An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley Open Access Collection


Obesity: Risk factors, complications, and strategies for sustainable long‐term weight management
Sharon m. fruh.
1 College of Nursing, University of South Alabama, Mobile, Alabama
Background and Purpose
The aims of this article are to review the effects of obesity on health and well‐being and the evidence indicating they can be ameliorated by weight loss, and consider weight‐management strategies that may help patients achieve and maintain weight loss.
Narrative review based on literature searches of PubMed up to May 2016 with no date limits imposed. Search included terms such as “obesity,” “overweight,” “weight loss,” “comorbidity,” “diabetes,” cardiovascular,” “cancer,” “depression,” “management,” and “intervention.”
Conclusions
Over one third of U.S. adults have obesity. Obesity is associated with a range of comorbidities, including diabetes, cardiovascular disease, obstructive sleep apnea, and cancer; however, modest weight loss in the 5%–10% range, and above, can significantly improve health‐related outcomes. Many individuals struggle to maintain weight loss, although strategies such as realistic goal‐setting and increased consultation frequency can greatly improve the success of weight‐management programs. Nurse practitioners have key roles in establishing weight‐loss targets, providing motivation and support, and implementing weight‐loss programs.
Implications for Practice
With their in‐depth understanding of the research in the field of obesity and weight management, nurse practitioners are well placed to effect meaningful changes in weight‐management strategies deployed in clinical practice.
Introduction
Obesity is an increasing, global public health issue. Patients with obesity are at major risk for developing a range of comorbid conditions, including cardiovascular disease (CVD), gastrointestinal disorders, type 2 diabetes (T2D), joint and muscular disorders, respiratory problems, and psychological issues, which may significantly affect their daily lives as well as increasing mortality risks. Obesity‐associated conditions are manifold; however, even modest weight reduction may enable patients to reduce their risk for CVD, diabetes, obstructive sleep apnea (OSA), and hypertension among many other comorbidities (Cefalu et al., 2015 ). A relatively small and simple reduction in weight, for example, of around 5%, can improve patient outcomes and may act as a catalyst for further change, with sustainable weight loss achieved through a series of incremental weight loss steps. In facilitating the process of losing weight for patients, nurse practitioners play an essential role. Through assessing the patient's risk, establishing realistic weight‐loss targets, providing motivation and support, and supplying patients with the necessary knowledge and treatment tools to help achieve weight loss, followed by tools for structured lifestyle support to maintain weight lost, the nurse practitioner is ideally positioned to help patient's achieve their weight‐loss—and overall health—targets.
The obesity epidemic
The World Health Organization (WHO) defines overweight and obesity as abnormal or excessive fat accumulation that presents a risk to health (WHO, 2016a ). A body mass index (BMI) ≥25 kg/m 2 is generally considered overweight, while obesity is considered to be a BMI ≥ 30 kg/m 2 . It is well known that obesity and overweight are a growing problem globally with high rates in both developed and developing countries (Capodaglio & Liuzzi, 2013 ; WHO, 2016a , 2016b ).
In the United States in 2015, all states had an obesity prevalence more than 20%, 25 states and Guam had obesity rates >30% and four of those 25 states (Alabama, Louisiana, Mississippi, and West Virginia) had rates >35% (Centres for Disease Control and Prevention, 2016 ; Figure Figure1). 1 ). Approximately 35% and 37% of adult men and women, respectively, in the United States have obesity (Yang & Colditz, 2015 ). Adult obesity is most common in non‐Hispanic black Americans, followed by Mexican Americans, and non‐Hispanic white Americans (Yang & Colditz, 2015 ). Individuals are also getting heavier at a younger age; birth cohorts from 1966 to 1975 and 1976 to 1985 reached an obesity prevalence of ≥20% by 20–29 years of age, while the 1956–1965 cohort only reached this prevalence by age 30–39 years (Lee et al., 2010 ). Additionally, the prevalence of childhood obesity in 2‐ to 17‐year‐olds in the United States has increased from 14.6% in 1999–2000 to 17.4% in 2013–2014 (Skinner & Skelton, 2014 ). Childhood obesity is an increasing health issue because of the early onset of comorbidities that have major adverse health impacts, and the increased likelihood of children with obesity going on to become adults with obesity (50% risk vs. 10% for children without obesity; Whitaker, Wright, Pepe, Seidel, & Dietz, 1997 ).

U.S. obesity epidemic 2015.
Source . Figure adapted from Centers for Disease Control and Prevention (CDC). Retrieved from https://www.cdc.gov/obesity/data/prevalence-maps.html .
Association of obesity with mortality and comorbid disease
Obesity is associated with a significant increase in mortality, with a life expectancy decrease of 5–10 years (Berrington de Gonzalez et al., 2010 ; Kuk et al., 2011 ; Prospective Studies Collaboration et al., 2009 ). There is evidence to indicate that all‐cause, CVD‐associated, and cancer‐associated mortalities are significantly increased in individuals with obesity, specifically those at Stages 2 or 3 of the Edmonton Obesity Staging System (EOSS; Kuk et al., 2011 ; Figure Figure2). 2 ). Mortality related to cancer is, however, also increased at Stage 1, when the physical symptoms of obesity are marginal (Figure (Figure2). 2 ). Recently, a large‐scale meta‐analysis that included studies that had enrolled over 10 million individuals, indicated that, relative to the reference category of 22.5 to <25 kg/m 2 , the hazard ratio (HR) for all‐cause mortality rose sharply with increasing BMI (The Global BMI Mortality Collaboration, 2016 ). For a BMI of 25.0 to <30.0 kg/m 2 , the HR was 1.11 (95% confidence interval [CI] 1.10, 1.11), and this increased to 1.44 (1.41, 1.47), 1.92 (1.86, 1.98), and 2.71 (2.55, 2.86) for a BMI of 30.0 to <35.0, 35.0 to <40.0, and 40.0 to <60.0 kg/m 2 , respectively.

Association between EOSS stage and risk of all‐cause (A), CVD (B), cancer (C), and non‐CVD or noncancer mortality (D) in men and women. © 2011.
Source . Reproduced with permission from NRC Research Press, from Kuk et al. ( 2011 ). CVD, cardiovascular disease; NW, normal weight.
Comorbidities
Obesity is a chronic disease that is associated with a wide range of complications affecting many different aspects of physiology (Dobbins, Decorby, & Choi, 2013 ; Guh et al., 2009 ; Martin‐Rodriguez, Guillen‐Grima, Marti, & Brugos‐Larumbe, 2015 ; summarized in Table Table1). 1 ). To examine these obesity‐related morbidities in detail is beyond the scope of this review and therefore only a brief overview of some of the key pathophysiological processes is included next.
Morbidities associated with obesity (Hamdy, 2016 ; Petry, Barry, Pietrzak, & Wagner, 2008 ; Pi‐Sunyer, 2009 ; Sakai et al., 2005 ; Smith, Hulsey, & Goodnight, 2008 ; Yosipovitch, DeVore, & Dawn, 2007 )
The progression from lean state to obesity brings with it a phenotypic change in adipose tissue and the development of chronic low‐grade inflammation (Wensveen, Valentic, Sestan, Turk Wensveen, & Polic, 2015 ). This is characterized by increased levels of circulating free‐fatty acids, soluble pro‐inflammatory factors (such as interleukin [IL] 1β, IL‐6, tumor necrosis factor [TNF] α, and monocyte chemoattractant protein [MCP] 1) and the activation and infiltration of immune cells into sites of inflammation (Hursting & Dunlap, 2012 ). Obesity is also usually allied to a specific dyslipidemia profile (atherogenic dyslipidemia) that includes small, dense low‐density lipoprotein (LDL) particles, decreased levels of high‐density lipoprotein (HDL) particles, and raised triglyceride levels (Musunuru, 2010 ). This chronic, low‐grade inflammation and dyslipidemia profile leads to vascular dysfunction, including atherosclerosis formation, and impaired fibrinolysis. These, in turn, increase the risk for CVD, including stroke and venous thromboembolism (Blokhin & Lentz, 2013 ).
The metabolic and cardiovascular aspects of obesity are closely linked. The chronic inflammatory state associated with obesity is established as a major contributing factor for insulin resistance, which itself is one of the key pathophysiologies of T2D (Johnson, Milner, & Makowski, 2012 ). Furthermore, central obesity defined by waist circumference is the essential component of the International Diabetes Federation (IDF) definition of the metabolic syndrome (raised triglycerides, reduced HDL cholesterol, raised blood pressure, and raised fasting plasma glucose; International Diabetes Federation, 2006 ).
Obesity is also closely associated with OSA. To start, a number of the conditions associated with obesity such as insulin resistance (Ip et al., 2002 ), systemic inflammation, and dyslipidemia are themselves closely associated with OSA, and concurrently, the obesity‐associated deposition of fat around the upper airway and thorax may affect lumen size and reduce chest compliance that contributes to OSA (Romero‐Corral, Caples, Lopez‐Jimenez, & Somers, 2010 ).
The development of certain cancers, including colorectal, pancreatic, kidney, endometrial, postmenopausal breast, and adenocarcinoma of the esophagus to name a few, have also been shown to be related to excess levels of fat and the metabolically active nature of this excess adipose tissue (Booth, Magnuson, Fouts, & Foster, 2015 ; Eheman et al., 2012 ). Cancers have shown to be impacted by the complex interactions between obesity‐related insulin resistance, hyperinsulinemia, sustained hyperglycemia, oxidative stress, inflammation, and the production of adipokines (Booth et al., 2015 ). The wide range of morbidities associated with obesity represents a significant clinical issue for individuals with obesity. However, as significant as this array of risk factors is for patient health, the risk factors can be positively modified with weight loss.
Obesity‐related morbidities in children and adolescents
As was referred to earlier, children and adolescents are becoming increasingly affected by obesity. This is particularly concerning because of the long‐term adverse consequences of early obesity. Obesity adversely affects the metabolic health of young people and can result in impaired glucose tolerance, T2D, and early‐onset metabolic syndrome (Pulgaron, 2013 ).There is also strong support in the literature for relationships between childhood obesity and asthma, poor dental health (caries), nonalcoholic fatty liver disease (NAFLD), and gastroesophageal reflux disease (GERD; Pulgaron, 2013 ). Obesity can also affect growth and sexual development and may delay puberty in boys and advance puberty in some girls (Burt Solorzano & McCartney, 2010 ). Childhood obesity is also associated with hyperandrogenism and polycystic ovary syndrome (PCOS) in girls (Burt Solorzano & McCartney, 2010 ). Additionally, obesity is associated with psychological problems in young people including attention deficit hyperactivity disorder (ADHD), anxiety, depression, poor self‐esteem, and problems with sleeping (Pulgaron, 2013 ).
Modest weight loss and its long‐term maintenance: Benefits and risks
Guidelines endorse weight‐loss targets of 5%–10% in individuals with obesity or overweight with associated comorbidities, as this has been shown to significantly improve health‐related outcomes for many obesity‐related comorbidities (Cefalu et al., 2015 ; Figure Figure3), 3 ), including T2D prevention, and improvements in dyslipidemia, hyperglycemia, osteoarthritis, stress incontinence, GERD, hypertension, and PCOS. Further benefits may be evident with greater weight loss, particularly for dyslipidemia, hyperglycemia, and hypertension. For NAFLD and OSA, at least 10% weight loss is required to observe clinical improvements (Cefalu et al., 2015 ).

Benefits of modest weight loss. Lines demonstrate the ranges in which weight loss has been investigated and shown to have clinical benefits. Arrows indicate that additional benefits may be seen with further weight loss.
Source . Figure adapted from Cefalu et al. ( 2015 ).
Importantly, the weight‐loss benefits in terms of comorbidities are also reflected in improved all‐cause mortality. A recent meta‐analysis of 15 studies demonstrated that relatively small amounts of weight loss, on average 5.5 kg in the treatment arm versus 0.2 kg with placebo from an average baseline BMI of 35 kg/m 2 , resulted in a substantial 15% reduction in all‐cause mortality (Kritchevsky et al., 2015 ).
Cardiovascular health
Weight loss is associated with beneficial changes in several cardiovascular risk markers, including dyslipidemia, pro‐inflammatory/pro‐thrombotic mediators, arterial stiffness, and hypertension (Dattilo & Kris‐Etherton, 1992 ; Dengo et al., 2010 ; Goldberg et al., 2014 ; Haffner et al., 2005 ; Ratner et al., 2005 ). Importantly, weight loss was found to reduce the risk for CVD mortality by 41% up to 23 years after the original weight‐loss intervention (Li et al., 2014 ; Figure Figure4). 4 ). Evidence including the biological effects of obesity and weight loss, and the increased risk for stroke with obesity indicates that weight loss may be effective for primary‐ and secondary‐stroke prevention (Kernan, Inzucchi, Sawan, Macko, & Furie, 2013 ).

Reduction in cardiovascular mortality with modest weight reduction. Cumulative incidence of CVD mortality during 23 years of follow‐up in the Da Qing study (Li et al., 2014 ). Figure © 2014 Elsevier.
Source . Reproduced with permission from Li et al. ( 2014 ).
Type 2 diabetes
Three major long‐term studies, the Diabetes Prevention Program (DPP), the Diabetes Prevention Study (DPS), and the Da Qing IGT and Diabetes (Da Qing) study, have demonstrated that modest weight loss through short‐term lifestyle or pharmacologic interventions can reduce the risk for developing T2D by 58%, 58%, and 31%, respectively, in individuals with obesity and prediabetes (DPP Research Group et al., 2009 ; Pan et al., 1997 ; Tuomilehto et al., 2001 ). Long‐term benefits were maintained following the interventions; for example, in the DPP, the risk reduction of developing T2D versus placebo was 34% at 10 years and 27% at 15 years following the initial weight‐loss intervention (DPP Research Group, 2015 ; DPP Research Group et al., 2009 ). Weight loss increased the likelihood of individuals reverting from prediabetes to normoglycemia (DPP Research Group et al., 2009 ; Li et al., 2008 ; Lindstrom et al., 2003 , 2006 ; Tuomilehto et al., 2001 ), and also improved other aspects of glycemic control including fasting and postprandial glucose, and insulin sensitivity (Haufe et al., 2013 ; Li et al., 2008 ).
Sleep apnea
Data indicate that weight loss is beneficial, although not curative, in patients with obesity who experience OSA. Meta‐analyses of patients who underwent treatment with either intensive lifestyle intervention (Araghi et al., 2013 ) or bariatric surgery (Greenburg, Lettieri, & Eliasson, 2009 ) demonstrated improvements in apnea‐hypopnea index (AHI) following treatment. In the first of these meta‐analyses, in randomized controlled trials, lifestyle intervention lead to a mean reduction in BMI of 2.3 kg/m 2 , which was associated with a decrease in mean AHI of 6.0 events/h. As expected, weight loss was much higher in the second meta‐analysis that investigated the effect of bariatric surgery on measures of OSA, and this was associated with greater reductions in AHI; the mean BMI reduction of 17.9 kg/m 2 resulted in AHI events being reduced by a mean of 38.2 events/h. Once these improvements in AHI have occurred, they seem to persist for some time, irrespective of a certain degree of weight regain. In one study, an initial mean weight loss of 10.7 kg resulted in a persistent improvement in AHI over a 4‐year period despite weight regain of approximately 50% by Year 4 (Kuna et al., 2013 ).
Intentional weight loss of >9 kg reduced the risk for a range of cancers including breast, endometrium, and colon in the large‐scale Iowa Women's Health Study (Parker & Folsom, 2003 ). The overall reduction in the incidence rate of any cancer was 11% (relative risk, 0.89; 95% CI 0.79, 1.00) for participants who lost more than 9 kg compared with those who did not achieve a more than 9 kg weight loss episode. Additionally, weight loss in participants with obesity has been established to be associated with reductions in cancer biomarkers including soluble E‐selectin and IL‐6 (Linkov et al., 2012 ).
Additional health benefits
The substantial weight loss associated with bariatric surgery has been shown to improve asthma with a 48%–100% improvement in symptoms and reduction in medication use (Juel, Ali, Nilas, & Ulrik, 2012 ); however, there is a potential threshold effect so that modest weight loss of 5%–10% may lead to clinical improvement (Lv, Xiao, & Ma, 2015 ). Similarly, modest weight loss of 5%–10% improves GERD (Singh et al., 2013 ) and liver function (Haufe et al., 2013 ). A study utilizing MRI scanning to examine the effects of weight loss on NAFLD has reported a reduction in liver fat from 18.3% to 13.6% ( p = .03), a relative reduction of 25% (Patel et al., 2015 ). Taking an active role in addressing obesity through behavioral modifications or exercise can also reduce the symptoms of depression (Fabricatore et al., 2011 ), improve urinary incontinence in men and women (Breyer et al., 2014 ; Brown et al., 2006 ), and improve fertility outcomes in women (Kort, Winget, Kim, & Lathi, 2014 ). Additionally, weight loss can reduce the joint‐pain symptoms and disability caused by weight‐related osteoarthritis (Felson, Zhang, Anthony, Naimark, & Anderson, 1992 ; Foy et al., 2011 ).
Mitigating risks
Despite the array of benefits, weight loss can also be linked with certain risks that may need to be managed. One such example is the risk for gallstones with rapid weight loss, which is associated with gallstone formation in 30%–71% of individuals. Gallstone formation is particularly associated with bariatric surgery when weight loss exceeds 1.5 kg/week and occurs particularly within the first 6 weeks following surgery when weight loss is greatest. Slower rates of weight loss appear to mitigate the risk for gallstone formation compared to the general population but may not eliminate it entirely; as was noted in the year‐long, weight‐loss, SCALE trial that compared liraglutide 3.0 mg daily use to placebo and resulted in gallstone formation in 2.5% of treated subjects compared to 1% of subjects taking placebo. For this reason, the risk for cholethiasis should be considered when formulating weight‐loss programs (Weinsier & Ullmann, 1993 ).
Strategies to help individuals achieve and maintain weight loss
Rogge and Gautam have covered the biology of obesity and weight regain within another section of this supplement (Rogge & Gautam, 2017 ), so here we focus on some of the clinical strategies for delivering weight loss and weight loss maintenance lifestyle programs. Structured lifestyle support plays an important role in successful weight management. A total of 34% of participants receiving structured lifestyle support from trained‐nursing staff achieved weight loss of ≥5% over 12 weeks compared with approximately 19% with usual care (Nanchahal et al., 2009 ). This particular structured program, delivered in a primary healthcare setting, included initial assessment and goal setting, an eating plan and specific lifestyle goals, personalized activity program, and advice about managing obstacles to weight loss. Additionally, data from the National Weight Control Registry (NWCR), which is the longest prospective compilation of data from individuals who have successfully lost weight and maintained their weight loss, confirm expectations that sustained changes to both diet and activity levels are central to successful weight management (Table (Table2). 2 ). Therefore, an understanding of different clinical strategies for delivery‐structured support is essential for the nurse practitioner.
Lifestyle factors associated with achieving and maintaining weight loss
Note . Data from (NWCR, 2016 ).
a Walking was the most common activity undertaken.
Realistic weight‐loss targets
From the outset, a patient's estimate of their achievable weight loss may be unrealistic. Setting realistic weight‐loss goals is often difficult because of misinformation from a variety of sources, including friends, media, and other healthcare professionals (Osunlana et al., 2015 ). Many individuals with obesity or overweight have unrealistic goals of 20%–30% weight loss, whereas a more realistic goal would be the loss of 5%–15% of the initial body weight (Fabricatore et al., 2007 ). Promoting realistic weight‐loss expectations for patients was identified as a key difficulty for nurse practitioners, primary care nurses, dieticians, and mental health workers (Osunlana et al., 2015 ). Visual resources showing the health and wellness benefit of modest weight loss may thus be helpful (Osunlana et al., 2015 ). Healthcare practitioners should focus on open discussion about, and re‐enforcement of, realistic weight‐loss goals and assess outcomes consistently according to those goals (Bray, Look, & Ryan, 2013 ).
Maintaining a food diary
The 2013 White Paper from the American Nurse Practitioners Foundation on the Prevention and Treatment of Obesity considers a food diary as an important evidence‐based nutritional intervention in aiding weight loss (ANPF). Consistent and regular recording in a food diary was significantly associated with long‐term weight‐loss success in a group of 220 women (Peterson et al., 2014 ). This group lost a mean of 10.4% of their initial body weight through a 6‐month group‐based weight‐management program and then regained a mean of 2.3% over a 12‐month follow‐up period, during which participants received bimonthly support in person, by telephone, or by e‐mail (Peterson et al., 2014 ). Over the 12‐month follow‐up, women who self‐monitored consistently (≥50% of the extended‐care year) had a mean weight loss of 0.98%, while those who were less consistent (<50%) gained weight (5.1%; p < .01). Therefore, frequent and consistent food monitoring should be encouraged, particularly in the weight‐maintenance phase of any program.
Motivating and supporting patients
Motivational interviewing is a technique that focuses on enhancing intrinsic motivation and behavioral changes by addressing ambivalence (Barnes & Ivezaj, 2015 ). Interviews focus on “change talk,” including the reasons for change and optimism about the intent for change in a supportive and nonconfrontational setting, and may help individuals maintain behavioral changes.
For patients that have achieved weight loss, the behavioral factors associated with maintaining weight loss include strong social support networks, limiting/avoiding disinhibited eating, avoiding binge eating, avoiding eating in response to stress or emotional issues, being accountable for one's decisions, having a strong sense of autonomy, internal motivation, and self‐efficacy (Grief & Miranda, 2010 ). Therefore, encouraging feelings of “self‐worth” or “self‐efficacy” can help individuals to view weight loss as being within their own control and achievable (Cochrane, 2008 ).
Strengthening relationships with patients with overweight or obesity to enhance trust may also improve adherence with weight‐loss programs. Patients with hypertension who reported having “complete trust” in their healthcare practitioner were more than twice as likely to engage in lifestyle changes to lose weight than those who lacked “complete trust” (Jones, Carson, Bleich, & Cooper, 2012 ). It may be prudent to ensure the healthcare staff implementing weight‐loss programs have sufficient time to foster trust with their patients.
Continued support from healthcare staff may help patients sustain the necessary motivation for lifestyle changes. A retrospective analysis of 14,256 patients in primary care identified consultation frequency as a factor that can predict the success of weight‐management programs (Lenoir, Maillot, Guilbot, & Ritz, 2015 ). Individuals who successfully maintained ≥10% weight loss over 12 months visited the healthcare provider on average 0.65 times monthly compared with an average of 0.48 visits/month in those who did not maintain ≥10% weight loss, and 0.39 visits/month in those who failed to achieve the initial ≥10% weight loss ( p < .001; Lenoir et al., 2015 ).
Educational and environmental factors
It is important to consider a patient's education and environment when formulating a weight loss strategy as environmental factors may need to be challenged to help facilitate weight loss. A family history of obesity and childhood obesity are strongly linked to adult obesity, which is likely to be because of both genetic and behavioral factors (Kral & Rauh, 2010 ). Parents create their child's early food experiences and influence their child's attitudes to eating through learned eating habits and food choices (Kral & Rauh, 2010 ). Families can also impart cultural preferences for less healthy food choices and family food choices may be affected by community factors, such as the local availability and cost of healthy food options (Castro, Shaibi, & Boehm‐Smith, 2009 ). Alongside this, genetic variation in taste sensation may influence the dietary palate and influence food choices (Loper, La Sala, Dotson, & Steinle, 2015 ). For example, sensitivity to 6‐n‐propylthiouracil (PROP) is genetically determined, and PROP‐tasting ability ranges from super taster to nontaster. When offered buffet‐style meals over 3 days, PROP nontasters consumed more energy, and a greater proportion of energy from fat compared with super tasters. So it is possible that a family's genetic profile could contribute to eating choices. To address behavioral factors, it is important to ensure that families have appropriate support and information and that any early signs of weight gain are dealt with promptly.
A healthy home food environment can help individuals improve their diet. In children, key factors are availability of fresh fruit and vegetables at home and parental influence through their own fresh fruit and vegetable intake (Wyse, Wolfenden, & Bisquera, 2015 ). In adults, unhealthy home food environment factors include less healthy food in the home and reliance on fast food ( p = .01) are all predictors of obesity (Emery et al., 2015 ).
Family mealtimes are strongly associated with better dietary intake and a randomized controlled trial to encourage healthy family meals showed a promising reduction in excess weight gain in prepubescent children (Fulkerson et al., 2015 ). Another study showed that adolescents with any level of baseline family meal frequency, 1–2, 3–4, and ≥5 family meals/week, had reduced odds of being affected by overweight or obesity 10 years later than adolescents who never ate family meals (Berge et al., 2015 ). Community health advocates have identified the failure of many families to plan meals or prepare food as a barrier to healthy family eating patterns (Fruh, Mulekar, Hall, Fulkerson et al., 2013 ). Meal planning allows healthy meals to be prepared in advance and frozen for later consumption (Fruh, Mulekar, Hall, Adams et al., 2013 ) and is associated with increased consumption of vegetables and healthier meals compared with meals prepared on impulse (Crawford, Ball, Mishra, Salmon, & Timperio, 2007 ; Hersey et al., 2001 ).
The role of the nurse practitioner
The initial and ongoing interactions between patient and nurse practitioner are keys for the determination of an effective approach and implementation of a weight loss program and subsequent weight maintenance. The initial interaction can be instigated by either the nurse practitioner or the patient and once the decision has been made to manage the patient's weight, the evaluation includes a risk assessment, a discussion about the patient's weight, and treatment goal recommendations (American Nurse Practitioner Foundation, 2013 ). Across this process, it may be advantageous to approach this using objective data and language that is motivational and/or nonjudgmental. Patients may struggle with motivation, and therefore, ongoing discussions around the health benefits and improvements to quality of life as a result of weight loss may be required (American Nurse Practitioner Foundation, 2013 ). It may be valuable to allocate personalized benefits to the weight loss such as playing with children/grandchildren (American Nurse Practitioner Foundation, 2013 ). Treatment approaches encompass nonpharmacological and pharmacological strategies; however, it is important to remember that any pharmacological agent used should be used as an adjunct to nutritional and physical activity strategies (American Nurse Practitioner Foundation, 2013 ). Pharmacotherapy options for weight management are discussed further in the article by Golden in this supplement.
Conclusions/summary
The importance of obesity management is underscored both by the serious health consequences for individuals, but also by its increasing prevalence globally, and across age groups in particular. Obesity promotes a chronic, low‐grade, inflammatory state, which is associated with vascular dysfunction, thrombotic disorders, multiple organ damage, and metabolic dysfunction. These physiological effects ultimately lead to the development of a range of morbidities, including CVD, T2D, OSA, and certain cancers along with many others, as well as causing a significant impact on mortality.
However, even modest weight loss of 5%–10% of total body weight can significantly improve health and well‐being, and further benefits are possible with greater weight loss. Weight loss can help to prevent development of T2D in individuals with obesity and prediabetes and has a positive long‐term impact on cardiovascular mortality. Beneficial, although not curative, effects have also been noted on OSA following >10% weight loss. In addition, weight loss reduces the risk for certain cancer types and has positive effects on most comorbidities including asthma, GERD, liver function, urinary incontinence, fertility, joint pain, and depression.
Weight‐loss programs that include realistic weight loss goals, frequent check‐in, and meal/activity diaries may help individuals to lose weight. Setting realistic weight‐loss goals can be difficult; however, visual resources showing the health and wellness benefit of weight loss may be helpful in discussing realistic goals, and help motivate the patient in maintaining the weight loss. Techniques such as motivational interviewing that focus on addressing resistance to behavioral change in a supportive and optimistic manner may help individuals in integrating these changes to allow them to become part of normal everyday life and thus help with maintaining the weight loss. Positive reinforcement in terms of marked early‐weight loss may also assist in improving adherence, so this should be a key goal for weight‐loss programs. Encouraging feelings of “self‐worth” or “self‐efficacy” can help individuals to view weight loss as being within their own control.
Nurse practitioners play a major role in helping patients achieve weight loss through all aspects of the process including assessment, support, motivation, goal‐setting, management, and treatment. With their in‐depth understanding of the research in the field of obesity and weight management, nurse practitioners are well placed to effect meaningful changes in the weight‐management strategies deployed in clinical practice.
List of helpful resources
Acknowledgments.
The authors are grateful to Watermeadow Medical for writing assistance in the development of this manuscript. This assistance was funded by Novo Nordisk, who also had a role in the review of the manuscript for scientific accuracy. The author discussed the concept, drafted the outline, commented in detail on the first iteration, made critical revision of later drafts, and has revised and approved the final version for submission.
Dr. Sharon Fruh serves on the Novo Nordisk Obesity Speakers Bureau. In compliance with national ethical guidelines, the author reports no relationship with business or industry that would post a conflict of interest.
Writing and editorial support was provided by Watermeadow Medical, and funded by Novo Nordisk.
The copyright line in this article was changed on 9 August 2018 after online publication.
- American Nurse Practitioner Foundation . (2013). Nurse practitioners and the prevention and treatment of adult obesity—A White Paper of the American Nurse Practitioner Foundation (electronic version) . Summer. Retrieved from https://international.aanp.org/Content/docs/ObesityWhitePaper.pdf
- Araghi, M. H. , Chen, Y. F. , Jagielski, A. , Choudhury, S. , Banerjee, D. , Hussain, S. , … Taheri, S. , et al. (2013). Effectiveness of lifestyle interventions on obstructive sleep apnea (OSA): Systematic review and meta‐analysis . Sleep , 36 ( 10 ), 1553–1562, 1562a–1562e. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Barnes, R. D. , & Ivezaj, V. (2015). A systematic review of motivational interviewing for weight loss among adults in primary care . Obesity Reviews , 16 ( 4 ), 304–318. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Berge, J. M. , Wall, M. , Hsueh, T. F. , Fulkerson, J. A. , Larson, N. , & Neumark‐Sztainer, D. (2015). The protective role of family meals for youth obesity: 10‐year longitudinal associations . Journal of Pediatrics , 166 ( 2 ), 296–301. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Berrington de Gonzalez, A. , Hartge, P. , Cerhan, J. R. , Flint, A. J. , Hannan, L. , MacInnis, R. J. , … Thun, M. J. , et al. (2010). Body‐mass index and mortality among 1.46 million white adults . New England Journal of Medicine , 363 ( 23 ), 2211–2219. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Blokhin, I. O. , & Lentz, S. R. (2013). Mechanisms of thrombosis in obesity . Current Opinion in Hematology , 20 ( 5 ), 437–444 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Booth, A. , Magnuson, A. , Fouts, J. , & Foster, M. (2015). Adipose tissue, obesity and adipokines: Role in cancer promotion . Hormone Molecular Biology and Clinical Investigation , 21 ( 1 ), 57–74. [ PubMed ] [ Google Scholar ]
- Bray, G. , Look, M. , & Ryan, D. (2013). Treatment of the obese patient in primary care: Targeting and meeting goals and expectations . Postgraduate Medical Journal , 125 ( 5 ), 67–77. [ PubMed ] [ Google Scholar ]
- Breyer, B. N. , Phelan, S. , Hogan, P. E. , Rosen, R. C. , Kitabchi, A. E. , Wing, R. R. , … the Look AHEAD Research Group , et al. (2014). Intensive lifestyle intervention reduces urinary incontinence in overweight/obese men with type 2 diabetes: Results from the Look AHEAD trial . Journal of Urology , 192 ( 1 ), 144–149. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brown, J. S. , Wing, R. , Barrett‐Connor, E. , Nyberg, L. M. , Kusek, J. W. , Orchard, T. J. , … Diabetes Prevention Program Research Group , et al. (2006). Lifestyle intervention is associated with lower prevalence of urinary incontinence: The Diabetes Prevention Program . Diabetes Care , 29 ( 2 ), 385–390. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Burt Solorzano, C. M. , & McCartney, C. R. (2010). Obesity and the pubertal transition in girls and boys . Reproduction , 140 ( 3 ), 399–410. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Capodaglio, P. , & Liuzzi, A. (2013). Obesity: A disabling disease or a condition favoring disability ? European Journal of Physical and Rehabilitation Medicine , 49 ( 3 ), 395–398. [ PubMed ] [ Google Scholar ]
- Castro, F. G. , Shaibi, G. Q. , & Boehm‐Smith, E. (2009). Ecodevelopmental contexts for preventing type 2 diabetes in Latino and other racial/ethnic minority populations . Journal of Behavioral Medicine , 32 ( 1 ), 89–105. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cefalu, W. T. , Bray, G. A. , Home, P. D. , Garvey, W. T. , Klein, S. , Pi‐Sunyer, F. X. , … Ryan, D. H. , et al. (2015). Advances in the science, treatment, and prevention of the disease of obesity: Reflections from a diabetes care editors' expert forum . Diabetes Care , 38 ( 8 ), 1567–1582. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Centres for Disease Control and Prevention . (2016). Overweight and obesity . Retrieved from https://www.cdc.gov/obesity/
- Cochrane, G. (2008). Role for a sense of self‐worth in weight‐loss treatments: Helping patients develop self‐efficacy . Canadian Family Physician , 54 ( 4 ), 543–547. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Crawford, D. , Ball, K. , Mishra, G. , Salmon, J. , & Timperio, A. (2007). Which food‐related behaviours are associated with healthier intakes of fruits and vegetables among women ? Public Health Nutrition , 10 ( 3 ), 256–265. [ PubMed ] [ Google Scholar ]
- Dattilo, A. M. , & Kris‐Etherton, P. M. (1992). Effects of weight reduction on blood lipids and lipoproteins: A meta‐analysis . American Journal of Clinical Nutrition , 56 ( 2 ), 320–328. [ PubMed ] [ Google Scholar ]
- Dengo, A. L. , Dennis, E. A. , Orr, J. S. , Marinik, E. L. , Ehrlich, E. , Davy, B. M. , & Davy, K. P. (2010). Arterial destiffening with weight loss in overweight and obese middle‐aged and older adults . Hypertension , 55 ( 4 ), 855–861. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Diabetes Prevention Program ( DPP) Research Group . (2015). Long‐term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15‐year follow‐up: The Diabetes Prevention Program Outcomes Study . Lancet Diabetes & Endocrinology , 3 ( 11 ), 866–875. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Diabetes Prevention Program ( DPP) Research Group , Knowler, W. C. , Fowler, S. E. , Hamman, R. F. , Christophi, C. A. , Hoffman, H. J. , … Nathan, D. M. , et al. (2009). 10‐year follow‐up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study . Lancet , 374 ( 9702 ), 1677–1686. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dobbins, M. , Decorby, K. , & Choi, B. C. (2013). The association between obesity and cancer risk: A meta‐analysis of observational studies from 1985 to 2011 . ISRN Preventive Medicine , 2013 , 680536 10.5402/2013/680536. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Eheman, C. , Henley, S. J. , Ballard‐Barbash, R. , Jacobs, E. J. , Schymura, M. J. , Noone, A. M. , … Edwards, B. K. , et al. (2012). Annual Report to the Nation on the status of cancer, 1975–2008, featuring cancers associated with excess weight and lack of sufficient physical activity . Cancer , 118 ( 9 ), 2338–2366. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Emery, C. F. , Olson, K. L. , Lee, V. S. , Habash, D. L. , Nasar, J. L. , & Bodine, A. (2015). Home environment and psychosocial predictors of obesity status among community‐residing men and women . International Journal of Obesity , 39 ( 9 ), 1401–1407. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fabricatore, A. N. , Wadden, T. A. , Higginbotham, A. J. , Faulconbridge, L. F. , Nguyen, A. M. , Heymsfield, S. B. , & Faith, M. S. (2011). Intentional weight loss and changes in symptoms of depression: A systematic review and meta‐analysis . International Journal of Obesity , 35 ( 11 ), 1363–1376. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fabricatore, A. N. , Wadden, T. A. , Womble, L. G. , Sarwer, D. B. , Berkowitz, R. I. , Foster, G. D. , & Brock, J. R. (2007). The role of patients' expectations and goals in the behavioral and pharmacological treatment of obesity . International Journal of Obesity , 31 ( 11 ), 1739–1745. [ PubMed ] [ Google Scholar ]
- Felson, D. T. , Zhang, Y. , Anthony, J. M. , Naimark, A. , & Anderson, J. J. (1992). Weight loss reduces the risk for symptomatic knee osteoarthritis in women. The Framingham Study . Annals of Internal Medicine , 116 ( 7 ), 535–539. [ PubMed ] [ Google Scholar ]
- Foy, C. G. , Lewis, C. E. , Hairston, K. G. , Miller, G. D. , Lang, W. , Jakicic, J. M. , … the Look AHEAD Research Group , et al. (2011). Intensive lifestyle intervention improves physical function among obese adults with knee pain: Findings from the Look AHEAD trial . Obesity (Silver Spring) , 19 ( 1 ), 83–93. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fruh, S. M. , Mulekar, M. S. , Hall, H. R. , Adams, J. R. , Lemley, T. , Evans, B. , & Dierking, J. (2013). Meal‐planning practices with individuals in health disparity zip codes . Journal for Nurse Practitioners , 9 ( 6 ), 344–349. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fruh, S. M. , Mulekar, M. S. , Hall, H. R. , Fulkerson, J. A. , Hanks, R. S. , Lemley, T. , … Dierking, J. , et al. (2013). Perspectives of community health advocates: Barriers to healthy family eating patterns . Journal for Nurse Practitioners , 9 ( 7 ), 416–421. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fulkerson, J. A. , Friend, S. , Flattum, C. , Horning, M. , Draxten, M. , Neumark‐Sztainer, D. , … Kubik, M. , et al. (2015). Promoting healthful family meals to prevent obesity: HOME Plus, a randomized controlled trial . International Journal of Behavioral Nutrition and Physical Activity , 12 , 154. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Goldberg, R. B. , Temprosa, M. G. , Mather, K. J. , Orchard, T. J. , Kitabchi, A. E. , & Watson, K. E. , for the Diabetes Prevention Program Research Group . (2014). Lifestyle and metformin interventions have a durable effect to lower CRP and tPA levels in the diabetes prevention program except in those who develop diabetes . Diabetes Care , 37 ( 8 ), 2253–2260. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Greenburg, D. L. , Lettieri, C. J. , & Eliasson, A. H. (2009). Effects of surgical weight loss on measures of obstructive sleep apnea: A meta‐analysis . American Journal of Medicine , 122 ( 6 ), 535–542. [ PubMed ] [ Google Scholar ]
- Grief, S. N. , & Miranda, R. L. (2010). Weight loss maintenance . American Family Physician , 82 ( 6 ), 630–634. [ PubMed ] [ Google Scholar ]
- Guh, D. P. , Zhang, W. , Bansback, N. , Amarsi, Z. , Birmingham, C. L. , & Anis, A. H. (2009). The incidence of co‐morbidities related to obesity and overweight: A systematic review and meta‐analysis . BMC Public Health , 9 , 88. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Haffner, S. , Temprosa, M. , Crandall, J. , Fowler, S. , Goldberg, R. , Horton, E. , … Diabetes Prevention Program Research Group , et al. (2005). Intensive lifestyle intervention or metformin on inflammation and coagulation in participants with impaired glucose tolerance . Diabetes , 54 ( 5 ), 1566–1572. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hamdy, O. (2016). Obesity . Retrieved from https://emedicine.medscape.com/article/123702-overview
- Haufe, S. , Haas, V. , Utz, W. , Birkenfeld, A. L. , Jeran, S. , Bohnke, J. , … Engeli, S. , et al. (2013). Long‐lasting improvements in liver fat and metabolism despite body weight regain after dietary weight loss . Diabetes Care , 36 ( 11 ), 3786–3792. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hersey, J. , Anliker, J. , Miller, C. , Mullis, R. M. , Daugherty, S. , Das, S. , … Olivia, A. H. , et al. (2001). Food shopping practices are associated with dietary quality in low‐income households . Journal of Nutrition Education , 33 ( Suppl 1 ), S16–S26. [ PubMed ] [ Google Scholar ]
- Hursting, S. D. , & Dunlap, S. M. (2012). Obesity, metabolic dysregulation, and cancer: A growing concern and an inflammatory (and microenvironmental) issue . Annals of the New York Academy of Sciences , 1271 , 82–87. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- International Diabetes Federation . (2006). The IDF consensus worldwide definition of the metabolic syndrome (electronic version). Retrieved from https://www.idf.org/webdata/docs/IDF_Meta_def_final.pdf
- Ip, M. S. , Lam, B. , Ng, M. M. , Lam, W. K. , Tsang, K. W. , & Lam, K. S. (2002). Obstructive sleep apnea is independently associated with insulin resistance . American Journal of Respiratory and Critical Care Medicine , 165 ( 5 ), 670–676. [ PubMed ] [ Google Scholar ]
- Johnson, A. R. , Milner, J. J. , & Makowski, L. (2012). The inflammation highway: Metabolism accelerates inflammatory traffic in obesity . Immunological Reviews , 249 ( 1 ), 218–238. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jones, D. E. , Carson, K. A. , Bleich, S. N. , & Cooper, L. A. (2012). Patient trust in physicians and adoption of lifestyle behaviors to control high blood pressure . Patient Education and Counseling , 89 ( 1 ), 57–62. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Juel, C. T. , Ali, Z. , Nilas, L. , & Ulrik, C. S. (2012). Asthma and obesity: Does weight loss improve asthma control? A systematic review . Journal of Asthma and Allergy , 5 , 21–26. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kernan, W. N. , Inzucchi, S. E. , Sawan, C. , Macko, R. F. , & Furie, K. L. (2013). Obesity: A stubbornly obvious target for stroke prevention . Stroke , 44 ( 1 ), 278–286. [ PubMed ] [ Google Scholar ]
- Kort, J. D. , Winget, C. , Kim, S. H. , & Lathi, R. B. (2014). A retrospective cohort study to evaluate the impact of meaningful weight loss on fertility outcomes in an overweight population with infertility . Fertility and Sterility , 101 ( 5 ), 1400–1403. [ PubMed ] [ Google Scholar ]
- Kral, T. V. , & Rauh, E. M. (2010). Eating behaviors of children in the context of their family environment . Physiology & Behavior , 100 ( 5 ), 567–573. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kritchevsky, S. B. , Beavers, K. M. , Miller, M. E. , Shea, M. K. , Houston, D. K. , Kitzman, D. W. , & Nicklas, B. J. (2015). Intentional weight loss and all‐cause mortality: A meta‐analysis of randomized clinical trials . PLoS One , 10 ( 3 ), e0121993. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kuk, J. L. , Ardern, C. I. , Church, T. S. , Sharma, A. M. , Padwal, R. , Sui, X. , … Blair, S. N. , et al. (2011). Edmonton obesity staging system: Association with weight history and mortality risk . Applied Physiology, Nutrition, and Metabolism , 36 ( 4 ), 570–576. [ PubMed ] [ Google Scholar ]
- Kuna, S. T. , Reboussin, D. M. , Borradaile, K. E. , Sanders, M. H. , Millman, R. P. , Zammit, G. , … Sleep AHEAD Research Group of the Look AHEAD Research Group , et al. (2013). Long‐term effect of weight loss on obstructive sleep apnea severity in obese patients with type 2 diabetes . Sleep , 36 ( 5 ), 641–649A. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lee, J. M. , Pilli, S. , Gebremariam, A. , Keirns, C. C. , Davis, M. M. , Vijan, S. , … Gurney, J. G. , et al. (2010). Getting heavier, younger: Trajectories of obesity over the life course . International Journal of Obesity , 34 ( 4 ), 614–623. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lenoir, L. , Maillot, M. , Guilbot, A. , & Ritz, P. (2015). Primary care weight loss maintenance with behavioral nutrition: An observational study . Obesity (Silver Spring) , 23 ( 9 ), 1771–777. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Li, G. , Zhang, P. , Wang, J. , An, Y. , Gong, Q. , Gregg, E. W. , … Bennett, P. H. , et al. (2014). Cardiovascular mortality, all‐cause mortality, and diabetes incidence after lifestyle intervention for people with impaired glucose tolerance in the Da Qing Diabetes Prevention Study: A 23‐year follow‐up study . Lancet Diabetes & Endocrinology , 2 ( 6 ), 474–480. [ PubMed ] [ Google Scholar ]
- Li, G. , Zhang, P. , Wang, J. , Gregg, E. W. , Yang, W. , Gong, Q. , … Bennett, P. H. , et al. (2008). The long‐term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: A 20‐year follow‐up study . Lancet , 371 ( 9626 ), 1783–1789. [ PubMed ] [ Google Scholar ]
- Lindstrom, J. , Eriksson, J. G. , Valle, T. T. , Aunola, S. , Cepaitis, Z. , Hakumaki, M. , … Tuomilehto, J. , et al. (2003). Prevention of diabetes mellitus in subjects with impaired glucose tolerance in the Finnish Diabetes Prevention Study: Results from a randomized clinical trial . Journal of the American Society of Nephrology , 14 ( 7 Suppl 2 ), S108–S113. [ PubMed ] [ Google Scholar ]
- Lindstrom, J. , Ilanne‐Parikka, P. , Peltonen, M. , Aunola, S. , Eriksson, J. G. , Hemio, K. , … Finnish Diabetes Prevention Study Group , et al. (2006). Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: Follow‐up of the Finnish Diabetes Prevention Study . Lancet , 368 ( 9548 ), 1673–1679. [ PubMed ] [ Google Scholar ]
- Linkov, F. , Maxwell, G. L. , Felix, A. S. , Lin, Y. , Lenzner, D. , Bovbjerg, D. H. , … DeLany, J. P. , et al. (2012). Longitudinal evaluation of cancer‐associated biomarkers before and after weight loss in RENEW study participants: Implications for cancer risk reduction . Gynecologic Oncology , 125 ( 1 ), 114–119. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Loper, H. B. , La Sala, M. , Dotson, C. , & Steinle, N. (2015). Taste perception, associated hormonal modulation, and nutrient intake . Nutrition Reviews , 73 ( 2 ), 83–91. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lv, N. , Xiao, L. , & Ma, J. (2015). Weight management interventions in adult and pediatric asthma populations: A systematic review . J Pulm Respir Med , 5 ( 232 ), pii: 1000232. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Martin‐Rodriguez, E. , Guillen‐Grima, F. , Marti, A. , & Brugos‐Larumbe, A. (2015). Comorbidity associated with obesity in a large population: The APNA study . Obesity Research & Clinical Practice , 9 ( 5 ), 435–447. [ PubMed ] [ Google Scholar ]
- Musunuru, K. (2010). Atherogenic dyslipidemia: Cardiovascular risk and dietary intervention . Lipids , 45 ( 10 ), 907–914. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nanchahal, K. , Townsend, J. , Letley, L. , Haslam, D. , Wellings, K. , & Haines, A. (2009). Weight‐management interventions in primary care: A pilot randomised controlled trial . British Journal of General Practice , 59 ( 562 ), e157–e166. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Osunlana, A. M. , Asselin, J. , Anderson, R. , Ogunleye, A. A. , Cave, A. , Sharma, A. M. , & Campbell‐Scherer, D. L.. (2015). 5As team obesity intervention in primary care: Development and evaluation of shared decision‐making weight management tools . Clinical Obesity , 5 ( 4 ), 219–225. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pan, X. R. , Li, G. W. , Hu, Y. H. , Wang, J. X. , Yang, W. Y. , An, Z. X. , … Howard, B. V. , et al. (1997). Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and diabetes study . Diabetes Care , 20 ( 4 ), 537–544. [ PubMed ] [ Google Scholar ]
- Parker, E. D. , & Folsom, A. R. (2003). Intentional weight loss and incidence of obesity‐related cancers: The Iowa Women's Health Study . International Journal of Obesity and Related Metabolic Disorders: Journal of the International Association for the Study of Obesity , 27 ( 12 ), 1447–1452. [ PubMed ] [ Google Scholar ]
- Patel, N. S. , Doycheva, I. , Peterson, M. R. , Hooker, J. , Kisselva, T. , Schnabl, B. , … Loomba, R. , et al. (2015). Effect of weight loss on magnetic resonance imaging estimation of liver fat and volume in patients with nonalcoholic steatohepatitis . Clinical Gastroenterology and Hepatology , 13 ( 3 ), 561–568 e561. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Peterson, N. D. , Middleton, K. R. , Nackers, L. M. , Medina, K. E. , Milsom, V. A. , & Perri, M. G. (2014). Dietary self‐monitoring and long‐term success with weight management . Obesity (Silver Spring) , 22 ( 9 ), 1962–1967. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Petry, N. M. , Barry, D. , Pietrzak, R. H. , & Wagner, J. A. (2008). Overweight and obesity are associated with psychiatric disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions . 70 ( 3 ), 288–297. [ PubMed ] [ Google Scholar ]
- Pi‐Sunyer, X. (2009). The medical risks of obesity . Postgraduate Medicine , 121 ( 6 ), 21–33. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Prospective Studies Collaboration , Whitlock, G. , Lewington, S. , Sherliker, P. , Clarke, R. , Emberson, J. , … Peto, R. , et al. (2009). Body‐mass index and cause‐specific mortality in 900 000 adults: Collaborative analyses of 57 prospective studies . Lancet , 373 ( 9669 ), 1083–1096. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pulgaron, E. R. (2013). Childhood obesity: A review of increased risk for physical and psychological comorbidities . Clin Ther 35 ( 1 ), A18–A32. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ratner, R. , Goldberg, R. , Haffner, S. , Marcovina, S. , Orchard, T. , Fowler, S. , … Diabetes Prevention Program Research Group , et al. (2005). Impact of intensive lifestyle and metformin therapy on cardiovascular disease risk factors in the diabetes prevention program . Diabetes Care , 28 ( 4 ), 888–894. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rogge, M. M. , & Gautam, B. (2017). Biology of obesity and weight regain: Implications for clinical practice . Journal of the American Association of Nurse Practitioners , 29 (Supplement 1), S15–S29. [ PubMed ] [ Google Scholar ]
- Romero‐Corral, A. , Caples, S. M. , Lopez‐Jimenez, F. , & Somers, V. K. (2010). Interactions between obesity and obstructive sleep apnea: Implications for treatment . Chest , 137 ( 3 ), 711–719. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sakai, R. , Matsui, S. , Fukushima, M. , Yasuda, H. , Miyauchi, H. , & Miyachi, Y. (2005). Prognostic factor analysis for plaque psoriasis . Dermatology , 211 ( 2 ), 103–106. [ PubMed ] [ Google Scholar ]
- Singh, M. , Lee, J. , Gupta, N. , Gaddam, S. , Smith, B. K. , Wani, S. B. , … Sharma, P. , et al. (2013). Weight loss can lead to resolution of gastroesophageal reflux disease symptoms: A prospective intervention trial . Obesity (Silver Spring) , 21 ( 2 ), 284–290. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Skinner, A. C. , & Skelton, J. A. (2014). Prevalence and trends in obesity and severe obesity among children in the United States, 1999–2012 . JAMA Pediatrics , 168 ( 6 ), 561–566. [ PubMed ] [ Google Scholar ]
- Smith, S. A. , Hulsey, T. , & Goodnight, W. (2008). Effects of obesity on pregnancy . J Obstet Gynecol Neonatal Nurs , 37 ( 2 ), 176–184. [ PubMed ] [ Google Scholar ]
- The Global BMI Mortality Collaboration . (2016). Body‐mass index and all‐cause mortality: Individual participant‐data meta‐analysis of 239 prospective studies in four continents . Lancet , 388 , 734–736. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- The National Weight Control Registry ( NWCR) . (2016). NCWR facts . Retrieved from https://www.nwcr.ws/
- Tuomilehto, J. , Lindstrom, J. , Eriksson, J. G. , Valle, T. T. , Hamalainen, H. , Ilanne‐Parikka, P. , … Finnish Diabetes Prevention Study Group , et al. (2001). Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance . New England Journal of Medicine , 344 ( 18 ), 1343–1350. [ PubMed ] [ Google Scholar ]
- Weinsier, R. L. , & Ullmann, D. O. (1993). Gallstone formation and weight loss . Obesity Research , 1 ( 1 ), 51–56. [ PubMed ] [ Google Scholar ]
- Wensveen, F. M. , Valentic, S. , Sestan, M. , Turk Wensveen, T. , & Polic, B. (2015). The "Big Bang" in obese fat: Events initiating obesity‐induced adipose tissue inflammation . European Journal of Immunology , 45 ( 9 ), 2446–2456. [ PubMed ] [ Google Scholar ]
- Whitaker, R. C. , Wright, J. A. , Pepe, M. S. , Seidel, K. D. , & Dietz, W. H. (1997). Predicting obesity in young adulthood from childhood and parental obesity . New England Journal of Medicine , 337 ( 13 ), 869–873. [ PubMed ] [ Google Scholar ]
- World Health Organization (WHO) . (2016a). 10 Facts on obesity . Retrieved from https://www.who.int/features/factfiles/obesity/facts/en/
- World Health Organization (WHO) . (2016b). Obesity . Retrieved from https://www.who.int/topics/obesity/en/
- Wyse, R. , Wolfenden, L. , & Bisquera, A. (2015). Characteristics of the home food environment that mediate immediate and sustained increases in child fruit and vegetable consumption: Mediation analysis from the Healthy Habits cluster randomised controlled trial . International Journal of Behavioral Nutrition and Physical Activity , 12 , 118. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Yang, L. , & Colditz, G. A. (2015). Prevalence of overweight and obesity in the United States, 2007–2012 . JAMA Internal Medicine , 175 ( 8 ), 1412–1413. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Yosipovitch, G. , DeVore, A. , & Dawn, A. (2007). Obesity and the skin: Skin physiology and skin manifestations of obesity . J Am Acad Dermatol , 56 ( 6 ), 901–916; quiz 917–920. [ PubMed ] [ Google Scholar ]
Obesity Essay
Last updated on: Feb 9, 2023
Obesity Essay: A Complete Guide and Topics
By: Nova A.
11 min read
Reviewed By: Jacklyn H.
Published on: Aug 31, 2021

Are you assigned to write an essay about obesity? The first step is to define obesity.
The obesity epidemic is a major issue facing our country right now. It's complicated- it could be genetic or due to your environment, but either way, there are ways that you can fix it!
Learn all about what causes weight gain and get tips on how you can get healthy again.

On this Page
What is Obesity
What is obesity? Obesity and BMI (body mass index) are both tools of measurement that are used by doctors to assess body fat according to the height, age, and gender of a person. If the BMI is between 25 to 29.9, that means the person has excess weight and body fat.
If the BMI exceeds 30, that means the person is obese. Obesity is a condition that increases the risk of developing cardiovascular diseases, high blood pressure, and other medical conditions like metabolic syndrome, arthritis, and even some types of cancer.
Obesity Definition
Obesity is defined by the World Health Organization as an accumulation of abnormal and excess body fat that comes with several risk factors. It is measured by the body mass index BMI, body weight (in kilograms) divided by the square of a person’s height (in meters).
Obesity in America
Obesity is on the verge of becoming an epidemic as 1 in every 3 Americans can be categorized as overweight and obese. Currently, America is an obese country, and it continues to get worse.

Paper Due? Why Suffer? That's our Job!
Causes of obesity
Do you see any obese or overweight people around you?
You likely do.
This is because fast-food chains are becoming more and more common, people are less active, and fruits and vegetables are more expensive than processed foods, thus making them less available to the majority of society. These are the primary causes of obesity.
Obesity is a disease that affects all age groups, including children and elderly people.
Now that you are familiar with the topic of obesity, writing an essay won’t be that difficult for you.
How to Write an Obesity Essay
The format of an obesity essay is similar to writing any other essay. If you need help regarding how to write an obesity essay, it is the same as writing any other essay.
Obesity Essay Introduction
The trick is to start your essay with an interesting and catchy sentence. This will help attract the reader's attention and motivate them to read further. You don’t want to lose the reader’s interest in the beginning and leave a bad impression, especially if the reader is your teacher.
A hook sentence is usually used to open the introductory paragraph of an essay in order to make it interesting. When writing an essay on obesity, the hook sentence can be in the form of an interesting fact or statistic.
Head on to this detailed article on hook examples to get a better idea.
Once you have hooked the reader, the next step is to provide them with relevant background information about the topic. Don’t give away too much at this stage or bombard them with excess information that the reader ends up getting bored with. Only share information that is necessary for the reader to understand your topic.
Next, write a strong thesis statement at the end of your essay, be sure that your thesis identifies the purpose of your essay in a clear and concise manner. Also, keep in mind that the thesis statement should be easy to justify as the body of your essay will revolve around it.
Body Paragraphs
The details related to your topic are to be included in the body paragraphs of your essay. You can use statistics, facts, and figures related to obesity to reinforce your thesis throughout your essay.
If you are writing a cause-and-effect obesity essay, you can mention different causes of obesity and how it can affect a person’s overall health. The number of body paragraphs can increase depending on the parameters of the assignment as set forth by your instructor.
Start each body paragraph with a topic sentence that is the crux of its content. It is necessary to write an engaging topic sentence as it helps grab the reader’s interest. Check out this detailed blog on writing a topic sentence to further understand it.
End your essay with a conclusion by restating your research and tying it to your thesis statement. You can also propose possible solutions to control obesity in your conclusion. Make sure that your conclusion is short yet powerful.
Obesity Essay Examples
Essay about Obesity (PDF)
Childhood Obesity Essay (PDF)
Obesity in America Essay (PDF)
Essay about Obesity Cause and Effects (PDF)
Satire Essay on Obesity (PDF)
Obesity Argumentative Essay (PDF)
Obesity Essay Topics
Choosing a topic might seem an overwhelming task as you may have many ideas for your assignment. Brainstorm different ideas and narrow them down to one, quality topic.
If you need some examples to help you with your essay topic related to obesity, dive into this article and choose from the list of obesity essay topics.
Childhood Obesity
As mentioned earlier, obesity can affect any age group, including children. Obesity can cause several future health problems as children age.
Here are a few topics you can choose from and discuss for your childhood obesity essay:
- What are the causes of increasing obesity in children?
- Obese parents may be at risk for having children with obesity.
- What is the ratio of obesity between adults and children?
- What are the possible treatments for obese children?
- Are there any social programs that can help children with combating obesity?
- Has technology boosted the rate of obesity in children?
- Are children spending more time on gadgets instead of playing outside?
- Schools should encourage regular exercises and sports for children.
- How can sports and other physical activities protect children from becoming obese?
- Can childhood abuse be a cause of obesity among children?
- What is the relationship between neglect in childhood and obesity in adulthood?
- Does obesity have any effect on the psychological condition and well-being of a child?
- Are electronic medical records effective in diagnosing obesity among children?
- Obesity can affect the academic performance of your child.
- Do you believe that children who are raised by a single parent can be vulnerable to obesity?
- You can promote interesting exercises to encourage children.
- What is the main cause of obesity, and why is it increasing with every passing day?
- Schools and colleges should work harder to develop methodologies to decrease childhood obesity.
- The government should not allow schools and colleges to include sweet or fatty snacks as a part of their lunch.
- If a mother is obese, can it affect the health of the child?
- Children who gain weight frequently can develop chronic diseases.
Obesity Argumentative Essay Topics
Do you want to write an argumentative essay on the topic of obesity?
The following list can help you with that!
Here are some examples you can choose from for your argumentative essay about obesity:
- Can vegetables and fruits decrease the chances of obesity?
- Should you go for surgery to overcome obesity?
- Are there any harmful side effects?
- Can obesity be related to the mental condition of an individual?
- Are parents responsible for controlling obesity in childhood?
- What are the most effective measures to prevent the increase in the obesity rate?
- Why is the obesity rate increasing in the United States?
- Can the lifestyle of a person be a cause of obesity?
- Does the economic situation of a country affect the obesity rate?
- How is obesity considered an international health issue?
- Can technology and gadgets affect obesity rates?
- What can be the possible reasons for obesity in a school?
- How can we address the issue of obesity?
- Is obesity a chronic disease?
- Is obesity a major cause of heart attacks?
- Are the junk food chains causing an increase in obesity?
- Do nutritional programs help in reducing the obesity rate?
- How can the right type of diet help with obesity?
- Why should we encourage sports activities in schools and colleges?
- Can obesity affect a person’s behavior?
Health Related Topics for Research Paper
If you are writing a research paper, you can explain the cause and effect of obesity.
Here are a few topics that link to the cause and effects of obesity.Review the literature of previous articles related to obesity. Describe the ideas presented in the previous papers.
- Can family history cause obesity in future generations?
- Can we predict obesity through genetic testing?
- What is the cause of the increasing obesity rate?
- Do you think the increase in fast-food restaurants is a cause of the rising obesity rate?
- Is the ratio of obese women greater than obese men?
- Why are women more prone to be obese as compared to men?
- Stress can be a cause of obesity. Mention the reasons how mental health can be related to physical health.
- Is urban life a cause of the increasing obesity rate?
- People from cities are prone to be obese as compared to people from the countryside.
- How obesity affects the life expectancy of people? What are possible solutions to decrease the obesity rate?
- Do family eating habits affect or trigger obesity?
- How do eating habits affect the health of an individual?
- How can obesity affect the future of a child?
- Obese children are more prone to get bullied in high school and college.
- Why should schools encourage more sports and exercise for children?
Tough Essay Due? Hire Tough Writers!
Topics for Essay on Obesity as a Problem
Do you think a rise in obesity rate can affect the economy of a country?
Here are some topics for your assistance regarding your economics related obesity essay.
- Does socioeconomic status affect the possibility of obesity in an individual?
- Analyze the film and write a review on “Fed Up” – an obesity epidemic.
- Share your reviews on the movie “The Weight of The Nation.”
- Should we increase the prices of fast food and decrease the prices of fruits and vegetables to decrease obesity?
- Do you think healthy food prices can be a cause of obesity?
- Describe what measures other countries have taken in order to control obesity?
- The government should play an important role in controlling obesity. What precautions should they take?
- Do you think obesity can be one of the reasons children get bullied?
- Do obese people experience any sort of discrimination or inappropriate behavior due to their weight?
- Are there any legal protections for people who suffer from discrimination due to their weight?
- Which communities have a higher percentage of obesity in the United States?
- Discuss the side effects of the fast-food industry and their advertisements on children.
- Describe how the increasing obesity rate has affected the economic condition of the United States.
- What is the current percentage of obesity all over the world? Is the obesity rate increasing with every passing day?
- Why is the obesity rate higher in the United States as compared to other countries?
- Do Asians have a greater percentage of obese people as compared to Europe?
- Does the cultural difference affect the eating habits of an individual?
- Obesity and body shaming.
- Why is a skinny body considered to be ideal? Is it an effective way to reduce the obesity rate?
Obesity Solution Essay Topics
With all the developments in medicine and technology, we still don’t have exact measures to treat obesity.
Here are some insights you can discuss in your essay:
- How do obese people suffer from metabolic complications?
- Describe the fat distribution in obese people.
- Is type 2 diabetes related to obesity?
- Are obese people more prone to suffer from diabetes in the future?
- How are cardiac diseases related to obesity?
- Can obesity affect a woman’s childbearing time phase?
- Describe the digestive diseases related to obesity.
- Obesity may be genetic.
- Obesity can cause a higher risk of suffering a heart attack.
- What are the causes of obesity? What health problems can be caused if an individual suffers from obesity?
- What are the side effects of surgery to overcome obesity?
- Which drugs are effective when it comes to the treatment of obesity?
- Is there a difference between being obese and overweight?
- Can obesity affect the sociological perspective of an individual?
- Explain how an obesity treatment works.
- How can the government help people to lose weight and improve public health?
Writing an essay is a challenging yet rewarding task. All you need is to be organized and clear when it comes to academic writing.
- Choose a topic you would like to write on.
- Organize your thoughts.
- Pen down your ideas.
- Compose a perfect essay that will help you ace your subject.
- Proofread and revise your paper.
Were the topics useful for you? We hope so!
However, if you are still struggling to write your paper, you can pick any of the topics from this list, and our essay writer will help you craft a perfect essay.
Are you struggling to write an effective essay?
If writing an essay is the actual problem and not just the topic, you can always hire an essay writing service for your help. Essay experts at 5StarEssays can help compose an impressive essay within your deadline.
All you have to do is contact us. We will get started on your paper while you can sit back and relax.
Place your order now to get an A-worthy essay.

Marketing, Thesis
As a Digital Content Strategist, Nova Allison has eight years of experience in writing both technical and scientific content. With a focus on developing online content plans that engage audiences, Nova strives to write pieces that are not only informative but captivating as well.
Was This Blog Helpful?
Keep reading.
- How to Write A Bio – Professional Tips and Examples

- Learn How to Write an Article Review with Examples

- How to Write a Poem Step-by-Step Like a Pro

- How To Write Poetry - 7 Fundamentals and Tips

- Know About Appendix Writing With the Help of Examples

- List of Social Issues Faced By the World

- How To Write A Case Study - Easy Guide

- Learn How to Avoid Plagiarism in 7 Simple Steps

- Writing Guide of Visual Analysis Essay for Beginners

- Learn How to Write a Personal Essay by Experts

- Character Analysis - A Step By Step Guide

- Thematic Statement: Writing Tips and Examples

- Expert Guide on How to Write a Summary

- How to Write an Opinion Essay - Structure, Topics & Examples

- How to Write a Synopsis - Easy Steps and Format Guide

- Learn How To Write An Editorial By Experts

- How to Get Better at Math - Easy Tips and Tricks

- How to Write a Movie Review - Steps and Examples

- Creative Writing - Easy Tips For Beginners

- Types of Plagiarism Every Student Should Know

People Also Read
- descriptive essay topics
- essay format
- synthesis essay writing
- types of autobiography
- literary analysis essay topics
Burdened With Assignments?
Advertisement
- Homework Services: Essay Topics Generator
© 2024 - All rights reserved

Prevention, prevention, prevention.
Losing weight is hard to do.
In the U.S., only one in six adults who have dropped excess pounds actually keep off at least 10 percent of their original body weight. The reason: a mismatch between biology and environment. Our bodies are evolutionarily programmed to put on fat to ride out famine and preserve the excess by slowing metabolism and, more important, provoking hunger. People who have slimmed down and then regain their weight don’t lack willpower—their bodies are fighting them every inch of the way.
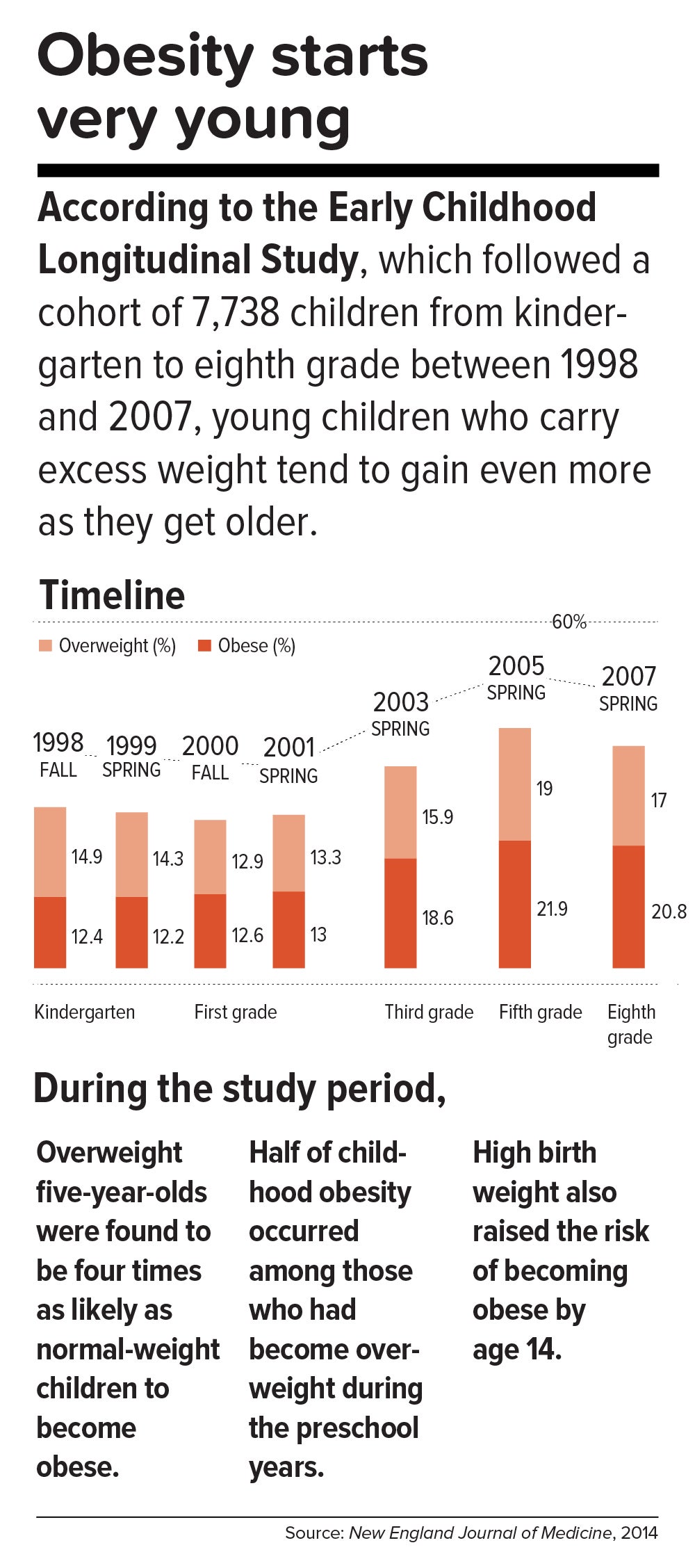
This inborn predisposition to hold on to added weight reverberates down the life course. Few children are born obese, but once they become heavy, they are usually destined to be heavy adolescents and heavy adults. According to a 2016 study in the New England Journal of Medicine , approximately 90 percent of children with severe obesity will become obese adults with a BMI of 35 or higher. Heavy young adults are generally heavy in middle and old age. Obesity also jumps across generations; having a mother who is obese is one of the strongest predictors of obesity in children.
All of which means that preventing child obesity is key to stopping the epidemic. By the time weight piles up in adulthood, it is usually too late. Luckily, preventing obesity in children is easier than in adults, partly because the excess calories they absorb are minimal and can be adjusted by small changes in diet—substituting water, for example, for sugary fruit juices or soda.
Still, the bulk of the obesity problem—literally—is in adults. According to Frank Hu, chair of the Harvard Chan Department of Nutrition, “Most people gain weight during young and middle adulthood. The weight-gain trajectory is less than 1 pound per year, but it creeps up steadily from age 18 to age 55. During this time, people gain fat mass, not muscle mass. When they reach age 55 or so, they begin to lose their existing muscle mass and gain even more fat mass. That’s when all the metabolic problems appear: insulin resistance, high cholesterol, high blood pressure.”
Adds Walter Willett, Frederick John Stare Professor of Epidemiology and Nutrition at Harvard Chan, “The first 5 pounds of weight gain at age 25—that’s the time to be taking action. Because someone is on a trajectory to end up being 30 pounds overweight by the time they’re age 50.”
The most realistic near-term public health goal, therefore, is not to reverse but rather to slow down the trend—and even this will require strong commitment from government at many levels. In May 2017, the Trump administration rolled back recently-enacted standards for school meals, delaying a rule to lower sodium and allowing waivers for regulations requiring cafeterias to serve foods rich in whole grains. If recent expansions in food entitlements and school meals are undermined, “It would be a ‘disaster,’ to use the president’s word,” says Marlene Schwartz, director of the Rudd Center for Obesity & Food Policy at the University of Connecticut. “The federal food programs are incredibly important, not just because of the food and money they provide families, but because supporting better nutrition in child care, schools, and the WIC [Women, Infants, and Children] program has created new social norms. We absolutely cannot undo the progress that we’ve made in helping this generation transition to a healthier diet.”
Get the science right.
It is impossible to prescribe solutions to obesity without reminding ourselves that nutrition scientists botched things decades ago and probably sent the epidemic into overdrive. Beginning in the 1970s, the U.S. government and major professional groups recommended for the first time that people eat a low-fat/high-carbohydrate diet. The advice was codified in 1977 with the first edition of The Dietary Goals for the United States , which aimed to cut diet-related conditions such as heart disease and diabetes. What ensued amounted to arguably the biggest public health experiment in U.S. history, and it backfired.
At the time, saturated fat and dietary cholesterol were believed to be the main factors responsible for cardiovascular disease—an oversimplified theory that ignored the fact that not all fats are created equal. Soon, the public health blitz against saturated fat became a war on all fat. In the American diet, fat calories plummeted and carb calories shot up.
“We can’t blame industry for this. It was a bandwagon effect in the scientific community, despite the lack of evidence—even with evidence to the contrary,” says Willett. “Farmers have known for thousands of years that if you put animals in a pen, don’t let them run around, and load them up with grains, they get fat. That’s basically what has been happening to people: We created the great American feedlot. And we added in sugar, coloring, and seductive promotion for low-fat junk food.”
Scientists now know that whole fruits and vegetables (other than potatoes), whole grains, high-quality proteins (such as from fish, chicken, beans, and nuts), and healthy plant oils (such as olive, peanut, or canola oil) are the foundations of a healthy diet.
But there is also a lot scientists don’t yet know. One unanswered question is why some people with obesity are spared the medical complications of excess weight. Another concerns the major mechanisms by which obesity ushers in disease. Although surplus body weight can itself directly cause problems—such as arthritis due to added load on joints, or breast cancer caused by hormones secreted by fat cells—in general, obesity triggers myriad biological processes. Many of the resulting conditions—such as atherosclerosis, diabetes, and even Alzheimer’s disease—are mediated by inflammation, in which the body’s immune response becomes damagingly self-perpetuating. In this sense, today’s food system is as inflammagenic as it is obesigenic.
Scientists also need to ferret out the nuanced effects of particular foods. For example, do fermented products—such as yogurt, tempeh, or sauerkraut—have beneficial properties? Some studies have found that yogurt protects against weight gain and diabetes, and suggest that healthy live bacteria (known as probiotics) may play a role. Other reports point to fruits being more protective than vegetables in weight control and diabetes prevention, although the types of fruits and vegetables make a difference.
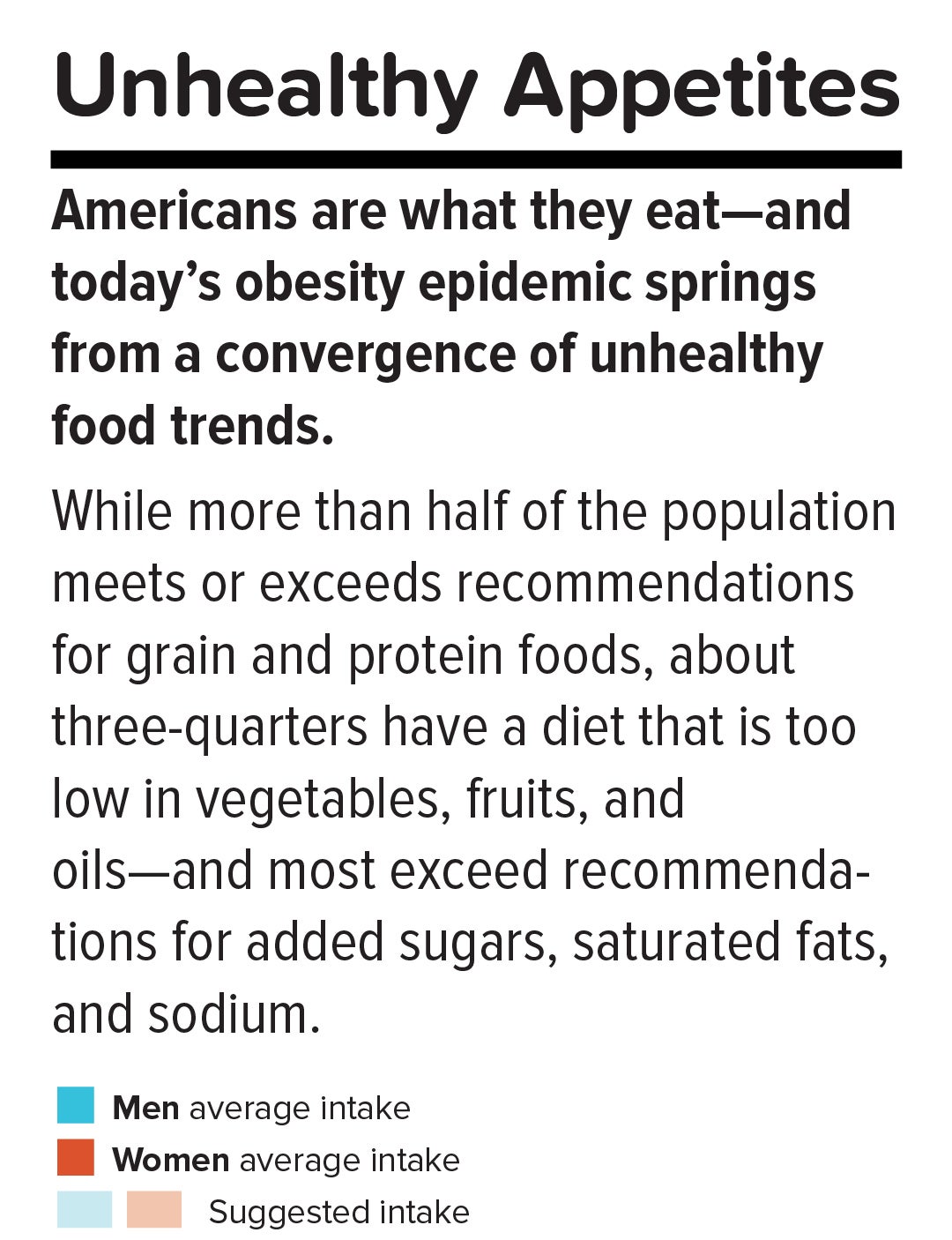
A 2017 article in the American Journal of Clinical Nutrition showed that substituting whole grains for refined grains led to a loss of nearly 100 calories a day—by speeding up metabolism, cutting the number of calories that the body hangs on to, and, more surprisingly, by changing the digestibility of other foods on the plate. That extra energy lost daily—by substituting, say, brown rice for white rice or barley for pita bread—was equivalent to a brisk 30-minute walk. One hundred calories a day, sustained over years, and multiplied by the population is one mathematical equivalent of the obesity epidemic.
A companion study found that adults who ate a whole-grain-rich diet developed healthier gut bacteria and improved immune responses. That particular foods alter the gut microbiome—the dense and vital community of bacteria and other microorganisms that work symbiotically with the body’s own digestive system—is another critical insight. The microbiome helps determine weight by controlling how our bodies extract calories and store fat in the liver, and the microbiomes of obese individuals are startlingly efficient at harvesting calories from food. [To learn more about Harvard Chan research on the gut microbiome, read “ Bugs in the System .”] The hormonal effects of sleep deprivation and stress—two epidemics concurrent and intertwined with the obesity trend—are other promising avenues of research.
And then there are the mystery factors. One recent hypothesis is that an agent known as adenovirus 36 partly accounts for our collective heft. A 2010 article in The Royal Society described a study in which researchers examined samples of more than 20,000 animals from eight species living with or around humans in industrialized nations, a menagerie that included macaques, chimpanzees, vervets, marmosets, lab mice and rats, feral rats, and domestic dogs and cats. Like their Homo sapiens counterparts, all of the study populations had gained weight over the past several decades—wild, domestic, and lab animals alike. The chance that this is a coincidence is, according to the scientists’ estimate, 1 in 10 million. The stumped authors surmise that viruses, gene expression changes, or “as-of-yet unidentified and/or poorly understood factors” are to blame.
Master the art of persuasion.
A 2015 paper in the American Journal of Public Health revealed the philosophical chasm that hampers America’s progress on obesity prevention. It found that 72 to 98 percent of obesity-related media reports emphasize personal responsibility for weight, compared with 40 percent of scientific papers.
A recent study by Drexel University researchers also quantified the political polarization around public health measures. From 1998 through 2013, Democrats voted in line with recommendations from the American Public Health Association 88.3 percent of the time, on average, while Republicans voted for the proposals just 21.3 percent of the time.
Clearly, we can’t count on bipartisan goodwill to stem the obesity crisis. But we can ask what kinds of messages appeal to politically divergent audiences. A stealth strategy may be to avoid even uttering the word “obesity.” On January 1 of this year, Philadelphia’s 1.5-cents-per-ounce excise tax on sugar-sweetened and diet beverages took effect. When Philadelphia Mayor Jim Kenney lobbied voters to approve the tax, his bid centered not on improving health—the unsuccessful pitch of his predecessor—but on raising $91 million annually for prekindergarten programs.
“That’s something lots of people care about and can get behind—it’s a feel-good policy, and it makes sense,” says psychologist Christina Roberto, assistant professor of medical ethics and health policy at the University of Pennsylvania, and a former assistant professor of social and behavioral sciences and nutrition at Harvard Chan. The provision for taxing diet beverages was also shrewd, she adds, because it spread the tax’s pain; since wealthier people are more likely than less-affluent individuals to buy diet drinks, the tax could not be slapped with the label “regressive.”
But Roberto sees a larger lesson in the Philadelphia story. Public health messaging that appeals to values that transcend the individual is less fraught, less stigmatizing, and perhaps more effective. As she puts it, “It’s very different to hear the message, ‘Eat less red meat, help the planet’ versus ‘Eat less red meat, help yourself avoid saturated fat and cardiovascular disease.’”
Supermarket makeovers
Supermarket aisles are other places where public health can shuffle a deck stacked against healthy consumer choices.
With slim profit margins and 50,000-plus products on their shelves, grocery stores depend heavily on food manufacturers’ promotional incentives to make their bottom lines. “Manufacturers pay slotting fees to get their products on the shelf, and they pay promotion allowances: We’ll give you this much off a carton of Coke if you put it on sale for a certain price or if you put it on an end-of-aisle display,” says José Alvarez, former president and chief executive officer of Stop & Shop/Giant-Landover, now senior lecturer of business administration at Harvard Business School. Such promotional payments, Alvarez adds, often exceed retailers’ net profits.
Healthy new products—like flash-frozen dinners prepared with heaps of vegetables and whole grains, and relatively little salt—can’t compete for prized shelf space against boxed mac and cheese or cloying breakfast cereals. One solution, says Alvarez, is for established consumer packaged goods companies to buy out what he calls the “hippie in the basement” firms that have whipped up more nutritious items. The behemoths could apply their production, marketing, and distribution prowess to the new offerings—and indeed, this has started to happen over the last five years.
Another approach is to make nutritious foods more convenient to eat. “We have all of these cooking shows and upscale food magazines, but most people don’t have the time or inclination—or the skills, quite frankly—to cook,” says Alvarez. “Instead, we should focus on creating high-quality, healthy, affordable prepared foods.”
An additional model is suggested by Jeff Dunn, a 20-year veteran of the soft drink industry and former president of Coca-Cola North America, who went on to become an advocate for fresh, healthy food. Dunn served as president and chief executive officer of Bolthouse Farms from 2008 to 2015, where he dramatically increased sales of baby carrots by using marketing techniques common in the junk food business. “We operated on the principles of the three 3 A’s: accessibility, availability, and affordability,” says Dunn. “That, by the way, is Coke’s more-than-70-year-old formula for success.”
Show them the money.
Obesity kills budgets. According to the Campaign to End Obesity, a collaboration of leaders from industry, academia, public health, and policymakers, annual U.S. health costs related to obesity approach $200 billion. In 2010, the nonpartisan Congressional Budget Office reported that nearly 20 percent of the rise in health care spending from 1987 to 2007 was linked to obesity. And the U.S. Centers for Disease Control and Prevention (CDC) found that full-time workers in the U.S. who are overweight or obese and have other chronic health conditions miss an estimated 450 million more days of work each year than do healthy employees—upward of $153 billion in lost productivity annually.
But making the money case for obesity prevention isn’t straightforward. For interventions targeting children and youth, only a small fraction of savings is captured in the first decade, since most serious health complications don’t emerge for many years. Long-term obesity prevention, in other words, doesn’t fit into political timetables for elected officials.
Yet lawmakers are keen to know how “best for the money” obesity-prevention programs can help them in the short run. Over the past two years, Harvard Chan’s Steve Gortmaker and his colleagues have been working with state health departments in Alaska, Mississippi, New Hampshire, Oklahoma, Washington, and West Virginia and with the city of Philadelphia and other locales, building cost-effectiveness models using local data for a wide variety of interventions—from improved early child care to healthy school environments to communitywide campaigns. “We collaborate with health departments and community stakeholders, provide them with the evidence base, help assess how much different options cost, model the results over a decade, and they pick what they want to work on. One constant that we’ve seen—and these are very different political environments—is a strong interest in cost-effectiveness,” he says.
In a 2015 study in Health Affairs , Gortmaker and colleagues outlined three interventions that would more than pay for themselves: an excise tax on sugar-sweetened beverages implemented at the state level; elimination of the tax subsidy for advertising unhealthy food to children; and strong nutrition standards for food and drinks sold in schools outside of school meals. Implemented nationally, these interventions would prevent 576,000, 129,100, and 345,000 cases of childhood obesity, respectively, by 2025. The projected net savings to society in obesity-related health care costs for each dollar invested: $31, $33, and $4.60, respectively.
Gortmaker is one of the leaders of a collaborative modeling effort known as CHOICES—for Childhood Obesity Intervention Cost-Effectiveness Study—an acronym that seems a pointed rebuttal to the reflexive conservative argument that government regulation tramples individual choice. Having grown up not far from Des Plaines, Illinois, site of the first McDonald’s franchise in the country, he emphasizes to policymakers that at this late date, America cannot treat its way out of obesity, given current medical know-how. Only a thoroughgoing investment in prevention will turn the tide. “Clinical interventions produce too small an effect, with too small a population, and at high cost,” Gortmaker says. “The good news is that there are many cost-effective options to choose from.”
While Gortmaker underscores the importance of improving both food choices and options for physical activity, he has shown that upgrading the food environment offers much more benefit for the buck. This is in line with the gathering scientific consensus that what we eat plays a greater role in obesity than does sedentary lifestyle (although exercise protects against many of the metabolic consequences of excess weight). “The easiest way to explain it,” Gortmaker says, “is to talk about a sugary beverage—140 calories. You could quickly change a kid’s risk of excess energy balance by 140 calories a day just by switching from a sugary drink a day to water or sparkling water. But for a 10-year-old boy to burn an extra 140 calories, he’d have to replace an hour-and-a-half of sitting with an hour-and-a-half of walking.”
Small tweaks in adults’ diets can likewise make a big difference in short order. “With adults, health care costs rise rapidly with excess weight gain,” Gortmaker says. “If you can slow the onset of obesity, you slow the onset of diabetes, and potentially not only save health care costs but also boost people’s productivity in the workforce.”
One of Gortmaker’s most intriguing calculations spins off of the food industry’s estimated $633 million spent on television marketing aimed at kids. Currently, federal tax treatment of advertising as an ordinary business expense means that the government, in effect, subsidizes hawking of junk food to children. Gortmaker modeled a national intervention that would eliminate this subsidy of TV ads for nutritionally empty foods and beverages aimed at 2- to 19-year-olds. Drawing on well-delineated relationships between exposure to these advertisements and subsequent weight gain, he found that the intervention would save $260 million in downstream health care costs. Although the effect would probably be small at the individual level, it would be significant at the population level.
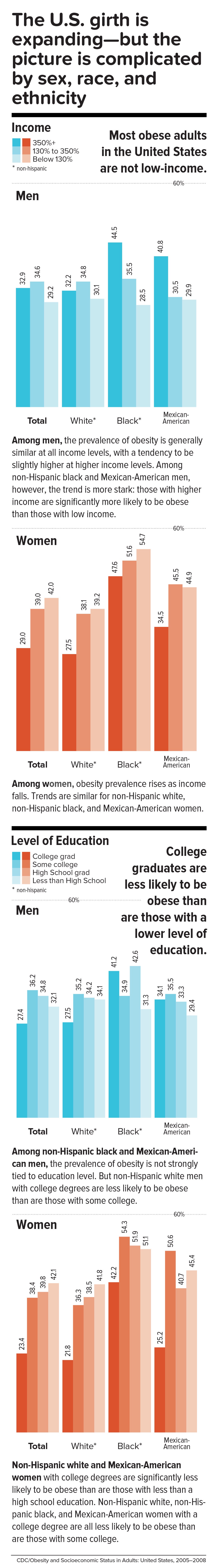
Level the playing field through taxes and regulation.
When public health took on cigarette smoking, starting in the 1960s, it did so with robust policies banning television ads and other marketing, raising taxes to increase prices, making public places smoke-free, and offering people treatment such as the nicotine patch. In 1965, the smoking rate for U.S. adults was 42.2 percent; today, it is 16.8 percent.
Similarly, America reduced the rate of deaths caused by motor vehicle accidents—a 90 percent decrease over the 20th century, according to the CDC—with mandatory seat belt laws, safer car designs, stop signs, speed limits, rumble strips, and the stigmatization of drunk driving.
Change the product. Change the environment. Change the culture. That is also the policy recipe for stopping obesity.
Laws that make healthy behaviors easier are often followed by positive changes in those behaviors. And people who are trying to adopt healthy behaviors tend to support policies that make their personal aspirations achievable, which in turn nudges lawmakers to back the proposals.
One debate today revolves around whether recipients of federal Supplemental Nutrition Assistance Program (SNAP) benefits (formerly known as food stamps) should be restricted from buying sodas or junk food. The largest component of the USDA budget, SNAP feeds one in seven Americans. A USDA report, issued last November, found that the number-one purchase by SNAP households was sweetened beverages, a category that included soft drinks, fruit juices, energy drinks, and sweetened teas, accounting for nearly 10 percent of SNAP money spent on food. Is the USDA therefore underwriting the soda industry and planting the seeds for chronic disease that the government will pay to treat years down the line?
Eric Rimm, a professor in the Departments of Epidemiology and Nutrition at the Harvard Chan School, frames the issue differently. In a 2017 study in the American Journal of Preventive Medicine , he and his colleagues asked SNAP participants whether they would prefer the standard benefits package or a “SNAP-plus” that prohibited the purchase of sugary beverages but offered 50 percent more money for buying fruits and vegetables. Sixty-eight percent of the participants chose the healthy SNAP-plus option.
“A lot of work around SNAP policy is done by academics and politicians, without reaching out to the beneficiaries,” says Rimm. “We haven’t asked participants, ‘What’s your say in this? How can we make this program better for you?’” To be sure, SNAP is riddled with nutritional contradictions. Under current rules, for example, participants can use benefits to buy a 12-pack of Pepsi or a Snickers bar or a giant bag of Lay’s potato chips but not real food that happens to be heated, such as a package of rotisserie chicken. “This is the most vulnerable population in the country,” says Rimm. “We’re not listening well enough to our constituency.”
Other innovative fiscal levers to alter behavior could also drive down obesity. In 2014, a trio of strong voices on food industry practices—Dariush Mozaffarian, DrPH ’06, dean of Tufts University’s Friedman School of Nutrition Science and Policy and former associate professor of epidemiology at the Harvard Chan School; Kenneth Rogoff, professor of economics at Harvard; and David Ludwig, professor in the Department of Nutrition at Harvard Chan and a physician at Boston Children’s Hospital—broached the idea of a “meaningful” tax on nearly all packaged retail foods and many chain restaurants, with the proceeds used to pay for minimally processed foods and healthier meals for school kids. In essence, the tax externalizes the social costs of harmful individual behavior.
“We made a straightforward proposal to tax all processed foods and then use the income to subsidize whole foods in a short-term, revenue-neutral way,” explains Ludwig. “The power of this idea is that, since there is so much processed food consumption, even a modest tax—in the 10 to 15 percent range—is not going to greatly inflate the cost of these foods. Their price would increase moderately, but the proceeds would not disappear into government coffers. Instead, the revenue would make healthy foods affordable for virtually the entire population, and the benefits would be immediately evident. Yes, people will pay moderately more for their Coke or for their cinnamon bear claw but a lot less for nourishing, whole foods.”
Another suggestion comes from Sandro Galea, dean of the Boston University School of Public Health, and Abdulrahman M. El-Sayed, a public health physician and epidemiologist. In a 2015 issue of the American Journal of Public Health , they called for “calorie offsets,” similar to the carbon offsets used to mitigate environmental harm caused by the gas and oil industries. A “calorie offset” scheme could hand the food and beverage industries a chance at redemption by inviting them to invest in such undertakings as city farms, cooking classes for parents, healthy school cafeterias, and urban green spaces.
These ambitious proposals face almost impossibly high hurdles. Political battle lines typically pit public health against corporations, with Big Food casting doubt on solid nutrition science, deeming government regulation a threat to free choice, and making self-policing pledges that it has never kept. On the website for the Americans for Food and Beverage Choice, a group spearheaded by the American Beverage Association, is the admonition: “[W]hether it’s at a restaurant or in a grocery store, it’s never the government’s job to decide what you choose to eat and drink.”
Yet surprisingly, many public health professionals are convinced that the only way to stop obesity is to make common cause with the food industry. “This isn’t like tobacco, where it’s a fight to the death. We need the food industry to make healthier food and to make a profit,” says Mozaffarian. “The food industry is much more diverse and heterogeneous than tobacco or even cars. As long as we can help them—through carrots and sticks, tax incentives and disincentives—to move towards healthier products, then they are part of the solution. But we have to be vigilant, because they use a lot of the same tactics that tobacco did.”
Sow what we want to reap.
Americans overeat what our farmers overproduce.
“The U.S. food system is egregiously terrible for human and planetary health,” says Walter Willett. It’s so terrible, Willett made a pie chart of American grain production consumed domestically. It shows that most of the country’s agricultural land goes to the two giant commodity crops: corn and soy. Most of those crops, in turn, go to animal fodder and ethanol, and are also heavily used in processed snack foods. Today, only about 10 percent of grain grown in the U.S. for domestic use is eaten directly by human beings. According to a 2013 report from the Union of Concerned Scientists, only 2 percent of U.S. farmland is used to grow fruits and vegetables, while 59 percent is devoted to commodity crops.
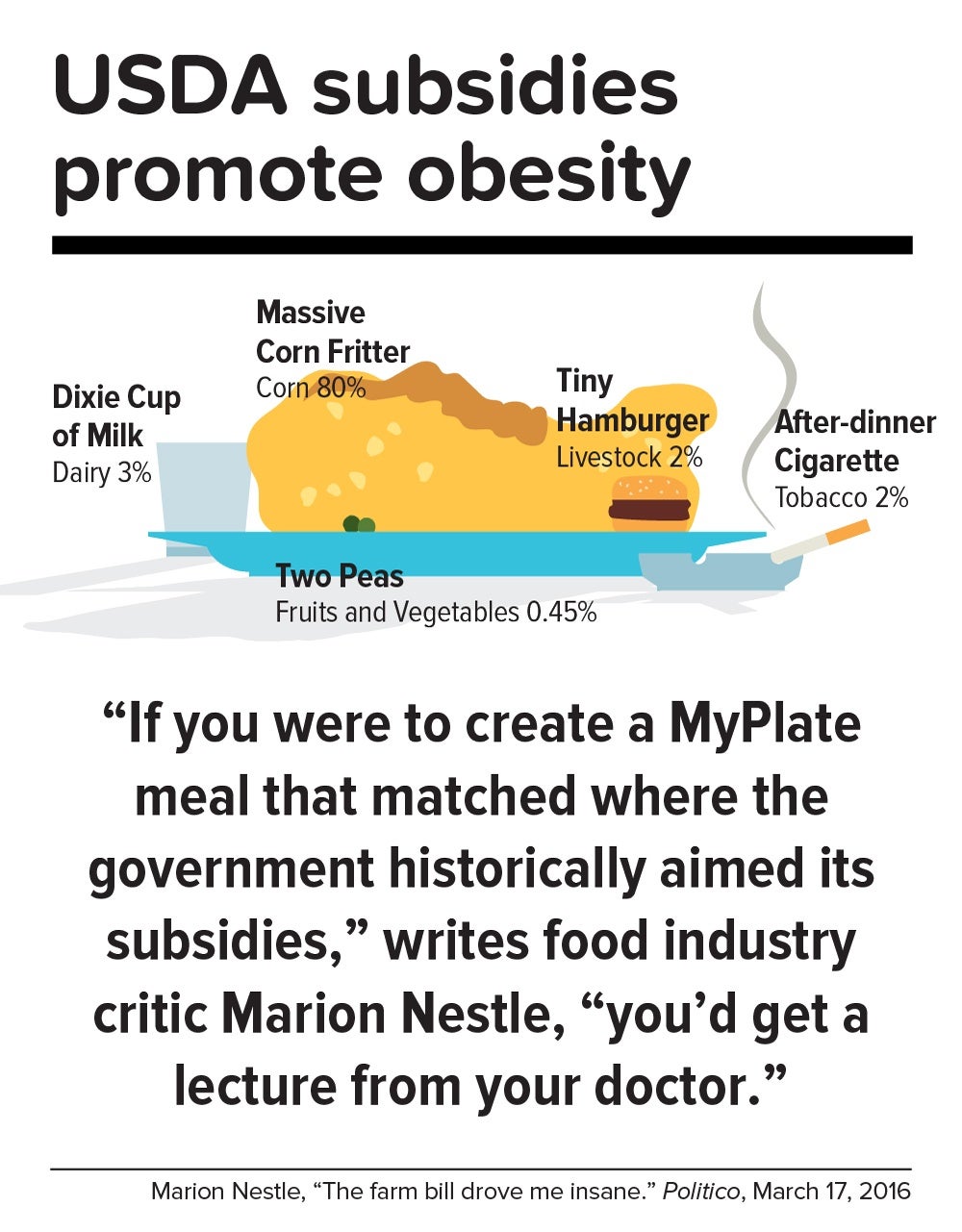
Historically, those skewed proportions made sense. Federal food policies, drafted with the goal of alleviating hunger, preferentially subsidize corn and soy production. And whereas corn or soybeans could be shipped for days on a train, fruits and vegetables had to be grown closer to cities by truck farmers so the produce wouldn’t spoil. But those long-ago constraints don’t explain today’s upside-down agricultural priorities.
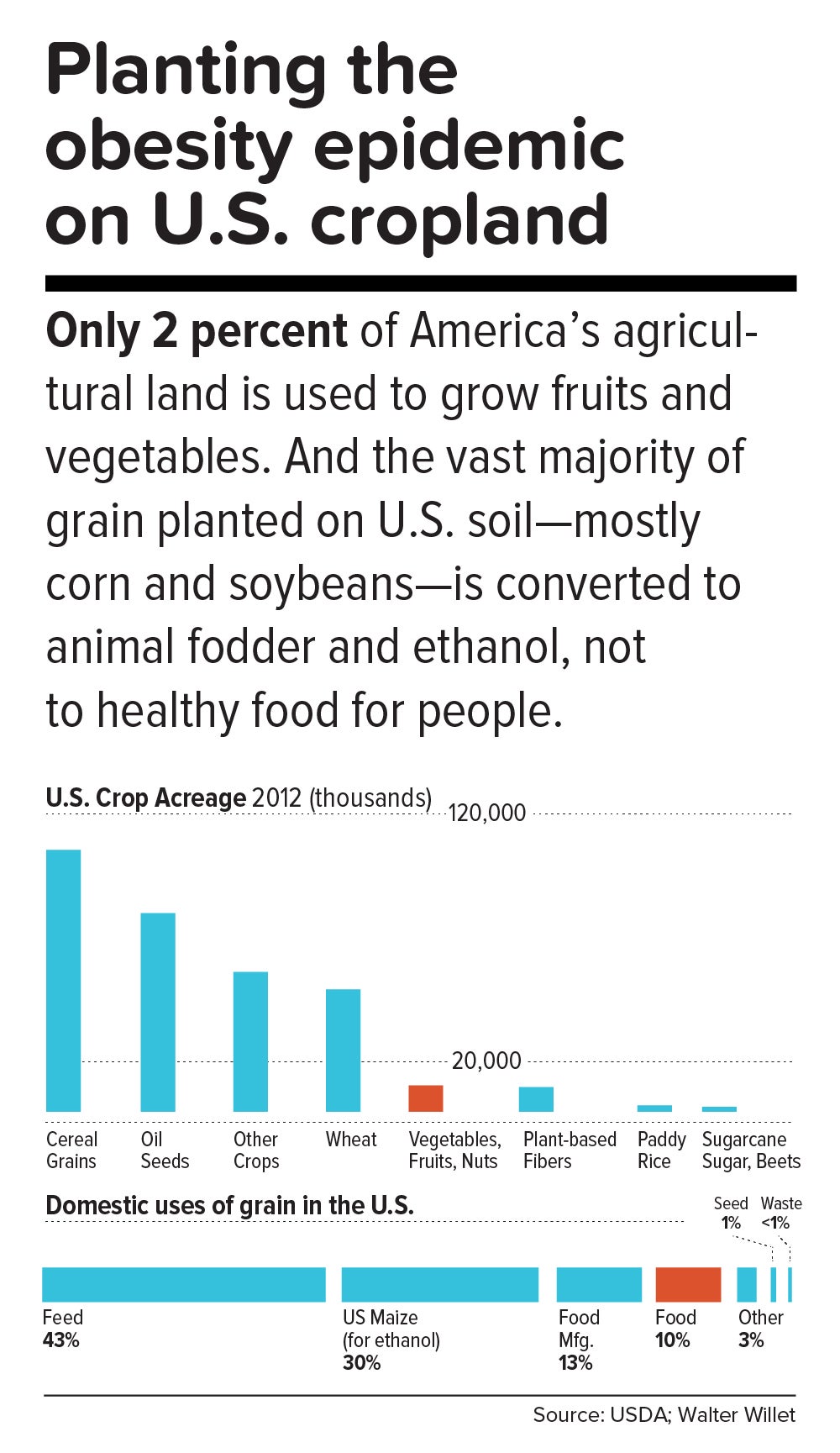
In a now-classic 2016 Politico article titled “The farm bill drove me insane,” Marion Nestle illustrated the irrational gap between what the government recommends we eat and what it subsidizes: “If you were to create a MyPlate meal that matched where the government historically aimed its subsidies, you’d get a lecture from your doctor. More than three-quarters of your plate would be taken up by a massive corn fritter (80 percent of benefits go to corn, grains and soy oil). You’d have a Dixie cup of milk (dairy gets 3 percent), a hamburger the size of a half dollar (livestock: 2 percent), two peas (fruits and vegetables: 0.45 percent) and an after-dinner cigarette (tobacco: 2 percent). Oh, and a really big linen napkin (cotton: 13 percent) to dab your lips.”
In this sense, the USDA marginalizes human health. Many of the foods that nutritionists agree are best for us—notably, fruits, vegetables, and tree nuts—fall under the bureaucratic rubric “specialty crops,” a category that also includes “dried fruits, horticulture, and nursery crops (including floriculture).” Farm bills, which get passed every five years or so, fortify the status quo. The 2014 Farm Bill, for example, provided $73 million for the Specialty Crop Block Grant Program in 2017, out of a total of about $25 billion for the USDA’s discretionary budget. (The next Farm Bill, now under debate, will be coming out in 2018.)
By contrast, a truly anti-obesigenic agricultural system would stimulate USDA support for crop diversity—through technical assistance, research, agricultural training programs, and financial aid for farmers who are newly planting or transitioning their land into produce. It would also enable farmers, most of whom survive on razor-thin profit margins, to make a decent living.
In the early 1970s, Finland’s death rate from coronary heart disease was the highest in the world, and in the eastern region of North Karelia—a pristine, sparsely populated frontier landscape of forest and lakes—the rate was 40 percent worse than the national average. Every family saw physically active men, loggers and farmers who were strong and lean, dying in their prime.
Thus was born the North Karelia Project, which became a model worldwide for saving lives by transforming lifestyles. The project was launched in 1972 and officially ended 25 years later. While its initial goal was to reduce smoking and saturated fat in the diet, it later resolved to increase fruit and vegetable consumption.
The North Karelia Project fulfilled all of these ambitions. When it started, for example, 86 percent of men and 82 percent of women smeared butter on their bread; by the early 2000s, only 10 percent of men and 4 percent of women so indulged. Use of vegetable oil for cooking jumped from virtually zero in 1970 to 50 percent in 2009. Fruit and vegetables, once rare visitors to the dinner plate, became regulars. Over the project’s official quarter-century existence, coronary heart disease deaths in working-age North Karelian men fell 82 percent, and life expectancy rose seven years.
The secret of North Karelia’s success was an all-out philosophy. Team members spent innumerable hours meeting with residents and assuring them that they had the power to improve their own health. The volunteers enlisted the assistance of an influential women’s group, farmers’ unions, homemakers’ organizations, hunting clubs, and church congregations. They redesigned food labels and upgraded health services. Towns competed in cholesterol-cutting contests. The national government passed sweeping legislation (including a total ban on tobacco advertising). Dairy subsidies were thrown out. Farmers were given strong incentives to produce low-fat milk, or to get paid for meat and dairy products based not on high-fat but on high-protein content. And the newly established East Finland Berry and Vegetable Project helped locals switch from dairy farming—which had made up more than two-thirds of agriculture in the region—to cultivation of cold-hardy currants, gooseberries, and strawberries, as well as rapeseed for heart-healthy canola oil.
“A mass epidemic calls for mass action,” says the project’s director, Pekka Puska, “and the changing of lifestyles can only succeed through community action. In this case, the people pulled the government—the government didn’t pull the people.”
Could the United States in 2017 learn from North Karelia’s 1970s grand experiment?
“Americans didn’t become an obese nation overnight. It took a long time—several decades, the same timeline as in individuals,” notes Frank Hu. “What were we doing over the past 20 years or 30 years, before we crossed this threshold? We haven’t asked these questions. We haven’t done this kind of soul-searching, as individuals or society as a whole.”
Today, Americans may finally be willing to take a hard look at how food figures in their lives. In a July 2015 Gallup phone poll of Americans 18 and older, 61 percent said they actively try to avoid regular soda (the figure was 41 percent in 2002); 50 percent try to avoid sugar; and 93 percent try to eat vegetables (but only 57.7 percent in 2013 reported they ate five or more servings of fruits and vegetables at least four days of the previous week).
Individual resolve, of course, counts for little in problems as big as the obesity epidemic. Most successes in public health bank on collective action to support personal responsibility while fighting discrimination against an epidemic’s victims. [To learn more about the perils of stigma against people with obesity, read “ The Scarlet F .”]
Yet many of public health’s legendary successes also took what seems like an agonizingly long time to work. Do we have that luxury?
“Right now, healthy eating in America is like swimming upstream. If you are a strong swimmer and in good shape, you can swim for a little while, but eventually you’re going to get tired and start floating back down,” says Margo Wootan, SD ’93, director of nutrition policy for the Center for Science in the Public Interest. “If you’re distracted for a second—your kid tugs on your pant leg, you had a bad day, you’re tired, you’re worried about paying your bills—the default options push you toward eating too much of the wrong kinds of food.”
But Wootan has not lowered her sights. “What we need is mobilization,” she says. “Mobilize the public to address nutrition and obesity as societal problems—recognizing that each of us makes individual choices throughout the day, but that right now the environment is stacked against us. If we don’t change that, stopping obesity will be impossible.”
The passing of power to younger generations may aid the cause. Millennials are more inclined to view food not merely as nutrition but also as narrative—a trend that leaves Duke University’s Kelly Brownell optimistic. “Younger people have been raised to care about the story of their food. Their interest is in where it came from, who grew it, whether it contributes to sustainable agriculture, its carbon footprint, and other factors. The previous generation paid attention to narrower issues, such as hunger or obesity. The Millennials are attuned to the concept of food systems.”
We are at a public health inflection point. Forty years from now, when we gaze at the high-resolution digital color photos from our own era, what will we think? Will we realize that we failed to address the obesity epidemic, or will we know that we acted wisely?
The question brings us back to the 1970s, and to Pekka Puska, the physician who directed the North Karelia Project during its quarter-century existence. Puska, now 71, was all of 27 and burning with big ideas when he signed up to lead the audacious effort. He knows the promise and the perils of idealism. “Changing the world may have been utopic,” he says, “but changing public health was possible.”
News from the School

From public servant to public health student

Exploring the intersection of health, mindfulness, and climate change

Conference aims to help experts foster health equity

Building solidarity to face global injustice
470 Obesity Essay Topic Ideas & Examples
Looking for obesity essay topics? Being a serious problem, obesity is definitely worth writing about.
Obesity: a 100 year perspective
- George A. Bray ORCID: orcid.org/0000-0001-9945-8772 1
International Journal of Obesity ( 2024 ) Cite this article
425 Accesses
23 Altmetric
Metrics details
- Biological techniques
- Health care
- Weight management
This review has examined the scientific basis for our current understanding of obesity that has developed over the past 100 plus years. Obesity was defined as an excess of body fat. Methods of establishing population and individual changes in levels of excess fat are discussed. Fat cells are important storage site for excess nutrients and their size and number affect the response to insulin and other hormones. Obesity as a reflection of a positive fat balance is influenced by a number of genetic and environmental factors and phenotypes of obesity can be developed from several perspectives, some of which have been elaborated here. Food intake is essential for maintenance of human health and for the storage of fat, both in normal amounts and in obesity in excess amounts. Treatment approaches have taken several forms. There have been numerous diets, behavioral approaches, along with the development of medications.. Bariatric/metabolic surgery provides the standard for successful weight loss and has been shown to have important effects on future health. Because so many people are classified with obesity, the problem has taken on important public health dimensions. In addition to the scientific background, obesity through publications and organizations has developed its own identity. While studying the problem of obesity this reviewer developed several aphorisms about the problem that are elaborated in the final section of this paper.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
251,40 € per year
only 20,95 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Obesity and the risk of cardiometabolic diseases

Obesity-induced and weight-loss-induced physiological factors affecting weight regain
Normal weight obesity and unaddressed cardiometabolic health risk—a narrative review
Quetelet, Adolphe Sur l’homme et le developpement de ses facultes, ou essai de physique sociale ; Paris: Bachelier, 1835 (Transl of L-A-J. A Treatise on Man and the Development of His Faculties. IN: Bray GA. The Battle of the Bulge: A History of Obesity Research . Pittsburgh: Dorrance Publishing, 2007 pp 423-36.
Bray GA. Quetelet: quantitative medicine. Obes Res. 1994;2:68–71.
Article CAS PubMed Google Scholar
Bray GA. Beyond BMI. Nutrients. 2023;15:2254.
Article PubMed PubMed Central Google Scholar
Flegal KM. Use and misuse of BMI categories. AMA J Ethics. 2023;25:E550–8.
Article PubMed Google Scholar
Keys A, Fidanza F, Karvonen MJ, Kimura N, Taylor HL. Indices of relative weight and obesity. J Chr Diseases. 1972;25:329–43.
Article CAS Google Scholar
Bray GA. Definition, measurement, and classification of the syndromes of obesity. Int J Obes. 1978;2:99–112.
CAS PubMed Google Scholar
Garrow JS. Treat Obesity Seriouslv-A Clinical Manual . Edinburgh: Churchill Livingstone; 1981.
Rodgers A, Woodward A, Swinburn B, Dietz WH. Prevalence trends tell us what did not precipitate the US obesity epidemic. Lancet Public Health. 2018;3:e162–3.
Bray GA. Body fat distribution and the distribution of scientific knowledge. Obes Res. 1996;4:189–92.
Janssen I, Katzmarzyk PT, Ross R. Waist circumference and not body mass index explains obesity-related health risk. Am J Clin Nutr. 2004;79:379–84.
Weeks RW. An experiment with the specialized investigation. Actuar Soc Am Trans. 1904;8:17–23.
Google Scholar
Vague J. La differenciation sexuelle facteur determinant des formes de l’obesite, Presse Medicale. 1947;55:339 340. [Translated. IN: Bray GA. The Battle of the Bulge: A History of Obesity Research . Pittsburgh: Dorrance Publishing, 2007 pp 693–5].
Vague J. The degree of masculine differentiation of obesities: a factor determining predisposition to diabetes, atherosclerosis, gout, and uric calculous disease. Am J Clin Nutr. 1956;4:20–34.
Larsson B, Svardsudd K, Welin L, Wihelmsen L, Bjorntorp P, Tibbllne G. Abdominal adipose tissue distribution, obesity and risk of cardiovascular disease and death: 13 year follow up of participants in the study of 792 men born in 1913. BMJ 1984;288:1401–4.
Article CAS PubMed PubMed Central Google Scholar
Bjorntorp P. Visceral obesity: a “civilization syndrome. Obes Res. 1993;1:206–22.
Behnke AR, Feen BG, Welham WC. The specific gravity of healthy men. JAMA 1942;118:495–8.
Article Google Scholar
Roentgen WC. Ueber eine neue Art von Strahlen. S.B. Phys-med Ges Wurzburg. 1895;132–41.
Wong MC, Bennett JP, Leong LT, Tian IY, Liu YE, Kelly NN, et al. Monitoring body composition change for intervention studies with advancing 3D optical imaging technology in comparison to dual-energy X-ray absorptiometry. Am J Clin Nutr. 2023:S0002-9165(23)04152-7
Church TS, Thomas DM, Tudor-Locke C, Katzmarzyk PT, Earnest CP, Rodarte RQ, et al. Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLoS ONE. 2011;6:e19657 https://doi.org/10.1371/journal.pone.0019657 .
Schwann TH; Smith H, Trans. Microsccopical researches into the accordance in the structure and growth of animals and plants . London: Sydenham Society 1847
Hassall A. Observations on the development of the fat vesicle. Lancet. 1849;1:163–4.
Hirsch J, Knittle JL. Cellularity of human obese and nonobese adipose tissue. Fed Proc. 1970;29:1516–21.
Garvey WT. New Horizons. A new paradigm for treating to target with second-generation obesity medications. JCEM. 2022;107:e1339–47.
Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM. Positional cloning of the mouse obese gene and its human homologue. Nature. 1994;372:425–32.
Lavoisier AL, DeLaPlace PS. Memoir on Heat. Read to the Royal Academy of Sciences 28 June 1783 [IN: Bray GA. The Battle of the Bulge: A History of Obesity Research . Pittsburgh: Dorrance Publishing, 2007 pp 498–512].
Bray GA. Lavoisier and Scientific Revolution: The oxygen theory displaces air, fire, earth and water. Obes Res. 1994;2:183–8.
Helmholtz, Hermann von. Uber die Erhaltung der Kraft, ein physikalische Abhandlung, vorgetragen in der Sitzung der physicalischen Gesellschaft zu Berlin am 23sten Juli 1847. Berlin: G. Reimer, 1847.
Bray GA. Commentary on Atwater classic. Obes Res. 1993;1:223–7.
Bray GA. Energy expenditure using doubly labeled water: the unveiling of objective truth. Obes Res. 1997;5:71–7.
Lifson N, Gordon GB, McClintock R. Measurement of total carbon dioxide production by means of D 2 0 18 . J Appl Physiol. 1955;7:704–10.
Lichtman SW, Pisarska K, Berman ER, Pestone M, Dowling H, Offenbacher E, et al. Discrepancy between self-reported and actual caloric intake and exercise in obese subjects. N Engl J Med. 1992;327(Dec):1893–8.
Bray GA. Commentary on classics of obesity 4. Hypothalamic obesity. Obes Res. 1993;1:325–8.
Bruch H. The froehlich syndrome: report of the original case. Am J Dis Child. 1939;58:1281–90.
Babinski JP. Tumeur du corps pituitaire sans acromegalie et arret de development des organs genitaux. Rev Neurol. 1900;8:531–3. [Translation IN: Bray GA. The Battle of the Bulge: A History of Obesity Research . Pittsburgh: Dorrance Publishing, 2007 pp 740–1]
Cushing H. The Pituitary Body and Its Disorders . Philadelphia. PA: JB Lippincott; 1912.
Bray GA. Laurence, moon, Bardet Biedl: reflect a syndrome. Obes Res. 1995;3:383–6.
Laurence JZ, Moon RC. Four cases of “Retinitis Pigmentosa,” Occurring in the same family, and accompanied by general imperfections of development. Opthalmol Rev. 1866;2:32–41.
Bardet G. Sur un Syndrome d’Obesity Conginitale avec Polydactylie et Retinite Pigmentaire (Contribution a l’etude des formes clinique de 1 ’Obesite hypophysaire) . Paris: 1920. Thesis [Translation IN: Bray GA. The Battle of the Bulge: A History of Obesity Research . Pittsburgh: Dorrance Publishing, 2007 pp 740–1].
Biedl A. Geschwisterpaar mit adiposo-genitaler Dystrophie. Dtsch Med Woche. 1922;48:1630.
Cuenot L. Pure strains and their combinations in the mouse. Arch Zoot Exptl Gen. 1905;122:123.
Ingalls AM, Dickie MM, Snell GD. Obese, new mutation in the mouse. J Hered. 1950;41:317–8.
Coleman DL. Obesity and diabetes: two mutant genescausing obesity-obesity syndromes in mice. Diabetalogia. 1978;14:141–8.
Zucker TF, Zucker LM. Fat accretion and growth in the rat. J Nutr. 1963;80:6–20.
Schwartz MW, Seeley RJ, Zeltser LM, Drewnowski A, Ravussin E, Redman LM, et al. Obesity pathogenesis: an endocrine society scientific statement. Endocr Rev. 2017;38:267–96.
Oral EA, Simha V, Ruiz E, Andewelt A, Premkumar A, Snell P, et al. Leptin-replacement therapy for lipodystrophy. N Engl J Med. 2002;346:570–8.
Loos RJF, Yeo GSH. The genetics of obesity: from discovery to biology. Nat Rev Genet. 2022;23:120–33.
Blüher M. Metabolically healthy obesity. Endocr Rev. 2020;41:405–20.
Acosta A, Camilleri M, Abu Dayyeh B, Calderon G, Gonzalez D, McRae A, et al. Selection of antiobesity medications based on phenotypes enhances weight loss: a pragmatic trial in an obesity clinic. Obes. 2021;29:662–71.
Bray GA. Commentary on classics in obesity. 6. Science and politics of hunger. Obes Res. 1993;19:489–93.
Cannon WB, Washburn AL. An explanation of hunger. Am J Physiol. 1912;29:441–54.
Carlson AJ. Contributions to the physiology of the stomach -II. the relation between the concentrations of the empty stomach and the sensation of hunger. Am J Physiol. 1912;31:175–92.
Carlson AJ. Control of Hunger in Health and Disease . Chicago, IL: University of Chicago Press; 1916.
Flint A, Raben A, Astrup A, Holst JJ. Glucagon-like peptide 1 promotes satiety and suppresses energy intake in humans. J Clin Invest. 1998;101:515–20.
Bray GA. Eat slowly - From laboratory to clinic; behavioral control of eating. Obes Res. 1996;4:397–400.
Pavlov IP; Thompson WH, trans. The Work of the Digestive Glands . London: Charles Griffin and Co.; 1910.
Skinner BF. Contingencies of Reinforcement: A Theoretical Analysis . New York: Meredith Corporation; 1969.
Ferster CB, Nurenberger JI, Levitt EG. The Control of Eating. J. Math 1964;1:87-109.
Stuart RB. Behavioral control of overeating. Behav Res Ther. 1967;5:357–65. [Also IN: Bray GA. The Battle of the Bulge: A History of Obesity Research . Pittsburgh: Dorrance Publishing, 2007 pp 793–9]
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM. et a; Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(Feb):393–403.
The Look AHEAD Research Group, Wadden TA, Bantle JP, Blackburn GL, Bolin P, Brancati FL, Bray GA, et al. Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity. 2014;22:5–13.
Bray GA, Suminska M. From Hippocrates to the Obesity Society: A Brief History. IN Handbook of Obesity (Bray GA, Bouchard C, Katzmarzyk P, Kirwan JP, Redman LM, Schauer PL eds). Boca Raton: Taylor & Francis 2024. Vol 2, pp 3–16.
Bray GA. Commentary on Banting Letter. Obes Res. 1993;1:148–52.
Banting W. Letter on Corpulence, Addressed to the Public . London: Harrison and Sons 1863. pp 1–21.
Harvey W. On corpulence in relation to disease” With some remarks of diet . London” Henry Renshaw, 1872.
Schwartz, H. Never Satisfied. A Cultural History of Diets, Fantasies and Fat . 1977.
Foxcroft, Louise. Calories and Corsets. A history of dieting over 2000 years . London: Profile Books, 2011.
Gilman, Sander L. Obesity. The Biography . Oxford: Oxford University Press, 2010.
Linn R Stuart SL. The Last Chance Diet . A Revolutionary New Approach to Weight Loss 1977.
Magendie F. Rapport fait a l’Academie des Sciences au le nom de la Commission diet la gelatine. C.R. Academie Sci (Paris) 1841:237-83.
Bray GA. “The Science of Hunger: Revisiting Two Theories of Feeding. IN Bray GA. The Battle of the Bulge. A History of Obesity Research . Pittsburgh, Dorrance Publishing 1977 p. 238.
Sours HE, Frattalli VP, Brand CD, et al. Sudden death associated with very low calorie weight regimes. Am J Clin Nutr. 1981;34:453–61.
Bray GA. From very-low-energy diets to fasting and back. Obes Res. 1995;3:207–9.
Benedict, F.G. A Study of prolonged fasting . Washington: Carnegie Institution of Washington (Publ No 203), 1915.
Keys A, Brozek J, Henschel A, Mickelsen O,Taylor HL. The biology of human starvation . Minneapolis: University of Minnesota Press, 1950.
Cahill GF Jr, Herrera MG, Morgan AP, Soeldner JS, Steinke J, Levy PL, et al. Hormone-fuel interrelationships during fasting. J Clin Invest. 1966;45:1751–69.
Benedict FG, Miles WR, Roth P, Smith HM. Human vitality and efficiency under prolonged restricted diet. Carnegie Instit Wash, Pub. No. 280. Washington: Carnegie Institution of Washington; 1919.
Evans FA, Strang JM. The treatment of obesity with low-calorie diets. JAMA 1931;97:1063–8.
Bloom WL. Fasting as an introduction to the treatment of obesity. Metabolism 1959;8:2 14–220.
CAS Google Scholar
Bray GA, Purnell JQ. An historical review of steps and missteps in the discovery of anti-obesity drugs. IN: Feingold KR, Anawalt B, Boyce A, Chrousos G, de Herder WW, Dhatariya K, Dungan K, et al. editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2022.
Lesses MF, Myerson A. Human autonomic pharmacology. NEJM 1938;218:119-24.
Cohen PA, Goday A, Swann JP. The return of rainbow diet pills. Am J Public Health. 2012;102:1676–86.
Bray GA. Nutrient intake is modulated by peripheral peptide administration. Obes Res. 1995;3:569S–572S.
Kissileff HR, Pi-Sunyer FX, Thornton J, Smith GP. C-terminal octapeptide of cholecystokinin decreases food intake in man. Am J Clin Nutr. 1981;34:154–60.
Wilding JPH, Batterham RL, Calanna S, Davies M, Van Gaal LF, Lingvay I, et al. STEP 1 study group. Once-weekly semaglutide in adults with overweight or obesity. N Engl J Med. 2021;384:989–1002.
Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jódar E, Leiter LA, et al. SUSTAIN-6 investigators. semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375:1834–44.
Jastreboff AM, Aronne LJ, Ahmad NN, Wharton S, Connery L, Alves B, et al. SURMOUNT-1 investigators. tirzepatide once weekly for the treatment of obesity. N. Engl J Med. 2022;387:205–16.
Jastreboff AM, Kaplan LM, Frías JP, Wu Q, Du Y, Gurbuz S, et al. Retatrutide phase 2 obesity trial investigators. Triple-hormone-receptor agonist retatrutide for obesity - a phase 2 trial. N Engl J Med. 2023;389:514–26.
Bray GA. Obesity and surgery for a chronic disease. Obes Res. 1996;4:301–3.
Kremen AJ, Linner JH, Nelson CH. An experimental evaluation of the nutritional importance of proximal and distal small intestine. Ann Surg. 1954;140:439–48.
Payne JH, DeWind LT, Commons RR. Metabolic observations in patients with jejuno-colic shunts. Am J Surg. 1963;106:273–89.
Payne JH, DeWind LT. Surgical treatment of obesity. Am J Surg. 1969;118:141–6.
Buchwald H, Varco RL. Partial ileal bypass for hypercholesterolemia and atherosclerosis. Surg Gynecol Obstet. 1967;124:1231.
Mason EE, Ito C. Gastric bypass in obesity. Surg Clin North Am. 1967;47:1345–135.
O’Brien PE, MacDonald L, Anderson M, Brennan L, Brown WA. Long-term outcomes after bariatric surgery: fifteen-year follow-up of adjustable gastric banding and a systematic review of the bariatric surgical literature. Ann Surg. 2013;257:87–94.
Arterburn D, Wellman R, Emiliano A, Smith SR, Odegaard AO, Murali S, et al. PCORnet bariatric study collaborative. Comparative effectiveness and safety of bariatric procedures for weight loss: a PCORnet cohort study. Ann Intern Med. 2018;169:741–50.
Picot J, Jones J, Colquitt JL, Gospodarevskaya E, Loveman E, Baxter L, et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess. 2009;13:1–190.
Christou NV, Sampalis JS, Liberman M, et al. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg. 2004;240:416–23.
Sjöström L. Review of the key results from the Swedish Obese Subjects (SOS) trial - a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013;273:219–34.
Sjöström L. Swedish Obese Subjects, SOS: A review of results from a prospective controlled intervention trial. In: Bray GA, Bochard C, eds. Handbook of Obesity, Volume 2: Clinical Applications. New York: Informa; 2014.
Sjöström L, Narbro K, Sjöström CD, Karason K, Larsson B, Wedel H, et al. Effects of bariatric surgery on mortality in Swedish Obese Subjects. N. Engl J Med. 2007;357:741–52.
Sjöström L, Peltonen M, Jacobson P, Sjöström CD, Karason K, Wedel H, et al. Bariatric surgery and long-term cardiovascular events. JAMA 2012;307:56–65.
Carlsson LM, Peltonen M, Ahlin S, Anveden Å, Bouchard C, Carlsson B, et al. Bariatric surgery and prevention of type 2 diabetes in Swedish Obese Subjects. The New England. J Med. 2012;367:695–704.
Pories WJ, Swanson MS, MacDonald KG, Long SB, Morris PG, Brown BM, et al. Who would have thought it? an operation proves to be the most effective therapy for adult-onset. Diabetes Mellit Ann Surg. 1995;222:339–52.
Bray GA. Life insurance and overweight. Obes Res. 1995;3:97–99.
The Association of Life Insurance Medical Directors and The Actuarial Society of America. Medico- Actuarial Mortality Investigation . New York: The Association of Life Insurance Medical Directors and ‘The Actuarial Society of America; 1913.
Keys A. Seven Countries: A Multivariate Analysis of Death and Coronary Heart Disease . Cambridge, MA: Harvard University Press; 1980.
Dawber TR. The Framingham Study: The Epidemiology of Atherosclerotic Disease . Cambridge, MA: Harvard University Press; 1980.
Bray, G.A. (Ed), Obesity in Perspective . Fogarty International Center Series on Preventive Med. Vol 2, parts 1 and 2, Washington, D.C.: U.S. Govt Prtg Office, 1976, DHEW Publication #75-708.
Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among adults aged 20 and over: United States, 1960–1962 through 2017–2018. NCHS Health E-Stats. 2020.
Bray GA. Obesity: Historical development of scientific and cultural ideas. Int J Obes. 1990;14:909–26.
Bray GA. The Battle of the Bulge: A History of Obesity Research . Pittsburgh: Dorrance Publishing, 2007 p 30.
Short, T. A Discourse Concerning the Causes and Effects of Corpulency Together with the Method for Its Prevention and Cure , J. Robert, London, 1727.
Flemyng, M. A Discourse on the Nature, Causes and Cure of Corpulency , L Davis and C Reymers, London, 1760.
Wadd, W. Comments on corpulency lineaments of leanness mems on diet and dietetics. London: John Ebers and Co, 1829.
Chambers, TK. Corpulence, or excess fat in the human body. London: Longman, 1850.
Rony HR. Obesity and Leanness . Philadelphia: Lea and Febiger, 1940.
Rynearson EH, Gastineau CF. Obesity . Springfield, IL: Charles C. Thomas, 1949.
Bray, G.A. The Obese Patient. Major Problems in Internal Medicine , Vol 9, Philadelphia, Pa.: W.B. Saunders Company, 1976, pp. 1-450.
Bray G.A. A Guide to Obesity and the Metabolic Syndrome: Origins and Treatment . New York: CRC Press: Taylor and Francis Group. 2011.
Howard AN. The history of the association for the study of obesity. Intern J Obes. 1992;16:S1–8.
Bray GA, Greenwood MRC, Hansen BC. The obesity society is turning 40: a history of the early years. Obesity. 2021;29(Dec):1978–81.
McLean Baird I, Howard AN. Obesity: Medical and Scientific Aspects : Proceedings of the First Symposium of the Obesity Association of Great Britain held in London , October 1968. Edinburgh & London: E. S. Livingston, 1968.
Bray GA, Howard AN. Founding of the international journal of obesity: a journey in medical journalism. Int J Obes. 2015;39:75–9.
Bray G. The founding of obesity research/obesity: a brief history. Obes. 2022;30:2100–2.
Ziman J. The Force of Knowledge. The Scientific Dimension of Society . Cambridge: Cambridge University Press, 1976.
Bray GA, Kim KK, Wilding JPH. Obesity: a chronic relapsing progressive disease process: a position paper of world obesity. Obes Rev. 2017;18:715–23.
Bray GA. Obesity is a chronic, relapsing neurochemical disease. Intern J Obes. 2004;28:34–8.
Allison DB, Downey M, Atkinson RL, Billington CJ, Bray GA, Eckel RH, et al. Obesity as a disease: a white paper on evidence and arguments commissioned by the Council of the Obesity Society. Obes. 2008;16:1161–77.
Garvey WT, Garber AJ, Mechanick JI, Bray GA, Dagogo-Jack S, Einhorn D, et al. American Association of Clinical Endocrinologists and American College of Endocrinology position statement on the 2014 advanced framework for a new diagnosis of obesity as a chronic disease. Endocr Pr. 2014;20:977–89.
Bray GA, Ryan DH. Evidence-based weight loss interventions: individualized treatment options to maximize patient outcomes. Diabetes Obes Metab. 2021;23:50–62.
Ge L, Sadeghirad B, Ball GDC, da Costa BR, Hitchcock CL, Svendrovski A, et al. Comparison of dietary macronutrient patterns of 14 popular named dietary programmes for weight and cardiovascular risk factor reduction in adults: systematic review and network meta-analysis of randomised trials. BMJ 2020;369:m696.
Sjöström L, Rissanen A, Andersen T, Boldrin M, Golay A, Koppeschaar HP, et al. Randomised placebo-controlled trial of orlistat for weight loss and prevention of weight regain in obese patients. European Multicentre Orlistat Study Group. Lancet 1998;352:167–72.
Pi-Sunyer FX, Aronne LJ, Heshmati HM, Devin J, Rosenstock J. Effect of rimonabant, a cannabinoid-1 receptor blocker, on weight and cardiometabolic risk factors in overweight or obese patients: RIO-North America: a randomized controlled trial. JAMA 2006;295:761–75.
Foster GD, Wadden TA, Vogt RA, Brewer G. What is a reasonable weight loss? Patients’ expectations and evaluations of obesity treatment outcomes. J Consult Clin Psychol. 1997;65:79–85.
DiFeliceantonio AG, Coppin G, Rigoux L, Thanarajah ES, Dagher A, Tittgemeyer M, et al. Supra-additive effects of combining fat and carbohydrate on food reward. Cell Metab. 2018;28:33–44.e3.
Thanarajah SE, Backes H, DiFeliceantonio AG, Albus K, Cremer AL, Hanssen R, et al. Food intake recruits orosensory and post-ingestive dopaminergic circuits to affect eating desire in humans. Cell Metab. 2019;29:695–706.e4.
Bray GA. Is sugar addictive? Diabetes 2016;65:1797–9.
Download references
Acknowledgements
The author thanks Dr. Jennifer Lyn Baker for her helpful comments during the early stage of preparing this manuscript.
Author information
Authors and affiliations.
Pennington Biomedical Research Center/LSU, Baton Rouge, LA, 70808, USA
George A. Bray
You can also search for this author in PubMed Google Scholar
Contributions
All contributions were made by the single author.
Corresponding author
Correspondence to George A. Bray .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
MSS # 2023IJO01171.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions

About this article
Cite this article.
Bray, G.A. Obesity: a 100 year perspective. Int J Obes (2024). https://doi.org/10.1038/s41366-024-01530-6
Download citation
Received : 13 November 2023
Revised : 23 April 2024
Accepted : 26 April 2024
Published : 07 May 2024
DOI : https://doi.org/10.1038/s41366-024-01530-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Patient Care & Health Information
- Diseases & Conditions
Obesity is a complex disease involving having too much body fat. Obesity isn't just a cosmetic concern. It's a medical problem that increases the risk of many other diseases and health problems. These can include heart disease, diabetes, high blood pressure, high cholesterol, liver disease, sleep apnea and certain cancers.
There are many reasons why some people have trouble losing weight. Often, obesity results from inherited, physiological and environmental factors, combined with diet, physical activity and exercise choices.
The good news is that even modest weight loss can improve or prevent the health problems associated with obesity. A healthier diet, increased physical activity and behavior changes can help you lose weight. Prescription medicines and weight-loss procedures are other options for treating obesity.
Products & Services
- A Book: The Mayo Clinic Diet Bundle
Body mass index, known as BMI, is often used to diagnose obesity. To calculate BMI , multiply weight in pounds by 703, divide by height in inches and then divide again by height in inches. Or divide weight in kilograms by height in meters squared. There are several online calculators available that help calculate BMI .
See BMI calculator
Asians with a BMI of 23 or higher may have an increased risk of health problems.
For most people, BMI provides a reasonable estimate of body fat. However, BMI doesn't directly measure body fat. Some people, such as muscular athletes, may have a BMI in the obesity category even though they don't have excess body fat.
Many health care professionals also measure around a person's waist to help guide treatment decisions. This measurement is called a waist circumference. Weight-related health problems are more common in men with a waist circumference over 40 inches (102 centimeters). They're more common in women with a waist measurement over 35 inches (89 centimeters). Body fat percentage is another measurement that may be used during a weight loss program to track progress.
When to see a doctor
If you're concerned about your weight or weight-related health problems, ask your health care professional about obesity management. You and your health care team can evaluate your health risks and discuss your weight-loss options.
More Information
Obesity care at Mayo Clinic
- What is insulin resistance? A Mayo Clinic expert explains
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Although there are genetic, behavioral, metabolic and hormonal influences on body weight, obesity occurs when you take in more calories than you burn through typical daily activities and exercise. Your body stores these excess calories as fat.
In the United States, most people's diets are too high in calories — often from fast food and high-calorie beverages. People with obesity might eat more calories before feeling full, feel hungry sooner, or eat more due to stress or anxiety.
Many people who live in Western countries now have jobs that are much less physically demanding, so they don't tend to burn as many calories at work. Even daily activities use fewer calories, courtesy of conveniences such as remote controls, escalators, online shopping, and drive-through restaurants and banks.
Risk factors
Obesity often results from a combination of causes and contributing factors:
Family inheritance and influences
The genes you inherit from your parents may affect the amount of body fat you store, and where that fat is distributed. Genetics also may play a role in how efficiently your body converts food into energy, how your body regulates your appetite and how your body burns calories during exercise.
Obesity tends to run in families. That's not just because of the genes they share. Family members also tend to share similar eating and activity habits.
Lifestyle choices
- Unhealthy diet. A diet that's high in calories, lacking in fruits and vegetables, full of fast food, and laden with high-calorie beverages and oversized portions contributes to weight gain.
- Liquid calories. People can drink many calories without feeling full, especially calories from alcohol. Other high-calorie beverages, such as sugared soft drinks, can contribute to weight gain.
- Inactivity. If you have an inactive lifestyle, you can easily take in more calories every day than you burn through exercise and routine daily activities. Looking at computer, tablet and phone screens is inactivity. The number of hours spent in front of a screen is highly associated with weight gain.
Certain diseases and medications
In some people, obesity can be traced to a medical cause, such as hypothyroidism, Cushing syndrome, Prader-Willi syndrome and other conditions. Medical problems, such as arthritis, also can lead to decreased activity, which may result in weight gain.
Some medicines can lead to weight gain if you don't compensate through diet or activity. These medicines include steroids, some antidepressants, anti-seizure medicines, diabetes medicines, antipsychotic medicines and certain beta blockers.
Social and economic issues
Social and economic factors are linked to obesity. It's hard to avoid obesity if you don't have safe areas to walk or exercise. You may not have learned healthy ways of cooking. Or you may not have access to healthier foods. Also, the people you spend time with may influence your weight. You're more likely to develop obesity if you have friends or relatives with obesity.
Obesity can occur at any age, even in young children. But as you age, hormonal changes and a less active lifestyle increase your risk of obesity. The amount of muscle in your body also tends to decrease with age. Lower muscle mass often leads to a decrease in metabolism. These changes also reduce calorie needs and can make it harder to keep off excess weight. If you don't consciously control what you eat and become more physically active as you age, you'll likely gain weight.
Other factors
- Pregnancy. Weight gain is common during pregnancy. Some women find this weight difficult to lose after the baby is born. This weight gain may contribute to the development of obesity in women.
- Quitting smoking. Quitting smoking is often associated with weight gain. And for some, it can lead to enough weight gain to qualify as obesity. Often, this happens as people use food to cope with smoking withdrawal. But overall, quitting smoking is still a greater benefit to your health than is continuing to smoke. Your health care team can help you prevent weight gain after quitting smoking.
- Lack of sleep. Not getting enough sleep can cause changes in hormones that increase appetite. So can getting too much sleep. You also may crave foods high in calories and carbohydrates, which can contribute to weight gain.
- Stress. Many external factors that affect mood and well-being may contribute to obesity. People often seek more high-calorie food during stressful situations.
- Microbiome. The make-up of your gut bacteria is affected by what you eat and may contribute to weight gain or trouble losing weight.
Even if you have one or more of these risk factors, it doesn't mean that you're destined to develop obesity. You can counteract most risk factors through diet, physical activity and exercise. Behavior changes, medicines and procedures for obesity also can help.
Complications
People with obesity are more likely to develop a number of potentially serious health problems, including:
- Heart disease and strokes. Obesity makes you more likely to have high blood pressure and unhealthy cholesterol levels, which are risk factors for heart disease and strokes.
- Type 2 diabetes. Obesity can affect the way the body uses insulin to control blood sugar levels. This raises the risk of insulin resistance and diabetes.
- Certain cancers. Obesity may increase the risk of cancer of the uterus, cervix, endometrium, ovary, breast, colon, rectum, esophagus, liver, gallbladder, pancreas, kidney and prostate.
- Digestive problems. Obesity increases the likelihood of developing heartburn, gallbladder disease and liver problems.
- Sleep apnea. People with obesity are more likely to have sleep apnea, a potentially serious disorder in which breathing repeatedly stops and starts during sleep.
- Osteoarthritis. Obesity increases the stress placed on weight-bearing joints. It also promotes inflammation, which includes swelling, pain and a feeling of heat within the body. These factors may lead to complications such as osteoarthritis.
- Fatty liver disease. Obesity increases the risk of fatty liver disease, a condition that happens due to excessive fat deposit in the liver. In some cases, this can lead to serious liver damage, known as liver cirrhosis.
- Severe COVID-19 symptoms. Obesity increases the risk of developing severe symptoms if you become infected with the virus that causes coronavirus disease 2019, known as COVID-19. People who have severe cases of COVID-19 may need treatment in intensive care units or even mechanical assistance to breathe.
Related information
- Link between extra pounds, severe COVID-19 illness grows stronger - Related information Link between extra pounds, severe COVID-19 illness grows stronger
Quality of life
Obesity can diminish the overall quality of life. You may not be able to do physical activities that you used to enjoy. You may avoid public places. People with obesity may even encounter discrimination.
Other weight-related issues that may affect your quality of life include:
- Depression.
- Disability.
- Shame and guilt.
- Social isolation.
- Lower work achievement.
- Overweight and obesity. National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health-topics/overweight-and-obesity. Accessed Dec. 21, 2022.
- Goldman L, et al., eds. Obesity. In: Goldman-Cecil Medicine. 26th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Dec. 21. 2022.
- Kellerman RD, et al. Obesity in adults. In: Conn's Current Therapy 2023. Elsevier; 2023. https://www.clinicalkey.com. Accessed Dec. 21, 2022.
- Feldman M, et al., eds. Obesity. In: Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. 11th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed Dec. 21, 2022.
- Perrault L. Obesity in adults: Prevalence, screening and evaluation. https://www.uptodate.com/contents/search. Accessed Dec. 21, 2022.
- Melmed S, et al. Obesity. In: Williams Textbook of Endocrinology. 14th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Dec. 21, 2022.
- COVID-19: People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed Dec. 21, 2022.
- Perrault L. Obesity in adults: Overview of management. https://www.uptodate.com/contents/search. Accessed Dec. 21, 2022.
- Healthy weight, nutrition and physical activity. Centers for Disease Control and Prevention. https://www.cdc.gov/healthyweight/index.html. Accessed Dec. 21, 2022.
- Ferri FF. Obesity. In: Ferri's Clinical Advisor 2023. Elsevier; 2023. https://www.clinicalkey.com. Accessed Jan. 20, 2023.
- Feldman M, et al., eds. Surgical and Endoscopic Treatment of Obesity. In: Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. 11th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed Dec. 21, 2022.
- BMI and waist circumference calculator
Associated Procedures
- Bariatric surgery
- Biliopancreatic diversion with duodenal switch (BPD/DS)
- Cholesterol test
- Gastric bypass (Roux-en-Y)
- Intragastric balloon
- Liver function tests
- Sleeve gastrectomy
News from Mayo Clinic
- Mayo Clinic Q & A: Supporting weight-loss medications with adequate, tailored nutrition May 02, 2024, 11:00 a.m. CDT
- Mayo Clinic researchers pave the way for individualized obesity therapy, tailoring interventions to a person's needs July 12, 2023, 03:00 p.m. CDT
- People with severe obesity and a genetic pathway variant have increased risk of hypertension, Mayo Clinic research finds April 18, 2023, 08:00 p.m. CDT
- Obesity makes it harder to diagnose and treat heart disease Feb. 28, 2023, 04:15 p.m. CDT
- Mayo Clinic Minute: Obesity and heart disease Feb. 23, 2023, 05:30 p.m. CDT
- Healthy Weight Awareness Month. Mayo Clinic innovations can help you lose weight, keep it off Jan. 05, 2023, 04:15 p.m. CDT
- Mayo Clinic Q and A: Probiotics, gut bacteria and weight -- what's the connection? Sept. 25, 2022, 11:00 a.m. CDT
- Addressing health care barriers during Hispanic Heritage Month Sept. 15, 2022, 04:30 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Search Menu
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Urban Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical Literature
- Classical Reception
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Papyrology
- Greek and Roman Archaeology
- Greek and Roman Epigraphy
- Greek and Roman Law
- Late Antiquity
- Religion in the Ancient World
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Evolution
- Language Reference
- Language Variation
- Language Families
- Language Acquisition
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Modernism)
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Media
- Music and Culture
- Music and Religion
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Science
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Lifestyle, Home, and Garden
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Society
- Law and Politics
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Clinical Neuroscience
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Medical Ethics
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Games
- Computer Security
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Ethics
- Business History
- Business Strategy
- Business and Technology
- Business and Government
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic History
- Economic Methodology
- Economic Systems
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Behaviour
- Political Economy
- Political Institutions
- Political Theory
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Politics and Law
- Public Policy
- Public Administration
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Developmental and Physical Disabilities Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

- < Previous chapter
26 Conclusion: Obesity and its prevention in the 21st century
- Published: September 2010
- Cite Icon Cite
- Permissions Icon Permissions
The case for a preventative approach to the obesity epidemic is compelling. Obesity poses what is arguably one of the most significant threats to population health that is currently faced. The data presented in this book highlight just how common obesity has become in children and in adults across the globe, and how it impacts disproportionately on the poor. This chapter presents a summary of the discussions in the preceding chapters.
Signed in as
Institutional accounts.
- Google Scholar Indexing
- GoogleCrawler [DO NOT DELETE]
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
- Add your ORCID iD
Institutional access
Sign in with a library card.
- Sign in with username/password
- Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Sign in through your institution
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- About Project
- Testimonials
Business Management Ideas

Essay on Obesity
List of essays on obesity, essay on obesity – short essay (essay 1 – 150 words), essay on obesity (essay 2 – 250 words), essay on obesity – written in english (essay 3 – 300 words), essay on obesity – for school students (class 5, 6, 7, 8, 9, 10, 11 and 12 standard) (essay 4 – 400 words), essay on obesity – for college students (essay 5 – 500 words), essay on obesity – with causes and treatment (essay 6 – 600 words), essay on obesity – for science students (essay 7 – 750 words), essay on obesity – long essay for medical students (essay 8 – 1000 words).
Obesity is a chronic health condition in which the body fat reaches abnormal level. Obesity occurs when we consume much more amount of food than our body really needs on a daily basis. In other words, when the intake of calories is greater than the calories we burn out, it gives rise to obesity.
Audience: The below given essays are exclusively written for school students (Class 5, 6, 7, 8, 9, 10, 11 and 12 Standard), college, science and medical students.
Introduction:
Obesity means being excessively fat. A person would be said to be obese if his or her body mass index is beyond 30. Such a person has a body fat rate that is disproportionate to his body mass.
Obesity and the Body Mass Index:
The body mass index is calculated considering the weight and height of a person. Thus, it is a scientific way of determining the appropriate weight of any person. When the body mass index of a person indicates that he or she is obese, it exposes the person to make health risk.
Stopping Obesity:
There are two major ways to get the body mass index of a person to a moderate rate. The first is to maintain a strict diet. The second is to engage in regular physical exercise. These two approaches are aimed at reducing the amount of fat in the body.
Conclusion:
Obesity can lead to sudden death, heart attack, diabetes and may unwanted illnesses. Stop it by making healthy choices.
Obesity has become a big concern for the youth of today’s generation. Obesity is defined as a medical condition in which an individual gains excessive body fat. When the Body Mass Index (BMI) of a person is over 30, he/ she is termed as obese.
Obesity can be a genetic problem or a disorder that is caused due to unhealthy lifestyle habits of a person. Physical inactivity and the environment in which an individual lives, are also the factors that leads to obesity. It is also seen that when some individuals are in stress or depression, they start cultivating unhealthy eating habits which eventually leads to obesity. Medications like steroids is yet another reason for obesity.
Obesity has several serious health issues associated with it. Some of the impacts of obesity are diabetes, increase of cholesterol level, high blood pressure, etc. Social impacts of obesity includes loss of confidence in an individual, lowering of self-esteem, etc.
The risks of obesity needs to be prevented. This can be done by adopting healthy eating habits, doing some physical exercise regularly, avoiding stress, etc. Individuals should work on weight reduction in order to avoid obesity.
Obesity is indeed a health concern and needs to be prioritized. The management of obesity revolves around healthy eating habits and physical activity. Obesity, if not controlled in its initial stage can cause many severe health issues. So it is wiser to exercise daily and maintain a healthy lifestyle rather than being the victim of obesity.
Obesity can be defined as the clinical condition where accumulation of excessive fat takes place in the adipose tissue leading to worsening of health condition. Usually, the fat is deposited around the trunk and also the waist of the body or even around the periphery.
Obesity is actually a disease that has been spreading far and wide. It is preventable and certain measures are to be taken to curb it to a greater extend. Both in the developing and developed countries, obesity has been growing far and wide affecting the young and the old equally.
The alarming increase in obesity has resulted in stimulated death rate and health issues among the people. There are several methods adopted to lose weight and they include different diet types, physical activity and certain changes in the current lifestyle. Many of the companies are into minting money with the concept of inviting people to fight obesity.
In patients associated with increased risk factor related to obesity, there are certain drug therapies and other procedures adopted to lose weight. There are certain cost effective ways introduced by several companies to enable clinic-based weight loss programs.
Obesity can lead to premature death and even cause Type 2 Diabetes Mellitus. Cardiovascular diseases have also become the part and parcel of obese people. It includes stroke, hypertension, gall bladder disease, coronary heart disease and even cancers like breast cancer, prostate cancer, endometrial cancer and colon cancer. Other less severe arising due to obesity includes osteoarthritis, gastro-esophageal reflux disease and even infertility.
Hence, serious measures are to be taken to fight against this dreadful phenomenon that is spreading its wings far and wide. Giving proper education on benefits of staying fit and mindful eating is as important as curbing this issue. Utmost importance must be given to healthy eating habits right from the small age so that they follow the same until the end of their life.
Obesity is majorly a lifestyle disease attributed to the extra accumulation of fat in the body leading to negative health effects on a person. Ironically, although prevalent at a large scale in many countries, including India, it is one of the most neglect health problems. It is more often ignored even if told by the doctor that the person is obese. Only when people start acquiring other health issues such as heart disease, blood pressure or diabetes, they start taking the problem of obesity seriously.
Obesity Statistics in India:
As per a report, India happens to figure as the third country in the world with the most obese people. This should be a troubling fact for India. However, we are yet to see concrete measures being adopted by the people to remain fit.
Causes of Obesity:
Sedentary lifestyle, alcohol, junk food, medications and some diseases such as hypothyroidism are considered as the factors which lead to obesity. Even children seem to be glued to televisions, laptops and video games which have taken away the urge for physical activities from them. Adding to this, the consumption of junk food has further aggravated the growing problem of obesity in children.
In the case of adults, most of the professions of today make use of computers which again makes people sit for long hours in one place. Also, the hectic lifestyle of today makes it difficult for people to spare time for physical activities and people usually remain stressed most of the times. All this has contributed significantly to the rise of obesity in India.
Obesity and BMI:
Body Mass Index (BMI) is the measure which allows a person to calculate how to fit he or she is. In other words, the BMI tells you if you are obese or not. BMI is calculated by dividing the weight of a person in kg with the square of his / her height in metres. The number thus obtained is called the BMI. A BMI of less than 25 is considered optimal. However, if a person has a BMI over 30 he/she is termed as obese.
What is a matter of concern is that with growing urbanisation there has been a rapid increase of obese people in India? It is of utmost importance to consider this health issue a serious threat to the future of our country as a healthy body is important for a healthy soul. We should all be mindful of what we eat and what effect it has on our body. It is our utmost duty to educate not just ourselves but others as well about this serious health hazard.
Obesity can be defined as a condition (medical) that is the accumulation of body fat to an extent that the excess fat begins to have a lot of negative effects on the health of the individual. Obesity is determined by examining the body mass index (BMI) of the person. The BMI is gotten by dividing the weight of the person in kilogram by the height of the person squared.
When the BMI of a person is more than 30, the person is classified as being obese, when the BMI falls between 25 and 30, the person is said to be overweight. In a few countries in East Asia, lower values for the BMI are used. Obesity has been proven to influence the likelihood and risk of many conditions and disease, most especially diabetes of type 2, cardiovascular diseases, sleeplessness that is obstructive, depression, osteoarthritis and some cancer types.
In most cases, obesity is caused through a combination of genetic susceptibility, a lack of or inadequate physical activity, excessive intake of food. Some cases of obesity are primarily caused by mental disorder, medications, endocrine disorders or genes. There is no medical data to support the fact that people suffering from obesity eat very little but gain a lot of weight because of slower metabolism. It has been discovered that an obese person usually expends much more energy than other people as a result of the required energy that is needed to maintain a body mass that is increased.
It is very possible to prevent obesity with a combination of personal choices and social changes. The major treatments are exercising and a change in diet. We can improve the quality of our diet by reducing our consumption of foods that are energy-dense like those that are high in sugars or fat and by trying to increase our dietary fibre intake.
We can also accompany the appropriate diet with the use of medications to help in reducing appetite and decreasing the absorption of fat. If medication, exercise and diet are not yielding any positive results, surgery or gastric balloon can also be carried out to decrease the volume of the stomach and also reduce the intestines’ length which leads to the feel of the person get full early or a reduction in the ability to get and absorb different nutrients from a food.
Obesity is the leading cause of ill-health and death all over the world that is preventable. The rate of obesity in children and adults has drastically increased. In 2015, a whopping 12 percent of adults which is about 600 million and about 100 million children all around the world were found to be obese.
It has also been discovered that women are more obese than men. A lot of government and private institutions and bodies have stated that obesity is top of the list of the most difficult and serious problems of public health that we have in the world today. In the world we live today, there is a lot of stigmatisation of obese people.
We all know how troubling the problem of obesity truly is. It is mainly a form of a medical condition wherein the body tends to accumulate excessive fat which in turn has negative repercussions on the health of an individual.
Given the current lifestyle and dietary style, it has become more common than ever. More and more people are being diagnosed with obesity. Such is its prevalence that it has been termed as an epidemic in the USA. Those who suffer from obesity are at a much higher risk of diabetes, heart diseases and even cancer.
In order to gain a deeper understanding of obesity, it is important to learn what the key causes of obesity are. In a layman term, if your calorie consumption exceeds what you burn because of daily activities and exercises, it is likely to lead to obesity. It is caused over a prolonged period of time when your calorie intake keeps exceeding the calories burned.
Here are some of the key causes which are known to be the driving factors for obesity.
If your diet tends to be rich in fat and contains massive calorie intake, you are all set to suffer from obesity.
Sedentary Lifestyle:
With most people sticking to their desk jobs and living a sedentary lifestyle, the body tends to get obese easily.
Of course, the genetic framework has a lot to do with obesity. If your parents are obese, the chance of you being obese is quite high.
The weight which women gain during their pregnancy can be very hard to shed and this is often one of the top causes of obesity.
Sleep Cycle:
If you are not getting an adequate amount of sleep, it can have an impact on the hormones which might trigger hunger signals. Overall, these linked events tend to make you obese.
Hormonal Disorder:
There are several hormonal changes which are known to be direct causes of obesity. The imbalance of the thyroid stimulating hormone, for instance, is one of the key factors when it comes to obesity.
Now that we know the key causes, let us look at the possible ways by which you can handle it.
Treatment for Obesity:
As strange as it may sound, the treatment for obesity is really simple. All you need to do is follow the right diet and back it with an adequate amount of exercise. If you can succeed in doing so, it will give you the perfect head-start into your journey of getting in shape and bidding goodbye to obesity.
There are a lot of different kinds and styles of diet plans for obesity which are available. You can choose the one which you deem fit. We recommend not opting for crash dieting as it is known to have several repercussions and can make your body terribly weak.
The key here is to stick to a balanced diet which can help you retain the essential nutrients, minerals, and, vitamins and shed the unwanted fat and carbs.
Just like the diet, there are several workout plans for obesity which are available. It is upon you to find out which of the workout plan seems to be apt for you. Choose cardio exercises and dance routines like Zumba to shed the unwanted body weight. Yoga is yet another method to get rid of obesity.
So, follow a blend of these and you will be able to deal with the trouble of obesity in no time. We believe that following these tips will help you get rid of obesity and stay in shape.
Obesity and overweight is a top health concern in the world due to the impact it has on the lives of individuals. Obesity is defined as a condition in which an individual has excessive body fat and is measured using the body mass index (BMI) such that, when an individual’s BMI is above 30, he or she is termed obese. The BMI is calculated using body weight and height and it is different for all individuals.
Obesity has been determined as a risk factor for many diseases. It results from dietary habits, genetics, and lifestyle habits including physical inactivity. Obesity can be prevented so that individuals do not end up having serious complications and health problems. Chronic illnesses like diabetes, heart diseases and relate to obesity in terms of causes and complications.
Factors Influencing Obesity:
Obesity is not only as a result of lifestyle habits as most people put it. There are other important factors that influence obesity. Genetics is one of those factors. A person could be born with genes that predispose them to obesity and they will also have difficulty in losing weight because it is an inborn factor.
The environment also influences obesity because the diet is similar in certain environs. In certain environments, like school, the food available is fast foods and the chances of getting healthy foods is very low, leading to obesity. Also, physical inactivity is an environmental factor for obesity because some places have no fields or tracks where people can jog or maybe the place is very unsafe and people rarely go out to exercise.
Mental health affects the eating habits of individuals. There is a habit of stress eating when a person is depressed and it could result in overweight or obesity if the person remains unhealthy for long period of time.
The overall health of individuals also matter. If a person is unwell and is prescribed with steroids, they may end up being obese. Steroidal medications enable weight gain as a side effect.
Complications of Obesity:
Obesity is a health concern because its complications are severe. Significant social and health problems are experienced by obese people. Socially, they will be bullied and their self-esteem will be low as they will perceive themselves as unworthy.
Chronic illnesses like diabetes results from obesity. Diabetes type 2 has been directly linked to obesity. This condition involves the increased blood sugars in the body and body cells are not responding to insulin as they should. The insulin in the body could also be inadequate due to decreased production. High blood sugar concentrations result in symptoms like frequent hunger, thirst and urination. The symptoms of complicated stages of diabetes type 2 include loss of vision, renal failure and heart failure and eventually death. The importance of having a normal BMI is the ability of the body to control blood sugars.
Another complication is the heightened blood pressures. Obesity has been defined as excessive body fat. The body fat accumulates in blood vessels making them narrow. Narrow blood vessels cause the blood pressures to rise. Increased blood pressure causes the heart to start failing in its physiological functions. Heart failure is the end result in this condition of increased blood pressures.
There is a significant increase in cholesterol in blood of people who are obese. High blood cholesterol levels causes the deposition of fats in various parts of the body and organs. Deposition of fats in the heart and blood vessels result in heart diseases. There are other conditions that result from hypercholesterolemia.
Other chronic illnesses like cancer can also arise from obesity because inflammation of body cells and tissues occurs in order to store fats in obese people. This could result in abnormal growths and alteration of cell morphology. The abnormal growths could be cancerous.
Management of Obesity:
For the people at risk of developing obesity, prevention methods can be implemented. Prevention included a healthy diet and physical activity. The diet and physical activity patterns should be regular and realizable to avoid strains that could result in complications.
Some risk factors for obesity are non-modifiable for example genetics. When a person in genetically predisposed, the lifestyle modifications may be have help.
For the individuals who are already obese, they can work on weight reduction through healthy diets and physical exercises.
In conclusion, obesity is indeed a major health concern because the health complications are very serious. Factors influencing obesity are both modifiable and non-modifiable. The management of obesity revolves around diet and physical activity and so it is important to remain fit.
In olden days, obesity used to affect only adults. However, in the present time, obesity has become a worldwide problem that hits the kids as well. Let’s find out the most prevalent causes of obesity.
Factors Causing Obesity:
Obesity can be due to genetic factors. If a person’s family has a history of obesity, chances are high that he/ she would also be affected by obesity, sooner or later in life.
The second reason is having a poor lifestyle. Now, there are a variety of factors that fall under the category of poor lifestyle. An excessive diet, i.e., eating more than you need is a definite way to attain the stage of obesity. Needless to say, the extra calories are changed into fat and cause obesity.
Junk foods, fried foods, refined foods with high fats and sugar are also responsible for causing obesity in both adults and kids. Lack of physical activity prevents the burning of extra calories, again, leading us all to the path of obesity.
But sometimes, there may also be some indirect causes of obesity. The secondary reasons could be related to our mental and psychological health. Depression, anxiety, stress, and emotional troubles are well-known factors of obesity.
Physical ailments such as hypothyroidism, ovarian cysts, and diabetes often complicate the physical condition and play a massive role in abnormal weight gain.
Moreover, certain medications, such as steroids, antidepressants, and contraceptive pills, have been seen interfering with the metabolic activities of the body. As a result, the long-term use of such drugs can cause obesity. Adding to that, regular consumption of alcohol and smoking are also connected to the condition of obesity.
Harmful Effects of Obesity:
On the surface, obesity may look like a single problem. But, in reality, it is the mother of several major health issues. Obesity simply means excessive fat depositing into our body including the arteries. The drastic consequence of such high cholesterol levels shows up in the form of heart attacks and other life-threatening cardiac troubles.
The fat deposition also hampers the elasticity of the arteries. That means obesity can cause havoc in our body by altering the blood pressure to an abnormal range. And this is just the tip of the iceberg. Obesity is known to create an endless list of problems.
In extreme cases, this disorder gives birth to acute diseases like diabetes and cancer. The weight gain due to obesity puts a lot of pressure on the bones of the body, especially of the legs. This, in turn, makes our bones weak and disturbs their smooth movement. A person suffering from obesity also has higher chances of developing infertility issues and sleep troubles.
Many obese people are seen to be struggling with breathing problems too. In the chronic form, the condition can grow into asthma. The psychological effects of obesity are another serious topic. You can say that obesity and depression form a loop. The more a person is obese, the worse is his/ her depression stage.
How to Control and Treat Obesity:
The simplest and most effective way, to begin with, is changing our diet. There are two factors to consider in the diet plan. First is what and what not to eat. Second is how much to eat.
If you really want to get rid of obesity, include more and more green vegetables in your diet. Spinach, beans, kale, broccoli, cauliflower, asparagus, etc., have enough vitamins and minerals and quite low calories. Other healthier options are mushrooms, pumpkin, beetroots, and sweet potatoes, etc.
Opt for fresh fruits, especially citrus fruits, and berries. Oranges, grapes, pomegranate, pineapple, cherries, strawberries, lime, and cranberries are good for the body. They have low sugar content and are also helpful in strengthening our immune system. Eating the whole fruits is a more preferable way in comparison to gulping the fruit juices. Fruits, when eaten whole, have more fibers and less sugar.
Consuming a big bowl of salad is also great for dealing with the obesity problem. A salad that includes fibrous foods such as carrots, radish, lettuce, tomatoes, works better at satiating the hunger pangs without the risk of weight gain.
A high protein diet of eggs, fish, lean meats, etc., is an excellent choice to get rid of obesity. Take enough of omega fatty acids. Remember to drink plenty of water. Keeping yourself hydrated is a smart way to avoid overeating. Water also helps in removing the toxins and excess fat from the body.
As much as possible, avoid fats, sugars, refined flours, and oily foods to keep the weight in control. Control your portion size. Replace the three heavy meals with small and frequent meals during the day. Snacking on sugarless smoothies, dry fruits, etc., is much recommended.
Regular exercise plays an indispensable role in tackling the obesity problem. Whenever possible, walk to the market, take stairs instead of a lift. Physical activity can be in any other form. It could be a favorite hobby like swimming, cycling, lawn tennis, or light jogging.
Meditation and yoga are quite powerful practices to drive away the stress, depression and thus, obesity. But in more serious cases, meeting a physician is the most appropriate strategy. Sometimes, the right medicines and surgical procedures are necessary to control the health condition.
Obesity is spreading like an epidemic, haunting both the adults and the kids. Although genetic factors and other physical ailments play a role, the problem is mostly caused by a reckless lifestyle.
By changing our way of living, we can surely take control of our health. In other words, it would be possible to eliminate the condition of obesity from our lives completely by leading a healthy lifestyle.
Health , Obesity
Get FREE Work-at-Home Job Leads Delivered Weekly!

Join more than 50,000 subscribers receiving regular updates! Plus, get a FREE copy of How to Make Money Blogging!
Message from Sophia!
Like this post? Don’t forget to share it!
Here are a few recommended articles for you to read next:
- Essay on Cleanliness
- Essay on Cancer
- Essay on AIDS
- Essay on Health and Fitness
No comments yet.
Leave a reply click here to cancel reply..
You must be logged in to post a comment.
Billionaires
- Donald Trump
- Warren Buffett
- Email Address
- Free Stock Photos
- Keyword Research Tools
- URL Shortener Tools
- WordPress Theme
Book Summaries
- How To Win Friends
- Rich Dad Poor Dad
- The Code of the Extraordinary Mind
- The Luck Factor
- The Millionaire Fastlane
- The ONE Thing
- Think and Grow Rich
- 100 Million Dollar Business
- Business Ideas
Digital Marketing
- Mobile Addiction
- Social Media Addiction
- Computer Addiction
- Drug Addiction
- Internet Addiction
- TV Addiction
- Healthy Habits
- Morning Rituals
- Wake up Early
- Cholesterol
- Reducing Cholesterol
- Fat Loss Diet Plan
- Reducing Hair Fall
- Sleep Apnea
- Weight Loss
Internet Marketing
- Email Marketing
Law of Attraction
- Subconscious Mind
- Vision Board
- Visualization
Law of Vibration
- Professional Life
Motivational Speakers
- Bob Proctor
- Robert Kiyosaki
- Vivek Bindra
- Inner Peace
Productivity
- Not To-do List
- Project Management Software
- Negative Energies
Relationship
- Getting Back Your Ex
Self-help 21 and 14 Days Course
Self-improvement.
- Body Language
- Complainers
- Emotional Intelligence
- Personality
Social Media
- Project Management
- Anik Singal
- Baba Ramdev
- Dwayne Johnson
- Jackie Chan
- Leonardo DiCaprio
- Narendra Modi
- Nikola Tesla
- Sachin Tendulkar
- Sandeep Maheshwari
- Shaqir Hussyin
Website Development
Wisdom post, worlds most.
- Expensive Cars
Our Portals: Gulf Canada USA Italy Gulf UK
Privacy Overview
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Preventing Childhood Obesity
- Health Care Strategies
- About Obesity
- What Can Be Done
- About Healthy Weight and Growth
- Body Mass Index (BMI)
- About Nutrition
- About Physical Activity
Risk Factors for Obesity
At a glance.
Obesity is a complex and costly chronic disease influenced by many factors. These factors include health behaviors, stress, health conditions and medications, genes, and people's environment. Knowing the risk factors can help individuals and communities take steps to prevent and reduce obesity.

Health behaviors
Certain health behaviors can contribute to excess weight gain and are risk factors for obesity:
- Lack of physical activity .
- Too many highly processed foods or added sugars , including too many sugar-sweetened beverages .
- Too little fiber and fruits and vegetables .
- Not enough sleep or poor quality sleep.
- Too much TV, computer, video games, and other screen time.
Long-term stress can affect your brain and trigger your body to make high levels of hormones, such as cortisol. These hormones help regulate energy balances and hunger urges. High levels of these hormones can increase your appetite and promote cravings for foods that are high in fats and added sugars. 1
Health conditions and medications
Some health conditions may lead to excess weight gain, obesity, or insulin resistance. These conditions include Cushing syndrome, polycystic ovary syndrome, or underactive thyroid.
Some medications may also cause weight gain by disrupting the brain's signals for hunger or through other mechanisms. These medications can include:
- Psychiatric medications, such as antipsychotics and antidepressants.
- Certain types of hormonal birth control, such as progestins.
- Anti-seizure or mood-stabilizing drugs.
- Certain blood pressure and diabetes medications.
In specific, rare, single-gene disorders, genes can directly cause obesity. Examples of these disorders are Bardet-Biedl syndrome and Prader-Willi syndrome.
It is more common for multiple genes to be responsible for a person's feelings of hunger, sense of fullness, and metabolism. 2
Systems and environment
Health is influenced by the conditions in which people live, learn, work, and play. Health can also be influenced by forces and policies that shape these conditions. These factors affect a person's ability to make healthy choices and influence their risk of gaining excess weight and developing obesity.
Examples include:
- Access to healthy, affordable foods and beverages.
- Access to safe places for physical activity .
- Community design to support activity-friendly routes to everyday destinations.
- Supportive childcare and school environments .
- Access to high-quality health care services .
- Safe housing and transportation .
- Economic stability .
Also, some chemicals in the environment can disrupt how our bodies work and cause excess weight gain. Understanding these factors and how we can use that knowledge to improve our health is ongoing.
- Scott KA, Melhorn SJ, Sakai RR. Effects of chronic social stress on obesity. Curr Obes Rep. 2012 Mar;1(1):16-25. doi: 10.1007/s13679-011-0006-3
- Mahmoud R, Kimonis V, Butler MG. Genetics of obesity in humans: a clinical review. Int J Mol Sci. 2022 Sep 20;23(19):11005. doi: 10.3390/ijms231911005
CDC's obesity prevention efforts focus on policy and environmental strategies to make healthy eating and active living accessible for everyone.
For Everyone
Health care providers, public health.
- Share full article
Advertisement
Supported by
Guest Essay
A Year on Ozempic Taught Me We’re Thinking About Obesity All Wrong

By Johann Hari
Mr. Hari is a British journalist and the author of “Magic Pill: The Extraordinary Benefits — and Disturbing Risks — of the New Weight Loss Drugs.”
Ever since I was a teenager, I have dreamed of shedding a lot of weight. So when I shrank from 203 pounds to 161 in a year, I was baffled by my feelings. I was taking Ozempic, and I was haunted by the sense that I was cheating and doing something immoral.
I’m not the only one. In the United States (where I now split my time), over 70 percent of people are overweight or obese, and according to one poll, 47 percent of respondents said they were willing to pay to take the new weight-loss drugs. It’s not hard to see why. They cause users to lose an average of 10 to 20 percent of their body weight, and clinical trials suggest that the next generation of drugs (probably available soon) leads to a 24 percent loss, on average. Yet as more and more people take drugs like Ozempic, Wegovy and Mounjaro, we get more confused as a culture, bombarding anyone in the public eye who takes them with brutal shaming.
This is happening because we are trapped in a set of old stories about what obesity is and the morally acceptable ways to overcome it. But the fact that so many of us are turning to the new weight-loss drugs can be an opportunity to find a way out of that trap of shame and stigma — and to a more truthful story.
In my lifetime, obesity has exploded, from being rare to almost being the norm. I was born in 1979, and by the time I was 21, obesity rates in the United States had more than doubled . They have skyrocketed since. The obvious question is, why? And how do these new weight-loss drugs work? The answer to both lies in one word: satiety. It’s a concept that we don’t use much in everyday life but that we’ve all experienced at some point. It describes the sensation of having had enough and not wanting any more.
The primary reason we have gained weight at a pace unprecedented in human history is that our diets have radically changed in ways that have deeply undermined our ability to feel sated. My father grew up in a village in the Swiss mountains, where he ate fresh, whole foods that had been cooked from scratch and prepared on the day they were eaten. But in the 30 years between his childhood and mine, in the suburbs of London, the nature of food transformed across the Western world. He was horrified to see that almost everything I ate was reheated and heavily processed. The evidence is clear that the kind of food my father grew up eating quickly makes you feel full. But the kind of food I grew up eating, much of which is made in factories, often with artificial chemicals, left me feeling empty and as if I had a hole in my stomach. In a recent study of what American children eat, ultraprocessed food was found to make up 67 percent of their daily diet. This kind of food makes you want to eat more and more. Satiety comes late, if at all.
One scientific experiment — which I have nicknamed Cheesecake Park — seemed to me to crystallize this effect. Paul Kenny, a neuroscientist at Mount Sinai Hospital in New York, grew up in Ireland. After he moved in 2000 to the United States, when he was in his 20s, he gained 30 pounds in two years. He began to wonder if the American diet has some kind of strange effect on our brains and our cravings, so he designed an experiment to test it. He and his colleague Paul Johnson raised a group of rats in a cage and gave them an abundant supply of healthy, balanced rat chow made out of the kind of food rats had been eating for a very long time. The rats would eat it when they were hungry, and then they seemed to feel sated and stopped. They did not become fat.
But then Dr. Kenny and his colleague exposed the rats to an American diet: fried bacon, Snickers bars, cheesecake and other treats. They went crazy for it. The rats would hurl themselves into the cheesecake, gorge themselves and emerge with their faces and whiskers totally slicked with it. They quickly lost almost all interest in the healthy food, and the restraint they used to show around healthy food disappeared. Within six weeks, their obesity rates soared.
After this change, Dr. Kenny and his colleague tweaked the experiment again (in a way that seems cruel to me, a former KFC addict). They took all the processed food away and gave the rats their old healthy diet. Dr. Kenny was confident that they would eat more of it, proving that processed food had expanded their appetites. But something stranger happened. It was as though the rats no longer recognized healthy food as food at all, and they barely ate it. Only when they were starving did they reluctantly start to consume it again.
Though Dr. Kenny’s study was in rats, we can see forms of this behavior everywhere. We are all living in Cheesecake Park — and the satiety-stealing effect of industrially assembled food is evidently what has created the need for these medications. Drugs like Ozempic work precisely by making us feel full. Carel le Roux, a scientist whose research was important to the development of these drugs, says they boost what he and others once called “satiety hormones.”
Once you understand this context, it becomes clear that processed and ultraprocessed food create a raging hole of hunger, and these treatments can repair that hole. Michael Lowe, a professor of psychology at Drexel University who has studied hunger for 40 years, told me the drugs are “an artificial solution to an artificial problem.”
Yet we have reacted to this crisis largely caused by the food industry as if it were caused only by individual moral dereliction. I felt like a failure for being fat and was furious with myself for it. Why do we turn our anger inward and not outward at the main cause of the crisis? And by extension, why do we seek to shame people taking Ozempic but not those who, say, take drugs to lower their blood pressure?
The answer, I think, lies in two very old notions. The first is the belief that obesity is a sin. When Pope Gregory I laid out the seven deadly sins in the sixth century, one of them was gluttony, usually illustrated with grotesque-seeming images of overweight people. Sin requires punishment before you can get to redemption. Think about the competition show “The Biggest Loser,” on which obese people starve and perform extreme forms of exercise in visible agony in order to demonstrate their repentance.
The second idea is that we are all in a competition when it comes to weight. Ours is a society full of people fighting against the forces in our food that are making us fatter. It is often painful to do this: You have to tolerate hunger or engage in extreme forms of exercise. It feels like a contest in which each thin person creates additional pressure on others to do the same. Looked at in this way, people on Ozempic can resemble athletes like the cyclist Lance Armstrong who used performance-enhancing drugs. Those who manage their weight without drugs might think, “I worked hard for this, and you get it for as little as a weekly jab?”
We can’t find our way to a sane, nontoxic conversation about obesity or Ozempic until we bring these rarely spoken thoughts into the open and reckon with them. You’re not a sinner for gaining weight. You’re a typical product of a dysfunctional environment that makes it very hard to feel full. If you are angry about these drugs, remember the competition isn’t between you and your neighbor who’s on weight-loss drugs. It’s between you and a food industry constantly designing new ways to undermine your satiety. If anyone is the cheat here, it’s that industry. We should be united in a struggle against it and its products, not against desperate people trying to find a way out of this trap.
There are extraordinary benefits as well as disturbing risks associated with weight-loss drugs. Reducing or reversing obesity hugely boosts health, on average: We know from years of studying bariatric surgery that it slashes the risks of cancer, heart disease and diabetes-related death. Early indications are that the new anti-obesity drugs are moving people in a similar radically healthier direction, massively reducing the risk of heart attack or stroke. But these drugs may increase the risk for thyroid cancer. I am worried they diminish muscle mass and fear they may supercharge eating disorders. This is a complex picture in which the evidence has to be weighed very carefully.
But we can’t do that if we remain lost in stories inherited from premodern popes or in a senseless competition that leaves us all, in the end, losers. Do we want these weight loss drugs to be another opportunity to tear one another down? Or do we want to realize that the food industry has profoundly altered the appetites of us all — leaving us trapped in the same cage, scrambling to find a way out?
Johann Hari is a British journalist and the author of “Magic Pill: The Extraordinary Benefits — and Disturbing Risks — of the New Weight Loss Drugs,” among other books.
Source photographs by seamartini, The Washington Post, and Zana Munteanu via Getty Images.
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .
Home — Essay Samples — Nursing & Health — Obesity — The Most Common Causes of Obesity
The Most Common Causes of Obesity
- Categories: Food Safety Medicare Obesity
About this sample

Words: 505 |
Published: Jan 8, 2020
Words: 505 | Page: 1 | 3 min read

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr Jacklynne
Verified writer
- Expert in: Science Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
1 pages / 476 words
5 pages / 2799 words
1 pages / 619 words
13 pages / 5869 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Obesity
Obesity is a prevalent disease in many countries today, leading to various complications and life-threatening illnesses. While medication intervention is not always necessary, lifestyle changes are often required to treat and [...]
In recent years, the issue of obesity has become a global epidemic. Obesity is a condition where a person has an excessive amount of fat, which can lead to numerous health problems. According to the World Health Organization [...]
Obesity has become a major health issue in recent times, with over 39% of adults around the world being overweight and 13% being obese. In the United States, 42.4% of adults are obese, costing the country a staggering $147 [...]
According to the World Health Organization, in 2016, more than 1.9 billion adults were overweight, of which around 650 million were obese. In the United States alone, more than 42% of the population is considered obese. This [...]
“What if a war on obesity only makes the problem worse”? argues Author Daniel Engber in his article “Glutton Intolerance”. Discrimination against the obese in our society makes the obesity problem worse. The treatment against [...]
It is well known today that the obesity epidemic is claiming more and more victims each day. The Centers for Disease Control and Prevention writes “that nearly 1 in 5 school age children and young people (6 to 19 years) in the [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Two decades of studies suggest health benefits associated with plant-based diets
But researchers caution against broad diet recommendations until remaining knowledge gaps are filled.
Vegetarian and vegan diets are generally associated with better status on various medical factors linked to cardiovascular health and cancer risk, as well as lower risk of cardiovascular diseases, cancer, and death, according to a new review of 49 previously published papers. Angelo Capodici and colleagues present these findings in the open-access journal PLOS ONE on May 15, 2024.
Prior studies have linked certain diets with increased risk of cardiovascular disease and cancer. A diet that is poor in plant products and rich in meat, refined grains, sugar, and salt is associated with higher risk of death. Reducing consumption of animal-based products in favor of plant-based products has been suggested to lower the risk of cardiovascular disease and cancer. However, the overall benefits of such diets remain unclear.
To deepen understanding of the potential benefits of plant-based diets, Capodici and colleagues reviewed 48 papers published between January 2000 and June 2023 that themselves compiled evidence from multiple prior studies. Following an "umbrella" review approach, they extracted and analyzed data from the 48 papers on links between plant-based diets, cardiovascular health, and cancer risk.
Their analysis showed that, overall, vegetarian and vegan diets have a robust statistical association with better health status on a number of risk factors associated with cardiometabolic diseases, cancer, and mortality, such as blood pressure, management of blood sugar, and body mass index. Such diets are associated with reduced risk of ischemic heart disease, gastrointestinal and prostate cancer, and death from cardiovascular disease.
However, among pregnant women specifically, those with vegetarian diets faced no difference in their risk of gestational diabetes and hypertension compared to those on non-plant-based diets.
Overall, these findings suggest that plant-based diets are associated with significant health benefits. However, the researchers note, the statistical strength of this association is significantly limited by the many differences between past studies in terms of the specific diet regimens followed, patient demographics, study duration, and other factors. Moreover, some plant-based diets may introduce vitamin and mineral deficiencies for some people. Thus, the researchers caution against large-scale recommendation of plant-based diets until more research is completed.
The authors add: "Our study evaluates the different impacts of animal-free diets for cardiovascular health and cancer risk showing how a vegetarian diet can be beneficial to human health and be one of the effective preventive strategies for the two most impactful chronic diseases on human health in the 21st century."
- Diet and Weight Loss
- Diseases and Conditions
- Colon Cancer
- Endangered Plants
- Veterinary Medicine
- Colorectal cancer
- Ovarian cancer
- Polyphenol antioxidant
- Stomach cancer
- Cervical cancer
- HPV vaccine
- Breast cancer
Story Source:
Materials provided by PLOS . Note: Content may be edited for style and length.
Journal Reference :
- Angelo Capodici, Gabriele Mocciaro, Davide Gori, Matthew J. Landry, Alice Masini, Francesco Sanmarchi, Matteo Fiore, Angela Andrea Coa, Gisele Castagna, Christopher D. Gardner, Federica Guaraldi. Cardiovascular health and cancer risk associated with plant based diets: An umbrella review . PLOS ONE , 2024; 19 (5): e0300711 DOI: 10.1371/journal.pone.0300711
Cite This Page :
Explore More
- Life Expectancy May Increase by 5 Years by 2050
- Toward a Successful Vaccine for HIV
- Highly Efficient Thermoelectric Materials
- Toward Human Brain Gene Therapy
- Whale Families Learn Each Other's Vocal Style
- AI Can Answer Complex Physics Questions
- Otters Use Tools to Survive a Changing World
- Monogamy in Mice: Newly Evolved Type of Cell
- Sustainable Electronics, Doped With Air
- Male Vs Female Brain Structure
Trending Topics
Strange & offbeat.

IMAGES
VIDEO
COMMENTS
Obesity has become a global epidemic and is one of today's most public health problems worldwide. Obesity poses a major risk for a variety of serious diseases including diabetes mellitus, non-alcoholic liver disease (NAFLD), cardiovascular disease, hypertension and stroke, and certain forms of cancer (Bluher, 2019).Obesity is mainly caused by imbalanced energy intake and expenditure due to a ...
Besides health complications, obesity causes an array of psychological effects, including inferiority complex among victims. Obese people suffer from depression, emanating from negative self-esteem and societal rejection. In some cases, people who become obese lose their friends and may get disapproval from teachers and other personalities ...
Despite public health efforts, these disorders are on the rise, and their consequences are burgeoning. 1 The Centers for Disease Control and Prevention report that during 2017 to 2018, the prevalence of obesity in the United States was 42.4%, which was increased from the prevalence of 30.5% during 1999 to 2002. 2 Among those afflicted with ...
Introduction. Obesity is an increasing, global public health issue. Patients with obesity are at major risk for developing a range of comorbid conditions, including cardiovascular disease (CVD), gastrointestinal disorders, type 2 diabetes (T2D), joint and muscular disorders, respiratory problems, and psychological issues, which may significantly affect their daily lives as well as increasing ...
Some genetic and lifestyle factors affect an individual's likelihood of adult obesity; thus, the significant clusters of obesity observed in specific geographical regions and contexts also signal the impact of socioeconomic and environmental factors in "obesogenic" environments [13].Understanding the causes and determinants of obesity is a critical step toward creating effective policy and ...
This essay will explore the various causes of obesity and their effects on individuals and society as a whole. One of the primary causes of obesity is dietary habits and nutritional intake. The consumption of high-calorie, low-nutrient foods, such as fast food, sugary beverages, and processed snacks, has become increasingly prevalent in modern ...
If you are writing a cause-and-effect obesity essay, you can mention different causes of obesity and how it can affect a person's overall health. The number of body paragraphs can increase depending on the parameters of the assignment as set forth by your instructor. Start each body paragraph with a topic sentence that is the crux of its content.
Obesity prevalence has increased in pandemic dimensions over the past 50 years. Obesity is a disease that can cause premature disability and death by increasing the risk of cardiometabolic ...
Statistics obscure suffering. According to 2014 national data, 35 percent of adult men and 40.4 percent of adult women are obese—that is, their body mass index, or BMI, a standard calculation of weight divided by height, is greater than or equal to 30. (Normal BMI is 18.5 to 24.9; overweight is 25 to 29.9.) Among youth 2 to 19 years old, the ...
carbohydrate is a crucial factor in the obesity epidemic. 18 Soft drinks, alcoholic beverages and fast food tend to be calorie rich. In Britain, there has been a signi cant rise in the amount of ...
Conclusion. In conclusion, obesity is a complex issue with multiple causes and significant effects on individuals and society. Poor dietary habits, sedentary lifestyles, and genetic factors contribute to its prevalence. The health consequences, economic costs, and social and psychological effects of obesity are profound and demand attention.
Obesity is a complex phenomenon which relates to social, environmental, economic, and cultural trends. Acknowledging this in your essay will show that you understand the subject. Moreover, researching various aspects of obesity may give you ideas on improving your arguments.
Introduction. The history of obesity over the last 100 or more years has been an exciting time for those of involved in the field. The scientific underpinnings have increased dramatically and ...
Obesity is a complex disease that occurs when an individual's weight is higher than what is considered healthy for his or her height. Obesity affects children as well as adults. Many factors can contribute to excess weight gain including eating patterns, physical activity levels, and sleep routines. Social determinants of health, genetics ...
Guest Essay. Scientists Don't Agree on What Causes Obesity, but They Know What Doesn't. Nov. 21, 2022. Credit... Hayley Wall. Share full article. By Julia Belluz. Ms. Belluz is a health ...
Obesity can also cause respiratory problems, sleep apnea, and osteoarthritis. Obesity is linked to various psychological problems such as depression, anxiety, and low self-esteem. The stigma associated with obesity can lead to social rejection, discrimination, and negative body image. These psychological problems can reduce the quality of life ...
These can include heart disease, diabetes, high blood pressure, high cholesterol, liver disease, sleep apnea and certain cancers. There are many reasons why some people have trouble losing weight. Often, obesity results from inherited, physiological and environmental factors, combined with diet, physical activity and exercise choices.
We know that obesity is a combination of genetic and epigenetic factors. People are eating highly processed, pesticide-laden foods with excessive amounts of high-fructose corn syrup, salt, junk ...
The main cause of obesity is junk food and an unbalanced diet rich in simple carbohydrates, fats, and sugars, plus a bunch of additives. Manufactured, processed, refined, and packaged meals are the most popular. Thanks to advances in technology, Americans have come to mass-produce meals that keep fresh longer and taste better.
Debates about whether it is our eating or activity that is more important as a cause of obesity, or whether preventing obesity is a personal or societal responsibility are unhelpful, and can only serve to distract us from acting to address the obesity epidemic.
Essay on obesity! Find high quality essays on 'Obesity' especially written for school, college, science and medical students. These essays will also guide you to learn about the causes, factors, treatment, management and complications related to obesity. Obesity is a chronic health condition in which the body fat reaches abnormal level.
Certain health behaviors can contribute to excess weight gain and are risk factors for obesity: Lack of physical activity. Unhealthy eating patterns such as: Too many highly processed foods or added sugars, including too many sugar-sweetened beverages. Too little fiber and fruits and vegetables. Not enough sleep or poor quality sleep.
In this essay I will be addressing why obesity is an important subject within health and wellbeing at present. Obesity still affects around one in four people that are adults and one in every 5 children around the ages of ten to eleven years old that live within the United Kingdom. ... The main cause of obesity is by consuming so much calories ...
Becky McCall. May 17, 2024. 0. VENICE, ITALY — Differences in how adipose tissue responds to insulin may account for why type 2 diabetes is more common in men than in women with obesity ...
They quickly lost almost all interest in the healthy food, and the restraint they used to show around healthy food disappeared. Within six weeks, their obesity rates soared. After this change, Dr ...
The Global Epidemic of Obesity: Causes, Effects, and Solutions Essay In recent years, the issue of obesity has become a global epidemic. Obesity is a condition where a person has an excessive amount of fat, which can lead to numerous health problems.
data suggests that inhaled particulate matter (such as pollution) plus obesity, is associated with ibrosis compared to either alone. This means that obesity may increase the risk of toxin exposure by acting as a depot or a sink. One of the patients enrolled in our study is an 18-year-old Hispanic male college student. He does
The Treat and Reduce Obesity Act (TROA), a bipartisan initiative, is crucial in providing Medicare beneficiaries access to effective treatments for obesity. Given the strong correlation between obesity and liver disease, this bill would provide crucial tools to address this urgent public health issue.
A diet that is poor in plant products and rich in meat, refined grains, sugar, and salt is associated with higher risk of death. Reducing consumption of animal-based products in favor of plant ...