Get the Reddit app
This subreddit is for discussing academic life, and for asking questions directed towards people involved in academia, (both science and humanities).

Taking a leave of absence from the PhD due to mental illness
I'm in my second-year of a humanities PhD at a top-ranked university in Canada. I've struggled with mental illness throughout my entire life (diagnosed bipolar disorder) and feel as if my health has just gotten worse during this program and especially during the pandemic. I've dealt with these issues before, including having had to take a few months off during my undergraduate studies after being hospitalized. I really thrived during the MA, but I think that was in part because less was expected of me than during the PhD and there was a clear end in sight (my MA program was only 12 months whereas average time to completion of my PhD program is over 7 years and often goes beyond the guaranteed funding period).
Over the past year and a half, I've noticed I've been ignoring my mental well-being in order to keep up with constant deadlines, research, writing, TAing and RAing duties, administrative responsibilities, etc., that I am just burning out and am not sure if finishing this program is even worth it (especially considering I've been doubting recently if I want to be in academia). I think it might be in my best interest to take a leave of absence for a semester or two in order to get my shit together. I've already finished coursework and would take time off after I complete my qualifying field exams in the summer. I would be ABD at this point.
TL;DR: Basically, I was wondering if there were those out there who took a LOA (especially because of mental illness) and what you did during your time off, and ultimately why or why didn't you decide to return to the PhD program?
Thanks for visiting! GoodRx is not available outside of the United States. If you are trying to access this site from the United States and believe you have received this message in error, please reach out to [email protected] and let us know.
Stack Exchange Network
Stack Exchange network consists of 183 Q&A communities including Stack Overflow , the largest, most trusted online community for developers to learn, share their knowledge, and build their careers.
Q&A for work
Connect and share knowledge within a single location that is structured and easy to search.
How to take a mental health related leave of absence (immediately before quals) without revealing mental illness to advisor
Recently due to burn out, my physical and mental health have been deteriorating to the point where I believe I need several months of leave to recover before I can be at a point where I can function normally again. I have been seeing a counsellor. However, now is a particularly 'bad' time to take leave because my PhD qualifying exams (first attempt) is very soon and in the month following, I have conferences/academic travels planned (which are great opportunities for furthering my career that my advisor has offered to me instead of to other students). Any one of these is enough exertion that I serious doubts that my physical and mental health will be recoverable afterwards, which makes me determined to take leave now, before it is too late. However, I am aware that having both these plans disrupted with short notice will not make my advisor or my department happy. Furthermore, while my relationship with my advisor is currently fine, it is not close enough that I feel comfortable confiding in him that I have a mental illness. His personality traits make me suspect that he might either not be particularly sympathetic/understanding, or he will be too afraid to 'break' me in the future. Therefore, I would prefer that the department and my advisor do not know that this leave of absence is due to mental health.
However, I need a compelling reason for the leave to be approved at this point in my studies and to have my qualifiers shifted to an unorthodox later date. My family are supportive of my decision for taking leave and have offered to invent some sort of family emergency which I can use as an excuse. However, my family are overseas, which is a fact known to both my advisor and my department (I am one of very few international students), yet I hope to be able to stay here during leave, where I have the support of both my husband and counsellor. We live close to campus and the counsellor is on campus in a small campus. So I am afraid that if I lie that I need to leave immediately for a family emergency, that during the time of my leave, my advisor/department secretary/chair will see me walking around campus and this might cause problems.
Are there any potential valid justifications for a leave of absence which do not mean that I have to mention mental illness, or leave the country? I will also be discussing this with my counsellor, but perhaps someone here has a clever idea that I have completely missed. Also it would be helpful for me if people can provide me with context/comparisons for just how bad/uncommon it would be to 1) take a leave of absence shortly before a qualifying exam (from the view of the department and advisor) and 2) take a leave of absence that disrupts travel plans where so far no money has been spent (from the view of the advisor), so that I can have some expectation of the resistance I might encounter.
- 6 I would not condone lying in this situation, talk to your advisor. – Solar Mike Apr 25, 2019 at 12:09
- This would honestly be one of the first lies I have ever told. I would also prefer to avoid lying, but questions like academia.stackexchange.com/questions/97439/… and academia.stackexchange.com/questions/77908/… and a suspicion he might ask me to just get over the next few months (and judge me harshly if I do not) make me very reluctant to be honest with him. – user108113 Apr 25, 2019 at 12:34
- 1 I have seen many students start with a lie and watch it unravel... Really causes more grief than you think it solves. – Solar Mike Apr 25, 2019 at 12:35
- 1 An on-campus counsellor should know the procedures for taking a leave of absence. If you have not done so already, I suggest getting their advice on this. They know more than any of us can about your university's policies and procedures, and your mental state. – Patricia Shanahan Apr 25, 2019 at 13:37
- Will you have visa issues as an international student if you try to stay in country while on leave from college? If you are not sure, discuss this on expatriates . You can just say you need the leave for medical reasons. – Patricia Shanahan Apr 25, 2019 at 13:40
Have you considered asking for leave due to "urgent health-related issues" without providing more detail than you feel comfortable providing? There is no need to explain exactly what issues you are dealing with at the moment. It is perfectly sufficient to state convincingly -- perhaps with supporting documents from a medical doctor or other health professional -- that the issue is urgent and requires that you take leave as soon as possible. How you phrase this is something to discuss with your counselor.
Personally, I don't think it's reasonable, when your mental health is at stake, to agonize over what your adviser might or might not think of you. Chances are they will be understanding and appreciate that you come to them now and not later, when your health has deteriorated further and more work has piled up. By contrast, if your adviser turns out to be unsupportive or worse, it's time for you to look for someone else to work with! Also this is worth finding out sooner rather than later, so you may see this request as a litmus test of your adviser's qualities.
As another aside, brooding over other people's impression of you is a habit that isn't conducive to mental well-being. I suggest talking this over with your counselor as well, and finding a way to assert your needs and boundaries with confidence. It will come in handy later in your (academic) career.
- +1. It´s a urgent health issue, period. Details are non of anyone´s business. – asquared Apr 25, 2019 at 13:38
- Thank you for your answer. The form for applying for a leave of absence differentiates between medical issues and psychological ones, so I would need to be specific. But yes, I could still go with the 'urgent mental health issue' line. – user108113 Apr 25, 2019 at 13:44
- And since you have physical health issues, you could just mention those if you wanted to. But that's entirely your choice. – jaia Apr 27, 2019 at 0:55
You must log in to answer this question.
Hot network questions.
- Effects if a human was shot by a femtosecond laser
- Can we find the equivalent resistance just by using series and parallel combinations?
- Why do airplanes sometimes turn more than 180 degrees after takeoff?
- Isomorphism of topological groups
- are "I will check your homework later" and "I will check on your homework later" similar?
- How to use cp's --update=none-fail option
- How much extra did a color RF modulator cost?
- Test for multicollinearity with binary and continuous independent variables
- Do you have an expression saying "when you are very hungry, bread is also delicious for you" or similar one?
- Can LLMs have intention?
- Who are the mathematicians interested in the history of mathematics?
- Why does the proposed Lunar Crater Radio Telescope suggest an optimal latitude of 20 degrees North?
- Is it legal to deposit a check that says pay to the order of cash
- How might a physicist define 'mind' using concepts of physics?
- Find the most isolated point
- unable to ping my router from outside
- Calculating Living Area on a Concentric Shellworld
- What is the U.N. list of shame and how does it affect Israel which was recently added?
- How to justify formula for area of triangle (or parallelogram)
- incorrect signature: void getDescribe() from the type Schema.DescribeFieldResult
- What’s the history behind Rogue’s ability to touch others directly without harmful effects in the comics?
- Transformer with same size symbol meaning
- LilyPond: tuplet bars don't seem to match time used
- Prove that "max independent set is larger than max clique" is NP-Hard
/images/cornell/logo35pt_cornell_white.svg" alt="mental health leave phd"> Cornell University --> Graduate School
Health leave.
Cornell recognizes that medical and mental health conditions can interfere with a student’s ability to be academically successful. Taking a health leave of absence (HLOA) provides students with a break from their studies to attend to treatment or management of a health condition. Any Cornell student can request to take an HLOA. The university’s goal is to enable students to address their health needs and return to complete their academic program.
In essence, a health leave of absence is a voluntary separation from the university for health reasons and allows the student to “stop the clock” on academic responsibilities while prioritizing health needs.
In some cases, reasonable accommodations may enable a student to complete academic coursework and remain on campus rather than taking an HLOA. A physical or mental impairment that substantially limits one or more major life activities is considered a disability and may warrant accommodations. A person who has a history of such an impairment or who is perceived by others as having such an impairment may also be eligible for accommodations (ADA). All students who are considering an HLOA are encouraged to consult with Student Disability Services to discuss eligibility for accommodations before requesting an HLOA.
Only the student can initiate the voluntary process. Graduate and professional students should be informed of the health leave of absence status, especially if health is negatively impacting academic performance.
Details about the health leave of absence process are available .
Any student who may be interested in initiating a health leave of absence should seek guidance from their health care provider, the Health Leaves Coordinator ( [email protected] ), or the Graduate School to help determine when this course of action is appropriate. Some common signs that a health leave might be beneficial include:
- Your medical condition has made it difficult for you to focus or concentrate.
- Your medical condition has left you lacking the motivation needed to successfully pursue graduate studies.
- Your medical condition has made it difficult to complete your academic or research requirements.
Often graduate and professional students will take a health leave of absence when:
- The individual students believe this is the best course of action for them.
- There has been a medical assessment from a provider who has recommended that the student take a break from their academic pursuits.
- Before the quality of their academic responsibilities suffer and becomes noticeable by the faculty. Typically, faculty members are very helpful and supportive when health is a concern; however, there can be limits to how long they are able to be supportive if your lack of academic progress due to health issues continues for an extended period of time. Aim to time a health leave to occur when you, your Special Committee Chair, and your DGS are in productive communications about your future academic plans.
Length of leave
The duration of the leave will depend upon the time you need for treatment and/or recovery, along with the resolution of any academic conditions determined by your graduate program.
The Graduate School allows health leave of absence status at increments of 12 months with a possible annual renewal for up to four years total. Depending on your academic program will determine the flexibility of when you will be able to return. You may not return from a leave within the semester that the leave was taken and you must return at the start of the Fall, Spring or Summer semesters.
For F-1 and J-1 International Students – Please note that if you choose to remain in the U.S. during your leave, you will need to maintain your student visa status. A reduced course load (i.e. health leave) is permitted for up to 12 months. For each semester of medical leave, you must provide medical documentation from a licensed medical doctor, doctor of osteopathy, or licensed clinical psychologist to substantiate the illness or medical condition. Please consult with the Office of Global Learning if you have more questions about the impact health leave of absence will have on your immigration status.
Time to degree
Time away does not count toward time to degree.
Financial support
Financial support is not available to a student on a health leave. By policy, “Students returning from approved health leave of absence within the four-year window are guaranteed any financial support remaining from their original offer of admission modified by any written changes to the financial commitment made prior to the health leave of absence, although the specific duties associated with that support may be adjusted and the return shall be timed to coincide with normal funding cycles.” Note: For U.S. citizens with educational loans, the repayment grace period starts the date the loans become active.
Cornell access
While you are on an HLOA, you will not be a registered student. This will have an impact on your access to university services, but there are some resources, particularly on the Ithaca campus, that students on HLOA can continue to use.
In brief, if you are on a health leave, you will no longer have access to campus facilities and services that you would normally access with your NetID. However, your Cornell email will remain for the duration of your health leave of absence. You may request library privileges with support from your academic advisor and director of graduate studies, and pay any applicable fees.
Health insurance
Review your health insurance coverage to find out how it might be impacted by an HLOA.
- Students who take HLOA mid-plan year may retain their Student Health Plan (SHP) coverage through the end of the plan year (through June 30). Visit the Student Health Benefits website or contact the Office of Student Health Benefits at [email protected] for detailed guidance about options for extending coverage.
- If you have another health insurance plan, contact the plan provider to clarify coverage using the phone number on your insurance card. In some cases, you may need to apply for continuation of coverage.
Access at Cornell Health
Students who are on a health leave of absence are not eligible to use Cornell Health services (including both medical and mental health services), except for pharmacy. If you elect to go on a health leave of absence, Cornell Health will be able to aid in transferring care from Cornell Health to other providers in the community and beyond. This is true for all students on a health leave regardless of individual health insurance plan.
International students
Taking a leave of absence may have implications for an international student’s visa status. If you are on an F-1 or J-1 student visa, you will need written documentation from a health care provider recommending a leave of absence or reduced course load for medical or mental health reasons. Immigration rules for a health leave of absence or reduced course load may not coincide with Cornell’s health leave requirements and limitations. Please contact the Office of Global Learning to discuss the impact of an HLOA on your visa status.
Academic plan
An important part of the process in taking a health leave of absence is that each graduate and professional degree student will receive an academic plan that is expected to be completed prior to returning to registered student status. The purpose of the academic plan is to:
- Determine if you have any outstanding academic work that should be addressed prior to returning from a health leave. It is not meant to be punitive or represent additional work, but instead should address delays or poor academic performance to any academic milestones that likely could not be addressed due to your health while here. Examples include incomplete coursework, drafts of outstanding papers, etc.
- Reiterate any future academic expectations to allow you to fully understand what would be expected upon return. Examples include timing of exams, additional required coursework, etc.
- Any specific needs that supports a smooth transition back into the program. Examples include informing program with plans to return (i.e. needing x months of lead time to secure funding), when a student can return (i.e. only x semester because of course sequencing), etc.
The plan may state that there is nothing academically for you to do during a health leave of absence but take care of health.
Initiating the health leave of absence process
The complete steps to initiate the process are outlined on the Student Disability Services (SDS) Health Leave of Absence webpage .
If you don’t know where to start or whom to contact, please email the Health Leaves Coordinator at [email protected] , who will work with you to facilitate consultations between you, your health care provider, SDS, and your college/school before granting a health leave of absence. If you would like to discuss your situation confidentially and evaluate all options in managing health with your academics and are not sure where to start, please contact Janna Lamey ( [email protected] ).
Return from the health leave of absence
When you are ready to return from an HLOA, you will need to complete a series of administrative processes that is outlined on the SDS HLOA webpage . You will need to make the request through the Health Leaves Coordinator, submit documentations that indicates your fitness to resume your education at Cornell, confirmation that your academic plan has been successfully completed, and consult with the Health Leaves Coordinator, SDS, Graduate School, and a health care provider. While requests to return from a health leave of absence will be accepted on a rolling basis to offer flexibility and accommodate each student’s individual health situation and academic program, please note the deadlines outlined.
Learn more about health leaves
- Read Student Disability Services Health Leave of Absence page
- Read University Policy 7.1 on voluntary leaves of absence for students
- Contact Cornell Health Leaves Coordinator ( [email protected] )
- Contact Janna Lamey ( [email protected] ), associate dean for graduate student life
See the complete FAQ .
- Graduate and Professional Student Parental Accommodation, Policy 1.6
- Graduate Student Assistantships, Policy 1.3
- Cornell Student Disability Services Office
Janna Lamey Associate Dean for Graduate Student Life [email protected]

‘You have to suffer for your PhD’: poor mental health among doctoral researchers – new research
Lecturer in Social Sciences, University of Westminster
Disclosure statement
Cassie Hazell has received funding from the Office for Students.
University of Westminster provides funding as a member of The Conversation UK.
View all partners
PhD students are the future of research, innovation and teaching at universities and beyond – but this future is at risk. There are already indications from previous research that there is a mental health crisis brewing among PhD researchers.
My colleagues and I studied the mental health of PhD researchers in the UK and discovered that, compared with working professionals, PhD students were more likely to meet the criteria for clinical levels of depression and anxiety. They were also more likely to have significantly more severe symptoms than the working-professional control group.
We surveyed 3,352 PhD students, as well as 1,256 working professionals who served as a matched comparison group . We used the questionnaires used by NHS mental health services to assess several mental health symptoms.
More than 40% of PhD students met the criteria for moderate to severe depression or anxiety. In contrast, 32% of working professionals met these criteria for depression, and 26% for anxiety.
The groups reported an equally high risk of suicide. Between 33% and 35% of both PhD students and working professionals met the criteria for “suicide risk”. The figures for suicide risk might be so high because of the high rates of depression found in our sample.
We also asked PhD students what they thought about their own and their peers’ mental health. More than 40% of PhD students believed that experiencing a mental health problem during your PhD is the norm. A similar number (41%) told us that most of their PhD colleagues had mental health problems.
Just over a third of PhD students had considered ending their studies altogether for mental health reasons.
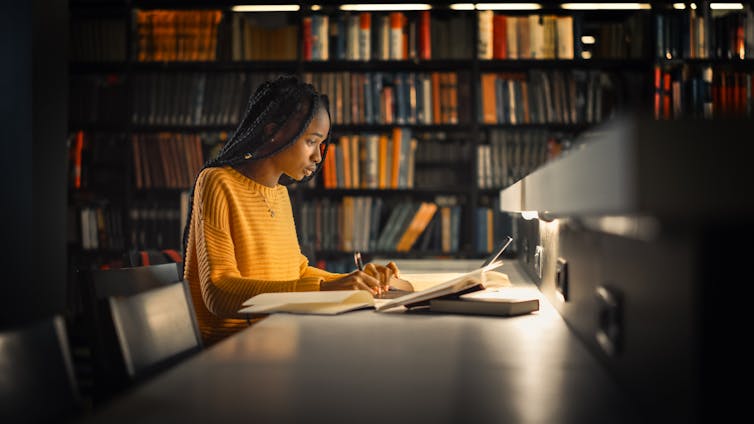
There is clearly a high prevalence of mental health problems among PhD students, beyond those rates seen in the general public. Our results indicate a problem with the current system of PhD study – or perhaps with academic more widely. Academia notoriously encourages a culture of overwork and under-appreciation.
This mindset is present among PhD students. In our focus groups and surveys for other research , PhD students reported wearing their suffering as a badge of honour and a marker that they are working hard enough rather than too much. One student told us :
“There is a common belief … you have to suffer for the sake of your PhD, if you aren’t anxious or suffering from impostor syndrome, then you aren’t doing it "properly”.
We explored the potential risk factors that could lead to poor mental health among PhD students and the things that could protect their mental health.
Financial insecurity was one risk factor. Not all researchers receive funding to cover their course and personal expenses, and once their PhD is complete, there is no guarantee of a job. The number of people studying for a PhD is increasing without an equivalent increase in postdoctoral positions .
Another risk factor was conflict in their relationship with their academic supervisor . An analogy offered by one of our PhD student collaborators likened the academic supervisor to a “sword” that you can use to defeat the “PhD monster”. If your weapon is ineffective, then it makes tackling the monster a difficult – if not impossible – task. Supervisor difficulties can take many forms. These can include a supervisor being inaccessible, overly critical or lacking expertise.
A lack of interests or relationships outside PhD study, or the presence of stressors in students’ personal lives were also risk factors.
We have also found an association between poor mental health and high levels of perfectionism, impostor syndrome (feeling like you don’t belong or deserve to be studying for your PhD) and the sense of being isolated .
Better conversations
Doctoral research is not all doom and gloom. There are many students who find studying for a PhD to be both enjoyable and fulfilling , and there are many examples of cooperative and nurturing research environments across academia.
Studying for a PhD is an opportunity for researchers to spend several years learning and exploring a topic they are passionate about. It is a training programme intended to equip students with the skills and expertise to further the world’s knowledge. These examples of good practice provide opportunities for us to learn about what works well and disseminate them more widely.
The wellbeing and mental health of PhD students is a subject that we must continue to talk about and reflect on. However, these conversations need to happen in a way that considers the evidence, offers balance, and avoids perpetuating unhelpful myths.
Indeed, in our own study, we found that the percentage of PhD students who believed their peers had mental health problems and that poor mental health was the norm, exceeded the rates of students who actually met diagnostic criteria for a common mental health problem . That is, PhD students may be overestimating the already high number of their peers who experienced mental health problems.
We therefore need to be careful about the messages we put out on this topic, as we may inadvertently make the situation worse. If messages are too negative, we may add to the myth that all PhD students experience mental health problems and help maintain the toxicity of academic culture.
- Mental health
- Academic life
- PhD research

Head of School, School of Arts & Social Sciences, Monash University Malaysia

Chief Operating Officer (COO)

Clinical Teaching Fellow

Data Manager

Director, Social Policy
Mental Health, PhD
Bloomberg school of public health, phd program description.
The PhD program is designed to provide key knowledge and skill-based competencies in the field of public mental health. To gain the knowledge and skills, all PhD students will be expected to complete required coursework, including courses that meet the CEPH competency requirements and research ethics; successfully pass the departmental comprehensive exam; select and meet regularly with a Thesis Advisory Committee (TAC) as part of advancing to doctoral candidacy; present a public seminar on their dissertation proposal; successfully pass the departmental and school-wide Preliminary Oral Exams; complete a doctoral thesis followed by a formal school-wide Final Oral Defense; participate as a Teaching Assistant (TA); attend Grand Rounds in the Department of Psychiatry; and provide a formal public seminar on their own research. Each of these components is described in more detail below. The Introduction to Online Learning course is taken before the start of the first term.
Department Organization
The PhD Program Director, Dr. Rashelle Musci ( [email protected] ), works with the Vice-Chair for Education, Dr. Judy Bass ( [email protected] ), to support new doctoral students, together with their advisers, to formulate their academic plans; oversee their completion of ethics training; assist with connections to faculty who may serve as advisers or sources for data or special guidance; provide guidance to students in their roles as teaching assistants; and act as a general resource for all departmental doctoral students. The Vice-Chair also leads the Department Committee on Academic Standards and sits on the School Wide Academic Standards Committee. Students can contact Drs. Musci or Bass directly if they have questions or concerns.
Within the department structure, there are several standing and ad-hoc committees that oversee faculty and student research, practice and education. For specific questions on committee mandate and make-up, please contact Dr. Bass or the Academic Program Administrator, Patty Scott, [email protected] .
Academic Training Programs
The Department of Mental Health houses multiple NIH-funded doctoral and postdoctoral institutional training programs:
Psychiatric Epidemiology Training (PET) Program
This interdisciplinary doctoral and postdoctoral program is affiliated with the Department of Epidemiology and with the Department of Psychiatry and Behavioral Sciences at the School of Medicine. The Program is co-directed by Dr. Peter Zandi ( [email protected] ) and Dr. Heather Volk ( [email protected] ). The goal of the program is to increase the epidemiologic expertise of psychiatrists and other mental health professionals and to increase the number of epidemiologists with the interest and capacity to study psychiatric disorders. Graduates are expected to undertake careers in research on the etiology, classification, distribution, course, and outcome of mental disorders and maladaptive behaviors. The Program is funded with a training grant from the National Institute of Mental Health.
Pre-doctoral trainees are required to take the four-term series in Epidemiologic Methods (340.751-340.754), as well as the four-term series in Biostatistics (140.621-624). In addition to the other departmental requirements for the doctoral degree, pre-doctoral trainees must also take four advanced courses in one of the domains of expertise they have selected to pursue: Genetic and Environmental Etiology of Mental Disorders, Mental Health Services and Outcomes, Mental Health and Aging, and Global Mental Health. Pre-doctoral trainees should consult with their adviser and the program director to select courses consistent with their training goals.
Postdoctoral fellows take some courses, depending on background and experience, and engage in original research under the supervision of a faculty member. They are expected to have mastery of the basic principles and methods of epidemiology and biostatistics. Thus, fellows are required to take 340.721 Epidemiologic Inference in Public Health, 330.603 Psychiatric Epidemiology, and some equivalent of 140.621 Statistical Methods in Public Health I and 140.622 Statistical Methods in Public Health II. They may be waived from these requirements by the program director if they can demonstrate equivalent prior coursework.
Drug Dependence Epidemiology Training (DDET) Program
This training program is co-led by Dr. Renee M. Johnson ( [email protected] ) and Dr. Brion Maher ( [email protected] ). The DDET program is designed to train scientists in the area of substance use and substance use disorders. Research training within the DDET Program focuses on: (1) genetic, biological, social, and environmental factors associated with substance use, (2) medical and social consequences of drug use, including HIV/AIDS and violence, (3) co-morbid mental health problems, and (4) substance use disorder treatment and services. The DDET program is funded by the NIH National Institute on Drug Abuse.
The program supports both pre-doctoral and postdoctoral trainees. Pre-doctoral trainees have a maximum of four years of support on the training grant. After completing required coursework, pre-doctoral trainees are expected to complete original research under the supervision of a faculty member affiliated with the DDET program. Postdoctoral trainees typically have two years of support on the training grant. They are required to engage in original research on a full-time basis, under the supervision of a DDET faculty member. Trainees’ research projects must be relevant to the field of substance use.
All trainees are required to attend a weekly seminar series focused on career development and substance use research. The DDET program supports trainees’ attendance at relevant academic meetings, including the Annual Meeting of the College on Problems of Drug Dependence (CPDD) each June. Training grant appointments are awarded annually and are renewable given adequate progress in the academic program, successful completion of program and departmental requirements, and approval of the training director.
Pre-doctoral trainees are required to take the required series in epidemiology and biostatistics, as well as The Epidemiology of Substance Use and Related Problems (330.602). In addition, they must take three advanced courses that enhance skills or content expertise in substance use and related problems: one in epidemiology (e.g., HIV/AIDS epidemiology), one in biostatistics, and one in social and behavioral science or health policy. The most appropriate biostatistics course will provide instruction on a method the trainee will use during the thesis research (e.g., survival analysis, longitudinal analysis methods). (Course requirements for trainees from other departments will be decided on a case-by-case basis.)
Postdoctoral trainees are expected to enter the program with mastery of the basic principles and methods of epidemiology and biostatistics. They are required to take The Epidemiology of Substance Use and Related Problems in their first year (330.602), as well as required ethics courses. Postdoctoral trainees are encouraged to take courses in scientific writing and grant writing.
Global Mental Health Training (GMH) Program
The Global Mental Health Training (GMH) Program is a training program to provide public health research training in the field of Global Mental Health. It is housed in the Department of Mental Health , in collaboration with the Departments of International Health and Epidemiology. The GMH Program is supported by a T32 research training grant award from the National Institute of Mental Health (NIMH). Dr. Judy Bass ( [email protected] ) is the training program director.
As part of this training program, trainees will undertake a rigorous program of coursework in epidemiology, biostatistics, public mental health and global mental health, field-based research experiences, and integrative activities that will provide trainees with a solid foundation in the core proficiencies of global mental health while giving trainees the opportunity to pursue specialized training in one of three concentration areas that are recognized as high priority: (1) Prevention Research; (2) Intervention Research; or (3) Integration of Mental Health Services Research.
Pre-doctoral trainees are required to take the required series in epidemiology and biostatistics and department of mental health required courses. In addition, they must take three courses that will enhance skills and content expertise in global mental health: 330.620 Qualitative and Quantitative Methods for Mental Health and Psychosocial Research in Low Resource Settings, 224.694 Mental Health Intervention Programming in Low and Middle Income Countries, and 330.680 Promoting Mental Health and Preventing Mental Disorder in Low and Middle Income Countries.
The Mental Health Services and Systems (MHSS) Program
The Mental Health Services and Systems (MHSS) program is an NIMH-funded T32 training program run jointly by the Department of Mental Health and the Department of Health Policy and Management and also has a close affiliation with the Johns Hopkins School of Medicine. Drs. Elizabeth Stuart ( [email protected] ) and Ramin Mojtabai ( [email protected] ) are the training program co-directors.
The goal of the MHSS Program is to train scholars who will become leaders in mental health services and systems research. This program focuses on producing researchers who can address critical gaps in knowledge with a focus on: (1) how healthcare services, delivery settings, and financing systems affect the well-being of persons with mental illness; (2) how cutting-edge statistical and econometric methods can be used in intervention design, policies, and programs to improve care; and (3) how implementation science can be used to most effectively disseminate evidence-based advances into routine practice. The program strongly emphasizes the fundamental principles of research translation and dissemination throughout its curriculum.
Pre-doctoral trainees in the MHSS program are expected to take a set of core coursework in epidemiology and biostatistics, 5 core courses related to the core elements of mental health services and systems (330.662: Public Mental Health, 330.664: Introduction to Mental Health Services, 140.664: Causal Inference in Medicine and Public Health, 550.601: Implementation Research and Practice, and 306.665: Research Ethics and Integrity), and to specialize in one of 3 tracks: (1) health services and economics; (2) statistics and methodology; or (3) implementation science applied to mental health. Trainees are also expected to participate in a biweekly training grant seminar every year of the program and take a year-long practicum course exposing them to real-world mental health service systems and settings.
For more details see this webpage: http://www.jhsph.edu/research/centers-and-institutes/center-for-mental-health-and-addiction-policy-research/training-opportunities/
Epidemiology and Biostatistics of Aging
This program offers training in the methodology and conduct of significant clinical- and population-based research in older adults. This training grant, funded by the National Institute on Aging, has the specific mission to prepare epidemiologists and biostatisticians who will be both leaders and essential members of the multidisciplinary research needed to define models of healthy, productive aging and the prevention and interventions that will accomplish this goal. The Associate Director of this program is Dr. Michelle Carlson ( [email protected]) .
The EBA training grant has as its aims:
- Train pre- and post-doctoral fellows by providing a structured program consisting of: a) course work, b) seminars and working groups, c) practica, d) directed multidisciplinary collaborative experience through a training program research project, and e) directed research.
- Ensure hands-on participation in multidisciplinary research bringing trainees together with infrastructure, mentors, and resources, thus developing essential skills and experience for launching their research careers.
- Provide in-depth knowledge in established areas of concentration, including a) the epidemiology and course of late-life disability, b) the epidemiology of chronic diseases common to older persons, c) cognition, d) social epidemiology, e) the molecular, epidemiological and statistical genetics of aging, f) measurement and analysis of complex gerontological outcomes (e.g, frailty), and g) analysis of longitudinal and survival data.
- Expand the areas of emphasis to which trainees are exposed by developing new training opportunities in: a) clinical trials; b) causal inference; c) screening and prevention; and d) frailty and the integration of longitudinal physiologic investigation into epidemiology.
- Integrate epidemiology and biostatistics training to form a seamless, synthesized approach whose result is greater than the sum of its parts, to best prepare trainees to tackle aging-related research questions.
These aims are designed to provide the fields of geriatrics and gerontology with epidemiologists and biostatisticians who have an appreciation for and understanding of the public health and scientific issues in human aging, and who have the experience collaborating across disciplines that is essential to high-quality research on aging. More information can be found at: https://coah.jhu.edu/graduate-programs-and-postdoctoral-training/epidemiology-and-biostatistics-of-aging/ .
Aging and Dementia Training Program
This interdisciplinary pre- and post-doctoral training program is an interdisciplinary program, funded by the National Institute on Aging, affiliated with the Department of Neurology and the Department of Psychiatry at the School of Medicine, the Department of Mental Health at the School of Public Health and the Department of Psychology and Brain Sciences at the School of Arts and Sciences. The Department of Mental Health contact is Dr. Michelle Carlson ( [email protected] ). The goal of this training program is to train young investigators in age-related cognitive and neuropsychiatric disorders.
Program Requirements
Course location and modality is found on the BSPH website .
Residence Requirements
All doctoral students must complete and register for four full-time terms of a regular academic year, in succession, starting with Term 1 registration in August-September of the academic year and continuing through Term 4 ending in May of that same academic year. Full-time registration entails a minimum of 16 credits of registration each term and a maximum of 22 credits per term.
Full-time residence means more than registration. It means active participation in department seminars and lectures, research work group meetings, and other socializing experiences within our academic community. As such, doctoral trainees are expected to be in attendance on campus for the full academic year except on official University holidays and vacation leave.
Course Requirements
Not all courses are required to be taken in the first year alone; students typically take 2 years to complete all course requirements.
Students must obtain an A or B in all required courses. If a grade of C or below is received, the student will be required to repeat the course. An exception is given if a student receives a C (but not a D) in either of the first two terms of the required biostatistics series, but then receives a B or better in both of the final two terms of the series; then a student will not be required to retake the earlier biostatistics course. However, the student cannot have a cumulative GPA lower than 3.0 to remain in good academic standing. Any other exceptions to this grade requirement must be reviewed and approved by the departmental CAS and academic adviser.
Below are the required courses for the PhD; further Information can be found on the PhD in Mental Health webpage.
BIOSTATISTICS
| Code | Title | Credits |
|---|---|---|
| Statistical Methods in Public Health I (first term) | 4 | |
| Statistical Methods in Public Health II (second term) | 4 | |
| Statistical Methods in Public Health III (third term) | 4 | |
| Statistical Methods in Public Health IV (fourth term) | 4 | |
| Total Credits | 16 | |
Must be completed to be eligible to sit for the departmental written comprehensive exams.
EPIDEMIOLOGY
| Code | Title | Credits |
|---|---|---|
| Epidemiologic Methods 1 (first term) | 5 | |
| Epidemiologic Methods 2 (second term) | 5 | |
| Epidemiologic Methods 3 (third term) | 5 |
DEPARTMENT OF MENTAL HEALTH COURSES
| Code | Title | Credits |
|---|---|---|
| Seminars in Research in Public Mental Health (all terms required for first year students) | 1 | |
| Psychopathology for Public Health (first term) | 3 | |
| Public Mental Health (first term) | 2 | |
| Psychiatric Epidemiology (second term) | 3 | |
| Social, Psychological, and Developmental Processes in the Etiology of Mental Disorders (third term) | 3 | |
| PREVENTION of MENTAL DISORDERS: PUBLIC HEALTH InterVENTIONS (third term) | 3 | |
| Introduction to Behavioral and Psychiatric Genetics (fourth term) | 3 | |
| Brain and Behavior in Mental Disorders (fourth term) | 3 | |
| Introduction to Mental Health Services (first term) | 3 | |
| The Epidemiology of Substance Use and Related Problems (second term) | 3 | |
| Statistics for Psychosocial Research: Measurement (first term) | 4 | |
| Grant Writing for the Social and Behavioral Sciences (fourth term) | 3 | |
| Writing Publishable Manuscripts for the Social and Behavioral Sciences (second year and beyond only - second term) | 2 | |
| Doctoral Seminar in Public Mental Health (2nd year PhD students only) | 1 | |
For Department of Mental Health doctoral students, a research paper is required entailing one additional course credit. PH.330.840 Special Studies and Research Mental Health listing Dr. Eaton as the mentor.
COURSE REQUIREMENTS OUTSIDE THE DEPARTMENT OF MENTAL HEALTH
The School requires that at least 18 credit units must be satisfactorily completed in formal courses outside the student's primary department. Among these 18 credit units, no fewer than three courses (totaling at least 9 credits) must be satisfactorily completed in two or more departments of the Bloomberg School of Public Health. The remaining outside credit units may be earned in any department or division of the University. This requirement is usually satisfied with the biostatistics and epidemiology courses required by the department.
Candidates who have completed a master’s program at the Bloomberg School of Public Health may apply 12 credits from that program toward this School requirement. Contact the Academic Office for further information.
SCHOOL-WIDE COURSES
Introduction to Online Learning taken before the first year.
ETHICS TRAINING
PH.550.860 Academic & Research Ethics at BSPH (0 credit - pass/fail) required of all students in the first term of registration.
Responsible Conduct of Research (RCR) connotes a broad range of career development topics that goes beyond the more narrowly focused “research ethics” and includes issues such as conflict of interest, authorship responsibilities, research misconduct, animal use and care, and human subjects research. RCR training requirements for JHPSH students are based on two circumstances: their degree program and their source of funding, which may overlap.
- All PhD students are required to take one of two courses in Responsible Conduct of Research, detailed below one time, in any year, during their doctoral studies.
- All students, regardless of degree program, who receive funding from one of the federal grant mechanisms outlined in the NIH notice below, must take one of the two courses listed below to satisfy the 8 in-person hours of training in specific topic areas specified by NIH (e.g., conflict of interest, authorship, research misconduct, human and animal subject ethics, etc.).
The two courses that satisfy either requirement are:
- PH.550.600 Living Science Ethics - Responsible Conduct of Research [1 credit, Evans]. Once per week, 1st term.
- PH.306.665 Research Ethics and integrity [3 credits, Kass]. Twice per week, 3rd term.
Registration in either course is recorded on the student’s transcript and serves as documentation of completion of the requirement.
- If a non-PhD or postdoctoral student is unsure whether or not their source of funding requires in-person RCR training, they or the PI should contact the project officer for the award.
- Students who have conflicts that make it impossible for them to take either course can attend a similar course offered by Sharon Krag at Homewood during several intensive sessions (sequential full days or half days) that meet either on weekends in October or April, a week in June, or intersessions in January. Permission is required. Elizabeth Peterson ( [email protected] ) can provide details on dates and times.
- Students who may have taken the REWards course (Research Ethics Workshops About Responsibilities and Duties of Scientists) in the SOM can request that this serve as a replacement, as long as they can provide documentation of at least 8 in-person contact hours.
- Postdoctoral students are permitted to enroll in either course but BSPH does not require them to take RCR training. However, terms of their funding might require RCR training and it is their obligation to fulfill the requirement.
- The required Academic Ethics module is independent of the RCR training requirement. It is a standalone module that must be completed by all students at the Bloomberg School of Public Health. This module covers topics associated with maintaining academic integrity, including plagiarism, proper citations, and cheating.
PhD in Mental Health
Department of Mental Health candidates for the degree Doctor of Philosophy (PhD) must fulfill all University and School requirements. These include, but are not limited to, a minimum of four consecutive academic terms at the School in full-time residency (some programs require 6 terms), continuous registration throughout their tenure as a PhD student, satisfactory completion of a Departmental Written Comprehensive Examination, satisfactory performance on a University Preliminary Oral Examination, readiness to undertake research, and preparation and successful defense of a thesis based upon independent research.
PhD Students are required to be registered full-time for a minimum of 16 credits per term and courses must be taken for letter grade or pass/fail. Courses taken for audit do not count toward the 16-credit registration minimum.
Students having already earned credit at BSPH from a master's program or as a Special Student Limited within the past three years for any of the required courses may be able to use them toward satisfaction of doctoral course requirements.
For a full list of program policies, please visit the PhD in Mental Health page where students can find more information and links to our handbook.
Completion of Requirements
The University places a seven-year maximum limit upon the period of doctoral study. The Department of Mental Health students are expected to complete all requirements in an average of 4-5 years.
Learning Outcomes
The PhD program is designed to provide key knowledge and skill-based competencies in the field of public mental health. Upon successful completion of the PhD in Mental Health, students will have mastered the following competencies:
- Evaluate the clinical presentations, incidence, prevalence, course and risk/protective factors for major mental and behavioral health disorders.
- Differentiate important known biological, psychological and social risk and protective factors for major mental and behavioral disorders and assess how to advance understanding of the causes of these disorders in populations.
- Evaluate and explain factors associated with resiliency and recovery from major mental and behavioral disorders.
- Evaluate, select, and implement effective methods and measurement strategies for assessment of major mental and behavioral disorders across a range of epidemiologic settings.
- Critically evaluate strategies for the prevention and treatment of major mental and behavioral disorders as well as utilization and delivery of mental health services over the life course, across a range of settings, and in a range of national contexts.
- Assess preventive and treatment interventions likely to prove effective in optimizing mental health of the population, reducing the incidence of mental and behavioral disorders, raising rates of recovery from disorders, and reducing risk of later disorder recurrence.
According to the requirements of the Council on Education for Public Health (CEPH), all BSPH degree students must be grounded in foundational public health knowledge. Please view the list of specific CEPH requirements by degree type .
- Mental Health
- PhD Stories
- Taking Time Off
How I took time out of my PhD to recover
- Posted by by Leafgrabbing
- 15. November 2019
- 7 minute read
After taking two months out of my PhD to reflect, heal and recharge, I have come back with a new focus. A new approach. A much more positive mental attitude. Here is what happened.
My purpose for taking on a PhD has maybe not always been the ‘right’ one. I applied because I was interested in pursuing research on my topic, which is woefully under-researched, particularly with regards to education in divided societies like Northern Ireland, where I come from. Awesome – tick! But, if I’m honest, another BIG push behind me starting a PhD was my fear that I wasn’t good enough to be a teacher, which was my original plan and education.
This fear came off the back of a comment made by another teacher during my first training placement – “maybe you should just think about lecturing adults” . The comment devastated me. Teaching has been the one job I ever really wanted to do. And, no matter the fact that I received an abundance of positive feedback on my teaching style (no one ever doubted my suitability for teaching at secondary level), this stuck with me.
Therefore, I entered into my PhD as a three (more than likely four) year trial that would test my intellect, will-power, endurance, and of course, my mental health .

Impostor syndrome takes its place in the backseat
From my low self-esteem, I adopted a blasé attitude to my work. I always met deadlines, I always did what needed to be done, but I treated my PhD like it was just a stop gap. I didn’t appreciate the position I was in. When I started to think about whether I wanted to do a PhD or not, I felt a deep-seated guilt for wasting the time of my supervisor, my colleagues… even for taking a place with funding that could have gone to someone more deserving.
My issue wasn’t that I didn’t want to do the PhD or that I wasn’t interested in my research. The issue was that I didn’t feel good enough. That I got here by a fluke. My reaction to that was to treat this like something that didn’t really matter or that I didn’t really care about. I had unwittingly been dealing with imposter syndrome .
I worked from home for the majority of my first and second year of research. I lived an hour away from campus and it was quite expensive to travel in every day. However, isolating myself only served to push my self-doubt further. I didn’t appreciate that I had an office full of supportive and encouraging colleagues, who, had I been more present, would have been the best motivation I could have asked for.
My turning point
Then came March 2019, when my world truly felt like it was crumbling around me.
On Sunday 24 th , I received a call from my mum to tell me that my best friend had committed suicide.
The term ‘best friend’ can be thrown about and may, at times, not really reflect the true depth of a friendship. This friend, my best friend, was my first friend. She was the sister I never had. I had never imagined a life without her. She knew everything there was to know about me. When I found out she was gone… I felt totally and completely lost. Incomplete. And for a time, I felt like there was no point to anything.

My supervisor’s reaction
During this time, my supervisor was a godsend. She was one of the first people I contacted when I heard the news. She was kind, empathetic and helped me through reorganising data collection commitments.
Once the dust had settled, she encouraged me to “stop the clock” and take time out of the PhD, so that I could grieve. Instead, I attempted to throw myself back into it.
Ignoring the pain takes its toll
I began preparing for my Annual Progress Review the week after my best friend’s funeral and scheduled in interviews and focus groups.
At the time, I felt like the quality of my data was deteriorating. I wasn’t able to engage as well as I should have with my participants during interviews. They became much more structured and closed – because my own mental health was severely declining.
In qualitative research, you MUST be able to engage with your participants. You must actively listen and ask pertinent, open questions while observing your use of language. When you feel as if you are limply grasping on to the edge of a cliff, this, unsurprisingly, can be difficult to do effectively.

Figuring out what is wrong
I didn’t really understand the influence my mental health was having on my work. Instead, I saw this episode as total incompetence on my side. On reflection, I didn’t fail during that time. The data I collected is not worthless, but, again, my self-doubt drove me to feeling I needed a way out of my PhD.
First, I sought counselling through my university. This was provided by an external organisation. Unfortunately, the counselling provided only allows for four sessions. While my counsellor was incredible, my grief and other issues could not adequately be addressed in such a short space of time. So, while I could give myself a pat on the back for trying, I hadn’t really sought out the level of help I truly needed.
Trying to run away from the problem
One important piece of advice: Do not make rash life-changing decisions while you are experiencing grief or mental health issues. Rather than trying to face my problems, I thought it best to run away.
My form of running away was to apply for a teaching position in my dream school. BIG mistake. During a period of all-time low self-esteem, inability to pick myself up and, in the immortal words of Taylor Swift, “shake it off”, I decided to throw sense to the wind. I was desperate to feel capable of something, to feel worthy. However, in my state at the time, I just opened myself to further disappointment. Needless to say, I didn’t get the job. I’m pretty sure I almost burst into tears during the interview. I had finally hit rock-bottom.
Upon receiving my rejection letter, I emailed my supervisor to ask for the period of temporary withdrawal that she had encouraged me to take long before then. She immediately got the ball rolling and I felt a little more free.
Taking time out of my PhD

My time off didn’t result in the honing of my painting skills, turn me into a guitar player or gain me a second-language. For the most part, I watched A LOT of Netflix and walked my dog around pretty places.
How you use your time really is up to you. I think now of all the things I could have done but I’m here, I feel stronger. Something worked. With my time, I did reflect on what I wanted to do with my life, why I was doing a PhD and what I could do to help myself.
What about quitting?
I flirted with the idea of quitting. My partner (the most patient man in the world) whole-heartedly supported me in whatever decision I wanted to make. However, it was only when I began opening up to friends about how I felt, that I finally started to get a bit of push back: “You only have a year left, why would you even think about leaving?”, “Are you mad?”, “That would be such a waste!” etc.

Initially, I was angry at them for not understanding how bad I felt, how demoralised I was and asking “why the hell weren’t they just patting me on the head and saying ‘there, there, pumpkin’”? I realised I had gotten used to being felt sorry for and it was only enabling my self-doubt and self-pity.
I’ve never told those friends how much they changed me that night but they really did. I decided I was going back to the PhD. I would give it another go. If I didn’t like it when I went back, well, at least I tried.
Being back after taking a break from my PhD
I did make some changes in the run up to starting back. I began to use a bullet journal. This gave me a little bit of a creative outlet while also encouraging me to set tasks and feel like I was able to achieve something, however small, every day.
I created a second Instagram account , removed from my friends or family, so that I could post whatever I wanted, whenever I wanted. I use it to post photos taken on those pretty dog walks and to be reflective regarding my journey through grief. I started exercising more regularly, walking, running, even a little yoga. I tried to adopt a more positive attitude.
I returned at the end of September 2019 and I’m still here.
I’ve recruited my last research site and participants – so I’m on my way to finishing data collection. I’ve attended a HEAP of training and workshops for postgraduates, including one on developing emotional intelligence and resilience – this one was amazing! I’ve started meeting up more with friends and fellow PhD students.
Where I arrived at
I’m trying to keep the positive attitude going and I am, genuinely, enjoying it. I’m in the office at least 4 days a week and I go to the gym regularly. I still have an immense source of support in my supervisor, who I try to be more honest with in terms of what I’m up to work-wise and any doubts I may be having.
I won’t say that my time off fixed everything, but it allowed me the space to grieve without feeling guilty about work. It allowed time to reflect on myself, on who I am and what I want. It gave me a fresh start at this whole PhD thing – at least, in terms of my own approach. I still have off days, but I don’t beat myself up about them or allow myself too much time to wallow.

Take time out of your PhD when you need it
My experience won’t be the same as yours, but maybe there are parts that resonate with you. My advice: Take time out of your PhD when you need it. Share your worries with people who will challenge you when you need to be challenged. Know that there is no shame in seeking professional help. Quitting is always an option but it’s not an easy way out. And, probably a little cliché but still – find a hobby that you actually enjoy.
Megan.
About the author
Megan is entering her third year of PhD study in Northern Ireland, within the field of education. She is Belfast born and bred and began her PhD straight after completing a teaching qualification in secondary education. Megan feels like she made some mistakes in the early days of her PhD, as we all do and wants to share her story about the time when she took time out of her PhD to help others who feel stuck.
What about you? Did you ever take time out of your PhD? Did it help you? Do you know someone who recovered through a PhD break? Share your thoughts in the comments section!
Leave a Comment
Leave a reply cancel reply.
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Related Articles

- 3 Min Sanity
Build your own safety net
- Posted by by Janika Liebig
- 4 minute read

- Opportunities
Marie Skłodowska-Curie PhD fellowship: How to apply and what to expect
- Posted by by Mónica Fernández Barcia

- Productivity
How to set SMART goals and become more productive
- Posted by by Kristin The PhD
- 3 minute read
Privacy Overview
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 27 April 2022
Navigating mental health challenges in graduate school
- Zachary F. Murguía Burton 1 &
- Xiangkun Elvis Cao ORCID: orcid.org/0000-0001-8601-6588 2 , 3
Nature Reviews Materials volume 7 , pages 421–423 ( 2022 ) Cite this article
14k Accesses
4 Citations
38 Altmetric
Metrics details
- Institutions
Many graduate students experience mental health struggles that lead them to question their place in academia. Two scientists who experienced extreme lows in graduate school reflect on what helped them during their low points, and suggest strategies for everyone to contribute to mentally healthier workplaces in academia.
We — Elvis and Zack — are two scientists who navigated mental health challenges during graduate school. Elvis is currently a postdoctoral researcher at MIT, and Zack is a mental health advocate and Stanford research affiliate still figuring out what his path as a scientist may look like.
With this piece, we hope to empower students who are facing similar struggles to understand they are not alone, and to call for more support at the institutional level. While we both ended up deciding to complete our PhDs, we want to emphasize that this is not the right choice for everyone — we each have numerous friends and former colleagues who are now leading healthier, happier lives after deciding to leave their graduate programmes. There are many ways to achieve a fulfilling career in and outside of academia, and, most importantly, there are many ways to achieve a fulfilling life.
Elvis’s experience
In November 2016, 3 months into my PhD in Mechanical Engineering at Cornell University, I planned to quit, even though I had wanted to pursue an academic career since my early childhood in China. I struggled to catch up with two advanced-level courses, could not fit into my first lab rotation, lost interest in my research project, and felt isolated as an international student in the small town of Ithaca. Daily frustrations added up to depression. That November, it started snowing in Ithaca, and I felt I had also entered a ‘snow season’ in my life. At that time, I thought pursuing a PhD at Cornell was the worst decision I had ever made and that I could not do it anymore.
Many international students share a similar experience. We choose to hide our struggles from our family and pretend everything is fine during video calls. We simply do not want to make our loved ones over-worried on the other side of the planet. In addition to the isolation from our families, job uncertainty and, for some of us, visa restrictions escalate our anxieties 1 .
I held on. I reached out to old friends back home to rebuild my positivity and confidence. I also spoke to the other international students in my PhD cohort to seek their support. We initially formed a group to support each other during the qualification exam preparation. When I spoke about my mental health challenges, I was surprised to find they resonated a lot with them, and we started openly discussing our issues to get advice from each other.
With the help of the Director of Graduate Studies in my field and the Graduate Field Assistant at Cornell, I switched to another research group within the department. I built connections with new colleagues and became passionate about my new project with the encouragement of my new PhD advisor. An immigrant himself, he provided substantial support: he was always there to help, from guiding my research project to supporting my professional development (for example, he wrote some 20 reference letters for me). After settling into my new research group, I landed on the Forbes 30 Under 30 list for my thesis project, and my side project was featured on the National Institute for Biomedical Imaging’s website . In 2021, I received two postdoctoral fellowships from the MIT Climate & Sustainability Consortium and the Alexander von Humboldt Foundation . Pursuing a PhD at Cornell turned out to be the right decision for me.
Looking back, my international peers in the support group helped me navigate the initial struggles in graduate school as I tried to fit into the new environment. The help I received from my department eased the pressure a lot, especially during the lab switch process. The support from my advisor and colleagues in the research group made my pursuit of science in a foreign country an enjoyable experience. As international students and scholars, we will inevitably face many additional challenges in the future, and knowing I have someone to count on greatly relieves my anxiety. I have not seen my family since 2019 owing to COVID, but the friendship and mentorship I received during graduate school made me call Ithaca my new home. More graduate students (especially international students) should be encouraged to form their own support groups and seek institutional support when problems arise. Research groups should be supportive, help lessen feelings of isolation and help students identify solutions for the problems they face.
Zack’s experience
In May 2017, 2 years into my PhD in Geological and Environmental Sciences at Stanford University, I was suicidal. I was hospitalized the morning of my doctoral qualifying exams. For months after, I felt like a failure — I was ashamed, my confidence was destroyed, and I did not think I belonged in academia.
I spent 11 days in the hospital, 6 weeks in all-day group therapy, and 5 months away from my dissertation. But, looking back, taking that time away from academia ended up being the best decision I could have made for my life as a scientist. My mental health crisis taught me the power of unplugging: to take that 2-week vacation; to check in with myself, friends and family rather than checking emails late at night; to actually treat weekends as ‘weekends’.
I also sought support from my California-based family and friends, and — critically — from my PhD advisor. He told me he would continue to fund me, and to take all the time I needed to care for myself. He shared encouraging stories of brilliant scientists he knew with mental health challenges.
Five months after my hospitalization, I passed my qualifying exams.
Since then, I’ve worked for the US Department of Energy and NASA, my research has appeared in Popular Science and CNN , and, in December 2020, I defended my PhD. Beyond the professional opportunities that arose after my lowest point in 2017, I have found purpose in giving back: I share openly about my mental health challenges to foster healthier and more inclusive spaces. I co-created The Manic Monologues (a play showcasing diverse true stories of mental health, made accessible to thousands worldwide), and I have spoken for Amazon’s diversity and inclusion series, NPR and — most meaningfully — for university students and hospital patients like I was.
I still struggle with my mental health. I have many good days, and I also have horrible days. But I am not alone. I take medication and I seek help from health-care professionals when needed, and I have built a wonderful support network of friends, family and colleagues: we all support each other, because we are all in this together.
Mental health issues among graduate students
Even before the COVID-19 pandemic, poor mental health was pervasive among graduate students and in academia 2 , 3 . In a 2019 global survey of 6,320 PhD students, 36% of respondents reported seeking help for anxiety or depression caused by their studies 4 . A synthesis of articles published through 2019 yielded a pooled estimate of “clinically significant symptoms of depression” in 24% of PhD students (across 16 studies covering 23,469 students) and of anxiety in 17% of PhD students (across 9 studies covering 15,626 students) — notably higher rates than among young adults in the general population 3 .
The pandemic has exacerbated this already dire situation. A 2020 survey of more than 15,000 graduate students at nine US research universities found that anxiety symptoms rose 50% compared with 2019 (ref. 5 ). The survey found that 32% of graduate students screened positive for symptoms of depression, and 39% screened positive for anxiety 5 . Among faculty, similarly worrying trends are observed. A poll of 1,122 US faculty members found that 70% felt stressed in 2020 versus 32% in 2019 and that more than 50% were seriously considering a career change or early retirement 2 . Another study found moderate to severe signs of mental distress in 78% of UK research staff during the pandemic.
In the USA, international students make up nearly half of all students entering science and engineering graduate programmes . Being an international student comes with many additional mental health challenges, including isolation and separation from family, visa and job prospect uncertainty, acculturation and potential subjection to racism and anti-immigrant rhetoric 4 , 6 , 7 . To make matters worse, mental health impacts may be magnified for groups already most marginalized in STEM and academia, including low-income, first-generation, LGBTQ + , Black, Latinx, Asian, Indigenous, women and non-binary students, as well as students with disabilities and intersecting identities 3 , 5 .
Reflections and strategies for mentally healthier graduate experiences
We navigated our mental health struggles through a combination of reaching out for help (for example, from family, friends, colleagues and supervisors, therapists and mental health professionals), building support groups and finding solidarity among peers, and achieving a better work–life balance by re-organizing priorities and values (Fig. 1 ). Meanwhile, we think it is essential to speak openly about what we went through so that others facing similar challenges know they are not alone. Alongside speaking openly, regular check-ins to see how colleagues are doing and speaking out against injustice are ways we can all help foster mentally healthier environments.
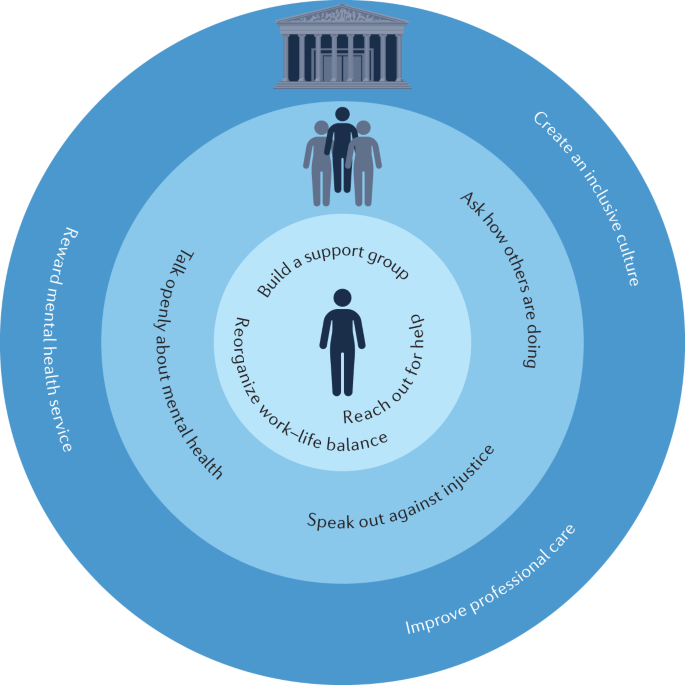
Strategies graduate students and faculty can use for themselves (inner circle) and for others (middle circle), and strategies for institutions to support mentally healthier graduate student experiences (outer circle).
Institutions must also help (Fig. 1 ). In addition to expanding and guaranteeing access to professional mental health services and improving both services and mental health-related policies, institutions must ensure that students are not disadvantaged or implicitly punished for making use of them (for example, via potentially harmful implementation of leave of absence policies ).
Institutions should acknowledge and reward service 8 towards improving mental health. For example, institutions should encourage faculty, staff and students to share vulnerably about their own experiences to create healthier environments and should recognize those who advocate for improved mental health support at the department and university level. Institutions should support and provide resources to graduate students to implement critical social support measures such as peer support groups 9 . Faculty should always strive to foster supportive and positive mentoring relationships with their graduate students, and institutions must support them in doing so. Institutions and graduate advisors alike should support and encourage students in taking healthy breaks when students are feeling stuck, burnt out or overwhelmed (and should explicitly highlight options and examples for taking such breaks). Institutions and faculty should also foster career optimism and remind students that many pathways (both inside and outside of academia and the sciences) can lead to fulfilling careers and lives. Above all, institutions must strive to create an inclusive and supportive culture.
As academics and scientists who faced mental health challenges during graduate school, we are asking individuals and institutions to pay attention to the mental health of students. We must support students — particularly those already under-represented in STEM — to create better workplaces, communities and science for all of us.
If you are struggling right now, you are not alone. We have both been at the lowest of lows. We did not think there was a place for us in academia or in the sciences. But, thankfully, we were wrong. Our lives and careers have never been as fulfilling as they are now.
Finally, we wish to acknowledge that this article is a product of our own experiences and reflections and those of others close to us and, therefore, may not resonate with everyone. Our suggestions similarly cannot be comprehensive in scope, but hopefully may nonetheless further this critical conversation and play some part in bringing about meaningful change to improve mental health support for all.
Cao, X. E., Liu, X. & Zhang, Y. Flourishing as international students and scholars in the US. Matter 5 , 768–771 (2022).
Article Google Scholar
Gewin, V. Pandemic burnout is rampant in academia. Nature 591 , 489–491 (2021).
Article CAS Google Scholar
Satinsky, E. N. et al. Systematic review and meta-analysis of depression, anxiety, and suicidal ideation among Ph.D. students. Sci. Rep. 11 , 14370 (2021).
Woolston, C. PhD poll reveals fear and joy, contentment and anguish. Nature 575 , 403–406 (2019).
Woolston, C. Pandemic and panic for US graduate students. Nature 585 , 147–148 (2020).
Mori, S. C. Addressing the mental health concerns of International Students. J. Couns. Dev. 78 , 137–144 (2000).
Ogunsanya, M. E., Bamgbade, B. A., Thach, A. V., Sudhapalli, P. & Rascati, K. L. Determinants of health-related quality of life in international graduate students. Curr. Pharm. Teach. Learn. 10 , 413–422 (2018).
Armani, A. M., Jackson, C., Searles, T. A. & Wade, J. The need to recognize and reward academic service. Nat. Rev. Mater. 6 , 960–962 (2021).
Charles, S. T., Karnaze, M. M. & Leslie, F. M. Positive factors related to graduate student mental health. J. Am. Coll. Health. https://doi.org/10.1080/07448481.2020.1841207 (2021).
Download references
Author information
Authors and affiliations.
School of Earth, Energy & Environmental Sciences, Stanford University, Stanford, CA, USA
Zachary F. Murguía Burton
Department of Chemical Engineering, Massachusetts Institute of Technology, Cambridge, MA, USA
Xiangkun Elvis Cao
MIT Climate & Sustainability Consortium, Massachusetts Institute of Technology, Cambridge, MA, USA
You can also search for this author in PubMed Google Scholar
Corresponding authors
Correspondence to Zachary F. Murguía Burton or Xiangkun Elvis Cao .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Related links.
Alexander von Humboldt Foundation’s German Chancellor Fellowship: https://www.engineering.cornell.edu/news/sibley-schools-xiangkun-elvis-cao-wins-german-chancellor-fellowship
Feature article by CNN: https://www.cnn.com/2021/02/03/world/martian-landslides-ice-salt-scn/index.html
Feature article by Popular Science: https://www.popsci.com/story/science/below-mars-surface-landslides-discovered/
Feature blog by Harvard: https://blog.petrieflom.law.harvard.edu/2022/03/18/disability-advocacy-stigma-covid/
Forbes 30 under 30 in energy profile: https://www.forbes.com/profile/xiangkun-elvis-cao/
Foreign-born students and workers in the U.S. science and engineering enterprise: https://www.nsf.gov/nsb/sei/one-pagers/Foreign-Born.pdf
Mental health check-in challenge: https://www.choc.org/mental-health-awareness-month/
MIT Climate & Sustainability Consortium fellowship: https://impactclimate.mit.edu/inaugural-cohort-impact-fellows/
NIBIB feature article: https://www.nibib.nih.gov/news-events/newsroom/rapid-test-delineates-diseases-similar-symptoms/
Potentially harmful leave of absence policies: https://georgetownvoice.com/2021/09/11/leaves-of-absence-mental-health/
The Manic Monologues: https://www.themanicmonologues.org/
What researchers think about the culture they work in: https://wellcome.org/reports/what-researchers-think-about-research-culture
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Murguía Burton, Z.F., Cao, X.E. Navigating mental health challenges in graduate school. Nat Rev Mater 7 , 421–423 (2022). https://doi.org/10.1038/s41578-022-00444-x
Download citation
Published : 27 April 2022
Issue Date : June 2022
DOI : https://doi.org/10.1038/s41578-022-00444-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

Should you quit your PhD?
Sep 25, 2023

Should you quit your PhD? There wasn’t a day that went by during my PhD when I didn’t think about quitting at least once. I’d ask myself why I was putting myself through the roller coaster, and whether I had made a mistake.
It’s comforting – or perhaps also a little worrying – to know that these feelings are largely normal. For many PhD students, working to overcome this inner voice is part of the challenge of completing a PhD.
PhDs are hard, there’s no escaping that, and at times stressful, but they shouldn’t be unbearable, at least not for any continued length of time. But there’s a danger that we risk telling students to ‘suck it up’ and in the process normalise suffering and genuine feelings of dissatisfaction. For many, quitting a PhD is the wrong decision. For those students, sure, they need to ‘suck it up’. But for others, quitting is the right decision. For those, sucking it up is the worst possible advice.
This article speaks to those who are thinking of quitting their PhDs, and instead of telling you to suck it up, it talks frankly about why you might want to and how to navigate such a decision. It is my hope that you might understand whether the feelings of dissatisfaction and overwhelm you might have for your PhD are normal, or whether you really are better off doing something else.
Deciding to quit anything, not least a PhD, is often laden with emotional weight, uncertainty, and implications for your future. Even the term quitting is so laden with negative connotations that it’s almost a slur. I almost contemplated avoiding the word entirely in this article. Quitting implies failure, rejection, not having what it takes. But whilst there’s a lot to be said for sticking with adversity, the emotional and cultural baggage around the very idea of quitting can be unhelpful for those who are ill-suited to academia, or those who are really having a horrid time. The stigma around quitting a PhD is naive, when you consider how many people actually do. In the US, for example, around 50% of people drop out of PhD programmes.
The decision to quit your PhD or stick with it is yours and yours alone. It’s not up to me or anyone else to tell you you should or shouldn’t quit. The difficulty in such a decision is understanding – truly understanding – whether any sense of dissatisfaction you’re feeling with your PhD journey is on the ‘normal’ end of the spectrum, or whether it’s on the problematic end. In other words, whether you should suck it up or move on to other things.
What can be helpful in working out where on that spectrum you are is to understand the reasons why other people decide to drop out.
This is not a normal blog subscription
Each week we send two short, thought-provoking emails that will make you think differently about what it means to be a PhD student. It is designed to be read in thirty seconds and thought about all day.
Common Reasons for Wanting to Quit a PhD
Unsurprisingly, there’s a lot of academic research around this topic. In an extensive review of the literature on this topic, Sverdlik, Hall, McAlpine & Hubbard (2018) categorised the factors that influenced this decision as external or internal to the student.
External factors
Supervision.
The most influential force in the doctoral experience is the supervisory relationship. When it is open, supportive and communicative, you can assume that students feel more successful and satisfied. Compatibility, whether in terms of research interests or working style, between the student and the supervisor, is also important. When these are missing, and when the supervisory relationship itself turns into a source of stress and anxiety, it’s not uncommon for students to feel a great deal of dissatisfaction.
Departmental structures and organisation
From the students we speak to, particularly those in our writing group , we know how important it is to feel connected and to feel as though you’re part of something bigger. Departments have a huge role to play in addressing this need, and when this type of support and integration is missing it can damage our feelings of belonging and overall morale.
There are two dimensions at play here. On a formal level, departments can do a lot to integrate and socialise students into departmental life, through things like funding opportunities, sharing information, teaching opportunities, and clear communication. On an informal level, there’s much they can do to make you feel welcome, such as socialising you into the departmental culture and making you feel as though you’re a valuable member of the department.
Where there is a mismatch between you and your department, whether informally or formally, it can be very easy to feel isolated and make the decision to leave the programme easier. This of course has not been helped by the pandemic. During the pandemic, and particularly lock-down, this isolation was particularly acute, for obvious reasons. But from our experience working with students since the pandemic, often things never really returned to the way they were before. There’s more time alone, more time on Zoom, less time in the department and less time interacting in the real world with peers. The ability to feel part of something bigger and supported by department structures is now more strained as a result.
Financial opportunities
It is perhaps unsurprising that whether or not funding opportunities are available can have a huge impact on your overall sense of worth and well-being, and can be a major driver in deciding whether or not to quit the PhD programme. For many, the years doing a PhD are years that could be spent in industry starting a career (and getting paid accordingly). As the years on the PhD programme go by, a fear of missing out kicks in, and you may start to question your financial acumen in deciding to go down this path. I certainly did; my stipend was around £12,000 per year, which was far, far less than I could have earned elsewhere, and well below minimum wage when taking into consideration the number of hours I was spending on the PhD. I was grateful to receive it of course, but fully aware of the opportunity cost of the PhD on any alternative careers or income.
On a more pragmatic level, the issue isn’t so much what you could be earning elsewhere, rather the more immediate concern of not having enough money in the first place. Academia is an elite institution, with too few students from working class and marginalised backgrounds. When me and other PhD students I worked with – all comfortable in our middle class lives – complained of having no money, what most of us really meant was ‘not having as much as we’d like’.
For many on our programme and many elsewhere though, not having enough money means just that. It means having to hold down one or more part-time jobs, and miss out on conferences, events, and other things crucial both to professional and personal wellbeing. For some, the decision to drop out can be a purely financial one, or one borne out of the stress and exhaustion that comes from simply staying afloat.
Another significant factor affecting a decision to stay in the programme is what happens after you graduate. For many disciplines and in many countries, the academic job market is poor, with little promise of job security or salaries to match the expertise and experience you have. Where there are limited job options or poor salary prospects, the decision to quit a PhD can become easier.
Internal factors
A common reason for quitting a PhD is a lack of motivation. The unstructured nature of PhD work, and the fact that you have to self-regulate and self-manage, means that motivation can be difficult to conjure up.
There is obviously a close relationship between the other factors I’ve discussed elsewhere and this one. Motivation might wane where there is a poor supervisor relationship, for example, or once you realise that there are poor job prospects. But it can also be influenced by why you decided to do a PhD in the first place. Broadly, we can break down a student’s motivations for starting a PhD into two spheres: intrinsic and extrinsic. Intrinsic reasons are a passion or interest for the subject. Extrinsic reasons are things like boosting your CV. Students who pursue a PhD for intrinsic reasons – because they’re passionate about a topic – are more likely to stick with it and feel more satisfied.
Self-worth and efficacy
At the heart of many PhD students’ struggles is a sense of not being ‘worthy’ of a PhD, or not having what it takes. Countering this prevailing self-depreciation is a big part of what we try to do here, because such self-critique is more often than not based on a faulty assessment of our own abilities and skills. When we think we’re worthless, the cost of quitting decreases significantly.
Personal and social lives
PhDs require a huge amount of physical and emotional energy. The often extensive demands of both formal and informal doctoral work means that health, wellbeing and social lives can go out of the window. It is when we fail to manage our well-being and maintain a holistic personal life beyond the PhD that we experience burnout, depression and low well-being. And when they rear their heads, you’re far more likely to want to leave.
There’s no getting away from the fact that the PhD will demand a huge amount of your time. But there’s absolutely no need to feel guilty about taking time away from it and focusing on your own health and your own personal life instead. Indeed, work-life balance is the strongest predictor of psychological distress in PhD students.

Your PhD Thesis. On one page.
Assessing your situation.
Whilst the research above looks at why students have dropped out, what it doesn’t look at is whether they’re the ‘right’ decision to drop out. I use the word ‘right’ here cautiously. There is no ‘right’ or ‘wrong’ reason for dropping out. Rather, there is just ‘a’ decision to drop out. What we might think of instead is whether the struggles and strains are on the normal, to-be-expected end of the PhD spectrum or whether life really is miserable and you really are better off leaving.
But how can you know on what end of the spectrum you lie?
It’s entirely normal in a PhD to feel like you’re not making any progress and to feel completely out of your depth. Research is an exercise in failing, over and over again. In order to work out what the correct path is, you need to go down all the wrong paths, find the dead ends, and retrace your steps to find another path to take. Eventually, you get to the end, perhaps without ever noticing when you finally made it onto the right path.
This trial-and-error approach, informed of course by an intelligent reading of the literature and your data, is, counterintuitively, how we make progress in research. We throw stuff at the wall and see what sticks. Further aggrevating that though is the fact that you’ve never really done any of this stuff before. You’re in at the very deepest end, learning on the job and, as we’ve seen, continually making mistakes.
It can be easy to see these mistakes as your failure, as something innate to your abilities (or perceived lack of them). But they’re not. Failure is progress, after all. And all that work is just plain hard. And isolating. If a PhD was easy, everyone would have one. But they’re not, so they don’t.
All this is to suggest that perhaps you shouldn’t quit a PhD if you feel like an imposter, or you feel like you’re making too many mistakes and haven’t got what it takes. Or if you find the work too hard (everyone does, and it gets easier).
But perhaps you should quit a PhD if you’ve traded your health (particularly your mental health) to stay on the journey. Or, because the more you go down the path the more you lost interest in the subject or the more you see that the career that lies ahead isn’t for you.
Consequences of Quitting
But as much as it is a personal decision, there are real-world, often external consequences. This step will have ramifications for your career, your sense of self, and possibly even your social circle. Before deciding to leave your programme, it’s important to know what you’re really signing up for.
Professional Implications
Choosing to step away from a PhD might feel like veering off an established career path. Within academia, the finished thesis is the route to a research or teaching position. But outside the academic walls, the reality is different. Many industries and sectors deeply value the skills you’ve acquired during your PhD journey—skills like in-depth research capabilities, critical thinking, and proficient project management. Even without that final thesis, and no matter how far through you end up, you come armed with a unique set of competencies that can be invaluable in various roles and settings.
Personal Growth
Irrespective of your decision about the PhD, the journey itself offers invaluable lessons about personal growth. Throughout this experience, you’ll discover more about yourself: the environments in which you flourish, the challenges you willingly embrace, and the aspects of work you truly value. Deciding whether to continue or step back isn’t just about the degree; it’s an extended exercise in self-awareness and in understanding your priorities. Whether you proceed or drop out, these insights into your character and preferences will guide many of your future choices.
Financial Considerations
The financial dimension of quitting a PhD is complex. You need to be mindful of existing funding agreements, scholarships, and any potential repayment obligations. Beyond that, consider the financial landscape of transitioning into a new field or profession. While the initial phase might come with financial challenges, especially if you’re retraining or shifting sectors, remember that many industries might value the unique skills and perspectives you bring from your PhD experience. Balancing immediate financial concerns with long-term prospects can help you make an informed decision.
Social Impacts
Making the decision about your PhD is deeply personal, but its ripple effects touch the people around you. You might find yourself on the receiving end of a spectrum of reactions from peers, mentors, family, and friends. While some might stand firmly by your side, understanding and supporting your choice, others might struggle to grasp the reasons behind your decision. During such times, it’s crucial to lean on a supportive network. Engaging in open conversations and seeking understanding can be cathartic. Surrounding yourself with empathetic individuals who respect your choices, even if they don’t fully understand them, can make this transition smoother and more reassuring. But above all, remember that is your choice alone to make, and you don’t need to justify it to anyone.
The Emotional Weight of Considering Quitting
Quitting your PhD is not a simple binary decision, and the weight of the decision is not just academic but emotional, affecting not just your work, but your sense of self and your future.
A key part of the challenge is that it can feel as though your entire education has led to you doing a PhD. That your entire identity is wrapped up in being an academic, and being smart, and the PhD is the final piece of the puzzle that is so tantalising close and worth risking everything for. This is largely nonsense. You will still be smart if you drop out. You will still have all the skills and experience you’ve gained in your education so far, and plenty of non-academic employers would love to hire you for them.
Quitting a PhD should therefore be seen as a positive. It’s you taking control over your well-being and changing something that wasn’t working for you. It’s you taking a risk, putting yourself first, and refusing to put up with something that you know isn’t good for you.
But nonetheless, you’re likely to go on an emotional rollercoaster in the run up and aftermath to leaving your programme.
Guilt and Shame
It’s entirely natural for you to grapple with feelings of guilt and shame when thinking about leaving a PhD behind. Societal norms, combined with personal expectations, can paint a picture where deviating from the path feels like a defeat. The weight of the world and your own aspirations can press heavily, making you feel like you’re not measuring up or that you’re letting yourself and others down. The idea of quitting is often shrouded in taboo, further intensified by the sunk cost fallacy – the notion that you’ve already invested so much time, energy, and perhaps finances, that turning back feels wasteful. However, it’s vital for you to remember that your journey is unique, and measuring your decisions against societal standards or past investments might not always reflect what’s best for your current and future well-being.
Contemplating the idea of stepping away from the PhD might initially be fraught with hesitations and doubts. However, as you delve deeper into the thought, you might find a palpable sense of relief washing over you. This emotional response can be enlightening. If merely considering a different path brings such a strong sense of relief, it might be an indication that redirecting your journey could indeed be the right choice for your well-being and future goals. Listening to this inner emotional compass can be crucial in making decisions that resonate with your true desires and needs.
Fear of the Unknown
Stepping into an uncertain future, especially when it deviates from a long-held plan like completing a PhD, can be incredibly daunting for you. The questions might swirl in your mind: What opportunities await without that coveted doctoral degree? How will the professional landscape perceive you? The ambiguity of not knowing can sometimes overshadow the reasons that led you to consider a different path. But remember, every significant life decision comes with its share of uncertainties. Embracing them, rather than fearing them, can open doors to opportunities you hadn’t previously imagined.
Embarking on a PhD is often a decision driven by your passion, curiosity, and aspirations for the future. But as the journey progresses, you might find a growing disconnect between the academic path and your evolving personal and professional goals. Recognising this misalignment isn’t a sign of failure but rather an act of self-validation. Understanding that the path you once felt was perfect might not align with your current aspirations is empowering, and a sign of a deeper understanding of your own needs and desires. This realisation isn’t about admitting defeat, but rather about acknowledging your evolving self-awareness and priorities. By doing so, you’re not only giving yourself the permission to seek out paths that resonate more with your current goals but also embracing an authentic commitment to your personal growth and future.
Alternatives to Quitting
Remember that quitting is not your only option, even when it feels like it. Whether it’s considering a leave of absence, consulting with mental health professionals, or even shifting your research focus, there are ways to make your PhD journey more bearable. Yes, you read it right—you don’t have to face the monumental task of single-handedly revolutionising your field. It’s your apprenticeship into academia, not a Nobel Prize race.
Considering a Leave of Absence
Before making a final decision, remember that many institutions provide an option to take a break. Opting for a leave of absence might offer you the breathing room you need, allowing you to step back, recharge, and assess your choices with a clearer mind. This pause can be instrumental in reevaluating your commitment to the program, granting you the time to contemplate whether your struggles are temporary setbacks or indicative of a deeper misalignment.
Reassessing Supervisory and Project Dynamics
If the crux of your unease stems from challenges with your supervisor or the nature of your research project, there’s a potential remedy. Consider discussing a switch in supervision or even pivoting your research direction. Sometimes, reshuffling these foundational elements can reignite your passion and satisfaction with the PhD journey, altering the course of your experience.
Weighing the Part-time PhD Option
The rigours of a full-time PhD can be overwhelming, especially if you’re juggling other life responsibilities or commitments. Some universities accommodate by offering a part-time PhD track. This could be a balanced middle-ground, allowing you to continue your academic pursuits at a more manageable pace while also engaging with other aspects of your life.
Turning to Counseling or Therapy
The emotional and mental strains of a PhD can be taxing. Engaging in counseling or therapy sessions can provide you with a space to articulate and process your feelings. A professional can offer insights, coping mechanisms, and strategies to manage stress, potentially equipping you with the tools to navigate the challenges of the doctoral journey.
Steps to Take If You Decide to Quit
If, after thorough reflection, you decide that leaving is the best course of action, there are official routes and less formal pathways out of your PhD. Exit degrees, other academic pursuits, or a pivot into industry could all be next steps in your post-PhD life.
Engaging with Your Supervisor and Department
Your decision impacts not just you but also your academic ecosystem. Open dialogue with your supervisor and department is crucial. These discussions offer clarity, ensure all parties understand the reasons behind your choice, and can sometimes open doors to alternative solutions you might not have considered.
Understanding the Withdrawal Process
Deciding to leave is more than just an emotional choice; there’s an administrative aspect to it. Familiarize yourself with the withdrawal process of your institution. Be clear on any obligations, potential repercussions, or financial considerations associated with your decision.
Leveraging Career Counseling
Your skills and experiences acquired during your PhD journey are valuable and transferrable. Career counseling can guide you in identifying these strengths and navigating job markets, ensuring you’re positioned favorably for roles outside of academia that resonate with your aspirations.

Maintaining Academic and Professional Connections
Exiting a PhD program doesn’t necessitate severing ties with the academic world. The relationships, networks, and bonds you’ve forged can continue to serve you well in various capacities. Maintain these connections; they can be sources of references, collaborations, or even job opportunities.
Wholeheartedly Embracing Your Decision
Whatever your choice, remember it’s grounded in your well-being and aspirations. It’s an act of courage and self-awareness. Celebrate this bravery and move forward with optimism and confidence, knowing you’re aligned with a path that resonates with your current and future goals.
Choosing to quit your PhD is an intensely personal decision that comes with its own set of complexities. Just like when you’re wrestling with your day-to-day PhD challenges, it’s crucial to be realistic about what you can and cannot do. If you decide to leave your PhD programme, know that it’s a decision that should be made with the utmost care, with due consideration given to both your present circumstances and your future prospects. But know that only you can make the decision, and being able to make it in good faith depends on whether you’re able to fully understand the feelings that you have and the relationship you have with your PhD. Is what you’re feeling a ‘normal’ part of the journey, or a cause for concern? It is my hope that this article has helped you to undersatnd the answer to this question a bit more clearly. Feel free to share your experience in the comments, or if you want to work on on one with me to work through pain points or struggles, learn more about my coaching programme .

Share this:
Wow, very spooky!! I just handed in my withdrawal notice today!! What sort of algorithm do you use there??!!
Well done for taking charge of your PhD. How does it feel?
Thank you for this very insightful and perspective-changing article. I am currently contemplating whether to drop out from the PhD programme as it has significantly affected my mental health, and I’ve also started to understand my priorities and values better in this first year of PhD journey. I love how you wrote about “This realisation isn’t about admitting defeat, but rather about acknowledging your evolving self-awareness and priorities”. I intend to uphold my values, prioritise my wellbeing and other values above a qualification. Regardless of what the future prospects are, you can’t achieve fulfillment without your health. So thank you so much for this very insightful, encouraging and validating piece. <3
Thanks for the lovely words. You’re very welcome.
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *

Search The PhD Knowledge Base
Most popular articles from the phd knowlege base.
The PhD Knowledge Base Categories
- Your PhD and Covid
- Mastering your theory and literature review chapters
- How to structure and write every chapter of the PhD
- How to stay motivated and productive
- Techniques to improve your writing and fluency
- Advice on maintaining good mental health
- Resources designed for non-native English speakers
- PhD Writing Template
- Explore our back-catalogue of motivational advice
Your Guide to Mental Health Leave—Because Sometimes You Need a Real Break

Nobody’s immune to bad days at work. You’ve had them too, right? Your to-do list and inbox feel like a giant game of whack-a-mole you can barely keep up with. You’re convinced you stuck your foot in your mouth during a team meeting and can’t stop replaying the experience in your head. You missed an important deadline and are beating yourself up over dropping the ball. While they’re absolutely disheartening, these types of hiccups and stressors are a normal part of our working lives.
But what happens when the odd bad day starts to snowball into something bigger? Maybe you’ve found that making it through the workday feels like dragging your feet through wet cement as you struggle to focus on your tasks. Or that your stomach’s tied in knots over projects that used to excite you. You feel completely drained, exhausted, and even a little hopeless—and you know that neither a quick vacation nor a simple self-care routine are going to right the ship.
You need a bigger solution—one that actually helps you get to the root of the issue. It’s at that point that you might think about taking a mental health leave from work. That’s what happened with Chauntelle Lewis, a freelance diversity and inclusion consultant and inclusive communities manager, who took a month-long mental health leave from a previous job before eventually changing employers, and with Jordan*, a tech professional in Boston, who experienced “deep burnout ” before opting for a mental health leave.
But what exactly is a mental health leave? How can you tell if you need one? And how do you actually handle the process? Here are the real answers—and the real stories—you need to hear.
What exactly is mental health leave?
How do you recognize if you need mental health leave, what are your options for taking mental health leave, how do you talk to your manager about mental health leave, what should you do during your mental health leave, does mental health leave actually help.
Mental health leave is exactly what it sounds like: It’s when you take a break from work in order to have dedicated time to focus on improving your mental health.
“Taking a mental health leave is a time for individuals to step away from the daily life of being a ‘human doing ’ and delve into the space of being a ‘human being ,’” explains Amira Johnson, a licensed master social worker at The Berman Center , a treatment and therapy center in Atlanta.
Pressing “pause” on work to focus on your mental well-being might sound like a pipe dream, but this type of leave is becoming more common as the pandemic pushes the importance of mental health into the spotlight. Between December 2020 and July 2021, for example, employees reported a 21% increase in burnout and a 17% increase in physical symptoms of stress. While those statistics are discouraging, there’s an upside: It’s opened the door for people to candidly discuss those shared experiences, with one psychiatrist saying that mental health is now part of the national conversation “unlike any other time since I started practicing medicine.”
Whether you’re experiencing increased stress and signs of burnout or are dealing with a diagnosable mental health condition like depression, a mental health leave gives you time to heal while ensuring your job is waiting for you, explains Karla Lever, PhD, licensed clinical mental health counselor supervisor and director of Atrium Health ’s Employee Assistance Program.
You might hear the terms “mental health leave” and “stress leave” used interchangeably and, medically speaking, that’s not exactly incorrect. But the words you choose could carry different meanings for you and your coworkers. “Stress is something we all experience, and using the term ‘stress leave’ might normalize the experience for others, rather than ‘mental health leave,’ which may bring up the idea that you have a mental illness,” says Dr. Candice Schaefer , a clinical psychologist and Global Head of Employee Wellness at Twitter.
“Emotions ebb and flow,” explains Muse career coach Benjamin Ritter , EdD, founder of LFY Consulting . “At times we may find ourselves on the low side of the emotional spectrum.” It’s inevitable. But how do you know when your lows are so low or so frequent that they require a bigger solution?
Your mental health is as unique as you are, so indicators can vary. However, the experts agree that there are some common red flags to look for, all of which interfere with a person’s ability to function normally at work. These include:
- Finding less pleasure in work you were once passionate about (or even feeling irritable about tasks you used to get excited about)
- Struggling to get yourself to actually show up for work (something that Lewis says she experienced herself, combined with “extreme anxiety and burnout”)
- Falling off your daily routine after an extended period of consistency
- Demonstrating mood changes, significant shifts in your behavior, and a lack of compassion or enthusiasm when communicating with coworkers
- Having difficulty concentrating or experiencing confused thinking
Those are somewhat early warning signs, but they can snowball to become even more serious and include difficulty sleeping, excessive crying or hopelessness, and even thoughts of suicide or homicide.
Think your coworkers or supervisor will be the ones to point out that you aren’t acting like yourself? That’s not always the case, especially if you work remotely. It’s entirely possible that you could be trudging along without others ever noticing a decline or difference in your attitude and output. “Most of my work was very independent and I was struggling to do that. But if somebody asked me for something, I was able to deliver,” Jordan says. “My boss didn’t see any change in my performance, but I knew I wasn’t performing at my best and that continued to spiral downward.”
If and when you notice a shift or decline in your mental health, it’s important to connect with a qualified mental health professional like a therapist or psychologist. Not only does this give you much-needed support and help you better understand what you’re dealing with, but it also equips you with documentation you might need in order to access mental health leave and other benefits.
When you determine that a pause from work is the best move for you, figuring out the next steps can be daunting—especially when you already feel like you’re barely keeping your head above water. But a smart place to start is understanding what benefits and types of leave are available to you.
There are two different categories of leave you could take:
- Continuous: Leave taken for an uninterrupted period of time (e.g., taking two months off)
- Intermittent: Leave taken sporadically (e.g., taking a few hours off here or a day off there or working half-days or three days a week over the course of a few months)
When it comes to actual leave benefits, employees can generally access mental health leave in a number of different ways:
- An employer-provided benefit: Some employers offer paid leave specifically for mental health, especially with a growing emphasis on mental well-being in the workplace. More than a third of employers updated their health plans to expand access to mental health benefits (this encompasses various benefits, not just leave) during the pandemic.
- Short-term disability : This is an insurance policy (usually provided or purchased through your employer) that could offer paid leave for mental health, depending on the specifics of your plan. Different policies have different definitions of “disability,” so you’ll need to consult your policy documents to see what’s covered.
- Family Medical Leave Act (FMLA) : This is a federal employment law that requires employers to offer up to 12 weeks of leave for a variety of family or medical reasons, including mental health concerns. While your job will be protected, note that this leave is entirely unpaid.
- Paid Family and Medical Leave (PFML) : A few states offer this type of paid leave that allows you to receive a portion of your salary from your state. That came into play for Jordan, who used a combination of their state paid leave and FMLA to take mental health leave.
Not sure which one(s) are available to you? Your HR department should be able to guide you.
With a better handle on some of the logistics, you’ve laid at least a little of the groundwork to connect with your manager. If your mouth is dry and your hands are clammy at the very thought of it, that’s normal. This can be a nerve-racking conversation to have—especially since mental health leaves usually involve personal details about your life.
In an ideal world, you’d have an open and honest relationship with your manager that empowers you to candidly share your struggles and challenges during your regular one-on-ones and other conversations. If that’s the case, then your desire for a mental health leave likely won’t come as a shock.
But even if you haven’t previously broached the subject with your supervisor, now is the time to schedule a private, dedicated conversation. You don’t need to give a detailed breakdown of what you want to discuss, but a brief heads up is helpful. You can keep it somewhat vague by saying that you’d like to discuss your recent work and ask for their guidance. Mental health leave is a big subject. Allot more time for the meeting than you think you’ll need so you don’t feel pressure to rush through it.
That discussion will be a lot smoother (and you’ll likely feel calmer) if you’re well-prepared. So ahead of your sit-down, it’s wise to:
- Understand how much you’re comfortable sharing about what you’re experiencing and why you want to take leave. While you’ll need to provide enough context, don’t feel obligated to elaborate on all of the details.
- Know what solution you’re aiming for. In this case, if you need to take leave, you should make that explicitly clear and ask what options are available for you to take that time off.
- Think about your desired timeline. For example, do you need to take leave immediately? Do you want to take it all at once?
“If you don’t feel comfortable approaching your manager or colleagues about taking leave, then you can always go directly to your HR team for assistance,” Schaefer says. “They will help you have that conversation with your manager and draw boundaries on what you are legally obligated to share.”
Here’s the short answer: Whatever helps you recover and feel recharged.
For Jordan, that involved investing a lot of time in hobbies like drawing, reading, biking, exercise, and developing new and healthier routines.
One big thing that had disappeared when they were experiencing burnout was executive function, Jordan says, referring to a group of mental skills related to memory, flexible thinking, and self-control. “It was trash. I couldn’t do anything.” For Jordan, “progress” meant being able to make a small plan for what they’d like to do the next day.
Other people might find healing and respite in other areas. Lewis prioritized connections and relationships with other people. “Speak to loved ones and trusted friends,” she says, as those people were a pillar of support for her during her own recovery period. Lewis also continued to work with a qualified mental health professional during her leave. “I was lucky at the time, as I already had a therapist who was able to check in with me,” she says. As far as what’s happening back at the office while you’re away? Well, that’s not your concern. Both Jordan and Lewis say they were completely disconnected from work during their leaves. With that said, you might have to fulfill some reporting or check-in obligations with your employer depending on what type of leave you’re taking. But that should be exclusively focused on complying with your benefits, not handling any normal responsibilities of your position. Your goal is to give yourself the time you need to feel better and restore your normal level of functioning. “Don’t expect too much of yourself on a mental health leave,” Jordan says. “Give yourself time to build back that capacity.”
An intentional pause in your work life offers a number of benefits that will allow you to dedicate more time and energy to your mental well-being. A leave can:
- Reduce stress by removing work obligations from the picture
- Provide adequate time to rest, recharge, and work with a mental health professional
- Offer a better sense of balance and connection between the mind and body
- Improve retention, which is good not only for the employer but also the employee, given that job loss can be an added stressor
But while this type of leave offers plenty of advantages that you likely wouldn’t experience if you continued to grit your teeth and push through work, it’s not always a fix-all that ends in a seamless and joyous return to your job.
For some, it gives them space to realize they need something different. Lewis’ month-long leave helped her realize that her work environment itself was no longer a good fit for her and that she needed to change employers. Jordan started with the intention of taking a four-week leave and later extended that by another four weeks before they realized it still wasn’t enough time to recover and resigned entirely.
Work is supposed to be a positive and fulfilling experience. “It offers a sense of purpose, self-esteem, a chance to keep our brains active, helps us be self-sufficient because of the money we earn, and offers a way to increase social connections, all of which are beneficial for our mental health,” Lever says. But when your work feels more like a subtraction than an addition, you may need a break in order to restore your positive relationship with your career.
Even if a mental health leave isn’t in your immediate future, Jordan recommends taking the time to familiarize yourself with what your options are. “When you do need them, you might not be in a position just mentally to get yourself through that process,” they say. So read your employee handbook, understand your policies, and ask HR questions about your benefits.
Finally, the biggest thing to remember is this: There shouldn’t be any guilt or shame in taking mental health leave. In fact, you might be pleasantly surprised by how supportive the people around you can be. You’re only human—and every single person you work with is too.
*Jordan’s name was changed to allow them to speak freely about their work experience.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Sage Choice

The pathway from mental health, leaves of absence, and return to work of health professionals: Gender and leadership matter
Ivy l. bourgeault.
1 University of Ottawa, Ottawa, Ontario, Canada.
Jelena Atanackovic
Kim mcmillan, henrietta akuamoah-boateng, sarah simkin.
Health professions are ranked among the most stressful occupations and have a much higher likelihood of absenteeism from work. In this article, we present findings from four health professional case studies in our Healthy Professional Worker partnership, involving surveys with 1,860 respondents and 163 interviews with nurses, physicians, midwives, and dentists conducted between December 2020 and April 2021. We found that the pathway from mental health experiences through to the decision to take a leave of absence and return to work differed between the health professions and that both gender and leadership matter greatly. There is a need to de-stigmatize mental health issues and encourage greater awareness and support from supervisors and colleagues. Leadership can play an important role in mitigating mental health issues, and as such investment in both leadership training and mentorship are important first steps in acting upon our research findings.
Introduction
Health professions are ranked among the most stressful occupations, 1 – 4 and health professionals experience burnout, 5 – 7 anxiety, 8 – 10 depression, 11 – 13 Post-Traumatic Stress Disorder (PTSD), 14 – 16 and substance use at rates higher than the general population. 17 , 18 These challenges are tied, in part, to the organization of work within the healthcare settings: irregular and inflexible work schedules, shift work, and required overtime. 1 , 4 , 19 These experiences are compounded by the emotionally demanding nature of this work; caring for patients and families through immensely challenging and stressful times (diagnosis, treatment, and palliation) can lead to compassion fatigue and moral distress. 20 These workers often experience conflict at work, high levels of cognitive and physical fatigue and illness, 21 , 22 workplace injury or violence, and subsequent PTSD. 23 Due to these intersecting factors, health workers are one and a half times more likely to be off work due to illness or disability than workers in other sectors of the Canadian economy. 24
These trends have only been exacerbated by the COVID-19 pandemic. Health workers occupy a unique position in the COVID-19 pandemic response. 25 As the backbone of health systems, they have been key frontline responders to the crisis and have faced and continue to face great risk of infection. 26 , 27 Findings from a 2021 Statistics Canada/CIHI survey suggest that seven in ten healthcare workers report worsening mental health linked to stressful working conditions. 28 The unique epidemiology and infectiousness of COVID-19 contributes to demand on the health workforce of unprecedented volume and acuity, while at the same time diminishing health worker supply. Frontline health workers have faced increased job demands, 29 , 30 complex and quickly evolving working environments, and riskier working conditions, all while navigating chronic staffing shortages that preceded COVID-19. 31 The pandemic has put additional stress on workers in the health sector, leading to elevated levels of psychological distress 32 , ranging from anxiety and depression to PTSD. 33 – 37 Risk of contamination, availability of appropriate personal protective equipment, and worker safety have been common concerns/stressors for workers in the healthcare sector during the current pandemic. 38 , 39 Although “these concerns manifested as individual distress, they also intersect with and are reflective of concerns relating to healthcare institutions’ policies, communication practices, and politics.” 38 Statistics Canada 40 reported that vacancies in healthcare and social assistance increased by nearly 60% from the second quarter of 2019 to the second quarter of 2021, the largest increase in any sector of the economy. Given the challenging working conditions and inherently stressful nature of healthcare, it is important to understand the factors that facilitate or hinder their psychological health and safety.
The behaviours and leadership styles of supervisors and managers are important influences on frontline health worker mental health. 41 , 42 Transformational leadership behaviours (communicating a vision, motivating the group toward higher goals, encouraging creative thinking, and being considerate of individual employees), for instance, have been found to be negatively associated with stress and burnout, and positively associated with self-rated psychosocial well-being. 43 – 46 Transformational leadership behaviours can also decrease staff absenteeism, 47 turnover intention, 48 , 49 and enhance staff retention 50 —concerns currently of paramount importance as record numbers of health professionals in Canada are leaving their respective professions. Literature also suggests that the reduction in absenteeism and improved retention applies to health workers at all career stages, ranging from novice to senior, 51 , 52 which is significant as health worker attrition is seen across the career trajectory.
The COVID-19 pandemic has highlighted the importance of leadership in responding to crisis. Some researchers have proposed or reviewed leadership models and frameworks that could be effective in different contexts (including healthcare) during the pandemic. 53 – 57 For instance, the LEADS leadership capabilities framework identifies the characteristics of good leaders (ie, lead self, engage others, achieve results, develop coalitions, and champion system transformation) but may require adaptation to context. 58
This study is part of a larger Healthy Professional Worker project that examines mental health, leaves of absence and return to work experiences of professional workers. In this paper, we present findings from four health professional case studies—Nursing, Medicine, Midwifery, and Dentistry—from surveys and interviews conducted between November 2020 and July 2021.
An interdisciplinary mixed methods approach was undertaken to accommodate the complexity of intersectional, contextualized experiences along the pathway from mental health through to leaves of absence and return to work.
Case studies
The professions we focus on represent a mix of gender composition and work context features that the literature suggests are important to mental health. Dentistry and Medicine are traditionally masculine professions that are feminizing, 59 , 60 whereas Nursing and Midwifery are traditionally feminine professions. Work contexts range from unionized salaried positions, with both regular and irregular schedules, to independent public sector contractors in solo or group practices, to owners of clinics in the private sector.
Worker surveys
Between the end of November 2020 and early May 2021, a bilingual (French-English) on-line, self-administered survey employing crowdsourcing recruitment via our partner organizations, direct e-mail and social media was undertaken. The survey design included cross-cutting questions asked of all case studies, particularly focusing on the mental health, leave of absence, and return to work pathway, but also including a component which assessed mental health, distress, presenteeism, and burnout during as compared to prior to the pandemic. In the context of this study, mental health issues include mental or psychological stress or distress, burnout, anxiety, depression, other mood disorders, substance use or dependence, PTSD or serious thoughts of suicide. For each case study, an additional set of customized questions specific to the unique work circumstances of the profession were included. An initial profession-specific question filtered participants to the appropriate questionnaire which employed a skip-logic invisible to the participants, resulting in a survey taking approximately 20 minutes to complete.
A total of 1,860 ( 1,569 who identified as women and 291 as men ) surveys that yielded at least a 90% completion score for the four case study professions were retained for analysis. Reported here are descriptive analyses of the survey data including frequency cross-tabulations where appropriate tests of significance were undertaken at a P < .05 significance threshold.
Worker interviews
Concurrent with the surveys, a total of 163 ( 132 who identified as women and 36 as men ) in-depth interviews were conducted either by phone or by Zoom, in French or English between January and July 2021. Recruitment for the interviews was undertaken directly through the same crowdsourcing approach as for the survey and indirectly where survey participants volunteered to undertake a follow-up interview after they completed the survey. A set of screening questions were sent to participants to ensure representation by gender, region, work setting, leave of absence experiences, and other criteria important to the individual case studies. Two team members conducted the interviews, with one member being the primary interviewer and the other member taking notes and interjecting to probe in more depth into specific issues. All interviews were audio recorded, transcribed with Otter.AI, reviewed and analyzed using NVIVO software. A combined a priori coding scheme that reflects both a set of standardized codes that cut across cases and case specific codes that were both developed a priori and have emerged through the coding process were applied to interview segments. To supplement the survey data, select quotes are included in the paper.
Background of survey respondents and interview participants
Table 1 provides an overview of the survey respondents by province. The largest number of responses came from the provinces of Ontario and Quebec with Nova Scotia, British Columbia, and Alberta figuring prominently.
HPW survey respondents by province a .
| Province | Dentistry | Medicine | Midwifery | Nursing | Total |
|---|---|---|---|---|---|
| BC | 63 | 29 | 30 | 77 | 199 |
| AB | 11 | 33 | 12 | 91 | 147 |
| SK | 0 | 14 | 0 | 40 | 54 |
| MB | 7 | 7 | 9 | 37 | 60 |
| ON | 217 | 120 | 111 | 185 | 633 |
| QC | 13 | 41 | 11 | 210 | 275 |
| NB | 0 | 0 | 0 | 106 | 106 |
| PE | 0 | 0 | 0 | 12 | 12 |
| NS | 27 | 9 | 0 | 108 | 144 |
| NL | 0 | 17 | 0 | 20 | 37 |
| NT/NU/YT | 0 | 0 | 0 | 0 | 0 |
| Missing | 44 | 33 | 19 | 120 | 216 |
a Some of the zeros in the table are suppressed data representing less than 5 respondents.
Also important for our consideration is the breakdown by gender identity where respondents who identify as women predominate, even in those professions where the gender breakdown is more balanced ( Table 2 ). There were a total of 231 respondents who identify as Black, Indigenous, or health professionals of colour.
Participants by case study and data collection method a .
| Professional worker surveys | Professional worker interviews | |
|---|---|---|
| Dentistry | 397 | 36: |
| Medicine | 310 | 29: |
| Midwifery | 202 | 44: |
| Nursing | 1,013 | 54: |
a The total numbers may not add up given we allowed participants to leave the question blank, to identify as non-binary or to self-describe.
b The Medicine and Midwifery cases included trainee participants in the survey and interviews.
Pathway from mental health, leaves of absence to return to work
Our primary research objective was to understand the pathway from the experience of mental health issues to the decision to contemplate or take a leave of absence and return to work. Figure 1 depicts the proportion of our survey respondents that embarked on this pathway, including steps in between, such as making changes to their work and considering taking a leave, even if one was not taken.

Experiences of mental health and the pathway to leaves of absence and return to work, by profession.
Overall, 62% of professional workers who responded to our survey report having any experience of mental ill-health at any time during work or training. This may seem high but respondents who have lived or living experience with mental health issues are likely self-selected to participate in a study focused on this topic and our definition was quite broad. Of those, 60% made changes to work in response to their mental health issue; 53% contemplated taking a leave but only 29% took a leave of absence from work due to their mental health experiences. The vast majority of those who took a leave (73%) returned to work.
Although caution should be exercised in comparing across professions because our respondents do not constitute a representative sample of the professional groups, some interesting differences are notable. In comparison to professional workers overall:
- (1) Respondents from Dentistry are significantly less likely to report having ever suffered from a mental health issue, whereas respondents from Midwifery and Nursing are significantly more likely.
- (2) Respondents from Dentistry were significantly less likely to contemplate a leave, whereas respondents from Nursing were significantly more likely to contemplate a leave.
- (3) Respondents from Nursing were significantly more likely to report taking a leave of absence from work, whereas respondents from Dentistry, Medicine, and Midwifery were significantly less likely to have taken a leave.
Notably, the differences we found along this pathway by gender identity were in the experience of mental health issues (reported by 65% of respondents who identified as women in comparison to 45% of respondents who identified as men); the consideration of taking a leave (54% among women and 40% among men); and actually, taking a leave (29% among women and 20% among men). There were no significant differences in the rates of return to work, largely due to small sample sizes.
Across all professional respondents, the main reason why mental health leaves were not taken was that they felt that the mental health issue they were experiencing was not severe enough to warrant a leave; the only exception was for respondents from Medicine for whom the most likely response was because of the stigma that disclosure of a mental health issue at work would entail ( Figure 2 ). Stigma and concern about the professional impact of taking a mental health leave from work was a close second for all professional respondents except those from Dentistry. Financial barriers to taking a leave were noted in the top three most frequent responses from Dentistry, Midwifery, and Nursing respondents.
“What pushed me to take that leave of absence was I wasn't able to, I didn't feel like I could take care of myself outside of work anymore. I felt as though I had given everything I had to, to thrive and work in this environment, that when I went home, I was done, exhausted.” Nursing Participant
“I think just the reluctance to talk about it for fear if word gets out it may affect their practice … So I think the barrier would be still the stigma surrounding this whole issue, this whole area of illness.” Dentistry Stakeholder

Top three reasons mental health leaves were not taken, by profession, percentage of respondents.
The factor that facilitated the taking of a leave of absence from work for mental health issues was most likely to be financial support or coverage while on leave, with supportive colleagues, supervisors, and family also figuring prominently ( Figure 3 ). Similarly, the barriers experienced when taking a leave most often cited by participants were unsupportive supervisors, colleagues, and union representatives and a lack of financial coverage while on leave ( Figure 4 ).
“Trying to accommodate everybody else and the resentment that comes from that. And I think it’s a time where resources are already stretched so midwives find that it’s easy to justify undue hardship.” Midwifery Stakeholder
“… you can’t get a locum here to save your life.” Medicine Participant
“… it’s just not financially feasible.” Medicine Participant

Top two facilitators to taking a leave of absence from work for mental health issues by profession, percentage of respondents.

Top two barriers experienced when taking a leave of absence from work for mental health issues by profession*, Percentage of respondents. *There were insufficient data to report for Dentistry.
Having supportive colleagues and supervisors figured prominently in facilitating return to work after a leave of absence due to mental health issues. Similarly, unsupportive supervisors and a lack of workplace accommodations, policies, and programs were barriers ( Figure 5 ).
“I was really fearful to go back and, and see that, you know, the environment hadn't changed, and everything is still the same … I went back into the same toxic environment.”
Nursing Participant
“… the first day is, is pretty brutal … having a structure when you can go back progressively, is very important, because otherwise it's very difficult mentally.” Medicine Participant

Facilitators and barriers identified by all health professional respondents who returned to work, percentage of respondents.
Midwifery and Nursing respondents were queried specifically about support they receive from their supervisors ( Figure 6 ). For both, they were more likely to report supervisors taking time to talk when they were upset than they were to tell them about resources that could help.

Mental health supports from supervisors by percentage of Midwifery and Nursing respondents.
Considering the significant mental health concerns that have arisen during the COVID-19 pandemic, these findings are of critical importance. Pandemic-focused research has revealed that supervisors have felt both ambiguity and at times under-prepared for certain roles in responding to the pandemic, including protecting worker psychological health and safety. 61 Supervisors are instrumental in supporting work-life satisfaction, psychological health and well-being at work, 43 - 46 and health worker retention 49 , 50 and as such we encourage those at all levels of health supervision and leadership to reflect on how their positions can uniquely mediate the psychological health and well-being of the health workforce. We encourage supervisors, managers, and those in leadership roles to take an explicit profession- and gender-based approach that recognizes the influence of individual, work, and family circumstances on health worker mental health. We also encourage those in supervisory positions to reflect upon their leadership style because it has the potential to improve workforce mental health and health worker retention. Given that leadership can play an important role in mitigating mental health issues, investment in both leadership training and mentorship is an important first step in acting upon our research findings.
In sum , the findings from our research on the pathway from the experience of mental health through to subsequent decisions to take a leave of absence from work ( or not ) and then to return reveal some important concerns and opportunities for intervention. Across professions, there is a need to de-stigmatize mental health issues and encourage greater awareness and support from leaders, supervisors, and colleagues recognizing that both gender and leadership matter greatly. Our findings of how this pathway differed among the health professions suggests that it will be important to study these phenomena in other health professions so as to further explore how different work context influences workers’ experiences of mental health.
Acknowledgements
We would also like to acknowledge the support provided by Renata Khalikova, Kennedy Onyechie and Christine Tulk to the data visualizations.
Funding: This work was supported by the Canadian Institutes of Health Research and Social Sciences and Humanities Research Council of Canada for the Healthy Professional Worker Partnership grant.
Ivy L. Bourgeault https://orcid.org/0000-0002-5113-9243

The Savvy Scientist
Experiences of a London PhD student and beyond
PhD Burnout: Managing Energy, Stress, Anxiety & Your Mental Health

PhDs are renowned for being stressful and when you add a global pandemic into the mix it’s no surprise that many students are struggling with their mental health. Unfortunately this can often lead to PhD fatigue which may eventually lead to burnout.
In this post we’ll explore what academic burnout is and how it comes about, then discuss some tips I picked up for managing mental health during my own PhD.
Please note that I am by no means an expert in this area. I’ve worked in seven different labs before, during and after my PhD so I have a fair idea of research stress but even so, I don’t have all the answers.
If you’re feeling burnt out or depressed and finding the pressure too much, please reach out to friends and family or give the Samaritans a call to talk things through.
Note – This post, and its follow on about maintaining PhD motivation were inspired by a reader who asked for recommendations on dealing with PhD fatigue. I love hearing from all of you, so if you have any ideas for topics which you, or others, could find useful please do let me know either in the comments section below or by getting in contact . Or just pop me a message to say hi. 🙂
This post is part of my PhD mindset series, you can check out the full series below:
- PhD Burnout: Managing Energy, Stress, Anxiety & Your Mental Health (this part!)
- PhD Motivation: How to Stay Driven From Cover Letter to Completion
- How to Stop Procrastinating and Start Studying
What is PhD Burnout?
Whenever I’ve gone anywhere near social media relating to PhDs I see overwhelmed PhD students who are some combination of overwhelmed, de-energised or depressed.
Specifically I often see Americans talking about the importance of talking through their PhD difficulties with a therapist, which I find a little alarming. It’s great to seek help but even better to avoid the need in the first place.
Sadly, none of this is unusual. As this survey shows, depression is common for PhD students and of note: at higher levels than for working professionals.
All of these feelings can be connected to academic burnout.
The World Health Organisation classifies burnout as a syndrome with symptoms of:
– Feelings of energy depletion or exhaustion; – Increased mental distance from one’s job, or feelings of negativism or cynicism related to one’s job; – Reduced professional efficacy. Symptoms of burnout as classified by the WHO. Source .
This often leads to students falling completely out of love with the topic they decided to spend years of their life researching!
The pandemic has added extra pressures and constraints which can make it even more difficult to have a well balanced and positive PhD experience. Therefore it is more important than ever to take care of yourself, so that not only can you continue to make progress in your project but also ensure you stay healthy.
What are the Stages of Burnout?
Psychologists Herbert Freudenberger and Gail North developed a 12 stage model of burnout. The following graphic by The Present Psychologist does a great job at conveying each of these.

I don’t know about you, but I can personally identify with several of the stages and it’s scary to see how they can potentially lead down a path to complete mental and physical burnout. I also think it’s interesting that neglecting needs (stage 3) happens so early on. If you check in with yourself regularly you can hopefully halt your burnout journey at that point.
PhDs can be tough but burnout isn’t an inevitability. Here are a few suggestions for how you can look after your mental health and avoid academic burnout.
Overcoming PhD Burnout
Manage your energy levels, maintaining energy levels day to day.
- Eat well and eat regularly. Try to avoid nutritionless high sugar foods which can play havoc with your energy levels. Instead aim for low GI food . Maybe I’m just getting old but I really do recommend eating some fruit and veg. My favourite book of 2021, How Not to Die: Discover the Foods Scientifically Proven to Prevent and Reduce Disease , is well worth a read. Not a fan of veggies? Either disguise them or at least eat some fruit such as apples and bananas. Sliced apple with some peanut butter is a delicious and nutritious low GI snack. Check out my series of posts on cooking nutritious meals on a budget.
- Get enough sleep. It doesn’t take PhD-level research to realise that you need to rest properly if you want to avoid becoming exhausted! How much sleep someone needs to feel well-rested varies person to person, so I won’t prescribe that you get a specific amount, but 6-9 hours is the range typically recommended. Personally, I take getting enough sleep very seriously and try to get a minimum of 8 hours.
A side note on caffeine consumption: Do PhD students need caffeine to survive?
In a word, no!
Although a culture of caffeine consumption goes hand in hand with intense work, PhD students certainly don’t need caffeine to survive. How do I know? I didn’t have any at all during my own PhD. In fact, I wrote a whole post about it .
By all means consume as much caffeine as you want, just know that it doesn’t have to be a prerequisite for successfully completing a PhD.
Maintaining energy throughout your whole PhD
- Pace yourself. As I mention later in the post I strongly recommend treating your PhD like a normal full-time job. This means only working 40 hours per week, Monday to Friday. Doing so could help realign your stress, anxiety and depression levels with comparatively less-depressed professional workers . There will of course be times when this isn’t possible and you’ll need to work longer hours to make a certain deadline. But working long hours should not be the norm. It’s good to try and balance the workload as best you can across the whole of your PhD. For instance, I often encourage people to start writing papers earlier than they think as these can later become chapters in your thesis. It’s things like this that can help you avoid excess stress in your final year.
- Take time off to recharge. All work and no play makes for an exhausted PhD student! Make the most of opportunities to get involved with extracurricular activities (often at a discount!). I wrote a whole post about making the most of opportunities during your PhD . PhD students should have time for a social life, again I’ve written about that . Also give yourself permission to take time-off day to day for self care, whether that’s to go for a walk in nature, meet friends or binge-watch a show on Netflix. Even within a single working day I often find I’m far more efficient when I break up my work into chunks and allow myself to take time off in-between. This is also a good way to avoid procrastination!
Reduce Stress and Anxiety
During your PhD there will inevitably be times of stress. Your experiments may not be going as planned, deadlines may be coming up fast or you may find yourself pushed too far outside of your comfort zone. But if you manage your response well you’ll hopefully be able to avoid PhD burnout. I’ll say it again: stress does not need to lead to burnout!
Everyone is unique in terms of what works for them so I’d recommend writing down a list of what you find helpful when you feel stressed, anxious or sad and then you can refer to it when you next experience that feeling.
I’ve created a mental health reminders print-out to refer to when times get tough. It’s available now in the resources library (subscribe for free to get the password!).

Below are a few general suggestions to avoid PhD burnout which work for me and you may find helpful.
- Exercise. When you’re feeling down it can be tough to motivate yourself to go and exercise but I always feel much better for it afterwards. When we exercise it helps our body to adapt at dealing with stress, so getting into a good habit can work wonders for both your mental and physical health. Why not see if your uni has any unusual sports or activities you could try? I tried scuba diving and surfing while at Imperial! But remember, exercise doesn’t need to be difficult. It could just involve going for a walk around the block at lunch or taking the stairs rather than the lift.
- Cook / Bake. I appreciate that for many people cooking can be anything but relaxing, so if you don’t enjoy the pressure of cooking an actual meal perhaps give baking a go. Personally I really enjoy putting a podcast on and making food. Pinterest and Youtube can be great visual places to find new recipes.
- Let your mind relax. Switching off is a skill and I’ve found meditation a great way to help clear my mind. It’s amazing how noticeably different I can feel afterwards, having not previously been aware of how many thoughts were buzzing around! Yoga can also be another good way to relax and be present in the moment. My partner and I have been working our way through 30 Days of Yoga with Adriene on Youtube and I’d recommend it as a good way to ease yourself in. As well as being great for your mind, yoga also ticks the box for exercise!
- Read a book. I’ve previously written about the benefits of reading fiction * and I still believe it’s one of the best ways to relax. Reading allows you to immerse yourself in a different world and it’s a great way to entertain yourself during a commute.
* Wondering how I got something published in Science ? Read my guide here .
Talk It Through
- Meet with your supervisor. Don’t suffer in silence, if you’re finding yourself struggling or burned out raise this with your supervisor and they should be able to work with you to find ways to reduce the pressure. This may involve you taking some time off, delegating some of your workload, suggesting an alternative course of action or signposting you to services your university offers.
Also remember that facing PhD-related challenges can be common. I wrote a whole post about mine in case you want to cheer yourself up! We can’t control everything we encounter, but we can control our response.
A free self-care checklist is also now available in the resources library , providing ideas to stay healthy and avoid PhD burnout.

Top Tips for Avoiding PhD Burnout
On top of everything we’ve covered in the sections above, here are a few overarching tips which I think could help you to avoid PhD burnout:
- Work sensible hours . You shouldn’t feel under pressure from your supervisor or anyone else to be pulling crazy hours on a regular basis. Even if you adore your project it isn’t healthy to be forfeiting other aspects of your life such as food, sleep and friends. As a starting point I suggest treating your PhD as a 9-5 job. About a year into my PhD I shared how many hours I was working .
- Reduce your use of social media. If you feel like social media could be having a negative impact on your mental health, why not try having a break from it?
- Do things outside of your PhD . Bonus points if this includes spending time outdoors, getting exercise or spending time with friends. Basically, make sure the PhD isn’t the only thing occupying both your mental and physical ife.
- Regularly check in on how you’re feeling. If you wait until you’re truly burnt out before seeking help, it is likely to take you a long time to recover and you may even feel that dropping out is your only option. While that can be a completely valid choice I would strongly suggest to check in with yourself on a regular basis and speak to someone early on (be that your supervisor, or a friend or family member) if you find yourself struggling.
I really hope that this post has been useful for you. Nothing is more important than your mental health and PhD burnout can really disrupt that. If you’ve got any comments or suggestions which you think other PhD scholars could find useful please feel free to share them in the comments section below.
You can subscribe for more content here:
Share this:
- Click to share on Facebook (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on Reddit (Opens in new window)
Related Posts

Minor Corrections: How To Make Them and Succeed With Your PhD Thesis
2nd June 2024 2nd June 2024

How to Master Data Management in Research
25th April 2024 27th April 2024

Thesis Title: Examples and Suggestions from a PhD Grad
23rd February 2024 23rd February 2024
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Notify me of follow-up comments by email.
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Privacy Overview
Navigating Clinical Psychology Ph.D. Programs: How To Choose The Appropriate Fit
If you’re interested in treating mental health disorders, a Ph.D. in clinical psychology is can be a significant step in your pursuit of a fulfilling and impactful career in mental health on your career path. The decision you make about where to pursue your clinical psychology doctorate can be pivotal, shaping not only your educational experience but also your future contributions to the field. As you consider the vast array of clinical psychology programs available, you're likely to face several questions and concerns.
The decision you make about where to pursue your clinical psychology doctorate is pivotal, shaping not only your educational experience but also your future contributions to the field. It's a decision that demands careful consideration., and that's where this comprehensive guide comes in.
This guide will help you navigate the complex landscape of clinical psychology Ph.D. programs. From understanding the various specializations and research opportunities to evaluating factors such as faculty expertise, program accreditation, and financial considerations, we'll provide you with the knowledge and insights necessary to make an informed choice.
This article will help you navigate the complex landscape of clinical psychology Ph.D. programs, whether you're a recent graduate eager to explore the field of clinical psychology or a seasoned professional seeking to advance your career. From understanding the various specializations and research opportunities to evaluating factors such as faculty expertise, program accreditation, and financial considerations, Whether you're a recent graduate eager to dive into the world of clinical psychology or a seasoned professional seeking to advance your career, we aim to empower you with the tools and information you need to embark on your academic journey with confidence. By the end, you'll have a clear understanding of how towe’re providing you with information that can help you choose the right clinical psychology Ph.D. program for you that aligns with your aspirations, ensuring a successful and fulfilling career in the field of mental health.
Understanding clinical psychology Ph.D. programs
Before we explore the specifics of choosing a clinical psychology PhD program, let's review what clinical psychology is all about. Clinical psychology is a field of study and practice that focuses on understanding and addressing mental health concerns. The goal of clinical psychology is to help individuals navigate their psychological challenges and improve their overall well-being. It seeks to understand the individual in their entirety, including their unique experiences, needs, desires, and attachments.
The goal of clinical psychology is to help individuals navigate and overcome their psychological challenges and improve their overall well-being. To achieve this goal, clinical psychologists use a range of assessment, intervention, and research techniques to provide evidence-based treatment and support.
A doctoral degrees allows adequate preparation can provide emerging clinical psychologists with the knowledge and skills necessary to excel in their practice areas. Additionally, a Ph.D. in clinical psychology equips graduates with the necessary skills and knowledge to conduct research that advances the field's understanding of mental health.
Pursuing a Ph.D. in clinical psychology is no small feat; it requires dedication , passion, and perseverance. As you work toward your PhD in clinical psychologyIf you decide to work toward this degree, you'll learn about various therapeutic modalities, treatment approaches, and theoretical orientations. You'll also also develop the critical thinking, research, and analytical skills necessary to understand complex psychological phenomena.
It's important to note that while clinical psychology is a broad field, it differs from other related disciplines like counseling psychology, psychiatry, and social work. Understanding these distinctions will can help you choose the right Ph.D. program for your specific career goals.
- Counseling psychology: Unlike clinical psychologists, who generally focus on address treating severe mental health conditions, counseling psychologists typically focus on helping clients with milder psychological concernslife challenges and milder psychological concerns. Counseling psychologists may work in university counseling centers or practice settings.
- Psychiatry: While clinical psychologists primarily use talk therapy to treat mental health disorders, psychiatrists are medical doctors trained to diagnose and treat mental illnesses using a combination of medication and, in some cases, psychotherapy and therapy.
- Social work: Although Like clinical psychologists, social workers may also provide therapy. Usually unable to diagnose conditions, however,, their primary focus is often on addressing societal and environmental issues that impact mental health. They often work in community-based settings.
While mental health professionals come from diverse backgrounds and disciplines, cThe academic rigor and practical training that clinical psychology Ph.D. programs offer a unique blend of academic rigor and practical training that preparescan adequately prepare graduates for their rewarding careers in mental health care in the field. Through specialized coursework, clinical practicum sexperiences, and research opportunities, these programs provide a comprehensive education that meets the highest standards of academic excellence.
Exploring specializations in clinical psychology
Within clinical psychology Ph.D. programs, there are various specializations that students can pursue. These specializations allow individuals to focus on specific areas of interest and develop expertise in those areas. Before choosing a Ph.D. program, it can be important to exploring explore the different various specializations clinical psychology specialties and considering consider which areas of focus best aligns best with your interests and career goals is important.
Some of the most common specializations within clinical psychology include:
- Neuropsychology: This specialization fNeuropsychologists focusocuses on understanding how brain function impacts behavior and cognition. Neuropsychologists They often work with individuals who have experienced a traumatic brain injury, stroke, or other neurological conditions.
- Child and adolescent psychology: As the name suggests, this specialization focuses on working with children and adolescents. This specialization involves addressing developmental disorders, behavioral challenges, or specific issues related to childhood trauma-related conditions, and other mental health concerns in children and teenagers.
- Geriatric psychology: This specialization focuses on geriatric psychologists understanding and treating address mental health concerns in older adults. Geriatric psychologists often work in nursing homes, assisted living facilities, or practice settings.
- Forensic psychology: This specialization focus area involves applying psychological principles in the legal system. Forensic psychologists may work with law enforcement, attorneys, and the court systems to evaluate individuals involved in legal proceedings or provide expert testimony.
These are just a few examples of specializations within clinical psychology; there are many others to explore. As you consider which specializations best fits your interestsyou’re interested in pursuing, you should also reflect on your personal experiences, strengths, and values. Choosing a specialization that aligns with these factors will not onlycan make your academic journey more fulfilling but also setand set you up for success in your future career.
How to pick the right clinical psychology Ph.D. program
Now that we have a better understanding of what clinical psychology is and the various specializations within the field, let's discuss how to pChoosingick the right Ph.D. program for you can help ensure you have a rewarding academic experience. In addition to researching programs online, you may want to take campus visits, ask to audit classes, and talk with professors and administrators. As with any major life decision, it's critical to approach this process thoughtfully and deliberately.
Here are some factors to consider as you evaluate different clinical psychology Ph.D. programs:
- Faculty expertise: One of the most crucial elements to consider is the fFaculty members within the a Ph.D. program. These individuals will guide your academic and professional development, so it's paramount to, so consider researching their expertise and qualifications.
- Accreditation and reputation: It's also important to consider whether aYou may want to limit your search to programs has that have been accredited by reputable organizations like the American Psychological Association (APA) . You may also want to researchcan also find information about a each program's reputation and ranking within the field.
- Financial considerations: Pursuing a Ph.D. is may involve a significant monetary investment, so it's it can be crucial important to understand the a program's tuition costs and available financial aid options. You'll likely also want to consider the how your potential long-term career prospects and how theywill align with your financial goals.
- Campus culture and environment: The campus cultureThe student life and setting of a school can play a significant role in your academic experience. Consider factors like location, campus resources, and the overall atmosphere of the program.
- Research opportunities and resources: Since research is a vital aspect of clinical psychology, exploring the research opportunities and resources available within a program is a must. These resources may includeit can help to know the extent to which a program connects students with access to specialized labs, funding for research projects, and collaborations with faculty members.
- Personal preferences: Last but certainly not least, don't forgetRemember to consider your personal preferences and lifestyle factors when evaluating clinical psychology Ph.D. programs. Your happiness and well-being are just as important as your academic and professional successare important, so make sureensure the program you choose aligns with your values and personal needs.
Finding the right clinical psychology Ph.D. program can requires a balance significant amount of research, self-reflection, and careful consideration. Accreditation status and faculty expertise are essential but don't forget toit can also be crucial to consider your personal passions and career goals. Remember that this is your journey, so choose a program that will support you in becoming the best clinical psychologist you can be.
Making your decision and how to apply
Once you have thoroughly researched and evaluated different clinical psychology Ph.D. programs, it's time toyou may be ready to make your decision. Remember that this is a significant investment in yourself and your future, so take the time to weigh all factors carefully.
When it comes to actually applying for a program, here are some tips to keep in mind:
- Createing a structured decision-making process: Developing a structured approach tothorough decision-making framework can help you stay organized as you choose a programnd make a well-informed choice. You might create a spreadsheet with criteria to evaluate each program school or simply make a list of pros and cons.
- Utilizing a decision matrix: A decision matrix is a helpful tool for evaluating and comparing different programs based on specific criteria. You can assign weights to each criterion and rank programs accordingly, which can help you visually seedecide which program schools aligns best with your personal and professional goals.
- Seeking advice and input: Don't be afraid to rConsider reachingeach out to mentors, advisors, and peers for their perspectives on different programs. They may offer have valuable insights or considerations that you hadn't thought of before.
Once you've chosen the a program that's right for you, it's time toyou can begin preparing your application. Your applicationThis may involve taking prerequisite courses, obtaining letters of recommendation, writing a personal statement or essay, and taking standardized tests like the GRE.
The Office of Program Consultation and Accreditation within the APA is an excellent helpful resource for understanding common application requirements and tips for crafting a compelling application. Additionally, it can be's beneficial to reach out directly to the department or school you're applying to for specific guidance on their application process.
Remember, don't be discouraged if you're not accepted into your top-choice program. It's normal for many applicants to apply to multiple programs and receive rejections before finding the right fit. Many schools also offer candidates the opportunity to reapply after they gaining have gained more experience or improving improved your their application materials. Patience and perseverance are can be key in this process.
Additional resources and support for your journey
In addition to academia, it's important to remember that those considering a Ph.D. program or seeking guidance for other sources and support are available to assist with personal and professional development in the field of clinical psychology, support is available. Graduates who are beginning their careers in clinical psychology might find it beneficial to seek utilize support from professional organizations, mentorship programs, and education resources.
Mental health professionals can benefit from seeking care themselves at times; and an online therapy platform like BetterHelp has become a significant part of mental health support can provide convenient, flexible means of receiving support, especially given recent global events. This mode of Online therapy provides access to mental health resources irrespective of location can connect you with mental health resources remotely, allowing you to work with a therapist through video call, voice call, or in-app messaging offering convenience and flexibility. As If you’re an emerging clinical psychologist or a busy professional of any kind, you may benefit from utilizing an online therapy platform to connect with experienced professionals and gain additional support and guidance participating in therapy on a schedule that works for you.
Cognitive behavioral therapy (CBT) Cognitive behavioral therapy (CBT) is a well-established, evidence-based approach to mental health treatment often utilized in online therapy. Clinical studies indicate it may can treat a range of mental health symptoms and conditions. In a study on the effects of an online cognitive behavioral therapy program for healthcare workers, participants reported experiencing reduced stress levels, improved self-care, and an increased capacity to cope with their emotions . If a rigorous PhD program leaves you feeling overwhelmed, consider turning to CBT techniques and resources for support. Burnout can be a common issue among students in high-stress occupations, and CBT has been shown to be helpful in promoting overall well-being.
Remember, it's important to prioritize your mental health and well-being throughout your journey as a clinical psychology PhD student. In the end, your personal and professional growth will benefit from taking care of yourself and utilizing the resources and support available to you.
Clinical psychology offers a world ofan array of opportunitiesy for those passionate about understanding and supporting treating mental health concerns. With the right program, resources, and support, you can embark on an empowering journey to becoming a highly skilled and compassionate clinical psychologist. Remember that, it's also important to prioritize your own mental health and well-being throughout your journey as a clinical psychology Ph.D. student. In the end, your personal and professional growth will benefit from taking care of yourself and utilizing the resources and support available to you.
Online therapy can also be a helpful tool for personal and professional development, so don't hesitate to utilize it as you navigate through your academic journey.
- What Are The Different Types Of Counseling Degrees? Medically reviewed by Melissa Guarnaccia , LCSW
- What Type Of Therapist Should I Be? Exploring Paths In Mental Health And Wellness Medically reviewed by Julie Dodson , MA
- Therapist Tools
- Relationships and Relations
Join us on campus for an undergraduate information session on Saturday, June 22.
- About Immaculata
- Why Choose Immaculata?
- Mission, Values and History
- Fast Facts, Rankings, Accreditations
- Diversity, Equity and Inclusion
- Sustainability
- Institutional Research
- Consumer Information
- Admissions Overview
- Transfer to IU
- Undergraduate Admissions
- Adult Professional Programs Admissions
- Graduate Admissions
- Visiting/Non-Degree Students
- International Students
- Military & Veterans
- Financial Aid
- Tuition & Fees
- Visit Campus
- Academics Overview
- Degrees & Programs
- Colleges & Departments
- Catalogs, Schedules & Calendar
- Academic Options
- Advising & Support Services
- Commencement
- Campus Life Overview
- Living on Campus
- Health & Counseling Services
- Campus Ministry
- Campus Safety
- Student Services
- New Student Orientation
- Athletics Overview
- Mighty Macs Athletics Site
- Campus Store
- Immaculata News
- Student Writing
- Alumni Profiles
- Events Calendar
- Immaculata Magazine
Counselor Education and Supervision, Ph.D.
Advance in the growing mental health field as an effective counselor educator, clinical supervisor, researcher or clinician.
Through theoretical and didactic content, along with practical and experiential activities, you will be instructed intensively in counseling pedagogy, clinical supervision, advanced counseling theory and techniques, quantitative and qualitative research methodology and social justice and advocacy standards. You will be prepared to:
- Teach in graduate counseling programs
- Use advanced counseling skills with client populations
- Supervise master’s-level counseling students and post-master’s counselors in need of licensure supervision
- Conduct high-quality and meaningful research
- Advocate for students, clients and the counseling profession
At A Glance
Program: ph.d. in counselor education and supervision, audience: graduate students, format: hybrid (face-to-face and online), next start date: fall 2025, cost: $990/credit, time to completion three years.
“As mental health continues to take priority for many, well-trained clinical mental health counselors are in demand. Doctoral students’ investment in learning to teach, provide clinical supervision and mentor the new generation of counselors is a privilege with the potential for exponential results.”
David Martinson, Ph.D. LPC Clinical Mental Health Counseling Professor and Chair of Immaculata’s Department of Psychology and Counseling
Career Outlook
Sample job titles and settings include:
- Counselor educator or faculty member in a university
- Clinical supervisor, clinician or supervisor in a hospital, outpatient mental health or substance abuse center, residential facility, health care facility or private practice
- According to the Bureau of Labor Statistics, the profession of substance abuse, behavioral disorder and mental health counseling is projected to grow 18% , much faster than average , over the next decade. Median salaries may range from $53,710 for mental health clinicians to $84,380 for academic faculty .
Program Highlights
- Hybrid delivery for working professionals —Pursue this Ph.D. with a blend of evening and weekend courses offered through online synchronous and face-to-face formats.
- Three-year program —Experiential and research-based components are integrated throughout the course sequencing, allowing you to complete the degree in as little as three years.
- Collaborative cohort model —Small class sizes provide a personalized experience while building your professional network.
- Affordability —Immaculata offers competitive tuition, with financial aid and graduate assistantship positions .
- Internships —Gain hands-on experience working in clinical, educational and supervisory settings via three 200-hour internships. Through our CACREP-accredited M.A. in Clinical Mental Health Counseling , you can engage in supervision and teaching experiences on site at Immaculata University.
- Research —Develop conceptual knowledge regarding a novel topic and acquire an in-depth understanding of the construct through research theory, methodology, strategies and application through the completion of the dissertation study.
- Ryan Bowers, Ph.D.
- David Hunt, Ph.D.
- David Martinson, Ph.D.
- Noah Schoch, Ph.D.
- Shayna Finn, Ph.D.
- Accreditation —The Ph.D. in Counselor Education and Supervision is structured and built upon the five pillars of knowledge and application set forth by the Council for Accreditation of Counseling and Related Educational Programs (CACREP), which are counseling, teaching, scholarship and research, supervision, and leadership/advocacy, in preparation for seeking accreditation. Immaculata University will apply for CACREP accreditation once students have been admitted into the program and the University has collected ample program evaluation data as required. The Ph.D. program will use the same structure and evaluation matrix as Immaculata’s already CACREP-accredited clinical mental health counseling program.
Course Overview
63 total credits
- CESD 701: Professional Orientation and Ethics in Counselor Education and Supervision (3 credits)
- CESD 702: Professional and Technical Writing for Counselor Education and Supervision (3 credits)
- CESD 703: Advanced Clinical Counseling Theory (3 credits)
- CESD 704: Counseling Supervision (3 credits)
- CESD 705: Counselor Education Pedagogy (3 credits)
- CESD 706: Qualitative Research I (3 credits)
- CESD 707: Quantitative Research I (3 credits)
- CESD 708: Quantitative Research II (3 credits)
- CESD 709: Diverse Leadership in Counselor Education and Supervision (3 credits)
- CESD 710: Clinical Counseling Internship* (min. 200 hours; 3 credits)
- CESD 711: Counselor Education Internship* (min. 200 hours; 3 credits)
- CESD 712: Counselor Supervision Internship* (min. 200 hours; 3 credits)
- CESD 713: Advanced Assessment in Counselor Education and Supervision (3 credits)
- CESD 714: Current Issues in Higher Education for Counselor Educators and Supervisors (3 credits)
- CESD 715: Qualitative Research II (3 credits)
- CESD 716: Counselor Education and Supervision Dissertation Seminar (3 credits)
- CESD 720: Clinical Mental Health Counseling Seminar (3 credits)
- CESD 721: School Counseling Seminar (3 credits)
- CESD 722: Addiction Counseling Seminar (3 credits)
- CESD 723: Student Affairs Counseling Seminar (3 credits)
- CESD 724: Program Evaluation and Consultation (3 credits)
- CESD 798: Counselor Education and Supervision Comprehensive Examination (0 credits)
- CESD 700: Counselor Education and Supervision Continuing Dissertation (1 credit)
Student Learning Outcomes
- Apply the integration of evidence-based theories to the conceptualization, interventions and personalization of clients while attending to multicultural competencies and being conscious of clinical effectiveness.
- Demonstrate legal and ethical evidence-based theoretical framework and models of counseling supervision through multimodal structures while attending to multicultural competencies and being conscious of clinical effectiveness.
- Demonstrate understanding through application of roles and responsibilities of being an effective counselor educator by using evidence-based pedagogy and multicultural applications for classroom effectiveness.
- Employ the consumption and creation of qualitative, quantitative and mixed-method research and data analysis through scholarship activities and creation of creative scholarship through action research.
- Demonstrate understanding of leadership and advocacy models and the application to professional organizations, consultation and clients at the individual, system and policy levels.
Admission Requirements
Qualified applicants must possess a master’s degree in counseling or related discipline from a regionally accredited institution meeting master’s level academic requirements. While completion of a CACREP-accredited program is preferred, it is not required. Students with a master’s degree in counseling from a non-CACREP-accredited program may have to complete additional courses at the master’s level, as determined by the program director and department chair.
Applications are due January 15 for fall admission. View complete admission requirements .
Ryan Bowers, Ph.D., LPC, NCC, CAADC
Assistant professor, ph.d. program director, discover immaculata, grounded in ihm tradition and charism since 1920, find out what an iu education can do for your mind, your character and your future..
- Share full article
Advertisement
Supported by
PTSD Has Surged Among College Students
The prevalence of post-traumatic stress disorder among college students rose to 7.5 percent in 2022, more than double the rate five years earlier, researchers found.

By Ellen Barry
Post-traumatic stress disorder diagnoses among college students more than doubled between 2017 and 2022, climbing most sharply as the coronavirus pandemic shut down campuses and upended young adults’ lives, according to new research published on Thursday.
The prevalence of PTSD rose to 7.5 percent from 3.4 percent during that period, according to the findings . Researchers analyzed responses from more than 390,000 participants in the Healthy Minds Study, an annual web-based survey.
“The magnitude of this rise is indeed shocking,” said Yusen Zhai, the paper’s lead author, who heads the community counseling clinic at the University of Alabama at Birmingham. His clinic had seen more young people struggling in the aftermath of traumatic events. So he expected an increase, but not such a large one.
Dr. Zhai, an assistant professor in the Department of Human Studies, attributed the rise to “broader societal stressors” on college students, such as campus shootings, social unrest and the sudden loss of loved ones from the coronavirus.
PTSD is a mental health disorder characterized by intrusive thoughts, flashbacks and heightened sensitivity to reminders of an event, continuing more than a month after it occurs.
It is a relatively common disorder , with an estimated 5 percent of adults in the United States experiencing it in any given year, according to the most recent epidemiological survey conducted by the Department of Health and Human Services. Lifetime prevalence is 8 percent in women and 4 percent in men, the survey found.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
COVID-19: Vaccine Program | Testing | Visitor Guidelines | Information for Employees MONKEYPOX: UConn Health is NOT currently offering the monkeypox vaccine. Please visit the CT DPH website for more information or contact your health provider directly. -->
School of Medicine
Department of Public Health Sciences
Maria (mayte) restrepo-ruiz, phd, is now an assistant professor.
Having received her PhD in our department in 2021 for her study titled, “Armed Conflict, Intimate Partner Violence and Women’s Mental Health: An Explanatory Mixed-Methods Study.” She will continue her work with the Connecticut Office of Early Childhood as well as teach a course on Global Health in the Program in Applied Public Health Sciences.
Currently, Dr. Restrepo is working on building a surveillance system for Adverse and Positive Childhood Experiences in Connecticut using publicly available and administrative data sources. Data from this system will be used to identify child populations at higher risk of adverse childhood experiences and gaps in the provision of prevention programs. She expects data from this system will be available to the public through a web portal in 2023. She is also collaborating with colleagues from Colombia and Puerto Rico on a project to understand better the role of potentially traumatic experiences in children’s mental health in socio-politically complex contexts. Dr. Restrepo’s goal is to advance her research in preventing adverse experiences in childhood by focusing on factors that have been found to promote positive health outcomes despite adversity.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *

Watch Morning Joe Highlights: June 7

The beating heart of Asbury: New book honors Jersey Shore's own Stone Pony

RNC hires a prominent 'Stop the Steal' advocate to help craft its 2024 platform
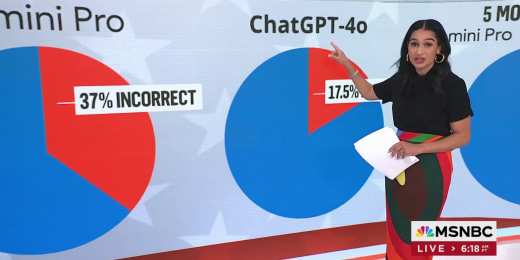
More than a quarter of election information shared by AI factually incorrect: study
'Much higher than expected': U.S. job market adds 272,000 positions in May
'James' re-tells 'Huckleberry Finn' from the perspective of Jim

Parents of Israeli American hostage continue the fight for his return

'The U.S. is standing with you': Biden apologizes to Zelenskyy for holdup in assistance to Ukraine

Officers who defended the Capitol on Jan. 6 booed at Pennsylvania state House
'A draft dodger': Vets slam Trump in new Biden campaign ad

Trump as much product of U.S. history as JFK, Lincoln, Reagan, writer argues

President Biden set to meet with Zelenskyy in Paris

Biden says he will not pardon son Hunter if convicted

Digging into the history passed along the Lincoln Highway
-m198pm.jpg)
Watch Morning Joe Highlights: June 6
Biden the best hope we have for continuing our democracy, says Pa. governor

Doris Kearns Goodwin: I hope 100 years from now, historians see we came to the challenge we're facing
Liz Cheney PAC honors D-Day, says Trump driven by 'spite, revenge and self-pity' in new ad

Secretary Blinken: Biden determined to stand up today as soldiers stood up 80 years ago
President Biden: The struggle between dictatorship and freedom is unending
Morning joe, mental health-related leaves of absence surge, largely driven by women.
- Share this -
Forbes Maggie McGrath and Huma Abedin discuss new research from mental health service provider ComPsych on how women are driving mental health leaves of absence. May 29, 2024
MSNBC HIGHLIGHTS (BEST OF MSNBC)
Alex Wagner Tonight
Discontent with supreme court builds as corruption scandals and political agenda mix.

A good week for reality, a bad week for the Big Lie

The Reidout
‘grifting on your race’: maga republicans' pitch to black voters slammed as 'cynical'.

‘Hateration’: Boom in WNBA ratings and interest brings controversy

Steve Bannon ordered to prison as waves of Trump allies face legal reckonings

The Beat with Ari
How gop may lose 24: trump conviction collides with maga legal 'war' on women, minorities, equality.
| You might be using an unsupported or outdated browser. To get the best possible experience please use the latest version of Chrome, Firefox, Safari, or Microsoft Edge to view this website. |
- Best Master's In Mental Health Counseling Online
Best Master’s In Mental Health Counseling Online Of 2024

Updated: Mar 21, 2024, 12:37pm
Mental health counselors evaluate, manage and treat various mental and emotional health issues, including depression and anxiety, relationship problems, addiction and substance use disorders, and post-traumatic stress disorder. They work with individuals, couples, families and groups, and some specialize in treating specific populations, like children.
If you like the idea of helping people improve their mental and emotional health and well-being, you might consider becoming a mental health counselor, because the career outlook is excellent. As the need for mental health services increases, jobs in the field are expected to grow much faster than average within the next decade.
As a mental health counselor, you’ll need a master’s degree and a state license to practice. An online master’s in mental health counseling can help you meet your state’s qualifications to become a licensed mental health counselor.
Explore some of the best master’s in mental health counseling online programs and find out how to choose the right fit for you.
Why You Can Trust Forbes Advisor Education
Forbes Advisor’s education editors are committed to producing unbiased rankings and informative articles covering online colleges, tech bootcamps and career paths. Our ranking methodologies use data from the National Center for Education Statistics , education providers, and reputable educational and professional organizations. An advisory board of educators and other subject matter experts reviews and verifies our content to bring you trustworthy, up-to-date information. Advertisers do not influence our rankings or editorial content.
- 6,290 accredited, nonprofit colleges and universities analyzed nationwide
- 52 reputable tech bootcamp providers evaluated for our rankings
- All content is fact-checked and updated on an annual basis
- Rankings undergo five rounds of fact-checking
- Only 7.12% of all colleges, universities and bootcamp providers we consider are awarded
Our Methodology
We scored 16 accredited, nonprofit colleges offering online master’s in mental health counseling degree programs in the U.S. using 16 data points in the categories of credibility, affordability, student outcomes, student experience and application process. We pulled the data for these categories from reliable resources such as the Integrated Postsecondary Education Data System ; private, third-party data sources; and individual school and program websites.
We scored schools based on the following categories:
Student Outcomes:
- Overall graduation rate
- Median earnings 10 years after graduation
Affordability:
- In-state graduate student tuition
- In-state graduate student fees
- Alternative tuition plans offered
- Median federal student loan debt
- Percentage of students in federal student loan deferment
Student Experience:
- Student-to-faculty ratio
- Socioeconomic diversity
- Availability of online coursework
- Total number of graduate assistants
- More than 50% of graduate students enrolled in at least some distance education
Credibility:
- Fully accredited
- Programmatic accreditation status
- Nonprofit status
Application Process:
- Acceptance rate
We chose the 10 best schools to display based on those receiving a curved final score of 81.18% or higher.
Find our full list of methodologies here .
- Best Master’s In ABA Online Degrees
- Best Online Master’s In Counseling Psychology
- Best Online Psychology Degrees
- Best Online Psychology Master’s Degrees
Best Online Mental Health Counseling Master’s Degree Options
Should you enroll in an online master’s in mental health counseling program, accreditation for online master’s in mental health counseling programs, how to find the right online mental health counseling master’s program for you, frequently asked questions (faqs) about master’s in mental health counseling online degrees, bradley university, prescott college, catawba college, grace college and theological seminary, malone university, hodges university, seton hall university, faulkner university, university of the southwest, lamar university.

Graduate Tuition
$1,039/credit
Percentage of Grad Students Enrolled in Distance Education
Overall Graduation Rate
Bradley University , based in Peoria, Illinois, offers a master’s in mental health counseling online degree accredited by the Council for Accreditation of Counseling and Related Educational Programs (CACREP). The M.A. in clinical mental health counseling can prepare you to take the national counselor exam and puts you on the path for licensure after graduation.
The curriculum explores neurocounseling, career counseling and research methodology. It includes significant experiential learning: two internships, one practicum and two virtual residencies.
- Our Flexibility Rating: Learn around your 9-to-5
- School Type: Private
- Application Fee: $40
- Degree Credit Requirements: 60 credits
- Program Enrollment Options: Full time
- Notable Major-Specific Courses: Neurocounseling: bridging brain and behavior
- Concentrations Available: N/A
- In-Person Requirements: Yes
$830/credit
You can earn a CACREP-accredited M.S. in counseling with a specialization in clinical mental health counseling from Prescott College , physically located in Prescott, Arizona. The program offers the following areas of emphasis: human sexuality counseling; marriage, couple and family counseling; social justice in counseling; and somatic counseling.
You can also add a graduate certificate in expressive arts therapies, adventure-based counseling or nature-based counseling. The online degree requires a six-credit internship and a three-credit practicum.
- Our Flexibility Rating: N/A
- Application Fee: N/A
- Notable Major-Specific Courses: Supervised counseling internship
$599/credit
The online master’s in mental health counseling program from Catawba College , based in Salisbury, North Carolina, provides experiential learning and small class sizes. Applicants do not need to submit GRE or GMAT scores.
Offered through the School of Health Sciences and Human Performance, the clinical mental health counseling degree holds CACREP accreditation. The 60-credit program includes 45 credits of classroom work and 15 credits of experiential learning. Students typically complete the degree in two years.
- Notable Major-Specific Courses: Multicultural diversity in counseling

$650/credit
Grace College and Theological Seminary , based in Winona Lake, Indiana, offers an online mental health counseling master’s degree that can prepare you to counsel clients from a Christian perspective. Admission requirements include a minimum 3.0 GPA, a professional reference, a faculty interview and a passing background check.
The CACREP-accredited program offers fully online coursework but requires a seven-day, on-campus residency each year. Students can transfer up to 12 credits toward the clinical mental health degree.
- Program Enrollment Options: Part time, full time
- Notable Major-Specific Courses: Theological foundations in counseling

$725/credit
Malone University in Canton, Ohio, offers a two- to three-year online master’s in mental health counseling with both synchronous and asynchronous course delivery options. The degree holds accreditation from CACREP and is approved by the State of Ohio Counselor, Social Worker, and Marriage and Family Therapist Board.
The curriculum, informed by a Christian perspective, includes coursework, internships and a practicum. The program invites applicants from any undergraduate background with a minimum 3.0 GPA. Applicants must complete a group online interview with program faculty.
- Our Flexibility Rating: Learn on your schedule
- Notable Major-Specific Courses: Counseling lesbian, gay, bisexual, transgender, queer and intersex populations

You can earn an online master’s in mental health counseling from Hodges University , physically located in Fort Myers, Florida. The CACREP-accredited program prepares students to pursue licensure and apply for entry-level mental health and substance abuse counseling positions. Applicants need a bachelor’s degree and a minimum 3.0 GPA to qualify for admission to the program.
The curriculum explores counseling theories and practice, adolescent therapy, and human growth and development. Students must complete a comprehensive exam and an internship component to graduate.
- Application Fee: None
- Notable Major-Specific Courses: Trauma therapy, human sexuality

$1,397/credit
You can earn a combined professional counseling M.A./Ed.S. degree online from the College of Education and Human Services at Seton Hall University , based in South Orange, New Jersey. This 60-credit program consists of 48 credits of counseling coursework plus 12 credits in the Ed.S. program.
Students must complete two on-site residencies. The curriculum includes a practicum, three internships and coursework that explores topics like counselor ethics, multicultural counseling and counseling theory.
- Application Fee: $75
- Notable Major-Specific Courses: Abnormal psychology

$555/credit
Faulkner University , physically located in Montgomery, Alabama, offers a mental health counseling master’s online degree that incorporates a Christian worldview. The program meets the educational requirements for professional counselor licensure in Alabama. Students can complete 85% of the degree online but must visit campus to complete two five-day clinical training sessions.
The program also requires a 600-hour internship and a 100-hour practicum. A background in clinical mental health is not required to qualify for admission to the program. Distance learners must pay an online course fee of $75 per credit and a general fee of $350 per semester.
- Degree Credit Requirements: 61 credits
- Notable Major-Specific Courses: Analysis of the helping relationship, crisis intervention in counseling

$649/credit
The University of the Southwest , based in Hobbs, New Mexico, is a Christian institution focused on the values of free enterprise, self-government, community service and servant leadership. Admissions criteria for the school’s CACREP-accredited online mental health counseling master’s program include a bachelor’s degree from a regionally accredited university and a minimum 3.0 GPA.
The curriculum explores abnormal behavior, addictions counseling and spirituality in counseling. It requires a two-part practicum and two-part internship. Students take synchronous online classes at set times and can finish the degree in two and a half years. Teaching faculty are mental health clinicians.
- Our Flexibility Rating: Learn on a set schedule
- Notable Major-Specific Courses: Clinical supervision of counselors

$342/credit
Lamar University , part of the Texas State University System, offers an online Master of Education in clinical mental health counseling. The whole 60-credit program costs $20,520 in tuition and distance learning fees, and students can graduate in as few as 30 months.
Learners complete two in-person residencies, a practicum and an internship. Graduates qualify to become Licensed Professional Counselors in Texas. Lamar’s clinical mental health counseling program offers multiple start dates each academic year.
- School Type: Public
- Application Fee: $25
- Program Enrollment Options: Full-time
- Notable Major-Specific Courses: Foundations of clinical mental health counseling, abnormal human behavior
- In-Person Requirements: Yes, for residencies, a practicum and an internship
An online master’s in mental health counseling program might be the perfect choice for you, but it depends on several factors. The below considerations can help you decide whether to pursue an online mental health counseling degree .
- What’s your learning style? Can you manage your own time, stay on task and motivate yourself to finish your work? If so, an online program might suit you well. However, not everyone finds it easy to succeed without the structure of attending class in person. These learners might prefer a face-to-face or hybrid program.
- What’s your budget? Distance learning is sometimes more affordable than an on-campus program, in part because online students avoid paying for on-campus housing and transportation. If you plan to enroll in an out-of-state public university, keep in mind that some schools charge a flat or discounted tuition rate to all online learners regardless of where they live, potentially sparing you steep out-of-state tuition rates.
- What’s your schedule? Many students find it easier to fit school into their lives by choosing an online program, especially one with asynchronous classes. Rather than traveling to campus at specific times each week, online students can learn wherever and whenever it makes the most sense for them. This flexibility can make it easier to work full time or meet other personal obligations without putting your education on hold.
Institutional accreditation evaluates the quality of an entire higher education institution. Institutionally accredited universities meet stringent academic standards, demonstrating that they can offer a high-quality education.
Schools can receive institutional accreditation from accrediting bodies recognized by the Council for Higher Education Accreditation (CHEA) or the U.S. Department of Education. Attending an institutionally accredited college is crucial if you want to be eligible for federal financial aid. You can research a school’s accreditation status on CHEA’s website .
Programmatic accreditation evaluates specific programs within an institution. This kind of accreditation can be important for getting a job in your chosen field, applying to graduate school or qualifying for a professional credential.
Many of the best master’s in mental health counseling online programs hold programmatic accreditation from the Council for Accreditation of Counseling and Related Educational Programs (CACREP). You can find out if a mental health counseling program holds programmatic accreditation by searching CACREP’s directory .
Mental health counseling master’s programs can also receive accreditation from the Masters in Psychology and Counseling Accreditation Council. However, CACREP accreditation is more prevalent.
Consider Your Future Goals
An online mental health counseling master’s degree can qualify you to launch a career as a mental health counselor or to pursue other related jobs. But not all programs are the same, so make sure to evaluate each option on its own merits and ensure it can help you reach your goals.
All states require mental health counselors to hold a license, so your degree should meet the education requirements laid out by the state where you intend to practice. More than half of U.S. states require a CACREP-accredited degree to qualify for mental health counseling licensure. Whether or not your state stipulates a specific accreditor, you will need to complete supervised clinical hours and pass an exam to earn your license and qualify for a job after graduation.
If you want to work with a specific client population, like children or adolescents, try to find a program that offers coursework and a field experience with this group. To learn more about this career path, see our guide on how to become a mental health counselor .
Understand Your Expenses and Financing Options
Tuition rates for the online mental health counseling master’s programs ranked on this page range from $342 to $1,039 per credit. The typical program requires about 60 credits, bringing the total tuition cost of the degree between $20,520 and $62,340.
For comparison, the National Center for Education Statistics reports that the average yearly cost for graduate school tuition and fees is $20,513, bringing the total for a two-year degree to around $41,000.
Fill out the Free Application for Federal Student Aid to find out your eligibility for federal student aid such as loans, grants and scholarships. Other popular ways to fund a graduate education include fellowships, assistantships and work-study programs.
What is the difference between an M.A. and an M.S. in counseling?
There isn’t much difference between an M.A. and an M.S. in counseling. Both graduate degrees can prepare you to become a professional mental health counselor. Regardless of whether you choose an M.A. or an M.S., confirm that the program meets licensure requirements in the state where you want to practice mental health counseling after you graduate.
What is the highest degree for a mental health counselor?
You typically need at least a master’s degree to become a licensed mental health counselor in any state. However, some mental health counselors may choose to earn a doctoral degree.
Can you get a master’s in counseling online?
Yes, many accredited schools offer online mental health counseling master’s programs, though some require on-site residencies or clinical training. Usually, online students can complete internships or practicums in their home areas if they do not live near their schools.
Can you be a counselor without a master’s degree?
Typically, you cannot become a counselor without a master’s degree, but it depends on how you define the term. To become a licensed professional counselor, you generally need to earn a master’s degree in mental health counseling or a related field, complete clinical supervision hours and pass an exam. However, some professions with “counselor” in the title are open to individuals with only a bachelor’s or even just a high school diploma. These include substance abuse and behavioral disorder counselors (in some cases) and peer counselors.

Liz Simmons has been writing for various online publications about career development, higher education and college affordability for nearly a decade. Her articles demystify the college application process and help prospective students figure out how to choose a major or career path.
Biochemistry and Molecular Biology
Biostatistics
Environmental Health and Engineering
Epidemiology
Health Policy and Management
Health, Behavior and Society
International Health
Mental Health
Molecular Microbiology and Immunology
Population, Family and Reproductive Health
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
The Challenges and Opportunities of an Aging Society
The new issue of Hopkins Bloomberg Public Health magazine explores how we can ensure that older adults remain as healthy as possible, for as long as possible. It also delves into the proliferation of counterfeit drugs, the repercussions of abortion bans, and the hunger gap facing adolescents.
Read the magazine Dean Mackenzie’s column
The Rise of Colorectal Cancers Among Younger People
Colorectal cancer diagnoses are rising in people under age 50. What’s behind this increase?
Bloomberg American Health Initiative Announces Eighth Cohort of Bloomberg Fellows
The Bloomberg American Health Initiative awards sixty individuals full scholarships to the Bloomberg School to address pressing public health challenges in the U.S.
Johns Hopkins Bloomberg School of Public Health Honors 1,273 New Graduates
Atul Gawande, assistant administrator for global health at USAID, joined Dean Ellen J. MacKenzie and student and faculty speakers at Bloomberg School’s 106 th convocation ceremony.
The Threat to Abortion Rights You Haven’t Heard Of
A century-old “zombie law” could usher in a nationwide abortion ban.
What to Know About COVID FLiRT Variants
A new family of COVID variants are becoming dominant in the U.S. at a crucial time for vaccine decision-making.
A Bold New Goal: Reduce Gun Violence 30% By 2030
The Center for Gun Violence Solutions has a new goal to reduce gun violence 30% by 2030.
Subscribe to Stay Informed
Connect with us, our academic program offerings.
Our programs welcome those from within and outside the traditional boundaries of public health. Whether you're a future college graduate, a midcareer public health leader, or someone looking to make a career change, we have a program for you.
Registration Now Open for the 2024 Summer Institutes
Designed for busy working professionals and students, the Johns Hopkins Bloomberg School of Public Health Summer Institutes allow you to complete credit or non-credit courses in a short period of time. With over 100 courses available, there is sure to be a course for everyone.
LEARN MORE REGISTER

Master of Public Health (MPH)
The Master of Public Health (MPH) is our most flexible degree. With 12 concentrations to choose from, students can tailor their degree to their unique goals while completing classes at their own pace on campus, fully online, or a mix of the two.
We are accepting applications for the online/part-time format starting in November 2024 or January 2025.
Master of Science in Public Health (MSPH)
The Master of Science in Public Health (MSPH) is a professional degree alternative to the Master of Public Health (MPH) degree for students who want more focused skills in a specific field of public health or who lack two years of health-related work experience to begin or advance a career as a public health professional. MSPH programs generally require one academic year of coursework, followed by a field placement. The field placement duration and location vary by department/concentration.

Why Choose the Johns Hopkins Bloomberg School of Public Health?
Ranked by U.S. News & World Report since 1994
and Largest School of Public Health
Courses Offered
Research Centers and Institutes
Alumni Living in over 160 Countries
Degree Programs
Certificate Programs
Student-to-Primary-Faculty Ratio
Our Departments
Meet our faculty.
Our faculty are world-renowned experts, and trusted advisers to our students, public health leaders, and the public.

Tanjala S. Purnell
Tanjala S. Purnell, PhD '12, MPH, uses epidemiology and health services research to advance equity in transplantation and related conditions, including kidney diseases, hypertension, and diabetes.

Barry Zirkin
Barry Zirkin, PhD, is a reproductive biologist involved in studies of the effects of aging and environmental toxicants on testicular testosterone production and spermatogenesis.

Gurumurthy Ramachandran
Gurumurthy Ramachandran, PhD, MS, conducts research focused on developing effective and accurate methods to assess health-related human exposure in occupational and non-occupational settings.

Avonne E. Connor
Avonne E. Connor, PhD, MPH, is a cancer epidemiologist who studies breast cancer and cancer health disparities among women and underserved populations across the cancer continuum.
Join Us in Baltimore
Pursue a degree at the #1 school of public health in one of America's best cities. With 50+ museums, a bustling restaurant scene, gorgeous parks, and more, Baltimore is a great place to study and live.
LEARN ABOUT BALTIMORE
Support Our Work
Our work is made possible in part by contributions from Bloomberg School donors.

IMAGES
VIDEO
COMMENTS
Your health is more important than a PhD degree. Having said that, many universities value the health of their students and employees and have resources in place to further that. These could be counselors, doctors or nurse-practitioners who are specifically tasked with finding ways to make the university work for members with health problems.
Mental health is just as important as anything else. You wouldn't be hard on yourself if you had to take a leave of absence for chemotherapy. I took a roughly 12 month LOA after 4.5 years in my PhD in engineering for mental illness. I then returned for a year and defended and graduated.
Mental Health and Your PhD: Resources and Support. Mental health is a serious issue that impacts students at any level. PhD students face unique stressors and pressure that can impact mental health. Use the resources in this guide to find the support you need. Author: Angela Myers. Editor: PhDs Editing Staff.
A mental health leave of absence is when you take time off work due to a mental health condition. You may need a break to undergo treatment for severe depression or anxiety, or another mental health condition.. If your workplace is covered, the Family and Medical Leave Act (FMLA) allows an unpaid medical or mental health leave of absence of up to 12 weeks.
However, now is a particularly 'bad' time to take leave because my PhD qualifying exams (first attempt) is very soon and in the month following, I have conferences/academic travels planned (which are great opportunities for furthering my career that my advisor has offered to me instead of to other students). ... Therefore, I would prefer that ...
The duration of the leave will depend upon the time you need for treatment and/or recovery, along with the resolution of any academic conditions determined by your graduate program. The Graduate School allows health leave of absence status at increments of 12 months with a possible annual renewal for up to four years total.
More than 40% of PhD students met the criteria for moderate to severe depression or anxiety. In contrast, 32% of working professionals met these criteria for depression, and 26% for anxiety. The ...
The PhD degree is a research-oriented doctoral degree. In the first two years, students take core courses in the Departments of Mental Health, Biostatistics, and Epidemiology, in research ethics, and attend weekly department seminars. Students must complete a written comprehensive exam (in January of their second year), a preliminary exam, two ...
PH.330.660. Grant Writing for the Social and Behavioral Sciences (fourth term) 3. PH.330.611. Writing Publishable Manuscripts for the Social and Behavioral Sciences (second year and beyond only - second term) 2. PH.330.605. Doctoral Seminar in Public Mental Health (2nd year PhD students only) 1.
At that time, 29% of 5,700 respondents listed their mental health as an area of concern — and just under half of those had sought help for anxiety or depression caused by their PhD study. Things ...
7 minute read. After taking two months out of my PhD to reflect, heal and recharge, I have come back with a new focus. A new approach. A much more positive mental attitude. Here is what happened. My purpose for taking on a PhD has maybe not always been the 'right' one. I applied because I was interested in pursuing research on my topic ...
Mental health issues among graduate students. Even before the COVID-19 pandemic, poor mental health was pervasive among graduate students and in academia 2, 3. In a 2019 global survey of 6,320 PhD ...
Organizational policies that are linked to mental health problems will lead individuals to quit their PhD studies or leave the research industry altogether (Podsakoff et al., 2007). Several studies of PhD students suggest that the dropout numbers range from 30 to 50 percent, depending on the scientific discipline and country ( Stubb et al., 2012 ).
Whether it's considering a leave of absence, consulting with mental health professionals, or even shifting your research focus, there are ways to make your PhD journey more bearable. Yes, you read it right—you don't have to face the monumental task of single-handedly revolutionising your field.
An intentional pause in your work life offers a number of benefits that will allow you to dedicate more time and energy to your mental well-being. A leave can: Reduce stress by removing work obligations from the picture. Provide adequate time to rest, recharge, and work with a mental health professional.
Within 2 years, though, it became clear that I was failing to master the skills I needed, and I found the work no more satisfying than during my master's. My mental health deteriorated. I would lie in bed wide awake for hours. There I was, in one of the top 10 most livable cities in the world, and yet I was unhappy.
Ivy L. Bourgeault, PhD, 1 Jelena Atanackovic, PhD, 1 Kim McMillan, RN, PhD, 1 Henrietta Akuamoah-Boateng, PhD, 1 and Sarah Simkin, MD, MSc 1 ... Stigma and concern about the professional impact of taking a mental health leave from work was a close second for all professional respondents except those from Dentistry. Financial barriers to taking ...
The World Health Organisation classifies burnout as a syndrome with symptoms of: - Feelings of energy depletion or exhaustion; - Increased mental distance from one's job, or feelings of negativism or cynicism related to one's job; - Reduced professional efficacy. Symptoms of burnout as classified by the WHO. Source.
While mental health professionals come from diverse backgrounds and disciplines, cThe academic rigor and practical training that clinical psychology Ph.D. programs offer a unique blend of academic rigor and practical training that preparescan adequately prepare graduates for their rewarding careers in mental health care in the field.
Advance in the growing mental health field as an effective counselor educator, clinical supervisor, researcher or clinician. Through theoretical and didactic content, along with practical and experiential activities, you will be instructed intensively in counseling pedagogy, clinical supervision, advanced counseling theory and techniques, quantitative and qualitative research methodology and ...
Health professions are ranked among the most stressful occupations, 1-4 and health professionals experience burnout, 5-7 anxiety, 8-10 depression, 11-13 Post-Traumatic Stress Disorder (PTSD), 14-16 and substance use at rates higher than the general population. 17,18 These challenges are tied, in part, to the organization of work within the healthcare settings: irregular and ...
The purpose of asking for a mental health leave of absence from work should be directly connected to your ability to perform the responsibilities of your gig. Dr. Seide says that while some ...
Dr. Samson Omotosho, PhD, CRNP-PMH, is a Psychiatry specialist practicing in Baltimore, MD with 36 years of experience. This provider currently accepts 2 insurance plans including Medicaid. New patients are welcome.
Lennie Waite, PhD. Certified Mental Performance Consultant and Olympian ... The sport can help runners manage other mental health disorders as well, including post-traumatic stress disorder ...
Use of mental health care increased nationally during the pandemic, as teletherapy made it far easier to see clinicians. Treatment for anxiety disorders increased most steeply, followed by PTSD ...
Having received her PhD in our department in 2021 for her study titled, "Armed Conflict, Intimate Partner Violence and Women's Mental Health: An Explanatory Mixed-Methods Study." She will continue her work with the Connecticut Office of Early Childhood as well as teach a course on Global Health in the Program in Applied Public Health ...
Forbes Maggie McGrath and Huma Abedin discuss new research from mental health service provider ComPsych on how women are driving mental health leaves of absence.May 29, 2024 ...
Mental health counselors evaluate, manage and treat various mental and emotional health issues, including depression and anxiety, relationship problems, addiction and substance use disorders, and ...
Licensure requirements generally include a master's or PhD in psychology. As you pursue a higher education degree, consider these fields as possible specialties. 1. Clinical psychology. Clinical psychologists provide behavioral and mental health care for individuals and families.
Protecting Health, Saving Lives—Millions at a Time. The Master of Science in Public Health (MSPH) is a professional degree alternative to the Master of Public Health (MPH) degree for students who want more focused skills in a specific field of public health or who lack two years of health-related work experience to begin or advance a career as a public health professional.