An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.


StatPearls [Internet].
Hypothesis testing, p values, confidence intervals, and significance.
Jacob Shreffler ; Martin R. Huecker .
Affiliations
Last Update: March 13, 2023 .
- Definition/Introduction
Medical providers often rely on evidence-based medicine to guide decision-making in practice. Often a research hypothesis is tested with results provided, typically with p values, confidence intervals, or both. Additionally, statistical or research significance is estimated or determined by the investigators. Unfortunately, healthcare providers may have different comfort levels in interpreting these findings, which may affect the adequate application of the data.
- Issues of Concern
Without a foundational understanding of hypothesis testing, p values, confidence intervals, and the difference between statistical and clinical significance, it may affect healthcare providers' ability to make clinical decisions without relying purely on the research investigators deemed level of significance. Therefore, an overview of these concepts is provided to allow medical professionals to use their expertise to determine if results are reported sufficiently and if the study outcomes are clinically appropriate to be applied in healthcare practice.
Hypothesis Testing
Investigators conducting studies need research questions and hypotheses to guide analyses. Starting with broad research questions (RQs), investigators then identify a gap in current clinical practice or research. Any research problem or statement is grounded in a better understanding of relationships between two or more variables. For this article, we will use the following research question example:
Research Question: Is Drug 23 an effective treatment for Disease A?
Research questions do not directly imply specific guesses or predictions; we must formulate research hypotheses. A hypothesis is a predetermined declaration regarding the research question in which the investigator(s) makes a precise, educated guess about a study outcome. This is sometimes called the alternative hypothesis and ultimately allows the researcher to take a stance based on experience or insight from medical literature. An example of a hypothesis is below.
Research Hypothesis: Drug 23 will significantly reduce symptoms associated with Disease A compared to Drug 22.
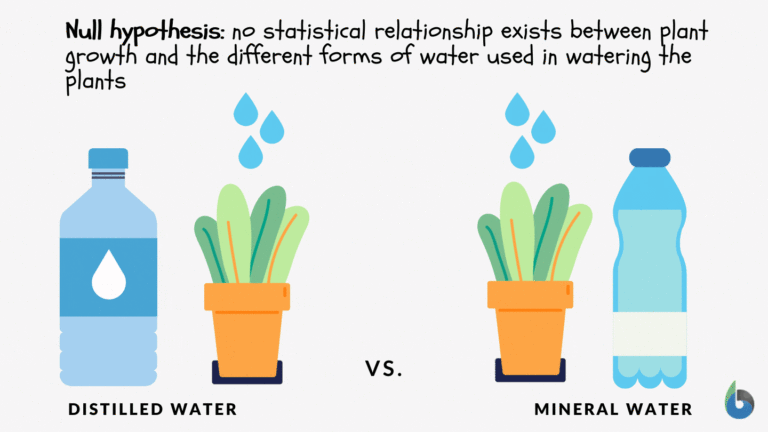
The null hypothesis states that there is no statistical difference between groups based on the stated research hypothesis.
Researchers should be aware of journal recommendations when considering how to report p values, and manuscripts should remain internally consistent.
Regarding p values, as the number of individuals enrolled in a study (the sample size) increases, the likelihood of finding a statistically significant effect increases. With very large sample sizes, the p-value can be very low significant differences in the reduction of symptoms for Disease A between Drug 23 and Drug 22. The null hypothesis is deemed true until a study presents significant data to support rejecting the null hypothesis. Based on the results, the investigators will either reject the null hypothesis (if they found significant differences or associations) or fail to reject the null hypothesis (they could not provide proof that there were significant differences or associations).
To test a hypothesis, researchers obtain data on a representative sample to determine whether to reject or fail to reject a null hypothesis. In most research studies, it is not feasible to obtain data for an entire population. Using a sampling procedure allows for statistical inference, though this involves a certain possibility of error. [1] When determining whether to reject or fail to reject the null hypothesis, mistakes can be made: Type I and Type II errors. Though it is impossible to ensure that these errors have not occurred, researchers should limit the possibilities of these faults. [2]
Significance
Significance is a term to describe the substantive importance of medical research. Statistical significance is the likelihood of results due to chance. [3] Healthcare providers should always delineate statistical significance from clinical significance, a common error when reviewing biomedical research. [4] When conceptualizing findings reported as either significant or not significant, healthcare providers should not simply accept researchers' results or conclusions without considering the clinical significance. Healthcare professionals should consider the clinical importance of findings and understand both p values and confidence intervals so they do not have to rely on the researchers to determine the level of significance. [5] One criterion often used to determine statistical significance is the utilization of p values.
P values are used in research to determine whether the sample estimate is significantly different from a hypothesized value. The p-value is the probability that the observed effect within the study would have occurred by chance if, in reality, there was no true effect. Conventionally, data yielding a p<0.05 or p<0.01 is considered statistically significant. While some have debated that the 0.05 level should be lowered, it is still universally practiced. [6] Hypothesis testing allows us to determine the size of the effect.
An example of findings reported with p values are below:
Statement: Drug 23 reduced patients' symptoms compared to Drug 22. Patients who received Drug 23 (n=100) were 2.1 times less likely than patients who received Drug 22 (n = 100) to experience symptoms of Disease A, p<0.05.
Statement:Individuals who were prescribed Drug 23 experienced fewer symptoms (M = 1.3, SD = 0.7) compared to individuals who were prescribed Drug 22 (M = 5.3, SD = 1.9). This finding was statistically significant, p= 0.02.
For either statement, if the threshold had been set at 0.05, the null hypothesis (that there was no relationship) should be rejected, and we should conclude significant differences. Noticeably, as can be seen in the two statements above, some researchers will report findings with < or > and others will provide an exact p-value (0.000001) but never zero [6] . When examining research, readers should understand how p values are reported. The best practice is to report all p values for all variables within a study design, rather than only providing p values for variables with significant findings. [7] The inclusion of all p values provides evidence for study validity and limits suspicion for selective reporting/data mining.
While researchers have historically used p values, experts who find p values problematic encourage the use of confidence intervals. [8] . P-values alone do not allow us to understand the size or the extent of the differences or associations. [3] In March 2016, the American Statistical Association (ASA) released a statement on p values, noting that scientific decision-making and conclusions should not be based on a fixed p-value threshold (e.g., 0.05). They recommend focusing on the significance of results in the context of study design, quality of measurements, and validity of data. Ultimately, the ASA statement noted that in isolation, a p-value does not provide strong evidence. [9]
When conceptualizing clinical work, healthcare professionals should consider p values with a concurrent appraisal study design validity. For example, a p-value from a double-blinded randomized clinical trial (designed to minimize bias) should be weighted higher than one from a retrospective observational study [7] . The p-value debate has smoldered since the 1950s [10] , and replacement with confidence intervals has been suggested since the 1980s. [11]
Confidence Intervals
A confidence interval provides a range of values within given confidence (e.g., 95%), including the accurate value of the statistical constraint within a targeted population. [12] Most research uses a 95% CI, but investigators can set any level (e.g., 90% CI, 99% CI). [13] A CI provides a range with the lower bound and upper bound limits of a difference or association that would be plausible for a population. [14] Therefore, a CI of 95% indicates that if a study were to be carried out 100 times, the range would contain the true value in 95, [15] confidence intervals provide more evidence regarding the precision of an estimate compared to p-values. [6]
In consideration of the similar research example provided above, one could make the following statement with 95% CI:
Statement: Individuals who were prescribed Drug 23 had no symptoms after three days, which was significantly faster than those prescribed Drug 22; there was a mean difference between the two groups of days to the recovery of 4.2 days (95% CI: 1.9 – 7.8).
It is important to note that the width of the CI is affected by the standard error and the sample size; reducing a study sample number will result in less precision of the CI (increase the width). [14] A larger width indicates a smaller sample size or a larger variability. [16] A researcher would want to increase the precision of the CI. For example, a 95% CI of 1.43 – 1.47 is much more precise than the one provided in the example above. In research and clinical practice, CIs provide valuable information on whether the interval includes or excludes any clinically significant values. [14]
Null values are sometimes used for differences with CI (zero for differential comparisons and 1 for ratios). However, CIs provide more information than that. [15] Consider this example: A hospital implements a new protocol that reduced wait time for patients in the emergency department by an average of 25 minutes (95% CI: -2.5 – 41 minutes). Because the range crosses zero, implementing this protocol in different populations could result in longer wait times; however, the range is much higher on the positive side. Thus, while the p-value used to detect statistical significance for this may result in "not significant" findings, individuals should examine this range, consider the study design, and weigh whether or not it is still worth piloting in their workplace.
Similarly to p-values, 95% CIs cannot control for researchers' errors (e.g., study bias or improper data analysis). [14] In consideration of whether to report p-values or CIs, researchers should examine journal preferences. When in doubt, reporting both may be beneficial. [13] An example is below:
Reporting both: Individuals who were prescribed Drug 23 had no symptoms after three days, which was significantly faster than those prescribed Drug 22, p = 0.009. There was a mean difference between the two groups of days to the recovery of 4.2 days (95% CI: 1.9 – 7.8).
- Clinical Significance
Recall that clinical significance and statistical significance are two different concepts. Healthcare providers should remember that a study with statistically significant differences and large sample size may be of no interest to clinicians, whereas a study with smaller sample size and statistically non-significant results could impact clinical practice. [14] Additionally, as previously mentioned, a non-significant finding may reflect the study design itself rather than relationships between variables.
Healthcare providers using evidence-based medicine to inform practice should use clinical judgment to determine the practical importance of studies through careful evaluation of the design, sample size, power, likelihood of type I and type II errors, data analysis, and reporting of statistical findings (p values, 95% CI or both). [4] Interestingly, some experts have called for "statistically significant" or "not significant" to be excluded from work as statistical significance never has and will never be equivalent to clinical significance. [17]
The decision on what is clinically significant can be challenging, depending on the providers' experience and especially the severity of the disease. Providers should use their knowledge and experiences to determine the meaningfulness of study results and make inferences based not only on significant or insignificant results by researchers but through their understanding of study limitations and practical implications.
- Nursing, Allied Health, and Interprofessional Team Interventions
All physicians, nurses, pharmacists, and other healthcare professionals should strive to understand the concepts in this chapter. These individuals should maintain the ability to review and incorporate new literature for evidence-based and safe care.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Jacob Shreffler declares no relevant financial relationships with ineligible companies.
Disclosure: Martin Huecker declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Shreffler J, Huecker MR. Hypothesis Testing, P Values, Confidence Intervals, and Significance. [Updated 2023 Mar 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- The reporting of p values, confidence intervals and statistical significance in Preventive Veterinary Medicine (1997-2017). [PeerJ. 2021] The reporting of p values, confidence intervals and statistical significance in Preventive Veterinary Medicine (1997-2017). Messam LLM, Weng HY, Rosenberger NWY, Tan ZH, Payet SDM, Santbakshsing M. PeerJ. 2021; 9:e12453. Epub 2021 Nov 24.
- Review Clinical versus statistical significance: interpreting P values and confidence intervals related to measures of association to guide decision making. [J Pharm Pract. 2010] Review Clinical versus statistical significance: interpreting P values and confidence intervals related to measures of association to guide decision making. Ferrill MJ, Brown DA, Kyle JA. J Pharm Pract. 2010 Aug; 23(4):344-51. Epub 2010 Apr 13.
- Interpreting "statistical hypothesis testing" results in clinical research. [J Ayurveda Integr Med. 2012] Interpreting "statistical hypothesis testing" results in clinical research. Sarmukaddam SB. J Ayurveda Integr Med. 2012 Apr; 3(2):65-9.
- Confidence intervals in procedural dermatology: an intuitive approach to interpreting data. [Dermatol Surg. 2005] Confidence intervals in procedural dermatology: an intuitive approach to interpreting data. Alam M, Barzilai DA, Wrone DA. Dermatol Surg. 2005 Apr; 31(4):462-6.
- Review Is statistical significance testing useful in interpreting data? [Reprod Toxicol. 1993] Review Is statistical significance testing useful in interpreting data? Savitz DA. Reprod Toxicol. 1993; 7(2):95-100.
Recent Activity
- Hypothesis Testing, P Values, Confidence Intervals, and Significance - StatPearl... Hypothesis Testing, P Values, Confidence Intervals, and Significance - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

The P value: What it really means
As nurses, we must administer nursing care based on the best available scientific evidence. But for many nurses, critical appraisal, the process used to determine the best available evidence, can seem intimidating. To make critical appraisal more approachable, let’s examine the P value and make sure we know what it is and what it isn’t.
Defining P value
The P value is the probability that the results of a study are caused by chance alone. To better understand this definition, consider the role of chance.
The concept of chance is illustrated with every flip of a coin. The true probability of obtaining heads in any single flip is 0.5, meaning that heads would come up in half of the flips and tails would come up in half of the flips. But if you were to flip a coin 10 times, you likely would not obtain heads five times and tails five times. You’d be more likely to see a seven-to-three split or a six-to-four split. Chance is responsible for this variation in results.
Just as chance plays a role in determining the flip of a coin, it plays a role in the sampling of a population for a scientific study. When subjects are selected, chance may produce an unequal distribution of a characteristic that can affect the outcome of the study. Statistical inquiry and the P value are designed to help us determine just how large a role chance plays in study results. We begin a study with the assumption that there will be no difference between the experimental and control groups. This assumption is called the null hypothesis. When the results of the study indicate that there is a difference, the P value helps us determine the likelihood that the difference is attributed to chance.
Competing hypotheses
In every study, researchers put forth two kinds of hypotheses: the research or alternative hypothesis and the null hypothesis. The research hypothesis reflects what the researchers hope to show—that there is a difference between the experimental group and the control group. The null hypothesis directly competes with the research hypothesis. It states that there is no difference between the experimental group and the control group.
It may seem logical that researchers would test the research hypothesis—that is, that they would test what they hope to prove. But the probability theory requires that they test the null hypothesis instead. To support the research hypothesis, the data must contradict the null hypothesis. By demonstrating a difference between the two groups, the data contradict the null hypothesis.
Testing the null hypothesis
Now that you know why we test the null hypothesis, let’s look at how we test the null hypothesis.
After formulating the null and research hypotheses, researchers decide on a test statistic they can use to determine whether to accept or reject the null hypothesis. They also propose a fixed-level P value. The fixed level P value is often set at .05 and serves as the value against which the test-generated P value must be compared. (See Why .05?)
A comparison of the two P values determines whether the null hypothesis is rejected or accepted. If the P value associated with the test statistic is less than the fixed-level P value, the null hypothesis is rejected because there’s a statistically significant difference between the two groups. If the P value associated with the test statistic is greater than the fixed-level P value, the null hypothesis is accepted because there’s no statistically significant difference between the groups.
The decision to use .05 as the threshold in testing the null hypothesis is completely arbitrary. The researchers credited with establishing this threshold warned against strictly adhering to it.
Remember that warning when appraising a study in which the test statistic is greater than .05. The savvy reader will consider other important measurements, including effect size, confidence intervals, and power analyses when deciding whether to accept or reject scientific findings that could influence nursing practice.
Real-world hypothesis testing
How does this play out in real life? Let’s assume that you and a nurse colleague are conducting a study to find out if patients who receive backrubs fall asleep faster than patients who do not receive backrubs.
1. State your null and research hypotheses
Your null hypothesis will be that there will be no difference in the average amount of time it takes patients in each group to fall asleep. Your research hypothesis will be that patients who receive backrubs fall asleep, on average, faster than those who do not receive backrubs. You will be testing the null hypothesis in hopes of supporting your research hypothesis.
2. Propose a fixed-level P value
Although you can choose any value as your fixed-level P value, you and your research colleague decide you’ll stay with the conventional .05. If you were testing a new medical product or a new drug, you would choose a much smaller P value (perhaps as small as .0001). That’s because you would want to be as sure as possible that any difference you see between groups is attributed to the new product or drug and not to chance. A fixed-level P value of .0001 would mean that the difference between the groups was attributed to chance only 1 time out of 10,000. For a study on backrubs, however, .05 seems appropriate.
3. Conduct hypothesis testing to calculate a probability value
You and your research colleague agree that a randomized controlled study will help you best achieve your research goals, and you design the process accordingly. After consenting to participate in the study, patients are randomized to one of two groups:
- the experimental group that receives the intervention—the backrub group
- the control group—the non-backrub group.
After several nights of measuring the number of minutes it takes each participant to fall asleep, you and your research colleague find that on average, the backrub group takes 19 minutes to fall asleep and the non-backrub group takes 24 minutes to fall asleep.
Now the question is: Would you have the same results if you conducted the study using two different groups of people? That is, what role did chance play in helping the backrub group fall asleep 5 minutes faster than the non-backrub group? To answer this, you and your colleague will use an independent samples t-test to calculate a probability value.
An independent samples t-test is a kind of hypothesis test that compares the mean values of two groups (backrub and non-backrub) on a given variable (time to fall asleep).
Hypothesis testing is really nothing more than testing the null hypothesis. In this case, the null hypothesis is that the amount of time needed to fall asleep is the same for the experimental group and the control group. The hypothesis test addresses this question: If there’s really no difference between the groups, what is the probability of observing a difference of 5 minutes or more, say 10 minutes or 15 minutes?
We can define the P value as the probability that the observed time difference resulted from chance. Some find it easier to understand the P value when they think of it in relationship to error. In this case, the P value is defined as the probability of committing a Type 1 error. (Type 1 error occurs when a true null hypothesis is incorrectly rejected.)
4. Compare and interpret the P value
Early on in your study, you and your colleague selected a fixed-level P value of .05, meaning that you were willing to accept that 5% of the time, your results might be caused by chance. Also, you used an independent samples t-test to arrive at a probability value that will help you determine the role chance played in obtaining your results. Let’s assume, for the sake of this example, that the probability value generated by the independent samples t-test is .01 (P = .01). Because this P value associated with the test statistic is less than the fixed-level statistic (.01 < .05), you can reject the null hypothesis. By doing so, you declare that there is a statistically significant difference between the experimental and control groups. (See Putting the P value in context.)
In effect, you’re saying that the chance of observing a difference of 5 minutes or more, when in fact there is no difference, is less than 5 in 100. If the P value associated with the test statistic would have been greater than .05, then you would accept the null hypothesis, which would mean that there is no statistically significant difference between the control and experimental groups. Accepting the null hypothesis would mean that a difference of 5 minutes or more between the two groups would occur more than 5 times in 100.
Putting the P value in context
Although the P value helps you interpret study results, keep in mind that many factors can influence the P value—and your decision to accept or reject the null hypothesis. These factors include the following:
- Insufficient power. The study may not have been designed appropriately to detect an effect of the independent variable on the dependent variable. Therefore, a change may have occurred without your knowing it, causing you to incorrectly reject your hypothesis.
- Unreliable measures. Instruments that don’t meet consistency or reliability standards may have been used to measure a particular phenomenon.
- Threats to internal validity. Various biases, such as selection of patients, regression, history, and testing bias, may unduly influence study outcomes.
A decision to accept or reject study findings should focus not only on P value but also on other metrics including the following:
- Confidence intervals (an estimated range of values with a high probability of including the true population value of a given parameter)
- Effect size (a value that measures the magnitude of a treatment effect)
Remember, P value tells you only whether a difference exists between groups. It doesn’t tell you the magnitude of the difference.
5. Communicate your findings
The final step in hypothesis testing is communicating your findings. When sharing research findings (hypotheses) in writing or discussion, understand that they are statements of relationships or differences in populations. Your findings are not proved or disproved. Scientific findings are always subject to change. But each study leads to better understanding and, ideally, better outcomes for patients.
Key concepts
The P value isn’t the only concept you need to understand to analyze research findings. But it is a very important one. And chances are that understanding the P value will make it easier to understand other key analytical concepts.
Selected references
Burns N, Grove S: The Practice of Nursing Research: Conduct, Critique, and Utilization. 5th ed. Philadelphia: WB Saunders; 2004.
Glaser DN: The controversy of significance testing: misconceptions and alternatives. Am J Crit Care. 1999;8(5):291-296.
Kenneth J. Rempher, PhD, RN, MBA, CCRN, APRN,BC, is Director, Professional Nursing Practice at Sinai Hospital of Baltimore (Md.). Kathleen Urquico, BSN, RN, is a Direct Care Nurse in the Rubin Institute of Advanced Orthopedics at Sinai Hospital of Baltimore.

NurseLine Newsletter
- First Name *
- Last Name *
- Hidden Referrer
*By submitting your e-mail, you are opting in to receiving information from Healthcom Media and Affiliates. The details, including your email address/mobile number, may be used to keep you informed about future products and services.
Test Your Knowledge
Recent posts.

Interpreting statistical significance in nursing research

Introduction to qualitative nursing research

Navigating statistics for successful project implementation

Nurse research and the institutional review board

Research 101: Descriptive statistics

Research 101: Forest plots

Understanding confidence intervals helps you make better clinical decisions

Differentiating statistical significance and clinical significance

Differentiating research, evidence-based practice, and quality improvement

Are you confident about confidence intervals?

Making sense of statistical power

The First Step: Ask; Fundamentals of Evidence-Based Nursing Practice
In this module, we will learn about identifying the problem, start the “Ask” process with developing an answerable clinical question, and learn about purpose statements and hypotheses.
Content includes:
- Identifying the problem
- Determining the Population, Intervention, Comparison, and Outcome (PICO)
- Asking a Research/Clinical Question (Based on PICO)
Statements of Purpose
Objectives:
- Describe the process of developing a research/practice problem.
- Describe the components of a PICO.
- Identify different types of PICOs.
- Distinguish function and form of statements of purpose.
- Describe the function and characteristics of hypotheses.
Development of a Research/Practice Problem
Practice questions frequently arise from day-to-day problems that are encountered by providers (Dearholt & Dang, 2012). Often, these problems are very obvious. However, sometimes we need to back up and take a close look at the status quo to see underlying issues. The basis for any research project is indeed the underlying problem or issue. A good problem statement or paragraph is a declaration of what it is that is problematic or what it is that we do not know much about (a gap in knowledge) (Polit & Beck, 2018).
The process of defining the practice/clinical problem begins by seeking answers to clinical concerns. This is the first step in the EBP process: To ask . We start by asking some broad questions to help guide the process of developing our practice problem.
- Is there evidence that the current treatment works?
- Does the current practice help the patient?
- Why are we doing the current practice?
- Should we be doing the current practice this way?
- Is there a way to do this current practice more efficiently?
- Is there a more cost-effective method to do this practice?
Problem Statements:
For our EBP Project, we will need to ask these broad questions and then develop our problem that exists. This establishes the “background” of the issue we want to know more about.
For example, if we are choosing a clinical question based on wanting to know if adjunct music therapy helps decrease postoperative pain levels than just pharmaceuticals alone, we might consider the underlying problems of:
- Postoperative pain is not adequately managed in greater than 80% of patients in the US, although rates vary depending on such factors as type of surgery performed, analgesic/anesthetic intervention used, and time elapsed after surgery (Gan, 2017).
- Poorly controlled acute postoperative pain is associated with increased morbidity, functional and quality-of-life impairment, delayed recovery time, prolonged duration of opioid use, and higher health-care costs (Gan, 2017).
- Multimodal analgesic techniques are widely used but new evidence is disappointing (Rawal, 2016).
In the above examples, we are establishing that poorly managed postoperative pain is a problem. Thus, looking at evidence about adjunctive music therapy may help to address how we might manage pain more effectively. These are our problem statements. This would be our introduction section on the EBP poster. For the sake of our EBP poster, you do not need to list these on the poster references. A heads up: The sources used to help develop our research/clinical program should not be the same resources that we use to answer our upcoming clinical question. In essence, we will be conducting two literature reviews: One, to establish the underlying problem; and, two: To find published research that helps to answer our developed clinical question.
Here is the introduction to the article titled, “The relationships among pain, depression, and physical activity in patients with heart failure” (Haedtke et al, 2017). You can read that the underlying problem is multifocal: 67% of patient with heart failure (HF) experience pain, depression is a comorbidity that affects 22% to 42% of HF patients, and that little attention has been paid to this relationship in patients with HF. The researchers have established the need for further research and why further research is needed.

Here is another example of how the clinical problem is addressed in an EBP poster that wants to appraise existing evidence related to dressing choice for decubitus ulcers.
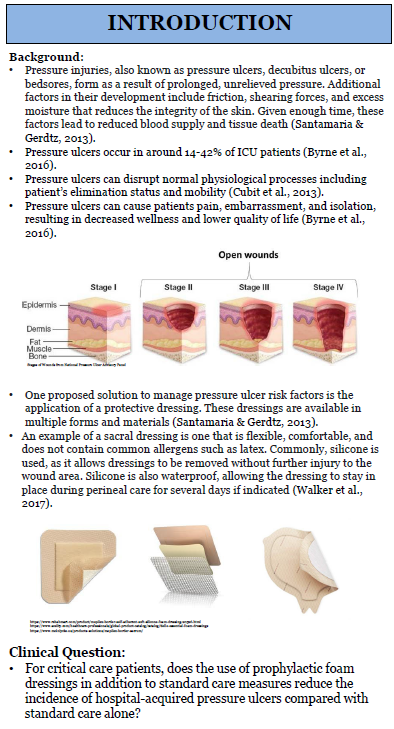
When trying to communicate clinical problems, there are two main sources (Titler et al, 1994, 2001):
- Problem-focused triggers : These are identified by staff during routine monitoring of quality, risk, adverse events, financial, or benchmarking data.
- Knowledge-focused triggers : There are identified through reading published evidence or learning new information at conferences or other professional meetings.
Sources of Evidence-Based Clinical Problems:
Most problem statements have the following components:
- Problem identification: What is wrong with the current situation or action?
- Background: What is the nature of the problem or the context of the situation? (this helps to establish the why)
- Scope of the problem: How many people are affected? Is this a small problem? Big problem? Potential to grow quickly to a large problem? Has been increasing/decreasing recently?
- Consequences of the problem: If we do nothing or leave as the status quo, what is the cost of not fixing the issue?
- Knowledge gaps: What information about the problem is lacking? We need to know what we do not know.
- Proposed solution: How will the information or evidence contribute to the solution of the problem?
If you are stumped on a topic, ask faculty, RNs at local facilities, colleagues, and key stakeholders at local facilities for some ideas! There is usually “something” that the nursing field is concerned about or has questions about.
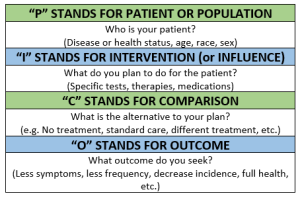
Components of a PICO Question
After we have asked ourselves some background questions, we need to develop a foreground (focused) question. A thoughtful development of a well-structured foreground clinical/practice question is important because the question drives the strategies that you will use to search for the published evidence. The question needs to be very specific, non-ambiguous , and measurable in order to find the relevant evidence needed and also increased the likelihood that you will find what you are looking for.
In developing your clinical/practice question, there is a helpful format to utilize to establish the key component. This format includes the Patient/Population, Intervention/Influence/Exposure, Comparison, and Outcome (PICO) (Richardson, Wilson, Nishikawa, & Hayward, 1995).
Let’s dive into each component to better understand.
P atient, population, or problem: We want to describe the patient, the population, or the problem. Get specific. We will want to know exactly who we are wanting to know about. Consider age, gender, setting of the patient (e.g. postoperative), and/or symptoms.
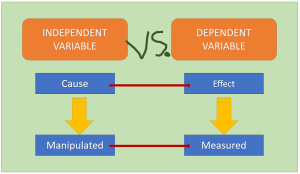
I ntervention: The intervention is the action or, in other words, the treatment, process of care, education given, or assessment approaches. We will come back to this in more depth, but for now remember that the intervention is also called the “Independent Variable”.
C omparison: Here we are comparing with other interventions. A comparison can be standard of care that already exists, current practice, an opposite intervention/action, or a different intervention/action.
O utcome: What is that that we are looking at for a result or consequence of the intervention? The outcome needs to have a metric for actually measuring results. The outcome can include quality of life, patient satisfaction, cost impacts, or treatment results. The outcome is also called the “Dependent Variable”.
The PICO question is a critical aspect of the EBP project to guide the problem identification and create components that can be used to shape the literature search.
Let’s watch a nice YouTube video, “PICO: A Model for Evidence-Based Research”:
“PICO: A Model for Evidence Based Research” by Binghamton University Libraries. Licensed CCY BY .
Great! Okay, let’s move on and discuss the various types of PICOs.
Types of PICOs
Before we start developing our clinical question, let’s go over the various types of PICOs and the clinical question that can result from the components. There are various types of PICOs but we are concerned with the therapy/treatment/intervention format of PICO for our EBP posters.
Let’s take a look at the various types of PICOs:
The first step in developing a research or clinical practice question is developing your PICO. Well, we’ve done that above. You will select each component of your PICO and then turn that into your question. Making the EBP question as specific as possible really helps to identify specific terms and narrow the search, which will result in reducing the time it times searching for relevant evidence.
Once you have your pertinent clinical question, you will use the components to begin your search in published literature for articles that help to answer your question. In class, we will practice with various situations to develop PICOs and clinical questions.
Many articles have the researcher’s statement of purpose (sometimes referred to as “aim”, “goal”, or “objective”) for their research project. This helps to identify what the overarching direction of inquiry may be. You do not need a statement of purpose/aim/goal/objective for your EBP poster. However, knowing what a statement of purpose is will help you when appraising articles to help answer your clinical question.
The following statement of purpose was written as an aim. The population (P) was identified as patients with HF, the interventions (I) included physical activity/exercise, and the outcomes (O) included pain, depression, total activity time, and sitting time as correlated with the interventions.
In the articles above, the authors made it easy and included their statements of purpose within the abstract at the beginning of the article. Most articles do not feature this ease, and you will need to read the introduction or methodology section of the article to find the statement of purpose, much like within article 3.1.
In qualitative studies, the statement of purpose usually indicates the nature of the inquiry, the key concept, the key phenomenon, and the population.
Function and Characteristics of Hypotheses.
A hypothesis (plural: hypothes es ) is a statement of predicted outcome. Meaning, it is an educated and formulated guess as to how the intervention (independent variable – more on that soon!) impacts the outcome (dependent variable). It is not always a cause and effect. Sometimes there can be just a simple association or correlation. We will come back to that in a few modules.
In your PICO statement, you can think of the “I” as the independent variable and the “O” as the dependent variable . Variables will begin making more sense as we go. But for now, remember this:
Independent Variable (IV): This is a measure that can be manipulated by the researcher. Perhaps it is a medication, an educational program, or a survey. The independent variable enacts change (or not) onto the independent variable.
Dependent Variable (DV): This is the result of the independent variable. This is the variable that we utilize statistical analyses to measure. For instance, if we are intervening with a blood pressure medication (our IV), then our DV would be the measurement of the actual blood pressure.
Most of the time, a hypothesis results from a well-worded research question. Here is an example:
Research Question : “Does sexual abuse in childhood affect the development of irritable bowel syndrome in women?”
Research Hypothesis : Women (P) who were sexually abused in childhood (I) have a higher incidence of irritable bowel syndrome (O) than women who were not abused (C).
You may note in that hypothesis that there is a predicted direction of outcome. One thing leads to something.
But, why do we need a hypothesis? First, they help to promote critical thinking. Second, it gives the researcher a way to measure a relationship. Suppose we conducted a study guided only by a research question. Take the above question, for example. Without a hypothesis, the researcher is seemingly prepared to accept any result (Polit & Beck, 2021). The problem with that is that it is almost always possible to explain something superficially after the fact, even if the findings are inconclusive. A hypothesis reduces the possibility that spurious results will be misconstrued (Polit & Beck, 2021).

Not all research articles will list a hypothesis. This makes it more difficult to critically appraise the results. That is not to say that the results would be invalidated, but it should ignite a spirit of further inquiry as to if the results are valid.
Hypotheses (also called alternative hypothesis) can be stated as:
- Directional or nondirectional
- Simple or complex
- Research or Null
Simple hypothesis : Statement of causal (cause and effect) relationship – one independent variable (intervention) and one dependent variable (outcome).
Example : If you stay up late, then you feel tired the next day.
Complex hypothesis : Statement of causal (cause and effect) or associative (not causal) between two or more independent variables (interventions) and/or two or more dependent variables (outcomes).
Example : Higher the poverty, higher the illiteracy in society, higher will be the rate of crime (three variables – two independent variables and one dependent variable).
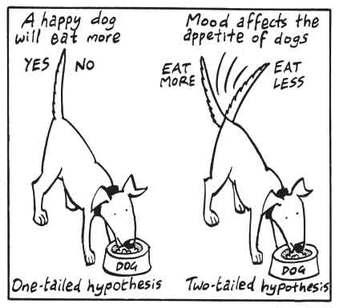
Directional hypothesis : Specifies not only the existence but also the expected direction of the relationship between the dependent (outcome) and the independent (intervention) variables. You will also see this called “One-tailed hypothesis”.
Example : Depression scores will decrease following a 6-week intervention.
Nondirectional hypothesis : Does not specify the direction of relationship between the variables. You will also see this called “Two-tailed hypothesis”.
Example : College students will perform differently from elementary school students on a memory task (without predicting which group of students will perform better).
Null hypothesis : The null hypothesis assumes that any kind of difference between the chosen characteristics that you see in a set of data is due to chance. Now, the null hypothesis is why the plain old hypothesis is also called alternative hypothesis. We don’t just assume that the hypothesis is true. So, it is considered an alternative to something just happening by chance (null).
Example : Let’s say our research question is, “Do teens use cell phones to access the internet more than adults?” – our null hypothesis could state: Age has no effect on how cell phones are used for internet access.
And then, further develop the problem and background through finding existing literature to help answer the following questions:
- Knowledge gaps: What information about the problem is lacking? We need to know what we do not know.
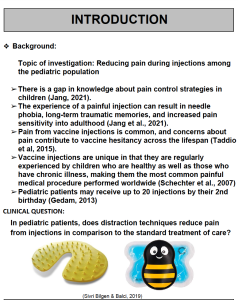
With the previous example of pain in the pediatric population, here is an example of an Introduction section from a past student poster:
- What was the research problem? Was the problem statement easy to locate and was it clearly stated? Did the problem statement build a coherent and persuasive argument for the new study?
- Does the problem have significance for nursing?
- Was there a good fit between the research problem and the paradigm (and tradition) within which the research was conducted?
- Did the report formally present a statement of purpose, research question, and/or hypotheses? Was this information communicated clearly and concisely, and was it placed in a logical and useful location?
- Were purpose statements or research questions worded appropriately (e.g., were key concepts/variables identified and the population specified?
- If there were no formal hypotheses, was their absence justified? Were statistical tests used in analyzing the data despite the absence of stated hypotheses?
- Were hypotheses (if any) properly worded—did they state a predicted relationship between two or more variables? Were they presented as research or as null hypotheses?
References & Attribution
“ Green check mark ” by rawpixel licensed CC0 .
“ Light bulb doodle ” by rawpixel licensed CC0 .
“ Magnifying glass ” by rawpixel licensed CC0
“ Orange flame ” by rawpixel licensed CC0 .
Chen, P., Nunez-Smith, M., Bernheim, S… (2010). Professional experiences of international medical graduates practicing primary care in the United States. Journal of General Internal Medicine, 25 (9), 947-53.
Dearholt, S.L., & Dang, D. (2012). Johns Hopkins nursing evidence-based practice: Model and guidelines (2nd Ed.). Indianapolis, IN: Sigma Theta Tau International.
Gan, T. (2017). Poorly controlled postoperative pain: Prevalence, consequences, and prevention. Journal of Pain Research, 10, 2287-2298.
Genc, A., Can, G., Aydiner, A. (2012). The efficiency of the acupressure in prevention of the chemotherapy-induced nausea and vomiting. Support Care Cancer, 21 , 253-261.
Haedtke, C., Smith, M., VanBuren, J., Kein, D., Turvey, C. (2017). The relationships among pain, depression, and physical activity in patients with heart failure. Journal of Cardiovascular Nursing, 32 (5), E21-E25.
Pankong, O., Pothiban, L., Sucamvang, K., Khampolsiri, T. (2018). A randomized controlled trial of enhancing positive aspects of caregiving in Thai dementia caregivers for dementia. Pacific Rim Internal Journal of Nursing Res, 22 (2), 131-143.
Polit, D. & Beck, C. (2021). Lippincott CoursePoint Enhanced for Polit’s Essentials of Nursing Research (10th ed.). Wolters Kluwer Health.
Rawal, N. (2016). Current issues in postoperative pain management. European Journal of Anaesthesiology, 33 , 160-171.
Richardson, W.W., Wilson, M.C., Nishikawa, J., & Hayward, R.S. (1995). The well-built clinical question: A key to evidence-based decisions. American College of Physicians, 123 (3), A12-A13.
Titler, M. G., Kleiber, C., Steelman, V.J. Rakel, B. A. Budreau, G., Everett,…Goode, C.J. (2001). The Iowa model of evidence-based practice to promote quality care. Critical Care Nursing Clinics of North America, 13 (4), 497-509.
Evidence-Based Practice & Research Methodologies Copyright © by Tracy Fawns is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License , except where otherwise noted.
Share This Book
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Write for Us
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 21, Issue 4
- How to appraise quantitative research
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
This article has a correction. Please see:
- Correction: How to appraise quantitative research - April 01, 2019
- Xabi Cathala 1 ,
- Calvin Moorley 2
- 1 Institute of Vocational Learning , School of Health and Social Care, London South Bank University , London , UK
- 2 Nursing Research and Diversity in Care , School of Health and Social Care, London South Bank University , London , UK
- Correspondence to Mr Xabi Cathala, Institute of Vocational Learning, School of Health and Social Care, London South Bank University London UK ; cathalax{at}lsbu.ac.uk and Dr Calvin Moorley, Nursing Research and Diversity in Care, School of Health and Social Care, London South Bank University, London SE1 0AA, UK; Moorleyc{at}lsbu.ac.uk
https://doi.org/10.1136/eb-2018-102996
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
Some nurses feel that they lack the necessary skills to read a research paper and to then decide if they should implement the findings into their practice. This is particularly the case when considering the results of quantitative research, which often contains the results of statistical testing. However, nurses have a professional responsibility to critique research to improve their practice, care and patient safety. 1 This article provides a step by step guide on how to critically appraise a quantitative paper.
Title, keywords and the authors
The authors’ names may not mean much, but knowing the following will be helpful:
Their position, for example, academic, researcher or healthcare practitioner.
Their qualification, both professional, for example, a nurse or physiotherapist and academic (eg, degree, masters, doctorate).
This can indicate how the research has been conducted and the authors’ competence on the subject. Basically, do you want to read a paper on quantum physics written by a plumber?
The abstract is a resume of the article and should contain:
Introduction.
Research question/hypothesis.
Methods including sample design, tests used and the statistical analysis (of course! Remember we love numbers).
Main findings.
Conclusion.
The subheadings in the abstract will vary depending on the journal. An abstract should not usually be more than 300 words but this varies depending on specific journal requirements. If the above information is contained in the abstract, it can give you an idea about whether the study is relevant to your area of practice. However, before deciding if the results of a research paper are relevant to your practice, it is important to review the overall quality of the article. This can only be done by reading and critically appraising the entire article.
The introduction
Example: the effect of paracetamol on levels of pain.
My hypothesis is that A has an effect on B, for example, paracetamol has an effect on levels of pain.
My null hypothesis is that A has no effect on B, for example, paracetamol has no effect on pain.
My study will test the null hypothesis and if the null hypothesis is validated then the hypothesis is false (A has no effect on B). This means paracetamol has no effect on the level of pain. If the null hypothesis is rejected then the hypothesis is true (A has an effect on B). This means that paracetamol has an effect on the level of pain.
Background/literature review
The literature review should include reference to recent and relevant research in the area. It should summarise what is already known about the topic and why the research study is needed and state what the study will contribute to new knowledge. 5 The literature review should be up to date, usually 5–8 years, but it will depend on the topic and sometimes it is acceptable to include older (seminal) studies.
Methodology
In quantitative studies, the data analysis varies between studies depending on the type of design used. For example, descriptive, correlative or experimental studies all vary. A descriptive study will describe the pattern of a topic related to one or more variable. 6 A correlational study examines the link (correlation) between two variables 7 and focuses on how a variable will react to a change of another variable. In experimental studies, the researchers manipulate variables looking at outcomes 8 and the sample is commonly assigned into different groups (known as randomisation) to determine the effect (causal) of a condition (independent variable) on a certain outcome. This is a common method used in clinical trials.
There should be sufficient detail provided in the methods section for you to replicate the study (should you want to). To enable you to do this, the following sections are normally included:
Overview and rationale for the methodology.
Participants or sample.
Data collection tools.
Methods of data analysis.
Ethical issues.
Data collection should be clearly explained and the article should discuss how this process was undertaken. Data collection should be systematic, objective, precise, repeatable, valid and reliable. Any tool (eg, a questionnaire) used for data collection should have been piloted (or pretested and/or adjusted) to ensure the quality, validity and reliability of the tool. 9 The participants (the sample) and any randomisation technique used should be identified. The sample size is central in quantitative research, as the findings should be able to be generalised for the wider population. 10 The data analysis can be done manually or more complex analyses performed using computer software sometimes with advice of a statistician. From this analysis, results like mode, mean, median, p value, CI and so on are always presented in a numerical format.
The author(s) should present the results clearly. These may be presented in graphs, charts or tables alongside some text. You should perform your own critique of the data analysis process; just because a paper has been published, it does not mean it is perfect. Your findings may be different from the author’s. Through critical analysis the reader may find an error in the study process that authors have not seen or highlighted. These errors can change the study result or change a study you thought was strong to weak. To help you critique a quantitative research paper, some guidance on understanding statistical terminology is provided in table 1 .
- View inline
Some basic guidance for understanding statistics
Quantitative studies examine the relationship between variables, and the p value illustrates this objectively. 11 If the p value is less than 0.05, the null hypothesis is rejected and the hypothesis is accepted and the study will say there is a significant difference. If the p value is more than 0.05, the null hypothesis is accepted then the hypothesis is rejected. The study will say there is no significant difference. As a general rule, a p value of less than 0.05 means, the hypothesis is accepted and if it is more than 0.05 the hypothesis is rejected.
The CI is a number between 0 and 1 or is written as a per cent, demonstrating the level of confidence the reader can have in the result. 12 The CI is calculated by subtracting the p value to 1 (1–p). If there is a p value of 0.05, the CI will be 1–0.05=0.95=95%. A CI over 95% means, we can be confident the result is statistically significant. A CI below 95% means, the result is not statistically significant. The p values and CI highlight the confidence and robustness of a result.
Discussion, recommendations and conclusion
The final section of the paper is where the authors discuss their results and link them to other literature in the area (some of which may have been included in the literature review at the start of the paper). This reminds the reader of what is already known, what the study has found and what new information it adds. The discussion should demonstrate how the authors interpreted their results and how they contribute to new knowledge in the area. Implications for practice and future research should also be highlighted in this section of the paper.
A few other areas you may find helpful are:
Limitations of the study.
Conflicts of interest.
Table 2 provides a useful tool to help you apply the learning in this paper to the critiquing of quantitative research papers.
Quantitative paper appraisal checklist
- 1. ↵ Nursing and Midwifery Council , 2015 . The code: standard of conduct, performance and ethics for nurses and midwives https://www.nmc.org.uk/globalassets/sitedocuments/nmc-publications/nmc-code.pdf ( accessed 21.8.18 ).
- Gerrish K ,
- Moorley C ,
- Tunariu A , et al
- Shorten A ,
Competing interests None declared.
Patient consent Not required.
Provenance and peer review Commissioned; internally peer reviewed.
Correction notice This article has been updated since its original publication to update p values from 0.5 to 0.05 throughout.
Linked Articles
- Miscellaneous Correction: How to appraise quantitative research BMJ Publishing Group Ltd and RCN Publishing Company Ltd Evidence-Based Nursing 2019; 22 62-62 Published Online First: 31 Jan 2019. doi: 10.1136/eb-2018-102996corr1
Read the full text or download the PDF:
- Physician Physician Board Reviews Physician Associate Board Reviews CME Lifetime CME Free CME
- Student USMLE Step 1 USMLE Step 2 USMLE Step 3 COMLEX Level 1 COMLEX Level 2 COMLEX Level 3 96 Medical School Exams Student Resource Center NCLEX - RN NCLEX - LPN/LVN/PN 24 Nursing Exams
- Nurse Practitioner APRN/NP Board Reviews CNS Certification Reviews CE - Nurse Practitioner FREE CE
- Nurse RN Certification Reviews CE - Nurse FREE CE
- Pharmacist Pharmacy Board Exam Prep CE - Pharmacist
- Allied Allied Health Exam Prep Dentist Exams CE - Social Worker CE - Dentist
- Point of Care
- Free CME/CE
Hypothesis Testing, P Values, Confidence Intervals, and Significance
Definition/introduction.
Medical providers often rely on evidence-based medicine to guide decision-making in practice. Often a research hypothesis is tested with results provided, typically with p values, confidence intervals, or both. Additionally, statistical or research significance is estimated or determined by the investigators. Unfortunately, healthcare providers may have different comfort levels in interpreting these findings, which may affect the adequate application of the data.
Issues of Concern
Register for free and read the full article, learn more about a subscription to statpearls point-of-care.
Without a foundational understanding of hypothesis testing, p values, confidence intervals, and the difference between statistical and clinical significance, it may affect healthcare providers' ability to make clinical decisions without relying purely on the research investigators deemed level of significance. Therefore, an overview of these concepts is provided to allow medical professionals to use their expertise to determine if results are reported sufficiently and if the study outcomes are clinically appropriate to be applied in healthcare practice.
Hypothesis Testing
Investigators conducting studies need research questions and hypotheses to guide analyses. Starting with broad research questions (RQs), investigators then identify a gap in current clinical practice or research. Any research problem or statement is grounded in a better understanding of relationships between two or more variables. For this article, we will use the following research question example:
Research Question: Is Drug 23 an effective treatment for Disease A?
Research questions do not directly imply specific guesses or predictions; we must formulate research hypotheses. A hypothesis is a predetermined declaration regarding the research question in which the investigator(s) makes a precise, educated guess about a study outcome. This is sometimes called the alternative hypothesis and ultimately allows the researcher to take a stance based on experience or insight from medical literature. An example of a hypothesis is below.
Research Hypothesis: Drug 23 will significantly reduce symptoms associated with Disease A compared to Drug 22.
The null hypothesis states that there is no statistical difference between groups based on the stated research hypothesis.
Researchers should be aware of journal recommendations when considering how to report p values, and manuscripts should remain internally consistent.
Regarding p values, as the number of individuals enrolled in a study (the sample size) increases, the likelihood of finding a statistically significant effect increases. With very large sample sizes, the p-value can be very low significant differences in the reduction of symptoms for Disease A between Drug 23 and Drug 22. The null hypothesis is deemed true until a study presents significant data to support rejecting the null hypothesis. Based on the results, the investigators will either reject the null hypothesis (if they found significant differences or associations) or fail to reject the null hypothesis (they could not provide proof that there were significant differences or associations).
To test a hypothesis, researchers obtain data on a representative sample to determine whether to reject or fail to reject a null hypothesis. In most research studies, it is not feasible to obtain data for an entire population. Using a sampling procedure allows for statistical inference, though this involves a certain possibility of error. [1] When determining whether to reject or fail to reject the null hypothesis, mistakes can be made: Type I and Type II errors. Though it is impossible to ensure that these errors have not occurred, researchers should limit the possibilities of these faults. [2]
Significance
Significance is a term to describe the substantive importance of medical research. Statistical significance is the likelihood of results due to chance. [3] Healthcare providers should always delineate statistical significance from clinical significance, a common error when reviewing biomedical research. [4] When conceptualizing findings reported as either significant or not significant, healthcare providers should not simply accept researchers' results or conclusions without considering the clinical significance. Healthcare professionals should consider the clinical importance of findings and understand both p values and confidence intervals so they do not have to rely on the researchers to determine the level of significance. [5] One criterion often used to determine statistical significance is the utilization of p values.
P values are used in research to determine whether the sample estimate is significantly different from a hypothesized value. The p-value is the probability that the observed effect within the study would have occurred by chance if, in reality, there was no true effect. Conventionally, data yielding a p<0.05 or p<0.01 is considered statistically significant. While some have debated that the 0.05 level should be lowered, it is still universally practiced. [6] Hypothesis testing allows us to determine the size of the effect.
An example of findings reported with p values are below:
Statement: Drug 23 reduced patients' symptoms compared to Drug 22. Patients who received Drug 23 (n=100) were 2.1 times less likely than patients who received Drug 22 (n = 100) to experience symptoms of Disease A, p<0.05.
Statement:Individuals who were prescribed Drug 23 experienced fewer symptoms (M = 1.3, SD = 0.7) compared to individuals who were prescribed Drug 22 (M = 5.3, SD = 1.9). This finding was statistically significant, p= 0.02.
For either statement, if the threshold had been set at 0.05, the null hypothesis (that there was no relationship) should be rejected, and we should conclude significant differences. Noticeably, as can be seen in the two statements above, some researchers will report findings with < or > and others will provide an exact p-value (0.000001) but never zero [6] . When examining research, readers should understand how p values are reported. The best practice is to report all p values for all variables within a study design, rather than only providing p values for variables with significant findings. [7] The inclusion of all p values provides evidence for study validity and limits suspicion for selective reporting/data mining.
While researchers have historically used p values, experts who find p values problematic encourage the use of confidence intervals. [8] . P-values alone do not allow us to understand the size or the extent of the differences or associations. [3] In March 2016, the American Statistical Association (ASA) released a statement on p values, noting that scientific decision-making and conclusions should not be based on a fixed p-value threshold (e.g., 0.05). They recommend focusing on the significance of results in the context of study design, quality of measurements, and validity of data. Ultimately, the ASA statement noted that in isolation, a p-value does not provide strong evidence. [9]
When conceptualizing clinical work, healthcare professionals should consider p values with a concurrent appraisal study design validity. For example, a p-value from a double-blinded randomized clinical trial (designed to minimize bias) should be weighted higher than one from a retrospective observational study [7] . The p-value debate has smoldered since the 1950s [10] , and replacement with confidence intervals has been suggested since the 1980s. [11]
Confidence Intervals
A confidence interval provides a range of values within given confidence (e.g., 95%), including the accurate value of the statistical constraint within a targeted population. [12] Most research uses a 95% CI, but investigators can set any level (e.g., 90% CI, 99% CI). [13] A CI provides a range with the lower bound and upper bound limits of a difference or association that would be plausible for a population. [14] Therefore, a CI of 95% indicates that if a study were to be carried out 100 times, the range would contain the true value in 95, [15] confidence intervals provide more evidence regarding the precision of an estimate compared to p-values. [6]
In consideration of the similar research example provided above, one could make the following statement with 95% CI:
Statement: Individuals who were prescribed Drug 23 had no symptoms after three days, which was significantly faster than those prescribed Drug 22; there was a mean difference between the two groups of days to the recovery of 4.2 days (95% CI: 1.9 – 7.8).
It is important to note that the width of the CI is affected by the standard error and the sample size; reducing a study sample number will result in less precision of the CI (increase the width). [14] A larger width indicates a smaller sample size or a larger variability. [16] A researcher would want to increase the precision of the CI. For example, a 95% CI of 1.43 – 1.47 is much more precise than the one provided in the example above. In research and clinical practice, CIs provide valuable information on whether the interval includes or excludes any clinically significant values. [14]
Null values are sometimes used for differences with CI (zero for differential comparisons and 1 for ratios). However, CIs provide more information than that. [15] Consider this example: A hospital implements a new protocol that reduced wait time for patients in the emergency department by an average of 25 minutes (95% CI: -2.5 – 41 minutes). Because the range crosses zero, implementing this protocol in different populations could result in longer wait times; however, the range is much higher on the positive side. Thus, while the p-value used to detect statistical significance for this may result in "not significant" findings, individuals should examine this range, consider the study design, and weigh whether or not it is still worth piloting in their workplace.
Similarly to p-values, 95% CIs cannot control for researchers' errors (e.g., study bias or improper data analysis). [14] In consideration of whether to report p-values or CIs, researchers should examine journal preferences. When in doubt, reporting both may be beneficial. [13] An example is below:
Reporting both: Individuals who were prescribed Drug 23 had no symptoms after three days, which was significantly faster than those prescribed Drug 22, p = 0.009. There was a mean difference between the two groups of days to the recovery of 4.2 days (95% CI: 1.9 – 7.8).
Clinical Significance
Recall that clinical significance and statistical significance are two different concepts. Healthcare providers should remember that a study with statistically significant differences and large sample size may be of no interest to clinicians, whereas a study with smaller sample size and statistically non-significant results could impact clinical practice. [14] Additionally, as previously mentioned, a non-significant finding may reflect the study design itself rather than relationships between variables.
Healthcare providers using evidence-based medicine to inform practice should use clinical judgment to determine the practical importance of studies through careful evaluation of the design, sample size, power, likelihood of type I and type II errors, data analysis, and reporting of statistical findings (p values, 95% CI or both). [4] Interestingly, some experts have called for "statistically significant" or "not significant" to be excluded from work as statistical significance never has and will never be equivalent to clinical significance. [17]
The decision on what is clinically significant can be challenging, depending on the providers' experience and especially the severity of the disease. Providers should use their knowledge and experiences to determine the meaningfulness of study results and make inferences based not only on significant or insignificant results by researchers but through their understanding of study limitations and practical implications.
Nursing, Allied Health, and Interprofessional Team Interventions
All physicians, nurses, pharmacists, and other healthcare professionals should strive to understand the concepts in this chapter. These individuals should maintain the ability to review and incorporate new literature for evidence-based and safe care.
Jones M, Gebski V, Onslow M, Packman A. Statistical power in stuttering research: a tutorial. Journal of speech, language, and hearing research : JSLHR. 2002 Apr:45(2):243-55 [PubMed PMID: 12003508]
Sedgwick P. Pitfalls of statistical hypothesis testing: type I and type II errors. BMJ (Clinical research ed.). 2014 Jul 3:349():g4287. doi: 10.1136/bmj.g4287. Epub 2014 Jul 3 [PubMed PMID: 24994622]
Fethney J. Statistical and clinical significance, and how to use confidence intervals to help interpret both. Australian critical care : official journal of the Confederation of Australian Critical Care Nurses. 2010 May:23(2):93-7. doi: 10.1016/j.aucc.2010.03.001. Epub 2010 Mar 29 [PubMed PMID: 20347326]
Hayat MJ. Understanding statistical significance. Nursing research. 2010 May-Jun:59(3):219-23. doi: 10.1097/NNR.0b013e3181dbb2cc. Epub [PubMed PMID: 20445438]
Ferrill MJ, Brown DA, Kyle JA. Clinical versus statistical significance: interpreting P values and confidence intervals related to measures of association to guide decision making. Journal of pharmacy practice. 2010 Aug:23(4):344-51. doi: 10.1177/0897190009358774. Epub 2010 Apr 13 [PubMed PMID: 21507834]
Infanger D, Schmidt-Trucksäss A. P value functions: An underused method to present research results and to promote quantitative reasoning. Statistics in medicine. 2019 Sep 20:38(21):4189-4197. doi: 10.1002/sim.8293. Epub 2019 Jul 3 [PubMed PMID: 31270842]
Dorey F. Statistics in brief: Interpretation and use of p values: all p values are not equal. Clinical orthopaedics and related research. 2011 Nov:469(11):3259-61. doi: 10.1007/s11999-011-2053-1. Epub [PubMed PMID: 21918804]
Liu XS. Implications of statistical power for confidence intervals. The British journal of mathematical and statistical psychology. 2012 Nov:65(3):427-37. doi: 10.1111/j.2044-8317.2011.02035.x. Epub 2011 Oct 25 [PubMed PMID: 22026811]
Tijssen JG, Kolm P. Demystifying the New Statistical Recommendations: The Use and Reporting of p Values. Journal of the American College of Cardiology. 2016 Jul 12:68(2):231-3. doi: 10.1016/j.jacc.2016.05.026. Epub [PubMed PMID: 27386779]
Spanos A. Recurring controversies about P values and confidence intervals revisited. Ecology. 2014 Mar:95(3):645-51 [PubMed PMID: 24804448]
Freire APCF, Elkins MR, Ramos EMC, Moseley AM. Use of 95% confidence intervals in the reporting of between-group differences in randomized controlled trials: analysis of a representative sample of 200 physical therapy trials. Brazilian journal of physical therapy. 2019 Jul-Aug:23(4):302-310. doi: 10.1016/j.bjpt.2018.10.004. Epub 2018 Oct 16 [PubMed PMID: 30366845]
Dorey FJ. In brief: statistics in brief: Confidence intervals: what is the real result in the target population? Clinical orthopaedics and related research. 2010 Nov:468(11):3137-8. doi: 10.1007/s11999-010-1407-4. Epub [PubMed PMID: 20532716]
Porcher R. Reporting results of orthopaedic research: confidence intervals and p values. Clinical orthopaedics and related research. 2009 Oct:467(10):2736-7. doi: 10.1007/s11999-009-0952-1. Epub 2009 Jun 30 [PubMed PMID: 19565303]
Gardner MJ, Altman DG. Confidence intervals rather than P values: estimation rather than hypothesis testing. British medical journal (Clinical research ed.). 1986 Mar 15:292(6522):746-50 [PubMed PMID: 3082422]
Cooper RJ, Wears RL, Schriger DL. Reporting research results: recommendations for improving communication. Annals of emergency medicine. 2003 Apr:41(4):561-4 [PubMed PMID: 12658257]
Doll H, Carney S. Statistical approaches to uncertainty: P values and confidence intervals unpacked. Equine veterinary journal. 2007 May:39(3):275-6 [PubMed PMID: 17520981]
Colquhoun D. The reproducibility of research and the misinterpretation of p-values. Royal Society open science. 2017 Dec:4(12):171085. doi: 10.1098/rsos.171085. Epub 2017 Dec 6 [PubMed PMID: 29308247]

Use the mouse wheel to zoom in and out, click and drag to pan the image
Nursing Research
- First Online: 24 January 2019
Cite this chapter
- Lars-Petter Jelsness-Jørgensen 3 , 4
1631 Accesses
Nurses play an increasingly active role in clinical research in IBD. By reviewing existing literature on the topic, this chapter provides a brief overview of some main concepts related to research in nursing. In addition, the chapter provides some general advice in relation to implementing evidence-based practice, as well as carrying out independent research.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Abrandt Dahlgren M, Higgs J, Richardson B (2004) Developing practice knowledge for health professionals. Butterworth-Heinemann, Edinburgh
Google Scholar
Bager P, Befrits R, Wikman O, Lindgren S, Moum B, Hjortswang H et al (2011) The prevalence of anemia and iron deficiency in IBD outpatients in Scandinavia. Scand J Gastroenterol 46(3):304–309
Article Google Scholar
Bager P, Befrits R, Wikman O, Lindgren S, Moum B, Hjortswang H et al (2012) Fatigue in out-patients with inflammatory bowel disease is common and multifactorial. Aliment Pharmacol Ther 35(1):133–141
Article CAS Google Scholar
Coenen S, Weyts E, Vermeire S, Ferrante M, Noman M, Ballet V et al (2017) Effects of introduction of an inflammatory bowel disease nurse position on the quality of delivered care. Eur J Gastroenterol Hepatol 29(6):646–650
Czuber-Dochan W, Ream E, Norton C (2013a) Review article: description and management of fatigue in inflammatory bowel disease. Aliment Pharmacol Ther 37(5):505–516
Czuber-Dochan W, Dibley LB, Terry H, Ream E, Norton C (2013b) The experience of fatigue in people with inflammatory bowel disease: an exploratory study. J Adv Nurs 69(9):1987–1999
Czuber-Dochan W, Norton C, Bassett P, Berliner S, Bredin F, Darvell M et al (2014a) Development and psychometric testing of inflammatory bowel disease fatigue (IBD-F) patient self-assessment scale. J Crohns Colitis 8(11):1398–1406
Czuber-Dochan W, Norton C, Bredin F, Darvell M, Nathan I, Terry H (2014b) Healthcare professionals’ perceptions of fatigue experienced by people with IBD. J Crohns Colitis 8(8):835–844
Dibley L, Norton C (2013) Experiences of fecal incontinence in people with inflammatory bowel disease: self-reported experiences among a community sample. Inflamm Bowel Dis 19(7):1450–1462
Dibley L, Bager P, Czuber-Dochan W, Farrell D, Jelsness-Jorgensen LP, Kemp K et al (2017) Identification of research priorities for inflammatory bowel disease nursing in Europe: a Nurses-European Crohn’s and Colitis Organisation Delphi Survey. J Crohns Colitis 11(3):353–359
PubMed Google Scholar
Dicenso A, Bayley L, Haynes RB (2009) Accessing pre-appraised evidence: fine-tuning the 5S model into a 6S model. Evid Based Nurs 12(4):99–101
Domecq JP, Prutsky G, Elraiyah T, Wang Z, Nabhan M, Shippee N et al (2014) Patient engagement in research: a systematic review. BMC Health Serv Res 14:89
Elwyn G, Edwards A, Thompson R (2016) Shared decision making in health care: achieving evidence-based patient choice, 3rd edn. Oxford University Press, Oxford
Book Google Scholar
Jaghult S, Larson J, Wredling R, Kapraali M (2007) A multiprofessional education programme for patients with inflammatory bowel disease: a randomized controlled trial. Scand J Gastroenterol 42(12):1452–1459
Jaghult S, Saboonchi F, Johansson UB, Wredling R, Kapraali M (2011) Identifying predictors of low health-related quality of life among patients with inflammatory bowel disease: comparison between Crohn’s disease and ulcerative colitis with disease duration. J Clin Nurs 20(11–12):1578–1587
Jelsness-Jorgensen LP (2015) Does a 3-week critical research appraisal course affect how students perceive their appraisal skills and the relevance of research for clinical practice? A repeated cross-sectional survey. Nurse Educ Today 35(1):e1–e5
Jelsness-Jorgensen LP, Moum B, Bernklev T (2011a) Worries and concerns among inflammatory bowel disease patients followed prospectively over one year. Gastroenterol Res Pract 2011:492034
Jelsness-Jorgensen LP, Bernklev T, Henriksen M, Torp R, Moum BA (2011b) Chronic fatigue is associated with impaired health-related quality of life in inflammatory bowel disease. Aliment Pharmacol Ther 33(1):106–114
Jelsness-Jorgensen LP, Bernklev T, Henriksen M, Torp R, Moum BA (2011c) Chronic fatigue is more prevalent in patients with inflammatory bowel disease than in healthy controls. Inflamm Bowel Dis 17(7):1564–1572
Jelsness-Jorgensen LP, Bernklev T, Henriksen M, Torp R, Moum B (2012a) Chronic fatigue is associated with increased disease-related worries and concerns in inflammatory bowel disease. World J Gastroenterol 18(5):445–452
Jelsness-Jorgensen LP, Bernklev T, Henriksen M, Torp R, Moum B (2012b) Is patient reported outcome (PRO) affected by different follow-up regimens in inflammatory bowel disease (IBD)? A one year prospective, longitudinal comparison of nurse-led versus conventional follow-up. J Crohns Colitis 6(9):887–894
Lindberg A, Ebbeskog B, Karlen P, Oxelmark L (2013) Inflammatory bowel disease professionals’ attitudes to and experiences of complementary and alternative medicine. BMC Complement Altern Med 13:349
Melnyk BM, Fineout-Overholt E, Stillwell SB, Williamson KM (2010) Evidence-based practice: step by step: the seven steps of evidence-based practice. Am J Nurs 110(1):51–53
Norton C, Dibley L (2013) Help-seeking for fecal incontinence in people with inflammatory bowel disease. J Wound Ostomy Continence Nurs 40(6):631–638; quiz E1-2
O’Connor M, Bager P, Duncan J, Gaarenstroom J, Younge L, Detre P et al (2013) N-ECCO consensus statements on the European nursing roles in caring for patients with Crohn’s disease or ulcerative colitis. J Crohns Colitis 7(9):744–764
Opheim R, Fagermoen MS, Bernklev T, Jelsness-Jorgensen LP, Moum B (2014a) Fatigue interference with daily living among patients with inflammatory bowel disease. Qual Life Res 23(2):707–717
Opheim R, Fagermoen MS, Jelsness-Jorgensen LP, Bernklev T, Moum B (2014b) Sense of coherence in patients with inflammatory bowel disease. Gastroenterol Res Pract 2014:989038
Oxelmark L, Magnusson A, Lofberg R, Hilleras P (2007) Group-based intervention program in inflammatory bowel disease patients: effects on quality of life. Inflamm Bowel Dis 13(2):182–190
Oxelmark L, Lindberg A, Lofberg R, Sternby B, Eriksson A, Almer S et al (2016) Use of complementary and alternative medicine in Swedish patients with inflammatory bowel disease: a controlled study. Eur J Gastroenterol Hepatol 28(11):1320–1328
Polit DF, Beck CT (2017) Nursing research: generating and assessing evidence for nursing practice, 10th edn. Wolters Kluwer, Philadelphia
Sackett DL, Rosenberg WM (1995) The need for evidence-based medicine. J R Soc Med 88(11):620–624
CAS PubMed PubMed Central Google Scholar
Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS (1996) Evidence based medicine: what it is and what it isn’t. BMJ (Clinical Research Ed) 312(7023):71–72
Williams B, Perillo S, Brown T (2015) What are the factors of organisational culture in health care settings that act as barriers to the implementation of evidence-based practice? A scoping review. Nurse Educ Today 35(2):e34–e41
Woodward S, Dibley L, Coombes S, Bellamy A, Clark C, Czuber-Dochan W et al (2016) Identifying disease-specific distress in patients with inflammatory bowel disease. Br J Nurs (Mark Allen Publishing) 25(12):649–660
Younge L, Norton C (2007) Contribution of specialist nurses in managing patients with IBD. Br J Nurs (Mark Allen Publishing) 16(4):208–212
Download references
Author information
Authors and affiliations.
Østfold University College, Department of Health Science, Halden, Norway
Lars-Petter Jelsness-Jørgensen
Østfold Hospital Trust, Department of Gastroenterology, Grålum, Norway
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Lars-Petter Jelsness-Jørgensen .
Editor information
Editors and affiliations.
DRK Kliniken Berlin Westend, Department of Gastroenterology, Berlin, Germany
Andreas Sturm
Gastroenterology Level 5, John Radcliffe Hospital, Oxford, UK
Lydia White
Rights and permissions
Reprints and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Jelsness-Jørgensen, LP. (2019). Nursing Research. In: Sturm, A., White, L. (eds) Inflammatory Bowel Disease Nursing Manual. Springer, Cham. https://doi.org/10.1007/978-3-319-75022-4_42
Download citation
DOI : https://doi.org/10.1007/978-3-319-75022-4_42
Published : 24 January 2019
Publisher Name : Springer, Cham
Print ISBN : 978-3-319-75021-7
Online ISBN : 978-3-319-75022-4
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Fastest Nurse Insight Engine
- MEDICAL ASSISSTANT
- Abdominal Key
- Anesthesia Key
- Basicmedical Key
- Otolaryngology & Ophthalmology
- Musculoskeletal Key
- Obstetric, Gynecology and Pediatric
- Oncology & Hematology
- Plastic Surgery & Dermatology
- Clinical Dentistry
- Radiology Key
- Thoracic Key
- Veterinary Medicine
- Gold Membership
Research Problems, Purposes, and Hypotheses
Chapter 5 Research Problems, Purposes, and Hypotheses Chapter Overview What Are Research Problems and Purposes? Identifying the Problem and Purpose in Quantitative, Qualitative, and Outcomes Studies Problems and Purposes in Types of Quantitative Studies Problems and Purposes in Types of Qualitative Studies Problems and Purposes in Outcomes Research Determining the Significance of a Study Problem and Purpose Influences Nursing Practice Builds on Previous Research Promotes Theory Testing or Development Addresses Nursing Research Priorities Examining the Feasibility of a Problem and Purpose Researcher Expertise Money Commitment Availability of Subjects, Facilities, and Equipment Ethical Considerations Examining Research Objectives, Questions, and Hypotheses in Research Reports Research Objectives or Aims Research Questions Hypotheses Understanding Study Variables and Research Concepts Types of Variables in Quantitative Research Conceptual and Operational Definitions of Variables in Quantitative Research Research Concepts Investigated in Qualitative Research Demographic Variables Key Concepts References Learning Outcomes After completing this chapter, you should be able to: 1. Identify research topics, problems, and purposes in published quantitative, qualitative, and outcomes studies. 2. Critically appraise the research problems and purposes in studies. 3. Critically appraise the feasibility of a study problem and purpose by examining the researcher’s expertise, money commitment, availability of subjects, facilities, and equipment, and the study’s ethical considerations. 4. Differentiate among the types of hypotheses (simple versus complex, nondirectional versus directional, associative versus causal, and statistical versus research) in published studies. 5. Critically appraise the quality of objectives, questions, and hypotheses presented in studies. 6. Differentiate the types of variables in studies. 7. Critically appraise the conceptual and operational definitions of variables in published studies. 8. Critically appraise the demographic variables measured and the sample characteristics described in studies. Key Terms Associative hypothesis, p. 149 Background for a problem, p. 131 Causal hypothesis, p. 149 Complex hypothesis, p. 150 Conceptual definition, p. 155 Confounding variables, p. 155 Demographic variables, p. 157 Dependent (outcome) variable, p. 153 Directional hypothesis, p. 150 Environmental variables, p. 154 Extraneous variables, p. 154 Feasibility of a study, p. 143 Hypothesis, p. 149 Independent (treatment or intervention) variable, p. 153 Nondirectional hypothesis, p. 150 Null hypothesis (H 0 ), p. 151 Operational definition, p. 155 Problem statement, p. 131 Research concepts, p. 156 Research hypothesis, p. 151 Research objective or aim, p. 145 Research problem, p. 131 Research purpose, p. 131 Research question, p. 147 Research topic, p. 130 Research variables, p. 154 Sample characteristics, p. 157 Significance of a research problem, p. 131 Simple hypothesis, p. 150 Statistical hypothesis, p. 151 Testable hypothesis, p. 152 Variables, p. 153 We are constantly asking questions to gain a better understanding of ourselves and the world around us. This human ability to wonder and ask creative questions is the first step in the research process. By asking questions, clinical nurses and nurse researchers are able to identify significant research topics and problems to direct the generation of research evidence for use in practice. A research topic is a concept or broad issue that is important to nursing, such as acute pain, chronic pain management, coping with illness, or health promotion. Each topic contains numerous research problems that might be investigated through quantitative, qualitative, and outcomes studies. For example, chronic pain management is a research topic that includes research problems such as “What is it like to live with chronic pain?” and “What strategies are useful in coping with chronic pain?” Qualitative studies have been conducted to investigate these problems or areas of concern in nursing ( Munhall, 2012 ). Quantitative studies have been conducted to address problems such as “What is the most accurate way to assess chronic pain?” and “What interventions are effective in managing chronic pain?” Outcomes research methodologies have been used to examine patient outcomes and the cost-effectiveness of care provided in chronic pain management centers ( Doran, 2011 ). The problem provides the basis for developing the research purpose. The purpose is the goal or focus of a study that guides the development of the objectives, questions, or hypotheses in quantitative and outcomes studies. The objectives, questions, or hypotheses bridge the gap between the more abstractly stated problem and purpose and the detailed design for conducting the study. Objectives, questions, and hypotheses include the variables, relationships among the variables, and often the population to be studied. In qualitative research, the purpose and broadly stated research questions guide the study of selected research concepts. This chapter includes content that will assist you in identifying problems and purposes in a variety of quantitative, qualitative, and outcomes studies. Objectives, questions, and hypotheses are discussed, and the different types of study variables are introduced. Also presented are guidelines that will assist you in critically appraising the problems, purposes, objectives, questions, hypotheses, and variables or concepts in published quantitative, qualitative, and outcomes studies. What Are Research Problems and Purposes? A research problem is an area of concern in which there is a gap in the knowledge needed for nursing practice. Research is required to generate essential knowledge to address the practice concern, with the ultimate goal of providing evidence-based nursing care ( Brown, 2014 ; Craig & Smyth, 2012 ). In a study, the research problem (1) indicates the significance of the problem, (2) provides a background for the problem, and (3) includes a problem statement. The significance of a research problem indicates the importance of the problem to nursing and health care and to the health of individuals, families, and communities. The background for a problem briefly identifies what we know about the problem area, and the problem statement identifies the specific gap in the knowledge needed for practice. Not all published studies include a clearly expressed problem, but the problem usually can be identified in the first page of the report. The research purpose is a clear, concise statement of the specific goal or focus of a study. In quantitative and outcomes studies, the goal of a study might be to identify, describe, or examine relationships in a situation, examine the effectiveness of an intervention, or determine outcomes of health care. In qualitative studies, the purpose might be to explore perceptions of a phenomenon, describe elements of a culture, develop a theory of a health situation or issue, or describe historical trends and patterns. The purpose includes the variables or concepts, the population, and often the setting for the study. A clearly stated research purpose can capture the essence of a study in a single sentence and is essential for directing the remaining steps of the research process. The research problem and purpose from the study of Piamjariyakul, Smith, Russell, Werkowitch, and Elyachar (2013) of the effectiveness of a telephone coaching program on heart failure home management by family caregivers are presented as an example. This example is critically appraised using the following guidelines. Critical Appraisal Guidelines Problems and Purposes in Studies 1. Is the problem clearly and concisely expressed early in the study? 2. Does the problem include the significance, background, and problem statement? 3. Does the purpose clearly express the goal or focus of the study? 4. Is the purpose focused on the study problem statement? 5. Are the study variables and population identified in the purpose? Research Example Problem and Purpose of a Quantitative Study Research Study Excerpt Problem Significance “Results of meta-analyses and American Heart Association (AHA) guidelines emphasize the critical importance of family caregivers’ involvement in home management of heart failure (HF). Family caregivers perform daily HF home management and provide essential support for patients in recognizing worsening symptoms (i.e., edema, shortness of breath; Riegel et al., 2009 ).” Piamjariyakul et al., 2013 , p. 32 Problem Background “Results of several studies have shown that HF rehospitalization is frequently precipitated by excess dietary sodium, inappropriate changes or reductions in taking prescribed medications, and respiratory infections, most of which family caregivers could help prevent if they were educated to be alert for these problems. . . . One intervention program found that a family partnership program on HF home care was helpful in adherence to diet with significant reductions in patients’ urine sodium ( Dunbar et al., 2005 ).” Piamjariyakul et al., 2013 , p. 32 Problem Statement “Yet, the few available studies on providing instruction for family caregivers are limited in content and lack guidance for implementing HF self-management strategies at home. . . . Also, in developing interventions that involve family caregivers, researchers need to measure caregiver outcomes (i.e., burden) to ensure that interventions do improve patient outcomes but do not have untoward negative impacts on the caregivers.” Piamjariyakul et al., 2013 , pp. 32-33 Research Purpose “The purpose of this study was to determine the feasibility and evaluate the helpfulness and costs of a coaching program for family caregiver HF home care management.” Piamjariyakul et al., 2013 , p. 33 Critical Appraisal Research Problem Piamjariyakul and colleagues (2013) presented a clear, concise research problem that had the relevant areas of (1) significance, (2) background, and (3) problem statement. HF is a significant, costly chronic illness to manage, and family caregivers are essential to the management process. A concise background of the problem was provided by discussing studies of the effects of caregivers on the outcomes of patients with HF. The discussion of the problem concluded with a concise problem statement that indicated the gap in the knowledge needed for practice and provided a basis for the study conducted by these researchers. Each problem provides the basis for generating a variety of research purposes and, in this study, the knowledge gap regarding the effectiveness of interventions on HF home management by family caregivers provides clear direction for the formulation of the research purpose. Research Purpose In a published study, the purpose frequently is reflected in the title of the study, stated in the study abstract, and restated after the literature review. Piamjariyakul and associates (2013) included the purpose of their study in all three places. The focus of this study was to examine the effectiveness of a telephone coaching program on HF home management (independent variable) on caregiving burden, confidence in providing HF care, preparedness, satisfaction, and program cost (dependent variables) for family caregivers (population). The purpose indicated the type of study conducted (quasi-experimental) and clearly identified the independent variable (telephone coaching program), population (patients with HF and their families), and setting (home). However, the dependent variables are not clearly identified in the study purpose but were discussed in the methods section of the study. The study purpose would have been strengthened by the inclusion of the dependent variables measured in this study. Implications for Practice The findings from the study by Piamjariyakul and co-workers (2013, p. 38) indicated that “The telephone coaching program was shown to reduce the caregiving burden and improve caregiver confidence and preparedness in HF home care management. . . . The cost for the program is considerably less than the cost for home healthcare providers ($120-160 per each visit), a single emergency department visit, or one inpatient hospitalization for HF due to poor HF home management.” This study has potential for use in practice to improve the quality of care provided to patients and families; however, the researchers did recognize the need for additional testing of the coaching program with a larger sample to determine its effectiveness. This type of study supports the Quality and Safety Education for Nurses ( QSEN, 2013 ; Sherwood & Barnsteiner, 2012 ) prelicensure competency to ensure safe, quality, and cost- effective health care that actively involves patients and families in this care process. Identifying the Problem and Purpose in Quantitative, Qualitative, and Outcomes Studies Quantitative, qualitative, and outcomes research approaches enable nurses to investigate a variety of research problems and purposes. Examples of research topics, problems, and purposes for different types of quantitative, qualitative, and outcomes studies are presented in this section. Problems and Purposes in Types of Quantitative Studies Example research topics, problems, and purposes for the different types of quantitative research (descriptive, correlational, quasi-experimental, and experimental) are presented in Table 5-1 . If little is known about a topic, researchers usually start with descriptive and correlational studies and progress to quasi-experimental and experimental studies as knowledge expands in an area. An examination of the problems and purposes in Table 5-1 will reveal the differences and similarities among the types of quantitative research. The research purpose usually reflects the type of study that was conducted ( Grove, Burns, & Gray, 2013 ). The purpose of descriptive research is to identify and describe concepts or variables, identify possible relationships among variables, and delineate differences between or among existing groups, such as males and females or different ethnic groups. Table 5-1 Quantitative Research Topics, Problems, and Purposes Type of Research Research Topic Research Problem and Purpose Descriptive research Hand hygiene (HH), HH opportunities, HH adherence, infection control, pediatric extended care facilities (ECFs), clinical and nonclinical caregivers Title of study: “Hand hygiene opportunities in pediatric extended care facilities” ( Buet et al., 2013, p. 72 ). Problem: “The population in pediatric ECFs [extended care facilities] is increasingly complex, and such children are at high risk of healthcare-associated infections (HAIs), which are associated with increased morbidity, mortality, resources use, and cost ( Burns et al., 2010 ) [problem significance]. . . . The Centers for Disease Control and Prevention (CDC) … and the World Health Organization ( WHO, 2009 ) have published evidence-based guidelines confirming the causal relationship between poor infection control practices, particularly hand hygiene (HH), and increased risk of HAIs [problem background]. However, most of the HH research has been focused in adult long term care facilities and acute care settings and findings from such studies are unlikely to be applicable to HH in pediatric ECFs given the different care patterns, including the relative distribution of different devices” [problem statement] ( Buet et al., 2013 , pp. 72-73). Purpose: “The purpose of this observational study was to assess the frequency and type of HH opportunities initiated by clinical (e.g., physicians and nurses) and non-clinical (e.g., parents and teachers) care givers, as well as evaluate HH adherence using the WHO’s ‘5 Moments for HH’ observation tool” ( Buet et al., 2013, p. 73 ). Correlational research Insulin resistance; anthropometric measurements (height, weight, body mass index [BMI], and waist circumference); systolic and diastolic blood pressure; laboratory values of lipids and triglycerides; and inflammatory marker high-sensitivity C-reactive protein (hsCRP) Title of study: “Biological correlates and predictors of insulin resistance among early adolescents” ( Bindler et al., 2013, p. 20 ). Problem: “Prevalence of obesity is at historic high levels among youth; for example, worldwide, obesity has doubled, and in developed countries, the numbers of youth who are overweight or obese have tripled in the last three decades ( WHO, 2011 ) [problem significance]. . . . Youth with obesity and insulin resistance (IR) are at increased risk of associated chronic conditions in adulthood, such as elevated blood pressure (BP), cardiovascular disease (CVD), type 2 diabetes, and several types of cancer ( Li et al., 2009 ) [problem background]. Despite the known relationships between IR and cardiometabolic factors, no study has yet examined the independent effects of these factors on a predictive model of IR among early adolescents” [problem statement] ( Bindler et al., 2013, pp. 20-21 ). Purpose: “Therefore, the purposes of this study among a group of early adolescents participating in the Teen Eating and Activity Mentoring in Schools (TEAMS) study were to describe the anthropometric and laboratory markers of the participants and to test the ability of these markers to predict risk of exhibiting IR” ( Bindler et al., 2013, p. 21 ). Quasi-experimental research Nurse-case-managed intervention, hepatitis A and B vaccine completion, sociodemographic factors, risk behaviors, and homeless adults Title of study: “Effects of a nurse-managed program on hepatitis A and B vaccine completion among homeless adults” ( Nyamathi et al., 2009, p. 13 ). Problem: “Hepatitis B virus (HBV) infection poses a serious threat to public health in the United States. Recent estimates place the true prevalence of chronic HBV in the United States at approximately 1.6 cases per 100,000 persons ( CDC, 2008 ). It is estimated that there were 51,000 new cases of HBV infection in 2005 ( Wasley et al., 2007 ), a financial burden reaching $1 billion annually. . . . Homeless populations are at particularly high risk of HBV infection due to high rates of unprotected sexual behavior and sharing of needles and other IDU [injection drug user] paraphernalia. Previous studies have reported that HBV infection rates among homeless populations range from 17% to 31% (i.e., from 17,000 to 31,000 per 100,000) compared with 2.1 per 100,000 in the general United States population [problem significance]. . . . Vaccination is the most effective way to prevent HBV infection ( CDC, 2006 ). . . . Improving vaccination adherence rates among homeless persons is an important step toward reducing the high prevalence of HBV infection in this population [problem background]. … Thus, little is known about adherence to HBV vaccination among community samples of urban homeless person[s] or about the effect of stronger interventions to incorporate additional strategies, such as nurse case management and targeted HBV education along with client tracking [problem statement]” ( Nyamathi et al., 2009, pp. 13-14 ). Purpose: The purpose of this study was to determine the “effectiveness of a nurse-case-managed intervention compared with that of two standard programs on completion of the combined hepatitis A virus (HAV) and HBV vaccine series among homeless adults and to assess sociodemographic factors and risk behaviors related to the vaccine completion” ( Nyamathi et al., 2009, p. 13 ). Experimental research Chronic widespread pain, aerobic exercise, analgesia, neurotrophin-3 synthesis, pain management, animal model Title of study: “Aerobic exercise alters analgesia and neurotrophin-3 [NT-3] synthesis in an animal model of chronic widespread pain” ( Sharma et al., 2010, p. 714 ). Problem: “Chronic widespread pain is complex and poorly understood and affects about 12% of the adult population in developed countries ( Rohrbeck et al., 2007 ) [problem significance]. . . . Management of chronic pain syndromes poses challenges for healthcare practitioners, and pharmacological interventions offer limited efficacy. . . . Exercise training has been long suggested to reduce pain and improve functional outcomes ( Whiteside et al., 2004 ) [problem background]. . . . Surprisingly, the current literature is mainly limited to human studies where the molecular basis for exercise training cannot be easily determined. Relatively few animal studies have addressed the effects and mechanisms of exercise on sensory modulation of chronic pain” [problem statement] ( Sharma et al., 2010, p. 715 ). Purpose: “The purpose of the present study was to examine the effects of moderate-intensity aerobic exercise on pain-like behavior and NT-3 in an animal model of widespread pain” ( Sharma et al., 2010, p. 714 ). Buet and co-workers (2013) conducted a descriptive study to identify the hand hygiene (HH) opportunities and adherence among clinical and nonclinical caregivers in extended pediatric care facilities. These researchers followed the World Health Organization “5 Moments for Hand Hygiene” ( WHO, 2009 ): before touching a patient, before clean or aseptic procedures, after body fluid exposure or risk, after touching a patient, and after touching patient surroundings. Researchers found that HH opportunities were numerous for clinical and nonclinical caregivers, but adherence to HH was low, especially for nonclinical individuals. This study supports the importance of HH in the delivery of quality, safe care based on current evidence-based guidelines ( Melnyk & Fineout-Overholt, 2011 ; QSEN, 2013 ). The purpose of correlational research is to examine the type (positive or negative) and strength of relationships among variables. In their correlational study, Bindler, Bindler, and Daratha (2013) examined the prediction of insulin resistance (IR) in adolescents using anthropometric measurements (height, weight, body mass index [BMI], and waist circumference), systolic and diastolic blood pressure, laboratory values [lipid and triglyceride levels], and the inflammatory marker of high-sensitivity, C-reactive protein (see Table 5-1 ). The researchers found that waist circumference and triglycerides were the strongest predictors of IR in adolescents. The findings from this study stressed the importance of nurses measuring waist circumference, height, and weight; calculating BMI; and examining lipid levels to identify youths at risk for IR. Quasi-experimental studies are conducted to determine the effect of a treatment or independent variable on designated dependent or outcome variables ( Shadish, Cook, & Campbell, 2002 ). Nyamathi and colleagues (2009) conducted a quasi-experimental study to examine the effectiveness of a nurse case-managed intervention on hepatitis A and B vaccine completion among homeless adults. The research topics, problem, and purpose for this study are presented in Table 5-1 . The findings from this study “revealed that a culturally sensitive comprehensive program, which included nurse case management plus targeted hepatitis education, incentives, and client tracking, performed significantly better than did a usual care program” ( Nyamathi et al., 2009 , p. 21). Thus the researchers recommended that public health program planners and funders use this type of program to promote increased completion of hepatitis A and B vaccinations for high-risk groups. Experimental studies are conducted in highly controlled settings, using a highly structured design to determine the effect of one or more independent variables on one or more dependent variables ( Grove et al., 2013 ). Sharma, Ryals, Gajewski, and Wright (2010) conducted an experimental study to determine the effects of an aerobic exercise program on pain like behaviors and neurotrophin-3 synthesis in mice with chronic widespread pain (see Table 5-1 ). These researchers found that moderate-intensity aerobic exercise had the effect of deep tissue mechanical hyperalgesia on chronic pain in mice. This finding provides a possible molecular basis for aerobic exercise training in reducing muscular pain in fibromyalgia patients. Problems and Purposes in Types of Qualitative Studies The problems formulated for qualitative research identify areas of concern that require investigation to gain new insights, expand understanding, and improve comprehension of the whole ( Munhall, 2012 ). The purpose of a qualitative study indicates the focus of the study, which may be a concept such as pain, an event such as loss of a child, or a facet of a culture such as the healing practices of a specific Native American tribe. In addition, the purpose often indicates the qualitative approach used to conduct the study. The basic assumptions for this approach are discussed in the research report ( Creswell, 2014 ). Examples of research topics, problems, and purposes for the types of qualitative research—phenomenological, grounded theory, ethnographic, exploratory-descriptive, and historical—commonly found in nursing are presented in Table 5-2 . Table 5-2 Qualitative Research Topics, Problems, and Purposes Type of Research Research Topic Research Problem and Purpose Phenomenological research Lived experience of children, asthma, health promotion, child health, chronic illness, fears of exacerbations, fears of being ostracized Title of study: “Children’s experiences of living with asthma: Fear of exacerbations and being ostracized” ( Trollvik et al., 2011, p. 295 ). Problem: “Asthma is the most common childhood disease and long-term medical condition affecting children ( Masoli et al., 2004 ). The prevalence of asthma is increasing, and atopic diseases are considered to be a worldwide health problem and an agent of morbidity in children significance]. . . . Studies show that children with asthma have more emotional/behavioral problems than healthy children… It has also been found that asthma control in children is poor and that healthcare professionals (HCPs) and children focus on different aspects of having asthma ( Price et al., 2002 ) [problem background]. . . . Few studies have considered very young children’s, 7-10 years old, perspectives; this study might contribute to new insights into their lifeworld experiences” [problem statement] ( Trollvik et al., 2011, pp. 295-296 ). Purpose: “The aim of this study was to explore and describe children’s everyday experiences of living with asthma to tailor an Asthma Education Program based on their perspectives. . . . In this study, a phenomenological and hermaneutical approach was used to gain an understanding of the children’s lifeworld” ( Trollvik et al., 2011 , p. 296). Grounded theory research Foster care, pregnancy prevention, prevention of sexually transmitted infections, patient-provider relationship Title of study: “Where do youth in foster care receive information about preventing unplanned pregnancy and sexually transmitted infections [STIs]” ( Hudson, 2012, p. 443 ). Problem: “Within the United States, approximately 460,000 children live in foster care, and adolescents comprise half of this population. . . . Children enter the foster care system as a result of sexual abuse, physical abuse, or physical neglect and abandonment ( Child Welfare League of America, 2007 ) [problem significance]. . . . With limited access to health promotion information and education about high-risk sexual behavior, it is not surprising that these young people have a high incidence of unplanned pregnancy and STIs compared with youth not in foster care [problem background]. Little research exists on the extent to which foster youth receive information about sexual activity from healthcare providers” [problem statement] ( Hudson, 2012, p. 443-444 ). Purpose: A grounded theory study was conducted to “describe how and where foster youth receive reproductive health and risk reduction information to prevent pregnancy and sexually transmitted infections. Participants also were asked to describe their relationship with their primary healthcare provider while they were in foster care” ( Hudson, 2012, p. 443 ). Ethnographic research Critical illness, mechanical ventilation, weaning, family presence, surveillance Title of study: “Family presence and surveillance during weaning from prolonged mechanical ventilation” ( Happ et al., 2007, p. 47 ). Problem: “During critical illness, mechanical ventilation imposes physical and communication barriers between family members and their critically ill loved ones [problem signicance]. . . . Most studies of family members in the intensive care unit (ICU) have focused on families’ needs for information, access to the patient, and participation in decisions to withdraw or withhold life-sustaining treatment. … Although numerous studies have been conducted of patient experiences with short- and long-term mechanical ventilation (LTMV), research has not focused on family interactions with patients during weaning from mechanical ventilation [problem background]. Moreover, the importance of family members’ bedside presence and clinicians’ interpretation of family behaviors at the bedside have not been critically examined” [problem statement] ( Happ et al., 2007, pp. 47-48 ). Purpose: “With the use of data from an ethnographic study of the care and communication processes during weaning from LTMV, we sought to describe how family members interact with the patients and respond to the ventilator and associated ICU bedside equipment during LTMV weaning” ( Happ et al., 2007, p. 48 ). Exploratory-descriptive qualitative research Intimate partner violence, abuse of spouse, supporting mothering, parent-child relationships, family health, providers’ perspective, social support Title of study: “Supporting mothering: Service providers’ perspectives of mothers and young children affected by intimate partner violence” ( Letourneau et al., 2011, p. 192 ). Problem: “Estimates of the percent of women with exposure to intimate partner violence (IPV) over their lifetimes by husbands, partners, or boyfriends range between 8% and 66%. . . . The high concentration of preschool-age children in households where women experience IPV… is a major concern [problem significance]. . . . Indeed, preschool-age children exposed to IPV may share many of the adjustment difficulties experienced by victims of direct physical and psychological abuse ( Litrownik et al., 2003 ) [problem background]. The degree to which children from birth to 36 months of age are affected by IPV, however, is not well understood. Even less is known of effective services and supports that target mothers and their young children exposed to IPV” [problem statement] ( Letourneau et al., 2011, p. 193 ). Purpose: “We conducted a qualitative descriptive study of service providers’ understandings of the impact of IPV on mothers, young children (birth to 36 months), and mother-infant/child relationships, and of the support needs of these mothers and young children” ( Letourneau et al., 2011, p. 192 ). Historical research Health disparities, childhood obesity, historical exemplar, prevention of infant mortality, public health nurses’ role Title of study: “Nurses’ role in the prevention of infant mortality in 1884-1925: Health disparities then and now ( Thompson & Keeling, 2012, p. 471 ). Problem: “Over the past several years, health policy makers have directed increased attention to issues of health disparities, an issue that has concerned the nursing profession for over a century[problem significance]. . . . Reutter and Kushner (2010) advocate that addressing health inequities are well within the nursing mandate and yet is an underutilized role [problem background]. . . . Nursing historical research lends insight into the complex health issues that nurses face today and may guide policy and nursing practice [problem statement]” ( Thompson & Keeling, 2012, p. 471 ). Purpose: The purpose of this historical study “was to evaluate the public health nurses’ (PHNs’) role with infant mortality during 1884-1925, specifically how nursing care impacted on conditions of poverty, poor nutrition, poor living conditions, lack of education, and lack of governmental policies that contributed to the poor health of infants a century ago” ( Thompson, & Keeling, 2012, p. 471 ). Phenomenological research is conducted to promote a deeper understanding of complex human experiences as they have been lived by the study participants ( Munhall, 2012 ). Trollvik, Nordbach, Silen, and Ringsberg (2011) conducted a phenomenological study to describe children’s experiences of living with asthma. The research topics, problem, and purpose for this study are presented in Table 5-2 . Findings from this study described two themes with five subthemes (identified in parentheses): fear of exacerbation (body sensations, frightening experiences, and loss of control) and fear of being ostracized (experiences of being excluded and dilemma of keeping the asthma secret or being open about it). The findings from this study emphasize that asthma management is not only a major issue for the children involved but also for their parents, teachers, and healthcare providers. Asthma educational programs need to be tailored to the individual child based on her or his perspectives and needs. This type of knowledge provides direction for accomplishing the QSEN (2013) competencies of providing patient-centered care. In grounded theory research, the problem identifies the area of concern and the purpose indicates the focus of the theory to be developed to account for a pattern of behavior of those involved in the study ( Wuest, 2012 ). For example, Hudson (2012, p. 443) conducted a grounded theory study to “describe how and where foster youth receive reproductive health and risk reduction information to prevent pregnancy and sexually transmitted infections (STIs)” (see Table 5-2 ). The following three thematic categories emerged from this study: “(a) discomfort visiting and disclosing, (b) receiving and not receiving the bare essentials, and (c) learning from community others” ( Hudson, 2012 , p. 445). The implications for practice were that primary care providers needed to provide time and confidential space for foster youths to disclose their sexual activities, and they (foster youths) need to receive more reproductive and risk prevention information from their school settings. In ethnographic research, the problem and purpose identify the culture and specific attributes of the culture that are to be examined, described, analyzed, and interpreted to reveal the social actions, beliefs, values, and norms of the culture ( Wolf, 2012 ). Happ, Swigart, Tate, Arnold, Sereika, and Hoffman (2007) conducted an ethnographic study of family presence and surveillance during weaning of their family member from a ventilator. Table 5-2 includes the research topics, problem, and purpose of this study. They concluded that “this study provided a potentially useful conceptual framework of family behaviors with long-term critically ill patients that could enhance the dialogue about family-centered care and guide future research on family presence in the intensive care unit” ( Happ et al., 2007 , p. 47). Exploratory-descriptive qualitative research is being conducted by several qualitative researchers to describe unique issues, health problems, or situations that lack clear description or definition. This type of research often provides the basis for future qualitative and quantitative research ( Creswell, 2014 ; Grove et al., 2013 ). Letourneau, Young, Secco, Stewart, Hughes, and Critchley (2011) conducted an exploratory-descriptive qualitative study of service providers’ understandings of the impact of intimate partner violence (IPV) on mothers and their young children to determine their needs for support (see Table 5-2 ). They found that these mothers and their children require more support than is currently available. In addition, the service providers had difficulty identifying interventions to promote and protect them and their children. The problem and purpose in historical research focus on a specific individual, characteristic of society, event, or situation in the past and usually identify the time period in the past that was examined by the study ( Lundy, 2012 ). For example, Thompson and Keeling (2012) examined the role of the public health nurse (PHN) in the prevention of infant mortality from 1884 to 1925 (see Table 5-2 ). They emphasized that studying the past role of PHNs and the health disparities then and now would increase our understanding of current nursing practice with regard to childhood health issues. They provided the following suggestions for nursing practice: “focus on health disparities in childhood obesity, in areas of environmental and policy change, and the development of social programs and education for families to support healthier living” ( Thompson & Keeling, 2012 , p. 471). Problems and Purposes in Outcomes Research Outcomes research is conducted to examine the end results of care ( Doran, 2011 ). This is a growing area of research in nursing to examine the relationships between the nursing process of care and patient outcomes. Table 5-3 includes the topics, problem, and purpose from an outcomes study by Ausserhofer and associates (2013) , who explored the relationship between patient safety climate (PSC) and selected patient outcomes in Swiss acute care hospitals. The adverse events or outcomes examined were medication errors, patient falls, pressure ulcers, and healthcare-associated infections that are common problems in U.S. hospitals ( Institute of Medicine, 2004 ). This study was guided by a common outcomes framework that focused on structure or work system, process of care, and patient outcomes (see Chapter 14 ). These researchers did not find a significant relationship of PSC to the selected patient outcomes. However, they stressed the need for additional research in this area and for selecting more reliable outcome measures. Table 5-3 Outcomes Research Topics, Problem, and Purpose Type of Research Research Topic Research Problem and Purpose Outcomes research Work system of patient safety climate (PSC) Process of care of nurses, workload work, and patient needs Outcomes of adverse events and patient satisfaction Title of study: “The association of patient safety climate and nurse-related organizational factors with selected patient outcomes: A cross-sectional survey” Ausserhofer et al., 2013, p. 240 ). Problem: “Today’s patient care in healthcare organizations is anything but safe, as between 2.9% and 16.6% of hospitalized patients are affected by adverse events such as medication errors, healthcare-associated infection, or patient falls. More than one-third of adverse events lead to temporary (34%) or permanent disability (6-9%) and between 3% and 20.8% of the patients experiencing an adverse event die [problem significance]. . . . As 37-70% of all adverse events are considered preventable, . . . harmful impacts on patients, such as psychological trauma, impaired functionality or loss of trust in the healthcare system as well as socio-economic costs, could be avoided ( Institute of Medicine, 2004 ). . . . Patient safety climate (PSC) is an important work environment factor determining patient safety and quality of care in healthcare organizations [problem background]. Few studies have investigated the relationship between PSC and patient outcomes, considering possible confounding effects of other nurse-related organizational factors [problem statement]” ( Ausserhofer et al., 2013, pp. 240-241 ). Purpose: “The purpose of this study was to explore the relationship between PSC and selected patients outcomes in Swiss acute care hospitals” ( Ausserhofer et al., 2013, p. 242 ).
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:
- Outcomes Research
- Understanding Statistics in Research
- Clarifying Quantitative Research Designs
- Examining Populations and Samples in Research
Stay updated, free articles. Join our Telegram channel
Comments are closed for this page.

Full access? Get Clinical Tree

- Open access
- Published: 13 May 2024
From incivility to outcomes: tracing the effects of nursing incivility on nurse well-being, patient engagement, and health outcomes
- Nourah Alsadaan ORCID: orcid.org/0000-0001-7285-0184 1 ,
- Osama Mohamed Elsayed Ramadan ORCID: orcid.org/0000-0002-9616-8590 1 &
- Mohammed Alqahtani 2
BMC Nursing volume 23 , Article number: 325 ( 2024 ) Cite this article
212 Accesses
1 Altmetric
Metrics details
Nursing incivility, defined as disrespectful behaviour toward nurses, is increasingly recognized as a pressing issue that affects nurses’ well-being and quality of care. However, research on the pathways linking incivility to outcomes is limited, especially in Saudi hospitals. Methods: This cross-sectional study examined relationships between perceived nursing incivility, nurse stress, patient engagement, and health outcomes in four Saudi hospitals. Using validated scales, 289 nurses and 512 patients completed surveys on exposure to incivility, stress levels, activation, and medication adherence. The outcomes included readmissions at 30 days and satisfaction. Results: More than two-thirds of nurses reported experiencing moderate to severe workplace incivility. Correlation and regression analyzes revealed that nursing incivility was positively associated with nursing stress. An inverse relationship was found between stress and patient participation. Serial mediation analysis illuminated a detrimental cascade, incivility contributing to increased nurse stress, subsequently diminishing patient engagement, ultimately worsening care quality. Conclusions The findings present robust evidence that nursing incivility has adverse ripple effects, directly impacting nurse well-being while indirectly affecting patient outcomes through reduced care involvement. Practical implications advocate for systemic interventions focused on constructive nursing cultures and patient empowerment to improve both healthcare provider conditions and quality of care. This study provides compelling information to inform policies and strategies to mitigate workplace mistreatment and encourage participation among nurses and patients to improve health outcomes.
Peer Review reports
Introduction
Nursing, a cornerstone of the healthcare system, plays an indispensable role in patient care and the broader health landscape [ 1 , 2 ]. This noble profession encompasses not only the administration of treatments and medications but also the provision of emotional support and education to patients and their families [ 3 , 4 ]. Nurses are often the primary point of contact for patients, which makes their role crucial in shaping patient experiences and outcomes [ 5 ]. The diverse responsibilities, from bedside care to patient advocacy, emphasize the multifaceted nature of nursing and its critical impact on the delivery of healthcare [ 6 , 7 ]. The work environment in which nurses work is crucial for both their well-being and their ability to provide quality care [ 6 , 8 ]. A positive and supportive environment not only improves job satisfaction and retention among nurses but also directly influences patient safety and quality of care [ 9 , 10 ]. Factors such as teamwork, communication, and organizational culture play an important role in shaping this environment [ 11 ]. In contrast, negative elements within the workplace can lead to burnout, decreased job satisfaction, and potentially compromise patient care [ 12 ].
Nursing incivility, an increasingly distressing concern, encompasses disrespectful behaviours [ 13 ], that violate workplace dignity norms ranging from subtle belittling to overt hostility [ 2 , 8 ]. This widespread phenomenon permeates most healthcare settings [ 14 , 15 ], with up to 85% of nurses encountering this mistreatment from various sources [ 16 ], resulting in a significantly disruptive organizational climate [ 17 ]. Beyond affecting nurse well-being through adverse psychological impacts, incivility breeds poor morale, compromised performance, increased attrition, and, critically, reduced quality of patient care [ 18 , 19 , 20 ]. Prioritizing healthy collegial environments remains crucial for upholding both nurse wellness and optimal patient outcomes [ 21 , 22 , 23 ]. Furthermore, organizational factors, such as leadership, communication, and workplace culture, may play a significant role in shaping the dynamics of nursing incivility, stress, and patient outcomes [ 24 , 25 ]. Investigating these factors could provide a more comprehensive understanding of the complex interplay between individual and systemic elements in the healthcare setting [ 26 , 27 ]. Nursing incivility can manifest itself in various forms, including, but not limited to, belittling comments, bullying, gossip, and exclusionary tactics [ 11 , 28 ]. These behaviours can originate from colleagues, superiors, patients, and their families [ 16 , 29 ]. Such conduct not only undermines professional relationships [ 30 ] but also can cause psychological distress for victims, preventing their ability to perform effectively [ 31 , 32 ].
Although the prevalence and nature of incivility in nursing have been well documented, there remains a significant gap in understanding its full impact [ 33 , 34 ]. The impact of nursing incivility extends beyond the immediate targets, affecting multiple aspects of healthcare delivery [ 35 , 36 ]. Incivility can have profound emotional consequences for nurses, leading to increased stress, burnout, and job dissatisfaction, which can compromise their ability to provide high-quality patient care [ 8 , 19 , 29 ]. Moreover, uncivil behaviors can strain nurse-patient interactions, potentially diminishing the quality of care and patient satisfaction [ 18 , 37 ]. At an organizational level, incivility can disrupt team dynamics, contribute to higher staff turnover rates, and negatively influence the overall culture within healthcare institutions [ 18 , 38 , 39 ]. Furthermore, the economic implications of nursing incivility, such as costs associated with staff replacement and lost productivity due to absenteeism and presenteeism, warrant further investigation [ 40 , 41 , 42 ]. Examining these multifaceted impacts is crucial for developing targeted interventions and policies to mitigate the detrimental effects of incivility on nurses, patients, and healthcare organizations [ 43 , 44 ].
Current literature has primarily focused on identifying forms and instances of uncivil behavior, often overlooking their deeper implications for nurses, patients, and healthcare systems. An underexplored area is the direct effect of incivility on nurses’ well-being [ 8 ]. This includes quantifying the emotional and professional toll, such as stress, burnout, and job dissatisfaction [ 31 ], which are crucial factors influencing nurse retention and mental health [ 45 , 46 ].
In summary, filling these gaps through robust empirical research is crucial. Such research is essential not only to transform current anecdotal and observational understandings into data-driven insights but also to develop effective strategies to mitigate the negative impacts of incivility [ 47 , 48 ]. These insights are vital to promoting a healthier, more respectful, and efficient healthcare environment, ultimately enhancing nurses’ well-being and patient care quality [ 3 , 5 ]. The primary objective of this study was to investigate the impact of nursing incivility on critical aspects of healthcare care delivery. By focusing on nurse stress, patient engagement, and health outcomes (defined as 30-day readmission rates and patient satisfaction scores), the study aimed to understand how incivility in the nursing environment affects both healthcare providers and recipients.
The study was conducted within the context of the Saudi healthcare system, which has undergone significant reforms in recent years [ 49 , 50 ]. The system is primarily government-funded, with a growing private-sector presence [ 51 ]. It aims to provide universal access to healthcare services for all citizens and residents, with a focus on improving quality and efficiency [ 52 ]. However, like many healthcare systems worldwide [ 53 , 54 ], it faces challenges related to workforce development, patient satisfaction, and the management of complex health conditions [ 55 ]. Understanding the impact of nursing incivility within this context is crucial for informing strategies to enhance the well-being of healthcare providers and the quality of patient care.
This study examined nurse stress, a direct consequence of incivility, and its subsequent effects on patient care. Additionally, it explored how incivility in nursing influenced patient participation, a crucial factor in successful health outcomes. Finally, the study assessed the broader implications of these variables on overall health outcomes, providing valuable insights for healthcare policy and practice.
This study’s findings can influence nursing practice and patient care significantly. By demonstrating the tangible impacts of nursing incivility, the study can inform the development of targeted interventions and policies to create a more respectful and supportive work environment for nurses. This, in turn, can lead to improved patient care and outcomes. Highlighting the importance of a respectful and supportive nursing environment is a key outcome of this study. By underscoring the detrimental effects of incivility, the research advocates for a cultural shift in healthcare settings toward more positive and collaborative interactions. These changes are vital for nurses’ well-being, patient care quality, and healthcare organizations’ overall effectiveness.
Materials and methods
Research objectives & research hypothesis.
Examine the relationships between nursing incivility, nurse stress (defined as emotional exhaustion and depersonalization), patient engagement (defined by patient activation levels and adherence to discharge protocols), and health outcomes (defined as 30-day readmission rates and patient satisfaction scores). H1a: Higher levels of nursing incivility will be positively associated with increased nurse stress. H1b: Higher levels of nurse stress will be negatively associated with patient engagement. H1c: Lower levels of patient engagement will be associated with poorer health outcomes.
Investigate how different perceived levels and types of nursing incivility, including overt (bullying, verbal abuse) and covert (gossip, exclusion) behaviours frequently reported by nurses, affect nurse stress and emotional exhaustion through a cross-sectional survey methodology.
H2a: Overt forms of nursing incivility will have a stronger positive association with nurse stress compared to covert forms of incivility. Overt forms of nursing incivility refer to more explicit and direct forms of uncivil behaviour, such as verbal abuse, bullying, or intimidation. Covert forms of nursing incivility refer to more subtle and indirect forms of uncivil behaviour, such as gossip, exclusion, or undermining actions.
H2b: A higher frequency of exposure to nursing incivility will be associated with higher levels of nurse stress and emotional exhaustion.
Evaluate how nursing incivility, nurse stress, and patient engagement (activation and adherence) impact patient health outcomes (30-day readmissions and satisfaction), mapping the relationships between these variables using multivariate regression techniques. H3a: Nursing incivility will have a direct negative effect on patient health outcomes. H3b: Nurse stress will mediate the relationship between nursing incivility and patient health outcomes. H3c: Patient engagement will mediate the relationship between nurse stress and patient health outcomes. H3d: The combined indirect effects of nurse stress and patient engagement will partially mediate the relationship between nursing incivility and patient health outcomes.
These hypothesized relationships form the conceptual foundation of our study, guiding our investigation into the complex interplay between nursing incivility, nurse well-being, patient engagement, and healthcare outcomes. By examining these relationships, we aim to provide insights into the potential cascading effects of uncivil behaviours in the nursing workplace and their ultimate impact on patient care. Figure 1 illustrates the hypothesized relationships between nursing incivility, nurse stress, patient engagement, and health outcomes. As depicted in Fig. 1 , we hypothesize that nursing incivility directly influences nurse stress and patient engagement. In turn, nurse stress is expected to have an indirect effect on health outcomes, mediated by patient engagement. Additionally, we anticipate that patient engagement directly impacts health outcomes, which are operationalized as readmission rates and patient satisfaction.
The arrows in Fig. 1 are used to represent the relationships and directional hypotheses between the constructs mentioned: Nursing Incivility, Nurse Stress, Patient Engagement, and Health Outcomes. Here’s how the arrows correspond to each hypothesis:
Solid Arrows indicate a direct relationship in the primary sequence of effects :
H1a: Nursing Incivility → Nurse Stress.
H1b: Nurse Stress → Patient Engagement.
H1c: Patient Engagement → Health Outcomes
Dashed Arrows represent different types of incivility (overt and covert) and their effect on Nurse Stress :
H2a: Nursing Incivility (Overt) → Nurse Stress.
H2b: Nursing Incivility (Covert) → Nurse Stress.
Dotted Arrows show both direct and mediated paths for complex relationships :
H3a: Direct effect from Nursing Incivility → Health Outcomes.
H3b: Mediated effect through Nurse Stress.
H3c: Mediated effect through Patient Engagement.
H3d: Combined mediation through Nurse Stress and Patient Engagement leading to Health Outcomes.
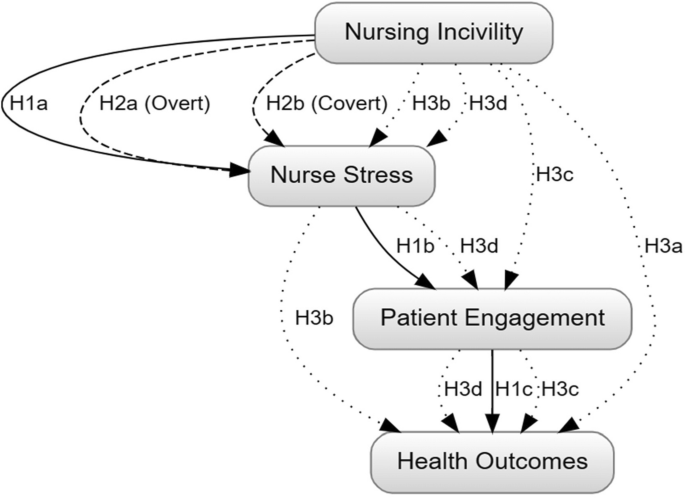
Hypothesized relationships between nursing incivility, nurse stress, patient engagement, and health outcomes
This study employed a cross-sectional correlational design to explore the relationships between nursing incivility, nurse stress, patient engagement, and health outcomes. This design involved collecting data from a defined population of nurses and patients in acute care settings simultaneously. This approach allows us to examine the associations between variables without actively manipulating any of them, providing a snapshot of the current state of these relationships.
The study was conducted in four hospitals located in the northwest region of Saudi Arabia. The participating hospitals are large, general medical and surgical facilities, with bed capacities ranging from 200 to 500. They provide a wide range of services, including inpatient and outpatient care, emergency services, critical care units, and specialized departments such as maternity, paediatrics, and mental health treatment. The patient population served by these hospitals is diverse, encompassing individuals seeking acute care for various medical conditions as well as those managing chronic illnesses such as diabetes, cardiovascular diseases, and respiratory disorders. The hospitals cater to both urban and rural communities within the northwest region. The nursing staff in these hospitals comprises a combination of Saudi and expatriate nurses, with varying levels of experience and educational qualifications. It is important to note that the findings of this study are specifically relevant to the northwest region of Saudi Arabia and may not be generalizable to other regions or healthcare settings. The unique cultural and socioeconomic characteristics of this region should be considered when interpreting the results and their implications for nursing practice and patient care.
Participant sample size determination
We calculated sample sizes for the nurse and patient groups to ensure statistical validity and practicality in our cross-sectional study. For the 289 nurses, we conducted a power analysis using a moderate effect size, 80% power, and a 0.05 alpha level, following the guidelines of Cohen (2013) on power analysis for behavioural sciences [ 56 ]. Although a small effect size might initially seem appropriate given the significant knowledge gap addressed by our study, the moderate effect size was chosen to maintain a balance between sensitivity and feasibility. This decision was particularly influenced by the practical challenges associated with securing a large enough sample to detect small effects within the logistical and resource constraints of our study setting. The moderate effect size was deemed most appropriate given the limited existing research on the specific relationships between nursing incivility, nurse stress, patient engagement, and health outcomes within the Saudi Arabian context, as highlighted in the introduction. Additionally, we accounted for potential variability and non-response rates for healthcare research, as suggested by Davern (2013).
The patient group required a larger sample size of 512 to accommodate greater variability and enable subgroup analyses. Patients were selected using a combination of random sampling and voluntary participation. Initially, a random sample of patients was drawn from the patient records of the participating hospitals, ensuring a representative mix of demographics, diagnoses, and hospital units. These patients were then invited to participate in the study voluntarily, which aimed to minimize selection bias while ensuring patient autonomy.
This approach also adhered to the standard power analysis methods [ 56 ] and included an upward adjustment for expected variability in patient responses, as recommended by Hulley et al. (2013) in their guidelines for clinical research [ 57 ]. Both sample sizes were further validated for feasibility within our resource constraints and specific healthcare settings, aligning with the practical considerations outlined by [ 58 ] in planning health research. In summary, the sample sizes of 289 nurses and 512 patients were determined using established statistical methods and customized to the unique aspects of our study, ensuring adequate power for reliable results. The selection process for both nurses and patients aimed to balance representativeness, statistical power, and ethical considerations, with patient selection particularly focused on combining random sampling with voluntary participation.
Eligibility criteria
Inclusion criteria.
Participants selected for this study were required to meet several conditions. First, they had to be registered nurses actively employed full-time, working ≥ 30 h per week, at one of the four identified healthcare hospitals. Their experience in the current institution should have spanned a minimum of six months. Furthermore, only those who could and were willing to provide informed consent were considered. Language proficiency was also crucial; Participants had to be fluent in Arabic or English to ensure they understood and completed the survey accurately. Lastly, the age bracket for eligible nurses was established between 25 and 60 years. Additionally, eligible participants must participate in direct patient care activities at least 10 h per week.
Exclusion criteria
Several factors led to the exclusion of potential participants from this study. Nurses who were currently not in active service, perhaps due to long-term leave or sabbatical, were not considered. We also considered the health aspect; nurses who self-declared cognitive impairments or mental health problems that could influence the accuracy of their responses were excluded. Nurses who had participated in a similar study or survey related to the topic in the last 6 months were excluded from this research. This exclusion criterion was implemented to minimize the potential influence of recent exposure to similar research questions or interventions on participants’ responses. By ensuring that a sufficient washout period had passed since any previous participation in related studies, we aimed to reduce the risk of response bias and enhance the validity of the collected data. This criterion contributes to the study’s rigour by minimizing the potential confounding effects of prior research experiences and promoting the collection of more independent and unbiased responses from participants.
Data collection tools
In this study, we employed the following validated instruments to measure the key variables, aligning with our research objectives and hypotheses:
Nursing incivility scale (NIS)
The Nursing Incivility Scale (NIS) is a quantitative instrument comprising 43 items designed to measure the frequency of perceived incivility from various sources, including patients, supervisors, coworkers, and physicians, over the preceding six months [ 59 ]. The NIS includes subscales that assess various sources of incivility, such as from nurses, supervisors, physicians, and patients. The items within these subscales capture both overt and covert forms of incivility, allowing for an assessment of the frequency and severity of each type of uncivil behaviour [ 60 ].
It employs a 5-point Likert scale ranging from “Never” to “Daily” and encompasses five subscales addressing different sources of incivility: nurses, the general workplace, supervisors, physicians, and patients The Nursing Incivility Scale (NIS) doesn’t provide a direct score but rather collects data on the frequency of uncivil behaviours experienced by nurses [ 60 , 61 ]. The NIS has demonstrated excellent internal reliability (Cronbach’s α > 0.90 across subscales) [ 56 ], and validity, making it well-suited for exploring the correlation between nursing incivility and nurse stress. Higher scores on the NIS subscales indicate a higher frequency of exposure to various forms of incivility from different sources.
Perceived stress scale (PSS)
The Perceived Stress Scale (PSS) is a 10-item self-report questionnaire that evaluates an individual’s stress appraisal over the preceding month, with a particular emphasis on predictability, control, and overload [ 62 ]. It employs a 5-point Likert scale ranging from “Never” to “Very Often.” The total PSS score typically ranges from 0 to 40 (assuming a 4-point scale), with higher scores indicating greater perceived stress and emotional exhaustion. A common interpretation guide categorizes scores as follows: 0–13 for low stress, 14–26 for moderate stress, and 27–40 for high perceived stress. The PSS has been extensively validated, exhibiting good internal reliability (Cronbach’s α = 0.78), rendering it pertinent for assessing stress levels and emotional exhaustion among nurses [ 63 ].
Patient activation measure (PAM)
A 13-item scale measuring patient self-efficacy in managing their health and care [ 64 ]. The Patient Activation Measure (PAM) employs a 4-point Likert scale, ranging from “Strongly Disagree” (1) to “Strongly Agree” (4), to assess the level of patient involvement in their healthcare. The raw scores from each question are summed, and this raw score is then mathematically transformed to a 0-100 scale. The final PAM score reflects the degree of a patient’s activation, with a score range of 1–46 indicating low activation, wherein patients tend to be overwhelmed and unprepared to take an active role in their health; 47–55 suggesting moderate activation, where patients are somewhat comfortable managing their health but might require assistance; 56–72 signifying high activation, with patients being comfortable in taking an active role in managing their health; and 73–100 representing very high activation, wherein patients are highly confident and skilled in managing their health [ 65 ].
Morisky Medication Adherence Scale (MMAS-8)
The Morisky Medication Adherence Scale (MMAS-8) is a validated 8-item self-report instrument designed to identify barriers to medication adherence [ 66 ]. It employs a binary response format (yes/no) to assess adherence issues over the past week. The MMAS-8 exhibits good internal consistency (Cronbach’s α = 0.83) and reliability, rendering it a crucial tool for evaluating patient engagement concerning medication adherence. Patients are categorized into different adherence levels based on their cumulative score ranging from 0 to 8, with a score of 8 indicating high adherence (likely following medication instructions), scores of 6 or 7 suggesting medium adherence (potential for missed medications), and scores below 6 signifying low adherence (high risk of not following instructions) [ 67 ].
Hospital Consumer Assessment of Healthcare Providers and systems (HCAHPS)
The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) is a survey instrument and data collection methodology to measure patients’ perceptions of their hospital experience [ 68 ]. The survey contains 29 questions about the recent hospital stay of patients, including communication with nurses and doctors, hospital staff responsiveness, cleanliness and quietness of the hospital environment, communication about medications, discharge information, overall hospital rating, and whether they would recommend the hospital [ 69 ]. The survey is administered to a random sample of adult patients across medical conditions between 48 h and six weeks after discharge. Publicly reported scores will be utilized as a proxy for patient satisfaction [ 70 ]. The HCAHPS data used in this study were collected independently from the other patient data and represented the publicly reported satisfaction scores for the participating hospitals during the study period.
Electronic Medical Records (EMR)
Electronic Medical Records (EMRs) served as a data source to extract 30-day hospital readmission rates, an objective measure that is pivotal to evaluating health outcomes in relation to nursing incivility, nurse stress, and patient engagement. Utilization of EMRs facilitates the collection of this crucial metric, allowing for a rigorous assessment of potential associations between the aforementioned variables and patient health outcomes, as reflected in readmission rates within 30 days after discharge.
Ethics approval
The study received ethical approval from the General Directorate of Health Affairs, Hail Healthy Cluster, Hail Region / IRB Registration Number with KACST, KSA: H-11–08 L-074 / IRB log number 2023-66. The approval process involved evaluating the study’s objectives, methods, instruments, and impacts while emphasizing adherence to ethical principles like respect, justice, beneficence, and non-maleficence. A detailed informed consent form was prepared to ensure the understanding and voluntary participation of the participants, along with measures to maintain privacy and confidentiality using unique participant identifiers. The protocol also included provisions for participant transparency, including the right to access results and withdraw at any time without repercussions. Following the review of the IRB, ethical clearance was granted, allowing the study to proceed in accordance with established ethical standards and guidelines.
Data collection was conducted between May 2023 and November 2023 in four public hospitals located in the northwest region of Saudi Arabia. These hospitals were strategically selected to represent the region’s geographic and demographic diversity, ensuring the sample reflected the wider context of Saudi healthcare. Nurses were recruited through targeted invitations sent to all eligible personnel, aiming for a broad representation of experiences and backgrounds. Patients were randomly selected from hospital records and invited to participate voluntarily. No incentives were offered to participants.
Paper-based surveys were administered to both nurses and patients. Nurses completed the surveys during their work shifts, while patients were surveyed independently of their hospital stay. Researchers were available to assist participants who needed clarification or faced difficulty understanding the questions. Patients completed the PAM and MMAS-8 surveys independently, typically within 2–4 weeks after discharge, to assess their activation levels and medication adherence during the post-hospitalization period.
The data collection process was designed to ensure participant privacy, reduce potential biases, and gather comprehensive responses without causing undue burden. Unique participant identifiers were assigned to each nurse and patient to maintain confidentiality throughout the study. All collected data were stored on secure, password-protected servers, with access restricted to authorized members of the research team. Physical copies of the surveys were stored in locked cabinets, and electronic data were encrypted to prevent unauthorized access.
Participants typically spent 15–20 min completing the surveys, which included the Nursing Incivility Scale (NIS) and the Perceived Stress Scale (PSS) for nurses, and the Patient Activation Measure (PAM) and the Morisky Medication Adherence Scale (MMAS-8) for patients. These instruments were selected based on their established validity and reliability in similar research contexts and their alignment with the study variables. The data collection process was designed to ensure participant privacy, reduce potential biases, and gather comprehensive responses without causing undue burden. The use of paper-based surveys accounted for participants’ varied preferences and technological comfort levels while minimizing potential technical issues.
Statistical analysis
This study employed descriptive statistics to establish the demographic profiles of nurse and patient participants, summarizing categorical variables through frequencies and percentages. For the Nursing Incivility Scale (NIS) and Perceived Stress Scale (PSS), we divided scores into tertiles for descriptive analyses, which offered an intuitive understanding of incivility and stress levels among participants. In our regression analyses, we used the continuous scores to preserve the rich variability inherent in these measures.
The statistical examination commenced with bivariate Pearson’s correlation analysis, identifying foundational relationships between key study variables. We then conducted multiple linear regression models to determine the direct effects of nursing incivility, nurse stress, patient activation, and medication adherence on health outcomes. Hierarchical multiple regression analyses were conducted, entering nursing role as a covariate in the first step, followed by the predictor variables (nursing incivility, nurse stress, patient activation, and medication adherence) in subsequent steps.
Further statistical exploration involved mediation analyses to investigate the indirect effects within our conceptual framework. Specifically, we examined the mediating role of nurse stress in the association between nursing incivility and health outcomes and the potential mediation of patient engagement between nurse stress and health outcomes. A serial mediation model elucidated the complex interplay and indirect pathways that link nursing incivility to patient outcomes through multiple mediator variables.
All statistical procedures were executed using SPSS Version 26. Missing data were managed via mean substitution for subscale averages. To ensure participant privacy and confidentiality, all analyses were performed using de-identified data, with unique participant identifiers replaced by numeric codes. Only aggregate results were reported, ensuring that no individual participant could be identified from the study findings. The significance threshold was set at an alpha level of 0.05, and effect sizes were calculated to contextualize the strength of associations.
Consistent with the structured complexity of our theoretical model, a serial mediation analysis was incorporated into the statistical strategy. This analysis enabled us to dissect the multi-step indirect effects and examine the potential sequential mediators, providing an integrated understanding of the relationships among the constructs of interest. The integrity of the analyses was maintained by stringent testing for normality, linearity, and homoscedasticity, ensuring the appropriateness of our regression models and the robustness of our findings. The analytical choices, carefully aligned with the objectives of the study and the nature of the data, facilitated a clear depiction of the causal pathways and supported the validity of our conclusions.
This section presents the empirical findings of the study, which aim to explore the relationships between nursing incivility, nurse stress, patient engagement, and health outcomes. The results are based on data from 289 nurses and 521 patients in four hospitals. Detailed statistical analyses, including descriptive statistics, correlations, and regression models, help to elucidate these relationships. The following tables provide a comprehensive summary of these analyses, shedding light on the nuances and key takeaways of the study findings. The scales used in this study demonstrated good to excellent reliability in the current sample. Cronbach’s alpha coefficients were as follows: Nursing Incivility Scale (NIS) α = 0.94, Perceived Stress Scale (PSS) α = 0.82, Patient Activation Measure (PAM) α = 0.89, and Morisky Medication Adherence Scale (MMAS-8) α = 0.79.
The demographic characteristics presented in Table 1 offer a comprehensive statistical overview of the study participants, encompassing both nurses ( N = 289) and patients ( N = 512). The age distribution among nurses is skewed toward younger age groups, with 38.7% aged 25–30 years and 30.1% aged 31–40 years. In contrast, the patient population exhibits a more evenly distributed age range, with the highest proportion (37.1%) in the 31–40 age group. Gender-wise, the nurse sample is predominantly female (66.8%), aligning with the traditional gender demographics of the nursing profession, while the patient sample shows a more balanced distribution (51.6% male, 48.4% female). The nursing roles represented include Registered Nurses (51.9%), Head Nurses (24.2%), and Supervisors (23.9%), reflecting a diverse representation of nursing staff. In terms of experience, the majority of nurses (51.6%) have 2–5 years of experience, followed by those with more than 5 years (25.3%) and less than 2 years (23.2%). The patient health status data reveals that 63.7% are categorized as healthy, 33.6% have a managed chronic condition, and 2.7% have an unmanaged chronic condition. Furthermore, the educational qualifications of nurses are well-represented, with 62.0% holding a Bachelor’s degree and 38.0% possessing a Master’s or Ph.D. degree. Finally, the distribution of participants across the four hospitals is relatively even, ranging from 24.4 to 25.8% for patients and 24.2–25.6% for nurses, ensuring a representative sample from various healthcare settings.
Table 2 presents a quantitative assessment of the severity distribution of nursing incivility scores among the nurse participants. The Nursing Incivility Scale (NIS) scores have been categorized into three distinct levels: mild incivility (scores ranging from 0 to 33), moderate incivility (scores ranging from 34 to 66), and severe incivility (scores ranging from 67 to 100). Out of the total 289 nurse participants, 90 (31.1%) reported experiencing mild levels of incivility, 125 (43.3%) experienced moderate incivility, and 74 (25.6%) experienced severe incivility. The data reveals that a significant proportion of nurses, nearly 69%, reported experiencing moderate to severe levels of incivility in their workplace, highlighting the prevalence of this issue within the nursing profession. The distribution of incivility levels provides a quantitative representation of the severity of the problem, which is crucial for developing targeted interventions and policies to address workplace incivility and promote a positive work environment for nurses.
Table 3 presents the distribution of Perceived Stress Scale (PSS) scores among the nurse participants, categorized into three levels: low stress (scores ranging from 0 to 13), moderate stress (scores ranging from 14 to 26), and high stress (scores ranging from 27 to 40). Out of the total 289 nurse participants, 95 (32.9%) reported low stress levels, 120 (41.5%) reported moderate stress levels, and 74 (25.6%) reported high stress levels. The data reveals that a significant proportion of nurses, approximately 67%, experienced moderate to high levels of stress, indicating the presence of substantial stress among the nursing workforce. The distribution of stress levels provides a quantitative representation of the prevalence and severity of stress experienced by nurses, which is crucial for developing targeted interventions and strategies to address and mitigate stress within the nursing profession.
Table 4 presents a comparative analysis of patient activation levels and medication adherence, as measured by the Patient Activation Measure (PAM) and the Morisky Medication Adherence Scale (MMAS-8), respectively. The scores for both measures are categorized into low/poor, moderate, and high ranges. For the PAM, the score ranges are 0–33 for low/poor activation, 34–66 for moderate activation, and 67–100 for high activation. The table shows that 150 patients scored in the low/poor range, 250 in the moderate range, and 112 in the high range. For the MMAS-8, the score ranges are 0–2 for low/poor adherence, 3–5 for moderate adherence, and 6–8 for high adherence. The table indicates that 200 patients scored in the low/poor range, 180 in the moderate range, and 132 in the high range. The table also provides p-values for the comparison between the low/poor and high categories for both measures. For the PAM, the p-value is reported as < 0.05, indicating a statistically significant difference between the low/poor and high activation groups. For the MMAS-8, the p-value is reported as < 0.01, suggesting a highly significant difference between the low/poor and high medication adherence groups.
Table 5 presents the bivariate correlation coefficients among the key study variables: Nursing Incivility (NIS), Nurse Stress (PSS), Patient Activation (PAM), and Medication Adherence (MMAS-8). The table is structured as a correlation matrix, where each cell represents the correlation coefficient between the corresponding row and column variables. The diagonal elements (1.00) represent the perfect correlation of each variable with itself. The correlation coefficient between Nursing Incivility (NIS) and Nurse Stress (PSS) is 0.45, indicating a moderate positive correlation. The correlation coefficients between Nursing Incivility (NIS) and Patient Activation (PAM), and Nursing Incivility (NIS) and Medication Adherence (MMAS-8) are − 0.30 and − 0.25, respectively, suggesting moderate negative correlations. The correlation coefficient between Nurse Stress (PSS) and Patient Activation (PAM) is -0.40, indicating a moderate negative correlation. The correlation coefficient between Nurse Stress (PSS) and Medication Adherence (MMAS-8) is -0.35, suggesting a moderate negative correlation. The correlation coefficient between Patient Activation (PAM) and Medication Adherence (MMAS-8) is 0.60, indicating a strong positive correlation.
Table 6 presents a nuanced understanding of how various factors related to nursing and patient engagement influence health outcomes, specifically 30-day readmission rates and patient satisfaction scores. The data indicate that nursing incivility has a detrimental effect on both health outcomes, suggesting that interventions aimed at reducing workplace incivility may improve patient care. Interestingly, nurse stress shows a positive correlation with both outcomes, indicating that higher stress levels could be linked to more frequent patient follow-up, possibly improving patient satisfaction despite higher readmission rates. This points to the complex role of stress in healthcare settings. Furthermore, patient activation is strongly negatively correlated with both outcomes, emphasizing the benefits of patient empowerment in their own care processes. Enhanced patient activation could lead to fewer readmissions and higher satisfaction. Similarly, medication adherence, which is negatively associated with readmission rates and positively with satisfaction scores, highlights its critical role in effective patient management. These insights reveal the interconnected nature of healthcare environments and underscore the importance of a multifaceted approach to improving patient outcomes.
Table 7 presents an intricate statistical investigation into the cascading effects of nursing incivility within a healthcare setting. The analysis thoughtfully dissects how nursing incivility impacts patient outcomes, notably through nurse stress and patient engagement mediating variables. The positive estimate (B = 0.08) for the path from nursing incivility to nurse stress, with a significant p-value of less than 0.001, underscores the strong influence of workplace incivility on nurse stress. Furthermore, both statistically significant, the adverse pathway from nursing incivility to patient engagement (B = -0.24) and from nurse stress to patient engagement (B = -0.41) highlights a detrimental cascade effect, where incivility indirectly undermines patient engagement through increased nurse stress. The substantial direct impact of patient engagement on patient outcomes (B = 0.52) emphasizes the critical role of patient involvement in their care. The analysis culminates in delineating the total and direct effects of nursing incivility on patient outcomes, with the indirect effects through nurse stress and patient engagement providing a deeper understanding of the underlying dynamics. The obtained relationships between nursing incivility, nurse stress, patient engagement, and health outcomes, along with their standardized regression coefficients (β) and significance levels (p-values), are visually summarized in Fig. 2 .
As illustrated in Fig. 2 , nursing incivility had a significant direct effect on both nurse stress (β = 0.08, p < 0.001) and patient engagement (β = -0.24, p = 0.003). Nurse stress, in turn, negatively influenced patient engagement (β = -0.41, p < 0.001). Furthermore, patient engagement had a strong positive impact on patient outcomes (β = 0.52, p < 0.001). The total effect of nursing incivility on patient outcomes was significant (β = -0.37, p < 0.001), with both direct (β = -0.22, p = 0.002) and indirect effects through nurse stress and patient engagement (β = -0.15, p = 0.004) contributing to this relationship. These findings provide evidence for the hypothesized cascading effects of nursing incivility on patient outcomes, highlighting the crucial role of nurse stress and patient engagement as mediating factors in this relationship. The results underscore the importance of addressing workplace incivility and promoting a positive work environment to enhance nurse well-being, patient engagement, and ultimately, patient outcomes.
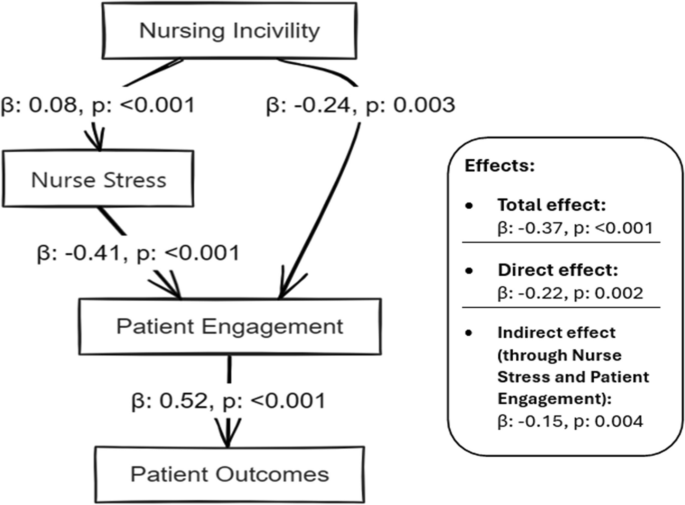
Relationships between nursing incivility, nurse stress, patient engagement, and health outcomes were obtained, with standardized regression coefficients (β) and significance levels ( p -values)
Additional analyses were conducted to examine potential differences in experiences of nursing incivility and stress among staff nurses, head nurses, and supervisors. One-way ANOVA tests revealed significant differences in NIS scores across nursing roles [F(2, 286) = 5.67, p = 0.004]. Post-hoc comparisons using Tukey’s HSD test indicated that staff nurses (M = 48.3, SD = 18.6) reported significantly higher levels of incivility compared to supervisors (M = 39.5, SD = 16.2, p = 0.003). However, no significant differences were found in PSS scores across nursing roles [F(2, 286) = 1.45, p = 0.236].
The additional analyses revealed significant differences in Nursing Incivility Scale (NIS) scores across nursing roles [F(2, 286) = 5.67, p = 0.004], with staff nurses (M = 48.3, SD = 18.6) reporting significantly higher levels of incivility compared to supervisors (M = 39.5, SD = 16.2, p = 0.003). To account for the potential influence of nursing role on the overall results, we included it as a covariate in subsequent regression analyses.
To further examine the robustness of our findings, we conducted a sensitivity analysis by removing head nurses and supervisors from the sample and re-running the analyses with only staff nurses. The results remained consistent with the original findings, suggesting that the observed relationships between nursing incivility, nurse stress, patient engagement, and health outcomes were not unduly influenced by the inclusion of head nurses and supervisors in the sample.
This cross-sectional study examined the relationships between perceived nursing incivility, nurse stress levels, patient engagement in care, and patient health outcomes. The findings reveal a multifaceted relationship where nursing incivility is directly detrimental to nurses’ well-being and indirectly affects patient outcomes through the mediating effects of nurse stress and patient engagement.
The positive correlation between nursing incivility and nurse stress aligns with previous research indicating that workplace incivility can lead to negative psychological outcomes and job dissatisfaction [ 71 , 72 , 73 , 74 , 75 ]. The findings here extend this understanding by quantifying the correlation and delineating the impact of different levels of incivility.
In contrast, some studies, such as [ 6 , 76 ], have suggested that certain coping mechanisms and organizational cultures can mitigate the impact of incivility on stress. However, this study highlights the widespread nature of incivility in nursing, suggesting that such coping strategies may not be sufficient in the face of severe or persistent incivility. The inverse relationship between nurse stress and patient engagement supports the notion that stressed nurses may be less able to effectively engage with patients, aligning with research [ 51 ], which showed that nurse burnout could lead to decreased quality of patient care. Conversely, a study [ 52 ] found that certain aspects of nurse engagement, like job satisfaction, could buffer the impact of stress on patient care. However, this study suggests that the stress level resulting from incivility can override such positive aspects of engagement.
The negative impact of nursing incivility on patient health outcomes, evidenced by increased readmission rates within 30 days and lower patient satisfaction scores, is consistent with previous findings [ 6 , 76 ]. This reinforces the idea that the nursing work environment, including the presence or absence of incivility, can directly influence patient outcomes such as readmission rates and satisfaction scores, which were measured at the 30-day mark in our study.
However, research [ 12 , 28 ] argued that the impact of the nursing work environment on patient outcomes is often indirect and moderated by other factors. This study refines this perspective by demonstrating a direct correlation, suggesting that the impact of incivility is immediate and significant [ 57 , 58 , 59 ]. underscore incivility as a significant workplace stressor that nurses face that can adversely affect their well-being. The severity analysis further highlights that a concerning 25.6% of nurses report experiencing severe incivility, while 43.3% encounter moderate levels. Such widespread uncivil behaviors from colleagues, supervisors, physicians, and patients create stressful work environments that diminish the ability of nurses to perform effectively [ 11 ].
However, contrary to some studies [ 8 , 77 ], our mediation analysis reveals only a moderate total effect size (β = -0.05) of nursing incivility on patient outcomes. This discrepancy could reflect cultural specificities within Saudi hospitals that shape inter-action dynamics differently than their western counterparts. However, the negative association remains noteworthy. In addition, stress exhibits an unexpected positive association with patient outcomes. This surprising finding warrants a deeper ethnographic investigation to elucidate the complex stress and coping mechanisms of nurses within the hospitals sampled that unexpectedly improved patient care. Critically, patient engagement registers the strongest impact on health outcomes (β = 0.52) [ 2 , 78 , 79 ]. Interestingly, 63.7% of patients fall under the ‘Healthy’ category, although 33.6% manage chronic conditions. This breakdown provides a favourable foundation for boosting patient activation efforts. However, the correlation and regression analyses reveal that improvements in workplace conditions for nurses could further improve patient engagement and care quality.
The study findings on the mediator effect of nurse stress, linking nursing incivility with poorer patient outcomes, add a new dimension to the existing literature. This aligns with the work of [ 12 ], who emphasized the importance of the emotional well-being of healthcare providers in ensuring patient safety. This contrasts with some views like those presented [ 6 ], who posited that organizational factors play a more substantial role in mediating the impact of incivility on outcomes. Our study suggests that individual stress levels are equally, if not more, critical in this context. The serial mediation analysis reveals the pathway from nursing incivility through nurse stress to patient engagement and outcomes, and it presents a comprehensive model that integrates various aspects of the nursing environment. This model is supported by research [ 6 ], which also emphasises the cascading effects of workplace dynamics on patient care. However, this finding challenges the argument [ 22 ] that the primary impact of the nursing environment on patient outcomes is through organizational efficiency rather than staff well-being.
Conclusions
This cross-sectional study conducted in four Saudi Arabian hospitals examined the complex relationships between nursing incivility, nurse stress, patient engagement, and health outcomes. The findings underscore the widespread impact of nursing incivility, which adversely affects nurse well-being and, through increased nurse stress, indirectly influences patient outcomes. Specifically, our analyzes demonstrate that nursing incivility is related to higher readmission rates at 30 days and lower patient satisfaction scores, providing concrete examples of its negative ramifications.
Our empirical evidence, derived from validated scales and robust multivariate regression analyzes, confirms that nursing incivility increases stress levels among nurses, corroborating existing literature that identifies uncivil behavior as a significant workplace stressor. In particular, more than two thirds of the participants reported experiencing moderate to severe levels of incivility, highlighting the widespread nature of this issue within healthcare settings. Theoretically, this research enriches the current understanding of the impacts of nursing incivility by situating them within a comprehensive framework that includes both direct and indirect effects on health outcomes.
Practically, the study lays a solid foundation for developing targeted interventions aimed at cultivating more respectful and collaborative nursing environments. Such interventions could include training programs focused on conflict resolution and stress management, which are critical to mitigating the effects of incivility and improving overall quality of care. Future research should explore the longitudinal effects of nursing incivility to better understand the causality and persistence of its impacts. Additionally, investigating the role of organizational factors such as leadership styles and workplace culture in modifying or exacerbating the effects of incivility could provide deeper insight into effective strategies to improve nurse and patient outcomes.
Limitations
The limitations of the study provide avenues for further research. Longitudinal approaches could establish causal claims more firmly. A longitudinal design that follows participants over an extended period could provide more insights into the temporal aspects of these relationships and strengthen our understanding of the causality between nursing incivility, nurse stress, patient engagement, and health outcomes.
Another limitation refers to the representativeness of the sample. Although efforts were made to ensure diversity through a combination of random sampling and voluntary participation, the generalizability of the findings may be limited. The study was conducted in four public hospitals in the northwest region of Saudi Arabia, and the unique cultural and socioeconomic characteristics of this region should be considered when interpreting the results and their implications for nursing practice and patient care. Future studies could explore these relationships in different healthcare settings, regions, and cultural contexts to assess the generalizability of the findings.
Furthermore, the current study did not investigate the role of organizational factors in contributing to nursing incivility, stress, and patient outcomes. While focusing on individual-level variables provides valuable insights, a more comprehensive understanding would require the inclusion of organizational factors such as leadership, communication, and workplace culture. Future research should aim to incorporate these measures to gain a holistic perspective on the relationships between nursing incivility, stress, and patient outcomes.
Practical implications and future directions
The findings of this study have significant practical implications, providing an evidence base for healthcare institutions to develop systemic strategies to address nursing incivility and its cascading impacts. Interventions should focus on cultivating positive workplace cultures, deescalating incivility through protocols, facilitating team building, and implementing self-care training. Regarding patients, patient education programs to promote activation and specialist referrals to improve adherence appear prudent. Future studies could build on these findings by testing such interventions through experimental or action methodologies to quantify long-term results.
Future research could also explore the role of organizational factors in contributing to nursing incivility, stress, and patient outcomes. Investigating aspects such as leadership styles, communication patterns, and workplace culture could provide valuable insights into the systemic elements that shape the dynamics of nursing incivility and its consequences. By examining the interaction between individual and organizational factors, future studies could offer a more holistic understanding of the complex relationships at play and inform the development of targeted interventions at the individual and organizational levels.
Related research might explore subgroup differences in perceptions by age or unit type or investigate relationships in private-sector hospitals compared to these public institutions. Furthermore, examining the broader organizational impact of nursing incivilities, such as its effects on team dynamics, staff turnover, and general healthcare culture, would contribute to a more comprehensive understanding of the phenomenon. Assessing the economic implications of incivility, including costs associated with staff replacement and lost productivity, could highlight the financial burden on healthcare organizations and inform strategic decisions to address this issue. Future studies could also employ qualitative methods to gain deeper insights into nurses’ experiences of incivility and its impact on their well-being and professional practice. As the Saudi healthcare system continues to evolve, mitigating workplace mistreatment and nurturing patient engagement will only grow in importance, making this study highly relevant.
Availability of data and materials
Data will be available upon request.
Zabin LM, Zaitoun RSA, Sweity EM, de Tantillo L. The relationship between job stress and patient safety culture among nurses: a systematic review. BMC Nurs. 2023;22:39.
Article PubMed PubMed Central Google Scholar
Alshehry AS. Nurse–patient/relatives conflict and patient safety competence among nurses. Inquiry. 2022;59:00469580221093186.
PubMed PubMed Central Google Scholar
Alquwez N. Nurses’ self-efficacy and well-being at work amid the COVID-19 pandemic: a mixed-methods study. Nurs Open. 2023;10:5165–76.
Vargas EA, Mahalingam R, Marshall RA. Witnessed incivility and perceptions of patients and visitors in hospitals. J Patient Exp. 2021;8:23743735211028092.
Kousha S, Shahrami A, Forouzanfar MM, Sanaie N, Atashzadeh-Shoorideh F, Skerrett V. Effectiveness of educational intervention and cognitive rehearsal on perceived incivility among emergency nurses: a randomized controlled trial. BMC Nurs. 2022;21:153.
Alquwez N. Examining the influence of workplace incivility on nurses’ patient safety competence. J Nurs Scholarsh. 2020;52:292–300.
Article PubMed Google Scholar
Park EJ, Kang H. Experiences of undergraduate nursing students with faculty incivility in nursing classrooms: a meta-aggregation of qualitative studies. Nurse Educ Pract. 2021;52:103002.
Mammen BN, Lam L, Hills D. Newly qualified graduate nurses’ experiences of workplace incivility in healthcare settings: an integrative review. Nurse Educ Pract. 2023;69:103611.
Callado A, Teixeira G, Lucas P. Turnover intention and organizational commitment of primary healthcare nurses. Healthcare (Basel). 2023;11:521.
Kim Y, Oh Y, Lee E, Kim SJ. Impact of nurse–physician collaboration, moral distress, and professional autonomy on job satisfaction among nurses acting as physician assistants. Int J Environ Res Public Health. 2022;19:661.
Armstrong N. Management of nursing workplace incivility in the health care settings: a systematic. Review. 2018;66:403–10 https://doi.org/10.1177/2165079918771106 .
Article Google Scholar
Alshehry AS, Alquwez N, Almazan J, Namis IM, Moreno-Lacalle RC, Cruz JP. Workplace incivility and its influence on professional quality of life among nurses from multicultural background: a cross-sectional study. J Clin Nurs. 2019;28:2553–64.
Shoorideh FA, Moosavi S, Balouchi A. Incivility toward nurses: a systematic review and meta-analysis. J Med Ethics Hist Med. 2021;14:15.
Google Scholar
Brennan D, Wendt L. Increasing quality and patient outcomes with staff engagement and shared governance. OJIN: The Online J Issues Nurs. 2021;26(2). https://doi.org/10.3912/OJIN.Vol26No02PPT23 .
Owen DC, Boswell C, Opton L, Franco L, Meriwether C. Engagement, empowerment, and job satisfaction before implementing an academic model of shared governance. Appl Nurs Res. 2018;41:29–35.
Article CAS PubMed Google Scholar
Bambi S, Foà C, De Felippis C, Lucchini A, Guazzini A, Rasero L. Workplace incivility, lateral violence and bullying among nurses. A review about their prevalence and related factors. Acta Biomed. 2018;89 Suppl 6:51.
Galletta M, Portoghese I, Carta MG, D’Aloja E, Campagna M. The effect of nurse-physician collaboration on job satisfaction, team commitment, and turnover intention in nurses. Res Nurs Health. 2016;39:375–85.
Keller S, Yule S, Zagarese V, Parker SH. Predictors and triggers of incivility within healthcare teams: a systematic review of the literature. BMJ Open. 2020;10:e035471.
Lewis C. The impact of interprofessional incivility on medical performance, service and patient care: a systematic review. Future Healthc J. 2023;10:69.
Lewis C. The impact of interprofessional incivility on medical performance, service and patient care: a systematic review. Future Healthc J. 2023;10:69–77.
Mabona JF, van Rooyen D, Ten Ham-Baloyi W. Best practice recommendations for healthy work environments for nurses: an integrative literature review. Health SA. 2022;27:1788.
Lucas P, Jesus É, Almeida S, Araújo B. Relationship of the nursing practice environment with the quality of care and patients’ safety in primary health care. BMC Nurs. 2023;22:1–10.
Waddell A, Oberlies AS. A post-pandemic review of American association of critical care nurses’s domains of establishing and sustaining healthy work environments: strategies for nurse leaders. Crit Care Nurs Clin North Am. 2024;0. https://doi.org/10.1016/j.cnc.2024.01.003 .
Hult M, Terkamo-Moisio A, Kaakinen P, Karki S, Nurmeksela A, Palonen M, et al. Relationships between nursing leadership and organizational, staff and patient outcomes: a systematic review of reviews. Nurs Open. 2023;10:5920.
Ystaas LMK, Nikitara M, Ghobrial S, Latzourakis E, Polychronis G, Constantinou CS. The impact of transformational leadership in the nursing work environment and patients’ outcomes: a systematic review. Nurs Rep. 2023;13:1271.
Alfadhalah T, Elamir H. Organizational culture, quality of care and leadership style in government general hospitals in Kuwait: a multimethod study. J Healthc Leadersh. 2021;13:243.
Koehorst MM, van Deursen AJAM, van Dijk JAGM, de Haan J. A systematic literature review of organizational factors influencing 21st-century skills. SAGE Open. 2021;11:21582440211067252.
Alshehry AS, Alquwez N, Almazan J, Namis IM, Cruz JP. Influence of workplace incivility on the quality of nursing care. J Clin Nurs. 2019;28:4582–94.
Jiang L, Xu X, Jacobs S. From incivility to turnover intentions among nurses: A multifoci and self-determination perspective. J Nurs Manag. 2023;2023. https://doi.org/10.1155/2023/7649047 .
Harms PD. Nursing: a critical profession in a perilous time. Ind Organ Psychol. 2021;14:264–6.
Wakefield MK, Williams DR, Menestrel S Le, Flaubert JL, editors. The future of nursing 2020–2030. 2021. https://doi.org/10.17226/25982 .
Marchiondo LA, Fisher GG, Cortina LM, Matthews RA. Disrespect at work, distress at home: a longitudinal investigation of incivility spillover and crossover among older workers. Work Aging Retire. 2020;6:153–64.
Blackstock S, Cummings G, Glanfield F, Yonge O. A review: developing an ecological model approach to co-worker incivility experiences of new graduate nurses. J Adv Nurs. 2022;78:1535–50.
Mikaelian B, Stanley D. Incivility in nursing: from roots to repair. J Nurs Manag. 2016;24:962–9.
Fontenot J, Hebert M, Stefanski R, Morris D. Systemic antecedents of academic incivility in nursing: An integrative review. Teach Learn Nurs. 2024;19(2):192–201. https://doi.org/10.1016/J.TELN.2024.01.015 .
Eyuboglu M, Eyuboglu D, Pala SC, Oktar D, Demirtas Z, Arslantas D, et al. Traditional school bullying and cyberbullying: prevalence, the effect on mental health problems and self-harm behavior. Psychiatry Res. 2021;297:113730.
Kwame A, Petrucka PM. A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward. BMC Nurs. 2021;20:1–10.
Cortina LM, Sandy Hershcovis M, Clancy KBH. The embodiment of insult: a theory of biobehavioral response to workplace incivility. J Manage. 2022;48:738–63.
PubMed Google Scholar
Ostroff C, Benincasa C, Rae B, Fahlbusch D, Wallwork N. Eyes on incivility in surgical teams: teamwork, well-being, and an intervention. PLoS One. 2023;18:e0295271.
Article CAS PubMed PubMed Central Google Scholar
Poon YSR, Lin YP, Griffiths P, Yong KK, Seah B, Liaw SY. A global overview of healthcare workers’ turnover intention amid COVID-19 pandemic: a systematic review with future directions. Hum Resour Health. 2022;20:70.
Kroning M, Annunziato S. New strategies to combat workplace incivility and promote joy. Nursing. 2023;53:45–50.
Vujanić J, Mikšić Š, Barać I, Včev A, Lovrić R. Patients’ and nurses’ perceptions of importance of caring nurse-patient interactions: do they differ? Healthcare. 2022;10:554.
Peng X. Advancing workplace civility: a systematic review and meta-analysis of definitions, measurements, and associated factors. Front Psychol. 2023;14:1277188.
Fleischer S, Berg A, Zimmermann M, Wüste K, Behrens J. Nurse-patient interaction and communication: a systematic literature review. J Public Health (Bangkok). 2009;17:339–53.
Harris WC, Usseglio J, Chapman-Rodriguez R, Licursi M, Larson E. A scoping review of validated tools to measure incivility in healthcare settings. J Nurs Adm. 2019;49:447–53.
Shi Y, Guo H, Zhang S, Xie F, Wang J, Sun Z, et al. Impact of workplace incivility against new nurses on job burn-out: a cross-sectional study in China. BMJ Open. 2018;8:e020461.
Tolotti A, Barello S, Vignaduzzo C, Liptrott SJ, Valcarenghi D, Nania T, et al. Patient engagement in oncology practice: a qualitative study on patients’ and nurses’ perspectives. Int J Environ Res Public Health. 2022;19:11644.
Barello S, Graffigna G, Pitacco G, Mislej M, Cortale M, Provenzi L. An educational intervention to train professional nurses in promoting patient engagement: a pilot feasibility study. Front Psychol. 2017;7:2020.
Almalki MJ, Elamin A, Jabour AM, Varghese J, Alotaibi AA, Moafa HN. In response to the Saudi healthcare reform: a cross-sectional study of awareness of and attitudes toward the public health model among health students. Front Public Health. 2023;11:1264615.
Gurajala S, Gurajala S. Healthcare system in the Kingdom of Saudi Arabia: an Expat Doctor’s perspective. Cureus. 2023;15:e38806.
AlJohani BA, Bugis BA. Advantages and challenges of implementation and strategies for health insurance in Saudi Arabia: a systemic review. Inquiry. 2024;61:469580241233447.
Gurajala S. Healthcare system in the Kingdom of Saudi Arabia: an Expat Doctor’s perspective. Cureus. 2023;15:e38806.
Al-Kahtani N, Alruwaie S, Al-Zahrani BM, Abumadini RA, Aljaafary A, Hariri B, et al. Digital health transformation in Saudi Arabia: a cross-sectional analysis using Healthcare Information and Management Systems Society’ digital health indicators. Digit Health. 2022;8:20552076221117744.
Saeed A, Saeed AB, AlAhmri FA. Saudi Arabia health systems: challenging and future transformations with artificial intelligence. Cureus. 2023;15:37826.
Justinia T. Saudi Arabia: transforming healthcare with technology. 2022. p. 755–69.
Cohen J. Statistical Power Analysis for the Behavioral Sciences. Statistical Power Analysis for the Behavioral Sciences. 2013. https://doi.org/10.4324/9780203771587 .
Hulley S, Cummings S, Browner W, Grady D, Hearst N, Newman T. Estimating sample size and power. Des Clin Res. 2001;2:85. https://books.google.com/books/about/Designing_Clinical_Research.html?id=_b62TBnoppYC .
Concannon TW, Grant S, Welch V, Petkovic J, Selby J, Crowe S, et al. Practical guidance for involving stakeholders in health research. J Gen Intern Med. 2019;34:458–63.
Guidroz AM, Burnfield-Geimer JL, Clark O, Schwetschenau HM, Jex SM. Nursing incivility scale. 2010.
Guidroz AM, Burnfield-Geimer JL, Clark O, Schwetschenau HM, Jex SM. The nursing incivility scale: development and validation of an occupation-specific measure. J Nurs Meas. 2010;18:176–200.
Hutton S, Gates D. Workplace incivility and productivity losses among direct care staff. AAOHN J. 2008;56:168–75.
Taylor JM. Psychometric analysis of the ten-item perceived stress scale. Psychol Assess. 2015;27:90–101.
Lee ES, Tan SY, Lee PSS, Koh HL, Soon SWW, Sim K, et al. Perceived stress and associated factors among healthcare workers in a primary healthcare setting: the Psychological Readiness and Occupational Training Enhancement during COVID-19 time (PROTECT) study. Singapore Med J. 2022;63:20.
Kearns R, Harris-Roxas B, McDonald J, Song HJ, Dennis S, Harris M. Implementing the Patient Activation Measure (PAM) in clinical settings for patients with chronic conditions: a scoping review. Integr Healthcare J. 2020;2(1):32. https://doi.org/10.1136/IHJ-2019-000032 .
Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39:1005–10026.
Tan X, Patel I, Chang J. Review of the four item Morisky Medication Adherence Scale (MMAS-4) and eight item Morisky Medication Adherence Scale (MMAS-8). Innov Pharm. 2014;5:5.
Arnet I, Metaxas C, Walter PN, Morisky DE, Hersberger KE. The 8-item Morisky Medication Adherence Scale translated in German and validated against objective and subjective polypharmacy adherence measures in cardiovascular patients. J Eval Clin Pract. 2015;21:271–7.
Dawn AG, Lee PP. Patient satisfaction instruments used at academic medical centers: results of a survey. Am J Med Qual. 2003;18:265–9.
Aoki T, Yamamoto Y, Nakata T. Original research: translation, adaptation and validation of the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) for use in Japan: a multicentre cross-sectional study. BMJ Open. 2020;10:e040240.
Mercier MR, Galivanche AR, David WB, Malpani R, Pathak N, Hilibrand AS, et al. Hospital consumer assessment of healthcare providers and systems survey response rates are significantly affected by patient characteristics and postoperative outcomes for patients undergoing primary total knee arthroplasty. PLoS One. 2021;16:e0257555.
Probst TM, Petitta L, Barbaranelli C, Austin C. Safety-related moral disengagement in response to job insecurity: counterintuitive effects of perceived organizational and supervisor support. J Bus Ethics. 2020;162:343–58.
Jia X, Liao S, Yin W. Job insecurity, emotional exhaustion, and workplace deviance: the role of corporate social responsibility. Front Public Health. 2022;10:1000628.
Parray ZA, Islam SU, Shah TA. Exploring the effect of workplace incivility on job outcomes: testing the mediating effect of emotional exhaustion. J Organ Eff. 2023;10:161–79.
Parray ZA, Islam SU, Shah TA. Impact of workplace incivility and emotional exhaustion on job outcomes – a study of the higher education sector. Int J Educ Manage. 2023;37:1024–41.
Gustiawan D, Noermijati N, Aisjah S, Indrawati NK, Hendryadi H. The link between workplace incivility, emotional exhaustion, and job embeddedness: examining the moderating role of power distance. J Organ Eff. 2023;10:349–67.
Shoorideh FA, Moosavi S, Balouchi A. Incivility toward nurses: a systematic review and meta-analysis. J Med Ethics Hist Med. 2021;14:2021.
Alyousef SM, Alhamidi SA. Exploring experiences of workplace violence and attempts to address violence among mental health nurses in the Kingdom of Saudi Arabia. SAGE Open Nurs. 2022;8:23779608221142716.
Ota M, Lam L, Gilbert J, Hills D. Nurse leadership in promoting and supporting civility in health care settings: a scoping review. J Nurs Manag. 2022;30:4221–33.
Alquwez N. Association between nurses’ experiences of workplace incivility and the culture of safety of hospitals: a cross-sectional study. J Clin Nurs. 2023;32:320–31.
Download references
Acknowledgements
Not applicable.
Institutional review board statement
This study was carried out with the approval of the General Directorate of Health Affairs, Hail Healthy Cluster, Hail Region / IRB Registration Number with KACST, KSA: H-11–08 L-074 / IRB log number 2023-66.
Informed consent statement
Informed consent was obtained from all participants involved in the study.
The Deanship of Scientific Research funded this work at Jouf University through the Fast-Trace Research Funding Program.
Author information
Authors and affiliations.
College of Nursing, Jouf University, Sakaka, 72388, Saudi Arabia
Nourah Alsadaan & Osama Mohamed Elsayed Ramadan
Department of Nursing, College of Applied Medical Sciences, King Faisal University, Alahsa, Saudi Arabia
Mohammed Alqahtani
You can also search for this author in PubMed Google Scholar
Contributions
O.M.E.R. contributed to the conception and design of the study, recruited patients, collected and analyzed data, interpreted the results, and drafted the manuscript. N.A.A. contributed to the study design, data collection, result analysis and interpretation, and manuscript review. M.A. contributed to patient recruitment, data collection, and manuscript review. All authors approved the final version of the manuscript.
Corresponding authors
Correspondence to Nourah Alsadaan or Osama Mohamed Elsayed Ramadan .
Ethics declarations
Consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Alsadaan, N., Ramadan, O.M.E. & Alqahtani, M. From incivility to outcomes: tracing the effects of nursing incivility on nurse well-being, patient engagement, and health outcomes. BMC Nurs 23 , 325 (2024). https://doi.org/10.1186/s12912-024-01996-9
Download citation
Received : 13 February 2024
Accepted : 07 May 2024
Published : 13 May 2024
DOI : https://doi.org/10.1186/s12912-024-01996-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Nursing incivility
- Workplace mistreatment
- Nurse stress
- Patient engagement
- Health outcomes
- Workplace intervention and healthcare quality
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]

Nursing Research: Importance, Hypothesis, Sampling, Ethics, and Scientific Method
Added on 2023-06-04
About this Document
End of preview
Want to access all the pages? Upload your documents or become a member.
Evidence Based Nursing Research lg ...
Predicting factors of depression and anxiety in mental health nurses lg ..., article analysis and evaluation of research ethics lg ..., nursing research and quantitative studies lg ..., quantitative critique rubric lg ..., self‐weighing and simple dietary advice for overweight and obese pregnant lg ....
International Journal of Nursing Science Practice and Research
- Other Journals
- For Readers
- For Authors
- For Librarians
- Announcements
- JournalsPub Home Page
- Editorial Board
- Publication Ethics & Malpractice Statement
Hypothesis Types and Research
Dennis F. Polit. Nursing Research: Generating and Assessing Evidence for Nursing Practice, 9th edition. New Delhi: Lippincott Williams and Wilkins; 2012, 58–93p.
Nursing Research society of India, Nursing research and statistics, 1st edition. India: Pearson Publication; 2013, 48–51p.
Polit DF, Hungler BP. Nursing Research Principles and Methods. Philadelphia: Lippincott; 1999.
- There are currently no refbacks.

IMAGES
VIDEO
COMMENTS
Medical providers often rely on evidence-based medicine to guide decision-making in practice. Often a research hypothesis is tested with results provided, typically with p values, confidence intervals, or both. Additionally, statistical or research significance is estimated or determined by the investigators. Unfortunately, healthcare providers may have different comfort levels in interpreting ...
The research hypothesis reflects what the researchers hope to show—that there is a difference between the experimental group and the control group. ... The P value isn't the only concept you need to understand to analyze research findings. But it is a very important one. ... The Practice of Nursing Research: Conduct, Critique, and ...
The research/clinical question is in the "background" planning phases of research projects. Meaning, the eventual hypothesis is developed from the research question and/or statement of purpose after a literature review is performed to determine what evidence already exists and establishing the research problem. Hot Tip!
So, Nurse Jory's research purpose is "The purpose of this research study is to explore barriers to appointment attendance.". After the research problem and purpose statement comes the research hypothesis, by identifying the research variables. Research variables are the concepts that are measured, manipulated, or controlled in a study.
Hypothesis. • A hypothesis is a formal statement of the expected relationship between two or more variables in a specified population. • The hypothesis translates the research problem and purpose into a clear explanation or prediction of the expected results or outcomes of the study.
Title, keywords and the authors. The title of a paper should be clear and give a good idea of the subject area. The title should not normally exceed 15 words 2 and should attract the attention of the reader. 3 The next step is to review the key words. These should provide information on both the ideas or concepts discussed in the paper and the ...
A hypothesis (from the Greek, foundation) is a logical construct, interposed between a problem and its solution, which represents a proposed answer to a research question. It gives direction to the investigator's thinking about the problem and, therefore, facilitates a solution. Unlike facts and assumptions (presumed true and, therefore, not ...
Editor's note: This is the 16th article in a series on clinical research by nurses. The series is designed to be used as a resource for nurses to understand the concepts and principles essential to research. Each column will present the concepts that underpin evidence-based practice—from research design to data interpretation.
Often a research hypothesis is tested with results provided, typically with p values, confidence intervals, or both. ... Significance is a term to describe the substantive importance of medical research. ... Understanding statistical significance. Nursing research. 2010 May-Jun:59(3):219-23. doi: 10.1097/NNR.0b013e3181dbb2cc. ...
Hypothesis testing is the process used to evaluate the strength of evidence from the sample and provides a framework for making determinations related to the population, ie, it provides a method for understanding how reliably one can extrapolate observed findings in a sample under study to the larger population from which the sample was drawn ...
1 Introduction: Research in Nursing. Nurses play an increasingly important role in the follow-up of IBD patients. This makes nurses perfectly situated in order to develop and improve clinical practice, not least through their knowledge of the patients' problems or concerns. Research and science have an essential place in our society.
A 2007 study by Woodward and colleagues in the Journal of Research in Nursing found that nurse clinicians engaged in research often perceive a lack of support from nurse managers and resentment from colleagues who see the research as taking them away from clinical practice. The distinction often drawn between nursing research and clinical ...
January 26, 2024. Research is a crucial aspect of nursing practice that significantly impacts patient care, healthcare policies, and the advancement of nursing practices. In this article, we will explore the role of research in nursing and its importance in enhancing clinical practice, patient safety, policy-making, and professional growth.
Research problems and hypotheses are important means for attaining valuable knowledge. They are pointers or guides to such knowledge, or as formulated by Kerlinger ( 1986, p. 19): " … they direct investigation.". There are many kinds of problems and hypotheses, and they may play various roles in knowledge construction.
rela onship between variables. When formula ng a hypothesis deduc ve. reasoning is u lized as it aims in tes ng a theory or rela onships. Finally, hypothesis helps in discussion of ndings and ...
Research concepts, p. 156. Research hypothesis, p. 151. Research objective or aim, p. 145. Research problem, p. 131 ... A research topic is a concept or broad issue that is important to nursing, such as acute pain, chronic pain management, coping with illness, or health promotion. Each topic contains numerous research problems that might be ...
3. Simple hypothesis. A simple hypothesis is a statement made to reflect the relation between exactly two variables. One independent and one dependent. Consider the example, "Smoking is a prominent cause of lung cancer." The dependent variable, lung cancer, is dependent on the independent variable, smoking. 4.
Binoy S. Significance of Hypothesis in Research. Ind J Holist Nurs 2019; 10(1): 31-33. Date of Submission: 2019-08-29 Date of Acceptance: 2019-10-08 INFO ABSTRACT Significance of Hypothesis in ...
Laura Panozzo is the Assistant Director for DNP Executive, PhD, and DNP/PHD Recruitment at Johns Hopkins School of Nursing. She can help you take the next step in your nursing career, contact her at 443-287-7430 or [email protected]. Research is what drives nursing innovation forward, and is an important part of improving health care delivery.
Research objectives & research hypothesis. 1. Examine the relationships between nursing incivility, nurse stress (defined as emotional exhaustion and depersonalization), patient engagement (defined by patient activation levels and adherence to discharge protocols), and health outcomes (defined as 30-day readmission rates and patient satisfaction scores).
This article covers the importance of nursing research, hypothesis, sampling, ethics, and scientific method. It also discusses the methods section, types of research, and principles of ethical conduct. The article is relevant for nursing students and professionals seeking to understand the basics of nursing research.
Hypothesis is nothing but the heat of the research. In the research without hypothesis, research cannot service properly. The researcher question identifies the study concepts and asks how the concepts might be related a hypothesis is the predicted answer. Three basic aspects important in the hypothesis are: difference that we are trying to ...