DNP VS. Ph.D. - 12 Key Differences Between DNP And Ph.D. In Nursing

Nursing is one of the few professions that’s associated with two different terminal degrees: the Doctor of Nursing Practice (DNP) and the Doctor of Philosophy in Nursing (Ph.D.). The former degree is a clinical doctorate designed for advanced practice nurses who are actively working to improve healthcare outcomes in medical settings and who are championing the leadership role that nurses play in bringing about those outcomes. The latter degree is a research-focused doctorate designed to advance the science behind nursing practice. As of 2019, 40,271 nurses in the U.S. held DNP degrees according to statistics generated by the American Association of Colleges of Nursing while 6,994 nurses held Ph.D.s in nursing. If you’re an advanced practice nurse who’s interested in reaching the highest echelons of your profession, the DNP vs. Ph.D. in nursing quandary may be one you find yourself thinking about frequently. Keep reading to discover 12 key differences between DNP and Ph.D. in nursing.

What is a DNP Degree?
What is a ph.d. in nursing degree, what concentrations are offered in a dnp degree, • family nurse practitioner (fnp):, • adult-gerontology nurse practitioner (agnp):, • pediatric nurse practitioner (pnp):, • neonatal nurse practitioner (nnp):, • women’s health nurse practitioner (whnp):, • psychiatric mental health nurse practitioner (pmhnp):, • certified registered nurse anesthetist (crna):, • clinical nurse midwife (cnm):, • clinical nurse specialist (cns):, • nursing education:, • executive leadership:, • nursing practice:, • health policy:, • public health:, • nursing administration:, what concentrations are offered in a ph.d. in nursing degree, • clinical nursing research:, • public health policy:, • nursing science:, • healthcare innovation:, how many years does a dnp degree take to complete, how many years does a ph.d. in nursing degree take to complete, where can you work after earning your dnp degree, where can you work after earning your ph.d. in nursing degree, how much does a dnp graduate make.
| $49.86 | ||||
| $8,640 | ||||
| $103,719 | ||||
| (Source: Payscale.Com) | ||||
How Much Does a Ph.D. In Nursing Graduate Make?
| $42.72 | ||||
| $7,400 | ||||
| $88,849 | ||||
| (Source: Payscale.Com) | ||||
DNP vs. Ph.D. in Nursing: What is the Difference?
1. the dnp focuses on clinical practice while the ph.d. focuses on academic research., 2. the ph.d. includes a dissertation project; the dnp includes a capstone project., 3. nursing ph.d. programs often involve a mentored teaching experience., 4. ph.d. programs prefer letters of recommendation that speak to the applicant’s academic history while dnp programs prefer letters of recommendation that speak to the applicant’s clinical experiences., 5. it takes longer to earn a nursing ph.d.., 6. dnp programs require a greater number of credits for completion of the degree., 7. dnps typically earn higher salaries than nursing ph.d.s., 8. dnps have a greater assortment of employment opportunities than nursing ph.d.s., 9. unless a nursing ph.d. is a certified nurse practitioner, his or her scope of practice is limited to bedside nursing., 10. nursing ph.d. graduates do not have to go through a periodic recertification process., 11. most universities will not offer tenure track teaching positions to dnps., 12. nursing ph.d. students are not responsible for completing a minimum number of clinical hours., conclusion - dnp vs. ph.d. in nursing: which one should you pursue.
Dissertations and DNP Projects
The Doctor of Philosophy (PhD) dissertation embodies the highest level of knowledge to influence and improve nursing science and the profession through various types of studies using quantitative, qualitative, or mixed methods. A hallmark of doctoral research training, the PhD dissertation focuses on the knowledge and skills needed to conduct rigorous studies that extend the body of nursing knowledge; address important health care issues; and improve health outcomes, equity, and inclusion, all while informing health policy.
A PhD dissertation, grounded in the philosophy of science and a PhD candidate’s expertise, represents a standard of excellence and the candidate’s ability to conduct rigorous research. A PhD dissertation at UMSON contributes to the advancement of nursing/health science, solves important health care issues, and informs stakeholders. Nursing research is critical to the nursing discipline and is necessary for building evidence for practice that promotes optimal nursing care.
View the List of PhD Dissertations
The Doctor of Nursing Practice (DNP) project embodies the highest level of knowledge in nursing practice. Influencing health care outcomes through leadership, policy, information technology, systems change, and patient-centered care, the DNP project focuses on translating science into clinical practice and the delivery of patient-centered and/or population-based care.
A DNP project’s collaborative and integrative experiences reflect the development and provision of safe, effective, timely, efficient, equitable, and person-centered care aimed at advancing health outcomes. The impact of UMSON DNP projects will reshape health care in the United States.
View the List of DNP Projects

All about the DNP project
Understanding the process helps ensure a successful project..
The final doctor of nursing practice (DNP) project provides students with the opportunity to systematically translate the best current evidence into practice. However, variability in how projects are implemented exists among programs. In response, the American Association of Critical Care Nurses (AACN) commissioned white papers from two internal task forces: the Implementation Task Force (ITF) and the Advanced Practice Registered Nurse Clinical Training Task Force. The ITF’s white paper, The Doctor of Nursing Practice: Current Issues and Clarifying Recommendations, describes and clarifies the characteristics of DNP graduate scholarship (including the DNP project), efficient resource use, program length, curriculum considerations, practice experiences, and collaborative partnership guidelines. The Advanced Practice Registered Nurse Clinical Task Force white paper, Re-envisioning the Clinical Education of Advanced Practice Registered Nurses , explores how APRN education can adapt to include more simulation opportunities, academic-practice partnerships, competency-based assessments, and nontraditional APRN clinical education models, such as technology or informatics. However, the AACN doesn’t make specific recommendations with regard to the final DNP project, pointing instead to the DNP Essentials to explain the project’s scope and depth.
This article discusses the issue of project variability, then explores DNP project fundamentals to help eliminate ambiguity and confusion and broaden students’ understanding of the project’s significance. Before initiating a DNP project, several key elements—mentoring, time management, organizational and academic support, potential institutional review board approval, and planning for dissemination—must be in place. (See 8 steps to completion.)
8 steps to completion
Students should take these eight steps to complete their doctor of nursing practice (DNP) projects.
- Identify and obtain approval for the area of interest.
- Write a proposal.
- Create a project timeline.
- Acquire institutional review board approval (if needed).
- Implement project.
- Write final report.
- Present an oral presentation.
- Disseminate the project.
Source: Anderson et al. 2015.
DNP project variability
With the increased volume of new programs and growing interest in the DNP degree, the profession must clarify the scope of the final project, including implementation, impact on system and practice outcomes, extent of collaborative efforts, dissemination, and degree of faculty mentorship and oversight. Some universities require students to complete a practice improvement project over the span of a course, whereas others require students to initiate an evidence-based practice (EBP) innovation project when they begin the program and continue it through the final semester.
Despite projects’ various forms, many elements—including planning, implementation, evaluation, and sustainability—must be consistent across programs. Without concrete guidelines, programs have employed several interpretations, including portfolios, case studies, systematic reviews, and writing projects. (See Project dissemination variability. )
Project dissemination variability
Several doctor of nursing practice (DNP) project types are included in the DNP Essentials . The table compares the American Association of Colleges of Nursing’s (AACN’s) white paper recommendations and AACN DNP Tool Kit with regard to dissemination.
| (not all recommendations have been adopted in the ) | (combines and white paper) | |
| · A student’s portfolio isn’t considered a DNP project or a form of dissemination. It’s a tool to document and evaluate professional development and learning. · At a minimum, an executive summary or a written report that’s disseminated or shared beyond the academic setting is recommended for DNP project outcomes. | · A student’s portfolio isn’t considered a DNP project or a form of dissemination. It’s a tool to document and evaluate professional development and learning. · At a minimum, an executive summary or a written report that’s disseminated or shared beyond the academic setting is recommended for DNP project outcomes. | |
| · Publication in a peer-reviewed print or on-line journal is recommended. Individual faculty or a faculty committee should carefully evaluate manuscripts for possible publication and select those most appropriate for submission. · Publication in a non-refereed lay publication. | · Publication in a peer-reviewed print or on-line journal is recommended. Individual faculty or a faculty committee should carefully evaluate manuscripts for possible publication and select those most appropriate for submission. · Publication in a non-refereed lay publication. | |
| · An integrative and systematic review alone isn’t considered a DNP project and doesn’t provide opportunities for students to develop and integrate scholarship into their practice. | · Not addressed | |
| · Not addressed in recommendations | · Not addressed | |
| · Dissemination is required for each project and should include a product that describes the project’s purpose, planning, implementation, and evaluation components of the project. | · Not addressed | |
| · Poster and podium presentations · Presentation of a written or verbal executive summary to stakeholders and/or the practice site/organization leadership · Development of a webinar presentation or video (e.g. via YouTube or other public site) · Oral presentation to the public-at-large · Development and presentation of a digital poster, a grand rounds presentation, and/or a PowerPoint presentation |
· Poster and podium presentations · Presentation of a written or verbal executive summary to stakeholders and/or the practice site/organization leadership) · Development of a webinar presentation or video (e.g. via YouTube or other public site) · Oral presentation to the public-at-large · Development and presentation of a digital poster, a grand rounds presentation, and/or a PowerPoint presentation · Financial and production resources to assist students | |
| · pilot study · program evaluation · quality improvement project · evaluation of a new practice model · consulting project · integrated critical literature review | Project should · focus on a change that impacts healthcare outcomes either through direct or indirect care · have a systems or population/aggregate focus and demonstrate implementation in the appropriate arena or area of practice · include a realistic (financial, systems, political) plan for sustainability · include an evaluation of processes and outcomes (formative or summative) · be designed so processes and outcomes will be evaluated to guide practice and policy · provide a foundation for future practice scholarship. | · Not addressed |
Reasons for variability include:
- lack of faculty familiarity with quality improvement (QI) and EBP methods
- strain on faculty capacity and time commitment for project completion
- lack of faculty expertise in DNP education
- inability to find clinical sites that allow students to implement projects
- lack of DNP faculty resulting in programs led by PhD faculty
- lack of graduate-level writing skills
- differing student education levels (for example, BSN-DNP, MSN-DNP)
- time constraints within the iterative process requiring multiple revisions of written work.
Although some program variability is expected, concern about the lack of adherence to the DNP Essentials exists . In response, the AACN is committed to enhancing program congruency. To ensure consistency, post-master’s and post-baccalaureate DNP students (who begin their doctoral programs with different education and practice backgrounds) should graduate with the same comprehensive skill set as described in the DNP Essentials .
Project fundamentals
The DNP project, previously called the capstone project or the scholarly project, should demonstrate translation of acquired knowledge into clinical practice and exhibit the student’s growth in clinical knowledge, expertise, and use of the DNP Essentials and DNP Tool Kit. (See DNP Essentials and Tool Kit.)
DNP Essentials and Tool Kit
The American Association of Colleges of Nursing’s (AACN’s) eight DNP program essentials prepare nurse leaders for advanced practice.
- Scientific underpinnings for practice
- Organizational and systems leadership for quality improvement and systems thinking
- Clinical scholarship and analytical methods for evidence-based practice
- Information systems/technology and patient care technology for the improvement and transformation of healthcare
- Healthcare policy for advocacy in healthcare
- Interprofessional collaboration for improving patient and population health outcomes
- Clinical prevention and population health for improving the nation’s health
- Advanced nursing practice
DNP Tool Kit
The DNP Tool Kit, which continues to evolve, provides schools with the resources for formatting a DNP program. It combines information from the DNP Essentials and recommendations from the AACN DNP white paper to provide templates, exemplars, frequently asked questions, and other resources.
Projects can focus on QI, executive outcomes management, or an EBP change initiative aimed at strengthening healthcare. (See DNP project examples.)
Project examples
The following are examples of doctor of nursing practice (DNP) projects completed by the authors when they were DNP students.
Quality improvement projects
- After evaluating evidence-based practices for type 2 diabetic foot management, the student developed a new standardized protocol for staff education and patient care practices for foot care assessment and management.
- The student reinforced nursing education as a means to overcoming adherence barriers to an evidence-based sedation protocol for improved ICU outcomes.
Evidence-based practice projects
- The DNP student used an evidence-based survey tool to measure student anxiety when caring for dying patients. Based on the results, an education module was developed to help students manage their stress.
- To decrease nonurgent use of the emergency department and increase fever knowledge, the student created an educational program for caregivers of pediatric patients.
Guideline development and improvement project
- After a systematic evidence search, the student developed a neonatal abstinence syndrome treatment guideline to standardize care and reduce treatment duration, symptom severity, length of hospitalization, and costs.
While working on their projects, students learn to build strong, collaborative partnerships with stakeholders and mentors.
DNP programs throughout the United States require students to conduct various types of projects, which contributes to ongoing confusion about DNP preparation and role. However, all projects should reflect the DNP Essentials in a single, cumulative work that evolves as the student progresses through the program. In addition, this scholarly synthesis should serve as a platform for future scholarship after graduation.
According to the AACN DNP Tool Kit, all projects should:
- focus on a change that impacts the outcome of healthcare through direct or indirect care
- have a systems (micro-, meso-, or macro-level) or population/aggregate focus
- demonstrate implementation in the appropriate practice area
- include a plan for sustainability (it should take into account financial, systems, or political realities, not only theoretical abstractions)
- include an evaluation of processes and outcomes (formative or summative).
Frequently, a project is the outcome of a student’s identified need for improvement in clinical practice or patient outcomes guided by the spirit of inquiry. The project results are a compendium of graduate education immersed in nursing leadership, education, health policy, or clinical practice.
Dissemination
All DNP projects should emphasize positive change that advances quality outcomes, attention to systems thinking, strategies for sustainability with an appraisal of processes and outcomes, and a structure for future practice. The expectation is that DNP-prepared nurses will contribute to the body of knowledge in nursing practice by sharing their work with others so that they can apply it to their practice roles. Platforms for dissemination include social media, peer-reviewed journals, presentations, professional conferences, brochures, posters, policy briefs, organizational team meetings, media interviews, academia, and press releases. Many programs require students to summarize their projects for publication in a peer-reviewed journal.
The final requirement of the DNP project is a student’s presentation before their institution’s doctoral panel. In this venue, students deliver elemental details about their project’s processes and impact, including purpose, evidence synthesis, project design, data analysis, frameworks, and dissemination.
Be a trailblazer
DNP students’ final projects reflect the culmination of their educational journey and prepare them to share their work with others to benefit patients, the healthcare system, and the nursing profession. The result is a body of information that bridges the gap between research theory and clinical practice. As trailblazers, DNP-prepared nurses can empower other professionals to improve patient outcomes and achieve benchmarks for practice change supported by collaborative endeavors.
The following authors are DNP graduates from the University of Texas at Tyler in Tyler: Barbara Chapman is a family NP with the INTUNE Mobile Unit and assistant clinical professor in the school of nursing at The University of Texas at Tyler. Chiquesha Davis is department head of post-licensure programs, graduate programs, and assistant professor at Tarleton State University in Stephenville, Texas. Sonya Grigsby is a critical care NP at CHRISTUS Mother Frances Hospital in Tyler, adjunct nursing faculty at University of Texas at Tyler, and locum NP at OSF St. Francis Medical Center in Peoria, Illinois. Cyndi B. Kelley is a nurse manager in the special care nursery and chair of the doctoral collaboration council at Texas Health Presbyterian Hospital of Dallas and adjunct faculty in the ADN-to-BSN program at Grand Canyon University in Phoenix, Arizona. Rebecca Shipley is a family NP at CHRISTUS Trinity Mother Frances Health System. Christian Garrett is a DNP student at the University of Texas at Tyler, a family NP at CHRISTUS Trinity Mother Frances Hospital, and an adjunct professor in the school of nursing at The University of Texas at Tyler.
Alexander S. Scholarship in clinical practice: An update on recommendations for doctor of nursing practice programs. Clin Nurse Spec. 2016;30(1):58-61. doi:10.1097/NUR.0000000000000177
American Association of Colleges of Nursing. The doctor of nursing practice (DNP) tool kit. aacnnursing.org/DNP/Tool-Kit
American Association of Colleges of Nursing. The Doctor of Nursing Practice: Current Issues and Clarifying Recommendations. August 2015. aacnnursing.org/Portals/42/DNP/DNP-Implementation.pdf
Anderson BA, Knestrick JM, Barroso R. DNP Capstone Projects: Exemplars of Excellence in Practice. New York, NY: Springer Publishing Company; 2014.
Bednash G, Breslin ET, Kirschling JM, Rosseter RJ. PhD or DNP: Planning for doctoral nursing education. Nurs Sci Q. 2014;27(4):296-301. doi:10.1177/0894318414546415
Broome ME, Riner ME, Allam ES. Scholarly publication practices of doctor of nursing practice-prepared nurses. J Nurs Educ. 2013;52(8):429-34. doi:10.3928/01484834-20130718-02
Brown MA, Crabtree K. The development of practice scholarship in DNP programs: A paradigm shift. J Prof Nurs. 2013;29(6):330-7. doi:10.1016/j.profnurs.2013.08.003
Dols JD, Hernández C, Miles H. The DNP project: Quandaries for nursing scholars. Nurs Outlook. 2017;65(1):84-93. doi:10.1016/j.outlook.2016.07.009
Dreher HM, Glasgow MES. DNP Role Development for Doctoral Advanced Nursing Practice. 2nd ed. New York, NY: Springer Publishing Company; 2017.
Grigsby S, Chapman B, Kelley CB, et al. DNP and PhD: Complementary roles. Am Nurse Today. 2018;13(7):8-13.
Holly C. Scholarly Inquiry and the DNP Capstone. New York, NY: Springer Publishing Company; 2014.
Moran KJ, Burson R, Conrad D. The Doctor of Nursing Practice Project: A Framework for Success. Burlington, MA: Jones & Bartlett Learning; 2019.
Murphy MP, Staffileno BA, Carlson E. Collaboration among DNP- and PhD-prepared nurses: Opportunity to drive positive change. J Prof Nurs. 2015;31(5):388-94. doi:10.1016/j.profnurs.2015.03.001
Pandi-Perumal SR, Akhter S, Zizi F, et al. Project stakeholder management in the clinical research environment: How to do it right. Front Psychiatry. 2015;6(71). doi:10.3389/fpsyt.2015.00071
Shipley R, Chapman B, Davis C, et al. (2019). DNPs: Healthcare change agents. Am Nurse Today. 2019;14(7):16-8.
White KA, Hitzler ET, Anderson KM, et al. Essential knowledge, skills, & attitudes of mentors and mentees for successful DNP scholarly projects. Nurse Educ Today. 2018;71:107-10. doi:10.1016/j.nedt.2018.09.015
Zaccagnini ME, White KW. The Doctor of Nursing Practice Essentials. 3rd ed. Burlington, MA: Jones & Bartlett Learning; 2017.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *

NurseLine Newsletter
- First Name *
- Last Name *
- Hidden Referrer
*By submitting your e-mail, you are opting in to receiving information from Healthcom Media and Affiliates. The details, including your email address/mobile number, may be used to keep you informed about future products and services.
Test Your Knowledge
Recent posts.

Writing retreats for nurses: Inspiration to share

FAQs: AI and prompt engineering

Breaking barriers: Nursing education in a wheelchair

Effective clinical learning for nursing students

Nursing professional development at night

Engaging nurses in scholarly work

NCLEX vs Next Generation

Native knowledge

Nursing student stress, role-modeling self-care

Dedicated academic advisors for nursing student athletes

LPNs in modified care delivery models

Patient care assistant training

You’re not cut out for this: Motivation to succeed

Informatics: An essential nursing career

Standardization of virtual simulation
- Clinical Mental Health Counseling
- School Counseling
- Chemical Dependency Certificate
- Online MBA-Data Analytics Track
- Online MBA-Healthcare Management Track
- Online MBA-Management Track
- Online MBA-Marketing Track
- MSN - PMHNP
- BSN to DNP-FNP
- BSN-DNP PMHNP
- Post Masters DNP (MSN to DNP)
- Post-Masters FNP
- Post-Masters PMHNP
- Other Online Programs
- Accreditation and Affiliations
- Meet Our Faculty
- Message from the President
- Online Experience
- Placement Services
- Field Experience
- State Authorization
- Student Testimonials
- Tuition and Financial Aid

DNP vs PhD: What’s the Difference?
If you are a nurse looking to advance your career through education, a doctoral degree may be closer than you think. The Doctor of Nursing Practice (DNP) and the Doctor of Philosophy (PhD) are both terminal degrees in nursing. One of the most common questions about DNP vs PhD is “what’s the difference?”
In the DNP vs PhD question, neither degree is “higher” or “better” than the other. So does it matter which path you pursue? Yes, when considering DNP vs PhD, there are some crucial differences.
While the DNP focuses on nursing practice, the PhD concentrates on research. Answering the question of which degree to pursue, a nurse should consider both professional and academic interests. This article will delve into the differences in career outlook and educational components when comparing DNP vs PhD.

What Is the Value of a Nursing Doctoral Degree?
The United States is experiencing growing needs for medical research, nursing education, advanced practice, and system leadership in health care. Accordingly, there is significantly increasing demand for nurses with advanced degrees.
Major healthcare organizations and public health initiatives emphasize this need by advocating for more doctorally prepared nurses. In the matter of DNP vs PhD, both are valuable in different ways.
The American Association of Colleges of Nursing, the National Academies of Medicine, and the Robert Wood Johnson Foundation are collaboratively promoting this cause. In 2011, the Institute of Medicine recommended a doubling in the number of nurses with doctorate degrees by 2020. The corresponding recommendations were detailed in The Future of Nursing , a 700-page book that explores:
- Education and medical training
- Health care quality
- Policy and public health
- Workforce considerations
However, even with these high-level calls for more advanced degrees, supply is low. Still, only about one percent of nurses in the United States have earned a doctorate. This makes a doctorally prepared nurse stand out among other candidates for the most sought-after jobs.
Evaluating DNP vs PhD is the first step.

DNP vs PhD: Differences in Career Path
When considering a DNP vs PhD, it is important to remember that both degrees represent the highest level of education in nursing. A DNP equips a nurse for practice roles, while a PhD prepares a nurse for research roles.
PhD programs emphasize scientific content and research methodology in an academic context. A PhD in nursing prepares a nurse to perform health care research that benefits nurses and other medical professionals in practice settings.
DNP programs emphasize delivery of high quality health care. A nurse with a DNP is positioned as a leader in improving health care systems and patient care, applying research to practice. The DNP-prepared nurse can meet critical practice needs in both primary care and other specialized areas of nursing and nursing education.
This is a summary of the differences when considering a DNP vs PhD:
| DNP | Phd | |
|---|---|---|
| Emphasis | Patient outcomes and leadership | Scientific study |
| Primary Tasks | Lead in clinical practice | Conduct studies and publish findings |
| Purpose | Application in improving systems | Knowledge for improving systems |

What Does a DNP-Prepared Nurse Do?
The DNP role emphasizes leadership in nursing practice for improved patient outcomes. This may take the form of direct patient care, organizational leadership, or education.
Direct Patient Care
Nurse practitioners are increasingly recognized for delivering high-quality care as they provide many of the same services as physicians. Clinical practice may specialize in family care or other focused areas such as pediatrics, adult gerontology, or mental health. In the DNP vs PhD question, a DNP is more appropriate for these clinical roles.
A DNP-prepared nurse is also ideally positioned to lead nursing teams and interprofessional teams. Since patient care often involves numerous aspects, a nurse practitioner—especially in primary care—is prepared to coordinate the interrelated parts. An article published by the National Institutes of Health identifies teamwork as a leading factor in delivering safe, quality outcomes.
The comprehensive, high-level components of a DNP program prepare nurses for advanced care responsibilities and team leader roles. Several influential health organizations have collaboratively issued a statement noting the value of DNP education for nurse practitioners.
An MSN degree is currently the entry-level degree for nurse practitioners, but there is a movement toward higher educational requirements. Leading organizations are actively engaged in discussions about establishing the DNP as a standard for nurse practitioners.
The National Organization of Nurse Practitioner Faculties recommends that the DNP be the entry-level for nurse practitioner education by 2025.

Job and Salary Outlook for Patient Care Roles
The demand for nurse practitioners is expected to increase by 28% from 2018–2028. That means more than 50,000 new jobs in a 10-year period. This compares to a growth rate of only 12% for registered nurses without advanced education.
A DNP-prepared nurse pursuing clinical practice will be equipped with the highest level of education in the field. The DNP credential offers added value for prospective employers seeking to fill nurse practitioner positions with the most highly qualified applicants. In the DNP vs PhD question, a DNP is more valuable for these patient care roles.
The median annual salary for a nurse practitioner is currently $109,820 , according to the Bureau of Labor Statistics. U.S. News & World Report reports that the top 25% of nurse practitioners earn more than $125,000 annually.
Advanced education is one factor that helps a nurse achieve top positions and salaries in nursing practice. One recent survey indicated that having a doctoral degree led to nurses earning about $9,000 more, on average, than those with only a master’s degree.
Factors Affecting the Job Market
Many areas across the country are experiencing critical needs for health care providers. The Association of American Medical Colleges expects a shortage of more than 55,000 primary care physicians in the next decade. Nurse practitioners are recognized as an important part of meeting the demand and will need to be equipped with optimal education and training.
Nurse practitioners have full practice authority in 22 states and Washington, DC. In other states, NPs deliver patient care in collaboration with or under the supervision of physicians.
Leading nursing advocates such as the Robert Wood Johnson Foundation have launched campaigns to remove restrictions for nurse practitioners. With increased freedom to practice, demand for nurse practitioners is expected to increase even more, expanding quality care to more people.

Organizational Leadership
Beyond direct patient care, a nurse practitioner often pursues administrative leadership roles in a clinical setting. When choosing between a DNP vs PhD, a DNP is optimal preparation for these roles.
A DNP-prepared nurse is prepared to be an agent of change in health care systems, extending influence in a broader context. Providing a unique viewpoint, the nurse leader can introduce strategic innovation and serve as a critical part of solving major challenges.
Earning a DNP also enhances a nurse’s credibility as a thought leader and influencer. With the highest credential in nursing clinical practice, a DNP-prepared nurse is positioned to contribute to strategic development and organizational growth.
Job and Salary Outlook for Organizational Leadership Roles
Nurse Journal projects a 23% growth rate in nursing leadership and management jobs. A doctorally prepared nurse will discover a wide range of career opportunities with a system focus. Evaluating a DNP vs PhD will depend primarily on the organizational emphasis. These are some examples:
- Health care administration
- Clinical care coordination
- Nursing education
- Systems project management
- Public policy
A recent study by the American Organization for Nursing Leadership explored the job titles, workplace settings, and compensation for today’s nurse leaders. According to a survey of thousands of nurse leaders, the most common job titles are:
- Director : 35%
- Manager : 21%
- Chief Nursing Officer (CNO)/Chief Nursing Executive (CNE) : 18%
The AON study also identified these primary types of employers for nurse leaders:
- Acute care hospital
- Academic medical center
- Academic institution
- Corporate system
- Ambulatory care facility
- Consulting firm
- Critical access hospital
Salaries for nurse leaders vary by title and level of responsibility. Across the board, however, salary potential for nurse leaders is strong, with more than half earning between $90,000 and $169,999 annually. Salaries for top positions such as chief nursing officers can exceed $300,000 annually.

Changing Trends in the Job Market
With shifting dynamics in today’s health care, nurse leaders are positioned for strategic impact. Issues like nursing shortages, technological changes, and new developments in medical treatments call for unprecedented expertise. Doctorally prepared nurses will be on the forefront of leadership and innovation. Choosing a DNP vs PhD depends on the context.
Nursing Education
When considering a DNP vs PhD for nursing education careers, a prospective student should primarily consider areas of interest in teaching. A DNP degree will best prepare nurse educators for clinical teaching roles and leadership roles in clinical programs. A PhD will more effectively prepare nurse educators for teaching or administrative positions in programs geared toward research.
For a DNP-prepared nurse with a passion for shaping the next generation of nurses, nursing education is a significant opportunity. To grow the current workforce of clinical nurses, the health care industry will need more nursing programs. This calls for a new influx of nurse educators and academic administrators.
The doctorally prepared nurse will be ready at the highest level of nursing to influence the growth of nursing education programs. In thinking about a DNP vs PhD, the aspiring nurse educator will again consider professional interests. A DNP-prepared nurse is specially equipped to influence education from a clinical perspective.
Job and Salary Outlook for DNP Nursing Education Roles
The Bureau of Labor Statistics projects a 20% increase in jobs for nursing instructors from 2018-2028. Areas for the highest expected increase are:
- Private colleges, universities, and professional schools : 30.8%
- State community colleges : 24.9%
- State colleges, universities, and professional schools : 19.6%
The American Association of Colleges of Nursing advises doctorate-level education for nurses pursuing faculty positions in four-year colleges and universities. Higher-level teaching roles put nurse educators in the highest salary ranges, ranging from $76,000 to more than $100,000.

There are tremendous needs for more nurses in many health care settings today, and meeting these needs will require expanded educational systems.
One CNN report describes “hospital deserts” in some parts of the United States. With large numbers of retiring nurses and physicians, there are big gaps in health care systems. Though many highly competent students are seeking nursing education, current educational systems cannot meet the demand.
Nurse leaders can have a powerful impact in shaping the future of nursing education programs that educate clinical nurses.
What Does a PhD-Prepared Nurse Do?
The PhD role focuses on nursing research that provides content for large-scale practical application. PhD-level opportunities are primarily in the areas of direct research and nursing education. If DNP vs PhD is the question, a nurse who is passionate about scientific inquiry may be more inclined toward a PhD.
Direct Research
PhD-educated nurse researchers advance health care through the discovery of new scientific knowledge. Research findings may be applied in clinical settings, at the organizational level, or in public health contexts affecting entire populations.
The Institute of Medicine has defined nursing research to prioritize these goals:
- Emphasize wellness for all age groups
- Foster quality of life through prevention
- Give attention to vulnerable populations
- Advance economic efficiencies in health care
For the DNP vs PhD question, generally, PhD nurses conduct research to be implemented by DNP nurses in achieving these goals.
Nursing research may focus on the functions and accountabilities of nursing, generating improvements in education and practice. Nurse researchers also study clinical issues related to cures and treatments for health conditions. Such research may be applied in treating chronic illness, managing side effects, and helping patients live more productively.
These are some examples of study topics published by the National Institute of Nursing Research:
- Traumatic brain injury
- Palliative care
- Sleep apnea
- Micronutrient deficiencies
- Microbiomes

Job and Salary Outlook for Nursing Research Roles
The number of nursing research jobs is expected to increase by 19% from 2012 to 2022. The reported average annual salary for nurse researchers is $95,000. Nurse researchers also have the opportunity to expand their influence through speaking engagements, consulting, and publishing.
Here again is the question of DNP vs PhD. With increasing needs for medical research, PhD nurses are in high demand in health care related organizations such as:
- Pharmaceutical providers
- Government agencies
- Scientific institutions
- Clinical facilities
The current Strategic Plan of the National Institute of Nursing Research identifies cultural contexts driving the need for more research.
These include:
- An aging population and longer life spans
- Increasing diversity
- Scientific advances in medical treatments
- Changing research methods
Major organizations such as the American Association of Colleges of Nursing are calling for significantly increased focus on nursing research. New initiatives in funding and education will continue to increase the demand for PhD-educated nurses.
In the question of DNP vs PhD, both options are viable routes to a nursing education career. Since PhD studies will emphasize research, aspiring nurse educators interested in promoting the science of nursing may find this option appealing. A PhD-prepared nurse has a significant opportunity to influence academic research in the field of nursing.
Job and Salary Outlook for PhD Nursing Education Roles
The projected 20% increase in jobs for nursing instructors mentioned earlier may apply to either DNP-focused education or PhD-focused education.
Payscale.com estimates the average salary for a nurse educator at approximately $76,000. This number, however, would include many instructors without a doctoral credential, since only about 50% of nursing faculty have earned doctorates. Earning a terminal degree improves career opportunities for nurse educators, and salaries for professors range from approximately $80,000 to $115,000 or more.

The field of nursing as a whole faces a significant national shortage of nursing educators. Current numbers indicate a faculty vacancy rate of almost eight percent, plus needs to increase above the vacancies. In more than 90% of these positions, a doctoral degree is required or preferred.
As funding and emphasis for nursing research continue to increase, this directly impacts the need for research-focused nursing education.
With leading organizations such as the AACN calling for increasing levels of nursing research, education will need to expand to meet the demand. Deficits in the number of doctorally prepared faculty, however, limit the advancement of education to drive research initiatives. Considering a DNP vs PhD, the PhD is particularly relevant here.
DNP vs PhD: Differences in the Educational Pathway
Just as the career outlooks for DNP vs PhD have similarities and differences, so do the educational pathways to those careers. DNP programs emphasize the clinical side of nursing, while PhD programs focus more on research. In recent years, growth in DNP programs has steadily increased , while enrollment in PhD programs has stayed relatively level.
For prospective students comparing a DNP vs PhD, the American Association of Colleges of Nursing (AACN) has developed a chart that gives an overview. Differences include:
- Career focus
- Faculty emphasis

Program Structure
Assessing DNP vs PhD programs includes a review of how the educational structures are designed . PhD students are primarily concerned with developing skills and understanding for conducting research. For a DNP student, the goal is applying research to practice.
Accordingly, there are differences in the particular expertise and background of faculty. DNP instructors and mentors more often have practice-based experience, while PhD instructors and mentors emphasize backgrounds in research.
Outside the classroom, PhD students will gain experience in settings for scientific exploration. DNP students will apply academic study in clinical practice settings. Technology use will be focused on patient care for DNP students, while PhD students will use technology for research.
Admission Requirements
DNP vs PhD standards for admission are similar in many ways. DNP programs and PhD programs both typically require:
- Completion of an undergraduate or master’s degree in nursing
- Explanation of career goals
- Minimum GPA documented by official transcripts
- Active, unencumbered RN license
A PhD program is more likely to call for a writing sample. A DNP program will typically require a minimum level of clinical nursing experience.
Since DNP programs are geared to clinical practice and PhD programs are focused on research, the academic requirements of DNP vs PhD reflect this distinction.

DNP Programs
A distinctive feature of DNP vs PhD programs is the DNP’s emphasis on clinical practice. DNP students will devote significant time to hands-on experience under the leadership of faculty mentors.
Charting the future course of DNP programs, the Association of Colleges of Nursing has issued a position statement on best practices. A subsequent publication, The Essentials of Doctoral Education for Advanced Practice Nursing outlines critical curriculum elements and gives standardized criteria. Meeting program essentials is required for accreditation by the Commission on Collegiate Nursing Education.
AACN member schools are required to follow standardized guidelines for required program length and clinical hours. Guidelines also include requirements for content related to:
- Interprofessional collaboration
A DNP final project also distinguishes the DNP degree. Following the AACN “DNP Essentials” for the final project, the DNP candidate will:
- Choose a topic related to patient outcomes
- Emphasize health care systems or populations
- Show application
- Develop ideas for sustainability
- Evaluate clinical significance
- Establish groundwork for ongoing practical research
PhD Programs
Foundational nursing PhD courses give an overview of historical and philosophical frameworks. Coursework also includes research methods, statistical techniques, and technology for scientific inquiry. Faculty mentors guide PhD candidates in writing for publication.
Comparing a DNP vs PhD, a PhD program requires intensive research rather than clinical practice hours. Independent research projects are followed by a dissertation on a topic of professional interest. PhD student research covers a broad range of topics, such as:
- Advancement of nursing practices
- Caring for patients with chronic illnesses
- Solutions for side effects of medical treatments
- Treatments for mental disorders
The hallmark of a PhD program is successful completion of the dissertation. The student will work with a faculty mentor and dissertation committee to demonstrate theoretical expertise and research implications for the topic studied.
DNP vs PhD: Which Pathway Is Right for You?
Whichever direction you pursue in your DNP vs PhD decision, you will be part of advancing the nursing profession and improving health outcomes for patients. If you are passionate about doing research that promotes knowledge, a PhD is likely the path for you. If you are eager for firsthand clinical practice and administration, a DNP program will be a better fit.
Either way in DNP vs PhD, you are part of filling a tremendous need for doctorally prepared nurses.

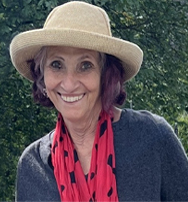
What Are the Benefits of Walsh University’s DNP Program?
If a DNP pathway is right for you, it will be important to choose a program that also fits your personal and professional values.
Walsh University’s DNP-FNP program prepares you as an empowered nurse leader committed to these outcomes:
- Leadership and advocacy
- Organizational expertise
- Data-driven quality improvement
In Walsh’s compassionate community, you will find ongoing support as you:
- Work with a placement coordinator who supports you with a preceptor and workplace sites for your clinicals
- Connect with engaged faculty of experienced nurses and benefit from small class sizes
- Receive proactive, dedicated support and one-on-one coaching to help you succeed
- Enjoy a flexible online format that allows you to continue working while earning your degree
Taking the next step in your education puts you closer to your professional goals. Walsh University’s dedicated admissions representatives are ready to guide you through each step of the process.
Find out how you can get started in Walsh University’s online DNP program.
Read more of Walsh University Online's top DNP blogs below:
1. MSN to DNP: 5 Benefits of Advancing Your Nursing Career
2. 10 Tips for Nurses to Maintain Worklife Balance
3. Doctor of Nursing Practice: Is a DNP the Right Degree for You?
4. Best Places for Nurses to Live and Work
5. MSN vs. DNP: What's the Difference?
Get More Information
Download Brochure
want more information?
Download a Brochure
Walsh University is not affiliated with Walsh College • All website content © Copyright 2024 Walsh University. All rights reserved. • Sitemap • Privacy Policy • California Privacy Notice
DNP-PhD Comparison
The DNP degree is a practice doctorate. The PhD is a research doctorate. Graduates of PhD programs are prepared to conduct independent research and disseminate their findings. The DNP will provide graduates with the skills and tools necessary to assess the evidence gained through nursing research, evaluate the impact of that research on their practice and, as necessary, make changes to enhance quality of care. Scholarship is an integral part of both doctoral degrees.
| Doctor of Nursing Practice | PhD in Nursing | |
|---|---|---|
| Nursing Practice | Nursing Research | |
| To create nursing leaders in interdisciplinary health care teams by providing students with the tools and skills necessary to translate evidence gained through nursing research into practice, improve systems of care and measure outcomes of patient groups, populations and communities. | To prepare nurse scientist to develop new knowledge for the science and practice of nursing. Graduates will lead interdisciplinary research teams, design and conduct research studies and disseminate knowledge for nursing and related disciplines, particularly addressing trajectories of chronic illness and care systems. | |
| Translation of Evidence to Practice, Transformation of Health Care, Health Care Leadership and Advanced Specialty Practice | Trajectories of Chronic Illness and Care Systems | |
| EBP I and II, Quantitative Methods, Data-Driven Health Care Improvement, Applied Finance & Budget Planning, Effective Leadership, Transforming the Nation's Health and Health Systems Transformation | Philosophy of Science & Theory Development, Advanced Research Methods, Statistics & Data Analysis, Longitudinal & Qualitative Research Methods, Chronic Illness & Care Systems | |
| Optional | Minimum of 140 hours | |
| 400 minimum within scholarly project | None | |
| Yes | No | |
| No | Yes | |
| Yes | No | |
| Yes, Program designed for working nurses | No | |
| BSN or master's in advanced nursing practice | BSN or MSN or related master's degree | |
| Five semesters for MSN entry; varies for BSN entry* | Four to five years | |
| 35 to 94* | 57 | |
| Health care administration, clinical nurse faculty | Nurse scientist, nursing faculty | |
| Not for students who have an earned master's | Not for students who have an earned PhD | |
| N/A | Full tuition, fees and health insurance paid by School of Nursing | |
| N/A | 12-month stipends are fully funded for the first two years of the program. Tuition and 9-month stipends are fully funded in years 3-5. | |
| * Program length and required credits depend on advanced practice specialty selected, 73 to 94 credits for BSN entry. For MSN entry, 35 to 41. | ||
| **All applicants should view the to learn more on financial aid options. | ||
LET US HELP
Welcome to Capella
Select your program and we'll help guide you through important information as you prepare for the application process.
FIND YOUR PROGRAM
Connect with us
A team of dedicated enrollment counselors is standing by, ready to answer your questions and help you get started.

- Capella University Blog
- PhD/Doctorate
The difference between a dissertation and doctoral capstone
May 30, 2023
Estimated reading time: 3-4 minutes
If youâve been researching doctoral degrees, you may notice that virtually all PhD programs require a dissertation, while some professional doctorates require a doctoral capstone or an alternative doctoral project.
So, whatâs the difference between the two?
What do a dissertation and doctoral capstone have in common?
All doctoral programs help prepare students to contribute evidence-based practice in their field. Students learn to apply leadership principles and strategies that promote community support, diversity and individuality in the workplace, and the community.
Completing either a dissertation or a doctoral capstone requires intense preparation and a strong foundation in writing and critical thinking. Both culminate in a final document or project that demonstrates a broadened knowledge of relevant theory and practice.
What are the main differences between a dissertation and a doctoral capstone?
The Capella doctoral experience offers a good comparison of the two types of final project.
The Capella dissertation is a traditional five-chapter research document that youâll develop as you work with a faculty mentor and dissertation committee members. Itâs meant to be a work of high-quality academic research that contributes to your field of study.
The doctoral capstone can take many different forms depending on your program, your specialization or area of interest within your subject and other variables. Working with a faculty mentor and committee, youâll complete a project that offers solutions or improvements to a real-world problem relevant to your field of study.
- Project focus
- Project deliverable
- Deliverable detail
Doctoral Capstone
- Extends or applies research to solve a real-world problem
- Provides a solution to a problem within a specific organizational setting
- Presents the results in a deliverable (paper, product, or portfolio) and a final report that describes the creation of the deliverable
Dissertation
- Involves a quest for new knowledge to solve a real-world problem
- Addresses a research problem in one field of specialization
- Involves either quantitative or qualitative research methods
- Paper, Product or Portfolio
- Action research
- Clinical Research Paper
- Program Curriculum
- Change Management Plan
- Chapter 1. Introduction and Statement of the Problem
- Chapter 2. Literature Review
- Chapter 3. Methodology
- Chapter 4. Data Analysis and Results
- Chapter 5. Conclusions and Recommendations
Ready to explore the doctoral path that could work best for you? Capella University offers PhD and professional doctorate degree programs ranging from business and education to health care and technology.
Learn more about Capellaâs online doctoral programs.
You may also like

Can I transfer credits into a doctoral program?
January 8, 2020

What are the steps in writing a dissertation?
December 11, 2019

What you need to know about paying for your doctorate
November 11, 2019
Start learning today
Get started on your journey now by connecting with an enrollment counselor. See how Capella may be a good fit for you, and start the application process.
Please Exit Private Browsing Mode
Your internet browser is in private browsing mode. Please turn off private browsing mode if you wish to use this site.
Are you sure you want to cancel?
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

A 10-year evaluation of projects in a doctor of nursing practice programme
AUTHOR CONTRIBUTION

Associated Data
Aims and objectives:.
The role of professional doctorates is receiving increased attention internationally. As part of building the rigour and scholarship of these programmes, we assessed projects undertaken as part of a doctor of nursing practice (DNP) programme at Johns Hopkins University. Recommendations for programme development in professional doctorates are provided.
Background:
Past research has described the methodologic limitations and dissemination of DNP projects. However, few studies have provided recommendations for strengthening these projects and alternative strategies for achieving scale in larger student cohorts.
A descriptive study reported in accordance with STROBE guidelines.
From 2009–2018, 191 final DNP project reports were obtained from the DNP programme administrator. Essential project characteristics from the papers were extracted, including use of theoretical framework, design, setting, sample and dissemination through publication. To determine whether the results of the projects had been published, the title and student’s name were searched in Google Scholar and Google.
Of the 191 projects, 83% focused on adults and 61% were conducted in the hospital setting. Sample sizes ranged from 7 to 24,702. Eighty per cent of the projects employed a pretest/post-test design, including both single and independent groups. The projects spanned six overarching themes, including process improvement, clinician development, patient safety, patient outcome improvement, access to care and workplace environment. Twenty-one per cent of the project findings were published in scholarly journals.
Conclusions:
Conducting a critical review of DNP projects has been useful in refining a strategy shifting from incremental to transformative changes in advanced practice.
1 |. INTRODUCTION
As nursing is a practice discipline, there is a strong movement to recognise this significance at the level of the terminal degree ( Fulton, Kuit, Sanders, & Smith, 2012 ). As long ago as the late 1970s, there have been widespread calls worldwide to bring doctoral education closer to practice ( Yam, 2005 ). The professional doctorate has emerged internationally to satisfy university requirements for a doctoral degree and meet the needs of various professional groups by preparing students to work within a professional context ( Yam, 2005 ). The professional doctorate is widespread and increasingly adopted by varied professions, often making it challenging to clearly delineate this credential between disciplines. However, the 2005 task force by the Council for Higher Education Accreditation and Council of Graduate Schools identified a number of core characteristics, recommending that the professional doctorate should (a) address an area of professional practice where other degrees are not currently meeting employer needs, (b) emphasise applied or clinical research or advanced practice and (c) include leaders of the profession who will drive the creative and knowledge-based development of its practices and the development of standards for others ( CGS in the USA, 2007 ; DEST, 1997 ). Professional doctorates have also grown more prevalent internationally ( CGS, 2006 ; CGS in the USA, 2007 ; DEST, 1997 ; Mellors-Bourne, Robinson, & Metcalfe, 2016 ) with the doctor of nursing practice (DNP) being one such professional doctorate that has been developed in recent years ( CGS in the USA, 2007 ).
The professional doctorate typically requires students to complete a dissertation or project to fulfil the requirements of a doctoral degree ( CGS in the USA, 2007 ). In 2015, the American Association of Colleges of Nursing (AACN) issued a report from the Task Force on the implementation of the DNP with a section addressing DNP projects. This document explained that DNP programmes prepare nurses in advanced nursing practice to influence health care outcomes at the individual or population level. It also provided six key elements that should be present in all DNP projects: (a) focus on a change impacting healthcare outcomes, (b) systems or population approach, (c) demonstration of implementation in the appropriate arena of practice, (d) plan for sustainability, (e) evaluation of a process and/or outcomes and (f) provide for future practice scholarship ( AACN, 2015 ). In 2018, a report from AACN provided more information on the scholarship of practice and gave several examples of projects in this category. While the report mentions the translation of research, quality improvement initiatives and the use of big data and system-wide data in the scholarship of practice, it avoids being overly prescriptive about methods to use in the scholarship of practice ( AACN, 2018 ). There have been several papers in the literature describing limitations in the design and reporting of DNP projects both within and across DNP programmes. The Johns Hopkins University School of Nursing is in its 130th year as a school and 10th year as a DNP programme. The authors take this occasion to describe and critique the DNP projects conducted by students in our DNP programme since its outset and provide recommendations to strengthen our programme that we hope may be useful to faculty in other schools with DNP programmes.
2 |. BACKGROUND
There have been several papers in the nursing literature between 2013–2019 that have described curricular and educational approaches to guiding students in the development of DNP projects ( Brown & Crabtree, 2013 ; Kirkpatrick & Weaver, 2013 ; Waldrop, Caruso, Fuchs, & Hypes, 2014 ), DNP project topics ( Howard & Williams, 2017 ; Minnick, Kleinpell, & Allison, 2019 ) and the quality of measurement and analyses used in DNP project reports across schools in the USA ( Dols, Hernandez, & Miles, 2017 ; Roush & Tesoro, 2018 ). Roush and Tesoro (2018) examined 65 DNP project reports stored in the electronic dissertation and thesis database, ProQuest®. The authors reported substantial methodological limitations in the project reports including inadequate description of the methods used for sample selection, intervention implementation and data analyses. The authors had several recommendations including greater attention to teaching these methods and publication of the DNP projects to allow for ongoing evaluation across schools.
Earlier reports of DNP projects at Johns Hopkins University School of Nursing included a report by Terhaar and Sylvia in 2015 examining 80 DNP project reports from the first five years of the DNP programme. The most common method of analysis of project findings was descriptive–comparative and more than half of the students used a pretest/post-test design. The authors noted that the scope and complexity of the projects increased from the first cohort to the fifth cohort and that students in the earlier cohorts were more likely to examine changes in knowledge than students in the later cohorts. In another paper describing publication outcomes of DNP students at Johns Hopkins University School of Nursing, Becker, Johnson, Rucker, and Finnell (2018) described the 156 students enrolled in between 2009–2016 and any publications that they had during their studies and after graduation. Fifty-eight (37%) students published their DNP Project papers and 20 (13%) published integrative reviews of the literature.
2.1 |. Description of the Johns Hopkins University School of Nursing DNP Executive Program
Johns Hopkins University School of Nursing launched a Post-Master’s DNP Executive Program in 2008 that was accredited by the Maryland Higher Education Commission and the Commission on Collegiate Nursing Education. The six-semester programme includes coursework in quality improvement for evidence-based practice, graduate-level biostatistics, finance, informatics, health policy and leadership. At least one full-time faculty member and an organisational mentor guide the student in completing a DNP Project that is relevant to the student’s practice. DNP project proposals are reviewed by the Johns Hopkins University Medicine Institutional Review Board (IRB). Most have been classified as performance improvement projects. A few have undergone an IRB review for human subjects research. Due to the large increases in number of students and subsequently DNP projects, the Johns Hopkins University School of Nursing has established its own internal IRB, in collaboration with the Johns Hopkins University Medicine IRB, to review future DNP projects starting in 2020. The School of Nursing internal IRB will decide whether projects are performance improvement, if projects are thought to be human subjects research, they will still be submitted to the Medicine IRB for review.
Johns Hopkins University School of Nursing saw its first DNP cohort graduate in 2009. The authors take this occasion on the 10th year of the DNP programme and the 130th year of Johns Hopkins University Nursing to describe the DNP projects completed by students in this programme up to 2018. In this descriptive study, we follow 10 cohorts of students and aim to (a) evaluate the publication of project outcomes over time; (b) describe the components of the DNP projects, including the topics addressed in the projects, theoretical underpinnings, designs, samples and methods of analysis; and (c) recommendations for the future direction of DNP projects and education. We offer recommendations for strengthening the DNP projects at our own school including a template to guide construction and reporting of the projects and a summary of common methods of analysis employed in these projects that may be useful to faculty and students in other schools with DNP programmes.
3 |. METHODS
Using the method of a descriptive study design, assessment of 191 projects submitted from cohorts graduating between 2009–2018, as part of course work requirements were assessed. Final versions of the DNP project reports were submitted to the DNP programme administrator to be retained on file as part of the collection of scholarly products of the DNP programme. The authors extracted essential project characteristics from the papers including use of theoretical framework, design, setting, sample and dissemination through publication. Three of the authors performed the initial extraction to an Excel spreadsheet. One co-author extracted information from all 191 projects on the DNP project theme, theoretical framework, sample and setting. The projects were then split evenly between the two co-first authors for verifying the previously extracted information and to extract additional information on project design, analysis and publication. All authors discussed any discrepancies and reached consensus to validate the project characteristics and outcomes. To determine whether the results of the projects had been published at any point since the student graduated from the programme, the two co-first authors searched the title and student’s name, from the list of programme graduates obtained from the DNP programme administrator, in Google Scholar and Google. In some cases when no publications were discovered in Google Scholar and Google, the authors also searched PubMed and CINAHL. The study was carried out according to the STROBE guidelines (see Appendix S1 ). This study was deemed exempt research by the Johns Hopkins University School of Medicine Institutional Review Board (IRB00248926).
4 |. RESULTS
The authors analysed all 191 DNP Executive project reports and Table 1 provides a summary of the key elements of the DNP projects. Eighty per cent of the projects employed a pretest/post-test design which included both single and independent groups. Sample sizes ranged from 7 to 24,702. Eighty-three per cent of the projects focused on adults and 61% were conducted in the hospital setting. Sixty-seven per cent of the projects did not specify a conceptual framework used.
DNP project characteristics
| = 191 | |
|---|---|
| Design | |
| Pretest/post-test | 153 (80%) |
| Post-test only | 17 (9%) |
| Randomised controlled trial | 5 (3%) |
| Other | 16 (8%) |
| Sample | |
| Patients/family/community members | 79 (41%) |
| Clinicians/Healthcare students and support staff | 55 (29%) |
| Both | 51 (27%) |
| Other | 6 (3%) |
| Age | |
| Adults | 159 (83%) |
| Paediatric | 10 (5%) |
| Both | 19 (10%) |
| NA | 2 (1%) |
| Unknown | 1 (1%) |
| Setting | |
| Inpatient/ED/OR | 117 (61%) |
| Outpatient/Community/Schools | 60 (31%) |
| Both | 5 (3%) |
| Other | 9 (5%) |
| Framework | |
| Yes | 63 (33%) |
| No | 128 (67%) |
| Published | |
| Yes | 41 (21%) |
| No | 150 (79%) |
4.1 |. Project themes
The main themes that were the focus of the DNP projects and one or two examples by theme are included in Table 2 . Six overarching themes were identified, including process improvement, clinician development, patient safety, patient outcome improvement, access to care and workplace environment. Many of the projects spanned multiple of the identified themes.
DNP project themes
| DNP project themes | Examples of DNP projects |
|---|---|
| 1. Process improvement | |
| a. Screening/early detection | Facilitate the recognition of juvenile fibromyalgia syndrome (JFS) by primary care providers in paediatric clinical setting through the development of a JFS recognition tool, education to providers and implementation of the tool |
| b. Documentation | Create, implement and evaluate a nursing care flow sheet and documentation guideline to improve quality of documentation |
| c. Adherence to guidelines | Development and use of an algorithm and nurse education to improve ED nurses' assessments, documentation and referrals provided to patients regarding intimate partner violence |
| d. Time to health care delivery | Examine the effect of a multidisciplinary system of communication on achieving 90-min first medical contact to open artery goals |
| e. Time to discharge | A care delivery model to facilitate the flow of level-3 patients through the ED to reduce ED crowding |
| f. Reducing readmission rates | Test the feasibility of an advanced practice nurse-led transitional care programme to reduce preventable readmissions |
| 2. Clinician development | |
| a. Leadership development | Development of leadership skills among bedside nurses: succession planning |
| b. Mentorship programmes | Evaluate the effectiveness of a peer-coach model to increase nurse competence in use of electronic health records |
| c. Continuing education to promote quality care | Development of leadership-training curriculum to reduce the prevalence rate of facility-acquired pressure ulcers |
| d. Training/education | Evaluating effectiveness of an educational training intervention to improve provider compliance with ACOG guidelines for HPV/Pap testing for primary screening in low-risk women aged 30+ years |
| e. Provider knowledge | Educational intervention to increase the knowledge of obstetrical providers on the guidelines for foetal echocardiography |
| f. Collaboration/communication | Use real-time data display of patient-specific information to improve communication and teamwork within the operating room suite |
| 3. Patient safety | |
| a. Medical errors | Evaluate a comprehensive laboratory tracking system with a multidisciplinary approach on tracking, follow-up, and reporting of laboratory test results to prevent medical errors |
| b. Medication administration | Increase knowledge among critical care nurses about identifying and reporting medication errors and near miss events, identify barriers in recognising and reporting such events, and pilot test a voluntary electronic reporting system from the Maryland Patient Safety |
| c. Infection control | Use of multidisciplinary strategies, including staff education, catheter care and best maintenance practices to reduce the number of positive urine cultures in critically ill children |
| d. Informed consent | Enhancement of consent process so that patient safety is a priority, and obtaining informed consent is a consistent process |
| 4. Patient outcome improvement | |
| a. Patient health outcomes | Development of checklist to decrease incidence of extubation failure in adult trauma patients |
| b. Patient lifestyle change | Evaluate the relationship between intrinsic and extrinsic motivators and exercise beliefs and attrition and completion rates of senior fit programme participants |
| c. Patient self-care | Test nurse practitioner use of 5A's intervention to improve adult type 2 diabetes self-management |
| d. Patient symptom management | Implement and examine impact of community health educator education intervention on using low-osmolarity oral rehydration solution and zinc supplements to improve home management of diarrhoeal disease in children in rural Nicaragua |
| e. Patient knowledge | The use of a multicomponent intervention to improve knowledge and minimise lymphedema risk among newly diagnosed breast cancer patients |
| f. Patient satisfaction | Develop and explore feasibility and acceptability of a web-based family resource for paediatric obesity prevention in a university health maintenance organisation patient population |
| 5. Access to care | |
| a. Follow-up appointment | To implement and evaluate site-specific appointment keeping processes to increase attendance rates among adult type II diabetics with follow-up appointments |
| b. Transitional care | Accomplish a smooth transition for high-risk neonates from the acute care setting into primary care setting |
| 6. Workplace environment | |
| a. Satisfaction | Number of patient-initiated calls, patients' satisfaction of nursing staffs' response to their calls via semistructured interviews, subset of Press Ganey Satisfaction survey to assess patients' satisfaction of promptness in response to calls and teamwork scores as assessed by the Nursing Teamwork Survey (NTS) |
| b. Retention | Implementation of National Database of Nursing Quality Indicators (NDNQI) Practice Environment survey to provide nurses with data to develop improvement projects that improve taking shift breaks and nurse retention |
| c. Burnout | Examine the effects of compassion fatigue resiliency training on compassion satisfaction, burnout, secondary traumatic stress and resiliency in emergency nurses |
| d.Safety | Impact changes to the work environment have on nurses' perceived and directly observed distractions and interruptions during medication administration |
4.1.1 |. Process improvement
Process improvement projects sought to increase efficiency of health care delivery related to human factors and systems integration. The processes examined included screening for disease conditions and health risks, documentation of care processes, adherence to guidelines, time to healthcare delivery, time to discharge and reduction of readmission rates. One project involved establishing a command centre for a nearly 1,000 bed hospital and examined admissions and interhospital transfers resulting in increased efficiency in these processes throughout the hospital ( Newton & Fralic, 2015 ).
4.1.2 |. Clinician development
Clinician development refers to improving clinician skills, knowledge and abilities. Projects focused on leadership, mentorship, educational approaches and interprofessional training. Multiple dimensions of communication were examined including the content and timing of communication and the confidence of the clinician communicating. Many of these projects measured knowledge before and after an educational intervention. One of these projects involved examining the effectiveness of short, frequent training sessions on nurses’ retention of initial cardiopulmonary resuscitation priorities and the most efficient training interval ( Sullivan et al., 2015 ).
4.1.3 |. Patient safety
Patient safety included patient protection from medical errors and other harms, including projects associated with reducing medical errors and improving medication administration, infection control, and the informed consent process. One of these projects involved examining the effectiveness of a mandatory computerised ordering tool that allowed for early interdisciplinary communication and evaluation by a Peripherally Inserted Central Catheter (PICC) team for suspected PICC infections and thromboses, on decreasing premature PICC removal rates and associated complications ( Kim-Saechao, Almario, & Rubin, 2016 ).
4.1.4 |. Patient outcome improvement
Projects focused on patient outcome improvement in the healthcare setting assessed various aspects of health, lifestyle behaviour, self-care, symptom management, knowledge and satisfaction. One of these projects involved examining the effectiveness of an education programme and increased patient support options, as well as increased provider education on continuous positive airway pressure adherence ( Dinapoli, 2015 ).
4.1.5 |. Access to care
Access to care refers to connections to care, such as improving patient attendance at follow-up appointments, and transitions of care, such as from the acute to the primary care and the paediatric to adult setting. One of these projects involved examining the effectiveness of a telemental health programme, in a rural setting, in improving time to consult as compared to face-to-face groups ( Southard, Neufeld, & Laws, 2014 ).
4.1.6 |. Workplace environment
Workplace environment included patient factors such satisfaction but also improvement of the work environment for nurses and other health professionals. One of these projects involved determining whether the implementation of a standardised handoff tool, reorganising interrupting processes and training on effective handoff communication could reduce the number of interruptions per intershift report ( Younan & Fralic, 2013 ).
4.2 |. Settings
Sixty-one per cent of projects took place in hospital settings including emergency rooms, inpatient medical or surgical units, critical care areas and the operating room. Thirty-one per cent of projects took place in schools, outpatient and community settings. An additional 3% of projects bridged both the hospital and outpatient/community settings.
4.3 |. Samples
Samples included patients, family members, community members, clinicians, students and healthcare support staff. Eighty-three per cent of projects included adult samples and 5% of projects included paediatric samples. An additional 10% of projects included both adult and paediatric samples. Some projects examined a single race or ethnic group. The locations for the projects relative to the university were local, national and global representing countries on multiple continents in North and Central America, Africa and the Middle East.
4.4 |. Theoretical framework
Thirty-three per cent of the reports described a theoretical framework that was used to guide the project. The most common were evidence translation models such as The Knowledge to Action Framework ( Graham et al., 2006 ), the Johns Hopkins University Translating Evidence into Practice Model ( Dang & Dearholt, 2017 ) and the Ottawa Model of Research Use Framework ( Logan & Graham, 1998 ). Some were broadly focused such as Rogers’ Diffusion of Innovation ( Rogers, 1962 ) and process improvement theories including The Content and Process Model of Strategic Change ( Pettigrew & Whipp, 1992 ). Others were focused on specific conditions such as chronic illness and addiction disorders. Examples of these included the Chronic Care Model ( Kane, 1999 ) and the National Center for HIV/AIDS, Viral Hepatitis, STDs and TB Prevention Framework ( CDC, 2009 ).
4.5 |. Designs
The various types of designs used for the projects are summarised in Table 1 and represent the breadth of advanced nursing practice. Eighty per cent of the projects used a pretest–post-test design and one of these was a mixed-methods study design. Some used the same sample while others used two different samples before and after the introduction of an intervention. Still others used post-test only with a historical comparison group. The remainder of the projects used a variety of designs including single sample post-test only, randomised controlled trial design, systematic review and proposal of strategies. Five of the DNP projects used a randomised controlled trial design. However, in these designs the control group largely consisted of usual care and blinding was not used. Four of these randomised controlled trials employed the typical two group, intervention and control design and one study employed a multi-group design.
4.6 |. Analyses
The majority of the projects used univariate analysis including independent or paired t test and chi-square. Only a few of the projects used regression analysis. Most students used the statistical package, SPSS to conduct their analyses. Most reports did not include a power analysis.
4.7 |. Sustainability
Eighteen per cent of reports included a plan for sustainability of the project. For example, many projects involved the adoption of the new performance improvement process in the unit practice or a plan was developed to adopt the new practice in the future.
4.8 |. Publications
All projects were presented orally or as posters. Publications were discovered for 21% of the projects reviewed in both nursing and interdisciplinary journals. The impact factor of these journals ranged from 0.1 to 5.9. These included both specialty journals, such as Resuscitation, Progress in Transplantation and Advances in Neonatal Care, and journals focused on performance improvement such as Journal of Nursing Care Quality.
5 |. DISCUSSION
Many of the projects undertaken as part of the DNP degree were designed to describe the implementation of a new evidence-based practice intervention and the patient and provider outcomes that followed within a particular practice setting. The evolution of our DNP programme has occurred in the context of significant development in both implementation science and quality improvement methodology. Implementation science is the study of methods for promoting the adoption and integration of evidence-based practices, interventions and policies into routine practice and has been codified in frameworks such as the Consolidated Framework for Implementation Research ( CFIR, 2019 ). Similarly, the Standards for QUality Improvement Reporting Excellence have increased both the rigour in design and reporting of quality improvement strategies ( Ogrinc et al., 2016 ). A strength of the DNP programme at Johns Hopkins University is the collaboration among faculty with research and advanced practice expertise in teaching and guiding DNP students in their DNP projects. This collaboration results in a range of methodological approaches to these projects. Cygan and Reed (2019) have described an approach to collaborative DNP-PhD scholarship that is consistent with what we have described here.
Within the curriculum, there is an emphasis on dissemination and all students present their work as an oral presentation or poster presentation at a School of Nursing conference to which our practice partner institutions are invited. In addition, 21% of students generated a peer-reviewed publication reporting the DNP project outcomes. As part of knowledge sharing and exchange, we also encourage students to place their project in the Sigma Theta Tau Virginia Henderson Repository ( Sigma Theta Tau, n.d. ).
5.1 |. Limitations of this review
This review of DNP projects has some limitations. First, we report that 21% of the projects generated publications. But it can take two or more years for students to publish a paper from their projects so this publication rate may be artificially low. Second, the DNP projects included in this review are solely from the Post-Master’s DNP Executive Track of the DNP programme at Johns Hopkins University School of Nursing. Thus, the findings may not be generalisable to the Post-Baccalaureate DNP Advanced Practice Track at Johns Hopkins University School of Nursing. However, we believe that our recommendations to improve our DNP Executive Track and the guidelines we provide will be useful for faculty in both Tracks. Finally, since this paper has looked at 191 DNP projects over the past 10 years, we provided a general overview of the findings. Faculty may wish to examine various subgroups by population, setting or type of intervention/practice guideline, to provide further detail. More importantly, these data reflect the maturation of the DNP programme and the implementation of the DNP essentials ( AACN, 2006 ) focusing on advanced nursing practice that is evidence-based, innovative and applies credible research findings. We have some exciting new programmes, including the dual degree programmes DNP-PhD and DNP-MBA which will extend our domain-specific knowledge to advance patient outcomes. As many programmes strive internationally to increase the focus on practice doctorate, this reflective analysis provides some useful signposts for increasing both the rigour and programme relevance.
5.2 |. Strengths of projects
One strength of the projects that reflects the strength of the Johns Hopkins University School of Nursing was the international diversity of the projects from countries in North and Central America, Africa and the Middle East. The projects reflected the diversity of nursing practice across these countries such as the nurses’ role in patient education and in leading process improvement initiatives in the practice setting.
Another strength was the number of publications that were generated. We found that 21% of the projects resulted in publication. This was lower than the 37% in a previous report that included DNP projects from Johns Hopkins University School of Nursing up to 2016 by Becker et al. (2018) . This may be because these authors, in addition to searching the literature using PubMed and Google Scholar also accepted a print version of a publication provided by the graduate. For this paper, we only searched the literature electronically and did not also examine publications that the graduates provided that were not found in the literature search.
The diversity of the settings in which the projects were conducted demonstrated the opportunities for nurses to lead initiatives resulting in improvements in patient outcomes. They also demonstrate the rich learning opportunities for nurses in DNP programmes to learn from colleagues who practise across the spectrum of healthcare delivery.
5.3 |. Opportunities for future development of DNP projects
In this section, we discuss the implications of our findings for future directions and improvement in DNP projects and education.
5.3.1 |. DNP project reports
Most studies were designed to evaluate factors influencing the translation of an evidence-based intervention into practice. However, one limitation identified was that only 33% of the project reports included the translation framework used although translational frameworks are a required part of the development of their project proposal. Moving forward, we have increased our teaching and guidance about how these frameworks guide the development of the project and how to incorporate the framework into the project report. The majority of our students did not report a power analysis when it would have been appropriate given the design. In order to promote accurate interpretation of the findings, this has become a requirement in cases where the significance of differences between pretest and post-test within a single group or between two or more groups is being assessed. Students have the opportunity to learn these methods in the curriculum and also have access to a designated statistician for consultation.
In order to promote coherence between the design used in the project and analysis of findings, we have developed a template to guide faculty and students that may be useful to faculty and students in other DNP programmes ( Appendix S2 ). We have also included a description of common DNP project designs ( Figure 1 ) and analyses ( Table 3 ) to guide faculty and students in project development.

DNP project designs
Guidelines for analysis by design
| Ordinal and interval/Ratio dependent variables | |||||
|---|---|---|---|---|---|
| Number of groups in independent variable | Nature of groups in independent variable | Sample size | Distribution of DV | Statistical test | |
| 1 group | ≥ 30 | Normally distributed | One-sample test or test | ||
| 30 | Normally distributed | One-sample test | |||
| Not normal | Sign test | ||||
| 2 groups | Independent | ≥ 30 | Normally distributed | test | |
| Not normal | Mann-Whitney or Wilcoxon rank- sum test | ||||
| < 30 | Normally distributed | test | |||
| Not normal | Mann-Whitney or Wilcoxon rank- sum test | ||||
| Paired | ≥ 30 | Normally distributed | Paired test | ||
| Not normal | Wilcoxon signed-rank test | ||||
| < 30 | Normally distributed | Paired test | |||
| Not normal | Wilcoxon signed-rank test | ||||
| 3 or more groups | Independent | NA | Normally distributed | 1 factor/IV | One-way ANOVA |
| ≥2 factors/IVs | Two-way or N-way ANOVA | ||||
| Not normal | Kruskal-Wallis one-way analysis of variance by ranks | ||||
| Dependent | NA | Normally distributed | Repeated-measures ANOVA | ||
| Not normal | Friedman two-way analysis of variance by ranks | ||||
| 1 group | and n(1-p) ≥ 5 | -approximation | |||
| or n(1-p) < 5 | Binomial | ||||
| 2 groups | Independent | Fisher exact test | |||
| ≥ 5 | Chi-squared test | ||||
| Paired/ Case control | McNemar | ||||
| 3 or more groups | Independent | < 5 | Collapse categories for chi-squared test | ||
| ≥ 5 | Chi-squared test | ||||
| Dependent | Cochran's | ||||
| Type of data | Distribution of dependent variables | Number of independent variables | Statistical test | ||
| Interval/ratio data | Normally distributed | 1 | Simple linear regression | ||
| >1 | Multiple linear regression | ||||
| Dichotomous data | NA | 1 or more | Binary logistic regression | ||
| Categorical (>2 categories) data | NA | 1 or more IVs | Multinomial regression | ||
5.3.2 |. Scope and depth of DNP projects
Opportunities for advancing the scope and depth of the projects in the future may involve group approaches that would allow two or more students to work on one project. This would allow student groups to focus on several dimensions of the same project. For example, among a student group interested in studying readmission rates among patients with congestive heart failure several dimensions the students could address include the following: lifestyle education, patient and caregiver knowledge, symptom management and follow-up care. This would enable each student to select one dimension and working together, and develop a more comprehensive and effective improvement project. Project design courses would need to incorporate elements on developing cohesive interventions supported by practice guidelines and research findings.
While the AACN supports group projects in which each student is accountable for at least one component of the project and a deliverable ( AACN, 2015 ), we have not yet had a group DNP project at Johns Hopkins University. Moving ahead, we are considering how we might engage students in group projects simultaneously or sequentially at different sites or focusing on different aspects of the same project. We are now finding that when the practice sites offer several potential projects to students and students select from among these, the practice site is more likely to be invested in DNP projects.
5.3.3 |. Sustainability of DNP projects
As noted, only 18% of the project reports included a plan for sustainability. Moving forward, the need for sustainability and ideas on how to achieve sustainability should be included in the curriculum at the beginning of project development. Potential methods for promoting sustainability of DNP projects may be through the pursual of longitudinal DNP projects with more than one DNP student participating. Another aspect in the future that will promote sustainability will be a more formal process for having the practice sites select the projects and having DNP students choose from among projects that are a priority to the clinical partner agency. Some challenges in having partner agencies select the project are that they may want to use a self-designed measure that has not been validated. In the light of this, the programme now seeks to emphasise the need to find validated instruments and guides students to the available resources in order to accomplish this goal.
The process of analysing these projects provided us with insight into some strengths and limitations of our programme and has guided our plans for improving our teaching and learning strategies in this programme. This comprehensive review of DNP projects is a critical process in striving for excellence in academic programming and ensuring fidelity to the DNP essentials in fostering advanced practice. We also consider that the recommendations based on this review have relevance for professional doctorates internationally.
In Table 4 , we provide additional recommendations for DNP programmes while conducting programme evaluation.
Recommendations for DNP programme evaluation
| Recommendation | Reasoning | Action Steps |
|---|---|---|
| DNP programmes should evaluate their DNP projects over multiple years | • Self-reflection is a critical component of quality improvement methodology to promote rigour ( ) • Evaluation over multiple years allows perspective on students' understanding of critical curriculum elements • Provides insight into extent faculty are experts in translational frameworks, designs and analyses | • Conduct programme evaluation as we have done here • Use implementation science ( ; ) as a framework to promote sustainability and impact of projects • Develop key performance indicators of programme success |
| Determine sustainability and impact of DNP projects | • Maintaining DNP project improvements in the organisational sites is imperative for sustaining impact | • Collaborate with clinical site mentors and graduates to determine if impact described in DNP report has been sustained after graduation • Enhance academic-practice collaboration by identifying DNP projects that are aligned with organisational needs and existing measures. This offers an enhanced and natural opportunity for sustainability and impact evaluation that continues after the studen’s project is completed. This approach supports hospitals pursuing or renewing Magnet designation; repeated measures are critical • Encourage the use of robust theoretical frameworks for practice change and implementation science |
| Provide guidance in the development, presentation and dissemination of DNP project | • Close mentorship and guidance during the development, implementation and reporting of students' DNP project is critical to student success | • Introduce writing workshops early in DNP programme and offer support for both analytical and writing skills and access to editorial support • Provide guidelines and template for construction and reporting of DNP projects • Encourage publication and dissemination |
| Follow-up with students after graduation to determine if they are continuing in leadership and process improvement roles | • Determine whether DNP programmes and their involvement in DNP projects has an impact on their career progression and involvement in process improvement | • Collaborate with graduates to determine their roles in leadership and process improvement in their work environment • Engage in a process of continual quality improvement in course design |
| Follow-up with students after graduation to determine the extent to which they have been productive in publishing work after their DNP project findings | • Dissemination of scholarly projects contributes best practice processes and outcomes which other sites and DNP students can replicate or build upon for future improvements | • Encourage faculty to assist students by taking a more substantive role in developing & submitting manuscripts from the DNP project • Develop contracts for dissemination of information |
6 |. CONCLUSION
Our review has found that process improvement, clinician development, patient safety, patient outcome improvement, access to care and workplace environment were a key focus of projects underscoring the relevance of the practice-focused degree. Ensuring graduates of clinical doctorates have the knowledge, skills and competencies for practice development is of critical importance. Ensuring that the capstone project demonstrates these attributes is essential for programme rigour.
7 |. RELEVANCE TO CLINICAL PRACTICE
DNP scholarly projects are a critical component of DNP curriculum in order to prepare nurses in advanced nursing practice to influence health care outcomes at the individual or population level. Therefore, evaluation of DNP scholarly projects is essential to improving DNP curriculum and ensuring DNP graduates are prepared to lead change in complex healthcare delivery systems. The findings from this descriptive study will provide insight to faculty at other schools with DNP programmes on ways to improve DNP projects that may lead to greater impact on clinical practice.
What does this paper contribute to the wider global clinical community?
- Outlines the importance of programme evaluation in professional doctorate programmes
- Profiles the challenges and opportunities for developing and refining a project aligned with delineated competencies
- Provides recommendations for achieving methodological rigour and programme efficiencies
Supplementary Material
S1 strobe statement checklist, appendix s2 dnp project template, acknowledgements.
The authors would like to acknowledge Denise Rucker, Academic Administrator for the DNP programme, for providing the DNP project report documents to review for this paper.
This study was supported in part by a grant from the Maryland Higher Education Commission (NSP II-17-107). RT is supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) of the National Institutes of Health under award number T32DK062707 and an award by the American Heart Association. ES is supported by the National Institute of Nursing Research of the National Institutes of Health under award numbers F31DR017328 and T32 NR012704.
Sponsors had no involvement in the study design; collection, analysis and interpretation of the data; in writing of the report; or in the decision to submit the article for publication.
SUPPORTING INFORMATION
Additional supporting information may be found online in the Supporting Information section.
Relevance to clinical practice: Programme evaluation is critical in order to sufficiently prepare nurses in advanced nursing practice to influence healthcare outcomes at the individual or population level.
CONFLICTS OF INTEREST
- American Association of Colleges of Nursing (2006). The essentials for doctoral education for advanced nursing practice . Retrieved from https://www.aacnnursing.org/Portals/42/Publications/DNPEssentials.pdf
- American Association of Colleges of Nursing (2015). The doctor of nursing practice: Current issues and clarifying recommendations: Report from the task force on the implementation of the DNP . Retrieved from https://www.aacnnursing.org/Portals/42/News/White-Papers/DNP-Implementation-TF-Report-8-15.pdf?ver=2017-10-18-151758-700
- American Association of Colleges of Nursing (2018). Defining scholarship for academic nursing: Task force consensus position statement . Retrieved from https://www.aacnnursing.org/Portals/42/News/Position-Statements/Defining-Scholarship.pdf
- Becker KD, Johnson S, Rucker D, & Finnell DS (2018). Dissemination of scholarship across eight cohorts of doctor of nursing practice students . Journal of Clinical Nursing , 27 ( 7–8 ), e1395–e1401. 10.1111/jocn.14237 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brewer N. (2011a, September 27). Observational research designs . Lecture conducted from the University of North Carolina at Chapel Hill. [ Google Scholar ]
- Brewer N. (2011b, November 2). True and Pre-Experimental Designs for Evaluation . Lecture conducted from the University of North Carolina at Chapel Hill. [ Google Scholar ]
- Brewer N. (2011c, November 8). Quasi-Experimental Study Designs . Lecture conducted from the University of North Carolina at Chapel Hill. [ Google Scholar ]
- Brown MA, & Crabtree K. (2013). The development of practice scholarship in DNP programs: A paradigm shift . Journal of Professional Nursing , 29 ( 6 ), 330–337. 10.1016/j.profnurs.2013.08.003 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Casey M, O’ Leary D, & Coghlan D. (2018). Unpacking action research and implementation science: Implications for nursing . Journal of Advanced Nursing , 74 ( 5 ), 1051–1058. 10.1111/jan.13494 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Centers for Disease Control and Prevention (2009). Program collaboration and service integration: Enhancing the prevention and control of HIV/AIDS, viral hepatitis, sexually transmitted diseases, and tuberculosis in the United States . Atlanta, GA: U.S. Department of Health and Human Services. Retrieved from https://www.cdc.gov/nchhstp/programintegration/docs/207181-c_nchhstp_pcsi-whitepaper-508c.pdf [ Google Scholar ]
- CFIR. Consolidated Framework for Implementation Research (2019).Retrieved from https://cfirguide.org/
- CGS (2006). Professional master’s education: A CGS guide to establishing programs . Washington, DC: CGS. [ Google Scholar ]
- Council of Graduate Schools in the United States. (2007). Task Force Report on the Professional Doctorate . Washington, DC: Council of Graduate Schools. [ Google Scholar ]
- Cygan HR, & Reed M. (2019). DNP and PhD scholarship: Making a case for collaboration . Journal of Professional Nursing , 35 ( 5 ), 353–357. 10.1016/j.profnurs.2019.03.002 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dang D, & Dearholt S. (2017). Johns Hopkins University nursing evidence-based practice: Model and guidelines (3rd ed.). Indianapolis, IN: Sigma Theta Tau International. [ Google Scholar ]
- Department of Education, Science, and Training (1997). Research-coursework Doctoral Programs in Australian Universities . Australia: Canberra: Australian Government Publishing Service. [ Google Scholar ]
- Dinapoli CM (2015). Improving continuous positive airway pressure adherence among adults . Journal of Nursing Education and Practice , 5 ( 2 ), 110. 10.5430/jnep.v5n2p110 [ CrossRef ] [ Google Scholar ]
- Dols JD, Hernandez C, & Miles H. (2017). The DNP project: Quandaries for nursing schools . Nursing Outlook , 65 ( 1 ), 84–93. 10.1016/j.outlook.2016.07.009 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Embree JL, Meek J, & Ebright P. (2018). Voices of chief nursing executives informing a doctor of nursing practice program . Journal of Professional Nursing , 34 ( 1 ), 12–15. 10.1016/j.profnurs.2017.07.008 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fulton J, Kuit J, Sanders G, & Smith P. (2012). The role of the professional doctorate in developing professional practice . Journal of Nursing Management , 20 ( 1 ), 130–139. 10.1111/j.1365-2834.2011.01345.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W, & Robinson N. (2006). Lost in knowledge translation: Time for a map? Journal of Continuing Education in the Health Professions , 26 ( 1 ), 13–24. 10.1002/chp.47 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Grove SK, Burns N, & Gray JR (eds.) (2013). Selecting a quantitative research design. In The practice of nursing research: Appraisal, synthesis, and generation of evidence (7th ed., pp. 214–263). St. Louis, MO: Elsevier Saunders. [ Google Scholar ]
- Howard PB, & Williams TE (2017). An academic-practice partnership to advance DNP education and practice . Journal of Professional Nursing , 33 ( 2 ), 86–94. 10.1016/j.profnurs.2016.08.010 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kane RL (1999). A new model of chronic care . Generations: Journal of the American Society on Aging , 23 ( 2 ), 35–37. [ Google Scholar ]
- Kim-Saechao SJ, Almario E, & Rubin ZA (2016). A novel infection prevention approach: Leveraging a mandatory electronic communication tool to decrease peripherally inserted central catheter infections, complications, and cost . American Journal of Infection Control , 44 ( 11 ), 1335–1345. 10.1016/j.ajic.2016.03.023 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kirkpatrick JM, & Weaver T. (2013). The doctor of nursing practice capstone project: Consensus or confusion? Journal of Nursing Education , 52 ( 8 ), 435–441. 10.3928/01484834-20130722-01 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Logan J, & Graham ID (1998). Toward a comprehensive interdisciplinary model of health care research use . Science Communication , 20 ( 2 ), 227–246. 10.1177/1075547098020002004 [ CrossRef ] [ Google Scholar ]
- Mellors-Bourne R, Robinson C, & Metcalfe J. (2016). Provision of professional doctorates in English HE Institutions . Cambridge: Careers Research and Advisory Centre. Retrieved from http://hdl.voced.edu.au/10707/393040 . [ Google Scholar ]
- Minnick AF, Kleinpell R, & Allison TL (2019). Reports of three organizations’ members about doctor of nursing practice project experiences and outcomes . Nursing Outlook , 67 ( 6 ), 671–679. 10.1016/j.outlook.2019.05.012 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Newton S, & Fralic M. (2015). Interhospital transfer center model: Components, themes, and design elements . Air Medical Journal , 34 ( 4 ), 207–212. 10.1016/j.amj.2015.03.008 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, & Stevens D. (2016). SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): Revised publication guidelines from a detailed consensus process . BMJ: Quality and Safety , 25 ( 12 ), 986–992. 10.1136/bmjqs-2015-004480 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pettigrew A, & Whipp R. (1992). Managing change and corporate performance. In Cool K, Neven DJ, & Walter I. (Eds.), European industrial restructuring in the 1990s (pp. 200–227). Houndmills, Basingstoke, Hampshire: Macmillan Academic and Professional. [ Google Scholar ]
- Rogers EM (1962). Diffusion of innovations (1st ed.). New York, NY: Free Press. [ Google Scholar ]
- Roush K, & Tesoro M. (2018). An examination of the rigor and value of final scholarly projects completed by DNP nursing students . Journal of Professional Nursing , 34 ( 6 ), 437–443. 10.1016/j.profnurs.2018.03.003 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sigma Theta Tau (n.d.). Sigma Theta Tau Virginia Henderson Repository .Retrieved from https://www.sigmarepository.org/ .
- Singleton RA Jr, & Straits BC (2010). Approaches to social research (5th ed.). New York, NY: Oxford University Press. [ Google Scholar ]
- Southard EP, Neufeld JD, & Laws S. (2014). Telemental health evaluations enhance access and efficiency in a critical access hospital emergency department . Telemedicine and e-Health , 20 ( 7 ), 664–668. 10.1089/tmj.2013.0257 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sullivan NJ, Duval-Arnould J, Twilley M, Smith SP, Aksamit D, Boone-Guercio P, … Hunt EA (2015). Simulation exercise to improve retention of cardiopulmonary resuscitation priorities for in-hospital cardiac arrests: A randomized controlled trial . Resuscitation , 86 , 6–13. 10.1016/j.resuscitation.2014.10.021 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sun GH, & Cherry B. (2019). Using the logic model framework to standardize quality and rigor in the DNP project . Nurse Educator , 44 ( 4 ), 183–186. 10.1097/NNE.0000000000000599 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Terhaar M, & Sylvia M. (2015). Scholarly work products of the doctor of nursing practice: One approach to evaluating scholarship, rigor and impact on quality . Journal of Clinical Nursing , 25 , 163–174. 10.1111/jocn.13113 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Waldrop J, Caruso D, Fuchs MA, & Hypes K. (2014). EC as PIE: Five criteria for executing a successful DNP final project . Journal of Professional Nursing , 30 ( 4 ), 300–306. 10.1016/j.profnurs.2014.01.003 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yam BM (2005). Professional doctorate and professional nursing practice . Nurse Education Today , 25 ( 7 ), 564–572. [ PubMed ] [ Google Scholar ]
- Younan LA, & Fralic MF (2013). Using “best-fit” interventions to improve the nursing intershift handoff process at a medical center in Lebanon . The Joint Commission Journal on Quality and Patient Safety , 39 ( 10 ), 460–467. 10.1016/S1553-7250(13)39059-X. [ PubMed ] [ CrossRef ] [ Google Scholar ]
Your web browser is out of date. Please, upgrade to Edge or another supported browser .

A Nurse's Step-By-Step Guide to Publishing a Dissertation or DNP Project
Early praise for a nurse's step-by-step guide to publishing a dissertation or dnp project :.
“The book breaks down the complexities of scholarly writing and provides key insight and vital guidance for publishing dissertations or DNP projects. A Nurse’s Step-By-Step Guide to Publishing a Dissertation or DNP Project will have a permanent place on my bookshelf and will be shared with new graduates and colleagues alike .”
— Nancy White Street, ScD, PPCNP-BC Julia and Harold Plotnick Professor of Global Nursing University of Massachusetts Dartmouth College of Nursing
“Karen Roush’s earlier book on writing a dissertation or scholarly project has become the ‘go-to’ resource for scores of doctoral students. In her new book, Roush has again demonstrated her unique knack for simplifying a process—the often-arduous steps necessary for turning a dissertation or capstone project into a manuscript worthy of publication. A must-read primer for anyone wanting to publish.”
— Wend y Budin, PhD, RN-BC, FAAN Professor & Associate Dean Entry to Baccalaureate Practice Division Editor-in-Chief, Journal of Perinatal Education Rutgers, The State University of New Jersey School of Nursing
INDIANAPOLIS — Creating a dissertation or academic project is a demanding and complicated process, presenting a unique set of challenges for authors. Navigating the publishing process presents further challenges. Creating the best article and finding the most appropriate journals often leaves first-time authors frustrated and intimidated.
In A Nurse’s Step-By-Step Guide to Publishing a Dissertation or DNP Project , award-winning author Karen Roush guides readers through the process of reworking a dissertation or DNP project into a high-quality manuscript and honing their writing skills. Roush then provides a step-by-step guide through the publication process, providing all the information necessary to fully understand and navigate the world of academic publishing.
“The full breadth and depth of nurses’ contributions are still not recognized by the healthcare community and the general public,” said Roush. “Publication is a powerful means of strengthening the voice of nursing and influencing how care is delivered.”
The author has also created material downloads, such as a Submission Checklist and a Top 10 Guide to Publishing, to support the use of this book in classroom and professional settings. These downloads are available for free at http://hdl.handle.net/10755/17097 .
This book is available at SigmaMarketplace.org/sigmabooks .
A Nurse’s Step-By-Step Guide to Publishing a Dissertation or DNP Project: Taking Your Paper From Graduation to Publication By Karen Roush, PhD, RN, FNP-BC Published by Sigma, 2019 ISBN-13: 9781948057370 EPUB ISBN: 9781948057387 PDF ISBN: 9781948057394 MOBI ISBN: 9781948057400 Price: US $39.95 Trade paperback, 208 pages Trim size: 5 3/8 x 8 3/8
About the author: Karen Roush, PhD, RN, FNP-BC, is founder of The Scholar’s Voice, which works to strengthen the voice of nursing through writing mentorship for nurses. A previous Editorial Director and Clinical Managing Editor for American Journal of Nursing, Roush is widely published, having authored multiple consumer healthcare books, nursing articles in peer-reviewed journals, essays, and poetry. She is also adjunct faculty at Pace University and The Graduate Center for the City University of New York.
About Sigma: The Sigma Theta Tau International Honor Society of Nursing (Sigma) is a nonprofit organization whose mission is advancing world health and celebrating nursing excellence in scholarship, leadership, and service. Founded in 1922, Sigma has more than 135,000 active members in over 100 countries and territories. Members include practicing nurses, instructors, researchers, policymakers, entrepreneurs, and others. Sigma’s more than 540 chapters are located at more than 700 institutions of higher education throughout Armenia, Australia, Botswana, Brazil, Canada, Colombia, England, Eswatini, Ghana, Hong Kong, Ireland, Israel, Jamaica, Japan, Jordan, Kenya, Lebanon, Malawi, Mexico, the Netherlands, Nigeria, Pakistan, Philippines, Portugal, Puerto Rico, Scotland, Singapore, South Africa, South Korea, Sweden, Taiwan, Tanzania, Thailand, the United States, and Wales.
Learn more at www.SigmaNursing.org .
Connect & Engage

This site uses cookies to keep track of your information. Learn more here . Accept and close .
We've made changes to our Privacy Policy to update how we work with international data and how we disclose your personal and non-personal data. Your continued use of this site represents your consent to these changes and to the site's use of cookies to monitor website traffic. Close

Guidelines for Theses, Dissertations, and DNP Projects
Introduction, requirements by program, recommended resources, find usu theses, dissertations, and dnp projects.
- Basic Style Guide
- Templates and Videos
- Further Assistance
Contact the LRC
Submit a Question
Browse Our FAQs
Email: [email protected]
Telephone: (301) 295-3350
Visit our online tutorial for assistance in navigating the USU Archives Digital Repository
This guide provides resources for USU students preparing their theses, dissertations, or DNP projects. Specific questions regarding requirements and formatting should be addressed by the individual school/college.
Graduate Education in Biomedical Sciences and Public Health (GEO)
- Graduate Education (GEO) Homepage
- USU GEO Thesis and Dissertation Guidelines (2022-2023)
Center for Health Professions Education (CHPE)
- CHPE Program and Course Requirements
- CHPE Graduate Learner Handbook 2022-2023
Submission Instructions for SOM/GEO
Before you submit your paper, please ensure that it includes:
- One PDF which combines: Final draft of paper + Digitally signed approval sheets + USU disclosure statement in one PDF
- No Personally Identifiable Information/PII (examples: SSN, date of birth, home address, personal phone numbers, or CVs/biographies)
- No Track Changes
- No PDF Portfolios
Once you have successfully defended your paper, the GEO/SOM office will submit it to the following workflow for clearance by VPE and submission to the USU Archives:
- USU Publications/Presentation ServiceNow Workflow
After submission, your paper will be routed for approval as follows:
- Department Head
- External Affairs for clearance (submitter receives a clearance approval email at this step)
- USU Archives
Final Step:
- USU Archives will upload the paper to the digital repository .
- USU Archives will collect all submissions and send them to DTIC annually.
- GSN Student Resources
- DNP and MSN Student Handbook
Submission Instructions for GSN
Once you have successfully defended your paper, the GSN office will submit it to the following workflow for clearance by VPE and submission to the USU Archives:
- PDC Research Guidelines and Requirements
Submission Instructions for PDC
Once you have successfully defended your paper, the PDC office will submit it to the following workflow for clearance by VPE and submission to the USU Archives:
- Copyright and Fair Use
- Avoiding Plagiarism
- Writing Guides
The USU Archives maintains an online collection of USU theses, dissertations, and DNP projects. The collection includes USU theses and dissertations from 1981, when the University began granting graduate degrees, through today. The collection includes over 150 theses and dissertations from the Graduate School of Nursing and over 500 from the School of Medicine. Also included are theses from the USU Postgraduate Dental College, which was established in 2010. As theses and dissertations are completed each year, the Archives adds those documents to the online collection.
Additionally, the collection includes Doctor of Nursing Practice (DNP) projects from the Daniel K. Inouye Graduate School of Nursing. These projects demonstrate the graduate's ability to evaluate and apply evidence to improve health and healthcare system outcomes. These original, innovative projects have informed clinical decisions, generated new policies and simulated process or practice changes, with the goal of improving care outcomes by increasing safety and effectiveness in the highly complex Military and Federal Healthcare Systems.
The views presented here are those of the author and are not to be construed as official or reflecting the views of the Uniformed Services University of the Health Sciences, the Department of Defense or the U.S. Government.
Search or Browse the Collection
- Next: Basic Style Guide >>
- Last Updated: Feb 23, 2024 9:09 AM
- URL: https://usuhs.libguides.com/thesisdissertationguidelines

DNP project guide: Designing your DNP project
- Support services
- Designing your DNP project
- Formatting tips
- Copyrighting
- Submitting to the SU Libraries
- Submitting to SOAR@SU
- Submitting to ProQuest
- Archiving in the Henderson Repository
DNP project design
- A Nurse's Step-By-Step Guide to Writing Your Dissertation or Capstone by Karen Roush Call Number: Available online Publication Date: 2015
- DNP capstone projects : exemplars of excellence in practice by Barbara A Anderson; Joyce M Knestrick; Rebeca Barroso Call Number: Available online Publication Date: 2015
- Inquiry and leadership : a resource for the DNP project by Kathleen Reavy Call Number: Available online Publication Date: 2016
- Proposal Writing for Nursing Capstones and Clinical Projects (2nd edition) by Wanda Dr PhD RN Bonnel; Katharine Dr PhD RN Smith Call Number: Available online Publication Date: 2017
- The doctor of nursing practice scholarly project : a framework for success by Katherine J Moran; Rosanne Burson; Dianne Conrad Call Number: RT75 .D57 2014 Publication Date: 2014
- The doctor of nursing practice scholarly project : a framework for success (2nd edition) by Katherine J Moran; Rosanne Burson; Dianne Conrad Call Number: On order for SU Libraries Publication Date: 2017
Sample DNP projects
- The Virginia Henderson Global Nursing e-Repository (Henderson Repository) A resource of the honor society of nursing, Sigma Theta Tau International and the only digital repository solely dedicated to openly sharing works created by nurses. Includes full-text nursing research and evidence-based practice materials.
- ProQuest Dissertations and Theses Open ProQuest's open access repository with over 200 DNP projects available in full text
- ProQuest Dissertations and Theses Global This link opens in a new window Provides access to digital dissertations, theses, and DNP projects worldwide
- DNP Final Document Projects From Ohio State University's institutional repository Knowledge Bank
- Nursing Commons Part of the Digital Commons Network. Includes a collection of DNP projects. From the menu on the left hand side, select Other Refinements - Publication - DNP Projects.
- Doctoral project repository From Doctors of Nursing Practice, Inc.
- << Previous: Support services
- Next: Formatting >>
- Last Updated: Sep 8, 2022 1:45 PM
- URL: https://libraryguides.salisbury.edu/DNPprojects
Outstanding PhD Dissertations and DNP Project Awards
AACN created this awards program to recognize and showcase outstanding dissertations and DNP projects completed by students in research- and practice-focused doctoral programs. Many doctoral students are advancing ground-breaking research and practice innovations that are worthy of national recognition and could serve as exemplars for other students to emulate.
Two awards will be presented each year, with one award presented in each of the following categories:
Excellence in Advancing Nursing Science Award for an outstanding dissertation from a student in a PhD in nursing (or DNS program). A dissertation is an original research project that focuses on advancing nursing science and developing new evidence with the potential to guide nursing practice. To apply, please fill out the online application .
Download PhD Nomination Information
Excellence in Advancing Nursing Practice Award for an outstanding final project from a student in a Doctor of Nursing Practice (DNP) program. A DNP project demonstrates high-level mastery of an area of advanced nursing practice and focuses on the translation of evidence into practice. To apply, please fill out the online application .
Download DNP Nomination Information
Nominations for these awards are due June 7, 2024.
Selection of Award Winners
A selection committee will review all complete nominations received and select award finalists. This committee reserves the right to decide not to recommend an award in any given year. Award finalists must be approved by the AACN Board of Directors.
Submission Process
Excellence in Advancing Nursing Science Award
Call for applications for this award is now open. To apply, please fill out the online application . The deadline is June 7, 2024.
Excellence in Advancing Nursing Practice Award
Award Presentation & Promotion
- The doctoral student/graduate receiving an award must attend AACN’s Doctoral Education Conference . The conference registration fee for the winners will be waived.
- The award will be presented by the AACN Chair at the start of conference.
- Award winners will present their abstracts on the second day of the Doctoral Education Conference.
- The award includes a “symbol” of appreciation and a $1,000 check. Winners will be announced via AACN publications and on its Website.
Past Award Recipients
2023 winners.

Background and Significance: Up to a million or more Americans live while traveling full-time in recreational vehicles (RVs). Many health policies are based on assumptions of stationary residency. Little study has been devoted to the healthcare experiences of Americans who are geographically mobile.
Purpose/Objective(s) and/or Specific Aims: The purpose of this study was to explore the experiences of RV-dwelling full-time American nomads when seeking healthcare in the U.S. and to identify barriers and facilitators of access to care. Levesque’s Conceptual Model of Access to Healthcare was used to generate questions for the interview guide. The principal investigator lived in an RV and traveled to a variety of campgrounds in several states to post recruitment flyers.
Methods: The exploratory, qualitative design was informed by interpretive description. Interviews were recorded and transcribed verbatim. Thematic analysis was conducted with a phronetic iterative approach using Atlas.ti software.
Results/Findings: Participants included American adults who lived for more than six months of the year in an RV while traveling to different regions of the U.S. Participants were located in a variety of campgrounds in several states including Oregon, Wyoming, Colorado, New Mexico, Texas, and Arizona. Twenty-five RV-dwelling nomads participated in semi-structured interviews. Three overarching themes described the experiences of RVers: overwhelming logistics, don’t need healthcare, and orchestrating a web of care. Some of the barriers identified included difficulty vetting healthcare resources in unfamiliar locations, caregivers’ lack of understanding of the nomadic lifestyle, limited resources in rural areas, and rules limiting care and payment for care by state. Some of the facilitators identified included caregiver collaboration, telehealth, national chains with shared records, information and support from other RVers, and self-advocacy.
Conclusion(s): RV-dwelling nomads are an understudied population that face complexity and barriers to healthcare access related to seeking care in unfamiliar locations, misunderstandings about their lifestyle, and policies that prevent the portability of healthcare across state lines.
 (1).jpg?ver=6RlDLFJUhm50FHhxALCnWg%3d%3d)
Background and Problem Statement: Adolescent mental health disorders are a growing public health issue globally. Though symptoms of mental health disorders were worsening before COVID-19, the pandemic exacerbated this crisis. Because adolescents spend most of their time in school, interventions focusing on mental health education and skill-building, reducing stigma, and increasing helping-seeking behaviors should be prioritized here. In a suburban Arizona school district, high school social workers and counselors are seeing increased social and emotional referrals and are looking for solutions. In 2021, the state of Arizona passed SB1376, mandating mental health education in public schools.
Purpose/Objective(s): This project aimed to evaluate the effectiveness of tMHFA (teen Mental Health First Aid) on high school students’ mental health literacy (MHL), mental health first-aid skills, and stigma perception. The project also qualitatively evaluated students’ opinions of tMHFA education and instruction. The implementation design included a phase two expansion and program sustainability by stakeholders within the existing district curriculum.
Procedures: Partnering with a large urban school district’s social work department, a teen Mental Health First Aid (tMHFA) pilot program was developed. Using the Iowa Model of Evidence-Based Practice (IMEBP) as a guide, the organizational priorities of teen mental health provided the trigger specific to this pilot project implementation. This model is fitting for working with a large public school organization and promoted expansion in the sustainability plan. tMHFA is a classroom-based mental health literacy and skill-building program for students aged 15-18 to promote mental health literacy, help-seeking behaviors, and attempts to reduce stigma while teaching adolescents to help a peer or friend through a mental health crisis. A "train the trainer" program was developed with key stakeholders (school district social workers) and the initial pilot project included eleventh-grade students who received three 90-minute classroom workshop sessions. The district chose one high school within the system for the pilot and provided class instruction time for the intervention. Parental consent and student assent were required to participate. tMHFA was delivered in three 90-minute classes on non-consecutive days. The initial pilot group included a class of nine (n = 9) adolescent students aged 17-18 years old. Using the Mental Health Literacy questionnaire (MHLq), a pre and post-test design was used to evaluate the program quantitatively and qualitatively. Descriptive statistics, two-tailed paired samples t-test, Shapiro-Wilk, and qualitative data were collected by student participants and project stakeholders.
Outcomes: Using the Mental Health Literacy questionnaire (MHLq), a pre and post-test design revealed a significant increase in the students’ mental health literacy, help-seeking behaviors, and decreased stigma (p<0.05). Students reported overall positive experiences based on a subjective question at the end of the survey. One student wrote, “I think all students should get a class like this.” Project stakeholders will continue the tMHFA using project trained staff who are school district employed social workers to offer the program to all eleventh grade students in the project school. The district plans to expand the program to three additional schools in the next academic school year. The tMHFA is now integrated into the district curriculum.
Conclusion(s): This pilot project using tMHFA significantly improved mental health literacy, mental health first-aid, and stigma perception. Students enjoyed and valued the programming, which is crucial when providing education to teenagers. The Iowa Model of Evidence-Based Practice provided implementation support to engage stakeholders, start the project with a small pilot, and develop a plan for expansion district-wide. After the original nine-student pilot, the district expanded to all junior-level students in one high school (800 students). It is now planning to deliver tMHFA to 2400 junior-level students in three of its high schools.
Background and Problem Statement: Unanticipated and adverse events are inevitable in healthcare. Second victim phenomenon (SVP), which happens when a clinician experiences personal or professional negative effects after a clinical event, can impact the psychological and physical health of the clinician and compromise subsequent care. One in five UTMB Department of Anesthesiology clinicians surveyed reported experiencing an emotionally distressing clinical event in the preceding 30 days. An alarming 88% knew of a colleague emotionally affected by a work event; only 20% felt these individuals had been adequately supported. Prior to the DNP project, no formal process was in place to facilitate peer support.
Purpose/Objective(s): This project served to implement evidence-informed strategies for emotional peer support and foster clinician resilience within the department of anesthesiology. A needs assessment survey indicated that over 90% of clinicians would likely look to a trusted colleague for support after an emotionally challenging clinical event. The project aim was that at least five UTMB Health Anesthesiology clinicians would participate in the emotional peer support process each week between September 26 – December 19, 2022.
Procedures: A diverse group of peer-nominated clinicians, led by the DNP project coordinator, completed specialized training to learn formal peer support. The pilot team, forU Peer Support, comprised all levels of anesthesia professionals, including physicians, APRNs, and residents. Trained peer supporters (TPS) collected de-identified information from interactions, including the precipitating event, provider type, and satisfaction. Encounter forms included an area for open-ended feedback for ideas to help improve the process, such as adding a badge-buddy with additional identification and tips. The department webmaster and project lead collaborated to add a Peer Support Resource hub to the intranet. Resources, including SVP awareness, coping strategies, emotional first-aid tips, a team roster, and professional mental health services contacts, were made available for 24-7 access. The project was promoted via multiple channels including grand rounds, email communications, and the use of branded badges and brochures. The proactive process included a standardized outreach email from forU to any provider involved with an internal morbidity and mortality (M&M) report. Data were collected and analyzed using a multi-pronged approach via surveys, training evaluations, website analytics, and encounter forms. The project coordinator followed encounter forms and monitored participation using a run chart which included the frequency of encounters and intranet resource access. The continuous quality improvement process utilized a rapid cycle Plan-Do-Study-Act (PDSA) approach to determine whether changes and additional interventions were necessary to achieve the project aim.
Outcomes: Fifteen percent of anesthesia providers at UTMB Health completed the formal training and continue to serve as support champions. Over three months, supporters recorded 33 encounters, with an average satisfaction rate of 4.76/5 stars. The intranet site, intended to destigmatize mental health resources and normalize SVP, was accessed over 100 times with high ratings. Before implementation, only 21% of clinicians agreed that adequate and timely emotional peer support resources were available, and post-implementation agreement increased to 77%. Many incidents warranting support were related to patient care and adverse events, but some were related to individual issues, such as work-life balance and workplace bullying. Survey results showed that awareness of the term second victim (advocated as the primary intervention in mitigating its negative effects) doubled. The project continues to have a strong team champion presence, with 25 clinicians being trained and identifiable by branded badges in the clinical setting.
Conclusion(s): This DNP-driven project was a leap forward in safeguarding clinician well-being and efforts have shown to be impactful and meaningful to clinicians. The project was collaborative and inclusive and used translational methods to improve outcomes for the healthcare team and enhance patient safety. While the incidence of challenging clinical events remain constant, the forU program models strategies to encourage substantial improvements in levels of perceived support. A thriving workforce is a necessary prerequisite to advancing patient safety and care, and the forU program helps ensure a culture of care that puts workforce well-being as a high priority.
2022 Winners

Background and Significance: Postoperative pulmonary complications (PPCs) are associated with high rates of mortality and morbidity, intensive care admission, hospital length of stay, and resource utilization. PPCs are attributable to both modifiable and non-modifiable risk factors associated with characteristics of patients, surgery, and anesthesia. Although many PPC risks are not modifiable, intraoperative ventilation parameters can be adjusted to reduce risk. Lung protective ventilation (LPV) has been adapted for intraoperative use to protect pulmonary parenchyma against ventilator-induced lung injury (VILI). Questions remain regarding “how”, “when”, and for “whom” LPV can be used to minimize VILI leading to PPCs.
Purpose/Objective(s) and/or Specific Aims: The overarching goal of the dissertation was to identify personalized care strategies that optimize ventilation parameters in order to reduce PPCs for adult patients undergoing a non-cardiothoracic non-obstetric surgery with general anesthesia and mechanical ventilation. The specific aims were to identify: (Aim 1) phenotypes based on preoperative patient and surgical nonmodifiable risk factors to understand the risk of PPC; and (Aim 2) optimal intraoperative ventilator parameters associated with the most desirable outcome for each phenotype.
Methods: A retrospective cohort observational study leveraging electronic health records (EHRs) was conducted. The study included 34,910 adult surgical patients (≥ 18 years of age) who underwent general anesthesia with mechanical ventilation for non-cardiothoracic non-obstetric procedures between 1/1/2018 and 8/31/2019 at a health system in the Southeast of the United States. The PPC outcome in this study was composed of two properties: PPC diagnosis and postoperative respiratory status (PRS) severity. The International Classification of Disease, Tenth Revision diagnosis codes (e.g., acute respiratory distress syndrome, pneumonia) were used to identify patients who developed PPCs. PRS severity was rated by the level of postoperative requirement for supplemental oxygen and ventilatory support.
For Aim 1, the least absolute shrinkage and selection operator (LASSO) regression was first employed to select variables. Then, the classification and regression tree (CART) was conducted for PPC diagnosis and PRS severity to identify phenotypes. For Aim 2, the stratified logistic regression of PPC diagnosis and multinomial logistic regressions of PRS severity with stepwise selection and forced inclusion of tidal volume (VT) and positive end expiratory pressure (PEEP) were performed within each phenotype. The area under the receiver operating characteristic curve was computed to identify the optimal values of VT and PEEP.
Results/Findings: CART identified 14 subgroups for PPC diagnosis (Phenotype 0 though 6) and PRS severity (Phenotype A thought G). The optimal PEEP and VT values ranged from 4 to 12 cmH2O and from 5.98 to 9.39 ml/kg predicted body weight across phenotypes, respectively. The parameters for Phenotype 0, which associated with the lowest PPC incidence (3.9%), 6.25 ml/kg and 5 cmH2O. Phenotype 5 had the highest likelihood of developing PPCs (71.4%), and their optimal parameters were 7.35 ml/kg and 5 cmH2O. Phenotypes A and C had the highest likelihood of having the most severe PRS level; the optimal parameters for Phenotype A were identified as 7.44 ml/kg and 6 cmH2O, and those for Phenotype C were 7.73 ml/kg and 6 cmH2O. In contrast, Phenotype E was associated with the lowest likelihood (3.3%) of having the most severe PRS, and the optimal parameters were 5.98 ml/kg and PEEP of 8 cmH2O.
Conclusion(s): This dissertation was the first to use CART to classify phenotypic subgroups based on risks for PPCs and classified the adult surgical patients into 14 phenotypes based on non-modifiable preoperative risks. The intraoperative mechanical ventilator parameters should be adjusted based on a patient phenotype to optimize the postoperative outcomes. This dissertation (a) offered a foundation for individualized care to optimize patients’ outcomes, and (b) identified several directions for future research to advance our understanding of care individualization aimed at reducing incidence of PPCs and alleviating PRS severity.

Background and Problem Statement: Patients older than age 65 seeking UCSF Health Emergency Department (ED) services represent 32-34% of total visits, contrasting the 20% national average. Published return to care data in this population (recidivism) at 30 days accounts for 6-28% of visits. Addressing medication management challenges, in real-time, can impact self-efficacy and recidivism during ED medication reconciliation thus improving the patient experience. Contributing to the challenge was 50% of older adults reporting medication non-adherence. As part of the institutional motivation California state law SB1254 required hospitals to complete medication reconciliation for all high-risk patients at any point in the continuum of care. The emergency department, as portal of entry to the health system, was a logical starting point. Published patient awareness of their plan of care, after discharge, across 4 domains varies from 24-64%.
Purpose/Objective(s): The aim of the project was to determine the impact of a structured medication reconciliation workflow on older adult medication self-efficacy as the primary outcome. As secondary outcomes, recidivism, and awareness of plan of care in the Emergency Department were also examined during data collection for a concordant period. As part of an evidenced-based study there is value in collecting qualitative data regarding interprofessional stakeholder experience. Post study lessons-learned was an opportunity for professional participants to share their insights.
Procedures: Following a pilot of the Medication Management Deficiencies in the Elderly (MedMalDE) a modified version was utilized during medication reconciliation. This was a convenience sample of 21 older adult patients assessed over four contiguous weeks in an academic 35-bed emergency department (ED) with 10 additional observation beds. Concurrently the Self-Efficacy for Appropriate Medication Use (SEAMS) confidence survey instrument was used as the outcome instrument applied prior to medication history or reconciliation in coordination with the pharmacy technicians. Additionally, 164 patients were assessed with only the MedMalDE over the same period without self-efficacy measurement due to a variety of factors. All patients were age 65 or older and primarily responsible for their medication management in this pre- and post- design. Primary language was not a barrier with video translation services at the bedside. Reconciliation interventions occurred at the index ED visit and the SEAMS was repeated via telephone at seven to fourteen days following their return to home whether discharged from the ED or post-hospitalization. A secondary outcome measure included a survey of 56 patient’s awareness of ED plan of care collected concurrently and during a pre-intervention period for comparison. Aggregate 30-day recidivism for study patients was another secondary outcome. It was assessed at 39 days prior to, during, and after the pre/post intervention to match the SEAMS four-week data collection and 7–14-day follow-up periods. Descriptive, Wilcoxon Signed Rank, and Mann-Whitney U Tests were used for statistical analysis where appropriate.
Outcomes: Descriptive statistics revealed patient demographics were similar for intervention and aggregate ED patients. Mean SEAMS scores were significantly improved following MedMalDE guided interventions using the Wilcoxon Signed Rank Test (Z=-2.6989, p=.0077). 30-day ED recidivism for intervention patients was 9.5% versus aggregate patients at 12.3% but not significantly different using Mann Whitney U. The qualitative data from 7-14-day SEAMS follow-up highlight the continued gaps in health system support for the post-discharge experience. The thematic qualitative findings from interviewing the Department of Pharmacy professionals highlighted their satisfaction with improvement study, insights into common medication self-management challenges, and value of caregiver participation.
Conclusion(s): A structured medication reconciliation for older adult ED patients can be incorporated in standard pharmacy workflows, identify common medication challenges addressed in real time, and improve self-efficacy. The qualitative findings collected during the post SEAMS telephone follow-up revealed the lack of uniformity of post-discharge problem-solving with patients and caregivers despite existing professional discharge support. Health systems need to adopt best practices to mitigate health care return to care by addressing gaps in the plan of care communication, assessment of functional, access, and knowledge deficits in medication management, and ensure patient discharge transitions are better supported.
2021 Winners
Raymond Romano, III, PhD University of Tennessee Health Science Center Early Diagnosis of Alzheimer's Disease in the Primary Care Setting Program Director - Carolyn Graff

Purpose/Objective(s) and/or Specific Aims: The overall aims of this program of research were to understand factors contributing to AD diagnosis variability in primary care practice settings and to find ways to improve early AD diagnosis by primary care providers. Four projects were undertaken to meet the aims and each resulted in a published manuscript.
Methods: Four studies were undertaken to achieve the aims. The first study reported the results of an integrated review estimating the prevalence of missed diagnosis in primary care when compared to trained raters’ diagnoses. The findings call to attention the difficulty primary care providers face to detect and diagnose AD at all levels of the healthcare system.
In order to understand the pain experience in those with worsening cognition, the second study was a secondary analysis of a cross-sectional age- and sex-matched two group cohort study and found that the experience of pain differs between males and females as a measure of cognition worsened suggesting a possible role of pain as a tool to distinguish those at risk for AD.
This finding led to the third study, which was a narrative review conducted to describe how alterations in senses have been associated with the diagnosis of AD. The results suggested differences in smell, taste, vision, hearing, and proprioception were associated with different levels of the AD continuum but points out an obvious gap in the literature concerning other senses. This led to the fourth study examining evidence that the e4 allele of Apolipoprotein E modifies the experience of pain in those individuals carrying the allele such that greater temperatures are required to elicit pain and the experience of that pain is more unpleasant.
Results/Findings: The first published manuscript, an integrative review, highlights the complexity of barriers that exist at each level of the health care system contributing to limit diagnoses of AD by PCPs. One study suggested that the complexity of the patients’ presenting problems makes it difficult to diagnose AD. The results of the second study demonstrate that the experience of pain, a common comorbidity seen in AD, differs between males and females as a measure of cognition worsens suggesting pain may be a useful marker of AD. The third study, a narrative review demonstrates differences in senses have been associated with the different diagnostic categories of AD.The fourth study found individuals at increased risk of AD experience pain based on their APOE4 status at a greater temperature and found that pain was more unpleasant when compared to those without the increased risk of AD.
Conclusion(s): The search to identify non invasive preclinical markers of AD would allow for earlier interventions and the potential use of disease modifying medications once approved in the primary care setting. Older adults and their loved ones often seek care from their primary care providers with initial concerns for memory. However, primary care providers’ diagnostic accuracy is poor and it takes about 17 years for research to catch up to in clinical practice (“2020 Alzheimer’s disease facts and figures” 2020). The evidence of this research suggests pain as a possible early marker of AD.
Bridget A. Chandler, DNP University of Washington Case Study: Seattle Public Schools' (SPS) 2019-20 Immunization Campaign to Protect Health and Prevent School Exclusion Program Director - Tatiana Sadak

Purpose/Objective(s):
- Develop and disseminate a nurse survey on use frequency and effectiveness of campaign tools, capture nurse expert opinion, and glean insight for improvements.
- Characterize nurse ratings of tools and strategies, summarize observations of campaign and risk factors for non-adherence, and summarize insights for improvement.
- Create a demographic and immunization database for two years following state vaccine law implementation.
- Analyze student data, using descriptive statistics and tests for differences.
- Characterize differences in non-adherence compared to all students and describe traits that may predispose students to non-adherence.
- Recommend improvements to protect health and prevent school exclusion.
- Disseminate findings to support vaccination efforts.
Procedures: The Knowledge To Action and Phenomenological frameworks guided evaluation of the SPS 2019-20 immunization campaign. Since this campaign was conducted primarily by school nurses as end-users, their voices are needed to improve ongoing immunization efforts. The Phenomenological framework guided the search for nurses’ meaning about the campaign. Project objectives were met through the following process:
- Problem Identification: Impetus was SPS’ desire to evaluate the immunization compliance campaign, seek nurses’ wisdom, analyze non-adherent cohorts for inequity-driven barriers, inform future SPS improvements, and share findings with the broader community.
- Reviewed literature and studied 17 articles and RCTs
- Catalogued tools and strategies used in the SPS campaign
- Created Excel database of de-identified SPS demographic and Washington State Immunization Information System (WAIIS) immunization data for all non-adherent students
- Sought guidance and expert opinion from local, state, and national vaccine experts
- Surveyed SPS nurses about tool use/effectiveness and observed risk factors for non-adherence. Open narrative option captured anything nurses wished to convey.
- Analyzed and characterized qualitative nurse survey data with REDCap
- District-wide data were compared with non-adherent student data before and after 2019 laws.
- Data: gender, grade, ethnicity, primary/home language, birth country, English language learner, disability, advanced learner, Running Start, foster, homeless, immigrant, equity tier, and adherence for DTaP, Tdap, Polio, HepB, MMR, and Varicella.
- Created and disseminated communication tools collaboratively with SPS
Outcomes: School Nurse Survey (60% response rate): Most frequent strategies: nurse outreach (families, students, providers). Most effective strategies: Head Start collaboration, conversations with families, Instructional Assistant outreach. Risk factors for non-adherence: family beliefs, low/high incomes, non-English home language, person of color, immigrant, homeless, distrusting health care. Non-adherence often result of barriers to access.
Student Data: Non-adherence decreased across time for all groups. Traits significant for non-adherence: Grade Level, immigrant, English Language Learner, Homeless, Ethnicity, Primary/home language, Equity Tier. Hispanic, African American/Black, and Native Hawaiian/Pacific Islander students not coming into adherence as quickly as White, Asian, Multiracial, and Alaska Native/Native American peers.
Conclusion(s): Practice inquiry shows nurses employed evidence-based practices to reach 97% immunization adherence. A variety of tools were used in a strategy of tailored outreach with increased intensity to prevent school exclusion. Nurse perceptions of risk factors for non-adherence were supported by data. Nurses express concern that enforcing laws requiring adherence to remain in school may have damaged relationships with students and families. Data support that many non-adherent students come from communities with historic and current experiences justifying distrust in health care systems. Non-adherence may be more a result of barriers to access than negative beliefs about vaccines.
2020 Winners

Jewel Scott, PhD, MSN Duke University Social Contributors to the Cardiovascular Health of Young Adult Black Females Program Director - Sharron Docherty
Background and Significance: Black females experience disparate rates of hypertension and earlier decline in cardiovascular health (CVH) than other females in the U.S. Most research on CVH in Black women has focused on deficit models of middle and older adults’ CVH behaviors as compared to women from other racial/ethnic groups. This approach has significantly limited our understanding of lifelong social exposures on Black women’s CVH. Importantly, few studies have examined how early life stress and social adversity contribute to premature decline in CVH, strengths that buffer against them, or within-group variations in exposures and outcomes to contextualize Black women’s CVH to mitigate disparities.
Purpose/Objective(s) and/or Specific Aims: The purpose of this dissertation was to fill a critical gap in Black women’s CVH research and refocus the field on earlier mitigation and strengths-based approaches. The aims were to: (1) examine the contribution of social contexts including adverse childhood experiences (ACEs) and racism, to the CVH of young adult Black women: and (2) determine the extent to which positive social determinants (e.g. spirituality, maternal relationship) in adolescence and young adulthood may promote CVH.
Methods: This study was a descriptive, secondary analysis of data from Black females who participated in the National Longitudinal Study of Adolescent to Adult Health (Add Health). A population representative sample of adolescents were enrolled in 1994 and followed prospectively with periodic, in-person data collection, and cardiovascular data was obtained in 2006 when the cohort were ages 24-32. The outcome for the first analysis was hypertension status and the outcome for the 2nd and 3rd analyses was ideal CVH, a summed score created by the American Heart Association consisting of self-reported health behaviors (e.g., smoking, diet) and objectively measured cardiovascular-associated biomarkers (e.g., glucose, cholesterol) that correlate with cardiovascular outcomes (e.g. myocardial infarction). All analyses were conducted using sampling weights to account for the complex survey design.
Analysis 1 was conducted with the publicly available data and used multivariable logistic regression to determine whether self-reported social adversities (social isolation, discrimination, perceived stress, subjective social status, child abuse) and sleep characteristics (delayed sleep onset, frequent awakening, short sleep, long sleep, and snoring) increased risk for hypertension. Analysis 2 used latent class analysis to examine patterns of social adversities (listed above plus food insecurity, housing insecurity, witnessing violence, victimization) on ideal CVH overall and for subgroups. Analyses 3 used principal components analysis to develop positive SDOH subscale scores (maternal relationship, spirituality) during adolescence and young adulthood. Multivariable regression was used to examine the influence of positive SDOH during adolescence and young adulthood, severity of ACEs, and their interactions on ideal CVH at young adulthood.
Results/Findings: In the first analysis (N=608), discrimination and frequent awakening were associated with higher odds of hypertension. The second analysis (N=1318) revealed three latent classes: low stress, high violence, and high stress. Although subclasses did not predict overall CVH, Black women who experienced high stress had a higher probability of being physically active and normotensive, while those with low stress had a higher probability of meeting dietary goals. The final analysis (N =1203) determined that greater spirituality in adolescence or young adulthood may promote CVH, but its influence diminished after accounting for factors such as mental health. The interaction of ACEs and spirituality showed that greater spirituality in adolescence or young adulthood buffered CVH regardless of ACEs level. Maternal relationship did not significantly predict CVH, but the interaction of ACEs and maternal relationship in young adulthood showed that ACEs scores were associated with worse CVH when the maternal relationship was stronger.
Conclusion: This study may be the first to explore CVH using a strengths-based approach and data from a within-group, population-representative sample of young adult Black women. Findings suggest that there are critical differences in how social contributors influence health, and, while many social constructs analyzed had little influence on health, they may not accurately reflect the underlying construct for different subpopulations. Importantly, there likely are other social factors that affect the health of Black women that are not well-captured in existing scientific research (e.g., frequency/type of microaggressions, racial identity, social connections) and require further research to advance CVH equity.
Team Award (Names listed below) Uniformed Services University of the Health Sciences Battlefield Acupuncture in the Management of Non-Traumatic Low Back Pain in Service Members Program Director - Heather Johnson
| Amber Birkle, DNP | Angelyn Brown, DNP | Diana Costa, DNP | Marita Prince, DNP | Vonya Gibbons, DNP |
Background and Problem Statement: Low back pain (LBP) among US active-duty service members (ADSMs) is a leading cause of permanent disability in the Army (Rhon & Fritz, 2015). The extraordinary pace of work, deployment cycles combined with heavy equipment operations, airborne maneuvers, and extensive physical demands increase the likelihood that ADSMs will incur lower back pain and injury (Roy, Fish, Lopez, & Piva, 2014; Armed Forces Health Surveillance Center [AFHSC], 2010). The high prevalence of LBP in ADSMs places significant burden on the overall strength and capability of the force. Battlefield Acupuncture (BFA), a form of auricular acupuncture, is a safe, effective, non-pharmacologic treatment for LBP and aligns with Department of Veteran’s Affairs (VA)/Department of Defense (DoD) Clinical Practice Guideline (CPG) recommendations. However, recent literature reveals numerous provider reported barriers such as lack of knowledge and training which pointedly limits the use of effective BFA treatments.
Purpose/Objective: The purpose of this DNP Team project was to increase provider knowledge of VA/DoD guidelines for the BFA treatment of LBP, and to mitigate perceived barriers to offering BFA in the primary care setting. The main objective of this project was to increase BFA intervention rates and explore patient self-reports of treatment effectiveness, as well as examine numbers of pain medication prescriptions, and duty-limiting profiles (activity restrictions) that impact individual Soldier readiness.
Procedures: A team of five Doctor of Nursing Practice family nurse practitioner students conducted an evidence-based practice project to increase use of BFA with ADSMs presenting with LBP at two large Army installations in North Carolina and in Texas. Using Rosswurm and Larrabee’s Model for Evidence-Based Practice Change (1999) as the organizing framework, a multifaceted program of BFA in the treatment of non-traumatic LBP was presented to primary care providers. Providers received a 30-minute in-service to review the 2017 VA/DoD LBP CPG, followed by a knowledge questionnaire related to BFA utilization perceived barriers related to use with LBP in the clinic. A retrospective record review was conducted for a three month timeframe to analyze rates of BFA being offered and administered, central nervous system (CNS) depressant medication prescriptions, and activity limiting temporary and permanent LBP profiles using ICD-10 diagnosis code M54.5 (low back pain). The DNP Team designed, operationalized and evaluated two supervised BFA walk-in clinics for 8 full weeks. Patient demographic data, and pre and post pain ratings using the Defense and Veterans Pain Rating Scale (DVPRS) were collected on all patients who accessed the walk-in BFA clinic.
Outcomes: Nearly all providers were trained and certified in BFA in two walk-in clinics, resulting in 231 patient encounters. At Ft Bragg, BFA treatments increased 212% with 82% of patients reporting immediate pain relief (2.1 reduction on 10-point scale). Patients were 93% less likely to obtain a new profile, 44% less likely to have a pre-existing profile, and 46% less likely to be prescribed a CNS depressant. Patients at Fort Hood saw 1.9 point decrease in pain with 43% reporting relief. They were also 30% less likely to obtain a new profile and 52% less likely to have a pre-existing profile.
Conclusion: The pervasiveness of LBP among ADSMs imposes substantial burden on military readiness. DNP Team project data suggests BFA is an effective, safe treatment for LBP. Increasing rates of BFA as a non-pharmacologic integrative therapy for LBP may improve soldier readiness in the form of decreased pain, fewer CNS depressant medication prescriptions, and fewer activity limiting profiles.

Background and Problem Statement: Mechanical ventilation (MV) is commonly used to support breathing and pulmonary gas exchange in critically ill patients who experience respiratory failure. More than 1/3 of intensive care unit (ICU) patients in the United States require MV (CDC, 2018). Aging patients with multiple comorbidities and hospital-acquired complications are at high risk of requiring prolonged MV. Prolonged MV puts patients at risk for MV associated complications such as barotrauma, diaphragmatic muscle atrophy, pneumonia, decreased cardiac output, and muscle weakness, and can increase the ICU and hospital length of stay (LOS), as well as mortality (CDC, 2018; Devlin et al, 2006; Wang et al, 2013). Paired spontaneous awakening trial (SAT) and spontaneous breathing trial (SBT) can significantly reduce the duration of MV and ICU LOS (Marelich et al., 2000; Roh et al., 2012; Dankers et al., 2013). Studies show that a nurse-driven SAT and SBT can have a positive impact on ventilator-associated outcomes.
Purpose/Objective: The purpose of this evidence-based (EBP) quality improvement project was to decrease the duration MV by implementing a registered nurse (RN) and respiratory therapist (RT) driven SAT and SBT protocol with intubated adults in a general ICU. Prior to the project, providers (MDs) used no standardized protocol to evaluate patient readiness for liberation from MV.
Procedures: This project was implemented in a16-bed medical-surgical ICU in a community hospital in a medium sized midwestern city. All stable adults (except cardiac surgery patients) undergoing MV were screened daily for participation. A patient safety screen was used to determine whether the SAT and SBT could be initiated by the RN and RT. Additional safety criteria were used by the RN and RT to determine whether the SAT or SBT should be stopped due to patient intolerance.
Duration of MV (hours), ICU LOS (hours), and number of 24-hour failed extubations (24hrFE) were measured to compare outcomes before implementation to post implementation. Measures of staff self-reported confidence in performing the SAT and SBT, and evidence of staff protocol adherence, from the electronic health record, were also recorded.
Evaluation goals were established prior to implementation. A goal of 15 % improvement was set for both duration of MV and ICU LOS. For 24hrFE the goal was no increase in 24hrFE. This outcome was included to determine if any reduction in duration of MV was associated with an increased need for re-intubation. The goal for staff self-reported confidence in protocol implementation was set as an improvement on a 1 – 5 scale. The goal for staff adherence with daily performance of the SAT and SBT protocol was set at 50 %. Implementation of the project began July 1, 2019 and was completed November 1, 2019.
Outcomes: Duration of MV decreased by 27 hours (38.6%) (Wilcoxon Rank-Sum Test, p=0.000802). ICU LOS decreased by 32 hours (27.9%) (Wilcoxon Rank-Sum Test, p=0.01248). 24-hour failed extubations decreased from 4 to 2 (Fischer’s Exact test, p=0.419). Pre- and post-survey of staff confidence utilizing the protocol yielded a 20% increase in confidence. Staff adherance with SAT and SBT protocol, measured using EMR data, revealed initial RN and RT adherance was 49% but increased to 90 % at the end of the project. Provider adherence to writing protocol orders increased from 70 % to 90 %. All project goals were met.
Conclusion: This project demonstrated the feasibility and positive impacts of implementing an RN and RT-driven MV liberation protocol in a community hospital ICU. Patient outcomes associated with MV were improved. Incidental findings support additional impact of this project. Sedation scores on the Richmond Agitation and Sedation Scale rose from -3 (moderately sedated) to -2 (lightly sedated) and hospital LOS decreased from 243 hours to 204 hours (1.65 days). Successfully improving patient outcomes and increasing staff confidence in use of the protocol also supports RN and RT autonomy, thereby advancing the impact of their professional contributions.
2019 Winners
Marliese Nist, PhD, RNC The Ohio State University Inflammatory Mediators of Stress Exposure and Neurodevelopment in Very Preterm Infants Program Director - Rita Pickler
Background and Significance: Preterm infants experience chronic stress exposure during their extended hospitalization in the neonatal intensive care unit as a result of the medical procedures and nursing care required for their survival. The Neonatal Stress Embedding (NSE) Model theorizes that chronic stress exposure affects multiple biological systems in preterm infants, including functioning of the immune system, autonomic nervous system, and hypothalamic-pituitary-adrenal axis and causes changes in gene expression that result in abnormal brain development and neurodevelopmental impairments. Specifically, the NSE Model posits that chronic stress exposure causes systemic inflammation that damages the immature brain. Purpose/Objective(s) and/or Specific Aims: The specific aims were to (1) determine the relationships among stress exposure, inflammation, and neurodevelopment in very preterm infants and determine the mediated effect of inflammation on the relationship between stress exposure and neurodevelopment, (2) describe cytokine trajectories in the weeks following birth and determine the effect of stress exposure on these trajectories, and (3) examine the relationship between chronic stress responses and stress exposure in preterm infants. Methods: This was a non-experimental, repeated measures study of very preterm infants born between 28-31 weeks post-menstrual age (PMA). Infants were enrolled from four neonatal intensive care units in a large Midwest metropolitan area. The Institutional Review Board approved the study, and mothers of eligible infants provided written informed consent prior to the initiation of any study procedures. Cumulative stress exposure was measured using the Neonatal Infant Stressor Scale (NISS) over the first 14 days of life. The NISS provides a count of acute (e.g. intubation, lab draw) and chronic (e.g. mechanical ventilation, sepsis) stressors that is weighted by stressor intensity. Data to complete the NISS were retroactively extracted from the electronic health record. Blood was collected weekly with a clinically-indicated lab draw until 35 weeks PMA to measure inflammation. Inflammation was operationalized as a panel of cytokines and chemokines, quantified by multiplex assay. Average levels of individual cytokines/chemokines and average composite z-scores that included all detectable cytokines/chemokines were used. Neurodevelopment was assessed at 35 weeks PMA using the cluster scores for motor development and vigor (MDV) and alertness/orientation (AO) from the Neurobehavioral Assessment of the Preterm Infant. Hair for the measurement of hair cortisol concentration was collected by shaving at the nape of the infant’s neck at 35 weeks PMA. Multiple linear regression models, conditional process analysis, and linear mixed models were used to analyze the data. Statistical models included interactions with PMA at birth and infant sex and controlled for overall illness acuity. Results/Findings: Seventy-three infants were enrolled in the study. We quantified plasma interleukin (IL)-6, tumor necrosis factor-alpha (TNF-α), monocyte chemoattractant protein-1 (MCP-1), IL-8, and IL-1 receptor antagonist (RA) but were unable to measure IL-1β, IL-4, IL-10, and IL-17 in the majority of plasma samples. Although stress exposure did not significantly predict neurodevelopment, some measures of inflammation predicted MDV and AO. TNF-α and IL-1RA were associated with MDV scores. Composite scores of inflammation (i.e. average composite z-scores) were associated with MDV and AO scores. There were significant interactions with PMA and infant sex. In the mediation models, only IL-1RA mediated the effect of stress exposure on neurodevelopment. Linear mixed models revealed significant trends in postnatal cytokines/chemokines that were not affected by stress exposure. Cumulative NISS scores, a measures of stress exposure, did not correlate with hair cortisol concentrations, a measure of chronic stress responses. Conclusion: While we could not confirm a relationship between stress exposure and neurodevelopment, inflammation may be an important predictor of short-term neurodevelopment. IL-1RA is an important cytokine for studies of preterm infant neurodevelopment. Moreover, composite z-scores may be a better measure of inflammation than individual cytokines/chemokines. Inflammation can be damaging to the immature brain and is a potential mechanism through which early life stress affects long-term outcomes. Stress does not appear to affect cytokine/chemokine trajectories. Cytokine/chemokine levels, most of which decrease over time, may be developmentally regulated or the result of resolving inflammation following preterm birth.

Background and Problem Statement: The prevalence of both type 1 and type 2 diabetes are increasing in the pediatric population (Alberti et al., 2004). In addition to milestones that accompany normal growth and development, children diagnosed with diabetes incur an additional set of challenges, physiologically as well as psychologically. Among youth with diabetes, death is more likely to occur due to an acute complication, such as DKA or hypoglycemia (Saydah et al., 2012). According to a report generated from Epic, the University of Mississippi Medical Center (UMMC) electronic health record, from November 2014 to November 2015 there were 195 hospital encounters including the ICD-10 code for DKA (this includes ER visits and hospital admissions), 141 of which resulted in hospital admissions. Of these 195 encounters, approximately 40% were repeat admissions (University of Mississippi Medical Center, 2019). Purpose/Objective: The purpose of this scholarly project was to determine the effect of the telehealth RPM system initiative on HbA1c and diabetes-related ER visits and hospital admissions in the pediatric diabetes population at UMMC. The goal of the RPM program was to reduce HbA1c levels, to prevent unnecessary hospital encounters, and to allow the provider to make insulin adjustments between visits, as the pediatric population requires frequent insulin adjustments during periods of growth. Procedures: UMMC Center for Telehealth, in collaboration with Children’s of Mississippi, Division of Pediatric Endocrinology, began to enroll pediatric patients with type 1 and type 2 diabetes into an RPM (remote patient monitoring) program in November of 2015. Patients receive a blue-tooth glucose meter and an iPad, and blood glucoses are transmitted via cellular service in real-time to the telehealth center, where nurses are monitoring the patients. The setting for the implementation of RPM was outpatient, UMMC, Division of Pediatric Endocrinology. Participants were patients aged 0-18 years with type 1 or 2 diabetes. Outcome data for participants was collected via retrospective chart review, for the 12 months prior to enrollment, and up to 12 months following enrollment. Outcome data collected included: HbA1c levels and diabetes related ER visits and hospital visits. Using SPSS, version 25, descriptive statistics were calculated and the paired t-test was conducted (using a level of significance of ≤ 0.05) to determine whether there was statistical evidence that the mean difference between standard care versus RPM for the outcomes of HbA1c, ER visits, and hospital admissions was significantly significant. Outcomes: Hemoglobin A1c levels decreased from baseline for patients enrolled for up to 3 months (p=0.146), 9 months (p=0.142), and 12 months (p=0.007), and increased for those enrolled for up to 6 months (p=0.743). Emergency room visits decreased for those enrolled for up to 3 months (p=0.037), 6 months (p=0.388), and 9 months (0.054); however an increase was noted for patients enrolled for up to 12 months (p=0.822). Finally, for hospital admissions, a decrease was found in those enrolled for up to 3 months (p=0.138), 6 months (p=0.005), 9 months (p=0.021), and 12 months (p=0.819). Conclusion: Consistent with the findings of other meta-analyses focusing on the use of outpatient telehealth, this study’s intervention also resulted in a more substantial decrease in HbA1c than with standard care alone. This may be due to the fact that there was increased contact with the telehealth RPM staff. Additionally, patients in this study received goal-specific education modules via the iPad, which may have also attributed to an overall increase in compliance with diabetes self-management. The ability of the healthcare provider to make insulin adjustments as necessary between visits likely contributed to a decrease in HbA1c levels as well.
2018 Winners

Marik Moen, PhD, RN University of Maryland Baltimore, MD Social Stability as a Consistent Measure of Social Context in a Low-Income Population PhD Program director - Dr. Mary Johantgen
Background and Significance: While researchers are modeling the social contexts in which people are living in studying health and disease, these social determinants of health (SDH) are often conceptualized and measured very differently. Both of these applications of SDH require reliable and valid measures. The construct of Social Stability (SS) developed by German and colleagues (2009) had several advantages: 1) more than one SS domain is necessary to create stability; 2) the inter-connectedness of domains; and 3) the importance of using a defined period of time in measurement. The six domains include: housing, residential/moving, income, employment, legal, and relationship stability over 12 months.
Purpose/Objective(s) and/or Specific Aims: The overall aim of this dissertation was to develop evidence for the use of SS in research and clinical practice. To examine reliability and validity, German’s SS measure was examined in a new population. In addition to overall stability, the prevalence and covariates of individual indicators were explored. Lastly, the relationship of SS to syndemic (co-occurring, interacting) risk behaviors (sexual, substance use, violence) was examined.
Methods: A cross-sectional analysis was conducted from a population (n=503) of heterosexuals at high-risk for HIV infection from the 2013 Baltimore site of National HIV Behavioral Surveillance Study. Data collection occurred via respondent driven sampling (RDS) where study seeds give coupons to potentially eligible participants and refer recruits to study site. This “weighted snowball” approach facilitates recruitment of often hidden populations. The final sample was predominantly African American, half male, with a median age of 37. The SS measure is a self-reported assessment of the six domains over the past year. Outcome variables include sexual risk, violence exposure, and alcohol and drug use variables. Sexual risk indicators include sexually transmitted infection (STI) or HIV diagnosis, multiple partners (2 or more sexual partners in the past year), concurrent partners (having sex with 2 or more partners during same time period), and exchange sex (receiving or giving drugs, money other goods for sex). Violence variables include experiencing threat by weapon, being in physical fight, experiencing physical violence from a partner, or forced sexual encounters. Both SS domain indicators and outcomes were analyzed for individual prevalence and in combination. A syndemic outcome was the co-occurrence of 2 or more of the risk indicators. Descriptive and latent class analyses (LCA) were used to characterize the prevalence and patterns of SS and risk behaviors and to identify SS subgroups. Logistic and latent class regression was applied to model the relationships of SS to risk behaviors and demographic covariates.
Results/Findings: Co-occurrence of SS indicators was common, with an average of 3.4 (SD=1.2) out of 6 indicators of stability. LCA showed evidence for 3 sub-classes: Class 1: overall high stability; Class 2: residential instability (moved in past year); and Class 3: low stability (income, employment instability). Perception or history of stability did not contribute to any improvement in identifying latent classes. Education was an influential covariate in LCA. Those with high school education/GED were nine times more likely to be in “high” vs. “low” SS class (OR=9.37; 95%CI: 2.75-31.82). The most common syndemic risk behaviors were sex-violence-drug, occurring in 18% of the sample. Ordinal and latent measurements of SS reliably predicted individual and combinations of sexual-substance use and violence risks. The latent approach showed higher odds of co-occurring risk for low vs. high SS class (OR= 6.25; 95%CI=2.46, 15.96) compared to using categories for low vs. high SS (OR=2.69; 95%CI=1.29, 5.59).
Conclusion: German’s measure of social stability captures inter-related social conditions across populations and identifies distinct subgroups of in/stability. Each domain of SS should be included and examined, with specific consideration for moving residence which was found to be important in the population studied. Further, ordinal and latent measurements of SS were reliably associated with risk in this population, demonstrating that as SS accumulates, co-occurring (or syndemic) risk diminishes. Furthermore, latent class analysis, which develops classes based on patterns of answers to a set of categorical variables, is a good approach to examine co-occurring predictors.
Background and Problem Statement: Sleep and epilepsy have a complex reciprocal relationship. Sleep-related breathing disorders that can occur in epilepsy are well recognized and a potentially dangerous risk factor for cardiovascular diseases, perioperative morbidities, increase in body mass index, cognitive impairment, unintentional injuries, changes in neuroendocrine, immune and inflammatory systems, depression, sudden unexpected death in epilepsy, increased frequency of seizures, and overall decreased quality of life (Faraut et al, 2012; Panossian et al., 2013). Undiagnosed and untreated obstructive sleep apnea (OSA) is also a potential dangerous risk factor for increased seizure frequency, particularly nocturnally, for adult patients with epilepsy. The American Academy of Neurology (AAN) in their clinical quality measures, indicate a need for provider’s to address safety issues and to intervene to reduce seizure frequency to zero. Patients can easily be screened for OSA with established markers that are strategically placed in the electronic health record (EHR) platform as a reminder to complete.
Purpose/Objective: The DNP student developed, implemented, and evaluated the effectiveness of adding an EHR alert with Assessment of Obstructive Sleep Apnea (AOSA) for assessment of patients with epilepsy by determining the percentage of patients referred for polysomnography (PSG). A 3-month retrospective chart review of adults with epilepsy was conducted to determine the percentage of patients screened for OSA and referred for PSG. The AOSA was added to the EHR to cue neurology providers to screen for OSA for 3 months. Percentages of referrals of patients with epilepsy for PSG before and after adding the AOSA EHR alert were compared.
Procedures: An urban university hospital was the setting for this study. Adult patients 18 years of age and older with epilepsy from the hospital’s seizure and neurology clinics were included. Children were excluded due to their sleep/wake cycle continuing to mature, changing body mass index (BMI), genetics, mandible, airway, tonsils and adenoid growth, and the behavioral factor of sleep-onset association disorder. After approval by the institutional review board, a review of the literature was conducted and an assessment tool was developed with 12 primary and 9 secondary risk factors with subsequent ordering of a PSG if >2 risk factors were present. The board-certified sleep medicine physician provided content validity. The AOSA tool was embedded in the EHR after approval by the institution’s EPIC steering committee. A 3-month retrospective chart review was conducted with the collection of sex, age, and data from OSA screening performed and referral for PSG. A second set of 3-month data were collected after inclusion and implementation of the AOSA in the EHR. The percentage of adult patients screened and referred for a PSG before and after integration of the AOSA in the EHR was determined. Pearson’s Chi Squared test (x2) was used for data analysis. The GraphPad Prism 7 program was used to calculate the Chi-Squared test for the quantitative data to determine if an increased proportion of patients were screened as positive for OSA with an EHR alert and referred for a PSG.
Outcomes: The three-month retrospective chart review indicated that no patients were formally screened for OSA prior to introduction of the EHR alert, yet 25 (7.2%) of the 346 subjects were sent for a PSG, presumably based on patient report, history and exam findings. Following the addition of a simple AOSA tool in the neurology section of the EHR, 405/414 patients (97.8%) of patients were screened for OSA and 134/405 (33.1%) were referred for a PSG. There was a significantly increased number of patients identified with OSA after the implementation of the AOSA (x2 value = 74.7, df = 1, p<0.001).
Conclusion: The results of this quality improvement project supported the assessment of adult patients with epilepsy for OSA with a prompt in the EHR. The added prompt increased the percentage of patients receiving a referral for a PSG to objectively determine OSA. In view of the clinical and public health implications of untreated OSA, screening in high-risk populations, such as patients with epilepsy, warrants implementation. Adoption of screening tools into the EHR may help to facilitate practice transformation and identify OSA as a potential risk factor for the proliferation of seizures in patients with epilepsy.
2017 Winners
Kristen Weaver, PhD, RN New York University New York, NY Brain-gut Axis Dysregulation in Patients with IBS; An Exploratory Investigation for Markers of Stress. PHD Program director - Dr. Allison Vorderstrasse

This three-part investigation analyzed participant data from a parent investigation at the National Institutes of Health. Participants included males and females who identified either as HC or patients with IBS. The first investigation (N=101) revealed differential findings in psychological stress markers by IBS diagnosis, as well as sex, race and subtype differences in the stress response of IBS participants. These findings were used to optimize the second investigation, which analyzed expression levels of genes that may affect psychological and gastrointestinal processes, through the creation of a custom PCR array. IBS participants were found to differ from HC (N=48) in expression levels of six genes associated with immune activation, stress, psychological and antimicrobial processes. Additional analyses within female IBS participants, revealed a significant difference between subtypes in gene expression levels related to pain sensation. The third dissertation study harnessed the power of shotgun proteomic analysis, to identify circulating serum proteins that differentiate a homogenous set of IBS participants from well-matched HC (N=6). Analysis of 1,317 proteins revealed a significant difference in 12 proteins between IBS and HC participants, with biological associations including platelet activation/degranulation, platelet alpha granule lumen, secretion by cell and extracellular region.
This dissertation investigation revealed preliminary though promising findings of psychological, physiological, genomic and proteomic differences between IBS participants and HC, and within IBS participants. By exploring downstream effects of noted sex and subtype differences, this study may foster insight on physiological underpinnings of IBS and promote understanding of BGA dysregulation. By illustrating the heterogeneity of the IBS patient population, this study highlights the importance of an individualized approach to patient care, thus working to improve clinical outcomes of patients living with the disorder.
Honorable Mention went to:
Latefa Dardas , PhD, RN, CDE; Duke University A Nationally Representative Survey of Depression Symptoms among Jordanian Adolescents: Associations with Depression Stigma, Depression Etiological Beliefs, and Likelihood to Seek Help for Depression.

Purposes/Aims: This project was designed to identify and evaluate key challenges a rural hospital has in providing a reliable best practice response for an Emergency Cesarean Section (ECS). Decision to Incision times (DIT) when confronted with an ECS along with newborn outcomes were studied. The study also conducted and analyzed staff questionnaires to evaluate staff attitudes, perceptions, role clarifications, driving and restraining forces in an ECS.
Rationale/Background: American Congress of Obstetrics and Gynecology (ACOG) recommend that obstetrical services be able to reliably perform an ECS DIT in 30 minutes or less. Seventy percent of neonatal brain injury may occur in the intrapartum period (AWHONN, 2015). Rural hospitals often perform all cesarean sections in the operating room domain with experienced operating room staff rather than obstetrical nurses trained in circulation and scrub. Rural hospitals are fraught with challenges around 24/7- hour/day availability of skilled anesthesia and surgical staff needed for an ECS. The Institute of Medicine, (2005) remarked that rural hospitals do not regularly have the census to finance operating rooms and anesthesia to be in house always. Rural multidisciplinary staff often feel unsupported and feel incompetent with oversaturated responsibilities. Night shifts (PM) and weekends are left vulnerable to prolonged DIT’s for an ECS.
Methods: Five years of Emergency Cesarean Section outcomes were analyzed (records review) to evaluate a rural hospital system in providing a reliable “best practice” response as recommended by ACOG. Outcomes (DIT’s and newborn) evaluated, included pre-intervention and post-intervention quality improvement(QI) project initiated by this author. Statistical tests include: t-Test for independent groups and mean scores, 5-minute Apgar mean scores, with nominal data for infant respiratory distress and hospital transfer. Staff questionnaires included a Likert scale that involved questions about staff encounters when an ECS was performed. The questionnaire also employed a ranking section about the staff’s personal perceptions about restraining and driving forces as described by the Kurt Lewin theory.
Outcomes achieved: Decision to Incision t-Test for independent groups analyzed, not statistically significant, (n=19, t=.88, alpha .05, two tailed, critical value,211, df17). Clinical significant ascertained that mean DIT scores were improved post-intervention by 7 minutes. Pre-intervention=DIT @ 37.2 minutes and Post-intervention=DIT @ 30.2 minutes. Evening shift (PM) and weekend, overall scores, demonstrated prolonged DIT mean scores, AM (n=8) =26 minute, PM/weekend (n=11) =42.3 minutes. Pre-implementation DIT AM=37.2-minute, Post implementation=25.6 minutes. Pre-implementation DIT PM/Weekend=41.2 minutes, Post=41.8 minutes. Staff questionnaires revealed that the staff believes that “best practices” are attainable for an ECS in this facility. The staff questionnaires also ranked that there was a lack of training surrounding an ECS, rural skill oversaturation requirements, and unity resistance between the Operating Room staff and Labor and Delivery staff when an ECS was called. The staff ranked the chief driving force as the importance of good newborn outcomes.
2016 Winners
Erin Downey, DNP Duke University Durham, NC Implementation of a Patient Agreement for Opioids and Stimulants in a Primary Care Practice Chair - Paula Tanabe, PhD
The dramatic increase in the consumption of controlled substances in North Carolina and across the nation has created a public health crisis with epidemic levels of medication diversion, misuse, abuse, unintentional overdose and death. Primary care providers are the principal prescribers of controlled substances and therefore at greatest risk of encountering patients that abuse medications. Guidelines recommend patient agreements with specific monitoring requirements when prescribing Schedule II medications (opioids and stimulants). Studies have focused solely on opioids and excluded stimulants and adherence to all recommended monitoring requirements has not been fully evaluated in the literature. Patient agreements were not previously used in the project practice site.
Implement a Schedule II controlled substance patient agreement and measure fidelity to components of the agreement.
A quality improvement framework using Plan-Do-Check-Act was used to design and implement the project. An opioid and stimulant prescribing policy and patient agreement was developed from sample agreements and based upon existing evidence with input from the practice partners. The policy applied to all patients aged 19 and over prescribed a long-term Schedule II medication for the chronic conditions of pain and/or attention deficit hyperactivity disorder. Examples of Schedule II narcotics include: hydrocodone, hydromorphone, oxycodone, fentanyl and methadone. Stimulants include: amphetamine, methamphetamine, and methylphenidate. All providers in the clinic received education about the policy. Adherence to the following outcome measures (elements of the protocol) were evaluated monthly: patient signed Schedule II agreement on file, prescription monitoring program (pmp) checked prior to writing a Schedule II prescription, urine toxicology screens, and prescriptions written without a mandatory visit. Monthly feedback was given to the providers over the course of the project. Modifications to improve adherence were made as needed. Outcomes were compared seven months pre- to seven months post-implementation of the patient agreement. Wilcoxon signed rank test and McNemar test were used to analyze differences in adherence between the pre and post implementation time period.
Fifty patients met study criteria and were included in the analysis. The mean (SD) age was 50.7 (16.3). The majority of patients were white (96.0%) and female (62.0%). An almost equal proportion of patients received medication for chronic pain (50%) and attention deficit hyperactivity disorder (46%). Four percent of participants received medication for both diagnoses. The percent of guideline adherence to each outcome improved from pre to post implementation: Signed agreement in chart (0%, 94%); urine screen guideline (5.3%, 71.1%); pmp checks (11.3%, 99.0%); prescriptions written without a visit guideline deviation, (20.6%, 0). All changes were significant (p < .001).
Implementation of a Schedule II controlled substance patient agreement and prescribing policy in a small primary care practice was feasible and adherence to the policy was excellent over a 7-month period.
Dissemination: The manuscript is under review for publication in the Journal of Family Medicine and Primary Care. The journal audience is family practice providers who frequently struggle with the complexity of prescribing chronic opioids. The project results will be shared at an evidence-based research conference scheduled for September 2016 at UCLA.
Continued implementation: All providers in the practice continue to follow the policy and are initiating patient agreements for new patients as well as following all aspects of the protocol. Monitoring for adherence is ongoing.
Sustainability and cost: The cost of implementation was not measured directly, but has proven to be minimal. In North Carolina, the prescription-monitoring program is state funded with free access to registered users. All project-associated tasks such as presentation and explanation of the patient agreement and urine collection were completed within the normal workday and did not require additional man-hours. In March 2016, the Centers for Disease Control and Prevention (CDC) issued the Guideline for Prescribing Opioids, http://www.cdc.gov/mmwr/volumes/65/rr/rr6501e1.htm.
The protocol we implemented included almost all aspects of the guideline, which should increase the probability of associated costs being covered by insurance. All of these factors enhance the project’s sustainability.
Sarah Farabi, PhD University of Illinois at Chicago Chicago, IL Sleep, Glucose Variability and Cardiovascular Disease Risk in Young Adults with Type 1 Diabetes Chair - Mariann Piano, PhD
People with type 1 diabetes mellitus (T1DM) experience high glucose variability and frequent hyperglycemia. Poor glucose control is known to contribute to accelerated cardiovascular disease (CVD), a leading cause of death in people with T1DM; however poor glucose control does not completely explain the increased risk. Good sleep also has been shown to play an important role in maintaining cardiovascular and metabolic health. Sleep quality is reduced in people with T1DM, but the reasons for poor sleep quality are not known. There has been minimal research into the relationship between glucose variability and sleep disruption in young adults with T1DM.
Hypotheses and Specific Aims: To test the hypotheses that glucose variations are causally related to sleep disruption and that sleep disruption mediates inflammation and CVD risk in individuals with T1DM, two aims were proposed: 1) to quantify sleep disturbances and to determine their relationship to glucose variability and 2) to define the relationship between sleep disruption and markers of CVD risk in young adults with T1DM.
A prospective, cross-sectional design was used. Young adults, age 18-30, who had diabetes for at least 5 years, wore an insulin pump and had a normal sleep schedule were enrolled. Subjects wore a continuous glucose monitor (CGM) and a sleep/activity monitor in home for three days and two nights and underwent a formal sleep study, polysomnography (PSG), while wearing the CGM in the laboratory at the University of Illinois at Chicago on the third night. The CGM is a validated tool that provides an updated glucose value every five minutes. Total time in bed was between 7-8 hours; blood was drawn just before lights out (pre-sleep); at lights on (awakening) and one hour after lights on(1-hr post awakening) to measure amounts of CVD risk markers, inflammatory cytokines, interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α). The amount of power in five electroencephalogram (EEG) Bands – Delta and Theta (characteristic of sleep); Alpha, Beta and Gamma (characteristic of wakefulness) – was tracked throughout the PSG study night. Wavelet coherence analysis was applied to determine time varying and frequency specific relationship between glucose levels and the five EEG bands. Granger causality analysis along with vector coefficient analysis was applied to the glucose and five EEG bands to determine if potential causal interactions between glucose and EEG during sleep. Levels of IL-6 and TNF-α were determined using Enzyme linked immunosorbent assays (ELISA) and one-way ANOVA (Scheffe’s test for multiple comparisons) was applied to compare between the pre-sleep, awakening and 1-hour post awakening time points.
27 subjects (11 males, average age 23.9±4.1 years) were included in the analysis. Wavelet Coherence Analysis revealed a strong time-varying and frequency specific coupling between glucose and EEG, rapid fluctuations were more strongly coupled and exhibited more instances of strong coupling through the night (p<0.0001). 96.2% of subjects exhibited at least one instance of significant Granger causality between Glucose and EEG bands. Increasing glucose was causally related to increasing Alpha and decreasing Theta and Delta power, changes in the EEG signal which are consistent with an arousal or sleep disturbance (p=0.01). Increases in Delta (increases during deep sleep) consistently caused increasing glucose levels while increasing Theta (increases during rapid eye movement sleep) caused decreasing glucose. TNF-α was higher on awakening (1.44±0.66 pg/ml [SD]) and 1-hour post awakening (1.6±0.62 pg/ml) compared to pre-sleep (0.96±0.48pg/ml) (p<0.0001 for each). Subjects with good glycemic control exhibited a normal pattern of decreased IL-6 upon awakening.
Findings from the present study support a potential bi-directional causal relationship between glucose and brain activity during sleep. Increasing glucose led to changes associated with a sleep disturbance (increasing arousals and awakenings). Further, normal changes in the sleep process, were causally related to changes in glucose. The current findings also support that the sleep period may play an important role in increasing inflammation, a key mechanism in development of cardiovascular disease in people with T1DM. Collectively, findings from this study highlight the importance of the sleep period for glycemic control and inflammation in people with T1DM.
Sleep is a potentially modifiable behavior is increasingly recognized as playing an important role in maintenance of health. The findings from this study highlight that glucose variability during sleep may play an important role in disturbance of sleep, but also that sleep may influence glycemic control. This foundational evidence provide motivation for future interventional studies aimed to determine the mechanisms underlying the relationship between glucose variability and sleep disruption as well as the role of this relationship in development of CVD. Understanding how glucose variability and sleep disruption accelerates CVD may allow for improved diabetes nursing management strategies. Nursing interventions aimed at improving glycemic variability or minimizing sleep disturbances may help to improve glycemic control, decrease CVD development and ultimately improve quality of life in people with T1DM.
2015 Winners
Jennifer Dine, PhD University of Missouri Columbia, Missouri Characterization of a Novel Regulator and Predictors of Sensitivity to TRAIL-induced Apoptosis in Breast Cancer Cells Chair - Dr. Jane M. Armer
Tumor necrosis factor-related apoptosis inducing ligand (TRAIL) is a protein that selectively induces apoptotic cell death via TRAIL receptor (TRAIL-R) activation in cancer cells. TRAIL-R agonists have been well-tolerated but demonstrated very little activity in patients. Interestingly, triple negative breast cancer (TNBC) cells were found to be sensitive to TRAIL-induced apoptosis while breast cancer cells representative of the other subtypes (estrogen/progesterone receptor positive or HER2 amplified) were comparatively resistant in vitro. Characterizing regulators and predictive biomarkers of TRAIL-R agonist sensitivity may help identify TRAIL-R sensitizing combinatorial therapies and TNBC-affected patients who might benefit the most from a TRAIL-R agonist therapy.
The first objective was to characterize the protein, gp78, as a negative regulator of TRAIL-induced apoptosis in breast cancer cells. The second objective was to evaluate the sensitivity of different subtypes of breast cancer cells in vitro to drozitumab, a TRAIL-R agonist that was well-tolerated in patients. The third objective was to identify potentially predictive biomarkers of TRAIL-R agonist sensitivity. The fourth objective was to evaluate expression of the potentially predictive biomarkers in patient samples. To address the first objective in evaluating the negative regulatory effects of gp78 on TRAIL pathway sensitivity, gp78 function was transiently inhibited using 10 gp78-targeting siRNAs in the TNBC cell lines MB231. gp78 function was also chronically inhibited by generating MB231 cells with stable gp78 knockdown. Cells with and without gp78 knockdown were then treated with and without TRAIL, and loss in cell viability and caspases-3/7 activity, which is a direct measure of TRAIL pathway activation, were assessed. To address the second objective, a panel of breast cancer cell lines representative of the different subtypes of disease (estrogen/progesterone receptor positive, HER2 amplified, and TNBC) were treated with and without drozitumab and evaluated for loss in viability. To address the third objective, immunoblot analyses were used to assess for potentially predictive protein markers of drozitumab sensitivity in the cell lines used in the second objective. Finally, to address the fourth objective, 177 TNBC tumor samples from a publically available cDNA microarray dataset were evaluated for the differential transcriptional regulation of genes whose protein products were identified as potentially predictive biomarkers of drozitumab sensitivity in the third objective. Additionally, 53 TNBC tumor samples were evaluated using immunohistochemistry to assess the protein expression of the identified potentially predictive biomarkers using a clinically relevant assay system.
The results from the first objective indicated that gp78 inhibited TRAIL-induced apoptosis in breast cancer cells in a mechanism that was dependent on the cell death-mediating proteins, caspases. The findings from the second objective demonstrated that TNBC cells, but not breast cancer cells representative of the other subtypes of breast cancer, were sensitive to drozitumab-induced cell death. In the third objective, the proteins Axl and vimentin were expressed only in the breast cancer cells that were sensitive to drozitumab-induced cell death. Axl and vimentin were thus selected as candidate predictive biomarkers of TRAIL-R sensitivity. Finally, in the fourth objective, Axl and imentin were found to be highly transcriptionally co-expressed (p<0.0001) in the cDNA microarray datasets of 177 TNBC tumors and were also highly co-expressed in the top quartile of Axl and vimentin-expressing tumor samples in the 53 TNBC tumor samples characterized by immunohistochemistry.
The findings from this study demonstrate that gp78 negatively regulates TRAIL-induced apoptosis in a caspase-dependent manner. TNBC cells were also determined to be sensitive to drozitumab, a TRAIL-R agonist, and those cells also expressed the proteins Axl and vimentin. Axl and vimentin were identified as candidate predictive biomarkers of drozitumab sensitivity and were determined to be expressed in human TNBC tumors at the transcriptional and protein levels. Therefore, Axl and vimentin expression in tumors may be utilized to aid in the selection of TNBC-affected patients who might benefit from a TRAIL-R agonist therapy.)
The findings from this study characterize the protein gp78 as a novel negative regulator of TRAIL-induced apoptosis. Little is known about the regulatory mechanisms that govern TRAIL sensitivity in cancer cells. Therefore, these findings contribute significantly to an area of TRAIL-related research that has been poorly described. The gp78 protein may also provide information about targetable pathways in cancer cells that could be inhibited or enhanced pharmacologically to promote TRAIL-R agonist activity in patients. The identification of the potentially predictive biomarkers of TRAIL-R agonist sensitivity, Axl and vimentin, may also aid in promoting TRAIL-R agonist activity in patients by helping identify those individuals whose TNBC tumors would most likely respond to a TRAIL-R agonist. In light of the limited success of TRAIL-R agonist strategies tested in clinical trials to date, using predictive biomarkers is a novel but potentially highly useful system for selecting patients for TRAIL-R agonist treatment. Collectively, these findings reflect elements from across the translational spectrum with respect to describing the fundamental regulatory processes of a biological system to the application of clinically relevant strategies for improving therapeutic effectiveness in patients.
Veronica Brady, PhD, RN, FNP-BC, BC-ADM, CDE; University of Texas Health Science Center at Houston Prevalence of Steroid Induced Hyperglycemia in Patients with Mantle Cell Carcinoma Receiving High Dose Steroid
Ariana Chao, PhD, FNP; Yale University Obesity-Related Eating Phenotypes and the Relationships with Food Cravings, Stress, and Metabolic Abnormalities
Michelle Davis, DNP, NNP, RNC-OB Arizona State University Implementing Skin-to-Skin Contact in the Operating Room Following a Cesarean Delivery DNP Program Advisor- Dr. Heather Ross
Cesarean delivery is the most common major surgical procedure in the United States, representing 38.2% of live births in 2012 (Boyle et al., 2013). Infants delivered by cesarean section may face a more difficult transition to extrauterine life due to retained fluid within the alveoli (Blake & Murray, 2006). Skin-to-skin contact (SSC) and breastfeeding have been shown to help these newborns. However, one large urban medical center in the Southwest US did not have a policy to support immediate SSC and breastfeeding after cesarean delivery. This was a barrier to obtaining “Baby-Friendly Hospital” status (Baby-Friendly USA, Inc., 2012), despite being a Magnet hospital credited by the American Nurses Credentialing Center for excellence in patient care – with a level III perinatal and neonatal unit. The medical center is a busy urban academic hospital with 5,847 infant deliveries in 2013.
An evidence-based pilot protocol for SSC in the operating room (OR) immediately following a cesarean delivery was implemented in order to provide clinical impact data. Immediate SSC in the OR helps newborns adapt to extrauterine life and assists with infant-parent bonding and breastfeeding success. SSC can decrease the amount of time the infant spends in the Neonatal Intensive Care Unit (NICU), resulting in fewer nursing hours and overall cost savings for both hospital and patients.
The EBP project was conducted with approval from the Institutional Review Board at Arizona State University with reciprocal hospital agreement. The 7-step Iowa Model of Evidence-Based Practice (EBP) guided the EBP project. Step 1: topic selection (discussed above). Step 2: EBP team was formed and met biweekly, with members including project lead (L&D nurse and DNP student), L&D nurse manager, surgical scrub technician, obstetrician, nursing representative from the nursery team, and anesthesiologist. Step 3: systematic evidence retrieval to support the “triggering" question. Step 4: EBP team critically appraised the evidence to build obstetric section stakeholder buy-in. Step 5: development of standards for the pilot SSC protocol. Step 6: 3-month implementation of the pilot SSC protocol for all mother-infant dyads admitted for scheduled or repeat cesarean delivery with a live, singleton fetus greater than 37 weeks gestation, with no pre-existing medical complications or fetal anomaly (n=193). Nursery staff tracked neonatal outcomes including temperature, respirations, glucose, and disposition during the two-hour transition after birth. These data were compared to historical data for mother-infant dyads meeting protocol inclusion criteria in the 3 months prior to protocol implementation (n=302). A double-entry process was used to verify the data. Data were analyzed using chi-square test to compare rates of SSC application and infant disposition, and paired t-test to compare pre- and post-protocol neonatal outcomes including temperature, heart rate, respiratory rate, and blood glucose. Step 7: evaluation of the overall SSC procedure, including process review, outcomes data, and staff feedback for protocol evaluation and modification.
There were no baseline demographic differences between pre- and post-intervention groups. Neonatal outcomes were significantly different for infant temperature (SSC = lower), heart rate (SSC = lower), respiratory rate (SSC = lower), and blood glucose (SSC = higher) between pre- and post-intervention groups. Notably, SSC resulted in statistically and clinically significant reduction in hypoglycemia (p = .002). Additional outcomes included an increase in exclusive breastfeeding by 38.3% (p=0.000) in the intervention group, and an 84% decrease in NICU admissions (p=0.000) in the intervention group. SSC in the OR is a valuable and feasible intervention following a cesarean delivery, with no additional expense to the facility, and potential for significant cost savings due to deceased NICU admissions. This EBP outcome supports the American Academy of Pediatrics’ (AAP) recommendation for SSC in the first hour after birth (AAP, 2005) and promotes exclusive breastfeeding, one of the Joint Commission’s mandated initiatives (United States Breastfeeding Committee [USBC], 2010) and Healthy People 2020 goal ((Office of Disease Prevention and Health Promotion, 2015). The average cost of NICU admission for a normal term infant for hypoglycemia and hypothermia is $76,164 (March of Dimes Perinatal Data Center, 2011). This EBP SSC intervention reduced NICU admissions by 84% for normal term cesarean section births, representing $2 million cost savings to the hospital over 3 months.
The results of this EBP study led to the medical center including the SSC intervention in all new hire training and required annual skills competency training for seasoned employees. This training addition required minimal resources and additional costs or staffing.
The SSC intervention is included in the existing charting system. This EBP project has been disseminated at the following events:
- Arizona Nurses Association Conference, October 2014 – poster
- Highlighted in the Chief Nursing Officer’s Weekly Journal - October 2014
- Medical Center’s Poster Walk Showcase, November 2014
- Voted as the “Best Practice” Innovation for the medical center
- Systemwide Shared Governance Conference April 2015 - podium
- Advance Practice Neonatal Forum in Washington, D.C., May 2015 – podium and poster
- Highlighted as part of the medical center’s Magnet Documentation and presented to Magnet recertification evaluators, July 2015
- Invited podium presentation at the National Phoenix Perinatal Associate Challenges in Obstetric Care Conference, April 2016
Susan Klein, DNP, FNP-C, OCN; University of San Diego Transition After Breast Cancer Treatment: Implementing Survivorship Care Plans
2014 Winners
Kathryn (Kim) Friddle, PhD, APRN, NNC-BC University of Utah College of Nursing Retinopathy of Prematurity: The Effects of Oxygen Saturation Targets in At-Risk Neonates PhD Program Chair - Dr. Patricia Aikins Murphy
Background and Significance: Retinopathy of prematurity (ROP) is a potentially blinding disorder estimated to affect 14,000 to 16,000 infants with 500-700 becoming legally blind annually. It is known to be associated with preterm birth, low birth weight, and the use of oxygen. An optimal oxygen saturation range of 85-93% is often targeted to minimize the risk of either hypoxia or hyperoxia. Maintaining premature infants within the targeted range can be difficult with many infants spending significant amounts of time both above 93% and below 85%.
Purpose/Objective(s) and/or Specific Aims : The purpose of this research was to evaluate whether the development of ROP can be explained by the average percentage of time in a 24-hour period that the infant spends out of the targeted oxygen saturation range in the weeks prior to the development of ROP or retinal maturity. Additionally, the effect of higher oxygen saturation targets while an infant is receiving 21% oxygen was evaluated to determine whether this increases the risk of developing ROP. Finally, the study addressed whether death before discharge can be explained using the average percentage of time during 24-hours that the infant spends out of the targeted oxygen saturation range.
Methodology/Procedures: The study used an observational, retrospective, and longitudinal design, tracking standard practice in a level IV referral center NICU. Weekly 24-hour histogram reports, generated from the Phillips IntelliVue™ Monitor detailing individual patient oxygen saturation levels, were collected and evaluated for the percentage of time the infant spent above and/or below a targeted saturation of 85% and 93%. Multinomial logistic regression was used to evaluate nested patient data of at-risk infants cared for at Primary Children’s Hospital, a free-standing children’s hospital, over a 3-year period. Data were entered longitudinally until retinal maturity/ROP occurred (N=241ROP study) or until death/discharge (N=250 survival study). Infants were excluded from both studies if ROP was present prior to admission, or death/discharge occurred without an eye exam or data collection. Survival analysis using a discrete-time hazard model was used to explain the risk of developing ROP (stage 1 or ≥ stage 2) or death, associated with the time above and below the targeted range, controlling for the effects of gestational age and birth weight using logistic regression. The ROP model included a cubic time trend to reflect the average change in probability of developing ROP, and the survival model used a quadratic time trend for the risk of death.
Results/Findings: The total time the infant was out of targeted saturation range had no effect on the development of ROP. However, for every 2.7% of the time the infant spent ≤ 85%, the risk for ROP increased by 48% (p<0.038), and the risk of death increased by 11% (p<.001). The percentage of time an infant spent >93% decreased their risk of ROP and death. For every 10% of time spend >93%, the risk of ROP decreased 21%, and the risk of death decreased 11%. The time breathing 21% oxygen was added into the regression equation at all levels, it was not found to be significant for the prediction of ROP.
Conclusion(s): The optimal saturation range for infants at risk for ROP is not known. These data raise concerns about the appropriateness of the current saturation targets of 85%-93%. This supports the current recommendation of many that the targeted saturation range for this population should be higher. A low saturation level of 85% cannot be recommended as safe given the results of this study. The upper limit of time for saturations >93% to be beneficial remains unknown and needs further research.
Implications/Recommendations for the Profession and/or Science: This is the first study to report the impact of the time a premature infant spends out of the targeted saturation range of 85-93%. It is also the first study to report the effects of high saturations while the infant is breathing 21% oxygen on the development of ROP. The current research study provides important information on the effects of time spent with both low and high oxygen saturations on the development of ROP and death. Infants in this study population largely represent infants in phase 2 ROP (31-44 weeks). It has shown that low saturations (≤ 85%) are detrimental, with increased risk for the outcomes of both ROP and/or death, while high saturations (> 93%) improves the risk of both of these outcomes. This study also supports the use of oxygen saturation histogram data in clinical practice to evaluate an infant’s ability to maintain a given saturation target to help guide respiratory management decision-making within this high risk population. These monitoring tools can help answer important clinical questions about the impact and management of low and/or high saturations.
Honorable mention went to:
Qiaohong Guo , PhD, RN, University of Massachusetts Amherst School of Nursing A Preliminary Model of Dignity Management in Hospice
Angela Smith Lillehei , PhD, MPH, RN, University of Minnesota School of Nursing Effects of Lavender Aromatherapy via Inhalation and Sleep Hygiene on Sleep in College Students with Self-reported Sleep Issues
Jessica Kozlowski, DNP, CPNP-PC Brandman University School of Nursing and Health Professions Pediatric Nurse Practitioner Management of Child Anxiety in the Rural Primary Care Clinic DNP Project Chair - Dr. Pamela Lusk
Background and Problem: Pediatric Nurse Practitioner (PNP) encounter children with concerns for a mental health disorder in their clinical practice, with only 20 percent of these children having any treatment often due to barriers to care such as poor mental health care access, social stigma, or other parental factors. Anxiety disorders are the most common pediatric mental health disorder an estimated prevalence of 5 to 18 percent. An estimated $247 billion is spent each year on childhood mental disorders including anxiety with 75 percent of these children presenting to the primary care setting for diagnosis and management. Because of the impact on children, families, and communities, children's mental disorders are an important public health issue in the States.
Purpose/Objective(s): The purpose of this capstone project was to offer evidence-based treatment option for PNP in the primary care setting for children with an anxiety disorder. The primary care setting in the model of care discussed by the Substance Abuse and Mental health Services Administration (SAMHSA –HRSA Center for Integrated Health Solutions) can be a location for screening (S) and brief intervention (B-I) before referral to subspecialty if needed. The brief intervention, Creating Opportunities for Personal Empowerment (COPE), is a manualized 7 –session program, that can be delivered by a trained PNP to offer skills similar to Cognitive Behavioral Therapy.
Procedures: This was a pilot study completed at a Federally Qualified Health Clinic in the rural Northwest area of Florida. A convenience sample of 14 children ages 8 to 13 years was utilized once they met the criteria of having an anxiety disorder based on DSM 5 criteria. Exclusion criteria included any mental retardation, psychosis, or current suicidal thoughts. The intervention, COPE appointments were 30 minutes in length and scheduled at the families preferred time. The core concept which is a subset of techniques in CBT was presented to the child; then reinforced through games, interactive activities, and finally real life application of these concepts.
Anxiety symptom reduction has been considered the gold standard of improvement after intervention which was measured utilizing the reliable SCARED symptom checklist with a score less than 25 equaling no anxiety symptoms. Level of functioning was assessed using the Clinical Global Impressions Scale. Children assess their improvement in functioning by answering the question “After the COPE program, how is your home and school life?” Improvement is seen with a score of 2 or higher (much improved to very much improved) which is consistently used in the literature with pediatric anxiety. Cognitive - behavioral skills learned through the COPE program were assessed through a 15 question content quiz given before and after all 7 sessions were complete. Finally, program satisfaction was measured through open-ended questions for both the parent and child.
Outcome(s): Children who participated had significant decreases in anxiety symptoms (13.88 points, SD = 17.96, 95% CI -1.13, 28.89) and on post assessment 50 percent of the participants no longer met criteria for an anxiety diagnosis. They also had increases in knowledge of cognitive – behavioral coping skills (M=11.38, CI 5.99, 8.26, p = 0.00) and 100% showed improved functioning at both school and home on self-evaluation. Evaluations by parents and children were positive with 100 % of participants and parents preferring delivery of COPE in the primary care setting and recommending the program to another child.
Conclusion(s): COPE visits fit into the fast - paced pediatric practice in 20 - 30 minute sessions. COPE sessions were billed and all were reimbursed by the insurance providers at the higher CPT code for time of over 50% of the visit in counseling (99214) indicating this is a cost effective intervention in primary care. Post COPE evaluations indicated improved patient outcomes. There was one child who had a worsening of anxiety score on SCARED after COPE delivery. This child was dealing with social changes that were identified during individual sessions. With the S-B-I-R-T treatment model in mind after COPE sessions were completed then the patient was referred to a mental health provider for a longer intervention.
Implications for Practice or System Change(s) : With the call to arms across both psychiatric and pediatric organizations to offer effective, evidence-based mental health treatment no matter the treatment location, the PNP is in a unique opportunity to intervene early in the child’s anxiety diagnosis. With early, effective interventions this anxiety diagnosis will be less likely to follow the child into adulthood.
The Triple Aim of Healthcare views successful interventions that are cost effective, patient centered and improve patient outcomes. The COPE program meets these three criteria, which was disseminated at the DNP Convention (Fa ll of 2014). PNPs continue to practice in the front lines in rural areas, with the largest need for mental health support. To offer this program to other PNPs this project will be presented at the National Association for Pediatric Nurse Practitioners conference in March. Journal submission has also been completed for consideration for the Journal of Pediatric Healthcare. The lead researcher continues to perform COPE in her daily practice, with 10 children completing since the project ended.
Kathryn Evans Kreider , DNP, FNP-BC, Duke University School of Nursing
2013 Winners
Nancy Crego, PhD, RN, CCRN University of Virginia Pediatric Sedation Safety Dissertation chair, Dr. Elizabeth I. Merwin
Background: Every year, thousands of children require sedation for diagnostic and interventional procedures. Despite regulations by accreditors and guidelines by professional organizations, adverse sedation events and variations in how sedation care is delivered continue to occur.
Purpose: This study presents a review of sedation standards shaping RN practice and exemplars of state Boards of Nursing sedation regulations in the United States.
Methods: The Pediatric Sedation Research Consortium (PSRC) database was used to learn more about RN sedation practices in diagnostic radiology; findings revealed that RNs often plan to achieve deep levels of sedation and administer combinations of two or more sedative medications for diagnostic procedures. Outcomes of sedation for cases where RNs monitored and delivered sedation alone were compared to outcomes of RN and physician teams and physicians working alone to deliver sedation. Cases in which RNs alone provided sedation had similar American Society of Anesthesiologists risk scores compared to cases with physicians alone and RN and physician sedation teams.
Results: Adverse event rates in sedated children range from 0.4% to 20.1% in the U.S., and include cases of desaturation, inadequate sedation, and respiratory depression requiring bag valve mask ventilation. The rate of sedation adverse events when RNs provide sedation is unknown due to small sample sizes and few RNs participating in reported studies. Limitations of most investigations regarding pediatric sedation include frequent use of single site samples, reporting on only one type of procedure, and using sample sizes that are underpowered to detect sedation adverse events that are estimated to occur once in many thousands of cases. Many studies of RN sedation practice have examined a particular aspect of sedation care, such as determining differences in outcomes of sedation using different sedative medication regimens or the number of failed sedations; these outcomes are not compared to other sedation provider outcomes. As a result, these studies provide limited information on the safety of RN administered procedural sedation, the factors that increase the likelihood of adverse sedation events, and the differences in sedation administered by RNs compared to other sedation providers. Findings revealed that cases in which RNs alone or physicians alone monitored and delivered sedation had lower odds of experiencing adverse events than when sedation was administered by RN and physician teams.
Conclusion: This study revealed inconsistencies in state Board of Nursing regulations and in RN sedation care standards in the U.S. Data from this study could be used to improve RN sedation care processes, and guide the development of consistent nursing sedation licensing regulations, hospital standards, and policies. The lack of data on RN sedation practice and safety hinders the development of evidence-based regulations. Differences in sedation care may be related to the type of specialist providing sedation, their scope of sedation practice, and methods used to induce sedation. Sedation is performed by a variety of health care providers including registered nurses (RNs), but there are limited data on current regulations governing RN sedation, descriptions of RN sedation practice, or comparisons of outcomes of sedation by different types of providers.
Erica Schorr , University of Minnesota
Yafen Wang , Case Western Reserve University
Jennifer L. Titzer, DNP, RN, RT(R), RCIS University of Southern Indiana Nurse Manager Succession Planning: Strengthening Health Systems for the Future Capstone Chair, Dr. Maria R. Shirey
Background: Traditional nurse manager selection methods usually result in promoting excellent clinicians lacking formal education and mentoring. Ineffective nurse manager selection increases role stress, unhealthy work environments, poor patient outcomes and turnover rates. Inconsistent leadership results in a loss of community and employee confidence. Competent and effective nurse managers contribute to a healthy work environment, improved employee morale and favorable outcomes. Succession planning increases nursing leadership competence and continuity. Ensuring a competent nurse manager pipeline demands deliberate and strategic succession planning methods. Healthcare lags behind other business industries in strategic succession planning threatening the future nursing leadership pipeline. Evidence regarding succession planning outcomes is limited and hinders implementation efforts. Deliberate and strategic implementation and evaluation of successful planning is critical.
Purpose: The purpose of the capstone was to develop, implement, and evaluate a nurse manager succession plan at an acute care hospital. The primary project objective was to create a strategic method for identifying and developing intellectual talent creating an internal leadership pipeline. Development of an internal leadership pipeline with the intent of reducing recruitment and replacement costs, decreasing nurse manager turnover, and increasing nurse satisfaction was the end goal.
Methods: Nurses working in an acute care hospital were recruited for participation in a 12 month leadership program. Recruitment included completion of a formal and systematic application process. A quasi-experimental one-group pre-test/post-test design evaluated program outcomes. The measurement tools included the Leadership Practices Inventory (LPI) and the Nurse Manager Skills Inventory (NMSI).
Results: A strategic succession planning process was developed at St. Mary’s Medical Center targeting the nursing director position. All staff nurses not formally in leadership roles were invited to apply. Selection was based on an objective scoring worksheet and interview process. There were a total of 12 participants selected and invited into a 12 month leadership development program. Six months into the program, one participant transferred to another facility due to re-location. The remaining 11 participants completed the program. Monthly, six-month, and final program evaluations were overwhelmingly positive and the pre/post leadership and management surveys indicated statistically significant increases in participants’ competency perceptions (p < 0.05). Five nurses from the leadership pool were promoted either during or after program completion (three nursing director and two unit coordinators). In addition, three participants transitioned into quality analyst, staff development specialist, and informatics roles.
Conclusion: The model created for the inaugural program provided a pilot that can be evaluated and adapted accordingly. Ongoing evaluation beyond the initial customer satisfaction and learning and growth metrics will provide a cost benefit analysis and determine a return on investment as well as the impact on the overall nursing satisfaction. Additional recommendations included offering similar programs to professional staff outside of nursing ensuring an organization wide leadership pipeline.
Joelle Hargraves , Chatham University
Rebecca Russo-Hill , Duke University
2012 Winners
Oleg Zaslavsy, PhD University of Washington Longitudinal Dynamics in Indicators of Frailty: Predictors and Long-Term Outcomes Dissertation chair, Dr. Barbara B. Cochrane
Background: Frailty is a common geriatric condition with a wide array of sequelae, including increased risks of mortality, morbidity and disability. Despite its long conceptual and operational history in research and publications, frailty and mechanisms of frailty development are still poorly understood. A detailed description of trajectories of frailty indicators was needed to provide vital insights on unfolding longitudinal dynamics involved in the development of frailty.
Purpose: The specific aims of this study were to: (I) Describe longitudinal (-10 years) trajectories of change in musculoskeletal and neuro-cognitive indicators of frailty in older (>/=65 years) women enrolled in the Women's Health Initiative (WHI) Clinical Trial; (2) Estimate the extent to which baseline factors (e.g., demographic characteristics, health status and behaviors) are associated with a likelihood of membership in the derived longitudinal clusters; and (3) determine the extent to which membership in longitudinal trajectories predicts the incidence of clinically relevant geriatric health outcomes (i.e., mortality and hospitalization) over 5-years of follow up in a model adjusted for all other baseline predictors.
Methods: Data for these analyses came from the WI-II, which included three randomized controlled clinical trials (CTs). Details of the design, recruitment strategies, data collection methods, and tabulations of baseline data are published elsewhere (Anderson eta!. (2003). Implementation of the Women's Health Initiative study design. Annals of Epidemiology, 13, S5-17.). In the present stud y we focused on data from \Vomen ages 65 years and older (at baseline) who emolled in one or more of the CTs and also consented to participate in 2005-2010 Extension Study. The final sample included 19,891 women. Measures of frailty indicators (e.g., physical performance-based tests), demographic, health behavior and status, comorbidity, personality and social factors were collected using well-established objective and self-report measures. Study outcomes of hospitali zat ion and mortality were based on mmual medical history update questionnaires from participants in the 2005-2010 WHI Extension Study. These self-reported outcomes were then used to obtain medical records for adjudication both locally and by a panel of central adjudicators. Latent class growth models were used to identify relatively homogeneous clusters of individuals following similar longitudinal trajectories of change. Trajectory parameters were estimated using maximum likelihood methods. A high-order polynomial function (i.e., quadratic) was fitted to the data, and parameters were estimated to define the shape of the trajectories and the probability of trajectory group membership. The number of clusters were chosen based on standard statistical selection criteria. Partial propmtional odds models were used to fit the data and test the effect of predictors on trajectory group membership. Cox proportional hazard models were used to predict mortality and first-incident overnight hospitalization in sequentially-fitted models.
Results: Study findings demonstrated a high degree of heterogeneity in longitudinal dynamics of individual frailty criteria. In addition, results showed that age, soda-demographic variables, health status, health behavior, environmental factors and personality traits are important determinants of individual frailty criteria, but their effect on frailty phenotype is complex, presumably due to the multidimensional nature offrailty phenomenon. Thirdly, the magnitude of risk carried by a membership in a certain longitudinal group for each of the defining elements of frailty is closely linked to the distance of that trajectory estimates from the one that represents the most optimal criterion-specific functioning over time. The futher the distance between trajectory estimates of an individual who maintained the highest level of performance (specific to that indicator) and those who demonstrated less optimal functioning, the higher the risk of incidence of adverse health events.
Conclusion: The study provided an empirical determination that distribution-based cross sectional partitioning of frailty criteria seems to be a valid method for defining frailty, given that elderly women maintained approximately similar levels of functioning over time without demonstrating clear accelerated or decelerated longitudinal patterns.
Tiffany Moore , University of Nebraska Medical Center
Erin Harnett, DNP New York University Integrating Preventive Dental Care in a Pediatric Oncology Center Capstone Project Advisor, Dr. Barbara Krainovich-Miller
Background: Dental caries is an infectious process, which may cause serious problems for children both during and after cancer treatment (Haytac, Dogan, & Antmen, 2004; Yeazel et al., 2004). The American Academy of Pediatrics (AAP, 2009, 2010) and the American Academy of Pediatric Dentistry (AAPD, 2008, 2010) recent policies have recommended that primary care providers perform oral assessment, provide preventive dental care during routine well child visits, and refer children to the dentist by age one year. The Surgeon General mandated that the evidence-base about the oral-systemic connection be used to improve the health of all by implementing it in the curricula of all health care practitioners and that a comprehensive oral assessment be a gold standard of practice (IOM, 2011) for the public. The needs assessment of this project uncovered the glaring gap between existing extensive evidence and recommendations regarding the need for oral health assessment and current practice. Although children being treated for cancer are seeing the pediatric oncology team on a regular basis, they are not receiving expected normal pediatric or dental preventive care prior to or during cancer treatment. This issue is of paramount concern as the development of oral problems during childhood cancer care results in pain, fever, delay in treatment, additional hospitalizations, and increased cost to families/significant others and the health care system which, in turn, impacts the public at large (Carrillo, Vizeu, Soares-Junior, Fava, & Filho, 2010; da Fonesca, 2004).
Methods: A Clinical Microsystems approach was used to ensure successful implementation of the project conducted by the DNP (PNP) student. She collaborated with members of a university dental school and the leadership of the major urban outpatient pediatric oncology cancer center and IRB to gain approval to implement her educational project for the pediatric oncology providers (pediatric oncology MDs, NPs, RNs) at the cancer center. The participants: (a) completed a pre-survey assessing their oral systemic health knowledge, current oral health practice, perceived barriers to dental referral and attitudes toward incorporating preventive oral health care into their oncology practice, and (b) attended an oral health educational intervention and fluoride varnish skills lab conducted by the DNP candidate (PNP), dental residents and dental fellows where they learned how to perform an oral assessment to detect the existence of carries, make a referral for caries if identified, and how to apply fluoride varnish on children who were to be treated for cancer. Participant knowledge and skills were assessed after the educational program and chart data indicated whether these new competencies were used with the pediatric population. A one year follow-up survey was instituted.
Results: The results of this innovative capstone project indicated that pediatric oncology providers were in a unique position to provide preventive oral health care and improve oral health outcomes in pediatric cancer patients. The educational program increased their oral health knowledge of the providers; a review of chart data indicated that children who came to the cancer center were now receiving oral health assessments, had fluoride varnish as needed, and referrals were being made as needed. In this center only children who were seen by a dental resident once a week had ever received this standard of care. Prior to this project none of the oncology providers (MDs, NPs, RNs) had included this in their practice. At the end of the projects, data indicated that children being treated by oncology providers, who participated in this project, had increased from zero to 100%. This educational program was adopted as a standard of practice at the center and all providers complete this oral health program. Fluoride varnish is now on the standard formulary; all pediatric patients receive this gold standard of oral health care prior to treatment. One-year follow up survey data indicate that this practice continues to be implemented by all providers. The improvement on care delivery demonstrated in this project may be replicated in other settings and serves as a model for pediatric oncology clinics across the country. Feedback from invited as well as competitive presentations at local, regional, and national interprofessional conferences, as well as quality improvement data provide evidence that this clinical project is realistic and can be easily replicated in other settings. Currently, it is being implemented on the in-patient unit at this major medical center.
Implications for Practice, Education, and Policy: The project has several implications for practice. DNP prepared advanced nursing practice NPs need to assume a clinical leadership role and instruct other providers regarding evidence-based standards of care that need to be instituted. Specifically DNP prepared PNPs must assume the role of educating health care providers who care for both well and chronically ill children to include oral health care in acute and chronic healthcare settings and schools. This project also has important implications for pediatric cancer survivors who may develop late effects from their cancer treatment that will require dental care. Interprofessional education and practice collaboration between medical, nursing, and dental providers must become an integral part of health care delivery systems. The implications for education of DNP programs that prepare NPs is that DNP graduates must obtain clinical leadership competencies that include: (a) use of an appropriate implementation framework, (b) the ability to critically appraise and synthesize the best available evidence in order to change the practice of health care providers, (b) making recommendations and creating policies based on the best appraised evidence, and (d) teaching oral health competencies and best practices as part of the standard of care regardless of the population. It further highlights the need for all health care provides to receive oral-systemic health care knowledge and related competencies during their education. The specific implications for policy are at the institutional practice setting level. When successful results are obtained from evidence-based clinical improvement projects, such as Dr. Hartnett’s, these practices will be sustained when they demonstrate positive clinical outcomes and become the expected gold standard policy.
Vicky Grossman , Duke University
Carrie Kairys , Johns Hopkins University
Contact Information
Please direct any questions related to this awards program to [email protected] .
Congratulations to the 2023 Award Recipients!
Ruth Tretter , PhD, RN Idaho State University (PhD Exploring RV-dwelling American Nomads’ Experiences When Seeking Healthcare Program Director - Mary A. Nies
Christina Jones , DNP, PMHNP Arizona State University Teen Mental Health Literacy: A School District’s Post-Pandemic Response Program Director - Diane Nunez
Amber High , DNP, CRNA University of Texas Medical Branch A Novel Peer Support Project: Quality Improvement for Workforce Well-being Program Director - Sharron Forest

Home > ETDs > DNP Projects
Doctor of Nursing Practice (DNP) Projects
Dnp projects from 2021 2021.
Building Excellence through Shared Governance and Continuous Process Improvement , Deborah Reitter
Streamlining Care for Children with Autism Spectrum Disorder , Siavash Rostami Jafarabad
Nurse Practitioner-Led Care Pods: A Team Communication Enhancement Model , Miranda Saint-Louis and Miranda Saint Louis
Use of Simulation to Improve Nurse's Response to COVID-19 Code Blue: A Literature Review , Charity Shelton
Using Simulation to Improve COVID-19 Code Blue Outcomes , Charity Shelton
Utilizing Group Prenatal Care to Support Underserved Pregnant Women , Kathleen Shrader
Utilizing Tracer Methodology to Evaluate the Effectiveness of a Hospital Antimicrobial Stewardship Program , Christine Smyth
Patient Placement Matters: The Impact of Unnecessary Lateral Movement on Patients , Jacqueline Strinden
The Effects of Naloxone Education Among Adults in Alameda County , Patricia Ronnica Tinglin
Prevention of Abusive Head Trauma Using an Educational Program for Parents/Caregivers , camile williams
Utilizing a Stress and Coping Model into a Preventive Abusive Head Trauma Parent/Caregiver Educational Program , Camile Williams
Successfully Spreading Improvement Work Using a Proven Framework , Rachel Lynn Wyatt
DNP Projects from 2020 2020
Ultrasound-Guided Peripheral Intravenous Catheter Insertion for Nurse Practitioners , Alvin Joseph Abad
Preconception Screening for Family Planning , Nnenna Abaeze
Pre-conception Screening Tool , Nnenna Abaeze
Healthcare Provider Education: Adult Jamaicans with Type 2 Diabetes , PATRICIA ANDERSON
Bisphenol-A (BPA) and Breast Cancer: Utilizing Risk Assessment and Education to Improve Preventative Care , Ashley Catherine Babcock
Continuous Glucose Monitoring and Diabetes Management During Pregnancy , Nicole Beamish
Workplace Violence: An Urgent Call for Integrated Staff Education in Acute Care Hospitals , Nicole Bellisario
Valley Fever: Education for Primary Care Providers and Allied Health Care Professionals , Michelle Elizabeth Bergen
Improving Clinicians’ Access to Patient Education and VA Resource Information , Ella Bermudez
Reducing Frustration with Wait Times Utilizing Technology and Education: A Patient Satisfaction Improvement Model , Tiffany Brown
Identification of Victims of Human Trafficking: Leading Change through a Global Pandemic , Connie Clemmons-Brown
Earlier Palliative Care Referrals for Nephrology Patients , Jerold Cohen
Implementation and Evaluation of Whole Health Opioid Safety Shared Medical Appointments in a Veteran Population: A Quality Improvement Study , Sherry Cox
Chief Nurse Executive Work Engagement: System Leadership Through a Natural Disaster, Strike, and Pandemic , Ryan Fuller
Program Implementation for New Graduate Nurses to go from Moral Distress to Moral Courage and Beyond , Melinda Furrer
Wound and Stoma Care Education for Primary Care Providers , Deanna Garza
Transformational Leadership for Frontline Leaders , Marta L. Hudson
USP Compliance: A Hazardous Drug Safe Handling PPE Toolkit for Infusion Nurses , Cynthia Huff
USP Compliance: A Hazardous Drug Safe-Handling Quality Improvement Project for Ambulatory Care Infusion Nurses , Cynthia Huff
Preceptor as Frontline Leader Utilizing Emotional Intelligence , Dwanette Judkins
Technology-Based End-of-Life Planning for an Underserved Population , Haley Kirkpatrick
Increasing Access to Medicare Annual Wellness Visits in Primary Care; Utilizing Registered Nurses as part of an Interdisciplinary Team Based Approach , Iyo Kubota
An Online Self-Directed Learning Module for Regional Stroke Survey Success , Winchell Rodriguez Kuttner
Application of Sustainability Framework for Quality Improvement in an Integrated Health System , Cristine Lacerna
Using Simulation for Oncology Nursing Competency Evaluation in Hospitals , DANA N. LITTLEPAGE
Using Simulation for Oncology Nursing Competency Evaluation in Hospitals , DANA LITTLEPGE
Optimizing Screening Mammography: Educating Underserved Individuals with Limited English Proficiency , Yao Luo
Improving Clinical Communication and Collaboration Through Technology , Michelle Machon
Initiating PrEP in Primary Care: Addressing the Adolescent and Young Adult High Risk Populations , Igor G. Mocorro
Fall Reduction Project in a Skilled Nursing Facility , Jalpa Patel
Implementing Virtual Sitters to Reduce Falls and Sitter Costs , Asia QuoVadis Williams Plahar
Implementation of Artificial Intelligence Initiated Rapid Responses to Reduce In-Hospital Cardiac Arrest , Alicia Potolsky
A Performance Improvement Nursing Fellowship to Enhance Timely Access to Care , Cheryl Reinking
Competency-Based Practicum Evaluation Tools for Family Nurse Practitioner Programs , Angelica Renteria
#Leadershipaccelerated: A Coach Mindset Focused Leadership Development Program , Diane Rindlisbacher
Illicit Substance Use in Acute Care Hospitals: Creating a Safe Environment , Christina Sanford
Improving Nurse Engagement through Unit Practice Councils , Pavna Sloan
Improving Nurse Engagement Through Unit Practice Councils: A Literature Review , Pavna Sloan
Unaddressed Challenges for the “Most Honest and Ethical Profession:” A Pilot Study of Web-Based Learning Strategies to Prevent Moral Distress , Kelly Straight
Wound Care Education for Primary Care Providers at a Regional Medical Center , Zaira Torres
An Education Program for Novice Nurses to Increase Case Management Knowledge , Emily Trefethen
Creating a Thriving Informatics Culture , Nicholas Webb
Reducing the Second Victim Phenomenon: Promoting Healing with Caritas Coaching , Shanda N. Whittle
Eliminating Barriers to Chinese American Diabetic Patients: Implementation of Diabetic Cantonese Group Visits , Sabrina Wong
Development of a Disaster Preparation Toolkit to Improve Community Resilience , Tiffany Wong
Evidence-based Suicide Screening and Prevention Protocol for Licensed Nursing Staff , Rose Zhang
Evidence-based Suicide Assessment and Prevention Training for Licensed Nursing Staff , Rose Waithira Zhang DNP(c), MSN-FNP-BC, BSN, RN
DNP Projects from 2019 2019
Caring Science Education: The Essence of Professional Practice for the Registered Nurse , Linda C. Ackerman
Collaborative Care in College Health: Care Team Training to Support Improved Integration , Elizabeth Adams
Implementing Foot Care Program in a Rural Clinic , Maliheh Bakhshi
Coaching Nurse Leaders in Conflict Management and Team Building to Improve Retention , Jeanette Black
Improving Nurse-Physician Collaboration: Building an Infrastructure of Support , Marshall Blue
Adolescent Sexual Reproductive Health Course: A Mixed Media Intervention and Quality Improvement Project in a School-Based Setting , Stephanie Calabrese
Implementation of a Mentor Program to Support Nurse Retention: A Pilot Project , Lucy Camarena
Clinical Pathway Adoption to Aid in Medication Calendar Procurement in a Pediatric Oncology Clinic , Cinnamon R. Chavez
A Toolkit for Administration of Antipsychotic Medications in Nursing Homes , Nino Dantes Flores
Applying the Model of Interrelationship Environments and Outcomes to Simulation for Nurse Leaders to Enhance the Professional Practice Work Environment: Creating a Mile One Nurse Leadership Simulation Toolkit , Alicia Garcia-Cisneros
Expanding Magnetic Resonance Imaging Access for Patients with Cardiovascular Implantable Electronic Devices , Rosalie Geronimo
School-Based Mental Health Screening: Improving Outcomes Through Interprofessional Communication and Collaboration , Tiffany Gishizky
Standardizing Mammogram Screening in Primary Care: Integrating an Evidence Based Approach , Lacrisha Go
Improving Access to Youth-Friendly Health Services in a Rural California Community , Elena Higley
Increasing Nursing Policy and Advocacy Engagement , Marketa Houskova
LARC Method Appropriateness in Substance Use Treatment: A Quality Improvement Project for Integrated Care , Malia Johnson DNP, FNP; Alexa Curtis PhD, FNP-BC; and Neda Afshar DNP, FNP-C, MSN, CGRN
Nursing Leadership Beyond 2020: A Succession Plan , Janet Jule
DNP Project: Development of a Nurse-Led Pop-Up Clinic Model in San Diego , Jennifer King
The Development and Implementation of Nurse-Managed Community-Based Medication Assisted Treatment Services for an Underserved Non-Metropolitan Northern California Community , Lauren Knapp
Strengthening the Advanced Practice Clinician Workforce Pipeline Through Preceptor Education and Support , Tarina Levitt-Trujillo
Developing a Culturally Tailored Support Program for Chinese Cancer Patients , Yan Li
A Quality Improvement Project to Implement Shared Medical Appointments for the Management of Type 2 Diabetes in Latino Patients , Denisse Maldonado
Enhancing Health Literacy Using Teach Back Method to Increase Patient Adherence to , Tram Mendoza
Nursing Practice Meets Theory , Debra J. Morton
Operationalizing a Theoretical Framework to Improve Patient Perception of Care , Debra J. Morton
Implementation of a Simulation-based Interprofessional Patient Safety Program , Mariko Nowicki
Hepatitis C Treatment in High Risk Patients: Implementation of a Successful Community Focused Program , Annie Pedlar and Jodie Sandhu DNP, FNP-C
Increasing Long Acting Reversible Contraception Use in Primary Care: Removing the Barriers , Jessamyn Phillips
Enhancing Nutrition Education for School Aged Children; a Preventive Health Measure and Quality Improvement Project , Fanny M. Powell
Increasing Utilization of Motivational Interviewing to Promote Pediatric Oral Health , Ulyses Reamico
Burnout, Depression and Suicide Prevention for Nurses in High-Intensity Settings , April Ritchie
Burnout, Depression and Suicide Prevention for Nursing Staff in High-Intensity Settings , April Ritchie
Reducing Critical Care Nurse Distress During End-of-Life Care: Change of Practice Intervention , Alexis S. Roschitsch-Preszlowski
Adopting Complex Case Management Competencies , Phyllis Stark
Nurse Manager Succession Planning: Building a Leadership Pipeline for the Future , Katie Stephens
The Impact of a Nurse Engagement Model Implementation on Patient Outcomes , Karen Strauman
Improving Chronic Hepatitis B Virus Screening at a Safety-Net Primary Care Clinic , Uwaezu J. Umeh
Addressing Childhood Obesity in a Rural Community Using Motivational Interviewing , Chituru Uwaoma
DNP Projects from 2018 2018
Promoting Transgender Cultural Awareness and Sensitivity through Education: It Starts with a Pronoun , Jacob Adkison
Colorectal Cancer Screening in Veterans Affairs , Neda Afshar
Improving Management of Obstetrical Emergencies: Using Simulation-Based Training , Amira Amatullah
Advanced Search
- Notify me via email or RSS
- Collections
- Disciplines
Author Corner
- Submit Research
- Nursing and Health Professions Submission Guide
Library Links
- Gleeson Library
- Zief Law Library
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright

Doctor of Nursing Practice project focuses on multidisciplinary collaboration to increase ICU patient early mobility

When considering a Doctor of Nursing Practice (DNP) as the next step in their education, many nurses share concerns regarding the program’s final project. Unlike a traditional doctoral dissertation, the goal of a DNP project is to allow students to showcase their ability to translate knowledge and research into practical applications and solutions to real-world problems, impacting health care outcomes at a systems or population level.
At UC College of Nursing, students work with faculty advisors to choose a DNP project topic that relates to their advanced-practice specialty. The nature of projects varies and can include:
- A quality improvement initiative
- Implementation and evaluation of evidence-based practice guidelines
- Policy analysis
- Design and evaluation of new models of care or health care programs
To provide additional insight into the planning and steps of a DNP final project, we interviewed Paige Dahlke, BSN, RN, CCRN, an adult-gerontology acute care DNP candidate whose project ranked top at the college’s Annual Doctoral Student Project Showcase .
Dahlke received her Bachelor of Science in Nursing from the University of Northern Colorado in 2016, before relocating with her husband to Dayton, Ohio where she worked closely with ICU nurse practitioners at Kettering Health Dayton.
“Watching my leadership exercise higher level thinking when making impactful decisions for patients inspired me to go back to school,” she says. “I enjoyed caring for critically ill patients and wanted to progress in my ability to care for them, so I decided the DNP in adult-gerontology acute care program was the path for me, since it allows me to not only care for patients at a higher level, but also implement quality improvement projects, teach and so much more.”
Given her previous work experience, Dahlke decided to pursue a quality improvement project focused on early mobility interventions for ICU staff.
Paige Dahlke, RN
“ICU patient care requires life-saving treatments that frequently relate to increased immobility. My literature review showed that prolonged immobility is detrimental to all systems and functional ability; even when patients recover from what landed them in the ICU, they’re still not doing great due to adverse effects such as ICU-acquired weakness,” Dahlke shares. “Getting patients up and moving leads to better patient outcomes, decreased length of stay, increased functional ability and better recovery after illness.”
Aware that the lack of collaboration among different disciplines providing patient care in the ICU is a consistent barrier to early mobility intervention completion, Dahlke decided to create and deliver an education module showcasing the safety and feasibility of early mobility interventions and shared a Level of Function Mobility (LOF) scale to assist in consistent care and seamless communication for care providers in the ICU.
Dahlke partnered with Kelsey Schweikert, BSN, RN, clinical nurse manager at Kettering Health, to present the education module and explain the LOF scale at the hospital’s ICU multidisciplinary meeting. She also showed where the LOF mobility scale and documentation for rating would be found in ICU patient rooms. To assess staff perceptions of the intervention and interdisciplinary collaboration, Dahlke collected surveys pre- and post-LOF scale use, in addition to data on length of stay and Morse Fall Risk Assessment before and after intervention and scale implementation. A statistical analysis showed an improvement in ICU length of stay, change in Morse Fall Risk and staff perceptions of early mobility. As the changes were not statistically significant, Dahlke concluded that, although the improvement in each of the metrics shows potential for the project, further evaluation—including longer implementation and additional resources—is necessary to potentially produce statistically significant results.
“My goal is to decrease the burden of one single discipline to complete early mobility interventions within the complex ICU,” says Dahlke. “A multidisciplinary approach will encourage collaboration and improve patient outcomes.”
When asked about her steps towards a successful DNP project, Dahlke praises the support she has received at the UC College of Nursing.
“Dr. Eilleen Werdman, my project chair, has been supportive of the project since day 1. DNP projects entail three well-defined phases—planning, implementation and data collection—each covered throughout the classes that walk you through the process for a successful project. You follow a well-defined process guided by faculty and your chair.”
Dahlke, who will welcome her first baby in July, graduate in August and move alongside her husband in September, is excited about her future professional options.
“I feel that the DNP has prepared me to do anything I want in my career. I may pursue cardiology or pulmonology, or another specialty. Even if I end up not going back to work in the ICU, I’m glad to have contributed to patient outcomes through my project,” she says.
Want to learn more about our DNP program? Let us know here .
- College of Nursing
Related Stories
Uc researcher dedicated to improving care for family caregivers.
November 2, 2022
UC researcher Tamilyn Bakas has received a $3 million National Institutes of Health grant to test her intervention program for family caregivers of stroke survivors.
UC Nursing interim dean shepherds compilation of workplace violence research
June 16, 2023
Interim Dean Gordon Gillespie served as guest editor of a special edition of the Journal of Emergency Nursing on workplace violence in emergency departments. Read more.
National rankings highlight UC’s co-op program, innovation
September 12, 2022
The University of Cincinnati’s co-op program stands at No. 4 in the U.S. News & World Report’s latest rankings, continuing its historical placement among the top five co-op programs in the country — and No. 1 for co-op among public universities. The latest 2023 issue of the magazine’s influential “Best Colleges” guide ranks UC in the top tier, including among the “most innovative among national universities,” (No. 68) — UC’s first-ever ranking in that category.

IMAGES
VIDEO
COMMENTS
PhD in Nursing vs. DNP: Put simply, the PhD in Nursing is a research doctoral degree, and the DNP is a practice doctoral degree. ... PhD in Nursing students defend a dissertation, and DNP students present a scholarly project. Both PhD- and DNP-trained nurses should be prepared to lead multidisciplinary teams that address health care issues.
The DNP is the terminal practice degree signifying a clinical expert who conducts DNP projects or QI to improve patient outcomes. The PhD is the terminal degree to conduct research in contributing to new knowledge and testing existing knowledge. The Table summarizes DNP and PhD terminology.
DNP VS. Ph.D. - 12 Key Differences Between DNP And Ph.D. In Nursing Written By: Pattie Trumble, MPP, MPH ... The Ph.D. includes a dissertation project; the DNP includes a capstone project. All Ph.D. programs, be they in nursing, mathematics, English literature or political science, require the completion of a dissertation, which is a long piece ...
A DNP project's collaborative and integrative experiences reflect the development and provision of safe, effective, timely, efficient, equitable, and person-centered care aimed at advancing health outcomes. The impact of UMSON DNP projects will reshape health care in the United States. View the List of DNP Projects.
The D.N.P. is a practice-focused degree that prepares nurses to improve the health of people and populations through practice, bold system change, as well as translation of research to patients and populations. This is the nurse who not only knows how to treat the bullet wound but also works with the community to reduce gun violence that ...
8 steps to completion. Students should take these eight steps to complete their doctor of nursing practice (DNP) projects. Identify and obtain approval for the area of interest. Write a proposal. Create a project timeline. Acquire institutional review board approval (if needed). Implement project.
Whereas PhD students typically complete original research to obtain the degree, DNP students complete a quality improvement project. Both are important to the advancement of nursing and quality patient care. The PhD student's project might focus on a new treatment intervention for example, while the DNP student's project might use the ...
DNP vs PhD standards for admission are similar in many ways. DNP programs and PhD programs both typically require: ... A DNP final project also distinguishes the DNP degree. Following the AACN "DNP Essentials" for the final project, the DNP candidate will: ... Independent research projects are followed by a dissertation on a topic of ...
The DNP degree is a practice doctorate. The PhD is a research doctorate. Graduates of PhD programs are prepared to conduct independent research and disseminate their findings. The DNP will provide graduates with the skills and tools necessary to assess the evidence gained through nursing research, evaluate the impact of that research on their practice and, as necessary, make changes to enhance ...
The two terminal degrees in nursing, the Doctor of Nursing Practice (DNP) and Doctor of Philosophy (PhD), are complementary degrees in moving the discipline of nursing forward. The role of nurses with either doctoral degree is discussed related to the overall stewardship of the nursing profession. Core elements and key differences between the ...
The Capella doctoral experience offers a good comparison of the two types of final project. The Capella dissertation is a traditional five-chapter research document that you'll develop as you work with a faculty mentor and dissertation committee members. It's meant to be a work of high-quality academic research that contributes to your ...
Like any other dissertation, this final project adds to the existing body of knowledge through original research done by the learner rather than finding a solution to an existing issue, which is the goal of a DNP final project. Choosing Between a DNP vs. PhD in Nursing.
The goal of the DNP program is to provide nurses with the foundation to excel in advanced clinical nursing practice. In contrast, the Ph.D. is more research-focused and may be better suited for pursuing a career in academia. DNP programs require clinicals or practicals, and the Ph.D. programs require research for a dissertation.
The professional doctorate typically requires students to complete a dissertation or project to fulfil the requirements of a doctoral degree (CGS in the USA, 2007). In 2015, the American Association of Colleges of Nursing (AACN) issued a report from the Task Force on the implementation of the DNP with a section addressing DNP projects.
program. A master's thesis is the capstone project associated with a master's degree, a doctoral dissertation is the original, creative project associated with a doctoral degree, and a DNP p roject is the final project submitted as part of a Doctor of Nursing Practice degree. Theses, dissertations, and DNP projects are
In A Nurse's Step-By-Step Guide to Publishing a Dissertation or DNP Project, award-winning author Karen Roush guides readers through the process of reworking a dissertation or DNP project into a high-quality manuscript and honing their writing skills. Roush then provides a step-by-step guide through the publication process, providing all the ...
Also included are theses from the USU Postgraduate Dental College, which was established in 2010. As theses and dissertations are completed each year, the Archives adds those documents to the online collection. Additionally, the collection includes Doctor of Nursing Practice (DNP) projects from the Daniel K. Inouye Graduate School of Nursing.
Navigating the DNP project was a large category in this study and included many aspects of developing, engaging in, completing, and disseminating the DNP project. Eleven of the 15 participants in this study described how they used their skills and established relationships. ... Mentoring students engaging in scholarly projects and dissertations ...
Sample DNP projects. A resource of the honor society of nursing, Sigma Theta Tau International and the only digital repository solely dedicated to openly sharing works created by nurses. Includes full-text nursing research and evidence-based practice materials. Part of the Digital Commons Network. Includes a collection of DNP projects.
The DNP projects of the 2020 graduates cross geographical and discipline boundaries to bridge gaps in evidence and practice. Self-described change experts, their impact on quality outcomes for patient-centric healthcare will be recognized across myriad ...
Excellence in Advancing Nursing Science Award for an outstanding dissertation from a student in a PhD in nursing (or DNS program). A dissertation is an original research project that focuses on advancing nursing science and developing new evidence with the potential to guide nursing practice. To apply, please fill out the online application.
DNP Projects from 2024 PDF. Fostering Interprofessional Collaboration in Community College Mental Health Centers: A Quality Improvement Project, Sara Jane Hamilton. PDF. Nurse-led Telehealth Visits for Patients with Multiple Sclerosis During the COVID-19 Pandemic and Beyond, Eun Hye Kim. PDF
DNP Projects from 2021 PDF. Building Excellence through Shared Governance and Continuous Process Improvement, Deborah Reitter. PDF. Streamlining Care for Children with Autism Spectrum Disorder, Siavash Rostami Jafarabad. PDF. Nurse Practitioner-Led Care Pods: A Team Communication Enhancement Model, Miranda Saint-Louis and Miranda Saint Louis. PDF
When considering a Doctor of Nursing Practice (DNP) as the next step in their education, many nurses share concerns regarding the program's final project. Unlike a traditional doctoral dissertation, the goal of a DNP project is to allow students to showcase their ability to translate knowledge and research into practical applications and solutions to real-world problems, impacting health ...