An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Community Hosp Intern Med Perspect
- v.7(1); 2017 Jan


The role of medical education in the development of the scientific practice of medicine
Lucien cardinal.
a Department of Internal Medicine , Stony Brook University School of Medicine , New York, NY, USA
b John T. Mather Memorial Hospital , Port Jefferson, NY, USA
The authors describe the important role of medical schools and graduate medical education programs (residencies) in relationship to the advances in Medicine witnessed during the twentieth century; diagnosis, prognosis and treatment were revolutionized. This historical essay details the evolution of the education system and the successful struggle to introduce a uniform, science-based curriculum and bedside education. The result was successive generations of soundly educated physicians prepared with a broad knowledge in science, an understanding of laboratory methods and the ability to practice medicine at the bedside. These changes in medical education created a foundation for the advancement of medicine.
During the last 150 years tremendous advances have taken place in the field of medical education. The product of these changes has been the development of physicians who have become progressively scientific in their mode of thought and practice over time. These physicians have been increasingly at the forefront of medicine, incorporating advances in every scientific field into the delivery of healthcare. A systematic and structured educational curriculum was created; this allowed the medical profession to train, through its educational institutions, physicians with the knowledge, skills and attitudes necessary for the scientific practice of medicine. Physicians were graduated with the capacity to study scientific advances, to interpret these advances relative to medicine and to incorporate pertinent elements into their medical practice. The practice of medicine today, contrasted with a century ago, has undergone a metamorphosis that could not have been predicted by the typical American medical graduate of 1900. Medicine has moved from a field based on dogma to one based on fact derived through scientific investigation and clinical observation.
Prior to the twentieth century there existed a plethora of theories explaining health and disease, each one of which conflicted with the other. After 1900 scientific medicine began to be practiced on the wards of several prestigious institutions, yet sectarianism and dogmatism continued to assert itself in the offices of the general practitioner for at least another 30 years, represented by such teachings as homeopathy, naturopathy, eclecticism and abramsism.[ 1 ] Each dogma proposed foundational principles of practice, closed to modification based on observation. There were 22 US homeopathic medical colleges in 1900; Boston University School of Medicine, Hahnemann School of Medicine in Philadelphia (now Drexel), and the New York Homeopathic Medical College (now the New York Medical College) are three examples of schools that were founded on homeopathic principles, later to continue successfully as scientifically based institutions.[ 2 ]
By the dawn of the twentieth century scientific thought and scientific medicine had taken deep root in Germany. However, in the USA the average physician still practiced medicine based largely on the fallacious dogmatic ipse dixits of the particular theory of human health and disease to which the physician subscribed. Most medical school curricula did not include or support the scientific method or attempt to bolster their teachings with the results of experimentation. The unthinking acceptance of dogma was immortalized in William Cowper’s poem, The Task.
Books are oft times talismans and spells , 1 By which the magic art of shrewder wits Holds an unthinking multitude enthrall’d. [ 3 ]
As early as the middle of the nineteenth century, a group of progressive medical leaders began to emerge in the USA. They recognized the need for advancement and advocated for political initiatives. In 1846 the Medical Society of the State of New York called for a national medical organization to be formed, stating that it ‘would be conducive to the elevation of the standard of medical education in the United States.’(p. 4). [ 4 ] This organization was founded as the American Medical Association (AMA) in the following year. Its constitution stated the following as central to its purpose: ‘cultivating and advancing medical knowledge’ and ‘elevating the standard of medical education.’ (p. 2). [ 5 ] Change did not come quickly over the next 50 years, so that in 1902 Dr John Wyeth, president of the AMA, astutely appointed a Committee on Medical Education. The following year, that committee restated under the ‘First Objective of the AMA’ that the organization was ‘formed for the purpose of elevating the standard of medical education.’[4] Sir William Osler, often referred to as the father of Internal Medicine, heralded the changes to come when he stated ‘A new school of practitioners has arisen … It seeks to study, rationally and scientifically …’ the practice of medicine.[ 6 ]
In the early years (1850–1900) medical schools in America, with a few exceptions, stood independent from universities and were proprietary in nature. These two factors tended to isolate the field of medicine from the other sciences. The most advanced medical schools were abroad and were part of established universities. German universities, with centers of learning in Vienna and Berlin, were held in high regard. American physicians frequently traveled to Germany, France and England to advance their post-graduate medical education. On returning home they emulated the practices of institutions they encountered abroad.[ 7 ] Henry P. Bowditch studied in Leipzig and was influenced by the physiological laboratory of Carl Ludwig. He subsequently developed the Institute for Experimental Medicine at Harvard, the first laboratory of its kind in the USA. Similarly, William Henry Welch studied with Ludwig and later went on to become the dean of the Johns Hopkins Medical School and one of the founding physicians of its hospital. He wrote ‘I hope that the Johns Hopkins … will be able to introduce German methods.’[ 8 ] In the early 1900s US physicians were handicapped because the leading medical journals were overwhelmingly in German and not available in the western hemisphere. Several quality US journals were founded in the 1800s and early 1900s to disseminate the findings of medical research. The American Journal of Medical Sciences, a well-respected journal in the USA and Europe, was established by Dr Isaac Hays in 1827. Hays is also credited with the preparation of the Code of Ethics of the AMA. The Journal of the American Medical Association was founded in 1883,[ 9 ] and in 1908 Heinrich Stern founded the Archives of Diagnosis, a leading medical journal of its time.[ 10 ] After attending a conference of the Royal College of Physicians in London in 1913, Stern returned intent on establishing a similar organization. He subsequently founded the American College of Physicians with the intent that it would foster the exchange of scientific information between physicians.[ 11 ]
Standards for admission to an American medical school were lax; a high school diploma was finally mandated in 1905.[ 4 ] New York, through the Department of Education, was one of the few states to require a high school diploma as a prerequisite for medical school admission. Harvard did not require a baccalaureate as a prerequisite until 1901.[ 12 ] Medical schools by and large were two-year programs devoted to bookwork with little exposure to patients at the bedside. The student had little personal contact with the professor, and education was often restricted to lectures heard in an educational amphitheater. Patients were sometimes wheeled in to demonstrate some aspect of medicine to the student.
In 1910, the Carnegie Foundation released a bulletin on medical education in the USA, authored by Abraham Flexner. It became known as the Flexner Report and was regarded as an accurate description of the low standards in medical education at the time. Advocates for the advancement of medical education used it to encourage change. Flexner detailed, over 346 pages, the lack of a systematic and unified approach to medical education, the absence of suitable premedical education and minimal patient-based learning. He also described the factors responsible for the situation and made suggestions for corrective action. Interestingly, Flexner singled out the specialty of Internal Medicine for praise, describing it as the backbone of clinical teaching. He went on to cite another author, quoting ‘… Internal Medicine is regarded as the mother of all other clinical divisions.’[ 13 ]
Over the subsequent 30 years the educational landscape slowly began to succumb to the forces of change. Medical schools defined required premedical coursework, extended the duration of study to four years and incorporated a science-based curriculum.[ 12 , 14 ] They affiliated with universities and teaching hospitals, creating clinical clerkships during the last two years of medical school, allowing students patient-based experiences at the bedside.[ 15 ] Schools that could not accommodate these changes were closed.
Additionally, and importantly, after medical school physicians began to commit themselves to additional specialized educational training by attending hospital-based residencies. Widespread adoption of half-year or single-year internships came quickly, but longer programs of organized training were uncommon. The Johns Hopkins Hospital was established along the lines of the German medical clinics, incorporating full-time professors (‘full-time system’), bedside teaching, clinical observation and laboratory science.[ 16 ] It also incorporated organized multi-year training. It opened its doors on 6 May 1889 and on 15 May admitted its first patient, a case of aortic aneurysm. This was the first patient to receive hospital-based care directly by graduate trainees who were part of an organized multi-year residency program.[ 17 ] Trainees were encouraged to evaluate the impact of treatment and effectiveness of diagnostic tests directly at the bedside. Such proof of action is one aspect of the scientific method. No longer would treatment and diagnosis be based solely on theory. Thus, graduate medical education (GME) was born. Osler, Professor of Medicine at Johns Hopkins, felt that his role in the development of GME was his most important contribution to medicine.[ 18 ] Despite this early development of a modern residency program at Johns Hopkins, medical educators in the USA did not rapidly establish many other multi-year residencies. This is primarily thought to be due to their focused efforts initially to establish rigorous and reputable medical schools, and later the interruptions of World Wars I and II. In lieu of a residency in a medical specialty a physician could attend a condensed course at a so-called post-graduate medical college. These courses were often only weeks in duration. In 1914 there were 17 post-graduate medical schools in the USA, five each in New York and Illinois.[ 19 ] In 1934 the state of Pennsylvania still had only five residency programs of three years or more in length registered with the AMA’s Council on Graduate Medical Education.[ 14 ] Multi-year residency programs preparing physicians for specialization were widely disseminated during the 10 years following the close of World War II.
The advances in medical education and the establishment of graduate medical education stand out as the most important developments in medicine in the last 150 years. They led to the graduation of successive generations of competent physicians, grounded in the scientific practice of medicine. Their openness to discoveries in all fields of science has allowed, with each passing year, for the expansion of medicine to ever-broader horizons.
Disclosure statement
No potential conflict of interest was reported by the authors.
- Search Menu
- Advance articles
- Author Guidelines
- Submission Site
- Open Access
- Why Publish with JHMAS?
- About Journal of the History of Medicine and Allied Sciences
- Editorial Board
- Advertising and Corporate Services
- Self-Archiving Policy
- Dispatch Dates
- Terms and Conditions
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Organization and outline of essays, remaking the case for history in medical education.
- Article contents
- Figures & tables
- Supplementary Data
Jacob Steere-Williams, Justin Barr, Claire D Clark, Raúl Necochea López, Remaking the Case for History in Medical Education, Journal of the History of Medicine and Allied Sciences , Volume 78, Issue 1, January 2023, Pages 1–8, https://doi.org/10.1093/jhmas/jrac049
- Permissions Icon Permissions
In a 2015 essay titled “Making the Case for History in Medical Education” in the Journal of the History of Medicine and Allied Sciences, David Jones, Jeremy Greene, Jacalyn Duffin, and John Harley Warner issued a challenge for historians of medicine. “In a world where many interests make demands for curriculum time and attention,” they argued, “historians of medicine need a more aggressive strategy.” 1 The article has since been one of the most frequently cited in the history of medicine. It was also a sign of the times. The authors pointed to repeated and ongoing efforts of clinicians and historians to integrate medical history into medical schools. They surveyed the wide range of arguments historians have made over the decades: how history buttresses a sense of professional identity, fosters holistic examinations of disease, and cautions against misguided practice.
But as our colleagues lamented in 2015, these potent rationales for medical history have not been altogether convincing enough to effect meaningful curricular change in medical education. Medical school administrators decry a lack of time in the curriculum for medical history, other disciplines fiercely compete for resources across medical schools, and historians sometimes struggle to translate the field in meaningful ways to medical students.
Many of these concerns, of course, are not new. In the first issue of this journal in 1946, George Rosen wrote the landmark essay, “What Is Past, Is Prologue,” lamenting that for seventy-five years the medical profession had “turned away from the history of medicine.” 2 Rosen identified two reasons: structural changes in medical education resulting from the specialization of American medicine in the early twentieth century; and, the failure of historians of medicine to make “medical history the living, dynamic thing that,” in his words, “we believe it to be.” “We do not want to cultivate medical history as a mere search for antiquities,” he concluded, “but rather as a vital, integral part of medicine.” 3
In their 2015 essay Jones et al. were re-stating a claim made by historians of medicine from the middle decades of the twentieth century, that medical history is an essential part of medical practice. As Rosen, Henry Sigerist, and Erwin Ackerknecht had argued seventy years prior, Jones et al. warned against the idea of a history of medicine that simply studies health and healing in the past for its own sake. Instead, they argued, medical history must be understood, communicated, and taught, as an “essential component of medical knowledge, reasoning, and practice.” Critically couching their case in this way, within the contemporary lexicon of competencies and entrustable professional activities, our colleagues in 2015 argued that medical history might be reframed as contributing to medical education in the same way anatomy, biochemistry, or pathophysiology do. 4 Seeing the striking similarities between Rosen in 1946 and Jones et al. in 2015, despite the vast changes in medical education in that time span, begs for a serious and ongoing reflection about the ways in which we communicate the value of the history of medicine to diverse public and professional audiences.
To the immense benefit of the field, Jones et al. in 2015 went beyond praising the virtues of the history of medicine to offer strategic resources for historians. They listed over a dozen distinct ways that history can directly contribute to medical education, including elucidating the social factors that shape health and illness, unpacking the cultural construction of disease categories, and addressing the imbalances of power, race, and gender in clinical care. Our colleagues implored historians of medicine to face curricular change in medical schools in creative ways that align with dominant approaches in medical education.
Competency-Based Medical Education (CBME) is the most important approach to clinical pedagogy in the US and Canada. Billed by the American Association of Medical Colleges (AAMC) since the late 1990s as a way to address the evolving needs of the health care system, CBME now establishes what observable abilities medical learners must display to be deemed competent clinicians. Given the ubiquity of the language of competencies, Jones et al. offered pragmatic advice to make the case for history of medicine in those terms. Their advice has aged well, though some qualifications are worth mentioning based on experiences of the last few years. CBME, while still the dominant approach to assessment in the US and Canada, has been criticized on empirical and theoretical grounds. 5 As with other educational activities, it is not simple to demonstrate direct causal links between historical learning and better doctoring. It behooves us, therefore, to support research that evaluates our contributions to the education of clinicians, and not only to assert our convictions regarding what we bring to the competencies table. In addition, two decades into the competencies regime, historians are no longer naive about the weight of educational leadership positions within our institutions. Curriculum reform leaders have privileged perches from which to identify insufficient pedagogical content, faculty development lacunae, and assessment needs that historical knowledge and methods can fulfill, particularly when it comes to areas such as systems-based practice and medical knowledge. There is no reason why historians should shy away from seeking these responsibilities. Furthermore, the cyclical nature of reviews by the Accreditation Council for Graduate Medical Education (ACGME) suggests that promoting change may be especially welcome in the period leading up to these institutional visits, and necessary in the period immediately following them. Our competency-driven environments, in other words, call for vigorous new engagement with developments such as competency-based evaluations, health curricular reform, and institutional accreditations.
Of all the trends in competency-based education in the last decade or so, perhaps the one that has resonated most powerfully with historians is the movement toward “structural competency.” In an article published in 2014, Jonathan Metzl and Helena Hansen used the language of competencies to “argue that increasing recognition of the ways in which social and economic forces produce symptoms or methylate genes then needs to be better coupled with medical models for structural change.” 6 Since then, historians and social scientists have leveraged the framework of structural competency to make the case that some medical knowledge is structurally racist and that understanding the racist history of the production of medical knowledge is integral to anti-racist curriculum reform efforts. 7 Historians have been among the leading educators in anti-racist curriculum reform efforts by, for example, curating academically rigorous reading lists, embarking on oral history projects, and elucidating the ways in which history can and must be used to make sense of structural violence in medicine. 8
This Special Issue builds upon this critical foundation. Acknowledging Rosen’s charge in 1946, we also recognize the longer historical arc of generative conversations, in this journal and in the broader field, about the value and the struggle of teaching medical history in medical schools. Rather than retelling this complex history or reframing the nature of the debates at hand, this Special Issue has more modest aims. What you will find in the essays that follow is a medical historian’s toolbox, a survey of interesting and innovative practical examples of how a small sampling of colleagues across the world are pushing the boundaries for the integration of the history of medicine within clinical education. This Special Issue provides examples of successful initiatives and the logistical details of how to implement them at organizational and pedagogical levels, thus creating models for others to emulate. Spanning a range of creative ideas, collaborations, and institutions, the breadth of the essays in this issue of JHMAS promises something for historians of medicine in various institutional settings, in the hope of generating ongoing developments of Clio in the Clinic. 9
In providing a set of instructive examples, readers will notice two features in this collection of essays. First, we argue that sustainable change requires thinking about medical education and medical history at both local and global levels. To address the structural and ideological problems of integrating the history of medicine into medical education in fundamental ways, we must acknowledge local contexts as critical, but we also need to push beyond the idea that curricular change or administrator buy-in are uniquely North American phenomena. Our students, many of whom seek out clinical experiences outside the US and Canada, provide us with another reason why understanding global learning conditions and tensions is a worthwhile endeavor. The examples assembled in this Special Issue are thus global in scope. Second, we propose that the boundaries of clinical education must encompass more than just medical schools. Indeed, the essays in this Special Issue demonstrate the ways that an ontologically essential view of medical history can be incorporated for health professionals and aspiring health professionals at all levels. Broadening the spectrum of who we traditionally view as the learners of medical history expands the opportunities to teach the history of medicine and imbed the field into multiple audiences of clinical education and practice.
This Special Issue offers no radical rethinking of the value of medical history in medical education. We are, however, acutely aware of the ongoing evolution of medical education, and of the broader social and political climate of 2022 that marks a stark change from 2015 when the journal last visited this topic. While already a trend a decade ago, in recent years we have seen the dramatic rise of medical and health humanities courses, programs, and centers in undergraduate institutions and medical schools. 10 Many medical schools now feature programs or centers in health or medical humanities, and several prominent scholars have even argued that the medical and health humanities may “save the life” of imperiled humanities disciplines. 11 The 2015 “Making the Case” essay that has been so central to our thinking for this Special Issue suggested that historians of medicine should be cautious in approaching the medical humanities, and to differentiate our theories, methods, and values from the broader trend towards medical and health humanities. Drawing on our own experiences in recent years, perhaps we need to rethink how to distinguish medical history from other humanities and social sciences in medical education.
Those of us who spend most of our teaching careers among budding physicians, nurses, pharmacists, and dentists can attest to the great value students derive from multi-focal analyses of health problems, from historical, ethical, and policy perspectives, among others. Furthermore, a number of departments in medical schools are de jure and de facto homes to a variety of different humanities specialists who enrich each other’s styles and toolboxes. New scholarly resources have emerged that deliberately and effectively cater to these educators since 2015, such as the New England Journal of Medicine ’s “Case Studies in Social Medicine.” 12 Asserting the value of historians’ theories and methods in these ecosystems is less of a priority than sustaining teaching environments in which the humanities can flourish amidst students’ ever-present concern to focus on intense pathophysiology studying in the first years, and on managing clinical rotation schedules in later years. Integrating our scholarly and teaching styles with those of other humanities and social science experts in narrative medicine, anthropology, philosophy, and ethics, for example, 13 and with those of supportive clinicians is not a pragmatic show of public comity but a necessity that flows from the collaborative spirit that animates the practice of modern medicine. 14 Working alongside fellow travelers can and does buttress historians’ influence on clinical curricula. Can we be effective medical educators while asserting our disciplinary independence, and even a privileged spot for history in clinical education? Possibly. But we might gain as much by collaborating with our fellow humanists and cultivating intellectual humility on an everyday basis while turning to our medical history conferences, large and small, for professional nourishment and renewed commitment to the vitality of our field.
In addition to the complexity of positioning history vis-a-vis other humanities disciplines in clinical education, another, more urgent development intervened between 2015 and the present. The devastating and ongoing COVID-19 pandemic has brought problems of health care access, vaccine equity and ethics, structural racism, xenophobia, and the social context of health to the center of public debate in unprecedented ways on a worldwide scale. Because these topics have long been central to the social and cultural history of medicine and public health, historians in our field have been at the forefront of engaging in public scholarship through op-eds, podcasts, public history and oral history projects, essays, and interviews, and also in working with local, regional, and international political groups to inform public policy. 15 We remain inspired by our colleagues across the world who have been engaged in and supported this work during a global emergency. And COVID-19 has not been the only crisis we have responded to of late, with historians of medicine relentlessly offering context to understand the US Supreme Court overturning of the right to abortion and the emerging stigma around monkeypox, for example. 16 All these efforts build on a tradition of prolific public conversations led by historians about the relevance of the past to act on contemporary health predicaments, whether they concern the HIV/AIDS epidemic, sexual and reproductive rights, drug policies, or even medical education itself. 17 In the short term, it will be difficult, and even undesirable, for these conversations to elide elements and concepts the COVID-19 pandemic has made central, including the erosion of biomedical authority and the socially inequitable burden of disease across populations and nations. Closer to our readers in the US and Canada, the centrality of intersectional and antiracist approaches in medical history means that now, perhaps more so than 1946 or 2015, we have a renewed opportunity to address publics who demand to understand whether and why present-day conditions resemble past ones. Yet, the challenge for our field is how to translate this moment into structural change, at our universities, in our communities, and particularly for the purposes of this Special Issue, in medical education? How can we make medical history instrumental in medical education—and, let us not forget, in public policy—without turning the field into an overly simple tool? 18
The essays that follow offer an institutional, intellectual, and geographical breadth of perspectives on innovative ways to integrate the history of medicine into medical education. Readers will find examples from North America, Europe, the Middle East, and East Asia, and authors as diverse as physicians, surgeons, librarians, archivists, and professional historians of medicine. Taken together, these essays offer an exciting range of ways to introduce, re-introduce, and re-re-introduce history into medical curricula. Readers will undoubtedly find struggles in the essays that follow similar to their own: constrained curricular time in medical education, limited interest by students or administrators, and the tendency of some learners to prefer heroic versions of the history of medicine. No single effort documented in these essays seems to have succeeded in hurdling these obstacles, as they remain common across our field in deeply global ways. Collectively, however, the essays offer a set of potentialities, a diverse toolbox, to introduce and integrate history into clinical practice. While we cannot aspire to comprehensively sample the exemplary local efforts of historians of medicine, public health, nursing, and pharmacy, we hope readers will find inspiration and perhaps a blueprint to continue this vital conversation integral to the history of medicine. 19
The Special Issue begins with an important contextual essay by health sciences librarians Kristine Alpi, Jordan Johnson, and Meg Langford. Their paper surveys the non-curricular history of medicine activities at thirty leading medical schools in the US. Alpi et al. identify a wide range of ways that scholars are currently incorporating the history of medicine in medical education outside of required coursework. These examples include medical history clubs and societies, lecture series, book clubs, funded awards, and local or regional publications. Alpi and colleagues rightly note the importance of these societies in fostering and maintaining a vocational interest in the field. The essay provides a current snapshot of broader trends in the history of medicine in medical education. The perspective of the authors as health sciences librarians underscores a point historians of medicine have long made: librarians and archivists play critical roles in fostering the history of medicine.
Essays two and three turn to specific pedagogical examples of innovative teaching in medical schools. Susan Lamb, in “History’s Toolbox,” first introduces a single skill-based classroom exercise that she uses at the University of Ottawa, a three-hour session directed at fourth-year medical students. Lamb demonstrates the value of teaching medical students historical thinking, not simply historical content, in order to inform clinical decision making. Using a metaphor from bacteriology, histological stains, Lamb instructs students to analyze a historical problem (often an epidemic) through a range of cultural, social, economic, political, and other lenses. In so doing, she provides students the skills to understand the complexities of contemporary problems such as the social determinants of health. Building off her twenty years of experience teaching medical students, Carla Keirns in essay three, “History of Health Policy: Explaining Complexity Through Time,” provides a suggested curriculum for teaching the history of health policy. Keirns shows students how the bewildering, bureaucratic morass that is the US health care system flabbergasts patients and providers alike. Keirns provides detailed teaching strategies for how to historicize critical themes in health policy today – medical training and licensing, nursing education, payment plans – as historically contingent problems, thus fostering the idea that historical thinking is fundamental to clinical care and health policy. In an innovative example that crystallizes her teaching philosophy, Keirns proposes that educators have learners explore the local history of medical schools, clinics, and neighborhoods in order to understand the broader patterns and struggles of American health care reform.
Staying in the institutional context of medical school education but shifting our gaze outside of North America, Alan Weber in essay four, “Clinical Applications of the History of Medicine in Muslim-Majority Nations,” starts with a survey how the history of medicine has been taught in Muslim majority countries. Weber then describes the cultural obstacles of teaching in this setting, particularly the way in which Muslim medical students tend to valorize the past, and how Muslim students, doctors, and patients accept a hybrid worldview that incorporates tenets from western medicine blended with traditional Islamic beliefs about disease, health, and the body. Weber demonstrates unique pedagogical strategies for Muslim nations, including exercises in narrative medicine, cross-cultural clinical competency, and notions of professional identity through the examination of historical medical oaths. In reviewing this expansive topic, Weber not only summarizes key events but also authenticates just how relevant historical knowledge is in the modern Middle-East where many patients combine western biomedicine with traditional understandings of disease. He also conveniently provides a syllabus and long list of sources for non-experts to utilize.
Essay five, by Justin Barr, Rachel Ingold, and Jeff Baker, argues that we need to rethink how, when, and to whom we teach medical history in medical schools. Their article “History of Medicine in Clerkships,” makes two significant points: that historical education can be effectively incorporated during clinical clerkships, and that learners best grasp historical thinking through artifacts in collaboration with librarians and archivists. The authors describe specific lesson plans for surgery, obstetrics/gynecology, and pediatrics, and show how to integrate ancient texts, primary sources, and material relics into instruction. The essay also includes an appendix of digital resources for educators if their institutions’ collections are less accessible or robust. Importantly, the flexibility inherent in clerkship schedules negates many of the traditional obstacles to curricular investment in historical training earlier in medical education.
Artifacts are central too in Harry Wu and Sampson Wong’s article “Spatial Relevance,” in essay six, which centers on experiential learning workshops at the Hong Kong Museum of Medical Sciences and associated heritage trail. A formal part of the curriculum for all first-year medical students since 2010, this three-hour session utilizes specially trained physicians as instructors, and historical analysis from medical historians. Wu and Wong argue that the shared medical backgrounds of teacher and pupil increased the acceptability and efficacy of the exercise, and that “who” teaches the history of medicine in clinical settings is an ongoing question that requires more research. Wu and Wong discuss in detail a specific exhibit that compares the Third Plague Pandemic with the outbreak of SARS in 2002 and show how historical training can help nuance the linearity and notions of progress that might constrain incorporating historical thinking into medical education.
Essay seven, by Frank Stahnisch, returns to North America in a wide-ranging historical study of the last fifty years of medical history education, outreach, and programming at the History of Medicine and Health Care Program in Calgary. Titled “Making Medical History Relevant to Medical Students,” it provides an important case study of the pitfalls, the successes, and the future of teaching history in medical schools. Stahnisch argues that central to this project is providing the support and infrastructure to ensure that learners engage in original historical research and present their findings to multiple audiences. In other words, he argues that medical history is not simply a topic students should learn, but that they must actively do. The essay concludes that fostering student interest in medical history requires an active local medical history society and outreach with physician-historians and community members. Embracing an experiential model of learning, Stahnisch shows how getting students invested in medical history will further clinical problem solving in the future, particularly around problems of health care access, the social contingency of disease concepts, and socio-economic dependencies of medical decision-making.
Essays eight and nine turn away from the institutional setting of medical schools to consider a wider range of ways that historical thinking can inform clinical practice. In essay eight, “Clio in the Operating Theatre,” Agnes Arnold-Forster employs theories and techniques from the history of emotions to rethink surgical stereotypes of emotionally detached, dispassionate surgeons. Explaining a series of Wellcome-funded workshops and small-group discussions with historians and practicing surgeons, Arnold-Forster provides a powerful, novel model of cross-disciplinary research. While surgical stereotypes of dispassion still predominate, Arnold-Forster shows that providing surgeons an alternative history where the emotions of doctors and patients takes center stage in the clinical encounter opens up a new way for surgeons today to embrace emotions into their practice. Building off of Arnold-Forster’s rethinking of surgery, Justin Barr, Don Nakayama, Meghan Kennedy, and Theodore Pappas describe in essay nine the broader institutional settings of incorporating historical thinking into the surgical profession. Activities within the American College of Surgeons, they argue, capture historical interest at all levels of the profession from student to senior clinician. The authors articulate a step-by-step guide for implementing various initiatives including poster contests, panel presentations, and an active blog.
The final essay in this collection, by Tequila Manning, Walter Ingram, and Christopher Crenner, concludes with a powerful example that broadens the history of medicine into the community. Drawing on the work of public history and memory studies, the authors explore a project at Kansas University Medical Center to rename one of its colleges after an influential former dean who intentionally propagated racist and segregationist practices against African-American students. The authors show how historical research in uncovering and documenting this history was critical, but so too was a local exhibit and a series of public discussions. The result was the renaming of the college in 2017 after Marjorie Cates, the first African-American female student to graduate from the school. This contribution demonstrates the power of the history of medicine beyond teaching medical students in the classroom, the clerkship, or in local museums. Our colleagues provide a powerful end to the Special Issue, showing how medical history can converge with an activist pursuit, one at the center of racial justice, commemoration, and the public understanding of medical education.
The collection of essays in this Special Issue offers no final words on how to integrate the history of medicine into medical education. They form, however, a series of innovative case studies for historians around the world to use in their own local settings, enacting, in their own way, the “aggressive strategy” Jones et al. invoked in 2015, but also highlighting the pedagogical partnerships the Special Issue contributors have built and their efforts to persuade students to see history as a tool to provide better and fairer care.
David S. Jones, Jeremy A. Greene, Jacalyn Duffin, and John Harley Warner, “Making the Case for History in Medical Education,” Journal of the History of Medicine and Allied Sciences 70:4 (2015), 623-652, 625.
George Rosen, “What Is Past, Is Prologue,” Journal of the History of Medicine and Allied Sciences, 1:1 (January 1946), 3-5.
Rosen, “What is Past Is Prologue,” 4.
Jones, Greene, Duffin and Warner, “Making the Case for History in Medical Education,” 639.
Ryan Brydges, Victoria A. Boyd, Walter Tavares, Shiphra Ginsburg, Ayelet Kuper, Melanie Anderson, Lynfa Stroud, “Assumptions About Competency-Based Education and the State of the Underlying Evidence: A Critical Narrative Review” Academic Medicine 96, no.2 (2022), 296-306.
Jonathan M. Metzl and Helena Hansen “Structural Competency: Theorizing a New Medical Engagement With Stigma and Inequality” Social Science & Medicine 103 (2014), 126.
Jonathan M. Metzl and Dorothy E. Roberts, “Structural Competency Meets Structural Racism: Race, Politics, and the Structure of Medical Knowledge,” AMA Journal of Ethics, 16: 9 (2014), 674-690. For more information on recent anti-racist curriculum efforts in medicine, see AAMC Statement on Dismantling Racism in Academic Medicine, February 23, 2021: https://www.aamc.org/news-insights/press-releases/aamc-statement-dismantling-racism-academic-medicine
See, for example, Essay Ten in this Special Issue. For broader context, see, Antoine S. Johnson, Elise A. Mitchell, and Ayah Nuriddin, “Syllabus: A History of Anti-Black Racism in Medicine,” Black Perspectives, August 12, 2020, https://www.aaihs.org/syllabus-a-history-of-anti-black-racism-in-medicine/; Raúl Necochea López, Jeffrey Baker, Jason Glenn, Aimee Medeiros, Dominique Tobbell, Ren Capucao, “Race Relations at Academic Health Centers: Historical Scholarship to Enrich Teaching and Community Engagement” Presentation at the 95th annual meeting of the American Association for the History of Medicine, Saratoga Springs, NY, April 22, 2022; Ayah Nuriddin, Graham Mooney, Alexandre IR White, “Reckoning with Histories of Medical Racism and Violence in the USA” The Lancet 396 (10256), 949-951.
Jacalyn Duffin, Clio in the Clinic: History in Medical Education (Toronto: University of Toronto Press, 2005).
In 2000 there were only 14 medical or health humanities baccalaureate programs in the US and Canada. By 2015 there were approximately 60, and today there are over 120. See, Erin Gentry Lamb, Sarah L. Berry, and Therese Jones, Health Humanities Baccalaureate Programs in the United States and Canada (Case Western Reserve School of Medicine, 2021): https://case.edu/medicine/bioethics/sites/case.edu.bioethics/files/2021-05/Health%20Humanities%20Report%202021.pdf
See, for example, the Health and Humanities Lab at the University of North Carolina, https://hhive.unc.edu ; Craig Klugman, “How Medical Humanities Will Save the Life of the Humanities,” Journal of Medical Humanities, 38: 4 (2017),419-430; Keith Wailoo, “Patients Are Humans Too: The Emergence of Medical Humanities,” Daedalus, 151:3 (2022): 194-20.
Scott D. Stonington, Seth M. Holmes, Helena Hansen, Jeremy A. Greene, Keith A. Wailoo, Debra Malina, Stephen Morrissey, Paul E. Farmer, Michael G. Marmot, “Case Studies in Social Medicine - Attending to Structural Forces in Clinical Practice,” New England Journal of Medicine, 370:20 (2018), 1959-1961.
Madeleine Noelle Olding, et al., “Black, White, and Gray: Student Perspectives on Medical Humanities and Medical Education,” Teaching and Learning in Medicine, Vol.34, Issue 2 (2022), 223-233.
Lisa Howley, Elizabeth Gaufberg, and Brandy King, The Fundamental Role of the Arts and Humanities in Medical Education (Washington DC: AAMC, 2020); American Association of Medical Colleges, Behavioral and Social Science Foundations for Future Physicians (Washington, DC: AAMC, 2011).
See, for example, the American Historical Association’s “Bibliography of Historians’ Responses to COVID-19: https://www.historians.org/news-and-advocacy/everything-has-a-history/a-bibliography-of-historians-responses-to-covid-19 . These efforts are both ongoing and global, see for instance, Jorge Lossio and Mariana Cruz, ¿Qué Hicimos Mal? La Tragedia de la COVID (Lima: IEP, 2022).
Leslie J. Reagan “What Alito Gets Wrong about the History of Abortion in America,” Politico, June 2, 2022, https://www.politico.com/news/magazine/2022/06/02/alitos-anti-roe-argument-wrong-00036174 ; Jim Downs, “Gay Men Need a Specific Warning About Monkeypox,” The Atlantic, May 28, 2022, https://www.theatlantic.com/ideas/archive/2022/05/monkeypox-outbreak-spread-gay-bisexual-men/643122/
Shane Doyle, Before HIV: Sexuality, Fertility, and Mortality in East Africa, 1900-1980 (Oxford: Oxford University Press, 2013); Dan Royles, To Make the Wounded Whole: The African American Struggle against HIV/AIDS (Chapel Hill: University of North Carolina Press, 2020); Raúl Necochea López, A History of Family Planning in Twentieth Century Peru (Chapel Hill: University of North Carolina Press, 2014); Johanna Schoen, Abortion after Roe (Chapel Hill: University of North Carolina Press, 2015); Claire D. Clark, The Recovery Revolution: The Battle over Addiction Treatment in the United States (New York: Columbia University Press, 2017); David Herzberg, White Market Drugs: Big Pharma and the Hidden History of Addiction in America (University of Chicago Press, 2020); Christopher D.E. Willoughby, Masters of Health: Racial Science and Slavery in U.S. Medical Schools (University of North Carolina Press, 2021).
Simon Szreter, “History, Policy, and the Social History of Medicine,” Social History of Medicine, 22:2 (August 2009), 235-244.
For example, see Macey Flood’s recent call to integrate Indigenous history into medical education, Macey Flood, “Indigenous History in Health Education,” Medical Humanities (2022), 10.1136/medhum-2022-012400.
Email alerts
Citing articles via.
- Recommend to your Library
- Journals Career Network
Affiliations
- Online ISSN 1468-4373
- Print ISSN 0022-5045
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

What Is Competency-Based Medical Education?

What is Competency-Based Medical Education (CBME)? Think flexible, lifelong learning, with knowledge and/or skills assessed throughout a continuum of learning. In a competency-based educational program, you don’t just acquire knowledge and then spit it back at the time of a final exam. Instead, the method of assessment is formative rather than summative, and you are evaluated on how you apply your knowledge to clinical situations that physicians often face. While summative exams, such as certification exams, play an important role in gauging levels of acquired knowledge, formative assessments are equally important.
Competency-based assessments are used to distinguish between the skills and knowledge that you already have and those for which you need more education and training. In contrast to time-based educational methods, CBME is a learner-centered, active, and lifelong experience that incorporates feedback between the teacher and the learner to fulfill the desired competency outcomes.
Adoption of the Competency-Based Medical Education Construct
The concept of competency-based training began in the 1920s, when U.S. industry and businesses started researching ways of teaching their employees the specific knowledge and skills needed to create a specific product in a standardized manner. However, in the 1960s, a movement to de-emphasize basic skills in education arose. The resulting decline in traditional scores of achievement eventually sparked a demand for the renewal of minimum standards and performance competencies.
The design of a competency-based system of education can be approached using the following steps:
- Identify the desired outcomes
- Define the level of performance for each competency
- Develop a framework for assessing competencies
- Evaluate the program on a continuous basis to be sure that the desired outcomes are being achieved
In 1999, the Accreditation Council for Graduate Medical Education (ACGME) and the American Board of Medical Specialties (ABMS) endorsed six domains of core competencies , and the outcome initiative (the Outcome Project) was soon launched.
The six ACGME Core Competencies are:
- Patient Care
- Medical Knowledge
- Professionalism
- Interpersonal and Communication Skills
- Practice-Based Learning and Improvement
- Systems-Based Practice
Even though there was standardized language around the core competencies of medical education, there were still no standardized assessment methods to determine whether or not a learner had achieved all of the core competencies prior to completion of residency training. This deficiency ultimately led to the creation of milestones to operationalize and implement the competencies. These milestones described the performance levels residents and fellows are expected to demonstrate for skills, knowledge, and behaviors in the six clinical competency domains and are significant points in development that are unique to each specialty.
In 2014, the ACGME required the reporting of milestones as part of the Next Accreditation System (NAS) for all ACGME-accredited residency and fellowship programs. In undergraduate medical education, there are two AAMC-defined performance levels: novice performance and performance expected of a graduating MD. In graduate medical education, there are five performance levels for each competency: novice, advanced beginner, competent individual, proficient individual, and expert physician.
The Next Goal
The Core Competencies are now the basic language for defining physician competence and are also the principles used in the training of physicians. The next goal of CBME is to link education in the competencies to improved quality of patient care. This ambitious step will require standardized methods to securely collect patient data and stratify for various clinical variables including disease specificity, overall patient health, and the multitude of health care professionals who care for each patient.
The shift to CBME was an important transition that allowed residents and fellows to be active agents in their own learning by comparing their milestone assessment and feedback data to their personal learning plans. However, the future of CBME is just being realized and offers many exciting opportunities moving forward.
You can read more about CBME here:
- Association of American Medical Colleges (AAMC) Core Competencies for Entering Medical Students
- Advancing Competency-Based Medical Education: A Charter for Clinician-Educators.
Share This Post!
21 comments.
The CBME is the basic and strong infrastructure of the excellent education . Thank you for your unbelievable inspiration .
The excellent medical education is capable of eliminating CVD/CAD, T2DM, and Cancer today’s growing epidemics. This will be realized when physicians will know CVD/CAD, T2DM and Cancer Inherited Real Risk, bedside diagnosed from birth and removed by unexpensive Quantum Therapy, rather than the CBME.
biology and the medical essay is interesting to read and your blog gives provide the diagnosed point, medical education tips of safety should know to every person.
The CBME is better & excellent education system. Very helpful, thanks for this.
Great information! Thanks for sharing. I would share this article at https://qanda.typicalstudent.org/ a platform for students, teachers and other related people to discuss their thoughts and experiences on learning and other topics.
Thanks a lot for allow me comment here
Over the last two decades, competency‐based frameworks have been internationally adopted as the primary educational approach in medicine. Yet competency‐based medical education (CBME) remains contested in the academic literature. We look broadly at the nature of this debate to explore how it may shape scholars’ understanding of CBME, and its implications for medical education research and practice. In doing so, we deconstruct unarticulated discourses and assumptions embedded in the CBME literature. Its really hard to garb a Government jobs with this competency.
After reading your article, I’m compelling to share your points on this topic. You have done a very good job with your attention to detail you put into this article.
Very helpful, thanks for this.
This will be realized when physicians will know CVD/CAD, T2DM and Cancer Inherited Real Risk, bedside diagnosed from birth and removed by unexpensive Quantum Therapy, rather than the CBME.
Great post, like’d your thoughts, thanks for sharing 🙂
I found this article good, interesting thoughts have been explained. keep it up, thanks for sharing
This is a very informative post for the blog writers and readers. Thanks for the sharing your concerned openly.
Great and Insightful post, Learnt a lot, for medical aspirants it is a must read. Keep posting such content.
have you developed curriculum for competence based learning .,or planning on the lines of Problem based learning.
After reading your article, I’m compelling to share your points on this topic.
The point of imparting medical education is to prepare graduates to effectively deal with the health needs of the general public. The present therapeutic training framework depends on an educational programs that is subject-focused and time based.
Great Article, i am reading your i gain lot of knowledge from this article keep post such content
In competency-based education, students work to ace abilities before they are introduced with new ideas. This gives students the opportunity to move at their own pace and take control of their education.
Some ideas of making this ingrained in knowledge: repetively teach, practice and test.from M1 to M4 the top 20 most urgent/import/deadly topic adding complexity to each year of Med Ed. Get MD input. For example:.
Top 20 most deadly diseases ie MI, Sepsis, Pulm Emboli, early Cancer detection Top 20 missed diagnoses Top 20 interpersonal physician-patient challenging discussions Top 20 ways to increase professionalism and stop being defensive Top 20 required for Boards or AACM/LCME in recognizing sings of uncommon diseases to refer to subspec. Every year do weekly practice and end of year Proficiency that the next higher medical students could teach and test with M4s being taguht and tested by either residents of MDs. Make it very straightforward, competency is goal, not trying to trick anyone. 100% to pass since so very practical and practiced and needed. Then residency and hospitals could continue adding complexity prn. Good luck and thank you!
Comments are closed.
AI in Medical Education: Global situation, effects and challenges
- Published: 10 July 2023
- Volume 29 , pages 4611–4633, ( 2024 )
Cite this article

- Wei Zhang 1 ,
- Mingxuan Cai 1 ,
- Hong Joo Lee 2 ,
- Richard Evans 3 ,
- Chengyan Zhu 4 &
- Chenghan Ming 5
2568 Accesses
5 Citations
Explore all metrics
Artificial Intelligence (AI) is transforming healthcare and shows considerable promise for the delivery of medical education. This systematic review provides a comprehensive analysis of the global situation, effects, and challenges associated with applying AI at the different stages of medical education.
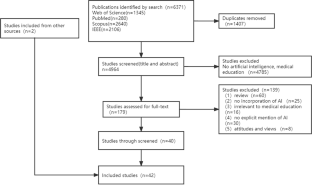
This review followed the PRISMA guidelines, and retrieved studies published on Web of Science, PubMed, Scopus, and IEEE Xplore, from 1990 to 2022. After duplicates were removed (n = 1407) from the 6371 identified records, the full text of 179 records were screened. In total, 42 records were eligible.
It revealed three teaching stages where AI can be applied in medical education (n = 39), including teaching implementation (n = 24), teaching evaluation (n = 10), and teaching feedback (n = 5). Many studies explored the effectiveness of AI adoption with questionnaire survey and control experiment. The challenges are performance improvement, effectiveness verification, AI training data sample and AI algorithms.
Conclusions
AI provides real-time feedback and accurate evaluation, and can be used to monitor teaching quality. A possible reason why AI has not yet been applied widely to practical teaching may be the disciplinary gap between developers and end-user, it is necessary to strengthen the theoretical guidance of medical education that synchronizes with the rapid development of AI. Medical educators are expected to maintain a balance between AI and teacher-led teaching, and medical students need to think independently and critically. It is also highly demanded for research teams with a wide range of disciplines to ensure the applicability of AI in medical education.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

AIM in Medical Education

AI’s Role and Application in Education: Systematic Review
Data availability.
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Aldeman, N. L. S., de SáUrtigaAita, K. M., Machado, V. P., da Mata Sousa, L. C. D., Coelho, A. G. B., da Silva, A. S., Silva Mendes, A. P., de Oliveira Neres, F. J., & do Monte, S. J. H. (2021). Smartpathk: A platform for teaching glomerulopathies using machine learning. BMC Medical Education, 21 (1), 248. https://doi.org/10.1186/s12909-021-02680-1
Article PubMed PubMed Central Google Scholar
Alonso-Silverio, G. A., Pérez-Escamirosa, F., Bruno-Sanchez, R., Ortiz-Simon, J. L., Muñoz-Guerrero, R., Minor-Martinez, A., & Alarcón-Paredes, A. (2018). Development of a Laparoscopic Box Trainer Based on Open Source Hardware and Artificial Intelligence for Objective Assessment of Surgical Psychomotor Skills. Surgical Innovation, 25 (4), 380–388. https://doi.org/10.1177/1553350618777045
Article PubMed Google Scholar
Baloul, M. S., Yeh, V.J.-H., Mukhtar, F., Ramachandran, D., Traynor, M. D., Shaikh, N., Rivera, M., & Farley, D. R. (2022). Video Commentary & Machine Learning: Tell Me What You See, I Tell You Who You Are. Journal of Surgical Education, 79 (6), e263–e272. https://doi.org/10.1016/j.jsurg.2020.09.022
Bienstock, J. L., Katz, N. T., Cox, S. M., Hueppchen, N., Erickson, S., & Puscheck, E. E. (2007). To the point: Medical education reviews—providing feedback. American Journal of Obstetrics and Gynecology, 196 (6), 508–513. https://doi.org/10.1016/j.ajog.2006.08.021
Bing-You, R., Hayes, V., Varaklis, K., Trowbridge, R., Kemp, H., & McKelvy, D. (2017). Feedback for Learners in Medical Education: What Is Known? A Scoping Review . Wolters Kluwer. https://doi.org/10.1097/ACM.0000000000001578
Bissonnette, V., Mirchi, N., Ledwos, N., Alsidieri, G., Winkler-Schwartz, A., Del Maestro, R. F., Yilmaz, R., Siyar, S., Azarnoush, H., Karlik, B., Sawaya, R., Alotaibi, F. E., Bugdadi, A., Bajunaid, K., Ouellet, J., & Berry, G. (2019). Artificial Intelligence Distinguishes Surgical Training Levels in a Virtual Reality Spinal Task. Journal of Bone and Joint Surgery-American, 101 (23), e127. https://doi.org/10.2106/JBJS.18.01197
Article Google Scholar
Borakati, A. (2021). Evaluation of an international medical E-learning course with natural language processing and machine learning. BMC Medical Education, 21 (1), 181. https://doi.org/10.1186/s12909-021-02609-8
Chan, H.-P., Samala, R. K., Hadjiiski, L. M., & Zhou, C. (2020). Deep Learning in Medical Image Analysis. In G. Lee & H. Fujita ( Ed.), Deep Learning in Medical Image Analysis: Challenges and Applications (pp. 3–21). Springer International Publishing. https://doi.org/10.1007/978-3-030-33128-3_1
Chan, K. S., & Zary, N. (2019). Applications and Challenges of Implementing Artificial Intelligence in Medical Education: Integrative Review. JMIR Medical Education, 5 (1), e13930. https://doi.org/10.2196/13930
Chen, C.-K. (2010). Curriculum Assessment Using Artificial Neural Network and Support Vector Machine Modeling Approaches: A Case Study. IR Applications. Volume 29. In Association for Institutional Research (NJ1) . Association for Institutional Research. https://eric.ed.gov/?id=ED524832
Chen, L., Chen, P., & Lin, Z. (2020). Artificial Intelligence in Education: A Review. Ieee Access, 8 , 75264–75278. https://doi.org/10.1109/ACCESS.2020.2988510
Cheng, C.-T., Chen, C.-C., Fu, C.-Y., Chaou, C.-H., Wu, Y.-T., Hsu, C.-P., Chang, C.-C., Chung, I.-F., Hsieh, C.-H., Hsieh, M.-J., & Liao, C.-H. (2020). Artificial intelligence-based education assists medical students’ interpretation of hip fracture. Insights into Imaging, 11 (1), 119. https://doi.org/10.1186/s13244-020-00932-0
de Lima, R. M., de Medeiros Santos, A., Mendes Neto, F. M., de Sousa, F., Neto, A., Leão, F. C. P., de Macedo, F. T., & de Paula Canuto, A. M. (2016). A 3D serious game for medical students training in clinical cases. IEEE International Conference on Serious Games and Applications for Health (SeGAH), 2016 , 1–9. https://doi.org/10.1109/SeGAH.2016.7586255
Dharmasaroja, P., & Kingkaew, N. (2016). Application of artificial neural networks for prediction of learning performances. 2016 12th International Conference on Natural Computation, Fuzzy Systems and Knowledge Discovery (ICNC-FSKD) , 745–751. https://doi.org/10.1109/FSKD.2016.7603268
Estai, M., & Bunt, S. (2016). Best teaching practices in anatomy education: A critical review. Annals of Anatomy - Anatomischer Anzeiger, 208 , 151–157. https://doi.org/10.1016/j.aanat.2016.02.010
Fajrianti, E. D., Sukaridhoto, S., Rasyid, M. U. H. A., Suwito, B. E., Budiarti, R. P. N., Hafidz, I. A. A., Satrio, N. A., & Haz, A. L. (2022). Application of Augmented Intelligence Technology with Human Body Tracking for Human Anatomy Education. IJIET: International Journal of Information and Education Technology , 12 (6), Article 6.
Fang, Z., Xu, Z., He, X., & Han, W. (2022).Artificial intelligence-based pathologic myopia identification system in the ophthalmology residency training program. Frontiers in Cell and Developmental Biology , 10 . https://doi.org/10.3389/fcell.2022.1053079
Fazlollahi, A. M., Bakhaidar, M., Alsayegh, A., Yilmaz, R., Winkler-Schwartz, A., Mirchi, N., Langleben, I., Ledwos, N., Sabbagh, A. J., Bajunaid, K., Harley, J. M., & Del Maestro, R. F. (2022). Effect of Artificial Intelligence Tutoring vs Expert Instruction on Learning Simulated Surgical Skills Among Medical Students: A Randomized Clinical Trial. JAMA Network Open, 5 (2), e2149008. https://doi.org/10.1001/jamanetworkopen.2021.49008
Fernández-Alemán, J. L., López-González, L., González-Sequeros, O., Jayne, C., López-Jiménez, J. J., & Toval, A. (2016). The evaluation of i-SIDRA – a tool for intelligent feedback – in a course on the anatomy of the locomotor system. International Journal of Medical Informatics, 94 , 172–181. https://doi.org/10.1016/j.ijmedinf.2016.07.008
Foss, C. L. (1987). Learning from errors in ALGEBRALAND . Institute for Research on Learning.
Furlan, R., Gatti, M., Menè, R., Shiffer, D., Marchiori, C., Levra, A. G., Saturnino, V., Brunetta, E., & Dipaola, F. (2021). A Natural Language Processing-Based Virtual Patient Simulator and Intelligent Tutoring System for the Clinical Diagnostic Process: Simulator Development and Case Study. JMIR Medical Informatics, 9 (4), e24073. https://doi.org/10.2196/24073
Gendia, A. (2022). Cloud Based AI-Driven Video Analytics (CAVs) in Laparoscopic Surgery: A Step Closer to a Virtual Portfolio. Cureus , 14 (9). https://doi.org/10.7759/cureus.29087
Gil, D. H., Heins, M., & Jones, P. B. (1984). Perceptions of medical school faculty members and students on clinical clerkship feedback. Academic Medicine, 59 (11), 856.
Article CAS Google Scholar
Goh, P. S. (2021). The vision of transformation in medical education after the COVID-19 pandemic. Korean Journal of Medical Education, 33 (3), 171–174. https://doi.org/10.3946/kjme.2021.197
Article MathSciNet PubMed PubMed Central Google Scholar
Gorospe-Sarasúa, L., Munoz-Olmedo, J. M., Sendra-Portero, F., & de Luis-García, R. (2022a). Challenges of Radiology education in the era of artificial intelligence . 6.
Gorospe-Sarasúa, L., Muñoz-Olmedo, J. M., Sendra-Portero, F., & de Luis-García, R. (2022b). Challenges of Radiology education in the era of artificial intelligence. Radiología (english Edition), 64 (1), 54–59. https://doi.org/10.1016/j.rxeng.2020.10.012
Han, R., Yu, W., Chen, H., & Chen, Y. (2022). Using artificial intelligence reading label system in diabetic retinopathy grading training of junior ophthalmology residents and medical students. BMC Medical Education , 22 (1), Article 1. https://doi.org/10.1186/s12909-022-03272-3
Hattie, J., & Timperley, H. (2007). The power of feedback. Review of educational research, 77 (1), 81–112. https://doi.org/10.3102/003465430298487
Hedderich, D. M., Keicher, M., Wiestler, B., Gruber, M. J., Burwinkel, H., Hinterwimmer, F., Czempiel, T., Spiro, J. E., Pinto dos Santos, D., Heim, D., Zimmer, C., Rückert, D., Kirschke, J. S., & Navab, N. (2021). AI for Doctors—A Course to Educate Medical Professionals in Artificial Intelligence for Medical Imaging. Healthcare , 9 (10), Article 10. https://doi.org/10.3390/healthcare9101278
Hewson, M. G., & Little, M. L. (1998). Giving Feedback in Medical Education. Journal of General Internal Medicine, 13 (2), 111–116. https://doi.org/10.1046/j.1525-1497.1998.00027.x
Article CAS PubMed PubMed Central Google Scholar
Hisan, U. K., & Amri, M. M. (2023). ChatGPT and Medical Education: A Double-Edged Sword. Journal of Pedagogy and Education Science , 2 (01), Article 01. https://doi.org/10.56741/jpes.v2i01.302
Hisey, R., Camire, D., Erb, J., Howes, D., Fichtinger, G., & Ungi, T. (2022). System for Central Venous Catheterization Training Using Computer Vision-Based Workflow Feedback. IEEE Transactions on Biomedical Engineering, 69 (5), 1630–1638. https://doi.org/10.1109/TBME.2021.3124422
Hosny, A., Parmar, C., Quackenbush, J., Schwartz, L. H., & Aerts, H. J. W. L. (2018). Artificial intelligence in radiology. Nature Reviews Cancer , 18 (8), Article 8. https://doi.org/10.1038/s41568-018-0016-5
Hu, H., Li, J., Lei, X., Qin, P., & Chen, Q. (2019). Design of health statistics intelligent education system based on Internet +. Journal of Physics: Conference Series, 1168 (6), 062003. https://doi.org/10.1088/1742-6596/1168/6/062003
Hwang, G.-J., Xie, H., Wah, B. W., & Gašević, D. (2020). Vision, challenges, roles and research issues of Artificial Intelligence in Education. Computers and Education: Artificial Intelligence, 1 , 100001. https://doi.org/10.1016/j.caeai.2020.100001
Islam, G., Kahol, K., Li, B., Smith, M., & Patel, V. L. (2016). Affordable, web-based surgical skill training and evaluation tool. Journal of Biomedical Informatics, 59 , 102–114. https://doi.org/10.1016/j.jbi.2015.11.002
Karambakhsh, A., Kamel, A., Sheng, B., Li, P., Yang, P., & Feng, D. D. (2019). Deep gesture interaction for augmented anatomy learning. International Journal of Information Management, 45 , 328–336. https://doi.org/10.1016/j.ijinfomgt.2018.03.004
Kirubarajan, A., Young, D., Khan, S., Crasto, N., Sobel, M., & Sussman, D. (2022). Artificial Intelligence and Surgical Education: A Systematic Scoping Review of Interventions. Journal of Surgical Education, 79 (2), 500–515. https://doi.org/10.1016/j.jsurg.2021.09.012
Klar, R., & Bayer, U. (1990). Computer-assisted teaching and learning in medicine. International Journal of Bio-Medical Computing, 26 (1–2), 7–27. https://doi.org/10.1016/0020-7101(90)90016-N
Article CAS PubMed Google Scholar
Kurniawan, M. H., Suharjito, Diana, & Witjaksono, G. (2018). Human Anatomy Learning Systems Using Augmented Reality on Mobile Application . 135 , 80–88. https://doi.org/10.1016/j.procs.2018.08.152
Lam, A., Lam, L., Blacketer, C., Parnis, R., Franke, K., Wagner, M., Wang, D., Tan, Y., Oakden-Rayner, L., Gallagher, S., Perry, S. W., Licinio, J., Symonds, I., Thomas, J., Duggan, P., & Bacchi, S. (2022a). Professionalism and clinical short answer question marking with machine learning. Internal Medicine Journal, 52 (7), 1268–1271. https://doi.org/10.1111/imj.15839
Lam, K., Chen, J., Wang, Z., Iqbal, F. M., Darzi, A., Lo, B., Purkayastha, S., & Kinross, J. M. (2022b). Machine learning for technical skill assessment in surgery: A systematic review. Npj Digital Medicine , 5(1), Article 1. https://doi.org/10.1038/s41746-022-00566-0
Lazarus, M. D., Truong, M., Douglas, P., & Selwyn, N. (2022). Artificial intelligence and clinical anatomical education: Promises and perils. Anatomical Sciences Education , n/a (n/a). https://doi.org/10.1002/ase.2221
Lee, J., Wu, A. S., Li, D., Kulasegaram, K., & (Mahan). (2021). Artificial Intelligence in Undergraduate Medical Education: A Scoping Review. Academic Medicine, 96 (11S), S62. https://doi.org/10.1097/ACM.0000000000004291
Lee, L. S., Aluwee, S. A. Z. S., Meng, G. C., Palanisamy, P., & Subramaniam, R. (2020). Interactive Tool Using Augmented Reality (AR) for Learning Knee and Foot Anatomy Based on CT Images 3D Reconstruction. 2020 International Conference on Computational Intelligence (ICCI) , 281–286. https://doi.org/10.1109/ICCI51257.2020.9247820
Li, Y., Bai, C., & Reddy, C. K. (2016). A distributed ensemble approach for mining healthcare data under privacy constraints. Information Sciences, 330 , 245–259. https://doi.org/10.1016/j.ins.2015.10.011
Li, Y. S., Lam, C. S. N., & See, C. (2021). Using a Machine Learning Architecture to Create an AI-Powered Chatbot for Anatomy Education. Medical Science Educator, 31 (6), 1729–1730. https://doi.org/10.1007/s40670-021-01405-9
Luan, H., Geczy, P., Lai, H., Gobert, J., Yang, S. J. H., Ogata, H., Baltes, J., Guerra, R., Li, P., & Tsai, C.-C. (2020). Challenges and Future Directions of Big Data and Artificial Intelligence in Education. Frontiers in Psychology , 11 . https://doi.org/10.3389/fpsyg.2020.580820
Martin, J. A., Regehr, G., Reznick, R., Macrae, H., Murnaghan, J., Hutchison, C., & Brown, M. (1997). Objective structured assessment of technical skill (OSATS) for surgical residents. BJS (british Journal of Surgery), 84 (2), 273–278. https://doi.org/10.1046/j.1365-2168.1997.02502.x
Mirchi, N., Bissonnette, V., Yilmaz, R., Ledwos, N., Winkler-Schwartz, A., & Del Maestro, R. F. (2020). The Virtual Operative Assistant: An explainable artificial intelligence tool for simulation-based training in surgery and medicine. Plos One, 15 (2), e0229596. https://doi.org/10.1371/journal.pone.0229596
Muller, S. (1984). Physicians for the twenty-first century: Report of the project panel on the general professional education of the physician and college preparation for medicine. Journal of Medical Education, 59 , 1–208.
Google Scholar
Nagaraj, M. B., Namazi, B., Sankaranarayanan, G., & Scott, D. J. (2023). Developing artificial intelligence models for medical student suturing and knot-tying video-based assessment and coaching. Surgical Endoscopy, 37 (1), 402–411. https://doi.org/10.1007/s00464-022-09509-y
Nakawala, H., Ferrigno, G., & De Momi, E. (2018). Development of an intelligent surgical training system for Thoracentesis. Artificial Intelligence in Medicine, 84 , 50–63. https://doi.org/10.1016/j.artmed.2017.10.004
Neves, S. E., Chen, M. J., Ku, C. M., Karan, S., DiLorenzo, A. N., Schell, R. M., Lee, D. E., Diachun, C. A. B., Jones, S. B., & Mitchell, J. D. (2021). Using Machine Learning to Evaluate Attending Feedback on Resident Performance. Anesthesia & Analgesia, 132 (2), 545–555. https://doi.org/10.1213/ANE.0000000000005265
Niitsu, H., Hirabayashi, N., Yoshimitsu, M., Mimura, T., Taomoto, J., Sugiyama, Y., Murakami, S., Saeki, S., Mukaida, H., & Takiyama, W. (2013). Using the Objective Structured Assessment of Technical Skills (OSATS) global rating scale to evaluate the skills of surgical trainees in the operating room. Surgery Today, 43 (3), 271–275. https://doi.org/10.1007/s00595-012-0313-7
Ötles, E., Kendrick, D. E., Solano, Q. P., Schuller, M., Ahle, S. L., Eskender, M. H., Carnes, E., & George, B. C. (2021). Using Natural Language Processing to Automatically Assess Feedback Quality: Findings From 3 Surgical Residencies. Academic Medicine, 96 (10), 1457. https://doi.org/10.1097/ACM.0000000000004153
Ouyang, F., Zheng, L., & Jiao, P. (2022). Artificial intelligence in online higher education: A systematic review of empirical research from 2011 to 2020. Education and Information Technologies . https://doi.org/10.1007/s10639-022-10925-9
Peter, H., & Goodridge, W. (2004). Integrating Two Artificial Intelligence Theories in a Medical Diagnosis Application. In M. Bramer & V. Devedzic ( Ed.), Artificial Intelligence Applications and Innovations (pp. 11–23). Springer US. https://doi.org/10.1007/1-4020-8151-0_2
Qian, X., Jingying, H., Xian, S., Yuqing, Z., Lili, W., Baorui, C., Wei, G., Yefeng, Z., Qiang, Z., Chunyan, C., Cheng, B., Kai, M., & Yi, Q. (2022). The effectiveness of artificial intelligence-based automated grading and training system in education of manual detection of diabetic retinopathy. Frontiers in Public Health, 10 , 1025271. https://doi.org/10.3389/fpubh.2022.1025271
Razzak, M. I., Naz, S., & Zaib, A. (2018). Deep Learning for Medical Image Processing: Overview, Challenges and the Future. In N. Dey, A. S. Ashour, & S. Borra ( Ed.), Classification in BioApps: Automation of Decision Making (pp. 323–350). Springer International Publishing. https://doi.org/10.1007/978-3-319-65981-7_12
Sadeghi Esfahlani, S., Izsof, V., Minter, S., Kordzadeh, A., Shirvani, H., & Esfahlani, K. S. (2020). Development of an Interactive Virtual Reality for Medical Skills Training Supervised by Artificial Neural Network. In Y. Bi, R. Bhatia, & S. Kapoor ( Ed.), Intelligent Systems and Applications (pp. 473–482). Springer International Publishing. https://doi.org/10.1007/978-3-030-29513-4_34
Shiang, T., Garwood, E., & Debenedectis, C. M. (2022). Artificial intelligence-based decision support system (AI-DSS) implementation in radiology residency: Introducing residents to AI in the clinical setting. Clinical Imaging, 92 , 32–37. https://doi.org/10.1016/j.clinimag.2022.09.003
Siyar, S., Azarnoush, H., Rashidi, S., Winkler-Schwartz, A., Bissonnette, V., Ponnudurai, N., & Del Maestro, R. F. (2020). Machine learning distinguishes neurosurgical skill levels in a virtual reality tumor resection task. Medical and Biological Engineering and Computing, 58 (6), 1357–1367. https://doi.org/10.1007/s11517-020-02155-3
Solano, Q. P., Hayward, L., Chopra, Z., Quanstrom, K., Kendrick, D., Abbott, K. L., Kunzmann, M., Ahle, S., Schuller, M., Ötleş, E., & George, B. C. (2021). Natural Language Processing and Assessment of Resident Feedback Quality. Journal of Surgical Education, 78 (6), e72–e77. https://doi.org/10.1016/j.jsurg.2021.05.012
Stephens, G. C., Rees, C. E., & Lazarus, M. D. (2021). Exploring the impact of education on preclinical medical students’ tolerance of uncertainty: A qualitative longitudinal study. Advances in Health Sciences Education, 26 (1), 53–77. https://doi.org/10.1007/s10459-020-09971-0
Sqalli, M. T., Al-Thani, D., Elshazly, M. B., & Al-Hijji, M. (2022). A Blueprint for an AI & AR-Based Eye Tracking System to Train Cardiology Professionals Better Interpret Electrocardiograms. In N. Baghaei, J. Vassileva, R. Ali, & K. Oyibo ( Ed.), Persuasive Technology (pp. 221–229). Springer International Publishing. https://doi.org/10.1007/978-3-030-98438-0_17
Szasz, P., Louridas, M., Harris, K. A., Aggarwal, R., & Grantcharov, T. P. (2015). Assessing Technical Competence in Surgical Trainees: A Systematic Review. Annals of Surgery, 261 (6), 1046. https://doi.org/10.1097/SLA.0000000000000866
Torre, D. M., Sebastian, J. L., & Simpson, D. E. (2003). Learning Activities and High-Quality Teaching: Perceptions of Third-Year IM Clerkship Students. Academic Medicine, 78 (8), 812.
Vayena, E., & Blasimme, A. (2017). Biomedical Big Data: New Models of Control Over Access, Use and Governance. Journal of Bioethical Inquiry, 14 (4), 501–513. https://doi.org/10.1007/s11673-017-9809-6
Voss, G., Bockholt, U., Los Arcos, J. L., Müller, W., Oppelt, P., & Stähler, J. (2000). Lahystotrain. Studies in Health Technology and Informatics, 70 , 359–364. https://doi.org/10.3233/978-1-60750-914-1-359
Wang, M., Sun, Z., Jia, M., Wang, Y., Wang, H., Zhu, X., Chen, L., & Ji, H. (2022). Intelligent virtual case learning system based on real medical records and natural language processing. BMC Medical Informatics and Decision Making, 22 (1), 60. https://doi.org/10.1186/s12911-022-01797-7
Willan, P. L. T., & Humpherson, J. R. (1999). Concepts of variation and normality in morphology: Important issues at risk of neglect in modern undergraduate medical courses. Clinical Anatomy, 12 (3), 186–190. https://doi.org/10.1002/(SICI)1098-2353(1999)12:3%3c186::AID-CA7%3e3.0.CO;2-6
Wolverton, S. E., & Bosworth, M. F. (1985). A survey of resident perceptions of effective teaching behaviors. Family Medicine, 17 (3), 106–108.
CAS PubMed Google Scholar
Wood, B. P. (2000). Feedback: A Key Feature of Medical Training. Radiology, 215 (1), 17–19. https://doi.org/10.1148/radiology.215.1.r00ap5917
Article MathSciNet CAS PubMed Google Scholar
Yang, W., Hebert, D., Kim, S., & Kang, B. (2019). MCRDR Knowledge-Based 3D Dialogue Simulation in Clinical Training and Assessment. Journal of Medical Systems, 43 (7), 200. https://doi.org/10.1007/s10916-019-1262-0
Yilmaz, Y., Nunez, A. J., Ariaeinejad, A., Lee, M., Sherbino, J., & Chan, T. M. (2022). Harnessing Natural Language Processing to Support Decisions Around Workplace-Based Assessment: Machine Learning Study of Competency-Based Medical Education. JMIR Medical Education, 8 (2), e30537. https://doi.org/10.2196/30537
Yilmaz-Recai, Winkler-Schwartz, A., Mirchi, N., Reich, A., Christie, S., Tran, D. H., Ledwos, N., Fazlollahi, A. M., Santaguida, C., Sabbagh, A. J., Bajunaid, K., & Del Maestro, R. (2022). Continuous monitoring of surgical bimanual expertise using deep neural networks in virtual reality simulation. Npj Digital Medicine , 5 (1), Article 1. https://doi.org/10.1038/s41746-022-00596-8
Zahiri, M., Booton, R., Siu, K.-C., & Nelson, C. A. (2016). Design and Evaluation of a Portable Laparoscopic Training System Using Virtual Reality. Journal of Medical Devices , 11(1). https://doi.org/10.1115/1.4034881
Zhao, S., Zhang, X., Jin, F., & Hahn, J. (2021). An Auxiliary Tasks Based Framework for Automated Medical Skill Assessment with Limited Data. 2021 43rd Annual International Conference of the IEEE Engineering in Medicine Biology Society (EMBC) , 1613–1617. https://doi.org/10.1109/EMBC46164.2021.9630498
Download references
This paper is supported by National Natural Science Foundation of China (Project No. 72104087, 72004070) and University-Industry Collaborative Education Program supported by Ministry of Education in China (220505084312449).
Author information
Authors and affiliations.
School of Medicine and Health Management, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
Wei Zhang & Mingxuan Cai
Department of Business Administration, The Catholic University of Korea, Seoul, Korea
Hong Joo Lee
Faulty of Computer Science, Dalhousie University, Halifax, Canada
Richard Evans
School of Political Science and Public Administration, Wuhan University, Wuhan, China
Chengyan Zhu
College of Public Administration and Law, Hunan Agricultural University, Changsha, China
Chenghan Ming
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Chengyan Zhu .
Ethics declarations
Conflict of interest, additional information, publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (DOCX 13 KB)
Supplementary file2 (docx 60 kb), rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Zhang, W., Cai, M., Lee, H.J. et al. AI in Medical Education: Global situation, effects and challenges. Educ Inf Technol 29 , 4611–4633 (2024). https://doi.org/10.1007/s10639-023-12009-8
Download citation
Received : 11 March 2023
Accepted : 26 June 2023
Published : 10 July 2023
Issue Date : March 2024
DOI : https://doi.org/10.1007/s10639-023-12009-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical education
- Artificial intelligence
- Applications of AIMED
- Effectiveness of AIMED
- Challenges of AIMED
- Find a journal
- Publish with us
- Track your research
EssayEmpire
Medical education essay.

The major features of contemporary medical schools took shape in the late nineteenth and early twentieth centuries. What occurred at that time thoroughly transformed medical education. Subsequent developments rarely had the same far-reaching effects as the changes put in place from the 1870s through the 1920s.
Early Medical Schools
Before the 1870s, most U.S. medical schools supplied only part of the education necessary to be a competent physician. The typical curriculum featured one year of courses in six to eight subjects. The instruction was didactic. A lecturer occasionally demonstrated procedures for the class to watch, but few instructors let their pupils carry out the tasks. Students spent little, if any, time in laboratories or with patients. To learn by doing required securing an apprenticeship, summer schooling, European study, or private instruction. What the medical school offered was a series of lectures from faculty who usually owned the school, concentrated on their private practices, and saw research and writing as optional rather than mandatory.
In contrast, medical education in France and Germany was more rigorous. In those countries, medicine was studied as an experimental science best grasped through investigation in the laboratory and service on the hospital ward. In exchange for free care, impoverished patients filled the hospitals where faculty undertook research and taught students. A year or two of European study capped the education of many ambitious American doctors, and they brought home the conviction that their colleagues should emulate the spirit of painstaking experimentation that pervaded the great medical centers of Paris, Berlin, and Vienna.
Another source of dissatisfaction with the patchy American medical curriculum stemmed from the surge of discoveries in the late nineteenth century. Advances in medical knowledge made the short course of study seem wholly inadequate to understand the germ theory of disease, vaccines and antitoxins, precise tests of bodily fluids and tissues, and other diagnostic and therapeutic breakthroughs. Medicine as a profession acquired a firmer and deeper knowledge base, even if many diseases were not yet fully understood. The greater authority and prestige of the profession elevated the standing of the better schools and pressured the weaker ones to improve or close.
The rise of research universities offered a third reason for revamping traditional medical education. As several dozen prominent colleges added graduate divisions and professional schools in order to become universities, they reassessed their relationships with local proprietary medical schools. What had been a casual connection often became a formal affiliation. Mergers appealed to the cadre of medical reformers who believed that the profession would never flourish in the absence of research careers for talented physicians. For the universities, the link was another way to establish their legitimacy as the best regional sources of theoretical and practical knowledge.
Turn-Of-The-Century Transformations
By the 1880s, several medical schools stood apart from others as models of what was possible. At Harvard, Michigan, and Pennsylvania, the three-year curriculum included extensive hands-on work in laboratory science courses taught by full-time faculty. The clinical courses took small groups of students to the bedside and to outpatient dispensaries. Written examinations replaced perfunctory oral exams, and instructors gradually began to test students on the practical work they did in laboratories or with patients. Entrance requirements also stiffened, with graduation from a good high school expected and some college coursework encouraged.
In the 1890s, the new standard bearer, Johns Hopkins, adopted a four-year curriculum and required a bachelor’s degree for admission. Above all, Hopkins led the way by virtue of extensive clinical opportunities in its teaching hospital. The senior faculty in the school controlled the major divisions of the hospital, where students served as clerks responsible for many aspects of patient care. In most hospitals, the board of trustees limited faculty involvement and instructional activity. Often, they regarded educational work with suspicion, and understandably so in an era when most medical students were meagerly trained. Hopkins and then other schools demonstrated that well-taught students and their faculty mentors enhanced patient care. Academic physicians were increasingly respected as the best physicians, and properly supervised students were desirable assistants. Previously seen as a branch of public welfare, the hospital redefined itself as the best place for anyone to receive state-of-the-art treatment.
Lack of money slowed the pace of change at many schools. The vision of good medical education was in sight long before the funding was in hand. Learning by doing cost much more than learning by listening. The student/teacher ratios fell markedly whenever large lecture classes gave way to small group instruction. Unlike part-time and adjunct faculty, full-time faculty were expensive. The space and equipment necessary for laboratory science were also costly. Without the support of local donors, state legislators, and rich philanthropists like J. P. Morgan, John D. Rockefeller, Edward Harkness, and Cornelius Vanderbilt, the transformation of American medical education would have been impossible. Benefactors shunned the proprietary schools, and by 1930, all for-profit medical schools had either closed or affiliated with a university.
Another ongoing challenge was the shape of the curriculum. There were constant discussions of how much time each subject deserved and when it should be taught. Those debates intensified as new fields such as biochemistry, immunology, and preventive medicine emerged. State licensing boards often stipulated how many hours to allocate each subject, but that rigidity provoked outcries about overburdened students with no free time to read, write, or study. How to link the first two years of basic science with the final two years of clinical study also baffled most instructors, as did the matter of special provisions for the very best students. Over time, most medical educators acknowledged the impossibility of covering everything and sought instead to cultivate habits of mind that would equip the young doctor to continue to learn after graduation. Through learning by doing, cross-disciplinary connections, and lifelong education, medical education embodied central tenets of progressive education, the vision of active learning designed to enliven American elementary and secondary schools.
By the 1920s, the enduring features of the modern American medical school had taken hold. No one questioned the value of teaching hospitals, university affiliations, faculty research, and hands-on learning. Medicine had become one of the most respected professions in the country, and the public no longer tolerated third-rate schools where an unprepared student could graduate quickly and easily.
The Price Of Prosperity
Not everyone benefited from the improvements in medical education. The longer course of study excluded some working-class youth who could not afford four years of tuition as well as an unpaid fifth year for a hospital internship, which became common after World War I. As the medical schools’ budgets soared, only one women’s medical school survived, and female enrollments elsewhere rarely exceeded 5 percent until the 1960s. The two schools for blacks barely stayed alive. Jewish students also suffered. When applications exceeded spaces in the 1920s, many schools discriminated against Jewish applicants, accepting only a few each year. Furthermore, as the number of medical schools declined from 1900 to 1930, the number of doctors per capita fell, with rural areas unable to attract as many new doctors as the cities, where lucrative practice as a specialist drew many graduates.
Even so, medical schools became one of the strongest branches of the university, and throughout the 1930s and 1940s, they flourished. Enrollments and endowments held up despite the economic and military turmoil in those decades. Research generated a steady flow of useful discoveries, including antibiotics and vitamins. Faculty salaries were far below what talented physicians could earn in private practice, but academic careers continued to attract many of the best doctors.
As support for research continued to rise throughout the 1950s and 1960s, the composition of the faculty changed. There were more specialists, including many PhDs. The size of the typical faculty expanded more rapidly than the student population, with some departments larger than the entire school had been twenty years earlier. Because promotion and tenure hinged on excellent research, many instructors gave less time to teaching. The overall shape of the curriculum remained unchanged, although a few schools created new courses around particular organs and diseases, and several others either shortened (the six year BA/MD) or extended (Stanford’s five-year MD) the traditional four-year time span.
What also altered the nature of faculty work was the dramatic increase in third-party payments for patient care. Private insurance as well as federal Medicare/Medicaid dollars reimbursed teaching hospitals for patient care that had been pro bono work. As a result, the fraction of faculty time devoted to patients rose sharply. The prosperity enlarged the size of the typical faculty, with nearly all the growth in the clinical ranks. From 1965 to 1990, patient care revenues rose from 6 percent to nearly 50 percent of medical schools’ annual income. Faculty salaries increased rapidly, approaching the earnings of colleagues in private practice. The size and scale of most medical schools, from the 1970s on, was immense, with annual revenue often more than $100 million. In contrast, only nine schools in 1910 had budgets over $100,000. Although cost containment efforts by insurance companies from the 1980s on, coupled with less robust growth in federal funds, forced modest retrenchments here and there, the overall financial health of medical schools usually matched or exceeded that of other professional schools in the university.
With research projects and patient care burgeoning, the task of teaching students became less central to the school’s work. Many senior faculty preferred teaching postdoctoral students and research fellows, delegating other instruction to adjuncts, interns, and the growing number of residents pursuing a specialty. The camaraderie between professors and students that marked turn-of-the-century schools diminished; the heavy workload and ensuing sense of exhaustion and stress did not. The rigorous expectations did not discourage a wider range of applicants from seeking and winning admission. The old restrictions on Jewish students ended after World War II, and in the 1970s, the number of female and minority students increased sharply. Financial aid allowed more working-class students to attend. Foreigners served as interns and residents, and some college seniors who were denied admission went abroad to inferior schools and then reapplied to an American school.
Counterbalancing the lower priority of teaching was renewed interest in curricular reforms. The familiar challenges of an overburdened curriculum, endless memorization of facts, and weak articulation of the basic sciences with the clinical work sparked a variety of innovations: fewer hours devoted to laboratory exercises, more emphasis on problem solving, and new opportunities to see patients and their families in the first two years. Many schools added instruction on interpersonal relations to encourage empathic concern for all aspects of patients’ well-being. As another sign of interest in educational improvement, most schools established divisions charged with the evaluation of teaching. Throughout their history, medical schools benefited from the keen American faith in science. The respect for physicians extended to physicians in training and their instructors. A good medical school was cherished by the community as a reliable sign of local vitality, not weakness. The ability of the profession to retain that trust will be necessary in the future to sustain the remarkable record achieved since the 1870s.
Bibliography:
- Bonner, T. N. (1999). Becoming a physician: Medical education in Britain, France, Germany, and the United States, 1750–1945. New York: Oxford University Press.
- Flexner, A. (1910). Medical education in the United States and Canada. New York: Carnegie Foundation for the Advancement of Teaching.
- Ludmerer, K. M. (1985). Learning to heal: The development of American medical education. New York: Basic Books.
- Ludmerer, K. M. (1999). Time to heal: American medical education from the turn of the century to the era of managed care. New York: Oxford University Press.
- Morantz-Sanchez, R. M. (1985). Sympathy and science: Women physicians in American medicine. New York: Oxford University Press.
- Rosenberg, C. E. (1987). The care of strangers: The rise of America’s hospital system. New York: Basic Books.
- Starr, P. (1982). The social transformation of American medicine. New York: Basic Books.
This example Medical Education Essay is published for educational and informational purposes only. If you need a custom essay or research paper on this topic please use our writing services. EssayEmpire.com offers reliable custom essay writing services that can help you to receive high grades and impress your professors with the quality of each essay or research paper you hand in.
- How to Write an Essay
- Education Essay Topics
- Education Essay Examples
ORDER HIGH QUALITY CUSTOM PAPER

Special offer!
GET 10% OFF WITH 24START DISCOUNT CODE
Related posts.

Getty Images
A compelling medical school admissions essay can address nearly any topic the applicant is interested in, as long as it conveys the applicant's personality.
A personal statement is often a pivotal factor in medical school admissions decisions.
"The essay really can cause me to look more deeply at the entire application," Dr. Stephen Nicholas, former senior associate dean of admissions with the Columbia University Vagelos College of Physicians and Surgeons , told U.S. News in 2017. "So I do think it's pretty important."
A compelling medical school admissions essay can address nearly any topic the applicant is interested in, as long as it conveys the applicant's personality, according to Dr. Barbara Kazmierczak, director of the M.D.-Ph.D. Program and a professor of medicine and microbial pathogenesis with the Yale School of Medicine.
“The passion that the writer is bringing to this topic tells us about the individual rather than the topic that they’re describing, and the essay is the place for us to learn about the applicant – who they are and what experiences have brought them to this point of applying to medical school,” she told U.S. News in 2017.
Rachel Rudeen, former admissions coordinator for the University of Minnesota Medical School , says personal statements help medical schools determine whether applicants have the character necessary to excel as a doctor. "Grit is something we really look for," she says.
Evidence of humility and empathy , Rudeen adds, are also pluses.
Why Medical Schools Care About Personal Statements
The purpose of a personal statement is to report the events that inspired and prepared a premed to apply to medical school, admissions experts say. This personal essay helps admissions officers figure out whether a premed is ready for med school, and it also clarifies whether a premed has a compelling rationale for attending med school, these experts explain.
When written well, a medical school personal statement conveys a student's commitment to medicine and injects humanity into an admissions process that might otherwise feel cold and impersonal, according to admissions experts.
Glen Fogerty, associate dean of admissions and recruitment with the medical school at the University of Arizona—Phoenix , put it this way in an email: "To me, the strongest personal statements are the ones that share a personal connection. One where a candidate shares a specific moment, the spark that ignited their passion to become a physician or reaffirmed why they chose medicine as a career."
Dr. Viveta Lobo, an emergency medicine physician with the Stanford University School of Medicine in California who often mentors premeds, says the key thing to know about a personal statement is that it must indeed be personal, so it needs to reveal something meaningful. The essay should not be a dry piece of writing; it should make the reader feel for the author, says Lobo, director of academic conferences and continuing medical education with the emergency medicine department at Stanford.
A great personal statement has an emotional impact and "will 'do' something, not just 'say' something," Lobo wrote in an email. Admissions officers "read hundreds of essays – so before you begin, think of how yours will stand out, be unique and different," Lobo suggests.
How to Write a Personal Statement for Medical School
Lobo notes that an outstanding personal statement typically includes all of the following ingredients:
- An intriguing introduction that gets admissions officers' attention.
- Anecdotes that illustrate what kind of person the applicant is.
- Reflections about the meaning and impact of various life experiences .
- A convincing narrative about why medical school is the logical next step.
- A satisfying and optimistic conclusion.
"You should sound excited, and that passion should come through in your writing," Lobo explains.
A personal statement should tie together an applicant's past, present and future by explaining how previous experiences have led to this point and outlining long-term plans to contribute to the medical profession, Lobo said during a phone interview. Medical school admissions officers want to understand not only where an applicant has been but also the direction he or she is going, Lobo added.
When premeds articulate a vision of how they might assist others and improve society through the practice of medicine, it suggests that they aren't self-serving or simply interested in the field because of its prestige, Lobo says. It's ideal when premeds can eloquently describe a noble mission, she explains.
Elisabeth Fassas, author of "Making Pre-Med Count: Everything I Wish I'd Known Before Applying (Successfully) to Medical School," says premeds should think about the doctors they admire and reflect on why they admire them. Fassas, a first-year medical student at the University of Maryland , suggests pondering the following questions:
- "Why can you really only see yourself being a physician?"
- "What is it about being a doctor that has turned you on to this field?"
- "What kind of doctor do you imagine yourself being?"
- "Who do you want to be for your patients?"
- "What are you going to do specifically for your patients that only you can do?"
Fassas notes that many of the possible essay topics a med school hopeful can choose are subjects that other premeds can also discuss, such as a love of science. However, aspiring doctors can make their personal statements unique by articulating the lessons they learned from their life experiences, she suggests.
Prospective medical students need to clarify why medicine is a more suitable calling for them than other caring professions, health care fields and science careers, Fassas notes. They should demonstrate awareness of the challenges inherent in medicine and explain why they want to become doctors despite those difficulties, she says.
Tips on Crafting an Excellent Medical School Personal Statement
The first step toward creating an outstanding personal statement, Fassas says, is to create a list of significant memories. Premeds should think about which moments in their lives mattered the most and then identify the two or three stories that are definitely worth sharing.
Dr. Demicha Rankin, associate dean for admissions at the Ohio State University College of Medicine , notes that a personal statement should offer a compelling portrait of a person and should not be "a regurgitation of their CV."
The most outstanding personal statements are the ones that present a multifaceted perspective of the applicant by presenting various aspects of his or her identity, says Rankin, an associate professor of anesthesiology.
For example, a premed who was a swimmer might explain how the discipline necessary for swimming is analogous to the work ethic required to become a physician, Rankin says. Likewise, a pianist or another type of musician applying to medical school could convey how the listening skills and instrument-tuning techniques cultivated in music could be applicable in medicine, she adds.
Rankin notes that it's apparent when a premed has taken a meticulous approach to his or her personal statement to ensure that it flows nicely, and she says a fine essay is akin to a "well-woven fabric." One sign that a personal statement has been polished is when a theme that was explored at the beginning of the essay is also mentioned at the end, Rankin says, explaining that symmetry between an essay's introduction and conclusion makes the essay seem complete.
Rankin notes that the author of an essay might not see flaws in his or her writing that are obvious to others, so it's important for premeds to show their personal statement to trusted advisers and get honest feedback. That's one reason it's important to begin the writing process early enough to give yourself sufficient time to organize your thoughts, Rankin says, adding that a minimum of four weeks is typically necessary.
Mistakes to Avoid in a Medical School Personal Statement
One thing premeds should never do in an admissions essay is beg, experts say. Rankin says requests of any type – including a plea for an admissions interview – do not belong in a personal statement. Another pitfall to avoid, Rankin says, is ranting about controversial political subjects such as the death penalty or abortion.
If premeds fail to closely proofread their personal statement, the essay could end up being submitted with careless errors such as misspellings and grammar mistakes that could easily have been fixed, according to experts. Crafting a compelling personal statement typically necessitates multiple revisions, so premeds who skimp on revising might wind up with sloppy essays, some experts say.
However, when fine-tuning their personal statements, premeds should not automatically change their essays based on what others say, Fogerty warns.
"A common mistake on personal statements is having too many people review your statement, they make recommendations, you accept all of the changes and then – in the end – the statement is no longer your voice," Fogerty wrote in an email. It's essential that a personal statement sound like the applicant and represent who he or she is as a person, Fogerty says.
Dr. Nicholas Jones, a Georgia-based plastic and reconstructive surgeon, says the worst error that someone can make in the personal statement is to be inauthentic or deceptive.
"Do not lie. Do not fabricate," he warns.
Jones adds that premeds should not include a story in their personal statement that they are not comfortable discussing in-depth during a med school admissions interview . "If it's something too personal or you're very emotional and you don't want to talk about that, then don't put it in a statement."

Medical School Personal Statement Examples
Here are two medical school admissions essays that made a strong, positive impression on admissions officers. The first is from Columbia and the second is from the University of Minnesota. These personal statements are annotated with comments from admissions officers explaining what made these essays stand out.
Searching for a medical school? Get our complete rankings of Best Medical Schools.
Tags: medical school , education , students , graduate schools
Popular Stories
Best Colleges

Applying to Graduate School

Paying for College

Medical School Admissions Doctor

Applying to College

You May Also Like
Get accepted to multiple top b-schools.
Anayat Durrani May 16, 2024
Premeds and Emerging Medical Research
Zach Grimmett May 14, 2024
How to Get a Perfect Score on the LSAT
Gabriel Kuris May 13, 2024

Premeds Take 5 Public Health Courses
Rachel Rizal May 7, 2024

Fortune 500 CEOs With a Law Degree
Cole Claybourn May 7, 2024

Why It's Hard to Get Into Med School
A.R. Cabral May 6, 2024

Pros, Cons of Unaccredited Law Schools
Gabriel Kuris May 6, 2024

An MBA and Management Consulting
Sammy Allen May 2, 2024

Med School Access for Minority Students
Cole Claybourn May 2, 2024

Different jobs with med degree
Jarek Rutz April 30, 2024

- Open access
- Published: 28 November 2014
Should essays and other “open-ended”-type questions retain a place in written summative assessment in clinical medicine?
- Richard J Hift 1
BMC Medical Education volume 14 , Article number: 249 ( 2014 ) Cite this article
17k Accesses
59 Citations
Metrics details
Written assessments fall into two classes: constructed-response or open-ended questions, such as the essay and a number of variants of the short-answer question, and selected-response or closed-ended questions; typically in the form of multiple-choice. It is widely believed that constructed response written questions test higher order cognitive processes in a manner that multiple-choice questions cannot, and consequently have higher validity.
An extensive review of the literature suggests that in summative assessment neither premise is evidence-based. Well-structured open-ended and multiple-choice questions appear equivalent in their ability to assess higher cognitive functions, and performance in multiple-choice assessments may correlate more highly than the open-ended format with competence demonstrated in clinical practice following graduation. Studies of construct validity suggest that both formats measure essentially the same dimension, at least in mathematics, the physical sciences, biology and medicine. The persistence of the open-ended format in summative assessment may be due to the intuitive appeal of the belief that synthesising an answer to an open-ended question must be both more cognitively taxing and similar to actual experience than is selecting a correct response. I suggest that cognitive-constructivist learning theory would predict that a well-constructed context-rich multiple-choice item represents a complex problem-solving exercise which activates a sequence of cognitive processes which closely parallel those required in clinical practice, hence explaining the high validity of the multiple-choice format.
The evidence does not support the proposition that the open-ended assessment format is superior to the multiple-choice format, at least in exit-level summative assessment, in terms of either its ability to test higher-order cognitive functioning or its validity. This is explicable using a theory of mental models, which might predict that the multiple-choice format will have higher validity, a statement for which some empiric support exists. Given the superior reliability and cost-effectiveness of the multiple-choice format consideration should be given to phasing out open-ended format questions in summative assessment. Whether the same applies to non-exit-level assessment and formative assessment is a question which remains to be answered; particularly in terms of the educational effect of testing, an area which deserves intensive study.
Peer Review reports
Learning and the stimulation of learning by assessment
Modern definitions of learning, such as that attributed to Siemens: “Learning is a continual process in which knowledge is transformed into something of meaning through connections between sources of information and the formation of useful patterns, which generally results in something that can be acted upon appropriately, in a contextually aware manner” [ 1 ],[ 2 ] essentially stress two points: firstly, that learning requires a much deeper, effortful and purposeful engagement with the material to be learned than the acquisition of factual knowledge alone; secondly, that learned knowledge does not exist in a vacuum; its existence is inferred from a change in the learner’s behaviour. This has led transfer theorists to postulate that knowledge transfer is the basis of all learning, since learning can only be recognised by observing the learner's ability to display that learning later [ 3 ],[ 4 ].
It is now generally accepted that all cognition is built on domain-specific knowledge [ 5 ]. Content-light learning does not support the ability to transfer knowledge to new situations and a comprehensive store of declarative or factual knowledge appears essential for transfer [ 4 ]. Furthermore, a high order of understanding and contextualization must accompany the declarative knowledge if it is to be successfully applied later. Where transfer – in other words, the successful application of knowledge to new situations – has been shown, the common factor appears to be deep learning, and the abstraction of general principles [ 6 ]-[ 8 ].
Indeed, knowledge may be acquired and held at varying depths. Aspects of this are reflected in the cognitive levels of learning constituting Bloom's taxonomy of learning [ 9 ]-[ 14 ] (Figure 1 ); the varying levels of clinical competence and performance described in Miller’s pyramid [ 15 ] (Figure 2 ) and the stages of proficiency postulated by Dreyfus and Dreyfus [ 16 ]. The extent to which different assessment formats measure proficiency over the entire range of complexity of understanding and performance is one of the central issues in assessment.
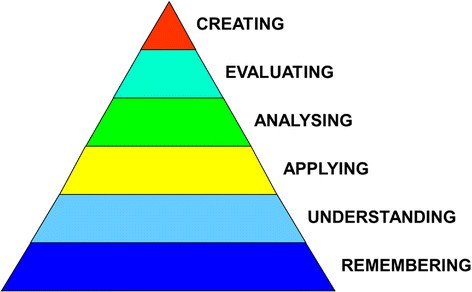
Modified bloom’s taxonomy [ [ 11 ] ].
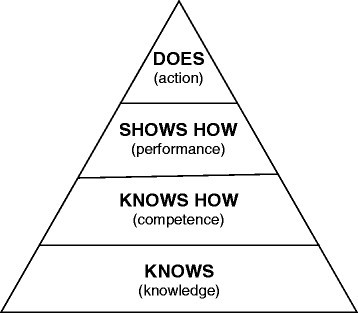
Miller’s pyramid of assessment of clinical skills, competence and performance [ [ 15 ] ].
Assessment is central to the educational process, and has benefits beyond that of measuring knowledge and competence alone; principally in directing and stimulating learning, and in providing feedback to teachers and learners [ 17 ]. Recent research supports a critical role for assessment in consolidating learning, and strengthening and facilitating memorisation and recall. There is accumulating evidence that the process of stimulating recall through testing enhances learning and retention of learned material. This has been termed the testing effect , and several hypotheses have been put forward to explain it, including increased cognitive effort, conceptual and semantic processing, and increased attention to the properties distinguishing the learnt item from similar items, which strengthens the relationship between the cue which triggers the memory and the memory item itself [ 18 ],[ 19 ]. It appears to be principally the act of retrieving information from memory which strengthens knowledge and knowledge retention [ 20 ],[ 21 ], irrespective of whether retrievable is covert or overt [ 22 ]. Importantly, high-level questions appear to stimulate deeper conceptual learning and better learning retention then those pitched at a lower level [ 23 ]. A number of strategies have been proposed to exploit this in educational practice, including those recently summarised for use in medical education [ 24 ]. This is in a sense related to the “generation effect”, where it has been shown that spontaneously generating information as opposed to learning it passively improves subsequent recall [ 18 ],[ 19 ].
Assessment in educational practice
It is accepted that standards of assessment are inherently variable. There is therefore an obligation, in summative assessment, to ensure that assessment meets certain minimum criteria [ 25 ]. Achieving this in the individual instance is challenging, given the wide range of skills and knowledge to be assessed, marked variation in the knowledge of assessment of those who must assess and the highly variable environments in which the assessment takes place. There is now an extensive literature on assessment, in terms of research, guidelines and recommendations [ 26 ],[ 27 ]. Importantly, modern approaches recognise that no single form of assessment is suitable for every purpose, and stressed the need for programmatic assessment , which explicitly recognises that assessment is best served by a careful combination of a range of instruments matched to a particular purpose at each stage of the learning cycle, such as for formative, diagnostic or summative purposes [ 25 ],[ 26 ],[ 28 ].
Written assessment
Despite the proliferation of assessment methodologies which attempt to test the competence of medical students directly, such as OSCE, OSPE, case-based assessment, mini-CEX and workplace-based assessment, written assessments remain in widespread use. Much of the knowledge base required by the clinician is not necessarily testable in the performance format. Additionally, in comparison with most practical assessment formats, written tests are easier to organize and deliver, requiring little more than pen and paper or a computer, a venue, question setters and markers who need not be physically present.
In general, all forms of written assessment may be placed into one of two categories. Constructed response or open-ended questions include a variety of written formats in which the student is required to generate an answer spontaneously in response to a question. The prototypical example is the essay. There are many variants including short answer questions (SAQ), mini-essay questions, single-word and single-sentence questions and the modified essay question (MEQ). The selected-response or closed-ended format is typified by the multiple-choice question (MCQ) assessment, where candidates select the most appropriate answer from a list of options rather than generating an answer spontaneously. Many variants of the multiple-choice format have been used: current best practice recommends the use of one-best-answer (of three, four or five possible answers), and extended matching item (EMI) formats [ 29 ]. In this debate I shall use the term open-ended when referring to the constructed-response format, and multiple-choice as a synonym for the selected-response format.
All high-stakes assessments should meet an adequate standard in terms of quality and fairness, as measured by a number of parameters, summarised recently in a consensus statement [ 30 ]. Principal among these are the classic psychometric parameters of reproducibility (reliability or consistency; that a result would not essentially change with retesting under similar conditions), and validity or coherence, which I describe in detail below. Other important measures by which assessments should be judged are equivalence (assessments administered at different institutions or during different testing cycles produce comparable outcomes), feasibility (particularly in terms of efficiency and cost effectiveness), educational effect (the student who takes the assessment is thereby motivated to undertake appropriate learning), catalytic effect (the assessment provides outcomes that, when fed back into the educational programme, result in better teaching and learning) and acceptability to both teachers and learners.
It is generally accepted that the multiple-choice format, in contrast to the open-ended format, has high reliability and is efficient, a consequence primarily of wide sampling, and to a lesser extent, of its objectivity. In support of the open-ended format, it has been widely held that this format is superior at testing higher cognitive levels of knowledge and has greater validity. This belief is intuitively appealing and appears to represent the viewpoint of many of those involved in medical assessment, including those with extensive knowledge and experience in medical education. In an attempt to gain the best of both formats, there has been a shift from the prototypical essay towards newer formats comprising a larger number of short, structured questions, a development intended to retain the perceived benefit of the open-ended question with the superior reliability of the MCQ.
Thus the two formats are generally seen to be in tension, MCQ being significantly more reliable, the open-ended format having greater validity. In this debate I will compare the performance of the open-ended format with MCQ in summative assessment, particularly in final exit examinations. I draw attention to the large body of evidence which supports the view that, in summative assessment, the multiple-choice format is intrinsically able to provide all the value of the open-ended format and does so more reliably and cost effectively, thus throwing into question the justification for the inclusion of the open-ended format in summative assessment. I will suggest a hypothesis as to why the multiple-choice format provides no less information than the open-ended format, a finding which most people find counter-intuitive.
A critical concept is that assessment is not only of learning, but also for learning [ 27 ],[ 31 ]. In the first case, the purpose of assessment is to determine whether that which is required to be learnt has in fact been learnt. In the second case, it is acknowledged that assessment may in itself be a powerful driver for learning at the cognitive level. This is supported by a body of evidence indicating the powerful effect of assessment on strengthening memorisation and recall [ 20 ],[ 22 ],[ 23 ]. In this debate I concentrate primarily on summative assessment in its role as assessment of learning ; one must however remain aware that those methods of assessment best suited to such summative assessment may not be identical to those best suited to assessment for learning ; indeed, it would be surprising if they were.
For the first part of the 20 th century, written assessment in medicine consisted largely of essay-writing [ 30 ]. Multiple-choice assessment was developed for psychological testing by Robert Yerkes immediately before the First World War and then rapidly expanded for the testing of army recruits. Yerkes was interested in assessing learning capacity—not necessarily human—and applied it to crows [ 32 ] and pigs [ 33 ] as well as psychiatric patients and mentally challenged subjects, a group among whom it was widely used for a number of years thereafter [ 34 ],[ 35 ]. Application to educational assessment has been credited to Frederick J. Kelly in 1914, who was drawn to it by its efficiency and objectivity [ 36 ].
Throughout its history, the multiple-choice format has had many detractors. Their principal arguments are that closed-ended questions do not stimulate or test complex constructive cognitive processes, and that if the ability to construct rather than choose a correct answer is not actively assessed, there is a potential that it will be neither taught nor learnt [ 37 ]-[ 41 ].
As Rotfield has stated: "Students proudly show off their high grades, from multiple-choice exams, as if their future careers will depend on knowing which choice to make instead of discerning which choices exist" [ 42 ]. Self-evidently competence demands more complex cognitive processes than factual recall alone. The ability to invoke these higher levels of cognition is clearly a skill which should be explicitly assessed. Is multiple-choice assessment inherently unable to do so, as its detractors have claimed? The belief that open-ended questions test high-order cognitive skills whereas multiple-choice questions do not and that therefore by inference open-ended questions evoke and test a reasoning process which is more representative of real-life problem-solving than multiple-choice, is a serious concern which I address in this review. We begin however with a comparison of the two formats in terms of reproducibility and feasibility.
Reliability and efficiency of open-ended and multiple-choice question formats
Wider sampling greatly increases reproducibility, compensating as it does for unevenness in a candidate’s knowledge, varying quality of questions and even the personality of examiners [ 43 ],[ 44 ]. That the reproducibility of the multiple-choice format is much higher than that of the open-ended format is borne out in numerous studies comparing the two formats [ 45 ]-[ 47 ]. Recognition of these shortcomings has led to the design of open-ended-formats specifically intended to increase reproducibility and objectivity, while maintaining the supposed advantages of this format in terms of validity. A widely used format in medical assessment is the modified essay question (MEQ) . The format is of a clinical scenario followed by a series of sequential questions requiring short answers. This was expressly designed to bridge a perceived gap between multiple-choice and SAQ as it was believed that it would prove better at testing high-order cognitive skills than multiple-choice while allowing for more standardised marking than the standard open-ended question [ 45 ].
Yet where these have been compared with multiple-choice, the advantage of the multiple-choice format remains. A large number of questions and multiple markers are required in order to provide acceptable reliability for MEQs and essay questions [ 45 ]. Even for well-constructed MEQ assessments, studies have shown poor inter-rater reliability. Thus in an MEQ paper in a final undergraduate medical exit examination marked in parallel by several assessors, statistically significant differences between the scores of the different examiners were shown in 50% of the questions, as well as significant differences in the median scores for the examination as a whole [ 47 ]. Nor were these differences trivial; a substantial difference in outcome in terms of likelihood of failure were shown. This is cause for concern. Schuwirth et al . have stressed the necessity for interpreting reliability in terms of outcome, particularly in terms of pass/fail misclassification, and not merely in terms of numeric scores such as Cronbach’s alpha [ 27 ]. In this and other such studies the open-ended questions were of the highest possible quality practically achievable, typically MEQ's carefully prepared by skilled question writers working in teams, reviewed for appropriateness and scored using an analytic scoring scheme designed to minimise inter-rater variability. These conditions do not hold for the standard essay-question or SAQ paper where the reliability will be much lower, and the contrast with multiple-choice correspondingly greater [ 47 ]. Open-ended items scored on a continuum, such as 0-100%, have much lower inter-rater reliability than those scored against a rigid marking schedule. Therefore the discrepancy in reliability for the "graded essay" marked on a continuum versus multiple-choice is much larger than it is for more objectively scored open-ended formats.
In contrast to the open-ended question format, the multiple-choice is objective and allows multiple sampling of a subject. The result is high reproducibility. Furthermore it substantially reduces the potential for a perception of examiner bias, and thus the opportunity for legal challenge by the unsuccessful candidate [ 48 ]. The multiple-choice format is efficient. Lukhele et al . studied a number of national university-entrance examinations which included both multiple-choice items and essay questions [ 49 ]. They found that 4-8 multiple-choice items provided the same amount of information as a single essay, and that the essay’s efficiency in providing information about the candidate’s ability per minute of testing was less than 10% of that of an average multiple-choice item. For a middle-level examinee, approximately 20 times more examination time was required for an essay to obtain the same information as could be obtained from a multiple-choice assessment. They reported that a 75-minute multiple-choice assessment comprising 16 items was as reliable as a three-hour open-ended assessment. Though the relative gain in efficiency using multiple-choice in preference to essay questions varies according to subject, it is an invariable finding [ 49 ].
Though the initial development of an multiple-choice assessment is labour-intensive, this decreases with increasing experience on the part of item-writers, and decreases further once a question bank has been developed from which questions can be drawn for re-use. The lower efficiency of the open-ended question is not restricted to examination time but also the requirement for grading by examiners. Typically an open-ended test requires from 4 to 40 times as long to administer as a multiple-choice test of equivalent reliability [ 50 ]. In one study, the cost of marking the open-ended items was 300 times that of the multiple-choice items [ 49 ]; the relative cost of scoring the papers may exceed a factor of 1000 for a large examination [ 50 ].
The multiple-choice format thus has a clear advantage over open-ended formats in terms of reproducibility, efficiency and cost-effectiveness. Why then are open-ended questions still widely used? Principally this is because of a belief that essay-type questions, SAQ and their variants test higher-order cognitive thinking in a manner that MCQ cannot, and consequently have higher validity. It has been repeatedly stated that the MCQ format is limited in its ability to test deep learning, and is suitable for assessing facts only, whereas open-ended questions assess dynamic cognitive processes such as the strength of interconnected rules, the use of the mental models, and the mental representations which follow [ 37 ]-[ 39 ]; in short that open-ended questions permit the assessment of logical and reasoning skills in a manner that multiple-choice does not [ 40 ],[ 41 ]. Is there evidence to support these assertions?
The ability to test higher-order cognitive skills
The revised Bloom's taxonomy of learning [ 9 ]-[ 12 ] is helpful in evaluating the level of cognition drawn upon by an assessment (Figure 1 ). By convention, assessment questions targeting the first two levels, are regarded as low-level questions, the third level as intermediate, and the fourth to sixth levels as high-level.
Those who understand the principles underlying the setting of high-quality multiple-choice items have no difficulty in accepting that multiple-choice is capable of assessing high-order cognition [ 10 ],[ 13 ],[ 14 ]. The shift from true-false questions, (which in order to avoid ambiguity frequently test factual information only) to the one-best-answer and EMI formats have facilitated this [ 29 ]. Indeed, there exist well-validated instruments specifically designed to assess critical thinking skills and to measure their development with progress through college-level educational programs, which are entirely multiple-choice based, such as the California Critical Thinking Skills Test [ 51 ],[ 52 ]. Schuwirth and Van der Vleuten [ 48 ] make a distinction between context-rich and context-free questions. In clinical assessment, a context-rich question is typically presented as a case vignette. Information within the vignette is presented to candidates in its original raw format, and they must then analyse, interpret and evaluate this information in order to provide the answer. The stimulus reflects the question which the candidate must answer and is therefore relevant to the content of the question. An example of a final-year question in Internal Medicine is shown in the following example. Such a question requires analysis ( What is the underlying problem? ), application ( How do I apply what I know to the treatment of this patient? ) and evaluation ( Which of several possible treatments is the most appropriate? ), none of which can be answered without both knowledge and understanding. Thus 5 of Bloom’s 6 levels have been tested.
Example of a context-rich multiple-choice item in internal medicine
A 24-year-old woman is admitted to a local hospital with a short history of epistaxis. On examination she is found to have a temperature of 36.9°C. She is wasted, has significant generalised lymphadenopathy and mild oral candidiasis but no dysphagia. A diffuse skin rash is noticed, characterised by numerous small purple punctate lesions. A full blood count shows a haemoglobin value of 110 g/L, a white cell count of 3.8×10 9 per litre and platelet count of 8.3×10 9 per litre. Which therapeutic intervention is most urgently indicated in this patient?
Antiretroviral therapy
Fluconazole
Platelet concentrate infusion
None of the options offered are obviously unreasonable or easily excluded by the candidate who attempts to shortcut the cognitive processes required in answering it by searching for clues in the options themselves. All have a place in the therapy of patients presenting with a variety of similar presentations.
Answering this item requires:
Analysis . In order to answer this item successfully, the candidate will have to recognise (1) that this patient is highly likely to be HIV-positive (given the lymphadenopathy, evidence of oral candidiasis and the high local prevalence of HIV), (2) that the presentation is suggestive of immune thrombocytopenic purpura (given the epistaxis, skin manifestations and very low platelet count), (3) that other commonly-seen concomitant features such as severe bacterial infection and extensive esophageal candidiasis are excluded by a number of negative findings.
Evaluation . Further, in order to answer this item successfully, the candidate will have to (1) consider the differential diagnosis for the principal components of the clinical vignette and, by process of evaluation, decide which are the most likely; (2) decide which of the diagnoses require treatment most urgently, (3) decide which form of therapy will be most appropriate for this.
Knowledge, understanding and application . It is utterly impossible to “recognise” the correct answer to this item without having worked through this process of analysis and evaluation, and the knowledge required to answer it must clearly be informed by deep learning, understanding and application. Hence five of the six levels of Bloom’s taxonomy have been tested. Furthermore it would appear an eminently reasonable proposition that the candidate who correctly answers this question will indeed be able to manage such a patient in practice, hence implying structural validity.
Though guessing has a 20% chance of providing the correct answer, this will be eliminated as a factor by assessing performance across multiple such items and applying negative marking to incorrect answers.
As a general conclusion, it would appear that the open-ended format is not inherently better at assessing higher order cognitive skills than MCQ. The fundamental determinant is the way in which the question is phrased in order to stimulate higher order thinking; if phrased inappropriately, the open-ended format will not perform any better than MCQ. A crucial corollary is that in comparing formats, it is essential to ensure that MCQ questions crafted to elicit high order thinking (particularly those which are context-rich) are compared with open-ended questions crafted to the same level; it is inappropriate to compare high-order items in one format with low order items in the other. Several studies have investigated the effect of the stimulus on thought processes in the open questions and have shown that the stimulus format is more important than the response format . Scores on questions in open-ended format and multiple-choice format correlate highly (approaching 100%) for context-rich questions testing the same material. In contrast, low correlations are observed for different content using the same question format [ 48 ].
In response to the low objectivity and reliability of the classic essay-type questions, modified open-ended formats have evolved which typically combine short answers, carefully crafted questions and rigid marking templates. Yet this increase in reliability appears to come at a significant cost to the presumed advantage of the open-ended format over the multiple-choice format in testing higher orders of cognition. Feletti and Smith have shown that as the number of items in the open-ended examination increases, questions probing high-order cognitive skills tend to be replaced by questions requiring factual recall alone [ 46 ]. Hence as accuracy and reliability increase, any difference between such an assessment and a multiple-choice assessment in terms of other indicators tends to disappear; ultimately they converge on an essentially identical assessment [ 47 ],[ 49 ].
Palmer and Devitt [ 45 ] analysed a large number of multiple-choice and MEQ questions used for summative assessment in a clinical undergraduate exam. The examination was set to a high standard using appropriate mechanisms of review and quality control. Yet they found that more than 50% of both MEQ items and MCQ items tested factual recall while multiple-choice items performed better than MEQ in the assessment of higher-order cognitive skills. They reported that "the modified essay question failed in its role of consistently assessing higher cognitive skills whereas the multiple-choice frequently tested more than mere recall of knowledge”.
In a subsequent study of a rigorously prepared and controlled set of exit examinations, they reported that the proportion of questions testing higher-level cognitive skills was lower in the MEQ paper then in the MCQ paper. More than 50% of the multiple-choice items assessed higher level cognition, as opposed to just 25% of the MEQ items. The problem was compounded by a higher frequency of item-writing flaws in the MEQ paper, and flaws were found in the marking scheme in 60% of the MEQ's. The authors conclude that “The MEQ paper failed to achieve its primary purpose of assessing higher cognitive skills” [ 47 ].
We therefore appear to be dealing with a general rule: the more highly open-ended questions are structured with the intention of increasing reliability, the more closely they converge on an equivalent multiple-choice question in terms of performance, thus negating any potential advantage of the open-ended format over the closed-ended [ 53 ]; indeed they appear frequently to underperform MCQ items in the very area in which they are believed to hold the advantage. Thus the shift to these newer forms of assessment may actually have had a perverse effect in diminishing the potential for the open-ended assessment to evaluate complex cognitive processes. This does not imply that open-ended items such as SAQ, MEQ and key-feature assessments, particularly those designed to assess clinical reasoning, are inherently inferior to MCQ; rather it is a warning that there is a very real risk in practice of “dumbing-down” such questions in an attempt to improve reliability, and empiric observations suggest that this is indeed a consequence frequently encountered even in carefully crafted assessments.
Combining multiple-choice and open-ended tests in the same assessment, in the belief that one is improving the strength of the assessment, leads to an overall less reliable assessment than is constituted by the multiple-choice section on its own [ 49 ], thus causing harm rather than adding benefit [ 50 ].
The second argument, frequently advanced in support of the open-ended format, is that it has greater validity; that spontaneously recalling and reproducing knowledge is a better predictor of the student’s eventual ability to handle complex problems in real-life then is the ability to select an answer from a list [ 54 ]. Indeed, this argument is intuitively highly appealing. The case for the retention of open-ended questions in medical undergraduate and postgraduate assessment largely rests on validity, with the assumption that asking the candidate to describe how they would diagnose, investigate and treat a patient predicts future clinical competence more accurately than does the ability to select the right response from a number of options [ 55 ],[ 56 ]. The question of validity is central. If the open-ended format is genuinely of higher validity than the multiple-choice format, then there is a strong case for retaining essay-type questions, SAQ and MEQ in the assessment protocol. If this contention cannot be supported, then the justification for retaining open-ended items in summative assessment may be questioned.
Is the contention true? Essentially, this may be explored at two levels. The first is to correlate outcomes between the two formats. The second is to perform appropriate statistical analysis to determine whether these formats are indeed testing different dimensions or “factors”.
Validity is an indicator of how closely the assessment actually measures the quality it purportedly sets out to test. It is self-evident that proficiency in many domains, including clinical practice, requires not only the ability to recall factual knowledge, but also the ability to generate and test hypotheses, integrate knowledge and apply it appropriately as required.
Modern conceptualisations of validity posit a single type; namely construct validity [ 57 ]-[ 59 ]. This is based on the premise that ultimately all validity rests on the fidelity with which a particular assessment reflects the underlying construct, “intangible collections of abstract concepts and principles which are inferred from behaviour and explained by educational or psychological theory” [ 60 ]. Construct validity is then defined as a process of investigation in which the constructs are carefully delineated, and evidence at multiple levels is sought which supports a valid association between scores on that assessment and the candidate's proficiency in terms of that construct. For example, five types of evidence have been proposed which may provide support for such an association [ 60 ],[ 61 ], namely content, the response process, internal structure, relationship to other variables and consequences. In this discussion we highlight the relevant to the last two methods; convergent correlations between the two forms of assessment, and the impact of test scores on later performance, particularly that requiring problem-solving under conditions encountered in the work situation. This “is particularly important to those employers more interested in hiring competent workers than good test takers” [ 62 ].
Direct comparisons of the open-ended and multiple-choice formats
Correlation.
Numerous studies have assessed the correlation of scores between the two formats. If scores are highly correlated, the two formats are essentially measuring the same thing in which case, in terms of validity, there is no advantage of one over the other. With few exceptions, studies indicate that scores on the two forms of assessment are highly correlated. Norman et al. compared the two formats prospectively and showed a strong correlation between the two sets of scores [ 63 ]. A similar result was found by Palmer et al. who suggested that the two types of examination were essentially testing similar characteristics [ 47 ]. Similarly Norcini et al. found that written patient management problems and multiple choice items appeared to be measuring essentially the same aspects of clinical competence, though the multiple-choice items did so more efficiently and with greater reliability [ 17 ]. Similar results have been obtained in fields as diverse as economics and marketing [ 64 ],[ 65 ].
In general correlations between the two formats are higher when the questions in each format are specifically designed to be similar (stem-equivalent), and lower where the items in the two formats differ. However, the difference is not great: in a meta-analysis, Rodriguez found a correlation across 21 studies of 0.92 for stem-equivalent items and 0.85 across 35 studies for non-stem-equivalent items. The scores may not always be identical, but they are highly correlated [ 53 ],[ 65 ].
Factor analysis: do the formats measure more than one construct?
Identification of the actual constructs measured in an assessment has proved challenging given the lack of congruence between the simple cognitive assumptions on which testing is often based and the very complex cognitive nature of the constructs underlying understanding [ 66 ]. A number of studies have used confirmatory factor analysis and principal component analysis to determine whether the constructs tested by the two formats lie along a single dimension or along two or more divergent dimensions. Bennett et al . compared a one factor model with a two factor model to examine the relationship of the open-ended and closed-ended formats and found that in general the single factor provided a better fit. This suggests that essentially the two formats are testing the same thing [ 67 ]. Similarly Bridgeman and Rock found, using a principal components model, that both formats appeared to load on the same factor, implying that the open-ended format was not providing information on a different dimension [ 68 ]. Thissen and Wainer found that both formats could largely be ascribed to a single shared factor but did find some specific open-ended factors for which only the open-ended items contributed [ 69 ]. Though Lissitz et al . [ 70 ] quote a study by JJ Manhart, which found a two-factor model generally more appropriate than a one factor model, this study has not been published and the significance of the divergence cannot be assessed.
In a study of high school assessments using confirmatory factor analysis, Lissitz et al. showed a correlation of 0.94 between the two formats in the domains of algebra and biology; a two-factor model provided a very slight increment over a one-factor model in terms of fit. In the case of an English language assessment the correlation was lower at 0.74 and a two-factor model provided a better fit. In a test of US government, intermediate results were found with the correlation of 0.83 and a slight superiority of a two-factor model. This suggests that the addition of open-ended items in biology and algebra provided little further information beyond the multiple-choice items, whereas in other domains—English and government—the two formats are to some degree measuring different constructs [ 70 ]. Indeed, the literature in general suggests that differences in format appeared to be of little significance in the precise sciences such as biology and mathematics, but may have some relevance in fields such as history and languages, as suggested by Traub and Fisher [ 71 ]. In summary, there is little evidence to support the belief that the open-ended format is testing dimensions which the multiple-choice format cannot [ 53 ],[ 70 ],[ 72 ].
Construct validity was specifically assessed by Hee-Sun et al . [ 73 ], who attempted to measure the depth of understanding among school-level science students revealed by multiple-choice and short written explanatory answers respectively. They reported that students who showed higher degrees of knowledge integration were more likely to score highly on multiple-choice, though the reverse did not hold true. They suggested that the multiple-choice items were less effective in distinguishing adjacent grades of understanding as opposed to distinguishing high-performance from low performance, a finding similar to that of Wilson and Wang [ 74 ] and Ercikan et al . [ 75 ]. Unfortunately the generalisability of these results is limited since the multiple-choice items were poorly standardised, both in format and in difficulty, and the circumstances under which the testing was conducted were essentially uncontrolled.
Lukhele et al . performed a rigorous analysis of high-quality university placement exams taken by thousands of candidates [ 49 ]. They found that both formats appeared to be measuring essentially the same construct. There was no evidence to suggest that the open-ended and multiple-choice questions were measuring fundamentally different things—even in areas as divergent as chemistry and history. Factorial analysis suggested that there were two variant dimensions reflected in the scores of the multiple-choice and open-ended sections, one slightly more related to multiple-choice and the other to the open-ended format. However these were highly correlated, whatever the factor is that is specifically measured by the open-ended format, multiple-choice would measure it almost as well. Thus for all practical purposes, in such summative assessments, multiple-choice assessments can satisfactorily replace open-ended assessments.
An important principle is that the variance introduced by measuring “the wrong thing” in the multiple-choice is small in comparison with the error variance associated with the open-ended format given its low reliability. This effectively cancels out any slight advantage in validity [ 49 ] (Figure 3 ). Indeed, Wainer and Thissen state that “measuring something that is not quite right accurately may yield far better measurement than measuring the right thing poorly” [ 50 ].
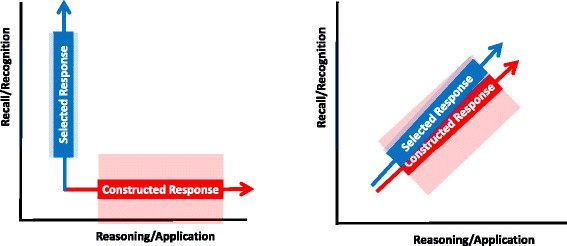
Stylized depiction of the contrasting ability of the presumed open-ended and multiple-choice formats to assess recognition and recall as opposed to higher forms of cognitive learning. Ideally, multiple-choice and open-ended questions would measure two different abilities (such as recall/recognition versus reasoning/application) – this may be shown as two divergent axes (shown on left). The error variance associated with each type of question is indicated by the shaded blocks, and is much greater for the open-ended question, given its inherent lower reliability. In practice, it appears that the two axes are closely aligned, implying that the two types of questions are measuring essentially the same thing (shown on right). What little additional information the open-ended question might be giving (as shown by a slight divergence in axis) is offset by its wide error variance, which in effect overlaps the information given by the multiple-choice question, thus significantly reducing the value of any additional information it provides.
In summary, where studies have suggested that the open-ended format is measuring something that multiple-choice does not (particularly in older studies), the effect has tended to be minimal, or possibly explicable on methodological grounds, or indefinable in terms of what is actually being measured. In contrast, methodologically sound studies converge on the conclusion that the difference in validity between the two formats is trivial. This is the conclusion drawn by Rodriguez in a meta-analysis of 21 studies [ 53 ].
Demonstrating an essential similarity for the two formats under the conditions of summative assessment does not necessarily mean that they provide identical information. It is possible and indeed likely that open-ended questions may make intermediate steps in thinking and understanding visible, thus serving a useful role in diagnostic as opposed to summative assessment [ 73 ],[ 75 ],[ 76 ]. Such considerations are particularly useful in using assessment to guide learning rather than merely as a judgment of competence [ 77 ]. In summative assessment at a stage prior to final exit from a programme, and particularly in formative assessment, the notion of assessment for learning becomes important; and considerations such as the generation effect and the potentiation of memory recall by testing cannot be ignored. Interestingly, a recent publication suggests that multiple-choice format testing is as effective as SAQ-format testing in potentiating memorisation and recall [ 23 ], thus supporting the contention that well-crafted MCQ and open-ended questions are essentially stimulating the same cognitive processes in the learner.
Some authors have raised the concern that students may constitutionally perform differentially on the two forms of assessment, and might be disadvantaged by a multiple-choice assessment should their strengths lie in the open-ended format. Studies in this area have been reassuring. Bridgeman and Morgan found that discrepant results were not predictive of poor academic performance as assessed by other parameters [ 78 ]. Ercikan et al . reported that discrepancies in the outcome between open-ended and multiple-choice tests were largely due to the low reliability of the open-ended component and inappropriate testing strategies [ 75 ]. A study which correlated the two formats with each other and with other measures of student aptitude showed a high degree of correlation and was unable to identify students who clearly had a propensity to perform consistently better on one format than the other [ 79 ]. Thus the belief that some students are constitutionally more suited to open-ended questions than to multiple-choice would appear to be unfounded.
An important question is whether the format of assessment effects the type of learning students use in preparation for it. As early as 1971, Hakstian suggested that anticipation of a specific form of examination did not result in any change in the amount or type of preparation, or any difference in performance in subsequent testing [ 80 ]. He concluded as follows: “The use of various types of tests to foster various kinds of study and learning, although widely advocated would seem to be a practice based on intuitive appeal, but not convincingly supported by empirical research. In particular, the contention that the superiority of the essay examination is its ability to promote more desirable study methods and higher performance on tasks requiring organisation, and deeper comprehension analysis of information should be re-evaluated in light of the evidence in the present study of no differences between groups in terms of study methods, the essay examination, or items from the higher levels of the cognitive domain”. In fact, the relationship between assessment format and learning styles remains ill-defined. Though some studies have suggested that students tended to make more use of surface learning strategies in preparation for MCQ and deeper learning strategies in preparation for open-ended questions [ 81 ],[ 82 ], other studies have failed to show such an association [ 80 ],[ 83 ]. Some studies have even failed to show that deep learning approaches correlated with better performance in applied MCQ’s and a written course project, both of which required high level cognitive performance [ 84 ],[ 85 ], though, a significant finding was that a surface learning strategy appeared deleterious for both factual and applied MCQ scores [ 85 ].
Indeed, a review of the literature on learning strategies suggests that the notion that one or other assessment format consistently calls forth a particular learning strategy is simplistic, and much of the evidence for this may have been misinterpreted [ 86 ]. The student’s choice of learning style appears to be dependent on multiple interacting and to some extent, confounding factors, most importantly the student’s innate learning motivation and preferred learning strategy. This is however subject to modification by other factors, particularly the student’s own perception of whether the assessment is directed at assessment of factual knowledge or of understanding, a perception which may frequently not coincide with the intentions of the examiner [ 87 ]. Individual differences in learning strategy probably outweigh any other consideration, including the assessment format, though this is not constant and students will adapt their preferred learning strategy according to their perception of the requirement for a particular assessment [ 88 ]. A further study has suggested that the approach to learning the student brings into the course is the strongest predictor of the learning style they will employ subsequently and, irrespective of the instructor’s best efforts, the only factor significantly correlated with the change in learning style is a change in the student’s perception of the cognitive demands of the assessment. Thus students are frequently strategic in their choice of learning strategy, but the strategies may be misplaced [ 87 ]. The student’s academic ability may be relevant; one study has shown that more academically able science students correctly identified the MCQ as requiring deep knowledge and adopted an appropriate learning strategy, whereas less able students interviewed the assessment as principally a test of recall and used a counter-productive surface-learning strategy.
Hadwin et al . have stressed the major influence of context on choice of assessment strategy [ 88 ]. There is for example evidence that students will modify their strategy according to whether the assessment is perceived as a final examination or as an interim assessment, irrespective of format [ 81 ]. So-called construct-irrelevant factors such as female gender and increasing maturity tend to correlate with selection of a deep learning strategy [ 85 ] independent of assessment format, while the association of anxiety and other emotional factors with a particular assessment will impair performance and thus operate as a confounding factor [ 89 ],[ 90 ]. In discussing their results, Smith and Miller stated that “Neither the hypothesis that multiple-choice examination will promote student use of surface strategy nor the hypothesis that essay examination will promote student use of deep strategy were supported” [ 91 ]. As a general conclusion, it would appear valid to say that current evidence is insufficient to suggest that the open-ended format should be preferred over MCQ or vice versa on the grounds that it promotes more effective learning strategies.
It is also important to be aware that open-ended assessments may bring confounding factors into play, for example testing language mastery or skills rather than the intended knowledge domain itself [ 70 ], and hand-written answers also penalise students with poor writing skills, low writing speeds and poor handwriting [ 65 ].
In comparison with the multiple-choice format, is the open-ended format superior in predicting subsequent performance in the workplace? This has been assessed and the answer, surprisingly, is that it may be less predictive. Rabinowitz and Hojat [ 92 ] correlated the single MEQ assessment and five multiple-choice assessments written at the conclusion of a series of six clerkships with performance after graduation. Results in multiple-choice assessment consistently demonstrated the highest correlations with subsequent national examination scores and with objective assessments of performance in the workplace. The MEQ questions showed the lowest correlation. Wilkinson and Frampton directly compared an assessment based on long and short essay-type questions with a subsequent assessment protocol containing short essay questions and two multiple-choice papers [ 56 ], correlating these with performance in the subsequent internship year using robust rating methodologies. They found no significant correlation between the scores of the open-ended question protocol and assessments of performance in the workplace after graduation. In contrast they found that the combination of the SAQ paper and two multiple-choice papers showed a highly significant correlation with subsequent performance. This study showed that the predominant use of multiple-choice in the assessment resulted in a significant improvement in the structural validity of the assessment in comparison with essay-type questions alone. It was unable to answer the question as to whether the open-ended questions are necessary at all since the multiple-choice component was not compared with the performance rating independently of the essay questions. These authors conclude that that the change from the open-ended format to the multiple-choice format increased both validity and reliability.
Recommendations from the literature
Wainer and Thissen stated that: “We have found no evidence of any comparison of the efficacy of the two formats (when a particular trait was specified and skilled item writers then constructed items to measure it) in which the multiple-choice item format was not superior” [ 50 ]. Lukhele et al . concluded: “Thus, while we are sympathetic to… the arguments… regarding the advantages of open-ended format, we have yet to see convincing psychometric evidence supporting them. We are awash in evidence of their drawbacks”, and further, “… We are forced to conclude that open-ended items provide this information in more time at greater cost than the multiple-choice items. This conclusion is surely discouraging to those who feel that open-ended items are more authentic and, hence, in some sense, more useful than multiple-choice items. It should be” [ 49 ].
Palmer et al . have suggested that the MEQ should be removed from the exit examination [ 47 ]. Given that MEQ's are difficult to write to a high standard and in such a way that they test high-order cognitive skills, and given the time required and the subjectivity in marking, their use does not represent an efficient use of resources. Indeed, they state “… MEQ's often do little more than test the candidate's ability to recall a list of facts and frustrate the examiner with a large pile of papers to be hand-marked”. They conclude there is no good measurement reason for including open-ended items in the high-stakes assessment, given that the MEQ performed poorly in terms of testing high-order thinking in comparison with the multiple-choice despite considerable effort to produce quality questions.
Schuwirth and Van der Vleuten too have suggested that there is no justification for the use of SAQ in assessment, since the stimulus of most SAQ can also be applied with multiple-choice. They recommend that SAQ should not be used in any situation except where the spontaneous generation of the answer is absolutely essential. Furthermore, they believe that there is little place for context-free questions in medical assessment as the context-rich stimulus approximates clinical practice more closely [ 48 ].
Why does the open-ended format persist in medical assessment?
Hence the evidence suggests that in written summative assessment the multiple-choice format is no less able to test high-order thinking than open-ended questions, may have higher validity and is superior in reliability and cost-effectiveness. Remarkably this evidence extends as far back as 1926 [ 53 ],[ 93 ], and the reasons underlying the persistence of the open-ended format in assessment are of some interest. I suggest a number of factors. Studies bear out the common-sense expectation that questions designed to test factual knowledge only—irrespective of whether these are presented as open-ended or in multiple-choice format—do not test the same level of reasoning as more complex questions [ 94 ]. Indeed, a recurring finding in the literature is that the so-called deficiencies of the multiple-choice format lie more with the quality of the individual question item (and by inference, with the question-setter), than with the format per se . This leads to a self-fulfilling prophecy: examiners who do not appreciate the versatility of the multiple-choice format set questions which only test low-order thinking and not surprisingly achieve results which confirm their bias. Palmer et al. state that criticism of multiple-choice as being incapable of testing high-order thinking is in fact criticism of poorly written questions, and that the same criticism can be directed at open-ended assessments [ 45 ]. There is indeed evidence that stem-equivalent items tend to behave similarly, irrespective of whether the item is phrased as an open-ended question or in MCQ format. It is therefore essential that in making comparisons, the items compared are specifically crafted to assess the same order of cognition. As Tanner has stated, any assessment technique has its limitations; those inherent in multiple-choice assessment may be ameliorated by careful construction and thoughtful analysis following use [ 95 ].
Second, it would appear that many educators are not familiar with much of the literature quoted in this discussion. The most persuasive material is found in the broader educational literature, and though there are brief references in the medical education literature to some of the studies to which I have referred [ 47 ],[ 48 ], as well as a few original studies performed in the medical assessment context [ 17 ],[ 45 ],[ 47 ],[ 63 ], the issue does not appear to have enjoyed prominence in debate and has had limited impact on actual assessment practice. In their consensus statement and recommendations on research and assessment, Schuwirth et al. stress the need for reference beyond the existing medical education literature to relevant scientific disciplines, including cognitive psychology [ 27 ]. In the teaching context, it is remarkable how the proposition that the open-ended format is more appropriate in testing the knowledge and skills ultimately required for the workplace has been repeatedly and uncritically restated in the literature in the absence of compelling evidence to support it.
Third is the counter-intuitiveness of this finding. Indeed, the proposition that the open-ended format is more challenging than MCQ is intuitively appealing. Furthermore, there is the “generation effect”; experimental work has shown that spontaneous generation of information, as opposed to reading enhances recall [ 18 ],[ 19 ]. Although this applies to learning rather than to assessment, many teachers implicitly attribute a similar but reversed process to the act of recall, believing that spontaneous recall is more valid than cued recall. However, validity at face value is an unreliable proxy for true validity, and the outcome in practice may contradict what seems intuitively correct [ 48 ]. As the literature on learning increases, it has become apparent that evidenced-based practice frequently fails to coincide with the intuitive appeal of a particular learning methodology. Examples include the observation that interleaved practice is more effective than blocked practice and distributed practice is more effective than massed practice in promoting acquisition of skills and knowledge [ 21 ]. There is a need for assessment to be evidence-based; to an extent assessment would appear to lag behind learning and teaching methodology in this respect. Rohrer and Pashler have suggested that underutilisation of learning strategies shown to be more effective than their traditional counterparts, such as learning through testing, distributed practice and interleaved practice, remain so because of “the widespread (but erroneous) feeling that these strategies are less effective than their alternatives” [ 21 ].
Fourth and perhaps most defensible is concern that there is much that as yet remains unknown about the nature of assessment; particularly seen from the viewpoint of assessment for learning, and given very interesting new insights into the cognitive basis of memorisation, recall and reasoning, a field which is as yet largely unexplored, and may be expected to have a significant impact on the choice of assessment format. For diagnostic purposes, the open-ended format may hold value, since it is better able to expose the students intermediate thinking processes and therefore allow precise identification of learning difficulties [ 72 ]. Newer observations such as the generation effect [ 18 ],[ 19 ], the testing effect [ 20 ],[ 23 ], the preassessment effect, where the act of preparation for an assessment is itself a powerful driver of learning [ 96 ], and the post-assessment effect, such as the effect of feedback [ 96 ] are clearly important; were it to be shown that a particular format of assessment, such as the open-ended question, was superior in driving learning, then this would be important information which might well determine the choice of assessment. At this point however no such reliable information exists. Preliminary work suggests that MCQ items are as effective as open-ended items in promoting the testing effect [ 23 ]. None of these considerations are as yet sufficiently well supported by experimental evidence to argue definitively for the inclusion of open-ended questions on the basis of their effect on learning, though the possibility clearly remains. Furthermore, this debate has concentrated on high-stakes, summative exit assessments where the learning effects of assessment are presumably less important than they are at other stages of learning. Certainly, open-ended assessment remains appropriate for those domains not well-suited to multiple-choice assessment such as data gathering, clinical judgement and professional attitudes [ 92 ] and may have value for a particular question which cannot be presented in any other format [ 48 ]. Though the evidence is less compelling, open-ended items may be superior in distinguishing between performances of candidates occupying the two extremes of performance [ 75 ].
Cognitive basis for the observation
The need for assessment of research to move beyond empiric observations to studies based on a sound theoretical framework has recently been stressed [ 27 ],[ 96 ]. There is as yet little written on the reasons for the counter-intuitive finding that MCQ is as valid as open-ended assessments in predicting clinical performance. I suggest that the observation is highly compatible with cognitive-constructivist and situated learning theory, and in particular the theory of conceptual change [ 97 ]. Fundamental to this theory is the concept of mental models. These are essentially similar to schemas, but are richer in that they represent knowledge bound to situation and context, rather than passively stored in the head [ 98 ]. Mental models may therefore be thought of as cognitive artifacts constructed by an individual based on his or her preconceptions, cognitive skills, linguistic comprehension, and perception of the problem, which evolve as they are modified through experience and instruction [ 99 ]. Conceptual change is postulated to represent the mechanism underlying meaningful learning, and is a process of progressively constructing and organizing a learner’s personal mental models [ 100 ],[ 101 ]. It is suggested that an effective mental model will integrate six different aspects: knowledge appropriately structured for a particular domain (structural knowledge), pathways for solving problems related to the domain (procedural knowledge), mental images of the system, associations (metaphors), the ability to know when to activate mental models (executive knowledge), and assumptions about the problem (beliefs) [ 102 ]. Therefore increasing proficiency in any domain is associated not just with an enlarging of store of knowledge and experience, but also with increasing complexity in the extent to which knowledge is organised and the manner in which it is stored and accessed [ 103 ], particularly as complex mental models which may be applied to problem-solving [ 104 ]. A counterpart in the domain of medical expertise is the hierarchy of constructs proposed by Schmidt et al . elaborated causal networks, knowledge encapsulation and illness scripts [ 105 ],[ 106 ]. Conceptual change theory has a clear relationship to our current understanding of expertise, which is postulated to emerge where knowledge and concepts are linked as mental representations into propositional networks which allow rapid processing of information and the omission of intermediate steps in reasoning [ 107 ],[ 108 ]; typically the expert’s knowledge is grouped into discrete packets or chunks, and manipulation of these equates to the manipulation of a large amount of information simultaneously without conscious attention to any individual component [ 104 ]. In comparison with non-experts, the representations of experts are richer, more organised and abstract and are based on deep knowledge; experts also recognise the conditions under which use of particular knowledge is appropriate [ 109 ]. As Norman has stated, “expert problem-solving in medicine is dependent on (1) prior experiences which can be used in routine solution of problems by pattern recognition processes and (2) elaborated conceptual knowledge applicable to the occasional problematic situation ” [ 110 ]. The processes of building expertise and that of constructing mental models are essentially parallel [ 99 ].
Therefore any form of assessment intended to measure proficiency must successfully sample the candidate’s organisation of and access to knowledge, and not just content knowledge alone [ 99 ],[ 111 ]. I have reviewed the empirical evidence which suggests that the multiple-choice format is indeed predictive of proficiency, which provides important evidence that it is valid. This is explicable in terms of mental models. An alternative view of a mental model is as an internal representation of a system that the learner brings to bear in a problem-solving situation [ 103 ],[ 104 ],[ 112 ]. The context-rich written assessment [ 48 ] is essentially an exercise in complex problem-solving, and fits the definition of problem-solving as “cognitive processing aimed at accomplishing certain goals when the solution is unknown” [ 103 ],[ 113 ].
Zhang has introduced the concept of a “distributed cognitive task”: a task requiring that information distributed across both the internal mind and the external environment is processed [ 114 ]. If we extend Zhang’s concept of external representation to include a hypothetical patient, the subject of the clinical vignette, who represents the class of all such patients, then answering the context-rich multiple-choice item may be seen as a distributed cognitive task. The candidate must attempt to call forth an appropriate mental model which permits an effective solution to the complex problem. In a sequence of events which parallels that described by Zhang, the candidate must internalise the information provided in the vignette, form an accurate internal representation (an equivalent concept is that of the problem space, a mental representation of the problem requiring solution [ 115 ]); this in turn activates and interacts with the relevant mental models and is followed by externalization: the return of the product of the interaction of internal representation and mental model to the external environment, and the selection of a solution. In effect a relationship has been defined between environmental information, activation of higher level cognition and externalisation of internal representations [ 114 ].
Assessment items which require complex problem-solving call on mental models appropriate to that particular context, and the item can only be answered confidently and correctly if the mental model is present at the level of proficiency. There is therefore no such thing as the student with generic expertise “in answering multiple-choice questions”, which explains the findings of Hakstian [ 80 ], Bridgeman and Morgan [ 78 ], Ercikan et al. [ 75 ] and Bleske-Rechek et al . [ 79 ], none of whom found convincing evidence for the existence of a class of student with a particular skill in answering multiple-choice questions.
Recent observations that retrieval of knowledge improves retention, and may be enhanced in the learning process by frequent testing [ 20 ],[ 21 ], and in particular a recent publication summarising four studies performed in an authentic learning environment which demonstrates that that testing using MCQ format is as effective as SAQ testing [ 23 ], supports the hypothesis that the MCQ format engages with high order cognitive processes, in both learning and retrieval of memory. This is further supported by their finding that high-level test questions stimulate deeper conceptual learning and better learning retention then do low-level test questions [ 23 ].
In summary, the multiple-choice item is testing the integrity and appropriateness of the candidate’s mental models, and in doing so, is in fact assessing proficiency. If the item is designed to test factual recall only then it will fail for this purpose, since it is the solution of a complex problem which tests the strength of the mental model and the cognitive processes which interact with it. Yet even a low-quality assessment based on factual recollection will correlate significantly with proficiency. Firstly, all mental models are based on a foundation of structural knowledge. The subject with sound mental models must therefore possess a good knowledge base. Secondly, possessing effective and appropriate mental models facilitates the retention and recall of knowledge [ 103 ]. Not surprisingly therefore, even on a fact-based assessment, good students will correctly recall the information and excel; students with deficient mental models, are less likely to be able to recall the information when needed. This is supported by the work of Jensen et al . [ 116 ] who found that high order questions stimulated deep conceptual understanding and retention, and correlated with higher performance on both subsequent high order assessment items and low-order assessment items. Indeed, recognition and recall are highly correlated [ 50 ]. There is evidence that the cognitive processes evoked by the multiple-choice format are not influenced by cueing [ 117 ], though the reasons for the frequent observation that MCQ scores are higher than those for equivalent open-ended item assessments raise concern that cueing may yet have a role [ 118 ]. However, where the stem and options have been well-designed―particularly such that the distractors all appear attractive to the candidate without the requisite knowledge― cueing should not be an issue [ 29 ],[ 48 ], and the common argument that it is easier to recognize an answer than it is to generate it spontaneously would appear not to hold true.
Problem-solving skills are poorly generalizable [ 41 ]. This is explicable in that mental models are essentially domain-specific, representing a particular set of knowledge and circumstances, but the actual process of developing them is highly dependent on domain-general processes including metacognition, self-regulation and cognitive flexibility [ 99 ].
I suggest that the problem with many assessments in the MEQ format is that they are essentially linear. By requiring the candidate to think one step at a time, the assessment effectively misses the crux of the problem-solving process, which is to look at and respond to a complex problem in its entirety, and not stepwise. The context-rich vignette-based multiple-choice item by contrast presents a complex problem which must be holistically assessed. Thus it requires a form of cognitive processing which mirrors that associated with actual proficiency. Hybrid formats such as key feature assessments in effect also break down the clinical reasoning process into a sequence of sequential steps; whether this is regarded as a drawback will depend on the relative importance ascribed to decision-making at critical points in the decision tree and global assessment of a problem viewed holistically. This is a critical area for future research in clinical reasoning.
Educators who mistrust the multiple-choice format have tended to concentrate on the final, and cognitively the least important, step in this whole process: the selection of a particular option as the answer, while ignoring the complex cognitive processes which precede the selection. Indeed, in a good assessment, the candidate is not “selecting” an answer at all. They recognise the external representation of a problem, subject the internalised representation to high level cognitive processing, and then externalise the product as a solution [ 119 ], which (almost as if coincidentally) should coincide with one of the options given.
The multiple-choice format is by no means unlimited in its capacity to test higher-order thinking. The literature on problem-solving stresses the importance of highly-structured complex problems, characterised by unknown elements with no clear path to the solution and indeed a potential for there to be many solutions or even no solution at all [ 99 ]. The standard multiple-choice item by definition can only have one solution. Thus, though it may be context-rich, it is limited in its complexity. It is difficult however to imagine how a practically achievable open-ended written assessment might perform better. In order to accommodate complexity, the question would essentially have to be unstructured—thereby eliminating all the structured short-answer progeny of the essay format, such as MEQ. In order to permit the candidate to freely demonstrate the application of all his or her mental resources to a problem more complex than that permitted by a multiple-choice vignette, one would in all probability require that the candidate is afforded the opportunity to develop an extensive, unstructured and essentially free-ranging, essay-length response; marking will be inherently subjective and we are again faced with the problem of narrow sampling, subjectivity and low reliability.
In effect the choice would then lie between an assessment comprising one or two unstructured essay length answers with low objectivity and reliability, and a large number of highly reliable multiple choice items which will effectively test high-order problem-solving, but will stop short of a fully complex situation. Perhaps this is a restatement of the assertion that “measuring something that is not quite right accurately may yield far better measurement than measuring the right thing poorly” [ 50 ], the situation depicted in Figure 3 .
Another way of understanding the validity of the multiple-choice format is by comparing the responses of candidates at different phases of the learning process with the stages of increasing proficiency posited by Dreyfus et al . [ 16 ] (Table 1 ). Here the first column comprises the stages of learning; in this context, we shall regard stage of learning as synonymous with level of proficiency or expertise, which is a measure of the effectiveness of problem-solving skill. The second column contains descriptors for each stage chosen for their relevance to complex problem-solving posed by a well-constructed context-rich multiple-choice item. The third column contains a description of the likely performance on that item of a candidate at that stage of proficiency. The relationship between proficiency and performance in a complex multiple-choice item is in fact remarkably direct. The candidate who has reached the stage of proficiency or expertise will be more likely to select the correct response than candidates at a lower level, and the more widely such proficiency is spread across the domain, the higher the aggregate score in the assessment. Though the score for a standard multiple-choice item is binary (all or nothing), the assessment as a whole is not. Whereas candidates in the top categories are likely to arrive at a correct solution most of the time, and students in the lowest category hardly ever, the middle order candidates with less secure mental models will answer with less confidence, but will in a number of items proportional to their proficiency, come up with the correct solution, their mental models proving to be sufficiently adequate for the purpose. Over a large number of items such a multiple-choice assessment will therefore provide a highly accurate indication of the level of proficiency of the candidate. To avoid all confounding variables however it is absolutely essential that the options are set such that cueing is eliminated.
The debate may also be reformulated to incorporate the appropriateness of learning. Deep learning is characterised by an understanding of the meaning underlying knowledge, reflection on the interrelationships of items of information, understanding of the application of knowledge to everyday experience, integration of information with prior learning, the ability to differentiate between principle and example and the organisation of knowledge into a coherent, synthetic structure [ 99 ],[ 100 ]—essentially an alternative formulation of the mental model. One can thus argue that the candidate who possesses deep knowledge has, by the very fact of that possession, demonstrated that they have the sort of comprehensive and intuitive understanding of the subject—in short, the appropriate mental models as described by Jonassen and Strobel [ 97 ],[ 101 ]—to allow the information to be used for problem-solving. Correspondingly, the weak student lacks deep knowledge, and this will be exposed by a well-constructed multiple-choice assessment, provided that the items are written in a manner which explores the higher cognitive levels of learning.
Therefore, if candidates demonstrate evidence of extensive, deeply-learned knowledge, and the ability to solve complex problems, be it through the medium of multiple-choice assessment or any other form of assessment, then it is safe to assume that they will be able to apply this knowledge in practice. This accounts for the extensive correlation noted between multiple-choice performance, performance in open-ended assessments, and tests of subsequent performance in an authentic environment.
The argument that open-ended questions do not test higher order cognitive skills, and consequently lack validity, is not supported by the evidence. Some studies may have been confounded by the unfair comparison of high-order items in one format with low-order items in another. This cannot be discounted as partly responsible for the discrepancies noted in some of the work I have referenced, such as that of Hee-Sun et al . [ 73 ], yet where the cognitive order of the items have been carefully matched, a number of careful studies suggest that, particularly in science and medicine, the two modalities assess constructs which though probably not identical, overlap to the extent that using both forms of assessment is redundant. Given the advantage of the multiple-choice format in reliability, efficiency and cost-effectiveness, the suggestion that open-ended items may be replaced entirely with multiple-choice items in summative assessment is one which deserves careful consideration. This counter-intuitive finding highlights our lack of understanding of the cognitive processes underlying both clinical competence and its assessment, and suggests that much further work remains to be done. Despite the MCQ format’s long pedigree, it is clear that we understand little about the cognitive architecture invoked by this form of assessment. The need for a greater role for theoretical models in assessment research has been stressed [ 27 ],[ 96 ]. As illustrated in this debate, medical teaching and assessment must be based on a solid theoretical framework, underpinned by reliable evidence. Hard evidence combined with a plausible theoretical model - which must attempt to explain the observations on the basis of cognition - will provide the strongest basis for the identification of effective learning and assessment methodologies.
That the multiple-choice format demonstrates high validity is due in part to the observation that well-constructed, context-rich multiple-choice questions are fully capable of assessing higher orders of cognition, and that they call forth cognitive problem-solving processes which exactly mirror those required in practice. On a theoretical basis it is even conceivable that the multiple-choice format will show superior performance in assessing proficiency in contrast with some versions of the open-ended format; there is indeed empirical evidence to support this in practice [ 56 ],[ 92 ]. Paradoxically, the open-ended format may demonstrate lower validity than well-written multiple-choice items; since attempts to improve reliability and reduce objectivity by writing highly focused questions marked against standardised, prescriptive marking templates frequently “trivialize” the question, resulting in some increase in reproducibility at the expense of a significant loss of validity [ 120 ]. Indeed, I have argued that, based on an understanding of human cognition and problem-solving proficiency, context-rich multiple-choice assessments may be superior in assessing the very characteristics which the proponents of the open-ended format claim as a strength of that format.
Though current evidence supports the notion that in summative assessment open-ended items may well be redundant, this conclusion should not be uncritically extrapolated to situations where assessment for learning is important, such as in formative assessment and in summative assessment at early and intermediate stages of the medical programme given that conclusive evidence with respect to the learning effects of the two formats is as yet awaited.
Author’s contribution
The author was solely responsible the literature and writing the article.
Author’s information
RJH is currently Dean and Head of the School of Clinical Medicine at the University of KwaZulu-Natal, Durban, South Africa. He studied at the University of Cape Town, specialising in Internal Medicine and subsequently hepatology, before moving to Durban as Professor of Medicine. He has a longstanding interest in medical education, and specifically in the cognitive aspects of clinical reasoning, an area in which he is currently supervising a number of research initiatives.
Abbreviations
Modified essay question
Multiple-choice question
Short answer question
Objective structured clinical examination
Siemens G: Connectivism: Learning as Network-Creation. [ http://www.elearnspace.org/Articles/networks.htm ]
Siemens G: Connectivism: A learning theory for the digital age. Int J Instr Technol Distance Learn. 2005, 2: 3-10.
Google Scholar
Perkins DN, Salomon G: Learning transfer. International Encyclopaedia of adult education and training. Edited by: Tuijnman AC. 1996, Pergamon Press, Tarrytown, NY, 422-427. 2
Haskell EH: Transfer of learning: Cognition, Instruction, and Reasoning. 2001, Academic Press, New York
Spelke E: Initial Knowledge: Six Suggestions. Cognition on cognition. Edited by: Mehler J, Franck S. 1995, The MIT Press, Cambridge, MA US, 433-447.
Barnett SM, Ceci SJ: When and where do we apply what we learn? A taxonomy for far transfer. Psychol Bull. 2002, 128: 612-637.
Brown AL: Analogical Learning and Transfer: What Develops?. Similarity and Analogical Reasoning. Edited by: Vosniadou S, Ortony A. 1989, Cambridge University Press, New York, 369-412.
Gick ML, Holyoak KJ: Schema Induction and Analogical Transfer. 2004, Psychology Press, New York, NY US
Bloom BS: The Cognitive Domain. Taxonomy of Educational Objectives, Handbook I. 1956, David McKay Co Inc, New York
Anderson LW, Krathwohl DR, Airasian PW, Cruikshank KA, Mayer RE, Pintrich PR, Raths J, Wittrock MC: A Taxonomy for Learning, Teaching, and Assessing: a revision of Bloom's Taxonomy of Educational Objectives. 2001, Longman, New York
Anderson LW, Sosniak LA: Bloom's Taxonomy: A Forty-year Retrospective. Ninety-third yearbook of the National Society for the Study of Education: Part II. Edited by: Anderson LW, Sosniak LA. 1994, University of Chicago Press, Chicago IL
Conklin J: A taxonomy for learning, teaching, and assessing: a revision of Bloom's taxonomy of educational objectives. Educ Horiz. 2005, 83: 154-159.
Haladyna TM, Downing SM: A taxonomy of multiple-choice item-writing rules. Appl Meas Educ. 1989, 2: 37-51.
Haladyna TM: Developing and Validating Multiple-choice Test Items . Mahwah NJ: L. Erlbaum Associates; 1999.
Miller GE: The assessment of clinical skills/competence/performance. Acad Med. 1990, 65: S63-S67.
Dreyfus HL, Dreyfus SE, Athanasiou T: Mind over Machine: The Power of Human Intuition and Expertise in the Era of the Computer. 1986, Free Press, New York
Norcini JJ, Swanson DB, Grosso LJ, Webster GD: Reliability, validity and efficiency of multiple choice question and patient management problem item formats in assessment of clinical competence. Med Educ. 1985, 19: 238-247.
Taconnat L, Froger C, Sacher M, Isingrini M: Generation and associative encoding in young and old adults: The effect of the strength of association between cues and targets on a cued recall task. Exp Psychol. 2008, 55: 23-30.
Baddeley AD, Eysenck MW, Anderson M: Memory. 2010, Psychology Press, New York
Karpicke J, Grimaldi P: Retrieval-based learning: a perspective for enhancing meaningful learning. Educ Psychol Rev. 2012, 24: 401-418.
Rohrer D, Pashler H: Recent research on human learning challenges conventional instructional strategies. Educ Res. 2010, 39: 406-412.
Smith MA, Roediger HL, Karpicke JD: Covert retrieval practice benefits retention as much as overt retrieval practice. J Exp Psychol Learn Mem Cogn. 2013, 39: 1712-1725.
McDermott KB, Agarwal PK, D’Antonio L, Roediger HL, McDaniel MA: Both multiple-choice and short-answer quizzes enhance later exam performance in middle and high school classes. J Exp Psychol Appl. 2014, 20: 3-21.
Cutting MF, Saks NS: Twelve tips for utilizing principles of learning to support medical education. Med Teach. 2012, 34: 20-24.
Schuwirth LWT, Van der Vleuten CPM: General overview of the theories used in assessment: AMEE Guide No. 57. Med Teach. 2011, 33: 783-797.
Van der Vleuten CP, Schuwirth LW: Assessing professional competence: from methods to programmes. Med Educ. 2005, 39: 309-317.
Schuwirth L, Colliver J, Gruppen L, Kreiter C, Mennin S, Onishi H, Pangaro L, Ringsted C, Swanson D, Van der Vleuten C, Wagner-Menghin M: Research in assessment: Consensus statement and recommendations from the Ottawa 2010 Conference. Med Teach. 2011, 33: 224-233.
Schuwirth LWT, Van der Vleuten CPM: Programmatic assessment and Kane's validity perspective. Med Educ. 2012, 46: 38-48.
Case SM, Swanson DB: Constructing Written Test Questions for the Basic and Clinical Sciences. 2002, National Board of Medical Examiners, Philadelphia, 3
Norcini J, Anderson B, Bollela V, Burch V, Costa MJ, Duvivier R, Galbraith R, Hays R, Kent A, Perrott V, Roberts T: Criteria for good assessment: Consensus statement and recommendations from the Ottawa 2010 Conference. Med Teach. 2011, 33: 206-214.
Shepard LA: The role of assessment in a learning culture. Educ Res. 2000, 29: 4-14.
Coburn CA, Yerkes RM: A study of the behavior of the crow corvus americanus Aud. By the multiple choice method. J Anim Behav. 1915, 5: 75-114.
Yerkes RM, Coburn CA: A study of the behavior of the pig Sus Scrofa by the multiple choice method. J Anim Behav. 1915, 5: 185-225.
Brown W, Whittell F: Yerkes' multiple choice method with human adults. J Comp Psychol. 1923, 3: 305-318.
Yerkes RM: A New method of studying the ideational behavior of mentally defective and deranged as compared with normal individuals. J Comp Psychol. 1921, 1: 369-394.
Davidson C: Davidson CN: Now You See It: How the Brain Science of Attention Will Transform the Way We Live, Work, and Learn. 2011, Viking Press, New York
Frederiksen JR, Collins A: A Systems Approach to Educational Testing. Technical Report No. 2. 1990, Center for Technology in Education, New York
Guthrie JT: Testing higher level skills. J Read. 1984, 28: 188-190.
Nickerson RS: New directions in educational assessment. Educ Res. 1989, 18: 3-7.
Stratford P, Pierce-Fenn H: Modified essay question. Phys Ther. 1985, 65: 1075-1079.
Wass V, Van der Vleuten C, Shatzer J, Jones R: Assessment of clinical competence. Lancet. 2001, 357: 945.
Rotfield H: Are we teachers or job trainers?. Acad Mark Sci Q. 1998, 2: 2.
Crocker L, Algina J: Introduction to Classical & Modern Test Theory. 1986, Holt, Rinehart and Winston, Inc., Fort Worth, TX
Angoff W: Test reliability and effective test length. Psychometrika. 1953, 18: 1-14.
Palmer EJ, Devitt PG: Assessment of higher order cognitive skills in undergraduate education: modified essay or multiple choice questions? Research paper. BMC Med Educ. 2007, 7: 49-49.
Feletti GI, Smith EK: Modified essay questions: Are they worth the effort?. Med Educ. 1986, 20: 126-132.
Palmer EJ, Duggan P, Devitt PG, Russell R: The modified essay question: its exit from the exit examination?. Med Teach. 2010, 32: e300-e307.
Schuwirth LW, Van der Vleuten CPM: Different written assessment methods: what can be said about their strengths and weaknesses?. Med Educ. 2004, 38: 974-979.
Lukhele R, Thissen D, Wainer H: On the relative value of multiple-choice, constructed response, and examinee-selected items on two achievement tests. J Educ Meas. 1994, 31: 234-250.
Wainer H, Thissen D: Combining multiple-choice and constructed-response test scores: toward a Marxist theory of test construction. Appl Meas Educ. 1993, 6: 103-118.
Facione PA: The California Critical Thinking Skills Test--College Level. Technical Report #1. Experimental Validation and Content Validity. 1990, California Academic Press, Millbrae CA
Facione PA, Facione NC, Blohm SW, Giancarlo CAF: The California Critical Thinking Skills Test [Revised]. In Millbrae CA: California Academic Press; 2007.
Rodriguez MC: Construct equivalence of multiple-choice and constructed-response items: A random effects synthesis of correlations. J Educ Meas. 2003, 40: 163-184.
Falk B, Ancess J, Darling-Hammond L: Authentic Assessment in Action: Studies of Schools and Students at Work. 1995, Teachers College Press, United States of America
Rethans JJ, Norcini JJ, Baron-Maldonado M, Blackmore D, Jolly BC, LaDuca T, Lew S, Page GG, Southgate LH: The relationship between competence and performance: implications for assessing practice performance. Med Educ. 2002, 36: 901-909.
Wilkinson TJ, Frampton CM: Comprehensive undergraduate medical assessments improve prediction of clinical performance. Med Educ. 2004, 38: 1111-1116.
Baker EL: Standards for Educational and Psychological Testing. Sage Publications, Inc; 2012.
Eignor DR: The Standards for Educational and Psychological Testing. APA Handbook of Testing and Assessment in Psychology, Vol 1: Test Theory and Testing and Assessment in Industrial and Organizational Psychology. Edited by: Geisinger KF, Bracken BA, Carlson JF, Hansen J-IC, Kuncel NR, Reise SP, Rodriguez MC. 2013, American Psychological Association, Washington, DC, US, 245-250.
Eignor DR: Standards for the development and use of tests: The Standards for Educational and Psychological Testing. Eur J Psychol Assess. 2001, 17: 157-163.
Downing SM: Validity: on the meaningful interpretation of assessment data. Med Educ. 2003, 37: 830.
Messick S: The interplay of evidence and consequences in the validation of performance assessments. Educ Res. 1994, 23: 13-23.
Kuechler WL, Simkin MG: Why is performance on multiple-choice tests and constructed-response tests Not more closely related? theory and an empirical test. Decis Sci J Innov Educ. 2010, 8: 55-73.
Norman GR, Smith EK, Powles AC, Rooney PJ: Factors underlying performance on written tests of knowledge. Med Educ. 1987, 21: 297-304.
Bacon DR: Assessing learning outcomes: a comparison of multiple-choice and short-answer questions in a marketing context. J Mark Educ. 2003, 25: 31-36.
Kastner M, Stangla B: Multiple choice and constructed response tests: Do test format and scoring matter?. Procedia - Social and Behav Sci. 2011, 12: 263-273.
Nichols P, Sugrue B: The lack of fidelity between cognitively complex constructs and conventional test development practice. Educ Measurement: Issues Pract. 1999, 18: 18-29.
Bennett RE, Rock DA, Wang M: Equivalence of free-response and multiple-choice items. J Educ Meas. 1991, 28: 77-92.
Bridgeman B, Rock DA: Relationships among multiple-choice and open-ended analytical questions. J Educ Meas. 1993, 30: 313-329.
Thissen D, Wainer H: Are tests comprising both multiple-choice and free-response items necessarily less unidimensional. J Educ Meas. 1994, 31: 113.
Lissitz RW, Xiaodong H, Slater SC: The contribution of constructed response items to large scale assessment: measuring and understanding their impact. J Appl Testing Technol. 2012, 13: 1-52.
Traub RE, Fisher CW: On the equivalence of constructed- response and multiple-choice tests. Appl Psychol Meas. 1977, 1: 355-369.
Martinez ME: Cognition and the question of test item format. Educ Psychol. 1999, 34: 207-218.
Hee-Sun L, Liu OL, Linn MC: Validating measurement of knowledge integration in science using multiple-choice and explanation items. Appl Meas Educ. 2011, 24: 115-136.
Wilson M, Wang W-C: Complex composites: Issues that arise in combining different modes of assessment. Appl Psychol Meas. 1995, 19: 51-71.
Ercikan K, Schwartz RD, Julian MW, Burket GR, Weber MM, Link V: Calibration and scoring of tests with multiple-choice and constructed-response item types. J Educ Meas. 1998, 35: 137-154.
Epstein ML, Lazarus AD, Calvano TB, Matthews KA, Hendel RA, Epstein BB, Brosvic GM: Immediate feedback assessment technique promotes learning and corrects inaccurate first responses. Psychological Record. 2002, 52: 187-201.
Schuwirth LWT, Van der Vleuten CPM: Programmatic assessment: From assessment of learning to assessment for learning. Med Teach. 2011, 33: 478-485.
Bridgeman B, Morgan R: Success in college for students with discrepancies between performance on multiple-choice and essay tests. J Educ Psychol. 1996, 88: 333-340.
Bleske-Rechek A, Zeug N, Webb RM: Discrepant performance on multiple-choice and short answer assessments and the relation of performance to general scholastic aptitude. Assessment Eval Higher Educ. 2007, 32: 89-105.
Hakstian AR: The Effects of Type of Examination Anticipated on Test Preparation and Performance. J Educ Res. 1971, 64: 319.
Scouller K: The influence of assessment method on Students' learning approaches: multiple choice question examination versus assignment essay. High Educ. 1998, 35: 453-472.
Thomas PR, Bain JD: Contextual dependence of learning approaches: The effects of assessments. Human Learning: J Pract Res Appl. 1984, 3: 227-240.
Watkins D: Factors influencing the study methods of Australian tertiary students. High Educ. 1982, 11: 369-380.
Minbashian A, Huon GF, Bird KD: Approaches to studying and academic performance in short-essay exams. High Educ. 2004, 47: 161-176.
Yonker JE: The relationship of deep and surface study approaches on factual and applied test-bank multiple-choice question performance. Assess Eval Higher Educ. 2011, 36: 673-686.
Joughin G: The hidden curriculum revisited: a critical review of research into the influence of summative assessment on learning. Assess Eval Higher Educ. 2010, 35: 335-345.
Scouller KM, Prosser M: Students' experiences in studying for multiple choice question examinations. Stud High Educ. 1994, 19: 267.
Hadwin AF, Winne PH, Stockley DB, Nesbit JC, Woszczyna C: Context moderates students' self-reports about how they study. J Educ Psychol. 2001, 93: 477-487.
Birenbaum M: Assessment and instruction preferences and their relationship with test anxiety and learning strategies. High Educ. 2007, 53: 749-768.
Birenbaum M: Assessment preferences and their relationship to learning strategies and orientations. High Educ. 1997, 33: 71-84.
Smith SN, Miller RJ: Learning approaches: examination type, discipline of study, and gender. Educ Psychol. 2005, 25: 43-53.
Rabinowitz HK, Hojat M: A comparison of the modified essay question and multiple choice question formats: their relationship to clinical performance. Fam Med. 1989, 21: 364-367.
Paterson DG: Do new and old type examinations measure different mental functions?. School Soc. 1926, 24: 246-248.
Schuwirth LW, Verheggen MM, Van der Vleuten CPM, Boshuizen HP, Dinant GJ: Do short cases elicit different thinking processes than factual knowledge questions do?. Med Educ. 2001, 35: 348-356.
Tanner DE: Multiple-choice items: Pariah, panacea or neither of the above?. Am Second Educ. 2003, 31: 27.
Cilliers FJ, Schuwirth LW, van der Vleuten CP: Modelling the pre-assessment learning effects of assessment: evidence in the validity chain. Med Educ. 2012, 46: 1087-1098.
Jonassen DH, Strobel J: Modeling for Meaningful Learning. Engaged Learning with Emerging Technologies. Edited by: Hung D. 2006, Springer, Amsterdam, 1-27.
Derry SJ: Cognitive schema theory in the constructivist debate. Educ Psychol. 1996, 31: 163-174.
Kim MK: Theoretically grounded guidelines for assessing learning progress: cognitive changes in Ill-structured complex problem-solving contexts. Educ Technol Res Dev. 2012, 60: 601-622.
Mayer RE: Models for Understanding. Rev Educ Res. 1989, 59: 43-64.
Jonassen D, Strobel J, Gottdenker J: Model building for conceptual change. Interact Learn Environ. 2005, 13: 15-37.
Jonassen DH: Tools for representing problems and the knowledge required to solve them. Edited by Tergan S-O, Keller T. Berlin, Heidelberg: Springer; 2005:82–94.
Bogard T, Liu M, Chiang Y-H: Thresholds of knowledge development in complex problem solving: a multiple-case study of advanced Learners' cognitive processes. Educ Technol Res Dev. 2013, 61: 465-503.
Van Gog T, Ericsson KA, Rikers RMJP: Instructional design for advanced learners: establishing connections between the theoretical frameworks of cognitive load and deliberate practice. Educ Technol Res Dev. 2005, 53: 73-81.
Schmidt HG, Norman GR, Boshuizen HP: A cognitive perspective on medical expertise: theory and implication. Acad Med. 1990, 65: 611-621.
Schmidt HG, Rikers RMJP: How expertise develops in medicine: knowledge encapsulation and illness script formation. Med Educ. 2007, 41: 1133-1139.
Norman G, Young M, Brooks L: Non-analytical models of clinical reasoning: the role of experience. Med Educ. 2007, 41: 1140-1145.
Ericsson KA, Prietula MJ, Cokely ET: The Making of an Expert. Harv Bus Rev. 2007, 85: 114-121.
Hoffman RR: How Can Expertise be Defined? Implications of Research From Cognitive Psychology. Exploring Expertise. Edited by: Williams R, Faulkner W, Fleck J. 1996, University of Edinburgh Press, Edinburgh, 81-100.
Norman GR: Problem-solving skills, solving problems and problem-based learning. Med Educ. 1988, 22: 279-286.
Ifenthaler D, Seel NM: Model-based reasoning. Comput Educ. 2013, 64: 131-142.
Jonassen D: Using cognitive tools to represent problems. J Res Technol Educ. 2003, 35: 362-381.
Mayer RE, Wittrock MC: Problem-Solving Transfer. Handbook of Educational Psychology. Edited by: Berliner DC, Calfee RC. 1996, Macmillan Library Reference USA, New York, NY, 47-62.
Zhang J, Norman DA: Representations in distributed cognitive tasks. Cogn Sci. 1994, 18: 87-122.
Simon HA: Information-Processing Theory of Human Problem Solving. Handbook of Learning & Cognitive Processes: V Human Information. Edited by: Estes WK. 1978, Lawrence Erlbaum, Oxford England, 271-295.
Jensen JL, Woodard SM, Kummer TA, McDaniel MA: Teaching to the test…or testing to teach: exams requiring higher order thinking skills encourage greater conceptual understanding. Educ Psychol Rev. 2014, 26: 307-329.
Cohen-Schotanus J, Van der Vleuten CPM: A standard setting method with the best performing students as point of reference: practical and affordable. Med Teach. 2010, 32: 154-160.
Desjardins I, Touchie C, Pugh D, Wood TJ, Humphrey-Murto S: The impact of cueing on written examinations of clinical decision making: a case study. Med Educ. 2014, 48: 255-261.
Pretz JE, Naples AJ, Sternberg RJ: Recognizing, Defining, and Representing Problems. The Psychology of Problem Solving. Edited by: Davidson JE, Sternberg RJ. 2003, Cambridge University Press, New York, NY US, 3-30.
Schuwirth LWT, Schuwirth LWT, Van der Vleuten CPM: ABC of learning and teaching in medicine: written assessment. BMJ: British Med J (International Edition). 2003, 326: 643-645.
Download references
Acknowledgements
The author would like to thank Dr Veena Singaram for her insightful and challenging appraisal of the manuscript.
Author information
Authors and affiliations.
Clinical and Professional Practice Research Group, School of Clinical Medicine, University of KwaZulu-Natal, Durban, 4013, South Africa
Richard J Hift
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Richard J Hift .
Additional information
Competing interests.
The author declares that he has no competing interests.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Authors’ original file for figure 2, authors’ original file for figure 3, rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/4.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Hift, R.J. Should essays and other “open-ended”-type questions retain a place in written summative assessment in clinical medicine?. BMC Med Educ 14 , 249 (2014). https://doi.org/10.1186/s12909-014-0249-2
Download citation
Received : 08 May 2014
Accepted : 07 November 2014
Published : 28 November 2014
DOI : https://doi.org/10.1186/s12909-014-0249-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Conceptual change
- Mental models
- Multiple choice
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
10 Successful Medical School Essays
Sponsored by.

-- Accepted to: Harvard Medical School GPA: 4.0 MCAT: 522
Sponsored by A ccepted.com : Great stats don’t assure acceptance to elite medical schools. The personal statement, most meaningful activities, activity descriptions, secondaries and interviews can determine acceptance or rejection. Since 1994, Accepted.com has guided medical applicants just like you to present compelling medical school applications. Get Accepted !
I started writing in 8th grade when a friend showed me her poetry about self-discovery and finding a voice. I was captivated by the way she used language to bring her experiences to life. We began writing together in our free time, trying to better understand ourselves by putting a pen to paper and attempting to paint a picture with words. I felt my style shift over time as I grappled with challenges that seemed to defy language. My poems became unstructured narratives, where I would use stories of events happening around me to convey my thoughts and emotions. In one of my earliest pieces, I wrote about a local boy’s suicide to try to better understand my visceral response. I discussed my frustration with the teenage social hierarchy, reflecting upon my social interactions while exploring the harms of peer pressure.
In college, as I continued to experiment with this narrative form, I discovered medical narratives. I have read everything from Manheimer’s Bellevue to Gawande’s Checklist and from Nuland’s observations about the way we die, to Kalanithi’s struggle with his own decline. I even experimented with this approach recently, writing a piece about my grandfather’s emphysema. Writing allowed me to move beyond the content of our relationship and attempt to investigate the ways time and youth distort our memories of the ones we love. I have augmented these narrative excursions with a clinical bioethics internship. In working with an interdisciplinary team of ethics consultants, I have learned by doing by participating in care team meetings, synthesizing discussions and paths forward in patient charts, and contributing to an ongoing legislative debate addressing the challenges of end of life care. I have also seen the ways ineffective intra-team communication and inter-personal conflicts of beliefs can compromise patient care.
Writing allowed me to move beyond the content of our relationship and attempt to investigate the ways time and youth distort our memories of the ones we love.
By assessing these difficult situations from all relevant perspectives and working to integrate the knowledge I’ve gained from exploring narratives, I have begun to reflect upon the impact the humanities can have on medical care. In a world that has become increasingly data driven, where patients can so easily devolve into lists of numbers and be forced into algorithmic boxes in search of an exact diagnosis, my synergistic narrative and bioethical backgrounds have taught me the importance of considering the many dimensions of the human condition. I am driven to become a physician who deeply considers a patient’s goal of care and goals of life. I want to learn to build and lead patient care teams that are oriented toward fulfilling these goals, creating an environment where family and clinician conflict can be addressed efficiently and respectfully. Above all, I look forward to using these approaches to keep the person beneath my patients in focus at each stage of my medical training, as I begin the task of translating complex basic science into excellent clinical care.
In her essay for medical school, Morgan pitches herself as a future physician with an interdisciplinary approach, given her appreciation of how the humanities can enable her to better understand her patients. Her narrative takes the form of an origin story, showing how a childhood interest in poetry grew into a larger mindset to keep a patient’s humanity at the center of her approach to clinical care.
This narrative distinguishes Morgan as a candidate for medical school effectively, as she provides specific examples of how her passions intersect with medicine. She first discusses how she used poetry to process her emotional response to a local boy’s suicide and ties in concern about teenage mental health. Then, she discusses more philosophical questions she encountered through reading medical narratives, which demonstrates her direct interest in applying writing and the humanities to medicine. By making the connection from this larger theme to her own reflections on her grandfather, Morgan provides a personal insight that will give an admissions officer a window into her character. This demonstrates her empathy for her future patients and commitment to their care.
Her narrative takes the form of an origin story, showing how a childhood interest in poetry grew into a larger mindset to keep a patient's humanity at the center of her approach to clinical care.
Furthermore, it is important to note that Morgan’s essay does not repeat anything in-depth that would otherwise be on her resume. She makes a reference to her work in care team meetings through a clinical bioethics internship, but does not focus on this because there are other places on her application where this internship can be discussed. Instead, she offers a more reflection-based perspective on the internship that goes more in-depth than a resume or CV could. This enables her to explain the reasons for interdisciplinary approach to medicine with tangible examples that range from personal to professional experiences — an approach that presents her as a well-rounded candidate for medical school.
Disclaimer: With exception of the removal of identifying details, essays are reproduced as originally submitted in applications; any errors in submissions are maintained to preserve the integrity of the piece. The Crimson's news and opinion teams—including writers, editors, photographers, and designers—were not involved in the production of this article.
-- Accepted To: A medical school in New Jersey with a 3% acceptance rate. GPA: 3.80 MCAT: 502 and 504
Sponsored by E fiie Consulting Group : “ EFIIE ” boasts 100% match rate for all premedical and predental registered students. Not all students are accepted unto their pre-health student roster. Considered the most elite in the industry and assists from start to end – premed to residency. EFIIE is a one-stop-full-service education firm.
"To know even one life has breathed easier because you have lived. This is to have succeeded." – Ralph Waldo Emerson.
The tribulations I've overcome in my life have manifested in the compassion, curiosity, and courage that is embedded in my personality. Even a horrific mishap in my life has not changed my core beliefs and has only added fuel to my intense desire to become a doctor. My extensive service at an animal hospital, a harrowing personal experience, and volunteering as an EMT have increased my appreciation and admiration for the medical field.
At thirteen, I accompanied my father to the Park Home Animal Hospital with our eleven-year-old dog, Brendan. He was experiencing severe pain due to an osteosarcoma, which ultimately led to the difficult decision to put him to sleep. That experience brought to light many questions regarding the idea of what constitutes a "quality of life" for an animal and what importance "dignity" plays to an animal and how that differs from owner to owner and pet to pet. Noting my curiosity and my relative maturity in the matter, the owner of the animal hospital invited me to shadow the professional staff. Ten years later, I am still part of the team, having made the transition from volunteer to veterinarian technician. Saving a life, relieving pain, sharing in the euphoria of animal and owner reuniting after a procedure, to understanding the emotions of losing a loved one – my life was forever altered from the moment I stepped into that animal hospital.
As my appreciation for medical professionals continued to grow, a horrible accident created an indelible moment in my life. It was a warm summer day as I jumped onto a small boat captained by my grandfather. He was on his way to refill the boat's gas tank at the local marina, and as he pulled into the dock, I proceeded to make a dire mistake. As the line was thrown from the dock, I attempted to cleat the bowline prematurely, and some of the most intense pain I've ever felt in my life ensued.
Saving a life, relieving pain, sharing in the euphoria of animal and owner reuniting after a procedure, to understanding the emotions of losing a loved one – my life was forever altered from the moment I stepped into that animal hospital.
"Call 911!" I screamed, half-dazed as I witnessed blood gushing out of my open wounds, splashing onto the white fiberglass deck of the boat, forming a small puddle beneath my feet. I was instructed to raise my hand to reduce the bleeding, while someone wrapped an icy towel around the wound. The EMTs arrived shortly after and quickly drove me to an open field a short distance away, where a helicopter seemed to instantaneously appear.
The medevac landed on the roof of Stony Brook Hospital before I was expeditiously wheeled into the operating room for a seven-hour surgery to reattach my severed fingers. The distal phalanges of my 3rd and 4th fingers on my left hand had been torn off by the rope tightening on the cleat. I distinctly remember the chill from the cold metal table, the bright lights of the OR, and multiple doctors and nurses scurrying around. The skill and knowledge required to execute multiple skin graft surgeries were impressive and eye-opening. My shortened fingers often raise questions by others; however, they do not impair my self-confidence or physical abilities. The positive outcome of this trial was the realization of my intense desire to become a medical professional.
Despite being the patient, I was extremely impressed with the dedication, competence, and cohesiveness of the medical team. I felt proud to be a critical member of such a skilled group. To this day, I still cannot explain the dichotomy of experiencing being the patient, and concurrently one on the professional team, committed to saving the patient. Certainly, this experience was a defining part of my life and one of the key contributors to why I became an EMT and a volunteer member of the Sample Volunteer Ambulance Corps. The startling ring of the pager, whether it is to respond to an inebriated alcoholic who is emotionally distraught or to help bring breath to a pulseless person who has been pulled from the family swimming pool, I am committed to EMS. All of these events engender the same call to action and must be reacted to with the same seriousness, intensity, and magnanimity. It may be some routine matter or a dire emergency; this is a role filled with uncertainty and ambiguity, but that is how I choose to spend my days. My motives to become a physician are deeply seeded. They permeate my personality and emanate from my desire to respond to the needs of others. Through a traumatic personal event and my experiences as both a professional and volunteer, I have witnessed firsthand the power to heal the wounded and offer hope. Each person defines success in different ways. To know even one life has been improved by my actions affords me immense gratification and meaning. That is success to me and why I want to be a doctor.
This review is provided by EFIIE Consulting Group’s Pre-Health Senior Consultant Jude Chan
This student was a joy to work with — she was also the lowest MCAT profile I ever accepted onto my roster. At 504 on the second attempt (502 on her first) it would seem impossible and unlikely to most that she would be accepted into an allopathic medical school. Even for an osteopathic medical school this score could be too low. Additionally, the student’s GPA was considered competitive at 3.80, but it was from a lower ranked, less known college, so naturally most advisors would tell this student to go on and complete a master’s or postbaccalaureate program to show that she could manage upper level science classes. Further, she needed to retake the MCAT a third time.
However, I saw many other facets to this student’s history and life that spoke volumes about the type of student she was, and this was the positioning strategy I used for her file. Students who read her personal statement should know that acceptance is contingent on so much more than just an essay and MCAT score or GPA. Although many students have greater MCAT scores than 504 and higher GPAs than 3.80, I have helped students with lower scores and still maintained our 100% match rate. You are competing with thousands of candidates. Not every student out there requires our services and we are actually grateful that we can focus on a limited amount out of the tens of thousands that do. We are also here for the students who wish to focus on learning well the organic chemistry courses and physics courses and who want to focus on their research and shadowing opportunities rather than waste time deciphering the next step in this complex process. We tailor a pathway for each student dependent on their health care career goals, and our partnerships with non-profit organizations, hospitals, physicians and research labs allow our students to focus on what matters most — the building up of their basic science knowledge and their exposure to patients and patient care.
Students who read her personal statement should know that acceptance is contingent on so much more than just an essay and MCAT score or GPA.
Even students who believe that their struggle somehow disqualifies them from their dream career in health care can be redeemed if they are willing to work for it, just like this student with 502 and 504 MCAT scores. After our first consult, I saw a way to position her to still be accepted into an MD school in the US — I would not have recommended she register to our roster if I did not believe we could make a difference. Our rosters have a waitlist each semester, and it is in our best interest to be transparent with our students and protect our 100% record — something I consider a win-win. It is unethical to ever guarantee acceptance in admissions as we simply do not control these decisions. However, we respect it, play by the rules, and help our students stay one step ahead by creating an applicant profile that would be hard for the schools to ignore.
This may be the doctor I go to one day. Or the nurse or dentist my children or my grandchildren goes to one day. That is why it is much more than gaining acceptance — it is about properly matching the student to the best options for their education. Gaining an acceptance and being incapable of getting through the next 4 or 8 years (for my MD/PhD-MSTP students) is nonsensical.
-- Accepted To: Imperial College London UCAT Score: 2740 BMAT Score: 3.9, 5.4, 3.5A
My motivation to study Medicine stems from wishing to be a cog in the remarkable machine that is universal healthcare: a system which I saw first-hand when observing surgery in both the UK and Sri Lanka. Despite the differences in sanitation and technology, the universality of compassion became evident. When volunteering at OSCE training days, I spoke to many medical students, who emphasised the importance of a genuine interest in the sciences when studying Medicine. As such, I have kept myself informed of promising developments, such as the use of monoclonal antibodies in cancer therapy. After learning about the role of HeLa cells in the development of the polio vaccine in Biology, I read 'The Immortal Life of Henrietta Lacks' to find out more. Furthermore, I read that surface protein CD4 can be added to HeLa cells, allowing them to be infected with HIV, opening the possibility of these cells being used in HIV research to produce more life-changing drugs, such as pre-exposure prophylaxis (PreP). Following my BioGrad laboratory experience in HIV testing, and time collating data for research into inflammatory markers in lung cancer, I am also interested in pursuing a career in medical research. However, during a consultation between an ENT surgeon and a thyroid cancer patient, I learnt that practising medicine needs more than a scientific aptitude. As the surgeon explained that the cancer had metastasised to her liver, I watched him empathetically tailor his language for the patient - he avoided medical jargon and instead gave her time to come to terms with this. I have been developing my communication skills by volunteering weekly at care homes for 3 years, which has improved my ability to read body language and structure conversations to engage with the residents, most of whom have dementia.
However, during a consultation between an ENT surgeon and a thyroid cancer patient, I learnt that practising medicine needs more than a scientific aptitude.
Jude’s essay provides a very matter-of-fact account of their experience as a pre-medical student. However, they deepen this narrative by merging two distinct cultures through some common ground: a universality of compassion. Using clear, concise language and a logical succession of events — much like a doctor must follow when speaking to patients — Jude shows their motivation to go into the medical field.
From their OSCE training days to their school’s Science society, Jude connects their analytical perspective — learning about HeLa cells — to something that is relatable and human, such as a poor farmer’s notable contribution to science. This approach provides a gateway into their moral compass without having to explicitly state it, highlighting their fervent desire to learn how to interact and communicate with others when in a position of authority.
Using clear, concise language and a logical succession of events — much like a doctor must follow when speaking to patients — Jude shows their motivation to go into the medical field.
Jude’s closing paragraph reminds the reader of the similarities between two countries like the UK and Sri Lanka, and the importance of having a universal healthcare system that centers around the just and “world-class” treatment of patients. Overall, this essay showcases Jude’s personal initiative to continue to learn more and do better for the people they serve.
While the essay could have benefited from better transitions to weave Jude’s experiences into a personal story, its strong grounding in Jude’s motivation makes for a compelling application essay.
-- Accepted to: Weill Cornell Medical College GPA: 3.98 MCAT: 521
Sponsored by E fie Consulting Group : “ EFIIE ” boasts 100% match rate for all premedical and predental registered students. Not all students are accepted unto their pre-health student roster. Considered the most elite in the industry and assists from start to end – premed to residency. EFIIE is a one-stop-full-service education firm.
Following the physician’s unexpected request, we waited outside, anxiously waiting to hear the latest update on my father’s condition. It was early on in my father’s cancer progression – a change that had shaken our entire way of life overnight. During those 18 months, while my mother spent countless nights at the hospital, I took on the responsibility of caring for my brother. My social life became of minimal concern, and the majority of my studying for upcoming 12th- grade exams was done at the hospital. We were allowed back into the room as the physician walked out, and my parents updated us on the situation. Though we were a tight-knit family and my father wanted us to be present throughout his treatment, what this physician did was give my father a choice. Without making assumptions about who my father wanted in the room, he empowered him to make that choice independently in private. It was this respect directed towards my father, the subsequent efforts at caring for him, and the personal relationship of understanding they formed, that made the largest impact on him. Though my decision to pursue medicine came more than a year later, I deeply valued what these physicians were doing for my father, and I aspired to make a similar impact on people in the future.
It was during this period that I became curious about the human body, as we began to learn physiology in more depth at school. In previous years, the problem-based approach I could take while learning math and chemistry were primarily what sparked my interest. However, I became intrigued by how molecular interactions translated into large-scale organ function, and how these organ systems integrated together to generate the extraordinary physiological functions we tend to under-appreciate. I began my undergraduate studies with the goal of pursuing these interests, whilst leaning towards a career in medicine. While I was surprised to find that there were upwards of 40 programs within the life sciences that I could pursue, it broadened my perspective and challenged me to explore my options within science and healthcare. I chose to study pathobiology and explore my interests through hospital volunteering and research at the end of my first year.
Though my decision to pursue medicine came more than a year later, I deeply valued what these physicians were doing for my father, and I aspired to make a similar impact on people in the future.
While conducting research at St. Michael’s Hospital, I began to understand methods of data collection and analysis, and the thought process of scientific inquiry. I became acquainted with the scientific literature, and the experience transformed how I thought about the concepts I was learning in lecture. However, what stood out to me that summer was the time spent shadowing my supervisor in the neurosurgery clinic. It was where I began to fully understand what life would be like as a physician, and where the career began to truly appeal to me. What appealed to me most was the patient-oriented collaboration and discussions between my supervisor and his fellow; the physician-patient relationship that went far beyond diagnoses and treatments; and the problem solving that I experienced first-hand while being questioned on disease cases.
The day spent shadowing in the clinic was also the first time I developed a relationship with a patient. We were instructed to administer the Montreal cognitive assessment (MoCA) test to patients as they awaited the neurosurgeon. My task was to convey the instructions as clearly as possible and score each section. I did this as best I could, adapting my explanation to each patient, and paying close attention to their responses to ensure I was understood. The last patient was a challenging case, given a language barrier combined with his severe hydrocephalus. It was an emotional time for his family, seeing their father/husband struggle to complete simple tasks and subsequently give up. I encouraged him to continue trying. But I also knew my words would not remedy the condition underlying his struggles. All I could do was make attempts at lightening the atmosphere as I got to know him and his family better. Hours later, as I saw his remarkable improvement following a lumbar puncture, and the joy on his and his family’s faces at his renewed ability to walk independently, I got a glimpse of how rewarding it would be to have the ability and privilege to care for such patients. By this point, I knew I wanted to commit to a life in medicine. Two years of weekly hospital volunteering have allowed me to make a small difference in patients’ lives by keeping them company through difficult times, and listening to their concerns while striving to help in the limited way that I could. I want to have the ability to provide care and treatment on a daily basis as a physician. Moreover, my hope is that the breadth of medicine will provide me with the opportunity to make an impact on a larger scale. Whilst attending conferences on neuroscience and surgical technology, I became aware of the potential to make a difference through healthcare, and I look forward to developing the skills necessary to do so through a Master’s in Global Health. Whether through research, health innovation, or public health, I hope not only to care for patients with the same compassion with which physicians cared for my father, but to add to the daily impact I can have by tackling large-scale issues in health.
Taylor’s essay offers both a straightforward, in-depth narrative and a deep analysis of his experiences, which effectively reveals his passion and willingness to learn in the medical field. The anecdote of Taylor’s father gives the reader insight into an original instance of learning through experience and clearly articulates Taylor’s motivations for becoming a compassionate and respectful physician.
Taylor strikes an impeccable balance between discussing his accomplishments and his character. All of his life experiences — and the difficult challenges he overcame — introduce the reader to an important aspect of Taylor’s personality: his compassion, care for his family, and power of observation in reflecting on the decisions his father’s doctor makes. His description of his time volunteering at St. Michael’s Hospital is indicative of Taylor’s curiosity about medical research, but also of his recognition of the importance of the patient-physician relationship. Moreover, he shows how his volunteer work enabled him to see how medicine goes “beyond diagnoses and treatments” — an observation that also speaks to his compassion.
His description of his time volunteering at St. Michael's Hospital is indicative of Taylor's curiosity about medical research, but also of his recognition of the importance of the patient-physician relationship.
Finally, Taylor also tells the reader about his ambition and purpose, which is important when thinking about applying to medical school. He discusses his hope of tackling larger scale problems through any means possible in medicine. This notion of using self interest to better the world is imperative to a successful college essay, and it is nicely done here.
-- Accepted to: Washington University
Sponsored by A dmitRx : We are a group of Chicago-based medical students who realize how challenging medical school admissions can be, so we want to provide our future classmates with resources we wish we had. Our mission at AdmitRx is to provide pre-medical students with affordable, personalized, high-quality guidance towards becoming an admitted medical student.
Running has always been one of my greatest passions whether it be with friends or alone with my thoughts. My dad has always been my biggest role model and was the first to introduce me to the world of running. We entered races around the country, and one day he invited me on a run that changed my life forever. The St. Jude Run is an annual event that raises millions of dollars for St. Jude Children’s Research Hospital. My dad has led or our local team for as long as I can remember, and I had the privilege to join when I was 16. From the first step I knew this was the environment for me – people from all walks of life united with one goal of ending childhood cancer. I had an interest in medicine before the run, and with these experiences I began to consider oncology as a career. When this came up in conversations, I would invariably be faced with the question “Do you really think you could get used to working with dying kids?” My 16-year-old self responded with something noble but naïve like “It’s important work, so I’ll have to handle it”. I was 16 years young with my plan to become an oncologist at St. Jude.
As I transitioned into college my plans for oncology were alive and well. I began working in a biochemistry lab researching new anti-cancer drugs. It was a small start, but I was overjoyed to be a part of the process. I applied to work at a number of places for the summer, but the Pediatric Oncology Education program (POE) at St. Jude was my goal. One afternoon, I had just returned from class and there it was: an email listed as ‘POE Offer’. I was ecstatic and accepted the offer immediately. Finally, I could get a glimpse at what my future holds. My future PI, Dr. Q, specialized in solid tumor translational research and I couldn’t wait to get started.
I was 16 years young with my plan to become an oncologist at St. Jude.
Summer finally came, I moved to Memphis, and I was welcomed by the X lab. I loved translational research because the results are just around the corner from helping patients. We began a pre-clinical trial of a new chemotherapy regimen and the results were looking terrific. I was also able to accompany Dr. Q whenever she saw patients in the solid tumor division. Things started simple with rounds each morning before focusing on the higher risk cases. I was fortunate enough to get to know some of the patients quite well, and I could sometimes help them pass the time with a game or two on a slow afternoon between treatments. These experiences shined a very human light on a field I had previously seen only through a microscope in a lab.
I arrived one morning as usual, but Dr. Q pulled me aside before rounds. She said one of the patients we had been seeing passed away in the night. I held my composure in the moment, but I felt as though an anvil was crushing down on me. It was tragic but I knew loss was part of the job, so I told myself to push forward. A few days later, I had mostly come to terms with what happened, but then the anvil came crashing back down with the passing of another patient. I could scarcely hold back the tears this time. That moment, it didn’t matter how many miraculous successes were happening a few doors down. Nothing overshadowed the loss, and there was no way I could ‘get used to it’ as my younger self had hoped.
I was still carrying the weight of what had happened and it was showing, so I asked Dr. Q for help. How do you keep smiling each day? How do you get used to it? The questions in my head went on. What I heard next changed my perspective forever. She said you keep smiling because no matter what happened, you’re still hope for the next patient. It’s not about getting used to it. You never get used to it and you shouldn’t. Beating cancer takes lifetimes, and you can’t look passed a life’s worth of hardships. I realized that moving passed the loss of patients would never suffice, but I need to move forward with them. Through the successes and shortcomings, we constantly make progress. I like to imagine that in all our future endeavors, it is the hands of those who have gone before us that guide the way. That is why I want to attend medical school and become a physician. We may never end the sting of loss, but physicians are the bridge between the past and the future. No where else is there the chance to learn from tragedy and use that to shape a better future. If I can learn something from one loss, keep moving forward, and use that knowledge to help even a single person – save one life, bring a moment of joy, avoid a moment of pain—then that is how I want to spend my life.
The change wasn’t overnight. The next loss still brought pain, but I took solace in moving forward so that we might learn something to give hope to a future patient. I returned to campus in a new lab doing cancer research, and my passion for medicine continues to flourish. I still think about all the people I encountered at St. Jude, especially those we lost. It might be a stretch, but during the long hours at the lab bench I still picture their hands moving through mine each step of the way. I could never have foreseen where the first steps of the St. Jude Run would bring me. I’m not sure where the road to becoming a physician may lead, but with helping hands guiding the way, I won’t be running it alone.
This essay, a description of the applicant’s intellectual challenges, displays the hardships of tending to cancer patients as a milestone of experience and realization of what it takes to be a physician. The writer explores deeper ideas beyond medicine, such as dealing with patient deaths in a way to progress and improve as a professional. In this way, the applicant gives the reader some insight into the applicant’s mindset, and their ability to think beyond the surface for ways to become better at what they do.
However, the essay fails to zero in on the applicant’s character, instead elaborating on life events that weakly illustrate the applicant’s growth as a physician. The writer’s mantra (“keep moving forward”) is feebly projected, and seems unoriginal due to the lack of a personalized connection between the experience at St. Jude and how that led to the applicant’s growth and mindset changes.
The writer explores deeper ideas beyond medicine, such as dealing with patient deaths in a way to progress and improve as a professional.
The writer, by only focusing on grief brought from patient deaths at St. Jude, misses out on the opportunity to further describe his or her experience at the hospital and portray an original, well-rounded image of his or her strengths, weaknesses, and work ethic.
The applicant ends the essay by attempting to highlight the things they learned at St. Jude, but fails to organize the ideas into a cohesive, comprehensible section. These ideas are also too abstract, and are vague indicators of the applicant’s character that are difficult to grasp.
-- Accepted to: New York University School of Medicine
Sponsored by MedEdits : MedEdits Medical Admissions has been helping applicants get into medical schools like Harvard for more than ten years. Structured like an academic medical department, MedEdits has experts in admissions, writing, editing, medicine, and interview prep working with you collaboratively so you can earn the best admissions results possible.
“Is this the movie you were talking about Alice?” I said as I showed her the movie poster on my iPhone. “Oh my God, I haven’t seen that poster in over 70 years,” she said with her arms trembling in front of her. Immediately, I sat up straight and started to question further. We were talking for about 40 minutes, and the most exciting thing she brought up in that time was the new flavor of pudding she had for lunch. All of sudden, she’s back in 1940 talking about what it was like to see this movie after school for only 5¢ a ticket! After an engaging discussion about life in the 40’s, I knew I had to indulge her. Armed with a plethora of movie streaming sights, I went to work scouring the web. No luck. The movie, “My Son My Son,” was apparently not in high demand amongst torrenting teens. I had to entreat my older brother for his Amazon Prime account to get a working stream. However, breaking up the monotony and isolation felt at the nursing home with a simple movie was worth the pandering.
While I was glad to help a resident have some fun, I was partly motivated by how much Alice reminded me of my own grandfather. In accordance with custom, my grandfather was to stay in our house once my grandmother passed away. More specifically, he stayed in my room and my bed. Just like grandma’s passing, my sudden roommate was a rough transition. In 8th grade at the time, I considered myself to be a generally good guy. Maybe even good enough to be a doctor one day. I volunteered at the hospital, shadowed regularly, and had a genuine interest for science. However, my interest in medicine was mostly restricted to academia. To be honest, I never had a sustained exposure to the palliative side of medicine until the arrival of my new roommate.
The two years I slept on that creaky wooden bed with him was the first time my metal was tested. Sharing that room, I was the one to take care of him. I was the one to rub ointment on his back, to feed him when I came back from school, and to empty out his spittoon when it got full. It was far from glamorous, and frustrating most of the time. With 75 years separating us, and senile dementia setting in, he would often forget who I was or where he was. Having to remind him that I was his grandson threatened to erode at my resolve. Assured by my Syrian Orthodox faith, I even prayed about it; asking God for comfort and firmness on my end. Over time, I grew slow to speak and eager to listen as he started to ramble more and more about bits and pieces of the past. If I was lucky, I would be able to stich together a narrative that may or may have not been true. In any case, my patience started to bud beyond my age group.
Having to remind him that I was his grandson threatened to erode at my resolve.
Although I grew more patient with his disease, my curiosity never really quelled. Conversely, it developed further alongside my rapidly growing interest in the clinical side of medicine. Naturally, I became drawn to a neurology lab in college where I got to study pathologies ranging from atrophy associated with schizophrenia, and necrotic lesions post stroke. However, unlike my intro biology courses, my work at the neurology lab was rooted beyond the academics. Instead, I found myself driven by real people who could potentially benefit from our research. In particular, my shadowing experience with Dr. Dominger in the Veteran’s home made the patient more relevant in our research as I got to encounter geriatric patients with age related diseases, such as Alzhimer’s and Parkinson’s. Furthermore, I had the privilege of of talking to the families of a few of these patients to get an idea of the impact that these diseases had on the family structure. For me, the scut work in the lab meant a lot more with these families in mind than the tritium tracer we were using in the lab.
Despite my achievements in the lab and the classroom, my time with my grandfather still holds a special place in my life story. The more I think about him, the more confident I am in my decision to pursue a career where caring for people is just as important, if not more important, than excelling at academics. Although it was a lot of work, the years spent with him was critical in expanding my horizons both in my personal life and in the context of medicine. While I grew to be more patient around others, I also grew to appreciate medicine beyond the science. This more holistic understanding of medicine had a synergistic effect in my work as I gained a purpose behind the extra hours in the lab, sleepless nights in the library, and longer hours volunteering. I had a reason for what I was doing that may one day help me have long conversations with my own grandchildren about the price of popcorn in the 2000’s.
The most important thing to highlight in Avery’s essay is how he is able to create a duality between his interest in not only the clinical, more academic-based side of medicine, but also the field’s personal side.
He draws personal connections between working with Alice — a patient in a hospital or nursing home — and caring intensely for his grandfather. These two experiences build up the “synergistic” relationship between caring for people and studying the science behind medicine. In this way, he is able to clearly state his passions for medicine and explain his exact motives for entering the field. Furthermore, in his discussion of her grandfather, he effectively employs imagery (“rub ointment on his back,” “feed him when I came back from school,” etc.) to describe the actual work that he does, calling it initially as “far from glamorous, and frustrating most of the time.” By first mentioning his initial impression, then transitioning into how he grew to appreciate the experience, Avery is able to demonstrate a strength of character, sense of enormous responsibility and capability, and open-minded attitude.
He draws personal connections between working with Alice — a patient in a hospital or nursing home — and caring intensely for his grandfather.
Later in the essay, Avery is also able to relate his time caring for his grandfather to his work with Alzheimer’s and Parkinson’s patients, showcasing the social impact of his work, as the reader is likely already familiar with the biological impact of the work. This takes Avery’s essay full circle, bringing it back to how a discussion with an elderly patient about the movies reminds him of why he chose to pursue medicine.
That said, the essay does feel rushed near the end, as the writer was likely trying to remain within the word count. There could be a more developed transition before Avery introduces the last sentence about “conversations with my own grandchildren,” especially as a strong essay ending is always recommended.
-- Accepted To: Saint Louis University Medical School Direct Admission Medical Program
Sponsored by Atlas Admissions : Atlas Admissions provides expert medical school admissions consulting and test preparation services. Their experienced, physician-driven team consistently delivers top results by designing comprehensive, personalized strategies to optimize applications. Atlas Admissions is based in Boston, MA and is trusted by clients worldwide.
The tension in the office was tangible. The entire team sat silently sifting through papers as Dr. L introduced Adam, a 60-year-old morbidly obese man recently admitted for a large open wound along his chest. As Dr. L reviewed the details of the case, his prognosis became even bleaker: hypertension, diabetes, chronic kidney disease, cardiomyopathy, hyperlipidemia; the list went on and on. As the humdrum of the side-conversations came to a halt, and the shuffle of papers softened, the reality of Adam’s situation became apparent. Adam had a few months to live at best, a few days at worst. To make matters worse, Adam’s insurance would not cover his treatment costs. With no job, family, or friends, he was dying poor and alone.
I followed Dr. L out of the conference room, unsure what would happen next. “Well,” she muttered hesitantly, “We need to make sure that Adam is on the same page as us.” It’s one thing to hear bad news, and another to hear it utterly alone. Dr. L frantically reviewed all of Adam’s paperwork desperately looking for someone to console him, someone to be at his side. As she began to make calls, I saw that being a physician calls for more than good grades and an aptitude for science: it requires maturity, sacrifice, and most of all, empathy. That empathy is exactly what I saw in Dr. L as she went out of her way to comfort a patient she met hardly 20 minutes prior.
Since high school, I’ve been fascinated by technology’s potential to improve healthcare. As a volunteer in [the] Student Ambassador program, I was fortunate enough to watch an open-heart surgery. Intrigued by the confluence of technology and medicine, I chose to study biomedical engineering. At [school], I wanted to help expand this interface, so I became involved with research through Dr. P’s lab by studying the applications of electrospun scaffolds for dermal wound healing. While still in the preliminary stages of research, I learned about the Disability Service Club (DSC) and decided to try something new by volunteering at a bowling outing.
As she began to make calls, I saw that being a physician calls for more than good grades and an aptitude for science: it requires maturity, sacrifice, and most of all, empathy.
The DSC promotes awareness of cognitive disabilities in the community and seeks to alleviate difficulties for the disabled. During one outing, I collaborated with Arc, a local organization with a similar mission. Walking in, I was told that my role was to support the participants by providing encouragement. I decided to help a relatively quiet group of individuals assisted by only one volunteer, Mary. Mary informed me that many individuals with whom I was working were diagnosed with ASD. Suddenly, she started cheering, as one of the members of the group bowled a strike. The group went wild. Everyone was dancing, singing, and rejoicing. Then I noticed one gentleman sitting at our table, solemn-faced. I tried to start a conversation with him, but he remained unresponsive. I sat with him for the rest of the game, trying my hardest to think of questions that would elicit more than a monosyllabic response, but to no avail. As the game ended, I stood up to say bye when he mumbled, “Thanks for talking.” Then he quickly turned his head away. I walked away beaming. Although I was unable to draw out a smile or even sustain a conversation, at the end of the day, the fact that this gentleman appreciated my mere effort completely overshadowed the awkwardness of our time together. Later that day, I realized that as much as I enjoyed the thrill of research and its applications, helping other people was what I was most passionate about.
When it finally came time to tell Adam about his deteriorating condition, I was not sure how he would react. Dr. L gently greeted him and slowly let reality take its toll. He stoically turned towards Dr. L and groaned, “I don’t really care. Just leave me alone.” Dr. L gave him a concerned nod and gradually left the room. We walked to the next room where we met with a pastor from Adam’s church.
“Adam’s always been like that,” remarked the pastor, “he’s never been one to express emotion.” We sat with his pastor for over an hour discussing how we could console Adam. It turned out that Adam was part of a motorcycle club, but recently quit because of his health. So, Dr. L arranged for motorcycle pictures and other small bike trinkets to be brought to his room as a reminder of better times.
Dr. L’s simple gesture reminded me of why I want to pursue medicine. There is something sacred, empowering, about providing support when people need it the most; whether it be simple as starting a conversation, or providing support during the most trying of times. My time spent conducting research kindled my interest in the science of medicine, and my service as a volunteer allowed me to realize how much I valued human interaction. Science and technology form the foundation of medicine, but to me, empathy is the essence. It is my combined interest in science and service that inspires me to pursue medicine. It is that combined interest that makes me aspire to be a physician.
Parker’s essay focuses on one central narrative with a governing theme of compassionate and attentive care for patients, which is the key motivator for her application to medical school. Parker’s story focuses on her volunteer experience shadowing of Dr. L who went the extra mile for Adam, which sets Dr. L up as a role model for Parker as she enters the medical field. This effectively demonstrates to the reader what kind of doctor Parker wants to be in the future.
Parker’s narrative has a clear beginning, middle, and end, making it easy for the reader to follow. She intersperses the main narrative about Adam with experiences she has with other patients and reflects upon her values as she contemplates pursuing medicine as a career. Her anecdote about bowling with the patients diagnosed with ASD is another instance where she uses a story to tell the reader why she values helping people through medicine and attentive patient care, especially as she focuses on the impact her work made on one man at the event.
Parker's story focuses on her volunteer experience shadowing of Dr. L who went the extra mile for Adam, which sets Dr. L up as a role model for Parker as she enters the medical field.
All throughout the essay, the writing is engaging and Parker incorporates excellent imagery, which goes well with her varied sentence structure. The essay is also strong because it comes back full circle at its conclusion, tying the overall narrative back to the story of Dr. L and Adam, which speaks to Parker’s motives for going to medical school.
-- Accepted To: Emory School of Medicine
Growing up, I enjoyed visiting my grandparents. My grandfather was an established doctor, helping the sick and elderly in rural Taiwan until two weeks before he died at 91 years old. His clinic was located on the first floor of the residency with an exam room, treatment room, X-ray room, and small pharmacy. Curious about his work, I would follow him to see his patients. Grandpa often asked me if I want to be a doctor just like him. I always smiled, but was more interested in how to beat the latest Pokémon game. I was in 8th grade when my grandfather passed away. I flew back to Taiwan to attend his funeral. It was a gloomy day and the only street in the small village became a mourning place for the villagers. Flowers filled the streets and people came to pay their respects. An old man told me a story: 60 years ago, a village woman was in a difficult labor. My grandfather rushed into the house and delivered a baby boy. That boy was the old man and he was forever grateful. Stories of grandpa saving lives and bringing happiness to families were told during the ceremony. At that moment, I realized why my grandfather worked so tirelessly up until his death as a physician. He did it for the reward of knowing that he kept a family together and saved a life. The ability for a doctor to heal and bring happiness is the reason why I want to study medicine. Medical school is the first step on a lifelong journey of learning, but I feel that my journey leading up to now has taught me some things of what it means to be an effective physician.
With a newfound purpose, I began volunteering and shadowing at my local hospital. One situation stood out when I was a volunteer in the cardiac stress lab. As I attached EKG leads onto a patient, suddenly the patient collapsed and started gasping for air. His face turned pale, then slightly blue. The charge nurse triggered “Code Blue” and started CPR. A team of doctors and nurses came, rushing in with a defibrillator to treat and stabilize the patient. What I noticed was that medicine was not only about one individual acting as a superhero to save a life, but that it takes a team of individuals with an effective leader, working together to deliver the best care. I want to be a leader as well as part of a team that can make a difference in a person’s life. I have refined these lessons about teamwork and leadership to my activities. In high school I was an 8 time varsity letter winner for swimming and tennis and captain of both of those teams. In college I have participated in many activities, but notably serving as assistant principle cellist in my school symphony as well as being a co-founding member of a quartet. From both my athletic experiences and my music experiences I learned what it was like to not only assert my position as a leader and to effectively communicate my views, but equally as important I learned how to compromise and listen to the opinions of others. Many physicians that I have observed show a unique blend of confidence and humility.
What I noticed was that medicine was not only about one individual acting as a superhero to save a life, but that it takes a team of individuals with an effective leader, working together to deliver the best care.
College opened me up to new perspectives on what makes a complete physician. A concept that was preached in the Guaranteed Professional Program Admissions in Medicine (GPPA) was that medicine is both an art and a science. The art of medicine deals with a variety of aspects including patient relationships as well as ethics. Besides my strong affinity for the sciences and mathematics, I always have had interest in history. I took courses in both German literature and history, which influenced me to take a class focusing on Nazi neuroscientists. It was the ideology of seeing the disabled and different races as test subjects rather than people that led to devastating lapses in medical ethics. The most surprising fact for me was that doctors who were respected and leaders in their field disregarded the humanity of patient and rather focused on getting results from their research. Speaking with Dr. Zeidman, the professor for this course, influenced me to start my research which deals with the ethical qualms of using data derived from unethical Nazi experimentation such as the brains derived from the adult and child euthanasia programs. Today, science is so result driven, it is important to keep in mind the ethics behind research and clinical practice. Also the development of personalized genomic medicine brings into question about potential privacy violations and on the extreme end discrimination. The study of ethics no matter the time period is paramount in the medical field. The end goal should always be to put the patient first.
Teaching experiences in college inspired me to become a physician educator if I become a doctor. Post-MCAT, I was offered a job by Next Step Test Prep as a tutor to help students one on one for the MCAT. I had a student who stated he was doing well during practice, but couldn’t get the correct answer during practice tests. Working with the student, I pointed out his lack of understanding concepts and this realization helped him and improves his MCAT score. Having the ability to educate the next generation of doctors is not only necessary, but also a rewarding experience.
My experiences volunteering and shadowing doctors in the hospital as well as my understanding of what it means to be a complete physician will make me a good candidate as a medical school student. It is my goal to provide the best care to patients and to put a smile on a family’s face just as my grandfather once had. Achieving this goal does not take a special miracle, but rather hard work, dedication, and an understanding of what it means to be an effective physician.
Through reflecting on various stages of life, Quinn expresses how they found purpose in pursuing medicine. Starting as a child more interested in Pokemon than their grandfather’s patients, Quinn exhibits personal growth through recognizing the importance of their grandfather’s work saving lives and eventually gaining the maturity to work towards this goal as part of a team.
This essay opens with abundant imagery — of the grandfather’s clinic, flowers filling the streets, and the village woman’s difficult labor — which grounds Quinn’s story in their family roots. Yet, the transition from shadowing in hospitals to pursuing leadership positions in high schools is jarring, and the list of athletic and musical accomplishments reads like a laundry list of accomplishments until Quinn neatly wraps them up as evidence of leadership and teamwork skills. Similarly, the section about tutoring, while intended to demonstrate Quinn’s desire to educate future physicians, lacks the emotional resonance necessary to elevate it from another line lifted from their resume.
This essay opens with abundant imagery — of the grandfather's clinic, flowers filling the streets, and the village woman's difficult labor — which grounds Quinn's story in their family roots.
The strongest point of Quinn’s essay is the focus on their unique arts and humanities background. This equips them with a unique perspective necessary to consider issues in medicine in a new light. Through detailing how history and literature coursework informed their unique research, Quinn sets their application apart from the multitude of STEM-focused narratives. Closing the essay with the desire to help others just as their grandfather had, Quinn ties the narrative back to their personal roots.
-- Accepted To: Edinburgh University UCAT Score: 2810 BMAT Score: 4.6, 4.2, 3.5A
Exposure to the medical career from an early age by my father, who would explain diseases of the human body, sparked my interest for Medicine and drove me to seek out work experience. I witnessed the contrast between use of bone saws and drills to gain access to the brain, with subsequent use of delicate instruments and microscopes in neurosurgery. The surgeon's care to remove the tumour, ensuring minimal damage to surrounding healthy brain and his commitment to achieve the best outcome for the patient was inspiring. The chance to have such a positive impact on a patient has motivated me to seek out a career in Medicine.
Whilst shadowing a surgical team in Texas, carrying out laparoscopic bariatric procedures, I appreciated the surgeon's dedication to continual professional development and research. I was inspired to carry out an Extended Project Qualification on whether bariatric surgery should be funded by the NHS. By researching current literature beyond my school curriculum, I learnt to assess papers for bias and use reliable sources to make a conclusion on a difficult ethical situation. I know that doctors are required to carry out research and make ethical decisions and so, I want to continue developing these skills during my time at medical school.
The chance to have such a positive impact on a patient has motivated me to seek out a career in Medicine.
Attending an Oncology multi-disciplinary team meeting showed me the importance of teamwork in medicine. I saw each team member, with specific areas of expertise, contributing to the discussion and actively listening, and together they formed a holistic plan of action for patients. During my Young Enterprise Award, I facilitated a brainstorm where everyone pitched a product idea. Each member offered a different perspective on the idea and then voted on a product to carry forward in the competition. As a result, we came runners up in the Regional Finals. Furthermore, I started developing my leadership skills, which I improved by doing Duke of Edinburgh Silver and attending a St. John Ambulance Leadership course. In one workshop, similar to the bariatric surgeon I shadowed, I communicated instructions and delegated roles to my team to successfully solve a puzzle. These experiences highlighted the crucial need for teamwork and leadership as a doctor.
Observing a GP, I identified the importance of compassion and empathy. During a consultation with a severely depressed patient, the GP came to the patient's eye level and used a calm, non-judgmental tone of voice, easing her anxieties and allowing her to disclose more information. While volunteering at a care home weekly for two years, I adapted my communication for a resident suffering with dementia who was disconnected from others. I would take her to a quiet environment, speak slowly and in a non-threatening manner, as such, she became talkative, engaged and happier. I recognised that communication and compassion allows doctors to build rapport, gain patients' trust and improve compliance. For two weeks, I shadowed a surgeon performing multiple craniotomies a day. I appreciated the challenges facing doctors including time and stress management needed to deliver high quality care. Organisation, by prioritising patients based on urgency and creating a timetable on the ward round, was key to running the theatre effectively. Similarly, I create to-do-lists and prioritise my academics and extra-curricular activities to maintain a good work-life balance: I am currently preparing for my Grade 8 in Singing, alongside my A-level exams. I also play tennis for the 1st team to relax and enable me to refocus. I wish to continue my hobbies at university, as ways to manage stress.
Through my work experiences and voluntary work, I have gained a realistic understanding of Medicine and its challenges. I have begun to display the necessary skills that I witnessed, such as empathy, leadership and teamwork. The combination of these skills with my fascination for the human body drives me to pursue a place at medical school and a career as a doctor.
This essay traces Alex's personal exploration of medicine through different stages of life, taking a fairly traditional path to the medical school application essay. From witnessing medical procedures to eventually pursuing leadership positions, this tale of personal progress argues that Alex's life has prepared him to become a doctor.
Alex details how experiences conducting research and working with medical teams have confirmed his interest in medicine. Although the breadth of experiences speaks to the applicant’s interest in medicine, the essay verges on being a regurgitation of the Alex's resume, which does not provide the admissions officer with any new insights or information and ultimately takes away from the essay as a whole. As such, the writing’s lack of voice or unique perspective puts the applicant at risk of sounding middle-of-the-road.
From witnessing medical procedures to eventually pursuing leadership positions, this tale of personal progress argues that Alex's life has prepared him to become a doctor.
The essay’s organization, however, is one of its strengths — each paragraph provides an example of personal growth through a new experience in medicine. Further, Alex demonstrates his compassion and diligence through detailed stories, which give a reader a glimpse into his values. Through recognizing important skills necessary to be a doctor, Alex demonstrates that he has the mature perspective necessary to embark upon this journey.
What this essay lacks in a unique voice, it makes up for in professionalism and organization. Alex's earnest desire to attend medical school is what makes this essay shine.
-- Accepted To: University of Toronto MCAT Scores: Chemical and Physical Foundations of Biological Systems - 128, Critical Analysis and Reading Skills - 127, Biological and Biochemical Foundations of Living Systems - 127, Psychological, Social, and Biological Foundations of Behavior - 130, Total - 512
Moment of brilliance.
Revelation.
These are all words one would use to describe their motivation by a higher calling to achieve something great. Such an experience is often cited as the reason for students to become physicians; I was not one of these students. Instead of waiting for an event like this, I chose to get involved in the activities that I found most invigorating. Slowly but surely, my interests, hobbies, and experiences inspired me to pursue medicine.
As a medical student, one must possess a solid academic foundation to facilitate an understanding of physical health and illness. Since high school, I found science courses the most appealing and tended to devote most of my time to their exploration. I also enjoyed learning about the music, food, literature, and language of other cultures through Latin and French class. I chose the Medical Sciences program because it allowed for flexibility in course selection. I have studied several scientific disciplines in depth like physiology and pathology while taking classes in sociology, psychology, and classical studies. Such a diverse academic portfolio has strengthened my ability to consider multiple viewpoints and attack problems from several angles. I hope to relate to patients from all walks of life as a physician and offer them personalized treatment.
I was motivated to travel as much as possible by learning about other cultures in school. Exposing myself to different environments offered me perspective on universal traits that render us human. I want to pursue medicine because I believe that this principle of commonality relates to medical practice in providing objective and compassionate care for all. Combined with my love for travel, this realization took me to Nepal with Volunteer Abroad (VA) to build a school for a local orphanage (4). The project’s demands required a group of us to work closely as a team to accomplish the task. Rooted in different backgrounds, we often had conflicting perspectives; even a simple task such as bricklaying could stir up an argument because each person had their own approach. However, we discussed why we came to Nepal and reached the conclusion that all we wanted was to build a place of education for the children. Our unifying goal allowed us to reach compromises and truly appreciate the value of teamwork. These skills are vital in a clinical setting, where physicians and other health care professionals need to collaborate as a multidisciplinary team to tackle patients’ physical, emotional, social, and psychological problems.
I hope to relate to patients from all walks of life as a physician and offer them personalized treatment.
The insight I gained from my Nepal excursion encouraged me to undertake and develop the role of VA campus representative (4). Unfortunately, many students are not equipped with the resources to volunteer abroad; I raised awareness about local initiatives so everyone had a chance to do their part. I tried to avoid pushing solely for international volunteerism for this reason and also because it can undermine the work of local skilled workers and foster dependency. Nevertheless, I took on this position with VA because I felt that the potential benefits were more significant than the disadvantages. Likewise, doctors must constantly weigh out the pros and cons of a situation to help a patient make the best choice. I tried to dispel fears of traveling abroad by sharing first-hand experiences so that students could make an informed decision. When people approached me regarding unfamiliar placements, I researched their questions and provided them with both answers and a sense of security. I found great fulfillment in addressing the concerns of individuals, and I believe that similar processes could prove invaluable in the practice of medicine.
As part of the Sickkids Summer Research Program, I began to appreciate the value of experimental investigation and evidence-based medicine (23). Responsible for initiating an infant nutrition study at a downtown clinic, I was required to explain the project’s implications and daily protocol to physicians, nurses and phlebotomists. I took anthropometric measurements and blood pressure of children aged 1-10 and asked parents about their and their child’s diet, television habits, physical exercise regimen, and sunlight exposure. On a few occasions, I analyzed and presented a small set of data to my superiors through oral presentations and written documents.
With continuous medical developments, physicians must participate in lifelong learning. More importantly, they can engage in research to further improve the lives of their patients. I encountered a young mother one day at the clinic struggling to complete the study’s questionnaires. After I asked her some questions, she began to open up to me as her anxiety subsided; she then told me that her child suffered from low iron. By talking with the physician and reading a few articles, I recommended a few supplements and iron-rich foods to help her child. This experience in particular helped me realize that I enjoy clinical research and strive to address the concerns of people with whom I interact.
Research is often impeded by a lack of government and private funding. My clinical placement motivated me to become more adept in budgeting, culminating in my role as founding Co-President of the UWO Commerce Club (ICCC) (9). Together, fellow club executives and I worked diligently to get the club ratified, a process that made me aware of the bureaucratic challenges facing new organizations. Although we had a small budget, we found ways of minimizing expenditure on advertising so that we were able to host more speakers who lectured about entrepreneurship and overcoming challenges. Considering the limited space available in hospitals and the rising cost of health care, physicians, too, are often forced to prioritize and manage the needs of their patients.
No one needs a grand revelation to pursue medicine. Although passion is vital, it is irrelevant whether this comes suddenly from a life-altering event or builds up progressively through experience. I enjoyed working in Nepal, managing resources, and being a part of clinical and research teams; medicine will allow me to combine all of these aspects into one wholesome career.
I know with certainty that this is the profession for me.
Jimmy opens this essay hinting that his essay will follow a well-worn path, describing the “big moment” that made him realize why he needed to become a physician. But Jimmy quickly turns the reader’s expectation on its head by stating that he did not have one of those moments. By doing this, Jimmy commands attention and has the reader waiting for an explanation. He soon provides the explanation that doubles as the “thesis” of his essay: Jimmy thinks passion can be built progressively, and Jimmy’s life progression has led him to the medical field.
Jimmy did not make the decision to pursue a career in medicine lightly. Instead he displays through anecdotes that his separate passions — helping others, exploring different walks of life, personal responsibility, and learning constantly, among others — helped Jimmy realize that being a physician was the career for him. By talking readers through his thought process, it is made clear that Jimmy is a critical thinker who can balance multiple different perspectives simultaneously. The ability to evaluate multiple options and make an informed, well-reasoned decision is one that bodes well for Jimmy’s medical career.
While in some cases this essay does a lot of “telling,” the comprehensive and decisive walkthrough indicates what Jimmy’s idea of a doctor is. To him, a doctor is someone who is genuinely interested in his work, someone who can empathize and related to his patients, someone who can make important decisions with a clear head, and someone who is always trying to learn more. Just like his decision to work at the VA, Jimmy has broken down the “problem” (what his career should be) and reached a sound conclusion.
By talking readers through his thought process, it is made clear that Jimmy is a critical thinker who can balance multiple different perspectives simultaneously.
Additionally, this essay communicates Jimmy’s care for others. While it is not always advisable to list one’s volunteer efforts, each activity Jimmy lists has a direct application to his essay. Further, the sheer amount of philanthropic work that Jimmy does speaks for itself: Jimmy would not have worked at VA, spent a summer with Sickkids, or founded the UWO finance club if he were not passionate about helping others through medicine. Like the VA story, the details of Jimmy’s participation in Sickkids and the UWO continue to show how he has thought about and embodied the principles that a physician needs to be successful.
Jimmy’s essay both breaks common tropes and lives up to them. By framing his “list” of activities with his passion-happens-slowly mindset, Jimmy injects purpose and interest into what could have been a boring and braggadocious essay if it were written differently. Overall, this essay lets the reader know that Jimmy is seriously dedicated to becoming a physician, and both his thoughts and his actions inspire confidence that he will give medical school his all.
The Crimson's news and opinion teams—including writers, editors, photographers, and designers—were not involved in the production of this content.

IMAGES
VIDEO
COMMENTS
The authors describe the important role of medical schools and graduate medical education programs (residencies) in relationship to the advances in Medicine witnessed during the twentieth century; diagnosis, prognosis and treatment were revolutionized. This historical essay details the evolution of the education system and the successful ...
The medical education system based on principles advocated by Flexner and Osler has produced generations of scientifically grounded and clinically skilled physicians whose collective experiences and contributions have served medicine and patients well. Yet sweeping changes launched around the turn of the millennium have constituted a revolution in medical education.
Aims and scope. BMC Medical Education is an open access journal publishing original peer-reviewed research articles in relation to the education and training of healthcare professionals. The journal welcomes studies on students and professionals across all levels of education; education delivery aspects; and other education-related topics.
For medical education research, the main lesson to draw from what we have presented above is the need to move beyond one-dimensional research designs that either focus on just one domain - qualification, socialization, or subjectification - and 'forget' to explore the interactions between the three or, even worse, that continue to ...
One of the earliest milestones in the improvement of U.S. medical education was, in fact, the founding of the AMA, in 1847, with the goals of setting standards for ethics and medical education. Later, in 1904, the AMA established its Council on Medical Education, which began rating medical schools as a way to measure quality.
Medical Education is the leading international journal for research about health professional education. As a pre-eminent medical education journal, we publish papers that are practically relevant and advance conceptual understanding of educational issues, reflecting worldwide or provocative issues and perspectives.
Introduction. Medical education research (MER) advances innovation in medical education and improves its quality. However, for novice clinician-educators, generating medical education scholarship can be daunting [Citation 1].The 'alien culture' of MER, with its own concepts and processes [Citation 2], and time-constraints [Citation 3], may hinder clinician-educators from appropriately ...
The 1910 Flexner Report, officially titled "Medical Education in the United States and Canada," was a landmark document that brought about medical education reform in North America. Abraham Flexner, a research scholar at the Carnegie Foundation, visited all 155 medical schools in operation at the time to assess the state of medical education.
In a 2015 essay titled "Making the Case for History in Medical Education" in the Journal of the History of Medicine and Allied Sciences, David Jones, Jeremy Greene, Jacalyn Duffin, and John Harley Warner issued a challenge for historians of medicine. "In a world where many interests make demands for curriculum time and attention," they argued, "historians of medicine need a more ...
In graduate medical education, there are five performance levels for each competency: novice, advanced beginner, competent individual, proficient individual, and expert physician. ... biology and the medical essay is interesting to read and your blog gives provide the diagnosed point, medical education tips of safety should know to every person.
A Systematic Scoping Review (SSR) is employed to map the employ, structuring and assessment of RW in medical education. An SSR-based review is especially useful in attending to qualitative data that does not lend itself to statistical pooling [40,41,42] whilst its broad flexible approach allows the identification of patterns, relationships and disagreements [] across a wide range of study ...
The drivers for promoting and developing high levels of reflective competency in medical education at all levels, within undergraduate, postgraduate and continuing professional development throughout a lifelong career, are individual learning and professional competence. Deep and Figure 1. Principal drivers for reflection in medical education
Purpose Artificial Intelligence (AI) is transforming healthcare and shows considerable promise for the delivery of medical education. This systematic review provides a comprehensive analysis of the global situation, effects, and challenges associated with applying AI at the different stages of medical education. Methods This review followed the PRISMA guidelines, and retrieved studies ...
Medical Education Essay. The major features of contemporary medical schools took shape in the late nineteenth and early twentieth centuries. What occurred at that time thoroughly transformed medical education. Subsequent developments rarely had the same far-reaching effects as the changes put in place from the 1870s through the 1920s.
Perspectives on Medical Education. Start Submission. Become a Reviewer. Latest news. Stop animation. Previous slide. Competence by Design. Special Collection. Competence by Design. Special Collection.
The essay should not be a dry piece of writing; it should make the reader feel for the author, says Lobo, director of academic conferences and continuing medical education with the emergency ...
Background Written assessments fall into two classes: constructed-response or open-ended questions, such as the essay and a number of variants of the short-answer question, and selected-response or closed-ended questions; typically in the form of multiple-choice. It is widely believed that constructed response written questions test higher order cognitive processes in a manner that multiple ...
Part 3: The medical school adversity essay Example adversity essay prompts. Example 1: "Share with us a difficult or challenging situation you have encountered and how you dealt with it.In your response, identify both the coping skills you called upon to resolve the dilemma, and the support person(s) from whom you sought advice." (University of Chicago Pritzker School of Medicine)
EFIIE is a one-stop-full-service education firm. sponsored by ... ESSAY. Exposure to the medical career from an early age by my father, who would explain diseases of the human body, sparked my ...
Arizona (Suggested reading: Medical Schools in Arizona: How to Get In) A.T. Still University School of Osteopathic Medicine. 2022-2023. ATSU-SOMA's osteopathic medical education model includes training at one of our partner Community Health Center (CHC) sites.