- About the Hub
- Announcements
- Faculty Experts Guide
- Subscribe to the newsletter

Explore by Topic
- Arts+Culture
- Politics+Society
- Science+Technology
- Student Life
- University News
- Voices+Opinion
- About Hub at Work
- Gazette Archive
- Benefits+Perks
- Health+Well-Being
- Current Issue
- About the Magazine
- Past Issues
- Support Johns Hopkins Magazine
- Subscribe to the Magazine
You are using an outdated browser. Please upgrade your browser to improve your experience.
Credit: Getty Images
What does the end of the COVID-19 pandemic look like?
Johns hopkins university public health experts offer insights into what will signal that sars-cov-2 is moving from pandemic to endemic, and how we might change our approach to the virus going forward.
By Amy Lunday
As the United States approaches the second anniversary of its initial COVID-19 shutdowns, we're daring to dream about what the end of the pandemic might look like. With omicron cases plummeting, indoor mask mandates in every state but Hawaii are set to expire —a change that would have seemed unthinkable just weeks ago.
Some are having an easier time than others embracing this shift in mindset. The idea of setting aside a bulk order of newly purchased, highly protective N95 masks might cause whiplash for some, while others gleefully head to their local pub to celebrate sans mask, NIOSH-approved or otherwise. Just because the rules are changing, does that mean the pandemic is really ending? Here, Johns Hopkins University public health experts offer insights into what signs their research tells them will signal that SARS-CoV-2 is moving from pandemic to endemic.
When it's less worrisome than the flu
David Dowdy , associate professor of epidemiology at the Johns Hopkins Bloomberg School of Public Health
I t's difficult to know exactly how the pandemic will "end," but I think there's at least a reasonable chance that COVID-19 ends up being less of a public health concern than the flu. Even now, for someone who is vaccinated and boosted, the risk of hospitalization is higher if they were to get the flu than if they were to get COVID-19. I think it's too early to say whether COVID-19 waves will happen every winter, more frequently, or less frequently. But to my mind, if COVID-19 is not causing more people to get seriously ill than another "non-pandemic" infectious disease (seasonal flu, for example), it makes sense to declare the COVID-19 pandemic over.
As states drop COVID-19 restrictions, some experts warn it's premature to declare victory
Post-omicron life can be downright maddening, we’re entering the control phase of the pandemic, estimated 73% of u.s. now immune to omicron: is that enough, a return to mostly normal life while rebuilding trust in public health.
Tara Kirk Sell , senior scholar at the Johns Hopkins Center for Health Security and an assistant professor at the Johns Hopkins Bloomberg School of Public Health
T here won't be a clean end to the pandemic but it will stop being so front-and-center. As cases go down, protective measures will wane. At certain points, there will be surges in cases and some efforts to reduce spread of disease, like masking, may come back into our lives temporarily. Additional booster shots might be needed, and some people will get them, but like influenza vaccines, many in the U.S. won't or will never have gotten vaccinated in the first place and so there will also be occasional surges in hospitals. But while we return to mostly normal life, some things won't go back to normal—trust in public health has taken a hit. Health-related misinformation is more powerful than ever. This will be the work of the next generation of leaders in public health.
Greater consideration for mental health
Elizabeth Stuart , professor in the departments of Mental Health, Biostatistics, and Health Policy and Management in the Johns Hopkins Bloomberg School of Public Health
A s we consider the next stage of the pandemic, with hopefully fewer severe infections and perhaps less worry about physical health implications, the mental health consequences of the pandemic—for adults and kids—will continue. This includes need to support individuals who may experience mental health challenges after being infected with COVID, children and adults who lost a loved one to COVID, and those who experienced financial or other stresses during the pandemic. The mental health system was overburdened before the pandemic, with limited supply of providers. As articulated in my blog post with colleagues from Johns Hopkins and Columbia , moving forward we need a population mental health approach, including public health media campaigns, expanded screening, targeted interventions, increased capacity, and more surveillance and research. Setting up such a system will improve health and help move the country and world toward recovery in a way that will benefit all in the short and long term.
Image credit : Getty Images
Less transmission, more normalcy
Crystal Watson , a senior scholar at the Johns Hopkins Center for Health Security and assistant professor in Environmental Health and Engineering at the Bloomberg School of Public Health
W hat I'm looking for is sustained reduced transmission. Also, if we do have new variants and new surges of cases, we want to see that immunity, through vaccination and prior infection, buffers against the large surges in hospitalizations and deaths that we've seen even with omicron. I think once we start to see infections and mild/moderate cases even more decoupled from hospitalizations and deaths, that's when we can start to take a deep breath and really think about how we treat this virus as a more routine infectious disease hazard rather than an acute pandemic threat.
A shift from pandemic to endemic, thanks to vaccines
Andrew Pekosz , professor of molecular microbiology and immunology at the Johns Hopkins Bloomberg School of Public Health
W e're really in a situation where vaccination has laid the groundwork for strong immune responses. And now, even if you do get infected, the end result is a milder disease and a stronger immune response to protect you from the next variant. While I've learned not to try and predict what SARS-CoV-2 will do, it is a safe bet that more immunity in the population will limit disease and eventually reduce virus infections as well. SARS-CoV-2 eventually will put itself in a pigeonhole where it won't have much ability to change drastically and get around immune responses, and that will be the time when we can really start talking about this as something more like seasonal flu, as opposed to the pandemic virus that it is still to this day.
Rethinking our approach to respiratory illnesses beyond COVID-19
Brian Garibaldi , medical director of the Johns Hopkins Biocontainment Unit and associate professor of medicine at the Johns Hopkins University School of Medicine
M y hope is that as we move beyond the last stages of the omicron surge, we start to rethink our approach to respiratory viral illnesses in general. We have the ability to use data about community transmission of viruses such as SARS-CoV-2, RSV, and influenza to drive common sense local recommendations about how we can protect the most vulnerable among us from the risk of severe disease or death from these preventable infections. I would have no problem wearing a mask indoors when there are high levels of transmission of these viruses in my community in order to protect myself, my family, and others from getting sick.
I do think that we are approaching a point at which individuals can start to decide for themselves what level of risk they are willing to tolerate when it comes to wearing masks to prevent COVID-19. But I am not sure we are quite there yet. While cases are decreasing rapidly in the U.S., there remains a high level of community transmission in many places, and there are still millions of Americans who are either unvaccinated, or unable to mount an effective response to vaccines. And we are in the middle of winter which means that in many parts of the country people are gathering indoors more often and in greater numbers. I am also concerned about what might happen in terms of community transmission as mask requirements are rescinded in schools, where the majority of 5- to 12-year-olds are not yet vaccinated. Personally I plan to wear a mask indoors for the foreseeable future, mostly so that I don't get sick and have to miss clinical shifts in the hospital at a time when everyone is tired from working extraordinarily hard over the last two years. Vaccines work and I am fully vaccinated and boosted, so my risk of a severe disease or death from COVID-19 is very low. I hope that as people weigh decisions about their own behavior (for COVID and beyond), they take into account the circumstances of those around them.
Posted in Health , Voices+Opinion
Tagged public health , coronavirus , covid-19
You might also like
News network.
- Johns Hopkins Magazine
- Get Email Updates
- Submit an Announcement
- Submit an Event
- Privacy Statement
- Accessibility
Discover JHU
- About the University
- Schools & Divisions
- Academic Programs
- Plan a Visit
- my.JohnsHopkins.edu
- © 2024 Johns Hopkins University . All rights reserved.
- University Communications
- 3910 Keswick Rd., Suite N2600, Baltimore, MD
- X Facebook LinkedIn YouTube Instagram
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
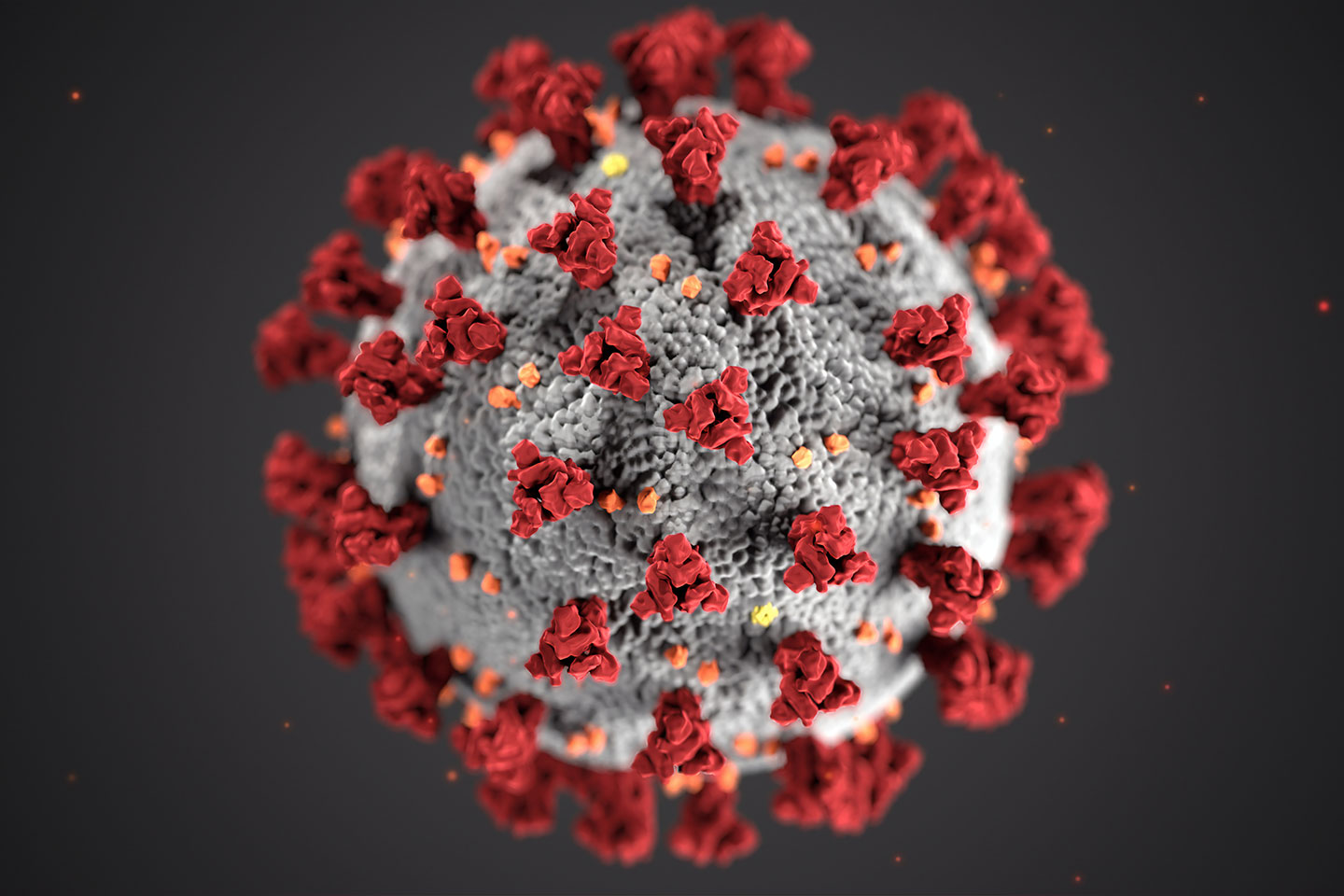
About COVID-19
What is covid-19.
COVID-19 (coronavirus disease 2019) is a disease caused by a virus named SARS-CoV-2. It can be very contagious and spreads quickly. Over one million people have died from COVID-19 in the United States.
COVID-19 most often causes respiratory symptoms that can feel much like a cold, the flu, or pneumonia. COVID-19 may attack more than your lungs and respiratory system. Other parts of your body may also be affected by the disease. Most people with COVID-19 have mild symptoms, but some people become severely ill.
Some people including those with minor or no symptoms will develop Post-COVID Conditions – also called “Long COVID.”
How does COVID-19 spread?
COVID-19 spreads when an infected person breathes out droplets and very small particles that contain the virus. Other people can breathe in these droplets and particles, or these droplets and particles can land on their eyes, nose, or mouth. In some circumstances, these droplets may contaminate surfaces they touch.
Anyone infected with COVID-19 can spread it, even if they do NOT have symptoms.
The risk of animals spreading the virus that causes COVID-19 to people is low. The virus can spread from people to animals during close contact. People with suspected or confirmed COVID-19 should avoid contact with animals.
What are antibodies and how do they help protect me?
Antibodies are proteins your immune system makes to help fight infection and protect you from getting sick in the future. A positive antibody test result can help identify someone who has had COVID-19 in the past or has been vaccinated against COVID-19. Studies show that people who have antibodies from an infection with the virus that causes COVID-19 can improve their level of protection by getting vaccinated.
Who is at risk of severe illness from COVID-19?
Some people are more likely than others to get very sick if they get COVID-19. This includes people who are older , are immunocompromised (have a weakened immune system), have certain disabilities , or have underlying health conditions . Understanding your COVID-19 risk and the risks that might affect others can help you make decisions to protect yourself and others .
What are ways to prevent COVID-19?
There are many actions you can take to help protect you, your household, and your community from COVID-19. CDC’s Respiratory Virus Guidance provides actions you can take to help protect yourself and others from health risks caused by respiratory viruses, including COVID-19. These actions include steps you can take to lower the risk of COVID-19 transmission (catching and spreading COVID-19) and lower the risk of severe illness if you get sick.
CDC recommends that you
- Stay up to date with COVID-19 vaccines
- Practice good hygiene (practices that improve cleanliness)
- Take steps for cleaner air
- Stay home when sick
- Seek health care promptly for testing and treatment when you are sick if you have risk factors for severe illness . Treatment may help lower your risk of severe illness.
Masks , physical distancing , and tests can provide additional layers of protection.
What are variants of COVID-19?
Viruses are constantly changing, including the virus that causes COVID-19. These changes occur over time and can lead to new strains of the virus or variants of COVID-19 . Slowing the spread of the virus, by protecting yourself and others , can help slow new variants from developing. CDC is working with state and local public health officials to monitor the spread of all variants, including Omicron.
- COVID-19 Testing
- COVID-19 Vaccines
- Preventing Respiratory Viruses
- Reinfection
- Difference Between Flu and COVID-19
- COVID Data Tracker
Search for and find historical COVID-19 pages and files. Please note the content on these pages and files is no longer being updated and may be out of date.
- Visit archive.cdc.gov for a historical snapshot of the COVID-19 website, capturing the end of the Federal Public Health Emergency on June 28, 2023.
- Visit the dynamic COVID-19 collection to search the COVID-19 website as far back as July 30, 2021.
To receive email updates about COVID-19, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
When will the COVID-19 pandemic end? Experts explain

McKinsey experts have analyzed what the 'end' of COVID-19 could look like. Image: REUTERS/Ritzau Scanpix Denmark
.chakra .wef-1c7l3mo{-webkit-transition:all 0.15s ease-out;transition:all 0.15s ease-out;cursor:pointer;-webkit-text-decoration:none;text-decoration:none;outline:none;color:inherit;}.chakra .wef-1c7l3mo:hover,.chakra .wef-1c7l3mo[data-hover]{-webkit-text-decoration:underline;text-decoration:underline;}.chakra .wef-1c7l3mo:focus,.chakra .wef-1c7l3mo[data-focus]{box-shadow:0 0 0 3px rgba(168,203,251,0.5);} Sarun Charumilind
Matt craven, jessica lamb, shubham singhal, matt wilson.

.chakra .wef-9dduvl{margin-top:16px;margin-bottom:16px;line-height:1.388;font-size:1.25rem;}@media screen and (min-width:56.5rem){.chakra .wef-9dduvl{font-size:1.125rem;}} Explore and monitor how .chakra .wef-15eoq1r{margin-top:16px;margin-bottom:16px;line-height:1.388;font-size:1.25rem;color:#F7DB5E;}@media screen and (min-width:56.5rem){.chakra .wef-15eoq1r{font-size:1.125rem;}} COVID-19 is affecting economies, industries and global issues

.chakra .wef-1nk5u5d{margin-top:16px;margin-bottom:16px;line-height:1.388;color:#2846F8;font-size:1.25rem;}@media screen and (min-width:56.5rem){.chakra .wef-1nk5u5d{font-size:1.125rem;}} Get involved with our crowdsourced digital platform to deliver impact at scale
Stay up to date:.
- This article includes updated perspectives of McKinsey experts on when the coronavirus pandemic will end based on the latest data.
- Among high-income countries, cases caused by the Delta variant reversed the transition toward normalcy first in the UK and then across the world.
- Analysis suggests that the Delta variant has effectively moved overall herd immunity out of reach in most countries for the time being.
- However, as the UK has weathered a wave of Delta-driven cases, it may be able to resume the transition toward normalcy.
- The 'end' of COVID-19 might mean the point at which is can be managed as an endemic disease; however, the emergence of a significant new variant is the greatest risk which could hinder this.
- The data shown in the piece was correct as of 23/08/21.
Since the March installment in this series, many countries, including the United States, Canada, and those in Western Europe, experienced a measure of relief from the COVID-19 pandemic when some locales embarked on the second-quarter transition toward normalcy that we previously discussed. This progress was enabled by rapid vaccine rollout, with most Western European countries and Canada overcoming their slower starts during the first quarter of 2021 and passing the United States in the share of the population that is fully immunized. However, even that share has been too small for them to achieve herd immunity, because of the emergence of the more transmissible and more lethal Delta variant and the persistence of vaccine hesitancy.
Among high-income countries, cases caused by the Delta variant reversed the transition toward normalcy first in the United Kingdom, where a summertime surge of cases led authorities to delay lifting public-health restrictions, and more recently in the United States and elsewhere. The Delta variant increases the short-term burden of disease, causing more cases, hospitalizations, and deaths. Delta’s high transmissibility also makes herd immunity harder to achieve: a larger fraction of a given population must be immune to keep Delta from spreading within that population (see sidebar, “Understanding the Delta variant”). Our own analysis supports the view of others that the Delta variant has effectively moved herd immunity out of reach in most countries for now, although some regions may come close to it.
While the vaccines used in Western countries remain highly effective at preventing severe disease due to COVID-19, recent data from Israel, the United Kingdom, and the United States have raised new questions about the ability of these vaccines to prevent infection from the Delta variant. Serial blood tests suggest that immunity may wane relatively quickly. This has prompted some high-income countries to start offering booster doses to high-risk populations or planning for their rollout. Data from the US Centers for Disease Control and Prevention also suggest that vaccinated people who become infected with the Delta variant may transmit it efficiently.
These events and findings have raised new questions about when the pandemic will end. The United Kingdom’s experience nevertheless suggests that once a country has weathered a Delta-driven wave of cases, it may be able to relax public-health measures and resume the transition toward normalcy. Beyond that, a more realistic epidemiological endpoint might arrive not when herd immunity is achieved but when countries are able to control the burden of COVID-19 enough that it can be managed as an endemic disease. The biggest risk to a country’s ability to do this would likely then be the emergence of a new variant that is more transmissible, more liable to cause hospitalizations and deaths, or more capable of infecting people who have been vaccinated.
Raising vaccination rates will be essential to achieving a transition toward normalcy. Vaccine hesitancy, however, has proven to be a persistent challenge, both to preventing the spread of the Delta variant and to reaching herd immunity. The US Food and Drug Administration has now fully approved Pfizer’s COVID-19 vaccine, and other full approvals may follow soon, which could help increase vaccination rates. Vaccines are also likely to be made available to children in the coming months, making it possible to protect a group that comprises a significant share of the population in some countries.
In this article, we review developments since our March update, offer a perspective on the situation and evidence as of this writing, and present our scenario-based analysis of when a transition toward normalcy could occur.
Even without herd immunity, a transition toward normalcy is possible
We have written previously about two endpoints for the COVID-19 pandemic: a transition toward normalcy, and herd immunity. The transition would gradually normalize aspects of social and economic life, with some public-health measures remaining in effect as people gradually resume prepandemic activities. Many high-income countries did begin such a transition toward normalcy during the second quarter of this year, only to be hit with a new wave of cases caused by the Delta variant and exacerbated by vaccine hesitancy.
Indeed, our scenario analysis suggests that the United States, Canada, and many European countries would likely have reached herd immunity by now if they had faced only the ancestral SARS-CoV-2 virus and if a high percentage of those eligible to receive the vaccine had chosen to take it. But as the more infectious Delta variant becomes more prevalent within a population, more people within that population must be vaccinated before herd immunity can be achieved (Exhibit 1).
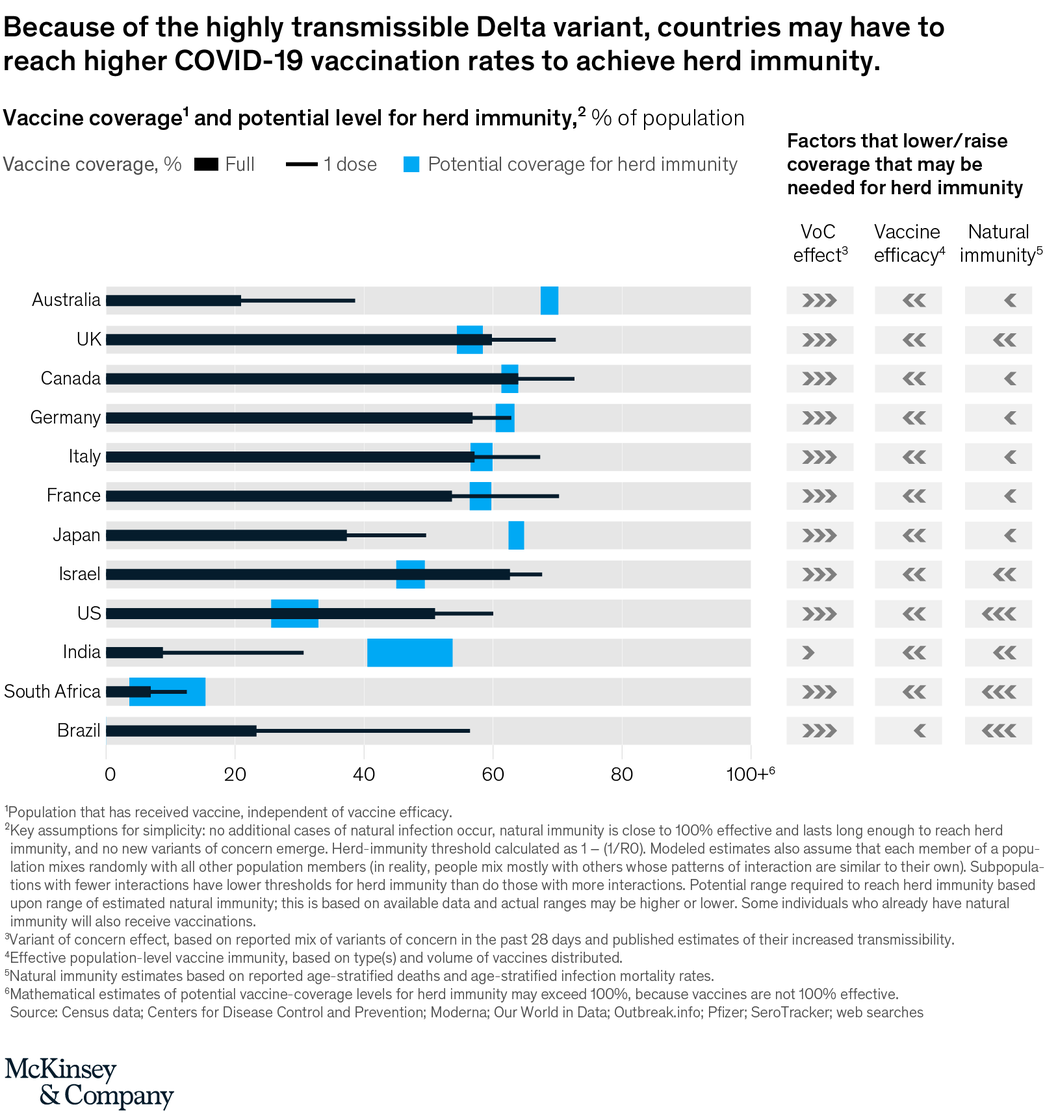
Vaccine hesitancy makes it all the more difficult to reach the population-wide vaccination level rates that confer herd immunity. Researchers are learning more about differences among individuals’ attitudes, which include both “cautious” and “unlikely to be vaccinated.” Meanwhile, social tolerance for vaccination incentives and mandates appears to be growing, with more European locations adopting vaccination passes and more large employers in the United States implementing vaccine mandates.
While it now appears unlikely that large countries will reach overall herd immunity (though some areas might), developments in the United Kingdom during the past few months may help illustrate the prospects for Western countries to transition back toward normalcy. Having suffered a wave of cases caused by the Delta variant during June and the first few weeks of July, the country delayed plans to ease many public-health restrictions and eventually did so on July 19, though expansive testing and genomic surveillance remain in place. UK case counts may fluctuate and targeted public-health measures may be reinstated, but our scenario analysis suggests that the country’s renewed transition toward normalcy is likely to continue unless a significant new variant emerges.
The United States, Canada, and much of the European Union are now in the throes of a Delta-driven wave of cases. While each country’s situation is different, most have again enacted public-health restrictions, thus reversing their transitions toward normalcy. The trajectory of the epidemic remains uncertain, but the United Kingdom’s experience and estimates of total immunity suggest that many of these countries are likely to see new cases peak late in the third quarter or early in the fourth quarter of 2021. As cases decline, our analysis suggests that the United States, Canada, and the European Union could restart the transition toward normalcy as early as the fourth quarter of 2021, provided that the vaccines used in these countries continue to be effective at preventing severe cases of COVID-19. Allowing for the risk of another new variant and the compound societal risk of a high burden of influenza, respiratory syncytial virus, and other winter respiratory diseases, the question for these countries will be whether they manage to arrive at a different epidemiological endpoint, as we discuss next.
Endemic COVID-19 may be a more realistic endpoint than herd immunity
We have previously written about herd immunity as a likely epidemiological endpoint for some countries, but the Delta variant has put this out of reach in the short term. Instead, it is most likely as of now that countries will reach an alternative epidemiological endpoint, where COVID-19 becomes endemic and societies decide—much as they have with respect to influenza and other diseases—that the ongoing burden of disease is low enough that COVID-19 can be managed as a constant threat rather than an exceptional one requiring society-defining interventions. One step toward this endpoint could be shifting the focus of public-health efforts from managing case counts to managing severe illnesses and deaths. Singapore’s government has announced that it will make this shift, and more countries may follow its lead.
Have you read?
Could covid-19 become endemic an expert explains what that means, 6 ways to ensure a fair and inclusive economic recovery from covid-19, covid-19 vaccine success can enable universal healthcare – here's how.
Other authors have compared the burden of COVID-19 with that of other diseases, such as influenza, as a way to understand when endemicity might occur. In the United States, COVID-19 hospitalization and mortality rates in June and July were nearing the ten-year average rates for influenza but have since risen. Today, the burden of disease caused by COVID-19 in vaccinated people in the United States is similar to or lower than the average burden of influenza over the last decade, while the risks from COVID-19 to unvaccinated people are significantly higher (Exhibit 2). This comparison should be qualified, insofar as the burden of COVID-19 is dynamic, currently increasing, and uneven geographically. It nevertheless helps illustrate the relative threat posed by the two diseases.

Countries experiencing a Delta-driven wave of cases may be more likely to begin managing COVID-19 as an endemic disease after cases go into decline. The United Kingdom appears to be making this shift now (though cases there were increasing as of this writing). For the United States and the European Union, scenario analysis suggests that the shift may begin in the fourth quarter of 2021 and continue into early 2022 (Exhibit 3). As it progresses, countries would likely achieve high levels of protection against hospitalization and death as a result of further vaccination efforts (which may be accelerated by fear of the Delta variant) and natural immunity from prior infection. In addition, boosters, full approval of vaccines (rather than emergency-use authorization), authorization of vaccines for children, and a continuation of the trend toward employer and government mandates and incentives for vaccination are all likely to increase immunity.
In 2000, Gavi, the Vaccine Alliance was launched at the World Economic Forum's Annual Meeting in Davos, with an initial pledge of $750 million from the Bill and Melinda Gates Foundation.
The aim of Gavi is to make vaccines more accessible and affordable for all - wherever people live in the world.
Along with saving an estimated 10 million lives worldwide in less than 20 years,through the vaccination of nearly 700 million children, - Gavi has most recently ensured a life-saving vaccine for Ebola.
At Davos 2016, we announced Gavi's partnership with Merck to make the life-saving Ebola vaccine a reality.
The Ebola vaccine is the result of years of energy and commitment from Merck; the generosity of Canada’s federal government; leadership by WHO; strong support to test the vaccine from both NGOs such as MSF and the countries affected by the West Africa outbreak; and the rapid response and dedication of the DRC Minister of Health. Without these efforts, it is unlikely this vaccine would be available for several years, if at all.
Read more about the Vaccine Alliance, and how you can contribute to the improvement of access to vaccines globally - in our Impact Story .

The authors wish to thank Xavier Azcue, Marie-Renée B-Lajoie, Andrew Doy, Bruce Jia, and Roxana Pamfil for their contributions to this article. This article was edited by Josh Rosenfield, an executive editor in the New York office.
Don't miss any update on this topic
Create a free account and access your personalized content collection with our latest publications and analyses.
License and Republishing
World Economic Forum articles may be republished in accordance with the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International Public License, and in accordance with our Terms of Use.
The views expressed in this article are those of the author alone and not the World Economic Forum.
Related topics:
The agenda .chakra .wef-n7bacu{margin-top:16px;margin-bottom:16px;line-height:1.388;font-weight:400;} weekly.
A weekly update of the most important issues driving the global agenda
.chakra .wef-1dtnjt5{display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;-webkit-flex-wrap:wrap;-ms-flex-wrap:wrap;flex-wrap:wrap;} More on Health and Healthcare Systems .chakra .wef-17xejub{-webkit-flex:1;-ms-flex:1;flex:1;justify-self:stretch;-webkit-align-self:stretch;-ms-flex-item-align:stretch;align-self:stretch;} .chakra .wef-nr1rr4{display:-webkit-inline-box;display:-webkit-inline-flex;display:-ms-inline-flexbox;display:inline-flex;white-space:normal;vertical-align:middle;text-transform:uppercase;font-size:0.75rem;border-radius:0.25rem;font-weight:700;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;line-height:1.2;-webkit-letter-spacing:1.25px;-moz-letter-spacing:1.25px;-ms-letter-spacing:1.25px;letter-spacing:1.25px;background:none;padding:0px;color:#B3B3B3;-webkit-box-decoration-break:clone;box-decoration-break:clone;-webkit-box-decoration-break:clone;}@media screen and (min-width:37.5rem){.chakra .wef-nr1rr4{font-size:0.875rem;}}@media screen and (min-width:56.5rem){.chakra .wef-nr1rr4{font-size:1rem;}} See all

Antimicrobial resistance is a leading cause of global deaths. Now is the time to act
Dame Sally Davies, Hemant Ahlawat and Shyam Bishen
May 16, 2024

Inequality is driving antimicrobial resistance. Here's how to curb it
Michael Anderson, Gunnar Ljungqvist and Victoria Saint
May 15, 2024

From our brains to our bowels – 5 ways the climate crisis is affecting our health
Charlotte Edmond
May 14, 2024

Health funders unite to support climate and disease research, plus other top health stories
Shyam Bishen
May 13, 2024

How midwife mentors are making it safer for women to give birth in remote, fragile areas
Anna Cecilia Frellsen
May 9, 2024

From Athens to Dhaka: how chief heat officers are battling the heat
Angeli Mehta
May 8, 2024
The end of the COVID-19 pandemic is in sight: WHO

Facebook Twitter Print Email
As the number of weekly reported deaths from COVID-19 plunged to its lowest since March 2020, the head of the World Health Organization (WHO) said on Wednesday that the end of the pandemic is now in sight.
“We have never been in a better position to end the pandemic”, Tedros Adhanom Ghebreyesus told journalists during his regular weekly press conference.
The UN health agency’s Director-General explained however, that the world is “not there yet”.
Finish line in sight
“A marathon runner does not stop when the finish line comes into view. She runs harder, with all the energy she has left. So must we. We can see the finish line. We’re in a winning position. But now is the worst time to stop running ”, he underscored.
He also warned that if the world does not take the opportunity now, there is still a risk of more variants, deaths, disruption, and uncertainty.
“So, let’s seize this opportunity”, he urged, announcing that WHO is releasing six short policy briefs that outline the key actions that all governments must take now to “finish the race”.

Urgent call
The policy briefs are a summary, based on the evidence and experience of the last 32 months, outlining what works best to save lives, protect health systems, and avoid social and economic disruption.
“[They] are an urgent call for governments to take a hard look at their policies and strengthen them for COVID-19 and future pathogens with pandemic potential”, Tedros explained.
The documents, which are available online , include recommendations regarding vaccination of most at-risk groups, continued testing and sequencing of the SARS-CoV-2 virus, and integrating effective treatment for COVID-19 into primary healthcare systems.
They also urge authorities to have plans for future surges, including the securing of supplies, equipment, and extra health workers.
The briefs also contain communications advice, including training health workers to identify and address misinformation, as well as creating high-quality informative materials.

Committed to the future
Tedros underscored that WHO has been working since New Year’s Eve 2019 to fight against the spread of COVID and will continue to do so until the pandemic is “truly over”.
“We can end this pandemic together, but only if all countries, manufacturers, communities and individuals step up and seize this opportunity”, he said.
Possible scenarios
Dr. Maria Van Kerkhove, WHO’s technical lead on COVID-19, highlighted that the virus is still “ intensely circulating” around the world and that the agency believes that case numbers being reported are an underestimate.
“We expect that there are going to be future waves of infection, potentially at different time points throughout the world caused by different subvariants of Omicron or even different variants of concern”, she said, reiterating her previous warning that the more the virus circulates, the more opportunities it has to mutate.
However, she said, these future waves do not need to translate into “waves or death” because there are now effective tools such as vaccines and antivirals specifically for COVID-19.
- History Classics
- Your Profile
- Find History on Facebook (Opens in a new window)
- Find History on Twitter (Opens in a new window)
- Find History on YouTube (Opens in a new window)
- Find History on Instagram (Opens in a new window)
- Find History on TikTok (Opens in a new window)
- This Day In History
- History Podcasts
- History Vault
COVID-19 Pandemic
By: History.com Editors
Updated: March 11, 2024 | Original: April 25, 2023

The outbreak of the infectious respiratory disease known as COVID-19 triggered one of the deadliest pandemics in modern history. COVID-19 claimed nearly 7 million lives worldwide. In the United States, deaths from COVID-19 exceeded 1.1 million, nearly twice the American death toll from the 1918 flu pandemic . The COVID-19 pandemic also took a heavy toll economically, politically and psychologically, revealing deep divisions in the way that Americans viewed the role of government in a public health crisis, particularly vaccine mandates. While the United States downgraded its “national emergency” status over the pandemic on May 11, 2023, the full effects of the COVID-19 pandemic will reverberate for decades.
A New Virus Breaks Out in Wuhan, China
In December 2019, the China office of the World Health Organization (WHO) received news of an isolated outbreak of a pneumonia-like virus in the city of Wuhan. The virus caused high fevers and shortness of breath, and the cases seemed connected to the Huanan Seafood Wholesale Market in Wuhan, which was closed by an emergency order on January 1, 2020.
After testing samples of the unknown virus, the WHO identified it as a novel type of coronavirus similar to the deadly SARS virus that swept through Asia from 2002-2004. The WHO named this new strain SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2). The first Chinese victim of SARS-CoV-2 died on January 11, 2020.
Where, exactly, the novel virus originated has been hotly debated. There are two leading theories. One is that the virus jumped from animals to humans, possibly carried by infected animals sold at the Wuhan market in late 2019. A second theory claims the virus escaped from the Wuhan Institute of Virology, a research lab that was studying coronaviruses. U.S. intelligence agencies maintain that both origin stories are “plausible.”
The First COVID-19 Cases in America
The WHO hoped that the virus outbreak would be contained to Wuhan, but by mid-January 2020, infections were reported in Thailand, Japan and Korea, all from people who had traveled to China.
On January 18, 2020, a 35-year-old man checked into an urgent care center near Seattle, Washington. He had just returned from Wuhan and was experiencing a fever, nausea and vomiting. On January 21, he was identified as the first American infected with SARS-CoV-2.
In reality, dozens of Americans had contracted SARS-CoV-2 weeks earlier, but doctors didn’t think to test for a new type of virus. One of those unknowingly infected patients died on February 6, 2020, but her death wasn’t confirmed as the first American casualty until April 21.
On February 11, 2020, the WHO released a new name for the disease causing the deadly outbreak: Coronavirus Disease 2019 or COVID-19. By mid-March 2020, all 50 U.S. states had reported at least one positive case of COVID-19, and nearly all of the new infections were caused by “community spread,” not by people who contracted the disease while traveling abroad.
At the same time, COVID-19 had spread to 114 countries worldwide, killing more than 4,000 people and infecting hundreds of thousands more. On March 11, the WHO made it official and declared COVID-19 a pandemic.
The World Shuts Down

Pandemics are expected in a globally interconnected world, so emergency plans were in place. In the United States, health officials at the Centers for Disease Control and Prevention (CDC) and the National Institutes of Health (NIH) set in motion a national response plan developed for flu pandemics.
State by state and city by city, government officials took emergency measures to encourage “ social distancing ,” one of the many new terms that became part of the COVID-19 vocabulary. Travel was restricted. Schools and churches were closed. With the exception of “essential workers,” all offices and businesses were shuttered. By early April 2020, more than 316 million Americans were under a shelter-in-place or stay-at-home order.
With more than 1,000 deaths and nearly 100,000 cases, it was clear by April 2020 that COVID-19 was highly contagious and virulent. What wasn’t clear, even to public health officials, was how individuals could best protect themselves from COVID-19. In the early weeks of the outbreak, the CDC discouraged people from buying face masks, because officials feared a shortage of masks for doctors and hospital workers.
By April 2020, the CDC revised its recommendations, encouraging people to wear masks in public, to socially distance and to wash hands frequently. President Donald Trump undercut the CDC recommendations by emphasizing that masking was voluntary and vowing not to wear a mask himself. This was just the beginning of the political divisions that hobbled the COVID-19 response in America.
Global Financial Markets Collapse
In the early months of the COVID-19 pandemic, with billions of people worldwide out of work, stuck at home, and fretting over shortages of essential items like toilet paper , global financial markets went into a tailspin.
In the United States, share prices on the New York Stock Exchange plummeted so quickly that the exchange had to shut down trading three separate times. The Dow Jones Industrial Average eventually lost 37 percent of its value, and the S&P 500 was down 34 percent.
Business closures and stay-at-home orders gutted the U.S. economy. The unemployment rate skyrocketed, particularly in the service sector (restaurant and other retail workers). By May 2020, the U.S. unemployment rate reached 14.7 percent, the highest jobless rate since the Great Depression .
All across America, households felt the pinch of lost jobs and lower wages. Food insecurity reached a peak by December 2020 with 30 million American adults—a full 14 percent—reporting that their families didn’t get enough to eat in the past week.
The economic effects of the COVID-19 pandemic, like its health effects, weren’t experienced equally. Black, Hispanic and Native Americans suffered from unemployment and food insecurity at significantly higher rates than white Americans.
Congress tried to avoid a complete economic collapse by authorizing a series of COVID-19 relief packages in 2020 and 2021, which included direct stimulus checks for all American families.
The Race for a Vaccine
A new vaccine typically takes 10 to 15 years to develop and test, but the world couldn’t wait that long for a COVID-19 vaccine. The U.S. Department of Health and Human Services (HHS) under the Trump administration launched “ Operation Warp Speed ,” a public-private partnership which provided billions of dollars in upfront funding to pharmaceutical companies to rapidly develop vaccines and conduct clinical trials.
The first clinical trial for a COVID-19 vaccine was announced on March 16, 2020, only days after the WHO officially classified COVID-19 as a pandemic. The vaccines developed by Moderna and Pfizer were the first ever to employ messenger RNA, a breakthrough technology. After large-scale clinical trials, both vaccines were found to be greater than 95 percent effective against infection with COVID-19.
A nurse from New York officially became the first American to receive a COVID-19 vaccine on December 14, 2020. Ten days later, more than 1 million vaccines had been administered, starting with healthcare workers and elderly residents of nursing homes. As the months rolled on, vaccine availability was expanded to all American adults, and then to teenagers and all school-age children.
By the end of the pandemic in early 2023, more than 670 million doses of COVID-19 vaccines had been administered in the United States at a rate of 203 doses per 100 people. Approximately 80 percent of the U.S. population received at least one COVID-19 shot, but vaccination rates were markedly lower among Black, Hispanic and Native Americans.
COVID-19 Deaths Heaviest Among Elderly and People of Color
In America, the COVID-19 pandemic impacted everyone’s lives, but those who died from the disease were far more likely to be older and people of color.
Of the more than 1.1 million COVID deaths in the United States, 75 percent were individuals who were 65 or older. A full 93 percent of American COVID-19 victims were 50 or older. Throughout the emergence of COVID-19 variants and the vaccine rollouts, older Americans remained the most at-risk for being hospitalized and ultimately dying from the disease.
Black, Hispanic and Native Americans were also at a statistically higher risk of developing life-threatening COVID-19 systems and succumbing to the disease. For example, Black and Hispanic Americans were twice as likely to be hospitalized from COVID-19 than white Americans. The COVID-19 pandemic shined light on the health disparities between racial and ethnic groups driven by systemic racism and lower access to healthcare.
Mental health also worsened during the COVID-19 pandemic. The anxiety of contracting the disease, and the stresses of being unemployed or confined at home, led to unprecedented numbers of Americans reporting feelings of depression and suicidal ideation.
A Time of Social & Political Upheaval

In the United States, the three long years of the COVID-19 pandemic paralleled a time of heightened political contention and social upheaval.
When George Floyd was killed by Minneapolis police on May 25, 2020, it sparked nationwide protests against police brutality and energized the Black Lives Matter movement. Because so many Americans were out of work or home from school due to COVID-19 shutdowns, unprecedented numbers of people from all walks of life took to the streets to demand reforms.
Instead of banding together to slow the spread of the disease, Americans became sharply divided along political lines in their opinions of masking requirements, vaccines and social distancing.
By March 2024, in signs that the pandemic was waning, the CDC issued new guidelines for people who were recovering from COVID-19. The agency said those infected with the virus no longer needed to remain isolated for five days after symptoms. And on March 10, 2024, the Johns Hopkins Coronavirus Resource Center stopped collecting data for its highly referenced COVID-19 dashboard.
Still, an estimated 17 percent of U.S. adults reported having experienced symptoms of long COVID, according to the Household Pulse Survey. The medical community is still working to understand the causes behind long COVID, which can afflict a patient for weeks, months or even years.
HISTORY Vault
Stream thousands of hours of acclaimed series, probing documentaries and captivating specials commercial-free in HISTORY Vault
“CDC Museum COVID Timeline.” Centers for Disease Control and Prevention . “Coronavirus: Timeline.” U.S. Department of Defense . “COVID-19 and Related Vaccine Development and Research.” Mayo Clinic . “COVID-19 Cases and Deaths by Race/Ethnicity: Current Data and Changes Over Time.” Kaiser Family Foundation . “Number of COVID-19 Deaths in the U.S. by Age.” Statista . “The Pandemic Deepened Fault Lines in American Society.” Scientific American . “Tracking the COVID-19 Economy’s Effects on Food, Housing, and Employment Hardships.” Center on Budget and Policy Priorities . “U.S. Confirmed Country’s First Case of COVID-19 3 Years Ago.” CNN .

Sign up for Inside History
Get HISTORY’s most fascinating stories delivered to your inbox three times a week.
By submitting your information, you agree to receive emails from HISTORY and A+E Networks. You can opt out at any time. You must be 16 years or older and a resident of the United States.
More details : Privacy Notice | Terms of Use | Contact Us
- Skip to main content
- Accessibility help
Information
We use cookies to collect anonymous data to help us improve your site browsing experience.
Click 'Accept all cookies' to agree to all cookies that collect anonymous data. To only allow the cookies that make the site work, click 'Use essential cookies only.' Visit 'Set cookie preferences' to control specific cookies.
Your cookie preferences have been saved. You can change your cookie settings at any time.
Coronavirus (COVID-19) and society: what matters to people in Scotland?
Findings from an open free text survey taken to understand in greater detail how the pandemic has changed Scotland.
- This research has captured the diversity and complexity of people’s experiences.
- People’s experiences of the pandemic and their ability to stay safe has been impacted by a range of factors, including: their geographical environment, their financial situation, profession, their living situation and if they have any physical or mental health conditions.
- Even though the direct level of threat from COVID-19 has reduced (for some people), there is still concern about the longer term harm and disruption that COVID-19 has caused to people and communities, and worry about the threat of future waves of infection.
- This report captures a number of specific suggestions for support. For example, support for key workers, creating safer public environments, wide-scale financial support, greater awareness around the experiences of those who are at higher risk to COVID-19 and putting in place robust processes for learning and reflection on the impact of the pandemic.
- Public engagement in this open and unfiltered format is an essential part of making sense of people’s attitudes and behaviours within the context of their life.
Email: [email protected]
There is a problem
Thanks for your feedback
Your feedback helps us to improve this website. Do not give any personal information because we cannot reply to you directly.
What is COVID-19 and how is it spread?
With nearly 550,000 people infected, almost 25,000 dead, and hundreds of millions in lockdown across the globe, the coronavirus pandemic has brought the world to a standstill. But what do we know about COVID-19 and what can we do to fight this pandemic?
- 27 March 2020
- by Priya Joi
Republish this article
If you would like to republish this article, please follow these steps: use the HTML below; do not edit the text; include the author’s byline; credit VaccinesWork as the original source; and include the page view counter script.
COVID-19 is a serious global infectious disease outbreak with nearly 550,000 cases and around 25,000 deaths worldwide. It is part of a family of viruses called coronaviruses that infect both animals and people. This particular one originated in China at the end of 2019, in the city of Wuhan, which has 11 million residents. In the past two decades coronavirus outbreaks have caused global concern, including one in 2003 with the Severe Acute Respiratory Syndrome (SARS) and more recently in 2012 with the Middle East Respiratory Syndrome (MERS).
COVID-19 can cause symptoms very similar to the flu – fever and a dry cough (the two most common symptoms) , fatigue, aches and pains, and nasal congestion. As the pandemic spread around the world, other symptoms such as a loss of sense of smell or taste have emerged – these are not yet conclusive evidence of infection with the new coronavirus, and the World Health Organization is investigating this.
Severe cases can lead to serious respiratory disease, and even pneumonia. Those most at risk are the elderly, or people with underlying medical issues, such as heart problems or diabetes. According to the most recent global numbers (27 March 2020), 14.8% of people over 80 years old, infected with the virus, have died from it, compared with 0.4% in people aged 40-49% and none in children under 9 years. The situation across countries is rapidly changing and these numbers will continue to change as the pandemic shifts.
Despite most deaths still being in older people, it is clear that many young people with the virus can still develop serious infection that requires hospitalisation.
The evidence so far indicates that the virus is spread from person to person through small respiratory droplets. When a person coughs or sneezes, these droplets can also land on nearby surfaces. There is also evidence that the COVID-19 virus can last on surfaces – especially plastic or metal – for up to 3 days. This is why advice to avoid catching COVID-19 has focused on handwashing with soap, the use of alcohol-based hand sanitising gels and keeping a distance from people who are symptomatic.
While many people can be seen to wear masks, especially on public transport, the World Health Organization (WHO) says that you only need to wear a mask if you are unwell or looking after someone who is sick and is in addition to the important measures above
IS THERE A TREATMENT OR VACCINE?
Right now, there are no antivirals or vaccines to treat or prevent COVID-19, although there are at least 44 potential coronavirus vaccines in development. Several antivirals, including those against flu and HIV are being tested to see if they could be used against the new coronavirus, as is chloroquine, a common antimalarial.
Even in an emergency, vaccines can take a long time to develop – no matter how quickly researchers race through the initial phase of identifying candidate vaccines and getting their vaccines into clinical testing. This is because taking the vaccine through the rigorous stages of testing for safety and efficacy can normally take several years. And it is still unclear whether the COVID-19 outbreak will have peaked before a vaccine can be rolled-out.
HOW BAD IS THIS PANDEMIC?
COVID-19 is a new coronavirus, which means that it is likely no-one has natural immunity to it. Coronaviruses such as MERS-CoV and SARS are on watchlists of infections with pandemic potential, along with Ebola and influenza . Since it began, COVID-19 has spread worldwide, leading the WHO to label it a pandemic and a “public health emergency of international concern.”
Based on available evidence, COVID-19 appears to have a fatality rate of 4.4%, much lower than 10% for SARS and around 30% for MERS-CoV. Yet this is not a reason to relax containment and control measures.
COVID-19 is more contagious than either SARS or MERS-CoV, and crucially, can be spread undetected. This is because many people with COVID-19 are either asymptomatic or have very mild symptoms, so they may not be adequately isolating themselves, and spreading the infection. Most countries around the world are now on lockdown to avoid spreading the virus any further, and allowing “a flattening of the curve” meaning avoiding cases from spiking and overwhelming health systems.
More from Priya Joi

How Africa is moving towards a homegrown response to health emergencies

Nanotechnology vaccines could protect against unknown coronaviruses

Malaria experts call for action on growing drug resistance in Africa

Nearly 7% of Americans struggle with Long COVID as infections surge
Recommended for you.

Could ‘Science Courts’ help build public trust?

Climate change is linked to worsening brain diseases – new study

The Viral Most Wanted: The Retroviruses
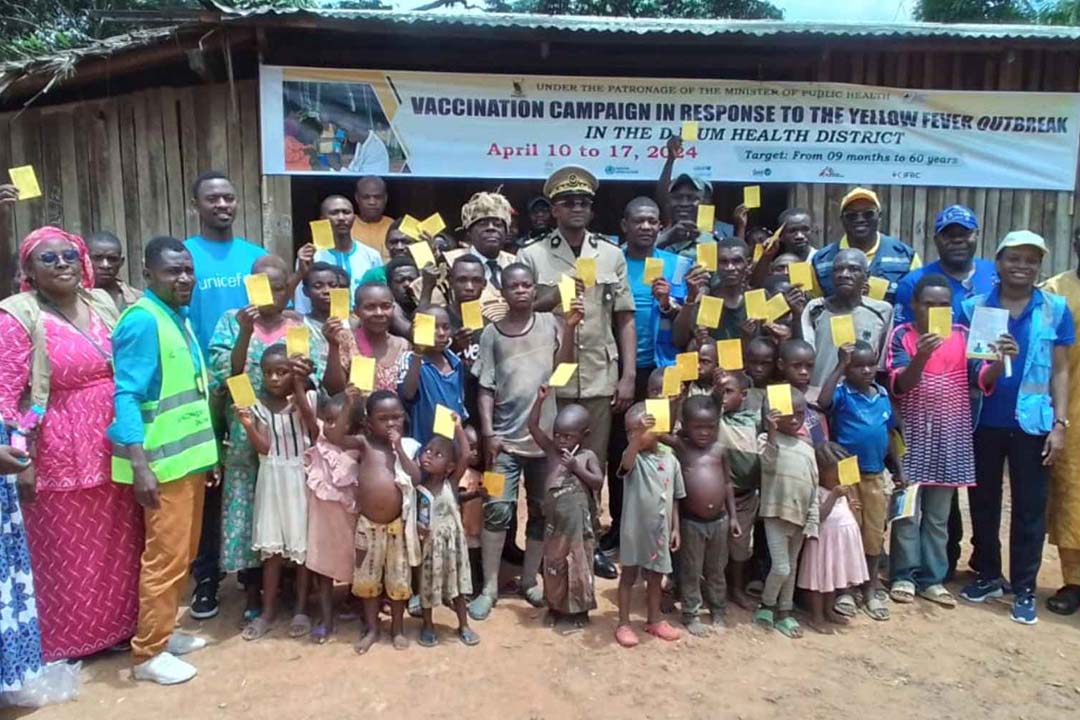
Cameroon hits back at yellow fever

From our brains to our bowels – 5 ways the climate crisis is affecting our health

In Sri Lanka, health workers go the extra mile to keep sex workers safe
Get the latest vaccineswork news, direct to your inbox.
Sign up to receive our top stories and key topics related to vaccination, including those related to the COVID-19 pandemic.
By clicking the "Subscribe" button, you are agreeing to receive the digital newsletter from Gavi, the Vaccine Alliance, agreeing to our terms of use and have read our privacy policy .
Website User Experience Survey
Thank you for visiting our website. Your input and time is valuable in helping us improve your experience. Please take less than a minute to provide feedback on your visit.
Thank you for visiting our website. Your input is important in helping us improve your experience. Please take a moment to answer a few questions about your visit.
- CORONAVIRUS COVERAGE
Here’s what the WHO report found on the origins of COVID-19
The long-awaited report answers some questions. But experts warn that discovering the virus’ true origins will take more digging.
A World Health Organization report released today says that SARS-CoV-2, the virus that causes COVID-19, most likely leapt from animals to humans through an emissary animal.
The dispatch marks the culmination of a month-long mission by a team of Chinese and international experts to uncover COVID-19’s true origins. According to the report, it’s probable the virus originated in a bat or pangolin before making the leap to people. The report also says that it’s “extremely unlikely” the highly transmissible virus escaped from a laboratory in China.
“All hypotheses remain on the table,” Tedros Adhanom Ghebreyesus, the WHO’s director general, said in a statement released today , indicating the organization’s research is ongoing.
While the 120-page report resolves some queries, it leaves others unanswered, including the geographic origin of the virus and exactly how it infected the first human. The methods used to gather physical evidence, as well as the way the report was written and compiled, have also raised alarm bells, causing some experts to question its credibility and to urge for more transparency in future studies.
“This report is a very important beginning, but it is not the end,” Ghebreyesus said, adding that until the source of the virus is found, “we must continue to follow the science and leave no stone unturned as we do.”
Path to infection
Most scientists are not surprised by the report’s conclusion that SARS-CoV-2 most likely jumped from an infected bat or pangolin to another animal and then to a human .
For Hungry Minds
“This is what many of us thought all along,” says Ian Lipkin , director of the Center for Infection and Immunity at Columbia University’s Mailman School of Public Health. But Lipkin adds that it’s “still speculative, because they haven’t identified an intermediary animal.” The report authors suggest examining supply chains from both livestock and wildlife farms to public markets to try and find out exactly which animals were involved.
If an intermediate host is part of the virus’ transmission chain, then it will be important to identify it so that mitigation measures can be put in place to prevent future outbreaks, says Theodora Hatziioannou , an associate professor of virology at Rockefeller University in New York City.
The report outlines another likely transmission scenario: that the virus leapt directly from a bat to a human. Robert Garry , a virologist at Tulane University School of Medicine who has studied the virus’s origin based on its genome, says such an event “is not too big a stretch.”
You May Also Like

Bird flu is spreading from pole to pole. Here’s why it matters.

What is white lung syndrome? Here's what to know about pneumonia

Multiple COVID infections can lead to chronic health issues. Here’s what to know.
However, the report questions whether the Huanan market was the location where the first animal-to-human transmission occurred, as some believed. The earliest reported case of COVID-19 did not have any link to the market. That suggests no firm conclusion can be drawn yet about the role of the Huanan market in the origin of the outbreak, or how the infection might have been introduced there, according to the report.
The hypothesis that frozen foods packaged and sold in markets might have played a role in SARS-CoV-2 transmission was also addressed. The report authors determined this so-called cold-chain route was possible and called for further case-control studies of outbreaks involving frozen products. They also recommended examining cold-chain products sold in the Huanan market from December 2019—if any are still available.
The report concludes that it was “extremely unlikely” the virus leaked from a Wuhan laboratory, a hypothesis propagated by former president Donald Trump but not often entertained by scientists. Robert Redfield, the former director of the Centers for Disease Control and Prevention, continued to spread the idea as recently as last week during a CNN interview .
“There is no record of viruses closely related to SARS-CoV-2 in any laboratory” before the first cases of COVID-19 were recorded in December 2019, the WHO report says, with the authors adding that the risk of accidentally introducing the novel coronavirus in a laboratory setting by infecting a human “is extremely low.” The report does not call for additional research into the possibility of a leak from one of Wuhan’s laboratories.
“The preliminary conclusions are not outrageous, and they make perfect sense,” Hatziioannou says. “I know a lot of people would like to think it escaped from the lab, but I find conspiracy theories like that extremely hard to believe.”
Setbacks and scrutiny
However, the report is already facing scrutiny. Although it’s a joint effort between Chinese and WHO officials, investigators representing the WHO were denied permission to visit the Wuhan market and collect other data in the initial phases of the research, leading some pundits to say that the WHO was ceding responsibility to China, its second biggest funder behind the United States.
China also held back information about the initial outbreak in Wuhan, which delayed the WHO’s investigation.
Today, a joint statement issued by the governments of 14 countries, including the U.S., raised concerns about the transparency of future research into the origins of the novel virus.
“It is critical for independent experts to have full access to all pertinent human, animal, and environmental data, research, and personnel involved in the early stages of the outbreak relevant to determining how this pandemic emerge,” the statement reads.
Despite the study’s setbacks, Tulane University’s Garry believes the WHO report is credible. “It’s a very detailed report—it’s not the type of data you can make up,” he says.
Lipkin agrees: “It’s thorough, it’s exhaustive, it’s well written,” he says. “It’s what we predicted. That’s not to say that it wasn’t important to do this, but there’s nothing here to say, Ah-ha, I never thought this would be the case.”
Related Topics
- CORONAVIRUS
- PUBLIC HEALTH
- ANIMAL DISEASES


Do bats take flight during a solar eclipse? Here’s what we learned.

COVID-19 is more widespread in animals than we thought

A deer may have passed COVID-19 to a person, study suggests

A mysterious new respiratory illness is spreading in dogs. Here’s what we know.

$1,500 for 'naturally refined' coffee? Here's what that phrase really means.
- Environment
- Perpetual Planet
History & Culture
- History & Culture
- History Magazine
- Mind, Body, Wonder
- Paid Content
- Terms of Use
- Privacy Policy
- Your US State Privacy Rights
- Children's Online Privacy Policy
- Interest-Based Ads
- About Nielsen Measurement
- Do Not Sell or Share My Personal Information
- Nat Geo Home
- Attend a Live Event
- Book a Trip
- Inspire Your Kids
- Shop Nat Geo
- Visit the D.C. Museum
- Learn About Our Impact
- Support Our Mission
- Advertise With Us
- Customer Service
- Renew Subscription
- Manage Your Subscription
- Work at Nat Geo
- Sign Up for Our Newsletters
- Contribute to Protect the Planet
Copyright © 1996-2015 National Geographic Society Copyright © 2015-2024 National Geographic Partners, LLC. All rights reserved
- Open access
- Published: 04 February 2022
Analysis of the COVID-19 pandemic: lessons towards a more effective response to public health emergencies
- Yibeltal Assefa ORCID: orcid.org/0000-0003-2393-1492 1 ,
- Charles F. Gilks 1 ,
- Simon Reid 1 ,
- Remco van de Pas 2 ,
- Dereje Gedle Gete 1 &
- Wim Van Damme 2
Globalization and Health volume 18 , Article number: 10 ( 2022 ) Cite this article
39k Accesses
35 Citations
10 Altmetric
Metrics details
The pandemic of Coronavirus Disease 2019 (COVID-19) is a timely reminder of the nature and impact of Public Health Emergencies of International Concern. As of 12 January 2022, there were over 314 million cases and over 5.5 million deaths notified since the start of the pandemic. The COVID-19 pandemic takes variable shapes and forms, in terms of cases and deaths, in different regions and countries of the world. The objective of this study is to analyse the variable expression of COVID-19 pandemic so that lessons can be learned towards an effective public health emergency response.
We conducted a mixed-methods study to understand the heterogeneity of cases and deaths due to the COVID-19 pandemic. Correlation analysis and scatter plot were employed for the quantitative data. We used Spearman’s correlation analysis to determine relationship strength between cases and deaths and socio-economic and health systems. We organized qualitative information from the literature and conducted a thematic analysis to recognize patterns of cases and deaths and explain the findings from the quantitative data.
We have found that regions and countries with high human development index have higher cases and deaths per million population due to COVID-19. This is due to international connectedness and mobility of their population related to trade and tourism, and their vulnerability related to older populations and higher rates of non-communicable diseases. We have also identified that the burden of the pandemic is also variable among high- and middle-income countries due to differences in the governance of the pandemic, fragmentation of health systems, and socio-economic inequities.
The COVID-19 pandemic demonstrates that every country remains vulnerable to public health emergencies. The aspiration towards a healthier and safer society requires that countries develop and implement a coherent and context-specific national strategy, improve governance of public health emergencies, build the capacity of their (public) health systems, minimize fragmentation, and tackle upstream structural issues, including socio-economic inequities. This is possible through a primary health care approach, which ensures provision of universal and equitable promotive, preventive and curative services, through whole-of-government and whole-of-society approaches.
The pandemic of Coronavirus Disease 2019 (COVID-19) is a timely reminder of the nature and impact of emerging infectious diseases that become Public Health Emergency of International Concern (PHEIC) [ 1 ]. The COVID-19 pandemic takes variable shapes and forms in how it affects communities in different regions and countries [ 2 , 3 ]. As of 12 January, 2022, there were over 314 million cases and over 5.5 million deaths notified around the globe since the start of the pandemic. The number of cases per million population ranged from 7410 in Africa to 131,730 in Europe while the number of deaths per million population ranged from 110 in Oceania to 2740 in South America. Case-fatality rates (CFRs) ranged from 0.3% in Oceania to 2.9% in South America [ 4 , 5 ]. Regions and countries with high human development index (HDI), which is a composite index of life expectancy, education, and per capita income indicators [ 6 ], are affected by COVID-19 more than regions with low HDI. North America and Europe together account for 55 and 51% of cases and deaths, respectively. Regions with high HDI are affected by COVID-19 despite their high universal health coverage index (UHCI) and Global Health Security index (GHSI) [ 7 ].
This seems to be a paradox (against the established knowledge that countries with weak (public) health systems capacity will have worse health outcomes) in that the countries with higher UHCI and GHSI have experienced higher burdens of COVID-19 [ 7 ]. The paradox can partially be explained by variations in testing algorithms, capacity for testing, and reporting across different countries. Countries with high HDI have health systems with a high testing capacity; the average testing rate per million population is less than 32, 000 in Africa and 160,000 in Asia while it is more than 800, 000 in HICs (Europe and North America). This enables HICs to identify more confirmed cases that will ostensibly increase the number of reported cases [ 3 ]. Nevertheless, these are insufficient to explain the stark differences between countries with high HDI and those with low HDI. Many countries with high HDI have a high testing rate and a higher proportion of symptomatic and severe cases, which are also associated with higher deaths and CFRs [ 7 ]. On the other hand, there are countries with high HDI that sustain a lower level of the epidemic than others with a similar high HDI. It is, therefore, vital to analyse the heterogeneity of the COVID-19 pandemic and explain why some countries with high HDI, UHCI and GHSI have the highest burden of COVID-19 while others are able to suppress their epidemics and mitigate its impacts.
The objective of this study was to analyse the COVID-19 pandemic and understand its variable expression with the intention to learn lessons for an effective and sustainable response to public health emergencies. We hypothesised that high levels of HDI, UHCI and GHSI are essential but not sufficient to prevent and control COVID-19.
We conducted an explanatory mixed-methods study to understand and explain the heterogeneity of the pandemic around the world. The study integrated quantitative and qualitative secondary data. The following steps were included in the research process: (i) collecting and analysing quantitative epidemiological data, (ii) conducting literature review of qualitative secondary data and (iii) evaluating countries’ pandemic responses to explain the variability in the COVID-19 epidemiological outcomes. The study then illuminated specific factors that were vital towards an effective and sustainable epidemic response.
We used the publicly available secondary data sources from Johns Hopkins University ( https://coronavirus.jhu.edu/data/new-cases ) for COVID-19 and UNDP 2020 HDI report ( http://hdr.undp.org/en/2019-report ) for HDI, demographic and epidemiologic variables. These are open data sources which are regularly updated and utilized by researchers, policy makers and funders. We performed a correlation analysis of the COVID-19 pandemic. We determined the association between COVID-19 cases, severity, deaths and CFRs at the 0.01 and 0.05 levels (2-tailed). We used Spearman’s correlation analysis, as there is no normal distribution of the variables [ 8 ].
The UHCI is calculated as the geometric mean of the coverage of essential services based on 17 tracer indicators from: (1) reproductive, maternal, newborn and child health; (2) infectious diseases; (3) non-communicable diseases; and, (4) service capacity and access and health security [ 9 ]. The GHSI is a composite measure to assess a country’s capability to prevent, detect, and respond to epidemics and pandemics [ 10 ].
We then conducted a document review to explain the epidemic patterns in different countries. Secondary data was obtained from peer-reviewed journals, reputable online news outlets, government reports and publications by public health-related associations, such as the WHO. To explain the variability of COVID-19 across countries, a list of 14 indicators was established to systematically assess country’s preparedness, actual pandemic response, and overall socioeconomic and demographic profile in the context of COVID-19. The indicators used in this study include: 1) Universal Health Coverage Index, 2) public health capacity, 3) Global Health Security Index, 4) International Health Regulation, 5) leadership, governance and coordination of response, 6) community mobilization and engagement, 7) communication, 8) testing, quarantines and social distancing, 9) medical services at primary health care facilities and hospitals, 10) multisectoral actions, 11) social protection services, 12) absolute and relative poverty status, 13) demography, and 14) burden of communicable and non-communicable diseases. These indicators are based on our previous studies and recommendation from the World Health Organization [ 3 , 4 ]. We conducted thematic analysis and synthesis to identify the factors that may explain the heterogeneity of the pandemic.
Heterogeneity of COVID-19 cases and deaths around the world: what can explain it?
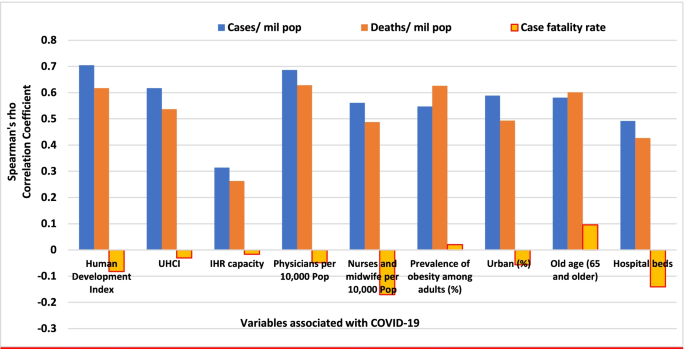
Table 1 indicates that the pandemic of COVID-19 is heterogeneous around regions of the world. Figure 1 also shows that there is a strong and significant correlation between HDI and globalisation (with an increase in trade and tourism as proxy indicators) and a corresponding strong and significant correlation with COVID-19 burden.
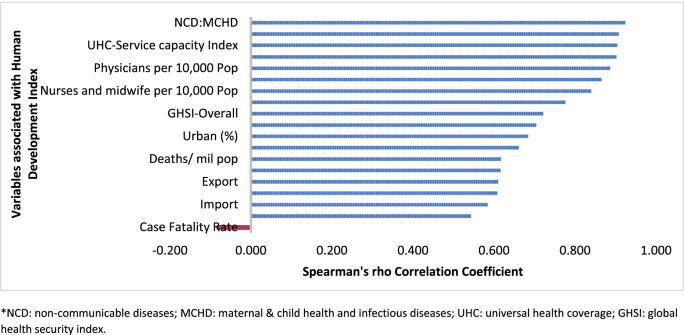
Human development index and its correlates associated with COVID-19 in 189 countries*
Globalisation and pandemics interact in various ways, including through international trade and mobility, which can lead to multiple waves of infections [ 11 ]. In at least the first waves of the pandemic, countries with high import and export of consumer goods, food products and tourism have high number of cases, severe cases, deaths and CFRs. Countries with high HDI are at a higher risk of importing (and exporting) COVID-19 due to high mobility linked to trade and tourism, which are drivers of the economy. These may have led to multiple introductions of COVID-19 into these countries before border closures.
The COVID-19 pandemic was first identified in China, which is central to the global network of trade, from where it spread to all parts of the world, especially those countries with strong links with China [ 12 ]. The epidemic then spread to Europe. There is very strong regional dimension to manufacturing and trading, which could be facilitate the spread of the virus. China is the heart of ‘Factory Asia’; Italy is in the heart of ‘Factory Europe’; the United States is the heart of ‘Factory North America’; and Brazil is the heart of ‘Factory Latin America’ [ 13 ]. These are the countries most affected by COVID-19 during the first wave of the pandemic [ 2 , 3 , 14 ].
It is also important to note that two-third of the countries currently reporting more than a million cases are middle-income countries (MICs), which are not only major emerging market economies but also regional political powers, including the BRICS countries (Brazil, Russia, India and South Africa) [ 3 , 15 ]. These countries participate in the global economy, with business travellers and tourists. They also have good domestic transportation networks that facilitate the internal spread of the virus. The strategies that helped these countries to become emerging markets also put them at greater risk for importing and spreading COVID-19 due to their connectivity to the rest of the world.
In addition, countries with high HDI may be more significantly impacted by COVID-19 due to the higher proportion of the elderly and higher rates of non-communicable diseases. Figure 1 shows that there is a strong and significant correlation between HDI and demographic transition (high proportion of old-age population) and epidemiologic transition (high proportion of the population with non-communicable diseases). Countries with a higher proportion of people older than 65 years and NCDs (compared to communicable diseases) have higher burden of COVID-19 [ 16 , 17 , 18 , 19 , 20 ]. Evidence has consistently shown a higher risk of severe COVID-19 in older individuals and those with underlying health conditions [ 21 , 22 , 23 , 24 , 25 ]. CFR is age-dependent; it is highest in persons aged ≥85 years (10 to 27%), followed by those among persons aged 65–84 years (3 to 11%), and those among persons aged 55-64 years (1 to 3%) [ 26 ].
On the other hand, regions and countries with low HDI have, to date, experienced less severe epidemics. For instance, as of January 12, 2022, the African region has recorded about 10.3 million cases and 233,000 deaths– far lower than other regions of the world (Table 1 ) [ 27 ]. These might be due to lower testing rates in Africa, where only 6.5% of the population has been tested for the virus [ 14 , 28 ], and a greater proportion of infections may remain asymptomatic [ 29 ]. Indeed, the results from sero-surveys in Africa show that more than 80% of people infected with the virus were asymptomatic compared to an estimated 40-50% asymptomatic infections in HICs [ 30 , 31 ]. Moreover, there is a weak vital registration system in the region indicating that reports might be underestimating and underreporting the disease burden [ 32 ]. However, does this fully explain the differences observed between Africa and Europe or the Americas?
Other possible factors that may explain the lower rates of cases and deaths in Africa include: (1) Africa is less internationally connected than other regions; (2) the imposition of early strict lockdowns in many African countries, at a time when case numbers were relatively small, limited the number of imported cases further [ 2 , 33 , 34 ]; (3) relatively poor road network has also limited the transmission of the virus to and in rural areas [ 35 ]; (4) a significant proportion of the population resides in rural areas while those in urban areas spend a lot of their time mostly outdoors; (5) only about 3% of Africans are over the age of 65 (so only a small proportion are at risk of severe COVID-19) [ 36 ]; (6) lower prevalence of NCDs, as disease burden in Africa comes from infectious causes, including coronaviruses, which may also have cross-immunity that may reduce the risk of developing symptomatic cases [ 37 ]; and (7) relative high temperature (a major source of vitamin D which influences COVID-19 infection and mortality) in the region may limit the spread of the virus [ 38 , 39 ]. We argue that a combination of all these factors might explain the lower COVID-19 burden in Africa.
The early and timely efforts by African leaders should not be underestimated. The African Union, African CDC, and WHO convened an emergency meeting of all African ministers of health to establish an African taskforce to develop and implement a coordinated continent-wide strategy focusing on: laboratory; surveillance; infection prevention and control; clinical treatment of people with severe COVID-19; risk communication; and supply chain management [ 40 ]. In April 2021, African Union and Africa CDC launched the Partnerships for African Vaccine Manufacturing (PAVM), framework to expanding Africa’s vaccine manufacturing capacity for health security [ 41 ].
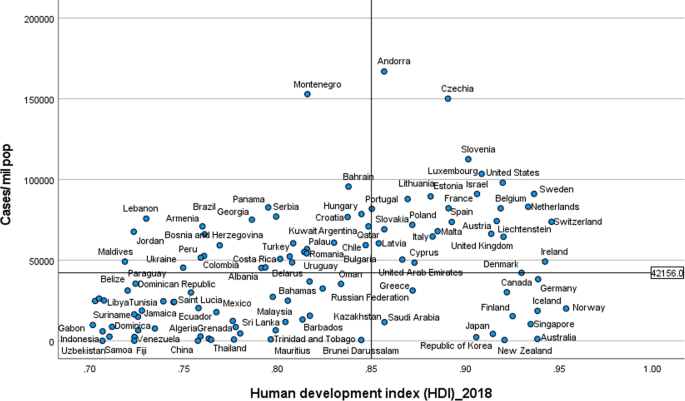
Heterogeneity of the pandemic among countries with high HDI: what can explain it?
Figures 2 and 3 illustrate the variability of cases and deaths due to the COVID-19 pandemic across high-income countries (HICs). Contrary to the overall positive correlation between high HDI and cases, deaths and fatality rates due to COVID-19, there are outlier HICs, which have been able to control the epidemic. Several HICs, such as New Zealand, Australia, South Korea, Japan, Denmark, Iceland, and Norway, managed to contain their epidemics (Figs. 2 and 3 ) [ 15 , 42 , 43 ]. It is important to note that most of these countries (especially the island states) have far less cross-border mobility than other HICs.
Scatter plot of COVID-19 cases per million population in countries with high human development index (> 0.70)
Scatter plot of COVID-19 deaths per million population in countries with high human development index (> 0.70)
HICs that have been successful at controlling their epidemics have similar characteristics, which are related to governance of the response [ 44 ], synergy between UHC and GHS, and existing relative socio-economic equity in the country. Governance and leadership is a crucial factor to explain the heterogeneity of the epidemic among countries with high HDI [ 45 ]. There has been substantial variation in the nature and timing of the public health responses implemented [ 46 ]. Adaptable and agile governments seem better able to respond to their epidemics [ 47 , 48 ]. Countries that have fared the best are the ones with good governance and public support [ 49 ]. Countries with an absence of coherent leadership and social trust have worse outcomes than countries with collective action, whether in a democracy or autocracy, and rapid mobilisation of resources [ 50 ]. The erosion of trust in the United States government has hurt the country’s ability to respond to the COVID-19 crisis [ 51 , 52 ]. The editors of the New England Journal of Medicine argued that the COVID-19 crisis has produced a test of leadership; but, the leaders in the United States had failed that test [ 47 ].
COVID-19 has exposed the fragility of health systems, not only in the public health and primary care, but also in acute and long-term care systems [ 49 ]. Fragmentation of health systems, defined here to mean inadequate synergy and/ or integration between GHS and UHC, is typical of countries most affected by the COVID-19 pandemic. Even though GHS and UHC agendas are convergent and interdependent, they tend to have different policies and practices [ 53 ]. The United States has the highest index for GHS preparedness; however, it has reported the world’s highest number of COVID-19 cases and deaths due to its greatly fragmented health system [ 54 , 55 ]. Countries with health systems and policies that are able to integrate International Health Regulations (IHR) core capacities with primary health care (PHC) services have been effective at mitigating the effects of COVID-19 [ 50 , 53 ]. Australia has been able to control its COVID-19 epidemic through a comprehensive primary care response, including protection of vulnerable people, provision of treatment and support services to affected people, continuity of regular healthcare services, protection and support of PHC workers and primary care services, and provision of mental health services to the community and the primary healthcare workforce [ 56 ]. Strict implementation of public health and social intervention together with UHC systems have ensured swift control of the epidemics in Singapore, South Korea, and Thailand [ 57 ].
The heterogeneity of cases and deaths, due to COVID-19, is also explained by differences in levels of socio-economic inequalities, which increase susceptibility to acquiring the infection and disease progression as well as worsening of health outcomes [ 58 ]. COVID-19 has been a stress test for public services and social protection systems. There is a higher burden of COVID-19 in Black, Asian and Minority Ethnic individuals due to socio-economic inequities in HICs [ 59 , 60 ]. Poor people are more likely to live in overcrowded accommodation, are more likely to have unstable work conditions and incomes, have comorbidities associated with poverty and precarious living conditions, and reduced access to health care [ 59 ].
The epidemiology of COVID-19 is also variable across MICs, with HDI between 0.70 and 0.85, around the world. Overall, the epidemic in MICs is exacerbated by the rapid demographic and epidemiologic transitions as well as high prevalence of obesity. While India and Brazil witnessed rapidly increasing rates of cases and deaths, China, Thailand, Vietnam have experienced a relatively lower disease burden [ 15 ]. This heterogeneity may be attributed to a number of factors, including governance, communication and service delivery. Thailand, China and Vietnam have implemented a national harmonized strategic response with decentralized implementation through provincial and district authorities [ 61 ]. Thailand increased its testing capacity from two to over 200 certified facilities that could process between 10,000 to 100,000 tests per day; moreover, over a million village health volunteers in Thailand supported primary health services [ 62 , 63 ]. China’s swift and decisive actions enabled the country to contain its epidemic though there was an initial delay in detecting the disease. China has been able to contain its epidemic through community-based measures, very high public cooperation and social mobilization, strategic lockdown and isolation, multi-sector action [ 64 ]. Overall, multi-level governance (effective and decisive leadership and accountability) of the response, together with coordination of public health and socio-economic services, and high levels of citizen adherence to personal protection, have enabled these countries to successfully contain their epidemics [ 61 , 65 , 66 ].
On the other hand, the Brazilian leadership was denounced for its failure to establish a national surveillance network early in the pandemic. In March 2020, the health minister was reported to have stated that mass testing was a waste of public funding, and to have advised against it [ 67 ]. This was considered as a sign of a collapse of public health leadership, characterized by ignorance, neoliberal authoritarianism [ 68 ]. There were also gaps in the public health capacity in different municipalities, which varied greatly, with a considerable number of Brazilian regions receiving less funding from the federal government due to political tension [ 69 ]. The epidemic has a disproportionate adverse burden on states and municipalities with high socio-economic vulnerability, exacerbated by the deep social and economic inequalities in Brazil [ 70 ].
India is another middle-income country with a high burden of COVID-19. It was one of the countries to institute strict measures in the early phase of the pandemic [ 71 , 72 ]. However, the government eased restrictions after the claim that India had beaten the pandemic, which lead to a rapid increase in disease incidence. Indeed, on 12 January 2022, India reported 36 million cumulative cases and almost 485,000 total deaths [ 15 ]. The second wave of the epidemic in India exposed weaknesses in governance and inadequacies in the country’s health and other social systems [ 73 ]. The nature of the Indian federation, which is highly centripetal, has prevented state and local governments from tailoring a policy response to suit local needs. A centralized one-size-fits-all strategy has been imposed despite high variations in resources, health systems capacity, and COVID-19 epidemics across states [ 74 ]. There were also loose social distancing and mask wearing, mass political rallies and religious events [ 75 ]. Rapid community transmission driven by high population density and multigenerational households has been a feature of the current wave in India [ 76 ]. In addition, several new variants of the virus, including the UK (B.1.1.7), the South Africa (20H/501Y or B.1.351), and Brazil (P.1), alongside a newly identified Indian variant (B.1.617), are circulating in India and have been implicated as factors in the second wave of the pandemic [ 75 , 76 ].
Heterogeneity of case-fatality rates around the world: what can explain it?
The pandemic is characterized by variable CFRs across regions and countries that are negatively associated with HDI (Fig. 1 ). The results presented in Fig. 4 show that the proportion of elderly population and rate of obesity are important factors which are positively associated with CFR. On the other hand, UHC, IHR capacity and other indicators of health systems capacity (health workforce density and hospital beds) are negatively associated with the CFR (Figs. 1 and 4 ).
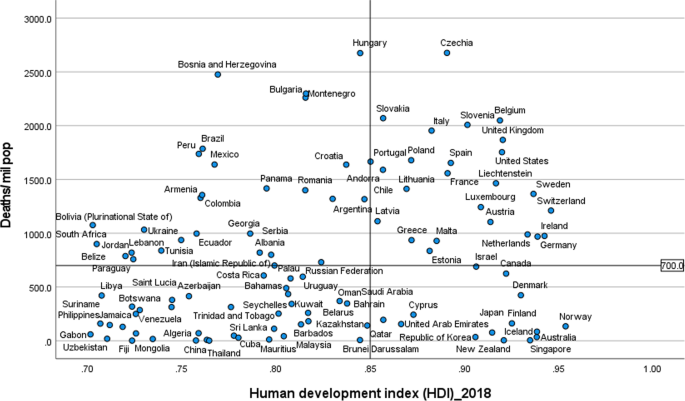
Correlates of COVID-19 cases, deaths and case-fatality rates in 189 countries
The evidence from several research indicates that heterogeneity can be explained by several factors, including differences in age-pyramid, socio-economic status, access to health services, or rates of undiagnosed infections. Differences in age-pyramid may explain some of the observed variation in epidemic severity and CFR between countries [ 77 ]. CFRs across countries look similar when taking age into account [ 78 ]. The elderly and other vulnerable populations in Africa and Asia are at a similar risk as populations in Europe and Americas [ 79 ]. Data from European countries suggest that as high as 57% of all deaths have happened in care homes and many deaths in the US have also occurred in nursing homes. On the other hand, in countries such as Mexico and India, individuals < 65 years contributed the majority of deaths [ 80 ].
Nevertheless, CFR also depends on the quality of hospital care, which can be used to judge the health system capacity, including the availability of healthcare workers, resources, and facilities, which affects outcomes [ 81 ]. The CFR can increase if there is a surge of infected patients, which adds to the strain on the health system [ 82 ]. COVID-19 fatality rates are affected by numerous health systems factors, including bed capacity, existence and capacity of intensive care unit (ICU), and critical care resources (such as oxygen and dexamethasone) in a hospital. Regions and countries with high HDI have a greater number of acute care facilities, ICU, and hospital bed capacities compared to lower HDI regions and countries [ 83 ]. Differences in health systems capacity could explain why North America and Europe, which have experienced much greater number of cases and deaths per million population, reported lower CFRs than the Southern American and the African regions, partly also due to limited testing capacity in these regions (Table 1 ) [ 84 , 85 , 86 ]. The higher CFR in Southern America can be explained by the relatively lower health systems surge capacity that could not adequately respond to the huge demand for health services [ 69 , 86 ]. The COVID-19 pandemic has highlighted existing health systems’ weaknesses, which are not able to effectively prepare for and respond to PHEs [ 87 ]. The high CFRs in the region are also exacerbated by the high social inequalities [ 69 ].
On the other hand, countries in Asia recorded lower CFRs (~ 1.4%) despite sharing many common risk factors (including overcrowding and poverty, weak health system capacity etc) with Africa. The Asian region shares many similar protective factors to the African region. They have been able to minimize their CFR by suppressing the transmission of the virus and flattening the epidemic curve of COVID-19 cases and deaths. Nevertheless, the epidemic in India is likely to be different because it has exceeded the health system capacity to respond and provide basic medical care and medical supplies such as oxygen [ 88 ]. Overall, many Asian countries were able to withstand the transmission of the virus and its effect due to swift action by governments in the early days of the pandemic despite the frequency of travel between China and neighbouring countries such as Hong Kong, Taiwan and Singapore [ 89 ]. This has helped them to contain the pandemic to ensure case numbers remain within their health systems capacity. These countries have benefited from their experience in the past in the prevention and control of epidemics [ 90 ].
There are a number of issues with the use of the CFR to compare the management of the pandemic between countries and regions [ 91 ], as it does not depict the true picture of the mortality burden of the pandemic. A major challenge with accurate calculation of the CFR is the denominator on number of identified cases, as asymptomatic infections and patients with mild symptoms are frequently left untested, and therefore omitted from CFR calculations. Testing might not be widely available, and proactive contact tracing and containment might not be employed, resulting in a smaller denominator, and skewing to a higher CFR [ 82 ]. It is, therefore, far more relevant to estimate infection fatality rate (IFR), the proportion of all infected individuals who have died due to the infection [ 91 ], which is central to understanding the public health impact of the pandemic and the required policies for its prevention and control [ 92 ].
Estimates of prevalence based on sero-surveys, which includes asymptomatic and mildly symptomatic infections, can be used to estimate IFR [ 93 ]. In a systematic review of 17 studies, seroprevalence rates ranged from 0.22% in Brazil to 53% in Argentina [ 94 ]. The review also identified that the seroprevalence estimate was higher than the cumulative reported case incidence, by a factor between 1.5 times in Germany to 717 times in Iran, in all but two studies (0.56 times in Brazil and 0.88 times in Denmark) [ 94 , 95 ]. The difference between seroprevalence and cumulative reported cases might be due to asymptomatic cases, atypical or pauci-symptomatic cases, or the lack of access to and uptake of testing [ 94 ]. There is only a modest gap between the estimated number of infections from seroprevalence surveys and the cumulative reported cases in regions with relatively thorough symptom-based testing. Much of the gap between reported cases and seroprevalence is likely to be due to undiagnosed symptomatic or asymptomatic infections [ 94 ].
Collateral effects of the COVID-19 pandemic
It is important to note that the pandemic has significant collateral effects on the provision of essential health services, in addition to the direct health effects [ 96 ]. Disruptions in the provision of essential health services, due to COVID-19, were reported by nearly all countries, though it is more so in lower-income than higher-income countries [ 97 , 98 ]. The biggest impact reported is on provision of day-to-day primary care to prevent and manage some of the most common health problems [ 99 ].
The causes of disruptions in service delivery were a mix of demand and supply factors [ 100 ]. Countries reported that just over one-third of services were disrupted due to health workforce-related reasons (the most common causes of service disruptions), supply chains, community mistrust and fears of becoming infected, and financial challenge s[ 101 ]. Cognizant of the disruptive effects of the pandemic, countries have reorganized their health system.
Countries with better response to COVID-19 have mobilized, trained and reallocated their health workforce in addition to hiring new staff, using volunteers and medical trainees and mobilizing retirees [ 102 ]. Several strategies have also been implemented to mitigate disruptions in service delivery and utilization, including: triaging to identify the most urgent patient needs, and postponing elective medical procedures; switching to alternative models of care, such as providing more home-based care and telemedicine [ 101 ].
This study identifies that the COVID-19 pandemic, in terms f cases and deaths, is heterogeneous around the world. This variability is explained by differences in vulnerability, preparedness, and response. It confirms that a high level of HDI, UHCI and GHSI are essential but not sufficient to control epidemics [ 103 ]. An effective response to public health emergencies requires a joint and reinforcing implementation of UHC, health emergency and disease control priorities [ 104 , 105 ], as well as good governance and social protection systems [ 106 ]. Important lessons have been learned to cope better with the COVID-19 pandemic and future emerging or re-emerging pandemics. Countries should strengthen health systems, minimize fragmentation of public health, primary care and secondary care, and improve coordination with other sectors. The pandemic has exposed the health effects of longstanding social inequities, which should be addressed through policies and actions to tackle vulnerability in living and working conditions [ 106 ].
The shift in the pandemic epicentre from high-income to MICs was observed in the second global wave of the pandemic. This is due to in part to the large-scale provision of vaccines in HICs [ 15 ] as well as the limitations in the response in LMICs, including inadequate testing, quarantine and isolation, contact tracing, and social distancing. The second wave of the pandemic in low- and middle-income countries spread more rapidly than the first wave and affected younger and healthier populations due to factors, including poor government decision making, citizen behaviour, and the emergence of highly transmissible SARS-CoV-2 variants [ 107 ]. It has become catastrophic in some MICs to prematurely relax key public health measures, such as mask wearing, physical distancing, and hand hygiene [ 108 ].
There is consensus that global vaccination is essential to ending the pandemic. Universal and equitable vaccine delivery, implemented with high volume, speed and quality, is vital for an effective and sustainable response to the current pandemic and future public health emergencies. There is, however, ongoing concern regarding access to COVID-19 vaccines in low-income countries [ 109 ]. Moreover, there is shortage of essential supplies, including oxygen, which has had a major impact on the prevention and control of the pandemic. It is, therefore, vital to transform (through good governance and financing mechanisms) the ACT-A platform to deliver vaccines, therapeutics, diagnostics, and other essential supplies [ 109 , 110 ]. The global health community has the responsibility to address these inequalities so that we can collectively end the pandemic [ 107 ].
The Omicron variant has a huge role in the current wave around the world despite high vaccine coverage [ 111 ]. Omicron appears to spread rapidly around the world ever since it was identified in November 2021 [ 112 ]. It becomes obvious that vaccination alone is inadequate for controlling the infection. This has changed our understanding of the COVID-19 pandemic endgame. The emergence of new variants of concern and their spread around the world has highlighted the importance of combination prevention, including high vaccination coverage in combination with other public health prevention measures [ 112 ].
Overall, the COVID-19 pandemic and the response to it emphasise valuable lessons towards an effective and sustainable response to public health emergencies. We argue that the PHC approach captures the different preparedness and response strategies required towards ensuring health security and UHC [ 113 ]. The PHC approach enables countries to progressively realize universal access to good-quality health services (including essential public health functions) and equity, empower people and communities, strengthen multi-sectoral policy and action for health, and enhance good governance [ 114 ]. These are essential in the prevention and control of public health emergencies, to suppress transmission, and reduce morbidity and mortality [ 115 ]. Access to high-quality primary care is at the foundation of any strong health system [ 116 ], which will, in turn, have effect on containing the epidemic, and reducing mortality and CFR [ 117 ]. Australia is a good example in this regard because it has implemented a comprehensive PHC approach in combination with border restrictions to ensure health system capacity is not exceeded [ 56 ]. The PHC approach will enable countries to develop and implement a context-specific health strategy, enhance governance, strengthen their (public) health systems, minimize segmentation and fragmentation, and tackle upstream structural issues, including discrimination and socio-economic inequities [ 118 ]. This is the type of public health approach (comprehensive, equity-focused and participatory) that will be effective and sustainable to tackle public health emergencies in the twenty-first century [ 119 , 120 ]. In addition, it is vital to transform the global and regional health systems, with a strong IHR and an empowered WHO at the apex [ 121 ]. We contend that this is the way towards a healthier and safer country, region and world.
The COVID-19 pandemic demonstrates that the world remains vulnerable to public health emergencies with significant health and other socio-economic impacts. The pandemic takes variable shapes and forms across regions and countries around the world. The pandemic has impacted countries with inadequate governance of the epidemic, fragmentation of their health systems and higher socio-economic inequities more than others. We argue that adequate response to public health emergencies requires that countries develop and implement a context-specific national strategy, enhance governance of public health emergency, build the capacity of their health systems, minimize fragmentation, and tackle socio-economic inequities. This is possible through a PHC approach that provides universal access to good-quality health services through empowered communities and multi-sectoral policy and action for health development. The pandemic has affected every corner of the world; it has demonstrated that “no country is safe unless other countries are safe”. This should be a call for a strong global health system based on the values of justice and capabilities for health.
Availability of data and materials
Data are available in a public, open access repository: Johns Hopkins University: https://coronavirus.jhu.edu/data/new-cases , and UNDP: http://hdr.undp.org/en/2019-report ; WHO: https://www.who.int/publications/m/item/weekly-epidemiological-update%2D%2D-22-december-2020
Abbreviations
Coronavirus Disease 2019
Case-fatality rates
Human development index
Universal health coverage index
Global Health Security index
High-income countries
Middle-income countries
El Zowalaty ME, Järhult JD. From SARS to COVID-19: A previously unknown SARS-CoV-2 virus of pandemic potential infecting humans–Call for a One Health approach. One Health. 2020;9:100124. https://doi.org/10.1016/j.onehlt.2020.100124 .
Van Damme W, Dahake R, Delamou A, Ingelbeen B, Wouters E, Vanham G, et al. The COVID-19 pandemic: diverse contexts; different epidemics—how and why? BMJ Glob Health. 2020;5(7):e003098.
Article PubMed Google Scholar
World Health Organization (WHO): Coronavirus disease ( COVID-19): situation report, 150. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200618-covid-19-sitrep-150.pdf .
Weekly epidemiological update - 22 December 2020 [ https://www.who.int/publications/m/item/weekly-epidemiological-update%2D%2D-22-december-2020 ].
Worldometer: COVID-19 coronavirus pandemic. 2020. https://www.worldometers.info/coronavirus/ .
Anand S, Sen A. Human Development Index: Methodology and Measurement. 1994. http://hdr.undp.org/en/content/human-development-index-methodology-and-measurement .
De Larochelambert Q, Marc A, Antero J, Le Bourg E, Toussaint J-F. Covid-19 mortality: a matter of vulnerability among nations facing limited margins of adaptation. Public Health. 2020;8. https://doi.org/10.3389/fpubh.2020.604339 .
de Winter JC, Gosling SD, Potter J. Comparing the Pearson and Spearman correlation coefficients across distributions and sample sizes: a tutorial using simulations and empirical data. Psychol Methods. 2016;21(3):273.
World Health Organization. Universal health coverage [ http://www.who.int/universal_health_coverage/en/ ].
Johns Hopkins Center for Health Security. Global Health Security Index [ https://www.ghsindex.org/ ].
Pol Antràs SJR. Esteban Rossi-Hansberg: how do globalisation and pandemics interact? Surprising insights from a new model. In: #LSEThinks | CEP | global development vol. 2020. London: London School of Economics; 2020.
Google Scholar
Cai P. Understanding China’s belt and road initiative; 2017.
Baldwin R, Tomiura E. Thinking ahead about the trade impact of COVID-19. Economics in the Time of COVID-19. 2020;59. https://repository.graduateinstitute.ch/record/298220?ln=en .
Organization WH: Coronavirus disease ( COVID-19): situation report, 182. 2020.
Johns Hopkins University: COVID-19 Map - Johns Hopkins Coronavirus Resource Center. In. Edited by Security JHUCfH; 2021. https://coronavirus.jhu.edu/map.html .
Wang T, Du Z, Zhu F, Cao Z, An Y, Gao Y, et al. Comorbidities and multi-organ injuries in the treatment of COVID-19. Lancet. 2020;395(10228):e52.
Article CAS PubMed PubMed Central Google Scholar
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. Jama. 2020;323(11):1061–9.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506.
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–13.
Hussain A, Bhowmik B, Do Vale Moreira NC. COVID-19 and diabetes: knowledge in progress. Diabetes Res Clin Pract. 2020;162:108142. https://doi.org/10.1016/j.diabres.2020.108142 . Epub 2020 Apr 9.
Covid C, COVID C, COVID C, Chow N, Fleming-Dutra K, Gierke R, Hall A, et al. Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019—United States, February 12–march 28, 2020. Morb Mortal Wkly Rep. 2020;69(13):382.
Group C-S. Characteristics of COVID-19 patients dying in Italy: report based on available data on March 20th, 2020. Rome: Instituto Superiore Di Sanita; 2020. https://www.epicentro.iss.it/coronavirus/bollettino/Report-COVID-2019_20_marzo_eng.pdf .
Guan W-j, Ni Z-y, Hu Y, Liang W-H, Ou C-Q, He J-X, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–20.
Article CAS PubMed Google Scholar
Arentz M, Yim E, Klaff L, Lokhandwala S, Riedo FX, Chong M, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington state. Jama. 2020;323(16):1612–4.
Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the new York City area. JAMA. 2020;323(20):2052–9. https://doi.org/10.1001/jama.2020.6775 .
Covid C, Team R. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12–march 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(12):343–6.
Article Google Scholar
Mbow M, Lell B, Jochems SP, Cisse B, Mboup S, Dewals BG, et al. COVID-19 in Africa: dampening the storm? Science. 2020;369(6504):624–6.
Kavanagh MM, Erondu NA, Tomori O, Dzau VJ, Okiro EA, Maleche A, et al. Access to lifesaving medical resources for African countries: COVID-19 testing and response, ethics, and politics. Lancet. 2020;395(10238):1735–8.
Nordling L. Africa's pandemic puzzle: why so few cases and deaths? In: American Association for the Advancement of Science; 2020.
Oran DP, Topol EJ. Prevalence of asymptomatic SARS-CoV-2 infection: a narrative review. Ann Intern Med. 2020;173(5):362–7. https://doi.org/10.7326/M20-3012 . Epub 2020 Jun 3.
Nikolai LA, Meyer CG, Kremsner PG, Velavan TP. Asymptomatic SARS coronavirus 2 infection: invisible yet invincible. Int J Infect Dis. 2020;100:112–6. https://doi.org/10.1016/j.ijid.2020.08.076 . Epub 2020 Sep 3.
Rao C, Bradshaw D, Mathers CD. Improving death registration and statistics in developing countries: lessons from sub-Saharan Africa. Southern Afr J Demography. 2004:81–99.
Mehtar S, Preiser W, Lakhe NA, Bousso A, TamFum J-JM, Kallay O, et al. Limiting the spread of COVID-19 in Africa: one size mitigation strategies do not fit all countries. Lancet Glob Health. 2020;8(7):e881–3. Published online 2020 Apr 28. https://doi.org/10.1016/S2214-109X(20)30212-6 .
Nachega J, Seydi M, Zumla A. The late arrival of coronavirus disease 2019 (COVID-19) in Africa: mitigating pan-continental spread. Clin Infect Dis. 2020;71(15):875–8.
Gwilliam K, Foster V, Archondo-Callao R, Briceno-Garmendia C, Nogales A, Sethi K. Africa infrastructure country diagnostic: roads in sub-Saharan Africa: The World Bank; 2008.
Guengant J-P. Africa’s population: history, current status, and projections. In: Africa's Population: In Search of a Demographic Dividend: Springer; 2017. p. 11–31.
Collaborators GOD, Bernabe E, Marcenes W, Hernandez C, Bailey J, Abreu L, et al. Global, regional, and national levels and trends in burden of oral conditions from 1990 to 2017: a systematic analysis for the global burden of disease 2017 study. J Dent Res. 2020;99(4):362–73.
Cambaza EM, Viegas GC, Cambaza C. Manuel a: potential impact of temperature and atmospheric pressure on the number of cases of COVID-19 in Mozambique, southern Africa. J Public Health Epidemiol. 2020;12(3):246–60.
Lawal Y. Africa’s low COVID-19 mortality rate: a paradox? Int J Infect Dis. 2021;102:118–22.
Nkengasong JN, Mankoula W. Looming threat of COVID-19 infection in Africa: act collectively, and fast. Lancet. 2020;395(10227):841–2.
African Union and Africa CDC. African union and Africa CDC launches partnerships for African vaccine manufacturing (PAVM), framework to achieve it and signs 2 MoUs: African Union and Africa CDC; 2021.
Forbes. What Do Countries With The Best Coronavirus Responses Have In Common? Women Leaders [ https://www.forbes.com/sites/avivahwittenbergcox/2020/04/13/what-do-countries-with-the-best-coronavirus-reponses-have-in-common-women-leaders/#603bd9433dec ].
University of Notre Dame. What can we learn from Austria’s response to COVID-19? [ https://keough.nd.edu/what-can-we-learn-from-austrias-response-to-covid-19/ ].
Stoller JK. Reflections on leadership in the time of COVID-19. BMJ Leader. 2020. https://doi.org/10.1136/leader-2020-000244 .
Houston Public Media. What 6 Of The 7 Countries With The Most COVID-19 Cases Have In Common [ https://www.npr.org/sections/goatsandsoda/2020/07/31/896879448/the-nations-with-the-most-to-lose-from-covid-19 ].
Hale T, Petherick A, Phillips T, Webster S. Variation in government responses to COVID-19. Blavatnik school of government working paper. 2020;31. https://en.unesco.org/inclusivepolicylab/sites/default/files/learning/document/2020/4/BSG-WP-2020-031-v3.0.pdf .
The Editors. Dying in a leadership vacuum. N Engl J Med. 2020;383(15):1479–80.
The Cable News Network. US and UK are bottom of the pile in rankings of governments' handling of coronavirus pandemic [ https://edition.cnn.com/2020/08/27/world/global-coronavirus-attitudes-pew-intl/index.html ].
Huston P, Campbell J, Russell G, Goodyear-Smith F, Phillips RL, van Weel C, et al. COVID-19 and primary care in six countries. BJGP Open. 2020;4(4):bjgpopen20X101128. https://doi.org/10.3399/bjgpopen20X101128 .
Goodyear-Smith F, Kinder K, Eden AR, Strydom S, Bazemore A, Phillips R, et al. Primary care perspectives on pandemic politics. Glob Public Health. 2021;16(8-9):1304–19. https://doi.org/10.1080/17441692.2021.1876751 . Epub 2021 Jan 24.
Rutledge PE. Trump, COVID-19, and the war on expertise. Am Rev Public Adm. 2020;50(6-7):505–11.
Ugarte DA, Cumberland WG, Flores L, Young SD. Public attitudes about COVID-19 in response to president trump's social media posts. JAMA Netw Open. 2021;4(2):e210101.
Article PubMed PubMed Central Google Scholar
Lal A, Erondu NA, Heymann DL, Gitahi G, Yates R. Fragmented health systems in COVID-19: rectifying the misalignment between global health security and universal health coverage. Lancet. 2021;397(10268):61–7. https://doi.org/10.1016/S0140-6736(20)32228-5 . Epub 2020 Dec 1.
Tromberg BJ, Schwetz TA, Pérez-Stable EJ, Hodes RJ, Woychik RP, Bright RA, et al. Rapid scaling up of Covid-19 diagnostic testing in the United States—the NIH RADx initiative. N Engl J Med. 2020;383(11):1071–7.
Marwaha J, Halamka J, Brat G. Lifesaving ventilators will sit unused without a national data-sharing effort; 2020.
Kidd MR. Five principles for pandemic preparedness: lessons from the Australian COVID-19 primary care response. Br J Gen Pract. 2020;70(696):316–7. https://doi.org/10.3399/bjgp20X710765 . Print 2020 Jul.
Hsu LY, Tan M-H. What Singapore can teach the US about responding to COVID-19. STAT News. 2020. https://www.statnews.com/2020/03/23/singapore-teach-united-states-about-covid-19-response/ .
Horton R. Offline: COVID-19 is not a pandemic. Lancet (London, England). 2020;396(10255):874.
Article CAS Google Scholar
Raisi-Estabragh Z, McCracken C, Bethell MS, Cooper J, Cooper C, Caulfield MJ, et al. Greater risk of severe COVID-19 in black, Asian and minority ethnic populations is not explained by cardiometabolic, socioeconomic or behavioural factors, or by 25 (OH)-vitamin D status: study of 1326 cases from the UK biobank. J Public Health. 2020;42(3):451–60.
Hamidianjahromi A. Why African Americans are a potential target for COVID-19 infection in the United States. J Med Internet Res. 2020;22(6):e19934.
Tangcharoensathien V, Bassett MT, Meng Q, Mills A. Are overwhelmed health systems an inevitable consequence of covid-19? Experiences from China, Thailand, and New York State. BMJ. 2021;372. https://doi.org/10.1136/bmj.n83 .
Organization WH: COVID-19 health system response monitor, Thailand. 2020.
Narkvichien M. Thailand’s 1 million village health volunteers-“unsung heroes”-are helping guard communities nationwide from COVID-19. Nonthaburi: World Health Organization; 2020.
Kupferschmidt K, Cohen J. Can China's COVID-19 strategy work elsewhere? In: American Association for the Advancement of Science; 2020.
Al Saidi AMO, Nur FA, Al-Mandhari AS, El Rabbat M, Hafeez A, Abubakar A. Decisive leadership is a necessity in the COVID-19 response. Lancet. 2020;396(10247):295–8.
Forman R, Atun R, McKee M, Mossialos E. 12 lessons learned from the management of the coronavirus pandemic. Health Policy. 2020;124(6):577–80. https://doi.org/10.1016/j.healthpol.2020.05.008 .
Barberia LG, Gómez EJ. Political and institutional perils of Brazil's COVID-19 crisis. Lancet. 2020;396(10248):367–8.
Ortega F, Orsini M. Governing COVID-19 without government in Brazil: ignorance, neoliberal authoritarianism, and the collapse of public health leadership. Global Public Health. 2020;15(9):1257–77.
Ezequiel GE, Jafet A, Hugo A, Pedro D, Ana Maria M, Carola OV, et al. The COVID-19 pandemic: a call to action for health systems in Latin America to strengthen quality of care. Int J Qual Health Care. 2021;33(1):mzaa062.
Rocha R, Atun R, Massuda A, Rache B, Spinola P, Nunes L, et al. Effect of socioeconomic inequalities and vulnerabilities on health-system preparedness and response to COVID-19 in Brazil: a comprehensive analysis. Lancet Glob Health. 2021;9(6):e782–92. https://doi.org/10.1016/S2214-109X(21)00081-4 . Epub 2021 Apr 12.
Lancet T. India under COVID-19 lockdown. Lancet (London, England). 2020;395(10233):1315.
Siddiqui AF, Wiederkehr M, Rozanova L, Flahault A. Situation of India in the COVID-19 pandemic: India’s initial pandemic experience. Int J Environ Res Public Health. 2020;17(23):8994.
Article CAS PubMed Central Google Scholar
Taneja P, Bali AS. India’s domestic and foreign policy responses to COVID-19. Round Table. 2021;110(1):46–61.
Choutagunta A, Manish G, Rajagopalan S. Battling COVID-19 with dysfunctional federalism: lessons from India. South Econ J. 2021;87(4):1267–99.
Mallapaty S. India's massive COVID surge puzzles scientists. Nature. 2021;592(7856):667–8.
Thiagarajan K. Why is India having a covid-19 surge? In: British Medical Journal Publishing Group; 2021.
Fisman DN, Greer AL, Tuite AR. Age is just a number: a critically important number for COVID-19 case fatality. Ann Intern Med. 2020;173(9):762–3.
Sudharsanan N, Didzun O, Bärnighausen T, Geldsetzer P. The contribution of the age distribution of cases to COVID-19 case fatality across countries: a 9-country demographic study. Ann Intern Med. 2020;173(9):714–20. https://doi.org/10.7326/M20-2973 . Epub 2020 Jul 22.
Think Global Health. The Myth of South Asian Exceptionalism. In: He Myth of South Asian Exceptionalism: South Asia's young population conceals the effects that COVID-19 has on its older and more vulnerable people. vol. 2020; 2020.
Ioannidis JP, Axfors C, Contopoulos-Ioannidis DG. Population-level COVID-19 mortality risk for non-elderly individuals overall and for non-elderly individuals without underlying diseases in pandemic epicenters. Environ Res. 2020;188:109890.
Kim D-H, Choe YJ, Jeong J-Y. Understanding and interpretation of case fatality rate of coronavirus disease 2019. J Korean Med Sci. 2020;35(12):e137. https://doi.org/10.3346/jkms.2020.35.e137 .
Rajgor DD, Lee MH, Archuleta S, Bagdasarian N, Quek SC. The many estimates of the COVID-19 case fatality rate. Lancet Infect Dis. 2020;20(7):776–7.
Sorci G, Faivre B, Morand S. Explaining among-country variation in COVID-19 case fatality rate. Sci Rep. 2020;10(1):1–11.
Sen-Crowe B, Sutherland M, McKenney M, Elkbuli A. A closer look into global hospital beds capacity and resource shortages during the COVID-19 pandemic. J Surg Res. 2021;260:56–63.
Li M, Zhang Z, Cao W, Liu Y, Du B, Chen C, et al. Identifying novel factors associated with COVID-19 transmission and fatality using the machine learning approach. Sci Total Environ. 2021;764:142810.
Undurraga EA, Chowell G, Mizumoto K. COVID-19 case fatality risk by age and gender in a high testing setting in Latin America: Chile, march–august 2020. Infect Dis Poverty. 2021;10(1):1–11.
Taylor L. How Latin America is fighting covid-19, for better and worse. BMJ. 2020;370:m3319. https://doi.org/10.1136/bmj.m3319 .
Bhuyan A. Covid-19: India looks to import oxygen as cases surge, overwhelming hospitals. In: British Medical Journal Publishing Group; 2021.
An BY, Tang S-Y. Lessons from COVID-19 responses in East Asia: institutional infrastructure and enduring policy instruments. Am Rev Public Adm. 2020;50(6-7):790–800.
Chen H, Shi L, Zhang Y, Wang X, Sun G. A cross-country core strategy comparison in China, Japan, Singapore and South Korea during the early COVID-19 pandemic. Glob Health. 2021;17(1):1–10.
Kahathuduwa CN, Dhanasekara CS, Chin S-H. Case fatality rate in COVID-19: a systematic review and meta-analysis. J Prev Med Hyg. 2021;62(2):E311–20. https://doi.org/10.15167/2421-4248/jpmh2021.62.2.1627 . eCollection 2021 Jun.
Meyerowitz-Katz G, Merone L. A systematic review and meta-analysis of published research data on COVID-19 infection-fatality rates. Int J Infect Dis. 2020.
Seoane B. A scaling approach to estimate the COVID-19 infection fatality ratio from incomplete data. PLoS One. 2021;16(2):e0246831. https://doi.org/10.1371/journal.pone.0246831 . eCollection 2021.
Byambasuren O, Dobler CC, Bell K, Rojas DP, Clark J, McLaws M-L, et al. Comparison of seroprevalence of SARS-CoV-2 infections with cumulative and imputed COVID-19 cases: systematic review. PLoS One. 2021;16(4):e0248946.
Shakiba M, Nazemipour M, Salari A, Mehrabian F, Nazari SSH, Rezvani SM, et al. Seroprevalence of SARS-CoV-2 in Guilan Province, Iran, April 2020. Emerg Infect Dis. 2021;27(2):636.
Blanchet K, Alwan A, Antoine C, Cros MJ, Feroz F, Guracha TA, et al. Protecting essential health services in low-income and middle-income countries and humanitarian settings while responding to the COVID-19 pandemic. BMJ Glob Health. 2020;5(10):e003675.
Thome J, Coogan AN, Fischer M, Tucha O, Faltraco F. Challenges for mental health services during the 2020 COVID-19 outbreak in Germany. Psychiatry Clin Neurosci. 2020;74(7):407. https://doi.org/10.1111/pcn.13019 . Epub 2020 May 26.
Riley T, Sully E, Ahmed Z, Biddlecom A. Estimates of the potential impact of the COVID-19 pandemic on sexual and reproductive health in low-and middle-income countries. Int Perspect Sex Reprod Health. 2020;46:73–6.
World Health Organization (WHO): Maintaining essential health services: operational guidance for the COVID-19 context: interim guidance, 1 June 2020. In.: World Health Organization; 2020. https://www.who.int/publications/i/item/WHO-2019-nCoV-essential_health_services-2020.2 .
World Health Organization (WHO): Pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report, 27 August 2020. In.: World Health Organization; 2020. https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-EHS_continuity-survey-2020.1 .
World Health Organization (WHO): Second round of the national pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report, 22 April 2021. In.: World Health Organization; 2021. https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS-continuity-survey-2021.1 .
Organization WH. COVID-19: operational guidance for maintaining essential health services during an outbreak: interim guidance, 25 march 2020: World Health Organization; 2020.
Chen Y-Y, Assefa Y. The heterogeneity of the COVID-19 pandemic and national responses: an explanatory mixed-methods study. BMC Public Health. 2021;21(1):1–15.
World Health Organization (WHO). Thirteenth general programme of work 2019–2023. The seventy-first world health assembly. Geneva (Switzerland): World Health Organization; 2018.
Mahjour J, Mirza Z, Rashidian A, Atta H, Hajjeh R, Thieren M, et al. " promote health, keep the world safe, serve the vulnerable" in the eastern Mediterranean region. East Mediterr Health J. 2018;24(4):323–4.
Rollston R, Galea S. COVID-19 and the social determinants of health. Am J Health Promot. 2020;34(6):687–9. https://doi.org/10.1177/0890117120930536b .
Nachega JB, Sam-Agudu NA, Masekela R, van der Zalm MM, Nsanzimana S, Condo J, et al. Addressing challenges to rolling out COVID-19 vaccines in African countries. Lancet Glob Health. 2021;9(6):e746–8. https://doi.org/10.1016/S2214-109X(21)00097-8 . Epub 2021 Mar 10.
Skegg D, Gluckman P, Boulton G, Hackmann H, Karim SSA, Piot P, et al. Future scenarios for the COVID-19 pandemic. Lancet. 2021;397(10276):777–8.
Nhamo G, Chikodzi D, Kunene HP, Mashula N. COVID-19 vaccines and treatments nationalism: challenges for low-income countries and the attainment of the SDGs. Global Public Health. 2021;16(3):319–39.
Figueroa JP, Bottazzi ME, Hotez P, Batista C, Ergonul O, Gilbert S, et al. Urgent needs of low-income and middle-income countries for COVID-19 vaccines and therapeutics. Lancet. 2021;397(10274):562–4.
He X, Hong W, Pan X, Lu G, Wei X. SARS-CoV-2 omicron variant: characteristics and prevention. Med Comm (2020). 2021;2(4):838–45. https://doi.org/10.1002/mco2.110 .
Karim SSA, Karim QA. Omicron SARS-CoV-2 variant: a new chapter in the COVID-19 pandemic. Lancet. 2021;398(10317):2126–8.
Sanders D, Nandi S, Labonté R, Vance C, Van Damme W. From primary health care to universal health coverage—one step forward and two steps back. Lancet. 2019;394(10199):619–21.
Hone T, Macinko J, Millett C. Revisiting Alma-Ata: what is the role of primary health care in achieving the sustainable development goals? Lancet. 2018;392(10156):1461–72.
Redwood-Campbell L, Abrahams J. Primary health care and disasters—the current state of the literature: what we know, gaps and next steps. Prehospital Disaster Med. 2011;26(3):184–91.
Bitton A, Ratcliffe HL, Veillard JH, Kress DH, Barkley S, Kimball M, et al. Primary health care as a foundation for strengthening health systems in low-and middle-income countries. J Gen Intern Med. 2017;32(5):566–71.
Dunlop C, Howe A, Li D, Allen LN. The coronavirus outbreak: the central role of primary care in emergency preparedness and response. BJGP Open. 2020;4(1):bjgpopen20X101041. https://doi.org/10.3399/bjgpopen20X101041 .
Assefa Y, Gilks CF, van de Pas R, Reid S, Gete DG, Van Damme W. Reimagining global health systems for the 21st century: lessons from the COVID-19 pandemic. BMJ Glob Health. 2021;6(4):e004882.
Loewenson R, Accoe K, Bajpai N, Buse K, Abi Deivanayagam T, London L, et al. Reclaiming comprehensive public health. BMJ Glob Health. 2020;5(9):e003886.
Rawaf S, Allen LN, Stigler FL, Kringos D, Quezada Yamamoto H, van Weel C, et al. Lessons on the COVID-19 pandemic, for and by primary care professionals worldwide. Eur J Gen Pract. 2020;26(1):129–33.
Gostin LO, Friedman EA. A retrospective and prospective analysis of the west African Ebola virus disease epidemic: robust national health systems at the foundation and an empowered WHO at the apex. Lancet. 2015;385(9980):1902–9.
Download references
Acknowledgements
Not applicable.
No funding was obtained for this study.
Author information
Authors and affiliations.
School of Public Health, the University of Queensland, Brisbane, Australia
Yibeltal Assefa, Charles F. Gilks, Simon Reid & Dereje Gedle Gete
Institute of Tropical Medicine, Antwerp, Belgium
Remco van de Pas & Wim Van Damme
You can also search for this author in PubMed Google Scholar
Contributions
YA conceived the idea of the research, collected and analysed the data, and prepared the first and subsequent drafts. DG participated in data collection and analysis. CFG, SR, RVDP, DG and WVD provided comments during subsequent drafts. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Yibeltal Assefa .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Assefa, Y., Gilks, C.F., Reid, S. et al. Analysis of the COVID-19 pandemic: lessons towards a more effective response to public health emergencies. Global Health 18 , 10 (2022). https://doi.org/10.1186/s12992-022-00805-9
Download citation
Received : 04 August 2021
Accepted : 14 January 2022
Published : 04 February 2022
DOI : https://doi.org/10.1186/s12992-022-00805-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Heterogeneity
Globalization and Health
ISSN: 1744-8603
- Submission enquiries: [email protected]
- General enquiries: [email protected]

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Fact Sheet: End of the COVID-19 Public Health Emergency
Based on current COVID-19 trends, the Department of Health and Human Services (HHS) is planning for the federal Public Health Emergency (PHE) for COVID-19, declared under Section 319 of the Public Health Service (PHS) Act, to expire at the end of the day on May 11, 2023.
Since HHS Secretary Xavier Becerra’s February 9, 2023, letter to Governors announcing the planned end of the COVID-19 PHE, the Department has been working closely with partners—including Governors; state, local, Tribal, and territorial agencies; industry; and advocates—to ensure an orderly transition out of the COVID-19 PHE.
Today, HHS is releasing a Fact Sheet with an update on current flexibilities enabled by the COVID-19 emergency declaration and how they will be impacted by the end of the COVID-19 PHE on May 11.
What has been accomplished:
Due to the Biden-Harris Administration’s whole-of-government approach to combatting COVID-19, we are now in a better place in our response than at any point of the pandemic and well-positioned to transition out of the emergency phase and end the COVID-19 PHE. Over the last two years, the Biden-Harris Administration has effectively implemented the largest adult vaccination program in U.S. history, with over 270 million people receiving at least one shot of a COVID-19 vaccine. The Administration has also made lifesaving treatments widely available, with more than 15 million courses administered. And through COVIDTests.gov, the Administration has distributed more than 750 million free COVID-19 tests shipped directly to more than 80 million households. The Administration has also administered more than 50 million diagnostic tests in-person at pharmacy and community-based sites. As a result of these and other efforts, COVID-19 is no longer the disruptive force it once was. Since January 2021, COVID-19 deaths have declined by 95% and hospitalizations are down nearly 91%.
As we approach the end of the COVID-19 PHE:
- We have successfully marshalled a whole-of-government response to make historic investments in vaccines, tests, and treatments that are broadly available to help us combat COVID-19.
- Our health care system and public health resources throughout the country are now better able to respond to any potential surge of COVID-19 cases without significantly affecting an individual’s ability to access resources or care.
- Our public health experts have issued guidance that allows individuals to understand mitigation measures, such as masking and testing to protect themselves and those around them.
- We have the tools to detect and respond to the potential emergence of a variant of high consequence as we continue to monitor the evolving state of COVID-19 and the emergence of virus variants.
Still, we know so many people continue to be affected by COVID-19, particularly seniors, people who are immunocompromised, and people with disabilities. That is why our response to the spread of SARS-CoV-2, the virus that causes COVID-19, remains a public health priority. To ensure an orderly transition, we have been working for months so that we can continue to meet the needs of those affected by COVID-19.
Even beyond the end of the COVID-19 PHE, we will continue to work to protect Americans from the virus and its worst impacts by supporting access to COVID-19 vaccines, treatments, and tests, including for people without health insurance. We will continue to advance research into new, innovative vaccines and treatments through an investment of $5 billion in Project NextGen, a dedicated program to accelerate and streamline the rapid development of the next generation of vaccines and treatments, including investments in research, development, and manufacturing capacity and advancing critical science. And we are continuing to invest in efforts to better understand and address Long COVID and to help mitigate the impacts.
What will not be affected by the end of the COVID-19 PHE:
The Administration’s continued response to COVID-19 is not fully dependent on the emergency declaration for the COVID-19 PHE, and there are significant flexibilities and actions that will not be affected when we transition from the current phase of our response on May 11.
Access to COVID-19 vaccinations and certain treatments, such as Paxlovid and Lagevrio, will generally not be affected. To help keep communities safe from COVID-19, HHS remains committed to maximizing continued access to COVID-19 vaccines and treatments.
At the end of the COVID-19 PHE on May 11, Americans will continue to be able to access COVID-19 vaccines at no cost, just as they have during the COVID-19 PHE, due to the requirements of the CDC COVID-19 Vaccination Program Provider Agreement. people will also continue to be able to access COVID-19 treatments just as they have during the COVID-19 PHE.
Once the federal government is no longer purchasing or distributing COVID-19 vaccines and treatments, payment, coverage, and access may change. In order to prepare for that transition, partners across the U.S. Government (USG) are planning for and have been developing plans to ensure a smooth transition for the provision of COVID-19 vaccines and certain treatments as part of the traditional health care market, which will occur in the coming months.
When that transition to the traditional health care market occurs, to protect families, the Administration has facilitated access to COVID-19 vaccines with no out-of-pocket costs for nearly all individuals and will continue to ensure that effective COVID-19 treatments, such as Paxlovid, are widely accessible.
The Department announced the “ HHS Bridge Access Program For COVID-19 Vaccines and Treatments ” (“Bridge” Program) on April 18, to maintain broad access to COVID-19 vaccines and treatments for uninsured Americans after the transition to the traditional health care market. For those with most types of private insurance, COVID-19 vaccines recommended by the Advisory Committee on Immunization Practices (ACIP) are a preventive health service and will be fully covered without a co-pay when provided by an in-network provider. Currently, COVID-19 vaccinations are covered under Medicare Part B without cost sharing, and this will continue. Medicare Advantage plans must also cover COVID-19 vaccinations in-network without cost sharing, and this will continue. Medicaid will continue to cover COVID-19 vaccinations without a co-pay or cost sharing through September 30, 2024 and will generally cover ACIP-recommended vaccines for most beneficiaries thereafter.
After the transition to the traditional health care market, out-of-pocket expenses for certain treatments, such as Paxlovid and Lagevrio, may change, depending on an individual’s health care coverage, similar to costs that one may experience for other covered drugs. Medicaid programs will continue to cover COVID-19 treatments without cost sharing through September 30, 2024. After that, coverage and cost sharing may vary by state.
For more information about the “Bridge” Program, visit Fact Sheet: HHS Announces ‘HHS Bridge Access Program For COVID-19 Vaccines and Treatments’ to Maintain Access to COVID-19 Care for the Uninsured . For more information about access to COVID-19 vaccinations and treatments, visit CMS Waivers, Flexibilities, and the End of the COVID-19 Public Health Emergency .
The Food and Drug Administration’s (FDA’s) Emergency Use Authorizations (EUAs) for COVID-19 products (including tests, vaccines, and treatments) will not be affected. FDA’s ability to authorize various products, including tests, treatments, or vaccines for emergency use will not be affected by the end of the COVID-19 PHE. To learn more, visit FDA’s FAQs: What happens to EUAs when a public health emergency ends?
Major telehealth flexibilities will not be affected. The vast majority of current Medicare telehealth flexibilities that people with Medicare—particularly those in rural areas and others who struggle to find access to care—have come to rely upon throughout the COVID-19 PHE, will remain in place through December 2024. Additionally, states already have significant flexibility with respect to covering and paying for Medicaid services delivered via telehealth. This flexibility was available prior to the COVID-19 PHE and will continue to be available after the COVID-19 PHE ends. To learn more, visit the Centers for Medicare & Medicaid Services’ (CMS) CMS Waivers, Flexibilities, and the End of the COVID-19 Public Health Emergency .
Our whole-of-government response to Long COVID will not change. The Department has and will continue to coordinate a whole-of-government response to the longer-term effects of COVID-19, including Long COVID and associated conditions. On April 5, HHS released this Fact Sheet outlining the progress made in responding to Long COVID and actions the Department is taking to address the needs of the growing population with Long COVID and associated conditions.
What will be affected by the end of the COVID-19 PHE:
Many COVID-19 PHE flexibilities and policies have already been made permanent or otherwise extended for some time, with others expiring after May 11.
Certain Medicare and Medicaid waivers and broad flexibilities for health care providers are no longer necessary and will end. During the COVID-19 PHE, CMS used a combination of emergency authority waivers, regulations, and sub-regulatory guidance to ensure and expand access to care and to give health care providers the flexibilities needed to help keep people safe. States, hospitals, nursing homes, and others are currently operating under hundreds of these waivers that affect care delivery and payment and that are integrated into patient care and provider systems. Many of these waivers and flexibilities were necessary to expand facility capacity for the health care system and to allow the health care system to weather the heightened strain created by COVID-19; given the current state of COVID-19, this excess capacity is no longer necessary.
For Medicaid, some additional COVID-19 PHE waivers and flexibilities will end on May 11, while others will remain in place for six months following the end of the COVID-19 PHE. But many of the Medicaid waivers and flexibilities, including those that support home and community-based services, are available for states to continue beyond the COVID-19 PHE, if they choose to do so. For example, states have used COVID-19 PHE-related flexibilities to increase the number of individuals served under a waiver, expand provider qualifications, and other flexibilities. Many of these options may be extended beyond the COVID-19 PHE. To learn more, visit CMS Waivers, Flexibilities, and the End of the COVID-19 Public Health Emergency
Coverage for COVID-19 testing will change, but USG is maintaining a strong stockpile and distribution channels so that tests remain accessible at no cost in certain community locations, and the USG will continue to distribute tests through COVIDtests.gov through the end of May. People with Traditional Medicare can continue to receive COVID-19 PCR and antigen tests with no cost-sharing when the lab tests are ordered by a physician or certain other health care providers, such as physician assistants and advanced practice registered nurses. People enrolled in Medicare Advantage plans can continue to receive COVID-19 PCR and antigen tests when the test is covered by Medicare, but their cost-sharing may change when the COVID-19 PHE ends. Additionally, the program that allowed Medicare coverage and payment for over-the-counter (OTC) COVID-19 tests will end when the COVID-19 PHE ends on May 11; Medicare Advantage plans may continue to cover the tests, and beneficiaries should check with their plan for details.
State Medicaid programs must provide coverage without cost sharing for COVID-19 testing until the last day of the first calendar quarter that begins one year after the last day of the COVID-19 PHE. That means with the COVID-19 PHE ending on May 11, 2023, this mandatory coverage will end on September 30, 2024, after which coverage may vary by state.
The requirement for private insurance companies to cover COVID-19 tests without cost sharing, both for OTC and laboratory tests, will end at the expiration of the PHE. However, coverage may continue if plans choose to do so. The Administration is encouraging private insurers to continue to provide such coverage going forward. For more information visit Coverage for COVID-19 Tests , Frequently Asked Questions: CMS Waivers, Flexibilities, and the End of the COVID-19 Public Health Emergency , FAQs About Families First Coronavirus Response Act, Coronavirus Aid, Relief, and Economic Security Act, and Health Insurance Portability and Accountability Act Implementation Part 58 .
Additionally, the USG may continue to distribute free COVID-19 tests from the Strategic National Stockpile through states and other community partners. Pending resource availability, the Centers for Disease Control and Prevention’s (CDC) Increasing Community Access to Testing (ICATT) program will continue to focus on no-cost testing for uninsured individuals and areas of high social vulnerability through pharmacies and community-based sites. For more information, visit CDC’s ICATT website .
Certain COVID-19 data reporting and surveillance will change. CDC COVID-19 data surveillance has been a cornerstone of our response, and during the PHE, HHS had the authority to require lab test reporting for COVID-19. At the end of the COVID-19 PHE, HHS will no longer have this express authority to require this data from labs, which will affect the reporting of negative test results and impact the ability to calculate percent positivity for COVID-19 tests in some jurisdictions. Hospital data reporting will continue as required by the CMS conditions of participation through April 30, 2024, but reporting will be reduced from the current daily reporting to weekly.
Despite these changes, CDC will continue to report valuable data to understand COVID-19 trends and to inform individual and community public health actions to protect those at highest risk of severe COVID-19. In fact, CDC will still have access to more data than is currently collected for other respiratory illnesses to inform public health action at all levels, with hospital data, which is available at the county level, becoming a primary data source to indicate severe COVID-19 in a community. To learn more, visit this CDC resource: End of the Federal COVID-19 Public Health Emergency (PHE) Declaration .
In March, FDA announced a transition plan for certain COVID-19-related guidance documents related to topics such as medical devices, clinical practice and supply chains, including which policies will end or be temporarily extended. To learn more, please visit FDA’s COVID-19-Related Guidance Documents for Industry, FDA Staff, and Other Stakeholders .
FDA’s ability to detect shortages of critical devices related to COVID-19 will be more limited. While FDA will still maintain its authority to detect and address other potential medical product shortages, it is seeking congressional authorization to extend the requirement for device manufacturers to notify FDA of interruptions and discontinuances of critical devices outside of a PHE which will strengthen the ability of FDA to help prevent or mitigate device shortages.
Public Readiness and Emergency Preparedness (PREP) Act liability protections will be amended. On April 14, 2023, HHS Secretary Becerra sent a letter and Fact Sheet to the nation’s governors announcing his intention to amend the PREP Act declaration to extend certain important protections that will continue to facilitate access to convenient and timely COVID-19 vaccines, treatments, and tests for individuals. The Secretary intends to amend the PREP Act declaration for the COVID-19 countermeasures to extend the protections referenced in that fact sheet as well as others and publish the amendment in the Federal Register as required by the PREP Act.
Sign Up for Email Updates
Receive the latest updates from the Secretary, Blogs, and News Releases
Subscribe to RSS
Receive latest updates

Related News Releases
Covid-19 vaccination public education campaign saved thousands of lives, billions of dollars, hhs, dhs, and fema announce completion of multi-year review of state efforts to provide language access during the covid-19 public health emergency, readout of hhs secretary becerra’s meeting with pharmacy ceos on covid-19 therapeutics commercialization, related blog posts.

Calling innovators! HHS Long COVID Healthathon launches with $25K in prizes
Reflections from the deputy director of the hhs office of long covid research and practice.

Driving Long COVID Innovation with Health+ Human-Centered Design
Media inquiries.
For general media inquiries, please contact [email protected] .
When Does the COVID-19 Pandemic End?
Neither WHO nor any other organization decides when a pandemic begins or ends.
When Does the Pandemic End?

Spencer Platt | Getty Images
A man carries a mask on May 11, 2023, in New York City.
The coronavirus is no longer in its emergency phase. But does that mean it's no longer a pandemic?
On March 11, 2020, the World Health Organization for the first time called COVID-19 a pandemic.
"We have rung the alarm bell loud and clear," Tedros Adhanom Ghebreyesus, WHO director-general, said at a news conference at the time.
In reality, neither WHO nor any other institution gets to decide when a pandemic begins or ends. The murky guidelines mean that there might never be a specific day everyone points to as the end of the COVID-19 pandemic.
WHO still considers COVID-19 to be a pandemic, but it decided on Friday that it is no longer a public health emergency of international concern, marking a major shift. It said that COVID-19 still poses a global threat.
“Last week, COVID-19 claimed a life every three minutes – and that’s just the deaths we know about,” Tedros said at a press conference. “As we speak, thousands of people around the world are fighting for their lives in intensive care units and millions more continue to live with the debilitating effects of post-COVID-19 condition.”
Cartoons on the Coronavirus

So when does the COVID-19 pandemic end? It depends on who you ask.
“In most cases, pandemics truly end when the next pandemic begins,” WHO’s Mike Ryan said during the press conference last week. “I know that's a terrible thought, but that is the history of pandemics.”
Don’t wait with bated breath for WHO to say the pandemic is over. In fact, Ryan said that he believes “there will not be a point where WHO comes along and says the pandemic is over.”
Pandemics may begin with a “bang” but they end with a “whimper,” according to White House COVID-19 response coordinator Ashish Jha. In the U.S., the Biden administration this week ended the public health emergency declaration related to COVID-19.
“That moment of March 11, it was like, whoa,” Jha told NPR, referring to the day WHO called COVID-19 a pandemic for the first time. “The idea of ending with a whimper is the idea that pandemics fade. There are moments we mark. Ending of a public health emergency is an important moment. And for a lot of people, this will feel like that transition.”
Despite WHO’s stance, many Americans have already moved on from the COVID-19 pandemic.
“But there's no question that for a lot of Americans, that what the pandemic represented is in the rearview mirror,” Jha continued. “And for other Americans, particularly who are immunocompromised, who are high risk, this moment, while a transition, doesn't make the threat go away.”
In light of the recent decisions from WHO and the Biden administration, some experts are ready to say the pandemic is over.
“The pandemic is over,” says Robert Murphy, the executive director of the Havey Institute for Global Health at Northwestern University Feinberg School of Medicine. “Now, could it come back? Yeah, because we don't really know. But what's happened is almost everybody in the world has become infected or taken a vaccine. And we've developed enough immunity as a population to keep it down to this basically dull roar where we are now.”
Others say it depends on how you define a pandemic.
“My reaction to the WHO announcement is really grounded in the true meaning to us all of the term pandemic,” Christopher Murray of the University of Washington’s Institute for Health Metrics and Evaluation said in a statement . “It is a formal epidemiological term, which is an epidemic that's covering many parts of the globe. And in that sense, COVID is still a pandemic. It's an infection, but it's moving from essentially a new threat to something that we are learning to live with.”
On the other hand, “if you think of the pandemic as something that requires a concerted set of quite extraordinary measures from governments and individuals to be able to manage it, then I think the pandemic ended when omicron showed up last year, because very soon, if you look at the institution of social distancing mandates or other efforts, within a couple of months of omicron showing up, there were very few mandates left in the world. And so in that sense, I think the WHO announcement is appropriate and perhaps might have come six months ago as well, reflecting that change from living with the disease as opposed to an emergency response to the disease,” he continued.
Still others say that the pandemic isn’t over yet, no matter how you slice it.
“We don’t want to confuse it with the fact that the pandemic is completely over,” leading infectious disease expert Anthony Fauci said about WHO’s decision that COVID-19 is no longer a public health emergency of international concern. “What is over is the emergency nature of it. And I think that’s what people get confused at. It doesn’t mean we should stop getting vaccinated, it doesn’t mean under certain circumstances we should stop wearing masks.”
While many people have already shifted to the mindset that the pandemic is over, others, including people with immunocompromised immune systems, have not. According to a Gallup poll published in March, nearly half of Americans don’t think their lives will ever return to pre-pandemic normalcy.
On the individual level, it doesn’t matter if institutions or experts say the pandemic is over if a person isn’t ready to move on from it, says Vincent Silenzio, a professor in the Department of Urban-Global Public Health at the Rutgers School of Public Health.
“If you're not personally ready to declare it over, it's fine,” Silenzio says.
And while the emergency phase may be over, COVID-19 is ultimately here to stay.
“COVID is not over,” Silenzio says. “There is still COVID out there, and it will be with us for a while.”
Join the Conversation
Tags: Coronavirus , CDC , World Health Organization
America 2024

Best States

Health News Bulletin
Stay informed on the latest news on health and COVID-19 from the editors at U.S. News & World Report.
Sign in to manage your newsletters »
Sign up to receive the latest updates from U.S News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
You May Also Like
The 10 worst presidents.
U.S. News Staff Feb. 23, 2024

Cartoons on President Donald Trump
Feb. 1, 2017, at 1:24 p.m.

Photos: Obama Behind the Scenes
April 8, 2022

Photos: Who Supports Joe Biden?
March 11, 2020

How Rare Are Brain Worms Like RFK Jr.’s?
Laura Mannweiler May 8, 2024

QUOTES: Israel's Rafah Attack
Cecelia Smith-Schoenwalder May 8, 2024

K-12 Officials Hit Back at Congress
Aneeta Mathur-Ashton May 8, 2024

The Trump Trials, Explained
Lauren Camera and Kaia Hubbard May 8, 2024

QUOTES: Stormy Daniels’ Testimony
Cecelia Smith-Schoenwalder May 7, 2024

Future of the Antisemitism Bill In Doubt
Aneeta Mathur-Ashton May 7, 2024


AstraZeneca’s COVID vaccine withdrawn – right to the end it was the victim of misinformation
Senior Research Fellow in Global Health, University of Southampton
Disclosure statement
Michael Head has previously received funding from the Bill & Melinda Gates Foundation and the UK Department for International Development, and currently receives funding from the UK Medical Research Foundation.
University of Southampton provides funding as a member of The Conversation UK.
View all partners
The Oxford-AstraZeneca vaccine was a critical part of the COVID-19 pandemic response. However, on May 7 2024, the European Commission announced the vaccine is no longer authorised for use.
This EU announcement was preceded by an application from AstraZeneca on March 27 2024 to withdraw the EU marketing authorisation. This development has been covered in various media outlets as primarily related to the known “adverse events”, namely a very small risk of blood clots. However, other factors are far more likely to be driving this decision.
You can listen to more articles from The Conversation, narrated by Noa .
The first AstraZeneca vaccine dose, outside of clinical trials, was administered on January 4 2021. In that year, about 2.5 billion doses were administered, and an estimated 6.3 million lives saved.
It was a key product at the peak of the pandemic. This includes during the emergence of the delta variant in India, across the first half of 2021 where, amid significant global supply issues, the AstraZeneca vaccine was one of the few tools available during that humanitarian crisis .

This COVID vaccine, like those from Pfizer, Moderna, Novavax and others, went through the appropriate levels of testing. The phase 3 trials (where the vaccine is tested on thousands of people) showed the AstraZeneca product was safe and effective. It was distributed in many countries in Europe in early 2021, including the UK.
The potential adverse events related to blood clots were publicly reported in February 2021, with, for example, the UK government and the drugs regulator (the MHRA) then publishing a statement about its continued use on March 18 2021.
Amid speculation and investigation, the European Medicines Agency and the World Health Organization both highlighted how the benefits of the vaccine greatly outweighed any possible risks.
This was a time when COVID levels were extremely high, and getting higher, with around 4 million confirmed new cases globally per week.
It is well established that COVID itself caused a significantly increased risk of these related blood clots and also thrombocytopenia (low platelet count). An August 2021, analysis of 30 million vaccinated people in the UK showed that the risks of thrombocytopenic events were much higher following a COVID infection, compared with any COVID-related vaccine.
From that study, the British Heart Foundation describe how for every 10 million people who are vaccinated with AstraZeneca, there are 66 extra cases of blood clots in the veins and seven extra cases of a rare type of blood clot in the brain. By comparisons, infection with COVID is estimated to cause 12,614 extra cases of blood clots in the veins and 20 cases of rare blood clots in the brain.
To put this into some perspective, these vaccine-associated blood clot rates are much lower than many widely prescribed medicines. For example, the combined contraception pill , prescribed widely to women, has blood clot-related risks of around one in 1,000. With women taking postmenopausal hormone therapy, around one in 300 per year are likely to develop a blood clot.
Poor public profile
The AstraZeneca vaccine did suffer from a poor public profile, arguably much of it undeserved. There was some poor quality reporting in Germany in January 2021, with claims that the vaccine was only “8% effective in the elderly”. This claim was widely repeated, but it turns out that 8% figure referred to the percentage of people aged over 65 years in the study and not the efficacy measure.
The antivaccine lobby had a field day with fuelling the “infodemic” , including other false claims such as fabricated links between the vaccine and female infertility. As with the blood clots, COVID infection is known to increase the risks of infertility , but there is no link between infertility and the vaccine.
For individuals and families likely to have been injured by any medicine, including any of the COVID vaccines, compensation schemes are available. Many claimants report difficulties and frustrations with accessing the compensation. This is an area where the government-led schemes should be more transparent, and also where the misinformation from the anti-vaccine lobby hinders those groups they are claiming to support.
So, why would AstraZeneca withdraw this high-profile product? One reason for the withdrawal is likely to be that other COVID vaccines, such as Pfizer and Moderna, are essentially better products.
AstraZeneca is very good, but the mRNA versions have better effectiveness and safety levels.
Read more: Our new vaccine could protect against coronaviruses that haven’t even emerged yet – new study
The initial concerns around the difficulties of the specialist refrigeration needed to transport and store the Pfizer and Moderna vaccines have been overcome, including in low-income countries. The mRNA vaccines are also easier to update when new variants emerge.
With those factors, orders for the AstraZeneca vaccine are probably much lower now than they were in previous years. It is being overlooked in favour of better-performing vaccines.
For the Oxford AstraZeneca vaccine, perhaps its time has indeed passed. But it has been a safe and effective vaccine and a key part of the pandemic response for most countries around the world.
Correction. The sentence that read: It is well established that COVID itself caused a significantly increased risk of these related blood clots (thrombocytopenia). Now says: It is well established that COVID itself caused a significantly increased risk of these related blood clots and also thrombocytopenia (low platelet count).
- AstraZeneca vaccine
- COVID-19 pandemic
- Audio narrated
- mRNA vaccines
- vaccine adverse events

Case Management Specialist

Lecturer / Senior Lecturer - Marketing

Assistant Editor - 1 year cadetship

Executive Dean, Faculty of Health

Lecturer/Senior Lecturer, Earth System Science (School of Science)
- New Hampshire
- North Carolina
- Pennsylvania
- West Virginia
- Online hoaxes
- Coronavirus
- Health Care
- Immigration
- Environment
- Foreign Policy
- Kamala Harris
- Donald Trump
- Mitch McConnell
- Hakeem Jeffries
- Ron DeSantis
- Tucker Carlson
- Sean Hannity
- Rachel Maddow
- PolitiFact Videos
- 2024 Elections
- Mostly True
- Mostly False
- Pants on Fire
- Biden Promise Tracker
- Trump-O-Meter
- Latest Promises
- Our Process
- Who pays for PolitiFact?
- Advertise with Us
- Suggest a Fact-check
- Corrections and Updates
- Newsletters
Get PolitiFact in your inbox.
- Weekly Email Newsletter
- Daily Email Newsletter
- Government Regulation
- Public Health
- Facebook Fact-checks
- Bret Weinstein

The World Health Organization’s pandemic plan won’t end free speech
If your time is short.
A draft of the World Health Organization’s pandemic accord says that the document will be used with respect to individual’s personal freedoms.
An expert told PolitiFact that the accord could neither change nor supersede the U.S. Constitution.
As the world emerged from a global pandemic, the World Health Organization began drafting a legal agreement to respond to future pandemics. Since then, the document has been a target of misinformation.
The WHO’s pandemic prevention, preparedness and response accord is a legal agreement the organization’s 194 member states, including the U.S., are negotiating to help prevent and better prepare for future pandemics.
In a clip from former Fox News anchor Tucker Carlson’s web show, author Bret Weinstein warned the WHO’s actions with regard to the accord could strip Americans of their constitutionally protected rights to free speech.
"So, you’re saying that an international health organization could just end the First Amendment?" Carlson asked Weinstein in the clip, which circulated Jan. 28 in an Instagram video and was attracting comments and interactions in late April.
"The ability to do it is currently under discussion at the international level," replied Weinstein, whose COVID-19 claims PolitiFact has previously fact - checked.
The Instagram post was flagged as part of Meta’s efforts to combat false news and misinformation on its News Feed. (Read more about our partnership with Meta , which owns Facebook and Instagram.)
The clip came from a video published Jan. 5 on the subscription-based Tucker Carlson Network website. The network also shared a longer clip of this portion of the video on its YouTube page .
The longer version shows a fuller exchange:
Carlson: "So, you’re saying that an international health organization could just end the First Amendment?"
Featured Fact-check

Weinstein: "Yes, and I know it sounds preposterous — "
Carlson: "It does not sound preposterous." Weinstein: "The ability to do it is currently under discussion at the international level."
Weinstein later said the WHO’s pandemic preparedness plan will be used to silence podcasters and eliminate " national and personal sovereignty ." Weinstein did not respond to PolitiFact’s request for comment.
But his assertion that the WHO’s work on this plan could eliminate Americans’ free speech protections is contradicted by the U.S. Constitution and the draft accord itself.
A March 28 WHO press release said the pandemic agreement’s draft will continue to be refined ahead of the World Health Assembly , set for May 27 to June 1 in Geneva, Switzerland. An April draft of the plan explicitly stated that the plan’s implementation will be with "full respect for the dignity, human rights and fundamental freedoms of persons" and that states have the sovereign right" to "adopt, legislate and implement legislation."
World Health Organization information also details that the governments themselves would determine the accord, with member states deciding the terms.
Lawrence Gostin, director of Georgetown University’s O’Neill Institute for National and Global Health Law, told PolitiFact that the pandemic accord contains no provision that would override any U.S. law.
"The Pandemic Agreement would not control what could or could not be written or said in the United States," Gostin said. "The regulation of speech, including online content, is entirely within the realm of the US Congress." He added that there is a domestic process for amending the constitution.
The process of changing the U.S. Constitution is lengthy . To eliminate the First Amendment, Congress would have to propose the change with a majority vote in both the House of Representatives and the Senate. An amendment can also be proposed during a constitutional convention called for by two-thirds of the state legislatures . For the amendment to be adopted, three-fourths of the states in the U.S would have to ratify it.
We rate the claim that the World Health Organization could "end the first amendment" False.
Read About Our Process
The Principles of the Truth-O-Meter
Our Sources
Instagram video ( archived ), Jan. 28, 2024
PolitiFact, No sign that the COVID-19 vaccines’ spike protein is toxic or ‘cytotoxic’ , June 16, 2021
PolitiFact, COVID-19 vaccines saved lives, did not cause 17 million deaths , Jan. 17, 2024
YouTube, Big Pharma HATES these podcasts. Here’s Why. , Jan. 7, 2024
World Health Organization, Proposal for the WHO Pandemic Agreement, April 22, 2024,
World Health Organization, Pandemic prevention, preparedness and response accord , June 28, 2023
PolitiFact, WHO pandemic accord doesn’t replace U.S. sovereignty , Feb. 21, 2023
PolitiFact, Explaining Ron DeSantis’ effort to call a convention of states and amend the US Constitution , Feb. 1, 2024
Tucker Carlson Network, The Tucker Carlson Encounter: Bret Weinstein , Jan. 5, 2024
World Health Organization, Governments agree to continue their steady progress on proposed pandemic agreement ahead of the World Health Assembly , May 10, 2024
World Health Organization, WHO Member States agree to resume negotiations aimed at finalizing the world’s first pandemic agreement , March 28, 2024
National Archives, Constitutional Amendment Process , accessed May 13, 2024
Email interview, Lawrence Gostin, Professor of Global Health Law, Georgetown Law School, May 13, 2024
Browse the Truth-O-Meter
More by sofia ahmed.

Support independent fact-checking. Become a member!
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- World J Diabetes
- v.14(5); 2023 May 15
- PMC10236999
COVID-19 vaccination and diabetic ketoacidosis
Academic Center, Sanitation1 Medical Academic Center, Bangkok 1033300, Thailand. moc.liamtoh@boojyueb
Viroj Wiwanitkit
Community Medicine, DY Patil Vidhyapeeth, Pune 233230, India
Corresponding author: Beuy Joob, PhD, Adjunct Associate Professor, Academic Center, Sanitation1 Medical Academic Center, Bangkok 1033300, Thailand. moc.liamtoh@boojyueb
An efficient coronavirus disease 2019 (COVID-19) vaccine is urgently required to fight the pandemic due to its high transmission rate and quick dissemination. There have been numerous reports on the side effects of the COVID-19 immu-nization, with a focus on its negative effects. Clinical endocrinology is extremely interested in the endocrine issue that arises after receiving the COVID-19 vaccine. As was already mentioned, after receiving the COVID-19 vaccine, many clinical problems could occur. Additionally, there are some compelling reports on diabetes. After receiving the COVID-19 vaccine, a patient experienced hyperosmolar hyperglycemia state, a case of newly-onset type 2 diabetes. There has also been information on a potential connection between the COVID-19 vaccine and diabetic ketoacidosis. Common symptoms include thirst, polydipsia, polyuria, palpitations, a lack of appetite, and weariness. In extremely rare clinical circumstances, a COVID-19 vaccine recipient may develop diabetes complications such as hyperglycemia and ketoacidosis. In these circumstances, routine clinical care has a successful track record. It is advised to give vaccine recipients who are vulnerable to problems, such as those with type 1 diabetes as an underlying illness, extra attention.
Core Tip: There has also been information on a potential connection between the coronavirus disease 2019 (COVID-19) vaccine and diabetic ketoacidosis. Common symptoms include thirst, polydipsia, polyuria, palpitations, a lack of appetite, and weariness. In extremely rare clinical circumstances, a COVID-19 vaccine recipient may develop diabetes complications such as hyperglycemia and ketoacidosis.
INTRODUCTION
Because of the pandemic's high transmission rate, an effective coronavirus disease 2019 (COVID-19) vaccine is urgently needed[ 1 ]. The available literature indicates that both vaccines help prevent severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. However, given that the vaccination is new, any potential side effects are of greater concern[ 2 - 3 ]. When a handful of novel vaccines created in response to the COVID-19 pandemic got emergency approval and were widely distributed in late 2020[ 2 ], pharmacovigilance was unwittingly thrust into the spotlight. An effective global post marketing safety surveillance system was emphasized due to the employment of cutting-edge technologies and the anticipated rapid and widespread deployment of the vaccinations. The vaccinations went through extensive clinical evaluation and regulatory authority review. Many reports on the adverse effects of the COVID-19 vaccination have focused on how diverse they are. Clinical endocrinology is quite concerned about the endocrine issue that manifests after receiving the COVID-19 vaccination. The main concern expressed by the authors of this paper is that diabetes can become a medical problem after receiving the COVID-19 vaccine. After getting the COVID-19 vaccination, numerous clinical issues could arise, as was already mentioned. There are also some interesting reports regarding diabetes. The key words are provided here with a brief explanation.
Diabetes and COVID-19 have a well-established association. There is a bidirectional causal relationship between COVID-19 and type 2 diabetes. Diabetes may exacerbate COVID-19 severity, and COVID-19 vulnerability may increase diabetes risk[ 4 ]. Diabetes patients should receive the COVID-19 vaccine, just like everyone else, to protect themselves from the disease. It is critical to discuss the risks of vaccination for those who currently have diabetes mellitus. Piccini et al [ 5 ] evaluate the likelihood of glycemic control modification, insulin dose adjustment, and adverse effects following COVID-19 vaccination in young people with type 1 diabetes who use varying degrees of technology[ 5 ]. Piccini et al [ 5 ] came to the conclusion that receiving the OVID-19 immunization did not significantly increase the risk of glycemic control disturbance in type 1 diabetes adolescents and young adults[ 5 ]. This information may be helpful clinically[ 6 ] when counseling families about the SARS-CoV-2 vaccine for young people with type 1 diabetes. In a study by D'Addio et al [ 6 ] that investigated the immunogenicity and security of SARS-CoV-2 mRNA vaccines, a cohort of individuals with type 1 diabetes took part[ 5 ]. The vaccination demonstrated both dependability and security, according to D'Addio et al [ 6 ].
Several reports claim that COVID-19 vaccine recipients have problems with their diabetes. The exacerbation of hyperglycemia in people with type 2 diabetes after receiving the COVID-19 vaccination is the first problem that needs to be addressed[ 7 ]. Mishra et al [ 7 ] claim that an early inflammatory reaction to the vaccine and a subsequent immunological response are likely to be the causes of a minor and transient rise in blood sugar levels[ 7 ]. Mishra et al [ 7 ] published a case series that substantiated the etiology of transient immuno-inflammation because all episodes of hyperglycemia were self-limited and did not require significant treatment modifications[ 7 ]. A rapid jump in blood sugar levels appears to be caused by a vaccine. The possibility of a mild to moderate rise in blood sugar levels following vaccination has been theorized[ 7 ]. One patient experienced new-onset type 2 diabetes after receiving the COVID-19 vaccine, which is known as hyperosmolar hyperglycemia state[ 8 ].
COVID-19 VACCINATION AND DIABETIC KETOACIDOSIS
Clinical diabetology has an intriguing discussion regarding the COVID-19 vaccine and diabetic ketoacidosis. As was already indicated, the immunization may cause hyperviscosity and have unintended side effects. Additionally, reports of a connection between the COVID-19 immunization and diabetic ketoacidosis have been made. Three days after the first dose of COVID-19 RNA-based vaccines, the patient typically experiences thirst, polydipsia, polyuria, palpitations, a lack of appetite, and exhaustion without a prior history of diabetes[ 9 ]. Hyperglycemia, anion gap metabolic acidosis, and ketonuria are the three main signs of classic diabetic ketoacidosis[ 9 ]. It is possible to detect insulin autoantibody positivity and latent thyroid autoimmunity[ 10 ]. Ganakumar et al [ 11 ] advised that people with diabetes, particularly those with type 1 diabetes mellitus and inadequate glycemic control, be constantly monitored for hyperglycemia and ketonemia for at least two weeks after receiving the COVID-19 vaccine[ 11 ]. Autoimmunity and genetic predisposition may have contributed to the onset of the disease, even if the precise pathophysiologic mechanisms underlying type 1 diabetes are still unknown[ 12 ].
According to Tang et al [ 12 ], vaccination could result in type 1 diabetes, irreversible islet beta cell loss, and autoimmunity in persons with susceptible genetic backgrounds[ 12 ]. The problem might be more serious and more likely to occur in situations where type 1 diabetes is already present. Yakou et al [ 13 ] advised that the immunization be cautiously administered to type 1 diabetes patients receiving strict insulin therapy and a sodium-glucose transporter[ 13 ] due to the increased risk of ketoacidosis. In the affected case, despite hyperglycemia and diabetic ketoacidosis (DKA) after SARS-CoV-2 immunization, low glycohemoglobin levels are a crucial indicator of COVID-19 vaccine-related DKA[ 14 ]. As a preventive measure, it is essential to counsel patients to continue getting insulin injections[ 13 ]. Due to the significant risk of ketoacidosis, the vaccination should be cautiously given to type 1 diabetes patients receiving rigorous insulin therapy and a sodium-glucose transporter[ 15 ]. When a patient becomes ill, it's crucial to remind them to continue taking their insulin injections and to drink enough fluids[ 13 ]. A similar preventative concern should be used in the case of the patient with poorly controlled type 2 diabetes, in addition to the patient with underlying type 1 diabetes. According to Kshetree et al [ 15 ], Type I or dysglycemia in Type 2 diabetes mellitus is becoming more frequently documented following COVID-19 vaccinations or infection[ 16 ]. The mechanisms could be autoimmunity following mRNA vaccinations, cytokine-mediated beta-cell injury, or as a component of an autoimmune syndrome brought on by vaccine adjuvants[ 15 ]. Further investigation into the negative effects of people prone to life-threatening illnesses is required, as suggested by Lin et al [ 14 ]. Also, there might be a need for postvaccination surveillance on both hyperglycemia and DKA problems[ 16 ].
Concerning the reported cases of a link between COVID-19 vaccination and diabetes ketoacidosis, an important clinical question is whether ketosis in type 1 diabetes is related to the use of sodium-glucose transport protein 2 (SGLT2) inhibitors. The clinical history of the vaccine recipients in the published articles on the clinical association usually revealed no use of SGLT2 inhibitors, which could be a clue to support the possible clinical association between COVID-19 vaccination and ketoacidosis. Last but not least, it should be noted that the mRNA COVID-19 vaccine is primarily associated with most findings on the relationship between COVID-19 immunization and diabetic ketoacidosis. There are, however, a few reports of clinical associations with other vaccination types (viral vector and inactivated COVID-19 vaccines) that have been documented[ 11 ]. The fact that the mRNA vaccination is currently the primary recommended COVID-19 vaccine may be the cause of the higher number of reported cases in the mRNA vaccine group. As previously stated, the COVID-19 vaccination may cause diabetic ketoacidosis in patients with type 1 or type 2 diabetes mellitus (Table (Table1 1 ).
Table summarizing the key information of coronavirus disease-19 vaccine related diabetic ketoacidosis in recipients with background type 1 and type 2 diabetes mellitus
There are significant differences in COVD-19 vaccine-induced diabetes ketoacidosis between recipients with type 1 and type 2 diabetes. COVID-19 vaccine induced diabetes ketoacidosis usually occurs in adolescent male cases with inadequate glycemic control in cases with background type 1 diabetes mellitus[ 11 ]. This is the same pattern seen in diabetic ketoacidosis caused by COVID-19 in type 1 diabetes patients[ 17 ]. There are fewer reported cases of COVID-19 vaccine-induced diabetes ketoacidosis in people with type 2 diabetes mellitus, and the patient is usually an elderly man with a long history of diabetic illness[ 15 ]. The background hemoglobin A1C level, on the other hand, has not been identified as a risk factor for the development of COVID-19 vaccine-induced diabetic ketoacidosis[ 18 ].
In general, the COVID-19 immunization should be given to the diabetic patient because it has been proven to be effective. Generally, it has been confirmed that it is secure. In exceedingly uncommon clinical situations, a COVID-19 vaccination recipient may experience diabetes-related problems such as hyperglycemia and ketoacidosis. Routine clinical care has a history of success in some situations. Users of vaccines who are more likely to develop problems, such as those who already have type 1 diabetes as an underlying illness, are advised to receive additional attention. Because there is a possible link between the COVID vaccine and ketoacidosis, the risk diabetic case must be closely monitored. There is still a need for more clinical research on this subject because there isn't any in vivo or in vitro experimental data at this time.
Conflict-of-interest statement: All the authors report no relevant conflicts of interest for this article.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: December 15, 2022
First decision: January 17, 2023
Article in press: April 12, 2023
Specialty type: Endocrinology and metabolism
Country/Territory of origin: Thailand
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Cai L, United States; Dong Z, China; Moreno-Gómez-Toledano R, Spain; Wu QN, China; Zhang F, China S-Editor: Li L L-Editor: A P-Editor: Zhang XD
Contributor Information
Beuy Joob, Academic Center, Sanitation1 Medical Academic Center, Bangkok 1033300, Thailand. moc.liamtoh@boojyueb .
Viroj Wiwanitkit, Community Medicine, DY Patil Vidhyapeeth, Pune 233230, India.

Senate GOP fails to roll back Treasury’s ‘abuse’ of COVID-19 relief funds
Senate Republicans failed to overturn new regulations from the Biden administration that give states greater flexibility in using COVID-19 relief funds.
Last fall, the Treasury Department issued new rules allowing states to “obligate” legal and administrative expenses associated with the funds past an end-of-year deadline. Sen. Eric Schmitt (R-MO) sponsored a disapproval resolution to reverse that rule change, arguing the Biden administration was violating the expiration dates laid out in the American Rescue Plan.
But the Senate rejected his attempt to roll back the regulation in a party-line vote on Wednesday. Forty-six Republicans voted in favor, with 49 Democrats and independents opposed.
The American Rescue Plan, signed into law in 2021, allocated $350 billion for states and localities dealing with the effects of the coronavirus pandemic. The fund was geared toward preserving government services but also the construction of broadband and other infrastructure.
What’s left three years later can continue to be obligated through the end of 2024. It must then be spent by 2026.
But Schmitt and other Republicans have taken issue with an exception to the 2024 deadline for qualified costs, namely compliance, record-keeping, and audit expenses that localities are allowed to estimate and then submit in the coming months.
In total, Schmitt calculates the rule change will cost the government $13 billion. “That's a lot of money; that's $1,200 for every American family,” he told reporters on Wednesday.
The resolution, which Democrats could not prevent from receiving a vote under the Congressional Review Act, feeds into common claims of waste and abuse by Republicans who want to claw back the COVID-19 relief funds.
The Treasury Department did not respond to a request for comment, but Sen. Ron Wyden (D-OR) argued from the Senate floor that the resolution could negatively affect thousands of projects nationwide.
CLICK HERE TO READ MORE FROM THE WASHINGTON EXAMINER
The White House issued a veto threat of the resolution Wednesday ahead of the vote, arguing repeal of the rule would "disrupt critical infrastructure and housing projects, risk layoffs of public safety workers, and create significant oversight gaps that could put taxpayer dollars at risk."
The resolution was just the latest CRA. Republicans have targeted everything from environmental to housing regulations crafted by the Biden administration under the law’s authority.

- Skip to main content
- Keyboard shortcuts for audio player
The huge solar storm is keeping power grid and satellite operators on edge

Geoff Brumfiel
Willem Marx

NASA's Solar Dynamics Observatory captured this image of solar flares early Saturday afternoon. The National Oceanic and Atmospheric Administration says there have been measurable effects and impacts from the geomagnetic storm. Solar Dynamics Observatory hide caption
NASA's Solar Dynamics Observatory captured this image of solar flares early Saturday afternoon. The National Oceanic and Atmospheric Administration says there have been measurable effects and impacts from the geomagnetic storm.
Planet Earth is getting rocked by the biggest solar storm in decades – and the potential effects have those people in charge of power grids, communications systems and satellites on edge.
The National Oceanic and Atmospheric Administration says there have been measurable effects and impacts from the geomagnetic storm that has been visible as aurora across vast swathes of the Northern Hemisphere. So far though, NOAA has seen no reports of major damage.

The Picture Show
Photos: see the northern lights from rare, solar storm.
There has been some degradation and loss to communication systems that rely on high-frequency radio waves, NOAA told NPR, as well as some preliminary indications of irregularities in power systems.
"Simply put, the power grid operators have been busy since yesterday working to keep proper, regulated current flowing without disruption," said Shawn Dahl, service coordinator for the Boulder, Co.-based Space Weather Prediction Center at NOAA.
NOAA Issues First Severe Geomagnetic Storm Watch Since 2005

- LISTEN & FOLLOW
- Apple Podcasts
- Google Podcasts
- Amazon Music
- Amazon Alexa
Your support helps make our show possible and unlocks access to our sponsor-free feed.
"Satellite operators are also busy monitoring spacecraft health due to the S1-S2 storm taking place along with the severe-extreme geomagnetic storm that continues even now," Dahl added, saying some GPS systems have struggled to lock locations and offered incorrect positions.
NOAA's GOES-16 satellite captured a flare erupting occurred around 2 p.m. EDT on May 9, 2024.
As NOAA had warned late Friday, the Earth has been experiencing a G5, or "Extreme," geomagnetic storm . It's the first G5 storm to hit the planet since 2003, when a similar event temporarily knocked out power in part of Sweden and damaged electrical transformers in South Africa.
The NOAA center predicted that this current storm could induce auroras visible as far south as Northern California and Alabama.
Extreme (G5) geomagnetic conditions have been observed! pic.twitter.com/qLsC8GbWus — NOAA Space Weather Prediction Center (@NWSSWPC) May 10, 2024
Around the world on social media, posters put up photos of bright auroras visible in Russia , Scandinavia , the United Kingdom and continental Europe . Some reported seeing the aurora as far south as Mallorca, Spain .
The source of the solar storm is a cluster of sunspots on the sun's surface that is 17 times the diameter of the Earth. The spots are filled with tangled magnetic fields that can act as slingshots, throwing huge quantities of charged particles towards our planet. These events, known as coronal mass ejections, become more common during the peak of the Sun's 11-year solar cycle.
A powerful solar storm is bringing northern lights to unusual places
Usually, they miss the Earth, but this time, NOAA says several have headed directly toward our planet, and the agency predicted that several waves of flares will continue to slam into the Earth over the next few days.
While the storm has proven to be large, predicting the effects from such incidents can be difficult, Dahl said.
Shocking problems
The most disruptive solar storm ever recorded came in 1859. Known as the "Carrington Event," it generated shimmering auroras that were visible as far south as Mexico and Hawaii. It also fried telegraph systems throughout Europe and North America.

Stronger activity on the sun could bring more displays of the northern lights in 2024
While this geomagnetic storm will not be as strong, the world has grown more reliant on electronics and electrical systems. Depending on the orientation of the storm's magnetic field, it could induce unexpected electrical currents in long-distance power lines — those currents could cause safety systems to flip, triggering temporary power outages in some areas.
my cat just experienced the aurora borealis, one of the world's most radiant natural phenomena... and she doesn't care pic.twitter.com/Ee74FpWHFm — PJ (@kickthepj) May 10, 2024
The storm is also likely to disrupt the ionosphere, a section of Earth's atmosphere filled with charged particles. Some long-distance radio transmissions use the ionosphere to "bounce" signals around the globe, and those signals will likely be disrupted. The particles may also refract and otherwise scramble signals from the global positioning system, according to Rob Steenburgh, a space scientist with NOAA. Those effects can linger for a few days after the storm.
Like Dahl, Steenburgh said it's unclear just how bad the disruptions will be. While we are more dependent than ever on GPS, there are also more satellites in orbit. Moreover, the anomalies from the storm are constantly shifting through the ionosphere like ripples in a pool. "Outages, with any luck, should not be prolonged," Steenburgh said.

What Causes The Northern Lights? Scientists Finally Know For Sure
The radiation from the storm could have other undesirable effects. At high altitudes, it could damage satellites, while at low altitudes, it's likely to increase atmospheric drag, causing some satellites to sink toward the Earth.
The changes to orbits wreak havoc, warns Tuija Pulkkinen, chair of the department of climate and space sciences at the University of Michigan. Since the last solar maximum, companies such as SpaceX have launched thousands of satellites into low Earth orbit. Those satellites will now see their orbits unexpectedly changed.
"There's a lot of companies that haven't seen these kind of space weather effects before," she says.
The International Space Station lies within Earth's magnetosphere, so its astronauts should be mostly protected, Steenburgh says.
In a statement, NASA said that astronauts would not take additional measures to protect themselves. "NASA completed a thorough analysis of recent space weather activity and determined it posed no risk to the crew aboard the International Space Station and no additional precautionary measures are needed," the agency said late Friday.

People visit St Mary's lighthouse in Whitley Bay to see the aurora borealis on Friday in Whitley Bay, England. Ian Forsyth/Getty Images hide caption
People visit St Mary's lighthouse in Whitley Bay to see the aurora borealis on Friday in Whitley Bay, England.
While this storm will undoubtedly keep satellite operators and utilities busy over the next few days, individuals don't really need to do much to get ready.
"As far as what the general public should be doing, hopefully they're not having to do anything," Dahl said. "Weather permitting, they may be visible again tonight." He advised that the largest problem could be a brief blackout, so keeping some flashlights and a radio handy might prove helpful.
I took these photos near Ranfurly in Central Otago, New Zealand. Anyone can use them please spread far and wide. :-) https://t.co/NUWpLiqY2S — Dr Andrew Dickson reform/ACC (@AndrewDickson13) May 10, 2024
And don't forget to go outside and look up, adds Steenburgh. This event's aurora is visible much further south than usual.
A faint aurora can be detected by a modern cell phone camera, he adds, so even if you can't see it with your eyes, try taking a photo of the sky.
The aurora "is really the gift from space weather," he says.
- space weather
- solar flares
- solar storm

IMAGES
COMMENTS
Amy Lunday. / Feb 21, 2022. As the United States approaches the second anniversary of its initial COVID-19 shutdowns, we're daring to dream about what the end of the pandemic might look like. With omicron cases plummeting, indoor mask mandates in every state but Hawaii are set to expire —a change that would have seemed unthinkable just weeks ago.
COVID-19 is a disease caused by a virus. The most common symptoms are fever, chills, and sore throat, but there are a range of others. ... Although WHO announced the end of the emergency phase of COVID-19 in May 2023, the Organization continues to coordinate the global response. Related. All information on COVID-19.
COVID-19 is a worldwide pandemic that puts a stop to economic activity and poses a severe risk to overall wellbeing. The global socio-economic impact of COVID-19 includes higher unemployment and poverty rates, lower oil prices, altered education sectors, changes in the nature of work, lower GDPs and heightened risks to health care workers.
COVID-19 is caused by a coronavirus known as severe acute respiratory syndrome coronavirus 2 ().The disease is transmitted primarily through contact with infectious material, particularly respiratory droplets that enter the environment when an infected person sneezes or coughs. Individuals nearby may inhale or come into contact with these droplets, resulting in disease transmission.
COVID-19 is the disease caused by a coronavirus called SARS-CoV-2. WHO first learned of this new virus on 31 December 2019, following a report of a cluster of cases of so-called viral pneumonia in Wuhan, People's Republic of China.
At the end of 1920, 1.7% of the world's people had expired of this illness, including an exceptionally high death rate for young adults aged between 20 and 40 years. In contrast to the Spanish flu, coronavirus is not so common, has caused in fewer fatalities, has a higher case fatality rate, is more harmful to older ages and is less risky for ...
COVID-19 (coronavirus disease 2019) is a disease caused by a virus named SARS-CoV-2. It can be very contagious and spreads quickly. Over one million people have died from COVID-19 in the United States. COVID-19 most often causes respiratory symptoms that can feel much like a cold, the flu, or pneumonia. COVID-19 may attack more than your lungs ...
Coronavirus disease (COVID-19) Coronavirus disease (COVID-19) is an infectious disease caused by the SARS-CoV-2 virus. Most people infected with the virus will experience mild to moderate respiratory illness and recover without requiring special treatment. However, some will become seriously ill and require medical attention.
What does have a formal meaning is a "public health emergency of international concern" — a status assigned to COVID-19 at the end of January 2020. That's the highest level of health alarm under ...
The COVID-19 pandemic, also known as the coronavirus pandemic, is a global pandemic of coronavirus disease 2019 (COVID-19) ... In May 2022, the WHO estimated the number of excess deaths by the end of 2021 to be 14.9 million compared to 5.4 million reported COVID-19 deaths, with the majority of the unreported 9.5 million deaths believed to be ...
The 'end' of COVID-19 might mean the point at which is can be managed as an endemic disease; however, the emergence of a significant new variant is the greatest risk which could hinder this. The data shown in the piece was correct as of 23/08/21. Since the March installment in this series, many countries, including the United States, Canada ...
14 September 2022 Health. As the number of weekly reported deaths from COVID-19 plunged to its lowest since March 2020, the head of the World Health Organization (WHO) said on Wednesday that the end of the pandemic is now in sight. "We have never been in a better position to end the pandemic", Tedros Adhanom Ghebreyesus told journalists ...
COVID-19 claimed nearly 7 million lives worldwide. In the United States, deaths from COVID-19 exceeded 1.1 million, ... By the end of the pandemic in early 2023, more than 670 million doses of ...
The COVID-19 pandemic is far from over and could yet evolve in unanticipated ways, but one of its most important lessons is already clear: preparation and early execution are essential in ...
Conclusion. This research has captured the diversity and complexity of people's experiences. ... there is still concern about the longer term harm and disruption that COVID-19 has caused to people and communities, and worry about the threat of future waves of infection. This report captures a number of specific suggestions for support. For ...
That's exactly right. And some scientists are starting to think that eventually, over time, COVID may turn into something similar to a type of disease like these other coronaviruses - a seasonal ...
Since it began, COVID-19 has spread worldwide, leading the WHO to label it a pandemic and a "public health emergency of international concern.". Based on available evidence, COVID-19 appears to have a fatality rate of 4.4%, much lower than 10% for SARS and around 30% for MERS-CoV. Yet this is not a reason to relax containment and control ...
Key Events in the Effort to Determine the Origins of the Covid-19 Pandemic. The joint WHO-China technical report published in March 2021 rated a zoonotic spillover as a "likely to very likely ...
The COVID-19 pandemic has led to a dramatic loss of human life worldwide and presents an unprecedented challenge to public health, food systems and the world of work. The economic and social disruption caused by the pandemic is devastating: tens of millions of people are at risk of falling into extreme poverty, while the number of ...
The coronavirus disease 2019 (COVID-19) pandemic is a global outbreak of coronavirus - an infectious disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Cases of novel coronavirus (nCoV) were first detected in China in December 2019, with the virus spreading rapidly to other countries across the world.
March 30, 2021. • 5 min read. A World Health Organization report released today says that SARS-CoV-2, the virus that causes COVID-19, most likely leapt from animals to humans through an emissary ...
Conclusion. The COVID-19 pandemic demonstrates that every country remains vulnerable to public health emergencies. The aspiration towards a healthier and safer society requires that countries develop and implement a coherent and context-specific national strategy, improve governance of public health emergencies, build the capacity of their ...
That means with the COVID-19 PHE ending on May 11, 2023, this mandatory coverage will end on September 30, 2024, after which coverage may vary by state. The requirement for private insurance companies to cover COVID-19 tests without cost sharing, both for OTC and laboratory tests, will end at the expiration of the PHE.
On March 11, 2020, the World Health Organization for the first time called COVID-19 a pandemic. "We have rung the alarm bell loud and clear," Tedros Adhanom Ghebreyesus, WHO director-general, said ...
Before Covid-19 emerged, a US government grant to EcoHealth had funded studies into bat coronaviruses at the lab in Wuhan, China. Although US-funded research at the lab has not been linked to the ...
The Oxford-AstraZeneca vaccine was a critical part of the COVID-19 pandemic response. However, on May 7 2024, the European Commission announced the vaccine is no longer authorised for use. This EU ...
PolitiFact, No sign that the COVID-19 vaccines' spike protein is toxic or 'cytotoxic', June 16, 2021 PolitiFact, COVID-19 vaccines saved lives, did not cause 17 million deaths , Jan. 17 ...
CONCLUSION. In general, the COVID-19 immunization should be given to the diabetic patient because it has been proven to be effective. Generally, it has been confirmed that it is secure. In exceedingly uncommon clinical situations, a COVID-19 vaccination recipient may experience diabetes-related problems such as hyperglycemia and ketoacidosis ...
Senate Republicans failed to overturn new regulations from the Biden administration that give states greater flexibility in using COVID-19 relief funds. Last fall, the Treasury Department issued ...
The huge solar storm is keeping power grid and satellite operators on edge. NASA's Solar Dynamics Observatory captured this image of solar flares early Saturday afternoon. The National Oceanic and ...