We use cookies to give you the best experience possible. By continuing we’ll assume you’re on board with our cookie policy

- A Research Guide
- Research Paper Topics
- 40 Drug Abuse & Addiction Research Paper Topics

40 Drug Abuse & Addiction Research Paper Topics
Drug Abuse and Sociology
Drug abuse and medicine, drug abuse and psychology.
- Drug abuse and the degradation of neuron cells
- The social aspects of the drug abuse. The most vulnerable categories of people
- Drugs and religion. Drug abuse as the part of the sacred rituals
- Chronic Lymphocytic Leukemia
- Drug abuse as the part of human trafficking and as psychological defence of victims
- Reversible and irreversible consequences of drug abuse
- Drug abuse and minors
- Ethnic and cultural traditions that may lead to drug abuse
- Medical marijuana. Can legalizing it lead to drug abuse?
- The ethical questions of abusing painkiller drugs or other drugs that ease the state of a person
- The “club culture”. May it enhance the danger of drug abuse?
- Preventing drug abuse. Mandatory examination or voluntary learning: what will help most?
- The abstinence after the drug abuse. Rehabilitation and resocialization of the victims of it
- The harm done by drug abuse to the family and social relations
- The types of drugs and the impact of their abuse to the human body
- The positive effects of drugs. May they be reached without drawbacks of drug abuse?
- Alcoholics Anonymous, similar organisations and their role in overcoming the dependency
- Is constant smoking a drug abuse? Quitting smoking: government and social decisions
- Exotic addictions: game addiction, porn addiction etc. Do they have the effects similar to drug abuse?
- Substance abuse during pregnancy and before conceiving. What additional harm it causes?
- The correlation between drugs and spreading of HIV/AIDS
- Drug abuse and crime rates
- History of drug abuse. Opium houses, heroin cough syrup and others
- Drunk driving and drunk violence. The indirect victims of alcohol abuse
- The social rejection of the former drug abusers and the way to overcome it
- The main causes of drug abuse in the different social groups
- Drug abuse and mental health
- LGBTQ+ and drug abuse
- The development of drug testing. The governmental implementation of it
- Geniuses and drug abuse. Did drugs really helped them to create their masterpieces?
- Shall the laws about drug abuse be changed?
- Health Care Information Technology
- Drug abuse and global health throughout the 20-21 centuries
- Personal freedom or the safety of society: can drugs be allowed for personal use?
- Legal drinking age in different countries and its connection to the cultural diversity
- The different attitude to drugs and drug abuse in the different countries. Why it differs so much?
- Teenage and college culture. Why substance abuse is considered to be cool?
- Drugs, rape and robbery. Drugging people intentionally as the way to prevent them defending themselves
- 12-Step Programs and their impact on healing the drug addiction
- Alcohol, tobacco and sleeping pills advertising. Can it lead to more drug abuse?
By clicking "Log In", you agree to our terms of service and privacy policy . We'll occasionally send you account related and promo emails.
Sign Up for your FREE account
- Signs of Addiction
Addiction Research
Discover the latest in addiction research, from the neuroscience of substance use disorders to evidence-based treatment practices. reports, updates, case studies and white papers are available to you at hazelden betty ford’s butler center for research..

Why do people become addicted to alcohol and other drugs? How effective is addiction treatment? What makes certain substances so addictive? The Butler Center for Research at the Hazelden Betty Ford Foundation investigates these and other questions and publishes its scientific findings in a variety of alcohol and drug addiction research papers and reports. Research topics include:
- Evidence-based treatment practices
- Addiction treatment outcomes
- Addiction, psychiatry and the brain
- Addictive substances such as prescription opioids and heroin
- Substance abuse in youth/teens, older adults and other demographic groups such as health care or legal professionals
These research queries and findings are presented in the form of updates, white papers and case studies. In addition, the Butler Center for Research collaborates with the Recovery Advocacy team to study special-focus addiction research topics, summarized in monthly Emerging Drug Trends reports. Altogether, these studies provide the latest in addiction research for anyone interested in learning more about the neuroscience of addiction and how addiction affects individuals, families and society in general. The research also helps clinicians and health care professionals further understand, diagnose and treat drug and alcohol addiction. Learn more about each of the Butler Center's addiction research studies below.
Research Updates
Written by Butler Center for Research staff, our one-page, topic-specific summaries discuss current research on topics of interest within the drug abuse and addiction treatment field.
View our most recent updates, or view the archive at the bottom of the page.
Patient Outcomes Study Results at Hazelden Betty Ford
Trends and Patterns in Cannabis Use across Different Age Groups
Alcohol and Tobacco Harm Reduction Interventions
Harm Reduction: History and Context
Racial and Ethnic Health Disparities and Addiction
Psychedelics as Therapeutic Treatment
Sexual and Gender Minority Youth and SUDs
Health Care Professionals and Mental Health
Grief and Addiction
Helping Families Cope with Addiction
Emerging Drug Trends Report and National Surveys
Shedding New Light on America’s No. 1 Health Problem
In collaboration with the University of Maryland School of Public Health and with support from the Butler Center for Research, the Recovery Advocacy team routinely issues research reports on emerging drug trends in America. Recovery Advocacy also commissions national surveys on attitudes, behaviors and perspectives related to substance use. From binge drinking and excessive alcohol use on college campuses, to marijuana potency concerns in an age of legalized marijuana, deeper analysis and understanding of emerging drug trends allows for greater opportunities to educate, inform and prevent misuse and deaths.
Each drug trends report explores the topic at hand, documenting the prevalence of the problem, relevant demographics, prevention and treatment options available, as well as providing insight and perspectives from thought leaders throughout the Hazelden Betty Ford Foundation.
View the latest Emerging Drug Trends Report:
Pediatricians First Responders for Preventing Substance Use
- Clearing Away the Confusion: Marijuana Is Not a Public Health Solution to the Opioid Crisis
- Does Socioeconomic Advantage Lessen the Risk of Adolescent Substance Use?
- The Collegiate Recovery Movement Is Gaining Strength
- Considerations for Policymakers Regarding Involuntary Commitment for Substance Use Disorders
- Widening the Lens on the Opioid Crisis
- Concerns Rising Over High-Potency Marijuana Use
- Beyond Binging: “High-Intensity Drinking”
View the latest National Surveys :
- College Administrators See Problems As More Students View Marijuana As Safe
College Parents See Serious Problems From Campus Alcohol Use
- Youth Opioid Study: Attitudes and Usage
About Recovery Advocacy
Our mission is to provide a trusted national voice on all issues related to addiction prevention, treatment and recovery, and to facilitate conversation among those in recovery, those still suffering and society at large. We are committed to smashing stigma, shaping public policy and educating people everywhere about the problems of addiction and the promise of recovery. Learn more about recovery advocacy and how you can make a difference.
Evidence-Based Treatment Series
To help get consumers and clinicians on the same page, the Butler Center for Research has created a series of informational summaries describing:
- Evidence-based addiction treatment modalities
- Distinctive levels of substance use disorder treatment
- Specialized drug and alcohol treatment programs
Each evidence-based treatment series summary includes:
- A definition of the therapeutic approach, level of care or specialized program
- A discussion of applicability, usage and practice
- A description of outcomes and efficacy
- Research citations and related resources for more information
View the latest in this series:
Motivational Interviewing
Cognitive Behavioral Therapy
Case Studies and White Papers
Written by Hazelden Betty Ford Foundation researchers and clinicians, case studies and white papers presented by the Butler Center for Research provide invaluable insight into clinical processes and complex issues related to addiction prevention, treatment and recovery. These in-depth reports examine and chronicle clinical activities, initiatives and developments as a means of informing practitioners and continually improving the quality and delivery of substance use disorder services and related resources and initiatives.
- What does it really mean to be providing medication-assisted treatment for opioid addiction?
Adolescent Motivational Interviewing
Peer Recovery Support: Walking the Path Together
Addiction and Violence During COVID-19
The Brain Disease Model of Addiction
Healthcare Professionals and Compassion Fatigue
Moving to Trauma-Responsive Care
Virtual Intensive Outpatient Outcomes: Preliminary Findings
Driving Under the Influence of Cannabis
Vaping and E-Cigarettes
Using Telehealth for Addiction Treatment
Grandparents Raising Grandchildren
Substance Use Disorders Among Military Populations
Co-Occurring Mental Health and Substance Use Disorders
Women and Alcohol
Prescription Rates of Opioid Analgesics in Medical Treatment Settings
Applications of Positive Psychology to Substance Use Disorder
Substance Use Disorders Among Legal Professionals
Factors Impacting Early Alcohol and Drug Use Among Youths
Animal-Assisted Therapy for Substance Use Disorders
Prevalence of Adolescent Substance Misuse
Problem Drinking Behaviors Among College Students
The Importance of Recovery Management
Substance Use Factors Among LGBTQ individuals
Prescription Opioids and Dependence
Alcohol Abuse Among Law Enforcement Officers
Helping Families Cope with Substance Dependence
The Social Norms Approach to Student Substance Abuse Prevention
Drug Abuse, Dopamine and the Brain's Reward System
Women and Substance Abuse
Substance Use in the Workplace
Health Care Professionals: Addiction and Treatment
Cognitive Improvement and Alcohol Recovery
Drug Use, Misuse and Dependence Among Older Adults
Emerging Drug Trends
Does Socioeconomic Advantage Lessen the Risk of Adolescent Substance Use
The Collegiate Recovery Movement is Gaining Strength
Involuntary Commitment for Substance Use Disorders
Widening the Lens of the Opioid Crisis
Beyond Binge Drinking: High Intensity Drinking
High Potency Marijuana
National Surveys
College Administrators See Problems as More Students View Marijuana as Safe
Risky Opioid Use Among College-Age Youth
Case Studies/ White Papers
What does it really mean to be providing medication-assisted treatment for opioid addiction
Are you or a loved one struggling with alcohol or other drugs? Call today to speak confidentially with a recovery expert. Most insurance accepted.
Harnessing science, love and the wisdom of lived experience, we are a force of healing and hope for individuals, families and communities affected by substance use and mental health conditions..
Identifying research gaps in substance use disorder: A systematic methodology and prioritized list
Affiliation.
- 1 a Psychological Health Center of Excellence, Defense Health Agency , Falls Church , VA , USA.
- PMID: 30668154
- DOI: 10.1080/00952990.2018.1558229
Background : This paper presents a new methodology for identifying and prioritizing research gaps, contributing to the nascent literature on systematic ways to identify research gaps. Objectives : The goal of this paper is to report on a gaps analysis of substance use disorder (SUD) research. Based on input from Military Health System stakeholders, we selected the following subtopics as priorities: alcohol use disorder (AUD) and comorbid conditions, prescription opioids, and novel synthetic drugs (NSDs), including synthetic cannabinoids, synthetic cathinones, novel synthetic opioids, and e-cigarette use. Methods: Statements of research needs were extracted from authoritative source reports. A work group of 13 subject matter experts then supplemented, consolidated, and refined the statements. Support for each statement was rated based on predetermined metrics to produce a list of high-priority potential research gaps. Work group members searched both published and ongoing research literature to determine whether these potential gaps were sufficiently addressed in the literature. Finally, to prioritize the gaps, work group members rated them on a set of metrics. Results : The work group reduced 175 statements of research needs to a list of 18 final prioritized gaps: nine for AUD, four for prescription opioids, and five for NSDs. For each topic, we present a prioritized list of gaps. Conclusions : This paper describes a method to identify and prioritize research gaps relevant to military and civilian research and presents the prioritized SUD gaps. Our methodology and findings can inform policy makers, researchers, and funding agencies as they consider investments in future research.
Keywords: Substance use disorder; alcohol use disorder; novel synthetic drugs; prescription opioids; research gap analysis.
- Analgesics, Opioid
- Biomedical Research / methods*
- Health Priorities*
- Military Health*
- Prescription Drugs
- Stakeholder Participation
- Substance-Related Disorders / prevention & control*
- Synthetic Drugs
- Systematic Reviews as Topic

Pathways of Addiction: Opportunities in Drug Abuse Research (1996)
Chapter: 1. introduction, 1 introduction.
Drug abuse research became a subject of sustained scientific interest by a small number of investigators in the late nineteenth and early twentieth centuries. Despite their creative efforts to understand drug abuse in terms of general advances in biomedical science, the medical literature of the early twentieth century is littered with now-discarded theories of drug dependence, such as autointoxication and antibody toxins, and with failed approaches to treatment. Eventually, escalating social concern about the use of addictive drugs and the emergence of the biobehavioral sciences during the post-World War II era led to a substantial investment in drug abuse research by the federal government (see Appendix B ). That investment has yielded substantial advances in scientific understanding about all facets of drug abuse and has also resulted in important discoveries in basic neurobiology, psychiatry, pain research, and other related fields of inquiry. In light of how little was understood about drug abuse such a short time ago, the advances of the past 25 years represent a remarkable scientific accomplishment. Yet there remains a disconnect between what is now known scientifically about drug abuse and addiction, the public's understanding of and beliefs about abuse and addiction, and the extent to which what is known is actually applied in public health settings.
During its brief history, drug abuse research has been supported mainly by the federal government, with occasional investments by major private foundations. At the federal level, the lead agency for drug abuse research is the National Institute on Drug Abuse (NIDA), which supports
85 percent of the world's research on drug abuse and addiction. Other sponsoring agencies include the National Institute of Mental Health (NIMH), the National Institute on Alcohol Abuse and Alcoholism (NIAAA), and the Substance Abuse and Mental Health Services Administration (SAMHSA), all in the Department of Health and Human Services; as well as the Office of Justice Programs (OJP) in the Department of Justice. Throughout the federal government, the FY 1995 investment in drug abuse research and development was $542.2 million, which represents 4 percent of the $13.3 billion spent by the federal government on drug abuse (ONDCP, 1996). By comparison, $8.5 billion (64 percent of the FY 1995 budget) was spent on criminal justice programs, 1 $2.7 billion (20 percent) on treatment of drug abuse, and $1.6 billion (12 percent) on prevention efforts.
In 1992, the General Accounting Office (GAO) released a report Drug Abuse Research: Federal Funding and Future Needs, which recommended that Congress review the place of research in drug control policy and its modest 4 percent share of the drug control budget. The report questioned whether the federal commitment to research was adequate, given the enormity of research needs (GAO, 1992), and whether adequate evaluation research was being conducted to determine the efficacy of various drug control programs. In FY 1995, drug abuse research was still little more than 4 percent of the entire drug control budget.
In January 1995, NIDA requested the Institute of Medicine (IOM) to examine accomplishments in drug abuse research and provide guidance for future research opportunities. This report by the IOM Committee on Opportunities in Drug Abuse Research focuses broadly on opportunities and priorities for future scientific research in drug abuse. After a brief review of major accomplishments in drug abuse research, the remainder of this chapter discusses the vocabulary and basic concepts used in the report, highlights the importance of the nation's investment in drug abuse research, and explores some of the factors that could improve the yield from that investment.
MAJOR ACHIEVEMENTS IN DRUG ABUSE RESEARCH
There have been remarkable achievements in drug abuse research over the past quarter of a century as researchers have learned more about the biological and psychosocial aspects of drug use, abuse, and dependence. Behavioral researchers have developed animal and human mod-
els of drug-seeking behavior, that have, for example, yielded objective measures of initiation and repeated administration of drugs, thereby providing the scientific foundation for assessments of "abuse liability" (i.e., the potential for abuse) of specific drugs (see Chapter 2 ). This information is an essential predicate for informed regulatory decisions under the Food, Drug and Cosmetic Act and the Controlled Substances Act. Taking advantage of technological advances in molecular biology, neuroscientists have identified receptors or receptor types in the brain for opioids, cocaine, benzodiazepines, and marijuana and have described the ways in which the brain adapts to, and changes after, exposure to drugs. Those alterations, which may persist long after the termination of drug use, appear to involve changes in gene expression. They may explain enhanced susceptibility to future drug exposure, thereby shedding light on the enigmas of withdrawal and relapse at the molecular level (see Chapter 3 ). Epidemiologists have designed and implemented epidemiological surveillance systems that enable policymakers to monitor patterns of drug use in the population ( Chapter 4 ) and that enable researchers to investigate the causes and consequences of drug use and abuse (Chapters 5 and 7 , respectively). Paralleling broader trends in health promotion and disease prevention in the past 20 years, the field of drug abuse prevention has made significant progress in evaluating the effectiveness of interventions implemented in a range of settings including communities, schools, and families (see Chapter 6 ).
Marked gains have also been made in treatment research, including improvements in diagnostic criteria; development of a wide range of treatment interventions and sophisticated methods to assess treatment outcome; and development and approval of Leo-alpha-acetylmethadol (LAAM), a medication for the treatment of opioid dependence. Pharmacological and psychosocial treatments, alone or in combination, have been shown to be effective for drug dependencies, and treatment has been shown to reduce drug use, HIV (human immunodeficiency virus) infection rates, health care costs, and criminal activity (see Chapter 8 ).
Drug abuse researchers have also made major contributions to knowledge in adjacent fields of scientific inquiry. For example, NIDA-sponsored research was the driving force in the identification of morphine-like substances that serve as neurotransmitters in specific neurons located throughout the central and peripheral nervous systems (Orson et al., 1994). Identification of these substances represents a dramatic breakthrough in understanding the mechanisms of pain, reinforcement, and stress. Additionally, the discovery of opioid peptides as neurotransmitters played a key role in the identification of numerous other peptide neurotransmitters (Cooper et al., 1991; Goldstein, 1994; Hokfelt et al., 1995). These discoveries have broadened the understanding of brain function and now
form the basis of many current strategies in the design of new drug treatments for neuropsychiatric disorders. Additionally, drug abuse research has contributed to the development of brain imaging techniques.
Drug abuse research has also provided a major impetus for neuropharmacological research in psychiatry since the late 1950s, when it was discovered that LSD (lysergic acid diethylamide; a hallucinogen that produces psychotic symptoms) affected the brain's serotonin systems (Cooper et al., 1991). That seminal discovery stimulated decades of research in the neuropharmacological basis of behavior and psychiatric disorders. The impact on antipsychotic research has been dramatic. In addition, stimulants (e.g., cocaine and amphetamine) were found to produce a state of paranoid psychosis, resembling schizophrenia, in some people. The actions of stimulants on the brain's dopamine pathways continue to inform researchers of the potential role of those pathways in the treatment, and perhaps the pathophysiology, of schizophrenia (Kahn and Davis, 1995). Drug abuse research also has had an impact on antidepressant research (e.g., the actions of drugs of abuse on the brain's serotonin systems have provided useful models with which to investigate the role of those systems in depression and mania). Depression is a risk factor for treatment failure in smoking cessation (Glassman et al., 1993) and depression-like symptoms are dominant during cocaine withdrawal (DiGregorio, 1990). Consequently, treatment of depression in nicotine and cocaine-dependent individuals has been an area of interest for drug abuse research.
Some drugs that are abused, most notably the opioid analgesics, have essential medical uses. Since its founding, NIDA has been the major supporter of research into brain mechanisms of pain and analgesia, analgesic tolerance, and analgesic pharmacology. The resulting discoveries have led to an understanding of which brain circuits are required to generate pain and pain relief (Wall and Melzack, 1994), have revolutionized the treatment of postoperative and cancer pain (Folly and Interesse, 1986; Car et al., 1992; Jacob et al., 1994), and have led to improved treatments for many other conditions that result in chronic pain (see Chapter 3 ).
VOCABULARY OF DRUG ABUSE
Ordinarily, scientific vocabulary evolves toward greater clarity and precision in response to new empirical discoveries and reconceptualizations. That creative process is evident within each of the disciplines of drug abuse research covered in various chapters of this report. Interestingly, however, the words describing the field as a whole, and connecting each chapter to the next, seem to defy the search for clarity and precision. Does "drug" include alcohol and tobacco? What is "abuse"? Are use and
abuse mutually exclusive categories? Are abuse and dependence mutually exclusive categories? Does use of illicit drugs per se amount to abuse? Does abuse include underage use of nicotine? Is addiction synonymous with dependence?
These ambiguities have persisted for decades because the vocabulary of drug abuse is inevitably influenced by peoples' attitudes and values. If the task were solely a scientific one, precise terminology would have emerged long before now. However, because the choice of words in this field always carries a nonscientific message, scientists themselves cannot always agree on a common vocabulary.
Consider the case of nicotine; from a pharmacological standpoint, nicotine is functionally similar to other psychoactive drugs. However, many researchers and policymakers choose to exclude nicotine from the category of drug. The same is true of alcohol; for example, other terms, such as ''chemical dependency" or "substance abuse," are often used as generic terms encompassing the abuse of nicotine and alcohol as well as abuse of illicit drugs. This semantic strategy is chosen to signify the difference in legal status among alcohol, nicotine, and illicit drugs. In recent years, however, a growing number of researchers have adopted a more inclusive use of the term drug. In the case of nicotine, this move tends to reflect a policy judgment that nicotine should be classified as a drug under the federal Food, Drug and Cosmetic Act.
In the committee's view, the term drug should be understood, in its generic sense, to encompass alcohol and nicotine as well as illicit drugs. It is very important for the general public to recognize that alcohol and nicotine constitute, by far, the nation's two largest drug problems, whether measured in terms of morbidity, mortality, or social cost. Abuse of and dependence on those drugs have serious individual and societal consequences. Continued separation of alcohol, nicotine, and illicit drugs in everyday speech is an impediment to public education, prevention, and therapeutic progress.
Although the committee uses the term drug, in its generic sense, to encompass alcohol and nicotine, the report focuses, at NIDA's request, on research opportunities relating to illicit drugs; research on alcohol and nicotine is discussed only when the scientific inquiries are intertwined. Because the report sometimes ranges more broadly than illicit drugs, however, the committee has adopted several semantic conventions to promote clarity and avoid redundancy. First, the term drug, unmodified, refers to all psychoactive drugs, including alcohol and nicotine. When reference is intended solely to illicit drugs such as heroin, cocaine, and other drugs regulated by the Controlled Substances Act, the committee says so explicitly. Occasionally, to ensure that the intended meaning is clear, the report refers to "illicit drugs and nicotine" or to "illicit drugs
and alcohol," as the case may be. Additionally, the words opiate and opioid are used interchangeably, although opiates are derivative of morphine and opioids are all compounds with morphine-like properties (they may be synthetic and not resemble morphine chemically).
The report employs the standard three-stage conceptualization of drug-taking behavior that applies to all psychoactive drugs, whether licit or illicit. Each stage—use, abuse, dependence—is marked by higher levels of use and increasingly serious consequences. Thus, when the report refers to the "use" of drugs, the term is usually employed in a narrow sense to distinguish it from intensified patterns of use. Conversely, the term "abuse" is used to refer to any harmful use, irrespective of whether the behavior constitutes a "disorder'' in the DSM-IV diagnostic nomenclature (see Appendix C ). When the intent is to emphasize the clinical categories of abuse and dependence, that is made clear.
The committee also draws a clear distinction between patterns of drug-taking behavior, however described, and the harmful consequences of that behavior for the individual and for society. These consequences include the direct, acute effects of drug taking such as a drug-induced toxic psychosis or impaired driving, the effects of repeated drug taking on the user's health and social functioning, and the effects of drug-seeking behavior on the individual and society. It bears emphasizing that adverse consequences can be associated with patterns of drug use that do not amount to abuse or dependence in a clinical sense, although the focus of this report and the committee's recommendations is on the more intensified patterns of use (i.e., abuse and dependence) since they cause the majority of the serious consequences.
DEFINITIONS AND BASIC CONCEPTS
Drug use may be defined as occasional use strongly influenced by environmental factors. Drug use is not a medical disorder and is not listed as such in either of the two most important diagnostic manuals—the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSMIV; APA, 1994); or the International Classification of Diseases (ICD-10; WHO, 1992). (See Appendix C for DSM-IV and ICD-10 diagnostic criteria.) Drug use implies intake for nonmedical purposes; it may or may not be accompanied by clinically significant impairment or distress on a given occasion.
Drug abuse is characterized in DSM-IV as including regular, sporadic, or intensive use of higher doses of drugs leading to social, legal, or interpersonal problems. Like DSM-IV, ICD-10 identifies a nondependent but problematic syndrome of drug use but calls it "harmful use" instead
of abuse. This syndrome is defined by ICD-10 as use resulting in actual physical or psychological harm.
Drug dependence (or addiction) is characterized in both DSM-IV and ICD-10 as drug-seeking behavior involving compulsive use of high doses of one or more drugs, either licit or illicit, for no clear medical indication, resulting in substantial impairment of health and social functioning. Dependence is usually accompanied by tolerance and withdrawal 2 and (like abuse) is generally associated with a wide range of social, legal, psychiatric, and medical problems. Unlike patients with chronic pain or persistent anxiety, who take medication over long periods of time to obtain relief from a specific medical or psychiatric disorder (often with resulting tolerance and withdrawal), persons with dependence seek out the drug and take it compulsively for nonmedical effects.
Tolerance occurs when certain medications are taken repeatedly. With opiates for example, it can be detected after only a few days of use for medical purposes such as the treatment of pain. If the patient suddenly stops taking the drug, a withdrawal syndrome may ensue. Physicians often confuse this phenomenon, referred to as physical dependence, with true addiction. That can lead to withholding adequate medication for the treatment of pain because of the very small risk that addiction with drug-seeking behavior may occur.
As a consequence of its compulsive nature involving the loss of control over drug use, dependence (or addiction) is typically a chronically relapsing disorder (IOM, 1990, 1995; Meter, 1996; O'Brien and McLennan, 1996; McLennan et al., in press). Although individuals with drug dependence can often complete detoxification and achieve temporary abstinence, they find it very difficult to sustain that condition and avoid relapse over time. Most persons who achieve sustained remission do so only after a number of cycles of detoxification and relapse (Dally and Marital, 1992). Relapse is caused by a constellation of biological, family, social, psychological, and treatment factors and is demonstrated by the fact that at least half of former cigarette smokers quit three or more times before they successfully achieve stable remission from nicotine addiction (Schilling, 1992). Similarly, within one year of treatment, relapse occurs in 30-50 percent of those treated for drug dependence, although the level
of drug use may not be as high as before treatment (Daley and Marlatt, 1992; McLellan et al., in press). Unlike those who use (or even abuse) drugs, individuals with addiction have a substantially diminished ability to control drug consumption, a factor that contributes to their tendency to relapse.
Another terminological issue arises in relation to the terms addiction and dependence. For some scientists, the proper terms for compulsive drug seeking is addiction, rather than dependence. In their view, addiction more clearly signifies the essential behavioral differences between compulsive use of drugs for their nonmedical effects and the syndrome of "physical dependence" that can develop in connection with repeated medical use. In response, many scientists argue that dependence has been defined in both ICD-10 and DSM-IV to encompass the behavioral features of the disorder and has become the generally accepted term in the diagnostic nomenclature. Moreover, some scientists object to the term addiction on the grounds that it is associated with stigmatizing social images and that a less pejorative term would help to promote public understanding of the medical nature of the condition. The committee has not attempted to resolve this controversy. For purposes of this report, the terms addiction and dependence are used interchangeably.
An inherent aspect of drug addiction is the propensity to relapse. Relapse should not be viewed as treatment failure; addiction itself should be considered a brain disease similar to other chronic and relapsing conditions such as hypertension, diabetes, and asthma (IOM, 1995; O'Brien and McLellan, 1996). In the latter, significant improvement is considered successful treatment even though complete remission or cure is not achieved. In the area of drug abuse, however, many individuals (both lay and professional) expect treatment programs to perform like vaccine programs, where one episode of treatment offers lifetime immunity. Not surprisingly, because of that expectation, people are inevitably disappointed in the relatively high relapse rates associated with most treatments. If, however, addiction is understood as a chronically relapsing brain disease, then—for any one treatment episode—evidence of treatment efficacy would include reduced consumption, longer abstention periods, reduced psychiatric symptoms, improved health, continued employment, and improved family relations. Most of those results are demonstrated regularly in treatment outcome studies.
The idea that drug addiction is a chronic relapsing condition, requiring long-term attention, has been resisted in the United States and in some other countries (Brewley, 1995). Many lay people view drug addiction as a character defect requiring punishment or incarceration. Proponents of the medical model, however, point to the fact that addiction is a distinct morbid process that has characteristics and identifiable signs and
symptoms that affect organ systems (Miller, 1991; Meter, 1996). Characterization of addiction as a brain disease is bolstered by evidence of genetic vulnerability to addiction, physical correlates of its clinical course, physiological changes as a result of repeated drug use, and fundamental changes in brain chemistry as evidenced by brain imaging (Volkow et al., 1993). This is not to say that behavioral, social, and environmental factors are immaterial—they all play a role in onset and outcome, just as they do in heart disease, kidney disease, tuberculosis, or other infectious diseases. Thus, the contemporary understanding of disease fully incorporates the voluntary behavioral elements that lead many people to be skeptical about the applicability of the medical model to drug addiction. In any case, the committee embraces the disease concept, not because it is indisputable but because this paradigm facilitates scientific investigation in many important areas of knowledge, without inhibiting or distorting scientific inquiry in other parts of the field.
IMPORTANCE OF DRUG ABUSE RESEARCH
The widespread prevalence of illicit drug use in the United States is well documented in surveys of households, students, and prison and jail inmates ( Chapter 4 ). Based on the National Household Survey on Drug Abuse (NHSDA), an annual survey presently sponsored by SAMHSA, it was estimated that in 1994, 12.6 million people had used illicit drugs (primarily marijuana) in the past month (SAMHSA, 1995). That figure represents 6 percent of the population 12 years of age or older. 3 The number of heavy drug users, using drugs at least once a week, is difficult to determine. It has been estimated that in 1993 there were 2.1 million heavy cocaine users and 444,000-600,000 heavy heroin users (Rhodes et al., 1995). This population represents a significant burden to society, not only in terms of federal expenditures but also in terms of costs related to the multiple consequences of drug abuse (see Chapter 7 ).
The ultimate aim of the nation's investment in drug abuse research is to enable society to take effective measures to prevent drug use, abuse, and dependence, and thereby reduce its adverse individual and social consequences and associated costs. The adverse consequences of drug abuse are numerous and profound and affect the individual's physical health and psychological and social functioning. Consequences of drug abuse include increased rates of HIV infection and tuberculosis (TB); education and vocational impairment; developmental harms to children of
drug-using parents associated with fetal exposure or maltreatment and neglect; and increased violence (see Chapter 7 ). It now appears that injection drug use is the leading risk factor for new HIV infection in the United States (Holmberg, 1996). Most (80 percent) HIV-infected heterosexual men and women who do not use injection drugs have been infected through sexual contact with HIV-infected injection drug users (IUDs). Thus, it is not surprising that the geographic distribution of heterosexual AIDS cases has been essentially the same as the distribution of male injection drug users' AIDS cases (Holmberg, 1996) Further, the IUDs-associated HIV epidemic in men is reflected in the heterosexual epidemic in women, which is reflected in HIV infection in children (CDC, 1995). Nearly all children who acquire HIV infection do so prenatal (see Chapter 7 ).
The extent of the impact of drug use and abuse on society is evidenced by its enormous economic burden. In 1990, illicit drug abuse is estimated to have cost the United States more than $66 billion. When the cost of illicit drug use and abuse is tallied with that of alcohol and nicotine ( Table 1.1 ), the collective cost of drug use and abuse exceeds the estimated annual $117 billion cost of heart disease and the estimated annual $104 billion cost of cancer (AHA, 1992; ACS, 1993; D. Rice, University of California at San Francisco, personal communication, 1995).
As noted above, the federal government accounts for a large segment of the societal expenditure on illicit drug abuse control—spending more than $13.3 billion in FY 1995 (ONDCP, 1996). About two-thirds was devoted to interdiction, intelligence, incarceration, and other law enforcement activities. Research, however, accounts for only 4 percent of federal outlays, a percentage that has remained virtually unchanged since 1981 (ONDCP, 1996) ( Figure 1.1 ). Given the social costs of illicit drug abuse and the enormity of the federal investment in prevention and control, research into the causes, consequences, treatment, and prevention of drug abuse should have a higher priority. Enhanced support for drug abuse research would be a socially sound investment, because scientific research can be expected to generate new and improved treatments, as well as prevention and control strategies that can help reduce the enormous social burden associated with drug abuse.
THE CONTEXT OF DRUG ABUSE RESEARCH
In the chapters that follow, the committee identifies research initiatives that seem most promising and most likely to lead to successful efforts to reduce drug abuse and its associated social costs. Although the yield from these initiatives will depend largely on the creativity and skill of scientists, the many contextual factors that will also have a major bear-
TABLE 1.1 Estimated Economic Costs (million dollars) of Drug Abuse, 1990

FIGURE 1.1 Federal drug control budget trends (1981-1995). NOTE: Figures are in current dollars. SOURCE: ONDCP (1996).
ing on the payoff from scientific inquiry cannot be ignored. The committee has identified six major factors that, if successfully addressed, could optimize the gains made in each area of drug abuse research: stable funding; use of a comprehensive public health framework; wider acceptance of a medical model of drug dependence; better translation of research findings into practice; raising the status of drug abuse research; and facilitating interdisciplinary research.
Stable Funding
A stable level of funding in any area of biomedical research is needed to sustain and build on research accomplishments, to retain a cadre of experts in a field, and to attract young investigators. Drug abuse research, in comparison with many other research venues, has not enjoyed consistent federal support (IOM, 1990, 1995; see also Appendix B ). The field has suffered from difficulties in recruiting and retaining young researchers and clinicians and in maintaining a stable research infrastructure (IOM, 1995). Society's capacity to contain and manage drug abuse
depends upon a stable, long-term investment in research. The vicissitudes in federal research funding often reflect changing currents in public opinion toward drugs and drug users ( Appendix B ). However, drug abuse will not disappear; it is an endemic social and public health problem. The nation must commit itself to a sustained effort. The social investment in research is an investment in "human capital" that must be sustained over the long term in order to reap the expected gains. An investment in this field is squandered if researchers who have been recruited and trained in drug abuse research are drawn to other fields because of uncertainty about the stability of future funding.
Adoption of a Comprehensive Public Health Framework
The social impact of drug abuse research can be enhanced significantly by conceptualizing goals and priorities within a comprehensive public health framework (Goldstein, 1994). All too often, public discourse about drug abuse is characterized by such unnecessary and fruitless disputes as whether drug abuse should be viewed as a social and moral problem or a health problem, whether the drug problem can best be solved by law enforcement or by medicine, whether priority should be placed on reducing supply or reducing demand, and so on. The truth is that these dichotomies oversimplify a brain disease impacted by a complex set of behaviors and a diverse array of potentially useful social responses. Forced choices of this nature also tend to inhibit or foreclose potentially useful research strategies. Confusion about social goals can lead to confusion about research priorities and can obscure the links between investigations viewing the subject through different lenses.
Some issues tend to recur. A prominent dispute centers on whether preventing drug use is important in itself or whether society should be more concerned with abuse or with the harmful consequences of use. The answer, of course, is that such a forced choice obscures, rather than clarifies, the issues. From a public health standpoint, drug use is a risk factor; the significance of use (whether of alcohol, nicotine, or illicit drugs) lies in the risk of harm associated with it (e.g., fires from smoking, impaired driving from alcohol or illicit drugs, or developmental setbacks) and in the risk that use will intensify, escalating to abuse or dependence. Those risks vary widely in relation to drug, user characteristics, social context, etc. Attention to the consequences of use and to the risk of escalation helps to set priorities (for research and policy) and provides a framework for assessing the impact of different interventions.
From a public policy standpoint, arguments about goals and priorities are fraught with controversy. From the standpoint of research strategy, however, the key lies in asking the right questions (e.g., What influ-
ences the pathways from use, to abuse, to dependence? What are the effects of needle exchange programs on illicit drug use and on HIV disease?) and in generating the knowledge required to facilitate informed policy debate. The main virtues of a comprehensive public health approach are that it helps to disentangle scientific questions from policy questions and that it encompasses all of the pertinent empirical questions, including the causes and consequences of use, abuse, and dependence, as well as the efficacy and cost of all types of interventions. In sum, the social payoff from drug abuse research can be enhanced substantially by integrating diverse strands of inquiry within a public health framework.
Acceptance of a Medical Model of Drug Dependence
Drug dependence is a chronic, relapsing brain disease that, like other diseases, can be evaluated and treated with the standard tools of medicine, including efforts in prevention, diagnosis, and treatment with medications and behavioral or psychosocial therapies. Unfortunately, the medical model of dependence is not universally accepted by health professionals and others in the treatment community; it is widely rejected within the law enforcement community and often by the public at large, which tends to view the complex and varied patterns of use, abuse, and dependence as an undifferentiated behavior rather than a medical problem.
Resistance to the medical model takes many forms. One is resistance to pharmacotherapies, such as methadone, that are seen as substituting licit drugs for illicit drugs without changing drug-taking behavior. Conversely, treatment approaches that adopt a rigid drug-free strategy preclude the use of medications for patients with other psychiatric disorders that are easily treated by pharmacotherapeutic approaches. On a subtler level, resistance to the use of pharmacotherapies is evidenced by the routine use of inadequate doses of methadone (D'Aunno and Vaughn, 1992). Finally, for others, all forms of drug abuse signify a failure of willpower or a moral weakness requiring punishment, incarceration, or moral education rather than treatment (Anglin and Hser, 1992).
Resistance to the medical model of drug dependence presents numerous barriers to research. Clinical researchers experience difficulty in soliciting participation by both treatment program administrators and patients, who are sometimes mistrustful of researchers' motives. If research involves a medication that is itself prone to abuse, there are additional regulatory requirements for drug scheduling, storage, and record keeping that act to discourage investigation (see Chapter 10 ; IOM, 1995). The ever-present threat of inappropriate intrusion by law enforcement agents has a chilling effect on treatment research (McDuff et al., 1993). All barri-
ers to inquiry, irrespective of whether they are legal or social in origin, raise the cost of research and discourage researchers from entering the field. Additionally, those barriers diminish the likelihood that a pharmaceutical company will invest in the development of antiaddiction medications (IOM, 1995). 4 Broader acceptance of the medical model of drug dependence would provide an incentive for researchers and clinicians to enter this field of research. Over time, a developing consensus in support of the medical model could facilitate common discourse, help to shape a shared research agenda within a public health framework, and diminish tensions between the research and treatment communities and the criminal justice system.
Better Translation of Research Findings into Practice and Policy
To benefit society, new research findings must be disseminated adequately to treatment providers, educators, law enforcement officials, and community leaders. In the case of prevention practices, it is often difficult for communities to change entrenched policies, particularly when combined with political imperatives for action to counteract drug abuse. In the case of treatment, technology transfer is impeded by the heterogeneity of providers and their marginalization at the outskirts of the medical community (see IOM, 1990, 1995; see also Chapter 8 ). Physicians and psychiatrists are seldom employed by specialized drug treatment facilities (approximately one-quarter employ medical doctors), and treatment is delivered by counselors whose training and supervision vary greatly and who have little access to and understanding of research results (Ball and Ross, 1991; Batten et al., 1993). These factors not only impede the transfer of research findings to the field but also impede communication from the field to the laboratory so that research designs can be modified in response to clinical realities (Pentz, 1994). Thus, there is a real need for bidirectional communication, from bench to bedside and back to the basic scientist (IOM, 1994).
The committee is aware, however, of recent technology transfer efforts in the field such as the Treatment Improvement Protocol Series, an initiative to establish guidelines for drug abuse treatment with an emphasis on incorporating research findings (SAMHSA, 1993), and the Prevention Enhancement Protocol System, a process implemented by the Center
for Substance Abuse Prevention in which scientists and practitioners develop protocols to identify and evaluate the strength of evidence on topics related to prevention interventions. Similar efforts will be invaluable for communicating and integrating research results to the treatment community.
Research frequently results in product development leading to changes in operations and an overall enhancement of the value of the enterprise. For example, in the pharmaceutical industry research often leads to the development of new medications or devices. In the public sector, however, research is often divorced from the implementation of findings and development. Research is often more basic than applied, and the fruits of research are not realized by the government, but by the private sector. Although that approach may be appropriate, it is unfortunately not always the most productive strategy for advancing research, knowledge, and product development. That is particularly true in the development of medications for opiate and cocaine addictions, where there is a great need for commitment from the private sector. However, many obstacles prevent active involvement of the pharmaceutical industry in this area of research and development (IOM, 1995).
A similar problem arises in relation to policymaking. Because debates about drug policy tend to be so highly polarized and politicized, research findings are often distorted, or selectively deployed, for rhetorical purposes. Researchers cannot prevent this practice, which is a common feature of political debate in a democratic society. However, researchers and their sponsors should not be indifferent to the disconnect between policy discourse and science. Researchers should establish and support institutional mechanisms for communicating an important message to policymakers and to the general public. Scientific research has produced a solid, and growing, body of knowledge about drug abuse and about the efficacy of various interventions that aim to prevent and control it. As long as drug abuse remains a poorly understood social problem, policy will be based mainly on wish and supposition; steps should be taken to educate policymakers about the scientific and technological advances in addiction research. Only then will it be possible for policymaking to support legislation that adequately funds new research and applies research findings. To some extent, persisting failure to reap the fruits of drug abuse research is attributable to the low visibility of the field—a problem to which the discussion now turns.
Raising the Status of Drug Abuse Research
Drug abuse research is often an undervalued area of inquiry, and most scientists and clinicians choose other disciplines in which to develop
their careers. Compared with other fields of research, investigators in drug abuse are often paid less, have less prestige among their peers, and must contend with the unique complexities of performing research in this area (e.g., regulations on controlled substances) (see IOM, 1995). The overall result is an insufficient number of basic and clinical researchers. IOM has recently begun a study, funded by the W. M. Keck Foundation of Los Angeles, to develop strategies to raise the status of drug abuse research. 5
Weak public support for this field of study is evident in unstable federal funding (see above), a lack of pharmaceutical industry investment in the development of antiaddiction medications (IOM, 1995), and inadequate funding for research training (IOM, 1995). NIDA's FY 1994 training budget, which is crucial to the flow of young researchers into the field, was about 2 percent of its extramural research budget, a percentage substantially lower than the overall National Institutes of Health (NIH) training budget, which averages 4.8 percent of its extramural research budget.
Beyond funding problems, investigators face a host of barriers to research: research subjects may pose health risks (e.g., TB, HIV/AIDS, and other infectious diseases), may be noncompliant, may deny their drug abuse problems, and may be involved in the criminal justice system. Even when research is successful and points to improvements in service delivery, the positive outcome may not be translated into practice or policy. For example, more than a year after the Food and Drug Administration's (FDA's) approval of levo-alpha-acetylmethadol (LAAM) as the first new medication for the treatment of opiate dependence in over 20 years, fewer than 1,000 patients nationwide actually had received the medication (IOM, 1995). More recently, scientific evidence regarding the beneficial effects of needle exchange programs (NRC, 1995) has received inadequate attention. Continuing indifference to scientific progress in drug abuse research inevitably depresses the status of the field, leading in turn to difficulties in recruiting new investigators.
Increasing Interdisciplinary Research
The breadth of expertise needed in drug abuse research spans many disciplines, including the behavioral sciences, pharmacology, medicine, and the neurosciences, and many fields of inquiry, including etiology, epidemiology, prevention, treatment, and health services research. Aspects of research relating to drug use tend to draw on developmental perspectives and to focus on general population samples in community settings, especially schools. Aspects of research relating to abuse and de-
pendence tend to be more clinical in nature, drawing on psychopathological perspectives. Additionally, a full account of any aspect of drug-taking behavior must also reflect an understanding of social context. The rich interplay between neuroscience and behavioral research and between basic and clinical research poses distinct challenges and opportunities.
Unfortunately, research tends to be fragmented within disciplinary boundaries. The difficulties in conducting successful interdisciplinary research are well known. Funds for research come from many separate agencies, such as the NIDA, NIMH, and SAMHSA. These agencies all have different programmatic emphases as they attempt to shape the direction of research in their respective fields. In times of funding constraints, agencies may be less inclined to fund projects at the periphery of their interests.
Additionally, NIH study sections, which rank grant proposals, are discipline specific, making it difficult for interdisciplinary proposals to ''qualify" (i.e., receive a high rank) for funding. Another problem is that the most advanced scientific literature tends to be compartmentalized within discipline or subject matter categories, making it difficult for scientists to see the whole field. The problem is exacerbated by what Tonry (1990) has called "fugitive literatures," studies carried out by private sector research firms or independent research agencies and available only in reports submitted to the sponsoring agency.
In light of lost opportunities for collaboration and interdisciplinary research, IOM (1995) previously recommended the creation and expansion of comprehensive drug abuse centers to coordinate all aspects of drug abuse research, training, and treatment. The field of drug abuse research presents a real opportunity to bridge the intellectual divide between the behavioral and neuroscience communities and to overcome the logistical impediments to interdisciplinary research.
INVESTING WISELY IN DRUG ABUSE RESEARCH
This report sets forth drug abuse research initiatives for the next decade based on a thorough assessment of what is now known and a calculated judgment about what initiatives are most likely to advance our knowledge in useful ways. This report is not meant to be a road map or tactical battle plan, but is best regarded as a strategic outline. Within each discipline of drug abuse research, the committee has highlighted priorities for future research. However, the committee did not make any attempt to prioritize recommendations across varied disciplines and fields of research. Prudent research planning must respond to newly emerging opportunities and needs while maintaining a steady commitment to the
achievement of long-term objectives. The ability to respond to new goals and needs may be the real challenge for the field of drug abuse research.
Drug abuse research is an important public investment. The ultimate aim of that investment is to reduce the enormous social costs attributable to drug abuse and dependence. Of course, drug abuse research must also compete for funding with research in other fields of public health, research in other scientific domains, and other pressing public needs. Recognizing the scarcity of resources, the committee has also considered ways in which the research effort can be harnessed most effectively to increase the yield per dollar invested. These include stable funding, use of a comprehensive public health framework, wider acceptance of a medical model of drug dependence, better translation of research findings into practice and policy, raising the status of drug abuse research, and facilitating interdisciplinary research.
The committee notes that there have been major accomplishments in drug abuse research over the past 25 years and commends NIDA for leading that effort. The committee is convinced that the field is on the threshold of significant advances, and that a sustained research effort will strengthen society's capacity to reduce drug abuse and to ameliorate its adverse consequences.
ORGANIZATION OF THE REPORT
This report sets forth a series of initiatives in drug abuse research. 6 Each chapter of the report covers a segment of the field, describes selected accomplishments, and highlights areas that seem ripe for future research. As noted, the committee has not prioritized areas for future research but, instead, has identified those areas that most warrant further exploration.
Chapter 2 describes behavioral models of drug abuse and demonstrates how the use of behavioral procedures has given researchers the ability to measure drug-taking objectively and to study the development, maintenance, and consequences of that behavior. Chapter 3 discusses drug abuse within the context of neurotransmission; it describes neurobiological advances in drug abuse research and provides the foundation for the current understanding of addiction as a brain disease. The epidemiological information systems designed to gather information on drug use in the United States are identified in Chapter 4 . The data collected from the systems provide an essential foundation for systematic study of
the etiology and consequences of drug abuse, which are addressed, respectively, in Chapters 5 and 7 . Chapter 6 addresses the efficacy of interventions designed to prevent drug abuse. The effectiveness of drug abuse treatment and the difficulties in treating special populations of drug users are discussed in Chapter 8 , while the impact of managed care on access, costs, utilization, and outcomes of treatment is addressed in Chapter 9 . Finally, Chapter 10 discusses the effects of drug control on public health and identifies areas for policy-relevant research.
Specific recommendations appear in each chapter. Although these recommendations reflect the committee's best judgment regarding priorities within the specific domains of research, the committee did not identify priorities or rank recommendations for the entire field of drug abuse research. Opportunities for advancing knowledge exist in all domains. It would be a mistake to invest too narrowly in a few fields of inquiry. At the present time, soundly conceived research should be pursued in all domains along the lines outlined in this report.
ACS (American Cancer Society). 1993. Cancer Facts and Figures, 1993 . Washington, DC: ACS.
AHA (American Heart Association). 1992. 1993 Heart and Stroke Fact Statistics . Dallas, TX: AHA.
Anglin MD, Hser Y. 1992. Treatment of drug abuse. In: Watson RR, ed. Drug Abuse Treatment. Vol. 3, Drug and Alcohol Abuse Reviews . New York: Humana Press.
APA (American Psychiatric Association). 1994. Diagnostic and Statistical Manual of Mental Disorders . 4th ed. Washington, DC: APA.
Ball JC, Ross A. 1991. The Effectiveness of Methadone Maintenance Treatment . New York: Springer-Verlag.
Batten H, Horgan CM, Prottas J, Simon LJ, Larson MJ, Elliott EA, Bowden ML, Lee M. 1993. Drug Services Research Survey Final Report: Phase I . Contract number 271-90-8319/1. Submitted to the National Institute of Drug Abuse. Waltham, MA: Bigel Institute for Health Policy, Brandeis University.
Brewley T. 1995. Conversation with Thomas Brewley. Addiction 90:883-892.
Carr DB, Jacox AK, Chapman CR, et al. 1992. Acute Pain Management: Operative or Medical Procedures and Trauma. Clinical Practice Guidelines . AHCPR Publication No. 92-0032. Rockville, MD: U.S. Public Health Service, Agency for Health Care Policy and Research.
CDC (Centers for Disease Control and Prevention). 1995. HIV/AIDS Surveillance Report 7(2).
Cooper JR, Bloom FE, Roth RH. 1991. The Biochemical Basis of Neuropharmacology . 6th ed. New York: Oxford University Press.
Daley DC, Marlatt GA. 1992. Relapse prevention: Cognitive and behavioral interventions. In: Lowinson JH, Ruiz P, Millman RB, Langrod JG, eds. Substance Abuse: A Comprehensive Textbook . Baltimore: Williams and Wilkins.
D'Aunno T, Vaughn TE. 1992. Variation in methadone treatment practices. Journal of the American Medical Association 267:253-258.
DiGregorio GJ. 1990. Cocaine update: Abuse and therapy. American Family Physician 41(1):247-250.
Foley KM, Inturrisi CE, eds. 1986. Opioid Analgesics in the Management of Clinical Pain. Advances in Pain Research and Therapy. Vol. 8. New York: Raven Press.
GAO (General Accounting Office). 1992. Drug Abuse Research: Federal Funding and Future Needs . GAO/PEMD-92-5. Washington, DC: GAO.
Glassman AH, Covey LS, Dalack GW, Stetner F, Rivelli SK, Fleiss J, Cooper TB. 1993. Smoking cessation, clonidine, and vulnerability to nicotine among dependent smokers. Clinical Pharmacology and Therapeutics 54(6):670-679.
Goldstein A. 1994. Addiction: From Biology to Drug Policy . New York: W.H. Freeman.
Hokfelt TGM, Castel MN, Morino P, Zhang X, Dagerlind A. 1995. General overview of neuropeptides. In: Bloom FE, Kupfer DJ, eds. Psychopharmacology: Fourth Generation of Progress . New York: Raven Press. Pp. 483-492.
Holmberg SD. 1996 . The estimated prevalence and incidence of HIV in 96 large U.S. metropolitan areas . American Journal of Public Health 86(5):642-654.
IOM (Institute of Medicine). 1990. Treating Drug Problems . Washington, DC: National Academy Press.
IOM (Institute of Medicine). 1994. AIDS and Behavior: An Integrated Approach . Washington, DC: National Academy Press.
IOM (Institute of Medicine). 1995. The Development of Medications for the Treatment of Opiate and Cocaine Addictions. Washington, DC: National Academy Press.
Jacox A, Carr DB, Payne R, et al. 1994. Management of Cancer Pain. Clinical Practice Guideline . AHCPR Publication No. 94-0592. Rockville, MD: U.S. Public Health Service, Agency for Health Care Policy and Research.
Kahn RS, Davis KL. 1995. New developments in dopamine and schizophrenia. In: Bloom FE, Kupfer DJ, eds. Psychopharmacology: Fourth Generation of Progress . New York: Raven Press. Pp. 1193-1204.
McDuff DR, Schwartz RP, Tommasello A, Tiegel S, Donovan T, Johnson JL. 1993. Outpatient benzodiazepine detoxification procedure for methadone patients. Journal of Substance Abuse Treatment 10:297-302.
McLellan AT, Metzger DS, Alterman Al, Woody GE, Durell J, O'Brien CP. In press. Is addiction treatment "worth it"? Public health expectations, policy-based comparisons. Milbank Quarterly .
Meyer R. 1996. The disease called addiction: Emerging evidence in a 200-year debate. Lancet 347:162-166.
Miller NS. 1991. Drug and alcohol addiction as a disease. In: Miller NS, ed. Comprehensive Handbook of Drug and Alcohol Addiction . New York: Marcel Dekker.
MMWR (Morbidity and Mortality Weekly Report). 1994. Medical care expenditures attributable to cigarette smoking, United States, 1993. Morbidity and Mortality Weekly Report 43(26):469-472.
NRC (National Research Council). 1995. Preventing HIV Transmission: The Role of Sterile Needles and Bleach . Washington, DC: National Academy Press.
O'Brien CP, McLellan AT. 1996. Myths about the treatment of addiction. Lancet 347:237-240.
Olson GA, Olson RD, Kastin AJ. 1994. Endogenous opiates, 1993. Peptides 15:1513-1556.
ONDCP (Office of National Drug Control Policy). 1996. National Drug Control Strategy . Washington, DC: ONDCP.
Pentz M. 1994. Directions for future research in drug abuse prevention. Preventive Medicine 23:646-652.
Rhodes W, Scheiman P, Pittayathikhun T, Collins L, Tsarfaty V. 1995. What America's Users Spend on Illegal Drugs, 1988-1993 . Prepared for the Office of National Drug Control Policy, Washington, DC.
Rice DP, Kelman S, Miller LS, Dunmeyer S. 1990. The Economic Costs of Alcohol and Drug Abuse and Mental Illness: 1985 . DHHS Publication No. (ADM) 90-1694. San Francisco: University of California, Institute for Health and Aging.
Rice DP, Max W, Novotny T, Shultz J, Hodgson T. 1992. The Cost of Smoking Revisited: Preliminary Estimates . Paper presented at the American Public Health Association Annual Meeting, November 23, 1992. Washington, DC.
SAMHSA (Substance Abuse and Mental Health Services Administration). 1993. Improving Treatment for Drug-Exposed Infants: Treatment Improvement Protocol (TIP) Series . Washington, DC: U.S. Department of Health and Human Services.
SAMHSA (Substance Abuse and Mental Health Services Administration). 1995. National Household Survey on Drug Abuse: Population Estimates 1994 . Washington, DC: U.S. Department of Health and Human Services.
Schelling TC. 1992 . Addictive drugs: The cigarette experience. Science 255:431-433.
Tonry M. 1990. Research on drugs and crime. In: Morris N, Tonry M, eds. Drugs and Crime . Vol. 13 . Chicago: University of Chicago Press.
Volkow ND, Fowler JS, Wang G-J, Hitzemann R, Logan J, Schlyer DJ, Dewey SI, Wolf AD. 1993. Decreased dopamine D2 receptor availability is associated with reduced frontal metabolism in cocaine abusers. Synapse 14:169-177.
Wall PD, Melzack R. 1994. Textbook of Pain . 3rd ed. Edinburg: Churchill-Livingstone.
WHO (World Health Organization). 1992. International Statistical Classification of Diseases and Related Health Problems . Tenth Revision. Geneva: WHO.
Drug abuse persists as one of the most costly and contentious problems on the nation's agenda. Pathways of Addiction meets the need for a clear and thoughtful national research agenda that will yield the greatest benefit from today's limited resources.
The committee makes its recommendations within the public health framework and incorporates diverse fields of inquiry and a range of policy positions. It examines both the demand and supply aspects of drug abuse.
Pathways of Addiction offers a fact-filled, highly readable examination of drug abuse issues in the United States, describing findings and outlining research needs in the areas of behavioral and neurobiological foundations of drug abuse. The book covers the epidemiology and etiology of drug abuse and discusses several of its most troubling health and social consequences, including HIV, violence, and harm to children.
Pathways of Addiction looks at the efficacy of different prevention interventions and the many advances that have been made in treatment research in the past 20 years. The book also examines drug treatment in the criminal justice setting and the effectiveness of drug treatment under managed care.
The committee advocates systematic study of the laws by which the nation attempts to control drug use and identifies the research questions most germane to public policy. Pathways of Addiction provides a strategic outline for wise investment of the nation's research resources in drug abuse. This comprehensive and accessible volume will have widespread relevance—to policymakers, researchers, research administrators, foundation decisionmakers, healthcare professionals, faculty and students, and concerned individuals.
READ FREE ONLINE
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.

- MJC Library & Learning Center
- Research Guides
Drug Abuse, Addiction, Substance Use Disorder
- Research Drug Abuse
Start Learning About Your Topic
Create research questions to focus your topic, find books in the library catalog, find articles in library databases, find web resources, cite your sources, key search words.
Use the words below to search for useful information in books and articles .
- substance use disorder
- substance abuse
- drug addiction
- substance addiction
- chemical dependency
- war on drugs
- names of specific drugs such as methamphetamine, cocaine, heroin
- opioid crisis
Background Reading:
It's important to begin your research learning something about your subject; in fact, you won't be able to create a focused, manageable thesis unless you already know something about your topic.
This step is important so that you will:
- Begin building your core knowledge about your topic
- Be able to put your topic in context
- Create research questions that drive your search for information
- Create a list of search terms that will help you find relevant information
- Know if the information you’re finding is relevant and useful
If you're working from off campus , you'll be prompted to log in just like you do for your MJC email or Canvas courses.
All of these resources are free for MJC students, faculty, & staff.
- Gale eBooks This link opens in a new window Use this database for preliminary reading as you start your research. Try searching these terms: addiction, substance abuse
Other eBooks from the MJC Library collection:
Use some of the questions below to help you narrow this broad topic. See "substance abuse" in our Developing Research Questions guide for an example of research questions on a focused study of drug abuse.
- In what ways is drug abuse a serious problem?
- What drugs are abused?
- Who abuses drugs?
- What causes people to abuse drugs?
- How do drug abusers' actions affect themselves, their families, and their communities?
- What resources and treatment are available to drug abusers?
- What are the laws pertaining to drug use?
- What are the arguments for legalizing drugs?
- What are the arguments against legalizing drugs?
- Is drug abuse best handled on a personal, local, state or federal level?
- Based on what I have learned from my research what do I think about the issue of drug abuse?
Why Use Books:
Use books to read broad overviews and detailed discussions of your topic. You can also use books to find primary sources , which are often published together in collections.
Where Do I Find Books?
You'll use the library catalog to search for books, ebooks, articles, and more.
What if MJC Doesn't Have What I Need?
If you need materials (books, articles, recordings, videos, etc.) that you cannot find in the library catalog , use our interlibrary loan service .
All of these resources are free for MJC students, faculty, & staff.
- EBSCOhost Databases This link opens in a new window Search 22 databases simultaneously that cover almost any topic you need to research at MJC. EBSCO databases include articles previously published in journals, magazines, newspapers, books, and other media outlets.
- Gale Databases This link opens in a new window Search over 35 databases simultaneously that cover almost any topic you need to research at MJC. Gale databases include articles previously published in journals, magazines, newspapers, books, and other media outlets.
- Psychology and Behavioral Sciences Collection This link opens in a new window Contains articles from nearly 560 scholarly journals, some dating as far back as 1965
- Access World News This link opens in a new window Search the full-text of editions of record for local, regional, and national U.S. newspapers as well as full-text content of key international sources. This is your source for The Modesto Bee from January 1989 to the present. Also includes in-depth special reports and hot topics from around the country. To access The Modesto Bee , limit your search to that publication. more... less... Watch this short video to learn how to find The Modesto Bee .
Use Google Scholar to find scholarly literature on the Web:

Browse Featured Web Sites:
- National Institute on Drug Abuse NIDA's mission is to lead the nation in bringing the power of science to bear on drug abuse and addiction. This charge has two critical components. The first is the strategic support and conduct of research across a broad range of disciplines. The second is ensuring the rapid and effective dissemination and use of the results of that research to significantly improve prevention and treatment and to inform policy as it relates to drug abuse and addiction.
- Drug Free America Foundation Drug Free America Foundation, Inc. is a drug prevention and policy organization committed to developing, promoting and sustaining national and international policies and laws that will reduce illegal drug use and drug addiction.
- Office of National Drug Control Policy A component of the Executive Office of the President, ONDCP was created by the Anti-Drug Abuse Act of 1988. ONDCP advises the President on drug-control issues, coordinates drug-control activities and related funding across the Federal government, and produces the annual National Drug Control Strategy, which outlines Administration efforts to reduce illicit drug use, manufacturing and trafficking, drug-related crime and violence, and drug-related health consequences.
- Drug Policy Alliance The Drug Policy Alliance (DPA) is the nation's leading organization promoting alternatives to current drug policy that are grounded in science, compassion, health and human rights.
Your instructor should tell you which citation style they want you to use. Click on the appropriate link below to learn how to format your paper and cite your sources according to a particular style.
- Chicago Style
- ASA & Other Citation Styles
- Last Updated: Apr 25, 2024 1:28 PM
- URL: https://libguides.mjc.edu/drugabuse
Except where otherwise noted, this work is licensed under CC BY-SA 4.0 and CC BY-NC 4.0 Licenses .
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Open access
- Published: 22 February 2021
Addiction as a brain disease revised: why it still matters, and the need for consilience
- Markus Heilig 1 ,
- James MacKillop ORCID: orcid.org/0000-0003-4118-9500 2 , 3 ,
- Diana Martinez 4 ,
- Jürgen Rehm ORCID: orcid.org/0000-0001-5665-0385 5 , 6 , 7 , 8 ,
- Lorenzo Leggio ORCID: orcid.org/0000-0001-7284-8754 9 &
- Louk J. M. J. Vanderschuren ORCID: orcid.org/0000-0002-5379-0363 10
Neuropsychopharmacology volume 46 , pages 1715–1723 ( 2021 ) Cite this article
89k Accesses
102 Citations
326 Altmetric
Metrics details
A Correspondence to this article was published on 03 May 2021
The view that substance addiction is a brain disease, although widely accepted in the neuroscience community, has become subject to acerbic criticism in recent years. These criticisms state that the brain disease view is deterministic, fails to account for heterogeneity in remission and recovery, places too much emphasis on a compulsive dimension of addiction, and that a specific neural signature of addiction has not been identified. We acknowledge that some of these criticisms have merit, but assert that the foundational premise that addiction has a neurobiological basis is fundamentally sound. We also emphasize that denying that addiction is a brain disease is a harmful standpoint since it contributes to reducing access to healthcare and treatment, the consequences of which are catastrophic. Here, we therefore address these criticisms, and in doing so provide a contemporary update of the brain disease view of addiction. We provide arguments to support this view, discuss why apparently spontaneous remission does not negate it, and how seemingly compulsive behaviors can co-exist with the sensitivity to alternative reinforcement in addiction. Most importantly, we argue that the brain is the biological substrate from which both addiction and the capacity for behavior change arise, arguing for an intensified neuroscientific study of recovery. More broadly, we propose that these disagreements reveal the need for multidisciplinary research that integrates neuroscientific, behavioral, clinical, and sociocultural perspectives.
Similar content being viewed by others
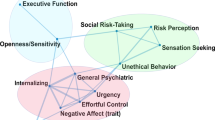
Subtypes in addiction and their neurobehavioral profiles across three functional domains

Drug addiction: from bench to bedside

The neurobiology of drug addiction: cross-species insights into the dysfunction and recovery of the prefrontal cortex
Introduction.
Close to a quarter of a century ago, then director of the US National Institute on Drug Abuse Alan Leshner famously asserted that “addiction is a brain disease”, articulated a set of implications of this position, and outlined an agenda for realizing its promise [ 1 ]. The paper, now cited almost 2000 times, put forward a position that has been highly influential in guiding the efforts of researchers, and resource allocation by funding agencies. A subsequent 2000 paper by McLellan et al. [ 2 ] examined whether data justify distinguishing addiction from other conditions for which a disease label is rarely questioned, such as diabetes, hypertension or asthma. It concluded that neither genetic risk, the role of personal choices, nor the influence of environmental factors differentiated addiction in a manner that would warrant viewing it differently; neither did relapse rates, nor compliance with treatment. The authors outlined an agenda closely related to that put forward by Leshner, but with a more clinical focus. Their conclusion was that addiction should be insured, treated, and evaluated like other diseases. This paper, too, has been exceptionally influential by academic standards, as witnessed by its ~3000 citations to date. What may be less appreciated among scientists is that its impact in the real world of addiction treatment has remained more limited, with large numbers of patients still not receiving evidence-based treatments.
In recent years, the conceptualization of addiction as a brain disease has come under increasing criticism. When first put forward, the brain disease view was mainly an attempt to articulate an effective response to prevailing nonscientific, moralizing, and stigmatizing attitudes to addiction. According to these attitudes, addiction was simply the result of a person’s moral failing or weakness of character, rather than a “real” disease [ 3 ]. These attitudes created barriers for people with substance use problems to access evidence-based treatments, both those available at the time, such as opioid agonist maintenance, cognitive behavioral therapy-based relapse prevention, community reinforcement or contingency management, and those that could result from research. To promote patient access to treatments, scientists needed to argue that there is a biological basis beneath the challenging behaviors of individuals suffering from addiction. This argument was particularly targeted to the public, policymakers and health care professionals, many of whom held that since addiction was a misery people brought upon themselves, it fell beyond the scope of medicine, and was neither amenable to treatment, nor warranted the use of taxpayer money.
Present-day criticism directed at the conceptualization of addiction as a brain disease is of a very different nature. It originates from within the scientific community itself, and asserts that this conceptualization is neither supported by data, nor helpful for people with substance use problems [ 4 , 5 , 6 , 7 , 8 ]. Addressing these critiques requires a very different perspective, and is the objective of our paper. We readily acknowledge that in some cases, recent critiques of the notion of addiction as a brain disease as postulated originally have merit, and that those critiques require the postulates to be re-assessed and refined. In other cases, we believe the arguments have less validity, but still provide an opportunity to update the position of addiction as a brain disease. Our overarching concern is that questionable arguments against the notion of addiction as a brain disease may harm patients, by impeding access to care, and slowing development of novel treatments.
A premise of our argument is that any useful conceptualization of addiction requires an understanding both of the brains involved, and of environmental factors that interact with those brains [ 9 ]. These environmental factors critically include availability of drugs, but also of healthy alternative rewards and opportunities. As we will show, stating that brain mechanisms are critical for understanding and treating addiction in no way negates the role of psychological, social and socioeconomic processes as both causes and consequences of substance use. To reflect this complex nature of addiction, we have assembled a team with expertise that spans from molecular neuroscience, through animal models of addiction, human brain imaging, clinical addiction medicine, to epidemiology. What brings us together is a passionate commitment to improving the lives of people with substance use problems through science and science-based treatments, with empirical evidence as the guiding principle.
To achieve this goal, we first discuss the nature of the disease concept itself, and why we believe it is important for the science and treatment of addiction. This is followed by a discussion of the main points raised when the notion of addiction as a brain disease has come under criticism. Key among those are claims that spontaneous remission rates are high; that a specific brain pathology is lacking; and that people suffering from addiction, rather than behaving “compulsively”, in fact show a preserved ability to make informed and advantageous choices. In the process of discussing these issues, we also address the common criticism that viewing addiction as a brain disease is a fully deterministic theory of addiction. For our argument, we use the term “addiction” as originally used by Leshner [ 1 ]; in Box 1 , we map out and discuss how this construct may relate to the current diagnostic categories, such as Substance Use Disorder (SUD) and its different levels of severity (Fig. 1) .
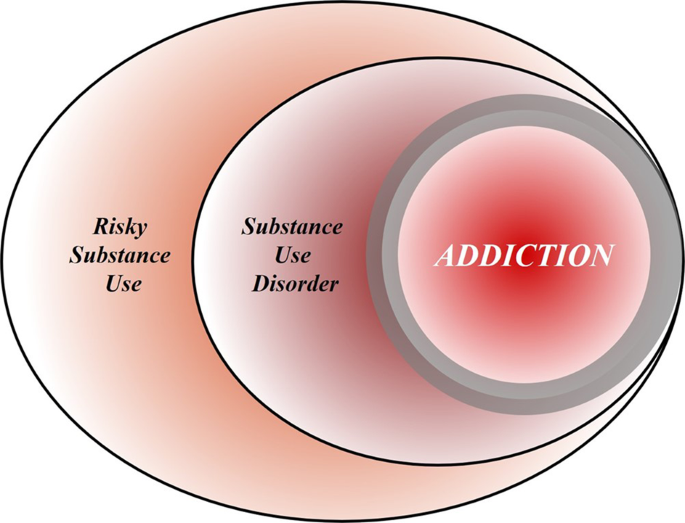
Risky (hazardous) substance use refers to quantity/frequency indicators of consumption; SUD refers to individuals who meet criteria for a DSM-5 diagnosis (mild, moderate, or severe); and addiction refers to individuals who exhibit persistent difficulties with self-regulation of drug consumption. Among high-risk individuals, a subgroup will meet criteria for SUD and, among those who have an SUD, a further subgroup would be considered to be addicted to the drug. However, the boundary for addiction is intentionally blurred to reflect that the dividing line for defining addiction within the category of SUD remains an open empirical question.
Box 1 What’s in a name? Differentiating hazardous use, substance use disorder, and addiction
Although our principal focus is on the brain disease model of addiction, the definition of addiction itself is a source of ambiguity. Here, we provide a perspective on the major forms of terminology in the field.
Hazardous Substance Use
Hazardous (risky) substance use refers to quantitative levels of consumption that increase an individual’s risk for adverse health consequences. In practice, this pertains to alcohol use [ 110 , 111 ]. Clinically, alcohol consumption that exceeds guidelines for moderate drinking has been used to prompt brief interventions or referral for specialist care [ 112 ]. More recently, a reduction in these quantitative levels has been validated as treatment endpoints [ 113 ].
Substance Use Disorder
SUD refers to the DSM-5 diagnosis category that encompasses significant impairment or distress resulting from specific categories of psychoactive drug use. The diagnosis of SUD is operationalized as 2 or more of 11 symptoms over the past year. As a result, the diagnosis is heterogenous, with more than 1100 symptom permutations possible. The diagnosis in DSM-5 is the result of combining two diagnoses from the DSM-IV, abuse and dependence, which proved to be less valid than a single dimensional approach [ 114 ]. Critically, SUD includes three levels of severity: mild (2–3 symptoms), moderate (4–5 symptoms), and severe (6+ symptoms). The International Classification of Diseases (ICD) system retains two diagnoses, harmful use (lower severity) and substance dependence (higher severity).
Addiction is a natural language concept, etymologically meaning enslavement, with the contemporary meaning traceable to the Middle and Late Roman Republic periods [ 115 ]. As a scientific construct, drug addiction can be defined as a state in which an individual exhibits an inability to self-regulate consumption of a substance, although it does not have an operational definition. Regarding clinical diagnosis, as it is typically used in scientific and clinical parlance, addiction is not synonymous with the simple presence of SUD. Nowhere in DSM-5 is it articulated that the diagnostic threshold (or any specific number/type of symptoms) should be interpreted as reflecting addiction, which inherently connotes a high degree of severity. Indeed, concerns were raised about setting the diagnostic standard too low because of the issue of potentially conflating a low-severity SUD with addiction [ 116 ]. In scientific and clinical usage, addiction typically refers to individuals at a moderate or high severity of SUD. This is consistent with the fact that moderate-to-severe SUD has the closest correspondence with the more severe diagnosis in ICD [ 117 , 118 , 119 ]. Nonetheless, akin to the undefined overlap between hazardous use and SUD, the field has not identified the exact thresholds of SUD symptoms above which addiction would be definitively present.
Integration
The ambiguous relationships among these terms contribute to misunderstandings and disagreements. Figure 1 provides a simple working model of how these terms overlap. Fundamentally, we consider that these terms represent successive dimensions of severity, clinical “nesting dolls”. Not all individuals consuming substances at hazardous levels have an SUD, but a subgroup do. Not all individuals with a SUD are addicted to the drug in question, but a subgroup are. At the severe end of the spectrum, these domains converge (heavy consumption, numerous symptoms, the unambiguous presence of addiction), but at low severity, the overlap is more modest. The exact mapping of addiction onto SUD is an open empirical question, warranting systematic study among scientists, clinicians, and patients with lived experience. No less important will be future research situating our definition of SUD using more objective indicators (e.g., [ 55 , 120 ]), brain-based and otherwise, and more precisely in relation to clinical needs [ 121 ]. Finally, such work should ultimately be codified in both the DSM and ICD systems to demarcate clearly where the attribution of addiction belongs within the clinical nosology, and to foster greater clarity and specificity in scientific discourse.
What is a disease?
In his classic 1960 book “The Disease Concept of Alcoholism”, Jellinek noted that in the alcohol field, the debate over the disease concept was plagued by too many definitions of “alcoholism” and too few definitions of “disease” [ 10 ]. He suggested that the addiction field needed to follow the rest of medicine in moving away from viewing disease as an “entity”, i.e., something that has “its own independent existence, apart from other things” [ 11 ]. To modern medicine, he pointed out, a disease is simply a label that is agreed upon to describe a cluster of substantial, deteriorating changes in the structure or function of the human body, and the accompanying deterioration in biopsychosocial functioning. Thus, he concluded that alcoholism can simply be defined as changes in structure or function of the body due to drinking that cause disability or death. A disease label is useful to identify groups of people with commonly co-occurring constellations of problems—syndromes—that significantly impair function, and that lead to clinically significant distress, harm, or both. This convention allows a systematic study of the condition, and of whether group members benefit from a specific intervention.
It is not trivial to delineate the exact category of harmful substance use for which a label such as addiction is warranted (See Box 1 ). Challenges to diagnostic categorization are not unique to addiction, however. Throughout clinical medicine, diagnostic cut-offs are set by consensus, commonly based on an evolving understanding of thresholds above which people tend to benefit from available interventions. Because assessing benefits in large patient groups over time is difficult, diagnostic thresholds are always subject to debate and adjustments. It can be debated whether diagnostic thresholds “merely” capture the extreme of a single underlying population, or actually identify a subpopulation that is at some level distinct. Resolving this issue remains challenging in addiction, but once again, this is not different from other areas of medicine [see e.g., [ 12 ] for type 2 diabetes]. Longitudinal studies that track patient trajectories over time may have a better ability to identify subpopulations than cross-sectional assessments [ 13 ].
By this pragmatic, clinical understanding of the disease concept, it is difficult to argue that “addiction” is unjustified as a disease label. Among people who use drugs or alcohol, some progress to using with a quantity and frequency that results in impaired function and often death, making substance use a major cause of global disease burden [ 14 ]. In these people, use occurs with a pattern that in milder forms may be challenging to capture by current diagnostic criteria (See Box 1 ), but is readily recognized by patients, their families and treatment providers when it reaches a severity that is clinically significant [see [ 15 ] for a classical discussion]. In some cases, such as opioid addiction, those who receive the diagnosis stand to obtain some of the greatest benefits from medical treatments in all of clinical medicine [ 16 , 17 ]. Although effect sizes of available treatments are more modest in nicotine [ 18 ] and alcohol addiction [ 19 ], the evidence supporting their efficacy is also indisputable. A view of addiction as a disease is justified, because it is beneficial: a failure to diagnose addiction drastically increases the risk of a failure to treat it [ 20 ].
Of course, establishing a diagnosis is not a requirement for interventions to be meaningful. People with hazardous or harmful substance use who have not (yet) developed addiction should also be identified, and interventions should be initiated to address their substance-related risks. This is particularly relevant for alcohol, where even in the absence of addiction, use is frequently associated with risks or harm to self, e.g., through cardiovascular disease, liver disease or cancer, and to others, e.g., through accidents or violence [ 21 ]. Interventions to reduce hazardous or harmful substance use in people who have not developed addiction are in fact particularly appealing. In these individuals, limited interventions are able to achieve robust and meaningful benefits [ 22 ], presumably because patterns of misuse have not yet become entrenched.
Thus, as originally pointed out by McLellan and colleagues, most of the criticisms of addiction as a disease could equally be applied to other medical conditions [ 2 ]. This type of criticism could also be applied to other psychiatric disorders, and that has indeed been the case historically [ 23 , 24 ]. Today, there is broad consensus that those criticisms were misguided. Few, if any healthcare professionals continue to maintain that schizophrenia, rather than being a disease, is a normal response to societal conditions. Why, then, do people continue to question if addiction is a disease, but not whether schizophrenia, major depressive disorder or post-traumatic stress disorder are diseases? This is particularly troubling given the decades of data showing high co-morbidity of addiction with these conditions [ 25 , 26 ]. We argue that it comes down to stigma. Dysregulated substance use continues to be perceived as a self-inflicted condition characterized by a lack of willpower, thus falling outside the scope of medicine and into that of morality [ 3 ].
Chronic and relapsing, developmentally-limited, or spontaneously remitting?
Much of the critique targeted at the conceptualization of addiction as a brain disease focuses on its original assertion that addiction is a chronic and relapsing condition. Epidemiological data are cited in support of the notion that large proportions of individuals achieve remission [ 27 ], frequently without any formal treatment [ 28 , 29 ] and in some cases resuming low risk substance use [ 30 ]. For instance, based on data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) study [ 27 ], it has been pointed out that a significant proportion of people with an addictive disorder quit each year, and that most afflicted individuals ultimately remit. These spontaneous remission rates are argued to invalidate the concept of a chronic, relapsing disease [ 4 ].
Interpreting these and similar data is complicated by several methodological and conceptual issues. First, people may appear to remit spontaneously because they actually do, but also because of limited test–retest reliability of the diagnosis [ 31 ]. For instance, using a validated diagnostic interview and trained interviewers, the Collaborative Studies on Genetics of Alcoholism examined the likelihood that an individual diagnosed with a lifetime history of substance dependence would retain this classification after 5 years. This is obviously a diagnosis that, once met, by definition cannot truly remit. Lifetime alcohol dependence was indeed stable in individuals recruited from addiction treatment units, ~90% for women, and 95% for men. In contrast, in a community-based sample similar to that used in the NESARC [ 27 ], stability was only ~30% and 65% for women and men, respectively. The most important characteristic that determined diagnostic stability was severity. Diagnosis was stable in severe, treatment-seeking cases, but not in general population cases of alcohol dependence.
These data suggest that commonly used diagnostic criteria alone are simply over-inclusive for a reliable, clinically meaningful diagnosis of addiction. They do identify a core group of treatment seeking individuals with a reliable diagnosis, but, if applied to nonclinical populations, also flag as “cases” a considerable halo of individuals for whom the diagnostic categorization is unreliable. Any meaningful discussion of remission rates needs to take this into account, and specify which of these two populations that is being discussed. Unfortunately, the DSM-5 has not made this task easier. With only 2 out of 11 symptoms being sufficient for a diagnosis of SUD, it captures under a single diagnostic label individuals in a “mild” category, whose diagnosis is likely to have very low test–retest reliability, and who are unlikely to exhibit a chronic relapsing course, together with people at the severe end of the spectrum, whose diagnosis is reliable, many of whom do show a chronic relapsing course.
The NESARC data nevertheless show that close to 10% of people in the general population who are diagnosed with alcohol addiction (here equated with DSM-IV “dependence” used in the NESARC study) never remitted throughout their participation in the survey. The base life-time prevalence of alcohol dependence in NESARC was 12.5% [ 32 ]. Thus, the data cited against the concept of addiction as a chronic relapsing disease in fact indicate that over 1% of the US population develops an alcohol-related condition that is associated with high morbidity and mortality, and whose chronic and/or relapsing nature cannot be disputed, since it does not remit.
Secondly, the analysis of NESARC data [ 4 , 27 ] omits opioid addiction, which, together with alcohol and tobacco, is the largest addiction-related public health problem in the US [ 33 ]. This is probably the addictive condition where an analysis of cumulative evidence most strikingly supports the notion of a chronic disorder with frequent relapses in a large proportion of people affected [ 34 ]. Of course, a large number of people with opioid addiction are unable to express the chronic, relapsing course of their disease, because over the long term, their mortality rate is about 15 times greater than that of the general population [ 35 ]. However, even among those who remain alive, the prevalence of stable abstinence from opioid use after 10–30 years of observation is <30%. Remission may not always require abstinence, for instance in the case of alcohol addiction, but is a reasonable proxy for remission with opioids, where return to controlled use is rare. Embedded in these data is a message of literally vital importance: when opioid addiction is diagnosed and treated as a chronic relapsing disease, outcomes are markedly improved, and retention in treatment is associated with a greater likelihood of abstinence.
The fact that significant numbers of individuals exhibit a chronic relapsing course does not negate that even larger numbers of individuals with SUD according to current diagnostic criteria do not. For instance, in many countries, the highest prevalence of substance use problems is found among young adults, aged 18–25 [ 36 ], and a majority of these ‘age out’ of excessive substance use [ 37 ]. It is also well documented that many individuals with SUD achieve longstanding remission, in many cases without any formal treatment (see e.g., [ 27 , 30 , 38 ]).
Collectively, the data show that the course of SUD, as defined by current diagnostic criteria, is highly heterogeneous. Accordingly, we do not maintain that a chronic relapsing course is a defining feature of SUD. When present in a patient, however, such as course is of clinical significance, because it identifies a need for long-term disease management [ 2 ], rather than expectations of a recovery that may not be within the individual’s reach [ 39 ]. From a conceptual standpoint, however, a chronic relapsing course is neither necessary nor implied in a view that addiction is a brain disease. This view also does not mean that it is irreversible and hopeless. Human neuroscience documents restoration of functioning after abstinence [ 40 , 41 ] and reveals predictors of clinical success [ 42 ]. If anything, this evidence suggests a need to increase efforts devoted to neuroscientific research on addiction recovery [ 40 , 43 ].
Lessons from genetics
For alcohol addiction, meta-analysis of twin and adoption studies has estimated heritability at ~50%, while estimates for opioid addiction are even higher [ 44 , 45 ]. Genetic risk factors are to a large extent shared across substances [ 46 ]. It has been argued that a genetic contribution cannot support a disease view of a behavior, because most behavioral traits, including religious and political inclinations, have a genetic contribution [ 4 ]. This statement, while correct in pointing out broad heritability of behavioral traits, misses a fundamental point. Genetic architecture is much like organ structure. The fact that normal anatomy shapes healthy organ function does not negate that an altered structure can contribute to pathophysiology of disease. The structure of the genetic landscape is no different. Critics further state that a “genetic predisposition is not a recipe for compulsion”, but no neuroscientist or geneticist would claim that genetic risk is “a recipe for compulsion”. Genetic risk is probabilistic, not deterministic. However, as we will see below, in the case of addiction, it contributes to large, consistent probability shifts towards maladaptive behavior.
In dismissing the relevance of genetic risk for addiction, Hall writes that “a large number of alleles are involved in the genetic susceptibility to addiction and individually these alleles might very weakly predict a risk of addiction”. He goes on to conclude that “generally, genetic prediction of the risk of disease (even with whole-genome sequencing data) is unlikely to be informative for most people who have a so-called average risk of developing an addiction disorder” [ 7 ]. This reflects a fundamental misunderstanding of polygenic risk. It is true that a large number of risk alleles are involved, and that the explanatory power of currently available polygenic risk scores for addictive disorders lags behind those for e.g., schizophrenia or major depression [ 47 , 48 ]. The only implication of this, however, is that low average effect sizes of risk alleles in addiction necessitate larger study samples to construct polygenic scores that account for a large proportion of the known heritability.
However, a heritability of addiction of ~50% indicates that DNA sequence variation accounts for 50% of the risk for this condition. Once whole genome sequencing is readily available, it is likely that it will be possible to identify most of that DNA variation. For clinical purposes, those polygenic scores will of course not replace an understanding of the intricate web of biological and social factors that promote or prevent expression of addiction in an individual case; rather, they will add to it [ 49 ]. Meanwhile, however, genome-wide association studies in addiction have already provided important information. For instance, they have established that the genetic underpinnings of alcohol addiction only partially overlap with those for alcohol consumption, underscoring the genetic distinction between pathological and nonpathological drinking behaviors [ 50 ].
It thus seems that, rather than negating a rationale for a disease view of addiction, the important implication of the polygenic nature of addiction risk is a very different one. Genome-wide association studies of complex traits have largely confirmed the century old “infinitisemal model” in which Fisher reconciled Mendelian and polygenic traits [ 51 ]. A key implication of this model is that genetic susceptibility for a complex, polygenic trait is continuously distributed in the population. This may seem antithetical to a view of addiction as a distinct disease category, but the contradiction is only apparent, and one that has long been familiar to quantitative genetics. Viewing addiction susceptibility as a polygenic quantitative trait, and addiction as a disease category is entirely in line with Falconer’s theorem, according to which, in a given set of environmental conditions, a certain level of genetic susceptibility will determine a threshold above which disease will arise.
A brain disease? Then show me the brain lesion!
The notion of addiction as a brain disease is commonly criticized with the argument that a specific pathognomonic brain lesion has not been identified. Indeed, brain imaging findings in addiction (perhaps with the exception of extensive neurotoxic gray matter loss in advanced alcohol addiction) are nowhere near the level of specificity and sensitivity required of clinical diagnostic tests. However, this criticism neglects the fact that neuroimaging is not used to diagnose many neurologic and psychiatric disorders, including epilepsy, ALS, migraine, Huntington’s disease, bipolar disorder, or schizophrenia. Even among conditions where signs of disease can be detected using brain imaging, such as Alzheimer’s and Parkinson’s disease, a scan is best used in conjunction with clinical acumen when making the diagnosis. Thus, the requirement that addiction be detectable with a brain scan in order to be classified as a disease does not recognize the role of neuroimaging in the clinic.
For the foreseeable future, the main objective of imaging in addiction research is not to diagnose addiction, but rather to improve our understanding of mechanisms that underlie it. The hope is that mechanistic insights will help bring forward new treatments, by identifying candidate targets for them, by pointing to treatment-responsive biomarkers, or both [ 52 ]. Developing innovative treatments is essential to address unmet treatment needs, in particular in stimulant and cannabis addiction, where no approved medications are currently available. Although the task to develop novel treatments is challenging, promising candidates await evaluation [ 53 ]. A particular opportunity for imaging-based research is related to the complex and heterogeneous nature of addictive disorders. Imaging-based biomarkers hold the promise of allowing this complexity to be deconstructed into specific functional domains, as proposed by the RDoC initiative [ 54 ] and its application to addiction [ 55 , 56 ]. This can ultimately guide the development of personalized medicine strategies to addiction treatment.
Countless imaging studies have reported differences in brain structure and function between people with addictive disorders and those without them. Meta-analyses of structural data show that alcohol addiction is associated with gray matter losses in the prefrontal cortex, dorsal striatum, insula, and posterior cingulate cortex [ 57 ], and similar results have been obtained in stimulant-addicted individuals [ 58 ]. Meta-analysis of functional imaging studies has demonstrated common alterations in dorsal striatal, and frontal circuits engaged in reward and salience processing, habit formation, and executive control, across different substances and task-paradigms [ 59 ]. Molecular imaging studies have shown that large and fast increases in dopamine are associated with the reinforcing effects of drugs of abuse, but that after chronic drug use and during withdrawal, brain dopamine function is markedly decreased and that these decreases are associated with dysfunction of prefrontal regions [ 60 ]. Collectively, these findings have given rise to a widely held view of addiction as a disorder of fronto-striatal circuitry that mediates top-down regulation of behavior [ 61 ].
Critics reply that none of the brain imaging findings are sufficiently specific to distinguish between addiction and its absence, and that they are typically obtained in cross-sectional studies that can at best establish correlative rather than causal links. In this, they are largely right, and an updated version of a conceptualization of addiction as a brain disease needs to acknowledge this. Many of the structural brain findings reported are not specific for addiction, but rather shared across psychiatric disorders [ 62 ]. Also, for now, the most sophisticated tools of human brain imaging remain crude in face of complex neural circuit function. Importantly however, a vast literature from animal studies also documents functional changes in fronto-striatal circuits, as well their limbic and midbrain inputs, associated with addictive behaviors [ 63 , 64 , 65 , 66 , 67 , 68 ]. These are circuits akin to those identified by neuroimaging studies in humans, implicated in positive and negative emotions, learning processes and executive functions, altered function of which is thought to underlie addiction. These animal studies, by virtue of their cellular and molecular level resolution, and their ability to establish causality under experimental control, are therefore an important complement to human neuroimaging work.
Nevertheless, factors that seem remote from the activity of brain circuits, such as policies, substance availability and cost, as well as socioeconomic factors, also are critically important determinants of substance use. In this complex landscape, is the brain really a defensible focal point for research and treatment? The answer is “yes”. As powerfully articulated by Francis Crick [ 69 ], “You, your joys and your sorrows, your memories and your ambitions, your sense of personal identity and free will, are in fact no more than the behavior of a vast assembly of nerve cells and their associated molecules”. Social and interpersonal factors are critically important in addiction, but they can only exert their influences by impacting neural processes. They must be encoded as sensory data, represented together with memories of the past and predictions about the future, and combined with representations of interoceptive and other influences to provide inputs to the valuation machinery of the brain. Collectively, these inputs drive action selection and execution of behavior—say, to drink or not to drink, and then, within an episode, to stop drinking or keep drinking. Stating that the pathophysiology of addiction is largely about the brain does not ignore the role of other influences. It is just the opposite: it is attempting to understand how those important influences contribute to drug seeking and taking in the context of the brain, and vice versa.
But if the criticism is one of emphasis rather than of principle—i.e., too much brain, too little social and environmental factors – then neuroscientists need to acknowledge that they are in part guilty as charged. Brain-centric accounts of addiction have for a long time failed to pay enough attention to the inputs that social factors provide to neural processing behind drug seeking and taking [ 9 ]. This landscape is, however, rapidly changing. For instance, using animal models, scientists are finding that lack of social play early in life increases the motivation to take addictive substances in adulthood [ 70 ]. Others find that the opportunity to interact with a fellow rat is protective against addiction-like behaviors [ 71 ]. In humans, a relationship has been found between perceived social support, socioeconomic status, and the availability of dopamine D2 receptors [ 72 , 73 ], a biological marker of addiction vulnerability. Those findings in turn provided translation of data from nonhuman primates, which showed that D2 receptor availability can be altered by changes in social hierarchy, and that these changes are associated with the motivation to obtain cocaine [ 74 ].
Epidemiologically, it is well established that social determinants of health, including major racial and ethnic disparities, play a significant role in the risk for addiction [ 75 , 76 ]. Contemporary neuroscience is illuminating how those factors penetrate the brain [ 77 ] and, in some cases, reveals pathways of resilience [ 78 ] and how evidence-based prevention can interrupt those adverse consequences [ 79 , 80 ]. In other words, from our perspective, viewing addiction as a brain disease in no way negates the importance of social determinants of health or societal inequalities as critical influences. In fact, as shown by the studies correlating dopamine receptors with social experience, imaging is capable of capturing the impact of the social environment on brain function. This provides a platform for understanding how those influences become embedded in the biology of the brain, which provides a biological roadmap for prevention and intervention.
We therefore argue that a contemporary view of addiction as a brain disease does not deny the influence of social, environmental, developmental, or socioeconomic processes, but rather proposes that the brain is the underlying material substrate upon which those factors impinge and from which the responses originate. Because of this, neurobiology is a critical level of analysis for understanding addiction, although certainly not the only one. It is recognized throughout modern medicine that a host of biological and non-biological factors give rise to disease; understanding the biological pathophysiology is critical for understanding etiology and informing treatment.
Is a view of addiction as a brain disease deterministic?
A common criticism of the notion that addiction is a brain disease is that it is reductionist and in the end therefore deterministic [ 81 , 82 ]. This is a fundamental misrepresentation. As indicated above, viewing addiction as a brain disease simply states that neurobiology is an undeniable component of addiction. A reason for deterministic interpretations may be that modern neuroscience emphasizes an understanding of proximal causality within research designs (e.g., whether an observed link between biological processes is mediated by a specific mechanism). That does not in any way reflect a superordinate assumption that neuroscience will achieve global causality. On the contrary, since we realize that addiction involves interactions between biology, environment and society, ultimate (complete) prediction of behavior based on an understanding of neural processes alone is neither expected, nor a goal.
A fairer representation of a contemporary neuroscience view is that it believes insights from neurobiology allow useful probabilistic models to be developed of the inherently stochastic processes involved in behavior [see [ 83 ] for an elegant recent example]. Changes in brain function and structure in addiction exert a powerful probabilistic influence over a person’s behavior, but one that is highly multifactorial, variable, and thus stochastic. Philosophically, this is best understood as being aligned with indeterminism, a perspective that has a deep history in philosophy and psychology [ 84 ]. In modern neuroscience, it refers to the position that the dynamic complexity of the brain, given the probabilistic threshold-gated nature of its biology (e.g., action potential depolarization, ion channel gating), means that behavior cannot be definitively predicted in any individual instance [ 85 , 86 ].

Driven by compulsion, or free to choose?
A major criticism of the brain disease view of addiction, and one that is related to the issue of determinism vs indeterminism, centers around the term “compulsivity” [ 6 , 87 , 88 , 89 , 90 ] and the different meanings it is given. Prominent addiction theories state that addiction is characterized by a transition from controlled to “compulsive” drug seeking and taking [ 91 , 92 , 93 , 94 , 95 ], but allocate somewhat different meanings to “compulsivity”. By some accounts, compulsive substance use is habitual and insensitive to its outcomes [ 92 , 94 , 96 ]. Others refer to compulsive use as a result of increasing incentive value of drug associated cues [ 97 ], while others view it as driven by a recruitment of systems that encode negative affective states [ 95 , 98 ].
The prototype for compulsive behavior is provided by obsessive-compulsive disorder (OCD), where compulsion refers to repeatedly and stereotypically carrying out actions that in themselves may be meaningful, but lose their purpose and become harmful when performed in excess, such as persistent handwashing until skin injuries result. Crucially, this happens despite a conscious desire to do otherwise. Attempts to resist these compulsions result in increasing and ultimately intractable anxiety [ 99 ]. This is in important ways different from the meaning of compulsivity as commonly used in addiction theories. In the addiction field, compulsive drug use typically refers to inflexible, drug-centered behavior in which substance use is insensitive to adverse consequences [ 100 ]. Although this phenomenon is not necessarily present in every patient, it reflects important symptoms of clinical addiction, and is captured by several DSM-5 criteria for SUD [ 101 ]. Examples are needle-sharing despite knowledge of a risk to contract HIV or Hepatitis C, drinking despite a knowledge of having liver cirrhosis, but also the neglect of social and professional activities that previously were more important than substance use. While these behaviors do show similarities with the compulsions of OCD, there are also important differences. For example, “compulsive” substance use is not necessarily accompanied by a conscious desire to withhold the behavior, nor is addictive behavior consistently impervious to change.
Critics question the existence of compulsivity in addiction altogether [ 5 , 6 , 7 , 89 ], typically using a literal interpretation, i.e., that a person who uses alcohol or drugs simply can not do otherwise. Were that the intended meaning in theories of addiction—which it is not—it would clearly be invalidated by observations of preserved sensitivity of behavior to contingencies in addiction. Indeed, substance use is influenced both by the availability of alternative reinforcers, and the state of the organism. The roots of this insight date back to 1940, when Spragg found that chimpanzees would normally choose a banana over morphine. However, when physically dependent and in a state of withdrawal, their choice preference would reverse [ 102 ]. The critical role of alternative reinforcers was elegantly brought into modern neuroscience by Ahmed et al., who showed that rats extensively trained to self-administer cocaine would readily forego the drug if offered a sweet solution as an alternative [ 103 ]. This was later also found to be the case for heroin [ 103 ], methamphetamine [ 104 ] and alcohol [ 105 ]. Early residential laboratory studies on alcohol use disorder indeed revealed orderly operant control over alcohol consumption [ 106 ]. Furthermore, efficacy of treatment approaches such as contingency management, which provides systematic incentives for abstinence [ 107 ], supports the notion that behavioral choices in patients with addictions remain sensitive to reward contingencies.
Evidence that a capacity for choosing advantageously is preserved in addiction provides a valid argument against a narrow concept of “compulsivity” as rigid, immutable behavior that applies to all patients. It does not, however, provide an argument against addiction as a brain disease. If not from the brain, from where do the healthy and unhealthy choices people make originate? The critical question is whether addictive behaviors—for the most part—result from healthy brains responding normally to externally determined contingencies; or rather from a pathology of brain circuits that, through probabilistic shifts, promotes the likelihood of maladaptive choices even when reward contingencies are within a normal range. To resolve this question, it is critical to understand that the ability to choose advantageously is not an all-or-nothing phenomenon, but rather is about probabilities and their shifts, multiple faculties within human cognition, and their interaction. Yes, it is clear that most people whom we would consider to suffer from addiction remain able to choose advantageously much, if not most, of the time. However, it is also clear that the probability of them choosing to their own disadvantage, even when more salutary options are available and sometimes at the expense of losing their life, is systematically and quantifiably increased. There is a freedom of choice, yet there is a shift of prevailing choices that nevertheless can kill.
Synthesized, the notion of addiction as a disease of choice and addiction as a brain disease can be understood as two sides of the same coin. Both of these perspectives are informative, and they are complementary. Viewed this way, addiction is a brain disease in which a person’s choice faculties become profoundly compromised. To articulate it more specifically, embedded in and principally executed by the central nervous system, addiction can be understood as a disorder of choice preferences, preferences that overvalue immediate reinforcement (both positive and negative), preferences for drug-reinforcement in spite of costs, and preferences that are unstable ( “I’ll never drink like that again;” “this will be my last cigarette” ), prone to reversals in the form of lapses and relapse. From a contemporary neuroscience perspective, pre-existing vulnerabilities and persistent drug use lead to a vicious circle of substantive disruptions in the brain that impair and undermine choice capacities for adaptive behavior, but do not annihilate them. Evidence of generally intact decision making does not fundamentally contradict addiction as a brain disease.
Conclusions
The present paper is a response to the increasing number of criticisms of the view that addiction is a chronic relapsing brain disease. In many cases, we show that those criticisms target tenets that are neither needed nor held by a contemporary version of this view. Common themes are that viewing addiction as a brain disease is criticized for being both too narrow (addiction is only a brain disease; no other perspectives or factors are important) or too far reaching (it purports to discover the final causes of addiction). With regard to disease course, we propose that viewing addiction as a chronic relapsing disease is appropriate for some populations, and much less so for others, simply necessitating better ways of delineating the populations being discussed. We argue that when considering addiction as a disease, the lens of neurobiology is valuable to use. It is not the only lens, and it does not have supremacy over other scientific approaches. We agree that critiques of neuroscience are warranted [ 108 ] and that critical thinking is essential to avoid deterministic language and scientific overreach.
Beyond making the case for a view of addiction as a brain disease, perhaps the more important question is when a specific level of analysis is most useful. For understanding the biology of addiction and designing biological interventions, a neurobiological view is almost certainly the most appropriate level of analysis, in particular when informed by an understanding of the behavioral manifestations. In contrast, for understanding the psychology of addiction and designing psychological interventions, behavioral science is the natural realm, but one that can often benefit from an understanding of the underlying neurobiology. For designing policies, such as taxation and regulation of access, economics and public administration provide the most pertinent perspectives, but these also benefit from biological and behavioral science insights.
Finally, we argue that progress would come from integration of these scientific perspectives and traditions. E.O. Wilson has argued more broadly for greater consilience [ 109 ], unity of knowledge, in science. We believe that addiction is among the areas where consilience is most needed. A plurality of disciplines brings important and trenchant insights to bear on this condition; it is the exclusive remit of no single perspective or field. Addiction inherently and necessarily requires multidisciplinary examination. Moreover, those who suffer from addiction will benefit most from the application of the full armamentarium of scientific perspectives.
Funding and disclosures
Supported by the Swedish Research Council grants 2013-07434, 2019-01138 (MH); Netherlands Organisation for Health Research and Development (ZonMw) under project number 912.14.093 (LJMJV); NIDA and NIAAA intramural research programs (LL; the content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health); the Peter Boris Chair in Addictions Research, Homewood Research Institute, and the National Institute on Alcohol Abuse and Alcoholism grants AA025911, AA024930, AA025849, AA027679 (JM; the content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health).
MH has received consulting fees, research support or other compensation from Indivior, Camurus, BrainsWay, Aelis Farma, and Janssen Pharmaceuticals. JM is a Principal and Senior Scientist at BEAM Diagnostics, Inc. DM, JR, LL, and LJMJV declare no conflict of interest.
Leshner AI. Addiction is a brain disease, and it matters. Science. 1997;278:45–7.
Article CAS PubMed Google Scholar
McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–95.
Schomerus G, Lucht M, Holzinger A, Matschinger H, Carta MG, Angermeyer MC. The stigma of alcohol dependence compared with other mental disorders: a review of population studies. Alcohol Alcohol. 2011;46:105–12.
Heyman GM. Addiction and choice: theory and new data. Front Psychiatry. 2013;4:31.
Article PubMed PubMed Central Google Scholar
Heather N, Best D, Kawalek A, Field M, Lewis M, Rotgers F, et al. Challenging the brain disease model of addiction: European launch of the addiction theory network. Addict Res Theory. 2018;26:249–55.
Article Google Scholar
Pickard H, Ahmed SH, Foddy B. Alternative models of addiction. Front Psychiatr.y 2015;6:20.
Google Scholar
Hall W, Carter A, Forlini C. The brain disease model of addiction: is it supported by the evidence and has it delivered on its promises? Lancet Psychiatr. 2015;2:105–10.
Hart CL. Viewing addiction as a brain disease promotes social injustice. Nat Hum Behav. 2017;1:0055.
Heilig M, Epstein DH, Nader MA, Shaham Y. Time to connect: bringing social context into addiction neuroscience. Nat Rev Neurosc.i 2016;17:592–9.
Article CAS Google Scholar
Jellinek EM. The disease concept of alcoholism. Hillhouse Press on behalf of the Christopher J. Smithers Foundation: New Haven, CT; 1960.
Stevenson A. Oxford dictionary of English. 3 ed. New York, NY: Oxford University Press; 2010.
Fan J, May SJ, Zhou Y, Barrett-Connor E. Bimodality of 2-h plasma glucose distributions in whites: the Rancho Bernardo study. Diabetes Care 2005;28:1451–6.
King AC, Vena A, Hasin D, De Wit D, O’Connor CJ, Cao D. Subjective responses to alcohol in the development and maintenance of alcohol use disorder (AUD). Am J Psychiatry. 2021. https://doi.org/10.1176/appi.ajp.2020.20030247 .
GBD. 2016 Alcohol and Drug Use Collaborators. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry. 2018;5:987–1012.
Edwards G, Gross MM. Alcohol dependence: provisional description of a clinical syndrome. Br Med J. 1976;1:1058–61.
Article CAS PubMed PubMed Central Google Scholar
Epstein DH, Heilig M, Shaham Y. Science-based actions can help address the opioid crisis. Trends Pharm Sci. 2018;39:911–16.
Amato L, Davoli M, Perucci CA, Ferri M, Faggiano F, Mattick RP. An overview of systematic reviews of the effectiveness of opiate maintenance therapies: available evidence to inform clinical practice and research. J Subst Abus Treat. 2005;28:321–9.
Cahill K, Stevens S, Perera R, Lancaster T. Pharmacological interventions for smoking cessation: an overview and network meta-analysis. Cochrane Datab System Rev. 2013;5:CD009329.
Jonas DE, Amick HR, Feltner C, Bobashev G, Thomas K, Wines R, et al. Pharmacotherapy for adults with alcohol use disorders in outpatient settings a systematic review and meta-analysis. JAMA. 2014;311:1889–900.
Article PubMed CAS Google Scholar
Mark TL, Kranzler HR, Song X. Understanding US addiction physicians’ low rate of naltrexone prescription. Drug Alcohol Depend. 2003;71:219–28.
Article PubMed Google Scholar
Nutt DJ, King LA, Phillips LD. Drug harms in the UK: a multicriteria decision analysis. Lancet. 2010;376:1558–65.
Wilk AI, Jensen NM, Havighurst TC. Meta-analysis of randomized control trials addressing brief interventions in heavy alcohol drinkers. J Gen Intern Med. 1997;12:274–83.
Laing RD. The divided self; a study of sanity and madness. London: Tavistock Publications; 1960.
Foucault M, Khalfa J. History of madness. New York: Routledge; 2006.
Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL. et al.Comorbidity of mental disorders with alcohol and other drug abuse. Results Epidemiologic Catchment Area (ECA) study.JAMA. 1990;264:2511–8.
Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–16.
Lopez-Quintero C, Hasin DS, de Los Cobos JP, Pines A, Wang S, Grant BF, et al. Probability and predictors of remission from life-time nicotine, alcohol, cannabis or cocaine dependence: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Addiction. 2011;106:657–69.
Humphreys K. Addiction treatment professionals are not the gatekeepers of recovery. Subst Use Misuse. 2015;50:1024–7.
Cohen E, Feinn R, Arias A, Kranzler HR. Alcohol treatment utilization: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2007;86:214–21.
Sobell LC, Cunningham JA, Sobell MB. Recovery from alcohol problems with and without treatment: prevalence in two population surveys. Am J Public Health. 1996;86:966–72.
Culverhouse R, Bucholz KK, Crowe RR, Hesselbrock V, Nurnberger JI Jr, Porjesz B, et al. Long-term stability of alcohol and other substance dependence diagnoses and habitual smoking: an evaluation after 5 years. Arch Gen Psychiatry. 2005;62:753–60.
Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830–42.
Skolnick P. The opioid epidemic: crisis and solutions. Annu Rev Pharm Toxicol. 2018;58:143–59.
Hser YI, Evans E, Grella C, Ling W, Anglin D. Long-term course of opioid addiction. Harv Rev Psychiatry. 2015;23:76–89.
Mathers BM, Degenhardt L, Bucello C, Lemon J, Wiessing L, Hickman M. Mortality among people who inject drugs: a systematic review and meta-analysis. Bull World Health Organ. 2013;91:102–23.
Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, et al. Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72:757–66.
Article PubMed PubMed Central CAS Google Scholar
Lee MR, Sher KJ. “Maturing Out” of binge and problem drinking. Alcohol Res: Curr Rev. 2018;39:31–42.
Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ. Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction. 2005;100:281–92.
Berridge V. The rise, fall, and revival of recovery in drug policy. Lancet. 2012;379:22–23.
Parvaz MA, Moeller SJ, d’Oleire Uquillas F, Pflumm A, Maloney T, Alia-Klein N, et al. Prefrontal gray matter volume recovery in treatment-seeking cocaine-addicted individuals: a longitudinal study. Addict Biol. 2017;22:1391–401.
Korponay C, Kosson DS, Decety J, Kiehl KA, Koenigs M. Brain volume correlates with duration of abstinence from substance abuse in a region-specific and substance-specific manner. Biol Psychiatry Cogn Neurosci Neuroimaging. 2017;2:626–35.
PubMed PubMed Central Google Scholar
Janes AC, Datko M, Roy A, Barton B, Druker S, Neal C, et al. Quitting starts in the brain: a randomized controlled trial of app-based mindfulness shows decreases in neural responses to smoking cues that predict reductions in smoking. Neuropsychopharmacology. 2019;44:1631–38.
Humphreys K, Bickel WK. Toward a neuroscience of long-term recovery from addiction. JAMA Psychiatry. 2018;75:875–76.
Verhulst B, Neale MC, Kendler KS. The heritability of alcohol use disorders: a meta-analysis of twin and adoption studies. Psychol Med. 2015;45:1061–72.
Goldman D, Oroszi G, Ducci F. The genetics of addictions: uncovering the genes. Nat Rev Genet. 2005;6:521–32.
Kendler KS, Jacobson KC, Prescott CA, Neale MC. Specificity of genetic and environmental risk factors for use and abuse/dependence of cannabis, cocaine, hallucinogens, sedatives, stimulants, and opiates in male twins. AJ Psychiatry. 2003;160:687–95.
Schizophrenia Working Group of the Psychiatric Genomics C. Biological insights from 108 schizophrenia-associated genetic loci. Nature. 2014;511:421–7.
Wray NR, Ripke S, Mattheisen M, Trzaskowski M, Byrne EM, Abdellaoui A, et al. Genome-wide association analyses identify 44 risk variants and refine the genetic architecture of major depression. Nat Genet. 2018;50:668–81.
Wray NR, Lin T, Austin J, McGrath JJ, Hickie IB, Murray GK, et al. From basic science to clinical application of polygenic risk scores: a primer. JAMA Psychiatry. 2021;78:101–9.
Walters RK, Polimanti R, Johnson EC, McClintick JN, Adams MJ, Adkins AE, et al. Transancestral GWAS of alcohol dependence reveals common genetic underpinnings with psychiatric disorders. Nat Neurosci. 2018;21:1656–69.
Visscher PM, Wray NR. Concepts and misconceptions about the polygenic additive model applied to disease. Hum Hered. 2015;80:165–70.
Heilig M, Leggio L. What the alcohol doctor ordered from the neuroscientist: theragnostic biomarkers for personalized treatments. Prog Brain Res. 2016;224:401–18.
Rasmussen K, White DA, Acri JB. NIDA’s medication development priorities in response to the Opioid Crisis: ten most wanted. Neuropsychopharmacology. 2019;44:657–59.
Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. AJ Psychiatry. 2010;167:748–51.
Kwako LE, Schwandt ML, Ramchandani VA, Diazgranados N, Koob GF, Volkow ND, et al. Neurofunctional domains derived from deep behavioral phenotyping in alcohol use disorder. AJ Psychiatry. 2019;176:744–53.
Kwako LE, Bickel WK, Goldman D. Addiction biomarkers: dimensional approaches to understanding addiction. Trends Mol Med. 2018;24:121–28.
Xiao P, Dai Z, Zhong J, Zhu Y, Shi H, Pan P. Regional gray matter deficits in alcohol dependence: a meta-analysis of voxel-based morphometry studies. Drug Alcohol Depend. 2015;153:22–8.
Ersche KD, Williams GB, Robbins TW, Bullmore ET. Meta-analysis of structural brain abnormalities associated with stimulant drug dependence and neuroimaging of addiction vulnerability and resilience. Curr Opin Neurobiol. 2013;23:615–24.
Klugah-Brown B, Di X, Zweerings J, Mathiak K, Becker B, Biswal B. Common and separable neural alterations in substance use disorders: a coordinate-based meta-analyses of functional neuroimaging studies in humans. Hum Brain Mapp. 2020;41:4459–77.
Volkow ND, Fowler JS, Wang GJ. The addicted human brain: insights from imaging studies. J Clin Investig. 2003;111:1444–51.
Goldstein RZ, Volkow ND. Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications. Nat Rev Neurosci. 2011;12:652–69.
Goodkind M, Eickhoff SB, Oathes DJ, Jiang Y, Chang A, Jones-Hagata LB, et al. Identification of a common neurobiological substrate for mental illness. JAMA Psychiatry. 2015;72:305–15.
Scofield MD, Heinsbroek JA, Gipson CD, Kupchik YM, Spencer S, Smith AC, et al. The nucleus accumbens: mechanisms of addiction across drug classes reflect the importance of glutamate homeostasis. Pharm Rev. 2016;68:816–71.
Korpi ER, den Hollander B, Farooq U, Vashchinkina E, Rajkumar R, Nutt DJ, et al. Mechanisms of action and persistent neuroplasticity by drugs of abuse. Pharm Rev. 2015;67:872–1004.
Luscher C, Malenka RC. Drug-evoked synaptic plasticity in addiction: from molecular changes to circuit remodeling. Neuron. 2011;69:650–63.
Everitt BJ. Neural and psychological mechanisms underlying compulsive drug seeking habits and drug memories–indications for novel treatments of addiction. Eur J Neurosci. 2014;40:2163–82.
Lesscher HM, Vanderschuren LJ. Compulsive drug use and its neural substrates. Rev Neurosci. 2012;23:731–45.
Cruz FC, Koya E, Guez-Barber DH, Bossert JM, Lupica CR, Shaham Y, et al. New technologies for examining the role of neuronal ensembles in drug addiction and fear. Nat Rev Neurosci. 2013;14:743–54.
Crick F. The astonishing hypothesis: the scientific search for the soul. Scribner; Maxwell Macmillan International: New York, NY; 1994.
Vanderschuren LJ, Achterberg EJ, Trezza V. The neurobiology of social play and its rewarding value in rats. Neurosci Biobehav Rev. 2016;70:86–105.
Venniro M, Zhang M, Caprioli D, Hoots JK, Golden SA, Heins C, et al. Volitional social interaction prevents drug addiction in rat models. Nat Neurosci. 2018;21:1520–29.
Martinez D, Orlowska D, Narendran R, Slifstein M, Liu F, Kumar D, et al. Dopamine type 2/3 receptor availability in the striatum and social status in human volunteers. Biol Psychiatry. 2010;67:275–8.
Wiers CE, Shokri-Kojori E, Cabrera E, Cunningham S, Wong C, Tomasi D, et al. Socioeconomic status is associated with striatal dopamine D2/D3 receptors in healthy volunteers but not in cocaine abusers. Neurosci Lett. 2016;617:27–31.
Morgan D, Grant KA, Gage HD, Mach RH, Kaplan JR, Prioleau O, et al. Social dominance in monkeys: dopamine D2 receptors and cocaine self-administration. Nat Neurosci. 2002;5:169–74.
Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017;2:e356–e66.
Gilbert PA, Zemore SE. Discrimination and drinking: a systematic review of the evidence. Soc Sci Med 2016;161:178–94.
Oshri A, Gray JC, Owens MM, Liu S, Duprey EB, Sweet LH, et al. Adverse childhood experiences and amygdalar reduction: high-resolution segmentation reveals associations with subnuclei and psychiatric outcomes. Child Maltreat. 2019;24:400–10.
Holmes CJ, Barton AW, MacKillop J, Galván A, Owens MM, McCormick MJ, et al. Parenting and salience network connectivity among African Americans: a protective pathway for health-risk behaviors. Biol Psychiatry. 2018;84:365–71.
Brody GH, Gray JC, Yu T, Barton AW, Beach SR, Galván A, et al. Protective prevention effects on the association of poverty with brain development. JAMA Pediatr. 2017;171:46–52.
Hanson JL, Gillmore AD, Yu T, Holmes CJ, Hallowell ES, Barton AW, et al. A family focused intervention influences hippocampal-prefrontal connectivity through gains in self-regulation. Child Dev. 2019;90:1389–401.
Borsboom D, Cramer A, Kalis A. Brain disorders? Not really… why network structures block reductionism in psychopathology research. Behav Brain Sci. 2018;42:1–54.
Field M, Heather N, Wiers RW. Indeed, not really a brain disorder: Implications for reductionist accounts of addiction. Behav Brain Sci. 2019;42:e9.
Pascoli V, Hiver A, Van Zessen R, Loureiro M, Achargui R, Harada M, et al. Stochastic synaptic plasticity underlying compulsion in a model of addiction. Nature. 2018;564:366–71.
James W. The dilemma of determinism. Whitefish, MT: Kessinger Publishing; 2005.
Gessell B. Indeterminism in the brain. Biol Philos. 2017;32:1205–23.
Jedlicka P. Revisiting the quantum brain hypothesis: toward quantum (neuro)biology? Front Mol Neurosci. 2017;10:366.
Heyman GM. Addiction: a disorder of choice. Cambridge, MA: Harvard University Press; 2010.
Heather NQ. Is addiction a brain disease or a moral failing? A: Neither. Neuroethics. 2017;10:115–24.
Ahmed SH, Lenoir M, Guillem K. Neurobiology of addiction versus drug use driven by lack of choice. Curr Opin Neurobiol. 2013;23:581–7.
Hogarth L, Lam-Cassettari C, Pacitti H, Currah T, Mahlberg J, Hartley L, et al. Intact goal-directed control in treatment-seeking drug users indexed by outcome-devaluation and Pavlovian to instrumental transfer: critique of habit theory. Eur J Neurosci. 2019;50:2513–25.
Mathis V, Kenny PJ. From controlled to compulsive drug-taking: the role of the habenula in addiction. Neurosci Biobehav Rev. 2019;106:102–11.
Luscher C, Robbins TW, Everitt BJ. The transition to compulsion in addiction. Nat Rev Neurosci. 2020;21:247–63.
Robinson TE, Berridge KC. Addiction. Annu Rev Psychol. 2003;54:25–53.
Everitt BJ, Robbins TW. Neural systems of reinforcement for drug addiction: from actions to habits to compulsion. Nat Neurosci. 2005;8:1481–89.
Koob GF, Volkow ND. Neurocircuitry of addiction. Neuropsychopharmacology. 2010;35:217–38.
Tiffany ST. A cognitive model of drug urges and drug-use behavior: role of automatic and nonautomatic processes. Psychol Rev. 1990;97:147–68.
Robinson TE, Berridge KC. The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Res Rev. 1993;18:247–91.
Koob GF, Le Moal M. Plasticity of reward neurocircuitry and the ‘dark side’ of drug addiction. Nat Neurosci. 2005;8:1442–4.
Stein DJ, Costa DLC, Lochner C, Miguel EC, Reddy YCJ, Shavitt RG, et al. Obsessive-compulsive disorder. Nat Rev Dis Prim. 2019;5:52.
Vanderschuren LJ, Everitt BJ. Drug seeking becomes compulsive after prolonged cocaine self-administration. Science 2004;305:1017–9.
American_Psychiatric_Association. Diagnostic and statistical manual of mental disorders: DSM-5™. 5th ed. Arlington, VA, US: American Psychiatric Publishing, Inc; 2013.
Book Google Scholar
Spragg SDS. Morphine addiction in chimpanzees. Comp Psychol Monogr. 1940;15:132–32.
Lenoir M, Cantin L, Vanhille N, Serre F, Ahmed SH. Extended heroin access increases heroin choices over a potent nondrug alternative. Neuropsychopharmacology. 2013;38:1209–20.
Caprioli D, Venniro M, Zeric T, Li X, Adhikary S, Madangopal R, et al. Effect of the novel positive allosteric modulator of metabotropic glutamate receptor 2 AZD8529 on incubation of methamphetamine craving after prolonged voluntary abstinence in a rat model. Biol Psychiatry. 2015;78:463–73.
Augier E, Barbier E, Dulman RS, Licheri V, Augier G, Domi E, et al. A molecular mechanism for choosing alcohol over an alternative reward. Science. 2018;360:1321–26.
Bigelow GE. An operant behavioral perspective on alcohol abuse and dependence. In: Heather N, Peters TJ, Stockwell T, editors. International handbook of alcohol dependence and problems. John Wiley & Sons Ltd; 2001. p. 299–315.
Higgins ST, Heil SH, Lussier JP. Clinical implications of reinforcement as a determinant of substance use disorders. Annu Rev Psychol. 2004;55:431–61.
Satel S, Lilienfeld SO. Brainwashed: the seductive appeal of mindless neuroscience. New York, NY: Basic Books; 2015.
Wilson EO. Consilience: the unity of knowledge. New York, NY: Vintage Books; 1999.
Saunders JB, Degenhardt L, Reed GM, Poznyak V. Alcohol use disorders in ICD-11: past, present, and future. Alcohol Clin Exp Res 2019;43:1617–31.
Organization. WH. ICD-11 for mortality and morbidity statistics. 2018. https://icd.who.int/browse11/l-m/en . Accessed 21 Oct 2020.
Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, brief intervention, and referral to treatment (SBIRT): toward a public health approach to the management of substance abuse. Subst Abus. 2007;28:7–30.
Witkiewitz K, Hallgren KA, Kranzler HR, Mann KF, Hasin DS, Falk DE, et al. Clinical validation of reduced alcohol consumption after treatment for alcohol dependence using the World Health Organization risk drinking levels. Alcohol Clin Exp Res 2017;41:179–86.
Hasin DS, O’Brien CP, Auriacombe M, Borges G, Bucholz K, Budney A, et al. DSM-5 criteria for substance use disorders: recommendations and rationale. AJ Psychiatry. 2013;170:834–51.
Rosenthal RJ, Faris SB. The etymology and early history of ‘addiction’. Addict Res Theory. 2019;27:437–49.
Martin CS, Steinley DL, Verges A, Sher KJ. The proposed 2/11 symptom algorithm for DSM-5 substance-use disorders is too lenient. Psychol Med. 2011;41:2008–10.
Degenhardt L, Bharat C, Bruno R, Glantz MD, Sampson NA, Lago L, et al. Concordance between the diagnostic guidelines for alcohol and cannabis use disorders in the draft ICD-11 and other classification systems: analysis of data from the WHO’s World Mental Health Surveys. Addiction. 2019;114:534–52.
PubMed Google Scholar
Lago L, Bruno R, Degenhardt L. Concordance of ICD-11 and DSM-5 definitions of alcohol and cannabis use disorders: a population survey. Lancet Psychiatry. 2016;3:673–84.
Lundin A, Hallgren M, Forsman M, Forsell Y. Comparison of DSM-5 classifications of alcohol use disorders with those of DSM-IV, DSM-III-R, and ICD-10 in a general population sample in Sweden. J Stud Alcohol Drugs. 2015;76:773–80.
Kwako LE, Momenan R, Litten RZ, Koob GF, Goldman D. Addictions neuroclinical assessment: a neuroscience-based framework for addictive disorders. Biol Psychiatry. 2016;80:179–89.
Rehm J, Heilig M, Gual A. ICD-11 for alcohol use disorders: not a convincing answer to the challenges. Alcohol Clin Exp Res. 2019;43:2296–300.
Download references
Acknowledgements
The authors want to acknowledge comments by Drs. David Epstein, Kenneth Kendler and Naomi Wray.
Author information
Authors and affiliations.
Center for Social and Affective Neuroscience, Department of Biomedical and Clinical Sciences, Linköping University, Linköping, Sweden
Markus Heilig
Peter Boris Centre for Addictions Research, McMaster University and St. Joseph’s Healthcare Hamilton, Hamilton, ON, Canada
- James MacKillop
Homewood Research Institute, Guelph, ON, Canada
New York State Psychiatric Institute and Columbia University Irving Medical Center, New York, NY, USA
Diana Martinez
Institute for Mental Health Policy Research & Campbell Family Mental Health Research Institute, Centre for Addiction and Mental Health (CAMH), Toronto, ON, Canada
Jürgen Rehm
Dalla Lana School of Public Health and Department of Psychiatry, University of Toronto (UofT), Toronto, ON, Canada
Klinische Psychologie & Psychotherapie, Technische Universität Dresden, Dresden, Germany
Department of International Health Projects, Institute for Leadership and Health Management, I.M. Sechenov First Moscow State Medical University, Moscow, Russia
Clinical Psychoneuroendocrinology and Neuropsychopharmacology Section, Translational Addiction Medicine Branch, National Institute on Drug Abuse Intramural Research Program and National Institute on Alcohol Abuse and Alcoholism Division of Intramural Clinical and Biological Research, National Institutes of Health, Baltimore and Bethesda, MD, USA
Lorenzo Leggio
Department of Population Health Sciences, Unit Animals in Science and Society, Faculty of Veterinary Medicine, Utrecht University, Utrecht, the Netherlands
Louk J. M. J. Vanderschuren
You can also search for this author in PubMed Google Scholar
Contributions
All authors jointly drafted the paper.
Corresponding author
Correspondence to Markus Heilig .
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Heilig, M., MacKillop, J., Martinez, D. et al. Addiction as a brain disease revised: why it still matters, and the need for consilience. Neuropsychopharmacol. 46 , 1715–1723 (2021). https://doi.org/10.1038/s41386-020-00950-y
Download citation
Received : 10 November 2020
Revised : 11 December 2020
Accepted : 14 December 2020
Published : 22 February 2021
Issue Date : September 2021
DOI : https://doi.org/10.1038/s41386-020-00950-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
The importance of choice and agency in animal models of addiction.
- Serge H. Ahmed
Journal of Neural Transmission (2024)
Neuromarkers in addiction: definitions, development strategies, and recent advances
- Nicholas R. Harp
- Tor D. Wager
What Do We Know About Informal Caregiving in the Field of Addiction?: A Scoping Review
- Mélissa Côté
- Eve-Emmanuelle Morency
- Nadine Blanchette-Martin
International Journal of Mental Health and Addiction (2024)
Persistent impacts of smoking on resting-state EEG in male chronic smokers and past-smokers with 20 years of abstinence
- Yoonji Jeon
- Dongil Chung
Scientific Reports (2023)
A contextualized reinforcer pathology approach to addiction
- Samuel F. Acuff
- James G. Murphy
Nature Reviews Psychology (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Addict Health
- v.14(4); 2022 Oct
- PMC10408746
A Review of the Prevention of Drug Addiction: Specific Interventions, Effectiveness, and Important Topics
Background:.
This study was a narrative review on prevention of addictive behaviors with an effort to clarify the major concepts of prevention and its dimensions.
The PsycInfo and MedInfo databases were used to identify prevention. Α total of 65 articles were found 46 of which were included in the review. Τhe data were analyzed using content analysis.
For a better understanding of the results, it was deemed advisable to categorize them into: (a) the types of major interventions and the theoretical approaches on which they were based, (b) the results of the review articles according to (1) variables and factors concerning the prevention proved important through the review and (2) a number of more general important topics which arose in the prevention of addictive behaviors.
Conclusion:
The results highlighted the greater effectiveness of community-based programs, applied primarily in broader contexts but also secondarily in high-risk groups. Τhe results were discussed based on the combination of the emerged factors with each other and prevention experience.
Introduction
One of the most important questions in the field of psychotropic substances addiction, including alcohol abuse, is which ways, methods, techniques, or interventions are effective in substance use prevention. Given the fact that there are various kinds of prevention strategies, this question becomes even more complicated as it is hard to find and systematize these factors. It is essential to continue research in this direction since the question why young people resort to substances and get addicted to them has not been fully answered yet. Furthermore, it is generally accepted that prevention is better than treatment.
Psychotropic substances addiction refers to the substance-related disorders as described by Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V). Although the psychological mechanism of addictive substance use is considered to be common with or at least similar to that of addiction to illegal substances and alcohol, in this study, the surveys that focus exclusively on alcohol were not included. The reason for this decision was that articles on alcohol prevention are numerous and could be investigated –as already done- in a separate study. Besides, alcohol use displays certain peculiarities; for example, it is a legal and easily accessible substance.
Traditionally, prevention strategies have been categorised into primary, secondary, and tertiary preventions. Primary prevention refers to the prevention of substance use and abuse. Secondary prevention refers to the early identification and treatment of individuals already using substances, while tertiary prevention refers to the treatment and reduction of harm in people who have already used substances and have consequences from their use. We can literally talk about prevention only in primary and partially in secondary types. Tertiary prevention is essentially not prevention but treatment and reduction of harm.
Another distinction that has been made in recent decades (e.g., National Advisory Mental Health Council Workgroup on Mental Disorders Prevention Research 1 ) classifies prevention strategies into universal, selective, and indicated preventions. The universal strategies apply to the general population (e.g., students) in order to inform and raise awareness about the issue of drugs. 2 Selective strategies target individuals at increased risk of substance use and abuse (e.g., children of addicts, children growing up in high-risk environments or neighborhoods). Indicated strategies are for people who may not already be addicted to drugs but have had a contact with them (e.g., young people experimenting with substances).
Preventive interventions in the three categories described above may have different goals, including the following: (a) increasing the knowledge about drugs in adolescents; (b) reducing the use of drugs; (c) delaying the onset of first use; (d) reducing abuse of drugs; and (e) minimising the harm caused by the use of drugs. 3 Additionally, regarding the context of implementation of prevention interventions, it is evident that these interventions can aim at different settings such as schools, families, the wider community, the media, 4 or even in places of gathering of young people e.g., cultural centres, parks, cafes, and so on.
The field of prevention is in general very broad as it includes prevention policies, designs, methods, techniques, and interventions. The design of interventions requires the appropriate theoretical background and the deployment of previous knowledge and results. Furthermore, it potentially includes various intervention implementation frameworks, a different extent of involvement, and participation of the individuals e.g., children, parents, and teachers.
There are a lot of important dimensions to be investigated in what is broadly defined as prevention. The effectiveness of the interventions is an important parameter. Effectiveness is usually defined as a reduction in substance use or a reduction in the positive attitude towards substances, after the implementation of a prevention program. The sustainment, however, of positive results on a long-term basis is an even more important dimension. The active participation of the involved members and the retention of the therapeutic results are other necessary components for the implementation of effective interventions.
As far as the evaluation of interventions is concerned, reliability should be tested as youth substance use programs are often of limited generalizability due to methodological restrictions and the absence of consistency in evaluation of interventions. 5
Furthermore, it should be mentioned that the concepts usually studied (e.g., self-efficacy, motivation for change, coping skills) are complex and hard to be assessed in self-report measures. In addition, these psychological processes may not be part of conscious awareness and thus may not be possible to be evaluated using self-report measures. Additionally, it is doubtful whether they are indeed related to the underlying pathology of addiction. 6
The main objective of this narrative review was to investigate the key modern trends in the prevention of psychotropic addiction and to identify which interventions are most effective and where and how they are performed.
A specific review of factors important for the prevention of drugs was conducted in PsycInfo and MedInfo databases, entering as search items for the factors the words “prevention”, “addiction”, “drug addiction”, “drugs”, “drug prevention strategies”, “substance use” and “dependence” or the combination of the above words. The data were collected from 2018 to 2021. The search included articles published from 2000 onwards. A total of 65 articles were found among which 46 articles were included in the review. Articles that clearly referred to the prevention of substance use (interventions, strategies, or prevention systems) were included in this study. Articles that indirectly referred to prevention or were restricted to medication or genetic aspects of prevention were excluded. Regarding the type of articles, 26 of them were research articles and 20 were review articles. Among the research articles, 11 were correlational quantitative studies, 9 were quasi-experimental studies, and 6 used qualitative designs. Concerning the participants, 34 of the studies were conducted on school-based programs and 9 on community-based prevention programs. The remaining ones did not refer to specific intervention programs and focused on theoretical elements or prevention and health policies systems.
Taking into consideration the above mentioned as well as the theoretical concerns and the steady need to improve the problematic parts, a search of relevant findings from research and review articles was conducted. Given the dissimilarity of the research studies found, the data were analyzed using content analysis and systematized in different categories according to the point on which each research focused. For a better understanding and categorization of the research results, it was deemed expedient to mention a) the major interventions and techniques used in the studies and b) the results categorized through the above-mentioned analysis.
(A) With regard to the type and the theoretical approach of the interventions applied in the studies found in this review, a wide range of theoretical approaches and techniques were identified that illustrate the preferred trends in prevention over the past years. Characteristically, there is a great heterogeneity among the programs and methods. 7 , 8 Before reviewing the results in the following section, these interventions are elaborated. The following categorization of interventions was chosen because it contributes to a systematic and comprehensive display ( Table 1 ).
a) A lot of studies used interventions that could be characterized as environmental interventions 9 - 11 which highlight mainly the implementation of interventions in a more natural, social, and cultural environment where the individuals act and behave. The aim of these interventions was to increase the cultural belonging to achieve which, a lot of interventions used culturally-based techniques. 12
b) A second category of studies, possibly the one encompassing the majority of them, includes the studies that used more cognitive-based techniques, namely interventions whose broader theoretical framework relies on the cognitive-behavioral approach. Thus, it specifically includes social skills interventions, strengthening families programs and life skills trainings, 13 enhancing communication channels interventions, CHAT- a solution focused strategies program, increasing self-efficacy methods, 14 - 16 McGuires’s persuasion, 17 CHOICE program, Cherokee self-reliance program, 18 Project ALERT program, Persuasion Communication Model, SMART program, random student drug testing, 19 development and monitoring of career goals, and internet-based prevention programs. 20
c) A third research category includes methods that could be characterized in a broader sense as humanistic. These methods are based on the restricted results of the mainly informative (based on providing information) and more cognitive approaches and illustrate the experiential character of prevention. Thus, a lot of prevention strategies deal with the promotion of youth development, 21 peer-to-peer mentoring, 22 motivational interviewing 23 , 24 (a method with a cognitive background as well), narrative therapy, educational and career counseling, and positive youth development strategies with the active participation of teachers and parents. 21 , 25 Obtaining insight and expertise from program personnel and school staff and administrators can bring the program to a point where these strategies can still be achieved and theoretical linkages made after a program has been implemented. This is a necessary foundation for measuring the success of an intervention. 21 A common characteristic of these methods is the intent of active participation of all the community members such as local media and teen networks. Some of them, when implemented in a school-based environment, are delivered by teachers, 26 not by specialized scientists alien to the school environment.
(B) In the second and main part of this section, the results of the reviewed articles are presented as categorized based on (a) variables and factors concerning the effectiveness proved important through the review and (b) a number of important topics highlighted for the prevention of addictive behaviors ( Table 2 ).
a) Concerning the variables and/or the factors that proved more or less important to the implementation of prevention programs, the self-efficacy variable is the most frequently mentioned one. Self-efficacy is the optimistic self-belief in one’s competence or chances of successfully accomplishing a task and producing a favorable outcome. 27 , 28 The building of self-efficacy seems to be a characteristic of addiction-proof children. 14 Apart from self-efficacy, other variables from the cognitive approach associated with successful efforts of prevention are motivational enhancement, life coping skills, decision-making, 20 enhanced drug resistance skills, increased knowledge, and behavior determinants (attitudes, subjective norms, self-efficacy, intention) more negative towards drugs. 13
The variables that derive from the humanitarian tradition and positive psychology have very positive results when included in prevention programs. Thus, the promotion of positive youth development and the cultivation of an optimistic future orientation, 21 the development of hopefulness, 29 harmony among family members, 30 and the strengths and the enforcement of a healthy lifestyle have been repeatedly associated with a reduction in use of addictive substances. The positive role of self-reliance which is defined as being true to one’s self and being connected, responsible, disciplined, and confident 18 can be included in the same context.
Other studies investigated the social support and generally the effect of the social environment on addiction prevention. The results are usually controversial. Therefore, the influence of friends and peer pressure 31 may be associated with high-risk behaviors, but friends are preferred in seeking help. 26 , 30 Self-evidently, having family members who use drugs and adverse life events are associated with high risk. 31 , 32 On the other hand, peer networks and dynamic group leaders can also help to motivate the students. 33 The role of the teachers in prevention is estimated to be positive, as their involvement in prevention programs is associated with lower risk. A positive impact seems to be attributed to parenting monitoring and strict parenting as well as religiosity. 26 Especially in the school context, it seems that belonging to the public school network, development of activities targeting sexuality, development of “Health at School Program” activities, offering extracurricular activities, and having an administrator that participated in training courses on drugs are associated with program implementation. 34
b) With regard to the more general important topics highlighted in substance addiction prevention, a first point is that a lot of researches were based on an informative approach about prevention (e.g., decision), 31 namely the provision of information to the target group (youths or students) about the negative effects of addiction that is expected to lead to a logical refusal of substance use. The major conclusion drawn is that prevention strategies based mainly or exclusively on information have poor results, 17 , 35 which is confirmed by a study according to which most youths were aware of the adverse health effects of substance use. 31 However, other studies based on internet-based interventions supported that intervention groups have more knowledge and are less likely to use cannabis. 20 It is recommended to adopt a broader approach which embraces other directly or indirectly involved individual groups (parents, teachers) and control the quantity and quality of the information provided. 35 , 36 Relevant to the provision of appropriately purposeful information about substance use was the finding about the inadequate awareness and messages in workplace, 37 an example of the expansion of prevention in environments outside the school.
The importance of development stages and the transition from one development stage to the next was another topic highlighted in the review. 38 Studies focused on the understanding and recognition of possible genetic risks and protective factors at the crucial age of children and teenagers. 39 , 40 Some data seem to be confirmed, such as the fact that the onset of substance use at a later stage reduces the problematic use. 12
A lot of studies 18 , 41 - 43 mentioned the effectiveness of culturally grounded interventions. These interventions are culturally sensitive, which means that they primarily take into consideration the cultural characteristics of the population on which the intervention is implemented. Quite often sub-techniques are used that deploy special cultural characteristics of a place (e.g. canoe). 41 The positive results of these efforts reinforce the poorer results of interventions, where a prevention program is transferred and implemented invariably from one country to another, mainly from a developed country to a so-called developing country. 42 Therefore, the integration of appropriate theory and cultural elements seems to be necessary. However, there are also findings that consider that risk and protective factors concerning majority-based research may also be predictors for minorities. 43
Similar to the above is the finding that a lot of preventive interventions followed the ground-up methodology, namely the configuration of interventions after relevant research in population members, where the intervention was implemented later on. 16 , 20 Therefore, in case the aim is to apply an intervention in the school-based environment, the prevention strategies are configurated and chosen after some preliminary work (e.g., focus groups) with the affected populations (e.g., teachers, students), which illustrates the needs of these particular individuals at a specific time. This is in contrast with the most common method (up-ground) where already tested interventions are applied to various populations. 40
As mentioned in the methods section, the greatest part of interventions took place in school-based environments that seem to be probably the most suitable ones for the implementation of interventions, as indicated by findings about effectiveness. 19 However, the findings are not always consistent, as there are also findings that suggest minor to insignificant positive results. 17 Furthermore, certain findings indicated a lower effectiveness in boys compared with girls and better results in children of a low socio-economic level compared with children of a higher socio-economic level. 42 With regard to the frequent implementation of prevention programs in school-based environments, a question of generalization is raised, as expected, namely to what extent the whatsoever results achieved in this environment can be sustained outside this environment. 20
A classic study indicated small- to medium- sized differences in behavioral problems between students who participate for the longest period of time and those who participate for the shortest time 19 which highlighted the importance of the sustainment of the results as well as the retention of students both in the school-based environment and the prevention programs. As noted, the impact of education and persuasion programs tended to be small, at best. When positive effects were found, they did not persist. 17 Furthermore, in terms of effectiveness, the flexibility in delivering the program, such as offering the program in different days and times, seems quite important. 22 However, low effectiveness, indicated even by large-scale studies, is probably attributed to issues of methodology, such as selection strategies. 43
A matter of greater importance with various social aspects that was highlighted was social responsibility with regard to addiction prevention. 44 The importance of the involvement of all the community members leads to the conclusion that prevention concerns potentially every member of the society and not just the populations included in the so-called high-risk groups. Thus, the involvement of school, neighborhood, family, and various associations and religious bodies 45 - 48 seems to be important as it enhances the conscientiousness and responsible behavior of the citizens towards such a vitally important matter. In the same context, the importance of a broader collaboration and consistency between policy design and implementation of educational interventions 17 is also highlighted; however, this is a very complex issue which faces various obstacles during its implementation such as the cost of the interventions. 4
The policy issue comes to the forefront when addiction prevention issues are dealt with. Roumeliotis 49 showed drug addiction is presented as a problem to be handled by experts rather than politics. This shows an important shift in the role of policies in prevention and treatment. Certainly, there is an increasing trend towards harm reduction and even educational approaches and other more traditional forms of prevention including harm reduction. 48 These matters are underlined by the necessity for transdisciplinary scientific collaborations that have the potential to strengthen substance use and abuse research and prevention. 49 Transdisciplinarity is distinguished from other forms of cross-disciplinary collaboration, such as multidisciplinarity and interdisciplinarity. Transdisciplinarity is the process whereby researchers work jointly using a shared conceptual framework that draws together discipline-specific theories, concepts, and approaches to address a common problem. 49
As indicated in the first part of the results, there is great heterogeneity in the interventions and techniques of addiction prevention. This might imply a great variety of available methods and strategies that can be used. The selection of the suitable methods in each case should be based on the needs of the population to which the respective program is applied and on the study of the effectiveness of the available interventions. Any combination of methods and techniques is legitimate as long as it is based on a justified theoretical background and previous experience from prevention programs. The reported trend of environmental interventions 8 - 10 is a positive step, as it takes into account people’s needs in the natural and social environment in which they act. Given the prevalence of cognitive-behavioral methods on a large scale in the treatment of mental disorders, it is absolutely natural for similar interventions to be used in prevention as well. 15 , 16 These interventions, which require a rational data processing, have a proven effectiveness; however, quite often they seem to be inadequate for the prevention of rather complex psychosocial problems, such as addiction. For this reason, there is a prevalence of more experiential interventions (either in combination with cognitive-behavioral techniques or not), which attempt to include not only the directly affected people (e.g., the students) but also parents, teachers, and other community members or bodies. 34 , 35 Apart from the above mentioned, other factors should be taken into account including ‘Who is training the trainers?’, ‘How can quality delivery be ensured on a large scale?’, ‘How can a universal program become part of a chain of prevention?’ and ‘How do we handle the needs of practitioners?’ 50 - 52
With regard to the factors/variables that play an important role in addiction prevention, as expected, the findings highlighted already known variables, such as self-efficacy 14 - 16 and the development of positive characteristics like hopefulness 29 and social support. 31 It could be assumed that based on the repeated findings, an effective prevention program could include the development of cognitive and social skills in line with the development of a positive lifestyle, way of thinking, feeling, and behaving. The introduction of complementary concepts and interventions from the field of positive psychology would be a suggested step at the therapeutic level. Such interventions could be the emergence and strengthening of strengths as well as mental resilience and positive emotions, such as hope and gratitude. According to Peele, 53 addiction-proof children have skills to gain real rewards in life, values that sustain moderation, and reject addiction in favor of pursuing positive goals, and confidence that they can achieve these goals. This is in contrast with addiction-prone children, who are more likely to come from backgrounds that deny them any opportunity, are plagued by bad feelings (depression, anxiety, lack of purpose), and have history of dependence. The reinforcement of these characteristics seems to be even more effective when teachers, parents, and the broader community are involved in the program. Therefore, prevention should concern a bigger part of society and should not be implemented fragmentarily only to the population at risk.
As indicated by the findings, in the review of substance addiction prevention, certain repeated matters raised which were evaluated in order to improve future choices and practices. Therefore, the restricted effectiveness of strategies based exclusively on information 17 , 35 has been confirmed, as aptly pointed out by Zafeiridis. 54 As we live in an era in which information constitutes a basic part of our lives, information is recommended to be provided at an initial stage of prevention, whereas later on it should become more experiential. As indicated, it is important to control the quantity and quality of the information 35 , 36 to be essentially helpful to parents, teachers, and children.
Prevention programs should also take into account the importance of development stages. 38 A reasonable conclusion drawn by the findings is that prevention should be applied at a young age (even at pre-school age), because the beginning of substance use later on reduces the possibility of problematic use. This is probably due to the fact that young people, from an age onwards, have already managed to develop important cognitive and emotional mechanisms of dealing with situations. The recognition of protective factors, as well as risk factors at a crucial age is also helpful in designing an effective intervention.
An issue dealt with in numerous researches was the importance of culturally-based interventions. 17 , 41 The programs implemented in developed countries can form a good knowledge and practice basis, but it is obvious that they should not be applied invariably in different cultural environments. A good suggestion in this regard would be the development of programs through the ground-up methodology, which initially illustrates the population needs, followed by the design of prevention interventions. To this end, the theoretical knowledge should be deployed and there should also be an integration of the appropriate theory and cultural elements.
With regard to the usual choice of implementing prevention programs in school-based environments, 19 it seems that school-based environment remains the most suitable one for these interventions as it combines the daily involvement of the child in a series of activities in the community environment where potentially significant others, such as teachers and parents, are also involved. The utilization of research findings is important in order to increase the so far minor positive results and generalize them in different conditions outside school.
On a broader level, it is commonplace that substance addiction prevention should be dealt with not only by the directly affected populations but by various bodies, such as associations, communities, religious bodies, as well as every individual member of the society. It is a reasonable assumption that the increase in social responsibility brings about an increase in individual responsibility and that the social well-being is interrelated with the individual one.
Finally, on a policy level, drug prevention is not something only experts should deal with, but requires an active political will and active involvement of the citizens. Accordingly, not only transdisciplinarity, but also the consistency of policy design and implementation of educational interventions is required and vital. To overcome possible obstacles, the cost of prevention should be calculated and compared to that of interventions. Effective prevention can, therefore, have multiple benefits on both personal and social levels.
The results of this study concerning the prevention of drug use showed the most effective interventions are those implemented in community contexts, such as schools, at a young age, and based on experiential methods tailored to the needs of each population. Humanitarian approaches are effective and can be applied in parallel with cognitive and behavioral approaches. In this context, methods from positive psychology could be used. It is important for clinicians working in the community to implement or recommend prevention programs with the above characteristics. Nevertheless, even for those clinicians who do not work in the community, it is important to know what really prevents substance use to make the right referrals and give the right directions. At the level of health services, it is important that prevention programs are implemented primarily universally in a broad context such as schools but also secondarily selectively in high-risk groups. Finally, it is important to emphasize that substance abuse prevention is not just for mental health professionals but also for the whole community, teachers, parents, and every individual citizen.
The present narrative review highlighted some important issues for addiction prevention. However, this was not a systematic review or meta-analysis. Further studies are recommended to conduct a more systematic review.
Acknowledgments
I thank the colleagues in the Department of Psychology at the University of Western Macedonia and the students in the course of psychopathology for their support.
Citation: Flora K. A review of the prevention of drug addiction: specific interventions, effectiveness, and important topics. Addict Health . 2022;14(4):288-295. doi:10.34172/ahj.2022.1348
Conflict of Interests
Author declares no conflict of interests.
Ethics Approval
Not applicable.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
May 6, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
reputable news agency
Parental deaths due to guns or drugs harmed nearly 100,000 US kids in 2020: Study
by Ernie Mundell

Nearly 100,000 U.S. children lost a parent in 2020 to gun violence or drug overdose, a three-fold rise since 1999, according to a new study.
Overall, these two causes made up nearly a quarter (23%) of parental losses in 2020, almost double the level cited in 1999, according to a team who reported its findings May 4 in the Journal of the American Medical Association ( JAMA ).
"US youth are at high and increasing risk of experiencing parental death by drugs or firearms," a team led by Mathew Kiang of the Stanford University School of Medicine concluded.
In the study, Kiang's team noted that, "the U.S. is experiencing dual overlapping public health crises of drug poisoning … and firearm deaths. Since 1999, more than 1 million residents of the U.S. have died by fatal drug poisonings and more than 750,000 by firearms."
Just how much is all this affecting the nation's children?
To find out, the researchers combed through federal death statistics, fertility data and population demographics to estimate how many parents lost their lives to drugs or gun violence in recent years.
Many of these parents died young: The study found the average age of fatal drug overdose or gun injury to a parent was just 42. Fathers were three times more likely to die from these causes than mothers.
Drug overdose deaths are rising especially fast among people in their 30s or 40s, the researchers noted. Approximately 72,800 kids lost a parent to a drug overdose in 2020, more than four times the 16,000 children who suffered such a tragedy in 1999.
Deaths to parents stemming from gun violence also rose by 39% during that period, Kiang's team reported. That's significantly higher than the 24% rise in the number of kids who lost a mother or father from other causes during that time.
Black children were three times more likely to lose a parent to drugs or gun violence compared to kids as a whole.
All of this means serious mental harm to more and more American children who are grieving these losses, said Robin Gurwitch, a psychologist and professor at the Duke University School of Medicine.
The shame around having a parent die from drugs or gun violence is part of the problem, she told CNN.
"When it can't be talked about openly and freely, it makes it harder for children to get the support they need," said Gurwitch, who was not involved in the new study.
"For children who hold those things inside, the risk of it leaking out into everything from severe behavior challenges to bereavement disorders to other types of mental health challenges—anxiety, depression or their own substance abuse—goes way up."
There's information on helping kids deal with grief at the Child Mind Institute.
© 2024 HealthDay . All rights reserved.
Explore further
Feedback to editors

Likelihood of kids and young people smoking and vaping linked to social media use
57 minutes ago

Primary health coverage found to have prevented more than 300,000 child deaths in four Latin American countries

Global life expectancy projected to increase by nearly 5 years by 2050 despite various threats

Number of people experiencing poor health, early death from metabolism-related risk factors has increased since 2000

Men at greater risk of major health effects of diabetes than women, study suggests

Discovery of a master neuron that controls movement in worms has implications for human disease
2 hours ago

First US trial of varenicline for e-cigarette cessation shows positive results
3 hours ago

Examining the mechanisms and clinical potential of a promising non-opioid pain therapy candidate

Machine learning method for predicting glioma mutations shows promise for personalized treatment

Study finds brain wiring predicted adolescents' emotional health during COVID-19 pandemic
4 hours ago
Related Stories

Steady rise in US suicides among adolescents, teens
Mar 29, 2024

Big rise seen in gun deaths, overdoses among U.S. kids
Oct 7, 2023

Guns and drugs are killing people in the US at increasing and unprecedented rates, 20-year study finds
Jul 6, 2023

The health and economic toll of gun violence in youth
Nov 6, 2023

New study calculates alarming lifetime risk of death from firearms and drug overdoses in the US
Aug 19, 2020

Dozens of US adolescents die from drug overdoses every month. An expert unpacks the grim numbers
Nov 28, 2023
Recommended for you

Genetics, environment and health disparities linked to increased stress and mental health challenges during adolescence
5 hours ago
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter

IMAGES
VIDEO
COMMENTS
40 Drug Abuse & Addiction Research Paper Topics. The research paper about the drug abuse can be of any subject: Sociology, Criminology, Psychology, Medicine, Pharmacology, Statistics, even History. This problem emerges at the very dawn of humanity. So, the topic itself is too vast to capture it all in one paper.
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol.When considering other substances, the report estimated that 4.4 million individuals ...
Research Topics. En español. The National Institute on Drug Abuse (NIDA) is the largest supporter of the world's research on substance use and addiction. Part of the National Institutes of Health, NIDA conducts and supports biomedical research to advance the science on substance use and addiction and improve individual and public health.
Introduction. Close to a quarter of a century ago, then director of the US National Institute on Drug Abuse Alan Leshner famously asserted that "addiction is a brain disease", articulated a set of implications of this position, and outlined an agenda for realizing its promise [].The paper, now cited almost 2000 times, put forward a position that has been highly influential in guiding the ...
While it is beyond the scope of this paper to provide a detailed analysis ... A second area for improvement in substance use and addiction research is the further integration of patient-important outcomes. ... next steps in the global research agenda on syringe access for injection drug users. Addiction, 105 (5), 860-861. doi: 10.1111/j.1360 ...
For much of the past century, scientists studying drugs and drug use labored in the shadows of powerful myths and misconceptions about the nature of addiction. When scientists began to study addictive behavior in the 1930s, people with an addiction were thought to be morally flawed and lacking in willpower. Those views shaped society's ...
employ comprehensive research, treatment, and policy reforms, as we do with other chronic illnesses such as diabetes, HIV/AIDS, and cancer. In 2016, the U.S. surgeon general released the first-ever "Facing Addiction in America: Surgeon General's Report on Alcohol, Drugs, and Health," which specifically called attention to the
The characterisation of the role of glia and the extracellular matrix (ECM) in drug-induced synaptic plasticity is an exciting emerging field of drug addiction research as it comes with promising ...
Substance use and addiction are often misunderstood and people do not realize the complexities of addiction and substance use disorder. One key to addressing this disease is education and awareness. There are awareness days and observance events around the globe that help with this. One of these is Red Ribbon Week, which provides a platform for ...
Inhibitory control, a core deficit in drug addiction, may be amenable to targeted prefrontal cortex interventions. ... Research Highlights 22 Sept 2023 Neuropsychopharmacology. Volume: 49, P: 357-358.
Access a wealth of information and downloadable full-text publications on a range of topics, including addiction science, medical consequences, trends and statistics, and the link between drugs and HIV. The NIDA Drug Pubs clearinghouse closed its doors on April 7, 2022. We will no longer be shipping hard copy NIDA publications.
This paper first introduces important conceptual and practical distinctions among three key terms: substance "use," "misuse," and "disorders" (including addiction), and goes on to describe and quantify the important health and social problems associated with these terms. National survey data are presented to summarize the prevalence ...
The current paper highlights the causes of drug abuse, and describes the treatment and prevention of drug abuse and addiction for proper management of the problem. Discover the world's research 25 ...
About Addiction Science. Many people don't understand why or how other people become addicted to drugs. They may mistakenly think that those who use drugs lack moral principles or willpower and that they could stop their drug use simply by choosing to. In reality, drug addiction is a complex disease, and quitting usually takes more than good ...
These research queries and findings are presented in the form of updates, white papers and case studies. In addition, the Butler Center for Research collaborates with the Recovery Advocacy team to study special-focus addiction research topics, summarized in monthly Emerging Drug Trends reports. Altogether, these studies provide the latest in ...
Background: This paper presents a new methodology for identifying and prioritizing research gaps, contributing to the nascent literature on systematic ways to identify research gaps.Objectives: The goal of this paper is to report on a gaps analysis of substance use disorder (SUD) research.Based on input from Military Health System stakeholders, we selected the following subtopics as priorities ...
85 percent of the world's research on drug abuse and addiction. Other sponsoring agencies include the National Institute of Mental Health (NIMH), the National Institute on Alcohol Abuse and Alcoholism (NIAAA), and the Substance Abuse and Mental Health Services Administration (SAMHSA), all in the Department of Health and Human Services; as well as the Office of Justice Programs (OJP) in the ...
How does science provide solutions for drug abuse and addiction? Scientists study the effects that drugs have on the brain and on people's behavior. They use this information to develop programs for preventing drug abuse and for helping people recover from addiction. Further research helps transfer these ideas into practice in our communities. 3
This charge has two critical components. The first is the strategic support and conduct of research across a broad range of disciplines. The second is ensuring the rapid and effective dissemination and use of the results of that research to significantly improve prevention and treatment and to inform policy as it relates to drug abuse and ...
The alcohol and addiction research domain criteria ... All data needed to evaluate the conclusions in the paper are present in the paper and/or in the materials cited herein. Additional data related to this paper may be requested from the authors. ... Implications for practice, research, and policy. Drug Alcohol Depend. 181, 162-169 (2017 ...
It starts with merely. smoking of cigarettes and gradually drowns the person into the trap of drug abuse. Stress, anxiety, peer pressure, poverty are some of the main causes of drug abuse.As is ...
The view that substance addiction is a brain disease, although widely accepted in the neuroscience community, has become subject to acerbic criticism in recent years. These criticisms state that ...
60+ Addiction Topics to Inspire You for a Great Paper. There are many forms of addictions that afflict humanity today. People who suffer from drug abuse, alcohol, or another type of addiction deserve to speak about their issues. Students among world-recognized universities unite to explore this problem, so the topic of drug addiction is ...
Despite the high prevalence of substance abuse and its often devastating outcomes, especially among disadvantaged populations, few Americans receive treatment for substance use disorders. However ...
b) With regard to the more general important topics highlighted in substance addiction prevention, a first point is that a lot of researches were based on an informative approach about prevention (e.g., decision), 31 namely the provision of information to the target group (youths or students) about the negative effects of addiction that is ...
by Ernie Mundell. Nearly 100,000 U.S. children lost a parent in 2020 to gun violence or drug overdose, a three-fold rise since 1999, according to a new study. Overall, these two causes made up ...