- Privacy Policy

Home » Research Recommendations – Examples and Writing Guide

Research Recommendations – Examples and Writing Guide
Table of Contents

Research Recommendations
Definition:
Research recommendations refer to suggestions or advice given to someone who is looking to conduct research on a specific topic or area. These recommendations may include suggestions for research methods, data collection techniques, sources of information, and other factors that can help to ensure that the research is conducted in a rigorous and effective manner. Research recommendations may be provided by experts in the field, such as professors, researchers, or consultants, and are intended to help guide the researcher towards the most appropriate and effective approach to their research project.
Parts of Research Recommendations
Research recommendations can vary depending on the specific project or area of research, but typically they will include some or all of the following parts:
- Research question or objective : This is the overarching goal or purpose of the research project.
- Research methods : This includes the specific techniques and strategies that will be used to collect and analyze data. The methods will depend on the research question and the type of data being collected.
- Data collection: This refers to the process of gathering information or data that will be used to answer the research question. This can involve a range of different methods, including surveys, interviews, observations, or experiments.
- Data analysis : This involves the process of examining and interpreting the data that has been collected. This can involve statistical analysis, qualitative analysis, or a combination of both.
- Results and conclusions: This section summarizes the findings of the research and presents any conclusions or recommendations based on those findings.
- Limitations and future research: This section discusses any limitations of the study and suggests areas for future research that could build on the findings of the current project.
How to Write Research Recommendations
Writing research recommendations involves providing specific suggestions or advice to a researcher on how to conduct their study. Here are some steps to consider when writing research recommendations:
- Understand the research question: Before writing research recommendations, it is important to have a clear understanding of the research question and the objectives of the study. This will help to ensure that the recommendations are relevant and appropriate.
- Consider the research methods: Consider the most appropriate research methods that could be used to collect and analyze data that will address the research question. Identify the strengths and weaknesses of the different methods and how they might apply to the specific research question.
- Provide specific recommendations: Provide specific and actionable recommendations that the researcher can implement in their study. This can include recommendations related to sample size, data collection techniques, research instruments, data analysis methods, or other relevant factors.
- Justify recommendations : Justify why each recommendation is being made and how it will help to address the research question or objective. It is important to provide a clear rationale for each recommendation to help the researcher understand why it is important.
- Consider limitations and ethical considerations : Consider any limitations or potential ethical considerations that may arise in conducting the research. Provide recommendations for addressing these issues or mitigating their impact.
- Summarize recommendations: Provide a summary of the recommendations at the end of the report or document, highlighting the most important points and emphasizing how the recommendations will contribute to the overall success of the research project.
Example of Research Recommendations
Example of Research Recommendations sample for students:
- Further investigate the effects of X on Y by conducting a larger-scale randomized controlled trial with a diverse population.
- Explore the relationship between A and B by conducting qualitative interviews with individuals who have experience with both.
- Investigate the long-term effects of intervention C by conducting a follow-up study with participants one year after completion.
- Examine the effectiveness of intervention D in a real-world setting by conducting a field study in a naturalistic environment.
- Compare and contrast the results of this study with those of previous research on the same topic to identify any discrepancies or inconsistencies in the findings.
- Expand upon the limitations of this study by addressing potential confounding variables and conducting further analyses to control for them.
- Investigate the relationship between E and F by conducting a meta-analysis of existing literature on the topic.
- Explore the potential moderating effects of variable G on the relationship between H and I by conducting subgroup analyses.
- Identify potential areas for future research based on the gaps in current literature and the findings of this study.
- Conduct a replication study to validate the results of this study and further establish the generalizability of the findings.
Applications of Research Recommendations
Research recommendations are important as they provide guidance on how to improve or solve a problem. The applications of research recommendations are numerous and can be used in various fields. Some of the applications of research recommendations include:
- Policy-making: Research recommendations can be used to develop policies that address specific issues. For example, recommendations from research on climate change can be used to develop policies that reduce carbon emissions and promote sustainability.
- Program development: Research recommendations can guide the development of programs that address specific issues. For example, recommendations from research on education can be used to develop programs that improve student achievement.
- Product development : Research recommendations can guide the development of products that meet specific needs. For example, recommendations from research on consumer behavior can be used to develop products that appeal to consumers.
- Marketing strategies: Research recommendations can be used to develop effective marketing strategies. For example, recommendations from research on target audiences can be used to develop marketing strategies that effectively reach specific demographic groups.
- Medical practice : Research recommendations can guide medical practitioners in providing the best possible care to patients. For example, recommendations from research on treatments for specific conditions can be used to improve patient outcomes.
- Scientific research: Research recommendations can guide future research in a specific field. For example, recommendations from research on a specific disease can be used to guide future research on treatments and cures for that disease.
Purpose of Research Recommendations
The purpose of research recommendations is to provide guidance on how to improve or solve a problem based on the findings of research. Research recommendations are typically made at the end of a research study and are based on the conclusions drawn from the research data. The purpose of research recommendations is to provide actionable advice to individuals or organizations that can help them make informed decisions, develop effective strategies, or implement changes that address the issues identified in the research.
The main purpose of research recommendations is to facilitate the transfer of knowledge from researchers to practitioners, policymakers, or other stakeholders who can benefit from the research findings. Recommendations can help bridge the gap between research and practice by providing specific actions that can be taken based on the research results. By providing clear and actionable recommendations, researchers can help ensure that their findings are put into practice, leading to improvements in various fields, such as healthcare, education, business, and public policy.
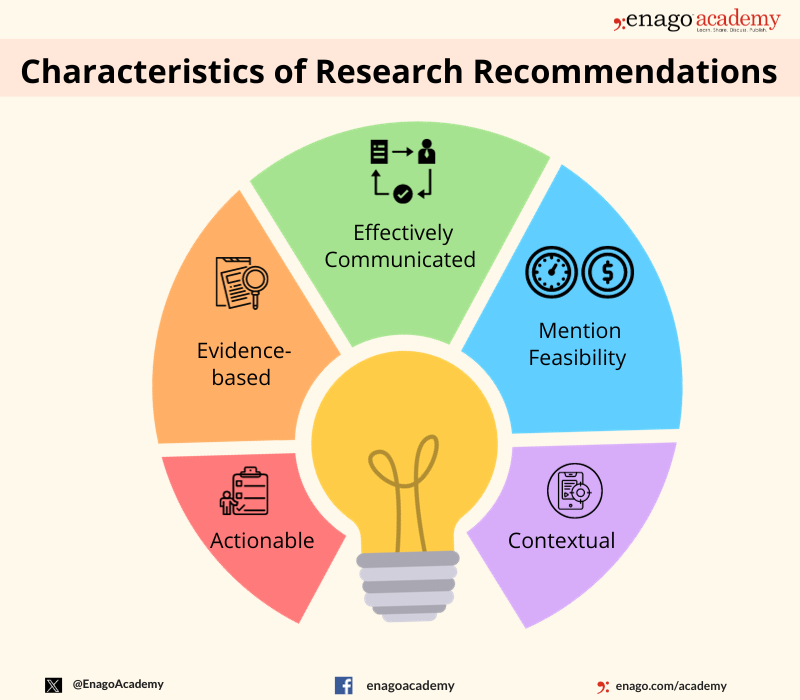
Characteristics of Research Recommendations
Research recommendations are a key component of research studies and are intended to provide practical guidance on how to apply research findings to real-world problems. The following are some of the key characteristics of research recommendations:
- Actionable : Research recommendations should be specific and actionable, providing clear guidance on what actions should be taken to address the problem identified in the research.
- Evidence-based: Research recommendations should be based on the findings of the research study, supported by the data collected and analyzed.
- Contextual: Research recommendations should be tailored to the specific context in which they will be implemented, taking into account the unique circumstances and constraints of the situation.
- Feasible : Research recommendations should be realistic and feasible, taking into account the available resources, time constraints, and other factors that may impact their implementation.
- Prioritized: Research recommendations should be prioritized based on their potential impact and feasibility, with the most important recommendations given the highest priority.
- Communicated effectively: Research recommendations should be communicated clearly and effectively, using language that is understandable to the target audience.
- Evaluated : Research recommendations should be evaluated to determine their effectiveness in addressing the problem identified in the research, and to identify opportunities for improvement.
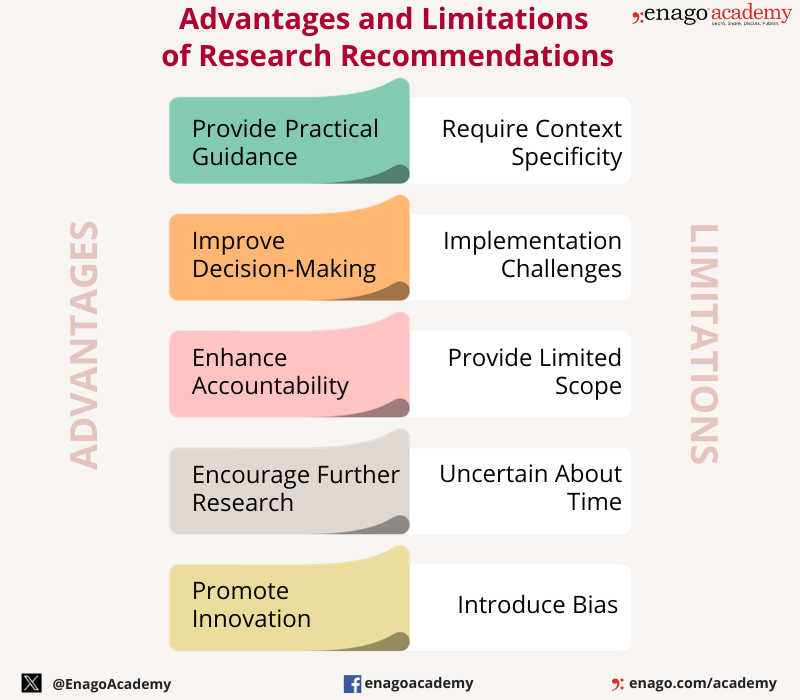
Advantages of Research Recommendations
Research recommendations have several advantages, including:
- Providing practical guidance: Research recommendations provide practical guidance on how to apply research findings to real-world problems, helping to bridge the gap between research and practice.
- Improving decision-making: Research recommendations help decision-makers make informed decisions based on the findings of research, leading to better outcomes and improved performance.
- Enhancing accountability : Research recommendations can help enhance accountability by providing clear guidance on what actions should be taken, and by providing a basis for evaluating progress and outcomes.
- Informing policy development : Research recommendations can inform the development of policies that are evidence-based and tailored to the specific needs of a given situation.
- Enhancing knowledge transfer: Research recommendations help facilitate the transfer of knowledge from researchers to practitioners, policymakers, or other stakeholders who can benefit from the research findings.
- Encouraging further research : Research recommendations can help identify gaps in knowledge and areas for further research, encouraging continued exploration and discovery.
- Promoting innovation: Research recommendations can help identify innovative solutions to complex problems, leading to new ideas and approaches.
Limitations of Research Recommendations
While research recommendations have several advantages, there are also some limitations to consider. These limitations include:
- Context-specific: Research recommendations may be context-specific and may not be applicable in all situations. Recommendations developed in one context may not be suitable for another context, requiring adaptation or modification.
- I mplementation challenges: Implementation of research recommendations may face challenges, such as lack of resources, resistance to change, or lack of buy-in from stakeholders.
- Limited scope: Research recommendations may be limited in scope, focusing only on a specific issue or aspect of a problem, while other important factors may be overlooked.
- Uncertainty : Research recommendations may be uncertain, particularly when the research findings are inconclusive or when the recommendations are based on limited data.
- Bias : Research recommendations may be influenced by researcher bias or conflicts of interest, leading to recommendations that are not in the best interests of stakeholders.
- Timing : Research recommendations may be time-sensitive, requiring timely action to be effective. Delayed action may result in missed opportunities or reduced effectiveness.
- Lack of evaluation: Research recommendations may not be evaluated to determine their effectiveness or impact, making it difficult to assess whether they are successful or not.
About the author
Muhammad Hassan
Researcher, Academic Writer, Web developer
You may also like

Data Collection – Methods Types and Examples

Delimitations in Research – Types, Examples and...

Research Process – Steps, Examples and Tips

Research Design – Types, Methods and Examples

Institutional Review Board – Application Sample...

Evaluating Research – Process, Examples and...

Research Recommendations – Guiding policy-makers for evidence-based decision making
Research recommendations play a crucial role in guiding scholars and researchers toward fruitful avenues of exploration. In an era marked by rapid technological advancements and an ever-expanding knowledge base, refining the process of generating research recommendations becomes imperative.
But, what is a research recommendation?
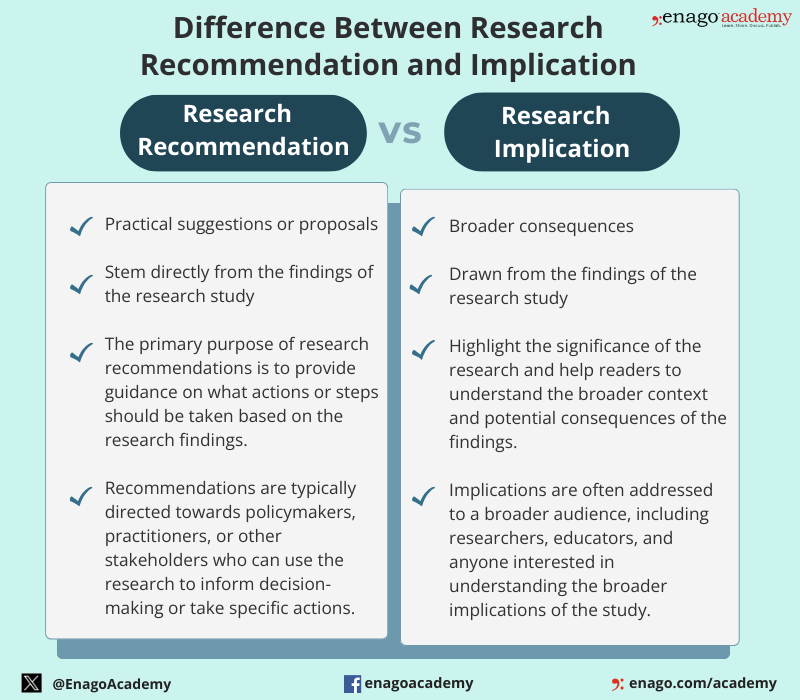
Research recommendations are suggestions or advice provided to researchers to guide their study on a specific topic . They are typically given by experts in the field. Research recommendations are more action-oriented and provide specific guidance for decision-makers, unlike implications that are broader and focus on the broader significance and consequences of the research findings. However, both are crucial components of a research study.
Difference Between Research Recommendations and Implication
Although research recommendations and implications are distinct components of a research study, they are closely related. The differences between them are as follows:
Types of Research Recommendations
Recommendations in research can take various forms, which are as follows:
These recommendations aim to assist researchers in navigating the vast landscape of academic knowledge.
Let us dive deeper to know about its key components and the steps to write an impactful research recommendation.
Key Components of Research Recommendations
The key components of research recommendations include defining the research question or objective, specifying research methods, outlining data collection and analysis processes, presenting results and conclusions, addressing limitations, and suggesting areas for future research. Here are some characteristics of research recommendations:
Research recommendations offer various advantages and play a crucial role in ensuring that research findings contribute to positive outcomes in various fields. However, they also have few limitations which highlights the significance of a well-crafted research recommendation in offering the promised advantages.
The importance of research recommendations ranges in various fields, influencing policy-making, program development, product development, marketing strategies, medical practice, and scientific research. Their purpose is to transfer knowledge from researchers to practitioners, policymakers, or stakeholders, facilitating informed decision-making and improving outcomes in different domains.
How to Write Research Recommendations?
Research recommendations can be generated through various means, including algorithmic approaches, expert opinions, or collaborative filtering techniques. Here is a step-wise guide to build your understanding on the development of research recommendations.
1. Understand the Research Question:
Understand the research question and objectives before writing recommendations. Also, ensure that your recommendations are relevant and directly address the goals of the study.
2. Review Existing Literature:
Familiarize yourself with relevant existing literature to help you identify gaps , and offer informed recommendations that contribute to the existing body of research.
3. Consider Research Methods:
Evaluate the appropriateness of different research methods in addressing the research question. Also, consider the nature of the data, the study design, and the specific objectives.
4. Identify Data Collection Techniques:
Gather dataset from diverse authentic sources. Include information such as keywords, abstracts, authors, publication dates, and citation metrics to provide a rich foundation for analysis.
5. Propose Data Analysis Methods:
Suggest appropriate data analysis methods based on the type of data collected. Consider whether statistical analysis, qualitative analysis, or a mixed-methods approach is most suitable.
6. Consider Limitations and Ethical Considerations:
Acknowledge any limitations and potential ethical considerations of the study. Furthermore, address these limitations or mitigate ethical concerns to ensure responsible research.
7. Justify Recommendations:
Explain how your recommendation contributes to addressing the research question or objective. Provide a strong rationale to help researchers understand the importance of following your suggestions.
8. Summarize Recommendations:
Provide a concise summary at the end of the report to emphasize how following these recommendations will contribute to the overall success of the research project.
By following these steps, you can create research recommendations that are actionable and contribute meaningfully to the success of the research project.
Download now to unlock some tips to improve your journey of writing research recommendations.
Example of a Research Recommendation
Here is an example of a research recommendation based on a hypothetical research to improve your understanding.
Research Recommendation: Enhancing Student Learning through Integrated Learning Platforms
Background:
The research study investigated the impact of an integrated learning platform on student learning outcomes in high school mathematics classes. The findings revealed a statistically significant improvement in student performance and engagement when compared to traditional teaching methods.
Recommendation:
In light of the research findings, it is recommended that educational institutions consider adopting and integrating the identified learning platform into their mathematics curriculum. The following specific recommendations are provided:
- Implementation of the Integrated Learning Platform:
Schools are encouraged to adopt the integrated learning platform in mathematics classrooms, ensuring proper training for teachers on its effective utilization.
- Professional Development for Educators:
Develop and implement professional programs to train educators in the effective use of the integrated learning platform to address any challenges teachers may face during the transition.
- Monitoring and Evaluation:
Establish a monitoring and evaluation system to track the impact of the integrated learning platform on student performance over time.
- Resource Allocation:
Allocate sufficient resources, both financial and technical, to support the widespread implementation of the integrated learning platform.
By implementing these recommendations, educational institutions can harness the potential of the integrated learning platform and enhance student learning experiences and academic achievements in mathematics.
This example covers the components of a research recommendation, providing specific actions based on the research findings, identifying the target audience, and outlining practical steps for implementation.
Using AI in Research Recommendation Writing
Enhancing research recommendations is an ongoing endeavor that requires the integration of cutting-edge technologies, collaborative efforts, and ethical considerations. By embracing data-driven approaches and leveraging advanced technologies, the research community can create more effective and personalized recommendation systems. However, it is accompanied by several limitations. Therefore, it is essential to approach the use of AI in research with a critical mindset, and complement its capabilities with human expertise and judgment.
Here are some limitations of integrating AI in writing research recommendation and some ways on how to counter them.
1. Data Bias
AI systems rely heavily on data for training. If the training data is biased or incomplete, the AI model may produce biased results or recommendations.
How to tackle: Audit regularly the model’s performance to identify any discrepancies and adjust the training data and algorithms accordingly.
2. Lack of Understanding of Context:
AI models may struggle to understand the nuanced context of a particular research problem. They may misinterpret information, leading to inaccurate recommendations.
How to tackle: Use AI to characterize research articles and topics. Employ them to extract features like keywords, authorship patterns and content-based details.
3. Ethical Considerations:
AI models might stereotype certain concepts or generate recommendations that could have negative consequences for certain individuals or groups.
How to tackle: Incorporate user feedback mechanisms to reduce redundancies. Establish an ethics review process for AI models in research recommendation writing.
4. Lack of Creativity and Intuition:
AI may struggle with tasks that require a deep understanding of the underlying principles or the ability to think outside the box.
How to tackle: Hybrid approaches can be employed by integrating AI in data analysis and identifying patterns for accelerating the data interpretation process.
5. Interpretability:
Many AI models, especially complex deep learning models, lack transparency on how the model arrived at a particular recommendation.
How to tackle: Implement models like decision trees or linear models. Provide clear explanation of the model architecture, training process, and decision-making criteria.
6. Dynamic Nature of Research:
Research fields are dynamic, and new information is constantly emerging. AI models may struggle to keep up with the rapidly changing landscape and may not be able to adapt to new developments.
How to tackle: Establish a feedback loop for continuous improvement. Regularly update the recommendation system based on user feedback and emerging research trends.
The integration of AI in research recommendation writing holds great promise for advancing knowledge and streamlining the research process. However, navigating these concerns is pivotal in ensuring the responsible deployment of these technologies. Researchers need to understand the use of responsible use of AI in research and must be aware of the ethical considerations.
Exploring research recommendations plays a critical role in shaping the trajectory of scientific inquiry. It serves as a compass, guiding researchers toward more robust methodologies, collaborative endeavors, and innovative approaches. Embracing these suggestions not only enhances the quality of individual studies but also contributes to the collective advancement of human understanding.
Frequently Asked Questions
The purpose of recommendations in research is to provide practical and actionable suggestions based on the study's findings, guiding future actions, policies, or interventions in a specific field or context. Recommendations bridges the gap between research outcomes and their real-world application.
To make a research recommendation, analyze your findings, identify key insights, and propose specific, evidence-based actions. Include the relevance of the recommendations to the study's objectives and provide practical steps for implementation.
Begin a recommendation by succinctly summarizing the key findings of the research. Clearly state the purpose of the recommendation and its intended impact. Use a direct and actionable language to convey the suggested course of action.
Rate this article Cancel Reply
Your email address will not be published.

Enago Academy's Most Popular Articles
![recommendation in research paper sample What is Academic Integrity and How to Uphold it [FREE CHECKLIST]](https://www.enago.com/academy/wp-content/uploads/2024/05/FeatureImages-59-210x136.png)
Ensuring Academic Integrity and Transparency in Academic Research: A comprehensive checklist for researchers
Academic integrity is the foundation upon which the credibility and value of scientific findings are…

- Industry News
- Publishing News
Unified AI Guidelines Crucial as Academic Writing Embraces Generative Tools
As generative artificial intelligence (AI) tools like ChatGPT are advancing at an accelerating pace, their…

- Reporting Research
How to Effectively Cite a PDF (APA, MLA, AMA, and Chicago Style)
The pressure to “publish or perish” is a well-known reality for academics, striking fear into…

- AI in Academia
- Trending Now
Using AI for Journal Selection — Simplifying your academic publishing journey in the smart way
Strategic journal selection plays a pivotal role in maximizing the impact of one’s scholarly work.…

- Career Corner
Recognizing the signs: A guide to overcoming academic burnout
As the sun set over the campus, casting long shadows through the library windows, Alex…
How to Optimize Your Research Process: A step-by-step guide
Digital Citations: A comprehensive guide to citing of websites in APA, MLA, and CMOS…
Choosing the Right Analytical Approach: Thematic analysis vs. content analysis for…

Sign-up to read more
Subscribe for free to get unrestricted access to all our resources on research writing and academic publishing including:
- 2000+ blog articles
- 50+ Webinars
- 10+ Expert podcasts
- 50+ Infographics
- 10+ Checklists
- Research Guides
We hate spam too. We promise to protect your privacy and never spam you.
I am looking for Editing/ Proofreading services for my manuscript Tentative date of next journal submission:

As a researcher, what do you consider most when choosing an image manipulation detector?
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, automatically generate references for free.
- Knowledge Base
- Dissertation
- How to Write Recommendations in Research | Examples & Tips
How to Write Recommendations in Research | Examples & Tips
Published on 15 September 2022 by Tegan George .
Recommendations in research are a crucial component of your discussion section and the conclusion of your thesis , dissertation , or research paper .
As you conduct your research and analyse the data you collected , perhaps there are ideas or results that don’t quite fit the scope of your research topic . Or, maybe your results suggest that there are further implications of your results or the causal relationships between previously-studied variables than covered in extant research.
Instantly correct all language mistakes in your text
Be assured that you'll submit flawless writing. Upload your document to correct all your mistakes.

Table of contents
What should recommendations look like, building your research recommendation, how should your recommendations be written, recommendation in research example, frequently asked questions about recommendations.
Recommendations for future research should be:
- Concrete and specific
- Supported with a clear rationale
- Directly connected to your research
Overall, strive to highlight ways other researchers can reproduce or replicate your results to draw further conclusions, and suggest different directions that future research can take, if applicable.
Relatedly, when making these recommendations, avoid:
- Undermining your own work, but rather offer suggestions on how future studies can build upon it
- Suggesting recommendations actually needed to complete your argument, but rather ensure that your research stands alone on its own merits
- Using recommendations as a place for self-criticism, but rather as a natural extension point for your work
Prevent plagiarism, run a free check.
There are many different ways to frame recommendations, but the easiest is perhaps to follow the formula of research question conclusion recommendation. Here’s an example.
Conclusion An important condition for controlling many social skills is mastering language. If children have a better command of language, they can express themselves better and are better able to understand their peers. Opportunities to practice social skills are thus dependent on the development of language skills.
As a rule of thumb, try to limit yourself to only the most relevant future recommendations: ones that stem directly from your work. While you can have multiple recommendations for each research conclusion, it is also acceptable to have one recommendation that is connected to more than one conclusion.
These recommendations should be targeted at your audience, specifically toward peers or colleagues in your field that work on similar topics to yours. They can flow directly from any limitations you found while conducting your work, offering concrete and actionable possibilities for how future research can build on anything that your own work was unable to address at the time of your writing.
See below for a full research recommendation example that you can use as a template to write your own.
The current study can be interpreted as a first step in the research on COPD speech characteristics. However, the results of this study should be treated with caution due to the small sample size and the lack of details regarding the participants’ characteristics.
Future research could further examine the differences in speech characteristics between exacerbated COPD patients, stable COPD patients, and healthy controls. It could also contribute to a deeper understanding of the acoustic measurements suitable for e-health measurements.
The only proofreading tool specialized in correcting academic writing
The academic proofreading tool has been trained on 1000s of academic texts and by native English editors. Making it the most accurate and reliable proofreading tool for students.

Correct my document today
While it may be tempting to present new arguments or evidence in your thesis or disseration conclusion , especially if you have a particularly striking argument you’d like to finish your analysis with, you shouldn’t. Theses and dissertations follow a more formal structure than this.
All your findings and arguments should be presented in the body of the text (more specifically in the discussion section and results section .) The conclusion is meant to summarize and reflect on the evidence and arguments you have already presented, not introduce new ones.
The conclusion of your thesis or dissertation should include the following:
- A restatement of your research question
- A summary of your key arguments and/or results
- A short discussion of the implications of your research
For a stronger dissertation conclusion , avoid including:
- Generic concluding phrases (e.g. “In conclusion…”)
- Weak statements that undermine your argument (e.g. “There are good points on both sides of this issue.”)
Your conclusion should leave the reader with a strong, decisive impression of your work.
In a thesis or dissertation, the discussion is an in-depth exploration of the results, going into detail about the meaning of your findings and citing relevant sources to put them in context.
The conclusion is more shorter and more general: it concisely answers your main research question and makes recommendations based on your overall findings.
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the ‘Cite this Scribbr article’ button to automatically add the citation to our free Reference Generator.
George, T. (2022, September 15). How to Write Recommendations in Research | Examples & Tips. Scribbr. Retrieved 14 May 2024, from https://www.scribbr.co.uk/thesis-dissertation/research-recommendations/
Is this article helpful?
Tegan George
Other students also liked, how to write a discussion section | tips & examples, how to write a thesis or dissertation conclusion, how to write a results section | tips & examples.

How to write recommendations in a research paper
Many students put in a lot of effort and write a good report however they are not able to give proper recommendations. Recommendations in the research paper should be included in your research. As a researcher, you display a deep understanding of the topic of research. Therefore you should be able to give recommendations. Here are a few tips that will help you to give appropriate recommendations.
Recommendations in the research paper should be the objective of the research. Therefore at least one of your objectives of the paper is to provide recommendations to the parties associated or the parties that will benefit from your research. For example, to encourage higher employee engagement HR department should make strategies that invest in the well-being of employees. Additionally, the HR department should also collect regular feedback through online surveys.
Recommendations in the research paper should come from your review and analysis For example It was observed that coaches interviewed were associated with the club were working with the club from the past 2-3 years only. This shows that the attrition rate of coaches is high and therefore clubs should work on reducing the turnover of coaches.
Recommendations in the research paper should also come from the data you have analysed. For example, the research found that people over 65 years of age are at greater risk of social isolation. Therefore, it is recommended that policies that are made for combating social isolation should target this specific group.
Recommendations in the research paper should also come from observation. For example, it is observed that Lenovo’s income is stable and gross revenue has displayed a negative turn. Therefore the company should analyse its marketing and branding strategy.
Recommendations in the research paper should be written in the order of priority. The most important recommendations for decision-makers should come first. However, if the recommendations are of equal importance then it should come in the sequence in which the topic is approached in the research.
Recommendations in a research paper if associated with different categories then you should categorize them. For example, you have separate recommendations for policymakers, educators, and administrators then you can categorize the recommendations.
Recommendations in the research paper should come purely from your research. For example, you have written research on the impact on HR strategies on motivation. However, nowhere you have discussed Reward and recognition. Then you should not give recommendations for using rewards and recognition measures to boost employee motivation.
The use of bullet points offers better clarity rather than using long paragraphs. For example this paragraph “ It is recommended that Britannia Biscuit should launch and promote sugar-free options apart from the existing product range. Promotion efforts should be directed at creating a fresh and healthy image. A campaign that conveys a sense of health and vitality to the consumer while enjoying biscuit is recommended” can be written as:
- The company should launch and promote sugar-free options
- The company should work towards creating s fresh and healthy image
- The company should run a campaign to convey its healthy image
The inclusion of an action plan along with recommendation adds more weightage to your recommendation. Recommendations should be clear and conscience and written using actionable words. Recommendations should display a solution-oriented approach and in some cases should highlight the scope for further research.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- How to formulate...
How to formulate research recommendations
- Related content
- Peer review
- Polly Brown ( pbrown{at}bmjgroup.com ) , publishing manager 1 ,
- Klara Brunnhuber , clinical editor 1 ,
- Kalipso Chalkidou , associate director, research and development 2 ,
- Iain Chalmers , director 3 ,
- Mike Clarke , director 4 ,
- Mark Fenton , editor 3 ,
- Carol Forbes , reviews manager 5 ,
- Julie Glanville , associate director/information service manager 5 ,
- Nicholas J Hicks , consultant in public health medicine 6 ,
- Janet Moody , identification and prioritisation manager 6 ,
- Sara Twaddle , director 7 ,
- Hazim Timimi , systems developer 8 ,
- Pamela Young , senior programme manager 6
- 1 BMJ Publishing Group, London WC1H 9JR,
- 2 National Institute for Health and Clinical Excellence, London WC1V 6NA,
- 3 Database of Uncertainties about the Effects of Treatments, James Lind Alliance Secretariat, James Lind Initiative, Oxford OX2 7LG,
- 4 UK Cochrane Centre, Oxford OX2 7LG,
- 5 Centre for Reviews and Dissemination, University of York, York YO10 5DD,
- 6 National Coordinating Centre for Health Technology Assessment, University of Southampton, Southampton SO16 7PX,
- 7 Scottish Intercollegiate Guidelines Network, Edinburgh EH2 1EN,
- 8 Update Software, Oxford OX2 7LG
- Correspondence to: PBrown
- Accepted 22 September 2006
“More research is needed” is a conclusion that fits most systematic reviews. But authors need to be more specific about what exactly is required
Long awaited reports of new research, systematic reviews, and clinical guidelines are too often a disappointing anticlimax for those wishing to use them to direct future research. After many months or years of effort and intellectual energy put into these projects, authors miss the opportunity to identify unanswered questions and outstanding gaps in the evidence. Most reports contain only a less than helpful, general research recommendation. This means that the potential value of these recommendations is lost.
Current recommendations
In 2005, representatives of organisations commissioning and summarising research, including the BMJ Publishing Group, the Centre for Reviews and Dissemination, the National Coordinating Centre for Health Technology Assessment, the National Institute for Health and Clinical Excellence, the Scottish Intercollegiate Guidelines Network, and the UK Cochrane Centre, met as members of the development group for the Database of Uncertainties about the Effects of Treatments (see bmj.com for details on all participating organisations). Our aim was to discuss the state of research recommendations within our organisations and to develop guidelines for improving the presentation of proposals for further research. All organisations had found weaknesses in the way researchers and authors of systematic reviews and clinical guidelines stated the need for further research. As part of the project, a member of the Centre for Reviews and Dissemination under-took a rapid literature search to identify information on research recommendation models, which found some individual methods but no group initiatives to attempt to standardise recommendations.
Suggested format for research recommendations on the effects of treatments
Core elements.
E Evidence (What is the current state of the evidence?)
P Population (What is the population of interest?)
I Intervention (What are the interventions of interest?)
C Comparison (What are the comparisons of interest?)
O Outcome (What are the outcomes of interest?)
T Time stamp (Date of recommendation)
Optional elements
d Disease burden or relevance
t Time aspect of core elements of EPICOT
s Appropriate study type according to local need
In January 2006, the National Coordinating Centre for Health Technology Assessment presented the findings of an initial comparative analysis of how different organisations currently structure their research recommendations. The National Institute for Health and Clinical Excellence and the National Coordinating Centre for Health Technology Assessment request authors to present recommendations in a four component format for formulating well built clinical questions around treatments: population, intervention, comparison, and outcomes (PICO). 1 In addition, the research recommendation is dated and authors are asked to provide the current state of the evidence to support the proposal.
Clinical Evidence , although not directly standardising its sections for research recommendations, presents gaps in the evidence using a slightly extended version of the PICO format: evidence, population, intervention, comparison, outcomes, and time (EPICOT). Clinical Evidence has used this inherent structure to feed research recommendations on interventions categorised as “unknown effectiveness” back to the National Coordinating Centre for Health Technology Assessment and for inclusion in the Database of Uncertainties about the Effects of Treatments ( http://www.duets.nhs.uk/ ).
We decided to propose the EPICOT format as the basis for its statement on formulating research recommendations and tested this proposal through discussion and example. We agreed that this set of components provided enough context for formulating research recommendations without limiting researchers. In order for the proposed framework to be flexible and more widely applicable, the group discussed using several optional components when they seemed relevant or were proposed by one or more of the group members. The final outcome of discussions resulted in the proposed EPICOT+ format (box).
A recent BMJ article highlighted how lack of research hinders the applicability of existing guidelines to patients in primary care who have had a stroke or transient ischaemic attack. 2 Most research in the area had been conducted in younger patients with a recent episode and in a hospital setting. The authors concluded that “further evidence should be collected on the efficacy and adverse effects of intensive blood pressure lowering in representative populations before we implement this guidance [from national and international guidelines] in primary care.” Table 1 outlines how their recommendations could be formulated using the EPICOT+ format. The decision on whether additional research is indeed clinically and ethically warranted will still lie with the organisation considering commissioning the research.
Research recommendation based on gap in the evidence identified by a cross sectional study of clinical guidelines for management of patients who have had a stroke
- View inline
Table 2 shows the use of EPICOT+ for an unanswered question on the effectiveness of compliance therapy in people with schizophrenia, identified by the Database of Uncertainties about the Effects of Treatments.
Research recommendation based on a gap in the evidence on treatment of schizophrenia identified by the Database of Uncertainties about the Effects of Treatments
Discussions around optional elements
Although the group agreed that the PICO elements should be core requirements for a research recommendation, intense discussion centred on the inclusion of factors defining a more detailed context, such as current state of evidence (E), appropriate study type (s), disease burden and relevance (d), and timeliness (t).
Initially, group members interpreted E differently. Some viewed it as the supporting evidence for a research recommendation and others as the suggested study type for a research recommendation. After discussion, we agreed that E should be used to refer to the amount and quality of research supporting the recommendation. However, the issue remained contentious as some of us thought that if a systematic review was available, its reference would sufficiently identify the strength of the existing evidence. Others thought that adding evidence to the set of core elements was important as it provided a summary of the supporting evidence, particularly as the recommendation was likely to be abstracted and used separately from the review or research that led to its formulation. In contrast, the suggested study type (s) was left as an optional element.
A research recommendation will rarely have an absolute value in itself. Its relative priority will be influenced by the burden of ill health (d), which is itself dependent on factors such as local prevalence, disease severity, relevant risk factors, and the priorities of the organisation considering commissioning the research.
Similarly, the issue of time (t) could be seen to be relevant to each of the core elements in varying ways—for example, duration of treatment, length of follow-up. The group therefore agreed that time had a subsidiary role within each core item; however, T as the date of the recommendation served to define its shelf life and therefore retained individual importance.
Applicability and usability
The proposed statement on research recommendations applies to uncertainties of the effects of any form of health intervention or treatment and is intended for research in humans rather than basic scientific research. Further investigation is required to assess the applicability of the format for questions around diagnosis, signs and symptoms, prognosis, investigations, and patient preference.
When the proposed format is applied to a specific research recommendation, the emphasis placed on the relevant part(s) of the EPICOT+ format may vary by author, audience, and intended purpose. For example, a recommendation for research into treatments for transient ischaemic attack may or may not define valid outcome measures to assess quality of life or gather data on adverse effects. Among many other factors, its implementation will also depend on the strength of current findings—that is, strong evidence may support a tightly focused recommendation whereas a lack of evidence would result in a more general recommendation.
The controversy within the group, especially around the optional components, reflects the different perspectives of the participating organisations—whether they were involved in commissioning, undertaking, or summarising research. Further issues will arise during the implementation of the proposed format, and we welcome feedback and discussion.
Summary points
No common guidelines exist for the formulation of recommendations for research on the effects of treatments
Major organisations involved in commissioning or summarising research compared their approaches and agreed on core questions
The essential items can be summarised as EPICOT+ (evidence, population, intervention, comparison, outcome, and time)
Further details, such as disease burden and appropriate study type, should be considered as required
We thank Patricia Atkinson and Jeremy Wyatt.
Contributors and sources All authors contributed to manuscript preparation and approved the final draft. NJH is the guarantor.
Competing interests None declared.
- Richardson WS ,
- Wilson MC ,
- Nishikawa J ,
- Hayward RSA
- McManus RJ ,
- Leonardi-Bee J ,
- PROGRESS Collaborative Group
- Warburton E
- Rothwell P ,
- McIntosh AM ,
- Lawrie SM ,
- Stanfield AC
- O'Donnell C ,
- Donohoe G ,
- Sharkey L ,
- Jablensky A ,
- Sartorius N ,
- Ernberg G ,
Purdue Online Writing Lab Purdue OWL® College of Liberal Arts
APA Sample Paper

Welcome to the Purdue OWL
This page is brought to you by the OWL at Purdue University. When printing this page, you must include the entire legal notice.
Copyright ©1995-2018 by The Writing Lab & The OWL at Purdue and Purdue University. All rights reserved. This material may not be published, reproduced, broadcast, rewritten, or redistributed without permission. Use of this site constitutes acceptance of our terms and conditions of fair use.
Note: This page reflects the latest version of the APA Publication Manual (i.e., APA 7), which released in October 2019. The equivalent resource for the older APA 6 style can be found here .
Media Files: APA Sample Student Paper , APA Sample Professional Paper
This resource is enhanced by Acrobat PDF files. Download the free Acrobat Reader
Note: The APA Publication Manual, 7 th Edition specifies different formatting conventions for student and professional papers (i.e., papers written for credit in a course and papers intended for scholarly publication). These differences mostly extend to the title page and running head. Crucially, citation practices do not differ between the two styles of paper.
However, for your convenience, we have provided two versions of our APA 7 sample paper below: one in student style and one in professional style.
Note: For accessibility purposes, we have used "Track Changes" to make comments along the margins of these samples. Those authored by [AF] denote explanations of formatting and [AWC] denote directions for writing and citing in APA 7.
APA 7 Student Paper:
Apa 7 professional paper:.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Research Council (US) and Institute of Medicine (US) Panel to Review the National Children's Study Research Plan. The National Children's Study Research Plan: A Review. Washington (DC): National Academies Press (US); 2008.

The National Children's Study Research Plan: A Review.
- Hardcopy Version at National Academies Press
6 Conclusions and Recommendations
D uring the past several months the panel has met and reviewed the research plan for the National Children’s Study (NCS), various working papers of the study, and additional documents provided by the National Institute of Child Health and Human Development. The panel believes that this landmark study offers an unparalleled opportunity to examine the effects of environmental influences on child health and development, as well as to explore the complex interactions between genes and environments. The database derived from the study will be valuable for investigating the hypotheses described in the research plan as well as additional hypotheses that will evolve.
The critique, suggestions, and recommendations offered in the preceding chapters, therefore, are intended to improve the capabilities of the study to carry out the important mandate of the Children’s Health Act of 2000. This chapter highlights the panel’s key conclusions and recommendations resulting from its review organized by chapter and subject area.
CHAPTER 2: NCS GOALS, CONCEPTUAL FRAMEWORK, AND CORE HYPOTHESES
Conclusion 2-1: The stated overall and specific goals for the NCS—and the design of the NCS to achieve those goals—largely reflect the stipulations of the Children’s Health Act of 2000. In the broadest terms, the NCS goals and design are responsive to the call in the act for a “national longitudinal study of environmental influences (including physical, chemical, biological, and psychosocial) on children’s health and development.” Conclusion 2-2: The large, nationally representative, equal probability sample design, together with the inclusion of a large number of outcome and exposure measures over a long time span, are major strengths of the NCS. In particular, the sample design is an appropriate platform for the study, considering resource constraints, the need to represent all population groups and geographic areas, and the difficulty of devising an alternative disproportionate sampling scheme that would not unduly disadvantage some groups and areas that turn out to be of analytical interest. Conclusion 2-3: In four overarching areas, the NCS design, as represented in the research plan, is not, or may not be, optimal for achieving the goals of the Children’s Health Act. These areas are: insufficient attention to understanding disparities in child health and development among population groups of children defined by race, ethnicity, language, socioeconomic status, and geographic area, which the act explicitly mandates; inadequate conceptualization of important constructs, including health and development, and an overemphasis on disease and impairment relative to health and functionality and on risk factors relative to protective health-promoting factors; impaired data collection schedules and types of measures to support evaluation of some of the effects of chronic and intermittent exposures on child health and development; and underappreciation of the challenges to obtaining the highest possible quality of data from an observational design, which include the decentralized data collection structure of the study and limitations on the frequency of home and clinic visits and on the collection of medical and other administrative records for study participants.
Recommendation 2-1: The NCS should give priority attention to seeking ways to bolster the ability of the study to contribute to understanding of health disparities among children in different racial, ethnic, and other population groups, including the reestablishment of a working group to oversee this area and the encouragement of appropriate adjunct studies. Recommendation 2-2: The NCS should seek resources and develop methods to obtain more frequent in-person measures and medical and other administrative records data on study participants.
Conceptual Framework
Recommendation 2-3: The NCS should clearly define the key constructs of child health and development and more fully develop a conceptual framework for understanding child health and development over the course of infancy, childhood, and adolescence.
Using the Vanguard Centers as Pilots
Recommendation 2-4: We strongly urge the NCS to delay enrollment at new sites to make effective use of initial findings from participant enrollment and data collection in the Vanguard Center sites to improve study procedures, as appropriate, and to refine key concepts, hypotheses, and measures of outcomes and exposures. Throughout the life of the study, the NCS should use the Vanguard Centers to pilot test and experiment with data collection methods and instrumentation.
CHAPTER 3: PRIORITY OUTCOME AND EXPOSURE MEASURES
Pregnancy outcomes.
Recommendation 3-1: The NCS should consider replacing research on subclinical maternal hypothyroidism as a factor in adverse pregnancy outcomes with research on the effects of a broader set of maternal physical and mental health conditions, such as maternal depression, maternal perceived stress, and maternal periodontal disease. Recommendation 3-2: The NCS should develop refined, detailed protocols for investigating all pregnancy outcomes, specifically a detailed protocol for obtaining information on various types of pregnancy loss, before beginning data collection at the Vanguard Centers, given that pregnancy outcomes are among the first outcomes to be examined; many outcomes lack clarity in measurement; and there are important questions regarding the adequacy of statistical power and the planned data collection (for example, the need for prepregnancy measurements of some exposures).
Neurodevelopment and Behavior and Child Health and Development
Recommendation 3-3: The NCS should develop a clearer rationale for the selection of specific neurodevelopment and behavior disorders to be considered in the study and a clearer conceptual basis for the assessment of normal child health and development trajectories and outcomes. Clarity is needed to guide the choice of outcome measures and exposure measures and the frequency and types of contacts (at the home, in clinics) with study participants in order to obtain the best information possible within resource and burden constraints.
Recommendation 3-4: The NCS should develop a clearer rationale for its hypotheses about factors that may increase the incidence of asthma. These should focus on prenatal and early life risk factors.
Obesity and Growth
Recommendation 3-5: The NCS should reevaluate its main hypotheses to be addressed in the study of childhood obesity and consider adopting a broader approach that incorporates social and psychological factors as well as biogenetic ones. Such an approach would help the study identify the constellations of key factors and their interrelationships that are important to understand in order to develop the most effective public health measures to reduce childhood obesity.
Recommendation 3-6: The NCS should consider replacing research on repeated mild traumatic brain injury (rMTBI) with more nuanced research on other injury-related topics, such as environmental factors in childhood injuries and the effects of clinical response to injury (treatment or nontreatment).
Hormonally Active Agents and Reproductive Development
Recommendation 3-7: The NCS should develop refined and detailed protocols for studying reproductive development outcomes, which, as presented in the research plan, often lack clarity in measurement and research design. Outcomes that are measured at birth for which there is little time to refine research protocols require immediate attention. The NCS should use results from the Vanguard Centers, such as estimates of the prevalence of specific reproductive development outcomes, to assist in protocol development, and it should consider the usefulness of substudies of high-exposure population groups.
Demographic and Socioeconomic Measures
Recommendation 3-8: The NCS should add to its well-planned battery of demographic and socioeconomic measures questions on immigrant generation, languages spoken, and, if possible, the legal status of the parents and child.
Chemical Exposure Measures
Recommendation 3-9: The NCS should consider the use of personal air sampling methods for a subsample of participating women and their children for measuring exposure to air pollutants. Recommendation 3-10: The NCS should incorporate methodology to measure paternal exposure to environmental chemicals (both persistent and nonpersistent). More generally, the NCS should consider collecting for fathers, not only chemical exposures, but also biological samples and interview data on paternal characteristics that may affect children’s health and development to the same degree as it collects such information for mothers.
Physical Exposure Measures
Recommendation 3-11: The NCS should provide a clearer rationale for some of the housing and neighborhood conditions it proposes to measure and revisit its data collection plans to ensure that needed measures are obtained at developmental stages when children may be more vulnerable to risk factors. The goal should be a set of measures and data collection plans that are optimal with regard to analytic utility and response burden.
Psychosocial Exposure Measures
Recommendation 3-12: The NCS should reconsider its psychosocial measures to ensure that they will provide high-quality data for outcomes of interest for child health and development. In the face of resource and respondent burden constraints, the NCS should emphasize the quality and analytic utility of information, even if some measures must be dropped in order to substitute other assessments more desirable on various grounds. Recommendation 3-13: The NCS should dedicate a portion of funds to support research and development of reliable and valid instruments of key psychosocial measures that are practical and economical to administer.
Biological Exposure Measures
Recommendation 3-14: The NCS should review some of the proposed measures of biological exposures, such as maternal glucose metabolism and child cortisol levels, to ensure that the proposed times for data collection are appropriate for capturing the underlying exposure.
Genetic Measures
Recommendation 3-15: The NCS should adopt a clear mechanism by which genetic association studies are internally and, optimally, externally validated before any results are published or released to the media. The NCS should also revise its proposed “established” candidate gene approach to take advantage of the new information emanating from the current wave of genome-wide association studies, with appropriate replication. Recommendation 3-16: The NCS should consider consolidating its genetics studies in order to reduce costs and to coordinate the best science at the least cost to the project. One approach would be to simply collect the biological samples and properly store them for later genetic analysis when a better selection of polymorphisms and cost-effective genotyping across studies are possible.
Missing Exposures
Recommendation 3-17: The NCS should add measures of access to and quality of services, including medical care, education, child care, and services, as potential mediators of health and development outcomes and to improve the assessment of information obtained through maternal reports.
Data Linkage
Recommendation 3-18: To facilitate linkages of NCS data with environmental exposures from other databases, such as measures of demographics, crime, government programs, and pollution, the NCS should develop a plan for geocoding the residential addresses from prebirth through adulthood of all participating children to standard census geographic units. In addition, the study should develop arrangements by which researchers, both inside and outside the NCS study centers, can access geocodes for respondent addresses and are encouraged to perform linkages and make their environmental information available to the NCS analysis community. Such arrangements must safeguard the confidentiality of NCS respondents.
CHAPTER 4: STUDY DESIGN, DATA COLLECTION, AND ANALYSIS
Sampling design.
Conclusion 4-1: We strongly endorse the use of probability sampling to select the NCS national sample of births. Conclusion 4-2: While we endorse the decision to select an equal probability national sample of births as a reasonable strategy given the many key scientific objectives of the NCS, we recognize that a proportionate representation of the study’s target population will result in estimates for some subgroups that are not as precise as they would be had those groups been oversampled. Conclusion 4-3: The process of identifying births from a national sample of households is complex and subject to numerous sources of attrition of uncertain magnitude. Because of this, it will be difficult to predict how many households must be initially selected to produce a probability sample of 1,000 births in each of the NCS sites. Recommendation 4-1: The NCS should consider modifying the sampling design to allow for flexibility in increasing the number of study participants in the event that the estimated number of screened households needed to reach 1,000 births per primary sampling unit (PSU) is incorrect. Recommendation 4-2: The NCS should consider the proposed household enumeration approach to be experimental and should conduct carefully designed field studies to clearly establish the statistical and practical implications of the proposed adjudicated listing approach. Recommendation 4-3: To ensure a diverse exposure profile in the sample, the NCS should consider a careful assessment of variation in ambient exposure to chemical agents within each PSU. If the set of segments in a PSU can be classified by combined exposure to a group of important chemical agents, this information could then be used to form varying exposure-level strata for segment sampling in each PSU and thus ensure a range of ambient exposure to relevant environmental agents.
Data Collection
Conclusion 4-4: The data collection model adopted by the NCS is complex, will challenge the abilities of the staff and coordinating center to achieve a uniform and consistent national data collection, and may compromise key study objectives. Conclusion 4-5: The NCS research plan does not provide sufficient information on the use of data collection guidelines and quality-control procedures to enable evaluation of the planned implementation of a uniform national data collection system. Conclusion 4-6: The NCS research plan does not address directly the issue of respondent burden, except to say that “some” effort is being made to reduce it, nor does the plan make clear the total number of hours the respondent must commit to the study. In particular, in light of the estimate of the interview length (4 hours) for the baseline interview, a critical collection for the study, the research plan pays little attention to respondent burden and its impact on the quality of the data. Conclusion 4-7: The NCS research plan provides little information concerning best methods for sample recruitment to achieve initial and follow-up target response rates, sample maintenance and sample retention procedures for implementation at the study sites, community involvement plans consistent with the uniform implementation of data collection procedures, or contingency plans to support study sites that do not achieve target response rates. Conclusion 4-8: The NCS research plan does not address the ongoing methodological needs of the study—to study data collection procedures and instruments, conduct experiments, and evaluate the quality of the survey operations and the quality of the data—nor does the plan make the best use of the Vanguard Centers. Recommendation 4-4: The NCS should consider ways in which the survey data collection could be consolidated into a smaller number of highly qualified survey organizations. Recommendation 4-5: Because of the complexity of the proposed organizational model for data collection and the difficulty of maintaining the quality and uniformity of data collection procedures across a large number of study sites, the NCS program office should establish and monitor strict standards for enrollment, retention, and data collection at each of the study sites and be prepared to take immediate corrective action if sites do not meet high-quality standards in data collection. Recommendation 4-6: The NCS should prepare a plan for monitoring progress of the study in reaching its sample size goals. As part of the plan, the NCS should take advantage of the experience of the Vanguard Centers to evaluate initial enrollment rates, the effectiveness and potential respondent burden of the interview instrument, and the ability of the Vanguard Centers to obtain the required household environmental measures reliably. Recommendation 4-7: To resolve issues that arise during data collection, the NCS should set aside sufficient resources to maintain an ongoing program of methods research and field experimentation. Among the issues that might be addressed in this research are the reliability and validity of previously untested survey questions and measurement strategies, the effectiveness of sample retention procedures, predictors of response outcomes associated with sample initial recruitment and subsequent annual retention, error implications of unit nonresponse, adjustment strategies for unit nonresponse, and methods for dealing with item nonresponse.
Data Analysis and Dissemination
Recommendation 4-8: The NCS should begin planning for the rapid dissemination of the core study data, subject to respondent protection, to the general research community and for supporting the use of the data after dissemination. The costs of implementing this plan should be estimated and set aside in future NCS budgets. Dissemination includes not only the publication of findings through reports and scientific papers and the production of documented data files for researchers, but also active support in the use of NCS data by the broadest possible range of qualified investigators.
CHAPTER 5: ETHICAL PROCEDURES AND COMMUNITY ENGAGEMENT
Criteria for giving information to participants.
Recommendation 5-1: The NCS should define the criteria and the process for deciding what individual clinical and research information, such as environmental assessments, test results, and survey scales, will be given to children and their families.
Protection and Release of Information
Recommendation 5-2: NCS and non-NCS investigators should be given equal access to the full NCS data as soon as they are cleaned and documented. To protect respondent confidentiality, all analyses should be performed with the kind of strict safeguards employed by the Census Bureau research data centers.
Community Engagement
Recommendation 5-3: The NCS should engage communities in selected study implementation, data analysis, and data interpretation activities that go beyond recruitment. The NCS should consider requiring every study center to formulate a more detailed plan to engage and collaborate with local communities.
In summary, it is clear from our review that the NCS offers not only enormous potential, but also a large number of conceptual, methodological, and administrative challenges. In addition, funding uncertainties make it difficult to plan beyond the relatively short period for which funds have been appropriated. Like the scientists associated with the study itself, we are eager for it to succeed. We present our conclusions and recommendations in the hope that, as it goes forward, the NCS will achieve its intended objectives and serve as a model of methodological and substantive contributions to important scientific and policy discussions on children’s health and development.
- Cite this Page National Research Council (US) and Institute of Medicine (US) Panel to Review the National Children's Study Research Plan. The National Children's Study Research Plan: A Review. Washington (DC): National Academies Press (US); 2008. 6, Conclusions and Recommendations.
- PDF version of this title (784K)
In this Page
- NCS GOALS, CONCEPTUAL FRAMEWORK, AND CORE HYPOTHESES
- PRIORITY OUTCOME AND EXPOSURE MEASURES
- STUDY DESIGN, DATA COLLECTION, AND ANALYSIS
- ETHICAL PROCEDURES AND COMMUNITY ENGAGEMENT
Other titles in this collection
- The National Academies Collection: Reports funded by National Institutes of Health
Recent Activity
- Conclusions and Recommendations - The National Children's Study Research Plan Conclusions and Recommendations - The National Children's Study Research Plan
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

- Walden University
- Faculty Portal
Reference List: Common Reference List Examples
Article (with doi).
Alvarez, E., & Tippins, S. (2019). Socialization agents that Puerto Rican college students use to make financial decisions. Journal of Social Change , 11 (1), 75–85. https://doi.org/10.5590/JOSC.2019.11.1.07
Laplante, J. P., & Nolin, C. (2014). Consultas and socially responsible investing in Guatemala: A case study examining Maya perspectives on the Indigenous right to free, prior, and informed consent. Society & Natural Resources , 27 , 231–248. https://doi.org/10.1080/08941920.2013.861554
Use the DOI number for the source whenever one is available. DOI stands for "digital object identifier," a number specific to the article that can help others locate the source. In APA 7, format the DOI as a web address. Active hyperlinks for DOIs and URLs should be used for documents meant for screen reading. Present these hyperlinks in blue and underlined text (the default formatting in Microsoft Word), although plain black text is also acceptable. Be consistent in your formatting choice for DOIs and URLs throughout your reference list. Also see our Quick Answer FAQ, "Can I use the DOI format provided by library databases?"
Jerrentrup, A., Mueller, T., Glowalla, U., Herder, M., Henrichs, N., Neubauer, A., & Schaefer, J. R. (2018). Teaching medicine with the help of “Dr. House.” PLoS ONE , 13 (3), Article e0193972. https://doi.org/10.1371/journal.pone.0193972
For journal articles that are assigned article numbers rather than page ranges, include the article number in place of the page range.
For more on citing electronic resources, see Electronic Sources References .
Article (Without DOI)
Found in a common academic research database or in print.
Casler , T. (2020). Improving the graduate nursing experience through support on a social media platform. MEDSURG Nursing , 29 (2), 83–87.
If an article does not have a DOI and you retrieved it from a common academic research database through the university library, there is no need to include any additional electronic retrieval information. The reference list entry looks like the entry for a print copy of the article. (This format differs from APA 6 guidelines that recommended including the URL of a journal's homepage when the DOI was not available.) Note that APA 7 has additional guidance on reference list entries for articles found only in specific databases or archives such as Cochrane Database of Systematic Reviews, UpToDate, ProQuest Dissertations and Theses Global, and university archives. See APA 7, Section 9.30 for more information.
Found on an Open Access Website
Eaton, T. V., & Akers, M. D. (2007). Whistleblowing and good governance. CPA Journal , 77 (6), 66–71. http://archives.cpajournal.com/2007/607/essentials/p58.htm
Provide the direct web address/URL to a journal article found on the open web, often on an open access journal's website. In APA 7, active hyperlinks for DOIs and URLs should be used for documents meant for screen reading. Present these hyperlinks in blue and underlined text (the default formatting in Microsoft Word), although plain black text is also acceptable. Be consistent in your formatting choice for DOIs and URLs throughout your reference list.
Weinstein, J. A. (2010). Social change (3rd ed.). Rowman & Littlefield.
If the book has an edition number, include it in parentheses after the title of the book. If the book does not list any edition information, do not include an edition number. The edition number is not italicized.
American Nurses Association. (2015). Nursing: Scope and standards of practice (3rd ed.).
If the author and publisher are the same, only include the author in its regular place and omit the publisher.
Lencioni, P. (2012). The advantage: Why organizational health trumps everything else in business . Jossey-Bass. https://amzn.to/343XPSJ
As a change from APA 6 to APA 7, it is no longer necessary to include the ebook format in the title. However, if you listened to an audiobook and the content differs from the text version (e.g., abridged content) or your discussion highlights elements of the audiobook (e.g., narrator's performance), then note that it is an audiobook in the title element in brackets. For ebooks and online audiobooks, also include the DOI number (if available) or nondatabase URL but leave out the electronic retrieval element if the ebook was found in a common academic research database, as with journal articles. APA 7 allows for the shortening of long DOIs and URLs, as shown in this example. See APA 7, Section 9.36 for more information.

Chapter in an Edited Book
Poe, M. (2017). Reframing race in teaching writing across the curriculum. In F. Condon & V. A. Young (Eds.), Performing antiracist pedagogy in rhetoric, writing, and communication (pp. 87–105). University Press of Colorado.
Include the page numbers of the chapter in parentheses after the book title.
Christensen, L. (2001). For my people: Celebrating community through poetry. In B. Bigelow, B. Harvey, S. Karp, & L. Miller (Eds.), Rethinking our classrooms: Teaching for equity and justice (Vol. 2, pp. 16–17). Rethinking Schools.
Also include the volume number or edition number in the parenthetical information after the book title when relevant.
Freud, S. (1961). The ego and the id. In J. Strachey (Ed.), The standard edition of the complete psychological works of Sigmund Freud (Vol. 19, pp. 3-66). Hogarth Press. (Original work published 1923)
When a text has been republished as part of an anthology collection, after the author’s name include the date of the version that was read. At the end of the entry, place the date of the original publication inside parenthesis along with the note “original work published.” For in-text citations of republished work, use both dates in the parenthetical citation, original date first with a slash separating the years, as in this example: Freud (1923/1961). For more information on reprinted or republished works, see APA 7, Sections 9.40-9.41.
Classroom Resources
Citing classroom resources.
If you need to cite content found in your online classroom, use the author (if there is one listed), the year of publication (if available), the title of the document, and the main URL of Walden classrooms. For example, you are citing study notes titled "Health Effects of Exposure to Forest Fires," but you do not know the author's name, your reference entry will look like this:
Health effects of exposure to forest fires [Lecture notes]. (2005). Walden University Canvas. https://waldenu.instructure.com
If you do know the author of the document, your reference will look like this:
Smith, A. (2005). Health effects of exposure to forest fires [PowerPoint slides]. Walden University Canvas. https://waldenu.instructure.com
A few notes on citing course materials:
- [Lecture notes]
- [Course handout]
- [Study notes]
- It can be difficult to determine authorship of classroom documents. If an author is listed on the document, use that. If the resource is clearly a product of Walden (such as the course-based videos), use Walden University as the author. If you are unsure or if no author is indicated, place the title in the author spot, as above.
- If you cannot determine a date of publication, you can use n.d. (for "no date") in place of the year.
Note: The web location for Walden course materials is not directly retrievable without a password, and therefore, following APA guidelines, use the main URL for the class sites: https://class.waldenu.edu.
Citing Tempo Classroom Resources
Clear author:
Smith, A. (2005). Health effects of exposure to forest fires [PowerPoint slides]. Walden University Brightspace. https://mytempo.waldenu.edu
Unclear author:
Health effects of exposure to forest fires [Lecture notes]. (2005). Walden University Brightspace. https://mytempo.waldenu.edu
Conference Sessions and Presentations
Feinman, Y. (2018, July 27). Alternative to proctoring in introductory statistics community college courses [Poster presentation]. Walden University Research Symposium, Minneapolis, MN, United States. https://scholarworks.waldenu.edu/symposium2018/23/
Torgerson, K., Parrill, J., & Haas, A. (2019, April 5-9). Tutoring strategies for online students [Conference session]. The Higher Learning Commission Annual Conference, Chicago, IL, United States. http://onlinewritingcenters.org/scholarship/torgerson-parrill-haas-2019/
Dictionary Entry
Merriam-Webster. (n.d.). Leadership. In Merriam-Webster.com dictionary . Retrieved May 28, 2020, from https://www.merriam-webster.com/dictionary/leadership
When constructing a reference for an entry in a dictionary or other reference work that has no byline (i.e., no named individual authors), use the name of the group—the institution, company, or organization—as author (e.g., Merriam Webster, American Psychological Association, etc.). The name of the entry goes in the title position, followed by "In" and the italicized name of the reference work (e.g., Merriam-Webster.com dictionary , APA dictionary of psychology ). In this instance, APA 7 recommends including a retrieval date as well for this online source since the contents of the page change over time. End the reference entry with the specific URL for the defined word.
Discussion Board Post
Osborne, C. S. (2010, June 29). Re: Environmental responsibility [Discussion post]. Walden University Canvas. https://waldenu.instructure.com
Dissertations or Theses
Retrieved From a Database
Nalumango, K. (2019). Perceptions about the asylum-seeking process in the United States after 9/11 (Publication No. 13879844) [Doctoral dissertation, Walden University]. ProQuest Dissertations and Theses.
Retrieved From an Institutional or Personal Website
Evener. J. (2018). Organizational learning in libraries at for-profit colleges and universities [Doctoral dissertation, Walden University]. ScholarWorks. https://scholarworks.waldenu.edu/cgi/viewcontent.cgi?article=6606&context=dissertations
Unpublished Dissertation or Thesis
Kirwan, J. G. (2005). An experimental study of the effects of small-group, face-to-face facilitated dialogues on the development of self-actualization levels: A movement towards fully functional persons [Unpublished doctoral dissertation]. Saybrook Graduate School and Research Center.
For further examples and information, see APA 7, Section 10.6.
Legal Material
For legal references, APA follows the recommendations of The Bluebook: A Uniform System of Citation , so if you have any questions beyond the examples provided in APA, seek out that resource as well.
Court Decisions
Reference format:
Name v. Name, Volume Reporter Page (Court Date). URL
Sample reference entry:
Brown v. Board of Education, 347 U.S. 483 (1954). https://www.oyez.org/cases/1940-1955/347us483
Sample citation:
In Brown v. Board of Education (1954), the Supreme Court ruled racial segregation in schools unconstitutional.
Note: Italicize the case name when it appears in the text of your paper.
Name of Act, Title Source § Section Number (Year). URL
Sample reference entry for a federal statute:
Individuals With Disabilities Education Act, 20 U.S.C. § 1400 et seq. (2004). https://www.congress.gov/108/plaws/publ446/PLAW-108publ446.pdf
Sample reference entry for a state statute:
Minnesota Nurse Practice Act, Minn. Stat. §§ 148.171 et seq. (2019). https://www.revisor.mn.gov/statutes/cite/148.171
Sample citation: Minnesota nurses must maintain current registration in order to practice (Minnesota Nurse Practice Act, 2010).
Note: The § symbol stands for "section." Use §§ for sections (plural). To find this symbol in Microsoft Word, go to "Insert" and click on Symbol." Look in the Latin 1-Supplement subset. Note: U.S.C. stands for "United States Code." Note: The Latin abbreviation " et seq. " means "and what follows" and is used when the act includes the cited section and ones that follow. Note: List the chapter first followed by the section or range of sections.
Unenacted Bills and Resolutions
(Those that did not pass and become law)
Title [if there is one], bill or resolution number, xxx Cong. (year). URL
Sample reference entry for Senate bill:
Anti-Phishing Act, S. 472, 109th Cong. (2005). https://www.congress.gov/bill/109th-congress/senate-bill/472
Sample reference entry for House of Representatives resolution:
Anti-Phishing Act, H.R. 1099, 109th Cong. (2005). https://www.congress.gov/bill/109th-congress/house-bill/1099
The Anti-Phishing Act (2005) proposed up to 5 years prison time for people running Internet scams.
These are the three legal areas you may be most apt to cite in your scholarly work. For more examples and explanation, see APA 7, Chapter 11.
Magazine Article
Clay, R. (2008, June). Science vs. ideology: Psychologists fight back about the misuse of research. Monitor on Psychology , 39 (6). https://www.apa.org/monitor/2008/06/ideology
Note that for citations, include only the year: Clay (2008). For magazine articles retrieved from a common academic research database, leave out the URL. For magazine articles from an online news website that is not an online version of a print magazine, follow the format for a webpage reference list entry.
Newspaper Article (Retrieved Online)
Baker, A. (2014, May 7). Connecticut students show gains in national tests. New York Times . http://www.nytimes.com/2014/05/08/nyregion/national-assessment-of-educational-progress-results-in-Connecticut-and-New-Jersey.html
Include the full date in the format Year, Month Day. Do not include a retrieval date for periodical sources found on websites. Note that for citations, include only the year: Baker (2014). For newspaper articles retrieved from a common academic research database, leave out the URL. For newspaper articles from an online news website that is not an online version of a print newspaper, follow the format for a webpage reference list entry.
OASIS Resources
Oasis webpage.
OASIS. (n.d.). Common reference list examples . Walden University. https://academicguides.waldenu.edu/writingcenter/apa/references/examples
For all OASIS content, list OASIS as the author. Because OASIS webpages do not include publication dates, use “n.d.” for the year.
Interactive Guide
OASIS. (n.d.). Embrace iterative research and writing [Interactive guide]. Walden University. https://academics.waldenu.edu/oasis/iterative-research-writing-web
For OASIS multimedia resources, such as interactive guides, include a description of the resource in brackets after the title.
Online Video/Webcast
Walden University. (2013). An overview of learning [Video]. Walden University Canvas. https://waldenu.instructure.com
Use this format for online videos such as Walden videos in classrooms. Most of our classroom videos are produced by Walden University, which will be listed as the author in your reference and citation. Note: Some examples of audiovisual materials in the APA manual show the word “Producer” in parentheses after the producer/author area. In consultation with the editors of the APA manual, we have determined that parenthetical is not necessary for the videos in our courses. The manual itself is unclear on the matter, however, so either approach should be accepted. Note that the speaker in the video does not appear in the reference list entry, but you may want to mention that person in your text. For instance, if you are viewing a video where Tobias Ball is the speaker, you might write the following: Tobias Ball stated that APA guidelines ensure a consistent presentation of information in student papers (Walden University, 2013). For more information on citing the speaker in a video, see our page on Common Citation Errors .
Taylor, R. [taylorphd07]. (2014, February 27). Scales of measurement [Video]. YouTube. https://www.youtube.com/watch?v=PDsMUlexaMY
OASIS. (2020, April 15). One-way ANCOVA: Introduction [Video]. YouTube. https://youtu.be/_XnNDQ5CNW8
For videos from streaming sites, use the person or organization who uploaded the video in the author space to ensure retrievability, whether or not that person is the speaker in the video. A username can be provided in square brackets. As a change from APA 6 to APA 7, include the publisher after the title, and do not use "Retrieved from" before the URL. See APA 7, Section 10.12 for more information and examples.
See also reference list entry formats for TED Talks .
Technical and Research Reports
Edwards, C. (2015). Lighting levels for isolated intersections: Leading to safety improvements (Report No. MnDOT 2015-05). Center for Transportation Studies. http://www.cts.umn.edu/Publications/ResearchReports/reportdetail.html?id=2402
Technical and research reports by governmental agencies and other research institutions usually follow a different publication process than scholarly, peer-reviewed journals. However, they present original research and are often useful for research papers. Sometimes, researchers refer to these types of reports as gray literature , and white papers are a type of this literature. See APA 7, Section 10.4 for more information.
Reference list entires for TED Talks follow the usual guidelines for multimedia content found online. There are two common places to find TED talks online, with slightly different reference list entry formats for each.
TED Talk on the TED website
If you find the TED Talk on the TED website, follow the format for an online video on an organizational website:
Owusu-Kesse, K. (2020, June). 5 needs that any COVID-19 response should meet [Video]. TED Conferences. https://www.ted.com/talks/kwame_owusu_kesse_5_needs_that_any_covid_19_response_should_meet
The speaker is the author in the reference list entry if the video is posted on the TED website. For citations, use the speaker's surname.
TED Talk on YouTube
If you find the TED Talk on YouTube or another streaming video website, follow the usual format for streaming video sites:
TED. (2021, February 5). The shadow pandemic of domestic violence during COVID-19 | Kemi DaSilvalbru [Video]. YouTube. https://www.youtube.com/watch?v=PGdID_ICFII
TED is the author in the reference list entry if the video is posted on YouTube since it is the channel on which the video is posted. For citations, use TED as the author.
Walden University Course Catalog
To include the Walden course catalog in your reference list, use this format:
Walden University. (2020). 2019-2020 Walden University catalog . https://catalog.waldenu.edu/index.php
If you cite from a specific portion of the catalog in your paper, indicate the appropriate section and paragraph number in your text:
...which reflects the commitment to social change expressed in Walden University's mission statement (Walden University, 2020, Vision, Mission, and Goals section, para. 2).
And in the reference list:
Walden University. (2020). Vision, mission, and goals. In 2019-2020 Walden University catalog. https://catalog.waldenu.edu/content.php?catoid=172&navoid=59420&hl=vision&returnto=search
Vartan, S. (2018, January 30). Why vacations matter for your health . CNN. https://www.cnn.com/travel/article/why-vacations-matter/index.html
For webpages on the open web, include the author, date, webpage title, organization/site name, and URL. (There is a slight variation for online versions of print newspapers or magazines. For those sources, follow the models in the previous sections of this page.)
American Federation of Teachers. (n.d.). Community schools . http://www.aft.org/issues/schoolreform/commschools/index.cfm
If there is no specified author, then use the organization’s name as the author. In such a case, there is no need to repeat the organization's name after the title.
In APA 7, active hyperlinks for DOIs and URLs should be used for documents meant for screen reading. Present these hyperlinks in blue and underlined text (the default formatting in Microsoft Word), although plain black text is also acceptable. Be consistent in your formatting choice for DOIs and URLs throughout your reference list.
Related Resources
Knowledge Check: Common Reference List Examples
Didn't find what you need? Email us at [email protected] .
- Previous Page: Reference List: Overview
- Next Page: Common Military Reference List Examples
- Office of Student Disability Services
Walden Resources
Departments.
- Academic Residencies
- Academic Skills
- Career Planning and Development
- Customer Care Team
- Field Experience
- Military Services
- Student Success Advising
- Writing Skills
Centers and Offices
- Center for Social Change
- Office of Academic Support and Instructional Services
- Office of Degree Acceleration
- Office of Research and Doctoral Services
- Office of Student Affairs
Student Resources
- Doctoral Writing Assessment
- Form & Style Review
- Quick Answers
- ScholarWorks
- SKIL Courses and Workshops
- Walden Bookstore
- Walden Catalog & Student Handbook
- Student Safety/Title IX
- Legal & Consumer Information
- Website Terms and Conditions
- Cookie Policy
- Accessibility
- Accreditation
- State Authorization
- Net Price Calculator
- Contact Walden
Walden University is a member of Adtalem Global Education, Inc. www.adtalem.com Walden University is certified to operate by SCHEV © 2024 Walden University LLC. All rights reserved.
Get science-backed answers as you write with Paperpal's Research feature
How to Write a Conclusion for Research Papers (with Examples)
The conclusion of a research paper is a crucial section that plays a significant role in the overall impact and effectiveness of your research paper. However, this is also the section that typically receives less attention compared to the introduction and the body of the paper. The conclusion serves to provide a concise summary of the key findings, their significance, their implications, and a sense of closure to the study. Discussing how can the findings be applied in real-world scenarios or inform policy, practice, or decision-making is especially valuable to practitioners and policymakers. The research paper conclusion also provides researchers with clear insights and valuable information for their own work, which they can then build on and contribute to the advancement of knowledge in the field.
The research paper conclusion should explain the significance of your findings within the broader context of your field. It restates how your results contribute to the existing body of knowledge and whether they confirm or challenge existing theories or hypotheses. Also, by identifying unanswered questions or areas requiring further investigation, your awareness of the broader research landscape can be demonstrated.
Remember to tailor the research paper conclusion to the specific needs and interests of your intended audience, which may include researchers, practitioners, policymakers, or a combination of these.
Table of Contents
What is a conclusion in a research paper, summarizing conclusion, editorial conclusion, externalizing conclusion, importance of a good research paper conclusion, how to write a conclusion for your research paper, research paper conclusion examples.
- How to write a research paper conclusion with Paperpal?
Frequently Asked Questions
A conclusion in a research paper is the final section where you summarize and wrap up your research, presenting the key findings and insights derived from your study. The research paper conclusion is not the place to introduce new information or data that was not discussed in the main body of the paper. When working on how to conclude a research paper, remember to stick to summarizing and interpreting existing content. The research paper conclusion serves the following purposes: 1
- Warn readers of the possible consequences of not attending to the problem.
- Recommend specific course(s) of action.
- Restate key ideas to drive home the ultimate point of your research paper.
- Provide a “take-home” message that you want the readers to remember about your study.

Types of conclusions for research papers
In research papers, the conclusion provides closure to the reader. The type of research paper conclusion you choose depends on the nature of your study, your goals, and your target audience. I provide you with three common types of conclusions:
A summarizing conclusion is the most common type of conclusion in research papers. It involves summarizing the main points, reiterating the research question, and restating the significance of the findings. This common type of research paper conclusion is used across different disciplines.
An editorial conclusion is less common but can be used in research papers that are focused on proposing or advocating for a particular viewpoint or policy. It involves presenting a strong editorial or opinion based on the research findings and offering recommendations or calls to action.
An externalizing conclusion is a type of conclusion that extends the research beyond the scope of the paper by suggesting potential future research directions or discussing the broader implications of the findings. This type of conclusion is often used in more theoretical or exploratory research papers.
Align your conclusion’s tone with the rest of your research paper. Start Writing with Paperpal Now!
The conclusion in a research paper serves several important purposes:
- Offers Implications and Recommendations : Your research paper conclusion is an excellent place to discuss the broader implications of your research and suggest potential areas for further study. It’s also an opportunity to offer practical recommendations based on your findings.
- Provides Closure : A good research paper conclusion provides a sense of closure to your paper. It should leave the reader with a feeling that they have reached the end of a well-structured and thought-provoking research project.
- Leaves a Lasting Impression : Writing a well-crafted research paper conclusion leaves a lasting impression on your readers. It’s your final opportunity to leave them with a new idea, a call to action, or a memorable quote.

Writing a strong conclusion for your research paper is essential to leave a lasting impression on your readers. Here’s a step-by-step process to help you create and know what to put in the conclusion of a research paper: 2
- Research Statement : Begin your research paper conclusion by restating your research statement. This reminds the reader of the main point you’ve been trying to prove throughout your paper. Keep it concise and clear.
- Key Points : Summarize the main arguments and key points you’ve made in your paper. Avoid introducing new information in the research paper conclusion. Instead, provide a concise overview of what you’ve discussed in the body of your paper.
- Address the Research Questions : If your research paper is based on specific research questions or hypotheses, briefly address whether you’ve answered them or achieved your research goals. Discuss the significance of your findings in this context.
- Significance : Highlight the importance of your research and its relevance in the broader context. Explain why your findings matter and how they contribute to the existing knowledge in your field.
- Implications : Explore the practical or theoretical implications of your research. How might your findings impact future research, policy, or real-world applications? Consider the “so what?” question.
- Future Research : Offer suggestions for future research in your area. What questions or aspects remain unanswered or warrant further investigation? This shows that your work opens the door for future exploration.
- Closing Thought : Conclude your research paper conclusion with a thought-provoking or memorable statement. This can leave a lasting impression on your readers and wrap up your paper effectively. Avoid introducing new information or arguments here.
- Proofread and Revise : Carefully proofread your conclusion for grammar, spelling, and clarity. Ensure that your ideas flow smoothly and that your conclusion is coherent and well-structured.
Write your research paper conclusion 2x faster with Paperpal. Try it now!
Remember that a well-crafted research paper conclusion is a reflection of the strength of your research and your ability to communicate its significance effectively. It should leave a lasting impression on your readers and tie together all the threads of your paper. Now you know how to start the conclusion of a research paper and what elements to include to make it impactful, let’s look at a research paper conclusion sample.

How to write a research paper conclusion with Paperpal?
A research paper conclusion is not just a summary of your study, but a synthesis of the key findings that ties the research together and places it in a broader context. A research paper conclusion should be concise, typically around one paragraph in length. However, some complex topics may require a longer conclusion to ensure the reader is left with a clear understanding of the study’s significance. Paperpal, an AI writing assistant trusted by over 800,000 academics globally, can help you write a well-structured conclusion for your research paper.
- Sign Up or Log In: Create a new Paperpal account or login with your details.
- Navigate to Features : Once logged in, head over to the features’ side navigation pane. Click on Templates and you’ll find a suite of generative AI features to help you write better, faster.
- Generate an outline: Under Templates, select ‘Outlines’. Choose ‘Research article’ as your document type.
- Select your section: Since you’re focusing on the conclusion, select this section when prompted.
- Choose your field of study: Identifying your field of study allows Paperpal to provide more targeted suggestions, ensuring the relevance of your conclusion to your specific area of research.
- Provide a brief description of your study: Enter details about your research topic and findings. This information helps Paperpal generate a tailored outline that aligns with your paper’s content.
- Generate the conclusion outline: After entering all necessary details, click on ‘generate’. Paperpal will then create a structured outline for your conclusion, to help you start writing and build upon the outline.
- Write your conclusion: Use the generated outline to build your conclusion. The outline serves as a guide, ensuring you cover all critical aspects of a strong conclusion, from summarizing key findings to highlighting the research’s implications.
- Refine and enhance: Paperpal’s ‘Make Academic’ feature can be particularly useful in the final stages. Select any paragraph of your conclusion and use this feature to elevate the academic tone, ensuring your writing is aligned to the academic journal standards.
By following these steps, Paperpal not only simplifies the process of writing a research paper conclusion but also ensures it is impactful, concise, and aligned with academic standards. Sign up with Paperpal today and write your research paper conclusion 2x faster .
The research paper conclusion is a crucial part of your paper as it provides the final opportunity to leave a strong impression on your readers. In the research paper conclusion, summarize the main points of your research paper by restating your research statement, highlighting the most important findings, addressing the research questions or objectives, explaining the broader context of the study, discussing the significance of your findings, providing recommendations if applicable, and emphasizing the takeaway message. The main purpose of the conclusion is to remind the reader of the main point or argument of your paper and to provide a clear and concise summary of the key findings and their implications. All these elements should feature on your list of what to put in the conclusion of a research paper to create a strong final statement for your work.
A strong conclusion is a critical component of a research paper, as it provides an opportunity to wrap up your arguments, reiterate your main points, and leave a lasting impression on your readers. Here are the key elements of a strong research paper conclusion: 1. Conciseness : A research paper conclusion should be concise and to the point. It should not introduce new information or ideas that were not discussed in the body of the paper. 2. Summarization : The research paper conclusion should be comprehensive enough to give the reader a clear understanding of the research’s main contributions. 3 . Relevance : Ensure that the information included in the research paper conclusion is directly relevant to the research paper’s main topic and objectives; avoid unnecessary details. 4 . Connection to the Introduction : A well-structured research paper conclusion often revisits the key points made in the introduction and shows how the research has addressed the initial questions or objectives. 5. Emphasis : Highlight the significance and implications of your research. Why is your study important? What are the broader implications or applications of your findings? 6 . Call to Action : Include a call to action or a recommendation for future research or action based on your findings.
The length of a research paper conclusion can vary depending on several factors, including the overall length of the paper, the complexity of the research, and the specific journal requirements. While there is no strict rule for the length of a conclusion, but it’s generally advisable to keep it relatively short. A typical research paper conclusion might be around 5-10% of the paper’s total length. For example, if your paper is 10 pages long, the conclusion might be roughly half a page to one page in length.
In general, you do not need to include citations in the research paper conclusion. Citations are typically reserved for the body of the paper to support your arguments and provide evidence for your claims. However, there may be some exceptions to this rule: 1. If you are drawing a direct quote or paraphrasing a specific source in your research paper conclusion, you should include a citation to give proper credit to the original author. 2. If your conclusion refers to or discusses specific research, data, or sources that are crucial to the overall argument, citations can be included to reinforce your conclusion’s validity.
The conclusion of a research paper serves several important purposes: 1. Summarize the Key Points 2. Reinforce the Main Argument 3. Provide Closure 4. Offer Insights or Implications 5. Engage the Reader. 6. Reflect on Limitations
Remember that the primary purpose of the research paper conclusion is to leave a lasting impression on the reader, reinforcing the key points and providing closure to your research. It’s often the last part of the paper that the reader will see, so it should be strong and well-crafted.
- Makar, G., Foltz, C., Lendner, M., & Vaccaro, A. R. (2018). How to write effective discussion and conclusion sections. Clinical spine surgery, 31(8), 345-346.
- Bunton, D. (2005). The structure of PhD conclusion chapters. Journal of English for academic purposes , 4 (3), 207-224.
Paperpal is a comprehensive AI writing toolkit that helps students and researchers achieve 2x the writing in half the time. It leverages 21+ years of STM experience and insights from millions of research articles to provide in-depth academic writing, language editing, and submission readiness support to help you write better, faster.
Get accurate academic translations, rewriting support, grammar checks, vocabulary suggestions, and generative AI assistance that delivers human precision at machine speed. Try for free or upgrade to Paperpal Prime starting at US$19 a month to access premium features, including consistency, plagiarism, and 30+ submission readiness checks to help you succeed.
Experience the future of academic writing – Sign up to Paperpal and start writing for free!
Related Reads:
- 5 Reasons for Rejection After Peer Review
- Ethical Research Practices For Research with Human Subjects
7 Ways to Improve Your Academic Writing Process
- Paraphrasing in Academic Writing: Answering Top Author Queries
Preflight For Editorial Desk: The Perfect Hybrid (AI + Human) Assistance Against Compromised Manuscripts
You may also like, how to write a high-quality conference paper, academic editing: how to self-edit academic text with..., measuring academic success: definition & strategies for excellence, phd qualifying exam: tips for success , ai in education: it’s time to change the..., is it ethical to use ai-generated abstracts without..., what are journal guidelines on using generative ai..., quillbot review: features, pricing, and free alternatives, what is an academic paper types and elements , should you use ai tools like chatgpt for....
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Handwashing
- Hand Hygiene as a Family Activity
- Hand Hygiene FAQs
- Handwashing Facts
- Publications, Data, & Statistics
- Health Promotion Materials
- Global Handwashing Day
- Life is Better with Clean Hands Campaign
- Clinical Safety
- Healthcare Training
- Clean Hands Count Materials
About Handwashing
- Many diseases and conditions are spread by not washing hands with soap and clean, running water.
- Handwashing with soap is one of the best ways to stay healthy.
- If soap and water are not readily available, use a hand sanitizer with at least 60% alcohol to clean your hands.

Why it's important
Washing hands can keep you healthy and prevent the spread of respiratory and diarrheal infections. Germs can spread from person to person or from surfaces to people when you:
- Touch your eyes, nose, and mouth with unwashed hands
- Prepare or eat food and drinks with unwashed hands
- Touch surfaces or objects that have germs on them
- Blow your nose, cough, or sneeze into hands and then touch other people's hands or common objects
Key times to wash hands
You can help yourself and your loved ones stay healthy by washing your hands often, especially during these key times when you are likely to get and spread germs:
- Before, during, and after preparing food
- Before and after eating food
- Before and after caring for someone at home who is sick with vomiting or diarrhea
- Before and after treating a cut or wound
- After using the toilet
- After changing diapers or cleaning up a child who has used the toilet
- After blowing your nose, coughing, or sneezing
- After touching an animal, animal feed, or animal waste
- After handling pet food or pet treats
- After touching garbage
How it works
Washing your hands is easy, and it’s one of the most effective ways to prevent the spread of germs. Follow these five steps every time.
- Wet your hands with clean, running water (warm or cold), turn off the tap, and apply soap.
- Lather your hands by rubbing them together with the soap. Lather the backs of your hands, between your fingers, and under your nails.
- Scrub your hands for at least 20 seconds . Need a timer? Hum the “Happy Birthday” song from beginning to end twice.
- Rinse your hands well under clean, running water.
- Dry your hands using a clean towel or an air dryer.
Use hand sanitizer when you can't use soap and water
Washing hands with soap and water is the best way to get rid of germs in most situations. If soap and water are not readily available, you can use an alcohol-based hand sanitizer that contains at least 60% alcohol. You can tell if the sanitizer contains at least 60% alcohol by looking at the product label.
What you can do
CDC has health promotion materials to encourage kids and adults to make handwashing part of their everyday lives.
- Share social media graphics and messages.
- Print stickers and place clings on bathroom mirrors.
- Promote handwashing on or around Global Handwashing Day , celebrated each year on October 15.
- Distribute fact sheets to share information about hand hygiene for specific audiences.
- Frequent Questions About Hand Hygiene
- Hand Hygiene in Healthcare Settings
- The Life is Better with Clean Hands Campaign
Clean Hands
Having clean hands is one of the best ways to avoid getting sick and prevent the spread of germs to others.
For Everyone
Health care providers.
- Open access
- Published: 10 May 2024
Adherence to sleep recommendations is associated with higher satisfaction with life among Norwegian adolescents
- Erik Grasaas 1 ,
- Sergej Ostojic 1 &
- Henriette Jahre 2
BMC Public Health volume 24 , Article number: 1288 ( 2024 ) Cite this article
267 Accesses
Metrics details
Sleep plays a crucial role in the health and well-being of adolescents; however, inadequate sleep is frequently reported in numerous countries. This current paper aimed to describe sleep duration, factors impacting sleep, consequences of insufficient sleep and satisfaction with life in Norwegian adolescents, stratified by sex and by adherence to the 8-hour sleep recommendation, and to examine potential associations between adherence to the 8-hours sleep recommendation and satisfaction with life.
This is a cross-sectional study using data from the Norwegian Ungdata Survey, collected in 2021. Adolescents from five Norwegian counties were included, comprising a total of 32,161 upper secondary school students. Study variables were collected through an electronic questionnaire administered during school hours and all data are anonymous. Descriptive data of sleep patterns are presented, and linear regressions were conducted adjusting for SES, perceived stress, physical activity level, over-the-counter analgesics use, grade level and screen time.
73% of adolescents did not adhere to the 8-hours of sleep recommendation per night, with similar results for girls and boys. 64% reported tiredness at school (minimum 1–2 days weekly) and 62% reported that screen time negatively affected their ability to sleep. 23% reported that gaming affected their sleep, with a higher prevalence in boys than girls. Satisfaction with life score was 7.0 ± 1.9 points (out of 10) for the total sample, with higher scores for boys (7.3 ± 1.8 points) than girls (6.9 ± 1.9 points). Regressions revealed a positive association with satisfaction with life (B = 0.31, 95% [0.15 to 0.48]) in adolescents adhering to sleep recommendation of 8h compared to the ones not adhering to the sleep recommendation.
Conclusions
Most Norwegian adolescents fail to adhere to the 8-hours of sleep recommendation and the majority feel tired at school or during activities. More than half of adolescents reported that screen time negatively affected their ability to sleep. Adhering to the sleep recommendation was associated with higher life satisfaction. Our findings highlight the importance of sufficient sleep in adolescents, while future research is needed to examine other sleep related measures on adolescents´ satisfaction with life.
Peer Review reports
Sleep is recognized as a crucial factor for children’s and adolescents’ health and wellbeing [ 1 ]. Sleep recommendation vary with age and according to the US National Sleep Foundation teenagers are recommended 8–10 h of sleep [ 2 ]. However, when Gariepy and colleagues examined sleep patterns in 24 European and North American Countries, including 165,793 adolescents, findings revealed that insufficient sleep is prevalent in many countries [ 3 ]. Insufficient sleep impacts the daytime functioning in adolescents, leading to various negative consequences in their lives [ 4 ]. Extensive research evidence has reported that insufficient sleep among adolescents increases the risk of physical, psychosocial, and behavioral problems, and is associated with worse health outcomes [ 4 , 5 , 6 , 7 , 8 , 9 ].
When examining sleep duration in adolescents, research evidence refers to both the time in bed (TIB) and the sleep onset time (SOT) until wakening as estimates of sleep duration. It is suggested that TIB might overestimate the sleep duration in adolescence [ 10 ], as adolescents don’t immediately fall asleep when they go to bed. The latency time from going to bed to SOT was reported to be on average around 17 min for older adolescents in 2002 [ 11 ]. However, considering the commonality of screen time use before bedtime nowadays, it is presumed that this average time has increased [ 12 , 13 ]. A recent Norwegian sleep study reported the average time between going to bed and SOT was over one hour, revealing that eight in ten adolescents in upper secondary school actually failed to obtain the minimum recommended amount of sleep (8 h) on school days [ 10 ].
Research evidence points to several causes of insufficient sleep in adolescence, which are commonly categorized into internal- and external factors. External factors may include reduced parental involvement, excessive homework or activities, perceived stress, and screen time usage, whereas internal factors refer to puberty and biological processes such as a shift in the circadian rhythm [ 4 , 14 , 15 , 16 , 17 , 18 ]. Regardless of its causes, insufficient sleep is reported to impact all aspects of adolescents’ daily life and wellbeing [ 4 , 5 , 6 , 7 , 9 , 14 , 16 , 17 , 19 , 20 , 21 ]. A well-known indicator of subjective well-being is Life Satisfaction measure, which serves as a useful complement for comparing data across ages and countries, and is assessed to evaluate their life as a whole rather than their current feelings [ 22 ]. Satisfaction with life is therefore a well-known measure to indicate happiness across countries and time [ 22 ]. According to Diener, the measure reflects the cognitive judgment of one´s satisfaction with life [ 23 ]. It has been reported that girls tend to report lower satisfaction with life compared to boys during adolescence, along with a general decrease in satisfaction with life throughout this period [ 24 ].
Since most Norwegian adolescents do not meet the recommended 8 h of sleep [ 10 ], it is crucial to investigate potential consequences for this age group. Since life satisfactions is a good indicator of adolescent’s well-being, and a proxy for happiness it would be interesting to investigate the relationship between sleep duration and satisfaction with life using large dataset with high response rate. Such research can provide substantial insights for both practice and policy development, potentially emphasizing the significance of adhering to the sleep recommendations in Norway. The main aims of the present study were (1) to describe sleep duration, factors impacting sleep, consequences of insufficient sleep and satisfaction with life in Norwegian adolescents, stratified by sex and by adherence to the 8-hour sleep recommendation, and (2) to examine potential association between adherence to the 8-hours of sleep recommendation and satisfaction with life in Norwegian adolescents.
We hypothesized that adolescents adhering to the 8-hour sleep recommendation would have a more positive association to satisfaction with life compared to adolescents sleeping seven hours or less.
This study is reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [ 25 ].
Study design
This is a cross-sectional study using data from the Norwegian Ungdata Survey, collected in 2021. Ungdata is conducted by Norwegian Social Research (NOVA) at Oslo Metropolitan University in collaboration with regional center for drug rehabilitation (KoRus) and the municipal sector’s organization (KS). It is a quality-assured system for carrying out repeated national surveys among pupils in lower and upper secondary schools related to all aspects of health and wellbeing [ 26 ].
The Ungdata survey includes adolescents from lower and upper secondary schools from almost all municipalities in Norway. The survey consists of a comprehensive electronic questionnaire, with a mandatory basic module for all the municipalities, and a set of optional, predefined questions, which municipalities and counties can choose from. In addition, self-composed questions may also be added by the municipalities, counties or collaborating universities. The Ungdata project is financed from the national budget through grants from the Norwegian Directorate of Health [ 26 ].
Ungdata is a free survey offered to all Norwegian counties and their respective municipalities. The yearly sampling is administered by including specific counties. Within the next two following years, the rest of the counties are recruited. According to Ungdata, within a three-year period, close to all Norwegian municipalities have participated in the survey [ 27 ]. Therefore, the national presented findings from Ungdata usually comprises data from the last three years, which results in a representative study sample for the whole target population. However, according to Ungdata, the survey from 2021 should be assessed more separately, due to the pandemic and due to the record high participation of municipalities this year [ 27 ]. In the supplementary information material provided by Ungdata, there are coding for different counties, municipalities, and schools. Indicating that schools were the primary sampling unit. However, the Ungdata dataset does not include a variable including the separate schools.
Study setting
The surveys take place during one school hour (45–55 min) and are carried out electronically by the respective teacher. Pupils who are not interested in taking the survey are provided other schoolwork. The research evidence extracted from the Ungdata Survey is well suited for planning and initiating work towards adolescents and public health [ 26 ].
Participants
Norwegian adolescents from upper secondary school (16–19 years of age) are included in this study. The response rate was 67% from the whole country [ 27 ]. Adolescents from five counties ( n = 32,161) are included in this specific study because they were the only counties that included sleep in their questionnaire (optional question). Number of participants were lower in questions regarding screentime/gaming affecting their sleep, as these questions were included in only two and three counties, respectively.
Exposure: sleep
Sleep duration was measured using the question “ How many hours of sleep did you get last night”. Seven response alternatives were provided, ranging from, 6 h or less or hourly up to 12 h or more. These response alternatives were recoded into a dichotomous variable to determine whether participants met (8 h or more) or did not meet (7 h or less) the international recommendations for sleep in adolescents [ 2 ]. Problems falling asleep and being tired in school or in activities was measured using four response alternatives, “no days”, “1–2 days”, “3–4 days” and “5 days or more”. If screentime or gaming affected their sleep was measured with two response alternatives, “yes” or “no”. These questions were formulated as: Has screentime affected you to not getting enough sleep and has gaming affected you to not getting enough sleep?
Outcome: satisfaction with life
Satisfaction with life was assessed using the question: “On a scale from 0 to10, how happy are you with your life these days?” Higher scores indicated greater satisfaction with life. This question on satisfaction with life was originally employed in a large Norwegian study called “Young in Oslo in 2018” [ 28 ], including 25,348 adolescents. Using a single-item measure for satisfaction with life has across samples demonstrated a substantial degree of validity and performed similar to the multiple-item satisfaction with life scale [ 29 ]. Especially in adolescence, its reported that a single-item life satisfaction measures perform as well the satisfaction with life scale [ 30 ].
Demographic variables and covariates
The Ungdata study includes demographic measures such as gender, grade level, respective county and municipality, and measures of socioeconomic status (SES). SES is measured by several questions related to parental educational level, books in their home and their level of prosperity. A total sum is calculated based on these three categories and recoded into values from 0 to 3, off which 0 represent lowest SES and 3 the highest SES [ 31 ]. This measure is reported as a validated construct of SES [ 26 ]. As the Ungdata Survey is anonymous, data on age is not available. For overview of study variables and response rate, see Table 1 .
Perceived stress level, physical activity level and use of over-the-counter analgesics (OTCA) are included as categorical covariates in the regression analysis [ 26 ].
Perceived stress level was measured by using the question “ Have you experience so much pressure the last week that you had problems managing it?” . Four response alternatives were provided, “not at all”, “to a small degree”, “to a large degree” and “to a very large degree” [ 26 ]. Perceived stress was found as a relevant psychological covariate in Norwegian adolescents due to the link to exposure and outcome [ 32 , 33 ].
Physical activity level was measured using the question “ How often are you so physical active that you become short of breath or sweaty? ” Six response alternatives were provided from “rare”, to different times a week, up to “at least 5 times a week” [ 26 ].
The use over OTCA was measured by using the question “How often have you used non-prescription drugs (Paracet, Ibux and similar) during the last month?” . Five response alternatives were provided ranging from “no times”, different times a week to “daily” [ 26 ].
Ethical consideration
Participation in the Ungdata survey is voluntary and informed written consent were provided by the adolescents. All questions from Ungdata included in this current study is approved by the Norwegian Agency for Shared Services in Education and Research (ref. 821,474), known as SIKT [ 34 ]. As the survey is conducted in May-June, adolescents in upper secondary school were 16 years or older and did not need parental consent. The study is conducted in accordance with the Helsinki Declaration.
Statistical analyses
All statistical analyses were conducted using IBM SPSS Statistics for Windows, Version 25.0 (IBM Corp., Armonk, NY, USA). For the descriptive measures, continuous variables are described using means and standard deviations (SDs), and categorical variables are presented with counts and percentages. Sleep variables are presented for the total study sample and stratified into girls and boys, and into those who achieved the recommended sleep duration or not. Linear regressions analyses were conducted to examine the association between achieving the recommended sleep duration (8 h or more) or not and satisfaction with life. Stratified regressions analyses for girls and boys were conducted to investigate potential sex differences in the associations. One sample proportion test revealed high precision (CI) in estimates across the descriptive study variables. Both crude and multiple regression analysis adjusted for SES, perceived stress, physical activity level, OTCA use, grade level and screen time are presented. The results are presented with beta coefficients with 95% confidence intervals and R-squared (R 2 ). P -values < 0.05 were considered statistically significant, and all tests were two‐sided. Sensitivity analysis using 7-hours as a cut-off were used to check the robustness of the results. Due to the large sample size and relatively small number of missing, no imputation or bootstrapping was considered necessary.
In total, 32,161 adolescents from five Counties in Norway were included in the analyses. Response rate remained high in selected study variables ranging from 92.5 to 99.9% (Table 1 ). More boys than girls participated (53% versus 47%), 42% of the participants were from 1st grade, 35% from 2nd grade, and 23% from 3rd grade (Table 2 ).
Descriptive data of sleep in Norwegian adolescents
Descriptive data of sleep variables are presented in Table 3 . 73% of adolescents did not adhere to the 8-hours of sleep recommendation, with similar results for girls and boys. 62% of respondents reported experiencing difficulties falling asleep on at least one day or more. This issue was more prevalent among girls (68%) than boys (56%). Feeling tired at school at least once a week was reported by 64%, by 71% of the girls and by 56% of the boys. 62% of participants stated that screen time negatively affected their ability to get enough sleep, 66% of girls and 57% of boys reported this. 23% of the adolescents reported that gaming affected their ability to get enough sleep, 11% of the girls and 38% of the boys. Satisfaction with life score was 7.0 ± 1.9 points for the total sample (Table 3 ), with higher scores for boys (7.3 ± 1.8 points) than in girls (6.9 ± 1.9 points) (Table 3 ).
Descriptive measures stratified by adhereing to the 8-hours of sleep recommendations or not showed that 54% of adolescents receiving more than 8 h of sleep had no problems with falling asleep, while 32% of adolescents that did not achieve sleep recommendation had these struggles.
50% of adolescents adhering to the recommended sleep duration reported that they never felt tired at school or in other activities, whereas this was reported by 30% of those who did not adhere to the recommendations. Screen time was descriptively reported to affect sufficient sleep in 45% of those who met the recommendations, and in 67% of those who did not. Gaming was descriptively reported to affect sleep for 15% of those who slept 8 h or more, and 26% in those who slept less (Table 4 ).
Associations between adhering to sleep recommendation or not on satisfaction with life
Adjusted multiple regression analysis stratified by sex showed that adhering to the recommended 8 h of sleep was positively associated with satisfaction with life in girls (B = 0.33; 95% CI [0.11–0.56]) and in boys (B = 0.27; 95% CI [0.02–0.52]) compared to those who did not adhere to the sleep recommendation (Table 5 ).
Crude regression analyses revealed a positive association between adhering to the 8-hours of sleep recommendation and satisfaction with life (B = 0.64; 95% CI [0.59–0.68]). Adjusted multiple regression analyses remained significant after adjusting for SES, perceived stress, physical activity level, OTCA use, grade level, screen time and sex (Table 6 ).
Sensitivity analyses
Adjusted sensitivity analysis using 7 h of sleep as a cut-off showed a stronger association with lower life satisfaction than 8 h of sleep for the total sample (B = 0.51 versus B = 0.31). Similar findings of stronger associations using 7 h cut-off were revealed in stratified analyses by gender, in boys (B = 0.39 versus 0.27) and girls (B = 0.60 versus B = 0.33).
In this study, we aimed to describe sleep duration, factors impacting sleep, consequences of insufficient sleep and satisfaction with life in Norwegian adolescents and examine possible associations between adherence to the 8-hours of sleep recommendation and satisfaction with life. Findings revealed that 73% of adolescents did not meet the recommended sleep duration of at least 8 h per night, with similar results for girls and boys. 64% reported that they felt tired at school or in activities, however more prevalent in girls than boys. Screen time had a negative impact for getting enough sleep in 62% and was more prevalent among girls than boys. Gaming disturbed sleep in 23% and was more prevalent among boys. Satisfaction with life score was 7 out of 10 for the total study sample, with somewhat higher scores for boys than girls. Adhering to the 8-hours sleep recommendation was positively associated with satisfaction with life, and there were similar findings in girls and boys. All findings remained statistically significant after adjusting for SES, perceived stress, physical activity level and OTCA use.
Our findings, revealing that 73% of the adolescents did not adhere to the 8-hours of sleep recommendation, are higher compared to international data, which shows that across countries, 32–86% of adolescents meet sleep recommendations [ 3 ]. However, not adhering to the sleep recommendation appears to be common in Norway. In a Norwegian study by Saxvig and colleagues, it was revealed that 84.8% of adolescents aged 16–17 did not adhere to the recommendation of 8-hour sleep [ 10 ]. These findings show a slightly higher prevalence compared to this current study, which may be due to several methodological differences in self-reporting. Saxvig and colleagues presents findings of sleep duration during schooldays, whereas the question provided by Ungdata refers to “how many hours did you sleep last night?”. Assuming that some Ungdata surveys were conducted on Mondays, the findings may be less comparable to data from schooldays, as adolescents commonly report a relatively large discrepancy between sleep duration on schooldays and weekends [ 35 ]. A recent Norwegian study from 2023 reported that younger Norwegian adolescents tend to sleep one and a half hours longer on weekends compared to schooldays [ 36 ]. Despite this, our findings point to the commonality of failing to obtain the recommendation of 8 h of sleep in the everyday life of Norwegian adolescents.
Estimating sleep duration by self-report in adolescence is challenging due to observed discrepancies between self-reported sleep and objectively measured sleep. However, research evidence suggests that adolescents aged 13–17 years may more precisely estimate their own sleep duration compared to when their parents report on their behalf, as parents tend to report an idealized version [ 37 ]. Objective measures, including actigraphy and the currently considered gold standard, polysomnography, offer potential clinical advantages compared to self-reporting [ 38 ]. However, these advantages are primarily related to pathological conditions, such as accurate diagnosis of sleep disorders and treatment monitoring. Lucas-Thompson and colleagues investigated the between- and within-person associations between self-reported and actigraph-measured nighttime sleep duration in adolescence [ 39 ]. The findings indicated that adolescents reporting longer average nighttime sleep also exhibited longer average actigraph measured sleep duration [ 39 ], suggesting that self-reporting in large samples of adolescence is likely to have high validity. Still, there are potential biases that should be discussed, which could be threating the validity of the study, such as self-report bias, including recall bias or social desirability bias. Despite the study is anonymous, there is no guarantee that adolescents´ didn’t under or overestimate their scores based on poor recollection or because of being afraid of observant classmates. Other relevant bias to mention is selection bias. Although the study includes the majority of Norwegian adolescents, findings may not accurately reflect the total target population.
Interestingly, our descriptive findings revealed similar sleep duration in girls and boys, which is in accordance with international data and other Norwegian sleep studies [ 10 , 36 , 40 ]. However, our descriptive findings revealed some differences in terms of feeling tired (sleepiness). Only 29% of girls reported they never felt sleepy during school or in activities, whereof 44% of the boys reported the same. There might be underlying mechanisms related to sleep quality or productivity differences between girls and boys that might interfere, or it could be related to other aspects of adolescents’ life, such as difference in physical activity levels and gender preferences for activities provided at schools. Nevertheless, Forest and colleagues also reported gender differences in daytime sleepiness during school and social activities in adolescents, with girls perceiving more interference from poor sleep on daytime functioning compared to boys [ 41 ]. Findings indicate other measures than sleep duration is needed for understanding daytime functioning in girls and boys. A meta-analytic review from a school setting, showed that sleepiness revealed the strongest association to school performance, followed by adolescents sleep quality and sleep duration [ 42 ].
Another gender difference was that more girls than boys reported that screen time negatively impacted their ability to sleep. It is reported that time spent in front of a screen usually comes at the expense of sleep [ 43 ]. The inability to sleep and screen time use at night are physiologically linked to the brightness and type of light, and such activity inhibit melatonin production, disrupt the circadian rhythm, and consequently affect adolescents´ feeling of sleepiness before bedtime [ 44 ]. Therefore, the systematic review by Hale et al., explicitly advises to limit or reduce screen time exposure, especially before or during bedtime hours, to minimize any harmful effects of screen time on sleep and well-being [ 13 ]. Moreover, Hale and colleagues reported that adolescents spend about 7 h per day in front of a screen [ 13 ]. Gaming might also contribute to the total screen time in adolescence. In our study, more boys than girls reported that gaming affected their ability to sleep. Time spent on video gaming in adolescence is also reported to be negatively associated with sleep duration [ 45 ].
It is interesting to link the differences in daytime sleepiness between girls and boys to the differences in satisfaction with life, as we suspect that there could be coinciding factors at play. Given that girls tend to experience more tiredness and sleepiness, it would presumably influence their subjective well-being and satisfaction with life, as sleepiness is strongly associated with adolescents’ overall quality of life [ 46 ]. Extensive research evidence has reported gender differences in health-related quality of life (HRQOL) and satisfaction with life, wherein girls tend to report lower scores than boys [ 24 , 47 , 48 , 49 , 50 ]. Moreover, our findings of satisfaction with life align with the “Better Life index” score from the OECD, which reports 7.3 as an average score for Norwegians [ 22 ]. Interestingly, in our study, both girls and those not adhering to the sleep recommendations had coinciding satisfaction with life scores below 7.0.
As hypothesized, the findings showed that adolescents adhering to the 8-hour sleep recommendation had higher life satisfaction compared to adolescents sleeping 7 h or less. Quite similar results were found in both girls and boys, despite a slightly lower p -value was revealed among girls compared to boys, both associations remained significant after adjusting for relevant covariates. Indicating respective associations relevant for the total study sample. Interestingly, a Norwegian study by Ness and Saksvik-Lehouillier investigated the relationship between sleep and satisfaction with life in Norwegian university students. Their results indicated that all sleep parameters, such as sleep quality, less variability in rise time, less variability in sleep duration, longer mean sleep duration were associated with better satisfaction with life. However, less variability of sleep duration was identified as a significant predictor for life satisfaction and not mean sleep duration, indicating that less variability of sleep duration might be more relevant to well-being than sleep duration itself [ 51 ]. Research evidence also reports higher risks of negative health outcomes with higher variability in sleep duration from weekdays to weekends in adolescents [ 35 , 52 ]. Further, a recent Norwegian study reported that sleep duration on weekdays was positively associated with all aspects of adolescents´ HRQOL, whereas sleep duration on weekends revealed mostly nonsignificant findings regarding aspects of HRQOL [ 36 ]. These findings highlight the vulnerability of using only one general sleep duration measure to understand the complexity between sleep and satisfaction with life. Nevertheless, our findings reinforce the importance of the 8-hours sleep recommendation for Norwegian adolescents. Sleep is a multifaceted concept, including different measures such as sleep variability, sleep quality and sleepiness, all of which can have distinct impacts on adolescents’ satisfaction with life. Therefore, it is worth exploring the possibility of sleep recommendations that encompass not only sleep duration, but also explicitly address sleep variability and daytime sleepiness in adolescence in the future.
Strengths and limitations
The primary strength of this study lies in its large sample size, comprising adolescents from both urban and rural regions of Norway, collected within a school-based setting. Additionally, the high response rate (99%) regarding variables related to sleep and life satisfaction enhances the study’s reliability. These factors suggest that the findings could be generalizable for a broader population of Norwegian adolescents attending school. The question regarding sleep duration is based on SOT until awakening time, which is considered an accurate estimation of sleep duration [ 10 ]. Further, Ungdata dataset is cleaned and they have several procedures for identifying unserious answers [ 26 ]. Moreover, reporting according to STROBE guidelines [ 25 ] should be considered a strength, as it provides transparency and accurate reporting of study method and results.
This study also has some limitations. The cross-sectional nature of the study hinders us from determining any causal inference between sleep duration and life satisfaction. Further, another limitation is the use of non-validated instruments regarding sleep as the respective questions in Ungdata derives from an unknown origin [ 27 ]. Moreover, the sleep questions did not distinguish between weekdays and weekends, which might have affected the results. Another limitation is that the scope of this paper was focused on adhering to sleep recommendations or not, and as a result, the sleep duration variable was dichotomized. This dichotomization reduced variability in data and excluded other potential sleep-related variables that could have impacted adolescents’ satisfaction with life. Another limitation is due to study variables are measured over different time frames, as exposure is measured within last day and outcome over a few days. The predicting sleep variable would be more robust if data was provided over a longer period, which would convey a better understanding of sleep variability and average sleep duration. Moreover, we do not have any information on the non-responders, which increases the risk of selection bias. Finally, despite significant statistical associations, caution should be exercised when interpeting the findings for clinical relevance. Still, sensitivity analysis using 7 h of sleep as a cut-off shows a stronger association with lower life satisfaction than 8 h of sleep. This might indicate that less sleep is more strongly related to lower life satisfaction. This should be further explored in future studies investigating sleep as a continuous variable. However, we chose to dichotomize the variable according to sleep recommendations to make it clear and easy to interpret for adolescents, practitioners, and policymakers.
Perspectives
This study showed that the majority of adolescents did not adhere to the 8-hours of sleep recommendation, and many of them reported feeling tired at school or in activities. Screen time and gaming were identified as descriptive factors affecting adolescent’s ability to get enough sleep. Our study added new findings to the research literature by uncovering that sleep recommendations were positively associated with higher life satisfaction by controlling for several relevant covariates in a large sample of Norwegian adolescents, underpinning essential information for people working with adolescents and caregivers. Finally, practice and policy aiming at increasing health and satisfaction with life in adolescents should include and highlight sleep recommendations.
This cross-sectional study demonstrated that almost three out of four Norwegian adolescents did not meet the sleep recommendations, and close to two thirds reported that they feel tired at school or in activities. Screen time negatively affected their ability to get enough sleep. Findings revealed a positive association between adhering to the 8-hours of sleep recommendation and satisfaction with life. These findings reinforce the importance of adhering the sleep recommendation for Norwegian adolescents. Adolescence is a critical time wherein insufficient sleep can have significant consequences. Further research is needed to examine other sleep related measures to adolescents’ satisfaction with life.
Data availability
The dataset that support the findings of this study is available upon reasonable request from the Norwegian Agency for Shared Services in Education and Research (SIKT) [ 34 ]. Dataset citation required from SIKT: https://doi.org/10.18712/NSD-NSD3007-V3 .
Abbreviations
time in bed
sleep onset time
confidence interval
standard deviation
socioeconomic status
Norwegian Social Research
regional center for drug rehabilitation
the municipal sector´s organization
Strengthening The Reporting Of Observational Studies
Norwegian Agency for Shared Services in Education and Research
better policies for better lives.
Matricciani L, et al. Children’s sleep and health: a meta-review. Sleep Med Rev. 2019;46:136–50.
Article PubMed Google Scholar
Hirshkowitz M, et al. National Sleep Foundation’s updated sleep duration recommendations: final report. Sleep Health. 2015;1(4):233–43.
Gariepy G, et al. How are adolescents sleeping? Adolescent sleep patterns and Sociodemographic Differences in 24 European and North American Countries. J Adolesc Health. 2020;66(6s):S81–8.
Owens JA, Weiss MR. Insufficient sleep in adolescents: causes and consequences. Minerva Pediatr. 2017;69(4):326–36.
Lee YJ, et al. Insufficient sleep and suicidality in adolescents. Sleep. 2012;35(4):455–60.
Article CAS PubMed PubMed Central Google Scholar
Palmer CA, et al. Associations among adolescent sleep problems, emotion regulation, and affective disorders: findings from a nationally representative sample. J Psychiatr Res. 2018;96:1–8.
Shochat T, Cohen-Zion M, Tzischinsky O. Functional consequences of inadequate sleep in adolescents: a systematic review. Sleep Med Rev. 2014;18(1):75–87.
Owens J. Insufficient sleep in adolescents and young adults: an update on causes and consequences. Pediatrics. 2014;134(3):e921–32.
Konjarski M, et al. Reciprocal relationships between daily sleep and mood: a systematic review of naturalistic prospective studies. Sleep Med Rev. 2018;42:47–58.
Saxvig IW, et al. Sleep in older adolescents. Results from a large cross-sectional, population-based study. J Sleep Res. 2021;30(4):e13263.
Thorleifsdottir B, et al. Sleep and sleep habits from childhood to young adulthood over a 10-year period. J Psychosom Res. 2002;53(1):529–37.
Article CAS PubMed Google Scholar
Baiden P, Tadeo SK, Peters KE. The association between excessive screen-time behaviors and insufficient sleep among adolescents: findings from the 2017 youth risk behavior surveillance system. Psychiatry Res. 2019;281:112586.
Hale L, Guan S. Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep Med Rev. 2015;21:50–8.
Roeser K, et al. Relationship of sleep quality and health-related quality of life in adolescents according to self- and proxy ratings: a questionnaire survey. Front Psychiatry. 2012;3:76.
Article PubMed PubMed Central Google Scholar
Schmidt RE, Van der M, Linden. The relations between Sleep, personality, behavioral problems, and School Performance in adolescents. Sleep Med Clin. 2015;10(2):117–23.
Yeo SC, et al. Associations of sleep duration on school nights with self-rated health, overweight, and depression symptoms in adolescents: problems and possible solutions. Sleep Med. 2019;60:96–108.
Gradisar M, Gardner G, Dohnt H. Recent worldwide sleep patterns and problems during adolescence: a review and meta-analysis of age, region, and sleep. Sleep Med. 2011;12(2):110–8.
Jakobsson M, Josefsson K, Högberg K. Reasons for sleeping difficulties as perceived by adolescents: a content analysis. Scand J Caring Sci. 2020;34(2):464–73.
Chaput JP, et al. Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41(6 Suppl 3):S266–82.
Gustafsson ML, et al. Association between amount of sleep, daytime sleepiness and health-related quality of life in schoolchildren. J Adv Nurs. 2016;72(6):1263–72.
Paiva T, Gaspar T, Matos MG. Sleep deprivation in adolescents: correlations with health complaints and health-related quality of life. Sleep Med. 2015;16(4):521–7.
Satisfaction with life. Accessed 03.10.23 . https://www.oecdbetterlifeindex.org/topics/life-satisfaction/
Diener E. Subjective well-being. Psychol Bull. 1984;95(3):542–75.
Chen X et al. Gender differences in life satisfaction among children and adolescents: a Meta-analysis. J Happiness Stud, 2020. 21.
von Elm E, et al. The strengthening the reporting of Observational studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573–7.
Article Google Scholar
Frøyland LR. Ungdata – Lokale ungdomsundersøkelser. Dokumentasjon av variablene i spørreskjemaet. NOVA. 2017 .
Bakken A. Ungdata 2021. Nasjonale resultater 2021.
05.10. 2023, A. Young in Oslo in 2018 . https://www.oslomet.no/forskning/forskningsprosjekter/ung-i-oslo-2018
Cheung F, Lucas RE. Assessing the validity of single-item life satisfaction measures: results from three large samples. Qual Life Res. 2014;23(10):2809–18.
Jovanović V. The validity of the satisfaction with Life Scale in adolescents and a comparison with single-item life satisfaction measures: a preliminary study. Qual Life Res. 2016;25(12):3173–80.
Bakken A, Frøyland LR, Sletten MA. Sosiale forskjeller i unges liv. Hva sier Ungdata-undersøkelsene? NOVA Rapport 3/2016:, 2016.
Grasaas E, et al. The relationship between stress and health-related quality of life and the mediating role of self-efficacy in Norwegian adolescents: a cross-sectional study. Health Qual Life Outcomes. 2022;20(1):162.
Thorsén F, et al. Sleep in relation to psychiatric symptoms and perceived stress in Swedish adolescents aged 15 to 19 years. Scand J Child Adolesc Psychiatr Psychol. 2020;8:10–7.
PubMed PubMed Central Google Scholar
Norwegian Agency for Shared Services in Education and Research (SIKT) . Accessed 05.10.2023; https://sikt.no/en/home
Kim J et al. The impact of Weekday-to-Weekend Sleep Differences on Health Outcomes among adolescent students. Child (Basel), 2022. 9(1).
Grasaas E, et al. Sleep duration in schooldays is associated with health-related quality of life in Norwegian adolescents: a cross-sectional study. BMC Pediatr. 2023;23(1):473.
Short MA, et al. Estimating adolescent sleep patterns: parent reports versus adolescent self-report surveys, sleep diaries, and actigraphy. Nat Sci Sleep. 2013;5:23–6.
Matthews KA, et al. Similarities and differences in estimates of sleep duration by polysomnography, actigraphy, diary, and self-reported habitual sleep in a community sample. Sleep Health. 2018;4(1):96–103.
Lucas-Thompson RG, Crain TL, Brossoit RM. Measuring sleep duration in adolescence: comparing subjective and objective daily methods. Sleep Health. 2021;7(1):79–82.
Saelee R, et al. Racial/Ethnic and Sex/Gender Differences in Sleep Duration Trajectories from Adolescence to Adulthood in a US National Sample. Am J Epidemiol. 2023;192(1):51–61.
Forest G, et al. Gender differences in the interference of sleep difficulties and daytime sleepiness on school and social activities in adolescents. Sleep Med. 2022;100:79–84.
Dewald JF, et al. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: a meta-analytic review. Sleep Med Rev. 2010;14(3):179–89.
Cheung CHM, et al. Daily touchscreen use in infants and toddlers is associated with reduced sleep and delayed sleep onset. Sci Rep. 2017;7(1):46104.
Wood B, et al. Light level and duration of exposure determine the impact of self-luminous tablets on melatonin suppression. Appl Ergon. 2013;44(2):237–40.
Pérez-Chada D et al. Screen use, sleep duration, daytime somnolence, and academic failure in school-aged adolescents. PLoS ONE, 2023. 18(2 February).
Ahmadi Z, Omidvar S. The quality of sleep and daytime sleepiness and their association with quality of school life and school achievement among students. J Educ Health Promot. 2022;11:159.
Meade T, Dowswell E. Health-related quality of life in a sample of Australian adolescents: gender and age comparison. Qual Life Res. 2015;24(12):2933–8.
Rabbitts JA, et al. Association between widespread Pain scores and functional impairment and health-related quality of life in clinical samples of children. J Pain. 2016;17(6):678–84.
Bisegger C, et al. Health-related quality of life: gender differences in childhood and adolescence. Soz Praventivmed. 2005;50(5):281–91.
Michel G, et al. Age and gender differences in health-related quality of life of children and adolescents in Europe: a multilevel analysis. Qual Life Res. 2009;18(9):1147–57.
Ness TEB, Saksvik-Lehouillier I. The relationships between life satisfaction and Sleep Quality, Sleep Duration and Variability of Sleep in University students. Journal of European Psychology Students; 2018.
Kim SJ, et al. Relationship between weekend catch-up sleep and poor performance on attention tasks in Korean adolescents. Arch Pediatr Adolesc Med. 2011;165(9):806–12.
Download references
Acknowledgements
We wish to thank all the adolescents participating in Ungdata, NOVA and KoRus for giving us access to the data and the Norwegian Directorate of Health for funding the survey.
The Ungdata project is financed from the Norwegian national budget through grants from the Norwegian Directorate of Health [ 26 ].
Open access funding provided by University of Agder
Author information
Authors and affiliations.
Department of Nutrition and Public Health, Faculty of Health and Sport Sciences, University in Agder, Kristiansand, Postbox 422, 4604, Norway
Erik Grasaas & Sergej Ostojic
Department of Rehabilitation Science and Health Technology, Center for Intelligent Musculoskeletal health, Oslo Metropolitan University, Oslo, Norway
Henriette Jahre
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to manuscript preparation. EG provided the first original draft of the manuscript and conducted the statistical analysis. SO and HJ contributed to the conceptualization, design and interpretation of findings. All read and approved the final manuscript.
Corresponding author
Correspondence to Erik Grasaas .
Ethics declarations
Ethics approval and consent to participate.
All study procedures were performed in accordance with the 1964 Helsinki declaration for ethical standards in research. Informed consent to participate was obtained from all of the participants. Permission to access and use data were given by Norwegian Agency for Shared Sevices in Education and Research (SIKT) on the 29.09.2023.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Grasaas, E., Ostojic, S. & Jahre, H. Adherence to sleep recommendations is associated with higher satisfaction with life among Norwegian adolescents. BMC Public Health 24 , 1288 (2024). https://doi.org/10.1186/s12889-024-18725-1
Download citation
Received : 02 November 2023
Accepted : 28 April 2024
Published : 10 May 2024
DOI : https://doi.org/10.1186/s12889-024-18725-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adolescents
- Satisfaction with life
- Quality of life
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Main Navigation
- Contact NeurIPS
- Code of Ethics
- Code of Conduct
- Create Profile
- Journal To Conference Track
- Diversity & Inclusion
- Proceedings
- Future Meetings
- Exhibitor Information
- Privacy Policy
NeurIPS 2024, the Thirty-eighth Annual Conference on Neural Information Processing Systems, will be held at the Vancouver Convention Center
Monday Dec 9 through Sunday Dec 15. Monday is an industry expo.

Registration
Pricing » Registration 2024 Registration Cancellation Policy » . Certificate of Attendance
Our Hotel Reservation page is currently under construction and will be released shortly. NeurIPS has contracted Hotel guest rooms for the Conference at group pricing, requiring reservations only through this page. Please do not make room reservations through any other channel, as it only impedes us from putting on the best Conference for you. We thank you for your assistance in helping us protect the NeurIPS conference.
Announcements
- The call for High School Projects has been released
- The Call For Papers has been released
- See the Visa Information page for changes to the visa process for 2024.
Latest NeurIPS Blog Entries [ All Entries ]
Important dates.
If you have questions about supporting the conference, please contact us .
View NeurIPS 2024 exhibitors » Become an 2024 Exhibitor Exhibitor Info »
Organizing Committee
General chair, program chair, workshop chair, workshop chair assistant, tutorial chair, competition chair, data and benchmark chair, diversity, inclusion and accessibility chair, affinity chair, ethics review chair, communication chair, social chair, journal chair, creative ai chair, workflow manager, logistics and it, mission statement.
The Neural Information Processing Systems Foundation is a non-profit corporation whose purpose is to foster the exchange of research advances in Artificial Intelligence and Machine Learning, principally by hosting an annual interdisciplinary academic conference with the highest ethical standards for a diverse and inclusive community.
About the Conference
The conference was founded in 1987 and is now a multi-track interdisciplinary annual meeting that includes invited talks, demonstrations, symposia, and oral and poster presentations of refereed papers. Along with the conference is a professional exposition focusing on machine learning in practice, a series of tutorials, and topical workshops that provide a less formal setting for the exchange of ideas.
More about the Neural Information Processing Systems foundation »
- Systematic Review
- Open access
- Published: 13 May 2024
Sarcopenia and sarcopenic obesity among older adults in the nordic countries: a scoping review
- Fereshteh Baygi 1 na1 ,
- Sussi Friis Buhl 1 na1 ,
- Trine Thilsing 1 ,
- Jens Søndergaard 1 &
- Jesper Bo Nielsen 1
BMC Geriatrics volume 24 , Article number: 421 ( 2024 ) Cite this article
325 Accesses
Metrics details
Sarcopenia and sarcopenic obesity (SO) are age-related syndromes that may compromise physical and mental health among older adults. The Nordic countries differ from other regions on prevalence of disease, life-style behavior, and life expectancy, which may impact prevalence of sarcopenia and SO. Therefore, the aim of this study is to review the available evidence and gaps within this field in the Nordic countries.
PubMed, Embase, and Web of science (WOS) were searched up to February 2023. In addition, grey literature and reference lists of included studies were searched. Two independent researcher assessed papers and extracted data.
Thirty-three studies out of 6,363 searched studies were included in this scoping review. Overall prevalence of sarcopenia varied from 0.9 to 58.5%. A wide prevalence range was still present for community-dwelling older adults when definition criteria and setting were considered. The prevalence of SO ranged from 4 to 11%, according to the only study on this field. Based on the included studies, potential risk factors for sarcopenia include malnutrition, low physical activity, specific diseases (e.g., diabetes), inflammation, polypharmacy, and aging, whereas increased levels of physical activity and improved dietary intake may reduce the risk of sarcopenia. The few available interventions for sarcopenia were mainly focused on resistance training with/without nutritional supplements (e.g., protein, vitamin D).
The findings of our study revealed inadequate research on SO but an increasing trend in the number of studies on sarcopenia. However, most of the included studies had descriptive cross-sectional design, small sample size, and applied different diagnostic criteria. Therefore, larger well-designed cohort studies that adhere to uniform recent guidelines are required to capture a full picture of these two age-related medical conditions in Nordic countries, and plan for prevention/treatment accordingly.
Peer Review reports
The number of older adults with age-related disorders is expected to increase worldwide [ 1 , 2 ]. Sarcopenia and sarcopenic obesity (SO) are both age-related syndromes that may compromise the physical and mental health of older adults and increase their need for health care services in old age [ 3 , 4 ], and this may challenge the sustainability of health care systems economically and by shortage of health care personnel [ 5 ].
Sarcopenia is characterized by low muscle mass in combination with low muscle strength [ 4 ]. SO is characterized by the co-existence of obesity (excessive adipose tissue) and sarcopenia [ 3 ]. Sarcopenia and SO are both associated with physical disability, risk of falls, morbidity, reduced quality of life and early mortality [ 4 , 6 , 7 , 8 , 9 ]. In SO the consequences of sarcopenia and obesity are combined and maximized [ 4 , 6 , 7 , 8 ].
Etiology of sarcopenia and SO is multifactorial and closely linked to multimorbidity [ 3 , 7 , 8 , 9 , 10 ]. Nevertheless, lifestyle and behavioral components particularly diet and physical activity, are important interrelated factors that potentially can be modified. Physical inactivity and sedentary behavior may accelerate age-related loss of muscle mass, reduce energy expenditure, and increase risk of obesity [ 3 , 11 ]. In addition, weight cycling (the fluctuations in weight following dieting and regain) and an unbalanced diet (particularly inadequate protein intake) may accelerate loss of muscle mass and increase severity of sarcopenia and SO in older adults [ 3 , 12 ]. International guideline for the treatment of sarcopenia emphasizes the importance of resistance training potentially in combination with nutritional supplementation to improve muscle mass and physical function [ 13 ]. Similar therapeutic approach is suggested for treatment of SO [ 14 ]. However, more research is needed to confirm optimal treatment of SO [ 14 ].
According to a recently published meta-analysis the global prevalence of sarcopenia ranged from 10 to 27% in populations of older adults ≥ 60 years [ 15 ]. Further the global prevalence of SO among older adults was 11% [ 8 ]. So, sarcopenia and SO are prevalent conditions, with multiple negative health outcomes and should be given special attention [ 16 ]. Despite the large burden on patients and health care systems, the awareness of the importance of skeletal muscle maintenance in obesity is low among clinicians and scientists [ 3 , 16 ].
A recent meta-analysis on publication trends revealed that despite an increase in global research on sarcopenia, the Nordic countries were only limitedly represented [ 6 ]. Nordic countries may differ from other regions on aspects associated with the prevalence and trajectory of sarcopenia and SO and challenge the representativeness of research findings from other parts of the world. These include a different prevalence pattern of noncommunicable diseases [ 17 ], different life-style behavior and life-style associated risk factors [ 15 , 18 ], and higher life expectancy [ 18 ].
The Nordic countries including Sweden, Finland, Iceland, Norway, Denmark, and three autonomous areas (Åland Islands, Greenland and Faroe Islands) share common elements of social and economic policies such as a comprehensive publicly financed health care system [ 18 , 19 ]. Additionally, these countries have a strong tradition of collaboration including a common vision of a socially sustainable region by promoting equal health and inclusive participation in society for older adults [ 20 ]. Therefore, more insight into the etiology, prevalence, and risk factors for sarcopenia and SO among older adults is a prerequisite for the development and implementation of effective strategies to prevent and treat these complex geriatric conditions in this geographic region. So, the aim of this study is to conduct a scoping review to systematically identify and map the available evidence while also addressing knowledge gaps and exploring the following research questions: (1) What are the prevalence of sarcopenia and SO in older adults living in the Nordic countries? (2) Which risk factors or contributing conditions are involved in the development of sarcopenia and SO in the Nordic Countries? (3) Which interventions to prevent or counteract negative health outcomes of sarcopenia and SO have been tested or implemented among older adults living in the Nordic countries?
Identification of relevant studies
The development and reporting of this review were done by following the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines [ 21 ].
The literature search was developed to target three main areas: Sarcopenia, sarcopenic obesity, and aging (See Appendix 1 for full search strategy). All studies published before the end of February 2023 were included in this scoping review. The optimal sensitivity of search was obtained by simultaneous search of the following databases: PubMed, Embase, and Web of science (WOS). Additionally, a detailed search for grey literature was performed in relevant databases (e.g., Research Portal Denmark, Libris, Oria, Research.fi). Besides, reference lists of the included studies were reviewed to identify eligible studies. Duplicates and non-peer reviewed evidence (e.g., PhD thesis) were excluded but if the latter contained published articles of relevance, these were included. If more than one publication on similar outcomes (e.g., prevalence) were based on a single study, just one publication was included. Data were extracted from large studies with combined data from several countries only when findings were presented separately for the Nordic countries.
Inclusion and exclusion criteria
The inclusion criteria were as follow : Broad selection criteria were used to be comprehensive: (1) studies with any outcome (e.g., prevalence, risk factors, etc.) to address our research questions on sarcopenia and SO, (2) studies on subjects with age ≥ 60 years in any type of settings (e.g., community, nursing homes, general practice, hospital, outpatients, homecare, etc.), (3) studies using any definition of sarcopenia and SO without restriction for criteria and cutoff values, (4) all type of study designs (e.g., randomized control trials, cohort studies, cross-sectional, etc.), (5) studies should be conducted in the Nordic countries The exclusion criteria are as follow : (1) studies without relevant outcome to sarcopenia or SO, (2) studies without sufficient information to determine eligibility.
Study selection and data extraction
Two independent researchers screened literature and conducted data extraction. Any discrepancies between them were resolved through discussion.
First, duplicates were removed by using EndNote 20.6 software, then titles and abstracts were screened to narrow down the list of potentially eligible studies. Finally, the full text review was done to examine in detail the studies that were not excluded in first step. For more clarification, the reasons for the exclusion were recorded (Fig. 1 ).
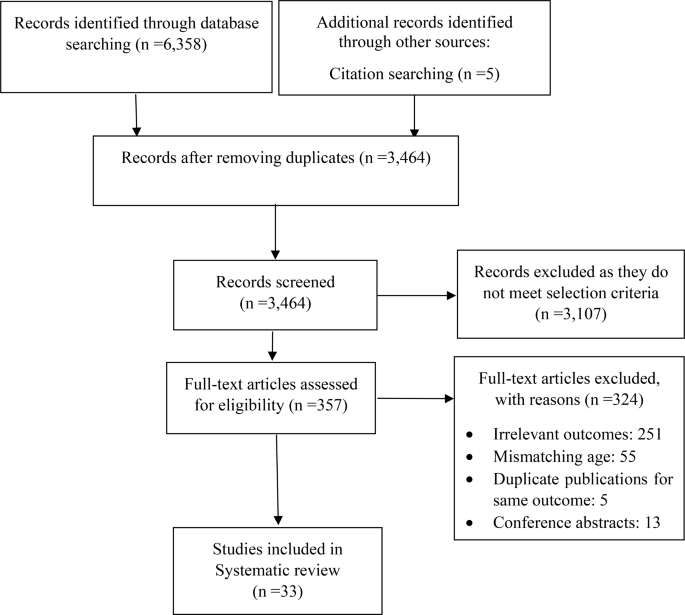
PRISMA diagram for searching resources
The following information was extracted: (1) study characteristics (e.g., first author’s name, country, year of publication), (2) characteristics of the target population (e.g., age, sex), (3) study design, setting, intervention duration and follow-up time (if applicable), measurements, tools, criteria, and results.
Study selection
A combined total of 6,358 studies were identified through the initial electronic database and grey literature searches. An additional five articles were identified through other sources (citation searching). After removing duplication, 3,464 articles remained. A total of 3107 articles were excluded based on screening titles and abstracts. Out of the remaining 357 studies, 324 were excluded after the full-text review. Finally, 33 studies met our inclusion criteria and were included in this current scoping review [ 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 ] (Fig. 1 ).
Study characteristics
Table 1 summarized characteristics of the included studies.
The number of documents showed an increasing trend between 2020 and 2021. A peak in the number of publications was observed in 2021 (24.2% of all documents). All the studies were conducted across four (Denmark, Norway, Sweden, and Finland) out of the five Nordic countries and three autonomous areas. The highest contribution in this field was made by Sweden ( n = 12).
Most studies were conducted in community-dwelling settings [ 22 , 23 , 24 , 28 , 30 , 31 , 35 , 36 , 38 , 39 , 40 , 42 , 45 , 46 , 47 , 48 , 49 , 54 ]. Seven studies included patients with acute diseases (hospital-setting) [ 26 , 27 , 33 , 37 , 50 , 51 , 52 ], while four studies included patients with chronic conditions (out-patient setting) [ 25 , 32 , 41 , 44 ], and one study including nursing-home residents [ 34 ]. In terms of study design, most of the studies were observation studies with a cross-sectional or longitudinal design ( 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 33 , 34 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 ), while three studies [ 32 , 35 , 46 ] applied interventions. It appears, however, that one study [ 32 ] out of the above three interventions is sub-project conducted within the framework of larger intervention program. Sample size ranged from 49 in a cross-sectional case control study [ 52 ] to 3334 in a cohort study [ 30 ].
Five studies were among males only [ 22 , 24 , 36 , 45 , 53 ] and three studies included females only [ 38 , 47 , 54 ]. The rest of the studies had a mixed sample. Top subject area was sarcopenia (31 out of the 33 included studies), and on this subject, publications were categorized into the following research areas (with some studies addressing more areas): prevalence [ 22 , 23 , 24 , 25 , 26 , 27 , 29 , 30 , 33 , 35 , 36 , 37 , 40 , 42 , 44 , 45 , 47 , 49 , 50 , 51 , 52 , 53 , 54 ], risk factors [ 24 , 27 , 28 , 30 , 31 , 34 , 38 , 40 , 42 , 44 , 47 , 49 , 50 , 51 ], and effectiveness of interventions on sarcopenia or indicator of sarcopenia [ 32 , 35 , 46 ].
In most studies sarcopenia was defined according to the criteria set by the European Working Group on Sarcopenia in Older People in the updated version from 2019 (EWGSOP2) ( n = 15) or the original version from 2010 (EWGSOP) ( n = 14). However, in some studies multiple criteria such as EWGSOP, EWGSOP2, and National Institutes of Health Sarcopenia Project definition (FNIH) were applied [ 27 , 39 , 43 ], and in other studies alternative criteria were used [ 26 , 33 , 35 , 45 , 57 ].
Different assessment methods of muscle mass including Dual energy X-ray absorptiometry (DXA) [ 22 , 24 , 25 , 27 , 29 , 30 , 32 , 33 , 38 , 39 , 40 , 41 , 45 , 46 , 47 , 52 , 53 , 54 ], Bioelectrical Impedance Analysis (BIA) [ 28 , 31 , 34 , 44 , 48 , 49 ], Bioimpedance Spectroscopy (BIS) [ 35 , 42 , 43 ], Computed Tomography (CT) [ 33 ], and Computed Tomography Angiogram (CTA) [ 26 ] were used in the included studies.
SO were defined by the co-existence of sarcopenia with obesity. Studies on SO used the EWGSOP2 criteria [ 39 ], or the EWGSOP2 criteria for hand grip strength only (probable sarcopenia) [ 23 ] in combination with obesity estimated from BMI cut points [ 23 , 39 ], waist circumference [ 23 , 39 ], and fat mass percentage [ 39 ]. Lastly, one study used measures of body composition measures that reflect adiposity as estimates of SO [ 48 ].
Four studies reported the prevalence of “probable sarcopenia” [ 23 , 30 , 36 , 45 ], while two studies reported the prevalence of sarcopenia and comorbidities (e.g., osteopenia, pre-frailty, malnutrition) [ 33 , 40 ].
Narrative synthesis
Due to the heterogeneity of the studies in definition of sarcopenia, settings, and sample size, the overall reported prevalence was variable and ranged from 0.9% [ 54 ] to 58.5% [ 26 ]. However, according to the most commonly used criteria (EWGSOP2) the highest (46%) and lowest (1%) prevalence of sarcopenia was reported in Sweden among inpatients in geriatric care [ 27 ], and community-dwelling older adults [ 30 ], respectively.
Prevalence of sarcopenia according to population and definition criteria is illustrated in Table 2 . Higher prevalence rates of sarcopenia were found in females compared to males among community-dwelling older adults [ 49 ] and in older adults acutely admitted to hospital [ 51 ]. Further, acutely admitted female patients also presented with more severe sarcopenia compared to male patients [ 51 ].
Frequency of sarcopenia was higher (9.1–40.0%) in patients with diabetes (with and without complications of charcot osteoarthropathy), compared to age-matched healthy adults [ 52 ].
The prevalence of “probable sarcopenia” ranged between 20.4% (reduced muscle strength only) and 38.1% (fulfilling one of the following criteria: reduced muscle strength, reduced muscle mass, or low physical function) in Finnish community-dwelling adults [ 23 , 36 ], while longitudinal studies on Swedish community-dwelling old (70 years) and very old adults (≥ 85 years) the prevalence of “probable sarcopenia” (reduced muscle strength only) ranged from 1.8 to 73%, respectively [ 30 , 45 ]. Lastly, in a Swedish study among nursing home residents the prevalence of probable sarcopenia was 44% (evaluated by an impaired chair stand test) [ 34 ].
Prevalence of Osteosarcopenia (sarcopenia and osteoporosis) was 1.5% [ 36 ], and the prevalence of co-occurrence of all three following conditions: pre-frail, malnutrition, and sarcopenia was 7% [ 34 ].
We only identified two studies with prevalence of SO [ 39 ] and probable SO [ 23 ]. The prevalence of SO in a Swedish population was 4% and 11% in females and males, respectively, while the prevalence of probable SO among Finnish community-dwelling ranged between 5.8% and 12.6%, depending on the criteria to define the obesity (e.g., BMI, waist circumference, etc.) [ 23 ].
Several studies investigated aspects of etiology and risk factors for sarcopenia [ 24 , 27 , 28 , 30 , 31 , 34 , 36 , 38 , 40 , 42 , 43 , 44 , 47 , 49 , 50 , 51 ] and one study focused on SO [ 49 ]. Higher physical activity was associated with a decreased likelihood of sarcopenia [ 30 ]. In addition, adhering to world health organization (WHO) guidlines for physical activity and the Nordic nutritional recommendations for protein intake was positively associated with greater physical function and lower fat mass in older female community-dwellers [ 38 ]. In older adults who are physically active, eating a healthy diet (based on the frequency of intake of favorable food like fish, fruits, vegetables, and whole grains versus unfavorable foods like red/processed meats, desserts/sweets/sugar-sweetened beverages, and fried potatoes) was associated with lower risk of sarcopenia [ 28 ]. Further, among older adults who already meet the physical activity guidelines, additional engagement in muscle-strengthening activities was associated with a lower sarcopenia risk score and improved muscle mass and chair rise time [ 31 ].
Associations between sarcopenia, risk of sarcopenia and malnutrition or nutritional status was identified in geriatric patients [ 27 , 51 ], older patients with hip fracture [ 50 ], nursing home residents [ 34 ] and in community-dwelling older adults [ 49 ]. Moreover, the importance of nutritional intake was investigated in the following studies [ 24 , 36 , 47 ]. A study among community-dwelling men revealed an inverse association between total energy intake, protein intake (total, plant, and fish protein), intake of dietary fibers, fat (total and unsaturated), and vitamin D with sarcopenia status [ 36 ]. In a cohort of 71-year-old men a dietary pattern characterized by high consumption of fruit, vegetables, poultry, rice and pasta was associated with lower prevalence of sarcopenia after 16 years [ 24 ]. A longitudinal Finnish study on sarcopenia indices among postmenopausal older women, showed that lower adherence to the Mediterranean (focuses on high consumption of olive oil) or Baltic Sea (focuses on the dietary fat quality and low-fat milk intake) diets resulted in higher loss of lean mass over a 3-year period [ 47 ]. Further, a higher adherence to the Baltic Sea diet was associated with greater lean mass and better physical function, and higher adherence to the Mediterranean diet was associated with greater muscle quality [ 47 ].
In a study of patients with hip fracture age, polypharmacy, and low albumin levels was associated with sarcopenia [ 50 ]. Exocrine pancreatic insufficiency was an independent risk factor for sarcopenia [ 44 ]. This study also revealed that sarcopenia was associated with reduced quality of life, physical function, and increased risk of hospitalization [ 44 ]. In a longitudinal study of community-dwelling adults (+ 75 years) at risk of sarcopenia, high physical function, muscle strength, muscle mass and low BMI predicted better physical function and reduced need for care after four years [ 42 ]. Furthermore, in community-dwelling adults with sarcopenia, muscle mass, muscle strength and physical function are independent predictors of all-cause mortality. As a result, they have been proposed by researchers as targets for the prevention of sarcopenia-related over-mortality [ 43 ]. Lastly, community-dwelling older adults with sarcopenia had lower bone mineral density compared to those without sarcopenia and they were more likely to develop osteoporosis (Osteosarcopenia) [ 40 ].
Regarding SO risk factors, a longitudinal study among community-dwelling older adults in Finland found that SO (operationalized by measures of adiposity) were associated with poorer physical function after ten years [ 48 ].
Our literature search identified three randomized controlled trials investigating the effectiveness of interventions to prevent or counteract sarcopenia in older adults of Norway, Finland, and Sweden, respectively [ 32 , 35 , 46 ]. The Norwegian study [ 32 ] was a double-blinded randomized controlled trial (RCT). The study included those who were at risk of developing sarcopenia, including patients with chronic obstructive pulmonary disease (COPD) or individuals who showed diagnostic indications of sarcopenia. Participants received either vitamin D 3 or placebo supplementation for 28 weeks. Additionally, resistance training sessions were provided to all participants from weeks 14 to 27. Vitamin D supplementation did not significantly affect response to resistance training in older adults at risk of sarcopenia with or without COPD [ 32 ].
Furthermore, a RCT among pre-sarcopenic Swedish older adults investigated the effectiveness of three weekly sessions of instructor-led progressive resistance training in combination with a non-mandatory daily nutritional supplement (175 kcal, 19 g protein) compared to control group. The 10 weeks intervention resulted in significant between group improvements of physical function and a significant improvement in body composition in the intervention group [ 46 ].
Another intervention study revealed that a 12-month intervention with two daily nutritional supplements (each containing 20 g whey protein) did not attenuate the deterioration of physical function and muscle mass in sarcopenic older community-dwelling adults compared to isocaloric placebo supplements or no supplementation. All participants were given instructions on home-based exercises, importance of dietary protein and vitamin D supplementation [ 35 ].
Based on our broad literature search 33 studies were identified that concerned sarcopenia and SO and met the inclusion criteria. However, research on SO was very limited with only three studies identified. Narrative synthesis of the included studies revealed that the most reported classification tool for sarcopenia in Nordic countries was the EWGSOP2. Moreover, some studies estimated sarcopenia using EWGSOP. The overall prevalence of sarcopenia in Nordic countries according to EWGSOP2 ranged between 1% and 46% [ 25 , 28 ]. The prevalence of SO, however, was reported only in one study in Sweden (4–11%) [ 39 ]. Even though the previous systematic reviews and meta-analysis have reported the prevalence of sarcopenia and SO in different regions and settings (e.g., community-dwelling, nursing home, etc.) [ 8 , 15 , 55 , 56 ], this current scoping review is to the best of our knowledge the first study that provides an overview of research on sarcopenia and SO in the Nordic countries.
Based on our findings from 24 studies, there were large variability in prevalence of sarcopenia in studies conducted in the Nordic countries. We think that the wide variation in estimated prevalence of sarcopenia in our scoping review might be due to a different definition/diagnostic criterion (e.g., EWGSOP, EWGSOP2, FNIH), methodology to measure muscle mass (DXA, BIA, CT), and heterogeneity in characteristics of the study population (e.g., setting, age, medical conditions, co-occurrence of multiple risk factors). A previous study on prevalence of sarcopenia in Swedish older people showed significant differences between prevalence of sarcopenia based on EWGSOP2 and EWGSOP1 [ 29 ]. Therefore, researchers stressed that prevalence is more dependent on cut-offs than on the operational definition [ 29 , 57 ]. Further, we know that various international sarcopenia working groups have issued expert consensus and such diagnostic criteria are being updated [ 4 , 58 ]. Since the revision of criteria focuses primarily on the adjustment of cut-off values, the main reason for differences in prevalence even when using an updated version of one diagnosis criteria is modification in cut-off values. For instance, if the cut-off value for gait speed was increased by 0.2 m/s, the prevalence of sarcopenia may increase by 8.5% [ 57 ]. Meaning that even a small change in cut-off value can have a big impact on how sarcopenia is diagnosed. Besides when we take definition criteria into account (Table 2 ), the prevalence of sarcopenia is still variable in the population of community-dwelling adults for instance. We believe it is basically because studies have applied different assessment tools and tests to identify older adults with low muscle mass and muscle strength, although using the same definition criteria (Table 1 ). Previous studies have illustrated that choice of methodology to assess muscle strength (e.g., hand grip strength, chair rise) [ 59 ] and muscle mass (e.g., DXA, BIA, anthropometry) [ 60 , 61 , 62 ] in older adults may impact findings and this variability may explain some of the variability in our findings. So, adherence to the latest uniform diagnostic criteria for future studies is recommended to simplify the comparison of findings within the same country, across countries, and regions. Moreover, we suggest that medical community particularly GPs to come to an agreement on assessment methods for muscle mass and muscle strength and the use of one set of definition criteria for sarcopenia.
In previous meta-analyses [ 15 ], sub-group analyses based on region and classification tool, revealed that the prevalence of sarcopenia was higher in European studies using EWGSOP (12%) compared to rest of the studies using Asian Working Group for Sarcopenia (AWGS), FNIH, and EWGSOP (3%) [ 15 ]. In our scoping review, we also found a high prevalence of sarcopenia in Nordic countries. Longevity and life expectancy is higher in the Nordic countries compared to estimates for rest of the world [ 18 ], which means that in this region many people reach old age, and consequently they are more likely to be diagnosed with sarcopenia as an age-related disorder. Therefore, the authors of this current scoping review emphasis the importance of preventive strategies targeted major risk factors and effective interventions to limit the consequences of sarcopenia in the Nordic populations. Besides, we think that the health care system in the Nordic countries should be better equipped with the necessary healthcare resources for both a timely diagnosis and dealing with this major age-related issue in the years to come. However, due to the limitations regarding the timely diagnosis, we highly recommend a comprehensive approach including establishment of support services, implement educational programs, offer training for health care professionals, and engage the community.
Many countries have conducted research on SO [ 7 , 39 , 63 , 64 , 65 ]. Based on our findings, however, among the Nordic countries only Sweden and Finland have investigated the prevalence of probable SO and SO [ 23 , 29 ]. Besides, we only found one study investigating the association between body adiposity and physical function over time [ 54 ]. We did not find any literature on risk factors or interventions among older adults with SO in this region. Therefore, we call on medical and research community in Nordic countries to attach importance to screening of SO in elderly people to capture a full picture of this public health risk to aging society and allocate healthcare resources accordingly.
In terms of risk factors for sarcopenia, our study revealed that malnutrition, low levels of physical activity, specific diseases (e.g., diabetes, osteoporosis), inflammation, polypharmacy (multiple medicines), BMI, and ageing are potential risk factor for sarcopenia in populations of the Nordic region. However, evidence on risk factors derived mainly from cross-sectional associations [ 27 , 28 , 30 , 31 , 34 , 40 , 44 , 49 , 50 , 51 ], and only to a limited extend from longitudinal studies [ 24 , 38 , 43 , 47 ]. Therefore, the associations between risk factors and sarcopenia should be interpreted with caution due to the possibility of reverse causality and confounding affecting the results. Moreover, our findings on risk factors mainly came from community-dwelling older adults, and only to a limited extend hospital and nursing home settings. We think that risk factors may vary depending on population characteristics (e.g., age, sex, health condition) and setting (e.g., hospital, nursing home, community). Therefore, we encourage researchers of the Nordic countries to perform well-designed prospective cohort studies in different settings to enhance the possibility to establish causal inference as well as understanding degree and direction of changes over time.
A recently published meta-analyses revealed a higher risk of having polypharmacy in Europe among individuals with sarcopenia compared to people without this condition [ 66 ]. A nationwide register-based study in Swedish population also showed that the prevalence of polypharmacy has increased in Sweden over the last decade [ 67 ]. Sarcopenia itself is associated with morbidity (identified by specific disease or inflammatory markers) and different health-related outcomes (e.g., disability) [ 7 ]; therefore, future research should investigate whether polypharmacy is a major factor to sarcopenia development [ 66 ]. Although we lack information on polypharmacy in Nordic countries other than Sweden, we encourage researchers in this region to examine the above research gap in their future studies.
According to previous studies physiological changes in ageing include systemic low-grade inflammation which results in insulin resistance, affect protein metabolism and leads to increased muscle wasting [ 68 ]. Acute and chronic disease may increase the inflammatory response and accelerate age-related loss of muscle mass and increase risk of sarcopenia [ 68 , 69 ]. Hence, we think that special attention should be made by health care professionals particularly GPs to older adults with acute or chronic conditions to limit the risk of sarcopenia.
Literature from the Nordic countries also indicated that higher levels of physical activity and different dietary patterns (e.g., higher protein intake, fruit, vegetables, fibers) were associated with reduced risk of sarcopenia or improvement in indicators of sarcopenia. There was a large heterogeneity in the studied aspect which makes direct comparison of studies difficult. Nevertheless, according to findings from a recent systematic review of meta-analyses on sarcopenia the identified risk factors are in alignment with previously identified risk factors globally [ 70 ]. Other potential lifestyle-related risk factors suggested from the above meta-analysis included smoking and extreme sleep duration. However, we did not identify studies investigating these health behaviors in the Nordic populations. Therefore, high-quality cohort studies are needed to deeply understand such associations with the risk of sarcopenia.
In this current review, we only found three intervention studies in Nordic countries. However, two of them were sub-projects of big intervention programs, meaning that such studies were not designed explicitly for the prevention/treatment of sarcopenia. Therefore, explicit intervention studies on sarcopenia in this region is recommended.
We believe that on a global level, research on sarcopenia will carry on with nutrition, exercise, and understanding of molecular mechanisms. Furthermore, examining the link between sarcopenia and other medical conditions/diseases would be the next step [ 6 ]. In the Nordic countries, however, already performed studies have a basic and descriptive design, so that, well-designed research and advanced analyses are lacking. Hence, we recommend conducting large well-designed and adequately powered studies to (a) explore the scale of this age-related health issue on country and regional level, (b) investigate the patterns of physical activity and sedentary behavior to understand if this should be a target in older adults with SO and sarcopenia, (c) determine whether elderly populations are suffering from nutritional deficiency or are at risk of malnutrition. The latest can support further studies to assess the impact of combined physical activity and dietary intake, which are still lacking globally [ 6 ].
A previous systematic review on therapeutic strategies for SO revealed that exercise-based interventions (e.g., resistance training) reduced total adiposity and consequently improved body composition. However, evidence of other therapeutic strategies (e.g., nutritional supplementation) was limited due to scarcity of data and lack of unique definition for SO [ 69 ]. Therefore, authors suggested that more research should be done to clarify optimal treatment options for various age-groups and not only for older adults [ 14 ].
In our scoping review, the included studies, did not provide a status of either SO or the prevention/treatment methods in this region. We believe that SO is practically neglected in clinical practice and research as well, and this is mainly because it is difficult to separate it from general obesity. The consequence of lacking knowledge in this research area is that when older adults with SO are recommended weight loss- a frequently used strategy for management of general obesity- this may accelerate the loss of muscle mass and increase the severity of the sarcopenia [ 3 ]. Consequently, we think that this issue may have adverse effects both on patients (e.g., decreasing quality of their life) and on the health care system (e.g., increasing the health care demands) of this region. Therefore, we encourage researchers to perform cohort studies to understand the epidemiology and etiological basis of SO, which are poorly understood even on a global scale [ 8 ]. We think that the consensus definition on SO from the European Society for Clinical Nutrition and Metabolism (ESPEN) and European Association for the Study of Obesity (EASO) which was published in 2022 [ 3 ], can positively affect the ability to define studies on prevalence and prevention of SO. Besides, we recommend conducting further research to find the optimal treatment for SO and reduce its adverse consequences both at individual and society levels. Additionally, we think that the concepts of sarcopenia and SO might be somehow unfamiliar to health care personnel. Therefore, it is highly recommended that more information be provided to bring their attention to the significance of prevention, timely diagnosis, and treatment of these two aging disorders.
Strengths and limitations of the study
This is the first study providing an overview of available evidence on sarcopenia and SO among older adults in the Nordic countries. These countries have important similarities in welfare sectors and on a population level and we believe that our findings will be a significant benefit for researchers and health care providers to understand the knowledge gaps and plan for future studies in this geographical region. However, the current scoping review has limitations. This review was limited to studies among individuals more than 60 years old which may limit the overview of available research in this field, as well as understanding risk factors, confounders for prevention, and the potential for early detection of these two diseases in younger age population. The included cross-sectional studies in our review cannot provide information on causality of the associations.
Sarcopenia and SO are generally prevalent syndromes among older adults in Nordic countries, even though the prevalence of them varies according to the criteria for definition, population, and setting. Research among older adults with SO was very limited in this region. Besides, studies on risk factors were primarily cross-sectional and only few intervention studies were identified. Therefore, we encourage researchers performing well-designed studies (e.g., prospective cohorts) to understand the epidemiology and etiological basis of these two age-related disorders. For the next step, implementation of interventions targeting risk factors (e.g., combined physical activity and dietary intake) and evaluating of their impact on prevention or treatment of sarcopenia and SO is recommended. Furthermore, for the comprehensive advancement of muscle health in older adults, we recommend implementing interventions directed at health care personnel and encouraging more collaboration among clinicians, professional societies, researchers, and policy makers to ensure comprehensive and effective approach to health care initiatives.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
sarcopenic obesity
Web of science
Preferred Reporting Items for Systematic Reviews and Meta-analyses
European Working Group on Sarcopenia in Older People in the updated version from 2019
National Institutes of Health Sarcopenia Project definition
Dual energy X-ray absorptiometry
Bioelectrical Impedance Analysis
Bioimpedance Spectroscopy
Computed Tomography
Computed Tomography Angiogram
World Health Organization
General Practitioner
Randomized Controlled Trial
Chronic Obstructive Pulmonary Disease
European Association for the Study of Obesity
United, Nations, Department of Economic and Social Affairs., Population Division (2019). World Population Prospects 2019: Highlights (ST/ESA/SER.A/423).
United, Nations, Department of Economic and Social Affairs., Population Division (2019). World Population Ageing 2019: Highlights (ST/ESA/SER.A/430).
Donini LM, Busetto L, Bischoff SC, Cederholm T, Ballesteros-Pomar MD, Batsis JA, Bauer JM, Boirie Y, Cruz-Jentoft AJ, Dicker D, Frara S, Frühbeck G, Genton L, Gepner Y, Giustina A, Gonzalez MC, Han HS, Heymsfield SB, Higashiguchi T, Laviano A, Lenzi A, Nyulasi I, Parrinello E, Poggiogalle E, Prado CM, Salvador J, Rolland Y, Santini F, Serlie MJ, Shi H, Sieber CC, Siervo M, Vettor R, Villareal DT, Volkert D, Yu J, Zamboni M, Barazzoni R. Definition and diagnostic criteria for sarcopenic obesity: ESPEN and EASO Consensus Statement. Obes Facts. 2022;15(3):321–35. doi: 10.1159/000521241. Epub 2022 Feb 23. PMID: 35196654; PMCID: PMC9210010.
Article PubMed PubMed Central Google Scholar
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, Cooper C, Landi F, Rolland Y, Sayer AA, Schneider SM, Sieber CC, Topinkova E, Vandewoude M, Visser M, Zamboni M, Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the Extended Group for EWGSOP2. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48(1):16–31. https://doi.org/10.1093/ageing/afy169 . Erratum in: Age Ageing. 2019;48(4):601. PMID: 30312372; PMCID: PMC6322506.
Article PubMed Google Scholar
Cylus J, Figueras J, Normand C. Will population ageing spell the end of the welfare state? A review of evidence and policy options [Internet]. Sagan A, Richardson E, North J, White C, editors. Copenhagen (Denmark): European Observatory on Health Systems and Policies; 2019. PMID: 31820887.
Yuan D, Jin H, Liu Q, Zhang J, Ma B, Xiao W, Li Y. Publication trends for Sarcopenia in the World: a 20-Year bibliometric analysis. Front Med (Lausanne). 2022;9:802651. https://doi.org/10.3389/fmed.2022.802651 . PMID: 35223902; PMCID: PMC8873525.
Marengoni A, Angleman S, Melis R, Mangialasche F, Karp A, Garmen A, Meinow B, Fratiglioni L. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. 2011;10(4):430–9. https://doi.org/10.1016/j.arr.2011.03.003 . Epub 2011 Mar 23. PMID: 21402176.
Gao Q, Mei F, Shang Y, Hu K, Chen F, Zhao L, Ma B. Global prevalence of sarcopenic obesity in older adults: a systematic review and meta-analysis. Clin Nutr. 2021;40(7):4633–41. https://doi.org/10.1016/j.clnu.2021.06.009 . Epub 2021 Jun 21. PMID: 34229269.
Molino S, Dossena M, Buonocore D, Verri M. Sarcopenic obesity: an appraisal of the current status of knowledge and management in elderly people. J Nutr Health Aging. 2016;20(7):780-8. https://doi.org/10.1007/s12603-015-0631-8 . PMID: 27499312.
Khadra D, Itani L, Tannir H, Kreidieh D, El Masri D, El Ghoch M. Association between sarcopenic obesity and higher risk of type 2 diabetes in adults: a systematic review and meta-analysis. World J Diabetes. 2019;10(5):311–23. https://doi.org/10.4239/wjd.v10.i5.311 . PMID: 31139318; PMCID: PMC6522758.
Aggio DA, Sartini C, Papacosta O, Lennon LT, Ash S, Whincup PH, Wannamethee SG, Jefferis BJ. Cross-sectional associations of objectively measured physical activity and sedentary time with Sarcopenia and sarcopenic obesity in older men. Prev Med. 2016;91:264–72. Epub 2016 Aug 26. PMID: 27575317; PMCID: PMC5061552.
Rossi AP, Rubele S, Calugi S, Caliari C, Pedelini F, Soave F, Chignola E, Vittoria Bazzani P, Mazzali G, Dalle Grave R, Zamboni M. Weight cycling as a risk factor for low muscle mass and strength in a population of males and females with obesity. Obesity (Silver Spring). 2019;27(7):1068–1075. https://doi.org/10.1002/oby.22493 . PMID: 31231958.
Dent E, Morley JE, Cruz-Jentoft AJ, Arai H, Kritchevsky SB, Guralnik J, Bauer JM, Pahor M, Clark BC, Cesari M, Ruiz J, Sieber CC, Aubertin-Leheudre M, Waters DL, Visvanathan R, Landi F, Villareal DT, Fielding R, Won CW, Theou O, Martin FC, Dong B, Woo J, Flicker L, Ferrucci L, Merchant RA, Cao L, Cederholm T, Ribeiro SML, Rodríguez-Mañas L, Anker SD, Lundy J, Gutiérrez Robledo LM, Bautmans I, Aprahamian I, Schols JMGA, Izquierdo M, Vellas B. International clinical practice guidelines for sarcopenia (ICFSR): screening, diagnosis and management. J Nutr Health Aging. 2018;22(10):1148–1161. https://doi.org/10.1007/s12603-018-1139-9 . PMID: 30498820.
Poggiogalle E, Parrinello E, Barazzoni R, Busetto L, Donini LM. Therapeutic strategies for sarcopenic obesity: a systematic review. Curr Opin Clin Nutr Metab Care. 2021;24(1):33–41. https://doi.org/10.1097/MCO.0000000000000714 . PMID: 33323715.
Petermann-Rocha F, Balntzi V, Gray SR, Lara J, Ho FK, Pell JP, Celis-Morales C. Global prevalence of Sarcopenia and severe Sarcopenia: a systematic review and meta-analysis. J Cachexia Sarcopenia Muscle. 2022;13(1):86–99. https://doi.org/10.1002/jcsm.12783 . Epub 2021 Nov 23. PMID: 34816624; PMCID: PMC8818604.
Prado CM, Wells JC, Smith SR, Stephan BC, Siervo M. Sarcopenic obesity: a critical appraisal of the current evidence. Clin Nutr. 2012;31(5):583–601. https://doi.org/10.1016/j.clnu.2012.06.010 . Epub 2012 Jul 17. PMID: 22809635.
Article CAS PubMed Google Scholar
Balaj M, Huijts T, McNamara CL, Stornes P, Bambra C, Eikemo TA. Non-communicable diseases and the social determinants of health in the nordic countries: findings from the European Social Survey (2014) special module on the social determinants of health. Scand J Public Health. 2017;45(2):90–102. Epub 2017 Jan 27. PMID: 28128015.
Nordic Burden of Disease Collaborators. Life expectancy and disease burden in the Nordic countries: results from the Global Burden of Diseases, Injuries, and Risk Factors Study 2017. Lancet Public Health. 2019;4(12): e658-e669. doi: 10.1016/S2468-2667(19)30224-5. Epub 2019 Nov 20. PMID: 31759894; PMCID: PMC7098475.
Stockmarr A, Hejgaard T, Matthiessen J. Obesity prevention in the Nordic Countries. Curr Obes Rep. 2016;5(2):156 – 65. https://doi.org/10.1007/s13679-016-0206-y . PMID: 27033877.
Cuadrado A, Stjernberg M, Huynh D. Active and healthy ageing: heterogenous perspectives and nordic indicators. Nordens välfärdscenter/Nordic Welfare Centre; 2022.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336 – 41. https://doi.org/10.1016/j.ijsu.2010.02.007 . Epub 2010 Feb 18. Erratum in: Int J Surg. 2010;8(8):658. PMID: 20171303.
Sallfeldt ES, Mallmin H, Karlsson MK, Mellström D, Hailer NP, Ribom EL. Sarcopenia prevalence and incidence in older men - a MrOs Sweden study. Geriatr Nurs. 2023 Mar-Apr;50:102–8. https://doi.org/10.1016/j.gerinurse.2023.01.003 . Epub 2023 Feb 10. PMID: 36774676.
Sääksjärvi K, Härkänen T, Stenholm S, Schaap L, Lundqvist A, Koskinen S, Borodulin K, Visser M. Probable Sarcopenia, obesity, and risk of all-cause mortality: a pooled analysis of 4,612 participants. Gerontology. 2023;69(6):706–15. Epub 2023 Jan 30. PMID: 36716714.
Karlsson M, Becker W, Cederholm TE, Byberg L. A posteriori dietary patterns in 71-year-old Swedish men and the prevalence of Sarcopenia 16 years later. Br J Nutr Camb Univ Press. 2022;128(5):909–20. https://doi.org/10.1017/S0007114521003901 .
Article CAS Google Scholar
Dolin TG, Mikkelsen MK, Jakobsen HL, Vinther A, Zerahn B, Nielsen DL, Johansen JS, Lund CM, Suetta C. The prevalence of Sarcopenia and cachexia in older patients with localized colorectal cancer. J Geriatr Oncol. 2023;14(1):101402. Epub 2022 Nov 21. PMID: 36424269.
Paajanen P, Lindström I, Oksala N, Väärämäki S, Saari P, Mäkinen K, Kärkkäinen JM. Radiographically quantified Sarcopenia and traditional cardiovascular risk assessment in predicting long-term mortality after endovascular aortic repair. J Vasc Surg. 2022;76(4):908–e9152. Epub 2022 Mar 31. PMID: 35367563.
Sobestiansky S, Åberg AC, Cederholm T. Sarcopenia and malnutrition in relation to mortality in hospitalised patients in geriatric care - predictive validity of updated diagnoses. Clin Nutr ESPEN. 2021;45:442–8. Epub 2021 Jul 16. PMID: 34620352.
Papaioannou KG, Nilsson A, Nilsson LM, Kadi F. Healthy eating is Associated with Sarcopenia Risk in physically active older adults. Nutrients. 2021;13(8):2813. https://doi.org/10.3390/nu13082813 . PMID: 34444973; PMCID: PMC8401667.
Article CAS PubMed PubMed Central Google Scholar
Wallengren O, Bosaeus I, Frändin K, Lissner L, Falk Erhag H, Wetterberg H, Rydberg Sterner T, Rydén L, Rothenberg E, Skoog I. Comparison of the 2010 and 2019 diagnostic criteria for Sarcopenia by the European Working Group on Sarcopenia in Older people (EWGSOP) in two cohorts of Swedish older adults. BMC Geriatr. 2021;21(1):600. https://doi.org/10.1186/s12877-021-02533-y . PMID: 34702174; PMCID: PMC8547086.
Scott D, Johansson J, Gandham A, Ebeling PR, Nordstrom P, Nordstrom A. Associations of accelerometer-determined physical activity and sedentary behavior with Sarcopenia and incident falls over 12 months in community-dwelling Swedish older adults. J Sport Health Sci. 2021;10(5):577–84. Epub 2020 Feb 5. PMID: 34088651; PMCID: PMC8500807.
Veen J, Montiel-Rojas D, Nilsson A, Kadi F. Engagement in muscle-strengthening activities lowers Sarcopenia Risk in older adults already adhering to the Aerobic Physical Activity guidelines. Int J Environ Res Public Health. 2021;18(3):989. https://doi.org/10.3390/ijerph18030989 . PMID: 33499423; PMCID: PMC7908493.
Mølmen KS, Hammarström D, Pedersen K, Lian Lie AC, Steile RB, Nygaard H, Khan Y, Hamarsland H, Koll L, Hanestadhaugen M, Eriksen AL, Grindaker E, Whist JE, Buck D, Ahmad R, Strand TA, Rønnestad BR, Ellefsen S. Vitamin D3 supplementation does not enhance the effects of resistance training in older adults. J Cachexia Sarcopenia Muscle. 2021;12(3):599–628. https://doi.org/10.1002/jcsm.12688 . Epub 2021 Mar 31. PMID: 33788419; PMCID: PMC8200443.
Simonsen C, Kristensen TS, Sundberg A, Wielsøe S, Christensen J, Hansen CP, Burgdorf SK, Suetta C, de Heer P, Svendsen LB, Achiam MP, Christensen JF. Assessment of Sarcopenia in patients with upper gastrointestinal tumors: prevalence and agreement between computed tomography and dual-energy x-ray absorptiometry. Clin Nutr. 2021;40(5):2809–16. Epub 2021 Mar 26. PMID: 33933747.
Faxén-Irving G, Luiking Y, Grönstedt H, Franzén E, Seiger Å, Vikström S, Wimo A, Boström AM, Cederholm T. Do malnutrition, sarcopenia and frailty overlap in nursing-home residents? J Frailty Aging. 2021;10(1):17–21. https://doi.org/10.14283/jfa.2020.45 . PMID: 33331617.
Björkman MP, Suominen MH, Kautiainen H, Jyväkorpi SK, Finne-Soveri HU, Strandberg TE, Pitkälä KH, Tilvis RS. Effect of protein supplementation on physical performance in older people with sarcopenia-a randomized controlled trial. J Am Med Dir Assoc. 2020;21(2):226–e2321. Epub 2019 Nov 14. PMID: 31734121.
Jyväkorpi SK, Urtamo A, Kivimäki M, Strandberg TE. Macronutrient composition and sarcopenia in the oldest-old men: the Helsinki businessmen study (HBS). Clin Nutr. 2020;39(12):3839–41. https://doi.org/10.1016/j.clnu.2020.04.024 . Epub 2020 Apr 24. PMID: 32376097.
Probert N, Lööw A, Akner G, Wretenberg P, Andersson ÅG. A comparison of patients with hip fracture, ten years apart: morbidity, malnutrition and sarcopenia. J Nutr Health Aging. 2020;24(8):870–877. https://doi.org/10.1007/s12603-020-1408-2 . PMID: 33009538.
Sjöblom S, Sirola J, Rikkonen T, Erkkilä AT, Kröger H, Qazi SL, Isanejad M. Interaction of recommended levels of physical activity and protein intake is associated with greater physical function and lower fat mass in older women: Kuopio osteoporosis risk Factor- (OSTPRE) and fracture-Prevention Study. Br J Nutr. 2020;123(7):826–39. Epub 2020 Jan 8. PMID: 31910914; PMCID: PMC7054249.
von Berens Å, Obling SR, Nydahl M, Koochek A, Lissner L, Skoog I, Frändin K, Skoglund E, Rothenberg E, Cederholm T. Sarcopenic obesity and associations with mortality in older women and men - a prospective observational study. BMC Geriatr. 2020;20(1):199. https://doi.org/10.1186/s12877-020-01578-9 . PMID: 32517653; PMCID: PMC7285448.
Nielsen BR, Andersen HE, Haddock B, Hovind P, Schwarz P, Suetta C. Prevalence of muscle dysfunction concomitant with osteoporosis in a home-dwelling Danish population aged 65–93 years -the Copenhagen Sarcopenia Study. Exp Gerontol. 2020;138:110974. https://doi.org/10.1016/j.exger.2020.110974 . Epub 2020 May 25. PMID: 32464171.
Van Ancum JM, Alcazar J, Meskers CGM, Nielsen BR, Suetta C, Maier AB. Impact of using the updated EWGSOP2 definition in diagnosing Sarcopenia: a clinical perspective. Arch Gerontol Geriatr 2020 Sep-Oct;90:104125. https://doi.org/10.1016/j.archger.2020.104125 . Epub 2020 May 23. PMID: 32534364.
Björkman M, Jyväkorpi SK, Strandberg TE, Pitkälä KH, Tilvis RS. Sarcopenia indicators as predictors of functional decline and need for care among older people. J Nutr Health Aging. 2019;23(10):916–922. https://doi.org/10.1007/s12603-019-1280-0 . PMID: 31781719.
Björkman MP, Pitkala KH, Jyväkorpi S, Strandberg TE, Tilvis RS. Bioimpedance analysis and physical functioning as mortality indicators among older sarcopenic people. Exp Gerontol. 2019;122:42–6. https://doi.org/10.1016/j.exger.2019.04.012 . Epub 2019 Apr 24. PMID: 31026498.
Olesen SS, Büyükuslu A, Køhler M, Rasmussen HH, Drewes AM. Sarcopenia associates with increased hospitalization rates and reduced survival in patients with chronic pancreatitis. Pancreatology. 2019;19(2):245–51. https://doi.org/10.1016/j.pan.2019.01.006 . Epub 2019 Jan 14. PMID: 30665702.
Sobestiansky S, Michaelsson K, Cederholm T. Sarcopenia prevalence and associations with mortality and hospitalisation by various sarcopenia definitions in 85–89 year old community-dwelling men: a report from the ULSAM study. BMC Geriatr. 2019;19(1):318. https://doi.org/10.1186/s12877-019-1338-1 . PMID: 31747923; PMCID: PMC6864927.
Vikberg S, Sörlén N, Brandén L, Johansson J, Nordström A, Hult A, Nordström P. Effects of resistance training on functional strength and muscle mass in 70-Year-old individuals with pre-sarcopenia: a randomized controlled trial. J Am Med Dir Assoc. 2019;20(1):28–34. Epub 2018 Nov 7. PMID: 30414822.
Isanejad M, Sirola J, Mursu J, Rikkonen T, Kröger H, Tuppurainen M, Erkkilä AT. Association of the baltic sea and mediterranean diets with indices of sarcopenia in elderly women, OSPTRE-FPS study. Eur J Nutr. 2018;57(4):1435–48. https://doi.org/10.1007/s00394-017-1422-2 . Epub 2017 Mar 16. PMID: 28303397.
Mikkola TM, von Bonsdorff MB, Salonen MK, Simonen M, Pohjolainen P, Osmond C, Perälä MM, Rantanen T, Kajantie E, Eriksson JG. Body composition as a predictor of physical performance in older age: a ten-year follow-up of the Helsinki Birth Cohort Study. Arch Gerontol Geriatr. 2018 Jul-Aug;77:163–8. doi: 10.1016/j.archger.2018.05.009. Epub 2018 May 14. PMID: 29783137; PMCID: PMC5994345.
Ottestad I, Ulven SM, Øyri LKL, Sandvei KS, Gjevestad GO, Bye A, Sheikh NA, Biong AS, Andersen LF, Holven KB. Reduced plasma concentration of branched-chain amino acids in sarcopenic older subjects: a cross-sectional study. Br J Nutr. 2018;120(4):445–53. Epub 2018 Jun 18. PMID: 29909813.
Steihaug OM, Gjesdal CG, Bogen B, Kristoffersen MH, Lien G, Ranhoff AH. Sarcopenia in patients with hip fracture: a multicenter cross-sectional study. PLoS ONE. 2017;12(9):e0184780. https://doi.org/10.1371/journal.pone.0184780 . PMID: 28902873; PMCID: PMC5597226.
Jacobsen EL, Brovold T, Bergland A, Bye A. Prevalence of factors associated with malnutrition among acute geriatric patients in Norway: a cross-sectional study. BMJ Open. 2016;6(9):e011512. https://doi.org/10.1136/bmjopen-2016-011512 . PMID: 27601491; PMCID: PMC5020767.
Jansen RB, Christensen TM, Bülow J, Rørdam L, Holstein PE, Svendsen OL. Sarcopenia and body composition in diabetic Charcot osteoarthropathy. J Diabetes Complications. 2015 Sep-Oct;29(7):937–42. https://doi.org/10.1016/j.jdiacomp.2015.05.020 . Epub 2015 Jun 5. PMID: 26139557.
Frost M, Nielsen TL, Brixen K, Andersen M. Peak muscle mass in young men and Sarcopenia in the ageing male. Osteoporos Int. 2015;26(2):749–56. https://doi.org/10.1007/s00198-014-2960-6 . Epub 2014 Nov 22. PMID: 25416073.
Patil R, Uusi-Rasi K, Pasanen M, Kannus P, Karinkanta S, Sievänen H. Sarcopenia and osteopenia among 70-80-year-old home-dwelling finnish women: prevalence and association with functional performance. Osteoporos Int. 2013;24(3):787–96. https://doi.org/10.1007/s00198-012-2046-2 . Epub 2012 Jun 12. PMID: 22688541.
Papadopoulou SK, Tsintavis P, Potsaki P, Papandreou D. Differences in the prevalence of sarcopenia in community-dwelling, nursing home and hospitalized individuals. a systematic review and meta-analysis. J Nutr Health Aging. 2020;24(1):83–90. https://doi.org/10.1007/s12603-019-1267-x . PMID: 31886813.
Mayhew AJ, Amog K, Phillips S, Parise G, McNicholas PD, de Souza RJ, Thabane L, Raina P. The prevalence of sarcopenia in community-dwelling older adults, an exploration of differences between studies and within definitions: a systematic review and meta-analyses. Age Ageing. 2019;48(1):48–56. https://doi.org/10.1093/ageing/afy106 . PMID: 30052707.
Cao M, Lian J, Lin X, Liu J, Chen C, Xu S, Ma S, Wang F, Zhang N, Qi X, Xu G, Peng N. Prevalence of Sarcopenia under different diagnostic criteria and the changes in muscle mass, muscle strength, and physical function with age in Chinese old adults. BMC Geriatr. 2022;22(1):889. https://doi.org/10.1186/s12877-022-03601-7 . PMID: 36418979; PMCID: PMC9682713.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinková E, Vandewoude M, Zamboni M, European working group on sarcopenia in older people. sarcopenia: European consensus on definition and diagnosis: report of the European working group on sarcopenia in older people. Age Ageing. 2010;39(4):412–23. https://doi.org/10.1093/ageing/afq034 . Epub 2010 Apr 13. PMID: 20392703; PMCID: PMC2886201.
Verstraeten LMG, de Haan NJ, Verbeet E, van Wijngaarden JP, Meskers CGM, Maier AB. Handgrip strength rather than chair stand test should be used to diagnose s in geriatric rehabilitation inpatients: restoring health of acutely unwell adulTs (RESORT). Age Ageing. 2022;51(11):afac242. https://doi.org/10.1093/ageing/afac242 . PMID: 36413590; PMCID: PMC9681126.
Cheng KY, Chow SK, Hung VW, Wong CH, Wong RM, Tsang CS, Kwok T, Cheung WH. Diagnosis of sarcopenia by evaluating skeletal muscle mass by adjusted bioimpedance analysis validated with dual-energy X-ray absorptiometry. J Cachexia Sarcopenia Muscle. 2021;12(6):2163–73. Epub 2021 Oct 4. PMID: 34609065; PMCID: PMC8718029.
Sousa-Santos AR, Barros D, Montanha TL, Carvalho J, Amaral TF. Which is the best alternative to estimate muscle mass for sarcopenia diagnosis when DXA is unavailable? Arch Gerontol Geriatr. 2021 Nov-Dec;97:104517. https://doi.org/10.1016/j.archger.2021.104517 . Epub 2021 Sep 3. PMID: 34547538.
González Correa CH, Marulanda Mejía F, Castaño González PA, Vidarte Claros JA, Castiblanco Arroyabe HD. Bioelectrical impedance analysis and dual x-ray absorptiometry agreement for skeletal muscle mass index evaluation in sarcopenia diagnosis. Physiol Meas. 2020;41(6):064005. https://doi.org/10.1088/1361-6579/ab8e5f . PMID: 32348971.
Hwang B, Lim JY, Lee J, Choi NK, Ahn YO, Park BJ. Prevalence rate and associated factors of sarcopenic obesity in Korean elderly population. J Korean Med Sci. 2012;27(7):748–55. https://doi.org/10.3346/jkms.2012.27.7.748 . Epub 2012 Jun 29. PMID: 22787369; PMCID: PMC3390722.
Kera T, Kawai H, Hirano H, Kojima M, Fujiwara Y, Ihara K, Obuchi S. Differences in body composition and physical function related to pure Sarcopenia and sarcopenic obesity: a study of community-dwelling older adults in Japan. Geriatr Gerontol Int. 2017;17(12):2602–9. https://doi.org/10.1111/ggi.13119 . Epub 2017 Jun 28. PMID: 28657168.
Aibar-Almazán A, Martínez-Amat A, Cruz-Díaz D, Jiménez-García JD, Achalandabaso A, Sánchez-Montesinos I, de la Torre-Cruz M, Hita-Contreras F. Sarcopenia and sarcopenic obesity in Spanish community-dwelling middle-aged and older women: Association with balance confidence, fear of falling and fall risk. Maturitas. 2018;107:26–32. Epub 2017 Oct 7. PMID: 29169576.
Prokopidis K, Giannos P, Reginster JY, Bruyere O, Petrovic M, Cherubini A, Triantafyllidis KK, Kechagias KS, Dionyssiotis Y, Cesari M, Ibrahim K, Scott D, Barbagallo M, Veronese N, the Task Force on Pharmaceutical Strategy of the European Geriatric Medicine Society (EuGMS). Special interest group in Systematic Reviews and Meta-analyses and sarcopenia is associated with a greater risk of polypharmacy and number of medications: a systematic review and meta-analysis. J Cachexia Sarcopenia Muscle. 2023;14(2):671–683. https://doi.org/10.1002/jcsm.13190 . Epub 2023 Feb 13. PMID: 36781175; PMCID: PMC10067503.
Zhang N, Sundquist J, Sundquist K, Ji J. An increasing Trend in the prevalence of polypharmacy in Sweden: a nationwide register-based study. Front Pharmacol. 2020;11:326. https://doi.org/10.3389/fphar.2020.00326 . PMID: 32265705; PMCID: PMC7103636.
Dalle S, Rossmeislova L, Koppo K. The role of inflammation in age-related sarcopenia. Front Physiol. 2017;8:1045. https://doi.org/10.3389/fphys.2017.01045 . PMID: 29311975; PMCID: PMC5733049.
Riuzzi F, Sorci G, Arcuri C, Giambanco I, Bellezza I, Minelli A, Donato R. Cellular and molecular mechanisms of sarcopenia: the S100B perspective. J Cachexia Sarcopenia Muscle. 2018;9(7):1255–68. https://doi.org/10.1002/jcsm.12363 . Epub 2018 Nov 30. PMID: 30499235; PMCID: PMC6351675.
Yuan S, Larsson SC. Epidemiology of sarcopenia: prevalence, risk factors, and consequences. Metabolism. 2023;144:155533. https://doi.org/10.1016/j.metabol.2023.155533 . Epub 2023 Mar 11. PMID: 36907247.
Download references
Acknowledgements
Not applicable.
Open access funding provided by University of Southern Denmark
This work was done without any fund.
Author information
Fereshteh Baygi, Sussi Friis Buhl contributed equally to this work.
Authors and Affiliations
Research Unit of General Practice, Department of Public Health, University of Southern Denmark, Odense, Denmark
Fereshteh Baygi, Sussi Friis Buhl, Trine Thilsing, Jens Søndergaard & Jesper Bo Nielsen
You can also search for this author in PubMed Google Scholar
Contributions
FB conceived and designed the review, participated in literature review, data extraction, interpretation of the results and wrote the manuscript. SFB designed the review, participated in literature review, data extraction, and revised the manuscript. TT, JBN and JS contributed to the conception of the study and revised the manuscript critically. All the authors approved the final manuscript.
Corresponding authors
Correspondence to Fereshteh Baygi or Sussi Friis Buhl .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Baygi, F., Buhl, S.F., Thilsing, T. et al. Sarcopenia and sarcopenic obesity among older adults in the nordic countries: a scoping review. BMC Geriatr 24 , 421 (2024). https://doi.org/10.1186/s12877-024-04970-x
Download citation
Received : 12 November 2023
Accepted : 12 April 2024
Published : 13 May 2024
DOI : https://doi.org/10.1186/s12877-024-04970-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Sarcopenic obesity
- Nordic countries
BMC Geriatrics
ISSN: 1471-2318
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Recommendations for future research should be: Concrete and specific. Supported with a clear rationale. Directly connected to your research. Overall, strive to highlight ways other researchers can reproduce or replicate your results to draw further conclusions, and suggest different directions that future research can take, if applicable.
The conclusions are as stated below: i. Students' use of language in the oral sessions depicted their beliefs and values. based on their intentions. The oral sessions prompted the students to be ...
For example, recommendations from research on climate change can be used to develop policies that reduce carbon emissions and promote sustainability. Program development: Research recommendations can guide the development of programs that address specific issues. For example, recommendations from research on education can be used to develop ...
Here is a step-wise guide to build your understanding on the development of research recommendations. 1. Understand the Research Question: Understand the research question and objectives before writing recommendations. Also, ensure that your recommendations are relevant and directly address the goals of the study. 2.
Recommendation in research example. See below for a full research recommendation example that you can use as a template to write your own. Recommendation section. The current study can be interpreted as a first step in the research on COPD speech characteristics. However, the results of this study should be treated with caution due to the small ...
Make sure your solutions cover all relevant areas within your research scope. Consider different contexts, stakeholders, and perspectives affected by the recommendations. Be thorough in identifying potential improvement areas and offering appropriate actions. Don't add new information to this part of your paper.
Basic differences between implications and recommendations in research. Implications and recommendations in research are two important aspects of a research paper or your thesis or dissertation. Implications discuss the importance of the research findings, while recommendations offer specific actions to solve a problem.
The following recommendations for research are based on the study findings: Limited and variable access to services in the wider health and social care system is a significant barrier to reducing inappropriate conveyance to A&E. More research is needed to identify effective ways of improving the delivery of care across service boundaries ...
The inclusion of an action plan along with recommendation adds more weightage to your recommendation. Recommendations should be clear and conscience and written using actionable words. Recommendations should display a solution-oriented approach and in some cases should highlight the scope for further research.
How to formulate research recommendations. "More research is needed" is a conclusion that fits most systematic reviews. But authors need to be more specific about what exactly is required. Long awaited reports of new research, systematic reviews, and clinical guidelines are too often a disappointing anticlimax for those wishing to use them ...
Table of contents. Step 1: Restate the problem. Step 2: Sum up the paper. Step 3: Discuss the implications. Research paper conclusion examples. Frequently asked questions about research paper conclusions.
Examples of literature reviews. Step 1 - Search for relevant literature. Step 2 - Evaluate and select sources. Step 3 - Identify themes, debates, and gaps. Step 4 - Outline your literature review's structure. Step 5 - Write your literature review.
The initially stated overarching aim of this research was to identify the contextual factors and mechanisms that are regularly associated with effective and cost-effective public involvement in research. While recognising the limitations of our analysis, we believe we have largely achieved this in our revised theory of public involvement in research set out in Chapter 8. We have developed and ...
kinds of recommendations—(a) for further research, and (b) for future directions in policy making and professional development planning. Research Design The investigator used two information-gathering tools to collect the data for this study—a survey instrument and a semi-structured telephone interview protocol. The faculty development
Here are a few guidelines to enable you to write a good recommendation for your research paper. 1. ... A sample size of 142 subjects was purposively drawn from a population of 27, 057 students ...
Media Files: APA Sample Student Paper , APA Sample Professional Paper This resource is enhanced by Acrobat PDF files. Download the free Acrobat Reader. Note: The APA Publication Manual, 7 th Edition specifies different formatting conventions for student and professional papers (i.e., papers written for credit in a course and papers intended for scholarly publication).
During the past several months the panel has met and reviewed the research plan for the National Children's Study (NCS), various working papers of the study, and additional documents provided by the National Institute of Child Health and Human Development. The panel believes that this landmark study offers an unparalleled opportunity to examine the effects of environmental influences on ...
determined in response to research problem 1. When considered by all respondents in the context of the ten potential organizers offered for consideration, construction was ranked fifth in the civic-life sphere, sixth in the personal-life sphere, and fifth in the work life sphere. Although the sample populatio ns were different, an interesting
Sample reference entry for House of Representatives resolution: Anti-Phishing Act, H.R. 1099, 109th Cong. (2005). ... they present original research and are often useful for research papers. Sometimes, researchers refer to these types of reports as gray literature, and white papers are a type of this literature. See APA 7, Section 10.4 for more ...
98 CHAPTER 5 SUMMARY, CONCLUSIONS, AND RECOMMENDATIONS This chapter presents a summary of the study and conclusions derived from the analysis of data. The chapter concludes with recommendations. Summary The purpose of this study was to design and test an instrument to measure elementary teachers' satisfaction with their involvement in school ...
the purpose, research questions and results of the study. The implications of these findings and the resultant recommendations will also be explained. Recommendations were based on the conclusions and purpose of the study. 5.2 OVERVIEW OF THE STUDY The study was an exploratory, descriptive and contextual qualitative study. The
Offers Implications and Recommendations: Your research paper conclusion is an excellent place to discuss the broader implications of your research and suggest potential areas for further study. It's also an opportunity to offer practical recommendations based on your findings. ... let's look at a research paper conclusion sample. Research ...
6.2.6 Chapter 6: Summary, conclusions and recommendations. Chapter six, this Chapt er, presents the conclusions, guided by the research questions. as outlined in section 1.4 and section 5.4 ...
Share information about the importance of handwashing. Why it's important. Washing hands can keep you healthy and prevent the spread of respiratory and diarrheal infections.
Sleep plays a crucial role in the health and well-being of adolescents; however, inadequate sleep is frequently reported in numerous countries. This current paper aimed to describe sleep duration, factors impacting sleep, consequences of insufficient sleep and satisfaction with life in Norwegian adolescents, stratified by sex and by adherence to the 8-hour sleep recommendation, and to examine ...
The Neural Information Processing Systems Foundation is a non-profit corporation whose purpose is to foster the exchange of research advances in Artificial Intelligence and Machine Learning, principally by hosting an annual interdisciplinary academic conference with the highest ethical standards for a diverse and inclusive community.
Sarcopenia and sarcopenic obesity (SO) are age-related syndromes that may compromise physical and mental health among older adults. The Nordic countries differ from other regions on prevalence of disease, life-style behavior, and life expectancy, which may impact prevalence of sarcopenia and SO. Therefore, the aim of this study is to review the available evidence and gaps within this field in ...