How to Write Limitations of the Study (with examples)
This blog emphasizes the importance of recognizing and effectively writing about limitations in research. It discusses the types of limitations, their significance, and provides guidelines for writing about them, highlighting their role in advancing scholarly research.
Updated on August 24, 2023

No matter how well thought out, every research endeavor encounters challenges. There is simply no way to predict all possible variances throughout the process.
These uncharted boundaries and abrupt constraints are known as limitations in research . Identifying and acknowledging limitations is crucial for conducting rigorous studies. Limitations provide context and shed light on gaps in the prevailing inquiry and literature.
This article explores the importance of recognizing limitations and discusses how to write them effectively. By interpreting limitations in research and considering prevalent examples, we aim to reframe the perception from shameful mistakes to respectable revelations.

What are limitations in research?
In the clearest terms, research limitations are the practical or theoretical shortcomings of a study that are often outside of the researcher’s control . While these weaknesses limit the generalizability of a study’s conclusions, they also present a foundation for future research.
Sometimes limitations arise from tangible circumstances like time and funding constraints, or equipment and participant availability. Other times the rationale is more obscure and buried within the research design. Common types of limitations and their ramifications include:
- Theoretical: limits the scope, depth, or applicability of a study.
- Methodological: limits the quality, quantity, or diversity of the data.
- Empirical: limits the representativeness, validity, or reliability of the data.
- Analytical: limits the accuracy, completeness, or significance of the findings.
- Ethical: limits the access, consent, or confidentiality of the data.
Regardless of how, when, or why they arise, limitations are a natural part of the research process and should never be ignored . Like all other aspects, they are vital in their own purpose.
Why is identifying limitations important?
Whether to seek acceptance or avoid struggle, humans often instinctively hide flaws and mistakes. Merging this thought process into research by attempting to hide limitations, however, is a bad idea. It has the potential to negate the validity of outcomes and damage the reputation of scholars.
By identifying and addressing limitations throughout a project, researchers strengthen their arguments and curtail the chance of peer censure based on overlooked mistakes. Pointing out these flaws shows an understanding of variable limits and a scrupulous research process.
Showing awareness of and taking responsibility for a project’s boundaries and challenges validates the integrity and transparency of a researcher. It further demonstrates the researchers understand the applicable literature and have thoroughly evaluated their chosen research methods.
Presenting limitations also benefits the readers by providing context for research findings. It guides them to interpret the project’s conclusions only within the scope of very specific conditions. By allowing for an appropriate generalization of the findings that is accurately confined by research boundaries and is not too broad, limitations boost a study’s credibility .
Limitations are true assets to the research process. They highlight opportunities for future research. When researchers identify the limitations of their particular approach to a study question, they enable precise transferability and improve chances for reproducibility.
Simply stating a project’s limitations is not adequate for spurring further research, though. To spark the interest of other researchers, these acknowledgements must come with thorough explanations regarding how the limitations affected the current study and how they can potentially be overcome with amended methods.
How to write limitations
Typically, the information about a study’s limitations is situated either at the beginning of the discussion section to provide context for readers or at the conclusion of the discussion section to acknowledge the need for further research. However, it varies depending upon the target journal or publication guidelines.
Don’t hide your limitations
It is also important to not bury a limitation in the body of the paper unless it has a unique connection to a topic in that section. If so, it needs to be reiterated with the other limitations or at the conclusion of the discussion section. Wherever it is included in the manuscript, ensure that the limitations section is prominently positioned and clearly introduced.
While maintaining transparency by disclosing limitations means taking a comprehensive approach, it is not necessary to discuss everything that could have potentially gone wrong during the research study. If there is no commitment to investigation in the introduction, it is unnecessary to consider the issue a limitation to the research. Wholly consider the term ‘limitations’ and ask, “Did it significantly change or limit the possible outcomes?” Then, qualify the occurrence as either a limitation to include in the current manuscript or as an idea to note for other projects.
Writing limitations
Once the limitations are concretely identified and it is decided where they will be included in the paper, researchers are ready for the writing task. Including only what is pertinent, keeping explanations detailed but concise, and employing the following guidelines is key for crafting valuable limitations:
1) Identify and describe the limitations : Clearly introduce the limitation by classifying its form and specifying its origin. For example:
- An unintentional bias encountered during data collection
- An intentional use of unplanned post-hoc data analysis
2) Explain the implications : Describe how the limitation potentially influences the study’s findings and how the validity and generalizability are subsequently impacted. Provide examples and evidence to support claims of the limitations’ effects without making excuses or exaggerating their impact. Overall, be transparent and objective in presenting the limitations, without undermining the significance of the research.
3) Provide alternative approaches for future studies : Offer specific suggestions for potential improvements or avenues for further investigation. Demonstrate a proactive approach by encouraging future research that addresses the identified gaps and, therefore, expands the knowledge base.
Whether presenting limitations as an individual section within the manuscript or as a subtopic in the discussion area, authors should use clear headings and straightforward language to facilitate readability. There is no need to complicate limitations with jargon, computations, or complex datasets.
Examples of common limitations
Limitations are generally grouped into two categories , methodology and research process .
Methodology limitations
Methodology may include limitations due to:
- Sample size
- Lack of available or reliable data
- Lack of prior research studies on the topic
- Measure used to collect the data
- Self-reported data

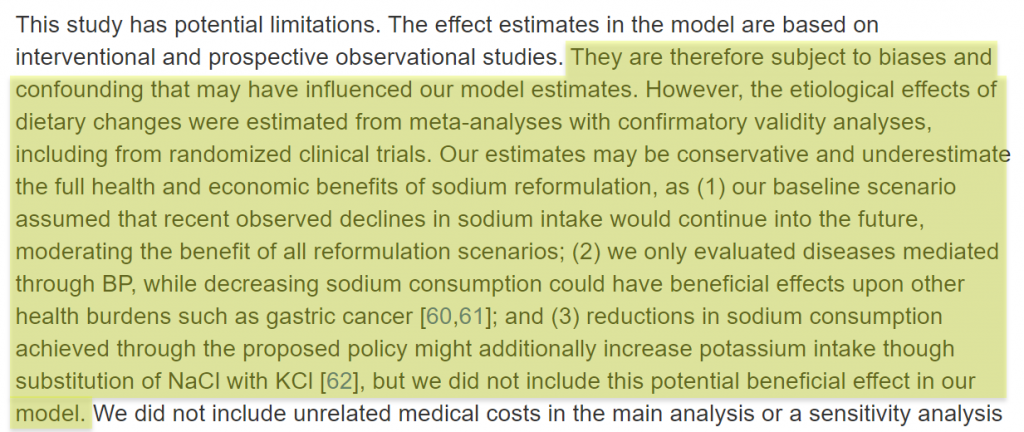
The researcher is addressing how the large sample size requires a reassessment of the measures used to collect and analyze the data.
Research process limitations
Limitations during the research process may arise from:
- Access to information
- Longitudinal effects
- Cultural and other biases
- Language fluency
- Time constraints

The author is pointing out that the model’s estimates are based on potentially biased observational studies.
Final thoughts
Successfully proving theories and touting great achievements are only two very narrow goals of scholarly research. The true passion and greatest efforts of researchers comes more in the form of confronting assumptions and exploring the obscure.
In many ways, recognizing and sharing the limitations of a research study both allows for and encourages this type of discovery that continuously pushes research forward. By using limitations to provide a transparent account of the project's boundaries and to contextualize the findings, researchers pave the way for even more robust and impactful research in the future.
Charla Viera, MS
See our "Privacy Policy"
Ensure your structure and ideas are consistent and clearly communicated
Pair your Premium Editing with our add-on service Presubmission Review for an overall assessment of your manuscript.
- USC Libraries
- Research Guides
Organizing Your Social Sciences Research Paper
- Limitations of the Study
- Purpose of Guide
- Design Flaws to Avoid
- Independent and Dependent Variables
- Glossary of Research Terms
- Reading Research Effectively
- Narrowing a Topic Idea
- Broadening a Topic Idea
- Extending the Timeliness of a Topic Idea
- Academic Writing Style
- Applying Critical Thinking
- Choosing a Title
- Making an Outline
- Paragraph Development
- Research Process Video Series
- Executive Summary
- The C.A.R.S. Model
- Background Information
- The Research Problem/Question
- Theoretical Framework
- Citation Tracking
- Content Alert Services
- Evaluating Sources
- Primary Sources
- Secondary Sources
- Tiertiary Sources
- Scholarly vs. Popular Publications
- Qualitative Methods
- Quantitative Methods
- Insiderness
- Using Non-Textual Elements
- Common Grammar Mistakes
- Writing Concisely
- Avoiding Plagiarism
- Footnotes or Endnotes?
- Further Readings
- Generative AI and Writing
- USC Libraries Tutorials and Other Guides
- Bibliography
The limitations of the study are those characteristics of design or methodology that impacted or influenced the interpretation of the findings from your research. Study limitations are the constraints placed on the ability to generalize from the results, to further describe applications to practice, and/or related to the utility of findings that are the result of the ways in which you initially chose to design the study or the method used to establish internal and external validity or the result of unanticipated challenges that emerged during the study.
Price, James H. and Judy Murnan. “Research Limitations and the Necessity of Reporting Them.” American Journal of Health Education 35 (2004): 66-67; Theofanidis, Dimitrios and Antigoni Fountouki. "Limitations and Delimitations in the Research Process." Perioperative Nursing 7 (September-December 2018): 155-163. .
Importance of...
Always acknowledge a study's limitations. It is far better that you identify and acknowledge your study’s limitations than to have them pointed out by your professor and have your grade lowered because you appeared to have ignored them or didn't realize they existed.
Keep in mind that acknowledgment of a study's limitations is an opportunity to make suggestions for further research. If you do connect your study's limitations to suggestions for further research, be sure to explain the ways in which these unanswered questions may become more focused because of your study.
Acknowledgment of a study's limitations also provides you with opportunities to demonstrate that you have thought critically about the research problem, understood the relevant literature published about it, and correctly assessed the methods chosen for studying the problem. A key objective of the research process is not only discovering new knowledge but also to confront assumptions and explore what we don't know.
Claiming limitations is a subjective process because you must evaluate the impact of those limitations . Don't just list key weaknesses and the magnitude of a study's limitations. To do so diminishes the validity of your research because it leaves the reader wondering whether, or in what ways, limitation(s) in your study may have impacted the results and conclusions. Limitations require a critical, overall appraisal and interpretation of their impact. You should answer the question: do these problems with errors, methods, validity, etc. eventually matter and, if so, to what extent?
Price, James H. and Judy Murnan. “Research Limitations and the Necessity of Reporting Them.” American Journal of Health Education 35 (2004): 66-67; Structure: How to Structure the Research Limitations Section of Your Dissertation. Dissertations and Theses: An Online Textbook. Laerd.com.
Descriptions of Possible Limitations
All studies have limitations . However, it is important that you restrict your discussion to limitations related to the research problem under investigation. For example, if a meta-analysis of existing literature is not a stated purpose of your research, it should not be discussed as a limitation. Do not apologize for not addressing issues that you did not promise to investigate in the introduction of your paper.
Here are examples of limitations related to methodology and the research process you may need to describe and discuss how they possibly impacted your results. Note that descriptions of limitations should be stated in the past tense because they were discovered after you completed your research.
Possible Methodological Limitations
- Sample size -- the number of the units of analysis you use in your study is dictated by the type of research problem you are investigating. Note that, if your sample size is too small, it will be difficult to find significant relationships from the data, as statistical tests normally require a larger sample size to ensure a representative distribution of the population and to be considered representative of groups of people to whom results will be generalized or transferred. Note that sample size is generally less relevant in qualitative research if explained in the context of the research problem.
- Lack of available and/or reliable data -- a lack of data or of reliable data will likely require you to limit the scope of your analysis, the size of your sample, or it can be a significant obstacle in finding a trend and a meaningful relationship. You need to not only describe these limitations but provide cogent reasons why you believe data is missing or is unreliable. However, don’t just throw up your hands in frustration; use this as an opportunity to describe a need for future research based on designing a different method for gathering data.
- Lack of prior research studies on the topic -- citing prior research studies forms the basis of your literature review and helps lay a foundation for understanding the research problem you are investigating. Depending on the currency or scope of your research topic, there may be little, if any, prior research on your topic. Before assuming this to be true, though, consult with a librarian! In cases when a librarian has confirmed that there is little or no prior research, you may be required to develop an entirely new research typology [for example, using an exploratory rather than an explanatory research design ]. Note again that discovering a limitation can serve as an important opportunity to identify new gaps in the literature and to describe the need for further research.
- Measure used to collect the data -- sometimes it is the case that, after completing your interpretation of the findings, you discover that the way in which you gathered data inhibited your ability to conduct a thorough analysis of the results. For example, you regret not including a specific question in a survey that, in retrospect, could have helped address a particular issue that emerged later in the study. Acknowledge the deficiency by stating a need for future researchers to revise the specific method for gathering data.
- Self-reported data -- whether you are relying on pre-existing data or you are conducting a qualitative research study and gathering the data yourself, self-reported data is limited by the fact that it rarely can be independently verified. In other words, you have to the accuracy of what people say, whether in interviews, focus groups, or on questionnaires, at face value. However, self-reported data can contain several potential sources of bias that you should be alert to and note as limitations. These biases become apparent if they are incongruent with data from other sources. These are: (1) selective memory [remembering or not remembering experiences or events that occurred at some point in the past]; (2) telescoping [recalling events that occurred at one time as if they occurred at another time]; (3) attribution [the act of attributing positive events and outcomes to one's own agency, but attributing negative events and outcomes to external forces]; and, (4) exaggeration [the act of representing outcomes or embellishing events as more significant than is actually suggested from other data].
Possible Limitations of the Researcher
- Access -- if your study depends on having access to people, organizations, data, or documents and, for whatever reason, access is denied or limited in some way, the reasons for this needs to be described. Also, include an explanation why being denied or limited access did not prevent you from following through on your study.
- Longitudinal effects -- unlike your professor, who can literally devote years [even a lifetime] to studying a single topic, the time available to investigate a research problem and to measure change or stability over time is constrained by the due date of your assignment. Be sure to choose a research problem that does not require an excessive amount of time to complete the literature review, apply the methodology, and gather and interpret the results. If you're unsure whether you can complete your research within the confines of the assignment's due date, talk to your professor.
- Cultural and other type of bias -- we all have biases, whether we are conscience of them or not. Bias is when a person, place, event, or thing is viewed or shown in a consistently inaccurate way. Bias is usually negative, though one can have a positive bias as well, especially if that bias reflects your reliance on research that only support your hypothesis. When proof-reading your paper, be especially critical in reviewing how you have stated a problem, selected the data to be studied, what may have been omitted, the manner in which you have ordered events, people, or places, how you have chosen to represent a person, place, or thing, to name a phenomenon, or to use possible words with a positive or negative connotation. NOTE : If you detect bias in prior research, it must be acknowledged and you should explain what measures were taken to avoid perpetuating that bias. For example, if a previous study only used boys to examine how music education supports effective math skills, describe how your research expands the study to include girls.
- Fluency in a language -- if your research focuses , for example, on measuring the perceived value of after-school tutoring among Mexican-American ESL [English as a Second Language] students and you are not fluent in Spanish, you are limited in being able to read and interpret Spanish language research studies on the topic or to speak with these students in their primary language. This deficiency should be acknowledged.
Aguinis, Hermam and Jeffrey R. Edwards. “Methodological Wishes for the Next Decade and How to Make Wishes Come True.” Journal of Management Studies 51 (January 2014): 143-174; Brutus, Stéphane et al. "Self-Reported Limitations and Future Directions in Scholarly Reports: Analysis and Recommendations." Journal of Management 39 (January 2013): 48-75; Senunyeme, Emmanuel K. Business Research Methods. Powerpoint Presentation. Regent University of Science and Technology; ter Riet, Gerben et al. “All That Glitters Isn't Gold: A Survey on Acknowledgment of Limitations in Biomedical Studies.” PLOS One 8 (November 2013): 1-6.
Structure and Writing Style
Information about the limitations of your study are generally placed either at the beginning of the discussion section of your paper so the reader knows and understands the limitations before reading the rest of your analysis of the findings, or, the limitations are outlined at the conclusion of the discussion section as an acknowledgement of the need for further study. Statements about a study's limitations should not be buried in the body [middle] of the discussion section unless a limitation is specific to something covered in that part of the paper. If this is the case, though, the limitation should be reiterated at the conclusion of the section.
If you determine that your study is seriously flawed due to important limitations , such as, an inability to acquire critical data, consider reframing it as an exploratory study intended to lay the groundwork for a more complete research study in the future. Be sure, though, to specifically explain the ways that these flaws can be successfully overcome in a new study.
But, do not use this as an excuse for not developing a thorough research paper! Review the tab in this guide for developing a research topic . If serious limitations exist, it generally indicates a likelihood that your research problem is too narrowly defined or that the issue or event under study is too recent and, thus, very little research has been written about it. If serious limitations do emerge, consult with your professor about possible ways to overcome them or how to revise your study.
When discussing the limitations of your research, be sure to:
- Describe each limitation in detailed but concise terms;
- Explain why each limitation exists;
- Provide the reasons why each limitation could not be overcome using the method(s) chosen to acquire or gather the data [cite to other studies that had similar problems when possible];
- Assess the impact of each limitation in relation to the overall findings and conclusions of your study; and,
- If appropriate, describe how these limitations could point to the need for further research.
Remember that the method you chose may be the source of a significant limitation that has emerged during your interpretation of the results [for example, you didn't interview a group of people that you later wish you had]. If this is the case, don't panic. Acknowledge it, and explain how applying a different or more robust methodology might address the research problem more effectively in a future study. A underlying goal of scholarly research is not only to show what works, but to demonstrate what doesn't work or what needs further clarification.
Aguinis, Hermam and Jeffrey R. Edwards. “Methodological Wishes for the Next Decade and How to Make Wishes Come True.” Journal of Management Studies 51 (January 2014): 143-174; Brutus, Stéphane et al. "Self-Reported Limitations and Future Directions in Scholarly Reports: Analysis and Recommendations." Journal of Management 39 (January 2013): 48-75; Ioannidis, John P.A. "Limitations are not Properly Acknowledged in the Scientific Literature." Journal of Clinical Epidemiology 60 (2007): 324-329; Pasek, Josh. Writing the Empirical Social Science Research Paper: A Guide for the Perplexed. January 24, 2012. Academia.edu; Structure: How to Structure the Research Limitations Section of Your Dissertation. Dissertations and Theses: An Online Textbook. Laerd.com; What Is an Academic Paper? Institute for Writing Rhetoric. Dartmouth College; Writing the Experimental Report: Methods, Results, and Discussion. The Writing Lab and The OWL. Purdue University.
Writing Tip
Don't Inflate the Importance of Your Findings!
After all the hard work and long hours devoted to writing your research paper, it is easy to get carried away with attributing unwarranted importance to what you’ve done. We all want our academic work to be viewed as excellent and worthy of a good grade, but it is important that you understand and openly acknowledge the limitations of your study. Inflating the importance of your study's findings could be perceived by your readers as an attempt hide its flaws or encourage a biased interpretation of the results. A small measure of humility goes a long way!
Another Writing Tip
Negative Results are Not a Limitation!
Negative evidence refers to findings that unexpectedly challenge rather than support your hypothesis. If you didn't get the results you anticipated, it may mean your hypothesis was incorrect and needs to be reformulated. Or, perhaps you have stumbled onto something unexpected that warrants further study. Moreover, the absence of an effect may be very telling in many situations, particularly in experimental research designs. In any case, your results may very well be of importance to others even though they did not support your hypothesis. Do not fall into the trap of thinking that results contrary to what you expected is a limitation to your study. If you carried out the research well, they are simply your results and only require additional interpretation.
Lewis, George H. and Jonathan F. Lewis. “The Dog in the Night-Time: Negative Evidence in Social Research.” The British Journal of Sociology 31 (December 1980): 544-558.
Yet Another Writing Tip
Sample Size Limitations in Qualitative Research
Sample sizes are typically smaller in qualitative research because, as the study goes on, acquiring more data does not necessarily lead to more information. This is because one occurrence of a piece of data, or a code, is all that is necessary to ensure that it becomes part of the analysis framework. However, it remains true that sample sizes that are too small cannot adequately support claims of having achieved valid conclusions and sample sizes that are too large do not permit the deep, naturalistic, and inductive analysis that defines qualitative inquiry. Determining adequate sample size in qualitative research is ultimately a matter of judgment and experience in evaluating the quality of the information collected against the uses to which it will be applied and the particular research method and purposeful sampling strategy employed. If the sample size is found to be a limitation, it may reflect your judgment about the methodological technique chosen [e.g., single life history study versus focus group interviews] rather than the number of respondents used.
Boddy, Clive Roland. "Sample Size for Qualitative Research." Qualitative Market Research: An International Journal 19 (2016): 426-432; Huberman, A. Michael and Matthew B. Miles. "Data Management and Analysis Methods." In Handbook of Qualitative Research . Norman K. Denzin and Yvonna S. Lincoln, eds. (Thousand Oaks, CA: Sage, 1994), pp. 428-444; Blaikie, Norman. "Confounding Issues Related to Determining Sample Size in Qualitative Research." International Journal of Social Research Methodology 21 (2018): 635-641; Oppong, Steward Harrison. "The Problem of Sampling in qualitative Research." Asian Journal of Management Sciences and Education 2 (2013): 202-210.
- << Previous: 8. The Discussion
- Next: 9. The Conclusion >>
- Last Updated: May 18, 2024 11:38 AM
- URL: https://libguides.usc.edu/writingguide
21 Research Limitations Examples
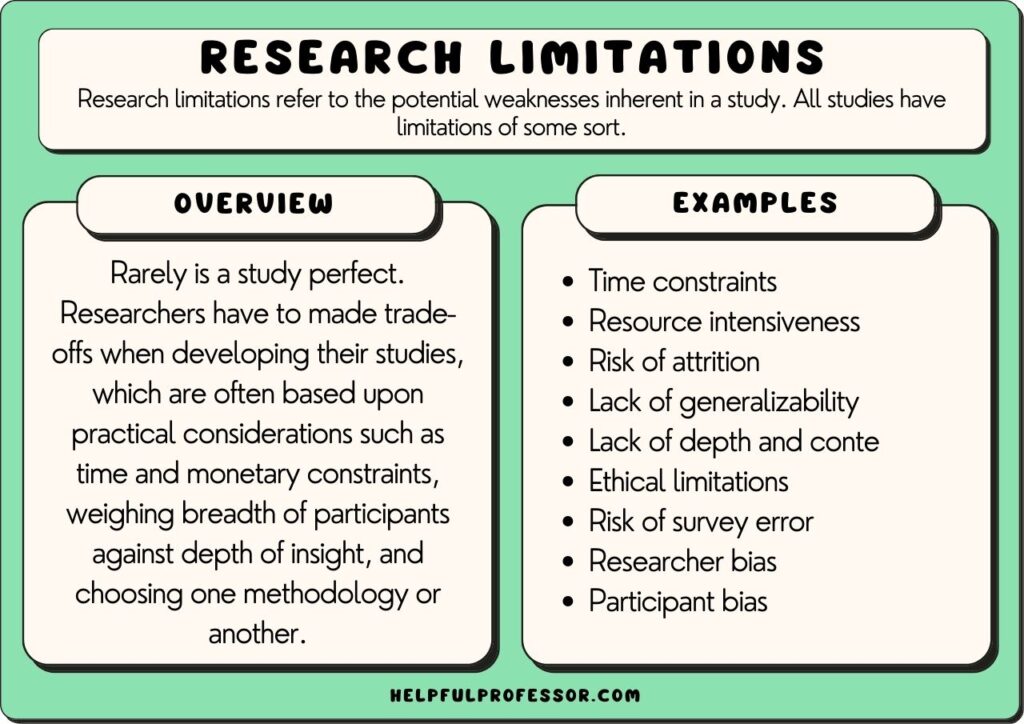
Research limitations refer to the potential weaknesses inherent in a study. All studies have limitations of some sort, meaning declaring limitations doesn’t necessarily need to be a bad thing, so long as your declaration of limitations is well thought-out and explained.
Rarely is a study perfect. Researchers have to make trade-offs when developing their studies, which are often based upon practical considerations such as time and monetary constraints, weighing the breadth of participants against the depth of insight, and choosing one methodology or another.
In research, studies can have limitations such as limited scope, researcher subjectivity, and lack of available research tools.
Acknowledging the limitations of your study should be seen as a strength. It demonstrates your willingness for transparency, humility, and submission to the scientific method and can bolster the integrity of the study. It can also inform future research direction.
Typically, scholars will explore the limitations of their study in either their methodology section, their conclusion section, or both.
Research Limitations Examples
Qualitative and quantitative research offer different perspectives and methods in exploring phenomena, each with its own strengths and limitations. So, I’ve split the limitations examples sections into qualitative and quantitative below.
Qualitative Research Limitations
Qualitative research seeks to understand phenomena in-depth and in context. It focuses on the ‘why’ and ‘how’ questions.
It’s often used to explore new or complex issues, and it provides rich, detailed insights into participants’ experiences, behaviors, and attitudes. However, these strengths also create certain limitations, as explained below.
1. Subjectivity
Qualitative research often requires the researcher to interpret subjective data. One researcher may examine a text and identify different themes or concepts as more dominant than others.
Close qualitative readings of texts are necessarily subjective – and while this may be a limitation, qualitative researchers argue this is the best way to deeply understand everything in context.
Suggested Solution and Response: To minimize subjectivity bias, you could consider cross-checking your own readings of themes and data against other scholars’ readings and interpretations. This may involve giving the raw data to a supervisor or colleague and asking them to code the data separately, then coming together to compare and contrast results.
2. Researcher Bias
The concept of researcher bias is related to, but slightly different from, subjectivity.
Researcher bias refers to the perspectives and opinions you bring with you when doing your research.
For example, a researcher who is explicitly of a certain philosophical or political persuasion may bring that persuasion to bear when interpreting data.
In many scholarly traditions, we will attempt to minimize researcher bias through the utilization of clear procedures that are set out in advance or through the use of statistical analysis tools.
However, in other traditions, such as in postmodern feminist research , declaration of bias is expected, and acknowledgment of bias is seen as a positive because, in those traditions, it is believed that bias cannot be eliminated from research, so instead, it is a matter of integrity to present it upfront.
Suggested Solution and Response: Acknowledge the potential for researcher bias and, depending on your theoretical framework , accept this, or identify procedures you have taken to seek a closer approximation to objectivity in your coding and analysis.
3. Generalizability
If you’re struggling to find a limitation to discuss in your own qualitative research study, then this one is for you: all qualitative research, of all persuasions and perspectives, cannot be generalized.
This is a core feature that sets qualitative data and quantitative data apart.
The point of qualitative data is to select case studies and similarly small corpora and dig deep through in-depth analysis and thick description of data.
Often, this will also mean that you have a non-randomized sample size.
While this is a positive – you’re going to get some really deep, contextualized, interesting insights – it also means that the findings may not be generalizable to a larger population that may not be representative of the small group of people in your study.
Suggested Solution and Response: Suggest future studies that take a quantitative approach to the question.
4. The Hawthorne Effect
The Hawthorne effect refers to the phenomenon where research participants change their ‘observed behavior’ when they’re aware that they are being observed.
This effect was first identified by Elton Mayo who conducted studies of the effects of various factors ton workers’ productivity. He noticed that no matter what he did – turning up the lights, turning down the lights, etc. – there was an increase in worker outputs compared to prior to the study taking place.
Mayo realized that the mere act of observing the workers made them work harder – his observation was what was changing behavior.
So, if you’re looking for a potential limitation to name for your observational research study , highlight the possible impact of the Hawthorne effect (and how you could reduce your footprint or visibility in order to decrease its likelihood).
Suggested Solution and Response: Highlight ways you have attempted to reduce your footprint while in the field, and guarantee anonymity to your research participants.
5. Replicability
Quantitative research has a great benefit in that the studies are replicable – a researcher can get a similar sample size, duplicate the variables, and re-test a study. But you can’t do that in qualitative research.
Qualitative research relies heavily on context – a specific case study or specific variables that make a certain instance worthy of analysis. As a result, it’s often difficult to re-enter the same setting with the same variables and repeat the study.
Furthermore, the individual researcher’s interpretation is more influential in qualitative research, meaning even if a new researcher enters an environment and makes observations, their observations may be different because subjectivity comes into play much more. This doesn’t make the research bad necessarily (great insights can be made in qualitative research), but it certainly does demonstrate a weakness of qualitative research.
6. Limited Scope
“Limited scope” is perhaps one of the most common limitations listed by researchers – and while this is often a catch-all way of saying, “well, I’m not studying that in this study”, it’s also a valid point.
No study can explore everything related to a topic. At some point, we have to make decisions about what’s included in the study and what is excluded from the study.
So, you could say that a limitation of your study is that it doesn’t look at an extra variable or concept that’s certainly worthy of study but will have to be explored in your next project because this project has a clearly and narrowly defined goal.
Suggested Solution and Response: Be clear about what’s in and out of the study when writing your research question.
7. Time Constraints
This is also a catch-all claim you can make about your research project: that you would have included more people in the study, looked at more variables, and so on. But you’ve got to submit this thing by the end of next semester! You’ve got time constraints.
And time constraints are a recognized reality in all research.
But this means you’ll need to explain how time has limited your decisions. As with “limited scope”, this may mean that you had to study a smaller group of subjects, limit the amount of time you spent in the field, and so forth.
Suggested Solution and Response: Suggest future studies that will build on your current work, possibly as a PhD project.
8. Resource Intensiveness
Qualitative research can be expensive due to the cost of transcription, the involvement of trained researchers, and potential travel for interviews or observations.
So, resource intensiveness is similar to the time constraints concept. If you don’t have the funds, you have to make decisions about which tools to use, which statistical software to employ, and how many research assistants you can dedicate to the study.
Suggested Solution and Response: Suggest future studies that will gain more funding on the back of this ‘ exploratory study ‘.
9. Coding Difficulties
Data analysis in qualitative research often involves coding, which can be subjective and complex, especially when dealing with ambiguous or contradicting data.
After naming this as a limitation in your research, it’s important to explain how you’ve attempted to address this. Some ways to ‘limit the limitation’ include:
- Triangulation: Have 2 other researchers code the data as well and cross-check your results with theirs to identify outliers that may need to be re-examined, debated with the other researchers, or removed altogether.
- Procedure: Use a clear coding procedure to demonstrate reliability in your coding process. I personally use the thematic network analysis method outlined in this academic article by Attride-Stirling (2001).
Suggested Solution and Response: Triangulate your coding findings with colleagues, and follow a thematic network analysis procedure.
10. Risk of Non-Responsiveness
There is always a risk in research that research participants will be unwilling or uncomfortable sharing their genuine thoughts and feelings in the study.
This is particularly true when you’re conducting research on sensitive topics, politicized topics, or topics where the participant is expressing vulnerability .
This is similar to the Hawthorne effect (aka participant bias), where participants change their behaviors in your presence; but it goes a step further, where participants actively hide their true thoughts and feelings from you.
Suggested Solution and Response: One way to manage this is to try to include a wider group of people with the expectation that there will be non-responsiveness from some participants.
11. Risk of Attrition
Attrition refers to the process of losing research participants throughout the study.
This occurs most commonly in longitudinal studies , where a researcher must return to conduct their analysis over spaced periods of time, often over a period of years.
Things happen to people over time – they move overseas, their life experiences change, they get sick, change their minds, and even die. The more time that passes, the greater the risk of attrition.
Suggested Solution and Response: One way to manage this is to try to include a wider group of people with the expectation that there will be attrition over time.
12. Difficulty in Maintaining Confidentiality and Anonymity
Given the detailed nature of qualitative data , ensuring participant anonymity can be challenging.
If you have a sensitive topic in a specific case study, even anonymizing research participants sometimes isn’t enough. People might be able to induce who you’re talking about.
Sometimes, this will mean you have to exclude some interesting data that you collected from your final report. Confidentiality and anonymity come before your findings in research ethics – and this is a necessary limiting factor.
Suggested Solution and Response: Highlight the efforts you have taken to anonymize data, and accept that confidentiality and accountability place extremely important constraints on academic research.
13. Difficulty in Finding Research Participants
A study that looks at a very specific phenomenon or even a specific set of cases within a phenomenon means that the pool of potential research participants can be very low.
Compile on top of this the fact that many people you approach may choose not to participate, and you could end up with a very small corpus of subjects to explore. This may limit your ability to make complete findings, even in a quantitative sense.
You may need to therefore limit your research question and objectives to something more realistic.
Suggested Solution and Response: Highlight that this is going to limit the study’s generalizability significantly.
14. Ethical Limitations
Ethical limitations refer to the things you cannot do based on ethical concerns identified either by yourself or your institution’s ethics review board.
This might include threats to the physical or psychological well-being of your research subjects, the potential of releasing data that could harm a person’s reputation, and so on.
Furthermore, even if your study follows all expected standards of ethics, you still, as an ethical researcher, need to allow a research participant to pull out at any point in time, after which you cannot use their data, which demonstrates an overlap between ethical constraints and participant attrition.
Suggested Solution and Response: Highlight that these ethical limitations are inevitable but important to sustain the integrity of the research.
For more on Qualitative Research, Explore my Qualitative Research Guide
Quantitative Research Limitations
Quantitative research focuses on quantifiable data and statistical, mathematical, or computational techniques. It’s often used to test hypotheses, assess relationships and causality, and generalize findings across larger populations.
Quantitative research is widely respected for its ability to provide reliable, measurable, and generalizable data (if done well!). Its structured methodology has strengths over qualitative research, such as the fact it allows for replication of the study, which underpins the validity of the research.
However, this approach is not without it limitations, explained below.
1. Over-Simplification
Quantitative research is powerful because it allows you to measure and analyze data in a systematic and standardized way. However, one of its limitations is that it can sometimes simplify complex phenomena or situations.
In other words, it might miss the subtleties or nuances of the research subject.
For example, if you’re studying why people choose a particular diet, a quantitative study might identify factors like age, income, or health status. But it might miss other aspects, such as cultural influences or personal beliefs, that can also significantly impact dietary choices.
When writing about this limitation, you can say that your quantitative approach, while providing precise measurements and comparisons, may not capture the full complexity of your subjects of study.
Suggested Solution and Response: Suggest a follow-up case study using the same research participants in order to gain additional context and depth.
2. Lack of Context
Another potential issue with quantitative research is that it often focuses on numbers and statistics at the expense of context or qualitative information.
Let’s say you’re studying the effect of classroom size on student performance. You might find that students in smaller classes generally perform better. However, this doesn’t take into account other variables, like teaching style , student motivation, or family support.
When describing this limitation, you might say, “Although our research provides important insights into the relationship between class size and student performance, it does not incorporate the impact of other potentially influential variables. Future research could benefit from a mixed-methods approach that combines quantitative analysis with qualitative insights.”
3. Applicability to Real-World Settings
Oftentimes, experimental research takes place in controlled environments to limit the influence of outside factors.
This control is great for isolation and understanding the specific phenomenon but can limit the applicability or “external validity” of the research to real-world settings.
For example, if you conduct a lab experiment to see how sleep deprivation impacts cognitive performance, the sterile, controlled lab environment might not reflect real-world conditions where people are dealing with multiple stressors.
Therefore, when explaining the limitations of your quantitative study in your methodology section, you could state:
“While our findings provide valuable information about [topic], the controlled conditions of the experiment may not accurately represent real-world scenarios where extraneous variables will exist. As such, the direct applicability of our results to broader contexts may be limited.”
Suggested Solution and Response: Suggest future studies that will engage in real-world observational research, such as ethnographic research.
4. Limited Flexibility
Once a quantitative study is underway, it can be challenging to make changes to it. This is because, unlike in grounded research, you’re putting in place your study in advance, and you can’t make changes part-way through.
Your study design, data collection methods, and analysis techniques need to be decided upon before you start collecting data.
For example, if you are conducting a survey on the impact of social media on teenage mental health, and halfway through, you realize that you should have included a question about their screen time, it’s generally too late to add it.
When discussing this limitation, you could write something like, “The structured nature of our quantitative approach allows for consistent data collection and analysis but also limits our flexibility to adapt and modify the research process in response to emerging insights and ideas.”
Suggested Solution and Response: Suggest future studies that will use mixed-methods or qualitative research methods to gain additional depth of insight.
5. Risk of Survey Error
Surveys are a common tool in quantitative research, but they carry risks of error.
There can be measurement errors (if a question is misunderstood), coverage errors (if some groups aren’t adequately represented), non-response errors (if certain people don’t respond), and sampling errors (if your sample isn’t representative of the population).
For instance, if you’re surveying college students about their study habits , but only daytime students respond because you conduct the survey during the day, your results will be skewed.
In discussing this limitation, you might say, “Despite our best efforts to develop a comprehensive survey, there remains a risk of survey error, including measurement, coverage, non-response, and sampling errors. These could potentially impact the reliability and generalizability of our findings.”
Suggested Solution and Response: Suggest future studies that will use other survey tools to compare and contrast results.
6. Limited Ability to Probe Answers
With quantitative research, you typically can’t ask follow-up questions or delve deeper into participants’ responses like you could in a qualitative interview.
For instance, imagine you are surveying 500 students about study habits in a questionnaire. A respondent might indicate that they study for two hours each night. You might want to follow up by asking them to elaborate on what those study sessions involve or how effective they feel their habits are.
However, quantitative research generally disallows this in the way a qualitative semi-structured interview could.
When discussing this limitation, you might write, “Given the structured nature of our survey, our ability to probe deeper into individual responses is limited. This means we may not fully understand the context or reasoning behind the responses, potentially limiting the depth of our findings.”
Suggested Solution and Response: Suggest future studies that engage in mixed-method or qualitative methodologies to address the issue from another angle.
7. Reliance on Instruments for Data Collection
In quantitative research, the collection of data heavily relies on instruments like questionnaires, surveys, or machines.
The limitation here is that the data you get is only as good as the instrument you’re using. If the instrument isn’t designed or calibrated well, your data can be flawed.
For instance, if you’re using a questionnaire to study customer satisfaction and the questions are vague, confusing, or biased, the responses may not accurately reflect the customers’ true feelings.
When discussing this limitation, you could say, “Our study depends on the use of questionnaires for data collection. Although we have put significant effort into designing and testing the instrument, it’s possible that inaccuracies or misunderstandings could potentially affect the validity of the data collected.”
Suggested Solution and Response: Suggest future studies that will use different instruments but examine the same variables to triangulate results.
8. Time and Resource Constraints (Specific to Quantitative Research)
Quantitative research can be time-consuming and resource-intensive, especially when dealing with large samples.
It often involves systematic sampling, rigorous design, and sometimes complex statistical analysis.
If resources and time are limited, it can restrict the scale of your research, the techniques you can employ, or the extent of your data analysis.
For example, you may want to conduct a nationwide survey on public opinion about a certain policy. However, due to limited resources, you might only be able to survey people in one city.
When writing about this limitation, you could say, “Given the scope of our research and the resources available, we are limited to conducting our survey within one city, which may not fully represent the nationwide public opinion. Hence, the generalizability of the results may be limited.”
Suggested Solution and Response: Suggest future studies that will have more funding or longer timeframes.
How to Discuss Your Research Limitations
1. in your research proposal and methodology section.
In the research proposal, which will become the methodology section of your dissertation, I would recommend taking the four following steps, in order:
- Be Explicit about your Scope – If you limit the scope of your study in your research question, aims, and objectives, then you can set yourself up well later in the methodology to say that certain questions are “outside the scope of the study.” For example, you may identify the fact that the study doesn’t address a certain variable, but you can follow up by stating that the research question is specifically focused on the variable that you are examining, so this limitation would need to be looked at in future studies.
- Acknowledge the Limitation – Acknowledging the limitations of your study demonstrates reflexivity and humility and can make your research more reliable and valid. It also pre-empts questions the people grading your paper may have, so instead of them down-grading you for your limitations; they will congratulate you on explaining the limitations and how you have addressed them!
- Explain your Decisions – You may have chosen your approach (despite its limitations) for a very specific reason. This might be because your approach remains, on balance, the best one to answer your research question. Or, it might be because of time and monetary constraints that are outside of your control.
- Highlight the Strengths of your Approach – Conclude your limitations section by strongly demonstrating that, despite limitations, you’ve worked hard to minimize the effects of the limitations and that you have chosen your specific approach and methodology because it’s also got some terrific strengths. Name the strengths.
Overall, you’ll want to acknowledge your own limitations but also explain that the limitations don’t detract from the value of your study as it stands.
2. In the Conclusion Section or Chapter
In the conclusion of your study, it is generally expected that you return to a discussion of the study’s limitations. Here, I recommend the following steps:
- Acknowledge issues faced – After completing your study, you will be increasingly aware of issues you may have faced that, if you re-did the study, you may have addressed earlier in order to avoid those issues. Acknowledge these issues as limitations, and frame them as recommendations for subsequent studies.
- Suggest further research – Scholarly research aims to fill gaps in the current literature and knowledge. Having established your expertise through your study, suggest lines of inquiry for future researchers. You could state that your study had certain limitations, and “future studies” can address those limitations.
- Suggest a mixed methods approach – Qualitative and quantitative research each have pros and cons. So, note those ‘cons’ of your approach, then say the next study should approach the topic using the opposite methodology or could approach it using a mixed-methods approach that could achieve the benefits of quantitative studies with the nuanced insights of associated qualitative insights as part of an in-study case-study.
Overall, be clear about both your limitations and how those limitations can inform future studies.
In sum, each type of research method has its own strengths and limitations. Qualitative research excels in exploring depth, context, and complexity, while quantitative research excels in examining breadth, generalizability, and quantifiable measures. Despite their individual limitations, each method contributes unique and valuable insights, and researchers often use them together to provide a more comprehensive understanding of the phenomenon being studied.
Attride-Stirling, J. (2001). Thematic networks: an analytic tool for qualitative research. Qualitative research , 1 (3), 385-405. ( Source )
Atkinson, P., Delamont, S., Cernat, A., Sakshaug, J., & Williams, R. A. (2021). SAGE research methods foundations . London: Sage Publications.
Clark, T., Foster, L., Bryman, A., & Sloan, L. (2021). Bryman’s social research methods . Oxford: Oxford University Press.
Köhler, T., Smith, A., & Bhakoo, V. (2022). Templates in qualitative research methods: Origins, limitations, and new directions. Organizational Research Methods , 25 (2), 183-210. ( Source )
Lenger, A. (2019). The rejection of qualitative research methods in economics. Journal of Economic Issues , 53 (4), 946-965. ( Source )
Taherdoost, H. (2022). What are different research approaches? Comprehensive review of qualitative, quantitative, and mixed method research, their applications, types, and limitations. Journal of Management Science & Engineering Research , 5 (1), 53-63. ( Source )
Walliman, N. (2021). Research methods: The basics . New York: Routledge.

Chris Drew (PhD)
Dr. Chris Drew is the founder of the Helpful Professor. He holds a PhD in education and has published over 20 articles in scholarly journals. He is the former editor of the Journal of Learning Development in Higher Education. [Image Descriptor: Photo of Chris]
- Chris Drew (PhD) https://helpfulprofessor.com/author/chris-drew-phd/ 15 Animism Examples
- Chris Drew (PhD) https://helpfulprofessor.com/author/chris-drew-phd/ 10 Magical Thinking Examples
- Chris Drew (PhD) https://helpfulprofessor.com/author/chris-drew-phd/ Social-Emotional Learning (Definition, Examples, Pros & Cons)
- Chris Drew (PhD) https://helpfulprofessor.com/author/chris-drew-phd/ What is Educational Psychology?
Leave a Comment Cancel Reply
Your email address will not be published. Required fields are marked *
- Affiliate Program

- UNITED STATES
- 台灣 (TAIWAN)
- TÜRKIYE (TURKEY)
- Academic Editing Services
- - Research Paper
- - Journal Manuscript
- - Dissertation
- - College & University Assignments
- Admissions Editing Services
- - Application Essay
- - Personal Statement
- - Recommendation Letter
- - Cover Letter
- - CV/Resume
- Business Editing Services
- - Business Documents
- - Report & Brochure
- - Website & Blog
- Writer Editing Services
- - Script & Screenplay
- Our Editors
- Client Reviews
- Editing & Proofreading Prices
- Wordvice Points
- Partner Discount
- Plagiarism Checker
APA Citation Generator
MLA Citation Generator
Chicago Citation Generator
Vancouver Citation Generator
- - APA Style
- - MLA Style
- - Chicago Style
- - Vancouver Style
- Writing & Editing Guide
- Academic Resources
- Admissions Resources
How to Present the Limitations of the Study Examples
What are the limitations of a study?
The limitations of a study are the elements of methodology or study design that impact the interpretation of your research results. The limitations essentially detail any flaws or shortcomings in your study. Study limitations can exist due to constraints on research design, methodology, materials, etc., and these factors may impact the findings of your study. However, researchers are often reluctant to discuss the limitations of their study in their papers, feeling that bringing up limitations may undermine its research value in the eyes of readers and reviewers.
In spite of the impact it might have (and perhaps because of it) you should clearly acknowledge any limitations in your research paper in order to show readers—whether journal editors, other researchers, or the general public—that you are aware of these limitations and to explain how they affect the conclusions that can be drawn from the research.
In this article, we provide some guidelines for writing about research limitations, show examples of some frequently seen study limitations, and recommend techniques for presenting this information. And after you have finished drafting and have received manuscript editing for your work, you still might want to follow this up with academic editing before submitting your work to your target journal.
Why do I need to include limitations of research in my paper?
Although limitations address the potential weaknesses of a study, writing about them toward the end of your paper actually strengthens your study by identifying any problems before other researchers or reviewers find them.
Furthermore, pointing out study limitations shows that you’ve considered the impact of research weakness thoroughly and have an in-depth understanding of your research topic. Since all studies face limitations, being honest and detailing these limitations will impress researchers and reviewers more than ignoring them.

Where should I put the limitations of the study in my paper?
Some limitations might be evident to researchers before the start of the study, while others might become clear while you are conducting the research. Whether these limitations are anticipated or not, and whether they are due to research design or to methodology, they should be clearly identified and discussed in the discussion section —the final section of your paper. Most journals now require you to include a discussion of potential limitations of your work, and many journals now ask you to place this “limitations section” at the very end of your article.
Some journals ask you to also discuss the strengths of your work in this section, and some allow you to freely choose where to include that information in your discussion section—make sure to always check the author instructions of your target journal before you finalize a manuscript and submit it for peer review .
Limitations of the Study Examples
There are several reasons why limitations of research might exist. The two main categories of limitations are those that result from the methodology and those that result from issues with the researcher(s).
Common Methodological Limitations of Studies
Limitations of research due to methodological problems can be addressed by clearly and directly identifying the potential problem and suggesting ways in which this could have been addressed—and SHOULD be addressed in future studies. The following are some major potential methodological issues that can impact the conclusions researchers can draw from the research.
Issues with research samples and selection
Sampling errors occur when a probability sampling method is used to select a sample, but that sample does not reflect the general population or appropriate population concerned. This results in limitations of your study known as “sample bias” or “selection bias.”
For example, if you conducted a survey to obtain your research results, your samples (participants) were asked to respond to the survey questions. However, you might have had limited ability to gain access to the appropriate type or geographic scope of participants. In this case, the people who responded to your survey questions may not truly be a random sample.
Insufficient sample size for statistical measurements
When conducting a study, it is important to have a sufficient sample size in order to draw valid conclusions. The larger the sample, the more precise your results will be. If your sample size is too small, it will be difficult to identify significant relationships in the data.
Normally, statistical tests require a larger sample size to ensure that the sample is considered representative of a population and that the statistical result can be generalized to a larger population. It is a good idea to understand how to choose an appropriate sample size before you conduct your research by using scientific calculation tools—in fact, many journals now require such estimation to be included in every manuscript that is sent out for review.
Lack of previous research studies on the topic
Citing and referencing prior research studies constitutes the basis of the literature review for your thesis or study, and these prior studies provide the theoretical foundations for the research question you are investigating. However, depending on the scope of your research topic, prior research studies that are relevant to your thesis might be limited.
When there is very little or no prior research on a specific topic, you may need to develop an entirely new research typology. In this case, discovering a limitation can be considered an important opportunity to identify literature gaps and to present the need for further development in the area of study.
Methods/instruments/techniques used to collect the data
After you complete your analysis of the research findings (in the discussion section), you might realize that the manner in which you have collected the data or the ways in which you have measured variables has limited your ability to conduct a thorough analysis of the results.
For example, you might realize that you should have addressed your survey questions from another viable perspective, or that you were not able to include an important question in the survey. In these cases, you should acknowledge the deficiency or deficiencies by stating a need for future researchers to revise their specific methods for collecting data that includes these missing elements.
Common Limitations of the Researcher(s)
Study limitations that arise from situations relating to the researcher or researchers (whether the direct fault of the individuals or not) should also be addressed and dealt with, and remedies to decrease these limitations—both hypothetically in your study, and practically in future studies—should be proposed.
Limited access to data
If your research involved surveying certain people or organizations, you might have faced the problem of having limited access to these respondents. Due to this limited access, you might need to redesign or restructure your research in a different way. In this case, explain the reasons for limited access and be sure that your finding is still reliable and valid despite this limitation.
Time constraints
Just as students have deadlines to turn in their class papers, academic researchers might also have to meet deadlines for submitting a manuscript to a journal or face other time constraints related to their research (e.g., participants are only available during a certain period; funding runs out; collaborators move to a new institution). The time available to study a research problem and to measure change over time might be constrained by such practical issues. If time constraints negatively impacted your study in any way, acknowledge this impact by mentioning a need for a future study (e.g., a longitudinal study) to answer this research problem.
Conflicts arising from cultural bias and other personal issues
Researchers might hold biased views due to their cultural backgrounds or perspectives of certain phenomena, and this can affect a study’s legitimacy. Also, it is possible that researchers will have biases toward data and results that only support their hypotheses or arguments. In order to avoid these problems, the author(s) of a study should examine whether the way the research problem was stated and the data-gathering process was carried out appropriately.
Steps for Organizing Your Study Limitations Section
When you discuss the limitations of your study, don’t simply list and describe your limitations—explain how these limitations have influenced your research findings. There might be multiple limitations in your study, but you only need to point out and explain those that directly relate to and impact how you address your research questions.
We suggest that you divide your limitations section into three steps: (1) identify the study limitations; (2) explain how they impact your study in detail; and (3) propose a direction for future studies and present alternatives. By following this sequence when discussing your study’s limitations, you will be able to clearly demonstrate your study’s weakness without undermining the quality and integrity of your research.
Step 1. Identify the limitation(s) of the study
- This part should comprise around 10%-20% of your discussion of study limitations.
The first step is to identify the particular limitation(s) that affected your study. There are many possible limitations of research that can affect your study, but you don’t need to write a long review of all possible study limitations. A 200-500 word critique is an appropriate length for a research limitations section. In the beginning of this section, identify what limitations your study has faced and how important these limitations are.
You only need to identify limitations that had the greatest potential impact on: (1) the quality of your findings, and (2) your ability to answer your research question.
Step 2. Explain these study limitations in detail
- This part should comprise around 60-70% of your discussion of limitations.
After identifying your research limitations, it’s time to explain the nature of the limitations and how they potentially impacted your study. For example, when you conduct quantitative research, a lack of probability sampling is an important issue that you should mention. On the other hand, when you conduct qualitative research, the inability to generalize the research findings could be an issue that deserves mention.
Explain the role these limitations played on the results and implications of the research and justify the choice you made in using this “limiting” methodology or other action in your research. Also, make sure that these limitations didn’t undermine the quality of your dissertation .
Step 3. Propose a direction for future studies and present alternatives (optional)
- This part should comprise around 10-20% of your discussion of limitations.
After acknowledging the limitations of the research, you need to discuss some possible ways to overcome these limitations in future studies. One way to do this is to present alternative methodologies and ways to avoid issues with, or “fill in the gaps of” the limitations of this study you have presented. Discuss both the pros and cons of these alternatives and clearly explain why researchers should choose these approaches.
Make sure you are current on approaches used by prior studies and the impacts they have had on their findings. Cite review articles or scientific bodies that have recommended these approaches and why. This might be evidence in support of the approach you chose, or it might be the reason you consider your choices to be included as limitations. This process can act as a justification for your approach and a defense of your decision to take it while acknowledging the feasibility of other approaches.
P hrases and Tips for Introducing Your Study Limitations in the Discussion Section
The following phrases are frequently used to introduce the limitations of the study:
- “There may be some possible limitations in this study.”
- “The findings of this study have to be seen in light of some limitations.”
- “The first is the…The second limitation concerns the…”
- “The empirical results reported herein should be considered in the light of some limitations.”
- “This research, however, is subject to several limitations.”
- “The primary limitation to the generalization of these results is…”
- “Nonetheless, these results must be interpreted with caution and a number of limitations should be borne in mind.”
- “As with the majority of studies, the design of the current study is subject to limitations.”
- “There are two major limitations in this study that could be addressed in future research. First, the study focused on …. Second ….”
For more articles on research writing and the journal submissions and publication process, visit Wordvice’s Academic Resources page.
And be sure to receive professional English editing and proofreading services , including paper editing services , for your journal manuscript before submitting it to journal editors.
Wordvice Resources
Proofreading & Editing Guide
Writing the Results Section for a Research Paper
How to Write a Literature Review
Research Writing Tips: How to Draft a Powerful Discussion Section
How to Captivate Journal Readers with a Strong Introduction
Tips That Will Make Your Abstract a Success!
APA In-Text Citation Guide for Research Writing
Additional Resources
- Diving Deeper into Limitations and Delimitations (PhD student)
- Organizing Your Social Sciences Research Paper: Limitations of the Study (USC Library)
- Research Limitations (Research Methodology)
- How to Present Limitations and Alternatives (UMASS)
Article References
Pearson-Stuttard, J., Kypridemos, C., Collins, B., Mozaffarian, D., Huang, Y., Bandosz, P.,…Micha, R. (2018). Estimating the health and economic effects of the proposed US Food and Drug Administration voluntary sodium reformulation: Microsimulation cost-effectiveness analysis. PLOS. https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1002551
Xu, W.L, Pedersen, N.L., Keller, L., Kalpouzos, G., Wang, H.X., Graff, C,. Fratiglioni, L. (2015). HHEX_23 AA Genotype Exacerbates Effect of Diabetes on Dementia and Alzheimer Disease: A Population-Based Longitudinal Study. PLOS. Retrieved from https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1001853
- Privacy Policy

Home » Limitations in Research – Types, Examples and Writing Guide
Limitations in Research – Types, Examples and Writing Guide
Table of Contents

Limitations in Research
Limitations in research refer to the factors that may affect the results, conclusions , and generalizability of a study. These limitations can arise from various sources, such as the design of the study, the sampling methods used, the measurement tools employed, and the limitations of the data analysis techniques.
Types of Limitations in Research
Types of Limitations in Research are as follows:
Sample Size Limitations
This refers to the size of the group of people or subjects that are being studied. If the sample size is too small, then the results may not be representative of the population being studied. This can lead to a lack of generalizability of the results.
Time Limitations
Time limitations can be a constraint on the research process . This could mean that the study is unable to be conducted for a long enough period of time to observe the long-term effects of an intervention, or to collect enough data to draw accurate conclusions.
Selection Bias
This refers to a type of bias that can occur when the selection of participants in a study is not random. This can lead to a biased sample that is not representative of the population being studied.
Confounding Variables
Confounding variables are factors that can influence the outcome of a study, but are not being measured or controlled for. These can lead to inaccurate conclusions or a lack of clarity in the results.
Measurement Error
This refers to inaccuracies in the measurement of variables, such as using a faulty instrument or scale. This can lead to inaccurate results or a lack of validity in the study.
Ethical Limitations
Ethical limitations refer to the ethical constraints placed on research studies. For example, certain studies may not be allowed to be conducted due to ethical concerns, such as studies that involve harm to participants.
Examples of Limitations in Research
Some Examples of Limitations in Research are as follows:
Research Title: “The Effectiveness of Machine Learning Algorithms in Predicting Customer Behavior”
Limitations:
- The study only considered a limited number of machine learning algorithms and did not explore the effectiveness of other algorithms.
- The study used a specific dataset, which may not be representative of all customer behaviors or demographics.
- The study did not consider the potential ethical implications of using machine learning algorithms in predicting customer behavior.
Research Title: “The Impact of Online Learning on Student Performance in Computer Science Courses”
- The study was conducted during the COVID-19 pandemic, which may have affected the results due to the unique circumstances of remote learning.
- The study only included students from a single university, which may limit the generalizability of the findings to other institutions.
- The study did not consider the impact of individual differences, such as prior knowledge or motivation, on student performance in online learning environments.
Research Title: “The Effect of Gamification on User Engagement in Mobile Health Applications”
- The study only tested a specific gamification strategy and did not explore the effectiveness of other gamification techniques.
- The study relied on self-reported measures of user engagement, which may be subject to social desirability bias or measurement errors.
- The study only included a specific demographic group (e.g., young adults) and may not be generalizable to other populations with different preferences or needs.
How to Write Limitations in Research
When writing about the limitations of a research study, it is important to be honest and clear about the potential weaknesses of your work. Here are some tips for writing about limitations in research:
- Identify the limitations: Start by identifying the potential limitations of your research. These may include sample size, selection bias, measurement error, or other issues that could affect the validity and reliability of your findings.
- Be honest and objective: When describing the limitations of your research, be honest and objective. Do not try to minimize or downplay the limitations, but also do not exaggerate them. Be clear and concise in your description of the limitations.
- Provide context: It is important to provide context for the limitations of your research. For example, if your sample size was small, explain why this was the case and how it may have affected your results. Providing context can help readers understand the limitations in a broader context.
- Discuss implications : Discuss the implications of the limitations for your research findings. For example, if there was a selection bias in your sample, explain how this may have affected the generalizability of your findings. This can help readers understand the limitations in terms of their impact on the overall validity of your research.
- Provide suggestions for future research : Finally, provide suggestions for future research that can address the limitations of your study. This can help readers understand how your research fits into the broader field and can provide a roadmap for future studies.
Purpose of Limitations in Research
There are several purposes of limitations in research. Here are some of the most important ones:
- To acknowledge the boundaries of the study : Limitations help to define the scope of the research project and set realistic expectations for the findings. They can help to clarify what the study is not intended to address.
- To identify potential sources of bias: Limitations can help researchers identify potential sources of bias in their research design, data collection, or analysis. This can help to improve the validity and reliability of the findings.
- To provide opportunities for future research: Limitations can highlight areas for future research and suggest avenues for further exploration. This can help to advance knowledge in a particular field.
- To demonstrate transparency and accountability: By acknowledging the limitations of their research, researchers can demonstrate transparency and accountability to their readers, peers, and funders. This can help to build trust and credibility in the research community.
- To encourage critical thinking: Limitations can encourage readers to critically evaluate the study’s findings and consider alternative explanations or interpretations. This can help to promote a more nuanced and sophisticated understanding of the topic under investigation.
When to Write Limitations in Research
Limitations should be included in research when they help to provide a more complete understanding of the study’s results and implications. A limitation is any factor that could potentially impact the accuracy, reliability, or generalizability of the study’s findings.
It is important to identify and discuss limitations in research because doing so helps to ensure that the results are interpreted appropriately and that any conclusions drawn are supported by the available evidence. Limitations can also suggest areas for future research, highlight potential biases or confounding factors that may have affected the results, and provide context for the study’s findings.
Generally, limitations should be discussed in the conclusion section of a research paper or thesis, although they may also be mentioned in other sections, such as the introduction or methods. The specific limitations that are discussed will depend on the nature of the study, the research question being investigated, and the data that was collected.
Examples of limitations that might be discussed in research include sample size limitations, data collection methods, the validity and reliability of measures used, and potential biases or confounding factors that could have affected the results. It is important to note that limitations should not be used as a justification for poor research design or methodology, but rather as a way to enhance the understanding and interpretation of the study’s findings.
Importance of Limitations in Research
Here are some reasons why limitations are important in research:
- Enhances the credibility of research: Limitations highlight the potential weaknesses and threats to validity, which helps readers to understand the scope and boundaries of the study. This improves the credibility of research by acknowledging its limitations and providing a clear picture of what can and cannot be concluded from the study.
- Facilitates replication: By highlighting the limitations, researchers can provide detailed information about the study’s methodology, data collection, and analysis. This information helps other researchers to replicate the study and test the validity of the findings, which enhances the reliability of research.
- Guides future research : Limitations provide insights into areas for future research by identifying gaps or areas that require further investigation. This can help researchers to design more comprehensive and effective studies that build on existing knowledge.
- Provides a balanced view: Limitations help to provide a balanced view of the research by highlighting both strengths and weaknesses. This ensures that readers have a clear understanding of the study’s limitations and can make informed decisions about the generalizability and applicability of the findings.
Advantages of Limitations in Research
Here are some potential advantages of limitations in research:
- Focus : Limitations can help researchers focus their study on a specific area or population, which can make the research more relevant and useful.
- Realism : Limitations can make a study more realistic by reflecting the practical constraints and challenges of conducting research in the real world.
- Innovation : Limitations can spur researchers to be more innovative and creative in their research design and methodology, as they search for ways to work around the limitations.
- Rigor : Limitations can actually increase the rigor and credibility of a study, as researchers are forced to carefully consider the potential sources of bias and error, and address them to the best of their abilities.
- Generalizability : Limitations can actually improve the generalizability of a study by ensuring that it is not overly focused on a specific sample or situation, and that the results can be applied more broadly.
About the author
Muhammad Hassan
Researcher, Academic Writer, Web developer
You may also like

How to Cite Research Paper – All Formats and...

Data Collection – Methods Types and Examples

Delimitations in Research – Types, Examples and...

Research Paper Format – Types, Examples and...

Research Process – Steps, Examples and Tips

Research Design – Types, Methods and Examples

Writing Limitations of Research Study — 4 Reasons Why It Is Important!
It is not unusual for researchers to come across the term limitations of research during their academic paper writing. More often this is interpreted as something terrible. However, when it comes to research study, limitations can help structure the research study better. Therefore, do not underestimate significance of limitations of research study.
Allow us to take you through the context of how to evaluate the limits of your research and conclude an impactful relevance to your results.
Table of Contents
What Are the Limitations of a Research Study?
Every research has its limit and these limitations arise due to restrictions in methodology or research design. This could impact your entire research or the research paper you wish to publish. Unfortunately, most researchers choose not to discuss their limitations of research fearing it will affect the value of their article in the eyes of readers.
However, it is very important to discuss your study limitations and show it to your target audience (other researchers, journal editors, peer reviewers etc.). It is very important that you provide an explanation of how your research limitations may affect the conclusions and opinions drawn from your research. Moreover, when as an author you state the limitations of research, it shows that you have investigated all the weaknesses of your study and have a deep understanding of the subject. Being honest could impress your readers and mark your study as a sincere effort in research.
Why and Where Should You Include the Research Limitations?
The main goal of your research is to address your research objectives. Conduct experiments, get results and explain those results, and finally justify your research question . It is best to mention the limitations of research in the discussion paragraph of your research article.
At the very beginning of this paragraph, immediately after highlighting the strengths of the research methodology, you should write down your limitations. You can discuss specific points from your research limitations as suggestions for further research in the conclusion of your thesis.
1. Common Limitations of the Researchers
Limitations that are related to the researcher must be mentioned. This will help you gain transparency with your readers. Furthermore, you could provide suggestions on decreasing these limitations in you and your future studies.
2. Limited Access to Information
Your work may involve some institutions and individuals in research, and sometimes you may have problems accessing these institutions. Therefore, you need to redesign and rewrite your work. You must explain your readers the reason for limited access.
3. Limited Time
All researchers are bound by their deadlines when it comes to completing their studies. Sometimes, time constraints can affect your research negatively. However, the best practice is to acknowledge it and mention a requirement for future study to solve the research problem in a better way.
4. Conflict over Biased Views and Personal Issues
Biased views can affect the research. In fact, researchers end up choosing only those results and data that support their main argument, keeping aside the other loose ends of the research.
Types of Limitations of Research
Before beginning your research study, know that there are certain limitations to what you are testing or possible research results. There are different types that researchers may encounter, and they all have unique characteristics, such as:
1. Research Design Limitations
Certain restrictions on your research or available procedures may affect your final results or research outputs. You may have formulated research goals and objectives too broadly. However, this can help you understand how you can narrow down the formulation of research goals and objectives, thereby increasing the focus of your study.
2. Impact Limitations
Even if your research has excellent statistics and a strong design, it can suffer from the influence of the following factors:
- Presence of increasing findings as researched
- Being population specific
- A strong regional focus.
3. Data or statistical limitations
In some cases, it is impossible to collect sufficient data for research or very difficult to get access to the data. This could lead to incomplete conclusion to your study. Moreover, this insufficiency in data could be the outcome of your study design. The unclear, shabby research outline could produce more problems in interpreting your findings.
How to Correctly Structure Your Research Limitations?
There are strict guidelines for narrowing down research questions, wherein you could justify and explain potential weaknesses of your academic paper. You could go through these basic steps to get a well-structured clarity of research limitations:
- Declare that you wish to identify your limitations of research and explain their importance,
- Provide the necessary depth, explain their nature, and justify your study choices.
- Write how you are suggesting that it is possible to overcome them in the future.
In this section, your readers will see that you are aware of the potential weaknesses in your business, understand them and offer effective solutions, and it will positively strengthen your article as you clarify all limitations of research to your target audience.
Know that you cannot be perfect and there is no individual without flaws. You could use the limitations of research as a great opportunity to take on a new challenge and improve the future of research. In a typical academic paper, research limitations may relate to:
1. Formulating your goals and objectives
If you formulate goals and objectives too broadly, your work will have some shortcomings. In this case, specify effective methods or ways to narrow down the formula of goals and aim to increase your level of study focus.
2. Application of your data collection methods in research
If you do not have experience in primary data collection, there is a risk that there will be flaws in the implementation of your methods. It is necessary to accept this, and learn and educate yourself to understand data collection methods.
3. Sample sizes
This depends on the nature of problem you choose. Sample size is of a greater importance in quantitative studies as opposed to qualitative ones. If your sample size is too small, statistical tests cannot identify significant relationships or connections within a given data set.
You could point out that other researchers should base the same study on a larger sample size to get more accurate results.
4. The absence of previous studies in the field you have chosen
Writing a literature review is an important step in any scientific study because it helps researchers determine the scope of current work in the chosen field. It is a major foundation for any researcher who must use them to achieve a set of specific goals or objectives.
However, if you are focused on the most current and evolving research problem or a very narrow research problem, there may be very little prior research on your topic. For example, if you chose to explore the role of Bitcoin as the currency of the future, you may not find tons of scientific papers addressing the research problem as Bitcoins are only a new phenomenon.
It is important that you learn to identify research limitations examples at each step. Whatever field you choose, feel free to add the shortcoming of your work. This is mainly because you do not have many years of experience writing scientific papers or completing complex work. Therefore, the depth and scope of your discussions may be compromised at different levels compared to academics with a lot of expertise. Include specific points from limitations of research. Use them as suggestions for the future.
Have you ever faced a challenge of writing the limitations of research study in your paper? How did you overcome it? What ways did you follow? Were they beneficial? Let us know in the comments below!
Frequently Asked Questions
Setting limitations in our study helps to clarify the outcomes drawn from our research and enhance understanding of the subject. Moreover, it shows that the author has investigated all the weaknesses in the study.
Scope is the range and limitations of a research project which are set to define the boundaries of a project. Limitations are the impacts on the overall study due to the constraints on the research design.
Limitation in research is an impact of a constraint on the research design in the overall study. They are the flaws or weaknesses in the study, which may influence the outcome of the research.
1. Limitations in research can be written as follows: Formulate your goals and objectives 2. Analyze the chosen data collection method and the sample sizes 3. Identify your limitations of research and explain their importance 4. Provide the necessary depth, explain their nature, and justify your study choices 5. Write how you are suggesting that it is possible to overcome them in the future
Excellent article ,,,it has helped me big
This is very helpful information. It has given me an insight on how to go about my study limitations.
Good comments and helpful
Rate this article Cancel Reply
Your email address will not be published.

Enago Academy's Most Popular Articles

- Diversity and Inclusion
- Trending Now
The Silent Struggle: Confronting gender bias in science funding
In the 1990s, Dr. Katalin Kariko’s pioneering mRNA research seemed destined for obscurity, doomed by…

- Promoting Research
Plain Language Summary — Communicating your research to bridge the academic-lay gap
Science can be complex, but does that mean it should not be accessible to the…

Addressing Barriers in Academia: Navigating unconscious biases in the Ph.D. journey
In the journey of academia, a Ph.D. marks a transitional phase, like that of a…

- Manuscripts & Grants
- Reporting Research
Unraveling Research Population and Sample: Understanding their role in statistical inference
Research population and sample serve as the cornerstones of any scientific inquiry. They hold the…

- Manuscript Preparation
- Publishing Research
Research Problem Statement — Find out how to write an impactful one!
What Is a Research Problem Statement? A research problem statement is a clear, concise, and…
How to Develop a Good Research Question? — Types & Examples
5 Effective Ways to Avoid Ghostwriting for Busy Researchers
Top 5 Key Differences Between Methods and Methodology

Sign-up to read more
Subscribe for free to get unrestricted access to all our resources on research writing and academic publishing including:
- 2000+ blog articles
- 50+ Webinars
- 10+ Expert podcasts
- 50+ Infographics
- 10+ Checklists
- Research Guides
We hate spam too. We promise to protect your privacy and never spam you.
I am looking for Editing/ Proofreading services for my manuscript Tentative date of next journal submission:

As a researcher, what do you consider most when choosing an image manipulation detector?
How to present limitations in research
Last updated
30 January 2024
Reviewed by
Limitations don’t invalidate or diminish your results, but it’s best to acknowledge them. This will enable you to address any questions your study failed to answer because of them.
In this guide, learn how to recognize, present, and overcome limitations in research.
- What is a research limitation?
Research limitations are weaknesses in your research design or execution that may have impacted outcomes and conclusions. Uncovering limitations doesn’t necessarily indicate poor research design—it just means you encountered challenges you couldn’t have anticipated that limited your research efforts.
Does basic research have limitations?
Basic research aims to provide more information about your research topic. It requires the same standard research methodology and data collection efforts as any other research type, and it can also have limitations.
- Common research limitations
Researchers encounter common limitations when embarking on a study. Limitations can occur in relation to the methods you apply or the research process you design. They could also be connected to you as the researcher.
Methodology limitations
Not having access to data or reliable information can impact the methods used to facilitate your research. A lack of data or reliability may limit the parameters of your study area and the extent of your exploration.
Your sample size may also be affected because you won’t have any direction on how big or small it should be and who or what you should include. Having too few participants won’t adequately represent the population or groups of people needed to draw meaningful conclusions.
Research process limitations
The study’s design can impose constraints on the process. For example, as you’re conducting the research, issues may arise that don’t conform to the data collection methodology you developed. You may not realize until well into the process that you should have incorporated more specific questions or comprehensive experiments to generate the data you need to have confidence in your results.
Constraints on resources can also have an impact. Being limited on participants or participation incentives may limit your sample sizes. Insufficient tools, equipment, and materials to conduct a thorough study may also be a factor.
Common researcher limitations
Here are some of the common researcher limitations you may encounter:
Time: some research areas require multi-year longitudinal approaches, but you might not be able to dedicate that much time. Imagine you want to measure how much memory a person loses as they age. This may involve conducting multiple tests on a sample of participants over 20–30 years, which may be impossible.
Bias: researchers can consciously or unconsciously apply bias to their research. Biases can contribute to relying on research sources and methodologies that will only support your beliefs about the research you’re embarking on. You might also omit relevant issues or participants from the scope of your study because of your biases.
Limited access to data : you may need to pay to access specific databases or journals that would be helpful to your research process. You might also need to gain information from certain people or organizations but have limited access to them. These cases require readjusting your process and explaining why your findings are still reliable.
- Why is it important to identify limitations?
Identifying limitations adds credibility to research and provides a deeper understanding of how you arrived at your conclusions.
Constraints may have prevented you from collecting specific data or information you hoped would prove or disprove your hypothesis or provide a more comprehensive understanding of your research topic.
However, identifying the limitations contributing to your conclusions can inspire further research efforts that help gather more substantial information and data.
- Where to put limitations in a research paper
A research paper is broken up into different sections that appear in the following order:
Introduction
Methodology
The discussion portion of your paper explores your findings and puts them in the context of the overall research. Either place research limitations at the beginning of the discussion section before the analysis of your findings or at the end of the section to indicate that further research needs to be pursued.
What not to include in the limitations section
Evidence that doesn’t support your hypothesis is not a limitation, so you shouldn’t include it in the limitation section. Don’t just list limitations and their degree of severity without further explanation.
- How to present limitations
You’ll want to present the limitations of your study in a way that doesn’t diminish the validity of your research and leave the reader wondering if your results and conclusions have been compromised.
Include only the limitations that directly relate to and impact how you addressed your research questions. Following a specific format enables the reader to develop an understanding of the weaknesses within the context of your findings without doubting the quality and integrity of your research.
Identify the limitations specific to your study
You don’t have to identify every possible limitation that might have occurred during your research process. Only identify those that may have influenced the quality of your findings and your ability to answer your research question.
Explain study limitations in detail
This explanation should be the most significant portion of your limitation section.
Link each limitation with an interpretation and appraisal of their impact on the study. You’ll have to evaluate and explain whether the error, method, or validity issues influenced the study’s outcome and how.
Propose a direction for future studies and present alternatives
In this section, suggest how researchers can avoid the pitfalls you experienced during your research process.
If an issue with methodology was a limitation, propose alternate methods that may help with a smoother and more conclusive research project. Discuss the pros and cons of your alternate recommendation.
Describe steps taken to minimize each limitation
You probably took steps to try to address or mitigate limitations when you noticed them throughout the course of your research project. Describe these steps in the limitation section.
- Limitation example
“Approaches like stem cell transplantation and vaccination in AD [Alzheimer’s disease] work on a cellular or molecular level in the laboratory. However, translation into clinical settings will remain a challenge for the next decade.”
The authors are saying that even though these methods showed promise in helping people with memory loss when conducted in the lab (in other words, using animal studies), more studies are needed. These may be controlled clinical trials, for example.
However, the short life span of stem cells outside the lab and the vaccination’s severe inflammatory side effects are limitations. Researchers won’t be able to conduct clinical trials until these issues are overcome.
- How to overcome limitations in research
You’ve already started on the road to overcoming limitations in research by acknowledging that they exist. However, you need to ensure readers don’t mistake weaknesses for errors within your research design.
To do this, you’ll need to justify and explain your rationale for the methods, research design, and analysis tools you chose and how you noticed they may have presented limitations.
Your readers need to know that even when limitations presented themselves, you followed best practices and the ethical standards of your field. You didn’t violate any rules and regulations during your research process.
You’ll also want to reinforce the validity of your conclusions and results with multiple sources, methods, and perspectives. This prevents readers from assuming your findings were derived from a single or biased source.
- Learning and improving starts with limitations in research
Dealing with limitations with transparency and integrity helps identify areas for future improvements and developments. It’s a learning process, providing valuable insights into how you can improve methodologies, expand sample sizes, or explore alternate approaches to further support the validity of your findings.
Should you be using a customer insights hub?
Do you want to discover previous research faster?
Do you share your research findings with others?
Do you analyze research data?
Start for free today, add your research, and get to key insights faster
Editor’s picks
Last updated: 11 January 2024
Last updated: 15 January 2024
Last updated: 17 January 2024
Last updated: 12 May 2023
Last updated: 30 April 2024
Last updated: 18 May 2023
Last updated: 25 November 2023
Last updated: 13 May 2024
Latest articles
Related topics, .css-je19u9{-webkit-align-items:flex-end;-webkit-box-align:flex-end;-ms-flex-align:flex-end;align-items:flex-end;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-flex-direction:row;-ms-flex-direction:row;flex-direction:row;-webkit-box-flex-wrap:wrap;-webkit-flex-wrap:wrap;-ms-flex-wrap:wrap;flex-wrap:wrap;-webkit-box-pack:center;-ms-flex-pack:center;-webkit-justify-content:center;justify-content:center;row-gap:0;text-align:center;max-width:671px;}@media (max-width: 1079px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}}@media (max-width: 799px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}} decide what to .css-1kiodld{max-height:56px;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;}@media (max-width: 1079px){.css-1kiodld{display:none;}} build next, decide what to build next.

Users report unexpectedly high data usage, especially during streaming sessions.

Users find it hard to navigate from the home page to relevant playlists in the app.

It would be great to have a sleep timer feature, especially for bedtime listening.

I need better filters to find the songs or artists I’m looking for.
Log in or sign up
Get started for free
Limitations of the study
Link to guide here.
Who It’s For: New and seasoned researchers who are unfamiliar with the different possible limitations of their study and/or are unsure of how to discuss limitations in their research paper.
Why We Love It: This resource is easy-to-follow and is great to start with and return to as you consider and write about the limitations of your study. It not only explains possible limitations of your research, but offers a hand ful of useful tips for writing about these limitations effectively.

Organizing Academic Research Papers: Limitations of the Study
- Purpose of Guide
- Design Flaws to Avoid
- Glossary of Research Terms
- Narrowing a Topic Idea
- Broadening a Topic Idea
- Extending the Timeliness of a Topic Idea
- Academic Writing Style
- Choosing a Title
- Making an Outline
- Paragraph Development
- Executive Summary
- Background Information
- The Research Problem/Question
- Theoretical Framework
- Citation Tracking
- Content Alert Services
- Evaluating Sources
- Primary Sources
- Secondary Sources
- Tertiary Sources
- What Is Scholarly vs. Popular?
- Qualitative Methods
- Quantitative Methods
- Using Non-Textual Elements
- Limitations of the Study
- Common Grammar Mistakes
- Avoiding Plagiarism
- Footnotes or Endnotes?
- Further Readings
- Annotated Bibliography
- Dealing with Nervousness
- Using Visual Aids
- Grading Someone Else's Paper
- How to Manage Group Projects
- Multiple Book Review Essay
- Reviewing Collected Essays
- About Informed Consent
- Writing Field Notes
- Writing a Policy Memo
- Writing a Research Proposal
- Acknowledgements
The limitations of the study are those characteristics of design or methodology that impacted or influenced the application or interpretation of the results of your study. They are the constraints on generalizability and utility of findings that are the result of the ways in which you chose to design the study and/or the method used to establish internal and external validity.
Importance of...
Always acknowledge a study's limitations. It is far better for you to identify and acknowledge your study’s limitations than to have them pointed out by your professor and be graded down because you appear to have ignored them.
Keep in mind that acknowledgement of a study's limitations is an opportunity to make suggestions for further research. If you do connect your study's limitations to suggestions for further research, be sure to explain the ways in which these unanswered questions may become more focused because of your study.
Acknowledgement of a study's limitations also provides you with an opportunity to demonstrate to your professor that you have thought critically about the research problem, understood the relevant literature published about it, and correctly assessed the methods chosen for studying the problem. A key objective of the research process is not only discovering new knowledge but also to confront assumptions and explore what we don't know.
Claiming limitiations is a subjective process because you must evaluate the impact of those limitations . Don't just list key weaknesses and the magnitude of a study's limitations. To do so diminishes the validity of your research because it leaves the reader wondering whether, or in what ways, limitation(s) in your study may have impacted the findings and conclusions. Limitations require a critical, overall appraisal and interpretation of their impact. You should answer the question: do these problems with errors, methods, validity, etc. eventually matter and, if so, to what extent?
Structure: How to Structure the Research Limitations Section of Your Dissertation . Dissertations and Theses: An Online Textbook. Laerd.com.
Descriptions of Possible Limitations
All studies have limitations . However, it is important that you restrict your discussion to limitations related to the research problem under investigation. For example, if a meta-analysis of existing literature is not a stated purpose of your research, it should not be discussed as a limitation. Do not apologize for not addressing issues that you did not promise to investigate in your paper.
Here are examples of limitations you may need to describe and to discuss how they possibly impacted your findings. Descriptions of limitations should be stated in the past tense.
Possible Methodological Limitations
- Sample size -- the number of the units of analysis you use in your study is dictated by the type of research problem you are investigating. Note that, if your sample size is too small, it will be difficult to find significant relationships from the data, as statistical tests normally require a larger sample size to ensure a representative distribution of the population and to be considered representative of groups of people to whom results will be generalized or transferred.
- Lack of available and/or reliable data -- a lack of data or of reliable data will likely require you to limit the scope of your analysis, the size of your sample, or it can be a significant obstacle in finding a trend and a meaningful relationship. You need to not only describe these limitations but to offer reasons why you believe data is missing or is unreliable. However, don’t just throw up your hands in frustration; use this as an opportunity to describe the need for future research.
- Lack of prior research studies on the topic -- citing prior research studies forms the basis of your literature review and helps lay a foundation for understanding the research problem you are investigating. Depending on the currency or scope of your research topic, there may be little, if any, prior research on your topic. Before assuming this to be true, consult with a librarian! In cases when a librarian has confirmed that there is a lack of prior research, you may be required to develop an entirely new research typology [for example, using an exploratory rather than an explanatory research design]. Note that this limitation can serve as an important opportunity to describe the need for further research.
- Measure used to collect the data -- sometimes it is the case that, after completing your interpretation of the findings, you discover that the way in which you gathered data inhibited your ability to conduct a thorough analysis of the results. For example, you regret not including a specific question in a survey that, in retrospect, could have helped address a particular issue that emerged later in the study. Acknowledge the deficiency by stating a need in future research to revise the specific method for gathering data.
- Self-reported data -- whether you are relying on pre-existing self-reported data or you are conducting a qualitative research study and gathering the data yourself, self-reported data is limited by the fact that it rarely can be independently verified. In other words, you have to take what people say, whether in interviews, focus groups, or on questionnaires, at face value. However, self-reported data contain several potential sources of bias that should be noted as limitations: (1) selective memory (remembering or not remembering experiences or events that occurred at some point in the past); (2) telescoping [recalling events that occurred at one time as if they occurred at another time]; (3) attribution [the act of attributing positive events and outcomes to one's own agency but attributing negative events and outcomes to external forces]; and, (4) exaggeration [the act of representing outcomes or embellishing events as more significant than is actually suggested from other data].
Possible Limitations of the Researcher
- Access -- if your study depends on having access to people, organizations, or documents and, for whatever reason, access is denied or otherwise limited, the reasons for this need to be described.
- Longitudinal effects -- unlike your professor, who can literally devote years [even a lifetime] to studying a single research problem, the time available to investigate a research problem and to measure change or stability within a sample is constrained by the due date of your assignment. Be sure to choose a topic that does not require an excessive amount of time to complete the literature review, apply the methodology, and gather and interpret the results. If you're unsure, talk to your professor.
- Cultural and other type of bias -- we all have biases, whether we are conscience of them or not. Bias is when a person, place, or thing is viewed or shown in a consistently inaccurate way. It is usually negative, though one can have a positive bias as well. When proof-reading your paper, be especially critical in reviewing how you have stated a problem, selected the data to be studied, what may have been omitted, the manner in which you have ordered events, people, or places and how you have chosen to represent a person, place, or thing, to name a phenomenon, or to use possible words with a positive or negative connotation. Note that if you detect bias in prior research, it must be acknowledged and you should explain what measures were taken to avoid perpetuating bias.
- Fluency in a language -- if your research focuses on measuring the perceived value of after-school tutoring among Mexican-American ESL [English as a Second Language] students, for example, and you are not fluent in Spanish, you are limited in being able to read and interpret Spanish language research studies on the topic. This deficiency should be acknowledged.
Brutus, Stéphane et al. Self-Reported Limitations and Future Directions in Scholarly Reports: Analysis and Recommendations. Journal of Management 39 (January 2013): 48-75; Senunyeme, Emmanuel K. Business Research Methods . Powerpoint Presentation. Regent University of Science and Technology.
Structure and Writing Style
Information about the limitations of your study are generally placed either at the beginning of the discussion section of your paper so the reader knows and understands the limitations before reading the rest of your analysis of the findings, or, the limitations are outlined at the conclusion of the discussion section as an acknowledgement of the need for further study. Statements about a study's limitations should not be buried in the body [middle] of the discussion section unless a limitation is specific to something covered in that part of the paper. If this is the case, though, the limitation should be reiterated at the conclusion of the section.
If you determine that your study is seriously flawed due to important limitations , such as, an inability to acquire critical data, consider reframing it as a pilot study intended to lay the groundwork for a more complete research study in the future. Be sure, though, to specifically explain the ways that these flaws can be successfully overcome in later studies.
But, do not use this as an excuse for not developing a thorough research paper! Review the tab in this guide for developing a research topic . If serious limitations exist, it generally indicates a likelihood that your research problem is too narrowly defined or that the issue or event under study is too recent and, thus, very little research has been written about it. If serious limitations do emerge, consult with your professor about possible ways to overcome them or how to reframe your study.
When discussing the limitations of your research, be sure to:
- Describe each limitation in detailed but concise terms;
- Explain why each limitation exists;
- Provide the reasons why each limitation could not be overcome using the method(s) chosen to gather the data [cite to other studies that had similar problems when possible];
- Assess the impact of each limitation in relation to the overall findings and conclusions of your study; and,
- If appropriate, describe how these limitations could point to the need for further research.
Remember that the method you chose may be the source of a significant limitation that has emerged during your interpretation of the results [for example, you didn't ask a particular question in a survey that you later wish you had]. If this is the case, don't panic. Acknowledge it, and explain how applying a different or more robust methodology might address the research problem more effectively in any future study. A underlying goal of scholarly research is not only to prove what works, but to demonstrate what doesn't work or what needs further clarification.
Brutus, Stéphane et al. Self-Reported Limitations and Future Directions in Scholarly Reports: Analysis and Recommendations. Journal of Management 39 (January 2013): 48-75; Ioannidis, John P.A. Limitations are not Properly Acknowledged in the Scientific Literature. Journal of Clinical Epidemiology 60 (2007): 324-329; Pasek, Josh. Writing the Empirical Social Science Research Paper: A Guide for the Perplexed . January 24, 2012. Academia.edu; Structure: How to Structure the Research Limitations Section of Your Dissertation . Dissertations and Theses: An Online Textbook. Laerd.com; What Is an Academic Paper? Institute for Writing Rhetoric. Dartmouth College; Writing the Experimental Report: Methods, Results, and Discussion. The Writing Lab and The OWL. Purdue University.
Writing Tip
Don't Inflate the Importance of Your Findings! After all the hard work and long hours devoted to writing your research paper, it is easy to get carried away with attributing unwarranted importance to what you’ve done. We all want our academic work to be viewed as excellent and worthy of a good grade, but it is important that you understand and openly acknowledge the limitiations of your study. Inflating of the importance of your study's findings in an attempt hide its flaws is a big turn off to your readers. A measure of humility goes a long way!
Another Writing Tip
Negative Results are Not a Limitation!
Negative evidence refers to findings that unexpectedly challenge rather than support your hypothesis. If you didn't get the results you anticipated, it may mean your hypothesis was incorrect and needs to be reformulated, or, perhaps you have stumbled onto something unexpected that warrants further study. Moreover, the absence of an effect may be very telling in many situations, particularly in experimental research designs. In any case, your results may be of importance to others even though they did not support your hypothesis. Do not fall into the trap of thinking that results contrary to what you expected is a limitation to your study. If you carried out the research well, they are simply your results and only require additional interpretation.
Yet Another Writing Tip
A Note about Sample Size Limitations in Qualitative Research
Sample sizes are typically smaller in qualitative research because, as the study goes on, acquiring more data does not necessarily lead to more information. This is because one occurrence of a piece of data, or a code, is all that is necessary to ensure that it becomes part of the analysis framework. However, it remains true that sample sizes that are too small cannot adequately support claims of having achieved valid conclusions and sample sizes that are too large do not permit the deep, naturalistic, and inductive analysis that defines qualitative inquiry. Determining adequate sample size in qualitative research is ultimately a matter of judgment and experience in evaluating the quality of the information collected against the uses to which it will be applied and the particular research method and purposeful sampling strategy employed. If the sample size is found to be a limitation, it may reflect your judgement about the methodological technique chosen [e.g., single life history study versus focus group interviews] rather than the number of respondents used.
Huberman, A. Michael and Matthew B. Miles. Data Management and Analysis Methods. In Handbook of Qualitative Research. Norman K. Denzin and Yvonna S. Lincoln, eds. (Thousand Oaks, CA: Sage, 1994), pp. 428-444.
- << Previous: 8. The Discussion
- Next: 9. The Conclusion >>
- Last Updated: Jul 18, 2023 11:58 AM
- URL: https://library.sacredheart.edu/c.php?g=29803
- QuickSearch
- Library Catalog
- Databases A-Z
- Publication Finder
- Course Reserves
- Citation Linker
- Digital Commons
- Our Website
Research Support
- Ask a Librarian
- Appointments
- Interlibrary Loan (ILL)
- Research Guides
- Databases by Subject
- Citation Help
Using the Library
- Reserve a Group Study Room
- Renew Books
- Honors Study Rooms
- Off-Campus Access
- Library Policies
- Library Technology
User Information
- Grad Students
- Online Students
- COVID-19 Updates
- Staff Directory
- News & Announcements
- Library Newsletter
My Accounts
- Interlibrary Loan
- Staff Site Login
FIND US ON
- Link to facebook
- Link to linkedin
- Link to twitter
- Link to youtube
- Writing Tips
How to Identify Limitations in Research

4-minute read
- 7th March 2022
Whether you’re a veteran researcher with years of experience under your belt or a novice to the field that’s feeling overwhelmed with where to start, you must understand that every study has its limitations. These are restrictions that arise from the study’s design, or the methodology implemented during the testing phase. Unfortunately, research limitations will always exist due to the subjective nature of testing a hypothesis. We’ve compiled some helpful information below on how to identify and accept research limitations and use them to your advantage. Essentially, we’ll show you how to make lemonade (a brilliant piece of academic work ) from the lemons you receive (the constraints your study reveals).
Research Limitations
So, let’s dive straight in, shall we? It’s always beneficial (and good practice) to disclose your research limitations . A common thought is that divulging these shortcomings will undermine the credibility and quality of your research. However, this is certainly not the case— stating the facts upfront not only reinforces your reputation as a researcher but also lets the assessor or reader know that you’re confident and transparent about the results and relevance of your study, despite these constraints.
Additionally, it creates a gap for more research opportunities, where you can analyze these limitations and determine how to incorporate or address them in a new batch of tests or create a new hypothesis altogether. Another bonus is that it helps readers to understand the optimum conditions for how to apply the results of your testing. This is a win-win, making for a far more persuasive research paper .
Now that you know why you should clarify your research limitations, let’s focus on which ones take precedence and should be disclosed. Any given research project can be vulnerable to various hindrances, so how do you identify them and single out the most significant ones to discuss? Well, that depends entirely on the nature of your study. You’ll need to comb through your research approach, methodology, testing processes, and expected results to identify the type of limitations your study may be exposed to. It’s worth noting that this understanding can only offer a broad idea of the possible restrictions you’ll face and may potentially change throughout the study.
We’ve compiled a list of the most common types of research limitations that you may encounter so you can adequately prepare for them and remain vigilant during each stage of your study.
Sample Size:
It’s critical that you choose a sample size that accurately represents the population you wish to test your theory on. If a sample is too small, the results cannot reliably be generalized across a large population.
Methodology:
The method you choose before you commence testing might seem effective in theory, but too many stumbling blocks during the testing phase can influence the accuracy and reliability of the results.
Find this useful?
Subscribe to our newsletter and get writing tips from our editors straight to your inbox.
Collection of Data:
The methods you utilize to obtain your research—surveys, emails, in-person interviews, phone calls—will directly influence the type of results your study yields.
Age of Data:
The nature of the information—and how far back it goes—affects the type of assumptions you can make. Extrapolating older data for a current hypothesis can significantly change the outcome of your testing.
Time Constraints:
Working within the deadline of when you need to submit your findings will determine the extent of your research and testing and, therefore, can heavily impact your results. Limited time frames for testing might mean not achieving the scope of results you were originally looking for.
Limited Budget:
Your study may require equipment and other resources that can become extremely costly. Budget constraints may mean you cannot acquire advanced software, programs, or travel to multiple destinations to interview participants. All of these factors can substantially influence your results.
So, now that you know how to determine your research limitations and the types you might experience, where should you document it? It’s commonly disclosed at the beginning of your discussion section , so the reader understands the shortcomings of your study before digging into the juicy bit—your findings. Alternatively, you can detail the constraints faced at the end of the discussion section to emphasize the requirements for the completion of further studies.
We hope this post will prepare you for some of the pitfalls you may encounter when conducting and documenting your research. Once you have a first draft ready, consider submitting a free sample to us for proofreading to ensure that your writing is concise and error-free and your results—despite their limitations— shine through.
Share this article:
Post A New Comment
Got content that needs a quick turnaround? Let us polish your work. Explore our editorial business services.
9-minute read
How to Use Infographics to Boost Your Presentation
Is your content getting noticed? Capturing and maintaining an audience’s attention is a challenge when...
8-minute read
Why Interactive PDFs Are Better for Engagement
Are you looking to enhance engagement and captivate your audience through your professional documents? Interactive...
7-minute read
Seven Key Strategies for Voice Search Optimization
Voice search optimization is rapidly shaping the digital landscape, requiring content professionals to adapt their...
Five Creative Ways to Showcase Your Digital Portfolio
Are you a creative freelancer looking to make a lasting impression on potential clients or...
How to Ace Slack Messaging for Contractors and Freelancers
Effective professional communication is an important skill for contractors and freelancers navigating remote work environments....
3-minute read
How to Insert a Text Box in a Google Doc
Google Docs is a powerful collaborative tool, and mastering its features can significantly enhance your...

Make sure your writing is the best it can be with our expert English proofreading and editing.
International Science Editing
June 6, 2019 by Lisa Clancy
Discussing your study’s limitations
Why include a limitations section.
Including a section on the limitations of your findings will demonstrate command over your research. A reviewer may look negatively upon your study if they spot a limitation that you failed to acknowledge. If you discuss each limitation in the context of future research—i.e., suggest ways to improve the validity of the research in future studies—your article is more likely to be cited, as it will inform the research questions of other researchers.
How to identify the limitations of your study
You should think about your study from two angles – internal validity and external validity.
Internal validity refers to the strength of the inferences from the study, i.e., how confident you are that the outcome observed was caused by the test variable. Could other factors have affected the outcome? If so, the internal validity of your study may be threatened.
External validity refers to the degree to which the results can be generalised to a more universal population. If you were to re-do the study in a different context, e.g., with different subjects or in a different setting, would you get a similar outcome? If not, the external validity of your study may be questionable.
Limitations should not be feared
It is important to remember that all studies are questionable in one way or another. Therefore, a study does not have to be limitation-free to be deemed acceptable.
In this post…
…we list the most commonly seen limitations in STEM studies and provide real-world examples. However, please be advised that this is not a comprehensive list. In addition, please note that these limitations are not mutually exclusive; many can overlap.

Examples of study limitations
Selection bias
Selection bias occurs when the selection of individuals, groups, or data for analysis is not randomised.
For example, imagine a study in which different surgical procedures are retrospectively compared in relation to mortality risk [e.g., 1]. One of the procedures is newer than the others. Surgeons typically choose the most ideal surgery candidates when testing new procedures. Therefore, the outcome of the study could be affected by surgeons selectively choosing a particular type of individual—ideal candidates for surgery—for only one of the treatment groups.
Confounding
A confounder is another, sometimes hidden, variable that affects the dependent variable. If a confounder is not accounted for, any relationships detected between the test variable and outcome could be inaccurate.
For example, imagine a study in which the use of eye-tracking applications to measure cognitive performance is examined [e.g., 2]. Cognitive performance is known to decrease with age. Therefore, if age is not included as a confounder in the study, the effect size could be under- or overestimated.
In another example, imagine a study in which the association between osteoarthritis and cardiovascular (CV) events is examined [e.g., 3]. CV events have been linked to many factors, including smoking status, abdominal obesity, family history of CV events … etc., all of which could confound the outcome if not controlled for.
Survivorship bias
Survivorship bias occurs if inferences are made on the basis of only those subjects that made it past some selection process and those that did not were overlooked, typically because of their lack of visibility.
For example, imagine a study in which the link between cycling and sexual dysfunction is examined [e.g., 4]. It is possible that a person who experiences sexual dysfunction due to cycling would quit the activity. Therefore, if only active cyclists were recruited in the study, such a person would be overlooked, constituting a bias that could affect the study outcome.
Study scope limitations
Unreliable or unavailable data can limit the scope of a study and thus the overall outcome.
For example, imagine a study in which heat generation in different world regions is examined [e.g., 5]. The researchers do not have data on the use of firewood in households. In some regions, e.g., developing countries, household firewood use contributes greatly to the total heat produced. Therefore, the heat generation for such regions could be underestimated.
Sample size limitations
A small sample size may make it difficult to determine if a particular outcome is a true finding and in some cases a type II error may occur, i.e., the null hypothesis is incorrectly accepted and no difference between the study groups is reported.
For example, imagine a study in which the efficacy of thrombolysis in treating acute myocardial infarction (AMI) is examined. Thrombolysis has an important but very small effect on AMI. Therefore, a study with a relatively small sample size may not have the (statistical) power to expose such a small effect, possibly resulting in a type II error [6].
Experimenter bias
Experimenter bias occurs when the individuals running the experiment inadvertently affect the outcome by unconsciously behaving in different ways to participants in the different treatment groups.
For example, imagine a study in which gamers are tested for their ability to know whether they are playing against a human or an AI avatar [e.g., 7]. The facilitator stands behind the participant and observes gameplay. If the facilitator is aware of the nature of the avatar, there is a chance that they could unintentionally influence the participant.
Referral bias
Referral bias refers to the phenomenon whereby patients that are referred from one clinic to another, often to specialised units, tend to be sicker than non-referred patients. In studies including many referrals, risk factors are likely to be overestimated.
For example, imagine a study in which the clinical characteristics of neuroarcoidosis are evaluated in a specialised referral centre [e.g., 8]. Chronic aseptic meningitis is found to be the most frequently reported pathology—37% of cases. This frequency is relatively higher compared with other studies. The centre is known to have specific expertise on chronic meningitis. Therefore, cases of this kind are more likely to be referred to the centre, constituting a referral bias.
Self-reported data
Self-reported data is subject to various biases, e.g., selective memory, exaggeration … etc., and cannot be independently verified.
For example, imagine a study in which the effectiveness of typing pressure in determining stress in smartphone users is examined [e.g., 9]. Participants are asked to recall a stressful experience and rank their stress on a scale, after which typing pressure is measured. For whatever reason, participants may over- or underestimate their stress levels, affecting the outcome of the study.
Limitations of exploratory studies
If there has been little or no prior research on a topic, researchers may be required to establish a benchmark in relation to the research question and study design. As there is no benchmark for comparison, the validity of the outcome is disputable.
For example, imagine an exploratory study in which TV users are tested for usability of a new type of remote controller [e.g., 10]. Rather than the typical pressing of buttons, actions can be performed by squeezing or puffing on the remote. Findings from this study cannot be deemed conclusive until the results are replicated.
Methodological limitations
This refers to limitations in relation to the methodology used in a study.
For example, imagine a study in which the utility of telomere length as a diagnostic parameter for dyskeratosis congenita (DC) is tested [e.g., 11]. The data of DC patients from two different hospitals are used in the study. Each hospital uses its own method for DNA extraction, one of which has been shown to extract shorter DNA, a limitation which could affect the study outcome.
In another example, imagine a study in which a novel technology is tested for its ability to monitor damage in structures known to be difficult to monitor (e.g., beneath bridges) [e.g., 12]. The study suggests that the new technology is promising; however, its coverage area is only 30 × 30 m, meaning it is only suitable for short-distance applications.
Systematic literature reviews
In a systematic literature review (SLR), researchers use a well-defined search strategy to search for literature relevant to a particular research question. However, depending on the search criteria, there is no guarantee that all relevant literature will be retrieved from the search; Often grey literature – e.g., theses and technical reports – are excluded; and often SLRs only include studies presented in one language, typically English.
Hawthorne effect
This refers to the phenomenon whereby participants behave differently when they are aware that they are being observed.
For example, imagine a study in which fear appeal messages are tested for their ability to promote security behaviour online [e.g., 13]. Participants are shown a fear appeal message detailing the prevalence and effects of cyber-attacks, after which they are surveyed on their behaviour online. Participants are surveyed again 4 weeks later to see if the effect of the fear appeal lasted over time and whether intentions were acted upon. Participants may fraudulently claim to have improved their behaviour in an effort to diminish shame at not having altered their behaviour or in an effort to please the study conductors.
Regression toward the mean
This refers to the phenomenon whereby a variable that is extreme (i.e., far away from the average) the first time it is measured will be less extreme the next time it is measured. This typically happens with asymmetric sampling, e.g., only the very worst or the very best performers are used in a study. However, it can occur by chance as well (see the example given).
For example, imagine a study in which the effects of haematocrit (the ratio of the volume of red blood cells to the total volume of blood) on avian flight performance is examined [e.g., 14]. In the pre-test, i.e., before their haematocrit is manipulated, birds in one of the treatment groups have considerably better flight performance compared to the other groups. Even without manipulation, the flight performance of these birds would likely be reduced if the test was repeated, due to the regression toward the mean effect. Therefore, the results of the post-test, i.e., after manipulation, may be influenced by this effect and may not be reflective of the true effects of the manipulation.
Repeated testing
Repeatedly testing participants may lead to bias. A pre-test may sensitise participants in unanticipated ways, influencing the results of the post-test.
For example, imagine a study in which the anxiety induced from different eye tests used to diagnose glaucoma is measured [e.g., 15]. Almost all of the participants have already experienced one of the tests. This could lead to an underestimation of the magnitude by which anxiety increases with this test.
Population validity
This refers to how representative the sample used in a study is to the target population.
For example, imagine a study in which the target population is all U.S. Internet users. It would not be representative to only use data from Twitter users, as U.S. adult Twitter users are younger and more likely to be Democrats compared to the general public [16].
How to present limitations
Study limitations are generally presented towards the end of the discussion section in the past tense (see our post on Verb Tenses in Scientific Manuscripts ). Start by stating the limitation. Mention if you took any steps to circumvent the issue. Describe any evidence that might lessen the effect of the limitation. Discuss how the limitation could affect the study outcome. Finally, if applicable, discuss the steps that could be taken to overcome the limitation in future studies.
- Stiles ZE, Behrman SW, Glazer ES, Deneve JL, Dong L, Wan JY, Dickson PV. Predictors and implications of unplanned conversion during minimally invasive hepatectomy: an analysis of the ACS-NSQIP database. HPB. 2017 Nov 1;19(11):957–65.
- Rosa PJ, Gamito P, Oliveira J, Morais D, Pavlovic M, Smyth O. Show me your eyes! The combined use of eye tracking and virtual reality applications for cognitive assessment. In Proceedings of the 3rd 2015 workshop on ICTs for Improving Patients Rehabilitation Research Techniques 2015 Oct 1 (pp. 135–138). ACM.
- Kendzerska T, Jüni P, King LK, Croxford R, Stanaitis I, Hawker GA. The longitudinal relationship between hand, hip and knee osteoarthritis and cardiovascular events: a population-based cohort study. Osteoarthr Cartilage. 2017 Nov 1;25(11):1771–80.
- Gaither TW, Awad MA, Murphy GP, Metzler I, Sanford T, Eisenberg ML, Sutcliffe S, Osterberg EC, Breyer BN. Cycling and female sexual and urinary function: results from a large, multinational, cross-sectional study. J Sex Med. 2018 Apr 1;15(4):510–8.
- Mekonnen MM, Gerbens-Leenes PW, Hoekstra AY. The consumptive water footprint of electricity and heat: a global assessment. Environ Sci-Water Res Technol. 2015;1(3):285–97.
- Jones SR, Carley S, Harrison M. An introduction to power and sample size estimation. Emerg Med J. 2003 Sep 1;20(5):453–8.
- Wehbe RR, Lank E, Nacke LE. Left Them 4 Dead: Perception of humans versus non-player character teammates in cooperative gameplay. In Proceedings of the 2017 Conference on Designing Interactive Systems 2017 Jun 10 (pp. 403–415). ACM.
- Leonhard SE, Fritz D, Eftimov F, van der Kooi AJ, van de Beek D, Brouwer MC. Neurosarcoidosis in a tertiary referral center: a cross-sectional cohort study. Medicine. 2016 Apr;95(14).
- Exposito M, Picard RW, Hernandez J. Affective keys: towards unobtrusive stress sensing of smartphone users. In Proceedings of the 20th International Conference on Human-Computer Interaction with Mobile Devices and Services Adjunct 2018 Sep 3 (pp. 139–145). ACM.
- Bernhaupt R, Desnos A, Pirker M, Schwaiger D. TV interaction beyond the button press. InIFIP Conference on Human-Computer Interaction 2015 Sep 14 (pp. 412–419). Springer, Cham.
- Gadalla SM, Khincha PP, Katki HA, Giri N, Wong JY, Spellman S, Yanovski JA, Han JC, De Vivo I, Alter BP, Savage SA. The limitations of qPCR telomere length measurement in diagnosing dyskeratosis congenita. Mol Genet Genomic Med. 2016 Jul;4(4):475–9.
- Kang D, Cha YJ. Autonomous UAVs for structural health monitoring using deep learning and an ultrasonic beacon system with geo‐tagging. Comput Aided Civ Inf. 2018 Oct;33(10):885–902.
- Jansen J, van Schaik P. The design and evaluation of a theory-based intervention to promote security behaviour against phishing. Int J Hum Comput Stud. 2019 Mar 1;123:40–55.
- Yap KN, Dick MF, Guglielmo CG, Williams TD. Effects of experimental manipulation of hematocrit on avian flight performance in high-and low-altitude conditions. J Exp Biol. 2018 Nov 15;221(22):jeb191056.
- Chew SS, Kerr NM, Wong AB, Craig JP, Chou CY, Danesh-Meyer HV. Anxiety in visual field testing. Br J Ophthalmol. 2016 Aug 1;100(8):1128–33.
- Pew Research Center. Sizing Up Twitter Users. 2019 Apr 24. Available from: https://www.pewinternet.org/2019/04/24/sizing-up-twitter-users/ [Accessed 6 June 2019].
European Office
Tel: +353 61 472818 International Science Editing Compuscript Ltd, Shannon Industrial Estate West, Shannon, Republic of Ireland.
Chinese Office
Tel: 0512-67621565, 0512-87661520 International Science Editing Room 2013, Locca Tower, 8th Jiarui Road, Suzhou Industrial Park, Suzhou, Jiangsu Province, China. 访问我们的中文网页
North American Office
Tel: 717-668-9325 International Science Editing 2930 Legacy Lane, York, Pennsylvania, 17402, U.S.A.
Privacy Overview
These cookies do not store any directly identifiable information. However, they are necessary for the Service to function. They are usually only set in response to actions made by you which amount to a request for services, such as setting your privacy preferences, logging in, or filling in forms. You can set your browser to block or alert you about these cookies, but without these cookies, some or all of the services you have asked for may not work properly.
Undefined cookies are those that are being analyzed and have not been classified into a category as yet.
These are analytics and research cookies that allow us to count visits and measure traffic, so we can measure and improve the performance of our Services. They also help us to know which pages are the most and least popular and see how visitors move around the site(s) or application(s). This helps us to improve the way our Services work and improve user experience. You can set your browser to block or alert you about these cookies. Blocking these cookies will not affect the service provided to you.
Preference cookies are used to store user preferences to provide content that is customized and convenient for the users, like the language of the website or the location of the visitor.
These files, or code may be included, either directly or from our advertising partners, on our website, in our emails, or mobile applications to record how you interact with us, to help us better analyse and improve our services to you, and will use this information to make the website, and, any advertising displayed to you more relevant to your interests. You can set your browser to block or alert you about these cookies. Blocking these cookies will not affect the service provided to you but will limit the targeted advertising that you will see or limit our ability to tailor the website experience to your needs.
Analytical cookies are used to understand how visitors interact with the website. These cookies help provide information on metrics the number of visitors, bounce rate, traffic source, etc.
Research Limitations & Delimitations
What they are and how they’re different (with examples)
By: Derek Jansen (MBA) | Expert Reviewed By: David Phair (PhD) | September 2022
If you’re new to the world of research, you’ve probably heard the terms “ research limitations ” and “ research delimitations ” being thrown around, often quite loosely. In this post, we’ll unpack what both of these mean, how they’re similar and how they’re different – so that you can write up these sections the right way.
Overview: Limitations vs Delimitations
- Are they the same?
- What are research limitations
- What are research delimitations
- Limitations vs delimitations
First things first…
Let’s start with the most important takeaway point of this post – research limitations and research delimitations are not the same – but they are related to each other (we’ll unpack that a little later). So, if you hear someone using these two words interchangeably, be sure to share this post with them!
Research Limitations
Research limitations are, at the simplest level, the weaknesses of the study , based on factors that are often outside of your control as the researcher. These factors could include things like time , access to funding, equipment , data or participants . For example, if you weren’t able to access a random sample of participants for your study and had to adopt a convenience sampling strategy instead, that would impact the generalizability of your findings and therefore reflect a limitation of your study.
Research limitations can also emerge from the research design itself . For example, if you were undertaking a correlational study, you wouldn’t be able to infer causality (since correlation doesn’t mean certain causation). Similarly, if you utilised online surveys to collect data from your participants, you naturally wouldn’t be able to get the same degree of rich data that you would from in-person interviews .
Simply put, research limitations reflect the shortcomings of a study , based on practical (or theoretical) constraints that the researcher faced. These shortcomings limit what you can conclude from a study, but at the same time, present a foundation for future research . Importantly, all research has limitations , so there’s no need to hide anything here – as long as you discuss how the limitations might affect your findings, it’s all good.
Research Delimitations
Alright, now that we’ve unpacked the limitations, let’s move on to the delimitations .
Research delimitations are similar to limitations in that they also “ limit ” the study, but their focus is entirely different. Specifically, the delimitations of a study refer to the scope of the research aims and research questions . In other words, delimitations reflect the choices you, as the researcher, intentionally make in terms of what you will and won’t try to achieve with your study. In other words, what your research aims and research questions will and won’t include.
As we’ve spoken about many times before, it’s important to have a tight, narrow focus for your research, so that you can dive deeply into your topic, apply your energy to one specific area and develop meaningful insights. If you have an overly broad scope or unfocused topic, your research will often pull in multiple, even opposing directions, and you’ll just land up with a muddy mess of findings .
So, the delimitations section is where you’ll clearly state what your research aims and research questions will focus on – and just as importantly, what they will exclude . For example, you might investigate a widespread phenomenon, but choose to focus your study on a specific age group, ethnicity or gender. Similarly, your study may focus exclusively on one country, city or even organization. As long as the scope is well justified (in other words, it represents a novel, valuable research topic), this is perfectly acceptable – in fact, it’s essential. Remember, focus is your friend.
Need a helping hand?
Conclusion: Limitations vs Delimitations
Ok, so let’s recap.
Research limitations and research delimitations are related in that they both refer to “limits” within a study. But, they are distinctly different. Limitations reflect the shortcomings of your study, based on practical or theoretical constraints that you faced.
Contrasted to that, delimitations reflect the choices that you made in terms of the focus and scope of your research aims and research questions. If you want to learn more about research aims and questions, you can check out this video post , where we unpack those concepts in detail.

Psst... there’s more!
This post was based on one of our popular Research Bootcamps . If you're working on a research project, you'll definitely want to check this out ...
You Might Also Like:

18 Comments
Good clarification of ideas on how a researcher ought to do during Process of choice
Thank you so much for this very simple but explicit explanation on limitation and delimitation. It has so helped me to develop my masters proposal. hope to recieve more from your site as time progresses
Thank you for this explanation – very clear.
Thanks for the explanation, really got it well.
This website is really helpful for my masters proposal
Thank you very much for helping to explain these two terms
I spent almost the whole day trying to figure out the differences
when I came across your notes everything became very clear
thanks for the clearly outlined explanation on the two terms, limitation and delimitation.
Very helpful Many thanks 🙏
Excellent it resolved my conflict .
I would like you to assist me please. If in my Research, I interviewed some participants and I submitted Questionnaires to other participants to answered to the questions, in the same organization, Is this a Qualitative methodology , a Quantitative Methodology or is it a Mixture Methodology I have used in my research? Please help me
How do I cite this article in APA format
Really so great ,finally have understood it’s difference now
Getting more clear regarding Limitations and Delimitation and concepts
I really appreciate your apt and precise explanation of the two concepts namely ; Limitations and Delimitations.
This is a good sources of research information for learners.
thank you for this, very helpful to researchers
Very good explained
Great and clear explanation, after a long confusion period on the two words, i can now explain to someone with ease.
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.56(5); 2021 Oct
A Focus on Evaluating Major Study Limitations in Order to Apply Clinical Trials to Patient Care: Implications for the Healthcare Team
Mary j. ferrill.
1 Taiwan Medical University, Columbia, SC, USA
Alireza FakhriRavari
2 Loma Linda University, Loma Linda, CA, USA
Jody Jacobson Wedret
3 University of California, Irvine Medical Center, Tustin Ranch, CA, USA
Background: With more than a million new biomedical articles published annually, healthcare providers must stay up to date in order to provide optimal evidence-based patient care. The concise ROOTs (relevance, observe validity, obtain clinically significant results, and translate results to clinical practice) format is a valuable tool to assist with literature evaluation. Purpose: To illustrate how major study limitations found in clinical trials might inhibit the ability to adopt the findings of such studies to patient care. Methods: Examples from published clinical trials that contain major study flaws were used to illustrate, if taken at face value, would lead to erroneous assumptions, and if adopted, could potentiallly harm patients. Conclusion: When evaluating the literature, it is crucial to identify limitations in the published literature that might reduce the internal validity, affect the results, or limit the external validity of clinical trials, hence affecting the usability of literature for patient care. This article provides examples of clinical trials that contain major study limitations with potentially erroneous assumptions. These illustrations are meant to show how important it is to delve deeper into an article before conclusions are drawn.
Introduction
The amount of information published annually in the biomedical literature, especially clinical trials, continues to expand which makes it a challenge for healthcare professionals to stay informed in order to provide optimal evidence-based patient care. The ROOTs (relevance, observe validity, obtain clinically significant results, and translate results to clinical practice) format was developed to streamline the literature evaluation process of clinical trials. It provides practitioners a guide to evaluate new information and assess relevance to a clinical situation. 1 While this tool was originally intended for journal club application, the evaluation process is equally useful for the sole practitioner or clinician reading and evaluating independently.
In the ROOTs manuscript, it mentions a few examples of study limitations that could deter extrapolation of study results to patient care, and that this piece is one of the principle shortcomings of an effective journal club. 1 Therefore, this article will provide examples of clinical trials published in the medical literature that contain major study limitations (see Table 1 ) to demonstrate why the evaluation of literature is so important in assuring against erroneously adopting conclusions which are not founded on good science. The table is divided into three sections, limitations that affect internal validity, results, and external validity to assist with organizing the evaluation process. Internal validity refers to the quality of a study’s methods or study design and the subsequent confidence readers can have in the results. External validity is the degree to which the study results are meaningful to practitioners and useful for patient care. 2 It should be noted that the internal validity of a study should be analyzed first prior to examining external validity because deficits in the study design might limit who the results can be applied to in the general population. The section on limitations that affect results contain errors that directly affect interpretation of the study results. Through the illustrations, clinicians should be able to accurately determine the utility of published clinical trials to improve patient care by incorporating evidence-based medicine into practice. For pharmacists working at the bedside, in clinics, in the community environment, in a managed care organization, or on a Pharmacy and Therapeutics committee, accurately evaluating study data provides support for a rational discussion to potentially negate incorrect conclusions or to provide evidence to champion why and in what circumstances a treatment makes sense. After all, it is the role of the pharmacist to promote rational and safe medication use.
Examples of Potential Major Clinical Trial Limitations.
Limitations That Reduce Internal Validity
Treatment regimen not appropriate: comparison with suboptimally dosed control or not the standard.
One aspect of a clinical trial that should be of special importance to pharmacists is that study drugs are given at therapeutically appropriate doses. If not, it is impossible to determine if the outcome would have been different if appropriate doses were administered. Berman et al 3 conducted a study to determine if aripiprazole was effective as adjunctive therapy in patients with major depressive disorder. The rationale for the study was that 60% of patients do not respond to at least one antidepressant when given at an adequate dose. In the study, patients with an inadequate response to standard antidepressant therapy were given aripiprazole or placebo. Results showed that patients in the aripiprazole group had a significant decrease in the primary outcome compared to placebo. The methods stated that patients received one of five different antidepressants at adequate doses. However, in the results, the average doses were significantly lower than the standard dosing in all but one of the five medications. If the patients had truly received an adequate dose, the beneficial effects of adjunctive aripiprazole might not have been significantly noted.
Treatment Regimen Not Appropriate: Intervention With Suboptimally Dosed Treatment
Suboptimal dosing of the control arm will bias the results in favor of the intervention arm while suboptimal dosing of the treatment arm may result in a false negative conclusion. Kollef et al conducted a noninferiority (NI) trial to compare a 7-day doripenem infusion to an imipenem-cilastatin infusion for patients with ventilator-associated pneumonia (VAP). 4 NI was not established as the study was terminated early after randomizing only 274 patients due to higher rates of clinical failure and mortality in the doripenem compared to the imipenem arm. It is most likely that the failure of doripenem to show NI to imipenem was due to a lack of an advised loading dose 5 , 6 when administering doripenem as a 4-hour extended infusion strategy whereas imipenem was administered using the shorter 1-hour standard infusion that does not require a loading dose. Based on this study, the FDA unfortunately changed the doripenem label in January 2012 warning that doripenem “carries an increased risk of death and lower clinical cure rates compared to use of imipenem and cilastatin.” 7 It is now known that 7 days of therapy is sufficient for most patients with VAP as recommended by the 2016 IDSA guideline for VAP. 8 It is more likely that the failure of doripenem to show NI to imipenem was due to a lack of advised loading dose as previously stated.
No Placebo Control
A placebo control, when appropriate, is essential to provide an accurate estimate of the treatment effect, especially when there is no established standard of care. A placebo group is also essential for establishing the safety profile of new treatments. The ION-1 trial included four arms evaluating the efficacy and safety of sofosbuvir/ledipasvir with or without ribavirin in treatment-naïve patients with hepatitis C virus genotype 1 infection. 9 A similar pattern of adverse effects was observed in all groups, with the most common adverse effects of fatigue, headache, insomnia, and nausea. While these adverse effects were attributed to sofosbuvir/ledipasvir, it is important to note that none of the four arms was a placebo. In contrast, the C-EDGE trial included two arms evaluating the efficacy and safety of grazoprevir/elbasvir compared to placebo. 10 A similar pattern of adverse effects was observed including in the placebo group, with the most common adverse effects of fatigue, headache, and nausea. It is more likely that these adverse effects are attributable to hepatitis C infection rather than the drugs. Conclusions should be developed with caution when determining the adverse effect profile of a new treatment in the absence of a placebo control.
Inappropriate Study Design (e.g., Crossover, Intention to Treat/Per Protocol)
In a crossover or repeated measures study design, subjects serve as their own control. Patients receive a study treatment, experience a period with no drug treatment or placebo (i.e., washout period) to prevent a carryover effect from one arm to the next, then receive a different therapy. Chronic diseases, such as mild to moderate hypertension would be appropriate to use a crossover design if an adequate washout period (estimated to be four to five half-lives of a medication) is utilized between different drug administration. Vinson et al conducted a crossover study to determine the efficacy of a green coffee bean extract to placebo as a weight loss agent. 11 Since weight should not be expected to return to baseline during a washout period, a crossover design would not be appropriate for this study and would confound the results. In addition, the authors’ blinding methods were questionable, as one of the arms received the treatment twice a day while the other two arms received their medication three times a day, and it was unclear whether the placebo was a true placebo (i.e., color, taste, appearance, smell, texture, shape, size, weight, packaging).
Trial Stopped Early
Occasionally, it is necessary to terminate a trial early if a group is unlikely to benefit from treatment or if patients are likely to be harmed with study continuation. During the course of a study, treatment effects are subject to highs and lows that confound the true treatment effect. 12 If a large treatment effect occurs early in the trial and as a result the study is stopped, the effect size will be highly exaggerated and deviate from the true effect size. The MERINO trial was such an NI trial. It compared piperacillin/tazobactam to meropenem for definitive treatment of bacteremia caused by ceftriaxone-resistant E. coli or K. pneumoniae . 13 The rate of 30-day mortality was 12.3% in the piperacillin/tazobactam group and 3.7% in the meropenem group which failed to show NI. The study was terminated early after an interim review since it was determined that NI was unlikely to be demonstrated. A subsequent systematic review determined that the rate of mortality was 15.2% with definitive carbapenem treatment and 16.2% with definitive beta-lactam/beta-lactamase inhibitors. 14 It is likely that early termination of the MERINO trial resulted in unexpectedly low mortality rates in the meropenem group, and hence exaggerating the treatment effect and potentially truncating secondary and safety outcomes.
Study Limitations That Affect Results
Absence of inferential statistics for comparison of arms (only descriptive statistics used).
Inferential statistics are crucial in clinical trials to provide a quantitative method to reject or accept the null hypothesis using P -values. This provides proof (or absence) of causation rather than association of the treatment effect when guarding against false positives or negatives. In the absence of inferential statistics and a direct biological association, concluding causation is inappropriate. The ION-2 trial evaluated the efficacy of sofosbuvir/ledipasvir with or without ribavirin for either 12 or 24 weeks (four possible combinations) in patients with hepatitis C virus genotype 1 infection who had failed prior treatment. 15 While the virologic response rate in each of the four arms was shown to be superior to the adjusted historical 25% response (primary outcome), the arms were not compared to each other. For patients with cirrhosis specifically, the response rate was reported to be 86% in the 12-week arm and 100% in the 24-week arm. While there were 440 patients in the study, only 20% (about 88 patients) had cirrhosis. The difference between the two arms among cirrhotic patients was found to be statistically significant ( P = .007) even though the study was not designed to compare the arms to each other. Consequently, the 2015 AASLD guidelines, based only on this study, recommended sofosbuvir/ledipasvir for 24 weeks for treatment-experienced cirrhotic patients with HCV genotype 1. 16 Further studies, designed to directly compare 12 weeks to 24 weeks of treatment, are needed to support AASLD’s recommendation.
Lack of Power or Not Reported Especially When Primary Outcome is Not Significant
When a study is underpowered and the results are not statistically significant, a follow-up study is typically needed with a larger sample size, longer duration of study, or both, to rule out a false negative. It is not uncommon to have scenarios in which it will not be feasible to have statistical power in a study when the number of events are rare or the disease is rare. A trial assigned immunocompromised patients with invasive aspergillosis (IA) to receive voriconazole with either andiulafungin (combination therapy; n = 135) or placebo (monotherapy; n = 142). 17 The study required 250 patients in the combination group to have 70% power to show an absolute reduction of 11.4% in all-cause mortality. After nearly 3 years of enrollment from 93 sites in 24 countries, 277 patients with probable or proven IA were included in the study. The rate of all-cause mortality at 6 weeks was 19.6% for combination therapy and 27.5% for monotherapy ( P = .087). The power of the study was reduced due to the higher rate of mortality in the monotherapy group than the anticipated 19% rate. Therefore, the results are likely due to a false negative. While further studies would be necessary to confirm the mortality benefit with combination therapy, the rarity of this disease makes it impractical. Though the trend in reduced mortality with combination therapy is not statistically significant, the results are considered clinically relevant and were adopted into the 2016 IDSA guideline recommendations for combination therapy in certain patients (especially those with hematologic malignancy and persistent neutropenia) with documented IA. 16
Secondary Outcomes Show Positive Findings and Conclusions are Drawn
The primary outcome should be specified prior to study commencement, and any secondary outcomes can indicate potential associations that can be explored in future research or support the primary outcome. Conclusions should not be drawn from secondary outcomes as they are generally considered only hypothesis generating. In addition, study designs are not centered around nor powered to assess secondary outcomes.
The pivotal trials that provided evidence for FDA approval of fluoxetine demonstrated that a secondary outcome of weight loss was significantly higher in the fluoxetine group compared to tricyclic antidepressants (TCAs). 18 - 20 This was considered a major advantage for fluoxetine as TCAs were known to cause weight gain. Some physicians in the US started prescribing fluoxetine for weight loss in patients without depression. The design of a study to examine weight loss versus depression would look very different such as the type of patients included (depression vs obese), or excluded (depression or patients taking an antidepressant would probably be an exclusion in obesity trials), and the length of the trial in depression would be shorter, weeks compared with months to years in obesity trials. The primary outcome in a depression trial would include a rating scale such as the Hamilton Depression Rating Scale (HAMD) whereas a trial for weight loss would evaluate body mass index (BMI), weight, and/or percent body fat. When trials were designed utilizing fluoxetine for weight loss as the primary outcome, fluoxetine was found to initially cause weight loss, but caused weight gain by the end of the trials. 21 - 23 Premature adaptation of a secondary outcome applied to an unrelated condition can result in inappropriate treatments and distrust of the medical field when intended results do not come to fruition as expected. Refer to the fluoxetine and weight loss example if in the future there is a temptation to make conclusions regarding secondary outcomes. 2
Limitations That Reduce External Validity
Inclusion/exclusion criteria that are too restrictive or vague.
Inclusion criteria are used to ensure patients in the study have the target disease being studied, and that all enrolled subjects have similar demographic and clinical characteristics. Each clinical trial should provide a complete and accurate list of entry and exclusion criteria, as this defines the study sample. These criteria help clinicians identify patients for whom the study results do not necessarily apply and for whom applying the treatment recommended could cause harm.
The SPRINT trial studied intensive (systolic blood pressure, SBP < 120 mm Hg) versus standard blood pressure control (SBP < 140 mm Hg). 24 The key exclusion criteria were patients < 50 years of age with diabetes and/or history of stroke. It was estimated that due to the inclusion and extensive exclusion criteria that the results applied to approximately 20% of patients with hypertension. 25 In the discussion section of the SPRINT trial, it was noted that only approximately 50% of patients with hypertension obtain the 140/90 mm Hg goal, 24 but it is unclear if the 20% estimate includes this information, so extrapolation could be even more limited.
Shortly after the SPRINT trial was released, Medscape posted a Fast Five Quiz entitled: How Much Do You Know About Hypertension? 26 The last question asked:
“According to the results of the Systolic Blood Pressure Intervention Trial (SPRINT) study, which of the following results in better cardiovascular outcomes?
- BP treatment initiation and goals are 150/100 mm Hg in patients younger than 60 years with diabetes.
- In non-black hypertensive patients aged 18 years or older, initiate treatment with a combination of ACE inhibitor and angiotensin receptor blocker.
- Initiation of therapy in all patients to lower BP < 120/80 mm Hg.
- In non-black hypertensive patients, thiazide-type diuretics alone are the only indicated treatment.” 26
Answer 1 and 2 are not correct since patients < 50 years of age were excluded. Answer 3 is not correct since there were many exclusions so the results would not apply to all patients. Answer 4 is not correct as the study did not examine specific treatment options. The correct answer listed in Medscape was answer 3 (59% of respondents chose this answer). Medscape stated: “According to the SPRINT findings, achieving a target systolic pressure of 120 mm Hg reduced cardiovascular events (e.g., myocardial infarction, heart failure) and stroke by nearly one-third and reduced risk for death by almost one-fourth when compared with a target of 140 mm Hg.” 26 It is important to utilize both the inclusion and exclusion criteria to ensure patient safety when extrapolating results to clinical practice.
Primary Outcome Not Appropriate, the Preferred Measure or Accurately Defined
The primary outcome needs to be clearly defined and appropriate for the disease state to be able to successfully answer the study objective, as well as for the reader to be able to compare the results to other studies and to extrapolate the results to clinical practice.
The 2013 REDUCE trial was a NI study that compared short-term (5 day) steroid treatment to traditional (14 day) for management of COPD in 134 patients admitted to the emergency department. The primary endpoint was time to exacerbation within 6 months. The investigators determined that NI was met for the primary outcome. 27 The 2014 GOLD (Global Initiative for Chronic Obstructive Lung Disease) guidelines included only this study in their recommendation to use 5 day instead of the traditional 14 day steroid (prednisone 40 mg) treatment although it was listed as Evidence B (“Source of evidence: randomized controlled trials (RCTs). Limited body of evidence. Definition: Evidence is from endpoints of intervention studies that include only a limited number of patients, post-hoc or subgroup analysis of RCTs, or meta-analysis of RCTs. In general, Category B pertains when few randomized trials exist, they are small in size, they are undertaken in a population of the recommendation, or the results are somewhat inconsistent.”) 28 Two major flaws in the study were that the primary outcome was determined using a nonpreferred measure and the study duration was inadequate. A shortened trial duration might truncate evidence for the occurrence of both the primary and secondary outcomes while the short duration might exaggerate the safety profile. The GOLD 2014 guidelines recommended that a patient’s risk of future exacerbations should be based on the rate of exacerbations as the preferred choice of the primary outcome, not the time to the next exacerbation, which was used in the Leuppi, et al study. In addition, the 2014 GOLD guidelines state that the risk of exacerbation is based on the number of exacerbations in the last 12 months and the Leuppi et al study was only 6 months in duration. 27 , 28 These oversights could lead to a conclusion that it was noninferior to time to exacerbation but after the first relapse could lead to even more exacerbations. It is important to verify study information in guidelines to determine the quality of information, especially when only one trial is used to change standard practice.
Use of Surrogate Outcome Measures When Not Proven to be Tied to Clinical Outcomes or Clinical Outcomes Are the Standard
A surrogate outcome is a measure that is thought to correlate with or be suggestive of a clinical outcome (e.g., elevated cholesterol levels might be a surrogate measure of atherosclerotic vascular disease); however, a correlation does not mean a true causational relationship exists between the two. Surrogate outcome measures are often used when the clinical endpoint occurs in small numbers of patients or requires longer periods of time to determine the outcome (e.g., adverse events or mortality).
Two initial studies evaluated various dosing regimens of enoxaparin among overweight patients requiring venous thromboembolism prophylaxis utilizing the surrogate primary outcome of anti-factor Xa levels rather than the standard clinical outcomes of incident of VTE, bleeding, and/or death. 29 , 30 In both studies, the authors concluded that 0.5 mg/kg/day was not associated with bleeding or thrombosis. However, the studies had small sample sizes, no comparator groups, and did not evaluate clinical outcomes so it is uncertain whether the surrogate marker of anti-Xa levels translates accordingly. A larger, more recent trial compared two fixed doses of enoxaparin: 40 mg daily (standard) and 60 mg daily and found consistent results with 31% versus 69% of patients achieving target anti-Xa levels (defined as 0.32 to 0.54 units/mL) for the 40 mg and 60 mg groups, respectively ( P = .007). Similarly, it was concluded that the 60 mg dose was superior without more bleeding. 31 Not only is there variability in what target anti-Xa levels should be for enoxaparin thromboprophylaxis, there is no strong evidence to support that low levels are associated with thrombosis or high levels are associated with bleeding. Although all three of these studies recorded the incidence of bleeding events and venous thromboembolism, there were zero thrombosis events and there was only a total of one bleeding event across all three studies. Given the lack of power to evaluate these clinical outcomes, conclusions that any of these studied regimens are not associated with adverse clinical events should be made with caution. Adequately powered studies focused on the clinical outcomes of bleeding and thrombosis are needed before the decision regarding whether or not anti-Xa levels are representative of bleeding and thrombosis can be made.
Number Needed to Treat/Harm Not Clinically Relevant
Number needed to treat (NNT) or number needed to harm (NNH) are calculated from confidence intervals (CIs) to determine clinical relevance of study results. 2 In most cases, NNT should be a low number whereas NNH should be a high number. A statement containing key components should be developed to obtain a complete picture of clinical relevance.
In the IMPROVE-IT study, ezetimibe 10 mg or placebo was given to patients with acute coronary syndrome receiving simvastatin 40 mg to examine the composite risk of death, major CV events and non-fatal stroke. The 7-year composite endpoint was 32.7% in the combination group versus 34.7% in the simvastatin only group, HR 0.94 (95% CI 0.89 to 0.98; P = .016). The authors concluded that ezetimibe added to simvastatin significantly lowered the risk of cardiovascular events more than simvastatin alone. 32 The authors only provided the absolute risk difference (2%) and not an NNT which was calculated to be 50. The most important component of an NNT is time. It is a very different matter for a treatment to take, for example 2 versus 7 years to reduce the number of events in 50 patients by one. The NNT statement in the IMPROVE-IT trial 32 is: 50 patients need to be treated with combination simvastatin 40 mg plus ezetimibe 10 mg for 7 years to prevent one additional composite endpoint of CV death, major coronary events or non-fatal stroke compared to treatment with simvastatin 40 mg. The results in the trial were shown to be statistically significant, but when considering the NNT, they did not show clinical relevance. When analyzing a clinical trial, a practitioner should analyze the results and, when appropriate, show why a particular recommendation supported in print should not be adopted. This conclusion of a lack of clinical relevance was validated when the FDA did not approve this new indication for ezetimibe in combination with simvastatin for a reduction in CV events based on this study. 33
After examining the clinical trial excerpts in this article, it is evident how superficial scanning of studies might lead to adopting unproven therapies and claims and could potentially lead to erroneous assumptions. Possible outcomes from using unproven therapies could range from unnecessary patient and healthcare costs to crippling, avoidable morbidity, and/or mortality. It is important to realize that many studies, whether intentional or not, contain biases in the study designs that could influence the authors’ stated conclusions. It is imperative that pharmacists be able to identify major study limitations and how those limitations could affect extrapolation of results to patient care.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.

Scientific Research and Methodology : An introduction to quantitative research and statistics
9 research design limitations.
So far, you have learnt to ask a RQ and designs studies. In this chapter , you will learn to identify:
- limitations to internally valid.
- limitations to externally valid.
- limitations to ecologically valid.

9.1 Introduction
The type of study and the research design determine how the results of the study should be interpreted. Ideally, a study would be perfectly externally and internally valid; in practice this is very difficult to achieve. Practically every study has limitations. The results of a study should be interpreted in light of these limitations. Limitations are not necessarily problems .
Limitations generally can be discussed through three components:
- Internal validity (Sect. 6.1 ): Discuss any limitations to internal validity due to the research design (such as identifying possible confounding variables). This is related to the effectiveness of the study within the sample (Sect. 9.2 ).
- External validity (Sect. 5.1 ): Discuss how well the sample represents the intended population. This is related to the generalisability of the study to the intended population (Sect. 9.3 ).
- Ecological validity : Discuss how well the study methods, materials and context approximate the real situation being studied. This is related to the practicality of the results to real life (Sect. 9.4 ).
Some of these limitations are imposed by the type of study. All these issues should be addressed when considering the study limitations.
Almost every study has limitations. Identifying potential limitations, and discussing the likely impact they have on the interpretation of the study results, is important and ethical.
Example 9.1 Delarue et al. ( 2019 ) discuss studies where subjects rate the taste of new food products. They note that taste-testing studies should (p. 78):
... allow generalizing the conclusions obtained with a consumer sample [...] to the general targeted population [i.e., external validity]... tests should be reliable in terms of accuracy and replicability [i.e., internal validity].
However, even with good internal and external validity, these studies often result in a 'high rate of failures of new launched products'. That is, the studies do not replicate the real world, and so lack ecological validity .
9.2 Limitations: internal validity
Internal validity refers to the extent to which a cause-and-effect relationship can be established in a study, eliminating other possible explanations (Sect. 6.1 ). A discussion of the limitations of internal validity should cover, as appropriate: possible confounding variables; the impact of the Hawthorne, observer, placebo and carry-over effects; the impact of any other design decisions.
If any of these issues are likely to compromise internal validity, the implications on the interpretation of the results should be discussed. For example, if the participants were not blinded, this should be clearly stated, and the conclusion should indicate that the individuals in the study may have behaved differently than usual.
Example 9.2 (Study limitations) Axmann et al. ( 2020 ) randomly allocated Ugandan farmers to receive, or not receive, hybrid maize seeds. One potential threat to internal validity was that farmers receiving the hybrid seeds could share their seeds with their neighbours.
Hence, the researchers contacted the \(75\) farmers allocated to receive the hybrid seeds; none of the contacted farmers reported selling or giving seeds to other farmers. This extra step increased the internal validity of the study.
Maximizing internal validity in observational studies is more difficult than in experimental studies (e.g., random allocation is not possible). The internal validity of experimental studies involving people is often compromised because people must be informed that they are participating in a study.

Example 9.3 (Internal validity) In a study of the hand-hygiene practices of paramedics ( Barr et al. 2017 ) , self -reported hand-hygiene practices were very different than what was reported by peers . That is, how people self-report their behaviours may not align with how they actually behave, which influenced the internal validity of the study.
A study evaluated using a new therapy on elderly men, and listed some limitations of their study:
... the researcher was not blinded and had prior knowledge of the research aims, disease status, and intervention. As such, these could all have influenced data recording [...] The potential of reporting bias and observer bias could be reduced by implementing blinding in future studies. --- Kabata-Piżuch et al. ( 2021 ) , p. 10
9.3 Limitations: external validity
External validity refers to the ability to generalise the findings made from the sample to the entire intended population (Sect. 5.1 ). For a study to be externally valid, it must first be internally valid: if the study of not effective in the sample studied (i.e., internally valid), the results may not apply to the intended population either.
External validity refers to how well the sample is likely to represent the intended population in the RQ.
If the population is Iowans, then the study is externally valid if the sample is representative of Iowans The results do not have to apply to people in the rest of the United States (though this can be commented on, too). The intended population is Iowans .
External validity depends on how the sample was obtained. Results from random samples (Sects. 5.5 to 5.9 ) are likely to generalise to the population and be externally valid. (The analyses in this book assume all samples are simple random samples .) Furthermore, results from approximately representative samples (Sect. 5.10 ) may generalise to the population and be externally valid if those in the study are not obviously different than those not in the study.
Example 9.4 (External validity) A New Zealand study ( Gammon et al. 2012 ) identified (for well-documented reasons) a population of interest: 'women of South Asian origin living in New Zealand' (p. 21). The women in the sample were 'women of South Asian origin [...] recruited using a convenience sample method throughout Auckland' (p. 21).
The results may not generalise to the intended population ( all women of South Asian origin living in New Zealand) because all the women in the sample came from Auckland, and the sample was not a random sample from this population anyway. The study was still useful however!
Example 9.5 (Using biochar) Farrar et al. ( 2018 ) studied growing ginger using biochar on one farm at Mt Mellum, Australia. The results may only generalise to growing ginger at Mt Mellum, but since ginger is usually grown in similar types of climates and soils, the results may apply to other ginger farms also.
9.4 Limitations: ecological validity
The likely practicality of the study results in the real world should also be discussed. This is called ecological validity .
Definition 9.1 (Ecological validity) A study is ecologically valid if the study methods, materials and context closely approximate the real situation of interest.
Studies don't need to be ecologically valid to be useful; much can be learnt under special conditions, as long as the potential limitations are understood when applying the results to the real world. The ecological validity of experimental studies may be compromised because the experimental conditions are sometimes artificially controlled (for good reason).

Example 9.6 (Ecological validity) Consider a study to determine the proportion of people that buy coffee in a reusable cup. People could be asked about their behaviour. This study may not be ecologically valid, as how people act may not align with how they say they will act.
An alternative study could watch people buy coffees at various coffee shops, and record what people do in practice. This second study is more likely to be ecologically valid , as real-world behaviour is observed.
A study observed the effect of using high-mounted rear brake lights ( Kahane and Hertz 1998 ) , which are now commonplace. The American study showed that such lights reduced rear-end collisions by about \(50\) %. However, after making these lights mandatory, rear-end collisions reduced by only \(5\) %. Why?
9.5 Limitations: study types
Experimental studies, in general, have higher internal validity than observational studies, since more of the research design in under the control of the researchers; for example, random allocation of treatments is possible to minimise confounding.
Only well-conducted experimental studies can show cause-and-effect relationships.
However, experimental studies may suffer from poor ecological validity; for instance, laboratory experiments are often conducted under controlled temperature and humidity. Many experiments also require that people be told about being in a study (due to ethics), and so internal validity may be comprised (the Hawthorne effect).
Example 9.7 (Retrofitting) giandomenico2022systematic studied retro-fitting houses with energy-saving devices, and found large discrepancies in savings for observational studies ( \(12.2\) %) and experimental studies ( \(6.2\) %). The authors say that 'this finding reinforces the importance of using study designs with high internal validity to evaluate program savings' (p. 692).
9.6 Chapter summary
The limitations in a study need to be identified, and may be related to:
- internal validity (effectiveness): how well the study is conducted within the sample, isolating the relationship of interest.
- external validity (generalisability): how well the sample results are likely to apply to the intended population.
- ecological validity (practicality): how well the results may apply to the real-world situation.
Many of the limitations are a results of the type of study.
9.7 Quick review questions
Are the following statements true or false ?
- When interpreting the results of a study, the steps taken to maximize internal validity should be evaluated TRUE FALSE
- If studies are not externally valid, then they are not useful. TRUE FALSE
- When interpreting the results of a study, the steps taken to maximize external validity do not need to be evaluated TRUE FALSE
- When interpreting the results of a study, ecological validity is about the impact of the study on the environment. TRUE FALSE
9.8 Exercises
Answers to odd-numbered exercises are available in App. E .
Exercise 9.1 A research study examined how people can save energy through lighting choices ( Gentile 2022 ) . The study states (p. 9) that the results 'are limited to the specific study and cannot be easily projected to other similar settings'.
What type of validity is being discussed here?
Exercise 9.2 Fill the blanks with the correct word: internal , external or ecological .
When interpreting the results of studies, we consider the practicality ( internal external ecological validity), the generalizability ( internal external ecological validity) and the effectiveness ( internal external ecological validity).
Exercise 9.3 A student project asked if 'the percentage of word retention higher in male students than female students?' When discussing external validity , the students stated:
We cannot say whether or not the general public have better or worse word retention compared to the students that we will be studying.
Why is the statement not relevant in a discussion of external validity?
Exercise 9.4 Yeh et al. ( 2018 ) conducted an experimental study to 'determine if using a parachute prevents death or major traumatic injury when jumping from an aircraft'.
The researchers randomised \(23\) volunteers into one of two groups: wearing a parachute, or wearing an empty backpack. The response variable was a measurement of death or major traumatic injury upon landing. From the study, death or major injury was the same in both groups (0% for each group). However, the study used 'small stationary aircraft on the ground, suggesting cautious extrapolation to high altitude jumps' (p. 1).
Comment on the internal, external and ecological validity.
Exercise 9.5 A study examined how well hospital patients sleep at night ( Delaney et al. 2018 ) . The researchers state that 'convenience sampling was used to recruit patients' (p. 2). Later, the researchers state (p. 7):
... while most healthy individuals sleep primarily or exclusively at night, it is important to consider that patients requiring hospitalization will likely require some daytime nap periods. This study looks at sleep only in the night-time period \(22\) : \(00\) -- \(07\) : \(00\) h, without the context of daytime sleep considered.
Discuss these issues using the language introduced in this chapter.
Exercise 9.6 Botelho et al. ( 2019 ) examined the food choices made when subjects were asked to shop for ingredients to make a last-minute meal. Half were told to prepare a 'healthy meal', and the other half told just to prepare a 'meal'. The authors stated (p. 436):
Another limitation is that results report findings from a simulated purchase. As participants did not have to pay for their selection, actual choices could be different. Participants may also have not behaved in their usual manner since they were taking part in a research study, a situation known as the Hawthorne effect.
What type of limitation is being discussed?
Exercise 9.7 Johnson et al. ( 2018 ) studied the use of over-the-counter menthol cough-drops in people with a cough. One conclusion from the observational study of \(548\) people was that, taking 'too many cough drops [...] may actually make coughs more severe', as one author explained in an interview about the study Critique this statement.
Research Limitations – Why Study Results Don’t Always Apply to You
Written by : Adam Tzur Last updated : 25.07.2022
Steve Hall of Revive Stronger has interviewed Adam about research limitations. Watch the video or read the article to learn more about exercise science.
The interview covers the following topics:
00:00 Philosophy of science 04:08 Study vs. anecdotes 05:51 Survivorship bias 11:52 Length of studies as a limitation 16:57 Number of participants and statistical power 19:33 Demographic 23:22 Adherence of participants 26:53 Having a coach? 29:02 Measuring tools 33:33 Funding bias 37:53 Personal biases 47:13 Core principles of science 49:22 Animal studies

Summary of Research Limitations
Contents →
Genetics as well as our life situation affects how well we adapt to a training program. Some people are low-responders (slow gains), others are high-responders (fast gains).
Many fitness and nutrition studies are short (i.e. 8 weeks). Results from an 8 week study do not necessarily apply to longer periods of time, like a year.
Representativeness
Most strength studies recruit untrained male university students in their early 20s. This limits representativeness , because study results apply to the population in the study.
Specificity
Many studies use programs that involve a single muscle group being trained (isolation training). The results then apply only to that muscle group.
Participants in training studies are often under direct supervision of study coaches when they train. This affects adherence (how likely they are to show up).
Body composition measurements
Machines like DEXA or BIA have inherent error margins. Results are affected by water retention, carbohydrate intake, muscle glycogen, supplements, and more.
Dark side of science
Some researchers miscite (misquote) other studies, or use animal studies to make claims about what works for humans. Sometimes, peer review is faked, or funding bias affects the results.
How to interpret scientific literature
We should have high standards and base our conclusions on the preponderance of the evidence from systematic reviews and meta-analyses.
The article continues below

The Science of Detraining: How Long You Can Take a Break from the Gym Before You Lose Muscle Mass & Strength
Scientific recommendations for strength and hypertrophy training from 150+ studies, gaining muscle mass in a deficit vs. bulking (research review), overview of research limitations in fitness science, genetics and individual variability.
Does everyone respond the same way to the same training program?
If we look at the figure below; the change in CSA (hypertrophy) after 12 weeks of strength training seems clear.
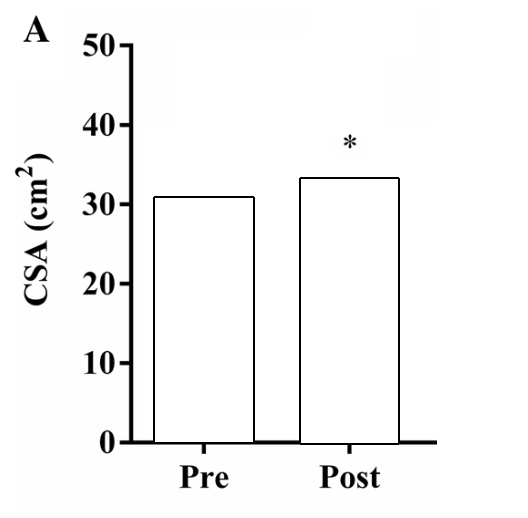
Figure by Angleri et al. ( 2017 ) (edited for clarity).
Should we assume from this that everyone who does strength training for 12 weeks will increase their CSA by ~3-4cm 2 ? It seems like a straightforward conclusion no? Not so fast!

Once we bring in inter-individual variability, we see that the answer is much more complicated. Some individuals barely improve while others improve at a much faster pace:

There’s even something called a non-responder . Below is an example from a 9 month strength training study (8 out of 83 beginners maintained or lost LBM). We could argue the participants who didn’t gain had diseases or inadequate recovery (i.e. poor sleep), but it remains speculative:

Why is there so much variation? Why can’t we all improve at the same rate ? Some researchers believe this is due to genetics and epigenetics which are affected by lifestyle factors (i.e. diet, sleep, life stressors, pollution of the environment you live in, differences in training programs, etc.) ( Simoneau and Bouchard, 1995 ; Mead, 2007 ; Bamman et al., 2007 ; Liu et al., 2009 ; Erskine et al., 2010 ; Puthucheary et al., 2011 ; Hughes et al., 2011 ; Ahmetov et al., 2012 ; Thalacker-Mercer et al., 2013 ; Guth and Roth, 2013 ; Kim et al., 2014 ; Mann et al., 2014 ; Schutte et al., 2016 ; Zarębska et al., 2016 ; Ahtiainen et al., 2016 ; Klimentidis et al., 2016 ; Broos et al., 2016 ; Gineviciene et al., 2016 ; Heffernan et al., 2016 ). Your genetic profile interacts with the environment to create a unique phenotype ( Denham et al., 2013 ; Schlichting and Wund, 2014 ; Hoppeller, 2016 ; Schutte et al., 2016 ). Different phenotypes have different responses to training.
We usually divide people into low-responders and high-responders ( Hubal et al., 2005 ; Davidsen et al., 2011 ; Mann et al., 2014 ; Parr et al., 2016 ; Ogasawara et al., 2016 ; Bonafiglia et al., 2016 ; Buckner et al., 2017 ).
“Diet- and exercise-based weight loss interventions result in large variability in responses between individuals that is often under-reported (…) This study provides new information demonstrating that the abundance of [microRNA] are modulated with exercise and diet, and [they] are differentially expressed between high and low responders before and after a chronic weight loss intervention.” Parr et al., 2016

Furthermore, it’s possible that some people respond better to certain types of diets or training programs ( Kikuchi and Nakazato, 2015 ; Parr et al., 2016 ; Jones et al., 2016 ; Bonafiglia et al., 2016 ). For example, you might be a high-responder to low volume high intensity training, but a low-responder to high volume low intensity training. This is something we need to account for when designing training programs, and it’s very easy to misinterpret study results as something that has to apply to everyone.
“In resistance training for hypertrophy, we propose that individuals with ACTN3 RR or RX genotypes who have relatively high strength and power should choose high-load low-repetition resistance training. In contrast, individuals with the XX genotype of ACTN3 should prefer a low load with high repetitions .” Kikuchi and Nakazato, 2015
Study duration and long-term effects
A limitation with many studies, in particular periodization studies, is their short duration (most training studies are 6-12 weeks long). Generally speaking, it takes 2 months to be able to tell whether a study leads to detectable and statistically significant hypertrophy gains. Sadly, most studies in this field are very short. It’s common in the periodization literature to say no difference was found between programs, but those differences might show themselves if the program was longer. So just because a study didn’t find significant gains, doesn’t mean that wouldn’t happen in a longer study with more subjects.
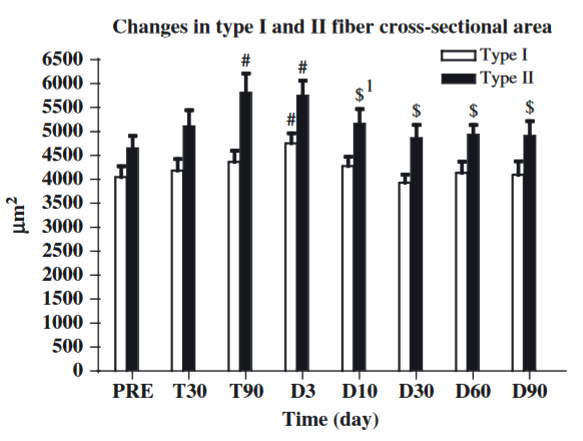
Beyond the short-term, it’s also possible that a certain program would become worse after a while. Let’s say training to failure every set is superior for 6 months. It’s possible this strategy would become less and less effective after this point in time, and that some sort of failure periodization would be necessary to continue optimal progress. We can’t tell whether this is the case with most studies today, because of their short duration.
Representativeness and convenience sampling
Many if not most fitness studies use convenience sampling to recruit participants. 20-something university student males are by far the most common participant type, though there are studies on elite athletes and older people as well. Women rarely participate. This limits representativeness. It’s possible people of different ages and genders would respond differently to the same training program or diet. For example, older people might be at greater risk of injury, hence they might want to train with lower intensities and not go to failure because failure increases injury risk. This might be a non-issue for younger lifters. There are also issues of anabolic resistance when it comes to age.
It’s important to note that there are gender differences in terms of total muscle mass and muscle distribution throughout the body. Men have more total muscle mass than women ( Abe et al., 1998 ; Janssen et al., 2000 ; Abe et al., 2003 ; Zheng et al., 2013 ; Healy et al., 2014 ). Hence, putting women and men together in the same study groups could lead to very large standard deviations in terms of total mass and strength.
“Whereas the women in the present study had 40% less muscle than men in the upper body, in the lower body gender differences in muscle mass were only 33% (…)” Janssen et al., 2000
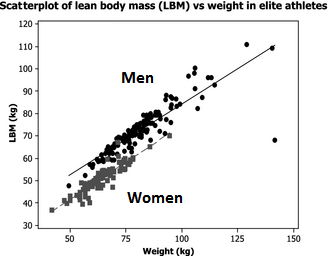
There seems to be disagreement in the literature whether the two sexes gain at the same pace or whether one sex gains faster than the other ( Ivey et al., 2000 ; Hubal et al., 2005 ; Liu et al., 2010 ; Ribeiro et al., 2015 ; Ahtiainen et al., 2016 ; Da Boit et al., 2016 ; Gentil et al., 2016 ; Mata et al., 2016 ). But the sex differences (such as differences in total LBM) do partially explain why men outperform women ( Healy et al., 2014 ).
Heterogeneity and specificity
The different methodologies, sample sizes, training programs, statistical methods, body composition measurement tools, durations, participants, etc. make the studies different from one another. This is called heterogeneity and it means that the studies are so different that it’s hard to directly compare them. Though it should be said that studies don’t need to be perfect replications of each other to compare them. But, they should have most variables be the same so that we can actually figure out which variable it is that is responsible for the change we’re looking to measure.
This also ties into how specific study results are. For example:
- Study A : 10 participants, male, untrained, 6 week duration, testing isometric strength, uses machine exercise, with protein supplement, concludes that it’s ideal to train a muscle group 5 times per week for maximal hypertrophy development.
- Study B : 30 participants, female, trained, 10 week duration, testing dynamic strength (1RM squat), no protein supplement, concludes that ideal training frequency is 3 times per week for maximal hypertrophy development.
So, which one of these is correct? What is the ideal training frequency? The answer is: neither. Like I mentioned, a study’s result is highly specific to the protocol within which it is used. So if you’re a trained female looking to improve your squat 1RM over a 10 week period, study B is much more applicable to you than study A. If you’re an untrained male looking to improve isometric strength using machines, then the results of study A apply to you.
This is something that is frequently overlooked when talking about studies, and it’s very easy to get the wrong picture if you just read the abstract. The abstract won’t always mention whether the participants are trained or not, sex is usually not mentioned either. And I’ve found that a surprising amount of studies will “hide” the fact that they only used isometric strength testing to assess strength. Isometric strength is basically when you hold a contraction without moving the limb/muscles that are under load. Isometric strength does not necessarily transfer to dynamic strength (contracting muscles through concentric and eccentric range of motion).

Another issue is that many studies will use machine exercises. And as we know, strength is highly specific to the movement, contraction type, ROM, etc. that is being performed ( Morrissey et al. 1995 ; Beardsley, 2015 ; Pritchard et al., 2016 ; Rhea et al., 2016 ) (we have an article on this in the works, will be published in a couple of weeks). So if a study concludes that a certain type of training is ideal for machine exercises, it doesn’t automatically mean this applies to a person doing barbell movements or free-weight exercise.
Though it’s surprising how many studies will try to generalize specific results into something that becomes speculative.
Ecological validity
Ecological validity means the study mimics real life. Some studies will only test two exercises versus each other. And the subjects will do no other exercises during the study. Let’s say you want to see what’s best: barbell bench press or dumbbell bench press? Group A only does barbell BP while group B only does dumbbell BP. The study finds that the barbell BP was superior for building muscle and strength. The problem here is that this effect may not exist in a normal training program. If subjects do a bench press plus other chest exercises, the effect of barbell vs. dumbbell could be negligible.
This type of reductionism is necessary in science but it might not apply to people in real life.
Hence, if you want to compare two exercises in an ecologically valid study, you should do it in the context of a complete training program.
Here’s an example of a study that aims for ecological validity:
- Effects of a Modified German Volume Training Program on Muscular Hypertrophy and Strength ( Amirthalingam et al., 2016 )
Adherence to training and gains
Training adherence (how closely you stick to a training program) is an important factor. It generally determines how well your strength and gains improve over time. This is also common sense, since skipping practice isn’t generally considered the best way to make progress. Though there are exceptions (i.e. overtraining, and complete beginners).
Training that is supervised by coaches could lead to greater gains compared to training by yourself, because subjects in studies might adhere more closely to the program and exert more effort ( Mazzetti et al., 2000 ; Coutts et al., 2004 ; Gentil and Bottaro, 2010 ; Amagliani et al., 2010 ).
It’s possible normal people would not push themselves as hard when they’re training alone and they might be more liable to skip workouts. Low training attendance might lead to slower gains ( Gentil and Bottaro, 2013 ). Though it depends on which group of people we look at. Complete beginners could take long training breaks and still rival the gains made by beginners who train continually ( Häkkinen et al., 2000 ; Ogasawara et al., 2011 ; Ogasawara et al., 2013 ):
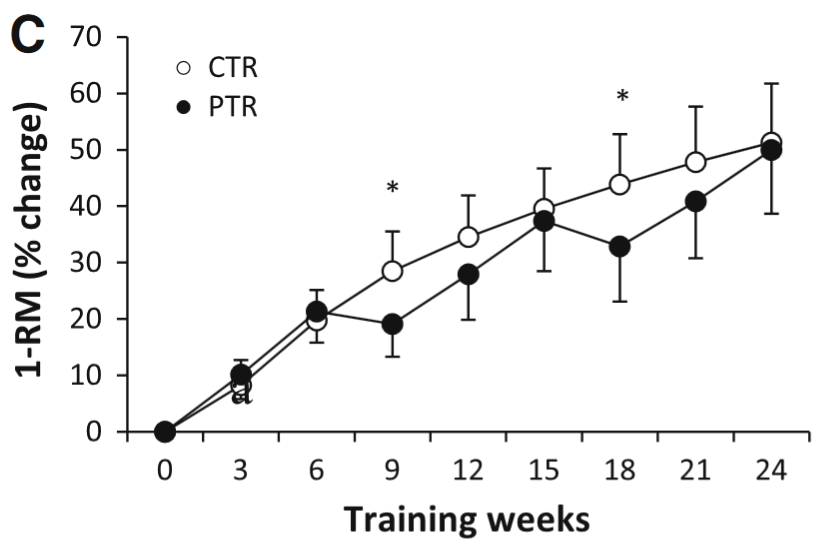
The figure shows how 1RM changes over the course of 24 weeks of training. The black lines (PTR group) trained for 6 weeks, then took a break for 3 weeks (rinse and repeat). The white line (CTR group) trained continuously. By the end there was little difference in maximum strength between groups. Figure by Ogasawara et al. ( 2013 ).

The figure shows how CSA [hypertrophy] changes over the course of 24 weeks of training. The black lines (PTR group) trained for 6 weeks, then took a break for 3 weeks (rinse and repeat). The white line (CTR group) trained continuously. By the end there was little change in gains. Note that the CTR group did a lot more volume because they never took a break: “the PTR group had 25 % fewer training sessions”. Figure by Ogasawara et al., 2013 .
Hence beginners might not need perfect adherence to training. Though we can speculate that adherence is more important for trained lifters or for beginners who are doing whole-body programs (participants in the Ogasawara study didn’t do a whole body program).
Funding bias
Does funding imply bias? Should a study be discarded on the basis of funding alone? I will argue both sides of the issue:
Why funding doesn ’t affect the results of a study
- Methods section is more important: How rigorous was the study?
- Many journals require Conflict of Interest (COI) to be disclosed
- A researcher risks his entire career by forging data/lying so that a study conforms to the expectations of the funder. If it is later discovered that he or she forged data, they might lose their job and reputation.
- Many studies have multiple funding sources, including state grants and self-funding by large universities. Multiple funders reduce the chance that a single funder “decides” the outcome.
- Several journals report that the funders had no hand in the design of the study or in the presentation of the results.
- Several of the most important and influential nutrition researchers are partially funded by the industry. Would people suggest that for example, Stuart Phillips, a highly regarded protein researcher, is corrupt because of prior funding? That’s quite a claim.
Why funding does affect the results of a study
- Conflicts of interest/funding are omitted from quite a few studies/books ( Roseman et al., 2011 ; Piper et al., 2015 ; Rasmussen et al., 2015 ; Resnik et al., 2017 )
- Several reviews suggest that funding bias might influence study results ( Lexchin et al., 2003 ; Huss et al., 2007 ; Lundh et al., 2012 ; Flacco et al., 2015 ; Shnier et al., 2016 ; Schillinger et al., 2016 ; Chartres et al., 2016 ). Though some disagree ( Mugambi et al., 2013 ). It might depend on which industry and field we are discussing (some fields might be inherently more at risk for funding bias). It seems like pharmacology is such a field.
- There are studies that are undertaken on behalf of a company that specifically produces, markets, and sells the product that is being tested. A dead giveaway is that the study has 0 citations even if it’s several years old. Perhaps it is only cited by the same authors. Examples: Oben et al. ( 2008 ) followed by Anderson ( 2013 )
“In conclusion, an appreciable portion of the content in pharmacology textbooks is open to the influence of undisclosed potential financial conflicts of interest. These resources are frequently consulted by many practicing physicians as well as other allied health professionals and are also integral to their education.” Piper et al., 2015
“In 75.0 % of guidelines at least one author, and in 21.4 % of guidelines all authors, disclosed FCOI with drug companies. In 54.0 % of guidelines at least one author, and in 28.6 % of guidelines over half of the authors, disclosed FCOI with manufacturers of drugs that they recommended” ( Shnier et al., 2016
Other considerations
- Most studies are industry funded, in some industries ( Flacco et al., 2015 ; Shnier et al., 2016 ). Though it depends on which industry we’re talking about
In conclusion, funding is something to look out for, but it isn’t the end-all-be-all of whether we should reject a study ( Resnik and Elliott, 2013 ). It’s equally important to identify: methodological quality, citations, journal, researcher background, what other studies conclude, etc. Furthermore, claiming that someone is biased is an assumption, and assumptions should be justified. If we can’t justify the answer beyond “all industry funded studies are biased” then we are on thin ice.
However, if a study exhibits several red flags like poor/biased methodology, unknown researchers, single funding by a company that produces/sells the product being tested, unknown journal, no citations, “extreme” results, then we can make a bias claim with much more certainty.
“Although it is widely acknowledged that financial interests can threaten the integrity of science, it is important to realize that having an economic stake in the outcome of a study does not automatically invalidate or taint one’s research . Most researchers with financial interests related to their work conduct good research, and most sponsors and institutions do not manipulate study design, execution, management, or oversight to promote their financial interests.” Resnik, 2014
“At least five factors can be examined to determine whether financial relationships are likely to enhance, undermine, or have no impact on the credibility of research. These include as follows: whether sponsors, institutions, or researchers have a significant financial stake in the outcome of a study; whether the financial interests of the sponsors, institutions, or researchers coincide with the goal of conducting research that is objective and reliable; whether the sponsor, institution, or researchers have a history of biasing research in order to promote their financial goals; how easy it is to manipulate the research in order to achieve financial goals; and whether oversight mechanisms are in place which are designed to minimize bias. Since these factors vary from case to case, evaluating the impact of financial relationships depends on the circumstances” Resnik and Elliott, 2013
Body composition measurement
Glycogen and gains: a confounder in beginner studies.
This section is taken from our article on detraining .
The body composition measurement tools mentioned above are useful, but they are also affected by how much glycogen we store in our muscles. So when muscle glycogen stores shrink during detraining, we “lose” muscle mass, or more accurately, the water contents of our muscles decreases ( Nygren et al., 2001 ).
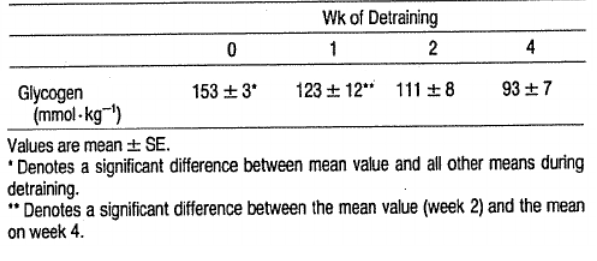
Glycogen depletion following 4 weeks of detraining in competitive swimmers ( Costill et al., 1985 )
When beginners start exercising, their muscle glycogen stores will grow quickly and they will retain more water, as shown below:
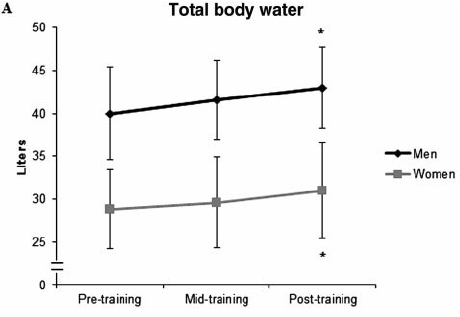
What 16 weeks of strength training does for total body water in beginners. Figure by Ribero et al., 2014
If researchers were to measure gains after a couple weeks of training, it could simply be increased muscle glycogen. On the other hand, if researchers are using tools that can detect water changes within our bodies, then they can measure “real” gains much better ( LaForgia et al., 1999 ; Mallinson et al., 2011 ). Indeed, a study found that endurance athletes lost muscle mass during a 3-week detraining period ( LaForgia et al., 1999 ). However, the muscle mass loss was only found using measurement tools that weren’t ideal for the job (2 and 3 compartment models). Check out a comparison of the models below:

Figure by Mallinson et al., 2011
Luckily, the same researchers also measured water mass using a 4 compartment model. They found that the 0.7 kg loss of lean mass was actually a loss of 0.7 kg total body water. Hence, the detrained athletes didn’t lose any muscle mass during a three week break from training ( LaForgia et al., 1999 ). But, their muscle glycogen stores did shrink.
This is why we have to take the atrophy and hypertrophy studies with a grain of salt.
However, let’s assume that 2-3 weeks detraining in beginners leads to muscle loss. Does it matter in the long-term? Studies by Ogasawara et al., 2011 and Ogasawara et al., 2013 suggest that it makes little difference:
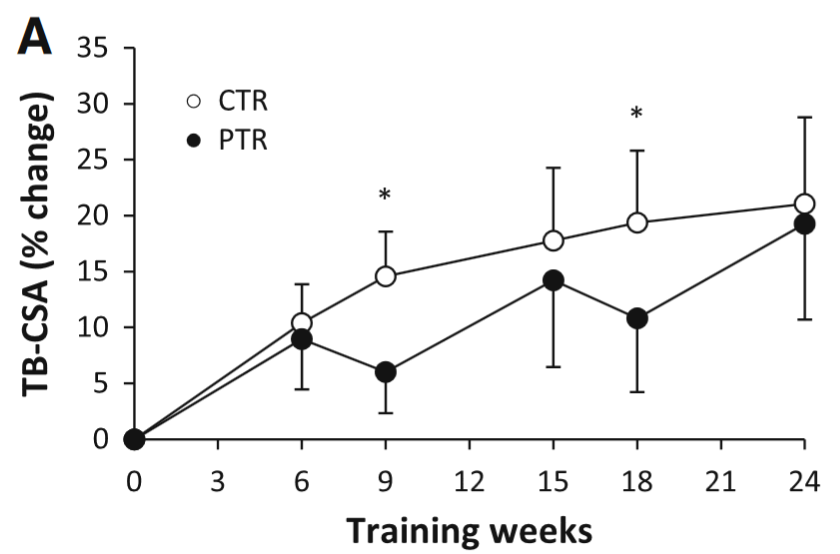
My bet is that muscle glycogen stores shrunk during the detraining phases, and rebounded during the training phases. Therefore, we are, to some extent, observing changes in muscle glycogen, not muscle mass. Though I don’t know exactly how much of the gains are glycogen gains compared to “dry” gains (the researchers didn’t control for body water). As you can see, the continuous group (CTR) made huge gains the first 6-9 weeks of training and then the curve becomes much flatter. I think this is because they made muscle gains and glycogen gains. Once the glycogen gains wear off, all we have is “pure” CSA gains.
Though I will write a counterpoint: Muscles can contain a maximum of 4g glycogen per 100g wet muscle ( Hansen, 1999 ). Glycogen can bind 3g of water per gram ( Ribero et al., 2014 ). So the maximum amount of glycogen + its bound water is:
= 16g (per 100g muscle).
The final answer is 16%. This shows us that glycogen and its bound water can’t make up huge changes in gains. But, it would explain small changes in muscle mass during detraining (for example a loss of 5-6% CSA as some studies have suggested ( Hortobágyi et al., 1993 ; Ogasawara et al., 2013 )). When it comes to filling muscles with glycogen, one study found that glycogen loading lead to a 3,5% CSA increase in untrained people ( Nygren et al., 2001 ). Perhaps glycogen loading/depletion plays an even bigger “hypertrophic” role in people who have at least 10-16 weeks of resistance training experience?
Peer review, as good as it sounds?
When an article is released in a peer-reviewed journal, we automatically assume it is of high quality and trustable. However, I’d argue we need to question that assumption. In 2013 , Bohannon sent a spoof-paper to 304 open-access journals.
He describes his article in the following way:
“[…] it should have been promptly rejected. Any reviewer with more than a high-school knowledge of chemistry and the ability to understand a basic data plot should have spotted the paper’s short-comings immediately. Its experiments are so hopelessly flawed that the results are meaningless.” Bohannon, 2013
And it looks like few journals questioned the quality:
“Acceptance was the norm, not the exception. The paper was accepted by journals hosted by industry titans Sage and Elsevier . The paper was accepted by journals published by prestigious academic institutions such as Kobe University in Japan. It was accepted by scholarly society journals. It was even accepted by journals for which the paper’s topic was utterly inappropriate, such as the Journal of Experimental & Clinical Assisted Reproduction.
the flagship journal of the Public Library of Science, PLOS ONE, was the only journal that called attention to the paper’s potential ethical problems , such as its lack of documentation about the treatment of animals used to generate cells for the experiment. The journal meticulously checked with the fictional authors that this and other prerequisites of a proper scientific study were met before sending it out for review. PLOS ONE rejected the paper 2 weeks later on the basis of its scientific quality .
Of the 255 papers that underwent the entire editing process to acceptance or rejection, about 60% of the final decisions occurred with no sign of peer review. For rejections, that’s good news: It means that the journal’s quality control was high enough that the editor examined the paper and declined it rather than send it out for review. But for acceptances, it likely means that the paper was rubber-stamped without being read by anyone.
By the time Science went to press, 157 of the journals had accepted the paper and 98 had rejected it.”
Beyond this issue of sloppy peer review, we have the problem of researchers faking research or peer review:
- Statement of Retraction. Replication of Obesity and Associated Signaling Pathways Through Transfer of Microbiota From Obese-Prone Rats : (This article was out since 2014, but wasn’t retracted until 2016:)
“The lead and corresponding authors wish to retract the above-cited article as an institutional investigation has identified that co-author Yassine Sakar falsified [data] .”
- 64 more papers retracted for fake reviews, this time from Springer journals
“ Springer is pulling another 64 articles from 10 journals after finding evidence of faked peer reviews , bringing the total number of retractions from the phenomenon north of 230. Given that there have been about 1,500 papers retracted overall since 2012, when we first reported on the phenomenon, faked reviews have been responsible for about 15% of all retractions in the past three years.”
- Publishing: The peer-review scam
“In the past 2 years, journals have been forced to retract more than 110 papers in at least 6 instances of peer-review rigging . What all these cases had in common was that researchers exploited vulnerabilities in the publishers’ computerized systems to dupe editors into accepting manuscripts, often by doing their own reviews. The cases involved publishing behemoths Elsevier, Springer, Taylor & Francis, SAGE and Wiley, as well as Informa, and they exploited security flaws that — in at least one of the systems — could make researchers vulnerable to even more serious identity theft.”
In short, we shouldn’t automatically assume research is of high quality, even if it is published in major peer-reviewed journals . Maybe authors are looking for the next big break? Maybe they are willing to do what it takes to get recognition? I don’t know, but we need to be aware that forging data and poor peer review are potential problems.
Misrepresenting citations
After having read many studies on fitness and nutrition research, I’ve discovered that several researchers will miscite (misquote) different research papers. By that I don’t mean they make some formal error and get the citations wrong that way. I mean they will cite studies that do not support the argument they are making. They probably do this because they (1) haven’t looked at the studies in enough detail and it’s a mistake, or (2) they do it consciously and hope people won’t check. This article isn’t meant to call out anybody, so I won’t link any to specific examples. All I can say is, if you start digging, you might find something that’s off ( Petrenuski et al., 2013 ; Hoffmaster et al., 2018 ). What this means in practice is that many conclusions will seem much more well-supported than they actually are. It’s also common to cite animal studies and use them as evidence for claims made about humans. See the animal studies section below for more details on this.
Poor methodology and reporting
Changing many variables at once.
Quite often, studies will alter multiple independent variables (for example group A will do 5 sets of 10 reps to failure while group B does 2 sets of 5 reps to non-failure). The results come in and they show group A gained more mass. The authors might conclude from this that group A was superior because they went to failure. This might be partially true, but it could also be the case that group A did much more volume, and so the combination of more volume and going to failure lead group A to be “better”.
Ideally, you would keep everything the same between groups and only change one variable. A surprising amount of studies do not do this, and it confounds their results and conclusions. Though this doesn’t apply to studies that look at ecological validity, because then it’s often the case that many variables are changed at the same time. For example, an ecological study might compare two different strength training programs, they might be completely different in terms of reps, sets, rest periods, use of failure, exercises, time under tension, etc. This wouldn’t matter, because you’re trying to figure out which program is best as a whole, you’re not looking at each individual variable in isolation.
Improper randomization
“trials with inadequate or unclear randomization tended to overestimate treatment effects up to 40% compared with those that used proper randomization” ( Kang et al., 2008 ).
In my experience, poor randomization isn’t as uncommon as it should be. In one study, women and men were unequally distributed between groups, which could influence results as per my discussion on sex differences.
No mention of adherence rates
As I’ve mentioned, adherence can be quite important, and if 30% of participants had less than say 60% adherence, then that is a big problem and it might influence the outcome. Adherence is a good measure of whether a program is unrealistic or not. High adherence means the program is probably relatively easy to follow and it might also motivate the participants. Very low adherence could mean the opposite.
Non-existent or flawed volume matching
When comparing two different strength training programs, it’s very important to match volume between the groups. This means that the groups should do the same number of hard sets to failure ( Dankel et al., 2016 ) or at the very least go very close to failure. A hard set to failure ensures that all participants get about the same level of fatigue and stimulus from the exercise. There are other ways to match volume, but these are suboptimal:
Matching total tonnage
This method might sound convincing at first. We match the total number of kilos/lbs the participants lift per week, for example. However, this method is flawed: it’s very easy to hit high tonnages using low-load high-rep training, but much more fatiguing and difficult to hit the same tonnages with high-intensity high-load training. For example, let’s say you’re doing 5 sets of 10RM bench press compared to 5 sets of 5RM bench press. Let’s say you can do 100kg for 5 reps for 5 sets. That is 2500kg total tonnage per session. If you can do 70kg for 10 reps for 5 sets, then you’re doing 3500kg total tonnage per session.
There are several studies that show similar gains when you do the same number of hard sets to failure . So these two protocols should lead to about the same level of hypertrophy, while the 70kg group will improve their muscular endurance more than the 100kg group who, most likely, will improve their 1RM more. So it doesn’t matter if the total tonnage is different, because the stimulus to grow will be about the same. If researchers follow the total tonnage method, they will reduce sets or reps for the 70kg group so that they match the total tonnage of the 100kg group. This tonnage matching, will, perhaps paradoxically to some, favour the 100kg group!
Matching total repetitions
It should go without saying that a repetition at 30% 1RM provides a completely different stimulus compared to a repetition at 90% 1RM.
Matching total sets without controlling fatigue :
Let’s say a study matched total sets between groups. If one group goes to failure on every set, while the other doesn’t, we have some issues. The main issue being that the failure group would be getting a different stimulus compared to the non-failure group. This is good if the purpose of the study is to test the difference between failure and non-failure. But if that isn’t the purpose, then all sets should be taken to the same level of fatigue by all participants (i.e. RPE 9 or 10).
Here’s an example of a situation where it could be a good idea to match volume: frequency studies. Several studies test whether it would be best to train a muscle group once or twice a week. If volume isn’t matched, we don’t know whether the study outcomes were because of the volume difference or the frequency difference. It should be said that there are many studies that do not do any sort of volume matching! And if studies do match volume, they usually use the wrong method. Like measuring total tonnage, but not the number of hard sets to failure.
Statistical power and low number of participants
Most strength training studies have anywhere from 6-20 participants. This diminished statistical power and it’s harder to show a true effect ( Ellis, 2010 ; Button et al., 2013 ). In other words, the fewer participants in a study, the greater the differences between the groups need to be ( Ellis, 2010 ). Since studies need a certain minimum level of power, some authors suggest doing a power analysis, because “ studies that have too much or too little statistical power are inherently wasteful, and potentially misleading “ ( Ellis, 2010 ). This also compounds on the duration issue (many studies have short durations).
“Power depends on several factors: magnitude of effect, sample size, N, and required level of statistical significance, α (the false-positive, or type I, error rate). Although N and α are determined by the experimenter, many of the factors that contribute to the effect size are typically unknown. In order to compute power, we are therefore required to make assumptions regarding what we expect to find.” ( Purcell et al., 2003 )
The graph below shows us how the sample size (number of participants) is connected to power and effect size (the magnitude of the difference):
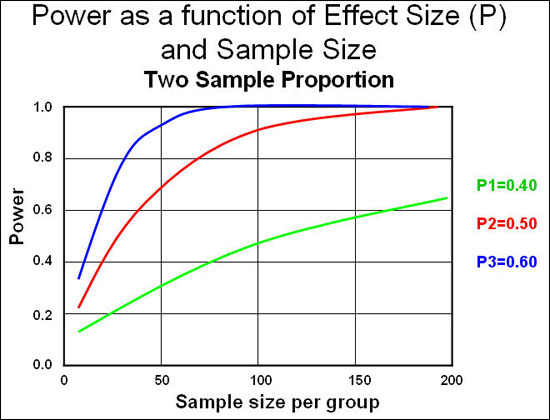
As you can see, power is very low when we have 10 participants per group (which is standard in fitness research) and we need to see very large effect sizes (differences between groups) to reach statistical significance. If we follow convention and aim for 80% (0.8) power, we need large effects or large sample sizes. In fitness research the effects are usually small, and so are the sample sizes. Hence we aren’t likely to detect a difference between groups even if it exists.
Correlations and outliers
“Outliers can have a very large effect on the line of best fit and the Pearson correlation coefficient, which can lead to very different conclusions regarding your data. This point is most easily illustrated by studying scatterplots of a linear relationship with an outlier included and after its removal, with respect to both the line of best fit and the correlation coefficient. This is illustrated in the diagram below:”
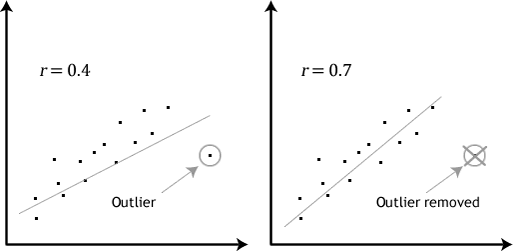
Statistical significance vs. clinical significance
Statistical significance does not automatically translate to real-world significance or clinical significance ( Bhardwaj, 2004 ; Ellis, 2010 ):
“An assessment of study power is essential in determining both the statistical significance and clinical relevance of any study and has serious implications for any conclusions that can be drawn. Consequences of an inappropriate sample size can be dangerous in either extreme. An excessively large sample may show statistical significance even when there is no clinical practicality; an inappropriately small sample will fail to demonstrate important clinically significant differences .” Bhardwaj, 2004
“The widespread practice of interpreting p values as evidence in support of hypothesized effects constitutes a blatant disregard for the limitations of statistical significance testing.” Ellis, 2010
Publication bias
Publication bias is when studies get “trashed” if they don’t confirm a hypothesis ( Dickersin et al., 1987 ; Fisher and Steele, 2012 ; Dwan et al., 2013 ; Song et al., 2014 ; Simonsohn et al., 2014 ). We then only get to see all the published studies that show a strong result, but not all the perfectly fine, but unpublished studies that had negative results. This could give us the impression that an effect is much stronger or more real than it really is.
Animal studies
I’m not even sure this needs to be mentioned, but animal studies are frequently used to make quite extraordinary claims about humans. There might be some overlap between species, but we shouldn’t assume that results of animal studies apply to humans ( Shanks et al., 2009 ; Uhl and Warner, 2015 ). If we do claim that an animal study applies, we need to justify it. It’s already difficult enough to compare different phenotypes within the species. How can we expect to compare different phenotypes across species with great accuracy?
“Experimental animal models are not fully reliable [but] reproduce at least some aspects of human disease. Expression and activation pattern of AMPK isoforms differs between rodent and human muscle and between muscle fiber types (149, 150). Furthermore, sex difference in muscle AMPK activation has been observed in humans, probably due to sex specific muscle morphology (higher proportion of type 1 muscle fibers in women)” (Viollet et al., 2009)
Other factors that can affect study outcomes
- Different limbs have different fiber type compositions. Muscle biopsies done on only one leg could affect outcomes ( Arevalo et a., 2016 )
- Determining CSA using MRI is imperfect (it measures intramuscular fat including FFM) ( Sions et al., 2017 ). This is primarily an issue in aging individuals ( McGregor et al., 2014 ). Muscles generate less force per unit of CSA with age ( Mitchell et al., 2012 ; McGregor et al., 2014 )
- Ambient conditions like temperature, noise levels, humidity etc. are not stated but could affect results ( Halperin et al., 2015 )
- Day and time of training should be stated ( Halperin et al., 2015 )
- Asking all participants to use the same number of reps as calculated from 1RM is not ideal (high individual variability) ( Arazi and Asadi, 2011 ; Richens and Cleather, 2014 ; Dankel et al., 2016 )
- ^Therefore, sets should be taken to failure to ensure uniform stress in all groups ( Dankel et al., 2016 )
- Measuring strength via peak torque, RFD, or isometric strength instead of “real world” 1RM improvements
- Using 2 or 3 compartment body analysis models like BIA to measure hypertrophy, not controlling water.
- Participants are sometimes classified as “resistance trained” in studies. But the standards scientists use for being resistance trained are much lower than what coaches would use. For example, researchers will describe a person as resistance trained if they have been doing strength training for one year. They sometimes measure how strong the person is at baseline, but rarely any sort of minimum strength criteria. Meaning, training time in months is usually the only criteria they use for being trained.
- Drugs: participants could’ve been on steroids years before or during the study (however some studies test for current drug usage during participant sampling).
- Experience: Some studies require participants to have strength training experience for x amount of years. This can’t be controlled and relies on the participant honestly recollecting his past training. Also, two people who have been training for the same amount of time could’ve had vastly different diets, training programs, etc. So time isn’t the best indicator for gains. You could be spinning your gears for a year or make serious progress.
- No mention of drop-outs in abstract: Several studies have had substantial drop outs during their intervention period, but some do not mention this in the abstract. This leads the reader to think the studies had more participants than what the study really had.
“To maintain a high degree of internal validity in performance and physiological testing , special consideration is warranted to reduce the risk of confounding variables affecting outcome measures . The sports science researcher and/or practitioner should typically control for age and gender of the subjects, caffeine and nutrient intake prior to testing, hour of the day and ambient temperature. Moreover, the effects of attentional focus, knowledge of exercise endpoint, verbal encouragement, positive and negative feedback, number and gender of observers, music and mental fatigue should also be considered given their meaningful effects on physical performance.” Halperin et al., 2015
Sci-Fit’s interpretation of the literature
Standards of evidence.
Generally speaking, we should have high standards for what we consider solid evidence. I generally want to see at least three different RCTs with human participants, solid methodologies, sufficient durations, done by different research teams. At this point, we can start to talk about whether an outcome is likely to be true, valid, and applicable to humans. Though that’s just the starting point. Ideally, we’d want to see even more studies and have them put into context via systematic reviews and meta-analyses.
Speculation and extrapolation
Since the literature is imperfect and limited, we are forced to speculate to some extent. I’ve consciously tried to minimize speculation as much as possible in my articles, but in some topics it’s inevitable that I have to mix real-life experience with the data from the research. This isn’t purely a limitation though, because scientific data needs to be placed in a real-life context to be useful. And there are very few studies that take into account whether the study protocol would work well in real life (see “ ecological validity ” for more info).
Scientific research deals with probabilities
Scientific studies can provide probabilistic support (with varying levels of quality and certainty) for a hypothesis or theory. Science can’t “prove” anything because a scientific field is not a homogeneous entity, nor does its answers exist in absolutes. When we say something is “proven” it implies it can’t change. It implies it is indisputable. In scientific fields, there are numerous research teams with multiple competing hypotheses, theories, data, etc. At any given time we can discuss which theory has the most support, but in science, theories evolve over time. Sometimes they are replaced entirely.
“ Scientific knowledge is inherently uncertain : experimental observations may be corrupted by noise, and no matter how many times a theory has been tested there is still the possibility that new experimental observations will refute it — as famously happened to Newtonian mechanics. Probability theory has from its conception been utilized to represent this uncertainty in scientific knowledge.”( Soldatova et al., 2013 )
Conclusion – How to apply research to your life
From the information presented in this article, I think it’s safe to conclude that we should be very careful about interpreting research. There are many reasons why studies don’t directly apply to our lives. Scientific studies can provide probabilistic support (with varying levels of quality) for a hypothesis or theory.
This begs the question: how can we apply the research to our lives?
To figure out whether something applies to us, we need to critically analyse the literature in its totality . Looking at one study in isolation is never enough. We should always strive to review the most relevant and important literature on any given topic and try to determine the preponderance of the evidence.
After we’ve looked at the literature and considered the drawbacks of every study, we can finally start to get a glimpse of what the truth could be. We then have to use our knowledge, experience, and intuition to apply what is done in the lab, to real life.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 14, Issue 5
- Social support in maintaining mental health and quality of life among community-dwelling older people with functional limitations in Malaysia: a population-based cross-sectional study
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-1590-5457 Nur Zahirah Balqis-Ali ,
- Weng Hong Fun
- Institute for Health Systems Research , Ministry of Health , Shah Alam , Selangor , Malaysia
- Correspondence to Dr Nur Zahirah Balqis-Ali; dr.nurbalqis{at}moh.gov.my
Objective This study aimed to examine the mediation role of perceived social support in the relationship between functional limitations, depressive symptoms and quality of life among older people in Malaysia.
Setting The Malaysian National Health Morbidity Survey 2018: Elderly Health was a cross-sectional health community survey among adults aged 50 and above.
Participants 3977 community-dwelling older Malaysians aged 60 and above.
Outcome measures Functional limitations were defined as personal activities of daily living (PADL) and instrumental activities of daily living (IADL), tested in separate paths in all analyses. PADL was measured using the Barthel Index, while IADL was measured using the Lawton and Brody scale. Perceived social support, depressive symptoms and quality of life were measured using the Duke Social Support Index, Geriatric Depression Scale-14 and Control, Autonomy, Self-Realisation and Pleasure-19 tools. We used mediation analysis through structural equation modelling to explore the role of perceived social support.
Results Perceived social support mediated the relationship between PADL and IADL with depressive symptoms, with the indirect effects at −0.079 and −0.103, respectively (p<0.001). Similarly, perceived social support mediated the relationship between PADL and IADL with quality of life, with the indirect effects at 0.238 and 0.301, respectively (p<0.001). We performed serial multiple mediation analysis and found that perceived social support and depressive symptoms mediated the path between PADL and IADL with quality of life, with the indirect effects at 0.598 and 0.747, respectively (p<0.001). The relationship between functional limitations and all outcomes remained significant in all mediation analyses.
Conclusion The present study provides evidence that perceived social support relieves the influence of functional limitations on depressive symptoms and declining quality of life among older people. Therefore, it is imperative to establish a social support system to improve the overall well-being of older people.
- quality of life
- depression & mood disorders
- social interaction
- social medicine
- statistics & research methods
Data availability statement
Data are available upon reasonable request. The data set analysed for this article is part of the National Health and Morbidity Survey 2018: Elderly Health study and belongs to the Ministry of Health Malaysia. Requests for the data can be obtained from the Sector for Biostatistics & Data Repository, National Institute of Health, Ministry of Health Malaysia, accessible at https://nihdars.nih.gov.my/ , with permission from the Director-General of Health, Malaysia.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2023-077046
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
STRENGTHS AND LIMITATIONS OF THIS STUDY
The National Health Morbidity Survey 2018 was a large and nationally representative health survey of older Malaysians, with 3977 respondents included in this study.
The primary factors and outcomes were measured using validated questionnaires and scales, allowing comparison with other studies.
Data was captured among older people living in the community, thus excluding older people residing in care facilities due to more severe functional limitations or depressive symptoms.
The functional limitations, social support, depression and quality of life measurement tools were rated based on respondents’ perceptions and interpretations, thus subject to personal bias.
This study analysed the perceived social support among the respondents while acknowledging that various other forms of social support exist.
Introduction
Ageing is a global challenge, driven by rising life expectancy, attributed to the improvement and higher quality of healthcare and falling fertility rates. 1 2 Globally, the proportion of the population aged 65 and above increased from 6% in 1990 to 9% in 2019 and is expected to increase further to 16% by 2050. 3 Similarly, the percentage of older people in Malaysia is projected to rise from merely 5% in 2010 to 14.5% in 2040. 4 This demographic shift has posed a significant challenge to healthcare systems, demanding greater adaptability to address the diverse needs of older people. 5
Among the major concerns for older people’s health are their mental well-being and quality of life. Of the various mental disorders, depression is among the highest contributor to disabilities and mortalities. 6 The WHO estimated that 3.8% of the global population is affected by major depression, and higher among older people (5.7%) in 2021, 7 while suicide is almost twice as frequent in older people than in younger populations. 8 Depression occurring at any age is debilitating as it may impair functioning and quality of life and lead to various health problems. 9 Late-life depression, or depression that begins or is detected in old age is associated with disability, increased mortality, poorer health outcomes and poorer quality of life as compared with those without depression. 10–12 Meanwhile, older people’s impaired quality of life signified a reduced ability to be independent, have autonomy and be satisfied with their lives. 13 , 14 On the other hand, evidence shows older people with a better quality of life tend to have better overall health, enabling them to age in place and live longer. 14–16 In Malaysia, depression among older people aged 60 and above in 2018 was 11.2%, while 28.6% perceived poor quality of life. 17
A significant risk factor for older people developing depression and having poor quality of life is functional limitations. 18–21 Functional limitations often refer to challenges, restrictions or reliance on others when performing personal activities of daily living (PADL) or instrumental activities of daily living (IADL). 22 23 PADL refers to a person’s ability to perform basic physical requirements, such as dressing, feeding, toileting, grooming, mobility and incontinence. 23 In contrast, IADL refers to activities that allow people to live independently in a community and are influenced by cognitive abilities. 22 The WHO reported that 38.1% of older people aged 60 and above experience some form of disability, which is higher in lower-income countries. 24 Such functional decline is debilitating, with the resulting functional limitation often leading to decreased independence, a reduction in quality of life, various health problems and may lead to depression. 25 26 While the relationship between functional limitations with both depression and poor quality of life is bidirectional and reciprocal, whereby each may impact the other in a progressive cycle, 20 27 functional limitations are more often found to be prodromal towards the deterioration in both mental health and quality of life. 24 Apart from the impact at the personal level, functional limitations and disability among older people impose a significant financial burden. The price of caring for a disabled, older person is tripled from a non-disabled older person. 28 In Malaysia, the National Health Morbidity Survey (NHMS) 2018 reports that 17.0% of older people aged 60 and above had functional limitations in PADL, while 42.9% had limitations in IADL. 17
The relationship between functional limitations, depressive symptoms and quality of life is complex and inter-related. While functional limitations are known to be risk factors associated with both depressive symptoms and quality of life, depressive symptoms alone are also risk factors for the quality of life. 29 30 Depressive symptoms impair the quality of life through physiological and behavioural mechanisms such as autonomic nervous system dysfunction, inflammation, endothelial dysfunction and decreased participation in health-promoting activities. 31 Thus, effective treatment and management of depressive symptoms predict a better quality of life. The study attempts to explain the dynamic and complex relationship between the primary factors (functional limitations) and outcomes (depressive symptoms and quality of life).
With various evidence linking functional limitations as significant risks of depression and poor quality of life among older people, research is shifting towards explaining the mechanism and ‘processes’ behind the development of the conditions. Evidence shows that one of the protective factors preventing or explaining the development of depression and declining quality of life among older people is having excellent social support. 32–35 The studies show that in the company of good or higher perceived social support, the decline in mental health and quality of life among older people who have developed functional limitations may be prevented. 32–35 Social support is any form of help made available to a person through their social connections with other people. It encompasses the benefits people gain from one another through information or expertise, emotional support, assistance and self-sufficiency. 36 While various forms of social support exist, perceived social support, defined as the satisfaction of feeling understood, respected and supported by a person’s social network, was found to have the most significant impact on improving older people’s well-being. 37 38
The examination of social support’s role necessitates contextual consideration. Malaysia, characterised by ethnic diversity, primarily comprises Malays, Chinese and Indians, each adhering to distinct religions. Despite these variations, cultural practices concerning support for older people, defined as those aged 60 and above, are notably shaped by a foundation of respect and responsibility towards them. 39 The prevalent approach involves close-knit familial support, often manifested through shared living arrangements dedicated to caring for older family members. Notably, approximately 70% of older people in Malaysia reside with family members, a pattern aligning with other Asian countries but exhibiting a lower prevalence compared with western nations. 40 41 Despite this, the NHMS 2018 reports that 30.8% of older people above 60 in Malaysia perceived having poor social support 17 ; this highlights the pressing need to enhance awareness and improve the provision of social support. In Malaysia, the healthcare system operates on a dichotomous model. The publicly funded health sector, financed through taxation, provides nearly free access to healthcare services for the entire population. Additionally, there exists a private health sector where services are fee-based. This dual approach ensures widespread accessibility to diverse healthcare services, encompassing the management of functional limitations and depressive symptoms. 42
As research progressed from estimating associations between factors to delving into the underlying mechanisms that come into play between a risk factor and an outcome, 26 a branch of study on mediation and moderation began to proliferate. In the context of the current study, social support is viewed as a mediator due to its potential role in explaining the changes in the depressive symptoms and quality of life of older people, as shown in various evidence. 34 35 43 One of the criteria for being a mediator is that the independent variable must explain the mediator being tested. 44 This study refers to functional limitations explaining social support. Evidence shows that those with functional limitations tend to lead towards isolation and loneliness, influencing how they perceive the social support they receive. 34 45 They may find it harder to get the support they need, as the functional limitation impairs their ability to get help and engage in social activities. At the same time, older people with functional limitations may feel like a burden to their social network, altering how they perceive social support. 34 A Malaysian study among older people aged 60 and above found that the ability to perform PADL and IADL significantly predict changes in social support levels. 46 Hence, social support potentially mediates the complex relationship between functional limitations-depressive symptoms-quality of life of older people.
Thus, we aim to contribute to the growing evidence of the role of social support in mediating the path between functional limitations and depression, as well as the quality of life among community-dwelling older people. We extend the analysis by incorporating serial mediation and testing both social support and depression in the trajectory of quality of life. Furthermore, social support is constructed and perceived differently across countries and contexts. We add depth to the evidence by reporting findings from a middle-income, Southeast Asian country with a unique culture shaping its social support practice and interpretation. This finding is critical for policymakers as an input to design appropriate interventions for the improved well-being of older people, looking from the perspective of social care.
Study design and setting
We used data from the NHMS 2018: Elderly Health, 17 a cross-sectional, community-based survey among adults aged 50 and above in Malaysia. It used a two-stage stratified cluster sampling design based on the Department of Statistics Malaysia’s sampling frame, from which 83 000 enumeration blocks (EB) of about 80–120 living quarters were considered. A total of 110 EB were randomly selected across all states and strata in Malaysia, giving a total of 5636 eligible living quarters to be included in the survey. The survey was conducted via face-to-face interviews at respondents’ places of residence between August and October 2018. The details of the study design and sample size determination for the NHMS 2018 can be found in the published report. 17 To focus on older people’s health in Malaysia, data from older people aged 60 and above, comprising 3977 respondents, were selected and analysed through a subpopulation analysis approach. This aligns with the guidelines set by the Malaysian Public Service Department, which designates the age of 60 as indicative of old age and retirement. 47 Furthermore, it adheres to the definition of older people outlined in the NHMS 2018, referring to the population aged 60 and above. All participants provided written informed consent before interviews during the NHMS 2018’s data collection.
Functional limitations
This study investigated both variables representing functional limitations, PADL and IADL, as independent variables. The original 10-item Barthel Index of PADL measured the ability to perform the activities. 48 A maximum score of 20 indicates a person’s absence of PADL functional limitation, while a decreasing score indicates a decline in functional ability.
The Lawton and Brody IADL scale measured the IADL, with a total score of 8, indicating the absence of IADL limitation. The decreasing score indicates worsening function. According to a local validation study, the Malay version of the Lawton IADL has an internal consistency of 0.838. 49
The Geriatric Depression Scale (GDS)-14, a 14-item index, was chosen by the NHMS study to determine the presence of depressive symptoms among older people in Malaysia. 17 The items explored depressive symptoms in the past week before the interview. Each item was answered either ‘Yes’ or ‘No’ based on the presence of symptoms. A response of ‘Yes’ was scored 1, while a response of ‘No’ was scored 0, resulting in a maximum possible total score of 14. A higher total score indicates a greater level of depression. The 14-item GDS was derived from the GDS-15 following a validation study in Malaysia, which found that one item had no discriminatory value in differentiating depression and non-depression. Hence, it was dropped from the scale. 50 The original tool from which GDS-14 was derived, the GDS-15, was used and validated through various studies. 51 52
Quality of life
The perceived quality of life of older people was measured using the quality of life scale of Control, Autonomy, Self-Realisation and Pleasure (CASP-19), with the total score generated by summing all 19 items between a score of 0–3 (0=never, 3=often), yielding a range of 0–57. 17 A higher score indicates a better quality of life. A local study translating the CASP-19 into two languages, Malay and Mandarin, found that the internal consistency was high for the original and translated versions (Cronbach’s alpha >0.8) and acceptable construct validity. 53
Social support
Perceived social support refers to the total score from the 11-item Duke Social Support Index (DSSI). The index was divided into two sections: the first on the size and structure of the social network (four items), while the second measures the older people’s satisfaction towards behavioural and emotional support received from their social network (seven items). Each item was scored from 1 to a maximum of 3 for a total maximum score of 33. A higher score indicates a higher level of perceived social support. The DSSI and its subscales had consistent patterns of low to moderate correlations. The availability of social integration had strong correlations with the overall DSSI score and its two subcomponents (0.57, 0.38, 0.53). 54 A study among 565 community-dwelling older people aged 70 and above found internal consistency using Cronbach’s alpha, with the overall index at 0.77 and test–retest ability scores ranging from 0.70 to 0.81. 54 The tool was translated into Malay in Malaysia and validated in a study among older people in Kuala Pilah in 2016 with a Cronbach’s alpha of 0.79. 55
Various covariates were included to control for socio-demographic and economic factors, including age, sex, ethnicity, strata location, highest education level, individual monthly income, employment status and marital status.
Statistical analysis
We described the characteristics of the community-dwelling older people aged 60 and above based on their socio-demographic and economic background. The sample was weighted to adjust for varying selection probabilities, non-response rate, strata, age and sex based on the 2018 Malaysian population data by the Department of Statistics Malaysia. 56 The weighted frequency (n) and percentage (%) described categorical data.
Multiple linear regressions were conducted to examine the impact of functional limitations and social support on depressive symptoms and quality of life, controlling for various covariates. These analyses allowed a comprehensive understanding of how independent variables and potential mediators affect the outcomes. Additionally, the score for depressive symptoms was added to the regression predicting quality of life to investigate the relationship between the two factors. A post-estimation analysis employing an omnibus test was performed to discern categorical predictors with more than two levels that exhibited significant associations with the outcome. Weightage was applied to all analyses.
To investigate the potential mediating role of social support between functional limitations and depressive symptoms and quality of life, a mediation analysis was performed using the structural equation modelling method. The analysis included adjustments for population estimation through the application of appropriate weighting. In separate models, the depressive symptoms and quality of life were entered as the dependent variables, the functional limitations (PADL and IADL) as independent variables and social support as the mediator being tested, adjusting for covariates found significantly associated with the outcomes from the previous multiple linear regressions. Figures 1(a) and (b) of online supplemental appendix A depict the relationship and hypothesis tested.
Supplemental material
A mediation effect was confirmed when functional limitations, either PADL or IADL or both, affect the dependent outcomes (depressive symptoms or quality of life, in separate models) through the potential intervening mediator (social support). In this analysis, the total effect (path c) refers to the impact of the independent variables on the dependent variable. It consisted of the independent variables’ direct effects (path c) on the dependent variables and the independent variables’ indirect effects (path a×b) on the dependent variables through the mediator. The coefficients and corresponding robust SEs were used to estimate the indirect effects, which indicated the magnitude of changes in the outcomes when the independent variables (functional limitations) were held constant and the mediator (social support) changed by the amount it would have changed if the independent variable had increased by one unit. 57 Bootstrapping was employed to assess the indirect effect of the mediation. A 95% CI level for the bias-corrected results was determined based on 5000 bootstrapped iterations. 58 In addition, the mediation effect was considered significant when the indirect effect mediated by social support did not contain 0 between the lower and upper confidence limits. 59 The proportion mediated by the indirect effect over the total effect and the standardised coefficients of the indirect effects were reported to represent the effect sizes. 60
Subsequently, a serial mediation analysis was performed, testing social support and depression as potential mediators affecting the trajectory between functional limitations and quality of life (figure 1(c) of online supplemental appendix A ). This model generated three indirect effects, with an additional path d indicating the effect between social support and depressive symptoms. The three indirect effects were calculated based on a1×b1, a2×b2 and a1×db2 (serial mediation).
To assess the robustness of the mediation models in estimating both direct and indirect effects when assumptions regarding confounding were potentially violated, we conducted additional mediations excluding the covariates. Subsequently, we conducted a sensitivity analysis on these models to quantify the strength of a confounder required to alter the conclusions drawn. This sensitivity analysis involved measuring the correlation parameter (ρ), which indicates the presence of omitted variables associated with the mediator and outcome. This parameter was incorporated into the average causal mediation effect calculations. 61 All analyses were conducted through Stata V.16.0 (StataCorp, College Station, Texas, USA), with the significant level set at 0.05.
Patient and public involvement
Patients and the public were not involved in this study’s design, conduct, reporting or dissemination plans.
The characteristics of community-dwelling older people above 60 involved in the NHMS 2018, comprising 3977 respondents, representing 3 230 340 older Malaysians, are shown in table 1 . The majority of respondents fell within the 60–69 age category, comprising 66.5% (95% CI: 63.7% to 69.1%) older people. Most respondents had up to the primary level of education (14.5% no formal education (95% CI: 12.5% to 16.9%), 43.6% primary education (95% CI: 39.4% to 47.9%)), were unemployed, 75.7% (95% CI: 73.6% to 77.7%), had less than Malaysian ringgit (MYR)1000, equivalent to US$216 of monthly income (exchange rate US$1=MYR4.62 62 ), 57.3% (95% CI: 53.4% to 61.1%) and were married, 67.9% (95% CI: 65.2% to 70.5%), at the time of the study. Respondents of Malay ethnicity were the most prevalent at 57.7% (95% CI: 48.7% to 66.2%).
- View inline
Socio-demographic and economic characteristics of community-dwelling older people above 60 (n=3977)
The mean scores of PADL, IADL, perceived social support, depressive symptoms and quality of life are shown in table 2 . In the multiple linear regressions, PADL, IADL and social support were significant predictors for both depressive symptoms and the quality of life of older people, adjusting for other covariates ( table 3 ). Depressive symptom scores decreased, indicating lesser depression, when functioning and social support increased. In contrast, the quality-of-life score increased with higher functioning and social support. Quality of life was found to be decreasing with higher depressive symptoms scores. All socio-demographic and economic factors were found to be significant covariates predicting depressive symptoms, except for age, marital status and strata. In contrast, only education and marital status were found to be significant covariates predicting quality of life. Each subsequent mediation analysis included the covariates that predicted the outcomes significantly.
Weighted means, SD and range of scores of the study variables (n=3977)
Multiple linear regressions of depressive symptoms and quality of life
Table 4 presents the results of the mediation analysis. The four paths where social support was tested as a potential mediator were shown as paths (A)—(D). In all paths, social support was found to play a significant mediator role. For example, in the path (A) between PADL and depressive symptoms, higher PADL was associated with lower depressive symptoms (β=−0.355, p<0.001). Still, the effect was altered when social support was included in the equation, with the effect toward depressive symptoms reduced (β=−0.275, p<0.001). In this mediation path, the indirect effect of perceived social support was −0.079 (−0.109 to −0.049). In this path, the proportion mediated by social support was 22.4%. A similar pattern and direction were observed in path (B) involving IADL with depressive symptoms, with 22.1% of the effect mediated by social support. The effect of functional limitations towards depressive symptoms remained significant with the mediation factor added, indicating a partial mediator role of social support. The relationships are also demonstrated in graphic figures in online supplemental appendix B . At the same time, the details of the path coefficients between all variables, including the covariates with depressive symptoms, are reported in online supplemental appendix C .
Weighted coefficients, SEs and CIs for mediation analysis, testing perceived social support as the potential mediator
Regarding the quality of life, both PADL and IADL (paths (C) and (D)) were found to be significantly associated with quality of life before adding social support (β=1.138, p<0.001 and β=1.521, p<0.001, respectively). However, social support reduced or mediated the effects (β=0.901, p<0.001 and β=1.219, p<0.001, respectively) through the indirect effects of 0.238 (0.143–0.332) in the PADL path and 0.301 (0.212–0.390) in the IADL path. Social support proportionately mediated each path by 20.8% and 19.8%, respectively. Similarly, the relationship between PADL and IADL with quality of life remained significant, with the mediation effect added into the equation, signalling the partial mediator role of social support. The relationships are also demonstrated in graphic figures in online supplemental appendix D . At the same time, the details of the path coefficients between all variables, including the covariates with quality of life, are reported in online supplemental appendix E .
The results of the serial mediation analysis are shown in table 5 . In the first analysis, the relationship between PADL and quality of life was tested (path (A)), with social support and depressive symptoms entered as multiple serial mediators into the path. The relationship between PADL and quality of life was significant (β=1.134, p<0.001) before adding the multiple mediations. The effect was brought lower (mediated) when social support and depressive symptoms were added into the equation (β=0.536, p<0.001). This coefficient value was lower than the previous single mediator paths, indicating that multiple mediations (social support-depressive symptoms) had more prominent roles in explaining the quality of life of older people than social support alone. The three indirect effects were found to be significant, indicating that both social support and depressive symptoms mediated the relationship between PADL and quality of life and social support affected depressive symptoms, which eventually affected the quality of life in the multiple mediations. The proportion mediated through the indirect effect was found to be 52.7%. The relationship between PADL and quality of life remained significant after adding multiple mediators into the equation, indicating partial mediation roles by social support and depressive symptoms. Similar findings were observed for IADL, as shown in path (B) in table 5 . The proportion mediated through the indirect effect was found to be 49.6%. The graphical representation is in online supplemental appendix F , while the path coefficients among all variables are reported in online supplemental appendix G .
Weighted coefficients, SEs and CIs in the serial mediation analysis
Replicating the mediation models without adjusting for covariates yielded a consistently significant result. The correlation coefficients necessary to nullify the indirect effect across all paths range between −0.2 and 0.4 ( online supplemental appendix H ).
Examining the complex relationship between various health factors through a mediation analysis revealed social support’s crucial role in influencing the well-being of community-dwelling older people. The presence of social support mediated the relationship between functional limitations and depressive symptoms, with social support indirectly accounting for reduced depressive symptoms. Similarly, social support also mediated the relationship between functional limitations and quality of life, indirectly improving the quality of life in the relationship. The serial mediation analysis found that social support affects depressive symptoms, influencing the quality of life. This finding suggests a serial mediation relationship between functional limitations and quality of life.
Higher functional limitations were significantly associated with lower depressive symptoms and better quality of life, confirming the findings in various studies. 18–21 The presence of social support explained the relationship. This finding reciprocated evidence from other studies. 34 35 45 63 64 Earlier work in 1996 found that lower reported social support was an essential reason for decreases in life satisfaction and increases in depressive symptoms among people in the USA. 34 In a Norwegian study, perceived social support was a significant mediator between functional limitations and depression among those aged 45 and above. 45 Similarly, a study among older people in China found that subjective support and utilisation of social support partially mediated the relationship between physical disability and depressive symptoms. In contrast, objective social support played no significant role. 35 Another study among older women in the USA found no significant role played by perceived social support in explaining depression. 64 It is important to note that all studies listed used different scales to measure all variables of interest and had diverse target populations and analytical methods in testing the mediation role, which may affect the similarities or differences observed from the current study.
Despite contrasting findings, the evidence thus far points towards social support explaining or being involved in the path of the relationship between depressive symptoms and quality of life among older people rather than merely a risk factor. As a person ages, many stressful life changes emerge, such as losing a spouse, retirement, relocations and changes in daily routines. 32 Stressors of this type are hypothesised to directly affect the risk and severity of illnesses, especially among those with functional limitations. 65 It has been proposed that, from a social aspect, having emotionally significant social relationships may be required to elicit the resilience necessary for successful adjustment to some of the stressors associated with ageing. 66 Biopsychosocial models of depressive symptoms and quality of life explain that disintegration in social support leads to social loneliness and unfulfillment of various needs of older people, making them vulnerable to declined mental health and life satisfaction. 67–69 Furthermore, in separate path analyses, this study explored two distinct categories of functional limitations in older adults: PADL and IADL. PADL encompasses essential self-care tasks, while IADL involves more complex activities supporting independent living. The research underscores the pivotal role of social support as a mediator for depressive symptoms and quality of life across both PADL and IADL domains. It emphasises the significance of integrating social support interventions into caregiving strategies, recognising their potential to mitigate functional limitations’ impact on older people’s well-being.
The implications of social support as a mediator are far-reaching. By identifying social support as a third variable in the relationship between functional limitations, depressive symptoms and quality of life, it becomes apparent that prevention and management activities should be extended beyond health services alone. This understanding allows for developing comprehensive strategies encompassing broader social interventions, ultimately leading to more optimal outcomes in later life. 32 In the current study, social support partially mediates, indicating that functional limitations were associated with depressive symptoms and quality of life independently and must be addressed vigorously. Nevertheless, the mediation analysis findings show that improving social support is crucial. In particular, the social aspect being tested in the current study revolved around perceived social support, requiring an understanding of its components to address the issue accurately. Perceived social support refers to the satisfaction of feeling understood, respected and supported by a person’s social network. 37 It does not involve the provision of aid, financial assistance or any other forms of tangible support. In fact, the economic factor was controlled as one of the potential confounders, which may be interpreted as regardless of financial background and other socio-demographic factors, variations in perceived social support played a role in influencing depressive symptoms and quality of life.
The prospects of improving the population’s health have shifted from improving healthcare alone to addressing the major social determinants of health, including accommodating better social support. 70 The more important questions to be addressed are: who is responsible for providing adequate social support, and what measures can be taken to improve the delivery of social support? In the context of the current study, whereby Malaysia is part of Asian countries, the responsibility of caring for and supporting the older people often rests on their children, although becoming more challenging due to urbanisation, the growing demands of the workforce and the relocation of children away from parents. 71 Nevertheless, over 70% of older Malaysians were found to be living with family and other members of their home, 21% were living with their spouse and only 9% were living alone. 40 Some strategies to strengthen family support towards older people include financial incentives and tax reliefs to families who continue caring for their older relatives. 72 Strengthening social activities for older people living in the community, such as social networking and educational classes held in community centres, has been associated with good outcomes among older people. 73 74
In the Malaysian context, various efforts have been put in place to improve social support for older people. For example, the Ministry of Women, Family and Community Development and Ministry of Health introduced various community-based programmes for older people, such as group physical activities, social gatherings and the establishment of committees overseeing and addressing older people’s needs in the community. 75 However, community-based services must be made widely accessible and affordable for older people for a successful outcome. In Malaysia, community-based initiatives, such as senior citizens’ activity centres, were gradually introduced in phases beginning in 2002. 76 The coverage has expanded over the years, but the implementation has faced challenges in coordinating activities across the social and health sectors. 76 77
A meta-analysis analysing social care services, which are defined as care that supports persons’ day-to-day needs delivered in their homes, found that the service led to lower hospital readmission rates and length of stay. 78 This profound evidence encapsulates the ability of persons, families, communities and governing bodies to enhance the delivery of social support for older people, ideally through an integrated approach that offers comprehensive support. In Malaysia, incentives and aid were available, including meals at home and monetary assistance to support the well-being of older people in the community. 75 79 However, the perceived social support remains low. In 2018, 30.8% of Malaysians above 60 perceived having poor social support, 17 highlighting the need for a more integrated approach to address the issue. A strategic consideration involves adopting a social prescribing service. In this paradigm, the health sector seamlessly integrates referrals for community-based social activities into the treatment plans for older people. 80 81 To effectively implement this initiative in Malaysia, a comprehensive approach is essential, beginning with the mapping and garnering support from various facilities that offer relevant services. This entails identifying and engaging stakeholders across different sectors to ensure alignment and collaboration. Another strategic move involves integrating assessments for the level of social support into the healthcare system’s protocols for addressing the health concerns of older people. Specifically, healthcare providers should be equipped to identify older people experiencing depression and low quality of life and assess their level of social support. This may involve implementing standardised screening tools and training healthcare professionals to recognise indicators of inadequate social support. To ensure effective intervention, seamless referral pathways should be established, directing older people with insufficient social support to appropriate resources such as social welfare departments or community support services. This necessitates raising awareness and training healthcare and social service providers about the importance of social support in improving the well-being of older people.
Depressive symptoms were also significantly associated with older people’s quality of life. The serial mediation analysis found that the multiple mediations by social support-depressive symptoms explain part of the quality of life among those with functional limitations. The regression analysis showed that social support was significantly associated with depressive symptoms, explaining the relationship. This relationship may be attributed to the positive influence of social support, as it enables older persons to engage more actively in health-promoting activities and access various healthcare or health-related resources. 82 Social support also provides coping mechanisms among older people in dealing with health or non-health-related issues, including depression. 83 Depression, conversely, excludes the experience of positive well-being and negatively influences a person’s living conditions, thus resulting in poorer quality of life. 84 This relationship highlights the importance of adopting a holistic and integrated approach to improve the quality of life of older people. Vigorous management of functional limitations should be accompanied by efforts to strengthen social support and manage depressive symptoms to enhance older people’s overall quality of life.
NHMS 2018 was conducted before the onset of the COVID-19 pandemic. Subsequent Malaysian studies have revealed the profound impact of the pandemic on the mental health and quality of life of Malaysians, mainly attributed to factors such as social isolation and economic instability. 85–87 Although the role of social support as a mediator during this period in Malaysia remains unexplored, existing research underscores its crucial role in preserving mental well-being and overall quality of life, particularly among older people. 88 89 A Malaysian study showed that older people with good social networks during the pandemic had better psychosocial outcomes. 90 Thus, it is postulated that the pandemic would have amplified the significance of social support as a mediator in mitigating these adverse effects.
While the NHMS 2018 is a large and nationally representative survey, it only captures older people living in the community, thus excluding older people residing in care facilities due to more severe functional limitations or depressive symptoms. Second, due to the study’s cross-sectional nature, causal establishment between relevant variables cannot be determined. The functional limitations, social support, depression and quality of life measurement tools were rated based on respondents’ perceptions and interpretations, thus subject to personal bias. Clinical assessment of depression and functional limitations and an observational or qualitative study to explore social support and quality of life may offer more accurate measurements. This study only analysed the perceived social support among the participants while acknowledging that various other forms of social support exist. Further research incorporating different forms of social support may offer a more comprehensive overview. Finally, our study was based on Malaysia’s unique cultural practice and healthcare systems, where countries with similar backgrounds may relate to the outcomes. Regardless, our analysis is one of the few examining the mediation analysis between functional limitations with two outcomes, depressive symptoms and quality of life, with additional serial mediation analysis.
This study reveals that perceived social support alleviates the relationship between functional limitations and depressive symptoms, as well as quality of life among older people. These findings provide valuable insights for designing and developing preventive measures and healthcare interventions to address depressive symptoms and improve quality of life. Consequently, promoting social support in the community-dwelling older population becomes vital for enhancing their well-being. Furthermore, by exploring the serial mediation roles of social support-depressive symptoms towards the quality of life, the study contributes to a better understanding of the complex interactions between various factors in influencing older people’s well-being. Enhancing social support for older people is vital for safeguarding their mental health and overall well-being. This involves expanding and formally integrating social activities into health and social sectors and increasing awareness for informal support within families and caregivers. Assessment of social support levels during regular medical visits and prescribing social activities may help older people feel more supported. Health and social care providers can improve their well-being and sense of belonging by understanding their social connections and suggesting activities they enjoy.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
All participants provided written informed consent before interviews during the NHMS 2018’s data collection. The NHMS survey protocol was approved by the Medical Research and Ethics Committee (MREC), Ministry of Health Malaysia (NMRR-17-2655-39047). The study was conducted by Good Clinical Practice guidelines and the Declaration of Helsinki.
Acknowledgments
We thank the Director-General of Health, Ministry of Health Malaysia, for permission to publish this paper and the Sector for Biostatistics and Data Repository, National Institutes of Health Malaysia, for providing the data.
- Officer A ,
- de Carvalho IA , et al
- United Nations DoEaSA
- Department of Statistics M
- World Health Organization
- Hoyert DL ,
- Xu J , et al
- Rapaport MH ,
- Fayyad R , et al
- Blazer DG ,
- Hybels CF ,
- Huang M-W ,
- Wang D-W , et al
- Gabriel Z ,
- Rondón García LM ,
- Ramírez Navarrro JM
- Sousa-Poza A
- Sixsmith A ,
- Institute for Public Health (IPH) NIH, Ministry of Health Malaysia
- Longfors J ,
- Fjeldstad AS , et al
- Browning CJ ,
- Rogers JC ,
- Martire LM , et al
- Rejeski WJ ,
- Garman KS ,
- Mlinac ME ,
- Su Y-Y , et al
- Faulkner JA ,
- Larkin LM ,
- Claflin DR , et al
- Freedman VA ,
- Martin LG ,
- Saraçlı Ö ,
- Atasoy N , et al
- Uchmanowicz I ,
- Gobbens RJJ
- Huffman JC ,
- Celano CM ,
- Beach SR , et al
- Bisconti TL ,
- Bergeman CS
- Newsom JT ,
- Yang Y , et al
- Rossmann MM ,
- McCubbin HI , et al
- Horwitz AV ,
- Merriam SB ,
- Hashim W , et al
- Yeung W-J ,
- Safurah J ,
- Kamaliah M ,
- Khairiyah A , et al
- Yao Y , et al
- Nes RB , et al
- Mahmud MA ,
- Muhammad EN , et al
- Bahagian Pencen JPA
- Mahoney FI ,
- Ibrahim S ,
- Razaob NA , et al
- Che Ismail H
- Malakouti SK ,
- Fatollahi P ,
- Mirabzadeh A , et al
- Sugishita K ,
- Sugishita M ,
- Hemmi I , et al
- Nalathamby N ,
- Mat S , et al
- Goodger B ,
- Higganbotham N , et al
- Sooryanarayana R ,
- Ahmad NA , et al
- Whittaker TA ,
- Schumacker RE
- Rockwood NJ
- Lachowicz MJ ,
- Preacher KJ ,
- Xe Currency Converter
- Travis LA ,
- Lyness JM ,
- Shields CG , et al
- Hutchinson SR ,
- Carstensen LL
- Garcia-Toro M ,
- Schotte CKW ,
- Van Den Bossche B ,
- De Doncker D , et al
- León LP de ,
- Mangin JPL ,
- Ballesteros S
- Braveman P ,
- Ministry of Health Singapore
- Escarbajal de Haro A ,
- de Miguel Lopez SMM ,
- Salmeron Aroca JA
- The Ministry of Women FaCD, Malaysia
- Ibrahim N ,
- Mat Saad Z ,
- Ahmad Ramly FZ
- Abd Wahab H
- Matthews FE ,
- Moffatt S , et al
- Johansson E ,
- Jonsson F ,
- Rapo E , et al
- Mulligan K , et al
- Greenglass E ,
- Fiksenbaum L ,
- Angermeyer MC ,
- Holzinger A ,
- Matschinger H , et al
- Hodori N ’Aqilah M
- Tung Y-Z , et al
- Chin SAFX ,
- Sathapan MSP , et al
- Bahari R , et al
- Vlachantoni A ,
- Evandrou M ,
- Falkingham J , et al
- Liu Z , et al
- Jamaluddin F ,
- Sheikh Dawood SR ,
- Ramli MW , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
Contributors NBZA: Conceived and designed the study; Performed the analysis; Analysed and interpreted the data; Wrote the paper. WHF: Conceived and designed the study; Analysed and interpreted the data; Wrote the paper. (1) ChatGPT—ChatGPT was used to improve the sentence structure. The authors wrote all the original sentences. ChatGPT was prompted to improve the structure of several sentences that the authors deemed could be further improved. (2) Grammarly—Grammarly was used to improve the grammar and choice of vocabularies used in the text. All original sentences were written by the authors. Grammarly checked, identified and suggested grammatical improvements to the sentences throughout the manuscript. NBZA is responsible for the overall content as the guarantor.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Effect of the HPV...
Effect of the HPV vaccination programme on incidence of cervical cancer and grade 3 cervical intraepithelial neoplasia by socioeconomic deprivation in England: population based observational study
Linked editorial.
HPV vaccine: the key to eliminating cervical cancer inequities
- Related content
- Peer review
- Milena Falcaro , senior statistician 1 ,
- Kate Soldan , scientist and epidemiologist 2 ,
- Busani Ndlela , cancer information analyst 3 ,
- Peter Sasieni , professor of cancer epidemiology 1
- 1 Centre for Cancer Screening, Prevention and Early Diagnosis, Wolfson Institute of Population Health, Queen Mary University of London, London EC1M 6BQ, UK
- 2 Blood Safety, Hepatitis, Sexually Transmitted Infections and HIV Division, UK Health Security Agency (UKHSA), London, UK
- 3 National Disease Registration Service (NDRS), NHS England, London, UK
- Correspondence to: P Sasieni p.sasieni{at}qmul.ac.uk (or @petersasieni on X)
- Accepted 27 March 2024
Objectives To replicate previous analyses on the effectiveness of the English human papillomavirus (HPV) vaccination programme on incidence of cervical cancer and grade 3 cervical intraepithelial neoplasia (CIN3) using 12 additional months of follow-up, and to investigate effectiveness across levels of socioeconomic deprivation.
Design Observational study.
Setting England, UK.
Participants Women aged 20-64 years resident in England between January 2006 and June 2020 including 29 968 with a diagnosis of cervical cancer and 335 228 with a diagnosis of CIN3. In England, HPV vaccination was introduced nationally in 2008 and was offered routinely to girls aged 12-13 years, with catch-up campaigns during 2008-10 targeting older teenagers aged <19 years.
Main outcome measures Incidence of invasive cervical cancer and CIN3.
Results In England, 29 968 women aged 20-64 years received a diagnosis of cervical cancer and 335 228 a diagnosis of CIN3 between 1 January 2006 and 30 June 2020. In the birth cohort of women offered vaccination routinely at age 12-13 years, adjusted age standardised incidence rates of cervical cancer and CIN3 in the additional 12 months of follow-up (1 July 2019 to 30 June 2020) were, respectively, 83.9% (95% confidence interval (CI) 63.8% to 92.8%) and 94.3% (92.6% to 95.7%) lower than in the reference cohort of women who were never offered HPV vaccination. By mid-2020, HPV vaccination had prevented an estimated 687 (95% CI 556 to 819) cervical cancers and 23 192 (22 163 to 24 220) CIN3s. The highest rates remained among women living in the most deprived areas, but the HPV vaccination programme had a large effect in all five levels of deprivation. In women offered catch-up vaccination, CIN3 rates decreased more in those from the least deprived areas than from the most deprived areas (reductions of 40.6% v 29.6% and 72.8% v 67.7% for women offered vaccination at age 16-18 and 14-16, respectively). The strong downward gradient in cervical cancer incidence from high to low deprivation in the reference unvaccinated group was no longer present among those offered the vaccine.
Conclusions The high effectiveness of the national HPV vaccination programme previously seen in England continued during the additional 12 months of follow-up. HPV vaccination was associated with a substantially reduced incidence of cervical cancer and CIN3 across all five deprivation groups, especially in women offered routine vaccination.
Introduction
Human papillomavirus (HPV) comprises a family of viruses, a subset of which are responsible for virtually all cervical and some anogenital and oropharyngeal cancers. 1 More than 100 countries worldwide have introduced prophylactic HPV vaccination as part of routine immunisation schedules. 2 One important outcome yet to be reported is whether vaccination has reduced or increased the inequalities seen for cervical disease in the UK and elsewhere.
In England, the national HPV vaccination programme started in 2008 using the bivalent Cervarix vaccine to prevent infections due to HPV types 16 and 18, which are estimated to cause around 80% of all cervical cancers in the UK. 3 Vaccination was offered routinely to 12-13 year old (school year 8) girls and as part of a catch-up campaign to those aged <19 years. 4 In September 2012 the programme switched to the quadrivalent vaccine (Gardasil), which additionally protects against HPV types 6 and 11 (responsible for genital warts), and in 2019 the programme was extended to 12-13 year old boys. Those who are eligible but not vaccinated can receive the vaccine free of charge from their general practitioner until their 25th birthday. 5
The introduction and implementation of HPV immunisation in this way means that noticeable discontinuities exist in the proportion of women vaccinated by date of birth, enabling a rigorous evaluation of the effectiveness of the programme. 6 For example, women born in August 1990 are unlikely to have received HPV vaccination, whereas among those born in the year from 1 September 1990 nearly 70% have received at least one dose of the vaccine.
Findings on the early effect of national HPV vaccination programmes have been encouraging. A wealth of real world evidence for the effect of vaccination on HPV prevalence exists 7 8 9 10 11 and evidence is growing for its effectiveness in reducing high grade cervical intraepithelial neoplasia (CIN) 12 13 14 15 and cervical cancer in vaccinated women. 14 16 17 18 19 For instance, we found that in England rates of grade 3 CIN (CIN3) and of cervical cancer were greatly reduced among those who were offered HPV vaccination, and that the magnitude of the reduction was greatest in the cohorts with the highest uptake and younger age at vaccination. 14 We estimated that by mid-2019 the immunisation programme had prevented cervical cancer in nearly 450 women and CIN3 in around 17 000 women.
Along with preventing ill health, a key aim of the NHS is to reduce health inequalities. 20 To this end, we investigated whether the effect of immunisation against HPV has resulted in a reduction in inequalities in cervical disease or a widening. Concern has been expressed that if the uptake of HPV vaccination is lower in those at greatest risk of cervical cancer, as has been seen in the US, 21 this could accentuate health inequalities. One study found that the introduction of HPV immunisation in England might initially have increased inequities in HPV related cancer incidence among ethnic minority groups because of the differential effect of herd protection in subpopulations with dissimilar vaccination coverage. 22 Previous studies have suggested that white people have a higher awareness of HPV and acceptance of the immunisation 23 and that vaccination uptake is lower in women from ethnic minority groups and more deprived areas. 24 Using data on HPV vaccination coverage by local area, however, a study found little variation by deprivation score in women offered routine vaccination (83% v 86% for most and least deprived areas, respectively) and only a small negative correlation between deprivation and vaccine uptake in those offered catch-up vaccination (47% v 53% for most and least deprived areas, respectively). 25 A full understanding of the effect of HPV vaccination across different socioeconomic groups is complicated by the poor uptake of cervical screening observed among younger women in the most deprived areas, leading to lower rates of screen detected cervical cancer and CIN3 at age 25 years compared with women in less deprived areas. 26 27
We replicated results from an analysis of population based cancer registry data to evaluate if the high vaccination effectiveness seen previously continued during an additional year of follow-up. The combined data were also used to investigate the effect of the vaccination programme by socioeconomic deprivation.
To represent socioeconomic deprivation, we used the index of multiple deprivation, a small area measure based on several domains of deprivation, such as income, employment, and health. The index is determined by using a standard statistical geographical unit, called lower super output area, which divides England into small areas of similar sized populations (on average about 1500 residents, or 650 households). 28 The lower super output areas are then ranked from the most to the least deprived and divided into five equal groups. The first and fifth groups correspond to the 20% most deprived and 20% least deprived lower super output areas in England, respectively.
We retrieved the records of all women aged 20-64 years resident in England with a diagnosis of invasive cervical cancer (ICD-10 (international classification of diseases, 10th revision) code C53) or CIN3 (ICD-10 code D06) between 1 January 2006 and 30 June 2020. These records are stored in the database managed by NHS England’s National Disease Registration Service, 29 and for each patient included information on index of multiple deprivation derived from the patient’s home postcode at the time of diagnosis. To convert these counts into rates, we used mid-year estimates of the female population for England by single year of age, calendar year (January 2006 to June 2020), and index of multiple deprivation (five groups). These estimates were retrieved from multiple tables publicly available on the website of the UK’s Office for National Statistics (ONS). 30 The supplementary material provides more details about the index of multiple deprivation versions used by the National Disease Registration Service and ONS, along with information on how we derived the population estimates required in our statistical analysis.
Statistical analysis
We separately analysed incidence rates of cervical cancer and CIN3 by using extensions of our previously described age-period-cohort Poisson model. 14 31 32 Data on women with cancer or CIN3 were aggregated by single month of age, calendar time (period), and date of birth (cohort). We derived the corresponding population risk time by subdividing the mid-year ONS population estimates into one month intervals for age, period, and cohort. For the analysis of the effectiveness by deprivation, we further split both the data on women with cancer or CIN3 and the population estimates by deprivation group (fifths). We then used the population risk time as the denominator for calculating rates (formally, the subdivided population estimates were log transformed and included in the Poisson regression model as an offset). Confidence intervals were computed using robust standard errors. 33 34
The code for the analysis was written and tested on synthetic data (extending the Simulacrum dataset) 35 by a statistician (MF) at King’s College London and then run on the real dataset by an analyst (BN) at the National Disease Registration Service.
We started by considering a core model where we included the main effects for age, period, and birth cohort, along with selected age by cohort and age by period interactions (see supplementary table S1). The interaction terms were included to account for variations in screening policy and historical events that affected cervical cancer rates. Specifically, we defined seven birth cohorts to capture differences in the age at first invitation to screening and the school years in which HPV vaccination was offered (see table 1 ). We added terms for seasonality and for events that may have affected registrations for cervical cancer and CIN3, such as the covid-19 lockdown, the “Jade Goody effect,” 36 37 and the 2019 cervical screening awareness campaign. In our previous paper, 14 we used several similar regression models to study the sensitivity of results to the precise way in which we adjusted for potential confounding factors. Because we found that the estimates of the cohort specific incidence rate ratios changed little across the various models, here we report on only a single model adjustment for confounders.
Characteristics of the birth cohorts
- View inline
Using the core model described, we investigated if the high effectiveness of the HPV immunisation programme reported previously 14 continued during an additional 12 months of follow-up. To do this we split the main effect of each cohort offered vaccination into two subgroup effects depending on whether the data related to the periods 1 January 2006 to 30 June 2019 or 1 July 2019 to 30 June 2020; this approach corresponded to adding three cohort by period interaction terms.
To evaluate the impact of socioeconomic deprivation on incidences of cervical cancer and CIN3, we extended the core model by adding main effects for deprivation and deprivation by cohort interactions. Specifically, we allowed the effect of each deprivation level to vary between unvaccinated women (cohorts 1-4) and those offered vaccination (cohorts 5-7), but we assumed it was otherwise constant within these two groups. We did not include further interactions between deprivation and other covariates as they were not of primary interest in this analysis. Using the fitted Poisson regression models, we made “what if” predictions by changing the value of one or more predictors and by leaving the others as observed. In this way it was possible to compare what happened (factual scenario) with what would have happened under an alternative (counterfactual) scenario.
We also carried out a sensitivity analysis where the effects of these deprivation by cohort interactions were allowed to vary across the three different groups offered vaccination (ie, we used 15 terms instead of five). For cervical cancer, owing to small numbers in cohort 7, we fitted a reduced model where the effects of these interactions were constrained to be the same for cohorts 6 and 7.
All analyses were performed in Stata, version 17. 38
Patient and public involvement
Patient and public involvement contributors were not formally involved in this research. We did, however, engage with Cancer Research UK (CRUK), Jo’s Cervical Cancer Trust, and the HPV Coalition on the importance of these analyses and the dissemination of the results. This included taking part in a video produced by ITN Business for World Cancer Day 2023, writing a piece for the 20th anniversary of the creation of CRUK, and engaging with international media about our research findings on the effect of the English HPV vaccination programme. We have also discussed the research and a draft of this paper with individual patients, journalists, and patient and public involvement representatives linked to broader research programmes.
Table 1 lists the characteristics of the birth cohorts included in the study. We defined the different cohorts so that each cohort is homogeneous in terms of the age women would have been offered HPV vaccination (if at all) and the age at which they would have first been invited for cervical screening.
Overall, there were 231.1 million women years of observation between 1 January 2006 and 30 June 2020 on women aged 20-64 years in England. During this time, 29 968 women received a diagnosis of invasive cervical cancer and 335 228 a diagnosis of CIN3 ( table 2 ). Observations between 1 July 2019 and 30 June 2020 have not been reported previously. With these additional 12 months of follow-up, there are, in the routine vaccination group (cohort 7), about twice the number of diagnoses compared with the same group in our previous study (we now have 13 v 7 previously for cervical cancer, 109 v 49 for CIN3; see supplementary table S2).
Summary statistics of study population
Our previously published findings on the effect of the national HPV vaccination were largely confirmed with the new data ( table 3 , also see supplementary table S3). The analysis showed that the previously observed low rates of disease and the estimated high effectiveness of the immunisation programme continued during the additional 12 months of follow-up (diagnoses in July 2019 to June 2020) among women born since 1 September 1990. In particular, the estimated effects of vaccination for that later period in cohort 7 (those born since 1 September 1995) imply a reduction in incidence of 83.9% (95% confidence interval (CI) 63.8% to 92.8%) for cervical cancer and 94.3% (92.6% to 95.7%) for CIN3 ( table 3 ). The relative risk reduction estimates for the earlier period are not identical to those reported previously because we also had new data for the unvaccinated cohorts that affected the baseline rates.
Estimated relative risk reductions (percentages) in incidence of invasive cervical cancer and CIN3 in the three cohorts offered HPV vaccination compared with the most recent unvaccinated cohort
Supplementary table S4 shows the full estimates from modelling the effects of vaccination in different levels of socioeconomic deprivation, with summary results reported in table 4 , table 5 , and table 6 . The highest incidence rates for invasive cervical cancer were observed among women living in the most deprived areas (first fifth) but, while in the reference unvaccinated group there was a strong downward gradient moving from women in the most deprived areas to those in the least deprived, little difference was found between the second and fifth fifths of deprivation in the groups offered vaccination. In both the reference and the vaccination cohorts the highest rates of CIN3 occurred in those from the most deprived areas, but no clear trend was observed among the other four fifths of deprivation (see supplementary tables S5 and S6).
Estimated number of invasive cervical cancers and CIN3s predicted and prevented by mid-2020 in the three cohorts of women offered HPV vaccination
Estimated cohort specific numbers of invasive cervical cancers predicted and prevented by mid-2020 among women in the least and most deprived areas
Estimated cohort specific numbers of CIN3 predicted and prevented by mid-2020 among women in the least and most deprived areas
Overall, our model estimated that 687 (95% CI 556 to 819) cervical cancers and 23 192 (22 163 to 24 220) CIN3s had been prevented by the vaccination programme up to mid-2020 among young women in England ( table 4 ). The greatest numbers for cervical cancer were prevented in women in the most deprived areas (192 and 199 for first and second fifths, respectively) and the fewest in women in the least deprived fifth (61 cancers prevented). The number of women with CIN3 prevented was high across all deprivation groups but greatest among women living in the more deprived areas: 5121 and 5773 for first and second fifths, respectively, compared with 4173 and 3309 in the fourth and fifth fifths, respectively. When we looked at the corresponding cohort specific figures ( table 5 and table 6 ), we noticed differences between the cohorts, particularly for CIN3. In all three cohorts offered vaccination the numbers and rates of prevented cervical cancers were much higher in women from the most deprived areas than least deprived areas ( table 5 ). The proportion of women with prevented cervical cancer in each cohort was, however, similar between the first and fifth fifths of deprivation. For CIN3 ( table 6 ), the results were more complicated. In women offered vaccination at age 16-18 years (cohort 5), the proportion of cervical cancers prevented was substantially less in those from the most deprived areas (29.6%) compared with those from the least deprived areas (40.6%). An inequality still existed in cohorts 6 and 7, but it was greatly reduced (67.7% v 72.8% in cohort 6 and 95.3% v 96.1% in cohort 7).
In England, the social-class gradient for cervical cancer is one of the steepest of any cancers: women in the most deprived fifth have had double the risk of those in the least deprived fifth. 39 40 Some of this results from differences in exposure to HPV and risk of an infection becoming persistent, 41 but differential uptake of cervical screening has also been an important factor. Previous research has highlighted the need for new engagement strategies to improve attendance for cervical screening among young women living in more socially deprived areas. 42 Encouragingly, the coverage of HPV vaccination has been (at least for the routine campaign and before the covid-19 pandemic) uniformly high. 43 It is, however, important to investigate whether immunisation—including the indirect effects achieved by high uptake—is helping to reduce health inequalities.
Using population based cancer registrations updated to mid-2020, which provided information on about twice the expected number of cancers in women offered HPV vaccination aged 12-13 years than in our previous analysis, we were able to show that the high vaccination effectiveness seen previously was confirmed with more recent data. The largest differences between the old and the new data were found for cohort 6 (the catch-up group offered the vaccine at age 14-16 years): for cervical cancer the estimated effectiveness increased, whereas for CIN3 it decreased. The reasons behind these differences are unclear. The results for cohorts 6 and 7 in the new data are more in keeping with what we would have expected given that the proportion of disease caused by HPV types 16 and 18 is greater for invasive cancer than for CIN3.
We also investigated the effect of the HPV immunisation programme by socioeconomic deprivation. Overall, we found that the programme was associated with a substantial reduction in the expected number of women with cervical cancers and CIN3 in all fifths of deprivation. For cervical cancer before vaccination, the downward gradient with decreasing deprivation was strong. In all cohorts offered vaccination, the highest rate was still seen among women living in the most deprived areas, but little difference was observed between women living in the second to fifth deprived areas. For CIN3, similar patterns were observed for the reference unvaccinated group and the three cohorts offered vaccination, but rates were greatly reduced in all fifths of deprivation in the latter. When we compared women in the most deprived areas with those in the least deprived areas in terms of percentage of disease averted, we observed differences across the cohorts for CIN3, with women in the least deprived areas in the older catch-up cohort (vaccine offered at age 16-18 years) having a greater proportion of averted CIN3s after HPV immunisation than women in the most deprived area (40.6% v 29.6%). The same, although to a much less extent, was observed for the younger catch-up cohort (72.8% v 67.7%). For invasive cervical cancer, we found no evidence of a less beneficial impact (in terms of percentage of cases averted) of the vaccination in women living in the most deprived areas; in fact, especially for the older catch-up cohort, the percentage was slightly higher in women in the most deprived areas compared with those in the least deprived areas.
The observed incidences of cervical cancer and CIN3 depend on three key factors: the intensity of exposure to HPV infections (including age at first exposure), the uptake of cervical screening, and HPV vaccination coverage. It is therefore difficult to disentangle the effects of these three drivers on the index of multiple deprivation specific rates with the data at hand. The health inequality in CIN3 in cohort 5 might result from the lower vaccination coverage among women in the most deprived areas since at age 16-18 years when they became eligible for vaccination more of those from the most deprived fifth may not have been in school or, for other reasons, may have missed the offer of HPV immunisation. These observations are consistent with previous understanding that higher uptake of catch-up vaccination was associated, although not as strongly as in some countries, with lower deprivation. 25 It is, however, reassuring that cohorts 6 and 7 showed little inequality in relative reductions in cancer (as in vaccination coverage).
However, since the UK has recently announced a change to a one dose schedule for routine HPV vaccination, ensuring this change achieves high coverage (including in the birth cohorts currently with lower coverage owing to covid-19 related interruption to schooling, and to immunisation services) is important to maintain the effects we have seen on cervical disease and on inequalities. Further investigations could be carried out in the future to check for any effect on cancer incidence caused by covid-19, gender neutral vaccination (since 2019), a change in the type of vaccine used, or reduced dose schedules.
Strengths and limitations of this study
Our analysis has several strengths. Our study provides direct evidence for the effect of a public health intervention (such as HPV vaccination) on cancer rates by deprivation. We used high quality data from population based cancer registries and were able to investigate the extent of socioeconomic inequalities in cohorts offered vaccination and whether the effectiveness of the HPV immunisation continued in an additional year of follow-up. The code for the analysis was written and tested using simulated data and an independent analyst later ran the code on the real dataset, guaranteeing reliable and robust results and preserving patient confidentiality.
The main limitations of our study are that it was observational and individual level data on vaccination status were not available. However, previous published research 14 provided detailed information on potential confounding factors and the best way to adjust for these in the analysis. Additionally, the discontinuities in vaccine uptake with date of birth makes this study powerful and less prone to biases from unobserved confounders than an analysis based on individual level data on HPV vaccination status.
Women born after 1 September 1999 were offered the Gardasil vaccine from 1 September 2012. As these women were at most aged 20 years and 10 months at the end of the study follow-up (30 June 2020), it is not yet possible with the data available to compare the effectiveness of the programme among those offered Cervarix and those offered Gardasil. This additional comparative analysis will become feasible with a longer follow-up on the recipients of Gardasil.
Policy implications
We found that the high effectiveness of the national HPV immunisation continued in the additional year of follow-up (July 2019 to June 2020). This is encouraging as it validates the previously published results and further supports consideration of more limited cervical screening for cohorts with high vaccination coverage aged 12-13 years. Moreover, although women living in the most deprived areas are still at higher risk of cervical cancer than those in less deprived areas, the HPV vaccination programme is associated with substantially lowered rates of disease across all fifths of socioeconomic deprivation. For cervical cancer, this has led to the levelling-up of the rates across the second to fifth fifths of deprivation so that the strong downward gradient observed in the reference unvaccinated cohort is no longer present in the cohorts offered vaccination. For CIN3, in the older catch-up cohorts women living in the least deprived areas seem to have benefited more from vaccination than those living in the most deprived areas, but the rates were still greatly reduced in all socioeconomic groups. Cervical screening strategies for women offered vaccination should carefully consider the differential effect both on rates of disease and on inequalities that are evident among women offered catch-up vaccination.
Conclusions
The HPV vaccination programme in England has not only been associated with a substantial reduction in incidence of cervical neoplasia in targeted cohorts, but also in all socioeconomic groups. This shows that well planned and executed public health interventions can both improve health and reduce health inequalities.
What is already known on this topic
In England, immunisation against human papillomavirus (HPV) has been associated with greatly reduced incidence rates of cervical cancer and grade 3 cervical intraepithelial neoplasia (CIN3) up to June 2019, especially among women offered routine vaccination at age 12-13 years
The social-class gradient for cervical cancer incidence has been one of the steepest of any cancers
Concern has been raised that HPV vaccination could least benefit those at highest risk of cervical cancer
What this study adds
The high effectiveness of vaccination against HPV seen previously continued during an additional year of follow-up, from July 2019 to June 2020
The English HPV vaccination programme was associated with substantially lower rates of cervical cancer and CIN3 in all fifths of socioeconomic deprivation, although the highest rates remained among women in the most deprived areas
For cervical cancer, the strong downward gradient from high to low deprivation observed in the reference unvaccinated cohort was no longer present among those offered vaccination
Ethics statements
Ethical approval.
Not required as the study used aggregated data from the National Disease Registration Service as well as publicly available information from the Office for National Statistics website.
Data availability statement
The cancer registry data analysed for this paper are securely held by the National Disease Registration Service (NDRS). Requests to access the data can be made through NHS England’s DARS service ( https://digital.nhs.uk/services/data-access-request-service-dars ). The Simulacrum ( https://simulacrum.healthdatainsight.org.uk/ ) is a synthetic dataset developed by Health Data Insight and derived from anonymous cancer data provided by NHS England’s NDRS. Mid-year population estimates are freely downloadable from the Office for National Statistics website ( https://www.ons.gov.uk/ ).
Acknowledgments
We thank Alejandra Castañon (LCP Health Analytics), Marta Checchi (UK Health Security Agency), and Lucy Elliss-Brookes (NHS England) for helpful comments on the study protocol, and Kwok Wong (NHS England) for contributing to the quality assurance of the data extraction code.
Contributors: PS had the original idea. He is the guarantor. MF and PS conceptualised the study and prepared the study protocol, which was subsequently reviewed by the other co-authors. MF wrote and tested the Stata code (checked by PS) for the data analysis and drafted the manuscript. BN extracted the dataset and ran the Stata code on it. All authors critically reviewed and approved the final submitted version. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: This work was supported by Cancer Research UK (grant No C8162/A27047). The funder had no role in the study design or in the collection, analysis, interpretation of data, writing of the report or decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ and declare support from Cancer Research UK for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Transparency: The lead author (the manuscript’s guarantor) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Dissemination to participants and related patient and public communities: The results of this research will be disseminated through the media, blogs and scientific meetings and will inform the design and implementation of interventions to reduce health inequalities. We will also work with others to produce information for the public to support human papillomavirus immunisation and cervical screening programmes and, if the opportunity arises, to contribute summary data for an international meta-analysis of similar studies.
Provenance and peer review: Not commissioned; externally peer reviewed.
This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/ .
- ↵ IARC. Human papillomaviruses. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, Volume 90. 2007.
- ↵ World Health Organization (WHO). Global Market Study: HPV 2022 https://cdn.who.int/media/docs/default-source/immunization/mi4a/who-mi4a-global-market-study-hpv.pdf?sfvrsn=649561b3_1&download=true .
- Cuschieri K ,
- Hibbitts S ,
- ↵ Public Health England (PHE). Human Papillomavirus (HPV) vaccine coverage in England, 2008/09 to 2013/14. A review of the full six years of the three-dose schedule: Public Health England (PHE); 2015. https://www.gov.uk/government/publications/human-papillomavirus-hpv-immunisation-programme-review-2008-to-2014 ; accessed 6 January 2021.
- ↵ UK Health Security Agency. HPV vaccination: guidance for healthcare practitioners (version 6) 2022 [updated April 2022]. https://www.gov.uk/government/publications/hpv-universal-vaccination-guidance-for-health-professionals ; accessed 24 August 2022.
- Lévesque LE ,
- Kaufman JS ,
- Brisson M ,
- HPV Vaccination Impact Study Group
- Thomas SL ,
- Tabrizi SN ,
- Brotherton JM ,
- Kaldor JM ,
- Markowitz LE ,
- Steinau M ,
- Hernandez-Aguado JJ ,
- Sánchez Torres DA ,
- Martínez Lamela E ,
- Lehtinen M ,
- Lagheden C ,
- Luostarinen T ,
- Falcaro M ,
- Castañon A ,
- Wallace L ,
- Pollock KG ,
- Elfström KM ,
- Skorstengaard M ,
- Thamsborg LH ,
- Dillner J ,
- Dehlendorff C ,
- Belmonte F ,
- ↵ NHS. The NHS long term plan 2019. https://www.longtermplan.nhs.uk/ ; accessed 24 August 2022.
- Johnson HC ,
- Lafferty EI ,
- Roberts SA ,
- Stretch R ,
- Sheridan A ,
- Pappas-Gogos G ,
- Douglas E ,
- McLennan D ,
- Henson KE ,
- Elliss-Brookes L ,
- Coupland VH ,
- ↵ Office for National Statistics. https://www.ons.gov.uk/ ; accessed 24 October 2022.
- Carstensen B
- Sasieni P ,
- ↵ Huber P. The behavior of maximum likelihood estimates under nonstandard conditions. Proceedings of the 5th Berkeley Symposium on Mathematical Statistics and Probability: University of California Press, 1967:221-33.
- Health Data Insight
- Lancucki L ,
- Patnick J ,
- Castanon A ,
- Thomson CS ,
- UK Association of Cancer Registries
- ↵ Cancer Research UK. Cervical Cancer Incidence Statistics 2015. https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/cervical-cancer/incidence ; accessed 14 March 2023.
- Currin LG ,
- Linklater KM ,
- Rahman MA ,
- Paranjothy S
- ↵ UK Health Security Agency (UKHSA). HPV vaccine uptake 2023. https://www.gov.uk/government/collections/vaccine-uptake#hpv-vaccine-uptake ; accessed 12 March 2023.
- Open access
- Published: 10 May 2024
Obesity and lipid indices as predictors of depressive symptoms in middle-aged and elderly Chinese: insights from a nationwide cohort study
- Xiaoyun Zhang 1 ,
- Ying Wang 1 ,
- Xue Yang 1 ,
- Yuqing Li 1 ,
- Jiaofeng Gui 1 ,
- Yujin Mei 1 ,
- Haiyang Liu 2 ,
- Lei-lei Guo 3 ,
- Jinlong Li 4 ,
- Yunxiao Lei 5 ,
- Xiaoping Li 6 ,
- Liu Yang 7 ,
- Ting Yuan 5 ,
- Congzhi Wang 7 ,
- Dongmei Zhang 8 ,
- Jing Li 9 ,
- Mingming Liu 9 ,
- Ying Hua 10 &
- Lin Zhang 7
BMC Psychiatry volume 24 , Article number: 351 ( 2024 ) Cite this article
213 Accesses
Metrics details
Depressive symptoms are one of the most common psychiatric disorders, with a high lifetime prevalence rate among middle-aged and elderly Chinese. Obesity may be one of the risk factors for depressive symptoms, but there is currently no consensus on this view. Therefore, we investigate the relationship and predictive ability of 13 obesity- and lipid-related indices with depressive symptoms among middle-aged and elderly Chinese.
The data were obtained from The China Health and Retirement Longitudinal Study (CHARLS). Our analysis includes individuals who did not have depressive symptoms at the baseline of the CHARLS Wave 2011 study and were successfully follow-up in 2013 and 2015. Finally, 3790 participants were included in the short-term (from 2011 to 2013), and 3660 participants were included in the long-term (from 2011 to 2015). The average age of participants in short-term and long-term was 58.47 years and 57.88 years. The anthropometric indicators used in this analysis included non-invasive [e.g. waist circumference (WC), body mass index (BMI), and a body mass index (ABSI)], and invasive anthropometric indicators [e.g. lipid accumulation product (LAP), triglyceride glucose index (TyG index), and its-related indices (e.g. TyG-BMI, and TyG-WC)]. Receiver operating characteristic (ROC) analysis was used to examine the predictive ability of various indicators for depressive symptoms. The association of depressive symptoms with various indicators was calculated using binary logistic regression.
The overall incidence of depressive symptoms was 20.79% in the short-term and 27.43% in the long-term. In males, WC [AUC = 0.452], LAP [AUC = 0.450], and TyG-WC [AUC = 0.451] were weak predictors of depressive symptoms during the short-term ( P < 0.05). In females, BMI [AUC = 0.468], LAP [AUC = 0.468], and TyG index [AUC = 0.466] were weak predictors of depressive symptoms during the long-term ( P < 0.05). However, ABSI cannot predict depressive symptoms in males and females during both periods ( P > 0.05).
The research indicates that in the middle-aged and elderly Chinese, most obesity- and lipid-related indices have statistical significance in predicting depressive symptoms, but the accuracy of these indicators in prediction is relatively low and may not be practical predictors.
Peer Review reports
Introduction
Depressive symptoms, as one of the most common psychiatric disorders among middle-aged and elderly in worldwide, have prevalence rates of 22.1% in the USA, 34.8% in Japan, 34.6% in France, and 42.0% in China [ 1 ]. The Chinese population is aging, and it is expected that by 2050, the number of Chinese citizens aged 65 and above will reach 400 million [ 2 ]. The increased risk of depressive symptoms caused by aging is a serious problem for China [ 3 ]. A meta-analysis consisting of 32 cross-sectional studies showed that the pooled prevalence of depression symptoms among elderly people in China was 22.7%, with a higher prevalence rate among females (24.2%) than males (19.4%) and a higher prevalence rate in rural areas (29.2%) than in urban areas (20.5%) [ 4 ]. It is reported that depressive symptoms are one of the top ten causes of disability and a risk factor for a series of chronic diseases such as cardiovascular disease, diabetes, and obesity [ 5 ]. According to a population-based cohort study [ 6 ], participants with two or more depressive symptoms had 31% higher odds of having general obesity and 26% higher odds of having central obesity. Furthermore, depressive symptoms have been shown associated with a higher risk of ischemic heart disease and its subtypes [ 7 ]. It harms personal physical function and quality of life, which in turn increases the pressure on medical resources and socio-economic conditions [ 8 ].
Indeed, obesity is a common disease that may occur simultaneously with depressive symptoms [ 9 ]. According to statistics, the prevalence of overweight and obesity among Chinese adults may reach 65.3%, and the population may reach 78.995 million by 2030 [ 10 ]. As an important public health issue, research shows that obesity will increase the death probability of many diseases and lead to a series of chronic diseases (including cancer, type 2 diabetes, and dyslipidemia), which greatly affects public health and increases social and economic burden [ 11 , 12 , 13 , 14 ]. Body mass index (BMI) and waist circumference (WC) are the most commonly used indicators for measuring obesity. They have been used in many studies [ 15 , 16 , 17 ] to explore the association between obesity and some diseases (such as diabetes, metabolic syndrome, and depressive symptoms). However, BMI is only a surrogate measure of body fatness and does not distinguish body composition (muscle and fat accumulation) [ 18 ]. While waist circumference (WC) effectively reflects body size, fat percentage, and distribution, its strong correlation with BMI complicates the differentiation of their respective contributions as separate epidemiological risk factors [ 19 , 20 ]. Therefore, many new obesity- and lipid-related indicators, including waist-height ratio (WHtR), visceral adiposity index (VAI), a body shape index (ABSI), body roundness index (BRI), lipid accumulation product (LAP), conicity index (CI), Chinese visceral adiposity index (CVAI), and triglyceride glucose (TyG) index have been proposed to use in epidemiological research [ 21 , 22 , 23 ].
Most previous studies [ 17 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 ] explored the relationship between depressive symptoms and obesity, and some of them have found positive associations [ 17 , 24 , 25 , 31 ], but others have suggested negative associations [ 26 , 27 , 28 , 29 , 32 ], or no associations [ 30 ]. The reasons for this inconsistency may be differences in population characteristics (including age, race, and cultural differences) [ 33 , 34 ], confounding factors [ 35 ], and different indices and standards for measuring obesity [ 36 , 37 ]. For example, a cross-sectional study conducted based on the Mexican population aged 20 or above found that obesity measured by BMI was positively associated with depressive symptoms in Mexican women [ 31 ]. In contrast, a study report on 2604 Chinese people aged 55 and above found a negative correlation between obesity and depressive symptoms measured by BMI, supporting the “fat and jolly” hypothesis [ 32 ]. The hypothesis proposes that obesity is negatively correlated with depressive symptoms and leads to a reduction in depressive symptoms [ 27 ]. So far, these studies are not representative in predicting depressive symptoms among middle-aged and elderly people in China, as most of them only describe one indicator and do not compare it with other indicators.
It is essential to emphasize the value of surrogate obesity-related indicators as efficient, cost-effective tools for the rapid screening and preliminary identification of individuals at high risk for depressive symptoms within large populations [ 38 , 39 , 40 ]. Previous studies [ 16 , 41 , 42 ] have compared the predictive power of simple surrogate obesity-related indices (including BMI, WHtR, VAI, BRI, ABSI, LAP, and TyG index) for metabolic syndrome, and have found that LAP and TyG index have stronger predictive power than other indicators. However, few studies have comprehensively examined the association between obesity- and lipid-related indices with depressive symptoms in the Chinese population, as well as the predictive strength for depressive symptoms. Thus, the association between obesity (measured by different indices) and depressive symptoms in middle-aged and elderly Chinese has to be further researched.
The purpose of this study is to investigate the relationship between 13 obesity- and lipid-related indices and depressive symptoms based on 2-year and 4-year longitudinal data from a nationally representative sample of community-dwelling Chinese participants aged 45 years or elderly. In addition, we also compared the screening and predictive abilities of different indicators in short-term (after 2 years follow-up) and long-term follow-up periods (after 4 years follow-up), and analyzed them separately based on sex.
Materials and methods
Study design and participants.
The China Health and Retirement Longitudinal Study (CHARLS) is a nationally representative cohort study that began in 2011 (Waves 1), targeting middle-aged and elderly people aged 45 and above in China and their spouses [ 43 ]. The participants are followed every two years through a face-to-face computer-assisted personal interview (CAPI), and data collection was carried out in 2013 (Waves 2) and 2015 (Waves 3). Data from CHARLS Waves 1, 2, and 3 were used in our study. We excluded individuals who met any of the following criteria at baseline: (1) missing data on depressive symptoms (excluding 7124 individuals) or Chinese version of the Center for Epidemiologic Studies Depression Scale (CES-D) ≥ 10 scores (excluding 7276 individuals), (2) missing data on any of the 13 indicators (excluding 3392 individuals), (3) missing data on age/sex/education levels/marital status/current residence/current smoking/alcohol consumption/taking activities/having regular exercise/chronic disease (excluding 1 individual). In addition, we excluded participants who did not have follow-up data (807 people lost to follow-up in 2013 and 937 people lost to follow-up in 2015). Finally, 3790 individuals who completed baseline surveys and short-term (from 2011–2013) follow-up surveys, and 3660 individuals who completed baseline surveys and long-term (from 2011–2015) follow-up surveys were enrolled in our research.
Depressive symptoms assessment
The depressive symptoms in the study were assessed using the Chinese version of the Center for Epidemiologic Studies Depression Scale (CES-D) [ 44 ]. The Chinese version of CES-D consists of 10 items that are intended to reflect the severity of the depressive symptoms over the previous week. Four-points are present for each item: the total scores varied from 0 to 30, with 0 representing rarely or never (< 1 day), 1 representing sometimes or sporadically (1–2 days), 2 representing a moderate amount of the time (3–4 days) and 3 representing frequently or always (5–7 days). Participants with a higher total score may be indicated “at risk” of depressive symptoms. CES-D ≥ 10 was a better cutoff point for indicating depressive symptoms and has been reported in previous studies [ 45 , 46 ]. When the CES-D value is 10, it provides the best discrimination ability when detecting individuals with or without a risk of depressive symptoms, with acceptable sensitivity, specificity, and accuracy [ 46 ]. The Chinese Version of CES-D has been confirmed to have better reliability and validity and was used frequently in predicting depressive symptoms [ 47 ].
Anthropometric measurements
The anthropometric measurements used in this analysis included non-invasive anthropometric indicators (including WC, BMI, WHtR, ABSI, BRI, and CI) and invasive anthropometric indicators (including VAI, LAP, CVAI, TyG index, TyG-BMI, TyG-WC, and TyG-WHtR) [ 48 , 49 , 50 , 51 ]. These indicators are widely used as markers for obesity and insulin resistance in epidemiological studies to predict the risk of diseases (such as metabolic syndrome, depression, and diabetes) [ 28 , 52 , 53 , 54 ]. However, most of these studies [ 28 , 52 , 53 , 54 ] use a single indicator to study the relationship between obesity and depression, without attempting to compare the predictive power of these indicators for depression. Therefore, based on previous literature [ 16 , 21 , 24 ], we selected 13 obesity and lipid-related indicators to investigate their correlation with depressive symptoms. WC was measured between the iliac crest and the lower ribs on both sides, at the end of expiratory breath. BMI was measured with weight (kg) /height 2 (m 2 ) [ 55 ]. Other anthropometric measurements are calculated using the following formula. It should be noted that invasive anthropometric indicators require blood sampling to evaluate TG and HDL-C levels.
\({\text{WHtR}}=\mathrm{WC }\left({\text{cm}}\right) /\mathrm{ Height} \left({\text{cm}}\right)\) [ 56 ]
Males: \({\text{VAI}}=\frac{WC\left(cm\right)}{39.68+\left(1.88\times BMI\right)}\times \frac{TG\left(mmol/l\right)}{1.03}\times \frac{1.31}{HDL-C\left(mmol/l\right)}\) [ 51 ]
Females: \({\text{VAI}}=\frac{WC\left(cm\right)}{36.58+\left(1.89\times BMI\right)}\times \frac{TG\left(mmol/l\right)}{0.81}\times \frac{1.52}{HDL-C\left(mmol/l\right)}\)
\({\text{ABSI}}=\frac{WC(m)}{{{Height(m)}^{1/2}\times BMI}^{2/3}}\) [ 56 ]
\({\text{BRI}}=364.2-365.5\sqrt{1-(\frac{(WC(m)/{(2\uppi ))}^{2}}{{\left(0.5\times Height(m)\right)}^{2}})}\) [ 57 ]
Males: \({\text{LAP}}=\left[\mathrm{WC }\left({\text{cm}}\right)-65\right]\times \mathrm{TG }\left({\text{mmo}}1/1\right)\) [ 21 ]
Females: \({\text{LAP}}=\left[\mathrm{WC }\left({\text{cm}}\right)-58\right]\times \mathrm{TG }\left({\text{mmo}}1/1\right)\)
\({\text{CI}}=\frac{WC\left(m\right)}{0.109\sqrt{\frac{weight\left(kg\right)}{height(m)}}}\) [ 23 ]
Males: \({\text{CVAI}}=-267.93+0.68\times {\text{age}}+0.03\times \mathrm{BMI }\left({\text{kg}}/{{\text{m}}}^{2}\right) +4.00\times \mathrm{WC }\left({\text{cm}}\right)+22.00\times {{\text{log}}}_{10}{\text{TG}} \left({\text{mmo}}1/1\right)-16.32\times {\text{HDL}}-{\text{C}} \left({\text{mmo}}1/1\right)\) [ 51 ]
Females: \({\text{CVAI}}=-187.32+1.71\times {\text{age}}+4.32\times \mathrm{BMI }\left({\text{kg}}/{{\text{m}}}^{2}\right) +1.12\times \mathrm{WC }\left({\text{cm}}\right)+39.76\times {{\text{log}}}_{10}{\text{TG}} \left({\text{mmo}}1/1\right)-11.66\times {\text{HDL}}-{\text{C}} \left({\text{mmo}}1/1\right)\)
\(\mathrm{TyG index}={\text{Ln}}\left[\left({\text{TG}}\left({\text{mg}}/{\text{dl}}\right)\times \mathrm{glucose }\left({\text{mg}}/{\text{dl}}\right)/2\right)\right]\) [ 21 ]
\({\text{TyG}}-{\text{BMI}}={\text{TyG}}\times {\text{BMI}}\) [ 50 ]
\({\text{TyG}}-{\text{WC}}={\text{TyG}}\times {\text{WC}}\) [ 50 ]
\({\text{TyG}}-{\text{WHtR}}={\text{TyG}}\times {\text{WHtR}}\) [ 50 ]
Socio-demographic characteristics include age, sex (1 = male, 2 = female), education levels, marital status, current residence, current smoking, alcohol consumption, taking activities, having regular exercise, and chronic disease. (1) age was sorted as four categories: 45–54, 55–64, 65–74, and above 75 years old; (2) education levels were classified into four groups: illiterate, less than elementary school, high school, and above vocational school; (3) marital status was classified into two categories: single and married; (4) current residence included the urban and rural; (5) current smoking was categorized into three groups: no smoker, former smoker and current smoker; (6) alcohol consumption was divided into three groups, which included never drinking, less than once a month, and more than once a month; (7) taking activities were sorted as two groups: the ever (at least once a month) and never; (8) having regular exercise included no exercise, less than exercises, and regular exercises; (9) the counts of chronic disease were classified into 0, 1–2, 3–14. Chronic diseases in our study, including hypertension, dyslipidemia, diabetes or hyperglycemia, malignant tumor, chronic lung disease, liver disease, heart disease, stroke, kidney disease, stomach or digestive system disease, mental and emotional diseases, memory-related diseases, arthritis or rheumatism, asthma. The presence of each disease is rated as 1, and the total score for all diseases ranges from 0 to 14. In terms of the number of chronic diseases, participants with three or more chronic diseases have a higher risk of depressive symptoms compared to those without any chronic disease [ 58 ]. These categories have been used extensively in our previous research [ 59 , 60 , 61 , 62 , 63 ].
Statistical analysis
Mean and standard deviation were used to express continuous variables. Categorical variables were expressed as frequencies and percentages. In order to calculate the differences in mean distribution by sex and with or without depressive symptoms, independent sample t-tests were utilized. Socio-demographic characteristics were categorized by sex and presented as frequencies and percentages. Differences between the male and female groups were tested for statistical significance using the Chi-square test. Binary logistic regression analysis was used to evaluate the associations between obesity- and lipid-related indices and depressive symptoms, with 13 indices as independent variables and depressive symptoms as dependent variables. Adjusting for age, sex, education levels, marital status, current residence, current smoking, alcohol consumption, taking activities, having regular exercise, and chronic disease, we reported odds ratios (ORs) and 95% confidence intervals (CIs). The receiver operating characteristic curve (ROC) was utilized to evaluate the performance of obesity- and lipid-related indices as predictors of depressive symptoms. The area under curve (AUC) and its 95% CIs were calculated to quantify this performance. The significance of the AUC is that an area greater than 0.9 indicates high accuracy, 0.71–0.9 indicates moderate accuracy and 0.5–0.7 indicates low accuracy [ 64 ]. Our data satisfies three assumptions required for statistical testing: normality, homogeneity of variance, and data independence. All of the statistical analyses were analyzed using the IBM SPSS version 25.0 (IBM Corp., Armonk, NY). P < 0.05 was considered statistically significant in all the analyses.
Table 1 showed the basic characteristics of the study participants. A total of 3790 participants were included in the short-term (2 years from 2011 to 2013) and 3660 in the long-term (4 years from 2011 to 2015). For the missing data, we found that there was no difference in socio-demographic characteristics compared to all the data, so we adopted a direct deletion method for the missing data. At baseline, 53.54% of the participants were males in the short-term, and 53.63% males in the long-term. The mean BMI, WHtR, VAI, ABSI, BRI, LAP, CI, CVAI, TyG index, TyG-BMI, TyG-WC and TyG-WHtR in females are higher than males during short- and long-term ( P < 0.05). During both short-term and long-term, we also observed the significant differences in age, education levels, marital status, current smoking, alcohol consumption between males and females, but observed no significant differences in the distribution of current residence, taking activities, and having regular exercises.
Table 2 showed the baseline characteristics of the study participants with and without depressive symptoms by sex at 2011 → 2013. After 2 years follow-up, approximately 20.79% of the participants had depressive symptoms (16.76% in males and 25.44% in females). Males with depressive symptoms had significant differences in current residence, current smoking, WC, WHtR, VAI, BRI, LAP, CI, CVAI, TyG-BMI, TyG-WC, and TyG-WHtR ( P < 0.05) during the short-term follow-up. Females with depressive symptoms had significant differences in current residence and chronic diseases ( P < 0.05).
Table 3 showed the baseline characteristics of the study participants with and without depressive symptoms by sex at 2011 → 2015. After 4 years follow-up, approximately 27.43% of the participants had depressive symptoms (21.50% in males and 34.30% in females). Marital status was significantly different between males with and without depressive symptoms during the long-term follow-up ( P < 0.05). Females with depressive symptoms had significant differences in current residence, taking activities, chronic diseases, WC, BMI, BRI, CVAI, TyG index, TyG-BMI, TyG-WC, and TyG-WHtR ( P < 0.05).
Table 4 showed the associations of obesity- and lipid-related indices with depressive symptoms. We use these indicators as continuous variables and depression as a binary variable, and the results are explained as how much the risk of depressive symptoms decreases or increases for every 1 unit increase in the indicators. In males, after controlling for age, educational levels, marital status, current residence, current smoking, alcohol consumption, taking activities, having regular exercises, and chronic diseases, WC (OR = 0.987, 95%CI: 0.974–1.000), LAP (OR = 0.996, 95%CI: 0.992–1.000), CVAI (OR = 0.997, 95%CI: 0.995–1.000), TyG-WC (OR = 0.999, 95%CI: 0.998–1.000) was significantly correlated with depressive symptoms during the short-term ( P < 0.05). For example, for every unit increase in WC and TyG-WC, the risk of depressive symptoms decreases by 0.013 and 0.001 times, respectively. In females, WC (OR = 0.983, 95%CI: 0.973–0.993), BMI (OR = 0.953, 95%CI: 0.926–0.979), WHtR (OR = 0.130, 95%CI: 0.026–0.647), BRI (OR = 0.908, 95%CI: 0.843–0.978), LAP (OR = 0.997, 95%CI: 0.994–1.000), CVAI (OR = 0.996, 95%CI: 0.993–0.998), TyG index (OR = 0.834, 95%CI: 0.708–0.983), TyG-BMI (OR = 0.995, 95%CI: 0.992–0.998), TyG-WC (OR = 0.998, 95%CI: 0.998–0.999), and TyG-WHtR (OR = 0.814, 95%CI: 0.707–0.936) were significantly associated with depressive symptoms during the long-term ( P < 0.05). For every unit increase in BMI and TyG-index, the risk of depressive symptoms decreases by 0.047 and 0.166 times, respectively. There were no significant associations between ABSI and depressive symptoms in males and females during both follow-up periods ( P > 0.05).
Table 5 showed the cut-off between area under curve, sensitivity, and specificity for obesity- and lipid-related indices to detect subsequent onset of depressive symptoms by sex. The ROC curves of each index for predicting depressive symptoms risk in males and females are shown in Fig. 1 and Fig. 2 during the short-term, Fig. 3 and Fig. 4 during the long-term, respectively. In males, WHtR (AUC = 0.462, SE = 0.017, 95% CI = 0.429–0.495, and optimal cut-off = 0.432) and BRI (AUC = 0.462, SE = 0.017, 95% CI = 0.429–0.495, and optimal cut-off = 2.176) had the largest predictive values among 13 indicators during the short-term ( P < 0.05). In females, BMI (AUC = 0.468, SE = 0.015, 95% CI = 0.439–0.496, and optimal cut-off = 19.378) and LAP (AUC = 0.468, SE = 0.015, 95% CI = 0.439–0.497, and optimal cut-off = 2.163) had the largest predictive values among 13 indicators during the long-term ( P < 0.05). However, there was no significant predictive ability of ABSI for depressive symptoms in both males and females during both follow-up periods ( P > 0.05).
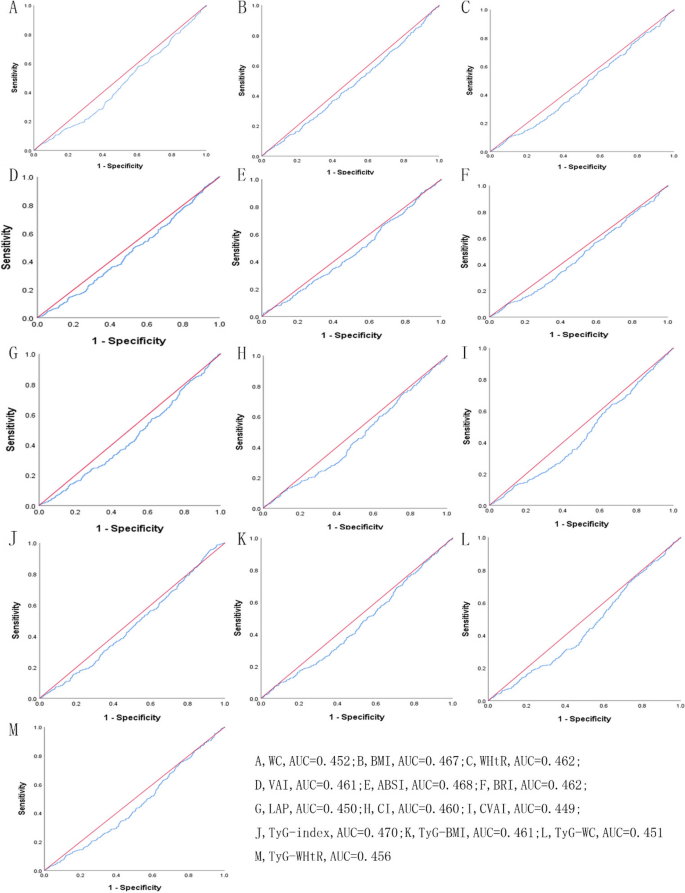
The ROC curves of each indicator in the prediction of depressive symptoms risk in males at 2011→2013
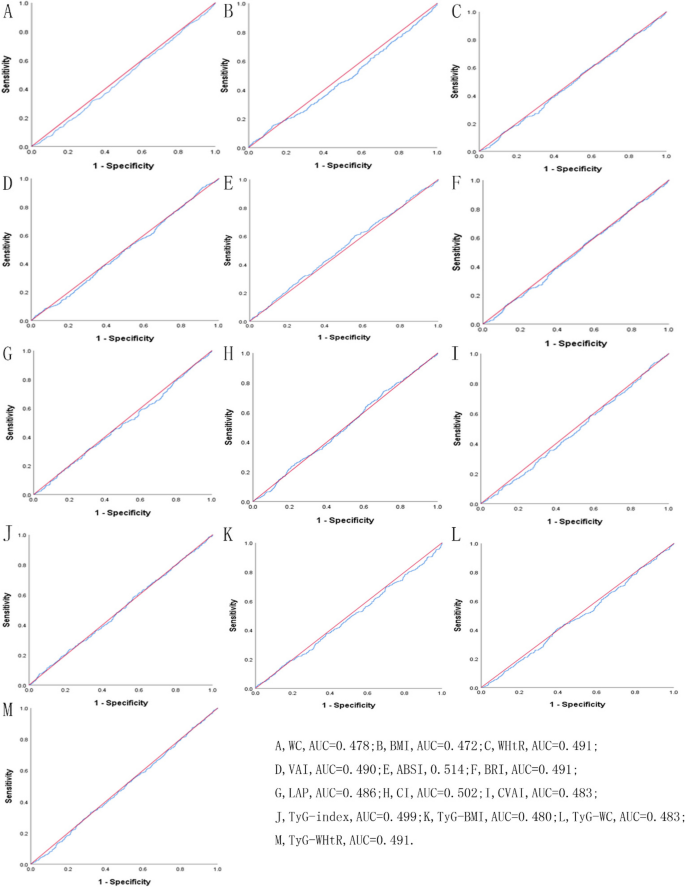
The ROC curves of each indicator in the prediction of depressive symptoms risk in females at 2011→2013
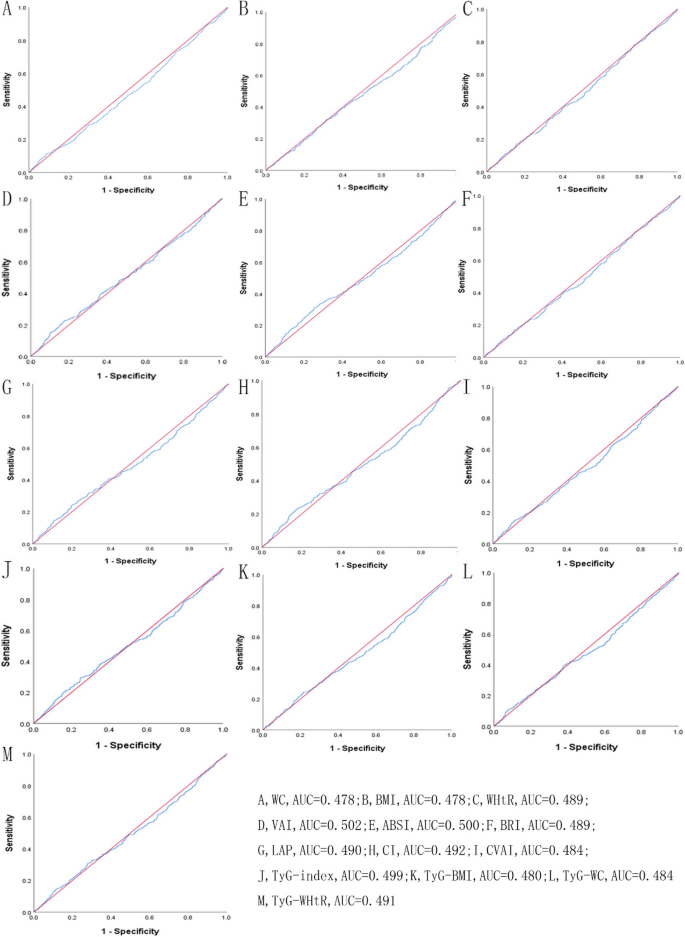
The ROC curves of each indicator in the prediction of depressive symptoms risk in males at 2011→2015
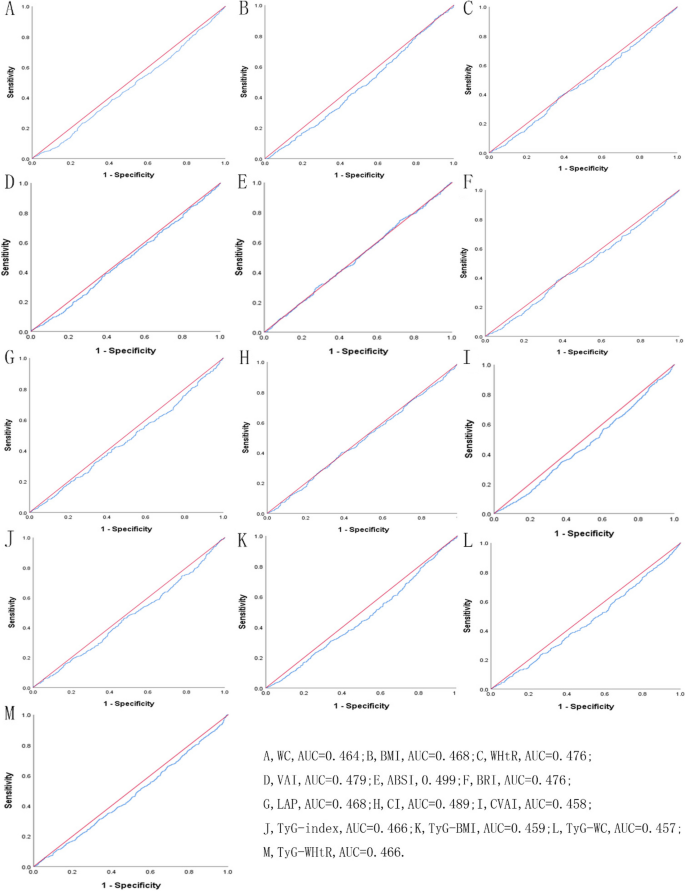
The ROC curves of each indicator in the prediction of depressive symptoms risk in females at 2011→2015
In our nationwide cohort study, we used ROC analysis to determine the predictive power of obesity- and lipid-related indicators for depressive symptoms. Our findings revealed that the AUC values of most indicators are below 0.5, indicating that the discriminative power of these indices is weak and not significantly better than random chance [ 64 ]. Although many previous studies [ 31 , 65 , 66 ] have reported a relationship between obesity and depressive symptoms, almost no research has investigated the predictive ability of indicators for depressive symptoms. Our study for the first time investigated the predictive ability of 13 indicators for depressive symptoms based on cohort studies, and found that all indicators had limited predictive ability for depressive symptoms.
We also found the incidence of depressive symptoms in females was 25.44% in short-term follow-up and 34.30% in long-term follow-up, consistently higher than in males during both follow-up periods. This is consistent with previous published studies [ 17 , 67 , 68 ]. Due to hormonal fluctuations (such as excessive sensitivity to hormonal fluctuations and menopausal hormonal changes), endocrine disorders can occur, making women prone to emotional fluctuations, depression, and reluctance to interact with others [ 69 ]. In, addition, psychosocial events, victimization, gender specific socialization, internalized coping strategies, and disadvantaged social status, females may be more prone to depression than males [ 70 , 71 ]. From the perspective of social differences, women may experience more stressful life events throughout their lives, and they are more sensitive to these events [ 70 ]. When faced with trouble, there is a significant difference in coping styles between women and men. Women are more inclined to focus on the emotions and repetitive thinking caused by problems, and this reflective coping style may lead to a higher incidence of depression.
Moreover, the significantly negative associations were found between depressive symptoms and most obesity- and lipid-related indicators, but differed by sex (male, female) and length of follow-up (2 years, 4 years). In males, the significant association between depressive symptoms and WC, LAP, CVAI, TyG-WC was observed in the short-term, but not observed in the long-term. No association between BMI and depressive symptom was observed in males during both follow-up periods. This could be because BMI is only a surrogate measure of body fatness and does not distinguish body composition (muscle and fat accumulation), especially for males who often have more muscle mass and less fat mass than females [ 18 ]. Therefore, if only BMI is considered, males may be more susceptible to these limitations. In females, the significant association between depressive symptoms and WC, TyG-WC was observed in the short-term, and WC, BMI, WHtR, BRI, LAP, CVAI, TyG index, TyG-BMI, TyG-WC, and TyG-WHtR was observed in the long-term. Compared to short-term follow-up, our study found that more indicators showed a significant negative correlation with depressive symptoms in females during long-term follow-up, which can be explained by cumulative effects.
However, we did not find the significant association between ABSI and depressive symptoms. Unlike our results, Lotfi K, Hassanzadeh Keshteli A, Saneei P, et al. found that ABSI was positively related to odds of depressive symptoms measured by the Hospital Anxiety and Depression Scale among Iranian females but not in males [ 72 ]. There are several points that can explain the differences between our survey results and the results of the aforementioned survey report. Firstly, previous research was conducted among Iranian adults, while our survey was conducted among the middle-aged and elderly population in China, with differences in demographic characteristics such as race and age. Secondly, Lotfi, K et al . used the Hospital Anxiety and Depression Scale. However, we used the Chinese version of the CES-D scale in our study, and there were differences in the diagnostic criteria for depression between the two measurement tools. Thirdly, previous research was a cross-sectional study, while ours is a cohort study with a larger sample size and analyzed the predictive ability of ABSI, therefore the current study has greater ability to detect these relationships. According to ROC analysis, the results for the ABSI AUC did not reach statistical significance in males and females during both follow-up periods ( P > 0.05), respectively. Hence, ABSI was not a valuable predictive indicator of depressive symptoms for both males and females.
According to our results, we supported the “fat and jolly” hypothesis in middle-age and elderly Chinese, in consistent with many previous studies [ 27 , 29 , 73 , 74 , 75 ]. Crisp AH, et al . first reported the "jolly fat" hypothesis in a middle-aged sample of the general population, which suggests a significant positive correlation between severe obesity in men and low levels of depression [ 75 ]. In addition, Yim G, Ahn Y, Cho J, et al. also found the association of obesity and depressive symptoms in 2210 Korean middle-aged women, supporting the “jolly fat” hypothesis, which suggests that women with general obesity were less likely to have depressive symptoms [ 74 ]. However, some cross-sectional studies suggest a positive correlation between obesity and depression [ 67 , 68 ]. Part of the reasons for the differences may be due to cultural differences, as people in different regions have different attitudes towards obesity. Weight bias is very common in American society. According to a survey, the prevalence of weight bias in the United States has increased by 66% in the past decade [ 76 ]. Weight stigmatization may be one of the risk factors for depression in obese individuals, and weight-based ridicule has been found to be a mediating factor in the relationship between obesity and depression [ 77 ]. A review summarizes evidence that internalization of weight bias is associated with negative mental health outcomes such as depression, anxiety, inferiority complex, and quality of life [ 78 ]. But in Chinese cultural tradition, the connection between happiness and obesity is described by a famous idiom " happy mind and fat body " [ 79 ]. Compared to Western culture, Chinese people believed that obesity is not a symbol of unhealthy behavior, as only wealthier people can afford more food and gain weight. In addition, middle-aged weight gain is considered a good omen of good luck, so people are willing to gain weight in their later years [ 28 ].
Strengths and limitations of the study
The main strength of our study are as follows: Firstly, we analyzed data based on a nationwide population-based longitudinal study. This study enrolled 3790 and 3660 middle-aged and elderly Chinese individuals in both short-term and long-term follow-up, the large sample size enhanced the generalizability and effectiveness of the research results. Secondly, it evaluated the impact of obesity- and lipid- related indicators on the depressive symptoms throughout two different interval periods. It helps us understand the short-term and long-term effects of 13 indicators on the incidence of depressive symptoms.
The study has several limitations should be noted. Firstly, depression symptoms were measured using the CES-D self-report scale, which has been shown to have acceptable psychological measurement characteristics and is suitable for a wider range of elderly participants. However, due to people tend to underreported their mental disease in the research, there may be reporting bias in the results. Secondly, with the deepening of aging, the incidence rate of depressive symptoms among middle-aged and elderly people is rising, which is a serious problem facing China. Therefore, this study included middle-aged and elderly people aged 45 and above in China. It is worth noting that the results of our study in the context of other age groups should be interpreted with caution. Lastly, our results indicate that the AUC values of most indicators are below 0.5, indicating low diagnostic accuracy and inability to effectively predict depression in clinical practice. In future research, we need to try to combine two or more indicators to see if it can improve diagnostic accuracy.
Among the obesity- and lipid-related indices, ABSI did not correlate with depressive symptoms and failed to serve as a valuable predictor for both males and females across all intervals. Our research findings indicate that most obesity- and lipid-related indicators have statistical significance in predicting depressive symptoms, but the accuracy of these indicators in prediction is relatively low and may not be practical predictive factors. The results of this study may be of great significance for the early identification and prevention of depressive symptoms in middle-aged and elderly Chinese. Given the urgency of early screening for high-risk individuals for depressive symptoms, future research can explore the use of multiple indicators in combination to test whether they can improve the predictive ability of depressive symptoms, and thus have practical applications in clinical practice.
Availability of data and materials
Data can be accessed via http://opendata.pku.edu.cn/dataverse/CHARLS .
Abbreviations
China Health and Retirement Longitudinal Study
Waist circumference
Body mass index
Waist-height ratio
Visceral adiposity index
A body shape index
Body roundness index
Lipid accumulation product
Conicity index
Chinese visceral adiposity index
Triglyceride glucose index
Triglyceride-glucose related to BMI
Triglyceride-glucose related to WC
Triglyceride-glucose related to WHtR
The Chinese version of the Center for Epidemiologic Studies Depression scale
Receiver operating characteristic curve
Area under curve
Statistical Product Service Solutions
Odds ratios
Confidence intervals
Standard error
Richardson RA, Keyes KM, Medina JT, Calvo E. Sociodemographic inequalities in depression among older adults: cross-sectional evidence from 18 countries. Lancet Psychiatry. 2020;7(8):673–81.
Article PubMed PubMed Central Google Scholar
Fang EF, Scheibye-Knudsen M, Jahn HJ, Li J, Ling L, Guo H, Zhu X, Preedy V, Lu H, Bohr VA, et al. A research agenda for aging in China in the 21st century. Ageing Res Rev. 2015;24(Pt B):197–205.
Qiu Q-W, Qian S, Li J-Y, Jia R-X, Wang Y-Q, Xu Y. Risk factors for depressive symptoms among older Chinese adults: a meta-analysis. J Affect Disord. 2020;277:341–6.
Article PubMed Google Scholar
Zhang L, Xu Y, Nie H, Zhang Y, Wu Y. The prevalence of depressive symptoms among the older in China: a meta-analysis. Int J Geriatr Psychiatry. 2012;27(9):900–6.
Penninx BWJH, Milaneschi Y, Lamers F, Vogelzangs N. Understanding the somatic consequences of depression: biological mechanisms and the role of depression symptom profile. BMC Med. 2013;11(1):129.
Mulugeta A, Zhou A, Power C, Hyppönen E. Obesity and depressive symptoms in mid-life: a population-based cohort study. BMC Psychiatry. 2018;18(1):297.
Liu S, Luo J, Zhang T, Zhang D, Zhang H. The combined role of obesity and depressive symptoms in the association with ischaemic heart disease and its subtypes. Sci Rep. 2022;12(1):14419.
Article CAS PubMed PubMed Central Google Scholar
Zormpas C, Kahl KG, Hohmann S, Oswald H, Stiel C, Veltmann C, Bauersachs J, Duncker D. Depressive symptoms and quality of life in patients with heart failure and an implantable cardioverter-defibrillator. Front Psychiatry. 2022;13:827967.
Milaneschi Y, Simmons WK, van Rossum EFC, Penninx BW. Depression and obesity: evidence of shared biological mechanisms. Mol Psychiatry. 2019;24(1):18–33.
Article CAS PubMed Google Scholar
Wang Y, Zhao L, Gao L, Pan A, Xue H. Health policy and public health implications of obesity in China. Lancet Diabetes Endocrinol. 2021;9(7):446–61.
Tápias FS, Otani VHO, Vasques DAC, Otani TZS, Uchida RR. Costs associated with depression and obesity among cardiovascular patients: medical expenditure panel survey analysis. BMC Health Serv Res. 2021;21(1):433.
Powell-Wiley TM, Poirier P, Burke LE, Després JP, Gordon-Larsen P, Lavie CJ, Lear SA, Ndumele CE, Neeland IJ, Sanders P, et al. Obesity and cardiovascular disease: a scientific statement from the American heart association. Circulation. 2021;143(21):e984–1010.
Pischon T, Nothlings U, Boeing H. Obesity and cancer. Proc Nutr Soc. 2008;67(2):128–45.
Williams EP, Mesidor M, Winters K, Dubbert PM, Wyatt SB. Overweight and obesity: prevalence, consequences, and causes of a growing public health problem. Curr Obes Rep. 2015;4(3):363–70.
Issaka A, Cameron AJ, Paradies Y, Kiwallo JB, Bosu WK, Houehanou YCN, Wesseh CS, Houinato DS, Nazoum DJP, Stevenson C. Associations between obesity indices and both type 2 diabetes and impaired fasting glucose among West African adults: results from WHO STEPS surveys. Nutr Metab Cardiovasc Dis. 2021;31(9):2652–60.
Gu Z, Zhu P, Wang Q, He H, Xu J, Zhang L, Li D, Wang J, Hu X, Ji G, et al. Obesity and lipid-related parameters for predicting metabolic syndrome in Chinese elderly population. Lipids Health Dis. 2018;17(1):289.
Frank P, Jokela M, Batty GD, Lassale C, Steptoe A, Kivimäki M. Overweight, obesity, and individual symptoms of depression: a multicohort study with replication in UK Biobank. Brain Behav Immun. 2022;105:192–200.
Gomez-Ambrosi J, Silva C, Galofre JC, Escalada J, Santos S, Millan D, Vila N, Ibanez P, Gil MJ, Valenti V, et al. Body mass index classification misses subjects with increased cardiometabolic risk factors related to elevated adiposity. Int J Obes (Lond). 2012;36(2):286–94.
Fang H, Berg E, Cheng X, Shen W. How to best assess abdominal obesity. Curr Opin Clin Nutr Metab Care. 2018;21(5):360–5.
Krakauer NY, Krakauer JC. A new body shape index predicts mortality hazard independently of body mass index. Plos One. 2012;7(7):e39504.
Ahn N, Baumeister SE, Amann U, Rathmann W, Peters A, Huth C, Thorand B, Meisinger C. Visceral adiposity index (VAI), lipid accumulation product (LAP), and product of triglycerides and glucose (TyG) to discriminate prediabetes and diabetes. Sci Rep. 2019;9(1):9693.
Calderón-García JF, Roncero-Martín R, Rico-Martín S, De Nicolás-Jiménez JM, López-Espuela F, Santano-Mogena E, Alfageme-García P, Sánchez Muñoz-Torrero JF. Effectiveness of Body Roundness Index (BRI) and a Body Shape Index (ABSI) in predicting hypertension: a systematic review and meta-analysis of observational studies. Int J Environ Res Public Health. 2021;18(21):11607.
Shenoy U. Jagadamba: influence of central obesity assessed by conicity index on lung age in young adults. J Clin Diagn Res. 2017;11(4):09–12.
Google Scholar
Fabricatore AN, Wadden TA, Higginbotham AJ, Faulconbridge LF, Nguyen AM, Heymsfield SB, Faith MS. Intentional weight loss and changes in symptoms of depression: a systematic review and meta-analysis. Int J Obes (Lond). 2011;35(11):1363–76.
Zhong W, Cruickshanks KJ, Schubert CR, Nieto FJ, Huang GH, Klein BE, Klein R. Obesity and depression symptoms in the Beaver Dam offspring study population. Depress Anxiety. 2010;27(9):846–51.
Zhang L, Liu K, Li H, Li D, Chen Z, Zhang LL, Guo LL. Relationship between body mass index and depressive symptoms: the “fat and jolly” hypothesis for the middle-aged and elderly in China. BMC Public Health. 2016;16(1):1201.
Liao W, Luo Z, Hou Y, Cui N, Liu X, Huo W, Wang F, Wang C. Age and gender specific association between obesity and depressive symptoms: a large-scale cross-sectional study. BMC Public Health. 2020;20(1):1565.
Zhang L, Li JL, Zhang LL, Guo LL, Li H, Yan W, Li D. Relationship between adiposity parameters and cognition: the “fat and jolly” hypothesis in middle-aged and elderly people in China. Medicine (Baltimore). 2019;98(10):e14747.
Qian J, Li N, Ren X. Obesity and depressive symptoms among Chinese people aged 45 and over. Sci Rep. 2017;7:45637.
Zhou Y, Yang G, Peng W, Zhang H, Peng Z, Ding N, Guo T, Cai Y, Deng Q, Chai X. Relationship between depression symptoms and different types of measures of obesity (BMI, SAD) in US Women. Behav Neurol. 2020;2020:9624106.
Zavala GA, Kolovos S, Chiarotto A, Bosmans JE, Campos-Ponce M, Rosado JL, Garcia OP. Association between obesity and depressive symptoms in Mexican population. Soc Psychiatry Psychiatr Epidemiol. 2018;53(6):639–46.
Ho RC, Niti M, Kua EH, Ng TP. Body mass index, waist circumference, waist-hip ratio and depressive symptoms in Chinese elderly: a population-based study. Int J Geriatr Psychiatry. 2008;23(4):401–8.
Geoffroy MC, Li L, Power C. Depressive symptoms and body mass index: co-morbidity and direction of association in a British birth cohort followed over 50 years. Psychol Med. 2014;44(12):2641–52.
Alberga AS, Pickering BJ, Alix Hayden K, Ball GD, Edwards A, Jelinski S, Nutter S, Oddie S, Sharma AM, Russell-Mayhew S. Weight bias reduction in health professionals: a systematic review. Clin Obes. 2016;6(3):175–88.
Xu Q, Anderson D, Lurie-Beck J. The relationship between abdominal obesity and depression in the general population: a systematic review and meta-analysis. Obes Res Clin Pract. 2011;5(4):e267–360.
Qiao T, Luo T, Pei H, Yimingniyazi B, Aili D, Aimudula A, Zhao H, Zhang H, Dai J, Wang D. Association between abdominal obesity indices and risk of cardiovascular events in Chinese populations with type 2 diabetes: a prospective cohort study. Cardiovasc Diabetol. 2022;21(1):225.
Nimptsch K, Konigorski S, Pischon T. Diagnosis of obesity and use of obesity biomarkers in science and clinical medicine. Metabolism. 2019;92:61–70.
Massimino M, Monea G, Marinaro G, Rubino M, Mancuso E, Mannino GC, Andreozzi F. The Triglycerides and Glucose (TyG) index is associated with 1-hour glucose levels during an OGTT. Int J Environ Res Public Health. 2022;20(1):787.
Locateli JC, Lopes WA, Simoes CF, de Oliveira GH, Oltramari K, Bim RH, de Souza Mendes VH, Remor JM, Lopera CA, Nardo Junior N. Triglyceride/glucose index is a reliable alternative marker for insulin resistance in South American overweight and obese children and adolescents. J Pediatr Endocrinol Metab. 2019;32(10):1163–70.
McGraw MB, Kohler LN, Shaibi GQ, Mandarino LJ, Coletta DK. A performance review of novel adiposity indices for assessing insulin resistance in a pediatric Latino population. Front Pediatr. 2022;10:1020901.
Bilgin Göçer D, Baş M, Çakır Biçer N, Hajhamidiasl L. Predicting metabolic syndrome by visceral adiposity index, body roundness index, dysfunctional adiposity index, lipid accumulation product index, and body shape index in adults. Nutr Hosp. 2022;39(4):794–802.
PubMed Google Scholar
Raimi TH, Dele-Ojo BF, Dada SA, Fadare JO, Ajayi DD, Ajayi EA, Ajayi OA. Triglyceride-Glucose index and related parameters predicted metabolic syndrome in Nigerians. Metab Syndr Relat Disord. 2021;19(2):76–82.
Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. 2014;43(1):61–8.
Radloff LS. The CES-D scale. Appl Psychol Meas. 2016;1(3):385–401.
Article Google Scholar
Fu H, Si L, Guo R. What is the optimal cut-off point of the 10-item center for epidemiologic studies depression scale for screening depression among Chinese individuals aged 45 and over? An exploration using latent profile analysis. Front Psychiatry. 2022;13:820777.
Boey KW. Cross-validation of a short form of the CES-D in Chinese elderly. Int J Geriatr Psychiatry. 1999;14(8):608–17.
Chen H, Mui AC. Factorial validity of the center for epidemiologic studies depression scale short form in older population in China. Int Psychogeriatr. 2014;26(1):49–57.
Arellano-Ruiz P, García-Hermoso A, García-Prieto JC, Sánchez-López M, Vizcaíno VM, Solera-Martínez M. Predictive ability of waist circumference and waist-to-height ratio for cardiometabolic risk screening among Spanish children. Nutrients. 2020;12(2):415.
Romero-Saldaña M, Fuentes-Jiménez FJ, Vaquero-Abellán M, Álvarez-Fernández C, Molina-Recio G, López-Miranda J. New non-invasive method for early detection of metabolic syndrome in the working population. Eur J Cardiovasc Nurs. 2016;15(7):549–58.
Zheng S, Shi S, Ren X, Han T, Li Y, Chen Y, Liu W, Hou PC, Hu Y. Triglyceride glucose-waist circumference, a novel and effective predictor of diabetes in first-degree relatives of type 2 diabetes patients: cross-sectional and prospective cohort study. J Transl Med. 2016;14(1):260.
Wan H, Wang Y, Xiang Q, Fang S, Chen Y, Chen C, Zhang W, Zhang H, Xia F, Wang N, et al. Associations between abdominal obesity indices and diabetic complications: Chinese visceral adiposity index and neck circumference. Cardiovasc Diabetol. 2020;19(1):118.
Ge Q, Li M, Xu Z, Qi Z, Zheng H, Cao Y, Huang H, Duan X, Zhuang X. Comparison of different obesity indices associated with type 2 diabetes mellitus among different sex and age groups in Nantong, China: a cross-section study. BMC Geriatr. 2022;22(1):20.
Duan Y, Zhang W, Li Z, Niu Y, Chen Y, Liu X, Dong Z, Zheng Y, Chen X, Feng Z, et al. Predictive ability of obesity- and lipid-related indicators for metabolic syndrome in relatively healthy Chinese adults. Front Endocrinol (Lausanne). 2022;13:1016581.
Ramírez-Vélez R, Pérez-Sousa M, González-Ruíz K, Cano-Gutierrez CA, Schmidt-RioValle J, Correa-Rodríguez M, Izquierdo M, Romero-García JA, Campos-Rodríguez AY, Triana-Reina HR, et al. Obesity- and lipid-related parameters in the identification of older adults with a high risk of prediabetes according to the American diabetes association: an analysis of the 2015 health, well-being, and aging study. Nutrients. 2019;11(11):2654.
Zhou BF. Effect of body mass index on all-cause mortality and incidence of cardiovascular diseases–report for meta-analysis of prospective studies open optimal cut-off points of body mass index in Chinese adults. Biomed Environ Sci. 2002;15(3):245–52.
Chen R, Ji L, Chen Y, Meng L. Weight-to-height ratio and body roundness index are superior indicators to assess cardio-metabolic risks in Chinese children and adolescents: compared with body mass index and a body shape index. Transl Pediatr. 2022;11(3):318–29.
Stefanescu A, Revilla L, Lopez T, Sanchez SE, Williams MA, Gelaye B. Using A Body Shape Index (ABSI) and Body Roundness Index (BRI) to predict risk of metabolic syndrome in Peruvian adults. J Int Med Res. 2020;48(1):300060519848854.
Jiang C-H, Zhu F, Qin T-T. Relationships between chronic diseases and depression among middle-aged and elderly people in China: a prospective study from CHARLS. Curr Med Sci. 2020;40(5):858–70.
Liu H, Yang X, Guo LL, Li JL, Xu G, Lei Y, Li X, Sun L, Yang L, Yuan T, et al. Frailty and incident depressive symptoms during short- and long-term follow-up period in the middle-aged and elderly: findings from the Chinese nationwide cohort study. Front Psychiatry. 2022;13:848849.
Zhang L, Li JL, Zhang LL, Guo LL, Li H, Li D. Association and interaction analysis of body mass index and triglycerides level with blood pressure in elderly individuals in China. Biomed Res Int. 2018;2018:8934534.
Zhang L, Li JL, Zhang LL, Guo LL, Li H, Li D. No association between C-reactive protein and depressive symptoms among the middle-aged and elderly in China: evidence from the china health and retirement longitudinal study. Medicine (Baltimore). 2018;97(38):e12352.
Zhang L, Li JL, Guo LL, Li H, Li D, Xu G. The interaction between serum uric acid and triglycerides level on blood pressure in middle-aged and elderly individuals in China: result from a large national cohort study. BMC Cardiovasc Disord. 2020;20(1):174.
Zhang L, Yang L, Wang C, Yuan T, Zhang D, Wei H, Li J, Lei Y, Sun L, Li X, et al. Mediator or moderator? The role of obesity in the association between age at menarche and blood pressure in middle-aged and elderly Chinese: a population-based cross-sectional study. BMJ Open. 2022;12(5):e051486.
Eusebi P. Diagnostic accuracy measures. Cerebrovasc Dis. 2013;36(4):267–72.
Simon GE, Ludman EJ, Linde JA, Operskalski BH, Ichikawa L, Rohde P, Finch EA, Jeffery RW. Association between obesity and depression in middle-aged women. Gen Hosp Psychiatry. 2008;30(1):32–9.
Zhao G, Ford ES, Li C, Tsai J, Dhingra S, Balluz LS. Waist circumference, abdominal obesity, and depression among overweight and obese U.S. Adults: national health and nutrition examination survey. BMC Psychiatry. 2011;11:130.
Hadi S, Momenan M, Cheraghpour K, Hafizi N, Pourjavidi N, Malekahmadi M, Foroughi M, Alipour M. Abdominal volume index: a predictive measure in relationship between depression/anxiety and obesity. Afr Health Sci. 2020;20(1):257–65.
Alshehri T, Boone S, de Mutsert R, Penninx B, Rosendaal F, le Cessie S, Milaneschi Y, Mook-Kanamori D. The association between overall and abdominal adiposity and depressive mood: a cross-sectional analysis in 6459 participants. Psychoneuroendocrinology. 2019;110:104429.
Sassarini DJ. Depression in midlife women. Maturitas. 2016;94:149–54.
Noble RE. Depression in women. Metabolism. 2005;54(5 Suppl 1):49–52.
Lu J, Xu X, Huang Y, Li T, Ma C, Xu G, Yin H, Xu X, Ma Y, Wang L, et al. Prevalence of depressive disorders and treatment in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2021;8(11):981–90.
Lotfi K, HassanzadehKeshteli A, Saneei P, Afshar H, Esmaillzadeh A, Adibi P. A body shape index and body roundness index in relation to anxiety, depression, and psychological distress in adults. Front Nutr. 2022;9:843155.
Luo H, Li J, Zhang Q, Cao P, Ren X, Fang A, Liao H, Liu L. Obesity and the onset of depressive symptoms among middle-aged and older adults in China: evidence from the CHARLS. BMC Public Health. 2018;18(1):909.
Yim G, Ahn Y, Cho J, Chang Y, Ryu S, Lim JY, Park HY. The “jolly fat” effect in middle-aged Korean women. J Womens Health (Larchmt). 2017;26(11):1236–43.
Crisp AH, McGuiness B. Jolly fat: relation between obesity and psychoneurosis in general population. BMJ. 1976;1(6000):7–9.
Andreyeva T, Puhl RM, Brownell KD. Changes in perceived weight discrimination among Americans, 1995–1996 through 2004–2006. Obesity. 2012;16(5):1129–34.
Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity. 2012;17(5):941–64.
Pearl RL, Puhl RM. Weight bias internalization and health: a systematic review. Obes Rev. 2018;19(8):1141–63.
Li ZB, Ho SY, Chan WM, Ho KS, Li MP, Leung GM, Lam TH. Obesity and depressive symptoms in Chinese elderly. Int J Geriatr Psychiatry. 2004;19(1):68–74.
Download references
Acknowledgements
We thank the members of the research as well as all participants for their contribution.
CHARLS was supported by the NSFC (70910107022, 71130002) and National Institute on Aging (R03-TW008358-01; R01-AG037031-03S1), and World Bank (7159234) and the Support Program for Outstanding Young Talents from the Universities and Colleges of Anhui Province for Lin Zhang(gxyqZD2021118).
Author information
Authors and affiliations.
Department of Graduate School, Wannan Medical College, 22 Wenchang West Road, Higher Education Park, Wuhu City, An Hui Province, People’s Republic of China
Xiaoyun Zhang, Ying Wang, Xue Yang, Yuqing Li, Jiaofeng Gui & Yujin Mei
Student Health Center, Wannan Medical College, 22 Wenchang West Road, Higher Education Park, Wuhu City, An Hui Province, People’s Republic of China
Haiyang Liu
Department of Surgical Nursing, School of Nursing, Jinzhou Medical University, No.40, Section 3, Songpo Road, Linghe District, Jinzhou City, Liaoning Province, People’s Republic of China
Lei-lei Guo
Department of Occupational and Environmental Health, Key Laboratory of Occupational Health and Safety for Coal Industry in Hebei Province, School of Public Health, North China University of Science and Technology, Tangshan, Hebei Province, People’s Republic of China
Obstetrics and Gynecology Nursing, School of Nursing, Wannan Medical College, 22 Wenchang West Road, Higher Education Park, Wuhu City, An Hui Province, People’s Republic of China
Yunxiao Lei & Ting Yuan
Department of Emergency and Critical Care Nursing, School of Nursing, Wannan Medical College, 22 Wenchang West Road, Higher Education Park, Wuhu City, An Hui Province, People’s Republic of China
Xiaoping Li & Lu Sun
Department of Internal Medicine Nursing, School of Nursing, Wannan Medical College, 22 Wenchang West Road, Higher Education Park, Wuhu City, An Hui Province, People’s Republic of China
Liu Yang, Congzhi Wang & Lin Zhang
Department of Pediatric Nursing, School of Nursing, Wannan Medical College, 22 Wenchang West Road, Higher Education Park, Wuhu City, An Hui Province, People’s Republic of China
Dongmei Zhang
Department of Surgical Nursing, School of Nursing, Wannan Medical College, 22 Wenchang West Road, Higher Education Park, Wuhu City, An Hui Province, People’s Republic of China
Jing Li & Mingming Liu
Rehabilitation Nursing, School of Nursing, Wannan Medical College, 22 Wenchang West Road, Higher Education Park, Wuhu City, An Hui Province, People’s Republic of China
You can also search for this author in PubMed Google Scholar
Contributions
Conceived and designed the research: LZ. Wrote the paper: X–y Z. Analyzed the data: X–y Z and LZ. Revised the paper: X–y Z, YW, XY, Y-q L, J-f G, Y-j M, LZ, H-y L, L-l G, J-l L, Y-x L, X-p L, LS, LY, TY, C-z W, D-m Z, JL, M-m L, and YH. The authors read and approved the final manuscript.
Corresponding author
Correspondence to Lin Zhang .
Ethics declarations
Ethics approval and consent to participate.
All data are openly published as microdata at http://opendata.pku.edu.cn/dataverse/CHARLS with no direct contact with all participants. Approval for this study was given by the medical ethics committee of Wannan medical college (approval number 2021–3).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Zhang, X., Wang, Y., Yang, X. et al. Obesity and lipid indices as predictors of depressive symptoms in middle-aged and elderly Chinese: insights from a nationwide cohort study. BMC Psychiatry 24 , 351 (2024). https://doi.org/10.1186/s12888-024-05806-z
Download citation
Received : 30 January 2023
Accepted : 02 May 2024
Published : 10 May 2024
DOI : https://doi.org/10.1186/s12888-024-05806-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Depressive symptoms
- Lipid-related index
- Anthropometric indicators
- Middle-aged and elderly
- Cohort study
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Some People Might Only Need a Colonoscopy Every 15 Years, Study Suggests
Pony Wang / Getty Images
Key Takeaways
- A new study suggests that some people who had negative findings on their first colonoscopy can safely wait 15 years, rather than 10, for a follow-up colonoscopy.
- The findings come from a population study of people in Sweden. Experts say the results may not be generalizable to the U.S.
- Extending the interval between colonoscopies may reduce costs and the potential harm of unnecessary complications.
U.S. guidelines recommend getting a colonoscopy every 10 years starting at age 45. However, a new study suggests healthy people with no family history of colorectal cancer can wait 15 years between colonoscopies if results from the last one were normal.
The study included more than 110,000 people in Sweden with no family history of colorectal cancer and a negative finding from their last colonoscopy. Each member of that group was matched with up to 18 control individuals of the same age and sex. The control group either never had a colonoscopy or had a positive finding during their last screening.
The findings indicate that extending the interval from 10 years to 15 after a negative colonoscopy results in missing only one or two early colorectal cancer cases and one colorectal cancer-related death per 1,000 people. This change could avoid 1,000 unnecessary colonoscopies.
“We found that individuals with a first negative colonoscopy experienced a significantly lower risk of colorectal cancer and death from colorectal cancer for 15 years compared to unscreened controls,” said Mahdi Fallah, MD, PhD , senior author of the study and head of the Risk Adapted Cancer Prevention Group at the German Cancer Research Center. “We expected a longer interval might miss more cancers, but the findings suggest the risk is minimal.”
However, some experts said these findings shouldn’t change how people approach colorectal cancer screening.
“I don’t think that you can make this generalizable to the remainder of the world, and especially to the U.S. population. The Swedish population is probably very different than the U.S. population—we’re such a mixture of so many different cultures and backgrounds,” Reezwana Chowdhury, MD , a gastroenterologist at Johns Hopkins Medicine, told Verywell.
“In their population, they showed that they didn’t miss that many additional cancers or cancer-related deaths, but I don’t see that being the same here,” she added.
Why Might Fewer Colonoscopies Benefit Patients?
Every time experts set or update a cancer screening guideline, they weigh the risks and benefits to individuals and the health system.
Colonoscopies can be a hassle to schedule, prepare, and pay for. And while colonoscopies are pretty safe procedures, they do carry some risks. The risk of perforation or bleeding during a colonoscopy is about four in 1,000.
Stretching the interval between colonoscopies could also save costs, which could be especially useful for certain underserved groups, said Robert Bresalier, MD, a professor of gastroenterology, hepatology, and nutrition at the University of Texas MD Anderson Cancer Center.
“[Colonoscopies] are associated with risk. If you could reduce the number over a lifetime, it would be more cost-effective and it would be safer,” Bresalier said.
In most parts of the world, people get a fecal occult blood test or other non-endoscopic test for colorectal cancer. If the test results are positive, they’re followed up with a colonoscopy. The U.S. is one of the few countries in which people typically get a colonoscopy first, largely because there are more gastroenterologists to perform the procedure here.
Limitations of the Study
While the Sweden study factored in participants’ age and sex, it excluded lots of other important information about their health status, Chowdhury said.
For instance, the study didn’t provide information about people’s comorbidities or lifestyle factors, like obesity and smoking history. Those factors could contribute to a person’s risk for colorectal cancer.
In the U.S., there are increasingly more young adults diagnosed with colorectal cancer. Chowdhury said she’s worried that encouraging fewer colonoscopies could lead some of those cases to be missed.
“To not do anything for 15 years makes me uncomfortable, even for the average person,” Chowdhury said.
Bresalier said there is a limit to how much someone can conclude from this study because it’s not a controlled trial. To do that, researchers would have had to give one group a colonoscopy every 10 years and another group a colonoscopy every 15 years and compare their outcomes. Doing so would take a long time and could be unethical since it’s well-known that colonoscopies effectively detect and prevent cancer.
Will U.S. Screening Guidelines Change?
Rather than indicate that the intervals between colonoscopies should be extended, Bresalier said the study strengthens the evidence that the 10-year interval is sufficient.
It usually takes 10 years for a polyp to develop from harmless to cancerous. A 2023 study showed that if someone has a normal colonoscopy, the likelihood of them developing colorectal cancer over 10 years is extremely small.
“I do think it’s reassuring and confirmatory of what we’ve found with studies and practice guidelines that a 10-year interval in a person with a normal index colonoscopy is okay,” Bresalier said. “People sometimes worry about the 10 years that it’s too long, and maybe we should do it sooner.”
Importantly, the researchers only tracked when study participants got colonoscopies, not when they took at-home stool tests , like Cologuard and FIT tests.
Stool tests can be useful for people who are at risk for anesthesia complications or those who don’t want an invasive procedure.
Fallah said that using cheaper, non-invasive stool-based tests could supplement a 15-year screening interval to help catch the one case per thousand that his team estimated an extended interval would miss.
However, it is only during a colonoscopy that a doctor can remove polyps to prevent colorectal cancer. While most of the current stool and blood tests are sensitive enough to pick up cancer, they aren’t very good at detecting pre-cancerous polyps.
Besides, Cologuard, a popular stool-based test in the U.S., has a false positive rate of up to 13%. A positive result from a fecal test may lead to CT scans and other expensive tests that could require more resources than an initial colonoscopy might have, Bresalier said.
“Doing anything is better than doing nothing,” Bresalier said. “The question is, how much tolerance do you have for a test that is not going to pick up every cancer and every polyp?”
It’s not out of the question that an extended interval is safe or that non-invasive tests could one day make for an adequate colonoscopy substitute, Bresalier said. For now, though, the research isn’t yet robust enough to change U.S. guidelines.
“A 15-year interval may, in the end, be a reasonable thing to do. But right now, we can feel comfortable with the 10-year interval and look to the future to see maybe a longer interval might be reasonable,” Bresalier said.
What This Means For You
People at average risk for colorectal cancer should start getting screened at age 45. Younger people who have a family history or a history of inflammatory bowel disease may get screened younger.
Liang Q, Mukama T, Sundquist K, et al. Longer interval between first colonoscopy with negative findings for colorectal cancer and repeat colonoscopy . JAMA Oncol. Published online May 2, 2024. doi:10.1001/jamaoncol.2024.0827
Lin JS, Piper MA, Perdue LA, et al. Screening for colorectal cancer: updated evidence report and systematic review for the US Preventive Services Task Force . JAMA . June 21, 2016;315(23):2576-94. doi:10.1001/jama.2016.3332
Heisser T, Kretschmann J, Hagen B, Niedermaier T, Hoffmeister M, Brenner H. Prevalence of colorectal neoplasia 10 or more years after a negative screening colonoscopy in 120 000 repeated screening colonoscopies . JAMA Intern Med . 2023;183(3):183-190. doi:10.1001/jamainternmed.2022.6215
Cotter TG, Burger KN, Devens ME, et al. Long-term follow-up of patients having false-positive multitarget stool DNA tests after negative screening colonoscopy: the LONG-HAUL Cohort Study . Cancer Epidemiol Biomarkers Prev . 2017;26(4):614-621. doi:10.1158/1055-9965.EPI-16-0800
By Claire Bugos Bugos is a senior news reporter at Verywell Health. She holds a bachelor's degree in journalism from Northwestern University.
Safety and Efficacy of Bone-Marrow Aspirate Concentrate in Hip Osteoarthritis: A Systematic Review of Current Clinical Evidence
- Review Article
- Published: 17 May 2024
Cite this article

- Sushma Chandrashekar 1 ,
- Madhan Jeyaraman ORCID: orcid.org/0000-0002-9045-9493 2 , 3 , 4 ,
- Prabu Mounissamy 5 ,
- Naveen Jeyaraman ORCID: orcid.org/0000-0002-4362-3326 2 , 3 ,
- Manish Khanna ORCID: orcid.org/0000-0002-2890-869X 3 , 6 &
- Ashim Gupta ORCID: orcid.org/0000-0003-1224-2755 3 , 4 , 7 , 8 , 9
Introduction
Hip osteoarthritis (OA) is one of the leading causes of disability and morbidity worldwide. It is estimated to affect 9.2% individuals globally with age over 45 years. Conventional treatment modalities have limitations and side-effects. To overcome these limitations, over the last decade, there has been an increased interest in the use of orthobiologics derived from autologous sources including platelet-rich plasma (PRP), bone-marrow aspirate concentrate (BMAC) and adipose tissue derived formulations. This review qualitatively presents the in-vitro, pre-clinical, clinical and on-going clinical studies exploring the safety and efficacy of BMAC for management of hip OA.
Materials and methods
The electronic database search was done through PubMed, Embase, Web of Science, Scopus, ProQuest and Google Scholar till February 2024. The search terms used were “osteoarthritis” OR “hip osteoarthritis” OR “orthobiologics” OR “efficacy or use of orthobiologic treatment” OR “bone-marrow concentrate” OR “bone-marrow aspirate concentrate”, AND “BMAC”. The inclusion criteria were clinical studies of any level of evidence written in the English language, published till February 2024, evaluating the safety and efficacy of intra-articular administration of BMAC for the management of hip OA.
A total of 5 studies were included in this review for qualitative data synthesis. The total number of patients who participated in the study was 182, ranging from 4 to 112 in a single study. No adverse events were reported throughout the duration of the study. In addition, intra-articular administration of BMAC led to reduced pain, and improved function and overall quality of life (QoL).
The results from this review demonstrated that administration of BMAC is safe and potentially efficacious in terms of reducing pain, improving function and overall QoL of patients with hip OA in short- and mid-term average follow-up based on the included studies. Nonetheless, more adequately powered, multi-center, prospective, double-blind, non-randomized and randomized controlled trials with long-term follow-up are warranted to establish long-term safety and efficacy of BMAC for management of hip OA and justify its routine clinical use.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Data Availability
All data is contained within the manuscript.
Long, H., Liu, Q., Yin, H., Wang, K., Diao, N., Zhang, Y., et al. (2022). Prevalence trends of site-specific osteoarthritis from 1990 to 2019: Findings from the global burden of disease study 2019. Arthritis & Rheumatology, 74 (7), 1172–1183.
Article Google Scholar
Fan, Z., Yan, L., Liu, H., Li, X., Fan, K., Liu, Q., et al. (2023). The prevalence of hip osteoarthritis: A systematic review and meta-analysis. Arthritis Research & Therapy, 25 (1), 51.
Turkiewicz, A., Petersson, I. F., Björk, J., Hawker, G., Dahlberg, L. E., Lohmander, L. S., et al. (2014). Current and future impact of osteoarthritis on health care: A population-based study with projections to year 2032. Osteoarthritis and cartilage, 22 (11), 1826–1832.
Article CAS PubMed Google Scholar
Steinmetz, J. D., Culbreth, G. T., Haile, L. M., Rafferty, Q., Lo, J., Fukutaki, K. G., et al. (2023). Global, regional, and national burden of osteoarthritis, 1990–2020 and projections to 2050: A systematic analysis for the global burden of disease study 2021. The Lancet Rheumatology, 5 (9), e508–e522. https://doi.org/10.1016/S2665-9913(23)00163-7
Neogi, T. (2013). The epidemiology and impact of pain in osteoarthritis. Osteoarthritis and cartilage, 21 (9), 1145–1153.
Article CAS PubMed PubMed Central Google Scholar
Hunter, D. J., March, L., & Chew, M. (2020). Osteoarthritis in 2020 and beyond: A lancet commission. The Lancet, 396 (10264), 1711–1712. https://doi.org/10.1016/S0140-6736(20)32230-3
Abbafati, C., Abbas, K. M., Abbasi-Kangevari, M., Abd-Allah, F., Abdelalim, A., Abdollahi, M., et al. (2020). Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the global burden of disease study 2019. The Lancet, 396 (10258), 1204–1222. https://doi.org/10.1016/S0140-6736(20)30925-9
da Costa, B. R., Reichenbach, S., Keller, N., Nartey, L., Wandel, S., Jüni, P., et al. (2017). Effectiveness of non-steroidal anti-inflammatory drugs for the treatment of pain in knee and hip osteoarthritis: A network meta-analysis. The Lancet, 390 (10090), e21–e33. https://doi.org/10.1016/S0140-6736(17)31744-0
Leite, V. F., Daud, A. J. E., & Buehler, A. M. (2018). Viscosupplementation for hip osteoarthritis: A systematic review and meta-analysis of the efficacy on pain and disability, and the occurrence of adverse events. Archives of Physical Medicine and Rehabilitation, 99 (3), 574–583. https://doi.org/10.1016/J.APMR.2017.07.010
Article PubMed Google Scholar
Pereira, L. C., Kerr, J., & Jolles, B. M. (2016). Intra-articular steroid injection for osteoarthritis of the hip prior to total hip arthroplasty: Is it safe? A systematic review. The bone & joint journal, 98 (8), 1027–1035.
Filardo, G., Kon, E., Longo, U. G., Madry, H., Marchettini, P., Marmotti, A., et al. (2016). Non-surgical treatments for the management of early osteoarthritis. Knee Surgery, Sports Traumatology, Arthroscopy, 24 , 1775–1785.
Kraeutler, M. J., Chahla, J., LaPrade, R. F., & Pascual-Garrido, C. (2017). Biologic options for articular cartilage wear (platelet-rich plasma, stem cells, bone-marrow aspirate concentrate). Clinics in Sports Medicine, 36 (3), 457–468.
Huddleston, H. P., Maheshwer, B., Wong, S. E., Chahla, J., Cole, B. J., & Yanke, A. B. (2020). An update on the use of orthobiologics: use of biologics for osteoarthritis. Operative Techniques in Sports Medicine . https://doi.org/10.1016/j.otsm.2020.150759
Jayaram, P., Ikpeama, U., Rothenberg, J. B., & Malanga, G. A. (2019). Bone-marrow-derived and adipose-derived mesenchymal stem cell therapy in primary knee osteoarthritis: a narrative review. PM&R, 11 (2), 177–191.
Han, F., Wang, J., Ding, L., Hu, Y., Li, W., Yuan, Z., et al. (2020). Tissue engineering and regenerative medicine: Achievements, future, and sustainability in Asia. Frontiers in Bioengineering and Biotechnology, 8 , 83. https://doi.org/10.3389/fbioe.2020.00083
Article PubMed PubMed Central Google Scholar
Abd, R. H., Bin, R., Chew, D., Kazezian, Z., & Bull, A. M. J. (2021). Autologous protein solution: A promising solution for osteoarthritis? EFORT Open Reviews, 6 (9), 716–726.
Hernigou, P., & Beaujean, F. (1993). Bone-marrow activity in the upper femoral extremity in avascular osteonecrosis. Rhum (Eng Ed), 60 , 610.
Google Scholar
Holton J., Imam M., Ward J., & Snow M. (2016). The basic science of bone-marrow aspirate concentrate in chondral injuries. Orthopedic Reviews, 8 (3), 6659. https://doi.org/10.4081/or.2016.6659
Imam, M. A., Mahmoud, S. S. S., Holton, J., Abouelmaati, D., Elsherbini, Y., & Snow, M. (2017). A systematic review of the concept and clinical applications of bone-marrow aspirate concentrate in orthopaedics. SICOT-J . https://doi.org/10.1051/SICOTJ/2017007
Filardo, G., Perdisa, F., Roffi, A., Marcacci, M., & Kon, E. (2016). Stem cells in articular cartilage regeneration. Journal of Orthopaedic Surgery and Research . https://doi.org/10.1186/S13018-016-0378-X
Lee, D. H., Ryu, K. J., Kim, J. W., Kang, K. C., & Choi, Y. R. (2014). Bone-marrow aspirate concentrate and platelet-rich plasma enhanced bone healing in distraction osteogenesis of the tibia. Clinical Orthopaedics and Related Research, 472 , 3789–3797.
Jager, M., Jelinek, E. M., Wess, K. M., Scharfstadt, A., Jacobson, M., Kevy, S., V, et al. (2009). Bone-marrow concentrate: A novel strategy for bone defect treatment. Current stem cell research & therapy, 4 (1), 34–43.
Muschler, G. F., Nitto, H., Matsukura, Y., Boehm, C., Valdevit, A., Kambic, H., et al. (2003). Spine fusion using cell matrix composites enriched in bone-marrow-derived cells. Clinical orthopaedics and related research, 407 , 102.
Southworth, T. M., Naveen, N. B., Nwachukwu, B. U., Cole, B. J., & Frank, R. M. (2019). Orthobiologics for focal articular cartilage defects. Clinics in sports medicine, 38 (1), 109–122. https://doi.org/10.1016/J.CSM.2018.09.001
Chahla, J., Alland, J. A., & Verma, N. N. (2018). Bone-marrow aspirate concentrate for orthopaedic use. Orthopedic nursing, 37 (6), 379–381. https://doi.org/10.1097/NOR.0000000000000502
Herberts, C. A., Kwa, M. S. G., & Hermsen, H. P. H. (2011). Risk factors in the development of stem cell therapy. Journal of translational medicine, 9 , 1–14.
Song, L. I. N., & Tuan, R. S. (2004). Transdifferentiation potential of human mesenchymal stem cells derived from bone-marrow. The FASEB Journal, 18 (9), 980–982.
Turner, L., & Knoepfler, P. (2016). Selling stem cells in the USA: Assessing the direct-to-consumer industry. Cell Stem Cell, 19 (2), 154–157.
Sullivan, S. W., Aladesuru, O. M., Ranawat, A. S., & Nwachukwu, B. U. (2021). The use of biologics to improve patient-reported outcomes in hip preservation. Journal of Hip Preservation Surgery, 8 (1), 3–13.
Tsitsilianos, N., Shirazi, Z., Lu, J., & Singh, J. R. (2022). Bone-marrow aspirate injection for osteoarthritis of the hip. A pilot study. Interventional Pain Medicine, 1 (4), 100163. https://doi.org/10.1016/J.INPM.2022.100163
Burnham, R., Smith, A., & Hart, D. (2021). The safety and effectiveness of bone-marrow concentrate injection for knee and hip osteoarthritis: a Canadian cohort. Regenerative Medicine, 16 (7), 619–628. https://doi.org/10.2217/RME-2021-0001
Whitney, K. E., Briggs, K. K., Chamness, C., Bolia, I. K., Huard, J., Philippon, M. J., et al. (2020). Bone-marrow concentrate injection treatment improves short-term outcomes in symptomatic hip osteoarthritis patients: A pilot study. Orthopaedic Journal of Sports Medicine, 8 (12), 1–7. https://doi.org/10.1177/2325967120966162
Rodriguez-Fontan, F., Piuzzi, N. S., Kraeutler, M. J., & Pascual-Garrido, C. (2018). Early clinical outcomes of intra-articular injections of bone-marrow aspirate concentrate for the treatment of early osteoarthritis of the hip and knee: A cohort study. PM and R, 10 (12), 1353–1359. https://doi.org/10.1016/j.pmrj.2018.05.016
Darrow, M., Shaw, B., Darrow, B., & Wisz, S. (2018). Short-term outcomes of treatment of hip osteoarthritis with 4 bone-marrow concentrate injections: A case series. Clinical Medicine Insights: Case Reports . https://doi.org/10.1177/1179547618791574
Fortier, L. A., Potter, H. G., Rickey, E. J., Schnabel, L. V., Foo, L. F., Chong, L. R., et al. (2010). Concentrated bone-marrow aspirate improves full-thickness cartilage repair compared with microfracture in the equine model. JBJS, 92 (10), 1927–1937.
Johnson R. G. (2014). Bone-marrow concentrate with allograft equivalent to autograft in lumbar fusions. Spine (Phila Pa 1976), 39 (9), 695-700. https://doi.org/10.1097/BRS.0000000000000254.
Filardo, G., Madry, H., Jelic, M., Roffi, A., Cucchiarini, M., & Kon, E. (2013). Mesenchymal stem cells for the treatment of cartilage lesions: From preclinical findings to clinical application in orthopaedics. Knee surgery, sports traumatology, arthroscopy, 21 , 1717–1729.
Hyer, C. F., Berlet, G. C., Bussewitz, B. W., Hankins, T., Ziegler, H. L., & Philbin, T. M. (2013). Quantitative assessment of the yield of osteoblastic connective tissue progenitors in bone-marrow aspirate from the iliac crest, tibia, and calcaneus. JBJS, 95 (14), 1312–1316.
Marx R. E., & Tursun R. (2013). A qualitative and quantitative analysis of autologous human multipotent adult stem cells derived from three anatomic areas by marrow aspiration: tibia, anterior ilium, and posterior ilium. Int J Oral Maxillofac Implants, 28 (5), e290-4. https://doi.org/10.11607/jomi.te10.
Hernigou, P. H., Poignard, A., Beaujean, F., & Rouard, H. (2005). Percutaneous autologous bone-marrow grafting for nonunions: Influence of the number and concentration of progenitor cells. JBJS, 87 (7), 1430–1437.
Hernigou, J., Picard, L., Alves, A., Silvera, J., Homma, Y., & Hernigou, P. (2014). Understanding bone safety zones during bone-marrow aspiration from the iliac crest: The sector rule. International orthopaedics, 38 , 2377–2384.
Hernigou, P., Homma, Y., Flouzat, L. C. H., Poignard, A., Allain, J., Chevallier, N., et al. (2013). Benefits of small volume and small syringe for bone-marrow aspirations of mesenchymal stem cells. International orthopaedics, 37 , 2279–2287.
Pittenger, M. F., Mackay, A. M., Beck, S. C., Jaiswal, R. K., Douglas, R., Mosca, J. D., et al. (1999). Multilineage potential of adult human mesenchymal stem cells. Science, 284 (5411), 143–147.
Themistocleous G. S., Chloros G. D., Kyrantzoulis I. M., Georgokostas I. A., Themistocleous M. S., Papagelopoulos P. J., et al. (2018). Effectiveness of a single intra-articular bone-marrow aspirate concentrate (BMAC) injection in patients with grade 3 and 4 knee osteoarthritis. Heliyon, 4 (10), e00871. https://doi.org/10.1016/j.heliyon.2018.e00871.
Fortier, L. A., Strauss, E. J., Shepard, D. O., Becktell, L., & Kennedy, J. G. (2019). Biological effects of bone-marrow concentrate in knee pathologies. The journal of knee surgery, 32 (01), 2–8.
Chahla, J., Dean, C. S., Moatshe, G., Pascual-Garrido, C., Serra, C. R., & LaPrade, R. F. (2016). Concentrated bone-marrow aspirate for the treatment of chondral injuries and osteoarthritis of the knee: A systematic review of outcomes. Orthopaedic journal of sports medicine, 4 (1), 2325967115625481.
Shapiro, S. A., Arthurs, J. R., Heckman, M. G., Bestic, J. M., Kazmerchak, S. E., Diehl, N. N., et al. (2019). Quantitative T2 MRI mapping and 12-month follow-up in a randomized, blinded, placebo controlled trial of bone-marrow aspiration and concentration for osteoarthritis of the knees. Cartilage, 10 (4), 432–443.
Shaw, B., Darrow, M., & Derian, A. (2018). Short-term outcomes in treatment of knee osteoarthritis with 4 bone-marrow concentrate injections. Clinical Medicine Insights: Arthritis and Musculoskeletal Disorders, 11 , 1179544118781080.
PubMed PubMed Central Google Scholar
Centeno, C. J., Al-Sayegh, H., Bashir, J., Goodyear, S., & Freeman, M. D. (2015). A dose response analysis of a specific bone-marrow concentrate treatment protocol for knee osteoarthritis. BMC Musculoskeletal Disorders, 16 , 1–8.
Centeno C. J., Al-Sayegh H., Bashir J., Goodyear S., & Freeman M. D. (2015). A prospective multi-site registry study of a specific protocol of autologous bone-marrow concentrate for the treatment of shoulder rotator cuff tears and osteoarthritis. Journal of Pain Research, 8, 269–276. https://doi.org/10.2147/JPR.S80872.
Darrow, M., Shaw, B., Schmidt, N., Boeger, G., & Budgett, S. (2019). Treatment of shoulder osteoarthritis and rotator cuff tears with bone-marrow concentrate and whole bone-marrow injections. Cogent Medicine, 6 (1), 1628883.
Sampson, S., Smith, J., Vincent, H., Aufiero, D., Zall, M., & Botto-van-Bemden, A. (2016). Intra-articular bone-marrow concentrate injection protocol: Short-term efficacy in osteoarthritis. Regenerative medicine, 11 (6), 511–520.
Centeno, C. J., Pitts, J. A., Al-Sayegh, H., & Freeman, M. D. (2014). Efficacy and safety of bone-marrow concentrate for osteoarthritis of the hip; treatment registry results for 196 patients. J Stem Cell Res Ther, 4 (10), 242.
Bain, B. J. (2003). Bone-marrow biopsy morbidity and mortality. British journal of haematology, 121 (6), 949–951.
Download references
Author information
Authors and affiliations.
Fellow in Orthopaedic Rheumatology, Dr RML National Law University, Lucknow, 226010, Uttar Pradesh, India
Sushma Chandrashekar
Department of Orthopaedics, ACS Medical College and Hospital, Dr MGR Educational and Research Institute, Chennai, 600077, Tamil Nadu, India
Madhan Jeyaraman & Naveen Jeyaraman
Indian Stem Cell Study Group (ISCSG) Association, Lucknow, 226010, Uttar Pradesh, India
Madhan Jeyaraman, Naveen Jeyaraman, Manish Khanna & Ashim Gupta
Department of Orthopaedics, South Texas Orthopaedic Research Institute (STORI Inc.), Laredo, TX, 78045, USA
Madhan Jeyaraman & Ashim Gupta
Department of Orthopaedics, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, 605006, India
Prabu Mounissamy
Department of Orthopaedics, Dr KNS Mayo Institute of Medical Sciences, Lucknow, 225001, Uttar Pradesh, India
Manish Khanna
Regenerative Orthopaedics, Noida, 201301, Uttar Pradesh, India
Ashim Gupta
Future Biologics, Lawrenceville, GA, 30043, USA
BioIntegrate, Lawrenceville, GA, 30043, USA
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Naveen Jeyaraman .
Ethics declarations
Conflict of interest .
No conflict of interest.
Ethical standard statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
For this type of study informed consent is not required.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Chandrashekar, S., Jeyaraman, M., Mounissamy, P. et al. Safety and Efficacy of Bone-Marrow Aspirate Concentrate in Hip Osteoarthritis: A Systematic Review of Current Clinical Evidence. JOIO (2024). https://doi.org/10.1007/s43465-024-01183-7
Download citation
Received : 30 March 2024
Accepted : 04 May 2024
Published : 17 May 2024
DOI : https://doi.org/10.1007/s43465-024-01183-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Orthobiologics
- Hip osteoarthritis
- Bone-marrow aspirate concentrate
- Regenerative medicine
- Find a journal
- Publish with us
- Track your research

Short-Term Energy Outlook
Release Date: May. 7, 2024 | Forecast Completed: May. 2, 2024 | Next Release Date: Jun. 11, 2024 | Full Report | Text Only | All Tables | All Figures
- Global oil markets
- Petroleum products
- Natural gas
- Electricity, coal, and renewables
- Economy, weather, and CO 2
- STEO Data browser
- Real Prices Viewer
- Data series changes
- Supplements
Release Date: May 14, 2024
STEO Perspectives: How might gasoline prices change if U.S. refiners face production and distribution limitations?
Analysis summary and key findings.
Refinery closures and increased gasoline production costs have increased gasoline prices, crack spreads , and household expenditures for gasoline over the past few summers. In our base case, we forecast U.S. retail gasoline prices will average about $3.70 per gallon (gal) for the summer driving season, which runs from May to September when the United States will have 3%, or 620,000 barrels per day (b/d) less refinery capacity compared with the 2019 peak. Falling refinery capacity and rising production costs suggest uncertainty and volatility in the gasoline supply chain could re-emerge this year.
Gasoline prices are determined by crude oil prices, refinery production costs, distribution and marketing costs, and taxes. These factors can differ by region or state in the United States.
In this report, we analyze retail gasoline prices in our High Refining Cost scenario where gasoline yields and production fall to recent historical lows because of constraints on the production of high-octane blending components, which are necessary for a gasoline blend stock that complies with summer fuel specifications . We also vary retail gasoline price premiums in two populous and high gasoline-consuming regions in the United States—the East Coast (PADD 1) and the West Coast (PADD 5)—and assume tight market conditions will push up regional prices to attract supplies. By extrapolating recent historical examples to the rest of 2024, we model the effects on retail gasoline prices and consumption heading into the summer driving season. We compare this scenario with our baseline case, which we published as our May 2024 Short-Term Energy Outlook (STEO) forecast.
In the High Refining Cost scenario, U.S. regular grade retail gasoline prices in the summer average just under 10 cents/gal higher than in our base case.
Scenario design
We used the May 2024 STEO regular grade retail gasoline price as our base case, using our forecasts of Brent crude oil price, global oil production, global oil consumption, U.S. refinery production, and wholesale petroleum product margins.
In our May STEO, we forecast the Brent crude oil spot price to remain near its April average of $90 per barrel (b) until October 2024. Similarly, we forecast the U.S. average regular grade retail gasoline prices to increase to $3.70/gal by June 2024 but fall to $3.40/gal by the end of 2024. We expect global inventory withdrawals in the second quarter of 2024, followed by mostly balanced markets in the second half of 2024 through 2025.
U.S. gasoline production is the result of refiners’ gasoline yield from crude oil and unfinished oil inputs to refineries. Our base case forecasts U.S. refinery utilization will be above the five-year average (2019-2023) this summer and near an operationally safe maximum rate. Gasoline yields will also be at or near average rates. We do not forecast refinery utilization or gasoline production by region.
Retail gasoline price spreads between the East Coast and the Gulf Coast vary seasonally and are responsive to local supply and demand conditions. In January, the East Coast premium to the Gulf Coast was 30% higher than the five-year average. In our base case, we forecast the premium to decline from the January high to an average of about 14% above the five-year average for the remainder of 2024. The highest premium in our base case is 25% in both May and June of 2024.
Similarly, West Coast retail gasoline prices are higher than those in the rest of the country and can develop wide price premiums, depending on local supply and demand conditions. As with the East Coast, the West Coast premium to the Gulf Coast has been increasing over the last five years. In April, the West Coast gasoline retail price premium to the Gulf Coast was $1.57/gal, 42% higher than the five-year average for April. In our base case, we estimate that this price premium will decrease, resulting in an annual average price premium that is 21% above the five-year average, for the remainder of 2024.
High Refining Cost scenario
Structural changes in U.S. refining since 2019 have increased production costs for summer-grade gasoline , which meets specifications for octane, volatility, and emissions. Lower refinery capacity, secondary conversion capacity , and tighter sulfur standards have all increased production costs. In this scenario, we analyzed U.S. gasoline prices if U.S. refineries produce less gasoline because of difficulties producing enough high-octane, low-sulfur gasoline blending components. Our analysis involved reducing our U.S. gasoline production yield from our base case to match the lowest motor gasoline yields during the past five years.
We calculate refinery motor gasoline yield by determining how much motor gasoline is produced relative to total refinery inputs of crude oil and unfinished oils. We account for refinery production of motor gasoline from petroleum by subtracting net inputs of fuel ethanol , butanes , and pentanes plus .
After reducing refinery production of gasoline to adjust the yield of gasoline to the five-year low through the summer, we analyzed the impact of this reduced production on gasoline wholesale prices, assuming a short-term price elasticity of demand equal to 0.3 . Price elasticity of demand reflects a percentage change in quantity demanded (from consumers) or quantity supplied (from producers) given a percentage change in price. Our assumption is based partially on academic studies of price elasticity and partially on observed wholesale gasoline price changes following gasoline production disruptions from unplanned refinery outages.
In this scenario, we forecast 1% less U.S. gasoline production than the base case this summer and about 2% less during the summer driving season (May—September). This decrease contributes to about a $0.04/gal increase in the U.S. average wholesale gasoline price forecast during the summer period. This price increase flows through to all U.S. regions, including the Gulf Coast.
We also varied regional prices in response to uncertainty regarding lower regional gasoline production. We assumed that lower supply results in higher prices in demand centers to attract supplies from other U.S. regions or imports. We analyzed what would happen to the U.S. average retail gasoline price if conditions in each region were tight enough that they pushed the relative price premiums higher.
The effects of higher octane costs and lower regional gasoline production result in tight market conditions on the East Coast and West Coast. On the East Coast, we analyze market conditions by increasing the price premium compared with the U.S. Gulf Coast to 30% above the five-year average for the rest of 2024, which aligns with the year-to-date high in January 2024. We analyze the West Coast by increasing the price premium to the Gulf Coast to 42% above the five-year average, which aligns with the year-to-date high in April 2024. These adjustments in this scenario contrast with the base case, where we forecast these spreads to fall over the summer. Gulf Coast prices in the High Refining Cost scenario increased slightly as a result of higher gasoline wholesale prices but are unchanged as a result of any additional regional factors.
Our High Refining Cost scenario targets four key changes in the refining industry and gasoline markets over the past five years:
- Gasoline specifications: Changing specifications, including tighter sulfur specifications since 2020, have increased prices for premium grade 93 octane gasoline blend stock relative to regular grade 87 octane gasoline blend stock. The widening spread reflects increasing costs of certain gasoline components that increase octane content while keeping Reid vapor pressure (RVP) and sulfur content low. Changing one specification often affects others, creating operational limitations. For example, refiners can reduce the sulfur content of gasoline components by hydrotreating—binding the sulfur in gasoline components with hydrogen—but doing so reduces the octane of the gasoline. In the STEO, our estimate of the octane price is reflected in the difference between the U.S. average retail price for regular gasoline and the U.S. average retail price for all grades.
- Reduced East Coast refinery capacity: When the Philadelphia Energy Solutions (PES) refinery—at the time the largest refiner on the East Coast—closed in summer 2019, the East Coast lost significant refinery capacity. Although the region still has some refinery capacity, petroleum product supply mostly comes by pipeline from the U.S. Gulf Coast, with growing pipeline volumes from the Midwest (PADD 2). The East Coast also imports gasoline from Canada and Europe. Significant pipeline infrastructure exists to supply the East Coast with petroleum products from the U.S. Gulf Coast, and additional volumes can be shipped over water to supply states like Florida. However, reduced refining capacity on the East Coast and increasing refining capacity on the Gulf Coast with no increase in pipeline capacity have widened price differentials between the two regions. In the STEO, we estimate the difference in price between the two regions by comparing regular-grade retail prices in the East Coast and Gulf Coast. Following the loss of PES, the price spread between the East Coast and the Gulf Coast has been increasing over the past five years. In 2019, East Coast retail prices ranged from $0.19/gal to $0.31/gal more than the Gulf Coast, and in 2023, the range increased from $0.22/gal to $0.48/gal.
- Reduced West Coast refinery capacity: When Marathon’s Martinez refinery closed in 2020 and petroleum refining operations at the Phillips 66 Rodeo refinery ended earlier this year, West Coast refinery capacity was reduced. Unlike the East Coast, the West Coast has historically been more isolated from other U.S. regional markets. It has very limited pipeline capacity connecting it to refining capacity on the U.S. Gulf Coast and faces higher costs associated with receiving waterborne gasoline from elsewhere in the United States because of geographic constraints. Supply constraints on the West Coast present a significant risk for heightened gasoline prices in the region that are further elevated by structural factors such as taxes, California’s unique CARB-gasoline formulation , and state Low Carbon Fuel Standards.
- Additional Gulf Coast refining capacity: The U.S. Gulf Coast added some refinery capacity in 2023 but it was less than the toal capacity lost due to closures on the East and West Coasts. Transportation costs and other constraints mean geographic changes in the refinery fleet can reduce refined product supply in some regions of the country that cannot be easily met from refinery expansions elsewhere. These transportation constraints can make gasoline imports more competitive than increasing transfers from elsewhere in the United States to meet marginal increases in demand. Furthermore, each refinery produces a unique yield of motor gasoline, distillate fuel oil, jet fuel, and other products based on its configuration, secondary unit capacity, and the specific crude oil grades it processes. As a result, a refinery closing in one part of the country and added capacity at another refinery somewhere else are unlikely to balance out, contributing to marginal changes in the broader yield structure of the U.S. refining fleet. Although each refinery has some ability to adjust its yield in response to price signals, this ability is significantly constrained by the refinery’s equipment and configuration and the crude oil grades available.
Key assumptions
Refiners face production limitations. In the High Refinery Cost scenario, we assume that limitations on refiners’ ability to produce high-octane blend components will reduce overall gasoline production and yield. Reduced gasoline production will widen crack spreads for gasoline and increase retail gasoline prices. We also assume that difficulty producing more octane will increase prices for premium-grade gasoline relative to regular grade.
Crude oil inputs to refineries do not change. We assume no changes to refinery crude oil net input volumes processed in the High Refinery Cost scenario compared with our base forecast, partially because in our base case, our U.S. refinery utilization forecast indicates that refiners will operate at above-average run rates. Although higher gasoline prices may encourage increased crude oil inputs to refineries, we assume refiners would be unable to increase crude oil purchases and arrange new supplies in time to increase runs. In addition, any increase in crude oil inputs presents challenges with overproducing lower-value gasoline components (such as low octane, straight run naphtha ), putting conflicting pressure on refiners.
Changes in marginal transportation costs are reflected in retail price spreads. We assume that the difference in regional average retail price spreads reflect the cost of transporting higher volumes of motor gasoline from one region to another. As lower-cost transportation capacity, like petroleum product pipelines, is filled, we assume higher inter-region retail price spreads reflect costs associated with acquiring more expensive gasoline cargoes, such as transfers by barge, or imports. The spreads also reflect more fixed elements such as state and local taxes.
No additional changes to gasoline consumption. We kept our modeled price elasticity of demand the same in both cases, resulting in a small decline in gasoline consumption because of higher retail prices in the High Refining Coast scenario. In the STEO, we do not forecast U.S. gasoline consumption by region.
Crude oil prices are the same as in the base case. Crude oil accounts for the largest share of the U.S. retail gasoline price, so changes in crude oil prices can contribute to large changes in gasoline prices. Crude oil prices can change in response to various factors, including global macroeconomic conditions, increases or decreases in crude oil production, or geopolitical risks, among others. However, we do not vary crude oil prices in the High Refinery Cost scenario compared with the base case because our purpose was to isolate the effects of refinery operations on fuel prices.
No adjustments to Midwest or Rocky Mountain price spreads. We made no additional changes to gasoline retail price spreads for the Midwest and Rocky Mountain regions, both of which meet a larger share of their internal gasoline consumption from local refinery production.
The High Refinery Cost scenario changes to gasoline production, wholesale prices, and retail price spreads on the East Coast and West Coast increased U.S. average regular grade retail gasoline prices compared with the base case. Retail gasoline prices increased by about $0.10/gal in this scenario compared with the base case. Total U.S. gasoline consumption is affected slightly because of the higher prices, reducing consumption by about 5,000 b/d compared with the base case.
Refinery and gasoline production limitations result in a U.S. average regular grade retail gasoline price of $3.80/gal in the summer, compared with $3.70/gal in the base case.
Just like the U.S. average, retail gasoline prices in the East Coast are also $0.10/gal higher in the High Refinery Cost scenario. Prices remain just below $3.70/gal at their highest point in August in our High Refinery Cost scenario. Gulf Coast gasoline prices remain almost unchanged (increasing by less than $0.05/gal) in response to reduced production, while West Coast gasoline prices increase by nearly $0.20/gal compared with the base case. The stronger impact on the West Coast pushes prices to more than $5.00/gal for several months in our scenario.
The limited impact on gasoline wholesale prices alone compared with the base case suggests that there would not necessarily be a call for additional, higher refinery runs overall. Although we do not model refinery runs on a regional basis in the STEO, this outcome does suggest that refiners on the East Coast and West Coast would have a stronger incentive to increase utilization relative to the Gulf Coast in the High Refining Cost scenario. This would also present a stronger opportunity for imports into these regions—annual average net imports of total gasoline increase by over 60,000 b/d in the High Refining Cost scenario compared with the base case.
Previous Supplements
How might gasoline prices change if U.S. refiners face production and distribution limitations? May 2024
U.S. hydropower generation expected to increase by 6% in 2024 following last year’s lows April 2024
Mild winter weather may lead to persistently high natural gas inventories through 2025 April 2024
How accurate were EIA’s Winter Fuels Outlook forecasts? April 2024
Four countries could account for most near-term petroleum liquids supply growth March 2024
About the Short-Term Energy Outlook
- STEO Release Schedule
- Contact STEO Experts
- Model Documentation
- Sign up for email updates
Previous STEO Forecasts:
- Changes in Forecast from Last Month
- STEO Archives
- April 2024 March 2024 February 2024 January 2024 December 2023 prior issues
Other EIA Forecasts:
- Annual Energy Outlook
- International Energy Outlook

IMAGES
VIDEO
COMMENTS
Common types of limitations and their ramifications include: Theoretical: limits the scope, depth, or applicability of a study. Methodological: limits the quality, quantity, or diversity of the data. Empirical: limits the representativeness, validity, or reliability of the data. Analytical: limits the accuracy, completeness, or significance of ...
Possible Limitations of the Researcher. Access-- if your study depends on having access to people, organizations, data, or documents and, for whatever reason, access is denied or limited in some way, the reasons for this needs to be described.Also, include an explanation why being denied or limited access did not prevent you from following through on your study.
"The study also had the limitations inherent to any retrospective study. However, given the extreme rarity of the disease, a prospective study of this population was infeasible." Providing a statement reiterating your study's particular strengths can remind reviewers of the value of the study's findings.
Research limitations are one of those things that students tend to avoid digging into, and understandably so. No one likes to critique their own study and point out weaknesses. Nevertheless, being able to understand the limitations of your study - and, just as importantly, the implications thereof - a is a critically important skill. In this post, we'll unpack some of the most common ...
21 Research Limitations Examples. By Chris Drew (PhD) / November 19, 2023. Research limitations refer to the potential weaknesses inherent in a study. All studies have limitations of some sort, meaning declaring limitations doesn't necessarily need to be a bad thing, so long as your declaration of limitations is well thought-out and explained.
Step 1. Identify the limitation (s) of the study. This part should comprise around 10%-20% of your discussion of study limitations. The first step is to identify the particular limitation (s) that affected your study. There are many possible limitations of research that can affect your study, but you don't need to write a long review of all ...
Limitations in Research. Limitations in research refer to the factors that may affect the results, conclusions, and generalizability of a study.These limitations can arise from various sources, such as the design of the study, the sampling methods used, the measurement tools employed, and the limitations of the data analysis techniques.
1 Answer to this question. Answer: The limitations of a study are its flaws or shortcomings which could be the result of unavailability of resources, small sample size, flawed methodology, etc. No study is completely flawless or inclusive of all possible aspects. Therefore, listing the limitations of your study reflects honesty and transparency ...
3. Identify your limitations of research and explain their importance. 4. Provide the necessary depth, explain their nature, and justify your study choices. 5. Write how you are suggesting that it is possible to overcome them in the future. Limitations can help structure the research study better.
Research process limitations. The study's design can impose constraints on the process. For example, as you're conducting the research, issues may arise that don't conform to the data collection methodology you developed. ... However, the short life span of stem cells outside the lab and the vaccination's severe inflammatory side ...
Writing the limitations of the research papers is often assumed to require lots of effort. However, identifying the limitations of the study can help structure the research better. Therefore, do not underestimate the importance of research study limitations. 3. Opportunity to make suggestions for further research.
Why We Love It: This resource is easy-to-follow and is great to start with and return to as you consider and write about the limitations of your study. It not only explains possible limitations of your research, but offers a handful of useful tips for writing about these limitations effectively. Research Quality Toolkit. Year: 2024. Type: Guide.
Acknowledgement of a study's limitations also provides you with an opportunity to demonstrate to your professor that you have thought critically about the research problem, understood the relevant literature published about it, and correctly assessed the methods chosen for studying the problem. A key objective of the research process is not ...
Well, that depends entirely on the nature of your study. You'll need to comb through your research approach, methodology, testing processes, and expected results to identify the type of limitations your study may be exposed to. It's worth noting that this understanding can only offer a broad idea of the possible restrictions you'll face ...
Small studies: strengths and limitations. A large number of clinical research studies are conducted, including audits of patient data, observational studies, clinical trials and those based on laboratory analyses. While small studies can be published over a short time-frame, there needs to be a balance between those that can be performed ...
Abstract. Study limitations represent weaknesses within a research design that may influence outcomes and conclusions of the research. Researchers have an obligation to the academic community to present complete and honest limitations of a presented study. Too often, authors use generic descriptions to describe study limitations.
Six tips for writing your limitations section. Focus on weaknesses in your design and analyses, rather than results. Start with a bold statement: "This study has some limitations.". Don't try to soften it with less obvious language. Enumerate the limitations, if you can. If you have three limitations to discuss, say so: "This study has ...
Examples of study limitations. Selection bias. Selection bias occurs when the selection of individuals, groups, or data for analysis is not randomised. For example, imagine a study in which different surgical procedures are retrospectively compared in relation to mortality risk [e.g., 1].
Research Limitations. Research limitations are, at the simplest level, the weaknesses of the study, based on factors that are often outside of your control as the researcher. These factors could include things like time, access to funding, equipment, data or participants.For example, if you weren't able to access a random sample of participants for your study and had to adopt a convenience ...
In the ROOTs manuscript, it mentions a few examples of study limitations that could deter extrapolation of study results to patient care, ... The 2013 REDUCE trial was a NI study that compared short-term (5 day) steroid treatment to traditional (14 day) for management of COPD in 134 patients admitted to the emergency department. ...
Limitations generally fall into some common categories, and in a sense we can make a checklist for authors here. Price and Murnan ( 2004) gave an excellent and detailed summary of possible research limitations in their editorial for the American Journal of Health Education. They discussed limitations affecting internal and external validity ...
9.2 Limitations: internal validity. Internal validity refers to the extent to which a cause-and-effect relationship can be established in a study, eliminating other possible explanations (Sect. 6.1).A discussion of the limitations of internal validity should cover, as appropriate: possible confounding variables; the impact of the Hawthorne, observer, placebo and carry-over effects; the impact ...
Study duration and long-term effects. A limitation with many studies, in particular periodization studies, is their short duration (most training studies are 6-12 weeks long). Generally speaking, it takes 2 months to be able to tell whether a study leads to detectable and statistically significant hypertrophy gains.
Objective This study aimed to examine the mediation role of perceived social support in the relationship between functional limitations, depressive symptoms and quality of life among older people in Malaysia. Setting The Malaysian National Health Morbidity Survey 2018: Elderly Health was a cross-sectional health community survey among adults aged 50 and above.
Strengths and limitations of this study. Our analysis has several strengths. Our study provides direct evidence for the effect of a public health intervention (such as HPV vaccination) on cancer rates by deprivation. We used high quality data from population based cancer registries and were able to investigate the extent of socioeconomic ...
VLS conceived the study and led the proposal and protocol development. GAJ, DA, DJH, MG, and KM contributed to study design and to development of the proposal. KS and MS collected data. VLS, MG, KS, and MS analyzed data. All authors contributed to the interpretation of data and to writing the drafts of the manuscript.
Strengths and limitations of the study. The main strength of our study are as follows: Firstly, we analyzed data based on a nationwide population-based longitudinal study. ... Factorial validity of the center for epidemiologic studies depression scale short form in older population in China. Int Psychogeriatr. 2014;26(1):49-57.
The study included more than 110,000 people in Sweden with no family history of colorectal cancer and a negative finding from their last colonoscopy. Each member of that group was matched with up to 18 control individuals of the same age and sex. ... Limitations of the Study . While the Sweden study factored in participants' age and sex, it ...
Introduction Hip osteoarthritis (OA) is one of the leading causes of disability and morbidity worldwide. It is estimated to affect 9.2% individuals globally with age over 45 years. Conventional treatment modalities have limitations and side-effects. To overcome these limitations, over the last decade, there has been an increased interest in the use of orthobiologics derived from autologous ...
Refinery and gasoline production limitations result in a U.S. average regular grade retail gasoline price of $3.80/gal in the summer, compared with $3.70/gal in the base case. Just like the U.S. average, retail gasoline prices in the East Coast are also $0.10/gal higher in the High Refinery Cost scenario.