women make decisions about breastfeeding in light of their own personal circumstances, it is important to note that these circumstances are shaped by larger structural, social, and cultural factors. For instance, mothers may feel reluctant to breastfeed in public, which may stem from their familiarity with dominant cultural perspectives that label breasts as objects for sexualized pleasure [ 48 ]. The reviewed literature also showed that, despite the initial support, mothers who continue to breastfeed past the first year may be judged and scrutinized by others [ 47 ]. Tailoring public health care messaging to local communities with their own unique breastfeeding-related beliefs might help to create a larger social change in sociocultural norms regarding breastfeeding practices.
The literature included in this scoping review identified the importance of support from community services and health care providers in facilitating women’s breastfeeding behaviours [ 22 , 24 ]. Unfortunately, some mothers felt that the support and information they received was inadequate, impractical, or infused with conflicting messaging [ 28 , 44 ]. To make breastfeeding support more accessible to women across different social positions and geographic locations, it is important to acknowledge the need for the development of formal infrastructure that promotes breastfeeding. This includes training health care providers to help women struggling with breastfeeding and allocating sufficient funding for such initiatives.
Overall, this scoping review revealed the need for healthcare professionals to provide practical breastfeeding advice and realistic solutions to women encountering difficulties with breastfeeding. Public health messaging surrounding breastfeeding must re-invent breastfeeding as a “family practice” that requires collaboration between the breastfeeding mother, their partner, as well as extended family to ensure that women are supported as they breastfeed [ 8 ]. The literature also highlighted the issue of healthcare professionals easily giving up on women who encounter problems with breastfeeding and automatically recommending the initiation of formula use without further consideration towards solutions for breastfeeding difficulties [ 19 ]. While some challenges associated with breastfeeding are informed by local culture or health care policies, most of the barriers experienced by breastfeeding women are remarkably universal. Women often struggle with initiation of breastfeeding, lack of support from their significant others, and lack of appropriate places and spaces to breastfeed [ 25 , 26 , 33 , 39 ]. A change in public health messaging to a more flexible messaging that recognizes the challenges of breastfeeding is needed to help women overcome negative feelings associated with failure to breastfeed. Offering more personalized advice and support to breastfeeding mothers can improve women’s experiences and increase the rates of breastfeeding while also boosting mothers’ sense of self-efficacy.
Limitations
This scoping review has several limitations. First, the focus on “women’s experiences” rendered broad search criteria but may have resulted in the over or underrepresentation of specific findings in this review. Also, the exclusion of empirical work published in languages other than English rendered this review reliant on the papers published predominantly in English-speaking countries. Finally, consistent with Arksey and O’Malley’s [ 18 ] scoping review methodology, we did not appraise the quality of the reviewed literature. Notwithstanding these limitations, this review provides important insights into women’s experiences of breastfeeding and offers practical strategies for improving dominant public health messaging on the importance of breastfeeding.
Women who breastfeed encounter many difficulties when they initiate breastfeeding, and most women are unsuccessful in adhering to current public health breastfeeding guidelines. This scoping review highlighted the need for reconfiguring public health messaging to acknowledge the challenges many women experience with breastfeeding and include women’s social networks as a target audience for such messaging. This review also shows that breastfeeding supports and counselling are needed by all women, but there is also a need to tailor public health messaging to local social norms and culture. The role social institutions and cultural discourses have on women’s experiences of breastfeeding must also be acknowledged and leveraged by health care professionals promoting breastfeeding.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Wolf JH. Low breastfeeding rates and public health in the United States. Am J Public Health. 2003;93(12):2000–2010. [cited 2021 Apr 21] Available from: http://ajph.aphapublications.org/doi/ https://doi.org/10.2105/AJPH.93.12.2000
World Health Organization, UNICEF. Global nutrition targets 2015: Breastfeeding policy brief 2014.
United Nations International Children’s Emergency Fund (UNICEF). Breastfeeding in the UK. 2019 [cited 2021 Apr 21]. Available from: https://www.unicef.org.uk/babyfriendly/about/breastfeeding-in-the-uk/
Semenic S, Loiselle C, Gottlieb L. Predictors of the duration of exclusive breastfeeding among first-time mothers. Res Nurs Health. 2008;31(5):428–441. [cited 2021 Apr 21] Available from: http://doi.wiley.com/ https://doi.org/10.1002/nur.20275
Hauck YL, Bradfield Z, Kuliukas L. Women’s experiences with breastfeeding in public: an integrative review. Women Birth. 2020;34:e217–27.
Hendaus MA, Alhammadi AH, Khan S, Osman S, Hamad A. Breastfeeding rates and barriers: a report from the state of Qatar. Int. J Women's Health. 2018;10:467–75 [cited 2021 Apr 20] Available from: /pmc/articles/PMC6110662/.
Google Scholar
Ogbo FA, Ezeh OK, Khanlari S, Naz S, Senanayake P, Ahmed KY, et al. Determinants of exclusive breastfeeding cessation in the early postnatal period among culturally and linguistically diverse (CALD) Australian mothers. Nutrients. 2019;11(7):1611 [cited 2021 Apr 21] Available from: https://www.mdpi.com/2072-6643/11/7/1611 .
Article Google Scholar
Ayton JE, Tesch L, Hansen E. Women’s experiences of ceasing to breastfeed: Australian qualitative study. BMJ Open. 2019;9(5):26234 [cited 2021 Apr 20] Available from: http://bmjopen.bmj.com/ .
Brown CRL, Dodds L, Legge A, Bryanton J, Semenic S. Factors influencing the reasons why mothers stop breastfeeding. Can J Public Heal. 2014;105(3):e179–e185. [cited 2021 Apr 20] Available from: https://link.springer.com/article/ https://doi.org/10.17269/cjph.105.4244
Sharma AJ, Dee DL, Harden SM. Adherence to breastfeeding guidelines and maternal weight 6 years after delivery. Pediatrics. 2014;134(Supplement 1):S42–S49. [cited 2021 Apr 21] Available from: www.pediatrics.org/cgi/doi/ https://doi.org/10.1542/peds.2014-0646H
Walters DD, Phan LTH, Mathisen R. The cost of not breastfeeding: Global results from a new tool. Health Policy Plan. 2019;34(6):407–17 [cited 2021 Apr 21] Available from: https://academic.oup.com/heapol/article/34/6/407/5522499 .
Friedman M. For whom is breast best? Thoughts on breastfeeding, feminism and ambivalence. J Mother Initiat Res Community Involv. 2009;11(1):26–35 [cited 2021 Apr 20] Available from: https://jarm.journals.yorku.ca/index.php/jarm/article/viewFile/22506/20986 .
Blixt I, Johansson M, Hildingsson I, Papoutsi Z, Rubertsson C. Women’s advice to healthcare professionals regarding breastfeeding: “offer sensitive individualized breastfeeding support” - an interview study. Int Breastfeed J 2019;14(1):51. [cited 2021 Apr 20] Available from: https://internationalbreastfeedingjournal.biomedcentral.com/articles/10.1186/s13006-019-0247-4
Obeng C, Dickinson S, Golzarri-Arroyo L. Women’s perceptions about breastfeeding: a preliminary study. Children. 2020;7(6):61 [cited 2021 Apr 21] Available from: https://www.mdpi.com/2227-9067/7/6/61 .
Choudhry K, Wallace LM. ‘Breast is not always best’: South Asian women’s experiences of infant feeding in the UK within an acculturation framework. Matern Child Nutr. 2012;8(1):72–87. [cited 2021 Apr 20] Available from: http://doi.wiley.com/ https://doi.org/10.1111/j.1740-8709.2010.00253.x
Da Silva TD, Bick D, Chang YS. Breastfeeding experiences and perspectives among women with postnatal depression: a qualitative evidence synthesis. Women Birth. 2020;33(3):231–9.
Kilanowski JF. Breadth of the socio-ecological model. J Agromedicine. 2017;22(4):295–7 [cited 2021 Apr 20] Available from: https://www.tandfonline.com/action/journalInformation?journalCode=wagr20 .
Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. Int J Soc Res Methodol Theory Pract. 2005;8(1):19–32 [cited 2021 Apr 20] Available from: https://www.tandfonline.com/action/journalInformation?journalCode=tsrm20 .
Brown A, Lee M. An exploration of the attitudes and experiences of mothers in the United Kingdom who chose to breastfeed exclusively for 6 months postpartum. Breastfeed Med. 2011;6(4):197–204. [cited 2021 Apr 20] Available from: http://www.liebertpub.com/doi/ https://doi.org/10.1089/bfm.2010.0097
Morns MA, Steel AE, Burns E, McIntyre E. Women who experience feelings of aversion while breastfeeding: a meta-ethnographic review. Women Birth. 2021;34:128–35.
Jackson KT, Mantler T, O’Keefe-McCarthy S. Women’s experiences of breastfeeding-related pain. MCN Am J Matern Nurs. 2019;44(2):66–72 [cited 2021 Apr 20] Available from: https://journals.lww.com/00005721-201903000-00002 .
Burns E, Schmied V, Sheehan A, Fenwick J. A meta-ethnographic synthesis of women’s experience of breastfeeding. Matern Child Nutr. 2009;6(3):201–219. [cited 2021 Apr 20] Available from: http://doi.wiley.com/ https://doi.org/10.1111/j.1740-8709.2009.00209.x
Claesson IM, Larsson L, Steen L, Alehagen S. “You just need to leave the room when you breastfeed” Breastfeeding experiences among obese women in Sweden - A qualitative study. BMC Pregnancy Childbirth. 2018;18(1):1–10. [cited 2021 Apr 20] Available from: https://link.springer.com/articles/ https://doi.org/10.1186/s12884-017-1656-2
Asiodu IV, Waters CM, Dailey DE, Lyndon • Audrey. Infant feeding decision-making and the influences of social support persons among first-time African American mothers. Matern Child Health J. 2017;21:863–72.
Forster DA, McLachlan HL. Women’s views and experiences of breast feeding: positive, negative or just good for the baby? Midwifery. 2010;26(1):116–25.
Demirci J, Caplan E, Murray N, Cohen S. “I just want to do everything right:” Primiparous Women’s accounts of early breastfeeding via an app-based diary. J Pediatr Heal Care. 2018;32(2):163–72.
Furman LM, Banks EC, North AB. Breastfeeding among high-risk Inner-City African-American mothers: a risky choice? Breastfeed Med. 2013;8(1):58–67. [cited 2021 Apr 20]Available from: http://www.liebertpub.com/doi/ https://doi.org/10.1089/bfm.2012.0012
Cottrell BH, Detman LA. Breastfeeding concerns and experiences of african american mothers. MCN Am J Matern Nurs. 2013;38(5):297–304 [cited 2021 Apr 20] Available from: https://journals.lww.com/00005721-201309000-00009 .
Wambach K, Domian EW, Page-Goertz S, Wurtz H, Hoffman K. Exclusive breastfeeding experiences among mexican american women. J Hum Lact. 2016;32(1):103–111. [cited 2021 Apr 21] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/0890334415599400
Regan P, Ball E. Breastfeeding mothers’ experiences: The ghost in the machine. Qual Health Res. 2013;23(5):679–688. [cited 2021 Apr 21] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/1049732313481641
Hinsliff-Smith K, Spencer R, Walsh D. Realities, difficulties, and outcomes for mothers choosing to breastfeed: Primigravid mothers experiences in the early postpartum period (6-8 weeks). Midwifery. 2014;30(1):e14–9.
Palmér L. Previous breastfeeding difficulties: an existential breastfeeding trauma with two intertwined pathways for future breastfeeding—fear and longing. Int J Qual Stud Health Well-being. 2019;14(1) [cited 2021 Apr 21] Available from: https://www.tandfonline.com/action/journalInformation?journalCode=zqhw20 .
Francis J, Mildon A, Stewart S, Underhill B, Tarasuk V, Di Ruggiero E, et al. Vulnerable mothers’ experiences breastfeeding with an enhanced community lactation support program. Matern Child Nutr 2020;16(3):16. [cited 2021 Apr 20] Available from: https://onlinelibrary.wiley.com/doi/abs/ https://doi.org/10.1111/mcn.12957
Palmér L, Carlsson G, Mollberg M, Nyström M. Breastfeeding: An existential challenge - Women’s lived experiences of initiating breastfeeding within the context of early home discharge in Sweden. Int J Qual Stud Health Well-being 2010;5(3). [cited 2021 Apr 21] Available from: https://www.tandfonline.com/action/journalInformation?journalCode=zqhw20https://doi.org/ https://doi.org/10.3402/qhw.v5i3.5397
Grant A, Mannay D, Marzella R. ‘People try and police your behaviour’: the impact of surveillance on mothers and grandmothers’ perceptions and experiences of infant feeding. Fam Relationships Soc. 2018;7(3):431–47.
Thomson G, Ebisch-Burton K, Flacking R. Shame if you do - shame if you don’t: women’s experiences of infant feeding. Matern Child Nutr. 2015;11(1):33–46. [cited 2021 Apr 21] Available from: http://doi.wiley.com/ https://doi.org/10.1111/mcn.12148
Dietrich Leurer M, Misskey E. The psychosocial and emotional experience of breastfeeding: reflections of mothers. Glob Qual. Nurs Res. 2015;2:2333393615611654 [cited 2021 Apr 20] Available from: http://www.ncbi.nlm.nih.gov/pubmed/28462320 .
Fahlquist JN. Experience of non-breastfeeding mothers: Norms and ethically responsible risk communication. Nurs Ethics. 2016;23(2):231–241. [cited 2021 Apr 20] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/0969733014561913
Gross TT, Davis M, Anderson AK, Hall J, Hilyard K. Long-term breastfeeding in African American mothers: a positive deviance inquiry of WIC participants. J Hum Lact. 2017;33(1):128–139. [cited 2021 Apr 20] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/0890334416680180
Spencer RL, Greatrex-White S, Fraser DM. ‘I thought it would keep them all quiet’. Women’s experiences of breastfeeding as illusions of compliance: an interpretive phenomenological study. J Adv Nurs. 2015;71(5):1076–1086. [cited 2021 Apr 21] Available from: http://doi.wiley.com/ https://doi.org/10.1111/jan.12592
Twamley K, Puthussery S, Harding S, Baron M, Macfarlane A. UK-born ethnic minority women and their experiences of feeding their newborn infant. Midwifery. 2011;27(5):595–602.
PubMed Google Scholar
Lutenbacher M, Karp SM, Moore ER. Reflections of Black women who choose to breastfeed: influences, challenges, and supports. Matern Child Health J. 2016;20(2):231–9.
Dowling S, Brown A. An exploration of the experiences of mothers who breastfeed long-term: what are the issues and why does it matter? Breastfeed Med. 2013;8(1):45–52. [cited 2021 Apr 20] Available from: http://www.liebertpub.com/doi/ https://doi.org/10.1089/bfm.2012.0057
Fox R, McMullen S, Newburn M. UK women’s experiences of breastfeeding and additional breastfeeding support: a qualitative study of baby Café services. BMC Pregnancy Childbirth 2015;15(1):147. [cited 2021 Apr 20] Available from: http://bmcpregnancychildbirth.biomedcentral.com/articles/ https://doi.org/10.1186/s12884-015-0581-5
Spencer B, Wambach K, Domain EW. African American women’s breastfeeding experiences: cultural, personal, and political voices. Qual Health Res. 2015;25(7):974–987. [cited 2021 Apr 21] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/1049732314554097
McBride-Henry K. The influence of the They: An interpretation of breastfeeding culture in New Zealand. Qual Health Res. 2010;20(6):768–777. [cited 2021 Apr 21] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/1049732310364220
Newman KL, Williamson IR. Why aren’t you stopping now?!’ Exploring accounts of white women breastfeeding beyond six months in the east of England. Appetite. 2018 Oct;1(129):228–35.
Dowling S, Pontin D. Using liminality to understand mothers’ experiences of long-term breastfeeding: ‘Betwixt and between’, and ‘matter out of place.’ Heal (United Kingdom). 2017;21(1):57–75. [cited 2021 Apr 20] Available from: http://journals.sagepub.com/doi/ https://doi.org/10.1177/1363459315595846
Payne D, Nicholls DA. Managing breastfeeding and work: a Foucauldian secondary analysis. J Adv Nurs. 2010;66(8):1810–1818. [cited 2021 Apr 21] Available from: http://doi.wiley.com/ https://doi.org/10.1111/j.1365-2648.2009.05156.x
Keely A, Lawton J, Swanson V, Denison FC. Barriers to breast-feeding in obese women: a qualitative exploration. Midwifery. 2015;31(5):532–9.
Afoakwah G, Smyth R, Lavender DT. Women’s experiences of breastfeeding: A narrative review of qualitative studies. Afr J Midwifery Womens Health. 2013 ;7(2):71–77. [cited 2021 Apr 21] Available from: https://www.magonlinelibrary.com/doi/abs/ https://doi.org/10.12968/ajmw.2013.7.2.71
Símonardóttir S. Getting the green light: experiences of Icelandic mothers struggling with breastfeeding. Sociol Res Online. 2016;21(4):1.
Szafranska M, Gallagher DL. Polish women’s experiences of breastfeeding in Ireland. Pract Midwife. 2016;19(1):30–2 [cited 2021 Apr 21] Available from: https://europepmc.org/article/med/26975131 .
Pratt BA, Longo J, Gordon SC, Jones NA. Perceptions of breastfeeding for women with perinatal depression: a descriptive phenomenological study. Issues Ment Health Nurs. 2020;41(7):637–644. [cited 2021 Apr 21] Available from: https://www.tandfonline.com/doi/abs/ https://doi.org/10.1080/01612840.2019.1691690
Durmazoğlu G, Yenal K, Okumuş H. Maternal emotions and experiences of mothers who had breastfeeding problems: a qualitative study. Res Theory Nurs Pract. 2020;34(1):3–20. [cited 2021 Apr 20] Available from: http://connect.springerpub.com/lookup/doi/ https://doi.org/10.1891/1541-6577.34.1.3
Burns E, Triandafilidis Z. Taking the path of least resistance: a qualitative analysis of return to work or study while breastfeeding. Int Breastfeed J. 2019;14(1):1–13.
Download references
Acknowledgements
The authors would like to acknowledge the assistance of Jackie Stapleton, the University of Waterloo librarian, for her assistance with developing the search strategy used in this review.
Not applicable.
Author information
Authors and affiliations.
School of Public Health Sciences, University of Waterloo, 200 University Ave West, Waterloo, ON, N2L 3G1, Canada
Bridget Beggs, Liza Koshy & Elena Neiterman
You can also search for this author in PubMed Google Scholar
Contributions
BB was responsible for the formal analysis and organization of the review. LK was responsible for data curation, visualization and writing the original draft. EN was responsible for initial conceptualization and writing the original draft. BB and LK were responsible for reviewing and editing the manuscript. All authors read and approved the final manuscript.
Authors’ information
BB is completing her Bachelor of Science (BSc) degree at the School of Public Health Sciences at the University of Waterloo.
LK is completing her Bachelor of Public Health (BPH) degree at the School of Public Health Sciences at the University of Waterloo.
EN (PhD), is a continuing lecturer at the School of Public Health Sciences at the University of Waterloo. Her areas of expertise are in women’s reproductive health and sociology of health, illness, and healthcare.
Corresponding author
Correspondence to Bridget Beggs .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Beggs, B., Koshy, L. & Neiterman, E. Women’s Perceptions and Experiences of Breastfeeding: a scoping review of the literature. BMC Public Health 21 , 2169 (2021). https://doi.org/10.1186/s12889-021-12216-3
Download citation
Received : 23 June 2021
Accepted : 10 November 2021
Published : 26 November 2021
DOI : https://doi.org/10.1186/s12889-021-12216-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breastfeeding
- Experiences
- Public health
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
- Open access
- Published: 12 May 2020
Helpful and challenging aspects of breastfeeding in public for women living in Australia, Ireland and Sweden: a cross-sectional study
- Yvonne L. Hauck 1 , 2 ,
- Lesley Kuliukas 2 ,
- Louise Gallagher 3 ,
- Vivienne Brady 3 ,
- Charlotta Dykes 4 &
- Christine Rubertsson ORCID: orcid.org/0000-0001-7416-6335 5
International Breastfeeding Journal volume 15 , Article number: 38 ( 2020 ) Cite this article
8420 Accesses
15 Citations
36 Altmetric
Metrics details
Breastfeeding in public continues to be contentious with qualitative evidence confirming that women face many challenges. It is therefore important to gain understanding of not only the challenges but also what women perceive is helpful to breastfeed in public.
A cross-sectional study was conducted with women living in Australia, Ireland or Sweden currently breastfeeding or having breastfed within the previous 2 years. Our objective was to explore and compare what women do when faced with having to breastfeed in the presence of someone they are uncomfortable with and what women think is helpful and challenging when considering whether to breastfeed in public. Data were collected in 2018 from an online survey over a 4 week period in each country. Content analysis revealed data similarity and theme names and definitions were negotiated until consensus was reached. How often each theme was cited was counted to report frequencies. Helpful and challenging aspects were also ranked by women to allow international comparison.
Ten themes emerged around women facing someone they were uncomfortable to breastfeed in the presence of with the most frequently cited being: ‘made the effort to be discreet’; ‘moved to a private location’; ‘turned away’ and ‘just got on with breastfeeding’. Nine themes captured challenges to breastfeed in public with the following ranked in the top five across countries: ‘unwanted attention’; ‘no comfortable place to sit’; ‘environment not suitable’; ‘awkward audience’ and ‘not wearing appropriate clothing’. Nine themes revealed what was helpful to breastfeed in public with the top five: ‘supportive network’; ‘quiet private suitable environment’; ‘comfortable seating’; ‘understanding and acceptance of others’ and ‘seeing other mothers’ breastfeed’.
Conclusions
When breastfeeding in public women are challenged by shared concerns around unwanted attention, coping with an awkward audience and unsuitable environments. Women want to feel comfortable when breastfeeding in a public space. How women respond to situations where they are uncomfortable is counterproductive to what they share would be helpful, namely seeing other mothers breastfeed. Themes reveal issues beyond the control of the individual and highlight how the support required by breastfeeding women is a public health responsibility.
The importance of breastfeeding is indisputable and comprehensively supported through recommendations from the World Health Organization (WHO) and United Nations Children’s Fund [ 1 , 2 ]. A recent UNICEF analysis from 123 countries highlighted that 95% of all babies received some breastmilk. However, rates vary between countries with 4% of babies from low and middle income countries never receiving breastmilk increasing to 21% for babies from high income countries [ 1 ]. Variations exist within high income countries with almost 98% of Swedish babies and 92% of Australian babies receiving breastmilk whereas 55% of Irish babies are breastfed [ 1 ].
Research has revealed challenges around women’s experience of breastfeeding, with one challenge being the management of breastfeeding in public. High income countries such as Sweden, Australia, New Zealand, England, and the United States have provided qualitative evidence on women’s experiences of breastfeeding in public. Although most research explored women’s experiences with breastfeeding in general, a recurring theme around the challenges of breastfeeding in public has consistently emerged.
An interpretative phenomenological study with five Australian mothers’ journey of exclusive breastfeeding to 6 months, revealed shared commonalities related to the difficulties with public breastfeeding with an emphasis on the sexuality of breasts [ 3 ]. To achieve exclusive breastfeeding to 6 months, those who could not overcome their awkwardness with the practice offered expressed breastmilk in a bottle to reach their goal [ 4 ]. Another recent Australian study explored views and beliefs of first time breastfeeding mothers and members of their social network and analysed nine family conversations involving 50 participants [ 5 ]. Participant views were that women were required to be “discreet and covered to not expose the breast, select an appropriate place to avoid discomforting others, guard against judgement and protect herself from unwanted male gaze” [ 5 ]. These common challenges experienced when breastfeeding in public were present and heightened for overweight and obese Swedish [ 6 ], American [ 7 ] and New Zealand women [ 8 ] due to larger breasts and difficulties with latching their babies, which made being discreet problematic and feeling ashamed and self-conscious due to exposure.
Research has identified other groups of breastfeeding women with heightened vulnerability around public breastfeeding which includes African immigrants and refugees. The breastfeeding experiences of 31 African refugee women living in Australia revealed how women perceived the lack of visibility of public breastfeeding contributed to stigma and shame [ 9 ]. Difficulties and being discouraged to breastfeed in public were also noted by 15 African American women who shared issues around sustaining their breastfeeding [ 10 ] and 22 African American mothers who felt stigmatised based upon ‘spectators’ actions’ [ 11 ].
Additional vulnerable groups included young mothers and those living in a country where legal protection to breastfeed in public was limited. An Australian study of 24 young (17 to 25 years of age) mothers focused upon their need for information and support, and found that when breastfeeding in public they felt more exposed as a ‘young mum’ which brought more attention to them: any attention was noted as predominantly negative [ 12 ]. Even British women who are legally protected to breastfeed in public for up to 6 months, but chose to breastfeed longer than 6 months, experienced suspicion and disapproval [ 13 ]. Eight women in this qualitative study shared how they experienced ‘really horrible looks’, ‘stigma from families and community’ and ‘feeling quite exposed’ (p.231).
The influence of perceived cultural norms around breastfeeding in public was also highlighted during interviews with 27 Chinese mothers, who expressed their struggle and embarrassment, given that exposing breasts in their culture was considered unacceptable and ‘uncivilized’ [ 14 ]. Women in Ireland ( n = 7) who shared experiences of being in a public health nurse led support group, valued being in a breastfeeding group that felt like a ‘cocoon of normality’ in a infant formula feeding culture, where breastfeeding was something to be ashamed of [ 15 ].
Research highlighting the experiences of women breastfeeding in public provides insight into this phenomenon whilst exploring breastfeeding experiences in general. Findings have been generated from qualitative research capturing the stories of breastfeeding women across international contexts and have predominately emphasised the negative or challenging aspects of the experience. Although breastfeeding rates to 6 months differ between Sweden (72%), Australia (60%) [ 16 ] and Ireland (26 to 29%) [ 17 , 18 ], similar categories were revealed when women from these countries shared what assisted them to breastfeed [ 19 ]. Informal face to face support and maternal determination ranked within the top five categories across the three countries [ 19 ]. Although regarding breastfeeding as a cultural norm was cited by women living in Australia, Ireland and Sweden, this category was ranked eight out of ten and focused upon the importance of having a strong family history of breastfeeding and having this reinforced with key role models. The issue of managing breastfeeding in public was not acknowledged.
The challenges around breastfeeding in public have been recognised in qualitative studies with small numbers of participants from high income countries. Women’s perceptions of what is helpful when considering whether to breastfeed in public have not been researched and presents a gap in knowledge. Greater insight into what breastfeeding women perceive can help and challenge them can inform initiatives and schemes to counter the challenges and enhance factors to better support their efforts to breastfeed in public. Due to the variation in breastfeeding across high income countries we chose two countries with high initiation rates (Australia and Sweden) and a third with lower rates (Ireland) [ 1 ]. Our international study focused on exploring and comparing what women from three high income countries perceive as helpful or challenging when breastfeeding in public, in addition to revealing what they do when faced with having to breastfeed in the presence of someone they are uncomfortable with.
A cross-sectional study was undertaken using an online survey with women living in Australia, Ireland and Sweden. Ethical approval to conduct the study was granted by Curtin University Human Research Ethics Committee in Australia (HRE2018–0037), Research and Ethics Committee, School of Nursing and Midwifery, Trinity College in Ireland (COM_35_17/18) and the Advisory Committee for Research Ethics in Health Education Lund University in Sweden (Reference Number 50–18). Women who were living in Australia, Ireland or Sweden and were currently breastfeeding or had breastfed within the previous 2 years were invited to participate in the online survey through social media.
Three specific research questions were posed: 1) What do women do when they are faced with having to breastfeed in front of someone they are uncomfortable with, 2) What do women think was most helpful when considering whether to breastfeed in public and 3) What do women think was most challenging when considering whether to breastfeed in public? Women were then asked to rank their responses to questions 2) and 3) as first, second or third in importance based upon what they felt were the most helpful and challenging aspects. The online survey was presented on a user-friendly platform suitable for completion on a mobile phone (Qualtrix in Australia, SurveyMonkey in Ireland and Sweden). In addition to the three open ended questions noted above, demographic data on maternal age, education level, number of children / number of children ever breastfed, and whether they were still breastfeeding their youngest child at the time of survey completion was collected.
A poster with a link to the online survey was developed for each country and with university approval circulated through social media. The initial screen was an information letter which included the inclusion criteria. Women had to confirm that they were living in the specified country, met the inclusion criteria and consented to participate prior to accessing the online survey. The original poster was included in a maternity consumer Facebook page in Australia that encouraged women to share with other mothers and within 24 h, over 2600 women had completed the online survey. In Sweden the translated poster was included in several Facebook pages mainly with parental interest such as Home parents network, Public breastfeeding, The breastfeeding help group, Baby slings and Close parenting. In Ireland a link to an online survey was posted on popular Breastfeeding support pages on Facebook. The post provided study details and clicking the link brought women to an information page where they consented to participate before commencing the survey.
Data were collected over a four-week period in 2018 in each country (March in Australia, April in Ireland and December in Sweden). Originally, we anticipated leaving the online survey open for 3 months but due to the overwhelming response from women in all three countries, data collection was ceased after a four-week period.
Responses to the three open ended questions provided rich data that was analysed using content analysis, which is often used with textual data from open-ended survey questions [ 20 ]. Responses to each question were exported from the online platforms into separate Word documents for analysis by investigators in each country. Content analysis involves description at a surface level around individual shared experiences presented in participants’ own words [ 21 ]. A systematic coding and categorising approach was conducted with this textual information to determine common themes [ 22 ]. Content analysis was undertaken by reviewing all responses from women who responded and continued until data saturation became apparent. Initial thematic analysis was conducted separately by two investigators in each country. Tentative themes from data in each country were then shared amongst the international team and it became apparent that themes were more similar than different. Therefore, to facilitate comparison between breastfeeding women living in the three countries, we negotiated final theme names and definitions until a consensus agreement was reached.
Once the final themes were confirmed between countries, we were then able to consider the possibility of counting how often each theme was cited and reported frequencies using descriptive statistics. Due to the numbers of women responding and after themes were confirmed separate SPSS databases were developed and data were then manually entered under each theme. This process facilitated counting how often each theme was cited and ranked as first, second or third in relation to being helpful or challenging when considering breastfeeding in public. At this stage all responses from women in Ireland and Sweden were entered to determine frequencies. As the Australian sample was up to four times larger, a systematic process to collect a representative sample (every second or third entry) was adopted. Statistics were only chosen to describe frequencies of the themes as our intention was not to make inferences or generalizations between women in each country.
Survey respondents included 10,910 women living in Australia, 1835 living in Ireland and 1520 living in Sweden. A summary of characteristics such as age, education level, parity, number of children ever breastfed and whether they were still breastfeeding when completing the survey are presented in Table 1 . The mean age of women living in Ireland was older (34.9 years) compared to women in Australia (32.3 years) or Sweden (32.8 years). The sample reflects women with a high level of education as 89.2% of Irish women had a university or college degree compared to 82.4% from Sweden and 70.6% from Australia. The majority (83.0%) of women living in Australia were born in Australia with 8.4% born in Europe. The majority (81.7%) of women living in Ireland were born in Ireland with 13.7% born in Europe. The majority (93%) of women living in Sweden were born in Sweden with 6% born in Europe.
Faced with having to breastfeed in front of someone they are uncomfortable with
A total of 4742 women living in Australia, 1139 living in Ireland and 1348 living in Sweden responded to this question. Content analysis revealed ten themes commonly cited by women from all three countries. The themes in no particular order were: Made the effort to be discreet; Moved to a private location; Turned away; Just got on with breastfeeding; Never felt uncomfortable; Not my problem; Flagged their intention to breastfeed; Tried to avoid the situation; Used expressed breastmilk (EBM) or infant formula and Had someone supportive with them. A definition of each theme with supporting quotes from women in Australia, Ireland and Sweden is provided in Table 2 .
All responses from women in Ireland ( N = 1139) and Sweden ( N = 1348) were entered into a statistical package to determine frequencies for each response being cited by women from each country. To achieve a number for comparison with Irish and Swedish data, every third response was entered from Australia data ( N = 1600). ‘Made the effort to be discreet’ was cited most frequently across all countries (62.1% in Australia; 44.9% in Ireland; 38.1% in Sweden). The frequencies for each theme are presented in an approximate descending order in Table 3 and were comparable across each country. However, one theme ‘Just got on with breastfeeding’ ranked third for women in Australia (22.8%) and Sweden (20.0%) and fourth at 9.0% for Irish women. Use of expressed breast milk (EBM) or infant formula was ninth for Australian women (1.4%) and Irish women (1.1%) but equal tenth for Swedish women (0.04%).
Challenges to breastfeeding in public
A total of 4596 women living in Australia, 1648 living in Ireland and 1220 living in Sweden provided a response to what was challenging about breastfeeding in public. Content analysis revealed nine themes commonly cited by women across the three countries. The themes were: Unwanted attention; No comfortable place to sit; Environment not suitable; Awkward audience, Not wearing appropriate clothing; Potential for baby to be distracted; Struggling with feeding issues; Managing a distressed baby and Having to manage other children. A definition of each theme with supporting quotes from women in Australia, Ireland and Sweden is provided in Table 4 .
Women were asked to rank their responses to challenges as first, second or third to reflect their importance (Table 5 ). All responses from women in Ireland ( n = 1648) and Sweden ( n = 1220) were entered into a statistical package to determine frequencies and to achieve a number for comparison, every second response was entered from Australia data ( n = 2332). ‘Unwanted attention’ was ranked as first by women in Australia (27.0%) and Sweden (38.2%) with the ‘environment not suitable’ ranked highest by women in Ireland (29.0%) with ‘unwanted attention’ marginally lower at 28.3%. ‘No comfortable place to sit’ was ranked second most frequently (20.1%) by Australian women, third (17.0%) by Irish women and fourth (6.6%) by Swedish women. “Having to manage other children’ was ranked lowest across the countries (1.9, 1.0, 0.2%)”.
One point of difference around perceived challenges noted in the data involved comments around sexism and was expressed by 90 women in Sweden. Examples of comments included: Peoples view on breasts, the sexism of breasts, how men look at you while breastfeeding, to get “undressed” in public and the feeling of being “naked” while breastfeeding. This terminology was not found in comments from women in Ireland or Australia and therefore was not considered a common theme.
Helpful to breastfeeding in public
A total of 4924 women living in Australia, 1744 living in Ireland and 1250 living in Sweden provided a response to what was helpful when considering whether to breastfeed in public. Content analysis revealed nine themes commonly cited by women across the three countries. The themes were: Supportive network; Quiet private suitable environment; Comfortable seating; Understanding and acceptance of others; Seeing other mothers breastfeed; Wearing suitable clothing or having a cover; Preparation and confidence; Breastfeeding is overtly welcomed; and Knowledge of mother’s and children’s rights. A definition of each theme with supporting quotes from women in all three countries is provided in Table 4 .
In a similar process to the challenges, women were asked to rank their responses to what was helpful as first, second or third (Table 5 ). All responses from women in Ireland ( n = 1744) and Sweden ( n = 1250) and every second response from Australia data ( n = 2466) were entered into a statistical package to determine frequencies for each response from women from each country. ‘Supportive network’ was ranked highest by women in Australia (18.6%) and Ireland (28.7%). ‘Understanding and acceptance of others’ ranked highest in Sweden (25.7%), and was second in Ireland (16.4%) and fourth in Australia (15.3%). ‘Seeing other mothers breastfeed’ was comparable across countries (8.2, 11.8, 10.1%) and ‘Knowledge of rights’ ranked lowest in Australia and Ireland (2.7 and 1.4%) whereas ‘Wearing suitable clothing or having a cover’ ranked lowest in Sweden (4.5%).
In summary, although ten themes emerged around strategies women used when facing someone they were uncomfortable to breastfeed in the presence of, the four most frequently cited were: ‘made the effort to be discreet’; ‘moved to a private location’; ‘turned away’ and ‘just got on with breastfeeding’. Nine themes captured challenges to breastfeed in public with ‘unwanted attention’ ranked highest for women in Australia and Sweden whereas ‘environment not suitable’ ranked highest for women in Ireland. Nine themes addressed what was helpful to breastfeed in public and ‘supportive network’ ranked highest for women in Australia and Ireland compared to ‘quiet private suitable environment’ for women in Sweden. ‘Seeing other mothers breastfeed’ ranked in the top five across all three countries.
Challenges to breastfeeding in public identified in this study are supported by previous research. Concepts noted in qualitative studies from seven countries focused on exposure of the body, feeling uncomfortable and vulnerable, embarrassment, perceived lack of acceptability, fear of confrontation or actual negative reactions, positioning challenges, being discreet, and minimising feeding around a particular audience. This synopsis of concepts reflects study findings from Australia [ 23 ], Ireland [ 15 ], Sweden [ 6 ], the United States [ 7 ], China [ 14 ], Canada [ 24 ] and the United Kingdom [ 25 , 26 ]. However, our findings offer further information around additional challenges mothers considered when deciding to breastfeed in public such as the ‘suitability of the environment’, ‘having a comfortable place to sit’, the ‘potential for the baby to be distracted’, ‘managing a distressed baby’, and ‘having to manage other children’. Innovative strategies to address these challenges warrant attention. One example that could be shared and replicated to other local contexts includes the use of technology. A recent study analysed reviews by British mothers on a ‘FeedFinder App’ which involved women sharing information on facilities, service, level of privacy and venue quality to assist decisions around where to breastfeed in public [ 27 ]. This innovation where women assist other women offers an empowering strategy which has implications for business owners as they would be motivated to ensure their facility was positively rated to boost rather than negatively impact their customer base.
Themes that were captured as enablers represent a novel approach with potential modifiable findings to enhance women’s experience of breastfeeding in public. Findings provide insight into areas to target changes and improvements to better support breastfeeding mothers which aligns with the salutogenic model and what contributes to the promotion and maintenance of health. Women’s sense of coherence delineated in the salutogenic model has been applied to infant feeding experiences using constructs such as comprehensibility (belief in understanding challenges), manageability (having sufficient resources) and meaningfulness (desire to respond to challenge) [ 28 ].
Some themes were the reverse of the challenges such as having a ‘supportive network’, the ‘understanding and acceptance of others’, a ‘quiet private suitable environment’, ‘comfortable seating’ and ‘having clothing or a cover’ if the mother chooses to be discreet. Having a supportive network extends beyond face to face contact to locating support through social media. A qualitative study of exclusive breastfeeding with 30 New Zealand mothers found that smartphone apps are a genuine option for promoting breastfeeding. Information is accessed and shared on Facebook amongst breastfeeding mothers who may not have a close relationship but are encouraged by a sense of community [ 29 ]. Even closed Facebook groups such as those hosted by the Australian Breastfeeding Association have been found to provide not only informational but emotional support to breastfeeding women [ 30 ]. Other themes identified in this international study highlight strategies that could be further promoted, such as signage to ‘overtly welcome breastfeeding mothers’, improving opportunities for mothers to ‘see other mothers breastfeeding’, and ensuring women and the general community are aware of ‘mothers’ and ‘children’s’ rights.
Specific themes in our findings address issues that are beyond the control of the individual and require addressing public attitudes to breastfeeding, so women encounter supportive networks that demonstrate understanding and acceptance of breastfeeding in public. Recognition that breastfeeding is a public health responsibility has been supported by evidence suggesting the barriers to breastfeeding extend beyond the individual mother to societal influences [ 31 ]. Increasing awareness of mothers’ and children’s rights around breastfeeding may present a necessary tactic to inform and educate the public of the importance of breastfeeding to our society and our future generations. Signage that overtly welcomes breastfeeding, that provides an environment with comfortable seating, gives a message that endorses a culture where breastfeeding is seen as ‘normal’. Community involvement is essential for any change process as illustrated in a recent inquiry approach to discover how communities can better support breastfeeding. Community conversation workshops were recently undertaken with Australian parents, grandparents, children’s services, local government, health services and retail owners [ 32 ]. Two related themes were revealed acknowledging the importance of PLACE: ‘sometimes a PLACE to breastfeed’ and ‘the parent room: a hidden and unsafe PLACE to breastfeed’. Although characteristics of communities that provided a ‘sanctuary’ were noted, the participants indicated that breastfeeding in public was rarely observed which supports the theme ‘seeing other mothers breastfeed’ as being an important enabling theme.
‘Made the effort to be discreet’ was the most frequently cited strategy that women across Australia, Ireland and Sweden noted when faced with having to breastfeed in front of someone they are uncomfortable with. Other themes included ‘moving to a private location’, ‘turning away’, and ‘tried to avoid the situation’ which are all activities counterproductive to the helpful theme of wanting to ‘see other mothers breastfeed’. A recent discussion paper on the requirement to justify breastfeeding in public suggests that if breastfeeding could be recognised as a “family way of life” and positive interaction this stance would support a “more right to breastfeeding in public without social sanction, whether one is able to breastfeed discreetly or not” [ 33 ].
Facilitating a culture where breastfeeding in public is acceptable and women feel comfortable require initiatives to address societal attitudes given that ‘unwanted attention’ and ‘awkward audience’ also ranked within the top four themes negatively influencing a decision to breastfeed in public. Interventions to change societal attitudes have met some success and highlight strategies that can be shared internationally. For example, a prime-time television clip depicting public breastfeeding decreased the extent to which American students believed breastfeeding should be private while improving attitudes and support for breastfeeding in public [ 34 ]. Use of a music video parody with young Canadian adults found that shorter intervals between seeing the video and shorter intervals between follow-up ratings measured increasing comfort levels thereby reinforcing the importance of being exposed to breastfeeding [ 35 ]. Finally, another study included use of posters to enhance comfort levels with members of the Canadian public surveyed at shopping centers and found that only 51.9% were comfortable with a woman breastfeeding anywhere in public but this increased to 84.5% in a doctor’s office or 81.4% in a park [ 36 ]. There were significant improvements in comfort levels following viewing of promotional posters depicting breastfeeding in a doctor’s office and restaurant.
The influence of seeing a woman breastfeed extends beyond being an enabler to existing breastfeeding women and can influence the decision whether to breastfeed at all. A systematic review focused on factors influencing expectant parents infant feeding choice revealed a bias towards negative factors relating to the breastfeeding decision as parents went through a process of weighing reasons for and against breastfeeding [ 37 ]. Factors influencing choice of infant feeding method included female role models, family and support network and feeding in front of others/public. Expectant parents are already aware and thinking about how they could manage breastfeeding in public [ 37 ]. A longitudinal study with 259 Scottish first time mothers who had never breastfed and agreed with a statement that ‘it was lovely to see her breastfeed’ were six times more likely to intend to breastfeed [ 38 ].
Coordinated action and targeted strategies must consider all factors to address the challenges women experience when breastfeeding in public. To facilitate the promotion and support of breastfeeding, all influencing factors must be acknowledged within an ecological model, such as the mother and infant dyad, the family, the health care system, the community and societal and culture factors [ 39 ]. Breastfeeding represents a complex experience. Results from a systematic review and meta-analysis recommended that multicomponent interventions be implemented across the childbirth continuum to include antenatal and postnatal periods, hospital and community contexts and the involvement of health professionals [ 40 ]. A multifaceted approach where support needs to be layered was recommended in a Health Promotion Strategic Framework in Australia to include mothers, family and community [ 41 ]. Awareness of this approach is apparent in the Australian National Breastfeeding Strategy that endorses the need for a social marketing campaign targeting specific audiences to change attitudes and behaviours regarded as unsupportive of breastfeeding [ 42 ].
More women from Sweden than Australia or Ireland shared comments about sexualization of the female body, the ‘male gaze’, and a feeling of being attributed to a sex object when breastfeeding. Without existing evidence, we cannot speculate the reason for the differences between countries and why Swedish women were more aware and outspoken about sexism. Therefore additional international research is warranted around this issue to further explore how awareness and expression of this concern may differ depending upon a particular context or culture.
Limitations to our international findings must acknowledge the demographic characteristics of the international samples. The women who responded were recruited through social media and therefore are connected to social networks; whether this connection is supportive or not cannot be determined. The sample strongly represents highly educated women, who are in their thirties with one child living in high income countries with varying breastfeeding initiation and prevalence rates. Participant characteristics were not unexpected as populations recognised as being more at risk of not breastfeeding include women under 25 years of age, with low socio-economic status, and low education levels [ 42 ]. Strategies to target hard to reach participants for research also acknowledge younger women and reasons cited for not completing assessments which include lack of time and loss of interest [ 43 ]. However, the response rate, achieved within 4 weeks of releasing the survey, does highlight the importance and passion that women feel toward the topic of breastfeeding in public, particularly in the Australian context.
The most challenging theme for mothers in Australia and in Sweden were ‘unwanted attention’ and for mothers in Ireland it was ‘environment not suitable. Women have indicated that a feeling of awkwardness and discomfort discourages breastfeeding in public. A ‘supportive network’ was cited as most helpful for women in Australia and Ireland with ‘understanding and acceptance of others’ being more helpful for women in Sweden. Breastfeeding women want to feel comfortable, accepted, supported and welcomed. Understanding the issues that help and challenge breastfeeding in public and addressing the concerns women have raised in this international study is one step forward. Encouraging and welcoming women to breastfeed in public may be one strategy that is helpful to women and promotes societal change to norms where it is hidden and an uncommon sight.
Availability of data and materials
The datasets generated and analysed during the current study are not publicly available as they are not all in English and were not combined but are available from the corresponding author on reasonable request.
United Nations Children’s Fund. Breastfeeding: a mother’s gift, for every child. New York: United Nations Children's Fund; 2018. p. 20. Available from: https://www.unicef.org/publications/files/UNICEF_Breastfeeding_A_Mothers_Gift_for_Every_Child.pdf .
Google Scholar
World Health Organization. Breastfeeding. Geneva: World Health Organization; 2019. Available from: https://www.who.int/nutrition/topics/exclusive_breastfeeding/en/ . [cited 2019 Aug 16].
Charlick SJ, Pincombe J, McKellar L, Gordon AL. Navigating the social complexities of breastfeeding: an interpretative phenomenological analysis of women's experiences. Evid Based Midwifery. 2018;16(1):21–8.
Charlick SJ, McKellar L, Gordon AL, Pincombe J. The private journey: an interpretative phenomenological analysis of exclusive breastfeeding. Women Birth. 2019;32(1):e34–42.
Article PubMed Google Scholar
Sheehan A, Gribble K, Schmied V. It's okay to breastfeed in public but. Int Breastfeed J. 2019;14:24.
Article PubMed PubMed Central Google Scholar
Claesson IM, Larsson L, Steen L, Alehagen S. “you just need to leave the room when you breastfeed” breastfeeding experiences among obese women in Sweden - a qualitative study. BMC Pregnancy Childbirth. 2018;18:39.
McKenzie SA, Rasmussen KM, Garner CD. Experiences and perspectives about breastfeeding in “public”: a qualitative exploration among normal-weight and obese mothers. J Hum Lact. 2018;34(4):760–7.
PubMed Google Scholar
Massov L. Clinically overweight and obese mothers and low rates of breastfeeding: exploring women's perspectives. NZ Coll Midwives J. 2015;51:23–9.
Article Google Scholar
Gallegos D, Vicca N, Streiner S. Breastfeeding beliefs and practices of African women living in Brisbane and Perth, Australia. Matern Child Nutr. 2015;11(4):727–36.
Lewallen LP, Street DJ. Initiating and sustaining breastfeeding in African American women. J Obstet Gynecol Neonatal Nurs. 2010;39(6):667–74.
Owens N, Carter SK, Nordham CJ, Ford JA. Neutralizing the maternal breast: accounts of public breastfeeding by African American mothers. J Fam Issues. 2018;39(2):430–50.
Noble-Carr D, Bell C. Exposed: younger mothers and breastfeeding. Breastfeed Rev. 2012;20(3):27–38.
Newman KL, Williamson IR. Why aren’t you stopping now?!’ exploring accounts of white women breastfeeding beyond six months in the east of England. Appetite. 2018;129:228–35.
Zhao Y, Ouyang YQ, Redding SR. Chinese women's experiences, emotions and expectations of breast-feeding in public: a qualitative study. Public Health Nutr. 2018;21(8):1565–72.
Leahy-Warren P, Creedon M, O'Mahony A, Mulcahy H. Normalising breastfeeding within a formula feeding culture: an Irish qualitative study. Women Birth. 2017;30(2):e103–e10.
Save the Children. Nutrition in the first 1000 days: state of the world’s mothers. London: Save the Children; 2012. p. 70. Available from: https://www.savethechildren.org/content/dam/usa/reports/advocacy/sowm/sowm-2012.pdf .
Begley C, Gallagher L, Carroll M, Clarke M, Millar S. The National Infant Feeding Survey. Dublin: Trinity College; 2008. Available from: https://nursing-midwifery.tcd.ie/assets/publications/pdf/report-of-the-national-infant-feeding-survey.pdf . [cited 2019 September 2].
Department of Health. Growing Up in Ireland: National Longitudinal Study of Children. The Infants and Their Families - Infant Cohort. Dublin: Department of Health, Ireland; 2010. Available from: http://www.thehealthwell.info/node/773789 . [cited 2019 September 2].
Hauck YL, Blixt I, Hildingsson I, Gallagher L, Rubertsson C, Thomson B, et al. Australian, Irish and Swedish women's perceptions of what assisted them to breastfeed for six months: exploratory design using critical incident technique. BMC Public Health. 2016;16(1):1067.
Kondracki NL, Wellman NS, Amundson DR. Content analysis: review of methods and their applications in nutrition education. J Nutr Educ Behav. 2002;34(4):224–30.
Willis DG, Sullivan-Bolyai S, Knafl K, Cohen MZ. Distinguishing features and similarities between descriptive phenomenological and qualitative description research. West J Nurs Res. 2016;38(9):1185–204.
Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs Health Sci. 2013;15(3):398–405.
Hauck YL. Factors influencing mothers’ decision to breastfeed in public. Breastfeed Rev. 2004;12(1):15–23.
Sheeshka J, Potter B, Norrie E, Valaitis R, Adams G, Kuczynski L. Women's experiences breastfeeding in public places. J Hum Lact. 2001;17(1):31–8.
Article CAS PubMed Google Scholar
Mahon-Daly P, Andrews GJ. Liminality and breastfeeding: women negotiating space and two bodies. Health Place. 2002;8(2):61–76.
Scott JA, Mostyn T, Members of the Greater Glasgow breastfeeding initiative management team. Women’s experiences of breastfeeding in a bottle-feeding culture. J Hum Lact. 2003;19(3):270–7.
Simpson E, Garbett A, Comber R, Balaam M. Factors important for women who breastfeed in public: a content analysis of review data from FeedFinder. BMJ Open. 2016;6(10):e011762.
Thomson G, Dykes F. Women’s sense of coherence related to their infant feeding experiences. Matern Child Nutri. 2011;7(2):160–74.
Alianmoghaddam N, Phibbs S, Benn C. “I did a lot of Googling”: a qualitative study of exclusive breastfeeding support through social media. Women Birth. 2019;32(2):147–56.
Bridges N, Howell G, Schmied V. Exploring breastfeeding support on social media. Int Breastfeed J. 2018;13:22.
Brown A. Breastfeeding as a public health responsibility: a review of the evidence. J Hum Nutr Diet. 2017;30(6):759–70.
Schmied V, Burns E, Sheehan A. Place of sanctuary: an appreciative inquiry approach to discovering how communities support breastfeeding and parenting. Int Breastfeed J. 2019;14:25.
Woollard F. Requirements to justify breastfeeding in public: a philosophical analysis. Int Breastfeed J. 2019;14:26.
Foss KA, Blake K. “It's natural and healthy, but I don't want to see it”: using entertainment-education to improve attitudes toward breastfeeding in public. Health Commun. 2019;34(9):919–30.
Austen EL, Beadle J, Lukeman S, Lukeman E, Aquino N. Using a music video parody to promote breastfeeding and increase comfort levels among young adults. J Hum Lact. 2017;33(3):560–9.
Vieth A, Woodrow J, Murphy-Goodridge J, O'Neil C, Roebothan B. The ability of posters to enhance the comfort level with breastfeeding in a public venue in rural Newfoundland and Labrador. J Hum Lact. 2016;32(1):174–81.
Roll CL, Cheater F. Expectant parents’ views of factors influencing infant feeding decisions in the antenatal period: a systematic review. Int J Nurs Stud. 2016;60:145–55.
Hoddinott P, Kroll T, Raja A, Lee AJ. Seeing other women breastfeed: how vicarious experience relates to breastfeeding intention and behaviour. Matern Child Nutr. 2010;6(2):134–46.
Tiedje LB, Schiffman R, Omar M, Wright J, Buzzitta C, McCann A, et al. An ecological approach to breastfeeding. MCN Am J Matern Child Nurs. 2002;27(3):154–61 quiz 62.
Kim SK, Park S, Oh J, Kim J, Ahn S. Interventions promoting exclusive breastfeeding up to six months after birth: a systematic review and meta-analysis of randomized controlled trials. Int J Nurs Stud. 2018;80:94–105.
Chronic Disease Prevention Directorate. Western Australian health promotion strategic framework 2017–2021. Perth: Department of Health, Western Australia; 2017.
Council of Australian Governments Health Council. Australian National Breastfeeding Strategy: 2019 and Beyond. Canberra: ACT. Department of Health; 2019. Available from: https://apo.org.au/sites/default/files/resource-files/2019/08/apo-nid253556-1379891.pdf . [cited 2019 December 20].
Di Noia J, Schultz S, Monica D. Recruitment and retention of WIC participants in a longitudinal dietary intervention trial. Contemp Clin Trials Commun. 2019;16:100438.
Download references
Acknowledgements
We thank all the women who contributed to the survey.
No external funding was obtained for this work. Open access funding provided by Lund University.
Author information
Authors and affiliations.
Department of Nursing and Midwifery Education and Research, King Edward Memorial Hospital, Perth, Western Australia, Australia
Yvonne L. Hauck
School of Nursing, Midwifery and Paramedicine, Curtin University, Perth, Western Australia, Australia
Yvonne L. Hauck & Lesley Kuliukas
School of Nursing and Midwifery, Trinity College Dublin, Dublin, D02 T283, Ireland
Louise Gallagher & Vivienne Brady
Skåne University Hospital, Lund, Sweden
Charlotta Dykes
Institute of Health Sciences, Medical Faculty, Lund University, Lund, Sweden
Christine Rubertsson
You can also search for this author in PubMed Google Scholar
Contributions
YH, LK, LG & CR contributed to the conception and study protocol. YH, LK, LG, VB, CD & CR all contributed to the analysis of data. The draft manuscript was developed by YH & LK with critical revisions contributed by LG, VB, CD & CR. All authors provided final approval of the version submitted for publication and are accountable to the accuracy and integrity of the work.
Corresponding author
Correspondence to Christine Rubertsson .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval to conduct the study was granted by Curtin University Human Research Ethics Committee in Australia (HRE2018–0037), Research and Ethics Committee, School of Nursing and Midwifery, Trinity College in Ireland (COM_35_17/18) and the Advisory Committee for Research Ethics in Health Education Lund University in Sweden (Reference Number 50–18).
Consent for publication
No individual person’s data in any form (individual details, images or videos) is contained in this manuscript.
Competing interests
We have no competing interests to be declared.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions

About this article
Cite this article.
Hauck, Y.L., Kuliukas, L., Gallagher, L. et al. Helpful and challenging aspects of breastfeeding in public for women living in Australia, Ireland and Sweden: a cross-sectional study. Int Breastfeed J 15 , 38 (2020). https://doi.org/10.1186/s13006-020-00281-0
Download citation
Received : 31 October 2019
Accepted : 22 April 2020
Published : 12 May 2020
DOI : https://doi.org/10.1186/s13006-020-00281-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breastfeeding in public
- Decision-making
- Experiences
International Breastfeeding Journal
ISSN: 1746-4358
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int Breastfeed J
- PMC10797811

Mothers’ experiences and perceptions of breastfeeding peer support: a qualitative systematic review
Yuanyuan yang.
1 Peking University School of Nursing, Beijing, China
2 Peking University Health Science Centre for Evidence-Based Nursing, Beijing, China
Huijuan Liu
3 Neonatal Disease Diagnosis and Treatment Center, Fifth Medical Center of Chinese People’s Liberation Army General Hospital, Beijing, China
Jingwen Meng
4 Peking University First Hospital, Beijing, China
Associated Data
All data generated or analyzed during this study are contained within the manuscript.
The global issue of low breastfeeding rates has been widely reported. Quantitative studies have shown the positive effects of peer support on breastfeeding. However, the experiences of mothers who receive breastfeeding peer support have been found to vary. To date, no systematic qualitative summary has been conducted to document the impact of peer support, nor to provide advice for its implementation from the perspective of breastfeeding mothers. This review aims to systematically synthesize qualitative findings on mothers’ experiences of breastfeeding peer support to provide evidence for optimizing peer support services and ultimately enhancing their role in promoting breastfeeding.
PubMed, Embase, Cochrane Library, Ovid, Web of Science, CINAHL, China National Knowledge Infrastructure (CNKI), WanFang Datebase, VIP Database and Chinese Biomedical Database (CBM) were searched from the inception of each database until January 2023, to collect qualitative studies and mixed methods studies that included qualitative findings on mothers’ experiences with breastfeeding peer support. The Joanna Briggs Institute Qualitative Assessment and Review Instrument (JBI-QARI) was used to extract data and evaluate the quality of the included articles. The meta-integration method was used to explain and integrate the research findings. The review process was carried out by two authors independently, and the disagreements were resolved through consensus.
A total of 15 articles were included in the study, consisting of 13 qualitative studies and 2 mixed methods studies. The analysis identified four integrated themes: (1) obtaining psycho-emotional support; (2) acquiring knowledge and skills; (3) expectations for breastfeeding peer support; and (4) feeding perceptions and behavior change. It should be noted that the articles reviewed are in English and mostly originate from developed countries or regions. Therefore, the generalizability of the integrated findings to underdeveloped regions or non-English speaking countries may be limited.
Mothers perceived that peer support had a positive impact on breastfeeding. To improve the effectiveness of peer support in promoting breastfeeding, it is important to consider the individual needs of each mother. It is recommended that peer support services should be standardized in the future, including the accreditation, training, supervision, and management of peer supporters.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13006-024-00614-3.
The World Health Organization (WHO) and UNICEF advocate that breastfeeding should continue until two years of age or longer due to significant benefits to both the mother and infant [ 1 ]. However, low breastfeeding rates are a global concern. According to the report released by WHO, the initiation rate of breastfeeding within one hour of birth was 47% in 2015–21, against the target of 70%. The exclusive breastfeeding rate at 6 months is 48%, falling short of the target of 70% by 2030. By two years of age, the breastfeeding rate drops to 45% [ 2 ]. Generally, breastfeeding duration is shorter in high-income countries than in low- and middle-income countries [ 3 ]. Therefore, efforts towards supporting breastfeeding must be amplified to reach the 2030 targets.
In recent years, the role of peer support in breastfeeding promotion has been recognized in several countries. Peer support isdefined as ‘the provision of emotional, appraisal, and informational assistance by a created social network member who possesses experiential knowledge of a specific behavior or stressor and similar characteristics as the target population [ 4 ]. Breastfeeding Peer Supporters, also known as Breastfeeding Peer Counselors (BPCs), are women with breastfeeding experience who volunteer to provide breastfeeding counseling to others in the community or hospital where they live [ 5 ]. Breastfeeding peer supporters are identified through selection or recruitment by health professionals, or through self-referral. Patterns of peer support vary widely around the world. Peer supporters also vary in the amount of training they receive.
There is evidence from quantitative studies that peer support is effective in supporting breastfeeding practices. A 2017 systematic review found that community-based peer support for mothers not only increased the duration of exclusive breastfeeding, particularly for infants aged three to six months in low- and middle-income countries, but also encouraged mothers to initiate breastfeeding early and prevented newborn prelacteal feeding of newborns [ 6 ]. A UK study found that one-to-one breastfeeding support provided by paid peer supporters and targeted at young mothers in the antenatal and postnatal periods was beneficial in increasing breastfeeding initiation and prevalence at two weeks [ 7 ]. Further studies have been conducted to explore what forms of peer support are feasible, acceptable, and effective. A home-based postnatal breastfeeding peer support programme delivered over six months in Hong Kong, China, was reported to be acceptable to women, but a more flexible approach to the number of visits and modification of the intensity of the intervention would be needed to increase retention [ 8 ]. In Australia, the RUBY trial conducted by Forster et al. demonstrated that the implementation and delivery of a proactive telephone breastfeeding peer support intervention was effective, feasible, sustainable and cost-effective [ 9 , 10 ].
To better understand ways to optimally implement peer support, qualitative studies of mothers’ experience have been conducted. One study in Lebanon focused on peer support during antenatal breastfeeding education through home visits and phone calls [ 11 ], while a study in the UK focused on peer support through face-to-face coaching, phone calls, and text messages during both the antenatal and postnatal periods [ 12 ]. Mothers’ perceptions of the role of peer support varied between studies. Some studies found that peer support led to mothers perceiving that their knowledge about breastfeeding had improved [ 11 , 12 ]; and Quinn’s study identified the impact of peer support on mothers’ social connectedness and the likelihood of mothers’ willingness to become breastfeeding advocates [ 13 ].
As can be seen, the timing, form, and role of peer support as well as mothers’ experience in the qualitative studies to date are diverse. There is a need to systematically review the current literature on mothers’ experiences of breastfeeding peer support. Despite two qualitative systematic reviews addressing breastfeeding peer support [ 14 , 15 ], no updated reviews focus specifically on mothers’ experience and perspectives on peer supporters’ breastfeeding support. The information synthesized from this review could help to explain the successes and failures in implementing breastfeeding support from the mothers’ viewpoint. Furthermore, this allows a comprehensive understanding of how breastfeeding support offered by peers can be effectively carried out in the future. Therefore, the present review aimed to consolidate the qualitative evidence exploring mothers’ perceptions and experiences of the breastfeeding support they received from peer supporters.
Inclusion and exclusion criteria
The PICoS model [ 16 ] was used to construct the inclusion criteria: ① P (population): mothers who are breastfeeding; ② I (phenomenon of interest): mothers’ perceptions and experiences of breastfeeding peer support; ③ Co (context) specific scenario: providing mothers with breastfeeding peer support; ④ S (study design) type of research: qualitative study and mixed methods study. Exclusion criteria: ① literature with no access to full text; ② literature with low methodological quality; ③ literature not published in English or Chinese.
Search strategy
Qualitative studies on mothers’ breastfeeding peer support experiences reported in PubMed, Embase, Cochrane Library, Ovid, Web of Science, CINAHL, China National Knowledge Infrastructure (CNKI), Wanfang database, VIP China Science and Technology Journal Database, and Chinese BioMedical Literature Database (CBM) were searched from inception to January 2023. Additionally, references to the included literature were manually searched for studies related to the topic. A combination of MeSH terms and free words was used to conduct the search. The search strategy was developed according to the specific requirements of different databases to collect relevant literature as comprehensively as possible. Search terms and structure in PubMed were presented in Table 1 . The Chinese search terms corresponding to the above English search terms were used in the search of Chinese databases.
Search terms and structure in PubMed
Literature screening and data extraction
Two researchers independently screened the literature, extracted the data from the literature, and then cross-checked it. Any disagreements were discussed until agreements were achieved. The articles were initially screened by reading the title and abstract and further screened by reading the full text to determine the final inclusion or not. An information extraction form was developed, and the data were extracted, including the authors, time of publication, study site, study methods, study population, phenomenon of interest, situational factors, and main findings. With regard to information that was lacking in the literature but essential for this review, the authors were contacted to obtain it if necessary.
Methodological quality assessment
The JBI Critical Appraisal Checklist for Qualitative Research [ 16 ] was used for methodological quality assessment. Two researchers independently evaluated the quality of the included literature, and each item was scored as “yes”, “no” or “unclear”. The quality of the literature was graded as A if the evaluation items were all scored as “yes”; B if they were partially scored as “yes”’ and C if they were all not scored as “yes”. When disagreements occurred, discussion or consulting with a third party was conducted until a final agreement was reached. Only articles with quality grades A and B were included in this study.
Data synthesis
Analysis of the included articles was conducted using the qualitative evidence synthesis method developed by JBI [ 16 ]. Each finding was read repeatedly, analyzed, and interpreted on the premise of critical appraisal. The findings with similar meaning were grouped to form new categories, and then the categories were pooled into syntheses. Subsequently, a comprehensive set of statements representing synthesized findings was generated. The qualitative evidence summation and synthesis were initially conducted by two researchers independently and then modified based on discussions with the entire research team.
The initial search yielded 633 articles. After removing duplicate records, 378 records were screened through titles and abstracts. Of those, 35 full-text articles were assessed for eligibility based on the inclusion criteria. Those not meeting the criteria were excluded, leaving 15 articles for this review (see Fig. 1 PRISMA flow diagram). The basic characteristics of the articles are shown in Table 2 . Regarding the quality of the studies included, two [ 13 , 17 ] were graded as A, and 13 [ 8 , 11 , 12 , 18 – 27 ] were graded as B (refer to Additional file 1).

PRISMA flow diagram
Characteristics of the included articles
Through analysis of the 15 included articles, similar findings were grouped into 12 new categories and finally synthesized into 4 integrated findings (see Fig. 2 Synthesized findings).

Synthesized findings
Synthesized findings 1: obtaining emotional support
Peer supporters provide emotional support to mothers, aiding them in reducing negative emotions, fostering positive emotions, feeling socially accepted, and gaining confidence in breastfeeding.
Category 1: dissolving negative emotions
Peer support helps dissipate negative emotions mothers experience due to breastfeeding difficulties. The emotional support provided by peers with similar experiences allows mothers to feel less stress. Peer support also works for relieving mothers’ depression.
My failures in breastfeeding made me feel very frustrated and I had postpartum depression at that time, so I kept crying when [the volunteers] came to my home the first two times. They gave me emotional support [ 8 ]. I was so stressed because I couldn’t express and don’t know how to express.. and she helped me and to relax me.. [ 18 ].
Moreover, peer supporters helped mothers cope with the pain of grief.
She would phone me to make sure that everything was all right and I was not in any pain or anything and if I was worried about anything she would come and see me to check it.. because I was worried about a lot, so she came out a lot to see me. [ 25 ].
Category 2: developing positive emotions
Peer support helps the mother keep calm and relaxed facing breastfeeding challenges.
She did a really useful thing actually, which was we did a map of people in my life that I could ask any help for feeding advice and things like that.. and just it just made me rethink and evaluate how much I appreciate having some family closer by. [ 12 ]. I was free with her because she’s a mother like me.” “.. The peer counsellor taught me during pregnancy and she came back after delivery when my breasts were very full, painful, and swollen, and then she helped me to express some breast milk and I felt relieved. [ 26 ].
Peers share their experiences, empathy, and encouragement enhancing the mother's sense of being understood and having positive feelings towards breastfeeding.
It’s just nice to speak to other women, and I’ve always felt more positive towards the feeding after going to the group. [ 21 ].
Category 3: gaining a sense of social connection
Peer supporters are always friendly and warm. They share their personal experiences and emotions with each other, which draws an emotional connection between them. This closeness gives the mother a sense of social acceptance.
I think it was to meet other mums really and.. have a bit of one-to-one contact with other people. [ 13 ]. I think just having that additional person to talk to makes you feel less alone.. so it puts you at ease really about how you can actually do it. I think that’s essentially what you want, you want someone to have the same experience as you, you want someone to be like no it’s fine, you are okay. [ 12 ].
Category 4: increasing self-efficacy
Peer supporters acknowledge and praise mothers for breastfeeding, which leads to positive feedback.
The counselor’s advice allowed me to be sure about my breastfeeding decision [ 23 ]. I always felt more positive about breastfeeding after attending the group. [ 22 ].
Mothers receive a self-efficacy boost with the help of their peers.
She [Peer supporter] gave me the confidence.. she passed me on an article, and I’d read that and we worked out things together... [ 13 ]. .. For me it was a really positive experience.. those calls and contacts through my first few months.. really gave me a lot of confidence to.. keep going.. [ 18 ].
Peer supporters share solutions for breastfeeding problems, and their experiences help mothers to believe in their ability to overcome difficulties and breastfeed successfully.
Very helpful to answer questions the midwives did not have time to go into; this makes a real difference in terms of motivation to continue breastfeeding. [ 24 ].
Synthesized findings 2: acquiring knowledge and skills
Peer supporters provide mothers with breastfeeding knowledge and skills that are tailored to their needs and practical.
Category 5: support that meets the needs
Peer supporters provide mothers with breastfeeding knowledge tailored to their needs.
Helped with my breastfeeding education.. that I needed. [ 23 ]. That’s what I need to know. Is it normal what he’s doing. I think if I’d found online groups and things earlier than I had, we might not have had so many tears in the first few weeks [ 22 ].
Peer supporters always know the effective way for mothers to be able to master breastfeeding knowledge and skills.
You could ask her questions and she’d explain them in a fashion that you could understand without being too medical.. and you could talk to her. [ 25 ]. .. I could understand what she taught me.. [ 26 ].
Category 6: practical breastfeeding knowledge and skills
The advice and approaches offered by the peers were more practical because they had the advantage of having similar experiences.
I feel very strongly that this useful and practical advice given in the comfort of your own home environment in those very early days was an invaluable support. I can only believe that if more women were given this support there would be much more tendency to breastfeed [ 24 ]. It’s like you could go to your GP [General practitioner] and say I’ve got a screaming baby but actually they’re a male GP and they don’t really know. It’s not quite the same. It’s not that I don’t trust the doctor but you have a bit more faith in someone who’s been there, someone who’s been in the situation and can sympathise and say yeah, it’s not easy to breastfeed [ 22 ].
Peer supporters help mothers overcome feeding dilemmas with tips and techniques, and their guidance is hands-on.
.. The peer counsellor showed me how to put my baby on my breast properly and since it was the first experience for me, it was useful [ 26 ]. I have heard from the girls’ good tips, which I found work. It wasn’t just one tip, they gave me a range of different tips for maybe over one problem [ 27 ]. ... I had some lumps in my breasts…and they were really, really sore.. um and I had an idea that they were.. some sort of blockage.. she did offer some very good advice for getting in the shower and.. So it never progressed any further than that... [ 18 ].
Synthesized findings 3: expectations for breastfeeding peer support
Mothers expect reliable breastfeeding support through friendly interactions with peer supporters. There are variations in their preference for peer support.
Category 7: need for more reliable information
Peer supporters generally do not have a medical background, so the information provided by them is not always perceived by mothers as completely reliable.
It is about your personal experience, just talking to other people in the same group.. There is no reliable information there. [ 13 ].
In particular, it was considered difficult to effectively identify information on digital platforms.
I have lingering doubts in my mind, especially about issues that I am concerned about, and I always think about the accuracy of some information [obtained on the internet]. [ 21 ].
Category 8: personalized peer support approach
Mothers had varied expectations for peer support, with some preferring digital technology, including phone calls, text messages, and social service platforms. Many mothers said they liked texting for peer support and communication..
... Text message was better because at that point I was always feeding him, so it was quite difficult to get the phone, so with the text it was more easy because I just answered when I could and she the same. [ 12 ].
Some mothers used to obtain peer support through online social media. Social media provides quicker and more timely access to information than face-to-face communication.
... Such as FaceTime, which is convenient for volunteers because they don’t have to do home visits, and also good for mothers; otherwise, the mothers have to arrange a time to meet [volunteers], which will be stressful. [ 8 ]. When I had nipple thrush, I definitely searched the internet for nipple thrush and read what people said about help for that. [ 13 ]. Facebook helps find the content of interest and offers help in a tailored way. [ 19 ].
Peer support in the form of groups can help mothers receive more rich input from a variety of different people.
People have different requests, but other people have given answers.. which is truly niche. [ 13 ]. I think it is great to have professionals involved as well. [ 20 ].
Because of different cultural backgrounds, mothers need support from specific breastfeeding peers with similar experiences, and they need support from dedicated media groups even more..
Well, we have many experiences that are unique to Black women that we cannot explain to other people, so an inclusive group is definitely needed. [ 17 ].
However, some mothers felt that it was still face-to-face peer support that allowed them to receive more beneficial help.
She calls you, but that is not enough to benefit from her. It is no better than someone who spends an hour and a half visiting you and teaching you baby care. [ 22 ].
Regarding the timing of peer support, some mothers wanted help early to receive longer and more frequent interactions to help them cope with any problems that might arise.
If I were well prepared before birth, it would be much better than preparing after birth. [ 8 ].
In contrast, some mothers preferred later.
I did not really want to acknowledge until the 20-week scan.. 12-weeks.. I do not think I was even thinking about post-birth. [ 12 ].
Category 9: friendlier interactions
Mothers felt that social platforms, due to their anonymity or nonface-to-face nature, led to more direct or carefree expressions from those online, leading to some negative emotional experiences for mothers. They would like to see friendlier discussions on social platforms.
I think sometimes conversations can get a little heated. And um, I think they’re a little harsh at times for people who may be, are not using the search feature or asking a very commonly, a common question and people just kind a pounce on them. So, I think people may get discouraged. [ 17 ]. You would want to get honest opinions from people, not criticism or something like that. [ 13 ]. I just got into a heated argument with someone I have never met before, and I do not think that would happen in real life. [ 22 ].
Synthesized findings 4: feeding perception and behavior change
Peer support has a significant impact on mothers’ perceptions and behaviors towards breastfeeding. It encourages them to accept and adhere to breastfeeding, and even inspires them to become breastfeeding peer supporters themselves.
Category 10: acceptance and support of breastfeeding
Peer support helps mothers accept breastfeeding by addressing misconceptions about breastfeeding.
... It’s sort of give me confidence to not really care about the rest of societies [society’s] opinions as long as I am happy with my own mothering and parenting. [ 22 ].
Breastfeeding images allow mothers to accept breastfeeding in public.
I feel the images are amazing. They’re so uplifting. There was one, um, that empowered me so much the other day. It was a woman breastfeeding her daughter at a restaurant, and today, I thought about that, and I’ve been thinking about it for days, and I went out today, and I did it... [ 17 ].
The support the mother gained from the peers reinforces her to continue breastfeeding.
Well originally before I came across the Breastfeeding in Northern Ireland page I think originally my goal was to get to the minimum six-month period and now having educated myself my goal is probably to get to either the age of two or a natural weaning point or when I get pregnant again and I can’t... [ 20 ] If I didn’t have the peer supporter to talk to about things I would be more likely to give up [ 24 ].
Mothers who received peer support were more likely to be breastfeeding advocates.
I think also it’s nice to be able to give support, because in these groups you’ve got people who have just had babies and it’s nice to be able to say actually I’ve been there now. So, where people have answered my questions, I can hopefully answer theirs [ 22 ].
Category 11: extended breastfeeding duration
Peer support increases mothers’ confidence to achieve their goal of breastfeeding longer.
Without this study I could have stopped breastfeeding from the first month.. Without the help of the peer support and consultant [ 11 ]. It’s been great to see that there’s women that do it for 12 months, two years, and so that six-month goal doesn’t seem so unachievable. It kind of almost makes you feel– it motivates you to keep going. [ 19 ].
Category 12: desire to be a peer supporter and give back to others
As mothers became more familiar with breastfeeding with the help of peer support, they became very willing to offer help to others.
Because it’s important to see women that look like us doing this stuff. Marrying that up with what I learned in the class that I took for the CLC [Certified Lactation Consultant]. So, yeah, this [breastfeeding] would have been a done deal, and I wouldn’t be this advocate. I wouldn’t be posting breastfeeding on my Facebook page, I wouldn’t be going to support groups if it wasn’t for the group. [ 17 ].
Providing support to other mothers not only gave them a sense of accomplishment but also enhanced their own breastfeeding experience.
... My need to empower other women with up to date, correct information is being met.. making new friends hopefully, and.. feeling the breastfeeding love.. [ 13 ].
This synthesis of findings on mothers’ perceptions and experiences of breastfeeding peer support through a meta-integration approach confirms the values of peer support, identifies ways to optimize the effect of peer support, and provided administrators with recommendations for the effective operation of peer support. Evidence from the included studies revealed that breastfeeding peer support has multiple positive effects for mothers. Peer supporters are empathetic to the mother’s breastfeeding experience because of their own breastfeeding experience, and can therefore provide them with emotional support that meets their needs and helps them overcome negative feelings such as loneliness, sadness, and depression during breastfeeding. In addition, peer support can improve mothers’ self-efficacy in achieving breastfeeding goals, and therefore help them to breastfeed more actively. Peers can provide mothers with more relevant and desired knowledge, although they are not professional healthcare providers. It is concluded that breastfeeding peer support is a worthwhile initiative to promote breastfeeding.
Most mothers wanted higher frequency, longer duration, and more interactive peer support. However, there was a wide variation in preference for forms of peer support. Some mothers felt that one-to-one face-to-face peer support could lead to a mutually supportive and decision-making experience [ 11 ], while others indicated that group-based peer support might be a better option because of the anxiety felt in one-to-one support [ 20 , 27 ]. Additionally, there were variations as to the peer support needed by mothers from different cultural backgrounds. African-American mothers preferred to be supported by teams composed of Black mothers because they felt that only Black mothers could understand their experiences [ 17 ]. Because the challenges mothers face during breastfeeding are always complex and the needs for peer supporters are dynamic, peer support teams from diverse backgrounds are better able to meet the mothers’ needs. Therefore, individualized peer support should be provided to mothers according to their needs and background.
Variability in the quality and competence of peer supporters leads to different experiences of peer support for mothers. Quality peer supporters are more likely to have a positive effect on mothers’ breastfeeding experience [ 17 ]. Peer supporters face transitional difficulties as they move from a voluntary to a professionalized role [ 28 ]. This suggests the need for professional training for peer supporters to respond to the needs of mothers. Training plays an important role in improving the attitudes of peer supporters as well as enhancing their knowledge [ 29 ]. Peers who have scientific knowledge and skills in breastfeeding are more likely to gain the trust of mothers and provide a good experience for them. Therefore, standardized training standards for breastfeeding peer support should be developed for peer support to be more effective.
With the development of digital technology, mothers are able to quickly access peer support from social networks with similar experiences. However, mothers do not always have the ability to recognize reliable information online [ 22 ]. They need reliable knowledge from healthcare professionals. It is suggested that a social platform for breastfeeding support can be built with the participation of health professionals [ 20 ]. Peers with similar experiences communicate and interact with mothers on this platform to provide peer support to mothers, and health professionals can provide timely supervision of the services of peer supporters to ensure reliable support.
Although currently, most of the peer supporters are volunteers, the peer support services require adequate funding for recruitment, training, and ongoing supervision of peer supporters, as well as paying them travel expenses. In addition, peer supporters, although their motivations to become a peer supporter are ‘give something back’ to the service that had supported them, some of them still expect to be paid. Limited funding causes a high turnover because they need to get back to paid employment. In the UK, peer support services are facing a reduction in available funding [ 29 ]. This impacted on the quality of peer support services. Accordingly, further investment must be made to establish effective breastfeeding peer support services.
There is also a need to facilitate the interface between breastfeeding peer support agencies and mothers. Effective communication methods can help mothers understand the usefulness of peer support and enable them to be willing to try the positive effects of peer support [ 26 ]. Mothers who receive peer support often show a greater willingness to provide peer support if they have a good experience, which further expands the number of peer supporters and is more conducive to sustainability [ 13 , 17 ].
In addition, research has shown that many mothers look forward to peer support from social media groups [ 19 , 20 , 22 ]. They often turned to online breastfeeding support due to a lack of face-to-face support [ 30 ]. From this perspective, online support provides a service that is of great need. Due to the time- and space-independent properties of online support, women have convenient access to online support [ 19 ]. Moreover, online support allows for large-scale outreach in a short period of time, quickly establishing a connection between peers and mothers. With the prevalence of mobile health, the online breastfeeding support may alleviate the financial burden for governments, and thus provide a cost-effective way to increase breastfeeding rates [ 20 ]. Therefore, the use of online platforms should be explored to provide a sustainable peer support model in the future.
Limitations
Since the literature included in this study was in English and mostly originated from developed countries or regions, the applicability of the integrated results to underdeveloped regions or non-English speaking countries was weak. Whereas, the fact that the studies came from different countries with different health care systems and cultural norms related to breastfeeding may also be seen as a strength. Moreover, gray literature was not searched and included, which may have led to an incomplete inclusion of literature. Additionally, this qualitative integration used a descriptive methodology which provides limited interpretation of meaning, but the method is applicable to studies that explore perspectives and experiences.
Implications for research and practice
First, most of the included studies were conducted in developed countries, indicating that mothers’ experience on breastfeeding peer support is less studied in underdeveloped regions, or that there are fewer relevant studies conducted in these regions published in English. Consequently, studies focusing on this topic are encouraged in these areas to enrich the recognition of breastfeeding peer support. Additionally, relevant studies exploring feasible and effective forms of breastfeeding peer support are also recommended from the perspectives of different stakeholders. Second, adequate funding should be provided to facilitate the breastfeeding peer support. Ongoing training mechanisms and dynamic peer support monitoring are recommended, in order to fully exert the role of peer support in promoting the breastfeeding.
This study systematically evaluated mothers’ experiences of breastfeeding peer support. The results confirmed that mothers perceived positive effects of peer support on breastfeeding. It is important to note that the peer support analyzed in the included studies varied in terms of the characteristics of the peer supporters and the training they received, as well as the form and timing of the support. Therefore, it is recommended that peer support services should be standardized, including the accreditation, training, supervision, and management of peer supporters in the future. Additionally, exploring measures to promote the sustainability of peer support is necessary. The review’s findings also suggest that individual needs of mothers should be assessed before providing peer support. Personalized and targeted peer support should be provided based on the individual’s preferences and willingness.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Not applicable.
Abbreviations
Author contributions.
Y.Y. contributed to the conception and design, performed the literature search and screening, conducted the quality assessment, integrated the data, and drafted the manuscript. H.L. contributed to quality assessment, data extraction and pooling, and the revision of the manuscript. X.C. contributed to the literature search and screening, quality assessment, and data extraction and pooling. J.M. contributed to the data pooling and revision of the manuscript. All authors read and approved the final version of the manuscript.
The study did not receive any external funding.
Data availability
Declarations.
The authors declare no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Benefits of Breastfeeding Versus Formula-Feeding Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Introduction
History of breastfeeding, advantages of breastfeeding over bottle-feeding, advantages of bottle-feeding over breastfeeding, importance of research.
Nowadays, one of the most challenging tasks many young mothers have to face is the necessity of choosing between breastfeeding and formula/bottle-feeding. It is easy to surf the web and find several correlational, cohort, or experimental studies where different authors defend their positions on the chosen topic. On the one hand, breastfeeding is deemed preferable due to its perfect balance of nutrients, protection against allergies and diseases, and easy digestion for babies.
On the other hand, formula-feeding is characterized by certain merits, such as the possibility for another person to feed a baby anytime, a mother’s freedom to be involved in different activities or even start working, and no dependence on the mother-child diet. Although some mothers might still choose to bottle-feed their infants with formula due to practical concerns, research shows that breastfeeding is preferable due to its impact on maternal and child health.
The history of breastfeeding is as long as the existence of life on the planet. In ancient cultures and in modern times women continued to breastfeed children to nourish them. However, some cultures did not focus on breastfeeding as an intimate link between the mother and the child. For example, while most ancient civilizations had mothers feed their children, more structurally segregated Western European countries created the role of a wet nurse – a woman whose job was to breastfeed children of royal and noblewomen.
Various cultures assigned different meanings to the process of breastfeeding and followed their sets of rules to determine how, when, and where to feed children. In ancient times, Egyptian and Greek civilizations did not treat breastfeeding as a job fit only for common folk and allowed women of all social statuses to feed their children. Nevertheless, wet nurses still had a place in the culture and were respected for their work. In Japan, breastfeeding was common but declined in popularity in the 20th century due to the interest of mothers in modern medicine and artificial feeding options. However, with a well-thought-out campaign, the government was able to elevate breastfeeding to be the primary choice of mothers in the country.
Western countries faced similar challenges earlier, during the middle ages, and then again at the beginning of the 19th century. Here, the history of breastfeeding was firmly connected to the cultural aspects of these civilizations. Countries with a rigid societal structure viewed breastfeeding as a job for lower classes and the process became plagued with many preconceptions. The combination of men’s opinions on breastfeeding and their lack of medical knowledge pressured women into declining breastfeeding. Later efforts in raising the popularity of breastfeeding emphasized health benefits for mothers and children and an establishment of an emotional connection between the parent and the child.
The breastfeeding vs. formula-feeding dilemma appears as soon as women find out that they are pregnant. They have to evaluate all the pros and cons of their pregnancy outcomes, understand if they want to take sick leave, and recognize the relationship between baby feeding and health. All circumstances have to be taken into consideration to make the best decision. Both methods, breastfeeding and bottle-feeding, have their advantages and disadvantages.
Sometimes, it is hard to make a choice, and extensive research is required. This dilemma may be considered through the prism of health, social factors, emotional stability, and personal convenience. In this paper, special attention to the works by Belfort et al. (2013), Boué et al. (2018), Fallon, Komninou, Bennett, Halford, and Harrold (2017), Horta and Victoria (2013) will be made to clarify if the benefits of breastfeeding prevail over the benefits of bottle-feeding in terms of health.
The first months after a baby is born may be defined as the period when it is necessary to choose to breastfeed over bottle-feeding and establish a strong mother-child contact. There are many short- and long-term health benefits for both participants of a process that may be enhanced through its exclusivity and duration (Fallon et al., 2017). The representatives of the World Health Organization admit that exclusive breastfeeding during the first six months can decrease morbidity from allergies and gastrointestinal diseases due to the presence of nutritional benefits in human milk (Horta & Victoria, 2013).
For example, the nutrient n-3 fatty acid docosahexaenoic acid (DHA) found in breast milk aims at improving the functions of the brain (Belfort et al., 2013). Therefore, when the advantages of breastfeeding have to be identified, this point plays an important role.
In addition to nutrients, breastfeeding is a method in terms of which infants can control their condition and take as much amount of milk as they may need. They do not take more or less, just the portion they need at that moment. Mothers should take responsibility for the quality of milk they offer to their children and follow simple hygiene rules and schedules.
Another important aspect that underlines the necessity of breastfeeding is the protection of children against diseases and other health threats. Probiotics and prebiotics, also known as important live microorganisms, protect the body and establish a gut microbiota that promotes positive health outcomes through the creation of barriers to pathogens, improvement of metabolic function, and energy salvation (Boué et al., 2018). Stomach viruses and other conditions that may cause discomfort are also significantly reduced with breastfeeding.
Allergies pose another serious threat to infants. It is hard for a mother to comprehend what product is safe for a child and what ingredients should be avoided. Breast milk is characterized by appropriate natural filters and the possibility to avoid ingesting real food until the body is properly developed. It helps babies digest food and uses the enzymes in a mother’s milk to speed up digestion and avoid complications.
Finally, breastfeeding is preferable because of the promotion of the bond between a mother and a child, and its price. This process of feeding is a unique chance for mothers to be relieved from anxiety and develop an emotional attachment to their children. Sometimes, it is not enough for mothers to talk to their children, observe their smile, and touch them. Breastfeeding is an exclusive type of contact that is not available to other people, including even the closest family members. This relationship is priceless. Indeed, when talking about the price, it is also necessary to admit that compared to bottle-feeding, which requires buying special ingredients, bottles, and hygienic goods, breastfeeding is a cheap process with no additional products except a mother and a child being present in it.
However, despite all the benefits of breastfeeding, it is wrong to believe that formula-feeding is solely negative or does not have important characteristics that breast-feeding cannot offer. Many significant aspects should be considered by mothers who still have some doubts about their choice. For example, some mothers may be challenged by poor health or inappropriate health status for breastfeeding.
Mothers may suffer from the inability to breastfeed as they are unable to produce milk or the milk is of poor quality. In these cases, mothers still want to find new ways to be close to their children and support them and formula-feeding is one option that they can rely on on under any condition. No connection between the health problems of a mother and a child is observed. Bottle-feeding creates several good opportunities for mothers to stabilize their personal and professional lives. Fallon et al. (2017) admit that the choice of the formula is usually explained by breastfeeding management, not biological issues. Therefore, the advantages of bottle-feeding over breastfeeding in terms of health care are based on the emotional aspects and mental health of mothers.
An understanding of the differences between breastfeeding and formula-feeding should be based on thorough research. For example, a study developed by Horta and Victoria (2013) asserts that formula-fed children may have serious hormonal and insulin responses to feeding and an increased number of adipocytes compared to breast-fed children. Bottles have to be cleaned and properly stored to avoid the growth of bacteria that may harm a child (Boué et al., 2018). Finally, the study by Fallon et al. (2017) shows that mothers may feel guilt and stigma in case they choose formula as the main method of feeding. All these studies prove that research is a crucial step to comprehend the benefits of breastfeeding nowadays.
In general, it is hard to neglect the existing dilemma of breastfeeding vs. bottle-feeding. Mothers have to weigh all the pros and cons of both processes and understand what method is more appropriate to them. Regarding the chosen cohort and experimental studies and past research, it is concluded that despite several positive socio-cultural and emotional outcomes of formula-feeding, breastfeeding remains the preferred method due to its effects on health, the establishment of mother-child relations, and the promotion of the cognitive development of children.
Belfort, M. B., Rifas-Shiman, S. L., Kleinman, K. P., Guthrie, L. B., Bellinger, D. C., Taveras, E. M.,… Oken, E. (2013). Infant feeding and childhood cognition at ages 3 and 7 years: Effects of breastfeeding duration and exclusivity. JAMA Pediatrics, 167 (9), 836-844.
Boué, G., Cummins, E., Guillou, S., Antignac, J. P., Le Bizec, B., & Membré, J. M. (2018). Public health risks and benefits associated with breast milk and infant formula consumption. Critical Reviews in Food Science and Nutrition, 58 (1), 126-145.
Fallon, V., Komninou, S., Bennett, K. M., Halford, J. C., & Harrold, J. A. (2017). The emotional and practical experiences of formula‐feeding mothers. Maternal & Child Nutrition, 13 (4), 1-14.
Horta, B. L., & Victoria, C. G. (2013). Long-term effects of breastfeeding: A systematic review . Geneva, Switzerland: WHO Press.
- Breastfeeding and Bottle Feeding: Pros and Cons
- Breastfeeding Health Teaching Project
- Transportation and Public Health Issues
- Breastfeeding and Children Immunity
- Angelman Syndrome, Communication and Behavior
- At-Risk Children's Healthcare Programs
- Premature Infants and Their Challenges
- Pediatric Health Care and Insurance in the USA
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2020, October 23). Benefits of Breastfeeding Versus Formula-Feeding. https://ivypanda.com/essays/benefits-of-breastfeeding-versus-formula-feeding/
"Benefits of Breastfeeding Versus Formula-Feeding." IvyPanda , 23 Oct. 2020, ivypanda.com/essays/benefits-of-breastfeeding-versus-formula-feeding/.
IvyPanda . (2020) 'Benefits of Breastfeeding Versus Formula-Feeding'. 23 October.
IvyPanda . 2020. "Benefits of Breastfeeding Versus Formula-Feeding." October 23, 2020. https://ivypanda.com/essays/benefits-of-breastfeeding-versus-formula-feeding/.
1. IvyPanda . "Benefits of Breastfeeding Versus Formula-Feeding." October 23, 2020. https://ivypanda.com/essays/benefits-of-breastfeeding-versus-formula-feeding/.
Bibliography
IvyPanda . "Benefits of Breastfeeding Versus Formula-Feeding." October 23, 2020. https://ivypanda.com/essays/benefits-of-breastfeeding-versus-formula-feeding/.

IMAGES
VIDEO
COMMENTS
This Thesis is brought to you for free and open access by the Graduate Theses, Dissertations, and Other Capstone ... Statement of the problem: Breastfeeding is an important topic in health education because of the many benefits that can be gained for babies, mothers, and communities. For example, the components of breast milk
Canadian mothers, Chalmers et al. (2009) found that women who were educated, were. older, had a high level of income, and had vaginal births were most likely to breastfeed. The majority of women (97.3%) in this study were Hispanic and only a few women. (9.3%) continued EBF until four weeks postpartum.
Exclusive breastfeeding (EBF) is recommended for the first six months of age by the World Health Organization. Mothers' good knowledge and positive attitude play key roles in the process of exclusive breastfeeding practices. In this study, we report on a systematic review of the literature that aimed to examine the status of mothers' knowledge, attitude, and practices related to exclusive ...
breastfeeding and instigate changes in individual behavior. This research was conducted to assess breastfeeding knowledge, and attitudes, beliefs, and intentions among students and professionals in health-related fields. A 5-year prospective study was conducted to investigate breastfeeding knowledge, and attitudes, beliefs, and intentions regarding
themes: the 'Breastfeeding Assumption,' Breastfeeding as Women's Business,' the Postnatal Breastfeeding Experience and 'Family as Enabler or Disabler'. Within the context of this study, breastfeeding is expressed as an activity within the family and social environment. The overall phenomenon that emerged was 'Social Conformity'
The vast majority ( n = 50) of the reviewed literature identified various barriers for successful breastfeeding. A sizeable proportion of literature (41%, n = 24) explored women's experiences with the physical aspects of breastfeeding [ 23, 33 ]. In particular, problems with latching and the pain associated with breastfeeding were commonly ...
Perceptions about breastfeeding. Women's perceptions about breastfeeding were covered in 83% (n = 49) of the papers.Most articles (n = 31) suggested that women perceived breastfeeding as a positive experience and believed that breastfeeding had many benefits [19, 20].The phrases "breast is best" and "breastmilk is best" were repeatedly used by the participants of studies included in ...
Breastfeeding offers strong protection against the effects of poverty and is a key strategy in reducing disparities between the rich and poor. Bartick and Reinhold's (2010) data revealed that breastfeeding had economic benefits. Additionally, this study found that breastfeeding significantly decreased health care costs and saved lives.
of women exclusively breastfeeding at three months and 13.3% exclusively breastfeeding at 6 months (Centers for Disease Control, 2009). These rates fall short of the HP 2020 goals of 81.9% of women initiating breastfeeding in the early postpartum period, 60.5% breastfeeding at six months, 34.1% at 12 months, 44.3% of women exclusively
stipulations prescribed by the author in the preceding statement. The author of this thesis is: Dashia Antunes 1238 Blueberry Trl Decatur, GA 30033 The director of this thesis is: Anita M. Nucci, PhD, RD, LD ... Breastfeeding (BF) is widely recognized as the ideal infant feeding method with a multitude of well-known infant and maternal benefits ...
mammalian milk, unmodified mammalian milk, formula made from grains or legumes, or. breast milk from another lactating mother (O'Conner, 1998). The utilization of modified mammalian milk was formula based on cow's milk. and was made available in the 20th century. Cow's milk or goat milk are examples of.
breastfeeding and longer duration of breastfeeding (Bolton, Chow,et al 2009; Ukegbu, et a l 2010), while others, associated low rates of exclusive breastfeeding with younger
Low rates of breastfeeding are a global public health issue. Despite national and international health agency recommendations for breastfeeding until infants are six months of age when solid foods are introduced and continued breastfeeding until 12 months of age or older, many mothers in the United States discontinue breastfeeding at an early age.
World Alliance for Breastfeeding Action (WABA) is a network of people working on a global scale to address and overcome challenges to breastfeeding. This study analyzed WABA's 2011 World Breastfeeding Week campaign, in an effort to assess the campaign's relative strengths and weaknesses, and to identify recommendations for future WBW campaigns.
An Eta coefficient value of .45 suggests a moderate relationship. between knowledge of breastfeeding as tested on the Information on Breastfeeding. Questionnaire and success of breastfeeding as measured at six weeks postpartum. Looking only at those with scores greater than 18 a slightly stronger relationship is.
Breastfeeding in public continues to be contentious with qualitative evidence confirming that women face many challenges. It is therefore important to gain understanding of not only the challenges but also what women perceive is helpful to breastfeed in public. A cross-sectional study was conducted with women living in Australia, Ireland or Sweden currently breastfeeding or having breastfed ...
breastfeeding mothers to improve breastfeeding self-efficacy4 Healthcare Professionals • Understand evil eye beliefs and the role they play in infant feeding practices via educational trainings or community briefings49-50 Community • Improve awareness and acceptability of breastfeeding in public via campaigns, posters, and media to
For 397 women (90.4%), breastfeeding creates a strong bond between the child and the mother, and 277 respondents (63.1%) stated that breastfeeding helps the mother's weight return to its pre-pregnancy state. 258 respondents (58.8%) stated that breastfeeding reduces the risk of breast and ovarian cancer. 228 mothers (51.9%) believe that ...
Breastfeeding in Public: Perceptions of College Students in South Mississippi. by. Kaitlyn Kendall. A Thesis Submitted to the Honors College of The University of Southern Mississippi in Partial Fulfillment of the Requirements for the Degree of Bachelor of Science in the Department of Child and Family Studies. May 2018.
Results. A total of 15 articles were included in the study, consisting of 13 qualitative studies and 2 mixed methods studies. The analysis identified four integrated themes: (1) obtaining psycho-emotional support; (2) acquiring knowledge and skills; (3) expectations for breastfeeding peer support; and (4) feeding perceptions and behavior change.
Advantages of bottle-feeding over breastfeeding. Finally, breastfeeding is preferable because of the promotion of the bond between a mother and a child, and its price. This process of feeding is a unique chance for mothers to be relieved from anxiety and develop an emotional attachment to their children. Sometimes, it is not enough for mothers ...
Step 2: Write your initial answer. After some initial research, you can formulate a tentative answer to this question. At this stage it can be simple, and it should guide the research process and writing process. The internet has had more of a positive than a negative effect on education.
Thesis Statement on Breastfeeding. Thesis statement: Research shows that breastfeeding is the best choice over formula because breastfeeding provides the infant with essential nutrients, helps with recovery from childbirth, and protects the infant against a number of chronic conditions. Baumgartel, K. L., & Spatz, D. L. (2013).