Greater Good Science Center • Magazine • In Action • In Education

11 Questions to Ask About COVID-19 Research
Debates have raged on social media, around dinner tables, on TV, and in Congress about the science of COVID-19. Is it really worse than the flu? How necessary are lockdowns? Do masks work to prevent infection? What kinds of masks work best? Is the new vaccine safe?
You might see friends, relatives, and coworkers offer competing answers, often brandishing studies or citing individual doctors and scientists to support their positions. With so much disagreement—and with such high stakes—how can we use science to make the best decisions?
Here at Greater Good , we cover research into social and emotional well-being, and we try to help people apply findings to their personal and professional lives. We are well aware that our business is a tricky one.
Summarizing scientific studies and distilling the key insights that people can apply to their lives isn’t just difficult for the obvious reasons, like understanding and then explaining formal science terms or rigorous empirical and analytic methods to non-specialists. It’s also the case that context gets lost when we translate findings into stories, tips, and tools, especially when we push it all through the nuance-squashing machine of the Internet. Many people rarely read past the headlines, which intrinsically aim to be relatable and provoke interest in as many people as possible. Because our articles can never be as comprehensive as the original studies, they almost always omit some crucial caveats, such as limitations acknowledged by the researchers. To get those, you need access to the studies themselves.
And it’s very common for findings and scientists to seem to contradict each other. For example, there were many contradictory findings and recommendations about the use of masks, especially at the beginning of the pandemic—though as we’ll discuss, it’s important to understand that a scientific consensus did emerge.
Given the complexities and ambiguities of the scientific endeavor, is it possible for a non-scientist to strike a balance between wholesale dismissal and uncritical belief? Are there red flags to look for when you read about a study on a site like Greater Good or hear about one on a Fox News program? If you do read an original source study, how should you, as a non-scientist, gauge its credibility?
Here are 11 questions you might ask when you read about the latest scientific findings about the pandemic, based on our own work here at Greater Good.
1. Did the study appear in a peer-reviewed journal?
In peer review, submitted articles are sent to other experts for detailed critical input that often must be addressed in a revision prior to being accepted and published. This remains one of the best ways we have for ascertaining the rigor of the study and rationale for its conclusions. Many scientists describe peer review as a truly humbling crucible. If a study didn’t go through this process, for whatever reason, it should be taken with a much bigger grain of salt.
“When thinking about the coronavirus studies, it is important to note that things were happening so fast that in the beginning people were releasing non-peer reviewed, observational studies,” says Dr. Leif Hass, a family medicine doctor and hospitalist at Sutter Health’s Alta Bates Summit Medical Center in Oakland, California. “This is what we typically do as hypothesis-generating but given the crisis, we started acting on them.”
In a confusing, time-pressed, fluid situation like the one COVID-19 presented, people without medical training have often been forced to simply defer to expertise in making individual and collective decisions, turning to culturally vetted institutions like the Centers for Disease Control (CDC). Is that wise? Read on.
2. Who conducted the study, and where did it appear?
“I try to listen to the opinion of people who are deep in the field being addressed and assess their response to the study at hand,” says Hass. “With the MRNA coronavirus vaccines, I heard Paul Offit from UPenn at a UCSF Grand Rounds talk about it. He literally wrote the book on vaccines. He reviewed what we know and gave the vaccine a big thumbs up. I was sold.”
From a scientific perspective, individual expertise and accomplishment matters—but so does institutional affiliation.
Why? Because institutions provide a framework for individual accountability as well as safety guidelines. At UC Berkeley, for example , research involving human subjects during COVID-19 must submit a Human Subjects Proposal Supplement Form , and follow a standard protocol and rigorous guidelines . Is this process perfect? No. It’s run by humans and humans are imperfect. However, the conclusions are far more reliable than opinions offered by someone’s favorite YouTuber .
Recommendations coming from institutions like the CDC should not be accepted uncritically. At the same time, however, all of us—including individuals sporting a “Ph.D.” or “M.D.” after their names—must be humble in the face of them. The CDC represents a formidable concentration of scientific talent and knowledge that dwarfs the perspective of any one individual. In a crisis like COVID-19, we need to defer to that expertise, at least conditionally.
“If we look at social media, things could look frightening,” says Hass. When hundreds of millions of people are vaccinated, millions of them will be afflicted anyway, in the course of life, by conditions like strokes, anaphylaxis, and Bell’s palsy. “We have to have faith that people collecting the data will let us know if we are seeing those things above the baseline rate.”
3. Who was studied, and where?
Animal experiments tell scientists a lot, but their applicability to our daily human lives will be limited. Similarly, if researchers only studied men, the conclusions might not be relevant to women, and vice versa.
Many psychology studies rely on WEIRD (Western, educated, industrialized, rich and democratic) participants, mainly college students, which creates an in-built bias in the discipline’s conclusions. Historically, biomedical studies also bias toward gathering measures from white male study participants, which again, limits generalizability of findings. Does that mean you should dismiss Western science? Of course not. It’s just the equivalent of a “Caution,” “Yield,” or “Roadwork Ahead” sign on the road to understanding.
This applies to the coronavirus vaccines now being distributed and administered around the world. The vaccines will have side effects; all medicines do. Those side effects will be worse for some people than others, depending on their genetic inheritance, medical status, age, upbringing, current living conditions, and other factors.
For Hass, it amounts to this question: Will those side effects be worse, on balance, than COVID-19, for most people?
“When I hear that four in 100,000 [of people in the vaccine trials] had Bell’s palsy, I know that it would have been a heck of a lot worse if 100,000 people had COVID. Three hundred people would have died and many others been stuck with chronic health problems.”
4. How big was the sample?
In general, the more participants in a study, the more valid its results. That said, a large sample is sometimes impossible or even undesirable for certain kinds of studies. During COVID-19, limited time has constrained the sample sizes.
However, that acknowledged, it’s still the case that some studies have been much larger than others—and the sample sizes of the vaccine trials can still provide us with enough information to make informed decisions. Doctors and nurses on the front lines of COVID-19—who are now the very first people being injected with the vaccine—think in terms of “biological plausibility,” as Hass says.
Did the admittedly rushed FDA approval of the Pfizer-BioNTech vaccine make sense, given what we already know? Tens of thousands of doctors who have been grappling with COVID-19 are voting with their arms, in effect volunteering to be a sample for their patients. If they didn’t think the vaccine was safe, you can bet they’d resist it. When the vaccine becomes available to ordinary people, we’ll know a lot more about its effects than we do today, thanks to health care providers paving the way.
5. Did the researchers control for key differences, and do those differences apply to you?
Diversity or gender balance aren’t necessarily virtues in experimental research, though ideally a study sample is as representative of the overall population as possible. However, many studies use intentionally homogenous groups, because this allows the researchers to limit the number of different factors that might affect the result.
While good researchers try to compare apples to apples, and control for as many differences as possible in their analyses, running a study always involves trade-offs between what can be accomplished as a function of study design, and how generalizable the findings can be.
The Science of Happiness
What does it take to live a happier life? Learn research-tested strategies that you can put into practice today. Hosted by award-winning psychologist Dacher Keltner. Co-produced by PRX and UC Berkeley’s Greater Good Science Center.
- Apple Podcasts
- Google Podcasts
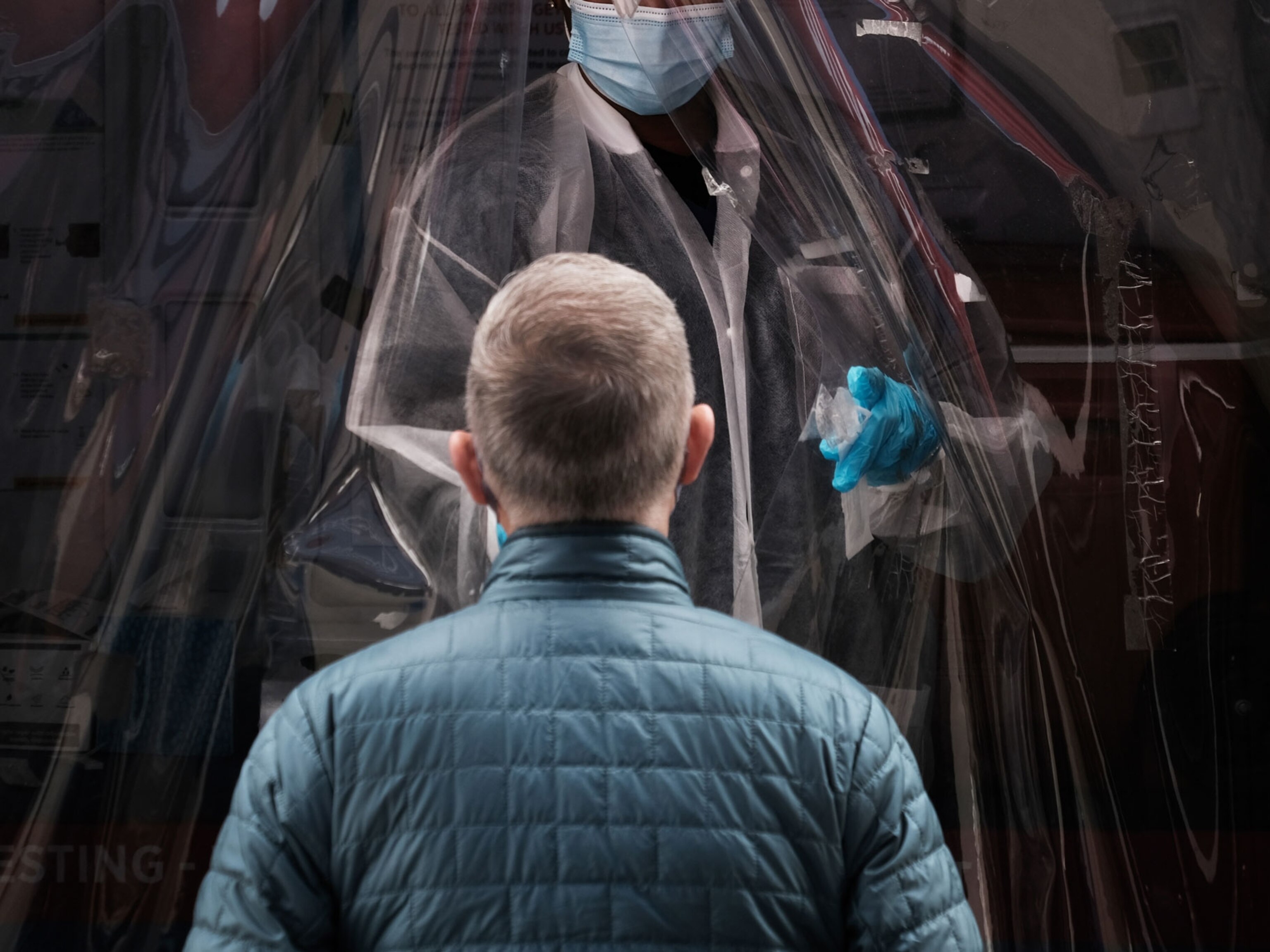
You also need to ask if the specific population studied even applies to you. For example, when one study found that cloth masks didn’t work in “high-risk situations,” it was sometimes used as evidence against mask mandates.
However, a look beyond the headlines revealed that the study was of health care workers treating COVID-19 patients, which is a vastly more dangerous situation than, say, going to the grocery store. Doctors who must intubate patients can end up being splattered with saliva. In that circumstance, one cloth mask won’t cut it. They also need an N95, a face shield, two layers of gloves, and two layers of gown. For the rest of us in ordinary life, masks do greatly reduce community spread, if as many people as possible are wearing them.
6. Was there a control group?
One of the first things to look for in methodology is whether the population tested was randomly selected, whether there was a control group, and whether people were randomly assigned to either group without knowing which one they were in. This is especially important if a study aims to suggest that a certain experience or treatment might actually cause a specific outcome, rather than just reporting a correlation between two variables (see next point).
For example, were some people randomly assigned a specific meditation practice while others engaged in a comparable activity or exercise? If the sample is large enough, randomized trials can produce solid conclusions. But, sometimes, a study will not have a control group because it’s ethically impossible. We can’t, for example, let sick people go untreated just to see what would happen. Biomedical research often makes use of standard “treatment as usual” or placebos in control groups. They also follow careful ethical guidelines to protect patients from both maltreatment and being deprived necessary treatment. When you’re reading about studies of masks, social distancing, and treatments during the COVID-19, you can partially gauge the reliability and validity of the study by first checking if it had a control group. If it didn’t, the findings should be taken as preliminary.
7. Did the researchers establish causality, correlation, dependence, or some other kind of relationship?
We often hear “Correlation is not causation” shouted as a kind of battle cry, to try to discredit a study. But correlation—the degree to which two or more measurements seem connected—is important, and can be a step toward eventually finding causation—that is, establishing a change in one variable directly triggers a change in another. Until then, however, there is no way to ascertain the direction of a correlational relationship (does A change B, or does B change A), or to eliminate the possibility that a third, unmeasured factor is behind the pattern of both variables without further analysis.
In the end, the important thing is to accurately identify the relationship. This has been crucial in understanding steps to counter the spread of COVID-19 like shelter-in-place orders. Just showing that greater compliance with shelter-in-place mandates was associated with lower hospitalization rates is not as conclusive as showing that one community that enacted shelter-in-place mandates had lower hospitalization rates than a different community of similar size and population density that elected not to do so.
We are not the first people to face an infection without understanding the relationships between factors that would lead to more of it. During the bubonic plague, cities would order rodents killed to control infection. They were onto something: Fleas that lived on rodents were indeed responsible. But then human cases would skyrocket.
Why? Because the fleas would migrate off the rodent corpses onto humans, which would worsen infection. Rodent control only reduces bubonic plague if it’s done proactively; once the outbreak starts, killing rats can actually make it worse. Similarly, we can’t jump to conclusions during the COVID-19 pandemic when we see correlations.
8. Are journalists and politicians, or even scientists, overstating the result?
Language that suggests a fact is “proven” by one study or which promotes one solution for all people is most likely overstating the case. Sweeping generalizations of any kind often indicate a lack of humility that should be a red flag to readers. A study may very well “suggest” a certain conclusion but it rarely, if ever, “proves” it.
This is why we use a lot of cautious, hedging language in Greater Good , like “might” or “implies.” This applies to COVID-19 as well. In fact, this understanding could save your life.
When President Trump touted the advantages of hydroxychloroquine as a way to prevent and treat COVID-19, he was dramatically overstating the results of one observational study. Later studies with control groups showed that it did not work—and, in fact, it didn’t work as a preventative for President Trump and others in the White House who contracted COVID-19. Most survived that outbreak, but hydroxychloroquine was not one of the treatments that saved their lives. This example demonstrates how misleading and even harmful overstated results can be, in a global pandemic.
9. Is there any conflict of interest suggested by the funding or the researchers’ affiliations?
A 2015 study found that you could drink lots of sugary beverages without fear of getting fat, as long as you exercised. The funder? Coca Cola, which eagerly promoted the results. This doesn’t mean the results are wrong. But it does suggest you should seek a second opinion : Has anyone else studied the effects of sugary drinks on obesity? What did they find?
It’s possible to take this insight too far. Conspiracy theorists have suggested that “Big Pharma” invented COVID-19 for the purpose of selling vaccines. Thus, we should not trust their own trials showing that the vaccine is safe and effective.
But, in addition to the fact that there is no compelling investigative evidence that pharmaceutical companies created the virus, we need to bear in mind that their trials didn’t unfold in a vacuum. Clinical trials were rigorously monitored and independently reviewed by third-party entities like the World Health Organization and government organizations around the world, like the FDA in the United States.
Does that completely eliminate any risk? Absolutely not. It does mean, however, that conflicts of interest are being very closely monitored by many, many expert eyes. This greatly reduces the probability and potential corruptive influence of conflicts of interest.
10. Do the authors reference preceding findings and original sources?
The scientific method is based on iterative progress, and grounded in coordinating discoveries over time. Researchers study what others have done and use prior findings to guide their own study approaches; every study builds on generations of precedent, and every scientist expects their own discoveries to be usurped by more sophisticated future work. In the study you are reading, do the researchers adequately describe and acknowledge earlier findings, or other key contributions from other fields or disciplines that inform aspects of the research, or the way that they interpret their results?

Greater Good’s Guide to Well-Being During Coronavirus
Practices, resources, and articles for individuals, parents, and educators facing COVID-19
This was crucial for the debates that have raged around mask mandates and social distancing. We already knew quite a bit about the efficacy of both in preventing infections, informed by centuries of practical experience and research.
When COVID-19 hit American shores, researchers and doctors did not question the necessity of masks in clinical settings. Here’s what we didn’t know: What kinds of masks would work best for the general public, who should wear them, when should we wear them, were there enough masks to go around, and could we get enough people to adopt best mask practices to make a difference in the specific context of COVID-19 ?
Over time, after a period of confusion and contradictory evidence, those questions have been answered . The very few studies that have suggested masks don’t work in stopping COVID-19 have almost all failed to account for other work on preventing the disease, and had results that simply didn’t hold up. Some were even retracted .
So, when someone shares a coronavirus study with you, it’s important to check the date. The implications of studies published early in the pandemic might be more limited and less conclusive than those published later, because the later studies could lean on and learn from previously published work. Which leads us to the next question you should ask in hearing about coronavirus research…
11. Do researchers, journalists, and politicians acknowledge limitations and entertain alternative explanations?
Is the study focused on only one side of the story or one interpretation of the data? Has it failed to consider or refute alternative explanations? Do they demonstrate awareness of which questions are answered and which aren’t by their methods? Do the journalists and politicians communicating the study know and understand these limitations?
When the Annals of Internal Medicine published a Danish study last month on the efficacy of cloth masks, some suggested that it showed masks “make no difference” against COVID-19.
The study was a good one by the standards spelled out in this article. The researchers and the journal were both credible, the study was randomized and controlled, and the sample size (4,862 people) was fairly large. Even better, the scientists went out of their way to acknowledge the limits of their work: “Inconclusive results, missing data, variable adherence, patient-reported findings on home tests, no blinding, and no assessment of whether masks could decrease disease transmission from mask wearers to others.”
Unfortunately, their scientific integrity was not reflected in the ways the study was used by some journalists, politicians, and people on social media. The study did not show that masks were useless. What it did show—and what it was designed to find out—was how much protection masks offered to the wearer under the conditions at the time in Denmark. In fact, the amount of protection for the wearer was not large, but that’s not the whole picture: We don’t wear masks mainly to protect ourselves, but to protect others from infection. Public-health recommendations have stressed that everyone needs to wear a mask to slow the spread of infection.
“We get vaccinated for the greater good, not just to protect ourselves ”
As the authors write in the paper, we need to look to other research to understand the context for their narrow results. In an editorial accompanying the paper in Annals of Internal Medicine , the editors argue that the results, together with existing data in support of masks, “should motivate widespread mask wearing to protect our communities and thereby ourselves.”
Something similar can be said of the new vaccine. “We get vaccinated for the greater good, not just to protect ourselves,” says Hass. “Being vaccinated prevents other people from getting sick. We get vaccinated for the more vulnerable in our community in addition for ourselves.”
Ultimately, the approach we should take to all new studies is a curious but skeptical one. We should take it all seriously and we should take it all with a grain of salt. You can judge a study against your experience, but you need to remember that your experience creates bias. You should try to cultivate humility, doubt, and patience. You might not always succeed; when you fail, try to admit fault and forgive yourself.
Above all, we need to try to remember that science is a process, and that conclusions always raise more questions for us to answer. That doesn’t mean we never have answers; we do. As the pandemic rages and the scientific process unfolds, we as individuals need to make the best decisions we can, with the information we have.
This article was revised and updated from a piece published by Greater Good in 2015, “ 10 Questions to Ask About Scientific Studies .”
About the Authors
Jeremy Adam Smith
Uc berkeley.
Jeremy Adam Smith edits the GGSC’s online magazine, Greater Good . He is also the author or coeditor of five books, including The Daddy Shift , Are We Born Racist? , and (most recently) The Gratitude Project: How the Science of Thankfulness Can Rewire Our Brains for Resilience, Optimism, and the Greater Good . Before joining the GGSC, Jeremy was a John S. Knight Journalism Fellow at Stanford University.
Emiliana R. Simon-Thomas
Emiliana R. Simon-Thomas, Ph.D. , is the science director of the Greater Good Science Center, where she directs the GGSC’s research fellowship program and serves as a co-instructor of its Science of Happiness and Science of Happiness at Work online courses.
You May Also Enjoy

Why Is COVID-19 Killing So Many Black Americans?

How to Keep the Greater Good in Mind During the Coronavirus Outbreak

In a Pandemic, Elbow Touches Might Keep Us Going

Why Your Sacrifices Matter During the Pandemic

How Does COVID-19 Affect Trust in Government?

How to Form a Pandemic Pod

A researcher’s view on COVID-19 vaccine hesitancy: The scientific process needs to be better explained
PhD Student in Microbiology-Immunology, Université Laval
Disclosure statement
Marc-Antoine De La Vega does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
Université Laval provides funding as a founding partner of The Conversation CA-FR.
Université Laval provides funding as a member of The Conversation CA.
View all partners
When I first wrote about the arrival of SARS-CoV-2 in early March 2020, the question was whether or not the new virus would become a pandemic. At the time, most experts believed that we had already reached the point of no return.
Today, 18 months later, the answer is clear. You don’t need to be a scientist to know it. This pandemic is the worst public health emergency of international concern that our modern society has faced. To date, more than 215 million cases have been confirmed and 4.5 million deaths have been reported globally .
These are just the reported cases. In reality, the number of cases is higher, and for a variety of reasons: lack of diagnostic capacity, infection without symptoms, unwillingness or inability to be tested or to visit a health facility, etc. The number of deaths due to COVID-19 is probably underestimated, both in Canada and worldwide .
In addition to changing the way we live our daily lives, the pandemic has brought scientific processes to public attention. Researchers, used to working in the shadows, now had to provide solutions — and explanations — to a very real threat, and they have been doing this under the watchful eye of the public.

One of these solutions, vaccination, is far from new. Yet no matter what the context, it has always generated news . So where are we now?
Still in our laboratories! I recently completed my PhD in microbiology-immunology at Laval University, research that I conducted under the supervision of Professor Gary Kobigner , who is known for co-developing an effective vaccine and treatment for Ebola. This fall, I will begin a postdoctoral fellowship at the Galveston National Laboratory in Texas, where I will continue my work on the transmission of, and vaccine development against, severe pathogens.
Relevant questions
The World Health Organization (WHO) currently lists 13 available COVID-19 vaccines, based on four different platforms, including mRNA vaccines and viral vector vaccines . Globally, more than five billion doses of vaccines have been administered. In Canada, five of these vaccines are currently approved for use: Pfizer-BioNTech, Moderna, AstraZeneca, COVISHIELD and Janssen , with Pfizer-BioNTech, Moderna and AstraZeneca in wide distribution. Combined, these vaccines have been administered to approximately 70 per cent of Canadians.

However, many people have raised questions about these vaccines . And it is fair to do so! The unknown has always been a source of anxiety for human beings, it is normal to ask questions .
So, after working tirelessly to develop vaccines against COVID-19, what are scientists and doctors doing now?
They are doing what they have always done: Practising the best science they can within the limits of current knowledge. This scientific practice means continuing to evaluate the effectiveness of these vaccines against new variants in labs, as the virus continues to mutate.
It means continuing to record who has experienced side-effects (serious or not) from vaccination and continuing to investigate the potential links between these side-effects and the vaccine. The science they are practising involves studying the virus day and night to understand how it makes people sick, how we can prevent infection and what our options are for getting rid of it as quickly as possible.
The term “current knowledge” is very important here. It is possible that more side-effects related to vaccination will be discovered much later. Here’s why.
The scientific method
When vaccines are initially developed in the laboratory and tested on animals, it is normal that not all side-effects are identified. A mouse is not a human, after all, and models cannot account for all the variables that can be found in a human. Humans live in a complex environment and society where individuals each have their own genetics, immunity and lifestyle (exercise, smoking, nutrition).
Furthermore, the more people are vaccinated, the greater the likelihood of detecting a serious side-effect. Clinical trials, where drugs and vaccines are evaluated in a small group of individuals before being made available to the general population, are designed to be safe. Volunteers are usually healthy adults, without serious pre-existing medical conditions .
Read more: Explainer: How clinical trials test COVID-19 vaccines
Vaccination is now widespread in many countries. It is therefore statistically normal that rarer effects (for example, ones that one in a million people develop) are now being observed. These effects are too rare to have been detected in a clinical trial of 10,000 people. This is the case for rare side-effects such as Guillain-Barré syndrome and Bell’s palsy .
The scientific method requires that the following process is followed: Observe a problem, formulate a hypothesis about its possible causes, evaluate it experimentally by controlling the variables, interpret the results and draw a conclusion.
It can turn out that our initial hypothesis is wrong, and that is equally acceptable. This is how science was designed. I think that before the pandemic, people considered science infallible. Opening up research to the general public has greatly changed this perception, especially as science quickly became embroiled in politics, particularly over the question of the origin of the pandemic .

Knowing how to communicate
And that’s where the problem comes from, among other things. The key to effective scientific communication is not the science. It’s the communication . The results of laboratory experiments and clinical trials are what they are. Either the vaccine or drug works to reduce mortality, or it doesn’t work, and we go back to the drawing board.
So where does the reluctance about vaccines come from? One of the main problems is not the lack of information about the safety of the vaccine. Almost everyone has access to this information on internet. The problem is the lack of trust in institutions, which has been growing globally in recent years .
Read more: How better conversations can help reduce vaccine hesitancy for COVID-19 and other shots
But this trust can be earned — or regained. It just takes time, respect and empathy. A study by researchers at the Centre Hospitalier Universitaire de Sherbrooke shows that an educational session about immunization that used motivational interviewing techniques with parents of infants resulted in a nine per cent increase in immunization rates compared with families who did not receive the sessions.
Finding the right answer to a question
Ultimately, the goal of science is to find the right answer to a question.
Of course, human nature being what it is, we are not immune to conflicts of interest. We need to ensure transparency about things like funding and links between scientists and potential investors. This is especially important since we are all responsible for funding research, whether through federal subsidies, which are partly derived from taxes paid by citizens, or through the ordinary purchase of drugs in pharmacies.
Since this concerns everyone, it is high time that the public became more involved. After all, scientific discoveries and health measures are everybody’s business. For example, few citizens are familiar with “ gain-of-function research .” These studies can involve a level of risk ranging from very low to very high. For example, producing a drug from a bacterium carries little risk and much benefit. However, increasing the virulence or transmissibility of a virus such as Ebola or Influenza could carry a lot of risk if such research were carried out by individuals with bad intentions, or in poorly secured laboratories.
Read more: Origins of SARS-CoV-2: Why the lab-leak idea is being considered again
As with any aspect of science, a risk-benefit analysis must be carried out. Note that in the vast majority of institutions where research is done, the committees assessing whether or not a study is worth doing are not only composed of scientists and students, but also members of the public.
Now each side just has to do its part. Scientists need to do a better job of communicating their results and the interpretation of them, as well as specifically answering questions of interest to the public and regaining their trust. They need to listen and stop hiding behind mountains of data, complicated words and scientific articles that are not easily accessible to the general public.
To those who are hesitant about vaccination, scientists should ask: “What data would make you change your mind?”, “Why do you think the current data are insufficient?”, “Why do you trust this individual, but not another or the institutions?” This is how constructive dialogue can be initiated and more in-depth reflection can begin.
For their part, citizens can adopt better practices when it comes to getting information and not only consider information that fits into their personal narrative. It is also important to avoid falling into a spiral of conspiracy theories and trust in false experts. It is important to not be afraid to doubt, to find other sources to confirm or refute what you have just read and to ask trusted experts around you what they think.
Do you have a question about COVID-19 vaccines? Email us at ca‑[email protected] and vaccine experts will answer questions in upcoming articles.
This article was originally published in French
- Science communication
- Scientific method
- Coronavirus
- AstraZeneca vaccine
- Vaccine hesitancy
- COVID-19 vaccines
- Moderna vaccine
- Pfizer-BioNTech vaccine
- Vaccine confidence
- Vaccine confidence in Canada
- Listen to this article

Head of School, School of Arts & Social Sciences, Monash University Malaysia

Chief Operating Officer (COO)

Clinical Teaching Fellow

Data Manager

Director, Social Policy
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Available Evidence and Ongoing Hypothesis on Corona Virus (COVID-19) and Psychosis: Is Corona Virus and Psychosis Related? A Narrative Review
Affiliations.
- 1 Department of Psychiatry, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia.
- 2 Department of Psychiatry, College of Health and Medical Sciences, Mettu University, Mettu, Ethiopia.
- PMID: 32903810
- PMCID: PMC7445510
- DOI: 10.2147/PRBM.S264235
Background: Corona virus (COVID-19) is an outbreak of respiratory disease caused by a novel corona virus and declared to be a global health emergency and a pandemic by the World Health Organization (WHO) on March 11, 2020. Prevention strategies to control the transmission of the COVID-19 pandemic, such as closing of schools, refraining from gathering, and social distancing, have direct impacts on mental well-being. SARS-CoV-2 has a devastating psychological impact on the mental health status of the community and, particularly when associated with psychotic symptoms, it could affect the overall quality-of-life. The virus also has the potential to enter and infect the brain. As a result, psychosis symptoms could be an emerging phenomenon associated with the corona virus pandemic. The presence of psychotic symptoms may complicate the management options of patients with COVID-19.
Objective: The aim of this article review is to elaborate the relationships between COVID-19 and psychotic symptoms.
Methodology: We independently searched different electronic databases, such as Google scholar, PubMed, Medline, CINAHL, EMBASE, PsychInfo, and other relevant sources published in English globally, by using the search terms "psychosis and COVID-19", "corona virus", "brief psychotic", "schizophrenia", "organic psychosis", "infectious disease", "mental illness", "pandemics", and "psychiatry" in various permutations and combinations.
Results: The results of the included studies revealed that patients with a novel corona virus had psychotic symptoms, including hallucination in different forms of modality, delusion, disorganized speech, and grossly disorganized or catatonic behaviors. The patients with COVID-19-related psychotic symptoms had responded with a short-term administration of the antipsychotic medication.
Conclusion and recommendation: A corona virus-related psychosis has been identified in different nations, but it is difficult to conclude that a novel corona virus has been biologically related to psychosis or exacerbates psychotic symptoms. Therefore, to identify the causal relationships between COVID-19 and psychosis, the researchers should investigate the prospective study on the direct biological impacts of COVID-19 and psychosis, and the clinicians should pay attention for psychotic symptoms at the treatment center and isolation rooms in order to reduce the complication of a novel corona virus.
Keywords: 2020; COVID-19; SARS-CoV-2; psychosis.
© 2020 Tariku and Hajure.
PubMed Disclaimer
Conflict of interest statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Similar articles
- COVID-19 associated psychosis. Messina A, Signorelli MS. Messina A, et al. Ind Psychiatry J. 2023 Jul-Dec;32(2):215-221. doi: 10.4103/ipj.ipj_27_23. Epub 2023 Jul 12. Ind Psychiatry J. 2023. PMID: 38161482 Free PMC article. Review.
- Letter to the Editor: THE IMPACT OF THE COVID-19 PANDEMIC ON SCHIZOPHRENIA PATIENTS. Hoşgelen EI, Alptekin K. Hoşgelen EI, et al. Turk Psikiyatri Derg. 2021 Fall;32(3):219-221. doi: 10.5080/u26175. Turk Psikiyatri Derg. 2021. PMID: 34750798 English, Turkish.
- Letter to the Editor: THE IMPACT OF THE COVID-19 PANDEMIC ON SCHIZOPHRENIA PATIENTS. Hoşgelen EI, Alptekin K. Hoşgelen EI, et al. Turk Psikiyatri Derg. 2021 Fall;32(3):219-221. Turk Psikiyatri Derg. 2021. PMID: 34637131 English, Turkish.
- Post COVID-19 Infection Psychosis: Could SARS-CoV-2 Virus Infection Be a Neuropsychiatric Condition That Triggers Psychotic Disorders? - A Case-Based Short Review. Vasile CI, Vasile MC, Zlati ML, Herbei EE, Lepădatu L, Munteanu C, Nechifor A, Tatu AL. Vasile CI, et al. Infect Drug Resist. 2022 Aug 22;15:4697-4705. doi: 10.2147/IDR.S373578. eCollection 2022. Infect Drug Resist. 2022. PMID: 36034176 Free PMC article.
- Psychosis during the COVID-19 pandemic: A systematic review of case reports and case series. Chaudhary AMD, Musavi NB, Saboor S, Javed S, Khan S, Naveed S. Chaudhary AMD, et al. J Psychiatr Res. 2022 Sep;153:37-55. doi: 10.1016/j.jpsychires.2022.06.041. Epub 2022 Jul 1. J Psychiatr Res. 2022. PMID: 35797814 Free PMC article. Review.
- Clinical Features and Prognosis of Coronavirus Disease 2019-Related Psychosis: A Retrospective Case Series. Du J, Zhou X, Guo Y, Jiang F, Yan M, Zhu Q. Du J, et al. Alpha Psychiatry. 2023 Nov 1;24(6):276-282. doi: 10.5152/alphapsychiatry.2023.231266. eCollection 2023 Nov. Alpha Psychiatry. 2023. PMID: 38313441 Free PMC article.
- Inflammation and viral infection as disease modifiers in schizophrenia. Klein HC, Guest PC, Dobrowolny H, Steiner J. Klein HC, et al. Front Psychiatry. 2023 Oct 2;14:1231750. doi: 10.3389/fpsyt.2023.1231750. eCollection 2023. Front Psychiatry. 2023. PMID: 37850104 Free PMC article. Review.
- New-onset acute psychosis as a manifestation of lupus cerebritis following concomitant COVID-19 infection and vaccination: a rare case report. Fekih-Romdhane F, Ghrissi F, Hallit S, Cheour M. Fekih-Romdhane F, et al. BMC Psychiatry. 2023 Jun 12;23(1):419. doi: 10.1186/s12888-023-04924-4. BMC Psychiatry. 2023. PMID: 37308940 Free PMC article.
- Recent outbreak of Marburg virus disease: Could it be a threat for global public health? Sohan M, Shahriar M, Bhuiyan MA, Islam MR. Sohan M, et al. Health Sci Rep. 2022 Nov 29;6(1):e971. doi: 10.1002/hsr2.971. eCollection 2023 Jan. Health Sci Rep. 2022. PMID: 36467750 Free PMC article. No abstract available.
- Rampal L, Seng LB. Coronavirus disease (COVID-19) pandemic. Med J Malaysia. 2020. - PubMed
- WHO. Novel coronavirus (2019-nCoV) situation report - 1. WHO Bull. 2020.
- Baig AM, Khaleeq A, Ali U, Syeda H. Evidence of the COVID-19 virus targeting the CNS: tissue distribution, host-virus interaction, and proposed neurotropic mechanisms. ACS Chem Neurosci. 2020;11(7):995–998. doi:10.1021/acschemneuro.0c00122 - DOI - PubMed
- Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77(6):683–690. doi:10.1001/jamaneurol.2020.1127 - DOI - PMC - PubMed
- Van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2009;39(2):179–195. doi:10.1017/S0033291708003814 - DOI - PubMed
Publication types
- Search in MeSH
Related information
Grants and funding, linkout - more resources, full text sources.
- Dove Medical Press
- Europe PubMed Central
- PubMed Central
Research Materials
- NCI CPTC Antibody Characterization Program
Miscellaneous
- NCI CPTAC Assay Portal

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- About This IR
- Scholar Commons
Advancing Education in Quantitative Literacy
Home > Open Access Journals > NUMERACY > Vol. 14 (2021) > Iss. 1
Using COVID-19 Vaccine Efficacy Data to Teach One-Sample Hypothesis Testing
Frank Wang , LaGuardia Community College, CUNY Follow
COVID-19, hypothesis testing, Bayes’s rule, quantitative reasoning
In late November 2020, there was a flurry of media coverage of two companies’ claims of 95% efficacy rates of newly developed COVID-19 vaccines, but information about the confidence interval was not reported. This paper presents a way of teaching the concept of hypothesis testing and the construction of confidence intervals using numbers announced by the drug makers Pfizer and Moderna publicized by the media. Instead of a two-sample test or more complicated statistical models, we use the elementary one-proportion z -test to analyze the data. The method is designed to be accessible for students who have only taken a one-semester elementary statistics course. We will justify the use of a z -distribution as an approximation for the confidence interval of the efficacy rate. Bayes’s rule will be applied to relate the probability of being in the vaccine group among the volunteers who were infected by COVID-19 to the more consequential probability of being infected by COVID-19 given that the person is vaccinated.
https://doi.org/10.5038/1936-4660.14.1.1383
Recommended Citation
Wang, Frank. "Using COVID-19 Vaccine Efficacy Data to Teach One-Sample Hypothesis Testing." Numeracy 14, Iss. 1 (2021): Article 7. DOI: https://doi.org/10.5038/1936-4660.14.1.1383
Creative Commons License
Since January 11, 2021
Included in
Clinical Trials Commons , Higher Education and Teaching Commons
- Journal Home
- About This Journal
- Editorial Board
- Instructions to Authors
- Ethics and Malpractice Statement
- Submit Article
- Most Popular Papers
- Receive Email Notices or RSS
Advanced Search
ISSN: 1936-4660 (Online)
Scholar Commons | About This IR | FAQ | My Account | Accessibility Statement
Privacy Copyright

- CORONAVIRUS COVERAGE
What you need to know about the COVID-19 lab-leak hypothesis
Newly reported information has revived scrutiny of this possible origin for the coronavirus, which experts still call unlikely though worth investigating.
Months after a World Health Organization investigation deemed it “extremely unlikely” that the novel coronavirus escaped accidentally from a laboratory in Wuhan, China, the idea is back in the news, giving new momentum to a hypothesis that many scientists believe is unlikely, and some have dismissed as a conspiracy theory .
The renewed attention comes on the heels of President Joe Biden’s ordering U.S. intelligence agencies on May 26 to “ redouble their efforts ” to investigate the origins of the coronavirus. On May 11, Biden’s chief medical adviser, Anthony Fauci, acknowledged he’s now “ not convinced ” the virus developed naturally—an apparent pivot from what he told National Geographic in an interview last year.
Also last month, more than a dozen scientists—top epidemiologists, immunologists, and biologists—wrote a letter published in the journal Science calling for a thorough investigation into two viable origin stories: natural spillover from animal to human, or an accident in which a wild laboratory sample containing SARS-CoV-2 was accidentally released. They urged that both hypotheses “be taken seriously until we have sufficient data,” writing that a proper investigation would be “transparent, objective, data-driven, inclusive of broad expertise, subject to independent oversight,” with conflicts of interest minimized, if possible.
“Anytime there is an infectious disease outbreak it is important to investigate its origin,” says Amesh Adalja, an infectious disease physician and senior scholar at the Johns Hopkins University Center for Health Security who did not contribute to the letter in Science . “The lab-leak hypothesis is possible—as is an animal spillover,” he says, “and I think that a thorough, independent investigation of its origins should be conducted.”
Unanswered questions
The origins of SARS-CoV-2, the virus that causes COVID-19 and has infected more than 171 million people, killing close to 3.7 million worldwide as of June 4, remain unclear. Many scientists, including those that participated in the WHO’s months-long investigation, believe the most likely explanation is that that it jumped from an animal to a person—potentially from a bat directly to a human, or through an intermediate host. Animal-to-human transmission is a common route for many viruses; at least two other coronaviruses, SARS and MERS , were spread through such zoonotic spillover.
Other scientists insist it’s worth investigating whether SARS-CoV-2 escaped from the Wuhan Institute of Virology, a laboratory that has studied coronaviruses in bats for more than a decade.
The WHO investigation —a joint effort between WHO-appointed scientists and Chinese officials—concluded it was “extremely unlikely” the highly transmissible virus escaped from a laboratory. But the WHO team suffered roadblocks that led some to question its conclusions; the scientists were not permitted to conduct an independent investigation and were denied access to any raw data. ( We still don’t know the origins of the coronavirus. Here are 4 scenarios .)
On March 30, when the WHO released its report, its director-general, Tedros Adhanom Ghebreyesus, called for further studies . “All hypotheses remain on the table,” he said at the time.
Then on May 11, Fauci told PolitiFact that while the virus most likely emerged via animal-to-human transmission, “it could have been something else, and we need to find that out.”
Recently disclosed evidence, first reported by the Wall Street Journal , has added fuel to the fire: Three researchers from the Wuhan Institute of Virology fell sick in November 2019 and sought hospital care, according to a U.S. intelligence report. In the final days of the Trump administration, the State Department released a statement that researchers at the institute had become ill with “symptoms consistent with both COVID-19 and common seasonal illness.”
You May Also Like

What is white lung syndrome? Here's what to know about pneumonia

COVID-19 is more widespread in animals than we thought

A deer may have passed COVID-19 to a person, study suggests
Most epidemiologists and virologists who have studied the novel coronavirus believe that it began spreading in November 2019. China says the first confirmed case was on December 8, 2019. During a briefing in Beijing this week, China’s foreign ministry spokesperson, Zhao Lijian, accused the U.S. of “ hyping up the theory of a lab leak ,” and asked, “does it really care about the study of origin tracing, or is it trying to divert attention?” Zhao also denied the Wall Street Journal report that three people had gotten sick.
Lab leak still ‘unlikely’
Some conservative politicians and commentators have embraced the lab-leak theory, while liberals more readily rejected it, especially early in the pandemic. The speculation has also heightened ongoing tensions between the U.S. and China.
On May 26, as the U.S. Senate passed a bill to declassify intelligence related to potential links between the Wuhan laboratory and COVID-19, Missouri Senator Josh Hawley, a Republican who sponsored the bill, said, “the world needs to know if this pandemic was the product of negligence at the Wuhan lab,” and lamented that “for over a year, anyone asking questions about the Wuhan Institute of Virology has been branded as a conspiracy theorist.”
Peter Navarro, Donald Trump’s former trade adviser, asserted in April 2020 that SARS-CoV-2 could have been engineered as a bioweapon, without citing any evidence.
The theory that SARS-CoV-2 was created as a bioweapon is “completely unlikely,” says William Schaffner, a professor of infectious diseases at Vanderbilt University Medical Center. For one thing, he explains, for a bioweapon to be successful, it must target an adversarial population without affecting one’s own. In contrast, SARS-CoV-2 “cannot be controlled,” he says. “It will spread, including back on your own population,” making it an extremely “counterproductive biowarfare agent.”
The more plausible lab-leak hypothesis, scientists say, is that the Wuhan laboratory isolated the novel coronavirus from an animal and was studying it when it accidentally escaped. “Not knowing the extent of its virulence and transmissibility, a lack of protective measures [could have] resulted in laboratory workers becoming infected,” initiating the transmission chain that ultimately resulted in the pandemic, says Rossi Hassad, an epidemiologist at Mercy College.
But Hassad adds he believes that this lab-leak theory is on the “extreme low end” of possibilities, and it “will quite likely remain only theoretical following any proper scientific investigation,” he says.
Biden ordered U.S. intelligence agencies to report back with their findings in 90 days, which would be August 26.
Based on the available information, Eyal Oren, an epidemiologist at San Diego State University, says it’s apparent why the most accepted hypothesis is that this virus originated in an animal and jumped to a human: “What is clear is that the genetic sequence of the COVID-19 virus is similar to other coronaviruses found in bats,” he says.
Some scientists remain skeptical that concrete conclusions can be drawn. “At the end, I anticipate that the question” of SARS-CoV-2’s origins “will remain unresolved,” Schaffner says.
In the meantime, science “moves much more slowly than the media and news cycles,” Oren says.
Related Topics
- CORONAVIRUS
- PUBLIC HEALTH
- WILDLIFE WATCHING

Seeking the Source of Ebola

5 things to know about COVID-19 tests in the age of Omicron
Here's what we know about the BA.2 Omicron subvariant driving a new COVID-19 wave

Hippos, hyenas, and other animals are contracting COVID-19

Humans are creating hot spots where bats could transmit zoonotic diseases
- Environment
- Paid Content
- Photography
History & Culture
- History & Culture
- History Magazine
- Mind, Body, Wonder
- Terms of Use
- Privacy Policy
- Your US State Privacy Rights
- Children's Online Privacy Policy
- Interest-Based Ads
- About Nielsen Measurement
- Do Not Sell or Share My Personal Information
- Nat Geo Home
- Attend a Live Event
- Book a Trip
- Inspire Your Kids
- Shop Nat Geo
- Visit the D.C. Museum
- Learn About Our Impact
- Support Our Mission
- Advertise With Us
- Customer Service
- Renew Subscription
- Manage Your Subscription
- Work at Nat Geo
- Sign Up for Our Newsletters
- Contribute to Protect the Planet
Copyright © 1996-2015 National Geographic Society Copyright © 2015-2024 National Geographic Partners, LLC. All rights reserved
Why the Pandemic Probably Started in a Lab, in 5 Key Points

By Alina Chan
Dr. Chan is a molecular biologist at the Broad Institute of M.I.T. and Harvard, and a co-author of “Viral: The Search for the Origin of Covid-19.”
This article has been updated to reflect news developments.
On Monday, Dr. Anthony Fauci returned to the halls of Congress and testified before the House subcommittee investigating the Covid-19 pandemic. He was questioned about several topics related to the government’s handling of Covid-19, including how the National Institute of Allergy and Infectious Diseases, which he directed until retiring in 2022, supported risky virus work at a Chinese institute whose research may have caused the pandemic.
For more than four years, reflexive partisan politics have derailed the search for the truth about a catastrophe that has touched us all. It has been estimated that at least 25 million people around the world have died because of Covid-19, with over a million of those deaths in the United States.
Although how the pandemic started has been hotly debated, a growing volume of evidence — gleaned from public records released under the Freedom of Information Act, digital sleuthing through online databases, scientific papers analyzing the virus and its spread, and leaks from within the U.S. government — suggests that the pandemic most likely occurred because a virus escaped from a research lab in Wuhan, China. If so, it would be the most costly accident in the history of science.
Here’s what we now know:

1 The SARS-like virus that caused the pandemic emerged in Wuhan, the city where the world’s foremost research lab for SARS-like viruses is located.
- At the Wuhan Institute of Virology, a team of scientists had been hunting for SARS-like viruses for over a decade, led by Shi Zhengli.
- Their research showed that the viruses most similar to SARS‑CoV‑2, the virus that caused the pandemic, circulate in bats that live r oughly 1,000 miles away from Wuhan. Scientists from Dr. Shi’s team traveled repeatedly to Yunnan province to collect these viruses and had expanded their search to Southeast Asia. Bats in other parts of China have not been found to carry viruses that are as closely related to SARS-CoV-2.

The closest known relatives to SARS-CoV-2 were found in southwestern China and in Laos.
Large cities
Mine in Yunnan province
Cave in Laos
South China Sea

The closest known relatives to SARS-CoV-2
were found in southwestern China and in Laos.
philippines

The closest known relatives to SARS-CoV-2 were found
in southwestern China and Laos.
Sources: Sarah Temmam et al., Nature; SimpleMaps
Note: Cities shown have a population of at least 200,000.

There are hundreds of large cities in China and Southeast Asia.

There are hundreds of large cities in China
and Southeast Asia.

The pandemic started roughly 1,000 miles away, in Wuhan, home to the world’s foremost SARS-like virus research lab.

The pandemic started roughly 1,000 miles away,
in Wuhan, home to the world’s foremost SARS-like virus research lab.

The pandemic started roughly 1,000 miles away, in Wuhan,
home to the world’s foremost SARS-like virus research lab.
- Even at hot spots where these viruses exist naturally near the cave bats of southwestern China and Southeast Asia, the scientists argued, as recently as 2019 , that bat coronavirus spillover into humans is rare .
- When the Covid-19 outbreak was detected, Dr. Shi initially wondered if the novel coronavirus had come from her laboratory , saying she had never expected such an outbreak to occur in Wuhan.
- The SARS‑CoV‑2 virus is exceptionally contagious and can jump from species to species like wildfire . Yet it left no known trace of infection at its source or anywhere along what would have been a thousand-mile journey before emerging in Wuhan.
2 The year before the outbreak, the Wuhan institute, working with U.S. partners, had proposed creating viruses with SARS‑CoV‑2’s defining feature.
- Dr. Shi’s group was fascinated by how coronaviruses jump from species to species. To find viruses, they took samples from bats and other animals , as well as from sick people living near animals carrying these viruses or associated with the wildlife trade. Much of this work was conducted in partnership with the EcoHealth Alliance, a U.S.-based scientific organization that, since 2002, has been awarded over $80 million in federal funding to research the risks of emerging infectious diseases.
- The laboratory pursued risky research that resulted in viruses becoming more infectious : Coronaviruses were grown from samples from infected animals and genetically reconstructed and recombined to create new viruses unknown in nature. These new viruses were passed through cells from bats, pigs, primates and humans and were used to infect civets and humanized mice (mice modified with human genes). In essence, this process forced these viruses to adapt to new host species, and the viruses with mutations that allowed them to thrive emerged as victors.
- By 2019, Dr. Shi’s group had published a database describing more than 22,000 collected wildlife samples. But external access was shut off in the fall of 2019, and the database was not shared with American collaborators even after the pandemic started , when such a rich virus collection would have been most useful in tracking the origin of SARS‑CoV‑2. It remains unclear whether the Wuhan institute possessed a precursor of the pandemic virus.
- In 2021, The Intercept published a leaked 2018 grant proposal for a research project named Defuse , which had been written as a collaboration between EcoHealth, the Wuhan institute and Ralph Baric at the University of North Carolina, who had been on the cutting edge of coronavirus research for years. The proposal described plans to create viruses strikingly similar to SARS‑CoV‑2.
- Coronaviruses bear their name because their surface is studded with protein spikes, like a spiky crown, which they use to enter animal cells. T he Defuse project proposed to search for and create SARS-like viruses carrying spikes with a unique feature: a furin cleavage site — the same feature that enhances SARS‑CoV‑2’s infectiousness in humans, making it capable of causing a pandemic. Defuse was never funded by the United States . However, in his testimony on Monday, Dr. Fauci explained that the Wuhan institute would not need to rely on U.S. funding to pursue research independently.

The Wuhan lab ran risky experiments to learn about how SARS-like viruses might infect humans.
1. Collect SARS-like viruses from bats and other wild animals, as well as from people exposed to them.

2. Identify high-risk viruses by screening for spike proteins that facilitate infection of human cells.

2. Identify high-risk viruses by screening for spike proteins that facilitate infection of
human cells.

In Defuse, the scientists proposed to add a furin cleavage site to the spike protein.
3. Create new coronaviruses by inserting spike proteins or other features that could make the viruses more infectious in humans.

4. Infect human cells, civets and humanized mice with the new coronaviruses, to determine how dangerous they might be.

- While it’s possible that the furin cleavage site could have evolved naturally (as seen in some distantly related coronaviruses), out of the hundreds of SARS-like viruses cataloged by scientists, SARS‑CoV‑2 is the only one known to possess a furin cleavage site in its spike. And the genetic data suggest that the virus had only recently gained the furin cleavage site before it started the pandemic.
- Ultimately, a never-before-seen SARS-like virus with a newly introduced furin cleavage site, matching the description in the Wuhan institute’s Defuse proposal, caused an outbreak in Wuhan less than two years after the proposal was drafted.
- When the Wuhan scientists published their seminal paper about Covid-19 as the pandemic roared to life in 2020, they did not mention the virus’s furin cleavage site — a feature they should have been on the lookout for, according to their own grant proposal, and a feature quickly recognized by other scientists.
- Worse still, as the pandemic raged, their American collaborators failed to publicly reveal the existence of the Defuse proposal. The president of EcoHealth, Peter Daszak, recently admitted to Congress that he doesn’t know about virus samples collected by the Wuhan institute after 2015 and never asked the lab’s scientists if they had started the work described in Defuse. In May, citing failures in EcoHealth’s monitoring of risky experiments conducted at the Wuhan lab, the Biden administration suspended all federal funding for the organization and Dr. Daszak, and initiated proceedings to bar them from receiving future grants. In his testimony on Monday, Dr. Fauci said that he supported the decision to suspend and bar EcoHealth.
- Separately, Dr. Baric described the competitive dynamic between his research group and the institute when he told Congress that the Wuhan scientists would probably not have shared their most interesting newly discovered viruses with him . Documents and email correspondence between the institute and Dr. Baric are still being withheld from the public while their release is fiercely contested in litigation.
- In the end, American partners very likely knew of only a fraction of the research done in Wuhan. According to U.S. intelligence sources, some of the institute’s virus research was classified or conducted with or on behalf of the Chinese military . In the congressional hearing on Monday, Dr. Fauci repeatedly acknowledged the lack of visibility into experiments conducted at the Wuhan institute, saying, “None of us can know everything that’s going on in China, or in Wuhan, or what have you. And that’s the reason why — I say today, and I’ve said at the T.I.,” referring to his transcribed interview with the subcommittee, “I keep an open mind as to what the origin is.”
3 The Wuhan lab pursued this type of work under low biosafety conditions that could not have contained an airborne virus as infectious as SARS‑CoV‑2.
- Labs working with live viruses generally operate at one of four biosafety levels (known in ascending order of stringency as BSL-1, 2, 3 and 4) that describe the work practices that are considered sufficiently safe depending on the characteristics of each pathogen. The Wuhan institute’s scientists worked with SARS-like viruses under inappropriately low biosafety conditions .

In the United States, virologists generally use stricter Biosafety Level 3 protocols when working with SARS-like viruses.
Biosafety cabinets prevent
viral particles from escaping.
Viral particles
Personal respirators provide
a second layer of defense against breathing in the virus.
DIRECT CONTACT
Gloves prevent skin contact.
Disposable wraparound
gowns cover much of the rest of the body.

Personal respirators provide a second layer of defense against breathing in the virus.
Disposable wraparound gowns
cover much of the rest of the body.
Note: Biosafety levels are not internationally standardized, and some countries use more permissive protocols than others.

The Wuhan lab had been regularly working with SARS-like viruses under Biosafety Level 2 conditions, which could not prevent a highly infectious virus like SARS-CoV-2 from escaping.
Some work is done in the open air, and masks are not required.
Less protective equipment provides more opportunities
for contamination.

Some work is done in the open air,
and masks are not required.
Less protective equipment provides more opportunities for contamination.
- In one experiment, Dr. Shi’s group genetically engineered an unexpectedly deadly SARS-like virus (not closely related to SARS‑CoV‑2) that exhibited a 10,000-fold increase in the quantity of virus in the lungs and brains of humanized mice . Wuhan institute scientists handled these live viruses at low biosafet y levels , including BSL-2.
- Even the much more stringent containment at BSL-3 cannot fully prevent SARS‑CoV‑2 from escaping . Two years into the pandemic, the virus infected a scientist in a BSL-3 laboratory in Taiwan, which was, at the time, a zero-Covid country. The scientist had been vaccinated and was tested only after losing the sense of smell. By then, more than 100 close contacts had been exposed. Human error is a source of exposure even at the highest biosafety levels , and the risks are much greater for scientists working with infectious pathogens at low biosafety.
- An early draft of the Defuse proposal stated that the Wuhan lab would do their virus work at BSL-2 to make it “highly cost-effective.” Dr. Baric added a note to the draft highlighting the importance of using BSL-3 to contain SARS-like viruses that could infect human cells, writing that “U.S. researchers will likely freak out.” Years later, after SARS‑CoV‑2 had killed millions, Dr. Baric wrote to Dr. Daszak : “I have no doubt that they followed state determined rules and did the work under BSL-2. Yes China has the right to set their own policy. You believe this was appropriate containment if you want but don’t expect me to believe it. Moreover, don’t insult my intelligence by trying to feed me this load of BS.”
- SARS‑CoV‑2 is a stealthy virus that transmits effectively through the air, causes a range of symptoms similar to those of other common respiratory diseases and can be spread by infected people before symptoms even appear. If the virus had escaped from a BSL-2 laboratory in 2019, the leak most likely would have gone undetected until too late.
- One alarming detail — leaked to The Wall Street Journal and confirmed by current and former U.S. government officials — is that scientists on Dr. Shi’s team fell ill with Covid-like symptoms in the fall of 2019 . One of the scientists had been named in the Defuse proposal as the person in charge of virus discovery work. The scientists denied having been sick .
4 The hypothesis that Covid-19 came from an animal at the Huanan Seafood Market in Wuhan is not supported by strong evidence.
- In December 2019, Chinese investigators assumed the outbreak had started at a centrally located market frequented by thousands of visitors daily. This bias in their search for early cases meant that cases unlinked to or located far away from the market would very likely have been missed. To make things worse, the Chinese authorities blocked the reporting of early cases not linked to the market and, claiming biosafety precautions, ordered the destruction of patient samples on January 3, 2020, making it nearly impossible to see the complete picture of the earliest Covid-19 cases. Information about dozens of early cases from November and December 2019 remains inaccessible.
- A pair of papers published in Science in 2022 made the best case for SARS‑CoV‑2 having emerged naturally from human-animal contact at the Wuhan market by focusing on a map of the early cases and asserting that the virus had jumped from animals into humans twice at the market in 2019. More recently, the two papers have been countered by other virologists and scientists who convincingly demonstrate that the available market evidence does not distinguish between a human superspreader event and a natural spillover at the market.
- Furthermore, the existing genetic and early case data show that all known Covid-19 cases probably stem from a single introduction of SARS‑CoV‑2 into people, and the outbreak at the Wuhan market probably happened after the virus had already been circulating in humans.

An analysis of SARS-CoV-2’s evolutionary tree shows how the virus evolved as it started to spread through humans.
SARS-COV-2 Viruses closest
to bat coronaviruses
more mutations

Source: Lv et al., Virus Evolution (2024) , as reproduced by Jesse Bloom

The viruses that infected people linked to the market were most likely not the earliest form of the virus that started the pandemic.

- Not a single infected animal has ever been confirmed at the market or in its supply chain. Without good evidence that the pandemic started at the Huanan Seafood Market, the fact that the virus emerged in Wuhan points squarely at its unique SARS-like virus laboratory.
5 Key evidence that would be expected if the virus had emerged from the wildlife trade is still missing.

In previous outbreaks of coronaviruses, scientists were able to demonstrate natural origin by collecting multiple pieces of evidence linking infected humans to infected animals.
Infected animals
Earliest known
cases exposed to
live animals
Antibody evidence
of animals and
animal traders having
been infected
Ancestral variants
of the virus found in
Documented trade
of host animals
between the area
where bats carry
closely related viruses
and the outbreak site

Infected animals found
Earliest known cases exposed to live animals
Antibody evidence of animals and animal
traders having been infected
Ancestral variants of the virus found in animals
Documented trade of host animals
between the area where bats carry closely
related viruses and the outbreak site

For SARS-CoV-2, these same key pieces of evidence are still missing , more than four years after the virus emerged.

For SARS-CoV-2, these same key pieces of evidence are still missing ,
more than four years after the virus emerged.
- Despite the intense search trained on the animal trade and people linked to the market, investigators have not reported finding any animals infected with SARS‑CoV‑2 that had not been infected by humans. Yet, infected animal sources and other connective pieces of evidence were found for the earlier SARS and MERS outbreaks as quickly as within a few days, despite the less advanced viral forensic technologies of two decades ago.
- Even though Wuhan is the home base of virus hunters with world-leading expertise in tracking novel SARS-like viruses, investigators have either failed to collect or report key evidence that would be expected if Covid-19 emerged from the wildlife trade . For example, investigators have not determined that the earliest known cases had exposure to intermediate host animals before falling ill. No antibody evidence shows that animal traders in Wuhan are regularly exposed to SARS-like viruses, as would be expected in such situations.
- With today’s technology, scientists can detect how respiratory viruses — including SARS, MERS and the flu — circulate in animals while making repeated attempts to jump across species . Thankfully, these variants usually fail to transmit well after crossing over to a new species and tend to die off after a small number of infections. In contrast, virologists and other scientists agree that SARS‑CoV‑2 required little to no adaptation to spread rapidly in humans and other animals . The virus appears to have succeeded in causing a pandemic upon its only detected jump into humans.
The pandemic could have been caused by any of hundreds of virus species, at any of tens of thousands of wildlife markets, in any of thousands of cities, and in any year. But it was a SARS-like coronavirus with a unique furin cleavage site that emerged in Wuhan, less than two years after scientists, sometimes working under inadequate biosafety conditions, proposed collecting and creating viruses of that same design.
While several natural spillover scenarios remain plausible, and we still don’t know enough about the full extent of virus research conducted at the Wuhan institute by Dr. Shi’s team and other researchers, a laboratory accident is the most parsimonious explanation of how the pandemic began.
Given what we now know, investigators should follow their strongest leads and subpoena all exchanges between the Wuhan scientists and their international partners, including unpublished research proposals, manuscripts, data and commercial orders. In particular, exchanges from 2018 and 2019 — the critical two years before the emergence of Covid-19 — are very likely to be illuminating (and require no cooperation from the Chinese government to acquire), yet they remain beyond the public’s view more than four years after the pandemic began.
Whether the pandemic started on a lab bench or in a market stall, it is undeniable that U.S. federal funding helped to build an unprecedented collection of SARS-like viruses at the Wuhan institute, as well as contributing to research that enhanced them . Advocates and funders of the institute’s research, including Dr. Fauci, should cooperate with the investigation to help identify and close the loopholes that allowed such dangerous work to occur. The world must not continue to bear the intolerable risks of research with the potential to cause pandemics .
A successful investigation of the pandemic’s root cause would have the power to break a decades-long scientific impasse on pathogen research safety, determining how governments will spend billions of dollars to prevent future pandemics. A credible investigation would also deter future acts of negligence and deceit by demonstrating that it is indeed possible to be held accountable for causing a viral pandemic. Last but not least, people of all nations need to see their leaders — and especially, their scientists — heading the charge to find out what caused this world-shaking event. Restoring public trust in science and government leadership requires it.
A thorough investigation by the U.S. government could unearth more evidence while spurring whistleblowers to find their courage and seek their moment of opportunity. It would also show the world that U.S. leaders and scientists are not afraid of what the truth behind the pandemic may be.
More on how the pandemic may have started

Where Did the Coronavirus Come From? What We Already Know Is Troubling.
Even if the coronavirus did not emerge from a lab, the groundwork for a potential disaster had been laid for years, and learning its lessons is essential to preventing others.
By Zeynep Tufekci

Why Does Bad Science on Covid’s Origin Get Hyped?
If the raccoon dog was a smoking gun, it fired blanks.
By David Wallace-Wells

A Plea for Making Virus Research Safer
A way forward for lab safety.
By Jesse Bloom
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .
Alina Chan ( @ayjchan ) is a molecular biologist at the Broad Institute of M.I.T. and Harvard, and a co-author of “ Viral : The Search for the Origin of Covid-19.” She was a member of the Pathogens Project , which the Bulletin of the Atomic Scientists organized to generate new thinking on responsible, high-risk pathogen research.
- Share full article
Advertisement
What is The Null Hypothesis & When Do You Reject The Null Hypothesis
Julia Simkus
Editor at Simply Psychology
BA (Hons) Psychology, Princeton University
Julia Simkus is a graduate of Princeton University with a Bachelor of Arts in Psychology. She is currently studying for a Master's Degree in Counseling for Mental Health and Wellness in September 2023. Julia's research has been published in peer reviewed journals.
Learn about our Editorial Process
Saul Mcleod, PhD
Editor-in-Chief for Simply Psychology
BSc (Hons) Psychology, MRes, PhD, University of Manchester
Saul Mcleod, PhD., is a qualified psychology teacher with over 18 years of experience in further and higher education. He has been published in peer-reviewed journals, including the Journal of Clinical Psychology.
Olivia Guy-Evans, MSc
Associate Editor for Simply Psychology
BSc (Hons) Psychology, MSc Psychology of Education
Olivia Guy-Evans is a writer and associate editor for Simply Psychology. She has previously worked in healthcare and educational sectors.
On This Page:
A null hypothesis is a statistical concept suggesting no significant difference or relationship between measured variables. It’s the default assumption unless empirical evidence proves otherwise.
The null hypothesis states no relationship exists between the two variables being studied (i.e., one variable does not affect the other).
The null hypothesis is the statement that a researcher or an investigator wants to disprove.
Testing the null hypothesis can tell you whether your results are due to the effects of manipulating the dependent variable or due to random chance.
How to Write a Null Hypothesis
Null hypotheses (H0) start as research questions that the investigator rephrases as statements indicating no effect or relationship between the independent and dependent variables.
It is a default position that your research aims to challenge or confirm.
For example, if studying the impact of exercise on weight loss, your null hypothesis might be:
There is no significant difference in weight loss between individuals who exercise daily and those who do not.
Examples of Null Hypotheses
| Research Question | Null Hypothesis |
|---|---|
| Do teenagers use cell phones more than adults? | Teenagers and adults use cell phones the same amount. |
| Do tomato plants exhibit a higher rate of growth when planted in compost rather than in soil? | Tomato plants show no difference in growth rates when planted in compost rather than soil. |
| Does daily meditation decrease the incidence of depression? | Daily meditation does not decrease the incidence of depression. |
| Does daily exercise increase test performance? | There is no relationship between daily exercise time and test performance. |
| Does the new vaccine prevent infections? | The vaccine does not affect the infection rate. |
| Does flossing your teeth affect the number of cavities? | Flossing your teeth has no effect on the number of cavities. |
When Do We Reject The Null Hypothesis?
We reject the null hypothesis when the data provide strong enough evidence to conclude that it is likely incorrect. This often occurs when the p-value (probability of observing the data given the null hypothesis is true) is below a predetermined significance level.
If the collected data does not meet the expectation of the null hypothesis, a researcher can conclude that the data lacks sufficient evidence to back up the null hypothesis, and thus the null hypothesis is rejected.
Rejecting the null hypothesis means that a relationship does exist between a set of variables and the effect is statistically significant ( p > 0.05).
If the data collected from the random sample is not statistically significance , then the null hypothesis will be accepted, and the researchers can conclude that there is no relationship between the variables.
You need to perform a statistical test on your data in order to evaluate how consistent it is with the null hypothesis. A p-value is one statistical measurement used to validate a hypothesis against observed data.
Calculating the p-value is a critical part of null-hypothesis significance testing because it quantifies how strongly the sample data contradicts the null hypothesis.
The level of statistical significance is often expressed as a p -value between 0 and 1. The smaller the p-value, the stronger the evidence that you should reject the null hypothesis.
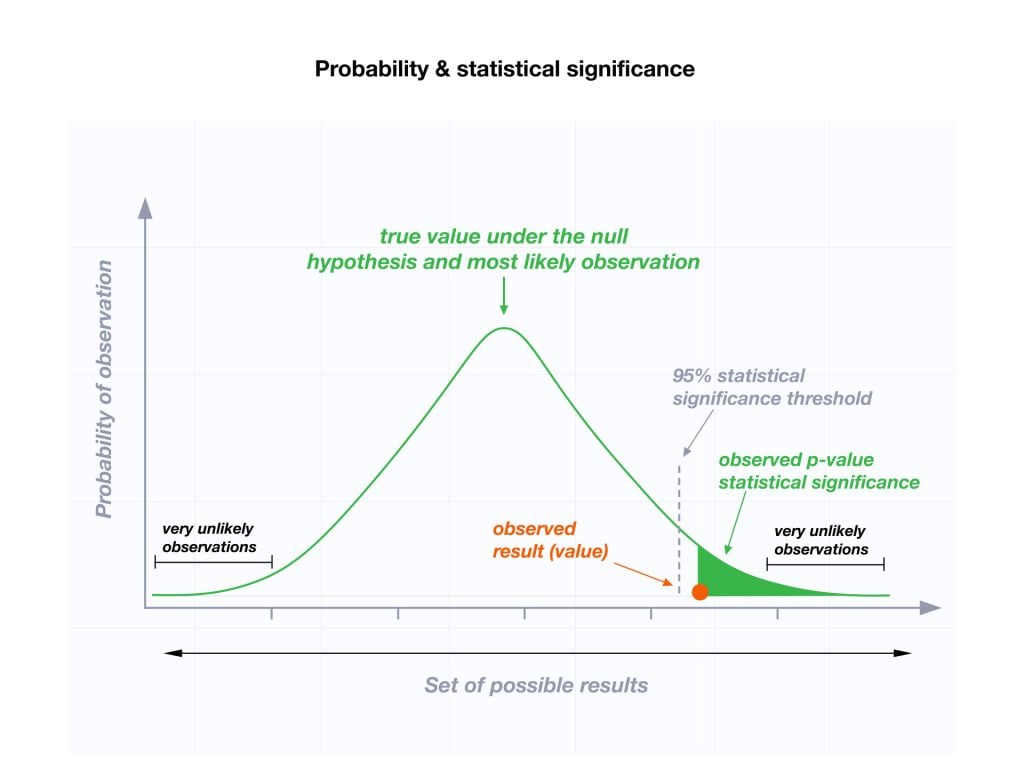
Usually, a researcher uses a confidence level of 95% or 99% (p-value of 0.05 or 0.01) as general guidelines to decide if you should reject or keep the null.
When your p-value is less than or equal to your significance level, you reject the null hypothesis.
In other words, smaller p-values are taken as stronger evidence against the null hypothesis. Conversely, when the p-value is greater than your significance level, you fail to reject the null hypothesis.
In this case, the sample data provides insufficient data to conclude that the effect exists in the population.
Because you can never know with complete certainty whether there is an effect in the population, your inferences about a population will sometimes be incorrect.
When you incorrectly reject the null hypothesis, it’s called a type I error. When you incorrectly fail to reject it, it’s called a type II error.
Why Do We Never Accept The Null Hypothesis?
The reason we do not say “accept the null” is because we are always assuming the null hypothesis is true and then conducting a study to see if there is evidence against it. And, even if we don’t find evidence against it, a null hypothesis is not accepted.
A lack of evidence only means that you haven’t proven that something exists. It does not prove that something doesn’t exist.
It is risky to conclude that the null hypothesis is true merely because we did not find evidence to reject it. It is always possible that researchers elsewhere have disproved the null hypothesis, so we cannot accept it as true, but instead, we state that we failed to reject the null.
One can either reject the null hypothesis, or fail to reject it, but can never accept it.
Why Do We Use The Null Hypothesis?
We can never prove with 100% certainty that a hypothesis is true; We can only collect evidence that supports a theory. However, testing a hypothesis can set the stage for rejecting or accepting this hypothesis within a certain confidence level.
The null hypothesis is useful because it can tell us whether the results of our study are due to random chance or the manipulation of a variable (with a certain level of confidence).
A null hypothesis is rejected if the measured data is significantly unlikely to have occurred and a null hypothesis is accepted if the observed outcome is consistent with the position held by the null hypothesis.
Rejecting the null hypothesis sets the stage for further experimentation to see if a relationship between two variables exists.
Hypothesis testing is a critical part of the scientific method as it helps decide whether the results of a research study support a particular theory about a given population. Hypothesis testing is a systematic way of backing up researchers’ predictions with statistical analysis.
It helps provide sufficient statistical evidence that either favors or rejects a certain hypothesis about the population parameter.
Purpose of a Null Hypothesis
- The primary purpose of the null hypothesis is to disprove an assumption.
- Whether rejected or accepted, the null hypothesis can help further progress a theory in many scientific cases.
- A null hypothesis can be used to ascertain how consistent the outcomes of multiple studies are.
Do you always need both a Null Hypothesis and an Alternative Hypothesis?
The null (H0) and alternative (Ha or H1) hypotheses are two competing claims that describe the effect of the independent variable on the dependent variable. They are mutually exclusive, which means that only one of the two hypotheses can be true.
While the null hypothesis states that there is no effect in the population, an alternative hypothesis states that there is statistical significance between two variables.
The goal of hypothesis testing is to make inferences about a population based on a sample. In order to undertake hypothesis testing, you must express your research hypothesis as a null and alternative hypothesis. Both hypotheses are required to cover every possible outcome of the study.
What is the difference between a null hypothesis and an alternative hypothesis?
The alternative hypothesis is the complement to the null hypothesis. The null hypothesis states that there is no effect or no relationship between variables, while the alternative hypothesis claims that there is an effect or relationship in the population.
It is the claim that you expect or hope will be true. The null hypothesis and the alternative hypothesis are always mutually exclusive, meaning that only one can be true at a time.
What are some problems with the null hypothesis?
One major problem with the null hypothesis is that researchers typically will assume that accepting the null is a failure of the experiment. However, accepting or rejecting any hypothesis is a positive result. Even if the null is not refuted, the researchers will still learn something new.
Why can a null hypothesis not be accepted?
We can either reject or fail to reject a null hypothesis, but never accept it. If your test fails to detect an effect, this is not proof that the effect doesn’t exist. It just means that your sample did not have enough evidence to conclude that it exists.
We can’t accept a null hypothesis because a lack of evidence does not prove something that does not exist. Instead, we fail to reject it.
Failing to reject the null indicates that the sample did not provide sufficient enough evidence to conclude that an effect exists.
If the p-value is greater than the significance level, then you fail to reject the null hypothesis.
Is a null hypothesis directional or non-directional?
A hypothesis test can either contain an alternative directional hypothesis or a non-directional alternative hypothesis. A directional hypothesis is one that contains the less than (“<“) or greater than (“>”) sign.
A nondirectional hypothesis contains the not equal sign (“≠”). However, a null hypothesis is neither directional nor non-directional.
A null hypothesis is a prediction that there will be no change, relationship, or difference between two variables.
The directional hypothesis or nondirectional hypothesis would then be considered alternative hypotheses to the null hypothesis.
Gill, J. (1999). The insignificance of null hypothesis significance testing. Political research quarterly , 52 (3), 647-674.
Krueger, J. (2001). Null hypothesis significance testing: On the survival of a flawed method. American Psychologist , 56 (1), 16.
Masson, M. E. (2011). A tutorial on a practical Bayesian alternative to null-hypothesis significance testing. Behavior research methods , 43 , 679-690.
Nickerson, R. S. (2000). Null hypothesis significance testing: a review of an old and continuing controversy. Psychological methods , 5 (2), 241.
Rozeboom, W. W. (1960). The fallacy of the null-hypothesis significance test. Psychological bulletin , 57 (5), 416.
Related Articles
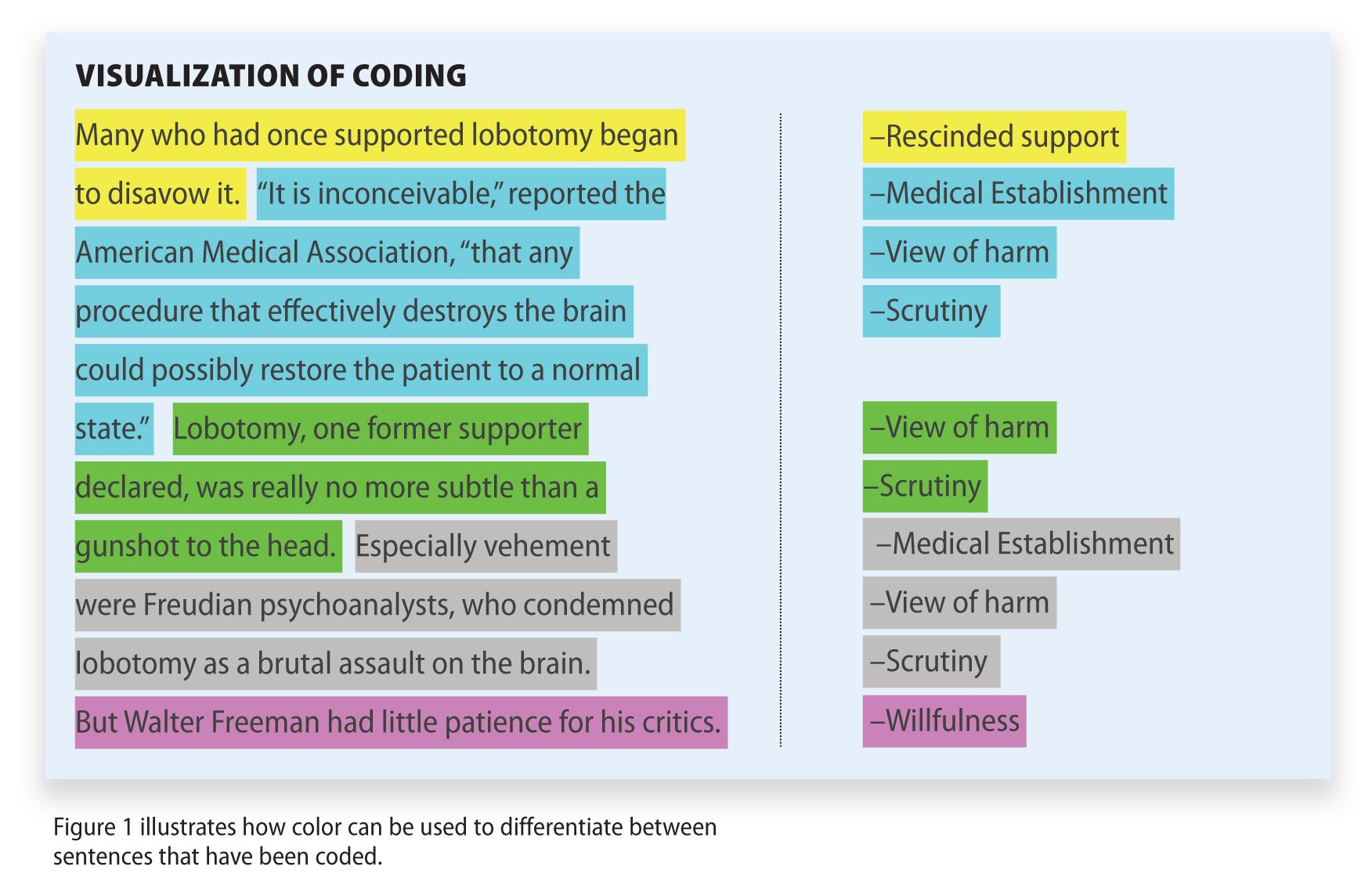
Research Methodology
Qualitative Data Coding

What Is a Focus Group?
Cross-Cultural Research Methodology In Psychology

What Is Internal Validity In Research?

Research Methodology , Statistics
What Is Face Validity In Research? Importance & How To Measure

Criterion Validity: Definition & Examples
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Korean Med Sci
- v.36(50); 2021 Dec 27

Formulating Hypotheses for Different Study Designs
Durga prasanna misra.
1 Department of Clinical Immunology and Rheumatology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India.
Armen Yuri Gasparyan
2 Departments of Rheumatology and Research and Development, Dudley Group NHS Foundation Trust (Teaching Trust of the University of Birmingham, UK), Russells Hall Hospital, Dudley, UK.
Olena Zimba
3 Department of Internal Medicine #2, Danylo Halytsky Lviv National Medical University, Lviv, Ukraine.
Marlen Yessirkepov
4 Department of Biology and Biochemistry, South Kazakhstan Medical Academy, Shymkent, Kazakhstan.
Vikas Agarwal
George d. kitas.
5 Centre for Epidemiology versus Arthritis, University of Manchester, Manchester, UK.
Generating a testable working hypothesis is the first step towards conducting original research. Such research may prove or disprove the proposed hypothesis. Case reports, case series, online surveys and other observational studies, clinical trials, and narrative reviews help to generate hypotheses. Observational and interventional studies help to test hypotheses. A good hypothesis is usually based on previous evidence-based reports. Hypotheses without evidence-based justification and a priori ideas are not received favourably by the scientific community. Original research to test a hypothesis should be carefully planned to ensure appropriate methodology and adequate statistical power. While hypotheses can challenge conventional thinking and may be controversial, they should not be destructive. A hypothesis should be tested by ethically sound experiments with meaningful ethical and clinical implications. The coronavirus disease 2019 pandemic has brought into sharp focus numerous hypotheses, some of which were proven (e.g. effectiveness of corticosteroids in those with hypoxia) while others were disproven (e.g. ineffectiveness of hydroxychloroquine and ivermectin).
Graphical Abstract

DEFINING WORKING AND STANDALONE SCIENTIFIC HYPOTHESES
Science is the systematized description of natural truths and facts. Routine observations of existing life phenomena lead to the creative thinking and generation of ideas about mechanisms of such phenomena and related human interventions. Such ideas presented in a structured format can be viewed as hypotheses. After generating a hypothesis, it is necessary to test it to prove its validity. Thus, hypothesis can be defined as a proposed mechanism of a naturally occurring event or a proposed outcome of an intervention. 1 , 2
Hypothesis testing requires choosing the most appropriate methodology and adequately powering statistically the study to be able to “prove” or “disprove” it within predetermined and widely accepted levels of certainty. This entails sample size calculation that often takes into account previously published observations and pilot studies. 2 , 3 In the era of digitization, hypothesis generation and testing may benefit from the availability of numerous platforms for data dissemination, social networking, and expert validation. Related expert evaluations may reveal strengths and limitations of proposed ideas at early stages of post-publication promotion, preventing the implementation of unsupported controversial points. 4
Thus, hypothesis generation is an important initial step in the research workflow, reflecting accumulating evidence and experts' stance. In this article, we overview the genesis and importance of scientific hypotheses and their relevance in the era of the coronavirus disease 2019 (COVID-19) pandemic.
DO WE NEED HYPOTHESES FOR ALL STUDY DESIGNS?
Broadly, research can be categorized as primary or secondary. In the context of medicine, primary research may include real-life observations of disease presentations and outcomes. Single case descriptions, which often lead to new ideas and hypotheses, serve as important starting points or justifications for case series and cohort studies. The importance of case descriptions is particularly evident in the context of the COVID-19 pandemic when unique, educational case reports have heralded a new era in clinical medicine. 5
Case series serve similar purpose to single case reports, but are based on a slightly larger quantum of information. Observational studies, including online surveys, describe the existing phenomena at a larger scale, often involving various control groups. Observational studies include variable-scale epidemiological investigations at different time points. Interventional studies detail the results of therapeutic interventions.
Secondary research is based on already published literature and does not directly involve human or animal subjects. Review articles are generated by secondary research. These could be systematic reviews which follow methods akin to primary research but with the unit of study being published papers rather than humans or animals. Systematic reviews have a rigid structure with a mandatory search strategy encompassing multiple databases, systematic screening of search results against pre-defined inclusion and exclusion criteria, critical appraisal of study quality and an optional component of collating results across studies quantitatively to derive summary estimates (meta-analysis). 6 Narrative reviews, on the other hand, have a more flexible structure. Systematic literature searches to minimise bias in selection of articles are highly recommended but not mandatory. 7 Narrative reviews are influenced by the authors' viewpoint who may preferentially analyse selected sets of articles. 8
In relation to primary research, case studies and case series are generally not driven by a working hypothesis. Rather, they serve as a basis to generate a hypothesis. Observational or interventional studies should have a hypothesis for choosing research design and sample size. The results of observational and interventional studies further lead to the generation of new hypotheses, testing of which forms the basis of future studies. Review articles, on the other hand, may not be hypothesis-driven, but form fertile ground to generate future hypotheses for evaluation. Fig. 1 summarizes which type of studies are hypothesis-driven and which lead on to hypothesis generation.

STANDARDS OF WORKING AND SCIENTIFIC HYPOTHESES
A review of the published literature did not enable the identification of clearly defined standards for working and scientific hypotheses. It is essential to distinguish influential versus not influential hypotheses, evidence-based hypotheses versus a priori statements and ideas, ethical versus unethical, or potentially harmful ideas. The following points are proposed for consideration while generating working and scientific hypotheses. 1 , 2 Table 1 summarizes these points.
| Points to be considered while evaluating the validity of hypotheses |
|---|
| Backed by evidence-based data |
| Testable by relevant study designs |
| Supported by preliminary (pilot) studies |
| Testable by ethical studies |
| Maintaining a balance between scientific temper and controversy |
Evidence-based data
A scientific hypothesis should have a sound basis on previously published literature as well as the scientist's observations. Randomly generated (a priori) hypotheses are unlikely to be proven. A thorough literature search should form the basis of a hypothesis based on published evidence. 7
Unless a scientific hypothesis can be tested, it can neither be proven nor be disproven. Therefore, a scientific hypothesis should be amenable to testing with the available technologies and the present understanding of science.
Supported by pilot studies
If a hypothesis is based purely on a novel observation by the scientist in question, it should be grounded on some preliminary studies to support it. For example, if a drug that targets a specific cell population is hypothesized to be useful in a particular disease setting, then there must be some preliminary evidence that the specific cell population plays a role in driving that disease process.
Testable by ethical studies
The hypothesis should be testable by experiments that are ethically acceptable. 9 For example, a hypothesis that parachutes reduce mortality from falls from an airplane cannot be tested using a randomized controlled trial. 10 This is because it is obvious that all those jumping from a flying plane without a parachute would likely die. Similarly, the hypothesis that smoking tobacco causes lung cancer cannot be tested by a clinical trial that makes people take up smoking (since there is considerable evidence for the health hazards associated with smoking). Instead, long-term observational studies comparing outcomes in those who smoke and those who do not, as was performed in the landmark epidemiological case control study by Doll and Hill, 11 are more ethical and practical.
Balance between scientific temper and controversy
Novel findings, including novel hypotheses, particularly those that challenge established norms, are bound to face resistance for their wider acceptance. Such resistance is inevitable until the time such findings are proven with appropriate scientific rigor. However, hypotheses that generate controversy are generally unwelcome. For example, at the time the pandemic of human immunodeficiency virus (HIV) and AIDS was taking foot, there were numerous deniers that refused to believe that HIV caused AIDS. 12 , 13 Similarly, at a time when climate change is causing catastrophic changes to weather patterns worldwide, denial that climate change is occurring and consequent attempts to block climate change are certainly unwelcome. 14 The denialism and misinformation during the COVID-19 pandemic, including unfortunate examples of vaccine hesitancy, are more recent examples of controversial hypotheses not backed by science. 15 , 16 An example of a controversial hypothesis that was a revolutionary scientific breakthrough was the hypothesis put forth by Warren and Marshall that Helicobacter pylori causes peptic ulcers. Initially, the hypothesis that a microorganism could cause gastritis and gastric ulcers faced immense resistance. When the scientists that proposed the hypothesis themselves ingested H. pylori to induce gastritis in themselves, only then could they convince the wider world about their hypothesis. Such was the impact of the hypothesis was that Barry Marshall and Robin Warren were awarded the Nobel Prize in Physiology or Medicine in 2005 for this discovery. 17 , 18
DISTINGUISHING THE MOST INFLUENTIAL HYPOTHESES
Influential hypotheses are those that have stood the test of time. An archetype of an influential hypothesis is that proposed by Edward Jenner in the eighteenth century that cowpox infection protects against smallpox. While this observation had been reported for nearly a century before this time, it had not been suitably tested and publicised until Jenner conducted his experiments on a young boy by demonstrating protection against smallpox after inoculation with cowpox. 19 These experiments were the basis for widespread smallpox immunization strategies worldwide in the 20th century which resulted in the elimination of smallpox as a human disease today. 20
Other influential hypotheses are those which have been read and cited widely. An example of this is the hygiene hypothesis proposing an inverse relationship between infections in early life and allergies or autoimmunity in adulthood. An analysis reported that this hypothesis had been cited more than 3,000 times on Scopus. 1
LESSONS LEARNED FROM HYPOTHESES AMIDST THE COVID-19 PANDEMIC
The COVID-19 pandemic devastated the world like no other in recent memory. During this period, various hypotheses emerged, understandably so considering the public health emergency situation with innumerable deaths and suffering for humanity. Within weeks of the first reports of COVID-19, aberrant immune system activation was identified as a key driver of organ dysfunction and mortality in this disease. 21 Consequently, numerous drugs that suppress the immune system or abrogate the activation of the immune system were hypothesized to have a role in COVID-19. 22 One of the earliest drugs hypothesized to have a benefit was hydroxychloroquine. Hydroxychloroquine was proposed to interfere with Toll-like receptor activation and consequently ameliorate the aberrant immune system activation leading to pathology in COVID-19. 22 The drug was also hypothesized to have a prophylactic role in preventing infection or disease severity in COVID-19. It was also touted as a wonder drug for the disease by many prominent international figures. However, later studies which were well-designed randomized controlled trials failed to demonstrate any benefit of hydroxychloroquine in COVID-19. 23 , 24 , 25 , 26 Subsequently, azithromycin 27 , 28 and ivermectin 29 were hypothesized as potential therapies for COVID-19, but were not supported by evidence from randomized controlled trials. The role of vitamin D in preventing disease severity was also proposed, but has not been proven definitively until now. 30 , 31 On the other hand, randomized controlled trials identified the evidence supporting dexamethasone 32 and interleukin-6 pathway blockade with tocilizumab as effective therapies for COVID-19 in specific situations such as at the onset of hypoxia. 33 , 34 Clues towards the apparent effectiveness of various drugs against severe acute respiratory syndrome coronavirus 2 in vitro but their ineffectiveness in vivo have recently been identified. Many of these drugs are weak, lipophilic bases and some others induce phospholipidosis which results in apparent in vitro effectiveness due to non-specific off-target effects that are not replicated inside living systems. 35 , 36
Another hypothesis proposed was the association of the routine policy of vaccination with Bacillus Calmette-Guerin (BCG) with lower deaths due to COVID-19. This hypothesis emerged in the middle of 2020 when COVID-19 was still taking foot in many parts of the world. 37 , 38 Subsequently, many countries which had lower deaths at that time point went on to have higher numbers of mortality, comparable to other areas of the world. Furthermore, the hypothesis that BCG vaccination reduced COVID-19 mortality was a classic example of ecological fallacy. Associations between population level events (ecological studies; in this case, BCG vaccination and COVID-19 mortality) cannot be directly extrapolated to the individual level. Furthermore, such associations cannot per se be attributed as causal in nature, and can only serve to generate hypotheses that need to be tested at the individual level. 39
IS TRADITIONAL PEER REVIEW EFFICIENT FOR EVALUATION OF WORKING AND SCIENTIFIC HYPOTHESES?
Traditionally, publication after peer review has been considered the gold standard before any new idea finds acceptability amongst the scientific community. Getting a work (including a working or scientific hypothesis) reviewed by experts in the field before experiments are conducted to prove or disprove it helps to refine the idea further as well as improve the experiments planned to test the hypothesis. 40 A route towards this has been the emergence of journals dedicated to publishing hypotheses such as the Central Asian Journal of Medical Hypotheses and Ethics. 41 Another means of publishing hypotheses is through registered research protocols detailing the background, hypothesis, and methodology of a particular study. If such protocols are published after peer review, then the journal commits to publishing the completed study irrespective of whether the study hypothesis is proven or disproven. 42 In the post-pandemic world, online research methods such as online surveys powered via social media channels such as Twitter and Instagram might serve as critical tools to generate as well as to preliminarily test the appropriateness of hypotheses for further evaluation. 43 , 44
Some radical hypotheses might be difficult to publish after traditional peer review. These hypotheses might only be acceptable by the scientific community after they are tested in research studies. Preprints might be a way to disseminate such controversial and ground-breaking hypotheses. 45 However, scientists might prefer to keep their hypotheses confidential for the fear of plagiarism of ideas, avoiding online posting and publishing until they have tested the hypotheses.
SUGGESTIONS ON GENERATING AND PUBLISHING HYPOTHESES
Publication of hypotheses is important, however, a balance is required between scientific temper and controversy. Journal editors and reviewers might keep in mind these specific points, summarized in Table 2 and detailed hereafter, while judging the merit of hypotheses for publication. Keeping in mind the ethical principle of primum non nocere, a hypothesis should be published only if it is testable in a manner that is ethically appropriate. 46 Such hypotheses should be grounded in reality and lend themselves to further testing to either prove or disprove them. It must be considered that subsequent experiments to prove or disprove a hypothesis have an equal chance of failing or succeeding, akin to tossing a coin. A pre-conceived belief that a hypothesis is unlikely to be proven correct should not form the basis of rejection of such a hypothesis for publication. In this context, hypotheses generated after a thorough literature search to identify knowledge gaps or based on concrete clinical observations on a considerable number of patients (as opposed to random observations on a few patients) are more likely to be acceptable for publication by peer-reviewed journals. Also, hypotheses should be considered for publication or rejection based on their implications for science at large rather than whether the subsequent experiments to test them end up with results in favour of or against the original hypothesis.
| Points to be considered before a hypothesis is acceptable for publication |
|---|
| Experiments required to test hypotheses should be ethically acceptable as per the World Medical Association declaration on ethics and related statements |
| Pilot studies support hypotheses |
| Single clinical observations and expert opinion surveys may support hypotheses |
| Testing hypotheses requires robust methodology and statistical power |
| Hypotheses that challenge established views and concepts require proper evidence-based justification |
Hypotheses form an important part of the scientific literature. The COVID-19 pandemic has reiterated the importance and relevance of hypotheses for dealing with public health emergencies and highlighted the need for evidence-based and ethical hypotheses. A good hypothesis is testable in a relevant study design, backed by preliminary evidence, and has positive ethical and clinical implications. General medical journals might consider publishing hypotheses as a specific article type to enable more rapid advancement of science.
Disclosure: The authors have no potential conflicts of interest to disclose.
Author Contributions:
- Data curation: Gasparyan AY, Misra DP, Zimba O, Yessirkepov M, Agarwal V, Kitas GD.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 30 May 2024
Longitudinal qualitative study on the psychological experiences of COVID-19 patients based on timing it right framework
- Liangyan Zhang 1 ,
- Chen Zhang 2 ,
- Kesang Li 1 &
- Yan Zhang 3
Scientific Reports volume 14 , Article number: 12409 ( 2024 ) Cite this article
175 Accesses
Metrics details
- Health care
Timing it right framework was used as a framework to explore the illness experiences of patients infected with COVID-19 and to analyze the patients' perceptions of the disease and their true inner feelings to provide a reference for the control of infectious diseases. This research adopted a phenomenological research approach to develop a longitudinal qualitative study. A purposive sampling method was used to select participants and 37 patients were recruited. Depending on the principle that participants should have maximum variation and sampling should cease when interviews content saturation is achieved, 16 COVID-19 patients in an isolation ward in Ningbo City, Zhejiang Province were finally included. Data were collected using semi-structured interviews, and the content of the interviews was analyzed by Colaizzi’s 7-step method. The themes of COVID-19 patients’ experiences at various phase were presented as follows: multiple emotions intertwined at the time of diagnosis (anxiety, stressful panic, facing the diagnosis calmly), multiple pressures during the hospitalization period (concerns about the disease, unable to adapt to the ward environment, worrying about future hardship), growth of positive illness experience during the isolation and observation period (sublimated outlook on life, affirmation of the government's anti-epidemic policy, more concerned about their own health), adjustment after returning to society (stigma, loss of previous living environment, problems caused by nucleic acid testing), and adaptation to social life (return to normal life, avoidance of illness experience, post-covid-19 syndrome). The illness experience of COVID-19 patients changed dynamically with time, but a sense of shame and uncertainty about recovery was present throughout the process. Interventions should be developed according to the needs of the patients at different times to inform subsequent optimization of care and management of infectious diseases.
Similar content being viewed by others

Long COVID: major findings, mechanisms and recommendations

Cerebral microstructural alterations in Post-COVID-condition are related to cognitive impairment, olfactory dysfunction and fatigue

Exploring the reported adverse effects of COVID-19 vaccines among vaccinated Arab populations: a multi-national survey study
Introduction.
The ongoing global epidemic of coronavirus disease 2019 (COVID-19) has had a significant impact on human society, primarily in terms of public health. As of 2 February 2023, the reported cumulative number of confirmed cases worldwide is approximately 753 million, with approximately 6,814,900 deaths 1 . Importantly, the actual number of infections worldwide may be higher than the reported data due to factors such as limited testing capacity. The Omicron and Delta strains are variants of coronaviruses with high loads, high infectivity, short incubation times, and antigenic escape 2 . Patients experience long viral nucleic acid conversion times and are more likely to develop severe and critical illnesses, with long periods of hospital isolation and medical observation 3 . Studies have shown 4 that patients with COVID-19 who stay in isolation are prone to psychological problems such as anxiety, depression, and fear. The study 5 showed that infected patients had problems such as fatigue, sleep difficulties, and anxiety after discharge from the hospital, and those with severe lung damage during hospitalization were even more likely to be in the target population for long-term rehabilitation interventions after discharge; however, the study was conducted on patients at the beginning of the 2019 outbreak, and the characteristics of the coronavirus variants can cause various psychological experiences in infected patients. There are currently few studies exploring mild COVID-19 patients' experiences during hospitalization and after reintegration into society 6 . The Timing it Right (TIR) framework was proposed by Cameron et al. 7 in the study of stroke care; it divides the process of disease development into five phases: diagnosis, stabilization, preparation, implementation and adaptation. At present, a number of scholars have used different research methods to study the dynamic needs of patients and caregivers with the TIR framework, and have achieved initial results 8 . Based on the TIR framework, it is possible to understand the changes in the experience of COVID-19 patients at different stages of illness, and formulate corresponding support plans, so that the intervention timing and intervention content can match the needs of patients at the current phase of disease 9 , 10 . Therefore, based on the five phases of disease development in the TIR framework, this research explore the illness experiences of COVID-19 patients in a longitudinal study to provide a reference for the subsequent care of patients with infectious diseases and the development of epidemic prevention and control strategies.
Design and participants
This study utilized a phenomenological research approach to develop a longitudinal qualitative study using the TIR framework. To conduct a longitudinal qualitative study, it is necessary to select specific time points for data collection, and the chosen time frame should be adequate for observing changes in the phenomenon under investigation 11 . In this study, the time frame for data collection was established through two interviews. The first interview (T1) took place during the period when the infected individuals were isolated, and the second interview (T2) occurred 6 months after their reintegration into society. The study employed a purposive sampling method to select patients who had been diagnosed with COVID-19 and were admitted to an isolation ward in Ningbo City, Zhejiang Province, between January and October 2022. The inclusion criteria were as follows: (1) confirmed COVID-19 infection; (2) age above 18 years; and (3) voluntary participation in this study and providing informed consent. The exclusion criteria were as follows: (1) those who were seriously ill and unable to communicate and (2) those with serious psychological or cognitive dysfunction. Those who automatically withdrew or were lost to follow-up during the interview were dropped from the study. A total of 37 patients were recruited for the study, and the sample size of the study was determined based on information saturation of the interviewees 12 . The specificity of the sampling was measured by demographic characteristics and the Self-Rating Depression Scale (SDS) 13 . Sampling ceased when interviews content saturation was achieved. Finally, 16 cases of representative infected patients were included in the study, including patients with no depression (9 cases, 56%), suspected mild depression (1 case, 6%), and suspected moderate depression (6 cases, 37.5%), numbered "N1" to "N16". In this study, two in-depth interviews were conducted with the infected patients, one during their isolation period and another after 6 months of reintegrating into society. Notably, during the second interview, two of the participants exhibited evasive behavior. For example, one participant was very talkative in the first interview, and he was able to talk more about his true feelings and describe them in more details based on the experience of the illness. However, in the second interview, he spoke less and only answered yes, no or fine, showing an evasive attitude. In order to fully understand the thoughts of the participants and enhance the integrity and continuity of the study, after obtaining informed consent, the interviewer supplemented the interview content by contacting their relatives, and returned the transcript of the interview content to the participants for confirmation, so as to ensure the authenticity of the content. The basic information of the study participants is shown in Table 1 .
Data collection
The participants provided informed consent and completed the demographic scale and SDS scale assessment before the interview. The interview outline was designed according to the five phases of diagnosis, stabilization, preparation, implementation and adaptation in the TIR framework. Longitudinal qualitative studies require researchers to use the insights gained from previous interviews to inform the focus of subsequent data collection 14 . The researcher preinterviewed two infected individuals prior to the formal interview and amended the interview outline. The interview outline was as follows. During Phase 1 (T1), the following questions were asked: ① How did you feel when you were diagnosed with COVID-19? ② What was your initial feeling after arriving at the isolation ward? ③ What are your needs and feelings during hospitalization? ④ How do you feel when you go to the quarantine point for medical observation? ⑤ How will the Spring Festival affect you? ⑥ If you are cured and returned to society, what expectations or concerns do you have? During Phase 2 (T2), the following questions were asked: ① What was your mood at the beginning of reintegration? Give an example of 1–2 things that were particularly impressive at that time. ② How do you feel now? How has your life changed? ③ Is there anything particularly troubling you at present? How do you solve these troubles? Do you have any hopes or suggestions? Due to the requirements of epidemic prevention and control, the interview was conducted by telephone, and the interview time was 15–60 min.
Data analysis
The interview content was analyzed by Colaizzi’s 7-step method. The steps are as follows: (1) two researchers carefully read all the original data; (2) they independently identify significant statements that were repeated by multiple participants and were important and meaningful to the research question; (3) they code repetitive and meaningful views by temporarily "suspending" their assumptions and value judgments; (4) they gather ideas after coding to form the prototype of the theme; (5) they write a detailed typical original description; (6) they identify similar ideas and condense them into themes; and (7) they return the topic structure to the participants for verification. The results of the SDS questionnaire were descriptive statistical analyzed by SPSS 25.0.
Quality control
SDS questionnaire collection: during hospitalization, a researcher issued and collected the questionnaire, explained the questions appropriately, and checked the completeness of the answers on the spot. (2) Interview data collection: all researchers in the study received professional training in qualitative research, and all interview data collection was completed by the first author (isolation ward nurse). The researcher kept in touch with the participants during the follow-up period to establish trust and friendly relationships. The researcher used the daily chat information as supplementary information. At the end of each interview, the researcher transcribed the audio-recorded information within 24 h and recorded the tone of voice, pitch change and other information of the participants. (3) Data analysis: data collection and analysis were carried out in parallel, with each of the 2 researchers listening to the audio-recordings and reading the textual information repeatedly, independently summarizing statements of significance, and summarizing the text of the statements. And the themes and subthemes extracted from the collected data were repeated to the participants by instant messaging software to further confirm whether they had the same feeling or experience and record any possible supplemental information. It was explained to the participants at the first interview that the preliminary results would be reported back to them for verification.
This study was reviewed and approved by the Ethics Committee of Ningbo No.2 Hospital (YJ-NBEY-KY-2022-102-01). All methods were performed in accordance with the relevant guidelines and regulations such as ethical standards of the institutional ethics committee and with the Declaration of Helsinki. All participants signed informed consent forms.
An interpretive understanding of the illness experiences of patients infected with COVID-19 was constructed in this study. The analysis yielded five categories and fifteen sub-categories (Table 2 ).
Theme 1: multiple emotions intertwined at the time of diagnosis
Due to different personality characteristics and understanding of the disease, infected patients showed the following emotional changes in the early stage of diagnosis.
Anxiety: since most infected patients learned about their infection suddenly, most of them had significant fidgeting, irritability, insomnia, and felt inexplicably nervous and worried when they were diagnosed or preparing for medical isolation. N5-T1: "I was so anxious when I was diagnosed that I felt like the sky was falling." N9-T1: "Since that time I have not been able to sleep well at night, I wake up after an hour of sleep." N2-T1: "I felt like it was going by so slowly and every day felt like years. Before the quarantine, I was worried that I wouldn't eat or sleep well, and that was true." Some of the infected patients felt upset when they were first diagnosed, as they received many calls for epidemiological investigations from various departments and organizations. N6-T1: "The initial phase has been very busy. I was the first to be infected, and there was a particular focus on me. At that time, my sleep was disturbed."
Stressful panic: the knowledge that there was no effective treatment, the uncertainty of the sequelae and the possibility of recurrence all put the infected patients in fear of the disease at the time of diagnosis, with three infected patients displaying more pronounced despair. N12-T1: "At that time, I was lying in bed for two days feeling like I was going to die. It was bad anyway. I was scared, scared of the after-effects, scared for my life (emotional)." N9-T1: "[Messages on my mobile phone] made me think nonsense. If the virus in my body had stayed, I would have been locked up forever. It gave me a feeling of panic."
Facing the diagnosis calmly: some of the infected patients were not so afraid of the diagnosis because people around them had already been infected. N1-T1: "The mood was a bit panicky, not particularly panicky. Because my in-laws have already been diagnosed, I already have a general idea in my mind." Some infected patients had a more comprehensive understanding of the corresponding symptoms of infection and were more receptive. N11-T1: "Not afraid of the disease. I have read the news that most of the foreign countries are infected, so I am calm." N3-T1: "It was mild… and curable, so I just didn't have much stress anyway."
Theme 2: multiple pressures during the hospitalization period
When patients were hospitalized, the disease itself, positivity for 2019-nCoV nucleic acid, and the specificity of the isolation environment made them feel deeply stressed.
Concerns about the disease: the threat to COVID-19 patients' lives and safety during hospitalization was stressful for those infected, either because of their own experiences of repositivity or because they witnessed others experiencing repositivity. N11-T1: "The biggest concern was that I didn't know how long it would take to be discharged from the hospital, how long it would take to recover … I didn't know if there were any after effects and whether there would be a relapse." N5-T1: "(After being repositive for the third time) I cried all the time during those 2 days when I was isolated again. The last 2 days were fine, (my mood) calmed down, and today I'm a little bit annoyed again, my wife and my youngest daughter they don't seem to have a good nucleic acid result. That aspect is affecting me a lot, a lot of stress (speaking faster)." N14-T1: "There is a feeling of fear in my heart. This is the first time I've had a repositive, and I've heard that there are a lot of repositive people, and I'm scared in my heart." Due to the special nature of COVID-19 patients, the vast majority of them chose to conceal their condition to avoid worrying about their families. N3-T1: "I didn't dare to make a video call to my mother. I was afraid that if my mother knew I was inside the hospital, she would have to worry about me."
Unable to adapt to the ward environment: most infected patients were transferred to isolation wards for medical observation and treatment, and the unfamiliar and confined environment often made them feel uncomfortable. N4-T1: "It feels unreal to be here, the air is treated and the rooms are airtight." Meanwhile, due to the shortage of beds, most isolation wards housed many people, to which some infected patients are not accustomed, and some infected patients were deeply stressed about secondary infections. N2-T2: "I don't like to sleep with other people in the same room. But, since I was a child, I have been timid and I am afraid to sleep alone. I am not used to sleeping in the hospital." N12-T1: "I was worried about my problems and whether sleeping in the same ward would spread the virus to each other, so I never took off my mask." Isolation also prevents infected patients from spending time with their families. During the festive season, which symbolizes reunion, they had to spend time alone. N10-T1: "The arrival of Chinese New Year had an impact on me. There are so many things I can't do because (I can't) be reunited with my family."
Worrying about future hardship: because the whole family was quarantined or because they themselves were the main laborer in the family, most infected patients reported that the long period of isolation had affected their financial income and were worried about the future. N5-T1: "There has been no income for a few months now, which means that life may be hard in the future." Due to the release of information from epidemiological surveys, infected patients are often worried about having the disease known to their acquaintances. N5-T2: "[The flow survey information] would be better to change that column where the surname is written to a number. Because we are the only ones infected in the factory, it is easy for others to guess." Infectious patients worry about social discrimination brought about by the disease and about whether they will still be able to have a suitable learning environment, job, and residence in the future. N5-T1: "I worry about whether it will affect my youngest daughter's ability to go to a better kindergarten." N10-T1: "I feel that I will not be able to find a job if people know about my disease. … I am sure I will be treated differently." "N2-T1: "We are renting a house outside, the landlord knows about it and may not let us stay in this place. What should we do?"
Theme 3: growth of positive illness experience during the isolation and observation period
Patients were under medical isolation and observation during this period. There is deeper thinking after enduring pressure from all sides, and some patients gain growth.
Sublimated outlook on life. Some infected patients were grateful for the dedication of healthcare workers. N1-T1: "Really, I feel that you are all very good. Doctors have it so hard. I didn't feel it before." Some patients thanked the teachers for caring for their children during the infection. N1-T2: "The teachers and classmates are very caring for my daughter. In particular, her class teacher was really nice. There was no one to look after her when she first came out (family members were quarantined for infection). My daughter was alone at home, and I was worried. Her teacher let my daughter go to her house. The teacher said I am not afraid." Some infected patients also said that during the isolation period, they had time to calm down and question their souls and thought more about life. N6-T1: "Actually, when I was in the isolation ward, I had more time and space to think, and then I might think more deeply about something, like the meaning of life. I would find so many things that I just naturally realized."
Affirmation of the government's anti-epidemic policy. N6-T1: "I think our government departments are very committed because our national situation is different from that of foreign countries, with a large population. If our country really doesn't care about controlling the epidemic at all, the medical resources can't keep up." N9-T1: "I fully comply with the rules and regulations of the isolation ward. The country invests a lot of resources. We eat and live medically for free."
More concerned about their own health. The experience of falling ill has made more patients pay more attention to their own health, and they actively participate in sports and pay attention to physical checkups and rest. N11-T1: "It's better to have a medical checkup to see if this virus has any other effects on your body. In the future, I will have regular medical check-ups once every six months or a year. Now, I also started to run (during the quarantine phase), I didn't run much before."
Theme 4: adjustment after returning to society
The infected often return to society in a state of fear and with a deep sense of stigma. Some infected patients have lost their former jobs and living environments, and their finances and lives have been greatly affected. At the same time, the nucleic acid test also brought troubles to their lives after returning to society.
Stigma: infected patients often have a heavy self-psychological burden when they return to society. They are afraid of being rejected and treated differently. The main manifestations are fear of stigma and concealment of medical history. N1-T2: "We definitely have to report to the community when we go back. We have to explain the situation. After explaining the situation, the people in the village will be scared to death, they will ostracize them (brother, parents), and then it will definitely have an impact on my parents and my brother's lives, so we didn't dare to go back." Some infected patients were worried that they would cause others to become infected, causing them to be quarantined as well. N16-T1: "I'm worried that if I go back to being positive in the future, I will infect others, even if it doesn't hurt, will I have to quarantine people for so many days?" With the shame of the disease, many infected patients were unable to go home to their families. N1-T2: "I would love to go back to my hometown. Because my parents are also 70 years old, and I can't take care of them when I'm out of town. But, now I can't go back to my hometown."
Loss of previous living environment. Some infected patients lost their original living and working environments after returning to society. Some COVID-19 patients moved away from their original environments of their own initiative because they were afraid that others would know that they had been infected by COVID-19. N1-T2: "We moved home. But, we are still afraid of bumping into people we know: "Some infected patients were asked not to go to work or to change their working environments for fear of mutual infection in their workplaces. N2-T2: "We were not allowed to go to work in the factory at that time because the other employees didn't agree to let us go to work." N9-T2: "She used to work in Department 5, but the original department didn't want her anymore." A new environment means a new start, which leads to greater pressure on the lives of infected patients. N1-T2: The pressure on my husband's life is too great. I also went to look for a job. After looking for a few days, I felt very sad and found that I could only do more flexible work like takeaway. Life is difficult, we've borrowed a lot of money now, and there's a lot of financial pressure and mental stress."
Problems caused by nucleic acid testing. Because of previous infections, policies require infected patients to have a separate nucleic acid test. This often meant that they had to spend time and effort looking for a separate site where they could do a separate nucleic acid test. N1-T2: "My child can't do a separate nucleic acid test at school anyway, so we have to find a nucleic acid test site by ourselves." When doing the nucleic acid test alone, they were split into two teams, separate from the people doing the mixed nucleic acid test, and the people in their team were faced with more inquiries about infection, which put more pressure on them." N1-T2: "When we went to do the nucleic acid test, the security guard at the door asked once, then the person who checked the identity after the questioning asked again, and the sampler asked again. I had nightmares every day." In addition, they were concerned that doing the nucleic acid test alone would increase the risk of reinfection. N5-T2: "When we do the nucleic acid test alone, we are with people who are at high risk. The book they have registered in we touch it again, register it again and go with them. If I get infected again, I reckon I'm going to go mad." Because of the fear of repositivity, infected patients are extremely concerned about the results of their own and their family's nucleic acid tests." N3-T2: "To be honest, some people, like my wife, have repeated repositive and go to quarantine sites over and over again. Very upset and depressed. I'm worried about my own and my wife's nucleic acid test results."
Theme 5: adaptation to social life
Six months after returning to society, most of the infected patients returned to normal life with the support and tolerance of society, but some of them still avoided infection and concealed their status as recovered persons. Some of the infected patients developed post-COVID-19 syndrome.
Return to normal life. Some infected patients integrated into society with the tolerance of colleagues and friends around them. N2-T2: "Still working as normal. My friends and I still play well and sit together for meals." N8-T2: "I was a bit afraid that my colleagues would laugh at me in various ways before I came to work. But, none of them did." Nucleic acid testing is also gradually becoming less frequent. N7-T2: "In the beginning, it was a single test, now it's all mixed." Some infected patients said that they no longer avoided the fact that they were infected under self-regulation and gradually returned to normal life. T12-N2: "When I first came out of quarantine, whenever people talked about this stuff, I wanted to avoid it and didn't want to hear about it. Now, when people talk about doing nucleic acids, I seem to slowly be able to accept it."
Avoidance of illness experience. Some infected patients still avoided infection and concealed their identities as a recovered person. N16-T2 Husband added: "Whoever mentions this, she is anxious about it. Some old folks called me and asked about this, and she was also a little anxious in her heart. There is nervousness in her heart, and she doesn't want to talk about it anymore." During the interview with N5-T2, the infected patient herself said, "I don't feel anything, it doesn't affect me at the moment. Everything is fine. Don't want to think about it." However, interviewing his lover, he said, "He used to look like a child, he used to laugh and joke around, but now he looks sad every day. He doesn't talk much in his free time." This experience has changed his personality.
Post-COVID-19 syndrome. Some infected patients still have residual weakness, chest tightness, loss of smell, sleep disorders, etc. N14-T2: "The body is a bit different anyway. I'm more tired than I used to be at work, and I'm not as fit as I used to be. Sleep has been bad, easy to wake up. I have no sense of smell." N15-T2: "I feel a bit breathless sometimes when I walk a few steps. I feel tired."
This study conducted a longitudinal exploration of COVID-19 patients' experience based on the TIR framework. In general, the TIR framework has played a good guiding role in the exploration of COVID-19 patients' illness experience. During the diagnosis phase, COVID-19 patients were usually very concerned about their own health problems, and due to great pressure caused by isolation, they were prone to psychological problems. The stabilization and preparation phase of COVID-19 patients were in the long isolation treatment. Patients gradually adapted to isolation treatment and started to plan their life after discharge. They were worried about discrimination and worried that they would never go back to the original life. In addition, because COVID-19 patients were kept in isolation for a long time, some patients began to reflect on the experience of the disease and the past life status, and thus gained growth. The stigma of COVID-19 patients was felt throughout the course of the illness, but it was particularly evident during the implementation and adaptation phase. Due to the stigma and discrimination, some patients actually made great changes to their work and life during this two phase. At this time, social support was particularly important for patients to reintegrate into society. The following discussion provides detailed analysis of the above phenomena.
The results of this study showed that all infected patients diagnosed for the first time had psychological problems such as anxiety, fear, and sleep disorders, and seven patients (43.75%) were suspected of having mild to moderate depression according to the SDS scores, which is similar to the results of the study by Deng et al. 15 . This may be due to the highly contagious nature of COVID-19 and the lack of specific treatment, resulting in infected patients being prone to excessive stress, panic, and even psychological stress disorder at the early stage of diagnosis 16 . At the same time, 14 cases (87.5%) of the infected patients expressed concern about the possibility of "repositivity" after recovery and the existence of sequelae. A related study found that noninfectious viral RNA persisted in most of the "repositive" cases, which may be due to slow disease regression 17 . A positive test does not always mean that the patient is infectious, as it may detect fragments of viral nucleic acid 18 . However, most patients know little about this and develop more anxiety and fear. In contrast, those patients who have knowledge of the new coronavirus tend to have less fear and worry. Cheng Hualing et al. 19 meta-integrated the psychological experience of COVID-19 patients in China and found that more information provided by medical personnel to infected patients about the treatment and prognosis of the disease could eliminate the anxiety caused by the patients' lack of knowledge. Therefore, health promotion should be strengthened, and patients should be encouraged to acquire knowledge of the disease in various aspects, including transmission channels, protective measures, symptom classification, prognosis, etc. Patients’ questions should be patiently answered based on their own conditions, and they should be encouraged to obtain correct information through official authoritative channels to avoid "information panic" 20 .
Four infected patients (25%) in this study indicated that the relatively confined environment and instruments in the isolation area caused feelings of loneliness and helplessness. The isolation treatment measures separated the patients from the outside world, as they left their familiar working and living environments to enter a state of isolation, confinement and monotony. The patients' original lifestyles were completely disrupted, and certain financial losses were incurred. The unfamiliar environment and medical equipment increased the patients' fear and loneliness while also hindering the discharge of their negative emotions. This is consistent with the findings of Wang et al. 20 and Shaban et al. 21 . A retrospective study 22 found that isolation may cause unexpected mental trauma for patients and may even lead to self-injurious behaviors such as suicide. These effects persisted 3 years after desegregation. Psychological disorders can lead to low immunity and reduced motivation for treatment, thus negatively affecting disease recovery 23 . Currently, the treatment and care of patients in isolation wards are mainly focused on the disease itself, with relatively little attention given to the physical and psychological effects of isolation. Improving the treatment environment in isolation areas, providing as much stimulation as possible during the normal routine of work and rest, establishing a good lifestyle, and diversifying hospital activities are of great significance in relieving emotional tension, breaking psychological barriers, and promoting disease recovery 24 . Studies have shown that having sufficient sunlight is particularly effective for psychological relief 25 . Isolation areas should be set up to face south, and lighting measures should be strengthened. Public corridors can be set up in the isolation area so that infected patients can stagger their activities appropriately. Healthcare workers who are fully "armed" can paste their names on their protective clothing to improve communication between doctors and patients and reduce patients' sense of isolation. There are also studies 26 suggesting the use of the Rosenthal effect, that is, using praise, trust and expectation, and other psychological hints to help patients regain confidence and obtain positive motivation to change their own behaviors. By communicating with patients to understand their psychological needs, sources of negative emotions and specific factors affecting their emotions, healthcare professionals, in collaboration with teams from various disciplines, can encourage infected patients to cope positively and provide social support and psychological guidance to improve their quality of life 27 . The patients in this study were often in a state of confusion and worry before discharge and were also often unable to adjust to a good rhythm of life within a short period after discharge. Healthcare professionals can help patients develop a postdischarge transition plan during inpatient isolation so that they can quickly return to their original lives. At the same time, a scale of social reintegration behavior of infected patients with infectious diseases that is suitable for our country should be developed to prospectively investigate the current status of social reintegration of infected patients and to understand the changes in social reintegration behaviors in different periods to take corresponding measures to help such people adapt to their situations as soon as possible.
As a contagious disease, COVID-19 can lead to fear among the population as well as stigma and discrimination against specific groups of people 28 , and patients develop a sense of shame about their illness as a result. The results of this study show that patients often want to keep their experience of the disease confidential. The vast majority of infected patients in this study chose to conceal their illness from their family members. Due to the existence of a sense of shame, patients not only kept their disease experience secret but also often consciously reduced their mobility after discharge from the hospital to avoid infecting others. Patients may actively distance themselves from their friends and relatives, resulting in the loss of an important source of social support and a sense of isolation 29 . There were also patients who did not actively conceal their condition, but friends and colleagues of the infected patients intentionally chose to distance themselves from the infected patients out of fear and rejection after learning of their condition. Six patients (37.5%) in this study were thus forced to leave their original places of residence or work, causing them to develop more negative emotions. On the other hand, the infected patients who indicated that their colleagues and friends treated them no differently than before reported that they resumed normal life more quickly after returning to society. Yuan et al. 19 showed that the social support system of infected patients is an important factor in their posttraumatic growth. Social support based on kinship is the main way for most Chinese people to obtain social support. If this basic relationship is damaged, it prevents infected patients from obtaining the understanding and support of others, which can have a great impact on their physical and mental health 30 . The establishment of a good social support system will enhance psychological health; in contrast, the accumulation of negative emotions will lead to a variety of psychological problems 31 . Healthcare workers in the diagnosis and treatment of COVID-19 patients not only need to give the necessary treatment measures but also need to comprehensively assess the degree of understanding of the disease and social support system of infected patients. Healthcare workers should encourage infected patients to inform their families of their illnesses through daily communication, collaborate with their families to provide relevant psychological care, and improve the level of posttraumatic growth of patients 32 . In addition, the limitations of the public's knowledge of the disease will increase the individual's self-psychological burden, which will deepen the self-perception and experience of public stigma, resulting in the internalization of stigma 33 . Therefore, it is necessary to strengthen the information dissemination of infectious diseases, set up relevant policies for social groups such as communities and companies to avoid the public's rough treatment of infected patients returning to society, to protect the normal work and lives of infected patients and to reduce economic losses. This study shows that the policy benefits given by the government make infected patients believe in the national epidemic prevention policy and thus have confidence in the diagnosis and treatment of the disease. Therefore, state policy supports the reintegration of COVID-19 patients into society through macrocontrol.
Six months after returning to the community, some of the patients in this study still had sequelae of COVID-19, such as malaise, insomnia, chest tightness, and loss of smell. A recent study published in The Lancet 34 also confirmed this phenomenon. Similar studies have shown that the acute phase of COVID-19 and subsequent health damage involves multiple systems, such as the respiratory, neurological, and cardiovascular systems 18 . Given that infected patients at this stage need professional guidance to avoid delaying their illness, we call for greater collaboration among scholars from different countries to share experiences in the treatment of the disease to improve the physical and mental health of the population in the face of the postinfection syndrome caused by the global pandemic of COVID-19 patients.
This study found that there is a lack of clarity in the division of labor between departments and duplication of investigations by various departments in the process of epidemiological investigation.. It is recommended that the relevant departments should strengthen the integration and sharing of information by using big data and increase training in epidemiological investigation to improve efficiency 26 . Knowing the benefits of epidemiological investigation and personal information protection can reduce the uneasiness of infected patients, it is recommended that the media increase the scientific knowledge of epidemiological investigations and, at the same time, hide patients’ last names in the publication of epidemiological investigation information to protect the privacy of infected patients, and prohibit malicious human searches and other behaviors.
Limitations
While the study has its merits, it also has its limitations. First, this study interviewed COVID-19 patients only in Ningbo and did not include patients from multiple regions and centers. Second, this study was conducted during the control phase of the epidemic in China, and except for filling out the SDS scale, which was face-to-face, both interviews were conducted over the phone, and preventing the use of visual aids.
Conclusions
The objective of this study was to explore the perceptions and comprehension of patients infected with COVID-19 during the Chinese new coronavirus epidemic. COVID-19 patients encounter numerous psychological challenges while simultaneously experiencing physical discomfort, isolation, a sense of shame, and uncertainty regarding recovery. While some patients eventually adapt to their circumstances, not all are able to do so. Therefore, it is crucial for healthcare providers and families to provide support in order to facilitate patient adjustment to normal life. Interventions should be tailored according to the specific needs of patients at different stages, informing subsequent optimization of care and management strategies for infectious diseases.
Data availability
The datasets generated and analysed during the current study are not publicly available due privacy protection but are available from the corresponding author on reasonable request.
World health organization (WHO). Coronavirus (COVID-19) dashboard [DB/OL] . https://covid19.who.int/ . 2023-02-03.
Chen, W. X. et al. Comparison of three experimental methods for detecting antibody levels after immunization with COVID-19 vaccine [J]. Chin. J. Microbiol. Immunol. 41 (6), 423–426 (2021).
MathSciNet Google Scholar
Zhou, X. Y., Wang, H., & Hang, H. R., et al. Epidemiological and clinical characteristics of SARS-CoV-2 Delta variant infected patients with COVID-19 in Gansu province [J/OL]. Nurs. J. Chin PLA 1–14 (2022).
Chen, H. L., & He, Q. A meta synthesis of qualitative research on the psychological experience of patients with COVID-19 infection in China. J. Southw. Jiaotong Univ. 2022 (06), 73–82 (2023). http://kns.cnki.net/kcms/detail/51.1586.c.20221123.1638.018.html .
Hanson, S. W. et al. Global burden of disease long COVID collaborators; Estimated global proportions of individuals with persistent fatigue, cognitive, and respiratory symptom clusters following symptomatic COVID-19 in 2020 and 2021 [J]. JAMA. 328 (16), 1604–1615. https://doi.org/10.1001/jama.2022.18931 (2022).
Article Google Scholar
Guo, M., Kong, M., Shi, W., Wang, M. & Yang, H. Listening to COVID-19 survivors: What they need after early discharge from hospital—A qualitative study [J]. Int. J. Qual. Stud. Health Well-being. 17 (1), 2030001. https://doi.org/10.1080/17482631.2022.2030001 (2022).
Article PubMed PubMed Central Google Scholar
Cameron, J. I. & Gigrac, M. A. “Timing It Right”: A conceptual framework for addressing the support needs of family caregivers to stroke survivors from the hospital to the home [J]. Patient Educ. Couns. 70 (3), 305–314. https://doi.org/10.1016/j.pec.2007.10.020 (2008).
Article PubMed Google Scholar
Liang, L. L. et al. Research progress on application of timing theory in disease nursing [J]. Chin. Nurs. Res. 30 (05), 524–525 (2016).
Google Scholar
Chu, H. L. et al. Sample size was determined for qualitative interviews based on the information efficacy model [J]. Chin. Gen. Pract. 24 (10), 1274–1276. https://doi.org/10.12114/j.issn.1007-9572.2020.00.415 (2021).
Ding, X. & Yao, J. Peer education intervention on adolescents’ anxiety, depression, and sleep disorder during the COVID-19 pandemic [J]. Psychiatr. Danub. 32 (3–4), 527–535. https://doi.org/10.24869/psyd.2020.527 (2020).
Balmer, D. F. & Richards, B. F. Conducting qualitative research through time: how might theory be useful in longitudinal qualitative research? [J]. Adv. Health Sci. Educ. Theory Pract. 27 (1), 277–288. https://doi.org/10.1007/s10459-021-10068-5 (2022).
Audulv, Å. et al. Qualitative longitudinal research in health research: A method study [J]. BMC Med. Res. Methodol. 22 (1), 255. https://doi.org/10.1186/s12874-022-01732-4 (2022).
Sun, J. et al. Psychological anxiety of patients with novel pneumonia during isolation period [J]. Hosp. Admin. J. Chin. People’s Liberation Army 28 (8), 758–760 (2021).
Zhang, W. et al. To summarize the experience of psychological intervention and rehabilitation of patients with COVID-19 in mobile cabin hospital [J]. Chin. J. Nurs. 55 (S1), 603–605. https://doi.org/10.3761/j.issn.0254-1769.2020.S1.231 (2020).
Article CAS Google Scholar
Deng, C. Y. et al. To analyze the depression level and its influencing factors in patients with COVID-19 [J]. Tianjin J. Nurs. 30 (04), 400–403. https://doi.org/10.3969/j.issn.1006-9143.2022.04.005 (2022).
Yao, L. Y. et al. To evaluate the mental health status and nursing of 45 patients injured in earthquake [J]. Chin. J. Nurs. 43 (12), 3. https://doi.org/10.3761/j.issn.0254-1769.2008.12.003 (2008).
Gidari, A. et al. Is recurrence possible in coronavirus disease 2019 (COVID-19)? Case series and systematic review of literature [J]. Eur. J. Clin. Microbiol. Infect. Dis. 40 (1), 1–12. https://doi.org/10.1007/s10096-020-04057-6 (2021).
Article CAS PubMed Google Scholar
Chen, H. et al. To explore the effects of life intervention on anxiety, depression and quality of life in patients with COVID-19 [J]. J. Nurs. Sci. 35 (09), 27–29 (2020).
Yuan, Z. F. et al. Current status and influencing factors of post-traumatic growth in patients with COVID-19 [J]. Chin. J. Nurs. 55 (S1), 587–589. https://doi.org/10.3761/j.issn.0254-1769.2020.S1.225 (2020).
Wang, J. Y. et al. A qualitative study on disease experience of 15 patients with COVID-19 [J]. J. Nurs. 27 (14), 63–67. https://doi.org/10.16460/j.issn1008-9969.2020.14.063 (2020).
Shaban, R. Z. et al. SARS-CoV-2 infection and COVID-19: The lived experience and perceptions of patients in isolation and care in an Australian healthcare setting [J]. Am. J. Infect. Control. 48 (12), 1445–1450. https://doi.org/10.1016/j.ajic.2020.08.032 (2020).
Brooks, S. K. et al. The psychological impact of quarantine and how to reduce it:rapid review of the evidence [J]. Lancet 395 (10227), 912–920 (2020).
Article CAS PubMed PubMed Central Google Scholar
Li, S. & Zhang, X. L. To analyze the effect of psychological nursing on elderly patients with chronic obstructive pulmonary disease [J]. China Rural Health 11 (24), 55 (2019).
Chen, J. G. et al. Study on the influencing factors of psychological status of confirmed COVID-19 patients and quarantine visitors [J]. J. Nurs. Admin. 20 (04), 247–251 (2020).
Korkut, S. Research of the coronavirus anxiety, post-traumatic stress, generalized anxiety disorder, quality of life, and stress coping styles in COVID-19 survivor [J]. Psychol. Rep. 125 (6), 3069–3083. https://doi.org/10.1177/00332941221129131 (2022).
Zhang, S. S. & Xie, W. Y. To explore the effect of psychological nursing based on Rosenthal effect on negative emotions of patients with suspected COVID-19 [J]. J. Nurs. Sci. 35 (09), 24–26 (2020).
Yuan, K. et al. A systematic review and meta-analysis on the prevalence of stigma in infectious diseases, including COVID-19: a call to action [J]. Mol. Psychiatry. 27 (1), 19–33. https://doi.org/10.1038/s41380-021-01295-8 (2022).
Huang, L. X. et al. Health outcomes in people 2 years after surviving hospitalization with COVID-19: A longitudinal cohort study [J]. Lancet Respir. Med. 10 (9), 863–876. https://doi.org/10.1016/S2213-2600(22)00126-6 (2022).
Wang, T. et al. Current status and influencing factors of stigma in patients after COVID-19 recovery [J]. Shanghai Nurs. 20 (10), 28–31 (2020).
Zhen, X. Y. Quality of life and related psychosocial factors in people living with HIV/AIDS [D] (Shanxi Medical University, 2011).
Zhou, S. J. et al. Common psychological conflicts and coping strategies of COVID-19 patients [J]. Chin. Mental Health J. 34 (03), 248–250. https://doi.org/10.3969/j.issn1000-6729.2020.3.021 (2020).
Nan, F. F. et al. Remote psychological crisis intervention service under the COVID-19 epidemic in Zhejiang province [J]. China J. Health Psychol. 29 (03), 367–370. https://doi.org/10.13342/j.cnki.cjhp.2021.03.010 (2021).
Li, R. J. et al. Qualitative research on psychological experience of pregnant women with COVID-19 [J]. Milit. Nurs. 39 (09), 49–52 (2022).
Huang, L. et al. 1-year outcomes in hospital survivors with COVID-19: A longitudinal cohort study [J]. Lancet. 398 (10302), 747–758. https://doi.org/10.1016/S0140-6736(21)01755-4 (2021).
Download references
This research was supported by Medical Scientific Research Foundation of Zhejiang Province under Grant No. 2023KY1091; Zhejiang Provincial Natural Science Foundation of China under Grant No. LY22H160006.
Author information
Authors and affiliations.
Hemtology Department, Ningbo No. 2 Hospital, Ningbo, Zhejiang, China
Liangyan Zhang & Kesang Li
Intensive Care Unit, Ningbo No. 2 Hospital, Ningbo, Zhejiang, China
Infection Department, Ningbo No. 2 Hospital, Ningbo, Zhejiang, China
You can also search for this author in PubMed Google Scholar
Contributions
Liangyan Zhang organized interviews and collected the data. Liangyan Zhang and Chen Zhang analyzed the data and wrote the main manuscript text. All authors reviewed the manuscript.
Corresponding author
Correspondence to Chen Zhang .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Zhang, L., Zhang, C., Li, K. et al. Longitudinal qualitative study on the psychological experiences of COVID-19 patients based on timing it right framework. Sci Rep 14 , 12409 (2024). https://doi.org/10.1038/s41598-024-63215-4
Download citation
Received : 17 December 2023
Accepted : 27 May 2024
Published : 30 May 2024
DOI : https://doi.org/10.1038/s41598-024-63215-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Longitudinal qualitative study
- Timing it right framework
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

IMAGES
VIDEO
COMMENTS
COVID-19 is a new, complex, multisystem disease caused by the novel coronavirus SARS-CoV-2. In slightly over 2 years, it infected nearly 500 million and killed 6 million human beings worldwide, causing an unprecedented coronavirus pandemic. Several vaccines, developed in record time, were approved for public use (Forni and Mantovani 2021 ...
The ongoing COVID-19 pandemic, caused by the novel severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2), has affected 212 countries worldwide at various degrees as of 8 May 2020. 1 In this paper we discuss a hypothesis that prior viral infections—either by SARS-CoV-2 or different strains of coronaviruses, or potentially even other respiratory viruses—may predispose to more ...
Yet well into the fourth year of the Covid-19 pandemic, intense political and scientific debates about its origins continue. The two major hypotheses are a natural zoonotic spillover, most likely ...
Core Tip: Understanding what contributes to the development of severe coronavirus disease 2019 (COVID-19) can be of considerable clinical and therapeutic advantage.Severe acute respiratory syndrome coronavirus 2 infection may present with different COVID-19 manifestations, where various host genetic factors influence the viral susceptibility, immune response, disease progression, and outcomes.
As reported by the CDC, from February 12 to April 2, 2020, of 149,760 cases of confirmed COVID-19 in the United States, 2572 (1.7%) were children aged <18 years, similar to published rates in ...
IHME COVID-19 Forecasting Team. Nature Med. 27, 94-105 (2021). New unknowns As the virus continues to surge across much of the world, new variants have emerged, and are prompting new ques -
In theory, COVID-19 could have come from a lab in a few ways. Researchers might have collected SARS-CoV-2 from an animal and maintained it in their lab to study, or they might have created it by ...
And this hypothesis that SARS-CoV-2 was in some frozen food that people then ate and that's how it started, this comes from a few different studies. ... I mean, in terms of the COVID-19 outbreak ...
COVID-19 originates from a novel coronavirus (SARS-CoV-2) and the scientific community is faced with the daunting task of creating a novel model for this pandemic or, in other words, creating novel science. This paper is the first part of a series of two papers that explore the intricate relationship between the different challenges that have ...
The Origins of Covid-19 — Why It Matters (and Why It Doesn't) Lawrence O. Gostin, J.D., and Gigi K. Gronvall, Ph.D. The Orig ns of C v d-19. When health emergencies arise, scientists seek to ...
7) Patients will become consumers. The Covid-19 pandemic literally impacts each and every one of us. The boundary between "healthy" and "sick" becomes blurred. People who have otherwise ...
When hundreds of millions of people are vaccinated, millions of them will be afflicted anyway, in the course of life, by conditions like strokes, anaphylaxis, and Bell's palsy. "We have to have faith that people collecting the data will let us know if we are seeing those things above the baseline rate.". 3.
HYPOTHESIS: The COVID-19 pandemic is a feedback signal from the biosphere that denotes the ecological overshoot of the human species (currently estimated at about 1.7 planets; GFN 2020). That means that efforts to control this pandemic, even if successful, will not solve the wider problem of overshoot and the prospect of further, more ...
The number of deaths due to COVID-19 is probably underestimated, ... The scientific method makes it possible to observe a problem, formulate a hypothesis about its causes, evaluate it ...
The COVID-19 model digraph can be expressed as a graph G = (N, L), where G is the model graph, N = (S, I, U, W, R) is the set of nodes (states), L = {v 1, v 2, v 3, v 4, v 5, v 6, v 7} is the set of links (reactions). Open in a separate window. Fig. 1. The model interaction individuals for the COVID-19 epidemic outbreak with reaction rates.
Background: Corona virus (COVID-19) is an outbreak of respiratory disease caused by a novel corona virus and declared to be a global health emergency and a pandemic by the World Health Organization (WHO) on March 11, 2020. Prevention strategies to control the transmission of the COVID-19 pandemic, such as closing of schools, refraining from gathering, and social distancing, have direct impacts ...
The COVID-19 pandemic has the potential to affect the human microbiome in infected and uninfected individuals, having a substantial impact on human health over the long term. This pandemic intersects with a decades-long decline in microbial diversity and ancestral microbes due to hygiene, antibiotics, and urban living (the hygiene hypothesis).
The ongoing COVID-19 pandemic, caused by the novel severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2), has affected 212 countries worldwide at various degrees as of 8 May 2020.1 In this paper we discuss a hypothesis that prior viral infections—either by SARS-CoV-2 or different strains of coronaviruses, or potentially even other respiratory viruses—may predispose to more ...
In late November 2020, there was a flurry of media coverage of two companies' claims of 95% efficacy rates of newly developed COVID-19 vaccines, but information about the confidence interval was not reported. This paper presents a way of teaching the concept of hypothesis testing and the construction of confidence intervals using numbers announced by the drug makers Pfizer and Moderna ...
The origins of SARS-CoV-2, the virus that causes COVID-19 and has infected more than 171 million people, killing close to 3.7 million worldwide as of June 4, remain unclear. Many scientists ...
Dr. Chan is a molecular biologist at the Broad Institute of M.I.T. and Harvard, and a co-author of "Viral: The Search for the Origin of Covid-19." This article has been updated to reflect news ...
COVID19 pandemic. After last year's assembly, the WHO agreed to sponsor the first phase of ... leak hypothesis, or to prove the alternative — that the virus has a natural origin. Many
A null hypothesis is rejected if the measured data is significantly unlikely to have occurred and a null hypothesis is accepted if the observed outcome is consistent with the position held by the null hypothesis. Rejecting the null hypothesis sets the stage for further experimentation to see if a relationship between two variables exists.
COVID-19 has the potential to enter and invade the brain cells and produce different neurological symptoms. The brain has been reported to express angiotensin converting enzyme 2 (ACE2) receptors that have been detected over glial cells and neurons, which makes them a potential target of COVID-19, and could be a probable cause to develop ...
June 3, 2024 12:17 pm. . Dr. Anthony Fauci, the former director of the National Institute of Allergy and Infectious Diseases, testified before Congress on Monday that COVID-19 may have come from a ...
In this paper we discuss a hypothesis that prior viral infections—either by SARS-CoV-2 or different strains of coronaviruses, or poten- tially even other respiratory viruses—may predispose to more severe forms of COVID- 19, following a secondary infection with SARS- CoV-2. Most COVID-19 infections are asymp- tomatic or manifest with mild to ...
Another hypothesis proposed was the association of the routine policy of vaccination with Bacillus Calmette-Guerin (BCG) with lower deaths due to COVID-19. This hypothesis emerged in the middle of 2020 when COVID-19 was still taking foot in many parts of the world.37,38 Subsequently, many countries which had lower deaths at that time point went ...
Before the outbreak of the COVID-19 pandemic, human lives and activities relatively progressed with certain levels of orderliness and predictability (Onah et al., 2021; Patel & Jernigan, 2020), which created an atmosphere of relative "normalcy" in many sectors of Society.Thus, people were enjoying the freedom of gathering; socio-political-economic and religious activities were thriving as ...
The global pandemic of Coronavirus disease 2019 (COVID-19) has triggered an "infodemic," which was identified by the World Health Organization (2020) as "too much information including false or misleading information in digital and physical environments during a disease outbreak." In particular, a relatively small but vocal number of conspiracy theories about COVID-19 have been ...
Based on the TIR framework, it is possible to understand the changes in the experience of COVID-19 patients at different stages of illness, and formulate corresponding support plans, so that the ...