- Dissertation
- PowerPoint Presentation
- Book Report/Review
- Research Proposal
- Math Problems
- Proofreading
- Movie Review
- Cover Letter Writing
- Personal Statement
- Nursing Paper
- Argumentative Essay
- Research Paper
- Discussion Board Post

How To Write A Strong Obesity Research Paper?

Table of Contents

Obesity is such a disease when the percent of body fat has negative effects on a person’s health. The topic is very serious as obesity poisons the lives of many teens, adults and even children around the whole world.
Can you imagine that according to WHO (World Health Organization) there were 650 million obese adults and 13% of all 18-year-olds were also obese in 2016? And scientists claim that the number of them is continually growing.
There are many reasons behind the problem, but no matter what they are, lots of people suffer from the wide spectrum of consequences of obesity.
Basic guidelines on obesity research paper
Writing any research paper requires sticking to an open-and-shut structure. It has three basic parts: Introduction, Main Body, and Conclusion.
According to the general rules, you start with the introduction where you provide your reader with some background information and give brief definitions of terms used in the text. Next goes the thesis of your paper.
The thesis is the main idea of all the research you’ve done written in a precise and simple manner, usually in one sentence.
The main body is where you present the statements and ideas which disclose the topic of your research.
In conclusion, you sum up all the text and make a derivation.
How to write an obesity thesis statement?
As I’ve already noted, the thesis is the main idea of your work. What is your position? What do you think about the issue? What is that you want to prove in your essay?
Answer one of those questions briefly and precisely.
Here are some examples of how to write a thesis statement for an obesity research paper:
- The main cause of obesity is determined to be surfeit and unhealthy diet.
- Obesity can be prevented no matter what genetic penchants are.
- Except for being a problem itself, obesity may result in diabetes, cancers, cardiovascular diseases, and many others.
- Obesity is a result of fast-growing civilization development.
- Not only do obese people have health issues but also they have troubles when it comes to socialization.

20 top-notch obesity research paper topics
Since the problem of obesity is very multifaceted and has a lot of aspects to discover, you have to define a topic you want to cover in your essay.
How about writing a fast food and obesity research paper or composing a topic in a sphere of fast food? Those issues gain more and more popularity nowadays.
A couple of other decent ideas at your service.
- The consequences of obesity.
- Obesity as a mental problem.
- Obesity and social standards: the problem of proper self-fulfilment.
- Overweight vs obesity: the use of BMI (Body Mass Index).
- The problem of obesity in your country.
- Methods of prevention the obesity.
- Is lack of self-control a principal factor of becoming obese?
- The least obvious reasons for obesity.
- Obesity: the history of the disease.
- The effect of mass media in augmentation of the obesity level.
- The connection between depression and obesity.
- The societal stigma of obese people.
- The role of legislation in reducing the level of obesity.
- Obesity and cultural aspect.
- Who has the biggest part of the responsibility for obesity: persons themselves, local authorities, government, mass media or somebody else?
- Why are obesity rates constantly growing?
- Who is more prone to obesity, men or women? Why?
- Correlation between obesity and life expectancy.
- The problem of discrimination of the obese people at the workplace.
- Could it be claimed that such movements as body-positive and feminism encourage obesity to a certain extent?
Best sample of obesity research paper outline
An outline is a table of contents which is made at the very beginning of your writing. It helps structurize your thoughts and create a plan for the whole piece in advance.
…Need a sample?
Here is one! It fits the paper on obesity in the U.S.
Introduction
- Hook sentence.
- Thesis statement.
- Transition to Main Body.
- America’s modern plague: obesity.
- Statistics and obesity rates in America.
- Main reasons of obesity in America.
- Social, cultural and other aspects involved in the problem of obesity.
- Methods of preventing and treating obesity in America.
- Transition to Conclusion.
- Unexpected twist or a final argument.
- Food for thought.
Specifics of childhood obesity research paper

A separate question in the problem of obesity is overweight children.
It is singled out since there are quite a lot of differences in clinical pictures, reasons and ways of treatment of an obese adult and an obese child.
Writing a child obesity research paper requires a more attentive approach to the analysis of its causes and examination of family issues. There’s a need to consider issues like eating habits, daily routine, predispositions and other.
Top 20 childhood obesity research paper topics
We’ve gathered the best ideas for your paper on childhood obesity. Take one of those to complete your best research!
- What are the main causes of childhood obesity in your country?
- Does obesity in childhood increase the chance of obesity in adulthood?
- Examine whether a child’s obesity affects academic performance.
- Are parents always guilty if their child is obese?
- What methods of preventing childhood obesity are used in your school?
- What measures the government can take to prevent children’s obesity?
- Examine how childhood obesity can result in premature development of chronic diseases.
- Are obese or overweight parents more prone to have an obese child?
- Why childhood obesity rates are constantly growing around the whole world?
- How to encourage children to lead a healthy style of life?
- Are there more junk and fast food options for children nowadays? How is that related to childhood obesity rates?
- What is medical treatment for obese children?
- Should fast food chains have age limits for their visitors?
- How should parents bring up their child in order to prevent obesity?
- The problem of socializing in obese children.
- Examine the importance of a proper healthy menu in schools’ cafeterias.
- Should the compulsory treatment of obese children be started up?
- Excess of care as the reason for childhood obesity.
- How can parents understand that their child is obese?
- How can the level of wealth impact the chance of a child’s obesity?
Childhood obesity outline example
As the question of childhood obesity is a specific one, it would differ from the outline on obesity we presented previously.
Here is a sample you might need. The topic covers general research on child obesity.
- The problem of childhood obesity.
- World’s childhood obesity rates.
- How to diagnose the disease.
- Predisposition and other causes of child obesity.
- Methods of treatment for obese children.
- Preventive measures to avoid a child’s obesity.
On balance…
The topic of obesity is a long-standing one. It has numerous aspects to discuss, sides to examine, and data to analyze.
Any topic you choose might result in brilliant work.
How can you achieve that?
Follow the basic requirements, plan the content beforehand, and be genuinely interested in the topic.
Option 2. Choose free time over struggle on the paper. We’ve got dozens of professional writers ready to help you out. Order your best paper within several seconds and enjoy your free time. We’ll cover you up!

How to Write a Cleanliness Essay
Why is a ‘how to write assignment’ request too common among learners.

Steps To Follow While Writing An Essay On Climate Change
Obesity Essay
Last updated on: Feb 9, 2023
Obesity Essay: A Complete Guide and Topics
By: Nova A.
11 min read
Reviewed By: Jacklyn H.
Published on: Aug 31, 2021

Are you assigned to write an essay about obesity? The first step is to define obesity.
The obesity epidemic is a major issue facing our country right now. It's complicated- it could be genetic or due to your environment, but either way, there are ways that you can fix it!
Learn all about what causes weight gain and get tips on how you can get healthy again.

On this Page
What is Obesity
What is obesity? Obesity and BMI (body mass index) are both tools of measurement that are used by doctors to assess body fat according to the height, age, and gender of a person. If the BMI is between 25 to 29.9, that means the person has excess weight and body fat.
If the BMI exceeds 30, that means the person is obese. Obesity is a condition that increases the risk of developing cardiovascular diseases, high blood pressure, and other medical conditions like metabolic syndrome, arthritis, and even some types of cancer.
Obesity Definition
Obesity is defined by the World Health Organization as an accumulation of abnormal and excess body fat that comes with several risk factors. It is measured by the body mass index BMI, body weight (in kilograms) divided by the square of a person’s height (in meters).
Obesity in America
Obesity is on the verge of becoming an epidemic as 1 in every 3 Americans can be categorized as overweight and obese. Currently, America is an obese country, and it continues to get worse.

Paper Due? Why Suffer? That's our Job!
Causes of obesity
Do you see any obese or overweight people around you?
You likely do.
This is because fast-food chains are becoming more and more common, people are less active, and fruits and vegetables are more expensive than processed foods, thus making them less available to the majority of society. These are the primary causes of obesity.
Obesity is a disease that affects all age groups, including children and elderly people.
Now that you are familiar with the topic of obesity, writing an essay won’t be that difficult for you.
How to Write an Obesity Essay
The format of an obesity essay is similar to writing any other essay. If you need help regarding how to write an obesity essay, it is the same as writing any other essay.
Obesity Essay Introduction
The trick is to start your essay with an interesting and catchy sentence. This will help attract the reader's attention and motivate them to read further. You don’t want to lose the reader’s interest in the beginning and leave a bad impression, especially if the reader is your teacher.
A hook sentence is usually used to open the introductory paragraph of an essay in order to make it interesting. When writing an essay on obesity, the hook sentence can be in the form of an interesting fact or statistic.
Head on to this detailed article on hook examples to get a better idea.
Once you have hooked the reader, the next step is to provide them with relevant background information about the topic. Don’t give away too much at this stage or bombard them with excess information that the reader ends up getting bored with. Only share information that is necessary for the reader to understand your topic.
Next, write a strong thesis statement at the end of your essay, be sure that your thesis identifies the purpose of your essay in a clear and concise manner. Also, keep in mind that the thesis statement should be easy to justify as the body of your essay will revolve around it.
Body Paragraphs
The details related to your topic are to be included in the body paragraphs of your essay. You can use statistics, facts, and figures related to obesity to reinforce your thesis throughout your essay.
If you are writing a cause-and-effect obesity essay, you can mention different causes of obesity and how it can affect a person’s overall health. The number of body paragraphs can increase depending on the parameters of the assignment as set forth by your instructor.
Start each body paragraph with a topic sentence that is the crux of its content. It is necessary to write an engaging topic sentence as it helps grab the reader’s interest. Check out this detailed blog on writing a topic sentence to further understand it.
End your essay with a conclusion by restating your research and tying it to your thesis statement. You can also propose possible solutions to control obesity in your conclusion. Make sure that your conclusion is short yet powerful.
Obesity Essay Examples
Essay about Obesity (PDF)
Childhood Obesity Essay (PDF)
Obesity in America Essay (PDF)
Essay about Obesity Cause and Effects (PDF)
Satire Essay on Obesity (PDF)
Obesity Argumentative Essay (PDF)
Obesity Essay Topics
Choosing a topic might seem an overwhelming task as you may have many ideas for your assignment. Brainstorm different ideas and narrow them down to one, quality topic.
If you need some examples to help you with your essay topic related to obesity, dive into this article and choose from the list of obesity essay topics.
Childhood Obesity
As mentioned earlier, obesity can affect any age group, including children. Obesity can cause several future health problems as children age.
Here are a few topics you can choose from and discuss for your childhood obesity essay:
- What are the causes of increasing obesity in children?
- Obese parents may be at risk for having children with obesity.
- What is the ratio of obesity between adults and children?
- What are the possible treatments for obese children?
- Are there any social programs that can help children with combating obesity?
- Has technology boosted the rate of obesity in children?
- Are children spending more time on gadgets instead of playing outside?
- Schools should encourage regular exercises and sports for children.
- How can sports and other physical activities protect children from becoming obese?
- Can childhood abuse be a cause of obesity among children?
- What is the relationship between neglect in childhood and obesity in adulthood?
- Does obesity have any effect on the psychological condition and well-being of a child?
- Are electronic medical records effective in diagnosing obesity among children?
- Obesity can affect the academic performance of your child.
- Do you believe that children who are raised by a single parent can be vulnerable to obesity?
- You can promote interesting exercises to encourage children.
- What is the main cause of obesity, and why is it increasing with every passing day?
- Schools and colleges should work harder to develop methodologies to decrease childhood obesity.
- The government should not allow schools and colleges to include sweet or fatty snacks as a part of their lunch.
- If a mother is obese, can it affect the health of the child?
- Children who gain weight frequently can develop chronic diseases.
Obesity Argumentative Essay Topics
Do you want to write an argumentative essay on the topic of obesity?
The following list can help you with that!
Here are some examples you can choose from for your argumentative essay about obesity:
- Can vegetables and fruits decrease the chances of obesity?
- Should you go for surgery to overcome obesity?
- Are there any harmful side effects?
- Can obesity be related to the mental condition of an individual?
- Are parents responsible for controlling obesity in childhood?
- What are the most effective measures to prevent the increase in the obesity rate?
- Why is the obesity rate increasing in the United States?
- Can the lifestyle of a person be a cause of obesity?
- Does the economic situation of a country affect the obesity rate?
- How is obesity considered an international health issue?
- Can technology and gadgets affect obesity rates?
- What can be the possible reasons for obesity in a school?
- How can we address the issue of obesity?
- Is obesity a chronic disease?
- Is obesity a major cause of heart attacks?
- Are the junk food chains causing an increase in obesity?
- Do nutritional programs help in reducing the obesity rate?
- How can the right type of diet help with obesity?
- Why should we encourage sports activities in schools and colleges?
- Can obesity affect a person’s behavior?
Health Related Topics for Research Paper
If you are writing a research paper, you can explain the cause and effect of obesity.
Here are a few topics that link to the cause and effects of obesity.Review the literature of previous articles related to obesity. Describe the ideas presented in the previous papers.
- Can family history cause obesity in future generations?
- Can we predict obesity through genetic testing?
- What is the cause of the increasing obesity rate?
- Do you think the increase in fast-food restaurants is a cause of the rising obesity rate?
- Is the ratio of obese women greater than obese men?
- Why are women more prone to be obese as compared to men?
- Stress can be a cause of obesity. Mention the reasons how mental health can be related to physical health.
- Is urban life a cause of the increasing obesity rate?
- People from cities are prone to be obese as compared to people from the countryside.
- How obesity affects the life expectancy of people? What are possible solutions to decrease the obesity rate?
- Do family eating habits affect or trigger obesity?
- How do eating habits affect the health of an individual?
- How can obesity affect the future of a child?
- Obese children are more prone to get bullied in high school and college.
- Why should schools encourage more sports and exercise for children?
Tough Essay Due? Hire Tough Writers!
Topics for Essay on Obesity as a Problem
Do you think a rise in obesity rate can affect the economy of a country?
Here are some topics for your assistance regarding your economics related obesity essay.
- Does socioeconomic status affect the possibility of obesity in an individual?
- Analyze the film and write a review on “Fed Up” – an obesity epidemic.
- Share your reviews on the movie “The Weight of The Nation.”
- Should we increase the prices of fast food and decrease the prices of fruits and vegetables to decrease obesity?
- Do you think healthy food prices can be a cause of obesity?
- Describe what measures other countries have taken in order to control obesity?
- The government should play an important role in controlling obesity. What precautions should they take?
- Do you think obesity can be one of the reasons children get bullied?
- Do obese people experience any sort of discrimination or inappropriate behavior due to their weight?
- Are there any legal protections for people who suffer from discrimination due to their weight?
- Which communities have a higher percentage of obesity in the United States?
- Discuss the side effects of the fast-food industry and their advertisements on children.
- Describe how the increasing obesity rate has affected the economic condition of the United States.
- What is the current percentage of obesity all over the world? Is the obesity rate increasing with every passing day?
- Why is the obesity rate higher in the United States as compared to other countries?
- Do Asians have a greater percentage of obese people as compared to Europe?
- Does the cultural difference affect the eating habits of an individual?
- Obesity and body shaming.
- Why is a skinny body considered to be ideal? Is it an effective way to reduce the obesity rate?
Obesity Solution Essay Topics
With all the developments in medicine and technology, we still don’t have exact measures to treat obesity.
Here are some insights you can discuss in your essay:
- How do obese people suffer from metabolic complications?
- Describe the fat distribution in obese people.
- Is type 2 diabetes related to obesity?
- Are obese people more prone to suffer from diabetes in the future?
- How are cardiac diseases related to obesity?
- Can obesity affect a woman’s childbearing time phase?
- Describe the digestive diseases related to obesity.
- Obesity may be genetic.
- Obesity can cause a higher risk of suffering a heart attack.
- What are the causes of obesity? What health problems can be caused if an individual suffers from obesity?
- What are the side effects of surgery to overcome obesity?
- Which drugs are effective when it comes to the treatment of obesity?
- Is there a difference between being obese and overweight?
- Can obesity affect the sociological perspective of an individual?
- Explain how an obesity treatment works.
- How can the government help people to lose weight and improve public health?
Writing an essay is a challenging yet rewarding task. All you need is to be organized and clear when it comes to academic writing.
- Choose a topic you would like to write on.
- Organize your thoughts.
- Pen down your ideas.
- Compose a perfect essay that will help you ace your subject.
- Proofread and revise your paper.
Were the topics useful for you? We hope so!
However, if you are still struggling to write your paper, you can pick any of the topics from this list, and our essay writer will help you craft a perfect essay.
Are you struggling to write an effective essay?
If writing an essay is the actual problem and not just the topic, you can always hire an essay writing service for your help. Essay experts at 5StarEssays can help compose an impressive essay within your deadline.
All you have to do is contact us. We will get started on your paper while you can sit back and relax.
Place your order now to get an A-worthy essay.

Marketing, Thesis
As a Digital Content Strategist, Nova Allison has eight years of experience in writing both technical and scientific content. With a focus on developing online content plans that engage audiences, Nova strives to write pieces that are not only informative but captivating as well.
Was This Blog Helpful?
Keep reading.
- How to Write A Bio – Professional Tips and Examples

- Learn How to Write an Article Review with Examples

- How to Write a Poem Step-by-Step Like a Pro

- How To Write Poetry - 7 Fundamentals and Tips

- Know About Appendix Writing With the Help of Examples

- List of Social Issues Faced By the World

- How To Write A Case Study - Easy Guide

- Learn How to Avoid Plagiarism in 7 Simple Steps

- Writing Guide of Visual Analysis Essay for Beginners

- Learn How to Write a Personal Essay by Experts

- Character Analysis - A Step By Step Guide

- Thematic Statement: Writing Tips and Examples

- Expert Guide on How to Write a Summary

- How to Write an Opinion Essay - Structure, Topics & Examples

- How to Write a Synopsis - Easy Steps and Format Guide

- Learn How To Write An Editorial By Experts

- How to Get Better at Math - Easy Tips and Tricks

- How to Write a Movie Review - Steps and Examples

- Creative Writing - Easy Tips For Beginners

- Types of Plagiarism Every Student Should Know

People Also Read
- writing reflective essay
- 10essential essay writing techniques for students
- reflective essay topics
- essay writing skills
- analytical essay writing
Burdened With Assignments?
Advertisement
- Homework Services: Essay Topics Generator
© 2024 - All rights reserved
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 07 May 2024
Epidemiology and Population Health
Obesity: a 100 year perspective
- George A. Bray ORCID: orcid.org/0000-0001-9945-8772 1
International Journal of Obesity ( 2024 ) Cite this article
737 Accesses
23 Altmetric
Metrics details
- Biological techniques
- Health care
- Weight management
This review has examined the scientific basis for our current understanding of obesity that has developed over the past 100 plus years. Obesity was defined as an excess of body fat. Methods of establishing population and individual changes in levels of excess fat are discussed. Fat cells are important storage site for excess nutrients and their size and number affect the response to insulin and other hormones. Obesity as a reflection of a positive fat balance is influenced by a number of genetic and environmental factors and phenotypes of obesity can be developed from several perspectives, some of which have been elaborated here. Food intake is essential for maintenance of human health and for the storage of fat, both in normal amounts and in obesity in excess amounts. Treatment approaches have taken several forms. There have been numerous diets, behavioral approaches, along with the development of medications.. Bariatric/metabolic surgery provides the standard for successful weight loss and has been shown to have important effects on future health. Because so many people are classified with obesity, the problem has taken on important public health dimensions. In addition to the scientific background, obesity through publications and organizations has developed its own identity. While studying the problem of obesity this reviewer developed several aphorisms about the problem that are elaborated in the final section of this paper.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
251,40 € per year
only 20,95 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Obesity and the risk of cardiometabolic diseases

Obesity-induced and weight-loss-induced physiological factors affecting weight regain
Normal weight obesity and unaddressed cardiometabolic health risk—a narrative review
Quetelet, Adolphe Sur l’homme et le developpement de ses facultes, ou essai de physique sociale ; Paris: Bachelier, 1835 (Transl of L-A-J. A Treatise on Man and the Development of His Faculties. IN: Bray GA. The Battle of the Bulge: A History of Obesity Research . Pittsburgh: Dorrance Publishing, 2007 pp 423-36.
Bray GA. Quetelet: quantitative medicine. Obes Res. 1994;2:68–71.
Article CAS PubMed Google Scholar
Bray GA. Beyond BMI. Nutrients. 2023;15:2254.
Article PubMed PubMed Central Google Scholar
Flegal KM. Use and misuse of BMI categories. AMA J Ethics. 2023;25:E550–8.
Article PubMed Google Scholar
Keys A, Fidanza F, Karvonen MJ, Kimura N, Taylor HL. Indices of relative weight and obesity. J Chr Diseases. 1972;25:329–43.
Article CAS Google Scholar
Bray GA. Definition, measurement, and classification of the syndromes of obesity. Int J Obes. 1978;2:99–112.
CAS PubMed Google Scholar
Garrow JS. Treat Obesity Seriouslv-A Clinical Manual . Edinburgh: Churchill Livingstone; 1981.
Rodgers A, Woodward A, Swinburn B, Dietz WH. Prevalence trends tell us what did not precipitate the US obesity epidemic. Lancet Public Health. 2018;3:e162–3.
Bray GA. Body fat distribution and the distribution of scientific knowledge. Obes Res. 1996;4:189–92.
Janssen I, Katzmarzyk PT, Ross R. Waist circumference and not body mass index explains obesity-related health risk. Am J Clin Nutr. 2004;79:379–84.
Weeks RW. An experiment with the specialized investigation. Actuar Soc Am Trans. 1904;8:17–23.
Google Scholar
Vague J. La differenciation sexuelle facteur determinant des formes de l’obesite, Presse Medicale. 1947;55:339 340. [Translated. IN: Bray GA. The Battle of the Bulge: A History of Obesity Research . Pittsburgh: Dorrance Publishing, 2007 pp 693–5].
Vague J. The degree of masculine differentiation of obesities: a factor determining predisposition to diabetes, atherosclerosis, gout, and uric calculous disease. Am J Clin Nutr. 1956;4:20–34.
Larsson B, Svardsudd K, Welin L, Wihelmsen L, Bjorntorp P, Tibbllne G. Abdominal adipose tissue distribution, obesity and risk of cardiovascular disease and death: 13 year follow up of participants in the study of 792 men born in 1913. BMJ 1984;288:1401–4.
Article CAS PubMed PubMed Central Google Scholar
Bjorntorp P. Visceral obesity: a “civilization syndrome. Obes Res. 1993;1:206–22.
Behnke AR, Feen BG, Welham WC. The specific gravity of healthy men. JAMA 1942;118:495–8.
Article Google Scholar
Roentgen WC. Ueber eine neue Art von Strahlen. S.B. Phys-med Ges Wurzburg. 1895;132–41.
Wong MC, Bennett JP, Leong LT, Tian IY, Liu YE, Kelly NN, et al. Monitoring body composition change for intervention studies with advancing 3D optical imaging technology in comparison to dual-energy X-ray absorptiometry. Am J Clin Nutr. 2023:S0002-9165(23)04152-7
Church TS, Thomas DM, Tudor-Locke C, Katzmarzyk PT, Earnest CP, Rodarte RQ, et al. Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLoS ONE. 2011;6:e19657 https://doi.org/10.1371/journal.pone.0019657 .
Schwann TH; Smith H, Trans. Microsccopical researches into the accordance in the structure and growth of animals and plants . London: Sydenham Society 1847
Hassall A. Observations on the development of the fat vesicle. Lancet. 1849;1:163–4.
Hirsch J, Knittle JL. Cellularity of human obese and nonobese adipose tissue. Fed Proc. 1970;29:1516–21.
Garvey WT. New Horizons. A new paradigm for treating to target with second-generation obesity medications. JCEM. 2022;107:e1339–47.
Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM. Positional cloning of the mouse obese gene and its human homologue. Nature. 1994;372:425–32.
Lavoisier AL, DeLaPlace PS. Memoir on Heat. Read to the Royal Academy of Sciences 28 June 1783 [IN: Bray GA. The Battle of the Bulge: A History of Obesity Research . Pittsburgh: Dorrance Publishing, 2007 pp 498–512].
Bray GA. Lavoisier and Scientific Revolution: The oxygen theory displaces air, fire, earth and water. Obes Res. 1994;2:183–8.
Helmholtz, Hermann von. Uber die Erhaltung der Kraft, ein physikalische Abhandlung, vorgetragen in der Sitzung der physicalischen Gesellschaft zu Berlin am 23sten Juli 1847. Berlin: G. Reimer, 1847.
Bray GA. Commentary on Atwater classic. Obes Res. 1993;1:223–7.
Bray GA. Energy expenditure using doubly labeled water: the unveiling of objective truth. Obes Res. 1997;5:71–7.
Lifson N, Gordon GB, McClintock R. Measurement of total carbon dioxide production by means of D 2 0 18 . J Appl Physiol. 1955;7:704–10.
Lichtman SW, Pisarska K, Berman ER, Pestone M, Dowling H, Offenbacher E, et al. Discrepancy between self-reported and actual caloric intake and exercise in obese subjects. N Engl J Med. 1992;327(Dec):1893–8.
Bray GA. Commentary on classics of obesity 4. Hypothalamic obesity. Obes Res. 1993;1:325–8.
Bruch H. The froehlich syndrome: report of the original case. Am J Dis Child. 1939;58:1281–90.
Babinski JP. Tumeur du corps pituitaire sans acromegalie et arret de development des organs genitaux. Rev Neurol. 1900;8:531–3. [Translation IN: Bray GA. The Battle of the Bulge: A History of Obesity Research . Pittsburgh: Dorrance Publishing, 2007 pp 740–1]
Cushing H. The Pituitary Body and Its Disorders . Philadelphia. PA: JB Lippincott; 1912.
Bray GA. Laurence, moon, Bardet Biedl: reflect a syndrome. Obes Res. 1995;3:383–6.
Laurence JZ, Moon RC. Four cases of “Retinitis Pigmentosa,” Occurring in the same family, and accompanied by general imperfections of development. Opthalmol Rev. 1866;2:32–41.
Bardet G. Sur un Syndrome d’Obesity Conginitale avec Polydactylie et Retinite Pigmentaire (Contribution a l’etude des formes clinique de 1 ’Obesite hypophysaire) . Paris: 1920. Thesis [Translation IN: Bray GA. The Battle of the Bulge: A History of Obesity Research . Pittsburgh: Dorrance Publishing, 2007 pp 740–1].
Biedl A. Geschwisterpaar mit adiposo-genitaler Dystrophie. Dtsch Med Woche. 1922;48:1630.
Cuenot L. Pure strains and their combinations in the mouse. Arch Zoot Exptl Gen. 1905;122:123.
Ingalls AM, Dickie MM, Snell GD. Obese, new mutation in the mouse. J Hered. 1950;41:317–8.
Coleman DL. Obesity and diabetes: two mutant genescausing obesity-obesity syndromes in mice. Diabetalogia. 1978;14:141–8.
Zucker TF, Zucker LM. Fat accretion and growth in the rat. J Nutr. 1963;80:6–20.
Schwartz MW, Seeley RJ, Zeltser LM, Drewnowski A, Ravussin E, Redman LM, et al. Obesity pathogenesis: an endocrine society scientific statement. Endocr Rev. 2017;38:267–96.
Oral EA, Simha V, Ruiz E, Andewelt A, Premkumar A, Snell P, et al. Leptin-replacement therapy for lipodystrophy. N Engl J Med. 2002;346:570–8.
Loos RJF, Yeo GSH. The genetics of obesity: from discovery to biology. Nat Rev Genet. 2022;23:120–33.
Blüher M. Metabolically healthy obesity. Endocr Rev. 2020;41:405–20.
Acosta A, Camilleri M, Abu Dayyeh B, Calderon G, Gonzalez D, McRae A, et al. Selection of antiobesity medications based on phenotypes enhances weight loss: a pragmatic trial in an obesity clinic. Obes. 2021;29:662–71.
Bray GA. Commentary on classics in obesity. 6. Science and politics of hunger. Obes Res. 1993;19:489–93.
Cannon WB, Washburn AL. An explanation of hunger. Am J Physiol. 1912;29:441–54.
Carlson AJ. Contributions to the physiology of the stomach -II. the relation between the concentrations of the empty stomach and the sensation of hunger. Am J Physiol. 1912;31:175–92.
Carlson AJ. Control of Hunger in Health and Disease . Chicago, IL: University of Chicago Press; 1916.
Flint A, Raben A, Astrup A, Holst JJ. Glucagon-like peptide 1 promotes satiety and suppresses energy intake in humans. J Clin Invest. 1998;101:515–20.
Bray GA. Eat slowly - From laboratory to clinic; behavioral control of eating. Obes Res. 1996;4:397–400.
Pavlov IP; Thompson WH, trans. The Work of the Digestive Glands . London: Charles Griffin and Co.; 1910.
Skinner BF. Contingencies of Reinforcement: A Theoretical Analysis . New York: Meredith Corporation; 1969.
Ferster CB, Nurenberger JI, Levitt EG. The Control of Eating. J. Math 1964;1:87-109.
Stuart RB. Behavioral control of overeating. Behav Res Ther. 1967;5:357–65. [Also IN: Bray GA. The Battle of the Bulge: A History of Obesity Research . Pittsburgh: Dorrance Publishing, 2007 pp 793–9]
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM. et a; Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(Feb):393–403.
The Look AHEAD Research Group, Wadden TA, Bantle JP, Blackburn GL, Bolin P, Brancati FL, Bray GA, et al. Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity. 2014;22:5–13.
Bray GA, Suminska M. From Hippocrates to the Obesity Society: A Brief History. IN Handbook of Obesity (Bray GA, Bouchard C, Katzmarzyk P, Kirwan JP, Redman LM, Schauer PL eds). Boca Raton: Taylor & Francis 2024. Vol 2, pp 3–16.
Bray GA. Commentary on Banting Letter. Obes Res. 1993;1:148–52.
Banting W. Letter on Corpulence, Addressed to the Public . London: Harrison and Sons 1863. pp 1–21.
Harvey W. On corpulence in relation to disease” With some remarks of diet . London” Henry Renshaw, 1872.
Schwartz, H. Never Satisfied. A Cultural History of Diets, Fantasies and Fat . 1977.
Foxcroft, Louise. Calories and Corsets. A history of dieting over 2000 years . London: Profile Books, 2011.
Gilman, Sander L. Obesity. The Biography . Oxford: Oxford University Press, 2010.
Linn R Stuart SL. The Last Chance Diet . A Revolutionary New Approach to Weight Loss 1977.
Magendie F. Rapport fait a l’Academie des Sciences au le nom de la Commission diet la gelatine. C.R. Academie Sci (Paris) 1841:237-83.
Bray GA. “The Science of Hunger: Revisiting Two Theories of Feeding. IN Bray GA. The Battle of the Bulge. A History of Obesity Research . Pittsburgh, Dorrance Publishing 1977 p. 238.
Sours HE, Frattalli VP, Brand CD, et al. Sudden death associated with very low calorie weight regimes. Am J Clin Nutr. 1981;34:453–61.
Bray GA. From very-low-energy diets to fasting and back. Obes Res. 1995;3:207–9.
Benedict, F.G. A Study of prolonged fasting . Washington: Carnegie Institution of Washington (Publ No 203), 1915.
Keys A, Brozek J, Henschel A, Mickelsen O,Taylor HL. The biology of human starvation . Minneapolis: University of Minnesota Press, 1950.
Cahill GF Jr, Herrera MG, Morgan AP, Soeldner JS, Steinke J, Levy PL, et al. Hormone-fuel interrelationships during fasting. J Clin Invest. 1966;45:1751–69.
Benedict FG, Miles WR, Roth P, Smith HM. Human vitality and efficiency under prolonged restricted diet. Carnegie Instit Wash, Pub. No. 280. Washington: Carnegie Institution of Washington; 1919.
Evans FA, Strang JM. The treatment of obesity with low-calorie diets. JAMA 1931;97:1063–8.
Bloom WL. Fasting as an introduction to the treatment of obesity. Metabolism 1959;8:2 14–220.
CAS Google Scholar
Bray GA, Purnell JQ. An historical review of steps and missteps in the discovery of anti-obesity drugs. IN: Feingold KR, Anawalt B, Boyce A, Chrousos G, de Herder WW, Dhatariya K, Dungan K, et al. editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2022.
Lesses MF, Myerson A. Human autonomic pharmacology. NEJM 1938;218:119-24.
Cohen PA, Goday A, Swann JP. The return of rainbow diet pills. Am J Public Health. 2012;102:1676–86.
Bray GA. Nutrient intake is modulated by peripheral peptide administration. Obes Res. 1995;3:569S–572S.
Kissileff HR, Pi-Sunyer FX, Thornton J, Smith GP. C-terminal octapeptide of cholecystokinin decreases food intake in man. Am J Clin Nutr. 1981;34:154–60.
Wilding JPH, Batterham RL, Calanna S, Davies M, Van Gaal LF, Lingvay I, et al. STEP 1 study group. Once-weekly semaglutide in adults with overweight or obesity. N Engl J Med. 2021;384:989–1002.
Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jódar E, Leiter LA, et al. SUSTAIN-6 investigators. semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375:1834–44.
Jastreboff AM, Aronne LJ, Ahmad NN, Wharton S, Connery L, Alves B, et al. SURMOUNT-1 investigators. tirzepatide once weekly for the treatment of obesity. N. Engl J Med. 2022;387:205–16.
Jastreboff AM, Kaplan LM, Frías JP, Wu Q, Du Y, Gurbuz S, et al. Retatrutide phase 2 obesity trial investigators. Triple-hormone-receptor agonist retatrutide for obesity - a phase 2 trial. N Engl J Med. 2023;389:514–26.
Bray GA. Obesity and surgery for a chronic disease. Obes Res. 1996;4:301–3.
Kremen AJ, Linner JH, Nelson CH. An experimental evaluation of the nutritional importance of proximal and distal small intestine. Ann Surg. 1954;140:439–48.
Payne JH, DeWind LT, Commons RR. Metabolic observations in patients with jejuno-colic shunts. Am J Surg. 1963;106:273–89.
Payne JH, DeWind LT. Surgical treatment of obesity. Am J Surg. 1969;118:141–6.
Buchwald H, Varco RL. Partial ileal bypass for hypercholesterolemia and atherosclerosis. Surg Gynecol Obstet. 1967;124:1231.
Mason EE, Ito C. Gastric bypass in obesity. Surg Clin North Am. 1967;47:1345–135.
O’Brien PE, MacDonald L, Anderson M, Brennan L, Brown WA. Long-term outcomes after bariatric surgery: fifteen-year follow-up of adjustable gastric banding and a systematic review of the bariatric surgical literature. Ann Surg. 2013;257:87–94.
Arterburn D, Wellman R, Emiliano A, Smith SR, Odegaard AO, Murali S, et al. PCORnet bariatric study collaborative. Comparative effectiveness and safety of bariatric procedures for weight loss: a PCORnet cohort study. Ann Intern Med. 2018;169:741–50.
Picot J, Jones J, Colquitt JL, Gospodarevskaya E, Loveman E, Baxter L, et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess. 2009;13:1–190.
Christou NV, Sampalis JS, Liberman M, et al. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg. 2004;240:416–23.
Sjöström L. Review of the key results from the Swedish Obese Subjects (SOS) trial - a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013;273:219–34.
Sjöström L. Swedish Obese Subjects, SOS: A review of results from a prospective controlled intervention trial. In: Bray GA, Bochard C, eds. Handbook of Obesity, Volume 2: Clinical Applications. New York: Informa; 2014.
Sjöström L, Narbro K, Sjöström CD, Karason K, Larsson B, Wedel H, et al. Effects of bariatric surgery on mortality in Swedish Obese Subjects. N. Engl J Med. 2007;357:741–52.
Sjöström L, Peltonen M, Jacobson P, Sjöström CD, Karason K, Wedel H, et al. Bariatric surgery and long-term cardiovascular events. JAMA 2012;307:56–65.
Carlsson LM, Peltonen M, Ahlin S, Anveden Å, Bouchard C, Carlsson B, et al. Bariatric surgery and prevention of type 2 diabetes in Swedish Obese Subjects. The New England. J Med. 2012;367:695–704.
Pories WJ, Swanson MS, MacDonald KG, Long SB, Morris PG, Brown BM, et al. Who would have thought it? an operation proves to be the most effective therapy for adult-onset. Diabetes Mellit Ann Surg. 1995;222:339–52.
Bray GA. Life insurance and overweight. Obes Res. 1995;3:97–99.
The Association of Life Insurance Medical Directors and The Actuarial Society of America. Medico- Actuarial Mortality Investigation . New York: The Association of Life Insurance Medical Directors and ‘The Actuarial Society of America; 1913.
Keys A. Seven Countries: A Multivariate Analysis of Death and Coronary Heart Disease . Cambridge, MA: Harvard University Press; 1980.
Dawber TR. The Framingham Study: The Epidemiology of Atherosclerotic Disease . Cambridge, MA: Harvard University Press; 1980.
Bray, G.A. (Ed), Obesity in Perspective . Fogarty International Center Series on Preventive Med. Vol 2, parts 1 and 2, Washington, D.C.: U.S. Govt Prtg Office, 1976, DHEW Publication #75-708.
Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among adults aged 20 and over: United States, 1960–1962 through 2017–2018. NCHS Health E-Stats. 2020.
Bray GA. Obesity: Historical development of scientific and cultural ideas. Int J Obes. 1990;14:909–26.
Bray GA. The Battle of the Bulge: A History of Obesity Research . Pittsburgh: Dorrance Publishing, 2007 p 30.
Short, T. A Discourse Concerning the Causes and Effects of Corpulency Together with the Method for Its Prevention and Cure , J. Robert, London, 1727.
Flemyng, M. A Discourse on the Nature, Causes and Cure of Corpulency , L Davis and C Reymers, London, 1760.
Wadd, W. Comments on corpulency lineaments of leanness mems on diet and dietetics. London: John Ebers and Co, 1829.
Chambers, TK. Corpulence, or excess fat in the human body. London: Longman, 1850.
Rony HR. Obesity and Leanness . Philadelphia: Lea and Febiger, 1940.
Rynearson EH, Gastineau CF. Obesity . Springfield, IL: Charles C. Thomas, 1949.
Bray, G.A. The Obese Patient. Major Problems in Internal Medicine , Vol 9, Philadelphia, Pa.: W.B. Saunders Company, 1976, pp. 1-450.
Bray G.A. A Guide to Obesity and the Metabolic Syndrome: Origins and Treatment . New York: CRC Press: Taylor and Francis Group. 2011.
Howard AN. The history of the association for the study of obesity. Intern J Obes. 1992;16:S1–8.
Bray GA, Greenwood MRC, Hansen BC. The obesity society is turning 40: a history of the early years. Obesity. 2021;29(Dec):1978–81.
McLean Baird I, Howard AN. Obesity: Medical and Scientific Aspects : Proceedings of the First Symposium of the Obesity Association of Great Britain held in London , October 1968. Edinburgh & London: E. S. Livingston, 1968.
Bray GA, Howard AN. Founding of the international journal of obesity: a journey in medical journalism. Int J Obes. 2015;39:75–9.
Bray G. The founding of obesity research/obesity: a brief history. Obes. 2022;30:2100–2.
Ziman J. The Force of Knowledge. The Scientific Dimension of Society . Cambridge: Cambridge University Press, 1976.
Bray GA, Kim KK, Wilding JPH. Obesity: a chronic relapsing progressive disease process: a position paper of world obesity. Obes Rev. 2017;18:715–23.
Bray GA. Obesity is a chronic, relapsing neurochemical disease. Intern J Obes. 2004;28:34–8.
Allison DB, Downey M, Atkinson RL, Billington CJ, Bray GA, Eckel RH, et al. Obesity as a disease: a white paper on evidence and arguments commissioned by the Council of the Obesity Society. Obes. 2008;16:1161–77.
Garvey WT, Garber AJ, Mechanick JI, Bray GA, Dagogo-Jack S, Einhorn D, et al. American Association of Clinical Endocrinologists and American College of Endocrinology position statement on the 2014 advanced framework for a new diagnosis of obesity as a chronic disease. Endocr Pr. 2014;20:977–89.
Bray GA, Ryan DH. Evidence-based weight loss interventions: individualized treatment options to maximize patient outcomes. Diabetes Obes Metab. 2021;23:50–62.
Ge L, Sadeghirad B, Ball GDC, da Costa BR, Hitchcock CL, Svendrovski A, et al. Comparison of dietary macronutrient patterns of 14 popular named dietary programmes for weight and cardiovascular risk factor reduction in adults: systematic review and network meta-analysis of randomised trials. BMJ 2020;369:m696.
Sjöström L, Rissanen A, Andersen T, Boldrin M, Golay A, Koppeschaar HP, et al. Randomised placebo-controlled trial of orlistat for weight loss and prevention of weight regain in obese patients. European Multicentre Orlistat Study Group. Lancet 1998;352:167–72.
Pi-Sunyer FX, Aronne LJ, Heshmati HM, Devin J, Rosenstock J. Effect of rimonabant, a cannabinoid-1 receptor blocker, on weight and cardiometabolic risk factors in overweight or obese patients: RIO-North America: a randomized controlled trial. JAMA 2006;295:761–75.
Foster GD, Wadden TA, Vogt RA, Brewer G. What is a reasonable weight loss? Patients’ expectations and evaluations of obesity treatment outcomes. J Consult Clin Psychol. 1997;65:79–85.
DiFeliceantonio AG, Coppin G, Rigoux L, Thanarajah ES, Dagher A, Tittgemeyer M, et al. Supra-additive effects of combining fat and carbohydrate on food reward. Cell Metab. 2018;28:33–44.e3.
Thanarajah SE, Backes H, DiFeliceantonio AG, Albus K, Cremer AL, Hanssen R, et al. Food intake recruits orosensory and post-ingestive dopaminergic circuits to affect eating desire in humans. Cell Metab. 2019;29:695–706.e4.
Bray GA. Is sugar addictive? Diabetes 2016;65:1797–9.
Download references
Acknowledgements
The author thanks Dr. Jennifer Lyn Baker for her helpful comments during the early stage of preparing this manuscript.
Author information
Authors and affiliations.
Pennington Biomedical Research Center/LSU, Baton Rouge, LA, 70808, USA
George A. Bray
You can also search for this author in PubMed Google Scholar
Contributions
All contributions were made by the single author.
Corresponding author
Correspondence to George A. Bray .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
MSS # 2023IJO01171.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Bray, G.A. Obesity: a 100 year perspective. Int J Obes (2024). https://doi.org/10.1038/s41366-024-01530-6
Download citation
Received : 13 November 2023
Revised : 23 April 2024
Accepted : 26 April 2024
Published : 07 May 2024
DOI : https://doi.org/10.1038/s41366-024-01530-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Prevention and Management of Childhood Obesity and its Psychological and Health Comorbidities
Justin d. smith.
1 Department of Psychiatry and Behavioral Sciences, Department of Preventive Medicine, and Department of Pediatrics, Northwestern University Feinberg School of Medicine, Chicago, 750 N. Lake Shore Drive, Illinois, 60611, USA
2 Department of Psychiatry and Behavioral Sciences, Northwestern University Feinberg School of Medicine, 750 N. Lake Shore Drive, Chicago, Illinois, 60611, USA
Marissa Kobayashi
3 Department of Public Health Sciences, University of Miami Miller School of Medicine, 1120 NW 14th Street, Suite 1009, Miami, FL 33136. Phone: (305) 972-9961
Childhood obesity has become a global pandemic in developed countries, leading to a host of medical conditions that contribute to increased morbidity and premature death. The causes of obesity in childhood and adolescence are complex and multifaceted, presenting researchers and clinicians with myriad challenges in preventing and managing the problem. This chapter reviews the state-of-the-science for understanding the etiology of childhood obesity, the preventive interventions and treatment options for overweight and obesity, and the medical complications and co-occurring psychological conditions that result from excess adiposity, such as hypertension, non-alcoholic fatty liver disease, and depression. Interventions across the developmental span, varying risk levels, and service contexts (e.g., community, school, home, and healthcare systems) are reviewed. Future directions for research are offered with an emphasis on translational issues for taking evidence-based interventions to scale in a manner that reduce the public health burden of the childhood obesity pandemic.
1.0. INTRODUCTION
Influenced by genetics, biology, psychosocial factors, and health behaviors, overweight and obesity (OW/OB) in childhood is a complex public health problem affecting the majority of developed countries worldwide. Additionally, the key contributors to obesity—poor diet and physical inactivity—are among the leading causes of preventable youth deaths, chronic disease, and economic health burden ( Friedemann et al 2012 , Hamilton et al 2018 ). Despite the remarkable need to prevent childhood obesity and to intervene earlier to prevent excess weight gain in later developmental periods, few interventions have demonstrated long-lasting effects or been implemented at such a scale to have an appreciable public health impact ( Hales et al 2018 ).
In this review, we describe the extent and nature of the childhood obesity pandemic, present conceptual and theoretical models for understanding its etiology, and take a translational-developmental perspective in reviewing intervention approaches within and across developmental stages and in the various contexts in which childhood OW/OB interventions are delivered. We pay particular attention to co-occurring psychological conditions intertwined with OW/OB for children, adolescents, and their families as they relate to both development/etiology and to intervention. For this reason, our review begins with interventions aimed at prevention and moves to management and treatment options for obesity and its psychological and medical comorbidities. Then, we discuss the state-of-the-science and expert recommendations for interventions to prevent and manage childhood OW/OB and what it would take to implement current evidence-based programs at scale. Last, we end by discussing identified gaps in the literature to inform future directions for research and the translation of research findings to real-world practice that can curb the pandemic. For readability, we use the term “interventions for the prevention and management of childhood OW/OB” to capture an array of approaches referred to by a variety of monikers in the literature, including primary prevention, prevention of excess weight gain, weight loss intervention, weight management, and treatment of obesity. More specific labels are used when needed.
2.0. EPIDEMIOLOGY OF CHILDHOOD OBESITY
Childhood OW/OB is determined by the child’s height and weight to calculate body mass index (BMI), which is adjusted according to norms based on the child’s age and gender. BMI between the 85th and 94th percentile is in the “overweight” range, whereas BMI ≥ 95 th percentile for age and gender is in the “obese” range ( Centers for Disease Control and Prevention [CDC] 2018 ). Rates of obesity among children and adolescents in developed countries worldwide, collected in 2013, were 12.9% for boys and 13.4% for girls ( Ng et al 2014 ). In the United States (US) from 1999–2016, 18.4% of children ages 2–19 years had obesity, and 5.2% had severe obesity, defined as BMI ≥120% of the 95th percentile for age and gender ( Skinner et al 2018 ). The prevalence of obesity has increased between 2011–2012 and 2015–2016 in children ages 2–5 and 16–19 years ( Hales et al 2018 ). Being in the obese range during childhood or adolescence makes the youth five times more likely to be obese in adulthood compared to peers who maintain a healthy weight ( Simmonds et al 2016 ). Compared to obesity, severe obesity is strongly linked with greater cardiometabolic risk, adult obesity, and premature death ( Skinner et al 2015 ).
OW/OB and its health consequences are disproportionately distributed across the US, with a higher prevalence among children of disadvantaged racial and socioeconomic backgrounds. Rates of OW/OB are significantly higher among Non-Hispanic black and Hispanic children compared to Non-Hispanic White children (e.g., Hales et al 2018 ). Such disparities are particularly pronounced among severe obesity, where 12.8% of African American children, and 12.4% of Hispanic children have severe obesity compared to 5.0% of Non-Hispanic White children ( Hales et al 2018 ). Youth in low socioeconomic households are more likely to develop OW/OB compared to their counterparts in high socioeconomic households. In 2011–2014, 18.9% of children ages 2–19 living in the lowest income group (≤130% of Federal Poverty Line) had obesity, whereas 10.9% of children in the highest income group (>350% Federal Poverty Line) had obesity ( Ogden et al 2018 ). Influences on multiple socioecological levels put racially diverse children of low socioeconomic status (SES) at higher risk of developing OW/OB, which is further exacerbated by limited access to health services that can prevent excess weight gain and its sequelae.
3.0. ETIOLOGY OF CHILDHOOD OBESITY
At the most basic level, childhood OW/OB emerges from consuming more calories than expended, resulting in excess weight gain and an excess body fat. Caloric imbalance is the result of, and can be further exacerbated by, a range of obesogenic behaviors. That is, behaviors that are highly correlated with excess weight gain. The most common obesogenic behaviors are high consumption of sugar sweetened beverages and low-nutrient, high saturated fat foods, low levels of physical activity and high levels of sedentary behaviors, and shortened sleep duration (e.g., Sisson et al 2016 ). Diet, physical activity, screen time, and sleep patterns are influenced by a myriad of factors and interactions involving genetics, interpersonal relationships, environment, and community (e.g., Russell & Russell 2019 , Smith et al 2018d ). Children living in the United States commonly consume the “Western Diet,” known as a diet high in calories, rich in sugars, trans and saturated fats, salt and food additives, and low in complex carbohydrates, and vitamins. Poor sleep patterns, defined as short duration and late timing, can contribute to obesity through changing levels of appetite-regulating hormones, and irregular eating patterns including late night snacking and eating ( Miller et al 2015 ). Children who experience shortened night time sleep from infancy to school age are at increased risk of developing OW/OB compared to same-aged children sleeping average, age-specific hours (e.g., Taveras et al 2014 ). Research indicates that children with higher rates of screen time also consume high levels of energy-dense snacks, beverages, and fast food, and fewer fruits and vegetables, and screen time is hypothesized to affect food and beverage consumption through distracted eating, reducing feelings of satiety or fullness, and exposure to advertisements for junk food (sweet and salty, calorically-dense foods) ( Robinson et al 2017 ). Screen time can also negatively affect children’s sleeping patterns, and is correlated with sedentary behaviors (e.g., watching television, playing video games) ( Hale & Guan 2015 ).
3.1. Conceptual Models for Understanding and Addressing Childhood OW/OB
Conceptualizing development of childhood OW/OB requires consideration of interplay of genetic, biological, psychological, behavioral, interpersonal, and environment factors ( Kumar & Kelly 2017 ). OW/OB interventions are typically designed to account for these multilevel factors to assist children in achieving expert recommendations for physical activity and fruit and vegetable consumption, while limiting sugar sweetened beverages intake and screen time, and regulating sleep patterns ( Kakinami et al 2019 ). Creating behavioral change requires understanding of the multi-level interactions to identify opportunities for intervention to prevent excess weight gain long-term. A variety of conceptual models exist to explain potential interactions and individual influences leading to obesogenic behaviors and development of childhood OW/OB, and targets for improving health behaviors and routines. Importantly, basic science and conceptual models can be translated to develop effective, targeted intervention programs for prevention of excess weight gain.
3.1.1. Biopsychosocial model
The biopsychosocial model combines biological foundations in child development with environmental and psychosocial influences to identify and address mechanisms and processes to prevent and manage development of childhood OW/OB ( Russell & Russell 2019 ). This model features biological factors, such as genetics, alongside environmental, psychosocial, and behavioral risk factors (e.g., family disorganization, parenting skills, feeding practices, child appetite, temperament), and the development of self-regulation. Such an approach can illustrate developmental processes interacting with biological underpinnings that can be targeted in prevention and management interventions for OW/OB. Intervening from a biopsychosocial model involves cognitive behavioral and behavioral therapy to reframe thoughts and replace unhealthy eating behaviors with new habits.
3.1.2. Ecological systems theory (EST)
EST embeds individual development and change within multiple proximal and distal contexts and emphasizes the need to understand how an “ecological niche” can contribute to the development of specific characteristics, and how such niches are embedded in more distal contexts ( Davison & Birch 2001 ). For example, a child’s ecological niche can be the family or school, which are embedded in larger social contexts, such as the community and society. Individual child characteristics, such as gender and age, interact within and between the family and community context levels, which all influence development of OW/OB. The EST model presents various predictors of childhood OW/OB through identifying risk factors moderated by intraindividual child characteristics. The structure of the EST is present in various studies examining influences of community exposures and children’s individual attributes on weight outcomes.
3.1.3. The Six C’s Model
The Six-C’s is a developmental ecological model that includes environmental (family, community, country, societal), personal, behavioral, and hereditary influences, and a system for categorizing environmental influences, all of which can be adapted to each stage of child development from infancy to adolescence ( Harrison et al 2011 ). The Six C’s stand for: cell, child, clan, community, country, and culture, which represent biology/genetics, personal behaviors, family characteristics, factors outside of the home including peers and school, state and national-level institutions, and culture-specific norms, respectively. Each C includes factors that contribute to child obesity that occur and interact simultaneously throughout child development. For example, among preschool age children, obesity-predisposing genes (cell), excessive media exposure (child), parent dietary intake (clan), unhealthful peer food choices (community), national economic recession, (country) and oversized portions (culture), are all factors associated with obesity that can occur simultaneously and interact during this developmental stage.
3.1.3. The developmental cascade model of pediatric obesity
The model described in the Smith et al. (2018b) article offers a longitudinal framework to elucidate the way cumulative consequences and spreading effects of multiple risk and protective factors, across and within biopsychosocial spheres and phases of development, can propel children towards OW/OB outcomes. The cascade model of pediatric obesity ( Figure 1 ) was developed using a theory-driven model-building approach and a search of the literature to identify paths and relationships in the model that were empirically based. The model allows for different pathways and interactions between different combinations of variables and constructs that contribute to pediatric obesity (equifinality), identifying multi-level risk and protective factors spanning from the prenatal stage to adolescence stage. The complete model can, but has yet to, be tested. The model focuses on intra- and inter-individual child processes and mechanisms (e.g., parenting practices), while acknowledging that individuals are embedded within the broader ecological systems. St. George et al (in press) then conducted a systematic review of the intervention literature to elucidate the ways in which the developmental cascade model of childhood obesity can inform and is informed by intervention approaches for childhood OW/OB.

Note. Bold text indicates strongest support based on our review of the literature. Reprinted with permission from Taylor and Francis Group: Originally published in Smith JD, Egan KN, Montaño Z, Dawson-McClure S, Jake-Schoffman DE, et al. 2018. A developmental cascade perspective of paediatric obesity: Conceptual model and scoping review. Health Psychology Review 12: 271–293.
3.2. Psychosocial Contributors
3.2.1. maternal mental and physical health.
An emerging body of literature has shown a significant relationship between higher levels of parental stress and youths’ higher weight status and unhealthy lifestyle behaviors ( Tate et al 2015 ). In a prospective study, Stout et al (2015) found that fetal exposure to stress, as evidenced by elevated maternal cortisol and corticotropin-releasing hormone, was related to patterns of increasing BMI over the first 24 months of life. Children of mothers experiencing psychological distress and anxiety during pregnancy had higher fat mass, BMI, subcutaneous and visceral fat indices, liver fat fraction, and risk of obesity at age 10 years compared to those whose mothers did not ( Vehmeijer et al 2019 ). Early stress can have long-lasting effects, and studies from a nationally-representative cohort study have shown that postnatal maternal stress during the first year has a positive longitudinal relationship with the child’s BMI up to age 5 ( Leppert et al 2018 ), and psychological distress at age 5 was associated with risk of obesity at age 11 in another nationally-representative cohort ( Hope et al 2019 ). Among Hispanic children and adolescents whose caregivers reported ≥ 3 chronic stressors, Isasi et al (2017) found an increased likelihood of childhood obesity when compared to those whose parents reported no chronic stressors. In a systematic review assessing the impact of maternal stress on children’s weight-related behaviors, O’Connor et al (2017) found mixed evidence for the relationship specific to dietary intake; however, researchers found consistent evidence for the detrimental impact on youths’ physical activity and sedentary behavior, which was often conceptualized as screen time. Understandably, highly stressed parents may have an increased reliance on convenient fast-food options versus grocery shopping and preparing fresh and healthy meals for their children and may not have the energy or wherewithal to support their youths’ physical activity, nor engage in limit-setting behaviors specific to their children’s screen time.
One of the few studies using a longitudinal design did not replicate the relationship between high parental stress and lower levels of youth physical activity, but the relationship held for high levels of parental stress and increased fast food consumption ( Baskind et al 2019 ). Interestingly, this study observed an interaction effect on the relationship of high parental stress and childhood obesity by only low-income households and among ethnic minority children, specifically non-Hispanic black children—explaining one of the factors that contributes to healthy disparities for childhood obesity rates in the US. In another study using a large, prospective cohort, Shankardass et al (2014) found a significant effect of parental stress on BMI. The researchers also observed a significantly larger effect among Hispanics versus the total sample population, further noting that the relationship was weaker and not statistically significant among non-Hispanic children. Due to the salient role of caregiver stress on child health behaviors, it seems that interventions for childhood OW/OB should incorporate stress reduction strategies for parents while simultaneously focusing efforts on reaching racial/ethnic minority families and the economically disadvantaged.
Maternal mental health, most commonly operationalized as depressive symptoms and diagnosis, relate to children’s risk for OW/OB. The longitudinal effects of postnatal maternal depressive symptoms predicted obesity risk in preschool-age children, and unhealthier lifestyle behaviors, such as high TV viewing time and low levels of physical activity ( Benton et al 2015 ). Children of mothers with severe depression were more likely to be obese compared to children of mothers with fewer symptoms ( Marshall et al 2018 ). Maternal mental health could negatively affect child feeding behaviors such that elevated depressive symptoms in low-income mothers have been associated with increased use of feeding to soothe children ( Savage & Birch 2017 ). Few interventions for childhood obesity to date specifically target caregiver depression, but some protocols provide guidance to engage caregivers in services to manage depression and related stressors ( Smith et al 2018c ).
3.2.2. Child mental health
Poor self-regulation and related constructs such as reactivity and impulsivity, are prospective obesogenic risk factors ( Bergmeier et al 2014 , Smith et al 2018d ). A child’s temperament describes behavioral tendencies in reactivity and self-regulation. Negative reactivity is characterized by a quick response with intense negative affect, and is difficult to soothe. Infants and children with negative reactivity are at high risk of excess weight gain, and developing obesity later on and toddlers with low self-regulation and inability to control impulses or behavior are at increased risk for obesity and rapid weight over the subsequent nine years compared to toddlers with higher self-regulation abilities ( Graziano et al 2013 ). Poorer emotional self-regulation at age 3 is an independent predictor of obesity at age 11 ( Anderson et al 2017 ). On the other hand, the ability to delay gratification at age 4 is associated with lower BMI 30 years later ( Schlam et al 2013 ). It is possible that parents of children with difficult temperament experience challenges effectively managing children’s behaviors and setting limits, leading to irregular health routines and increased obesity risk ( Bergmeier et al 2014 , Smith et al 2018d ). Further, parents could overuse food and feeding to soothe children ( Anzman-Frasca et al 2012 ). Throughout childhood, emotional regulation deficits and other mental health disorders continue to predict obesity and weight gain. Emotional regulation in conjunction with stress during childhood is highly linked to low physical activity, emotional eating, irregular and disrupted sleep, and later development of obesity ( Aparicio et al 2016 ). A longitudinal study examining emotional psychopathology in preadolescence saw that boys diagnosed with a social phobia, panic disorder or dysthymia (persistent depressive disorder) had higher waist circumference and/or BMI, and girls diagnosed with dysthymia had increased waist circumference at the three-year follow-up ( Aparicio et al 2013 ). In a prospective study, overweight children who reported binge eating at ages 6–12 years gained 15% more fat mass over a period of four years compared to overweight children with no binge eating ( Tanofsky-Kraff et al 2006 ). The predictive role of mental health on physical health conditions and subsequent comorbidities can be costly and burdensome. Children with obesity-related health conditions (e.g., type 2 diabetes, metabolic syndrome) and a comorbid psychiatric diagnosis (e.g., depressive mood disorder, bipolar disorder, attachment disorder) have higher healthcare utilization and costs per year compared to children without a comorbid psychiatric diagnosis ( Janicke et al 2009a )
There is an association between OW/OB and depression in childhood and adolescence, but there is mixed evidence of the directionality of this effect among children and adolescents. A review of high quality studies by Mühlig et al (2016) saw that among nine studies examining the influence of depression on weight status, six found no significant influence. Of the studies that reported significant associations, one study saw effects only among female adolescents, another only for male adolescents, and a third showed effects of adolescent depressive symptoms on adult obesity at age 53 years only in women. Conversely, OW/OB status can have significant influences on risk of low self-esteem and depressive symptoms/diagnosis in adolescence, as discussed later in this paper.
3.2.3. Stigma/bullying
Weight-related stigma, defined as subtly or overtly having discriminatory actions against individuals with obesity, toward children with obesity can impair quality of life, and contributes to unhealthy behaviors that can worsen obesity such as social isolation, decreased physical activity, and avoidance of health care services ( Pont et al 2017 ). Unfortunately, stigma is widespread and tolerated in society, furthering the reach of negative harm. Children with obesity face explicit weight bias and stigma from multiple environments including from parents, obesity researchers, clinical settings, and school. Parents not only demonstrate implicit bias against childhood obesity, but also implicit and explicit biases against children with obesity ( Lydecker et al 2018 ). Even among obesity researchers and health professionals, significant implicit and explicit anti-fat bias, and explicit anti-fat attitudes increased between 2001–2013 ( Tomiyama et al 2015 ). Exposure to stigma and weight bias can have damaging psychosocial effects on children, such that stigma can mediate the relationship between BMI, depression, and body dissatisfaction ( Stevens et al 2017 ).
Weight stigma can also initiate bullying and weight related teasing, which can have serious psychological consequences such as depression among children, further weight gain and lessen motivation to change. A nationally representative sample of children ages 10–17 years saw that OW/OB adolescents were at higher odds of being a victim of bullying, and also higher odds of perpetrating bullying and victimizing others ( Rupp & McCoy 2019 ). The children at higher odds of engaging in bullying, or being bullied were also at significantly higher odds of having depression, difficulty making friends, and conduct problems compared to OW/OB adolescents who were not bullies or victims of bullying. The relationship between obesity and bullying needs to be addressed through bullying engagement, and coping skills for victimization to prevent and manage associated behavioral and depressive symptoms.
3.2.4. Family functioning and home environment
Evidence suggests a link between general family functioning, parent–child relationships, communication, and use of positive behavior support strategies and childhood OW/OB (see Smith et al 2017a ). Influence of general parenting styles, as opposed to the more specific feeding styles, have been extensively studied and linked to children’s diet, physical activity, and weight ( Shloim et al 2015 ). Children raised with an authoritative (warm and demanding) parenting style had healthier diet, higher physical activity levels, and lower BMI’s than those raised with the other styles ( Sleddens et al 2011 ). Parents proactively structuring home environments to support and positively reinforce healthy dietary and physical activity behaviors also play a key role in children’s healthy lifestyles ( Smith et al 2017b ). Children exposed to less supportive environments consisting of family stress, father absence, maternal depression, confinement, and unclean home environments at 1 year of age has been associated with high BMI at age 21 ( Bates et al 2018 ). Taken together, family participation and building parenting skills can play a salient role in the prevention of childhood OW/OB ( Pratt & Skelton 2018 , Wen et al 2011 ).
4.0. PREVENTION AND MANAGEMENT OF OVERWEIGHT AND OBESITY
This section discusses the state-of-the-science in childhood OW/OB prevention and management along with salient factors related to their implementation in varied healthcare delivery systems. The current climate is being shaped by the position of the American Medical Association. In 2013, the Board voted to classify obesity as a disease that requires medical attention. This classification aimed to emphasize health risks of obesity, remove individual blame, and create new implications and opportunities for intervention. This classification can help to further: 1) a broader public understanding of the obesity condition and associated stigma; 2) prevention efforts; 3) research for treatment and management; 4) insurance reimbursement for intervention; and 5) medical education ( Kyle et al 2016 ). In primary healthcare settings specifically, the US Preventive Services Task Force (USPSTF) gave childhood obesity screening and family-based intervention a “B” grade for evidence of effectiveness ( US Preventive Services Task Force 2017 ), which is sufficient to open insurance reimbursement streams for activities related to the prevention and management of childhood OW/OB that did not exist before. Reimbursement has been a significant barrier to uptake of effective interventions and the impact of the USPSTF in removing this impediment is not yet fully known.
A number of high-quality systematic reviews and meta-analyses have been published in recent years, which provide the most contemporary perspective of the effectiveness of interventions for prevention and management, as well as revealing wide variability and inconsistent findings. For example, Peirson et al (2015a) saw that prevention interventions were associated with slightly improved weight outcomes compared to control groups in mixed-weight children and adolescents. However, intervention effects were not consistent among each intervention strategy tested, suggesting that specific characteristics of the interventions, such as setting, participants, dose, and tailoring, should be examined to determine what is and is not effective in achieving desired outcomes.
Intervention strategies for the prevention and management of child OW/OB occur in various contexts and within, and in coordination with, multiple service delivery systems. This is due in large part to the risk factors inherent to familial, school, and community/societal levels. Relatedly, for prevention in particular, there is some correspondence between the sample being targeted and the context, such that community and school-based interventions are far more likely to be universal (sample does not consider weight status) or selective (target sample is overweight or specifically targeted due to being at-risk for obesity; e.g., ethnic minority, low income) compared to the indicated (majority of target sample is in the obese range) models more commonly found in primary and specialty healthcare systems. Unsurprisingly, the specific intervention targets and behavior change strategies align with the context and approach ( St. George et al in press ).
4.1. Community Interventions
Community interventions are defined as incorporating policies and strategies aimed at reducing the population risk of obesity through legislation, modifications to the built environment, provision of accessible resources, and changes in economic/pricing/food subsidies ( Bleich et al 2013 ). Community interventions can involve the use of media, businesses (e.g., restaurants), community health services, community gardens, community or recreational centers, city planning, and the local governments ( Karacabeyli et al 2018 ). Interventions delivered in community settings have the ability to provide high degrees of access and exposure to strategies and programs to racially diverse, low-income children, who are at the highest risk of OW/OB. Interventions delivered in community settings can be effective, but the impact could be diminished through the lower likelihood of intervention completion due to living in lower socioeconomic circumstances and other obstacles ( Fagg et al 2015 ).
In comparison to other settings, such as the school and family level, there were fewer studies conducted at the community level in a recent review ( Bleich et al 2018 ). This may be due to the numerous challenges and complications involved in building community capacity and engaging community leaders, stakeholders, community agencies, and city organizations. Alternatively, it could reflect a greater focus to date on other contexts and intervention targets, which we discuss in the following sections. To address effectiveness and sustainability, a combined clinical and community intervention could hold promise, especially for racially diverse children living in a low-income community, who are most at-risk. A study by Hoffman et al (2018) showed that an integrated clinic-community model is feasible and improves physical activity and quality of life when compared to multidisciplinary treatment only in clinical care settings.
To summarize, there is promise in community-based interventions that involve either the health clinic and community partnerships or community and school partnerships. Interventions using a community-based participatory approach and a strong quasi-experimental design could achieve the long term goal of reducing both child BMI, the prevalence of OW/OB in childhood, and remission of obesity in children ( Economos & Hammond 2017 ).
4.2. School-Based Interventions
School-based interventions are defined as taking place during school hours or after-school hours for children in kindergarten through high school, and being focused exclusively in the school or delivered primarily in the school setting with secondary settings of family/home, primary care, or community ( Bleich et al 2018 ). Considering that the majority of children spend a significant amount of their day in school, many preventive interventions have leveraged schools as an entry point to improve the obesogenic environment by promoting more physical activity in physical education classes and recess, improving school playgrounds and nutritional options in school cafeterias, and providing healthy lifestyle education in classes or other school policies ( Ickes et al 2014 ). Previous reviews recommend using multi-component interventions targeting two or more health behaviors (i.e., physical activity, dietary outcomes, sedentary behavior) to improve adiposity outcomes when compared to single-component interventions (e.g., Wang et al 2015 ). Interestingly, well-designed school-based studies are effective in improving dietary behavior, but typically do not see statistically significant differences in child BMI between intervention and control schools, except for among children who are already in the obese range ( Bogart et al 2016 ). While increasing fruit, vegetable and water consumption are important, the health behavior modifications are not sufficient for significant long-term obesity management. A way this has been addressed is partnerships between schools and community-based interventions which also engage parents. In a review, Ickes et al (2014) found that less than half of childhood obesity interventions incorporated parents; of those studies involving parents, 75% demonstrated positive outcomes in reducing BMI or weight status. In a synthesis of systematic reviews and meta-analyses of school-based interventions, long-term interventions with a combination of diet and physical activity components and family or parental involvement significantly reduced weight among children ( Khambalia et al 2012 ). Aligned with previous research, Bleich et al (2018) found that school-based interventions that used a multi-component approach of both physical activity and nutrition with some intervention with families in the home had the largest effects. A systematic review and meta-analysis by Wang et al (2015) observed that strength of evidence of obesity prevention programs for children ages 2–18 years was dependent on intervention type, and delivery setting(s). Strength of evidence was high for physical activity-only interventions delivered in school settings with home involvement, or combined diet and physical activity interventions delivered in school settings with home and community involvement. They also found moderately strong evidence when delivering combined interventions in school-based settings alone, in schools with home or community component, or in community with a school component.
Bleich et al (2018) also reviewed a smaller number of pre-school interventions and found some promise in both single component interventions—focusing solely on physical activity—and multi-component interventions. In two other reviews evaluating early child care center-based interventions, both found promising evidence for multi-component interventions and multiple levels influencing the child, parent, teachers/staff, and class ( Sisson et al 2016 , Ward et al 2017 ). An exemplar study, Natale et al (2017) conducted an early childhood multi-level obesity intervention, which included menu modifications at the child care center, a nutrition and physical activity educational curriculum for preschoolers, and a healthy meal preparation and role modeling curriculum for parents. At two-years follow-up, the researchers observed significantly less increase in BMI percentile among the intervention group versus controls. Overall, strong obesity prevention interventions in early care and education settings were associated with healthy eating and anthropometric outcomes, which was further improved by parental engagement. In sum, the preschool and school contexts hold promise for improving weight-related behaviors and adiposity outcomes; however, evidence is clear that parents should be engaged in the process of supporting and reinforcing their children’s health behaviors for these programs to be maximally effective ( Ward et al 2017 ).
4.3. Family-Based Interventions
The home environment (e.g., family routines, limit setting, household chaos, crowding) has long been considered one of the most powerful influences on children’s healthy behaviors and OW/OB outcomes ( Bates et al 2018 ). Playing an integral role in physical activity, diet, screen time, and sleep, parents can exhibit positive parenting practices (e.g., limit-setting, role modeling) and provide a healthy, supportive environment (e.g., provisions of fresh fruits and vegetables), thereby shaping their children’s lifelong habits and preventing the onset of childhood obesity (for a review see Smith et al 2018d ). Family-based interventions are defined as involving either passive or active parental involvement, often with parents viewed as the primary or sole agents of change ( Sung-Chan et al 2013 ). Active parental involvement entails repeated engagement, such as participation in workshops, counseling, or educational sessions; passive involvement does not integrally involve the parent or guardian (e.g., brochures, newsletters).
In a review evaluating family-based interventions for OW/OB prevention, Ash et al (2017) found a significant increase in the number of family-based interventions with just six studies published in 2008 compared to 35 studies in 2013. The majority of studies employed rigorous RCT study designs (73%), but almost two thirds of the studies were short-term and implemented for less than a year. A fraction of studies occurred in multiple settings and over half targeted multiple components beyond diet and physical activity, such as screen time or sleep. Many preventive studies targeting young children (pre-natal to five years old) tend to use home or primary-care based settings with parental involvement, whereas interventions targeting older children tended to take place in community- and school-based settings. These findings are commensurate with the review of St. George et al (in press) , which showed a decrease in parental involvement and family-based intervention strategies with child age. This dovetails with the conclusions of Kothandan (2014) that family-based interventions demonstrated effectiveness for children younger than twelve, but for children twelve and up, school-based interventions were most effective in the short-term.
Regarding preventive interventions specifically, the majority of interventions have been tested among low SES families and predominantly white families ( Ash et al 2017 ). Hispanics/Latinx have been well-represented in US intervention studies in comparison to other ethnic minorities (i.e., African Americans, Asians, and indigenous groups). Latinx are particularly well-suited to participate in family-based interventions given their cultural emphasis on familial values; however, a recent meta-analysis noted diminishing intervention effects with a higher proportion of Hispanic children ( Ling et al 2016 ), which was attributed to a lack of culturally competent interventions to address language barriers and dietary preferences. In addition to incorporating other ethnic minorities and culturally appropriate interventions, Ash et al (2017) suggested that preventive family-based interventions should account for non-traditional families and their different needs and family dynamics.
In regard to family dynamics and interactions, poor family functioning has been linked with an increased risk of obesity, obesogenic behaviors, and adverse health outcomes (e.g., Pratt & Skelton 2018 ). Family-based care for childhood OW/OB involves targeting dietary and physical activity behaviors along with the rules of the family unit, family health routines, communication, and dynamics ( Pratt & Skelton 2018 ). Existing protocols involve family counseling for diet and physical activity change in the home environment, with some approaches also targeting more general parenting and family management skills that have been found to impact OW/OB status of the child ( Smith et al 2018a , Smith et al 2018b , Smith et al 2017b ). Interventions including both parents and children have shown more positive short and long-term effects on child weight when compared to parent-only interventions and controls in some studies ( Yackobovitch-Gavan et al 2018 ), whereas others have found comparable effects for parent-only and child-involved family-based approaches ( Boutelle et al 2017 ). Further, parent-only interventions have been shown to be more cost-effective ( Janicke et al 2009b ). In a meta-analysis evaluating comprehensive behavioral family lifestyle interventions treating pediatric obesity, Janicke et al (2014) found an overall standardized effect size of 0.47, which indicates a small-to-moderate effect on BMI. The dose of treatment (i.e., number of intervention sessions, minutes spent in treatment) was positively related to the treatment effect, which provides support for the notion that more intense and longer interventions are associated with better outcomes, a conclusion also made by ( Whitlock et al 2010 ). In addition, age was a significant moderator for weight outcomes indicating that older children had larger and more beneficial intervention effects than younger children.
Specifically, family-based interventions targeting positive behavior support have been used to address key mechanisms of change specific to promoting children’s healthy lifestyle behaviors ( Smith et al 2017b ). Positive behavior support has been identified as a way to reduce weight gain through improving the caregiver’s ability to support and work with the child toward a healthier diet and improved physical activity. Long-term prevention trials using family-based intervention to target positive behavior support found that children randomized to the intervention had lower BMI in the years following participation ( Smith et al 2015 ). This finding was particularly promising given that these trials did not explicitly focus on child weight in any way; thus, prevention of childhood OW/OB was a spillover effect.
Given the various ways individual, interpersonal, and family health behaviors contribute to child obesity, a tailored family-based intervention could be effective in identifying specific family needs and providing appropriate resources. In a family-based tailored intervention, Taylor et al (2015) saw that the children of families randomized to the tailored treatment had significantly lower BMI compared to families in the usual care group. Additionally, children in the tailored treatment had better dietary behaviors and were more physically active than children in the treatment as usual group. Smith, Berkel et al. (2018b) adapted the highly effective and well-known individually-tailored family-based prevention program called the Family Check-Up ® ( Dishion et al 2008 ) to specifically target obesogenic behaviors with the aim of preventing obesity and excess weight gain in children ages 2 to 12 years. This adaptation is referred to as the Family Check-Up ® 4 Health and is being tested in two large RCTs in coordination with pediatric primary care ( Smith et al 2018a ) and with community-based family resource centers and public schools ( Berkel et al 2019 ) in low-income neighborhoods with racially/ethnically-diverse families at highest risk for childhood OW/OB.
4.4. Primary Healthcare
Primary care interventions are defined as health promotion or weight management programs conducted within or in close coordination with the primary healthcare system. Primary care is viewed as an ideal, real world environment for weight management interventions because of accessibility and frequency of visits (i.e., routine well-child visits) ( Davis et al 2007 ). In a meta-analysis evaluating weight management interventions delivered in primary-care settings, Mitchell et al (2016) found an overall effect size of 0.26, indicating a small treatment effect, and a smaller effect than has been found in broader meta-analytic reviews (e.g., Janicke et al 2014 , Whitlock et al 2010 ). The dose-response relationship was significant, where the number of treatment contacts, length of treatment in months, and the number of visits with the pediatrician was associated with larger treatment effects.
A systematic review examining randomized control trials targeting obesity management in children ages 2–5 years saw five of six interventions, all in ambulatory healthcare settings, had significant decreases in child weight, with sustained intervention effects through follow-up ( Ling et al 2016 ). The effective interventions actively involved parents in health education, group meetings, physical activity sessions, or behavioral therapy.
4.5. Interventions by Developmental Period
In a review of interventions of OW/OB from birth to age 18, St. George et al (in press) identified 74 distinct interventions reported across the 141 included articles. They were categorized based on the child’s age at entry into the intervention: prenatal/infancy (< 2 years; n = 4), early childhood (2–5 years; n = 11), childhood (6–11 years; n = 38), early adolescence (12–15 years; n = 18), and late adolescence (16–18 years; n = 3). Developmental stage of the child has also been found to align with the strategy, such that interventions in the prenatal and infancy periods are nearly all universal, whereas during childhood and adolescence, as compared to early childhood, the burden of disease is larger and intervention strategies more often target selected and indicated samples with greater intensity ( St. George et al in press ).
5.0. EXPERT RECOMMENDATIONS
5.1. youth health behaviors.
It is recommended that children and adolescents aged 6–17 years should achieve ≥ 60 minutes of physical activity each day ( Piercy et al 2018 ). The 2015–2020 Dietary Guidelines for Americans recommend consuming a variety of fruits and vegetables, whole grains, proteins, low-fat dairy products, and limiting intake of sodium, solid fats and added sugars beginning at age 2 years ( DeSalvo et al 2016 ). Unfortunately, only 21.6% of children 6–19 years reach the recommended 60 minutes of physical activity at least five days per week ( Alliance 2016 ). Dietary quality impacts weight gain and OW/OB, and it is estimated that the obesity epidemic largely contributed to statistics showing a declining life expectancy, which occurred in 2015 for the first time in 30 years ( Ludwig 2016 ).
The American Academy of Pediatrics (AAP) recommends that children under 18 months should have no screen time aside from video-chatting, and children ages 2–5 years engage in one hour of screen time per day of high-quality programs with parents. Children ages 6 and above should have limited media exposure, ≤ 2 hours per day, which should not interfere with sleep, physical activity, or other health behaviors. The AAP recommends that families should have “media-free” time together, and “media-free” locations such as in the dining room or bedroom to avoid interfering with meals and sleep duration ( American Academy of Pediatrics Council on Communications and Media 2016 ). The World Health Organization asserts that screen time brings no benefit to children, and infants younger than one year should have no electronic screen exposure, and children age 2–4 years should not have more than one hour of daily “sedentary screen time.” In recent years, the portability of screen devices has led to an overall increase in screen time, with the majority of US youth exceeding screen time guidelines by a wide margin (averaging more than 7 hours daily) ( Barnett Tracie et al 2018 ).
The most recent AAP guidelines recommend that children ages 1–2 years sleep 11–14 hours per 24 hours, children 3–5 sleep 10–13 hours, children 6–12 sleep 9–12 hours, and teenagers ages 13–18 should regularly sleep 8–10 hours ( Paruthi et al 2016 ). Certain behaviors such as a regular routine, avoiding large meals close to bedtime, being physically active during the day time, and eliminating electronic devices in the bedroom are associated with better sleep ( Irish et al 2015 ). According to the CDC, 60% of middle schoolers and 70% of high schoolers do not meet regular sleep recommendations.
5.2. Behavioral Intervention
Family-based intervention is recommended by The National Academy of Medicine, the American Academy of Pediatrics, and the Endocrine Society, among others, as the preferred approach for the management of OW/OB from infancy to adolescence. Based on a systematic review, the USPSTF concluded that lifestyle-based weight loss interventions (not necessarily family-based) consisting of 26 or more hours of intervention engagement are likely to assist children and adolescents in weight management ( O’Connor et al 2017 ). Recommendations from a number of expert committees and task forces support targeting the following behaviors for prevention and management of childhood OW/OB: limiting consumption of sugar sweetened beverages, consuming daily recommended fruit and vegetables, limiting screen time, increasing physical activity, eating breakfast, limiting eating out at restaurants, encouraging family meals, and limiting portion sizes. The majority of existing interventions target multiple behaviors, but some have been designed for discrete behaviors.
5.3. Pharmacologic Intervention
Orlistat is the only FDA-approved medication for treating obesity for pediatric patients ages 12 years and older. Side effects in the gastrointestinal area are common in children, and further clinical trials are needed to evaluate medication risk and benefits among pediatric patients ( Chao et al 2018 ). Expert opinion states that Orlistat, in conjunction to lifestyle changes, leads to modest weight loss and could benefit children in the indicated age range with obesity but tolerability limits its use ( Kelly & Fox 2018 ). And results are not unequivocal. In a meta-analysis looking at primary-care based interventions, Peirson et al (2015b) found a medium effect (standardized effect size [ES] = −0.54) favoring behavioral interventions when compared to Orlistat plus behavioral intervention components (ES = −0.43). Additional research is needed on both effectiveness and tolerability in youth. Additionally, new pharmacologic options continue to be developed and tested and could reach the market in the next few years if approval is granted ( Kelly & Fox 2018 ).
5.4. Surgical Intervention
The American Society for Metabolic and Bariatric Surgery Pediatric Committee’s best practice guidelines selection criteria are based on systematic reviews of co-morbidities, risks and outcomes, important team members, and patient selection. They recommend that adolescents being considered for a bariatric procedure should have a BMI of ≥35 kg/m 2 with major co-morbidities such as type-2 diabetes mellitus, moderate to severe sleep apnea, or severe nonalcoholic steatohepatitis ( Michalsky et al 2012 ). Data show that bariatric surgery in morbidly obese adolescents can greatly impact weight loss, and attenuate or resolve associated chronic disease. However, adolescents undergoing bariatric surgery should be assessed for capability to adhere to follow-up care regimens to ensure proper nutrition intake and care. The committee also recommends a multidisciplinary team for adolescents undergoing bariatric surgery, which could include an experienced bariatric surgeon, pediatric specialist, registered dietitian, mental health specialist, care coordinator, and exercise physiologist.
6.0. CLINICAL IMPLICATIONS OF CO-OCCURRING MEDICAL AND PSYCHOLOGICAL CONDITIONS
6.1. co-occurring medical conditions.
The pro-inflammatory disease nature of obesity and contributing health behaviors affects normal physiology and metabolism, and can cause many associated diseases ( Gonzalez-Muniesa et al 2017 ). If left untreated, obesity can lead to serious health conditions including type-2 diabetes, cardiovascular disease, asthma, obstructive sleep apnea, high blood pressure/hypertension, non-alcoholic fatty liver disease, hepatocellular carcinoma, and psychosocial problems (e.g., Nobili et al 2015 ). Recent research indicates increased risk of cardiovascular disease incidence, morbidity (ischemic heart disease, stroke), and mortality in adulthood associated with being in the obese BMI range in childhood or adolescence ( Sommer & Twig 2018 ). Obesity prevention and management interventions in childhood are imperative for averting the burden of associated comorbidities.

6.1.1. Type-2 diabetes
Children with obesity are four times as likely to develop type-2 diabetes compared to children with a normal BMI ( Abbasi et al 2017 ). Ethnic minority children of low income are at increased risk, and have limited maintenance and glycemic control, furthering the probability of developing additional health complications down the line ( Pulgaron & Delamater 2014 ). Metformin is the main treatment of type-2 diabetes in youth and adults, though emerging evidence implicates a role in treating children with obesity and a family history of type-2 diabetes (e.g., Warnakulasuriya et al 2018 ). Exercise and lifestyle interventions have had significantly positive health effects in adults, however trials evaluating effects in youth with type-2 diabetes are limited. Given the data from adult trials, the American Diabetes Association recommends that youth with type-2 diabetes meet the 1-hour per day physical activity goal to manage symptoms and decrease health risks ( Colberg et al 2016 ).
6.1.2. Obstructive sleep apnea
Pediatric obstructive sleep apnea (OSA) involves a child having disrupted breathing due to partially or completely blocked upper airways during sleep ( Narang & Mathew 2012 ). Obesity confers the most significant risk for OSA. As many as 60% of children and adolescents with obesity have OSA, or some sort of disrupted breathing during sleep ( Narang & Mathew 2012 ). Obesity and OSA have additional comorbidities and impairments including excessive daytime sleepiness, neurocognitive function, reduced physical activity, cardiovascular burden, and hypertension, further complicating quality life of children with obesity ( Blechner & Williamson 2016 ). Obesity management such as increased physical activity and a healthy diet are recommended for OSA treatment, as well as surgical procedures, if appropriate.
6.1.3. Asthma
Asthma is one of the most common chronic diseases among children and adolescents: 10.1% of children ages 5–14 years had asthma in 2016 ( National Center for Health Statistics 2019 ). Although both obesity and asthma rates have been increasing, it does not appear that obesity has been contributing to the increased asthma prevalence rate ( Akinbami et al 2018 ). This does not discount the risks of obesity on asthma and its unique effects on asthma symptoms. OW/OB children have been observed to have higher prevalence of asthma, and exacerbation as early as preschool age compared to normal weight children ( Lang et al 2018 ). Additionally, OW/OB children have reported distinct asthma symptoms, such as greater shortness of breath, reduced airway hyperresponsiveness, and loss of asthma control, compared to normal weight children ( Lang et al 2015 ). The relationship between asthma and OW/OB should be further investigated.
6.1.4. Hypertension
Hypertension, like obesity, has been increasing among youth and is associated with increased cardiovascular disease risk throughout the lifetime ( May et al 2012 ). The greatest risk factor for pediatric hypertension is elevated BMI ( Falkner et al 2006 ). About 3% of children in the general population have hypertension, compared to about 25% of obese children ( Shatat & Brady 2018 ). In a meta-analysis examining cardiovascular risk factors, compared with normal weight children, systolic blood pressure was higher by 4.54 mm Hg (n=12169, 8 studies) in overweight children, and by 7.49 mm Hg (n=8074, 15 studies) in obese children ( Friedemann et al 2012 ). A study examining childhood hypertension and OW/OB in school children saw that 2.2% of the sample had hypertension, and 37% of those cases could be attributed to OW/OB status ( Chiolero et al 2007 ). A review shows that children with obesity-related hypertension are at increased risk of cardiovascular morbidity and mortality ( Wuhl 2019 ). About 3.8%–24.8% of children with OW/OB have hypertension, though these rates could be higher due to inconsistences and challenges with diagnoses ( Flynn et al 2017 ). The risks of hypertension on children’s lifetime health emphasize the importance of preventing obesity early on.
6.1.5. Nonalcoholic fatty liver disease (NAFLD)
NAFLD is the leading cause of liver disease, leading to a shorter life expectancy due to associated comorbidities; one of which, non-alcoholic steatohepatitis, is projected to be the leading indication for pediatric liver transplant by 2025 ( Charlton et al 2011 ). Epidemiological studies consistently show associations between NAFLD and adiposity, unhealthy diet, and sedentary behavior ( Dunn & Schwimmer 2008 ). Prevalence of NAFLD is especially high in young people who have obesity such that 22.5%–52.8% of children with obesity have NAFLD compared to 2.6% of all children ( Anderson et al 2015 ). Child obesity has the highest risk in the development of NAFLD during childhood ( Hays & McGinnis 2018 ). A longitudinal study of participants ages 3–18 years were followed for 31 years, and saw that child OW/OB was associated with increased risk for adult NAFLD ( Cuthbertson et al 2018 ). The associated risk was removed if participants obtained a normal range BMI by adulthood, emphasizing the salient role of weight management. The high prevalence of NAFLD among children with obesity, and effectiveness of weight change in treating this condition, emphasizes the need for prevention and management of obesity. Smith et al (2017a) found that among children who had NAFLD, poorer family functioning was significantly related to higher BMI, elevated levels of cholesterol, HbA1c, and glucose. Their study exposes the critical role of family functioning on child health, and the importance of using targeted intervention to prevent, and manage obesity and associated disease using a family-centered approach. Weight being the most modifiable factor, the mainstay of NAFLD treatment is lifestyle behavior modifications aimed at weight loss ( Marchesini et al 2015 ).
6.2. Co-Occurring Psychological Conditions
6.2.1. self-esteem/depression.
Children with OW/OB are more likely to experience low self-esteem, and develop depressive symptoms during adolescence compared to normal weight peers (e.g., Mühlig et al 2016 ). This relationship can be attributed to multi-level factors including health behaviors, parenting styles, and family functioning. A review by Hoare et al (2014) suggests that obesogenic risk factors, such as infrequent physical activity, sedentary behavior, poor diet quality, and adiposity were associated with depressive symptoms in adolescents. Conversely, healthier eating patterns were associated with decreased depressive symptoms. Child eating disorder pathology, emotionally-manipulative parenting style, and lower child social status have been associated with depressive symptomatology among children with OW/OB ( Sheinbein et al 2019 ). Children in poorly functioning families with low self-esteem participating in weight loss interventions have been observed to have poor 6-month outcomes, suggesting that multiple social-ecological factors need to be addressed when targeting depressive symptoms in children with OW/OB ( Taylor et al 2017 ). Further, negative psychological experiences more generally, such as trauma and stigma, trigger emotional eating, leading to an ongoing obesity-depression cycle ( Milaneschi et al 2019 ).
6.2.2. Eating disorders
Children with OW/OB have a high prevalence of disordered eating attitudes and behaviors, which can increase risk of developing eating disorders in adulthood. A high proportion of adolescents with restrictive eating disorders report a history of OW/OB ( Lebow et al 2015 ). Additionally, it is estimated that over a quarter of youth with OW/OB have binge and loss of control eating ( He et al 2017 ). Adolescent girls with OW/OB experiencing overvaluation of weight—so concerned with weight that self-evaluation is influenced—are at higher risk of starting to binge eat weekly 2 years later, have more severe depressive symptoms, and continuous overvaluation ( Sonneville et al 2015 ). The bidirectional relationship of obesity and eating disorders, including eating disorder psychopathology, should be properly evaluated during treatment planning.
7.0. IMPLEMENTATION AND RESEARCH TRANSLATION CHALLENGES
One of the abundant challenges for the field is the translation and implementation of effective interventions to the real-world service delivery systems that can reach those most in need. This so-called research-practice gap is pronounced in obesity prevention and management given the preponderance of untested, usual care approaches currently in use; the persistence of debunked myths about causes and effective intervention approaches (e.g., fad diets); and the incongruence between what is being developed by experts and what is acceptable, feasible, and sustainable in existing systems given the constraints of the workforce, space, and funding. This says nothing about the consumer of evidence-based interventions, who historically have had only cursory involvement in the design and deployment of interventions. This has contributed to low engagement rates and high attrition from more intensive OW/OB interventions ( Lydecker & Grilo 2016 ). Raising public and caregiver concern about the risks posed by OW/OB in childhood and adolescence would also facilitate engagement and retention. Currently, many parents with children with obesity underestimate their children’s weight ( Lydecker & Grilo 2016 ) and are thus unlikely to seek intervention or to follow through with a referral for intervention. Add the stigma in society surrounding obesity and the shame parents experience concerning their child’s weight, and traditional approaches to care will continue to be underutilized.
While many of the aforementioned conceptual models encapsulate the multiple levels contributing to childhood obesity, researchers are trying to elucidate which combination of levels and service contexts have greatest effectiveness, and which implementation strategies best address the complexity at levels of the community, school, family, and primary care. Implementation strategies are defined as the methods or techniques used to enhance the adoption, implementation, and sustainability of a clinical program or practice ( Proctor et al 2013 ). They are the actions taken on agents in the system of care itself, and rarely only on the patient or client that is the recipient of the clinical program or practice. The first iteration of the Childhood Obesity Research Demonstration Projects (CORD 1.0), a program of research administered by the CDC, examined multi-sector intervention implementation in schools, community centers, early care and health centers, and pediatric primary care practices. The three projects around the US, identified the facilitators and barriers of implementing multi-setting interventions targeting levels of the socioecologial model in racially diverse, lower-income communities ( Dooyema et al 2017 ). CORD 1.0 projects identified common implementation barriers in schools, rural communities and community centers, including staff turnover, limited resources, and competing needs for existing requirements (such as standardized testing in schools) ( Chuang et al 2016 , Ganter et al 2017 ). Interventions in rural communities and multiple settings benefited from engaging parents and obtaining support from organization members and leadership ( Chuang et al 2016 , Ganter et al 2017 ). Facilitators of school interventions included using the principal as a champion and using students to engage other students ( Blaine et al 2017 ). Low-income primary care settings showed that only about 27% of referred patients enrolled in the intervention ( Barlow et al 2017 ). Such knowledge assists in the design of future studies to develop effective, accessible, and acceptable interventions for those needing it most.
These implementation challenges are not unique to childhood obesity but the complexity of the problem will require more rapid translation of discoveries in research with bidirectional input from successes and failures in practice back to researchers. Last, improving the packaging of evidence-based programs can provide potential implementers with a “ready off the shelf” product that requires less involvement by the intervention developers, which is a primary contributor to the high cost of adopting a new program ( Jordan et al 2019 ), and can arguably aid implementers in delivering interventions with fidelity. This is the goal of the CDC’s Childhood Obesity Research Demonstration (CORD) 3.0 Project ( https://www.cdc.gov/obesity/strategies/healthcare/cord3.html ). However, the scale up penalty—reduced effects as interventions are widely disseminated and adopted—has been shown in the childhood obesity literature to be about 75% of efficacy studies ( McCrabb et al 2019 ), but implementation scientists have argued for dynamic adaptation that retains effectiveness while also increasing sustainability (e.g., Chambers et al 2013 ). This is an area in need of attention as interventions are taken to scale.
8.0. RECOMMENDATIONS FOR FUTURE RESEARCH
Reviews of interventions for childhood OW/OB show variability in effectiveness, often changing health behaviors but not weight, thus exposing the difficulties of addressing and managing this public health crisis. There are a number of directions for future research to improve outcomes and address the challenges of wide-scale implementation.
1) Interventions need to be integrated across systems.
Given the multifaceted, multilevel, and interrelated nature of OW/OB development, if interventions are to be maximally effective there needs to be an integration of multiple service systems (primary care, schools, communities, child care, the home) for the delivery of multicomponent interventions that utilize behavioral, structural, environmental, policy, and biomedical approaches.
2) There is no “one size fits all.”
More complex, individual child and family interventions need to be tailored both in terms of content and implementation strategy to best align with the personal needs of those involved. This means flexible, adaptive, or modularized intervention protocols addressing the cadre of potential health behaviors and related individual and familial risk factors of OW/OB present, and getting the intervention to families in a manner that is engaging, accessible, and has wide reach.
3) Consider implementation earlier.
Researchers developing interventions for childhood OW/OB ought to consider their implementability from the beginning using the framework of “designing for dissemination and implementation” ( Dearing et al 2013 ), which considers the capacities, needs, and preferences of the end users (service delivery systems, children/families, funding mechanisms) during design and testing. Another method for speeding translation is to adapt existing programs for new service contexts and new populations, rather than following the traditional pipeline of treating something different as “new” and having to establish efficacy and effectiveness before moving to implement. This concept has been referred to as “scaling out” ( Aarons et al 2017 ) and it has been applied in childhood OW/OB prevention and management ( Smith et al 2018b ). Scaling out is a critical method for implementation research to address the health inequities and disparities of childhood obesity ( McNulty et al 2019 ).
4) Engage the community to enhance scalability and sustainability.
Berkel et al (in press) engaged a diverse group of stakeholders, including payors, in the adaptation and delivery processes of a recent trial of the Family Check-Up ® 4 Health as a means of increasing the likelihood of sustained adoption beyond the funded trial. Economos and Hammond (2017) suggest that community-level research should employ novel techniques of systems mapping and causal loop diagramming, which can help stakeholders to visualize the interrelated processes and elements that are relevant to the intervention. They also suggest using agent-based modeling and other simulation methods to help encapsulate the complex dynamics involved in implementing successful community-based interventions. Tailoring strategies to local communities and deepening engagement holds promise in enhancing sustainability and scalability of community-based interventions.
5) Research rigor—scale up balance.
Future directions should address the shortcomings of less rigorous study designs, which inherently increases the risk of confounding and presents challenges in attributing changes in the outcome to intervention effects, but as research translation moves toward scaling up after establishing effectiveness, this tradeoff is both expected and encouraged to increase external validity. Additionally, research is needed to determine the appropriate length and dosage of interventions, along with clear reporting of outcomes, consistency of measures, and long-term follow ups ( Bleich et al 2018 , Ickes et al 2014 , St. George et al in press ). Echoing Karacabeyli et al (2018) , we also recommend collecting process evaluation and outcome data in order to understand the complex causal chain and to help bolster inferences in regard to the effectiveness and implementation of the intervention using hybrid designs .
6) Engagement and participation are critical challenges.
Large community trials in particular often suffer high attrition rates because of mobile populations who move to different residences, which can impact the ability to track and communicate with participants. And this relates to effectiveness. Children completing >75% of a community-based intervention program experienced beneficial change in BMI as well as associated health behaviors (physical activity, screen time, unhealthy food consumption) compared with children completing <75% of the program ( Hardy et al 2015 ). A way to attenuate attrition in research on community-level interventions could be through adjusting study intervention design. The majority of community-based interventions used a quasi-experimental design, which is often attributed to practicality and sustainability ( Bleich et al 2018 , Karacabeyli et al 2018 ). Interestingly, less rigorous study designs (e.g., quasi-experimental vs. RCTs) demonstrated significant reductions in child weight ( Karacabeyli et al 2018 ). By removing randomization, the authors reported that communities with the resources, engagement/buy-in, and capacity could be selected to participate, which optimized community support for the obesity intervention efforts through both sustainable partnerships and buy-in from the community and its champions. This participatory approach could potentially lead to lasting positive health changes that extend beyond the study period. In addition, Karacabeyli et al (2018) described the benefits of a quasi-experimental design which lends itself to selecting at-risk communities that could greatly benefit from intervention efforts. For example, using a stepped wedge or randomized rollout trial design where all at-risk communities selected would eventually receive the intervention at different time periods but none serve as “no intervention” controls (see Landsverk et al 2017 ).
9. CONCLUSIONS
There are signs that progress is being made in stemming the tide of childhood obesity and evidence-based interventions are available across development and for various contexts and systems that affected and at-risk children routinely encounter. Tremendous challenges remain in connecting the dots between etiology, development, and intervention targets, as well as when and where to intervene. There needs to be a push to scale up effective interventions as even small changes in weight can yield significant impact on multiple cardiometabolic indices ( Lloyd-Jones et al 2010 ) that can improve quality and length of life. Clinical health psychologists are ideally suited to conduct research on this complex problem but transdisciplinary teams will be needed to increasingly move the dial.
SUMMARY POINTS
- Childhood obesity is a complex, multidetermined, preventable chronic disease that increases risk for premature death and psychological problems.
- Evidence-based interventions for obesity are available for all stages of development from birth to 18 years.
- Specific interventions can be delivered in community, school, home, and healthcare settings depending on the type of strategy and risk level of the targeted population.
- Associated co-occurring medical and psychological conditions of childhood obesity present an opportunity for clinical and health psychology researchers and practitioners.
FUTURE ISSUES
- Future research ought to focus on translational considerations from the start and ways to scale up delivery of effective interventions.
- Research is needed on interventions and their implementation to more effectively reach minority and underserved populations at greatest risk for obesity.
- Increasing engagement and retention in childhood obesity interventions is a promising focus for future research.
ACKNOWLEDGEMENTS
The authors wish to thank Sara St. George for feedback on an earlier version of this review and to acknowledge support of this work from the Centers for Disease Control and Prevention (grant U18DP006255) and the United States Department of Agriculture (grant 2018-68001-27550), awarded to Justin Smith and Cady Berkel; and the National Institute on Drug Abuse (grant P30 DA027828), to C. Hendricks Brown, in support of Justin Smith.
DISCLOSURE STATEMENT
Justin D. Smith is co-developer of the Family Check-Up ® 4 Health intervention for childhood obesity. The authors are not aware of any other affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this review.
LITERATURE CITED
- Aarons GA, Sklar M, Mustanski B, Benbow N, Brown CH. 2017. “Scaling-out” evidence-based interventions to new populations or new health care delivery systems . Implementation Science 12 : 111. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Abbasi A, Juszczyk D, van Jaarsveld CHM, Gulliford MC. 2017. Body Mass Index and Incident Type 1 and Type 2 Diabetes in Children and Young Adults: A Retrospective Cohort Study . Journal of the Endocrine Society 1 : 524–37 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Akinbami LJ, Rossen LM, Fakhouri THI, Fryar CD. 2018. Asthma prevalence trends by weight status among US children aged 2–19 years, 1988–2014 . Pediatric Obesity 13 : 393–96 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Alliance NPAP. 2016. 2016 US report card on physical activity for children and youth
- American Academy of Pediatrics Council on Communications and Media. 2016. Media and Young Minds . Pediatrics 138 : e20162591. [ PubMed ] [ Google Scholar ]
- Anderson EL, Howe LD, Jones HE, Higgins JP, Lawlor DA, Fraser A. 2015. The Prevalence of Non-Alcoholic Fatty Liver Disease in Children and Adolescents: A Systematic Review and Meta-Analysis . PLoS One 10 : e0140908. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Anderson SE, Sacker A, Whitaker RC, Kelly Y. 2017. Self-regulation and household routines at age three and obesity at age eleven: longitudinal analysis of the UK Millennium Cohort Study . International Journal Of Obesity 41 : 1459. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Anzman-Frasca S, Stifter CA, Birch LL. 2012. Temperament and childhood obesity risk: A review of the literature . Journal of Developmental & Behavioral Pediatrics 33 : 732–45 [ PubMed ] [ Google Scholar ]
- Aparicio E, Canals J, Arija V, De Henauw S, Michels N. 2016. The role of emotion regulation in childhood obesity: implications for prevention and treatment . Nutrition Research Reviews 29 : 17–29 [ PubMed ] [ Google Scholar ]
- Aparicio E, Canals J, Voltas N, Hernandez-Martinez C, Arija V. 2013. Emotional psychopathology and increased adiposity: Follow-up study in adolescents . Journal of Adolescence 36 : 319–30 [ PubMed ] [ Google Scholar ]
- Ash T, Agaronov A, Young T, Aftosmes-Tobio A, Davison KK. 2017. Family-based childhood obesity prevention interventions: a systematic review and quantitative content analysis . The international journal of behavioral nutrition and physical activity 14 : 113. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Barlow SE, Butte NF, Hoelscher DM, Salahuddin M, Pont SJ. 2017. Strategies to Recruit a Diverse Low-Income Population to Child Weight Management Programs From Primary Care Practices . Preventing chronic disease 14 : E138–E38 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Barnett Tracie A, Kelly Aaron S, Young Deborah R, Perry Cynthia K, Pratt Charlotte A, et al. 2018. Sedentary Behaviors in Today’s Youth: Approaches to the Prevention and Management of Childhood Obesity: A Scientific Statement From the American Heart Association . Circulation 138 : e142–e59 [ PubMed ] [ Google Scholar ]
- Baskind MJ, Taveras EM, Gerber MW, Fiechtner L, Horan C, Sharifi M. 2019. Parent-Perceived Stress and Its Association With Children's Weight and Obesity-Related Behaviors . Prev Chronic Dis 16 : E39. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bates CR, Buscemi J, Nicholson LM, Cory M, Jagpal A, Bohnert AM. 2018. Links between the organization of the family home environment and child obesity: A systematic review . Obesity Reviews 19 : 716–27 [ PubMed ] [ Google Scholar ]
- Benton PM, Skouteris H, Hayden M. 2015. Does maternal psychopathology increase the risk of pre-schooler obesity? A systematic review . Appetite 87 : 259–82 [ PubMed ] [ Google Scholar ]
- Bergmeier H, Skouteris H, Horwood S, Hooley M, Richardson B. 2014. Child temperament and maternal predictors of preschool children's eating and body mass index. A prospective study . Appetite 74 : 125–32 [ PubMed ] [ Google Scholar ]
- Berkel C, Rudo-Stern J, Villamar JA, Wilson C, Flanagan E, et al. in press. Recommendations from community partners to promote sustainable implementation of evidence-based programs in primary care . Journal of Community Psychology [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Berkel C, Smith JD, Bruening MM, Jordan N, Grimm K, et al. 2019. The Family Check-Up 4 Health: A Health Maintenance Approach to Improve Nutrition and Prevent Early Childhood Obesity . Presented at Society for Nutrition Education and Behavior Annual Conference Orlando, FL [ Google Scholar ]
- Blaine RE, Franckle RL, Ganter C, Falbe J, Giles C, et al. 2017. Using School Staff Members to Implement a Childhood Obesity Prevention Intervention in Low-Income School Districts: the Massachusetts Childhood Obesity Research Demonstration (MA-CORD Project), 2012-2014 . Prev Chronic Dis 14 : E03. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Blechner M, Williamson AA. 2016. Consequences of Obstructive Sleep Apnea in Children . Current Problems in Pediatric and Adolescent Health Care 46 : 19–26 [ PubMed ] [ Google Scholar ]
- Bleich SN, Segal J, Wu Y, Wilson R, Wang Y. 2013. Systematic Review of Community-Based Childhood Obesity Prevention Studies . Pediatrics 132 : e201. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bleich SN, Vercammen KA, Zatz LY, Frelier JM, Ebbeling CB, Peeters A. 2018. Interventions to prevent global childhood overweight and obesity: a systematic review . The lancet. Diabetes & endocrinology 6 : 332–46 [ PubMed ] [ Google Scholar ]
- Bogart LM, Elliott MN, Cowgill BO, Klein DJ, Hawes-Dawson J, et al. 2016. Two-Year BMI Outcomes From a School-Based Intervention for Nutrition and Exercise: A Randomized Trial . Pediatrics 137 : e20152493. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Boutelle KN, Rhee KE, Liang J, Braden A, Douglas J, et al. 2017. Effect of Attendance of the Child on Body Weight, Energy Intake, and Physical Activity in Childhood Obesity Treatment: A Randomized Clinical Trial . JAMA Pediatrics 171 : 622–28 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Centers for Disease Control and Prevention. 2018. Defining Childhood Obesity . [ Google Scholar ]
- Chambers DA, Glasgow R, Stange K. 2013. The dynamic sustainability framework: addressing the paradox of sustainment amid ongoing change . Implement Sci 8 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chao AM, Wadden TA, Berkowitz RI. 2018. The safety of pharmacologic treatment for pediatric obesity . Expert Opinion on Drug Safety 17 : 379–85 [ PubMed ] [ Google Scholar ]
- Charlton MR, Burns JM, Pedersen RA, Watt KD, Heimbach JK, Dierkhising RA. 2011. Frequency and outcomes of liver transplantation for nonalcoholic steatohepatitis in the United States . Gastroenterology 141 : 1249–53 [ PubMed ] [ Google Scholar ]
- Chiolero A, Cachat F, Burnier M, Paccaud F, Bovet P. 2007. Prevalence of hypertension in schoolchildren based on repeated measurements and association with overweight . Journal of Hypertension 25 : 2209–17 [ PubMed ] [ Google Scholar ]
- Chuang E, Brunner J, Moody J, Ibarra L, Hoyt H, et al. 2016. Factors Affecting Implementation of the California Childhood Obesity Research Demonstration (CA-CORD) Project, 2013 . Prev Chronic Dis 13 : E147. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Colberg SR, Sigal RJ, Yardley JE, Riddell MC, Dunstan DW, et al. 2016. Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association . Diabetes Care 39 : 2065. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cuthbertson DJ, Brown E, Koskinen J, Magnussen CG, Hutri-Kähönen N, et al. 2018. Longitudinal analysis of risk of non-alcoholic fatty liver disease in adulthood . Liver International 0 [ PubMed ] [ Google Scholar ]
- Davis MM, Gance-Cleveland B, Hassink S, Johnson R, Paradis G, Resnicow K. 2007. Recommendations for prevention of childhood obesity . Pediatrics 120 : S229–S53 [ PubMed ] [ Google Scholar ]
- Davison KK, Birch LL. 2001. Childhood overweight: A contextual model and recommendations for future research . Obesity Reviews 2 : 159–71 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dearing JW, Smith DK, Larson RS, Estabrooks CA. 2013. Designing for Diffusion of a Biomedical Intervention . American Journal of Preventive Medicine 44 : S70–S76 [ PubMed ] [ Google Scholar ]
- DeSalvo KB, Olson R, Casavale KO. 2016. Dietary Guidelines for AmericansDietary Guidelines for AmericansDietary Guidelines for Americans . JAMA 315 : 457–58 [ PubMed ] [ Google Scholar ]
- Dishion TJ, Shaw DS, Connell A, Gardner FEM, Weaver C, Wilson M. 2008. The Family Check-Up with high-risk indigent families: Preventing problem behavior by increasing parents' positive behavior support in early childhood . Child Development 79 : 1395–414 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dooyema CA, Belay B, Blanck HM. 2017. Implementation of Multisetting Interventions to Address Childhood Obesity in Diverse, Lower-Income Communities: CDC's Childhood Obesity Research Demonstration Projects . Prev Chronic Dis 14 : E140. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dunn W, Schwimmer J. 2008. The obesity epidemic and nonalcoholic fatty liver disease in children . Curr Gastroenterol Rep 10 : 67–72 [ PubMed ] [ Google Scholar ]
- Economos CD, Hammond RA. 2017. Designing effective and sustainable multifaceted interventions for obesity prevention and healthy communities . Obesity 25 : 1155–56 [ PubMed ] [ Google Scholar ]
- Fagg J, Cole TJ, Cummins S, Goldstein H, Morris S, et al. 2015. After the RCT: who comes to a family-based intervention for childhood overweight or obesity when it is implemented at scale in the community? Journal of Epidemiology and Community Health 69 : 142. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Falkner B, Gidding SS, Ramirez-Garnica G, Wiltrout SA, West D, Rappaport EB. 2006. The relationship of body mass index and blood pressure in primary care pediatric patients . J Pediatr 148 : 195–200 [ PubMed ] [ Google Scholar ]
- Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al. 2017. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents . Pediatrics 140 : e20171904. [ PubMed ] [ Google Scholar ]
- Friedemann C, Heneghan C, Mahtani K, Thompson M, Perera R, Ward AM. 2012. Cardiovascular disease risk in healthy children and its association with body mass index: systematic review and meta-analysis . BMJ : British Medical Journal 345 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ganter C, Aftosmes-Tobio A, Chuang E, Kwass JA, Land T, Davison KK. 2017. Lessons Learned by Community Stakeholders in the Massachusetts Childhood Obesity Research Demonstration (MA-CORD) Project, 2013-2014 . Prev Chronic Dis 14 : E08. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gonzalez-Muniesa P, Martinez-Gonzalez MA, Hu FB, Despres JP, Matsuzawa Y, et al. 2017. Obesity . Nature reviews. Disease primers 3 : 17034 [ PubMed ] [ Google Scholar ]
- Graziano PA, Kelleher R, Calkins SD, Keane SP, Brien MO. 2013. Predicting weight outcomes in preadolescence: the role of toddlers' self-regulation skills and the temperament dimension of pleasure . International journal of obesity (2005) 37 : 937–42 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hale L, Guan S. 2015. Screen time and sleep among school-aged children and adolescents: a systematic literature review . Sleep medicine reviews 21 : 50–8 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. 2018. Trends in obesity and severe obesity prevalence in us youth and adults by sex and age, 2007-2008 to 2015-2016 . JAMA 319 : 1723–25 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hamilton D, Dee A, Perry IJ. 2018. The lifetime costs of overweight and obesity in childhood and adolescence: a systematic review . Obesity Reviews 19 : 452–63 [ PubMed ] [ Google Scholar ]
- Hardy LL, Mihrshahi S, Gale J, Nguyen B, Baur LA, O’Hara BJ. 2015. Translational research: are community-based child obesity treatment programs scalable? BMC Public Health 15 : 652. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Harrison K, Bost KK, McBride BA, Donovan SM, Grigsby-Toussaint DS, et al. 2011. Toward a developmental conceptualization of contributors to overweight and obesity in childhood: The Six-Cs model . Child Development Perspectives 5 : 50–58 [ Google Scholar ]
- Hays SM, McGinnis C. 2018. Nonalcoholic Fatty Liver Disease in Children: Beyond Metabolic Syndrome . The Journal for Nurse Practitioners 14 : 725–31 [ Google Scholar ]
- He J, Cai Z, Fan X. 2017. Prevalence of binge and loss of control eating among children and adolescents with overweight and obesity: An exploratory meta-analysis . Int J Eat Disord 50 : 91–103 [ PubMed ] [ Google Scholar ]
- Hoare E, Skouteris H, Fuller-Tyszkiewicz M, Millar L, Allender S. 2014. Associations between obesogenic risk factors and depression among adolescents: a systematic review . Obesity Reviews 15 : 40–51 [ PubMed ] [ Google Scholar ]
- Hoffman J, Frerichs L, Story M, Jones J, Gaskin K, et al. 2018. An Integrated Clinic-Community Partnership for Child Obesity Treatment: A Randomized Pilot Trial . Pediatrics 141 : e20171444. [ PubMed ] [ Google Scholar ]
- Hope S, Micali N, Deighton J, Law C. 2019. Maternal mental health at 5 years and childhood overweight or obesity at 11 years: evidence from the UK Millennium Cohort Study . International Journal of Obesity 43 : 43–52 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ickes MJ, McMullen J, Haider T, Sharma M. 2014. Global school-based childhood obesity interventions: a review . Int J Environ Res Public Health 11 : 8940–61 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Irish LA, Kline CE, Gunn HE, Buysse DJ, Hall MH. 2015. The role of sleep hygiene in promoting public health: A review of empirical evidence . Sleep Medicine Reviews 22 : 23–36 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Isasi CR, Hua S, Jung M, Carnethon MR, Perreira K, et al. 2017. The Association of Parental/Caregiver Chronic Stress with Youth Obesity: Findings from the Study of Latino Youth and the Hispanic Community Health Study/Study of Latinos Sociocultural Ancillary Study . Childhood obesity (Print) 13 : 251–58 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Janicke DM, Harman JS, Kelleher KJ, Zhang J. 2009a. The Association of Psychiatric Diagnoses, Health Service Use, and Expenditures in Children with Obesity-related Health Conditions . Journal of Pediatric Psychology 34 : 79–88 [ PubMed ] [ Google Scholar ]
- Janicke DM, Sallinen BJ, Perri MG, Lutes LD, Silverstein JH, Brumback B. 2009b. Comparison of Program Costs for Parent-Only and Family-Based Interventions for Pediatric Obesity in Medically Underserved Rural Settings . The Journal of Rural Health 25 : 326–30 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Janicke DM, Steele RG, Gayes LA, Lim CS, Clifford LM, et al. 2014. Systematic review and meta-analysis of comprehensive behavioral family lifestyle interventions addressing pediatric obesity . Journal of Pediatric Psychology [ PubMed ] [ Google Scholar ]
- Jordan N, Graham AK, Berkel C, Smith JD. 2019. Budget impact analysis of preparing to implement the Family Check-Up 4 Health in primary care to reduce pediatric obesity . Prevention Science 20 : 655–64 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kakinami L, Houle-Johnson SA, Demissie Z, Santosa S, Fulton JE. 2019. Meeting fruit and vegetable consumption and physical activity recommendations among adolescents intending to lose weight . Preventive Medicine Reports 13 : 11–15 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Karacabeyli D, Allender S, Pinkney S, Amed S. 2018. Evaluation of complex community-based childhood obesity prevention interventions . Obes Rev 19 : 1080–92 [ PubMed ] [ Google Scholar ]
- Kelly AS, Fox CK. 2018. Role of Pharmacotherapy in the Treatment of Pediatric Obesity and Its Comorbidities In Pediatric Obesity: Etiology, Pathogenesis and Treatment , ed. Freemark MS, pp. 613–27. Cham: Springer International Publishing [ Google Scholar ]
- Khambalia AZ, Dickinson S, Hardy LL, Gill T, Baur LA. 2012. A synthesis of existing systematic reviews and meta-analyses of school-based behavioural interventions for controlling and preventing obesity . Obes Rev 13 : 214–33 [ PubMed ] [ Google Scholar ]
- Kothandan SK. 2014. School based interventions versus family based interventions in the treatment of childhood obesity- a systematic review . Archives of public health = Archives belges de sante publique 72 : 3. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kumar S, Kelly AS. 2017. Review of Childhood Obesity: From Epidemiology, Etiology, and Comorbidities to Clinical Assessment and Treatment . Mayo Clinic Proceedings 92 : 251–65 [ PubMed ] [ Google Scholar ]
- Kyle TK, Dhurandhar EJ, Allison DB. 2016. Regarding Obesity as a Disease: Evolving Policies and Their Implications . Endocrinology and metabolism clinics of North America 45 : 511–20 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Landsverk J, Brown CH, Smith JD, Chamberlain P, Palinkas LA, et al. 2017. Design and analysis in dissemination and implementation research In Dissemination and implementation research in health: Translating research to practice , ed. Brownson RC, Colditz GA, Proctor EK, pp. 201–27. New York: Oxford University Press [ Google Scholar ]
- Lang JE, Fitzpatrick AM, Mauger DT, Guilbert TW, Jackson DJ, et al. 2018. Overweight/obesity status in preschool children associates with worse asthma but robust improvement on inhaled corticosteroids . Journal of Allergy and Clinical Immunology 141 : 1459–67.e2 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lang JE, Hossain MJ, Lima JJ. 2015. Overweight children report qualitatively distinct asthma symptoms: analysis of validated symptom measures . The Journal of allergy and clinical immunology 135 : 886–93.e3 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lebow J, Sim LA, Kransdorf LN. 2015. Prevalence of a History of Overweight and Obesity in Adolescents With Restrictive Eating Disorders . Journal of Adolescent Health 56 : 19–24 [ PubMed ] [ Google Scholar ]
- Leppert B, Junge KM, Röder S, Borte M, Stangl GI, et al. 2018. Early maternal perceived stress and children’s BMI: longitudinal impact and influencing factors . BMC Public Health 18 : 1211. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ling J, Robbins LB, Wen F. 2016. Interventions to prevent and manage overweight or obesity in preschool children: A systematic review . International Journal of Nursing Studies 53 : 270–89 [ PubMed ] [ Google Scholar ]
- Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, et al. 2010. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s strategic impact goal through 2020 and beyond . Circulation 121 : 586–613 [ PubMed ] [ Google Scholar ]
- Ludwig DS. 2016. Lifespan Weighed Down by DietDiet and Decreasing LifespanDiet and Decreasing Lifespan . JAMA 315 : 2269–70 [ PubMed ] [ Google Scholar ]
- Lydecker JA, Grilo CM. 2016. The apple of their eye: Attitudinal and behavioral correlates of parents’ perceptions of child obesity . Obesity 24 : 1124–31 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lydecker JA, O’Brien E, Grilo CM. 2018. Parents have both implicit and explicit biases against children with obesity . Journal of Behavioral Medicine 41 : 784–91 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Marchesini G, Petta S, Dale Grave R. 2015. Diet, Weight Loss, and Liver Health in NAFLD: Pathophysiology, Evidence and Practice . Hepatology [ PubMed ]
- Marshall SA, Ip EH, Suerken CK, Arcury TA, Saldana S, et al. 2018. Relationship between maternal depression symptoms and child weight outcomes in Latino farmworker families . Maternal & Child Nutrition 14 : e12614. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- May AL, Kuklina EV, Yoon PW. 2012. Prevalence of cardiovascular disease risk factors among us adolescents, 1999–2008 . Pediatrics 129 : 1035–41 [ PubMed ] [ Google Scholar ]
- McCrabb S, Lane C, Hall A, Milat A, Bauman A, et al. 2019. Scaling-up evidence-based obesity interventions: A systematic review assessing intervention adaptations and effectiveness and quantifying the scale-up penalty . Obesity Reviews 20 : 964–82 [ PubMed ] [ Google Scholar ]
- McNulty M, Smith JD, Villamar J, Burnett-Zeigler I, Vermeer W, et al. 2019. Implementation Research Methodologies for Achieving Scientific Equity and Health Equity . In Ethnicity & disease , pp. 83–92 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Michalsky M, Reichard K, Inge T, Pratt J, Lenders C. 2012. ASMBS pediatric committee best practice guidelines . Surgery for obesity and related diseases : official journal of the American Society for Bariatric Surgery 8 : 1–7 [ PubMed ] [ Google Scholar ]
- Milaneschi Y, Simmons WK, van Rossum EFC, Penninx BWJH. 2019. Depression and obesity: evidence of shared biological mechanisms . Molecular Psychiatry 24 : 18–33 [ PubMed ] [ Google Scholar ]
- Miller AL, Lumeng JC, LeBourgeois MK. 2015. Sleep patterns and obesity in childhood . Current Opinion in Endocrinology Diabetes and Obesity 22 : 41–47 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mitchell TB, Amaro CM, Steele RG. 2016. Pediatric Weight Management Interventions in Primary Care Settings: A Meta-Analysis . Health Psychol [ PubMed ]
- Mühlig Y, Antel J, Föcker M, Hebebrand J. 2016. Are bidirectional associations of obesity and depression already apparent in childhood and adolescence as based on high-quality studies? A systematic review . Obesity Reviews 17 : 235–49 [ PubMed ] [ Google Scholar ]
- Narang I, Mathew JL. 2012. Childhood obesity and obstructive sleep apnea . J Nutr Metab 2012 : 134202–02 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Natale RA, Messiah SE, Asfour LS, Uhlhorn SB, Englebert NE, Arheart KL. 2017. Obesity Prevention Program in Childcare Centers: Two-Year Follow-Up . American journal of health promotion : AJHP 31 : 502–10 [ PubMed ] [ Google Scholar ]
- National Center for Health Statistics. 2019. National Asthma Data (2017 National Health Interview Survey) , Centers for Disease Control and Prevention [ Google Scholar ]
- Ng M, Fleming T, Robinson M, Thomson B, Graetz N, et al. 2014. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013 . The Lancet 384 : 766–81 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nobili V, Alkhouri N, Alisi A, Della Court C, Fitzpatrick E, et al. 2015. Nonalcoholic fatty liver disease: A challenge for pediatricians . JAMA Pediatrics 169 : 170–76 [ PubMed ] [ Google Scholar ]
- O'Connor SG, Maher JP, Belcher BR, Leventhal AM, Margolin G, et al. 2017. Associations of maternal stress with children's weight-related behaviours: a systematic literature review . Obesity Reviews 18 : 514–25 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- O’Connor EA, Evans CV, Burda BU, Walsh ES, Eder M, Lozano P. 2017. Screening for Obesity and Intervention for Weight Management in Children and Adolescents: Evidence Report and Systematic Review for the US Preventive Services Task ForceUSPSTF Evidence Report: Screening for Obesity in Children and YouthUSPSTF Evidence Report: Screening for Obesity in Children and Youth . JAMA 317 : 2427–44 [ PubMed ] [ Google Scholar ]
- Ogden CL, Carroll MD, Fakhouri TH, Hales CM, Fryar CD, et al. 2018. Prevalence of obesity among youths by household income and education level of head of household—United States 2011–2014 . Morbidity and Mortality Weekly Report 67 : 186. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Paruthi S, Brooks LJ, D'Ambrosio C, Hall WA, Kotagal S, et al. 2016. Recommended Amount of Sleep for Pediatric Populations: A Consensus Statement of the American Academy of Sleep Medicine . J Clin Sleep Med 12 : 785–86 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Peirson L, Fitzpatrick-Lewis D, Morrison K, Ciliska D, Kenny M, et al. 2015a. Prevention of overweight and obesity in children and youth: a systematic review and meta-analysis . CMAJ open 3 : E23 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Peirson L, Fitzpatrick-Lewis D, Morrison K, Warren R, Usman Ali M, Raina P. 2015b. Treatment of overweight and obesity in children and youth: a systematic review and meta-analysis . CMAJ open 3 : E35–E46 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, et al. 2018. The Physical Activity Guidelines for AmericansPhysical Activity Guidelines for AmericansPhysical Activity Guidelines for Americans . JAMA 320 : 2020–28 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pont SJ, Puhl R, Cook SR, Slusser W. 2017. Stigma Experienced by Children and Adolescents With Obesity . Pediatrics 140 : e20173034. [ PubMed ] [ Google Scholar ]
- Pratt KJ, Skelton JA. 2018. Family Functioning and Childhood Obesity Treatment: a Family Systems Theory-Informed Approach . Academic Pediatrics [ PMC free article ] [ PubMed ]
- Proctor E, Powell BJ, McMillen JC. 2013. Implementation strategies: recommendations for specifying and reporting . Implement Sci 8 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pulgaron ER, Delamater AM. 2014. Obesity and type 2 diabetes in children: epidemiology and treatment . Current diabetes reports 14 : 508. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Robinson TN, Banda JA, Hale L, Lu AS, Fleming-Milici F, et al. 2017. Screen Media Exposure and Obesity in Children and Adolescents . Pediatrics 140 : S97–S101 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rupp K, McCoy SM. 2019. Bullying Perpetration and Victimization among Adolescents with Overweight and Obesity in a Nationally Representative Sample . Childhood Obesity [ PMC free article ] [ PubMed ]
- Russell CG, Russell A. 2019. A biopsychosocial approach to processes and pathways in the development of overweight and obesity in childhood: Insights from developmental theory and research . Obesity Reviews 20 : 725–49 [ PubMed ] [ Google Scholar ]
- Savage JS, Birch LL. 2017. WIC mothers' depressive symptoms are associated with greater use of feeding to soothe, regardless of perceived child negativity . Pediatr Obes 12 : 155–62 [ PubMed ] [ Google Scholar ]
- Schlam TR, Wilson NL, Shoda Y, Mischel W, Ayduk O. 2013. Preschoolers' delay of gratification predicts their body mass 30 years later . J Pediatr 162 : 90–3 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Shankardass K, McConnell R, Jerrett M, Lam C, Wolch J, et al. 2014. Parental stress increases body mass index trajectory in pre-adolescents . Pediatr Obes 9 : 435–42 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Shatat IF, Brady TM. 2018. Editorial: Pediatric Hypertension: Update . Frontiers in Pediatrics 6 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sheinbein DH, Stein RI, Hayes JF, Brown ML, Balantekin KN, et al. 2019. Factors associated with depression and anxiety symptoms among children seeking treatment for obesity: A social-ecological approach . Pediatr Obes : e12518. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Shloim N, Edelson LR, Martin N, Hetherington MM. 2015. Parenting Styles, Feeding Styles, Feeding Practices, and Weight Status in 4-12 Year-Old Children: A Systematic Review of the Literature . Front Psychol 6 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Simmonds M, Llewellyn A, Owen CG, Woolacott N. 2016. Predicting adult obesity from childhood obesity: a systematic review and meta-analysis . Obesity Reviews 17 : 95–107 [ PubMed ] [ Google Scholar ]
- Sisson SB, Krampe M, Anundson K, Castle S. 2016. Obesity prevention and obesogenic behavior interventions in child care: A systematic review . Preventive Medicine 87 : 57–69 [ PubMed ] [ Google Scholar ]
- Skinner AC, Perrin EM, Moss LA, Skelton JA. 2015. Cardiometabolic Risks and Severity of Obesity in Children and Young Adults . New England Journal of Medicine 373 : 1307–17 [ PubMed ] [ Google Scholar ]
- Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC. 2018. Prevalence of Obesity and Severe Obesity in US Children, 1999–2016 . Pediatrics 141 : e20173459. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sleddens EFC, Gerards SMPL, Thijs C, de Vries NK, Kremers SPJ. 2011. General parenting, childhood overweight and obesity-inducing behaviors: A review . International Journal of Pediatric Obesity 6 : e12–e27 [ PubMed ] [ Google Scholar ]
- Smith JD, Berkel C, Jordan N, Atkins DC, Narayanan SS, et al. 2018a. An individually tailored family-centered intervention for pediatric obesity in primary care: Study protocol of a randomized type II hybrid implementation-effectiveness trial (Raising Healthy Children study) . Implementation Science 13 : 1–15 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Smith JD, Berkel C, Rudo-Stern J, Montaño Z, St George SM, et al. 2018b. The Family Check-Up 4 Health (FCU4Health): Applying implementation science frameworks to the process of adapting an evidence-based parenting program for prevention of pediatric obesity and excess weight gain in primary care . Frontiers in public health 6 : 293. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Smith JD, Berkel C, Rudo-Stern J, Montaño Z, St. George SM, et al. 2018c. The Family Check-Up 4 Health (FCU4Health): Applying implementation science frameworks to the process of adapting an evidence-based parenting program for prevention of pediatric obesity and excess weight gain in primary care . Frontiers in Public Health [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Smith JD, Egan KN, Montaño Z, Dawson-McClure S, Jake-Schoffman DE, et al. 2018d. A developmental cascade perspective of paediatric obesity: Conceptual model and scoping review . Health Psychology Review 12 : 271–93 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Smith JD, Montaño Z, Dishion TJ, Shaw DS, Wilson MN. 2015. Preventing weight gain and obesity: Indirect effects of a family-based intervention in early childhood . Prevention Science 16 : 408–19 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Smith JD, Montaño Z, Maynard A, Miloh T. 2017a. Family Functioning Predicts Body Mass Index and Biochemical Levels of Youths with Nonalcoholic Fatty Liver Disease . Journal of Developmental & Behavioral Pediatrics 38 : 155–60 [ PubMed ] [ Google Scholar ]
- Smith JD, St. George SM, Prado G. 2017b. Family-centered positive behavior support interventions in early childhood to prevent obesity . Child Development 88 : 427–35 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sommer A, Twig G. 2018. The Impact of Childhood and Adolescent Obesity on Cardiovascular Risk in Adulthood: a Systematic Review . Curr Diab Rep 18 : 91. [ PubMed ] [ Google Scholar ]
- Sonneville KR, Grilo CM, Richmond TK, Thurston IB, Jernigan M, et al. 2015. Prospective association between overvaluation of weight and binge eating among overweight adolescent girls . The Journal of adolescent health : official publication of the Society for Adolescent Medicine 56 : 25–9 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- St. George SM, Agosto Y, Rojas L, Soares M, Bahamon M, et al. in press. A developmental cascade perspective of pediatric obesity: A systematic review of preventive interventions from infancy through late adolescence . Obesity Reviews [ PMC free article ] [ PubMed ]
- Stevens SD, Herbozo S, Morrell HE, Schaefer LM, Thompson JK. 2017. Adult and childhood weight influence body image and depression through weight stigmatization . Journal of health psychology 22 : 1084–93 [ PubMed ] [ Google Scholar ]
- Stout SA, Espel EV, Sandman CA, Glynn LM, Davis EP. 2015. Fetal programming of children's obesity risk . Psychoneuroendocrinology 53 : 29–39 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sung-Chan P, Sung YW, Zhao X, Brownson RC. 2013. Family-based models for childhood-obesity intervention: A systematic review of randomized controlled trials . Obesity Reviews 14 : 265–78 [ PubMed ] [ Google Scholar ]
- Tanofsky-Kraff M, Cohen ML, Yanovski SZ, Cox C, Theim KR, et al. 2006. A Prospective Study of Psychological Predictors of Body Fat Gain Among Children at High Risk for Adult Obesity . Pediatrics 117 : 1203–09 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Tate EB, Wood W, Liao Y, Dunton GF. 2015. Do stressed mothers have heavier children? A meta-analysis on the relationship between maternal stress and child body mass index . Obesity reviews : an official journal of the International Association for the Study of Obesity 16 : 351–61 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Taveras EM, Gillman MW, Peña M-M, Redline S, Rifas-Shiman SL. 2014. Chronic Sleep Curtailment and Adiposity . Pediatrics 133 : 1013–22 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Taylor JH, Xu Y, Li F, Shaw M, Dziura J, et al. 2017. Psychosocial predictors and moderators of weight management programme outcomes in ethnically diverse obese youth . Pediatric Obesity 12 : 453–61 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Taylor RW, Cox A, Knight L, Brown DA, Meredith-Jones K, et al. 2015. A Tailored Family-Based Obesity Intervention: A Randomized Trial . Pediatrics 136 : 281. [ PubMed ] [ Google Scholar ]
- Tomiyama AJ, Finch LE, Belsky ACI, Buss J, Finley C, et al. 2015. Weight bias in 2001 versus 2013: Contradictory attitudes among obesity researchers and health professionals . Obesity 23 : 46–53 [ PubMed ] [ Google Scholar ]
- US Preventive Services Task Force. 2017. Screening for Obesity in Children and Adolescents: US Preventive Services Task Force Recommendation Statement . JAMA 317 : 2417–26 [ PubMed ] [ Google Scholar ]
- Vehmeijer FOL CV Silva C, Derks IPM, El Marroun H, Oei EHG, et al. 2019. Associations of Maternal Psychological Distress during Pregnancy with Childhood General and Organ Fat Measures . Childhood Obesity [ PubMed ] [ Google Scholar ]
- Wang Y, Cai L, Wu Y, Wilson RF, Weston C, et al. 2015. What childhood obesity prevention programmes work? A systematic review and meta-analysis . Obesity Reviews 16 : 547–65 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ward DS, Welker E, Choate A, Henderson KE, Lott M, et al. 2017. Strength of obesity prevention interventions in early care and education settings: A systematic review . Preventive Medicine 95 : S37–S52 [ PubMed ] [ Google Scholar ]
- Warnakulasuriya LS, Fernando MMA, Adikaram AVN, Thawfeek ARM, Anurasiri WL, et al. 2018. Metformin in the Management of Childhood Obesity: A Randomized Control Trial . Childhood obesity (Print) 14 : 553–65 [ PubMed ] [ Google Scholar ]
- Wen M, Simpson JM, Baur LA, Rissel C, Flood VM. 2011. Family functioning and obesity risk behaviors: Implications for early obesity intervention . Obesity 19 : 1252–58 [ PubMed ] [ Google Scholar ]
- Whitlock EP, O'Connor EA, Williams SB, Beil TL, Lutz KW. 2010. Effectiveness of weight management interventions in children: A targeted systematic review for the USPSTF . Pediatrics 125 : e396–e418 [ PubMed ] [ Google Scholar ]
- Wuhl E 2019. Hypertension in childhood obesity . Acta paediatrica (Oslo, Norway : 1992) 108 : 37–43 [ PubMed ] [ Google Scholar ]
- Yackobovitch-Gavan M, Wolf Linhard D, Nagelberg N, Poraz I, Shalitin S, et al. 2018. Intervention for childhood obesity based on parents only or parents and child compared with follow-up alone . Pediatric Obesity 13 : 647–55 [ PubMed ] [ Google Scholar ]
- Search Menu
- Advance articles
- Author Guidelines
- Submission Site
- Open Access
- About Family Practice
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Lay summary, introduction, conclusions, acknowledgements, ethical approval, conflict of interest, data availability.
- < Previous
Doctors and patients’ perspectives on obesity. A Q-methodology study
Both authors contributed equally to the study.
- Article contents
- Figures & tables
- Supplementary Data
Qays Shahed, Karolina Baranowska, Marije C Galavazi, Yang Cao, Michiel A van Nieuwenhoven, Doctors and patients’ perspectives on obesity. A Q-methodology study, Family Practice , Volume 39, Issue 4, August 2022, Pages 694–700, https://doi.org/10.1093/fampra/cmab169
- Permissions Icon Permissions
Obesity is associated with stigma and discrimination. Health care providers should approach these patients professionally and without stigma, since treatment of obesity requires a relationship with mutual understanding between the doctor and patient.
To explore how patients and general practitioners (GPs) perceive obesity, using Q-methodology, which allows quantitative analysis of qualitative data.
A Q-methodology study, comprising 24 patients with obesity and 24 GPs. We created 48 statements with viewpoints on obesity. All participants sorted these statements in a forced grid with a quasi-normal distribution ranking from −5 (most disagree) to +5 (most agree). Subsequently, factor analysis was performed. Six patients were interviewed to explain their viewpoints.
Analysis yielded 3 dominant groups (factors) of patients: (i) They acknowledge the importance of healthy lifestyle and feel mistreated by health care. (ii) They have a decreased quality of life, but do not blame health care, and (iii) They don’t need treatment and don’t have an impaired quality of life. For the GPs, the 3 dominant factors were: (i) They have understanding for the patients and feel that health care is insufficient, (ii) They believe that obesity may be hereditary but mainly is a lifestyle problem, and (iii) They believe obesity can be treated but is very difficult.
Viewpoints on obesity were different, both within and between the groups. Some GPs consider obesity mainly as a lifestyle problem, rather than a chronic disease. If patients and doctors can find mutual viewpoints on obesity, both patient satisfaction and a treatment strategy will be more effective.
Obesity affects quality of life and increases the risk of diseases such as type 2 diabetes, fatty liver disease, cardiovascular disease, and cancer. Achieving and maintaining weight loss is difficult and for this reason a mutual understanding between the general practitioner (GP) and the patient is crucial. We used Q-methodology to study the patients and GPs perspectives on obesity. We show that there are different groups of patients that have different perspectives on obesity, but also different groups of doctors who have different perspectives on obesity. If the GP is aware of the fact that the patients’ viewpoints regarding obesity may be different than his/her own viewpoints, it allows improvement of the doctor–patient communication and hence, patient satisfaction.
Viewpoints on obesity differ, both within and between patients and GPs.
Different subgroups of viewpoints on obesity can be identified with Q-methodology.
Some GPs consider obesity a lifestyle problem, rather than a chronic disease.
Q-method is suitable for investigating subjective experiences and perspectives.
The misconception that obesity is a lifestyle choice, that can be reversed simply by exercising willpower, has become cemented in the minds of the general public and much of the medical profession. However, obesity has now been acknowledged by the European Commission as a disease in its own right. 1 The obesity pandemic is getting worse in both adults and children and adolescents. 2 In Sweden, 15% of women and 16% of men suffer from obesity. 3 It is a complex chronic metabolic disease with a multifactorial pathogenesis, 4 associated with type 2 diabetes mellitus, nonalcoholic fatty liver disease, cardiovascular diseases, and different types of cancer. 5 In addition, obesity has consequences for mental health as a result of weight stigma and discrimination, and may lead to social isolation. 6 Current treatments for obesity comprise lifestyle changes including diet and exercise, drugs, psychotherapy, and bariatric surgery. 7
The general practitioner (GP) is often the first doctor who meets the patient with obesity-related problems. However, as mentioned above, many GPs do not consider obesity as a serious medical condition that requires treatment, 8 but rather as a lifestyle problem. This discrepancy has a negative impact on the relationship between doctors and patients. In addition, there is scepticism regarding the treatment options for obesity, but GPs still recommended them in order to maintain a good relationship with the patient. 9 Previous research demonstrates the importance of good communication between GPs and patients to increase the probability that an intervention will become successful. 10
One method to study people’s perspectives on a certain topic is via Q-methodology, which is a combined qualitative and quantitative method for investigating subjectivity. 11 , 12 This method is well-established in the social sciences, but remains a relatively novel approach in the medical sciences. It provides a systematic procedure for examining the subjective components of human behaviour, where all the viewpoints of the subjects are clustered into different groups, called factors. 11
Firstly, the researcher gathers all kinds of opinions, beliefs, and information about a topic from different sources, such as previous research and interviews 13 and creates statements about the topic. This is followed by an evaluation of the statements, performed by a group of experts within the topic, to increase the value and content, but also to minimize researcher bias. This evaluation leads to the creation of a so-called Q-set; the final set of statements that will be used. Secondly, the study population is selected, and the viewpoints of the participants should match the research question. 14 Subsequently, the participants rank the statements from their individual perspective using a grid with a quasi-normal, forced distribution (see Fig. 1 ). The grid has the same number of cells as there are statements and has a rating scale from −5 to +5 which represents “most disagree” to “most agree.” All statements must be placed in the grid. 11 In addition, qualitative information can be collected by interviewing participants about their most extreme rankings. When the ranking is completed, all responses are reduced to a few different factors. 14 Each factor represents a distinct group of participants who share similar views. 12 The number of extracted factors is usually between 3 and 6. 14 Thereafter, a factor rotation is performed to make the factors more explainable. Each factor provides information that defines that factor. 11

Score grid for Q-sorting.
The aim of our study was to analyse both the patients and the GPs perceptions about obesity using Q-methodology, and to compare them with each other.
Setting and data sources
We searched for opinions and viewpoints on obesity in different articles and in forums. This led to 52 statements. An expert group from the Obesity Unit (consisting of a doctor, a nurse, a dietician, a psychologist, and a physiotherapist) evaluated these statements and selected a Q-set comprising 48 statements. We transferred the Q-set to www.qmethodsoftware.com , and evaluated the statements to confirm that the language was understandable and that the Q-set could be distributed within the forced-choice grid without conflicts.
Twenty-four doctors, all GPs or GP residents (16 men and 8 women), and 24 patients with obesity (21 women and 3 men) were included. The number of participants is based on the convention that 1 needs roughly half as many participants as there are statements. Patients with obesity were recruited face to face via the obesity unit of the University hospital in Örebro. The participating GPs were recruited during a local primary health care conference. The inclusion criteria for the patients were: (i) body mass index >30 kg/m 2 and (ii) that they had not started with a weight-loss program provided by the Obesity Unit, since we did not want them to be influenced by the information that they would receive during this program. All participants were informed about the purpose and procedure of the study and signed an informed consent. There was no dropping-out. For the patients, the Q-methodology data were collected at the Obesity Unit, Örebro University Hospital. For the GPs, the Q-methodology data were collected at their workplace. No other individuals were present during the data collection. One member of the research team (KB, female, medical doctor) also consecutively interviewed 6 patients to obtain qualitative information about their most extreme rankings, and field notes were made. No standard questionnaire was used for the interviews. The transcripts were not returned to the patients but were verified directly on the spot. Each interview took approximately 30 min. There was no earlier relationship between the participants and the research group. The research group was not biased in any way with respect to viewpoints regarding obesity.
Data analysis
Two members from the research team (QS and KB) imported the anonymized results in PQMethod software. 8 The first step in the analysis was data reduction to summarize factors based on principal component analysis (PCA). The factors were extracted from both the patient and the GP group. We calculated the Z -scores, based on the factor scores from the PCA for every statement, which represented how much each factor agreed or disagreed on every statement. 12 A Pearson’s correlation analysis was performed (SPSS Statistics version 25, IBM Corp, Armonk, NY) to compare the 2 groups, using the Z -scores from every statement from the patient and GP factors.
We extracted 3 different factors from each group. Each factor represented a general viewpoint and was named after their distinguishing statements, as shown in Tables 1 and 2 . Correlations between Z -scores for each statement between all factors are presented in Table 3 .
Distinguishing statements for the patient factors and their rank scores.
Bold value shows the rank score of significant statements for the specified patient factor.
Distinguishing statements for the GP factors and their rank scores.
Correlations between Z -scores for each statement between all factors according to Pearson’s correlation analysis ( P values).
The table shows that the correlations between the factors varied. Patient factor 1 had the highest correlation ( r = 0.808, P = <0.001) with GP factor 1. However, it has a weak correlation with other GP factors. Patient factor 2 correlated well with all GP factors, meanwhile, patient factor 3 had a moderate correlation with 2 GP factors and the lowest correlation with GP factor 2.
Table 4 shows the statements where the different patients and GP factors agreed and disagreed on most. The extracted factors from the patients explained 62% of the variance of the original Q-sorts and the extracted 3 factors from the GPs also explained 62% of the variance. In factor analysis, this is considered as a valid and acceptable proportion of variance explained by a construct.
Statements where the different patients and GP factors agreed and disagreed on most.
The table shows the similarities and differences between the patient factors and GP factors. Among the patients, many personal statements were ranked highly. Among the GPs, medical facts about obesity were ranked highly. The majority disagreed with statement 26 and the majority agreed with statement 27. All GP factors and 1 patient factor agreed the most with statement 21, meanwhile 2 patient factors and 1 GP factor ranked statement 25 very highly.
Factor 1 (patients): have knowledge about healthy food- and exercise habits and feel mistreated by health care providers
Nine patients showed knowledge about lifestyle changes that lead to weight loss but they do not have good experiences with these lifestyle changes. In contrast to the other patients’ viewpoints, these patients strongly feel that health care is mistreating them.
One patient said:
I received documentation about a gastric bypass when I sought care for a urinary tract infection. They only think that I have to train more, eat a low-calorie diet or should have a gastric bypass. You do not get help or support for anything else. Factor 2 (patients): suffering from obesity for a long time but do not blame health care providers
Seven patients with obesity highlighted that early childhood is the time when food- and exercise habits are developed and that there is a hereditary component. These patients confirm that obesity affects their quality of life. They believe that doctors have sufficient knowledge about obesity and that they receive support from health care providers. One patient said:
“I have had problems with my weight and hypothyroidism since birth and even though I am told to eat right and despite doing so, you are criticized that you do not. Throughout my whole childhood, I have eaten according to the plate model but I am still not properly treated.”
This patient explained that she felt criticized by her environment and although she felt that she was not treated adequately, she understood how difficult it is to treat obesity.
Factor 3 (patients): do not think that obesity has an impact on the quality of life and do not think they need any help
Five patients believed that obesity does not affect the quality of life and that it is not a hereditary condition. Although they are aware of their condition, they do not think they need treatment, and in contrast to other viewpoints, they do not think that obesity is a lifelong disease. One patient said:
I think obesity depends on many things, both medications but also life situation. I think that if you look backward and look when you became obese, you can relate it to something that happened during that time.
Factor 1 (GP): understand the patients and believe that health care provides insufficient support
Ten doctors believed they have insufficient knowledge about obesity and that health care providers treat the patients with obesity worse than those without obesity. There is a certain understanding for these patients. Distinguishing for this viewpoint is that they are not sure whether there is an effective treatment for obesity.
Factor 2 (GP): believe that obesity is hereditary and an eating disorder
Four doctors believed that obesity is an eating disorder, as well as a hereditary condition. They agreed the least with the statement that people with obesity are negatively judged and disagreed the least with the statement that losing weight is easy.
Factor 3 (GPs): obesity is not a lifelong disease but it is difficult to lose weight
Seven doctors believed that patients with obesity have a healthy lifestyle and that it is sufficient to change food habits to lose weight. However, they do not have an opinion regarding whether weight loss increases the quality of life or whether exercise leads to weight loss. Distinguishing from the other viewpoints, they believe that obesity is not a lifelong disease.
Several studies have shown the importance of good communication between GPs and patients. 10 In our study we focussed on the different perspectives on obesity both within and between GPs and patients. Our findings show some differences and similarities in ranking between the distinguishing statements for the patients and GPs, leading to 6 different factors on obesity. Three factors from patients and 3 factors from GPs were considered important in this study.
Comparison to existing literature
Patient factor 1 underlined their belief of the importance of combining diet and exercise for an effective weight loss 15 even though other studies suggest that also behavioural strategies such as self-monitoring are required for a successful result. 16 Besides that, this group agreed strongly on the statement that health care providers treat patients with obesity worse than those without obesity, which the other groups did not. This patient factor had a high correlation with GP factor 1. The correlation between patient factor 1 and the other GP factors was much lower, which may be explained by the fact that these GPs did not highlight statements that were associated with discrimination and lack of knowledge about obesity. Instead, they highlighted medical facts about obesity, which these patients did not take into consideration.
In patient factor 2, this group seemed to have struggled with obesity for a long time and they were unsure whether health care providers could do more for them. This patient group believed that patients with obesity have unhealthy eating habits, and they were neutral about their knowledge regarding obesity-associated health risks. They confirmed that doctors have adequate knowledge about obesity, and did not feel that they were treated any differently than patients without obesity. This is in line with studies in which patients with obesity reported positive experiences with health care. 17 They also confirmed that obesity has an impact on quality of life, thus confirming previous research regarding the relationship between obesity and a decreased quality of life. 18 This viewpoint had a similar correlation with all the GP viewpoints, which means that they share similar opinions about these statements.
Patient factor 3 differed from the other patient factors and showed a believe that patients with obesity neither need treatment, nor have an impaired quality of life. This shows that there are patients with obesity who are less affected by their condition. These patients strongly disagreed on the statement that patients with obesity suffer from impaired mental health, although previous studies demonstrate that obesity and depression often coexist and are interrelated. 19 , 20 They also disagreed on the statement that obesity is a hereditary condition, and they were neutral about obesity as being a persons’ own choice, as well as that they agreed on that patients with obesity have healthy food habits. These patients neither seemed to feel bad about having obesity, nor did they want any help and nor did they consider obesity as a lifelong disease, which almost all other viewpoints did, except GP factor 3. Patient factor 3 had the lowest correlation with all GP viewpoints, especially with GP factor 2, who strongly agreed on obesity as an eating disorder and strongly agreed on obesity as a hereditary condition. Obviously, this group do not consider obesity as a chronic metabolic disease.
Strengths and limitations
We used a method that is well established in the social sciences, but remains a relatively novel approach in medical sciences. The major strength of this method is that Q-methodology allows statistical interpretation of qualitative data and provides a powerful method to investigate differences and similarities in viewpoints between doctors and patients regarding their condition.
There are some limitations. Selection bias may have been introduced. The GPs who participated may have been more interested in obesity and were motivated to make a change, compared with the GPs that did not choose to participate. Secondly, the participating patients may have had more negative experiences with health care providers and they may experience a more impaired health and participated for this reason.
We showed that viewpoints on obesity are different, both within and between patients and GPs. A patient may have completely different viewpoints regarding his/her condition than the GP. Some GPs show viewpoints that are not supported by the current knowledge, such as considering obesity mainly as a lifestyle problem, rather than a chronic disease. In addition, our findings show that a considerable number of patients feel stigmatized because of their obesity, and experience impaired quality of life. For these reasons, awareness of these differences is relevant for clinical practice; if the GP and the patient are able to find mutual viewpoints about obesity, patient satisfaction will improve and a treatment and/or support strategy will be more effective.
The study was funded by departmental resources.
We thank the professionals at the Obesity Unit at the Örebro University Hospital for their support with the review of the Q-sort statements.
Ethical approval was granted by the Etikprövningsmyndigheten Uppsala (Dnr 2019-04756).
None declared.
The data underlying this article will be shared on reasonable request to the corresponding author.
Burki T. European Commission classifies obesity as a chronic disease [published online ahead of print, 2021 Jun 1]. Lancet Diabetes Endocrinol . 2021 ; 9 ( 7 ): 418 . doi: 10.1016/S2213-8587(21)00145-5
Google Scholar
Engin A. The definition and prevalence of obesity and metabolic syndrome. Adv Exp Med Biol . 2017 ; 960 : 1 – 17 .
Statistik om övervikt och fetma—Folkhälsomyndigheten. n.d . Övervikt och fetma . [accessed 2020 Oct 22 ]. https://www.folkhalsomyndigheten.se/folkhalsorapportering-statistik/tolkad-rapportering/folkhalsans-utveckling/resultat/halsa/overvikt-och-fetma/
Google Preview
Manna P , Jain SK. Obesity, oxidative stress, adipose tissue dysfunction, and the associated health risks: causes and therapeutic strategies. Metab Syndr Relat Disord . 2015 ; 13 ( 10 ): 423 – 444 .
Goossens GH. The metabolic phenotype in obesity: fat mass, body fat distribution, and adipose tissue function. Obes Facts . 2017 ; 10 ( 3 ): 207 – 215 .
Brewis A , SturtzSreetharan C , Wutich A. Obesity stigma as a globalizing health challenge. Global Health . 2018 ; 14 ( 1 ): 20 .
Natvik E , Råheim M , Andersen JR , Moltu C. Living a successful weight loss after severe obesity. Int J Qual Stud Health Well-being . 2018 ; 13 ( 1 ): 1487762 .
Schwenke M , Luppa M , Welzel FD , Löbner M , Luck-Sikorski C , Kersting A , Blüher M , Riedel-Heller SG. Attitudes and treatment practice of general practitioners towards patients with obesity in primary care. BMC Fam Pract . 2020 ; 21 ( 1 ): 169 .
Epstein L , Ogden J. A qualitative study of GPs’ views of treating obesity. Br J Gen Pract . 2005 ; 55 ( 519 ): 750 – 754 .
Ogden J , Bandara I , Cohen H , Farmer D , Hardie J , Minas H , Moore J , Qureshi S , Walter F , Whitehead MA. General practitioners’ and patients’ models of obesity: whose problem is it? Patient Educ Couns . 2001 ; 44 ( 3 ): 227 – 233 .
Akhtar-Danesh N. Qfactor: a command for Q-methodology analysis. Stata J . 2018 ; 18 ( 2 ): 432 – 446 .
Zabala A , Pascual U. Bootstrapping Q methodology to improve the understanding of human perspectives. PLoS One . 2016 ; 11 ( 2 ): e0148087 .
Klooster P , Visser M , de Jong M. Comparing two image research instruments: the Q-sort method versus the Likert attitude questionnaire. Food Qual Prefer . 2008 ; 19 ( 5 ): 511 – 518 .
Watts S. Develop a Q methodological study. Educ Prim Care . 2015 ; 26 ( 6 ): 435 – 437 .
Ramage S , Farmer A , Eccles KA , McCargar L. Healthy strategies for successful weight loss and weight maintenance: a systematic review. Appl Physiol Nutr Metab . 2014 ; 39 ( 1 ): 1 – 20 .
Berg C , Forslund HB. The influence of portion size and timing of meals on weight balance and obesity. Curr Obes Rep . 2015 ; 4 ( 1 ): 11 – 18 .
Thomas SL , Hyde J , Karunaratne A , Herbert D , Komesaroff PA. Being ‘fat’ in today’s world: a qualitative study of the lived experiences of people with obesity in Australia. Health Expect . 2008 ; 11 ( 4 ): 321 – 330 .
Kolotkin RL , Andersen JR. A systematic review of reviews: exploring the relationship between obesity, weight loss and health-related quality of life. Clin Obes . 2017 ; 7 ( 5 ): 273 – 289 .
Nigatu YT , Bültmann U , Schoevers RA , Penninx BWJH , Reijneveld SA. Does obesity along with major depression or anxiety lead to higher use of health care and costs? A 6-year follow-up study. Eur J Public Health . 2017 ; 27 ( 6 ): 965 – 971 .
Lupinno FS , de Wit LM , Bouvy PF , Stijnen T , Cuijpers P , Penninx BWJH , Zitman FG. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry . 2010 ; 67 ( 3 ): 220 – 229 .
Author notes
- client satisfaction
- quality of life
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1460-2229
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
470 Obesity Essay Topic Ideas & Examples
Looking for obesity essay topics? Being a serious problem, obesity is definitely worth writing about.
9.1 Developing a Strong, Clear Thesis Statement
Learning objectives.
- Develop a strong, clear thesis statement with the proper elements.
- Revise your thesis statement.
Have you ever known a person who was not very good at telling stories? You probably had trouble following his train of thought as he jumped around from point to point, either being too brief in places that needed further explanation or providing too many details on a meaningless element. Maybe he told the end of the story first, then moved to the beginning and later added details to the middle. His ideas were probably scattered, and the story did not flow very well. When the story was over, you probably had many questions.
Just as a personal anecdote can be a disorganized mess, an essay can fall into the same trap of being out of order and confusing. That is why writers need a thesis statement to provide a specific focus for their essay and to organize what they are about to discuss in the body.
Just like a topic sentence summarizes a single paragraph, the thesis statement summarizes an entire essay. It tells the reader the point you want to make in your essay, while the essay itself supports that point. It is like a signpost that signals the essay’s destination. You should form your thesis before you begin to organize an essay, but you may find that it needs revision as the essay develops.
Elements of a Thesis Statement
For every essay you write, you must focus on a central idea. This idea stems from a topic you have chosen or been assigned or from a question your teacher has asked. It is not enough merely to discuss a general topic or simply answer a question with a yes or no. You have to form a specific opinion, and then articulate that into a controlling idea —the main idea upon which you build your thesis.
Remember that a thesis is not the topic itself, but rather your interpretation of the question or subject. For whatever topic your professor gives you, you must ask yourself, “What do I want to say about it?” Asking and then answering this question is vital to forming a thesis that is precise, forceful and confident.
A thesis is one sentence long and appears toward the end of your introduction. It is specific and focuses on one to three points of a single idea—points that are able to be demonstrated in the body. It forecasts the content of the essay and suggests how you will organize your information. Remember that a thesis statement does not summarize an issue but rather dissects it.
A Strong Thesis Statement
A strong thesis statement contains the following qualities.
Specificity. A thesis statement must concentrate on a specific area of a general topic. As you may recall, the creation of a thesis statement begins when you choose a broad subject and then narrow down its parts until you pinpoint a specific aspect of that topic. For example, health care is a broad topic, but a proper thesis statement would focus on a specific area of that topic, such as options for individuals without health care coverage.
Precision. A strong thesis statement must be precise enough to allow for a coherent argument and to remain focused on the topic. If the specific topic is options for individuals without health care coverage, then your precise thesis statement must make an exact claim about it, such as that limited options exist for those who are uninsured by their employers. You must further pinpoint what you are going to discuss regarding these limited effects, such as whom they affect and what the cause is.
Ability to be argued. A thesis statement must present a relevant and specific argument. A factual statement often is not considered arguable. Be sure your thesis statement contains a point of view that can be supported with evidence.
Ability to be demonstrated. For any claim you make in your thesis, you must be able to provide reasons and examples for your opinion. You can rely on personal observations in order to do this, or you can consult outside sources to demonstrate that what you assert is valid. A worthy argument is backed by examples and details.
Forcefulness. A thesis statement that is forceful shows readers that you are, in fact, making an argument. The tone is assertive and takes a stance that others might oppose.
Confidence. In addition to using force in your thesis statement, you must also use confidence in your claim. Phrases such as I feel or I believe actually weaken the readers’ sense of your confidence because these phrases imply that you are the only person who feels the way you do. In other words, your stance has insufficient backing. Taking an authoritative stance on the matter persuades your readers to have faith in your argument and open their minds to what you have to say.
Even in a personal essay that allows the use of first person, your thesis should not contain phrases such as in my opinion or I believe . These statements reduce your credibility and weaken your argument. Your opinion is more convincing when you use a firm attitude.
On a separate sheet of paper, write a thesis statement for each of the following topics. Remember to make each statement specific, precise, demonstrable, forceful and confident.
- Texting while driving
- The legal drinking age in the United States
- Steroid use among professional athletes
Examples of Appropriate Thesis Statements
Each of the following thesis statements meets several of the following requirements:
- Specificity
- Ability to be argued
- Ability to be demonstrated
- Forcefulness
- The societal and personal struggles of Troy Maxon in the play Fences symbolize the challenge of black males who lived through segregation and integration in the United States.
- Closing all American borders for a period of five years is one solution that will tackle illegal immigration.
- Shakespeare’s use of dramatic irony in Romeo and Juliet spoils the outcome for the audience and weakens the plot.
- J. D. Salinger’s character in Catcher in the Rye , Holden Caulfield, is a confused rebel who voices his disgust with phonies, yet in an effort to protect himself, he acts like a phony on many occasions.
- Compared to an absolute divorce, no-fault divorce is less expensive, promotes fairer settlements, and reflects a more realistic view of the causes for marital breakdown.
- Exposing children from an early age to the dangers of drug abuse is a sure method of preventing future drug addicts.
- In today’s crumbling job market, a high school diploma is not significant enough education to land a stable, lucrative job.
You can find thesis statements in many places, such as in the news; in the opinions of friends, coworkers or teachers; and even in songs you hear on the radio. Become aware of thesis statements in everyday life by paying attention to people’s opinions and their reasons for those opinions. Pay attention to your own everyday thesis statements as well, as these can become material for future essays.
Now that you have read about the contents of a good thesis statement and have seen examples, take a look at the pitfalls to avoid when composing your own thesis:
A thesis is weak when it is simply a declaration of your subject or a description of what you will discuss in your essay.
Weak thesis statement: My paper will explain why imagination is more important than knowledge.
A thesis is weak when it makes an unreasonable or outrageous claim or insults the opposing side.
Weak thesis statement: Religious radicals across America are trying to legislate their Puritanical beliefs by banning required high school books.
A thesis is weak when it contains an obvious fact or something that no one can disagree with or provides a dead end.
Weak thesis statement: Advertising companies use sex to sell their products.
A thesis is weak when the statement is too broad.
Weak thesis statement: The life of Abraham Lincoln was long and challenging.
Read the following thesis statements. On a separate piece of paper, identify each as weak or strong. For those that are weak, list the reasons why. Then revise the weak statements so that they conform to the requirements of a strong thesis.
- The subject of this paper is my experience with ferrets as pets.
- The government must expand its funding for research on renewable energy resources in order to prepare for the impending end of oil.
- Edgar Allan Poe was a poet who lived in Baltimore during the nineteenth century.
- In this essay, I will give you lots of reasons why slot machines should not be legalized in Baltimore.
- Despite his promises during his campaign, President Kennedy took few executive measures to support civil rights legislation.
- Because many children’s toys have potential safety hazards that could lead to injury, it is clear that not all children’s toys are safe.
- My experience with young children has taught me that I want to be a disciplinary parent because I believe that a child without discipline can be a parent’s worst nightmare.
Writing at Work
Often in your career, you will need to ask your boss for something through an e-mail. Just as a thesis statement organizes an essay, it can also organize your e-mail request. While your e-mail will be shorter than an essay, using a thesis statement in your first paragraph quickly lets your boss know what you are asking for, why it is necessary, and what the benefits are. In short body paragraphs, you can provide the essential information needed to expand upon your request.
Thesis Statement Revision
Your thesis will probably change as you write, so you will need to modify it to reflect exactly what you have discussed in your essay. Remember from Chapter 8 “The Writing Process: How Do I Begin?” that your thesis statement begins as a working thesis statement , an indefinite statement that you make about your topic early in the writing process for the purpose of planning and guiding your writing.
Working thesis statements often become stronger as you gather information and form new opinions and reasons for those opinions. Revision helps you strengthen your thesis so that it matches what you have expressed in the body of the paper.
The best way to revise your thesis statement is to ask questions about it and then examine the answers to those questions. By challenging your own ideas and forming definite reasons for those ideas, you grow closer to a more precise point of view, which you can then incorporate into your thesis statement.
Ways to Revise Your Thesis
You can cut down on irrelevant aspects and revise your thesis by taking the following steps:
1. Pinpoint and replace all nonspecific words, such as people , everything , society , or life , with more precise words in order to reduce any vagueness.
Working thesis: Young people have to work hard to succeed in life.
Revised thesis: Recent college graduates must have discipline and persistence in order to find and maintain a stable job in which they can use and be appreciated for their talents.
The revised thesis makes a more specific statement about success and what it means to work hard. The original includes too broad a range of people and does not define exactly what success entails. By replacing those general words like people and work hard , the writer can better focus his or her research and gain more direction in his or her writing.
2. Clarify ideas that need explanation by asking yourself questions that narrow your thesis.
Working thesis: The welfare system is a joke.
Revised thesis: The welfare system keeps a socioeconomic class from gaining employment by alluring members of that class with unearned income, instead of programs to improve their education and skill sets.
A joke means many things to many people. Readers bring all sorts of backgrounds and perspectives to the reading process and would need clarification for a word so vague. This expression may also be too informal for the selected audience. By asking questions, the writer can devise a more precise and appropriate explanation for joke . The writer should ask himself or herself questions similar to the 5WH questions. (See Chapter 8 “The Writing Process: How Do I Begin?” for more information on the 5WH questions.) By incorporating the answers to these questions into a thesis statement, the writer more accurately defines his or her stance, which will better guide the writing of the essay.
3. Replace any linking verbs with action verbs. Linking verbs are forms of the verb to be , a verb that simply states that a situation exists.
Working thesis: Kansas City schoolteachers are not paid enough.
Revised thesis: The Kansas City legislature cannot afford to pay its educators, resulting in job cuts and resignations in a district that sorely needs highly qualified and dedicated teachers.
The linking verb in this working thesis statement is the word are . Linking verbs often make thesis statements weak because they do not express action. Rather, they connect words and phrases to the second half of the sentence. Readers might wonder, “Why are they not paid enough?” But this statement does not compel them to ask many more questions. The writer should ask himself or herself questions in order to replace the linking verb with an action verb, thus forming a stronger thesis statement, one that takes a more definitive stance on the issue:
- Who is not paying the teachers enough?
- What is considered “enough”?
- What is the problem?
- What are the results
4. Omit any general claims that are hard to support.
Working thesis: Today’s teenage girls are too sexualized.
Revised thesis: Teenage girls who are captivated by the sexual images on MTV are conditioned to believe that a woman’s worth depends on her sensuality, a feeling that harms their self-esteem and behavior.
It is true that some young women in today’s society are more sexualized than in the past, but that is not true for all girls. Many girls have strict parents, dress appropriately, and do not engage in sexual activity while in middle school and high school. The writer of this thesis should ask the following questions:
- Which teenage girls?
- What constitutes “too” sexualized?
- Why are they behaving that way?
- Where does this behavior show up?
- What are the repercussions?
In the first section of Chapter 8 “The Writing Process: How Do I Begin?” , you determined your purpose for writing and your audience. You then completed a freewriting exercise about an event you recently experienced and chose a general topic to write about. Using that general topic, you then narrowed it down by answering the 5WH questions. After you answered these questions, you chose one of the three methods of prewriting and gathered possible supporting points for your working thesis statement.
Now, on a separate sheet of paper, write down your working thesis statement. Identify any weaknesses in this sentence and revise the statement to reflect the elements of a strong thesis statement. Make sure it is specific, precise, arguable, demonstrable, forceful, and confident.
Collaboration
Please share with a classmate and compare your answers.
In your career you may have to write a project proposal that focuses on a particular problem in your company, such as reinforcing the tardiness policy. The proposal would aim to fix the problem; using a thesis statement would clearly state the boundaries of the problem and tell the goals of the project. After writing the proposal, you may find that the thesis needs revision to reflect exactly what is expressed in the body. Using the techniques from this chapter would apply to revising that thesis.
Key Takeaways
- Proper essays require a thesis statement to provide a specific focus and suggest how the essay will be organized.
- A thesis statement is your interpretation of the subject, not the topic itself.
- A strong thesis is specific, precise, forceful, confident, and is able to be demonstrated.
- A strong thesis challenges readers with a point of view that can be debated and can be supported with evidence.
- A weak thesis is simply a declaration of your topic or contains an obvious fact that cannot be argued.
- Depending on your topic, it may or may not be appropriate to use first person point of view.
- Revise your thesis by ensuring all words are specific, all ideas are exact, and all verbs express action.
Writing for Success Copyright © 2015 by University of Minnesota is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License , except where otherwise noted.
- Research article
- Open access
- Published: 15 February 2021
Body size perception, knowledge about obesity and factors associated with lifestyle change among patients, health care professionals and public health experts
- Virginija Zelenytė ORCID: orcid.org/0000-0001-9644-7816 1 ,
- Leonas Valius 2 ,
- Auksė Domeikienė 1 , 2 ,
- Rita Gudaitytė 3 ,
- Žilvinas Endzinas 3 ,
- Linas Šumskas 1 , 4 &
- Almantas Maleckas 3 , 5
BMC Family Practice volume 22 , Article number: 37 ( 2021 ) Cite this article
5948 Accesses
6 Citations
Metrics details
The attitudes towards obesity may have an important role on healthier behavior. The goal of the present study was to explore the attitudes towards obesity and to investigate how these attitudes were associated with lifestyle-changing behavior among the patients attending primary care centers, health care professionals and public health experts.
This cross-sectional survey study was performed in 10 primary care offices in different regions in Lithuania and in 2 public health institutions. Nine hundred thirty-four patients, 97 nurses, 65 physicians and 30 public health experts have filled the questionnaire about attitudes towards obesity and presented data about lifestyle-changing activities during last 12 months. The attitudes were compared between different respondent groups and factors associated with healthier behaviors were analyzed among overweight/obese individuals in our study population.
Participants failed to visually recognize correct figure corresponding to male and female with obesity. Majority of respondents’ perceived obesity as a risk factor for heart diseases and diabetes but had less knowledge about other diseases associated with weight. About one third of respondents changed their lifestyle during last 12 months. Overweight individuals with age < 45 years (OR 1.64, 1.06–2.55; p = 0.025) were more likely and those who overestimated current weight (OR 0.44, 0.20–0.96; p = 0.036) less likely to change their lifestyle. Disappointment with their current weight (OR 2.57, 1.36–4.84; p = 0.003) was associated with healthier behavior among participants with obesity.
Participants had similar body size perception and knowledge about obesity. Younger age had significant association with lifestyle changing behavior among overweight individuals and disappointment with current weight among obese participants.
Peer Review reports
The prevalence of obesity is increasing worldwide and has nearly tripled since 1975 [ 1 ]. Obesity is the well-known risk factor for many diseases including type 2 diabetes mellitus (T2DM), hypertension, atherosclerotic diseases and some types of cancer. It has detrimental effect on life expectancy and is associated with increased medical costs, which has a direct negative impact on public health systems [ 2 , 3 ]. Despite all this, it is a condition with substantial unmet medical needs due to lack of agreement among various guidelines, shortfalls in obesity-related clinical training and complexities in reimbursement of services [ 4 ].
Representative quality of care survey in US-ambulatory care settings revealed that nearly 50% of Patients Record Forms lacked complete weight and height data and obesity diagnosis was not reported in 70% of patients with BMI ≥30.0 [ 5 ]. The frequency of counselling for diet, exercise or weight reduction increased from 37% among patients with BMI ≥30.0 to 55% among those with reported obesity diagnosis [ 5 ]. However, underreported diagnosis or counselling activities in survey studies may not reflect real situation about obesity care. Patient-doctor relationship is core in such care and is rather complex. Evaluation of it should include also process measures such as shared decision making on when the patient is ready to tackle obesity based on patient’s weight loss history and/or patient’s presence in particular stage of change. In weight control as well as in some other problem behaviors before acting patients go through precontemplation and contemplation stages [ 6 ]. It was shown that increase in pros drives patients from precontemplation to contemplation stage and decrease in cons – from contemplation stage to action [ 6 ]. In order to increase pros of changing behaviour among patients with obesity the GPs should address patients’ perception of obesity as a major health issue [ 7 ] and estimate real weight status as there is an observed tendency towards visual biases in judging the body weight [ 8 ]. However, the major concern is the fact, that primary care physicians spent a great portion of the visit time on technical tasks and more time on discussing exercise than educating patients with obesity about their health [ 9 ].
In this context communication between the patient and the doctor is crucial. Health professionals such as primary care doctors and nurses may give adequate information to the patient taking into account patient’s stage of change. However, the nurses and doctors themselves may fail to recognize obesity because they compare their patient body dimensions to newly accepted reference size, which is culturally appropriate and became common standard in the community [ 10 ]. Furthermore, on the national scale similar problems may be encountered among public health experts (PHE) and may have an effect on the future strategies about obesity prevention and treatment.
The goal of the present study was to explore the attitudes towards obesity among the patients attending primary care centers, as well as to get better insight into attitudes of health care professionals and PHE. Also, we investigated how these perceptions, attitudes were associated with lifestyle-changing behavior among individuals with overweight and obesity in our study population.
This study was performed as a cross-sectional survey on attitudes towards obesity and related health risks with comparison between patients, nurses, physicians and PHE.
At the moment of the study initiation the Department of Family Medicine, Lithuanian University of Health Sciences had teaching centers in 15 primary care offices and 11 centers were randomly selected to participate in this survey. Finally, the data were collected from 10 primary care centers in different regions in Lithuania (Kaunas 3, Šiauliai 1, Panevėžys 1, Kaišiadorys 1, Kėdainiai 1, Biržai 1, Skuodas 1, Pagėgiai 1). The patients were eligible, if they were 18 years or older, attended primary care office for chronic or acute condition. The healthcare professionals were eligible if they were in practice for more than 2 years and were involved in the patient care. Researchers and professionals who monitor and diagnose the health concerns as well as promote healthy practices and behaviors on the population level were defined as PHE and were recruited from public health related departments of Lithuanian University of Health Sciences as well as from Lithuanian Hygiene Institute in Vilnius. Interviewing survey took place between November 2018 and November 2019. All respondents provided informed consent before participating in the survey. Bioethical approval (No. BE-2-76, 2018.10.08) was obtained from Kaunas Regional Bioethical Committee.
Questionnaire
In this study we followed the methodology which was developed and previously used by Public Health England experts. This questionnaire was applied to measure public attitudes to obesity in UK [ 11 ]. The official permission was obtained from Public Health England to use the questionnaire for survey in Lithuania. The translation of questionnaire into Lithuanian language was performed by two translators. One was aware of the concepts the questionnaire intends to measure and the other was naive translator. Inconsistencies between the translations were discussed and resolved, and questionnaire was back translated by 2 independent translators. After backward translation the same process with review of disparities of translations was performed and final version of translated questionnaire was produced and piloted.
The questionnaire survey form covered 40 questions on perceptions and understanding of obesity, responsibility and possible solutions, as well as social stigma issues. All participants also were asked to report their weight and height. The main reason for choosing self-reported data was the fact that we were unable to provide uniform measurements in the different settings and between different participants’ groups. The BMI was calculated by dividing weight by height in square meters. In the current article we have provided research analysis only for some questionnaire items: a) perceptions of others weight; b) perception of own body weight; c) satisfaction on the own body weight; and d) understanding of causes and health risks associated with obesity.
In order to evaluate ability to recognize obesity in others’ the participants were given two sets of pictures with 8 figures presented in order of increasing body mass index (BMI). One set of male figures and the other of females. The participants were asked at what point the picture shows a male/female figure, which is called obese. In both cases correct answer was a figure with BMI just over 32. The participants were also given the same pictures of females and males (as appropriate) and were asked, which figure best represents their own body size. The answers about individual’s body size were compared with self-reported BMI.
Further, the respondents were asked what they think about their own current weight: is he/she very underweight, underweight, about the right weight, a bit overweight or very overweight. When analyzing own-weight perceptions we compared it with actual self-reported BMI and separately presented results for normal weight, overweight and participants with obesity. The other question was asked on satisfaction by the own body weight. It was asked how happy the respondents are with their current weight: very happy, happy, neutral, unhappy or very happy. The answers were grouped according to BMI of respondents – normal weight, overweight and obesity.
The list of ten possible diseases (heart disease, high blood pressure, diabetes, stroke, arthritis, depression, some cancers, liver disease, asthma and zoster) was presented and the respondents were asked, which conditions individuals with obesity are more likely to get. The question about zoster was included to show for the respondents that not all presented diseases are associated with obesity. The knowledge about causes of obesity was explored asking, if respondents strongly agree, agree, neither agree nor disagree, disagree or strongly disagree with the statements, that people become obese because they eat too much, exercise too little, have low metabolism or inherit it.
Finally, the respondents in all groups were asked, if during last 12 months they have changed their lifestyle behavior. In case, if individuals have changed their lifestyle they were asked, if those changes were associated with healthier diet, increased physical activity or both.
Statistical analysis
We intended to include 1200 patients, 100 nurses, 70 GPs and 30 public health experts based on statistical power, cost and feasibility of recruitment. Statistical analysis was performed using SPSS (IBM, version 25.0). Only data from those who completed the survey were included in the analyses. Data were presented as means (standard deviations), medians, and frequencies, and compared by chi square, ANOVA tests among respondent groups, when appropriate. P < 0.01, using 2-tailed tests was considered statistically significant. Forward conditional binary logistic regression analysis was performed to identify independent factors associated with lifestyle changes during last 12 month. Factors were included into multivariate regression analysis, if during univariate analysis p value was < 0.05.
In total, 1199 patients, 105 nurses, 79 GPs and 30 PHE were invited as eligible to participate in the study. Finally, 934 patients (77.9% of all invited), 97 nurses (92.4%), 65 general practitioners (82.3%) and 30 (100%) PHE filled in questionnaires (Fig. 1 ). Characteristics of patients, nurses, physicians and PHE are presented in Table 1 . Patients and PHE were significantly younger (41.9 and 39.9 years, respectively) in comparison with GPs and nurses (47.1 and 47.1, respectively). Fewer male participants were involved among all groups of respondents. On average, respondents had BMI 26.4 (5.8). BMI was highest in the group of patients 26.5 (6.0) and lowest – in the group of public health professionals 24.4 (4.7). There was no significant difference for average self-reported BMI and self-reported BMI category. Sixty percent of the patients had higher education. Significantly higher monthly incomes were observed in GPs and PHE groups.
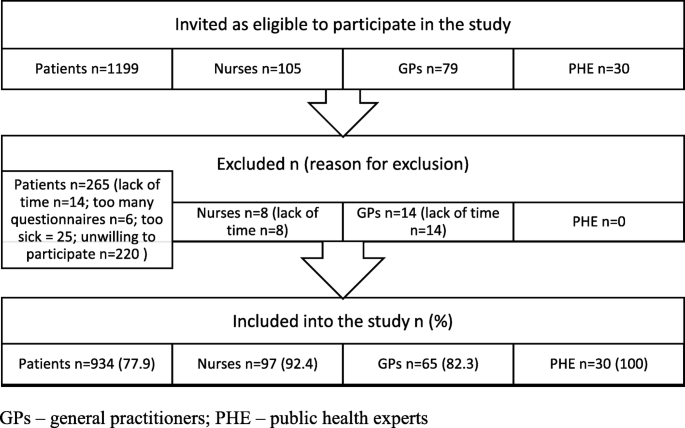
Study flow diagram
Perceptions of others weight
Only 8.1 and 12.3% of all respondents correctly identified the exact male and female figure, respectively, which was the first on the picture to present individual with obesity (Table 2 ). The nurses (17.5%) and doctors (15.4%) were more precise than patients (6.9%) and PHE (0%) to recognize the figure of male with obesity. The correct response rate for the figure of the female with obesity was similar between the groups. The figure with BMI around 42 was median response in all participants groups for males and in patients’ and nurses’ groups for females. Only GPs and PHE were slightly more precise in defining obesity in females with BMI around 36 as median response (Table 2 ).
Perceptions of own weight
Most of the participants (69.9%) with BMI 25.0–29.9 correctly identified that they were overweight (Table 3 ). Overweight nurses and doctors were better to perceive their weight category as compared to patients and PHE of whom 21.2 and 27.3%, respectively, underestimated their weight. Nearly similar percentage (63.5%) of participants with obesity responded that they are very overweight, the rest stated that they have overweight (Table 3 ). There was no significant difference between the study groups. Males tend to have a higher rate of weight misperception as compared to females (Fig. 2 ). Only male doctors had similar weight misperception rate as female doctors. Among overweight respondents, significantly more have overestimated their figure BMI than underestimated, without larger difference between study groups. Majority of respondents with obesity in all groups have chosen correct figures (Table 4 ).
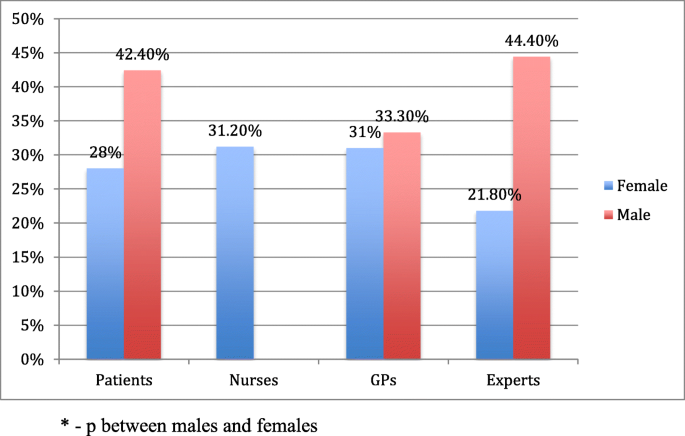
The rate of their own body weight misperception by gender and different groups of respondents
Satisfaction with the own body weight
The feelings about current weight were significantly different between those who had normal BMI as compared to individuals with overweight/obesity. Participants with normal BMI were mostly happy while those who had overweight/obesity were mostly unhappy with their weight (Fig. 3 ). Among respondents with overweight/obesity doctors had the highest mean scores (3.80/4.31) showing that this group was more disappointed with their weight than other participant groups. The mean scores for patients, nurses and PHE with overweight/obesity were 3.33/3.94, 3.52/3.68 and 3.18/3.67, respectively.

Satisfaction about current own body weight among respondents by BMI category in different groups of respondents
Understanding of causes and health risks associated with obesity
Majority of respondents were aware that obesity is associated with increased risk of 5 health outcomes - heart diseases, high blood pressure and stroke, as well as T2DM and arthritis (Figs. 4 and 5 ). GPs showed the highest awareness of mentioned health conditions related to obesity (rate of correct answers 91, 91, 74, 99 and 72%, respectively). Patients also presented quite high percentage of correct answers – 83, 74, 55, 75 and 59%, respectively.
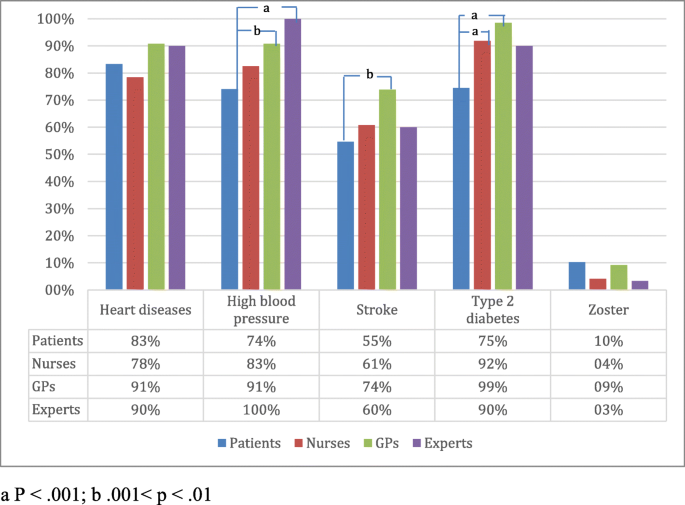
Awareness of respondents how chronic diseases are associated with obesity: percentage of respondents who reported the listed diseases
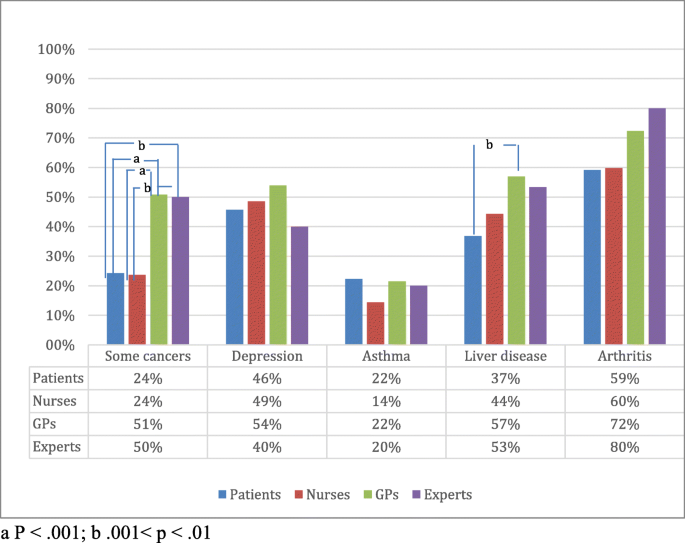
Other diseases associated with obesity (% say more likely to get, if obese)
The respondents in all groups were less aware of other risk factors associated with obesity (Fig. 5 ). Less than half of respondents thought that obesity is a risk factor for depression. Half of PHE and GPs answered that obesity is associated with the increased risk of some cancers, while only quarter of patients and nurses identified this relationship. Was included to show for the respondents that not all presented diseases are associated with obesity. Majority in all groups have correctly answered the reference question that zoster is not associated with obesity.
Most of the respondents in all groups agreed that eating too much and exercising too little causes obesity (Fig. 6 ). Nearly half of patients (48.6%) and nurses (51.6%) agreed that low metabolism is a cause of obesity. However, significantly less PHE (6.7%) and GPs (24.6%) agreed with such statement.
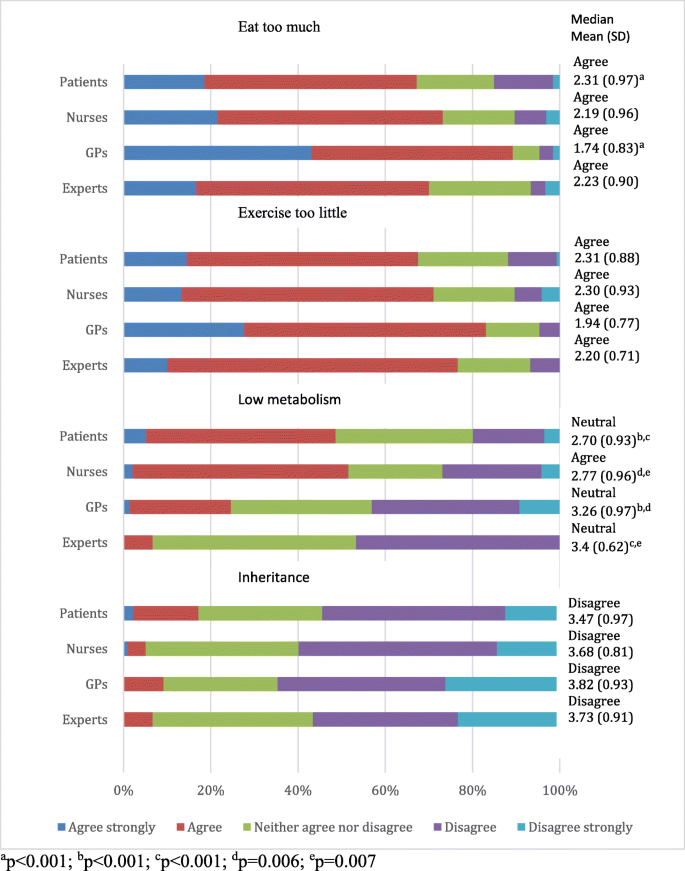
Beliefs about the causes of obesity by respondent groups
Factors associated with lifestyle changes
About one third of respondents in all groups reported the changes in their lifestyle during last 12 months (Table 1 ). Majority of them started more healthier diet and increased physical activity.
Univariate and multivariate analysis have demonstrated that overweight individuals were more likely to change their lifestyle, if they were younger than 45 years (OR 1.64, 1.06–2.55; p = 0.025) and less likely, if they overestimated their current weight (OR 0.44, 0.20–0.96; p = 0.036) (Table 5 ). Individuals with obesity were engaged in lifestyle changing activities, if they were females (OR 1.77, 1.01–3.10; p = 0.047), had higher education (1.81, 1.05–3.10; p = 0.031) and were unhappy with their current weight (2.57, 1.36–4.84; p = 0.003). Individuals with obesity were less likely to make changes in their lifestyle, if they underestimated their current weight (0.49, 0.28–0.84; p = 0.010). Only unhappiness with the current weight was found to be statistically significant independent factor. Realistic perception of others and own body size, knowledge about diseases related to weight and causes of obesity as well as respondents’ group and incomes had no significant association with healthier behavior among individuals with overweight/obesity (Table 5 ).
Discussion and conclusion
Our study showed that significant visual body size misperception exists in all respondent groups in estimating others weight, however, they were reasonably accurate in estimating their own body weight. Majority of respondents share similar attitudes about the causes of obesity, knows major cardiovascular diseases associated with obesity, however, the knowledge about other risks of obesity is inadequate. Age, realistic weight perception and feelings about own weight are associated with lifestyle changing behavior.
The first step in treating obesity is to diagnose it and clearly communicate diagnosis to the patient. Our study reveals that healthcare professionals and PHE have similar level of visual body size misperception as the patients. People tend to recognize visually only extreme, high-risk class III obesity and neglect early stages. One possible explanation could be that in general there is a greater acceptance of heavier body weights in the population [ 12 ]. Beside this, people make choices for food consumption based on how individual weight compares to social norms [ 13 ]. In the questionnaire that was used in the current study there was the question how people feel about their weight. None of the overweight nurses and only 8% doctors with overweight replied that they are “about the right weight”. In contrast, about one fifth of the overweight patients and one fourth of overweight PHE have chosen this answer. Similar results were established in the National Health and Nutrition Examination Survey (NHANES) in the United States. Twenty four percent of overweight individuals from US civilian population thought that their weight was about the right [ 14 ].
Only 2.5% of patients with obesity in our study replied that their weight is about the right, while nobody among healthcare providers or PHE have chosen this definition for their current weight. By contrast, 3% of women and 12% of males with obesity in US population thinks that they have about the right weight [ 15 ]. Participants with obesity in our study were less likely to be engaged in lifestyle change, if they underestimated their weight category. Underestimation of weight category maybe caused due to the lack of information about personal weight and obesity definition, or because of the belief that their weight is normal. However, the information about real weight status provided by physicians increases likelihood that the patients with overweight/obesity will attempt to lose weight [ 16 ].
Individual’s body size perception was evaluated asking which figure represents their body shape best. More than half of the overweight individuals overestimated their body size. Such findings correlate well with the data from the other studies [ 17 , 18 ]. Overestimation of body size may have a negative influence on self-esteem and rise psychological, social and dietary issues [ 19 ]. It must be noted that female patients perceive their body size more realistically than males. Male patients think that they are thinner than they are, and this is more evident with increasing body size or weight status [ 20 ]. The other aspect is feelings about individual body size. Several studies have pointed on direct relation between increasing BMI and dissatisfaction with the body size [ 21 , 22 ]. Moreover, these studies also revealed that dissatisfaction with body size is an important motivator for engaging in weight loss activities. However, feelings about height or specific body areas may also be included in the concept of satisfaction with body size [ 23 ]. In our study we narrowed the idea of body size and asked participants only how they feel about their current weight. Individuals with obesity were mostly unhappy with their weight and only 5% of patients and nurses responded that they are happy with their current weight. Results similar to those from current international study by Caterson ID et al. [ 24 ] where only 6% of patients with obesity were happy with their weight. Respondents with obesity, but not overweight, were more likely to change their lifestyle if they were dissatisfied with their current weight.
Several theories and conceptual models are used to understand health behavioral change [ 25 ]. In most of them motivation to change is based on attitudes, possible benefits, perceived threat or risk of a specific condition, or desire to achieve positive outcomes. Motivation alone without intentions is not enough to change lifestyle. GPs may form appropriate intentions however, it is important to consider how much intended behaviour is driven by attitudinal or normative considerations, or by feelings of perceived behavioral control [ 26 ]. Moreover, patients are more likely to be engaged in a particular behavior, if it is presented as an action with a target, performed within a given context and at a certain point in time [ 26 ]. If the patients already intend to act, it is unlikely that they need more information. However, if the patients are going to be engaged in the class of behaviors such as lifestyle change, they may need stronger motivation, proper context and much longer time. Awareness of the risks associated with obesity may motivate people to change lifestyle. The results of our study as well as the data from the literature reveal that individuals and health care providers recognizes heart disease, high blood pressure and T2DM as adverse health consequences of obesity [ 27 , 28 , 29 ]. However, nearly half of the PHE and GPs failed to recognize association of obesity with some types of cancer and depression, and even more with asthma. The knowledge of the nurses about obesity as a risk factor was similar to that of the patients. French study has found that GPs who subscribed medical journals or have taken CME courses about the management of weight problems felt more effective in treating individuals with obesity [ 29 ]. Failure to recognize diseases associated with obesity may be a barrier for weight loss counseling especially in overweight patients. Also, misperception of risks associated with obesity may prevent strong action on the society level.
In this study respondent beliefs about biological and lifestyle factors as a cause of obesity was investigated. All respondent groups agreed that exercising too little and eating too much causes obesity. Moreover, all groups disagreed that inheritance is a cause of obesity. Similar results were found in Caterson ID et al. study [ 24 ] where patients and healthcare providers emphasized life-style related factors, but not a genetic predisposition as a barrier to weight loss. By contrast, it is now widely recognized that obesity has a genetic predisposition and obesogenic environment increases genetic risk for obesity [ 30 ]. In general, influence of genes has to be discussed with the patient as this may diminish self-blame and the patients have to be informed that genetic risk for obesity maybe reduced by increasing physical activity and avoiding some specific dietary components [ 24 , 30 ].
One third of individuals with overweight and half of those with obesity have changed their lifestyle during last 12 month in our study population and there was no difference between patients, healthcare providers and PHE. In comparison, 61% of US adults with obesity over the last 12 months tried to lose weight [ 31 ]. Among overweight individuals those who were younger than 45 years were more likely to change their lifestyle. Individuals with obesity were more prone to adopt healthier lifestyle if they had higher education, were females and were unhappy with their weight. Beside higher education and female gender, increasing BMI, insurance coverage, comorbidities such as diabetes or arthritis and Hispanic race were associated with more weight loss activities among US adults with obesity [ 31 ]. Overestimation of weight among individuals with overweight and underestimation among those with obesity precluded lifestyle changes in our study population. These data are similar to Duncan DT et al. [ 32 ] findings that weight misperception was a strong predictor of weight loss activities for both genders and all racial/ethnic groups among US adults with overweight and obesity.
This study explored attitudes about obesity in different social groups. Healthcare providers as well as PHE in general have similar attitudes to those of general population. It seems that attitudes and beliefs rooted in society is hard to change even with specialized education. More focused teaching should be aimed at paradigm shift. The people fail to recognize obesity in the others in an early stage, when weight control can be more efficient. People themselves tend to be realistic about their weight. The data from this study and the literature show, that individuals with overweight and obesity are more motivated to lose weight, if they have realistic perception of their weight. But they need support. Recent international multicenter study found that it took a median of 3 years and a mean of 6 years between the time when individuals started struggling with excess weight or obesity and when they had a first weight management conversation with a healthcare provider. Moreover, 46% of individuals have initiated discussion themselves [ 24 ]. BMI estimation and assessment of individuals’ health profile maybe an effective way to start such conversations [ 33 ]. Timely interventions may prevent potential complications of obesity. Furthermore, education may help for individuals to understand less apparent relationship between obesity and health. The lack of information is likely to compromise patients’ abilities to make informed choices about their health. Swift JA et al. [ 34 ] observed that intended weight loss was positively associated with health beliefs. However, in our study knowledge about obesity as a risk factor for cardiovascular and non-cardiovascular diseases had no impact on healthier behavior.
Our study has some limitations. First, the majority of the patient respondents questioned were women. This could be due to the fact that in overall, percentage of women in the population is higher (especially in age over 60), also women are covered by larger number of prevention programs and attend GPs office more frequently. In addition, they do accept invitation to participate in the survey more positively in comparison with men. Second, the primary care centers that participated in our survey are teaching centers and are affiliated with Lithuanian University of Health Sciences. In all centers family medicine residents have their practice. Thus, GPs and nurses who participate in the teaching activities may have more knowledge than healthcare providers from other primary care offices. Third, we used self-reported weight and height to estimate BMI of the patients, and this approach is subject to the bias [ 35 ]. However, the percentage of individuals with overweight and obesity among the respondents was similar to the data from population studies performed in Lithuania [ 36 ]. Fourth, we did not ask participants, if adoption of healthier lifestyle was motivated by necessity to lose weight. By presenting a broader question we intended to cover also individuals whose primary goal was to increase physical activity and/or adopt healthier diet not only for weight loss purposes. Finally, from cross-sectional survey data we were unable to establish causal association between body weight satisfaction and healthier lifestyle. It is unclear whether dissatisfaction with weight motivates to change lifestyle or change in lifestyle alters perception of weight and results in the feelings of dissatisfaction.
Participants from different groups have similar body size perception and knowledge about obesity. Younger age and overestimated current weight are associated with healthier behavior among overweight individuals and disappointment with current weight among participants with obesity. Diagnosing obesity only by visual means is inaccurate. BMI estimation during the visit to primary care office is simple and important tool that facilitates diagnosis of obesity. Combining information from perceived body image with weight status and feelings about current weight may give more insight into individual’s views and motivation to adopt healthier lifestyle behavior. Serious knowledge gaps exist among healthcare providers about the impact of obesity on non-cardiovascular diseases. In the age when the amount of information in medicine grows exponentially, continuous education of healthcare providers is vital.
Availability of data and materials
Data could be provided by the request to authors of manuscript.
Abbreviations
Body mass index
National Health and Nutrition Examination Survey
United States
Type 2 diabetes mellitus
- Public health experts
- General practitioners
Continuing medical education
WHO. Obesity and overweight; 2019. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight , (Accessed 21 Mar 2020)
Google Scholar
Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. JAMA. 2003;289:187–93.
Article Google Scholar
Finkelstein EA, Fiebelkorn IC, Wang G. National medical spending attributable to overweight and obesity: how much, and who's paying? Health Aff. 2003; Suppl1: Web Exclusives, W3-219-26.
Ritten A, LaManna J. Unmet needs in obesity management: from guidelines to clinic. J Am Assoc Nurse Pract. 2017;29:S30–42.
Ma J, Xiao L, Stafford RS. Adult obesity and office-based quality of care in the United States. Obesity (Silver Spring). 2009;17:1077–85.
Bleich SN, Pickett-Blakely O, Cooper LA. Physician practice patterns of obesity diagnosis and weight-related counseling. Patient Educ Couns. 2011;82:123–9.
Bertakis KD, Azari R. The impact of obesity on primary care visits. Obes Res. 2005;13:1615–23.
Volpp KG, Mohta NS. Patient engagement survey: the failure of obesity efforts and the collective nature of solutions. NEJM Catal. 2018; https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0092 .
Johnson F, Cooke L, Croker H, Wardle J. Changing perceptions of weight in Great Britain: comparison of two population surveys. BMJ. 2008;337:a494.
Article CAS Google Scholar
Oldham M, Robinson E. Visual weight status misperceptions of men: why overweight can look like a healthy weight. J Health Psychol. 2016;21:1768–77.
Curtice J. Attitudes to obesity: findings from the 2015 British social attitudes survey. Nat Cen Soc Res. 2015.
Robinson E, Christiansen P. The changing face of obesity: exposure to and acceptance of obesity. Obesity (Silver Spring). 2014;22:1380–6.
Burke MA, Heiland F. Social dynamics of obesity. Econ Inq. 2007;45:571–91.
Han L, You D, Zeng F, Feng X, Astell-Burt T, Duan S, et al. Trends in self-perceived weight status, weight loss attempts, and weight loss strategies among adults in the United States, 1999-2016. JAMA Netw Open. 2019;2:e1915219.
Burke MA, Heiland FW, Nadler CM. From “overweight” to “about right”: evidence of a generational shift in body weight norms. Obesity (Silver Spring). 2010;18:1226–34.
Post RE, Mainous AG 3rd, Gregorie SH, Knoll ME, Diaz VA, Saxena SK. The influence of physician acknowledgment of patients’ weight status on patient perceptions of overweight and obesity in the United States. Arch Intern Med. 2011;171:316–21.
Paul T, Sciacca R, Bier M, Rodriguez J, Song S, Giardina E-G. Size misperception among overweight and obese families. J Gen Intern Med. 2015;30:43–50.
Lerner HM, Klapes B, Mummert A, Cha E. Eat Weight Disord. 2016;21:487–92.
Jauregui-Lobera I, Ezquerra-Cabrera M, Carbonero-Carreno R, Ruiz-Prieto I. Weight misperception, self-reported physical fitness, dieting and some psychological variables as risk factors for eating disorders. Nutrients. 2013;5:4486–502.
Pulvers KM, Kaur H, Nollen NL, Greiner KA, Befort CA, Hall S, et al. Comparison of body perceptions between obese primary care patients and physicians: implications for practice. Patient Educ Couns. 2008;73:73–81.
Anderson LA, Eyler AA, Galuska DA, Brown DR, Brownson RC. Relationship of satisfaction with body size and trying to lose weight in a national survey of overweight and obese women aged 40 and older, United States. Prev Med. 2002;35:390–6.
Millstein RA, Carlson SA, Fulton JE, Galuska DA, Zhang J, Blanck HM, et al. Relationships between body size satisfaction and weight control practices among US adults. Medscape J Med. 2008;10:119.
PubMed PubMed Central Google Scholar
Grogan S. Body image and health: contemporary perspectives. J Health Psychol. 2006;11:523–30.
Caterson ID, Alfadda AA, Auerbach P, Coutinho W, Cuevas A, Dicker D, et al. Gaps to bridge: misalignment between perception, reality and actions in obesity. Diabetes Obes Metab. 2019;21:1914–24.
Baranowski T, Cullen KW, Nicklas T, Thompson D, Baranowski J. Are current health behavioral change models helpful in guiding prevention of weight gain efforts? Obes Res. 2003;11:23S–43S.
Fishbein M. A reasoned action approach to health promotion. Med Decis Mak. 2008;28:834–44.
Lake Snell Perry & Associates. Obesity as a public health issue: a look at solutions: results from a national poll; 2003.
Soriano R, Ponce de León Rosales S, García R, García-García E, Méndez JP. High knowledge about obesity and its health risks, with the exception of cancer, among Mexican individuals. J Cancer Educ. 2012;27:306–11.
Bocquier A, Verger P, Basdevant A, Andreotti G, Baretge J, Villani P, et al. Overweight and obesity: knowledge, attitudes, and practices of general practitioners in France. Obes Res. 2005;13:787–95.
Goodarzi MO. Genetics of obesity: what genetic association studies have taught us about the biology of obesity and its complications. Lancet Diabetes Endocrinol. 2018;6:223–36.
Stokes A, Collins JM, Grant BF, Hsiao CW, Johnston SS, Ammann EM, et al. Prevalence and determinants of engagement with obesity care in the United States. Obesity (Silver Spring). 2018;26:814–8.
Duncan DT, Wolin KY, Scharoun-Lee M, Ding EL, Warner ET, Bennett GG. Does perception equal reality? Weight misperception in relation to weight-related attitudes and behaviors among overweight and obese US adults. Int J Behav Nutr Phys Act. 2011;8:20.
Speer SA, McPhillips R. Initiating discussions about weight in a non-weight-specific setting: what can we learn about the interactional consequences of different communication practices from an examination of clinical consultations? Br J Health Psychol. 2018;23:888–907.
Swift JA, Glazebrook C, Anness A, Goddard R. Obesity-related knowledge and beliefs in obese adults attending a specialist weight-management service: implications for weight loss over 1 year. Patient Educ Couns. 2009;74:70–6.
Connor Gorber S, Tremblay M, Moher D. Gorber B. a comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obes Rev. 2007;8:307–26.
Grabauskas V, Klumbienė J, Petkevičienė J, Šakytė E, Kriaučionienė V, Veryga A. Health behaviour among Lithuanian adult population, 2014. Kaunas: Lithuanian University of Health Sciences; 2015.
Download references
Acknowledgements
The authors are grateful to the respondents who participated.
No funding source was available for this research.
Author information
Authors and affiliations.
Department of Preventive Medicine, Medical Academy, Lithuanian University of Health Sciences, A. Mickevičiaus st. 9, LT-44307, Kaunas, Lithuania
Virginija Zelenytė, Auksė Domeikienė & Linas Šumskas
Department of Family Medicine, Medical Academy, Lithuanian University of Health Sciences, A. Mickevičiaus st. 9, LT-44307, Kaunas, Lithuania
Leonas Valius & Auksė Domeikienė
Department of Surgery, Medical Academy, Lithuanian University of Health Sciences, A. Mickevičiaus st. 9, LT-44307, Kaunas, Lithuania
Rita Gudaitytė, Žilvinas Endzinas & Almantas Maleckas
Institute of Health Research, Medical Academy, Lithuanian University of Health Sciences, Kaunas, Lithuania
Linas Šumskas
Department of Gastrosurgical Research and Education, Sahlgrenska Academy, University of Gothenburg, Bla Straket 5, SE-41345, Gothenburg, Sweden
Almantas Maleckas
You can also search for this author in PubMed Google Scholar
Contributions
VZ - Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Writing - original draft. LV - Conceptualization; Methodology; Resources; Writing - review & editing. AD - Resources; Supervision; Writing - review & editing. RG - Data curation; Formal analysis; Investigation. ŽE - Conceptualization; Formal analysis; Supervision; Writing - review & editing. LŠ - Conceptualization; Data curation; Formal analysis; Methodology; Project administration; Resources; Supervision; Writing - review & editing. AM - Conceptualization; Data curation; Formal analysis; Methodology; Supervision; Roles/Writing - original draft. The authors read and approved the final manuscript.
Corresponding author
Correspondence to Virginija Zelenytė .
Ethics declarations
Ethics approval and consent to participate.
Bioethical approval (No. BE-2-76, 2018.10.08) was obtained from Kaunas Regional Bioethical Committee and all participants have signed an informed consent before inclusion into the study.
Consent for publication
“Not applicable”. All patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the story.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Zelenytė, V., Valius, L., Domeikienė, A. et al. Body size perception, knowledge about obesity and factors associated with lifestyle change among patients, health care professionals and public health experts. BMC Fam Pract 22 , 37 (2021). https://doi.org/10.1186/s12875-021-01383-2
Download citation
Received : 13 September 2020
Accepted : 04 February 2021
Published : 15 February 2021
DOI : https://doi.org/10.1186/s12875-021-01383-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Body size perception
BMC Primary Care
ISSN: 2731-4553
- General enquiries: [email protected]
Exploring patient beliefs and perceptions regarding obesity as a disease, obesity causation and treatment
Affiliations.
- 1 Diabetes Complications Research Centre, Conway Institute, School of Medicine and Medical Sciences, University College Dublin, Dublin, Ireland. [email protected].
- 2 MedFit Proactive Healthcare, Blackrock, Dublin, Ireland. [email protected].
- 3 MedFit Proactive Healthcare, Blackrock, Dublin, Ireland.
- 4 Department of Upper Gastrointestinal Surgery, Southmead Hospital, Bristol, UK.
- 5 Diabetes Complications Research Centre, Conway Institute, School of Medicine and Medical Sciences, University College Dublin, Dublin, Ireland.
- PMID: 32696243
- DOI: 10.1007/s11845-020-02319-y
Introduction: In patients with obesity (PwO) and heath care providers (HcPs), there appears to exist a discrepancy between recognition of obesity as a disease and the underlying biology of the disease. This is evident when considering PwO and HcPs appear to agree obesity is a disease but position lifestyle related factors as the main barriers to treatment with "eat less and move more" considered the best treatment approach. This does not align with current evidence regarding obesity treatments and the underlying pathophysiology. An understanding of PwO beliefs and perceptions may facilitate improved communication strategies with regard to the underlying pathophysiology of obesity as a disease. This has the potential to lead to improvements in both prevention and treatment strategies. Therefore, we evaluated PwO beliefs and perceptions of obesity as a disease, obesity causation and obesity treatment recorded during clinical evaluation.
Methods: As part of usual clinical practice we record 9 items to investigate beliefs and perceptions of obesity in PwO. We used a clinical audit to determine how frequently this information was formally recorded and to explore the association between beliefs and perceptions.
Results: The information was formally recorded in the patients' chart in 52 out of 108 patients (49%) who were part of an intensive lifestyle and medication program between 2018 and 2020. We found PwO tend to agree that obesity is a disease and that weight loss maintenance is dependent on willpower. A strong tendency towards agreement was present for the statement exercise is essential for weight loss. For the statement exercise is as effective as diet alone for weight loss, a tendency towards disagreement was present. Seventy-nine percent of PwO claimed to know the recommended guidelines for exercise with average response aligning with the America College of Sports Medicine recommendations. In exploring the relationship between responses, a number of significant associations were present which may facilitate future approaches to changing the narrative around obesity as a disease and isolating specific aspects of the message that need to be focused upon for the PwO.
Conclusion: PwO appear to have conflicting beliefs regarding obesity as a disease and the underlying biology. This has the potential to hinder attempts to treat the disease via lifestyle intervention and may also reduce likelihood to consider alternative treatment options. These beliefs and perceptions need to be explored further, along with those of HcPs, policy makers and the general public. Collectively this may facilitate changing the narrative around obesity as a disease and positively impact both the prevention and treatment of this disease.
Keywords: Management; Obesity; Patient beliefs; Treatment.
- Middle Aged
- Obesity / etiology*
- Obesity / pathology
- Obesity / therapy*
- Weight Loss / physiology*
- Young Adult

COMMENTS
Next goes the thesis of your paper. The thesis is the main idea of all the research you've done written in a precise and simple manner, usually in one sentence. The main body is where you present the statements and ideas which disclose the topic of your research. In conclusion, you sum up all the text and make a derivation.
15. On how many of the past 7 days did you exercise or take part in physical activity that made your heart beat fast and made you breathe hard for at least 20 minutes. (For example: basketball, soccer, running, or jogging, fast dancing, swimming laps, tennis, fast bicycling, or similar aerobic activities). 16.
Obesity and BMI (body mass index) are both tools of measurement that are used by doctors to assess body fat according to the height, age, and gender of a person. If the BMI is between 25 to 29.9, that means the person has excess weight and body fat. If the BMI exceeds 30, that means the person is obese. Obesity is a condition that increases the ...
thesis will study the effectiveness of the CSH programs' components and of school authorities in reducing childhood obesity, and their shortcomings. The results will help guide school health policies and practices regarding interventions in this area. The structure of this paper proceeds as follows: Section 2 provides background on
Introduction. Excess weight in children is prevalent worldwide. Although plateauing trends were observed in many high-income countries in Europe, in medium and low-income countries childhood obesity prevalence has increased in the last decade ().In Romania, almost one in four children has overweight or obesity, as shown in a pooled analysis of more than 25,000 school age Romanian children and ...
Some genetic and lifestyle factors affect an individual's likelihood of adult obesity; thus, the significant clusters of obesity observed in specific geographical regions and contexts also signal the impact of socioeconomic and environmental factors in "obesogenic" environments [13].Understanding the causes and determinants of obesity is a critical step toward creating effective policy and ...
APPENDIX 2: Statements Made by Authoritative Bodies Regarding Obesity as a Disease. 1. The National Academy of Sciences, established by an act of Congress in 1863, is composed of four organizations. One, the Institute of Medicine, created the Food and Nutrition Board.
According to Wang. and Lim (2012), the global prevalence of overweight and obesity in preschool-aged children increased from 4% to 7% within a 10-year span. An estimated 43 million. children worldwide are obese or overweight and 35 million of these children live in less-. developed countries (Wang & Lim, 2012).
We identified seven obesity-related myths concerning the effects of small sustained increases in energy intake or expenditure, establishment of realistic goals for weight loss, rapid weight loss ...
measurement. The homeostatic theory of obesity and social cognitive theory talks mainly of the theory behind childhood and adolescent obesity. However, the impact of lifestyle, nutrition, and measurement to guide regarding obesity cannot be left out. That is why all these are explained extensively. 2.1 Homeostatic Theory of Obesity:
Childhood Obesity 2 Abstract Obesity is a chronic health condition that is increasing at alarming rates in the United States, particularly among low-income children. This literature review examines several of the factors that place low-income children at risk for developing obesity: environmental (i.e., lack of access
Introduction. The history of obesity over the last 100 or more years has been an exciting time for those of involved in the field. The scientific underpinnings have increased dramatically and ...
The Obesity Society (TOS) first published a position statement on obe-sity as a disease in 2008 (1). This statement reflected the thoughtful deliberations and consensus of Society members that was published in the same year (2). In 2016, an updated in-house position paper affirmed the 2008 declaration, stating, "TOS recommits to its position ...
Abstract. Childhood obesity has become a global pandemic in developed countries, leading to a host of medical conditions that contribute to increased morbidity and premature death. The causes of obesity in childhood and adolescence are complex and multifaceted, presenting researchers and clinicians with myriad challenges in preventing and ...
A Q-methodology study, comprising 24 patients with obesity and 24 GPs. We created 48 statements with viewpoints on obesity. All participants sorted these statements in a forced grid with a quasi-normal distribution ranking from −5 (most disagree) to +5 (most agree). Subsequently, factor analysis was performed.
Obesity is an alarmingly increasing global public health issue. Obesity is labeled as a national epidemic, and obesity affects one in three adults and one in six children in the United States of America. Several countries worldwide have witnessed a double or triple escalation in the prevalence of obesity in the last three decades (Figure 1 ...
such as obesity for effective prevention and intervention (Link and Phelan, 1995). Obesity is defined as an excessively high amount of body fat or adipose tissue in relation to lean body mass. Obesity is currently on the rise in the United States; about 31 percent of U. S. adults are now obese, which is twice the rate of twenty years ago.
Obesity in children is defined as a BMI-z score above the 95th percentile (Ogden C. L., Carroll, Curtin, Lamb, & Flegal, 2010). The increasing prevalence of childhood obesity worldwide is considered a major global public health problem. While many factors contribute to the development of obesity, an imbalance between
Here we've gathered top obesity topics for presentation, research paper, or other project. 470 Obesity essay examples are an inspiring bonus! ... Thesis Statement Generator Paraphrasing Tool Title Page Generator Lit. Guides; More. Expert Q&A Study Blog About Us Writing Help Login ... School Nurses Role Regarding Obesity in School-Age Children ...
You can cut down on irrelevant aspects and revise your thesis by taking the following steps: 1. Pinpoint and replace all nonspecific words, such as people, everything, society, or life, with more precise words in order to reduce any vagueness. Working thesis: Young people have to work hard to succeed in life.
percent of children age 6-11 were obese, compared to just 7 percent in 1980 (Centers for Disease. Control, 2012). Obesity rates among older age groups are even higher, peaking at 31 percent. among 45-64 year olds (Mendez, 2010). Obesity also has a powerful effect on personal and. public healthcare costs.
Perceptions of others weight. Only 8.1 and 12.3% of all respondents correctly identified the exact male and female figure, respectively, which was the first on the picture to present individual with obesity (Table 2).The nurses (17.5%) and doctors (15.4%) were more precise than patients (6.9%) and PHE (0%) to recognize the figure of male with obesity.
Introduction: In patients with obesity (PwO) and heath care providers (HcPs), there appears to exist a discrepancy between recognition of obesity as a disease and the underlying biology of the disease. This is evident when considering PwO and HcPs appear to agree obesity is a disease but position lifestyle related factors as the main barriers to treatment with "eat less and move more ...
Thesis Statement Regarding Childhood Obesity - Free download as PDF File (.pdf), Text File (.txt) or read online for free. Scribd is the world's largest social reading and publishing site.
This study aimed to compare and relate the body composition (obtained through anthropometry with the pentacompartmental model and the tricompartmental model by DXA) with bone mineral density and biochemical and nutritional parameters in Chilean adults with overweight/obesity and normal weight from La Araucanía region, Chile. A case-control study was conducted with 116 adults and volunteers ...