- Testimonials
- How it works
- Paper Writers Team
- Essay Writing Guide
- Free plagiarism checker
- Essay title generator
- Conclusion Generator
- Citation Generator
- Can ChatGPT Write Essays?
- Types of Essays
- Essay Writing Formats
- Essay Topics
- Best Research Paper Topics
- Essays by Subject
- Breast Cancer Research Paper

A GUIDE TO WRITING A BREAST CANCER RESEARCH PAPER
Table of contents, how to write a breast cancer research paper, your breast cancer research paper thesis, breast cancer outline for research paper, introduction for breast cancer research paper, breast cancer research paper body paragraphs, breast cancer research paper conclusion, breast cancer research paper example and other help.
Breast cancer is a serious public health issue that impacts people from every walk of life. There are very few people who will not have their lives impacted in some way by this disease. Because it is so prevalent, there is much research that has been done and much research that is currently in progress. As a result, breast cancer is a popular topic for students in the medical and healthcare fields. In addition to this, breast cancer is also an appropriate topic for courses in political science, education, even business. This guide will provide you with important advice on writing a research paper on this serious disease.
Once you’ve chosen your topic, and conducted the appropriate research, you’ll need to construct a thesis. This is the statement that you will support in your research paper.
Sample Breast Cancer Research Paper
Writer144311.
Writer144311 has a background in marketing, technology, and business intelligence. S/he enjoys writing about data science, BI, new marketing trends and branding strategies. On TrustMyPaper s/he shares her practical experience through academic writing.
Now that your topic and thesis are in hand, you can begin the process of creating an outline. Think of this as a foundation for your completed paper. It will help you decide on the structure of your paper, and choose the most important points to support your research paper.
Your introduction paragraph should contain the following elements:
- A hook such as an interesting fact about breast cancer
- A few sentences to introduce the specific topic of your paper
- Your thesis
Best breast cancer research paper topics
- The Impact of Pinkwashing on Breast Cancer Research
- The Prevalence of Breast Cancer in Men
- Are Natural Treatments Ever Appropriate for Breast Cancer?
- What is the Role of CBD in Breast Cancer Treatment?
- How to Tell if a Breast Cancer Charity is Legitimate
- Providing Emotional Support to Loved Ones with Breast Cancer
- Breast Cancer in Film and Literature
- New Research in Breast Cancer Immunotherapy
- New Treatment Options for Metastatic Breast Cancer
- Problems with Current Approaches to Breast Cancer Research
- Treatment Options for Patients Who Cannot Receive Chemotherapy
The body paragraphs are the ‘meat’ of your research paper. This is where you will present facts to your readers. Remember to cite your sources , and to rely on data and academic studies to present your case.
Your concluding paragraph should summarize the points made in your research paper. Show the readers how your research comes together to prove your thesis to be correct.
If you need assistance with a research paper on breast cancer, we recommend looking at an example paper. We are happy to provide such a paper to you, or assistance with writing your own research paper on the subject of breast cancer. We have writers, editors, and customer support reps who are available to help you 7 days per week.
External links
- Breast Cancer Research Papers - Academia.edu . (n.d.). Www.Academia.Edu. Retrieved February 19, 2020, from http://www.academia.edu/Documents/in/Breast_Cancer
- Breast Cancer Research Articles . (2019, May 23). National Cancer Institute; Cancer.gov. https://www.cancer.gov/types/breast/research/articles
How ready is your essay?
Don`t have an account?
Password recovery instructions have been sent to your email
Back to Log in
Breast Cancer - Free Essay Examples And Topic Ideas
Breast cancer is a type of cancer that develops from breast tissue. Essays on this topic could explore the causes, diagnosis, treatment, and prevention of breast cancer. Additionally, discussions might delve into the psychological and social impact of breast cancer on patients and their families, the ongoing research towards finding a cure, and the broader societal awareness and support systems available for those affected. We have collected a large number of free essay examples about Breast Cancer you can find at Papersowl. You can use our samples for inspiration to write your own essay, research paper, or just to explore a new topic for yourself.

Micro Needle Thermocouple for Detection of Breast Cancer
Hundreds and thousands of people are affected by cancer each year; it is one of the most fatal diseases and a leading cause of death and disability for humans (Iranifam 2014). There are several types of cancer than can affect different areas of the body, some being less life-threatening than others. A vast amount of patients suffer from late diagnosis or recurrence of their disease in spite of all the advances in diagnosis and treatment of breast cancer. Modern cancer […]
The Role of Histology in the Breast Cancer
Breast cancer is an uncontrolled growth of breast cell that can be benign, not dangerous, but it can also metastasize and invade different and distant tissues in our body. Breast Cancer is the most common cancer in female of any age and although the risk increases, as you get older, many different factors affect the chance of a woman to get breast cancer. I chose this specific topic because breast cancer is something that I’ve dealt with in my personal […]
Corporate Social Responsibility against Cancer
Abstract As an assistant manager at Kenta Law Firm, based in Monroe, I intend to collaborate with the Susan B. Komen Foundation a non-organization corporation that is interested in reducing issues of breast cancer among women. Kenta law firm has noted that a significant populace of Monroe’s youth especially women and young children specifically those who are homeless are suffering from breast cancer. In this CSR partnership, our law firm will collaborate with the Susan B. Komen Foundation in addressing […]
We will write an essay sample crafted to your needs.
Why is Screening for Breast Cancer Important
The impact this disease has, on not only the individual but the people around them, is powerful. Even though the tests show cancer, I am thankful that I had the annual test. It is true that stress, anxiety, and money can be saved by waiting until the age of 50 years old because of misinterpretation and overdiagnosis. However, early detection is the key to success in the battle against breast cancer. There are many different options for detection scans that […]
Breast Cancer: Casuses and Treatment
Cancer is defined as “when the body’s cells begin to divide without stopping and spread into surrounding tissues.” (“What is cancer?”, 2017), caused by mutations that lead to the cell cycle to proceed, regardless if the cell is qualified to. The mutations block the use of the G1, G2, and M checkpoints in the cell cycle. These checkpoints are important in “sensing defects that occur during essential processes, and induce a cell cycle arrest in response until the defects are […]
Breast Reconstruction after Mastectomy
Breast cancer is always personal. As a physician who counsels women at different steps during the healing process, I am acutely aware of this undeniable fact. Every decision she makes from the point at which she is diagnosed with breast cancer will require her focused engagement and a physician who is central to understanding her need for clarity of options. It is an intimate relationship where trust is a requirement and every woman faced with the many unknowns ahead will […]
Breast Cancer History Research Paper
Breast cancer is a disease in which most commonly occurs in all women no matter their size, shape, race, or ethnicity. About one in eight women will be diagnosed with breast cancer every year, a fatal disease if not discovered early. Early detection of breast cancer is key so that cancerous cells found in the breast do not spread through other parts of the body. With an increasing prevalence in breast cancer today, the evolution of technology has been improved […]
New Healthcare Inventions on Breast Cancer
Abstract Background: The Ki67 labeling index (LI) for breast carcinoma is essential for therapy. It is determined by visual assessment under a microscope which is subjective, thus has limitations due to inter-observer variability. A standardized method for evaluating Ki67 LI is necessary to reduce subjectivity and improve precision. Therefore, automated Digital Image Analysis (DIA) has been attempted as a potential method for evaluating the Ki67 index. Materials and Method: We included 48 cases of invasive breast carcinoma in this study. […]
Understanding Breast Cancer
This paper will clarify what Breast Cancer is. It will explain the symptoms, treatment options, and other useful information regarding this disease. The first thing to know about Breast Cancer is understanding what it is. According to the Cancer.org website, breast cancer begins when cells in the bosom begin to spread out of control. The tumor that is formed from these cells may be detected on an x-ray or can be felt as a lump. Malignancy can advance into neighboring […]
Breast Cancer in African American Women
Summary Despite the fact that Caucasian women in the United States have a higher incidence rate of breast cancer than any other racial group, African-Americans succumb notably worse to the disease and record the highest mortality rate. To comprehend the barriers and challenges that predispose African-American women to these disparities, this research was conducted to get a better understanding from the perspective of oncologists. With diverse ethnicity and gender representation, the participation of seven medical, surgical and radiation oncologists that […]
Essential Breast Cancer Screening Techniques and their Complements
It is with great distress that each year a large number of females suffer and die from breast cancer. Medicine practitioners and researchers have been striving to save lives from breast cancer, and how they manage to do this includes two major parts—diagnosis and treatment. What comes first on the stage of diagnosis is the detection of tumor. Thus, the development of breast imaging techniques is at the highest priority for diagnosing breast cancer, and individuals’ focus is on earlier […]
Breast Cancer Prevention and Treatment
The human body is made up of cells. When a cell dies the body automatically replaces it with a new healthy cell, but sometimes the cell is not healthy and grows out of control. These cells group together and form a lump that can be seen on an x-ray. Breast cancer is a tumor in the cells of person’s breast. It can spread throughout the breast to the person’s lymph nodes and other parts of the body. Sometimes it occurs […]
Breast Cancer Diagnosis
I. Executive Summary Breast cancer is concerning a large number of female individuals worldwide. This disease comes from abnormally developed breast tissue, which usually begins in either lobules or ducts of the breast. Generally speaking, breast cancer is divided into two types—non-invasive and invasive. The core criteria to distinguish in between these two types of breast cancers is the location of cancer cells. Cancer cells remain on their initial positions for a non-invasive breast cancer, whereas they grow, or “invade”, […]
Understanding a Breast Cancer Diagnosis
Breast cancer is often known as an aggressive cancer. It forms when cells grow uncontrollably in the tissues of the breast, leading to a tumor. Over 190,000 individuals are diagnosed yearly (Cancer Center). Breast cancer is the second leading cause of death, and the rate increases every year in women, and occasionally in men. Over 12 percent of women in the United States of America will face breast cancer in their lifetime. It is the most common cause of death […]
Breast Cancer in the Era of Precision Medicine
Introduction: Precision medicine is concerned with the diagnosis of patients according to their biological, genetic, and molecular status. As cancer is a genetic disease, its treatment comes among the first medical disciplines as an application of precision medicine. Breast cancer is a highly complex, heterogeneous, and multifactorial disease; it is also one of the most common diseases among women in the world. Usually, there are no clear symptoms, so regular screening is important for early detection. Scientists recently started using […]
Exome Sequencing to Identify Rare Mutations Associated with Breast Cancer Susceptibility
Abstract Background - Breast cancer predisposition has been known to be caused by hereditary factors. New techniques particularly exome sequencing have allowed/ helped us to identify new and novel variants that exhibit a phenotype. Method - In this review we discuss the advantages of exome sequencing and how it could help in understanding the familial breast cancer. In particular, we will discuss about the studies by Noh et al.(1), Thompson et al.(2), and Kiiski et al.(3), on how they have […]
A Novel Therapeutic Strategy for HER2 Breast Cancer by Nanoparticles Combined with Macrophages
Abstract:In recent years, the cell membrane bionic nanoparticles as a new drug delivery system is widely used in small molecule drugs, vaccines and targeted delivery of macromolecular drugs, because of its inherited the specific receptors on the cell membrane and membrane proteins can be used to implement specific targeted delivery, and the tumor showed a good treatment effect on the disease such as model, this topic with a huge bite cell membrane of the role of tumor capture, chemical modification, […]
Essays About Breast Cancer Breast Cancer is one of the most common cancers in women and is a disease by which the cells in the breast area grow out of control. Breast cancer tends to begin in the ducts or lobules of a breast and there are different types of cancer. In the US alone 1 in 8 women will develop breast cancer at some stage in their lives. In many academic fields; from science to medicine the study of breast cancer and essays about breast cancer are required as part of the curriculum. An essay on breast cancer can seem daunting due to the amount of research and several varying scientific approaches used to talk about the topic. We offer essay examples, or research paper guidance and free essay samples. These can be used to gauge how to approach the topic and are an informative look at all factors that contribute to breast cancer and prevention. We also factor breast cancer awareness into our essay samples and ensure essays for both university and college build a strong foundation to understanding the disease, but also draw criticism when necessary and a strong conclusion on whatever element of breast cancer the focus of the essay is on.
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers
IMPACT OF THE BREAST CANCER IMMUNE MICROENVIRONMENT ON RACIAL DISPARITIES AND RECURRENCE
Add to collection, downloadable content.
- Affiliation: School of Medicine, Department of Pathology and Laboratory Medicine
- Growing evidence supports the importance of the immune microenvironment in the clinical course of breast cancer, where multiple studies have demonstrated positive prognostic utility of tumor infiltrating lymphocytes among triple-negative and HER2-positive breast cancers. Despite the abundance of studies investigating the immune microenvironment in breast cancer, biomarkers of immune response are lacking, particularly in estrogen receptor (ER)-positive breast cancer, and Black women are underrepresented in these studies. This is important because Black women suffer higher incidence of poor-prognosis subtypes and worse stage-specific mortality. Given the rapidly evolving landscape of immunotherapies in breast cancer and ongoing efforts to expand currently limited treatment eligibility, investigations of the breast cancer immune microenvironment and identification of biomarkers that associate with immune-mediated survival in diverse patient populations, is an unmet clinical need. To address this knowledge gap, the current body of work leveraged three major breast cancer studies rich in molecular, histological, clinical and epidemiological data: 1) the Carolina Breast Cancer Study (CBCS; N= 1,952), a large population-based study designed to investigate racial disparities in breast cancer, 2) The Cancer Genome Atlas (TCGA) breast cancer dataset (N= 1,095), a well-known study with multiple data platforms for each sample, and 3) the Molecular Taxonomy of Breast Cancer International Consortium (METABRIC) dataset (N= 1,904). Aim 1 of this study characterized global phenotypes of immune response using cell-type specific markers for 10 immune cell populations and evaluated associations with clinical and demographic variables, and recurrence. Aim 2 leveraged RNA expression profiling to investigate markers of genomic instability in association with breast cancer immunogenicity and immune-mediated patterns of recurrence. This work identified strong associations between phenotypes of immune response and tumor subtype, grade, patient age, BMI and self-reported race. In addition, RNA-based pathway assessment of genomic instability markers (HRD, APOBEC, and TP53 pathways) identified immunogenic tumors with strong adaptive immune responses that associated with recurrence-free survival regardless of ER status. Collectively, this work contributes novel findings about the breast cancer immune microenvironment that may aid in precision medicine approaches for breast cancer prevention and intervention, and highlights the importance of diversity in impactful and equitable clinical research.
- breast cancer
- immune microenvironment
- Epidemiology
- disparities
- genomic instability
- https://doi.org/10.17615/t7kp-1598
- Dissertation
- In Copyright - Educational Use Permitted
- Calhoun, Benjamin C
- Hoadley, Katherine A
- Troester, Melissa A
- Love, Michael I
- Williams, Scott E
- Doctor of Philosophy
- University of North Carolina at Chapel Hill Graduate School
This work has no parents.
Select type of work
Master's papers.
Deposit your masters paper, project or other capstone work. Theses will be sent to the CDR automatically via ProQuest and do not need to be deposited.
Scholarly Articles and Book Chapters
Deposit a peer-reviewed article or book chapter. If you would like to deposit a poster, presentation, conference paper or white paper, use the “Scholarly Works” deposit form.
Undergraduate Honors Theses
Deposit your senior honors thesis.
Scholarly Journal, Newsletter or Book
Deposit a complete issue of a scholarly journal, newsletter or book. If you would like to deposit an article or book chapter, use the “Scholarly Articles and Book Chapters” deposit option.
Deposit your dataset. Datasets may be associated with an article or deposited separately.
Deposit your 3D objects, audio, images or video.
Poster, Presentation, Protocol or Paper
Deposit scholarly works such as posters, presentations, research protocols, conference papers or white papers. If you would like to deposit a peer-reviewed article or book chapter, use the “Scholarly Articles and Book Chapters” deposit option.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 18 May 2024
Disparities in quality of life among patients with breast cancer based on surgical methods: a cross-sectional prospective study
- Yi Wang 1 ,
- Yibo He 1 ,
- Shiyan Wu 1 &
- Shangnao Xie 1
Scientific Reports volume 14 , Article number: 11364 ( 2024 ) Cite this article
112 Accesses
Metrics details
- Breast cancer
- Quality of life
To determine the impact of breast conservation on quality of life and identify treatment-related and other demographic factors associated with post-breast cancer treatment quality of life. A prospective study was conducted on 392 women who underwent breast cancer surgery at Hangzhou Cancer Hospital from January 1, 2013, to December 31, 2022. Operable breast cancer patients who had completed all treatments except endocrine therapy were included. Patients with tumor recurrence/metastasis, bilateral or male breast cancer, and other primary malignancies were excluded. After enrollment, patients were asked to complete the BREAST-Q scale, and their pathological and medical records were reviewed. Analysis of variance was used to compare the quality of life scores among the groups. Univariate and multivariate linear regression analyses were performed to identify independent factors associated with quality of life scores in different domains. Participants completed the BREAST-Q scale at a median of 4.6 years after surgery. Quality of life scores varied based on the therapeutic strategy. Breast conservation has significant advantages over mastectomy in terms of breast satisfaction, psychosocial, and sexual well-being. Compared to oncoplastic breast-conserving surgery, mastectomy was independently associated with decreased breast satisfaction, psychosocial, and sexual well-being, while conventional breast-conserving surgery showed comparable outcomes to oncoplastic breast-conserving surgery in terms of these factors. Breast conservation leads to an improvement in quality of life compared to mastectomy. Oncoplastic breast-conserving surgery does not lead to a decrease in quality of life compared to conventional breast-conserving surgery and offers better outcomes compared to mastectomy.
Similar content being viewed by others

Acute health-related quality of life outcomes and systemic inflammatory markers following contemporary breast cancer surgery

Health-related quality of life and its influencing factors in patients with breast cancer based on the scale QLICP-BR
Primary breast cancer and health related quality of life in Spanish women: The EpiGEICAM case-control study
Introduction.
Breast cancer is a prevalent global malignancy 1 , and breast-conserving surgery (BCS) with adjuvant radiotherapy (RT) is a well-established treatment for early-stage breast cancer 2 , 3 . However, up to 30% of BCS recipients express dissatisfaction with their postoperative appearance, necessitating corrective interventions 4 . In the 1980s, European surgeons introduced "oncoplastic breast-conserving surgery" (OBCS), which incorporates plastic surgery techniques for post-BCS breast defect reconstruction 5 .
While OBCS offers satisfactory long-term oncological results and broadens treatment possibilities for patients who would typically undergo mastectomies 6 , it involves more extensive incisions, additional tissue manipulation, and potential flap reconstruction in comparison to conventional breast-conserving surgery (cBCS) 7 , 8 . The procedures involved in OBCS are more complex, time-consuming, and costly. Given these complexities, is it still worthwhile to pursue breast conservation by OBCS? Some researchers have proposed whether the use of OBCS should be reduced 9 .
Understanding the impact on the quality of life of breast cancer survivors is crucial given its significant influence on medical decision-making 10 , 11 . Despite the widespread utilization of OBCS to conserve the breast and enhance its aesthetics, research on its impact on quality of life is limited and complicated due to the variability of surgical approaches. Consequently, this study aimed to assess the effect of breast conservation by OBCS on the quality of life of patients with operable breast cancer treated at Hangzhou Cancer Hospital from January 1, 2013, to December 31, 2022, and to elucidate the treatment and demographic factors associated with postoperative quality of life.
Materials and methods
This prospective, cross-sectional, case–control study was conducted at a single center. The inclusion criteria were operable breast cancer patients treated at Hangzhou Cancer Hospital between January 1, 2013, and December 31, 2022, who had completed all treatments except endocrine therapy and provided participation consent. The exclusion criteria were patients with tumor recurrence/metastasis, bilateral or male breast cancer, or other primary malignancies. Participants were categorized into two groups: BCS group (cBCS with RT subgroup and OBCS with RT subgroup), and unilateral MAST group (MAST with RT subgroup and MAST without RT subgroup). This study utilized the BREAST-Q scale 12 , which includes separate modules for BCS and MAST without reconstruction. The BCS module was used for the OBCS with RT subgroup because OBCS in this study predominantly referred to oncoplastic lumpectomy/glandular remodeling. BREAST-Q assesses six distinct domains: satisfaction with breasts, psychosocial well-being, physical well-being, sexual well-being, satisfaction with overall outcome, and satisfaction with care. Due to the elapsed time between surgery and questionnaire completion in this study, the domains of satisfaction with the overall outcome and satisfaction with care were excluded. Each domain was scored on a scale from 0 to 100, with higher scores indicating an enhanced quality of life. Differences in BREAST-Q scores were categorized as small (2–3 points), moderate (4–7 points), and large (8–10 points) 13 . Patient characteristics, collected using the questionnaire, included employment status, educational level, marital status, and economic status. Patients’ medical and pathological records were reviewed to determine the disease tumor, node, and metastasis (TNM) staging 14 , erythroblastic oncogene B (ERBB2; formerly HER2/neu or HER2) status, hormone receptor status, and body mass index (BMI). Information on surgery, chemotherapy (yes/no), RT, and endocrine therapy (yes/no) was obtained using a questionnaire in conjunction with medical records. The lymphedema status (yes/no) was assessed using the questionnaire's question regarding arm swelling. This study was approved by the Ethics Committee of Hangzhou Cancer Hospital, and all participants provided written informed consent. The study was performed in accordance with the Declaration of Helsinki and followed the guidelines of the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) reporting guidelines.
Statistical analysis
The experimental data were statistically analyzed using SPSS (version 29.0) software, and categorical covariates were expressed as numbers (percentages). Analysis of variance (ANOVA) was used to compare quality of life scores among the different groups. Univariate and multivariate linear regression analyses were used to determine the independent factors associated with the quality of life scores in each domain. Variables with two-tailed P ≤ 0.15 in the univariate analysis were included in the multivariate analysis model using a stepwise method to establish the final multivariate model. Differences with P < 0.05 were considered statistically significant.
Ethics approval and consent to participate
This study was reviewed and approved by the ethics committee of Hangzhou Cancer Hospital (approval number: [hzch-2023] HS no.007). Written informed consent was obtained from every patient.
Patient enrollment
After screening, 623 eligible patients were invited, 456 provided written informed consent and completed the survey, but three were found to not meet the inclusion criteria after enrollment. After excluding 61 participants who only completed a brief questionnaire, a total of 392 patients’ data were included in the statistical analysis.
Patient, disease, and treatment characteristics
The interval between surgery and scale completion averaged 4.6 years (range: 0.33 to 9.83 years). Patient characteristics are detailed in Table 1 . Majority were married, employed, had moderate economic status (income ¥30,000–200,000 per year), and high school or higher education. At surgery, 324 (82.7%) patients had a body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) within the normal range (18.5 to 23.9 kg/m 2 ), and 56 (14.3%) patients had a BMI of 24 kg/m 2 or above. Among the patients, 39 (9.9%) had stage 0 breast cancer, 154 (39.3%) had stage I breast cancer, 158 (40.3%) had stage II breast cancer, and 41 (10.5%) had stage III breast cancer. The lesions on imaging before surgery of 253 (64.5%) patients measured two centimeters or less, 134 (34.2%) two to five centimeters, and 5 (1.3%) more than five centimeters. Chemotherapy was administered to 293 (74.7%) patients, with 121(30.9%) receiving neoadjuvant chemotherapy, and 273 (69.6%) patients received hormone therapy.
Treatment details including surgery, RT, and lymphedema are presented in Table 1 . Among the patients, 88 (22.4%) underwent OBCS, 51 (13.0%) underwent cBCS, and 253 (64.5%) underwent unilateral MAST, among which 100 (25.5%) patients who underwent unilateral MAST received postoperative RT. All patients underwent axillary surgery, with 255 (65.1%) patients undergoing sentinel lymph node biopsy only and 137 (34.9%) patients undergoing axillary lymph node dissection. 61 (15.6%) patients reported having lymphedema.
BREAST-Q results by breast surgery strategy
Figure 1 illustrates unadjusted mean BREAST-Q scores by breast surgery strategy. Satisfaction with breasts, psychosocial well-being and sexual well-being were significantly different among the groups ( P < 0.001). BCS group showed higher scores in satisfaction with breasts (61.70), psychosocial well-being (76.01), physical well-being (83.52) and sexual well-being (55.06), while the scores for MAST group is lower (satisfaction with breasts: 57.30, psychosocial well-being: 70.83, physical well-being: 82.40 and sexual well-being: 49.21).
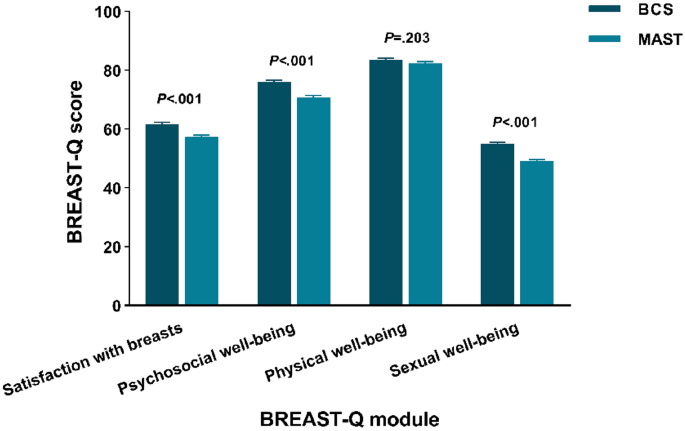
Unadjusted BREAST-Q mean scores by breast surgery strategy. BCS: breast-conserving surgery; MAST: mastectomy.
Satisfaction with breasts
Higher scores in satisfaction with breasts correlated independently with age ≥ 60 (β = 4.662; 95% CI = 2.345 to 6.979; P < 0.001) and patient-reported income ≥ 200,000 (β = 5.068; 95% CI = 2.781 to 7.356; P < 0.001). Lower scores were associated with BMI ≥ 24 (β = − 2.528; 95% CI = − 4.977 to − 0.079; P = 0.043), axillary dissection (β = − 4.875; 95% CI = − 6.704 to − 3.046; P < 0.001) and MAST (β = − 3.927; 95% CI = − 5.741 to − 2.113; P < 0.001) (Fig. 2 A). Patient-reported income < 30,000 and lymphedema showed significance only in univariate analysis. Other factors exhibited no significant association.
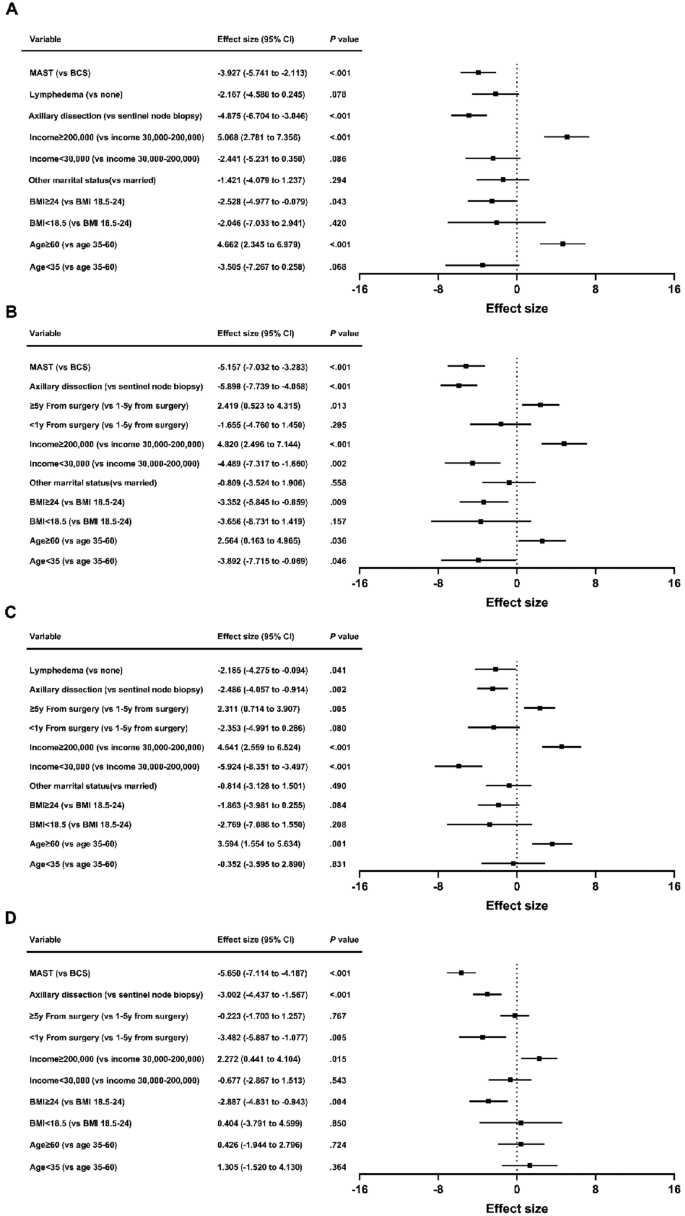
Patient and treatment factors associated with breast satisfaction ( A ), psychosocial well-being ( B ), physical well-being ( C ) and sexual well-being ( D ) scores by breast surgery strategy. MAST: mastectomy; BCS: breast-conserving surgery; BMI: body mass index; CI: confidence interval.
Psychosocial well-being
Better psychosocial well-being correlated with age ≥ 60 (β = 2.564; 95% CI = 0.163 to 4.965; P = 0.036), patient-reported income ≥ 200,000 (β = 4.820; 95% CI = 2.496 to 7.144; P < 0.001), and ≥ 5y from surgery (β = 2.419; 95% CI = 0.523 to 4.315; P = 0.013). Poor psychosocial well-being was linked to age < 35 (β = − 3.892; 95% CI = − 7.715 to − 0.069; P = 0.046), BMI ≥ 24 (β = − 3.352; 95% CI = − 5.845 to − 0.859; P = 0.009), patient-reported income < 30,000 (β = − 4.489; 95% CI = − 7.317 to − 1.660; P = 0.002), axillary dissection (β = − 5.898; 95% CI = − 7.739 to − 4.058; P < 0.001) and MAST (β = − 5.157; 95% CI = − 7.032 to − 3.283; P < 0.001) (Fig. 2 B). Chemotherapy was only significant in univariate analysis. Other variables showed no significant association.
Physical well-being
Factors associated with better physical well-being were age ≥ 60 (β = 3.594; 95% CI = 1.554 to 5.634; P = 0.001), patient-reported income ≥ 200,000 (β = 4.541; 95% CI = 2.559 to 6.524; P < 0.001), and ≥ 5y from surgery (β = 2.311; 95% CI = 0.714 to 3.907; P = 0.005). Conversely, patient-reported income < 30,000 (β = − 5.924; 95% CI = − 8.351 to − 3.497; P < 0.001), axillary dissection (β = − 2.486; 95% CI = − 4.057 to − 0.914; P = 0.002) and lymphedema (β = − 2.185; 95% CI = − 4.275 to − 0.094; P = 0.041) were associated with poorer physical well-being (Fig. 2 C). < 1y from surgery was only significant in univariate analysis. Other factors lacked significant association.
Sexual well-being
Multivariate analysis indicated lower sexual well-being scores with BMI ≥ 24 (β = − 2.887; 95% CI = − 4.831 to − 0.943; P = 0.004), < 1y from surgery (β = − 3.482; 95% CI = − 5.887 to − 1.077; P = 0.005), axillary dissection (β = − 3.002; 95% CI = − 4.437 to − 1.567; P < 0.001), and MAST (β = − 5.650; 95% CI = − 7.114 to − 4.187; P < 0.001). Patient-reported income ≥ 200,000 (β = 2.272; 95% CI = 0.441 to 4.104; P = 0.015) correlated with elevated sexual well-being (Fig. 2 D). Lymphedema was significant in univariate analysis. Other variables exhibited no significant correlation.
BREAST-Q results by local therapy strategy
To assess if there were enhancements in quality of life among women who underwent OBCS, we performed similar analyses among the subgroups. Figure 3 illustrates unadjusted mean BREAST-Q scores by local therapy strategy. All four domains were significantly different ( P < 0.05). OBCS with RT group showed highest scores in satisfaction with breasts (61.99), psychosocial well-being (76.27) and sexual well-being (55.53). cBCS with RT group yielded the highest physical well-being score (84.10). The lowest domain scores were in MAST with RT group (satisfaction with breasts: 53.11, psychosocial well-being: 65.49, physical well-being: 79.89 and sexual well-being: 46.24).
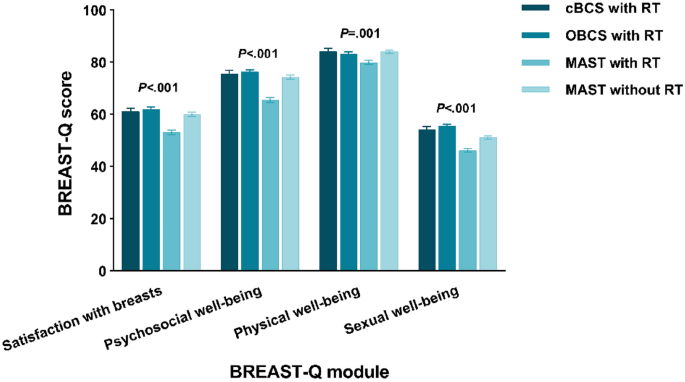
Unadjusted BREAST-Q mean scores by local therapy strategy. RT: radiotherapy; cBCS: conventional breast-conserving surgery; OBCS: oncoplastic breast-conserving surgery; MAST: mastectomy.
Multivariate analysis indicated that MAST with RT was associated with poor breast satisfaction (β = − 8.381; 95% CI = − 10.858 to − 5.905; P < 0.001), psychosocial well-being (β = − 11.491; 95% CI = − 14.039 to − 8.943; P < 0.001), physical well-being (β = − 3.607; 95% CI = − 5.782 to − 1.432; P = 0.001) and sexual well-being (β = − 9.493; 95% CI = − 11.454 to − 7.533; P < 0.001). MAST without RT was associated with decreased breast satisfaction (β = − 2.536; 95% CI = − 4.817 to − 0.255; P = 0.029), psychosocial well-being (β = − 3.171; 95% CI = − 5.487 to − 0.855; P = 0.007) and sexual well-being (β = − 4.739; 95% CI = − 6.530 to − 2.947; P < 0.001). cBCS with RT was not associated with BREAST-Q scores on univariate or multivariate analysis. The statistically significant factors correlated with BREAST-Q scores were mostly consistent with the outcomes of the breast surgery models (Fig. 4 ).
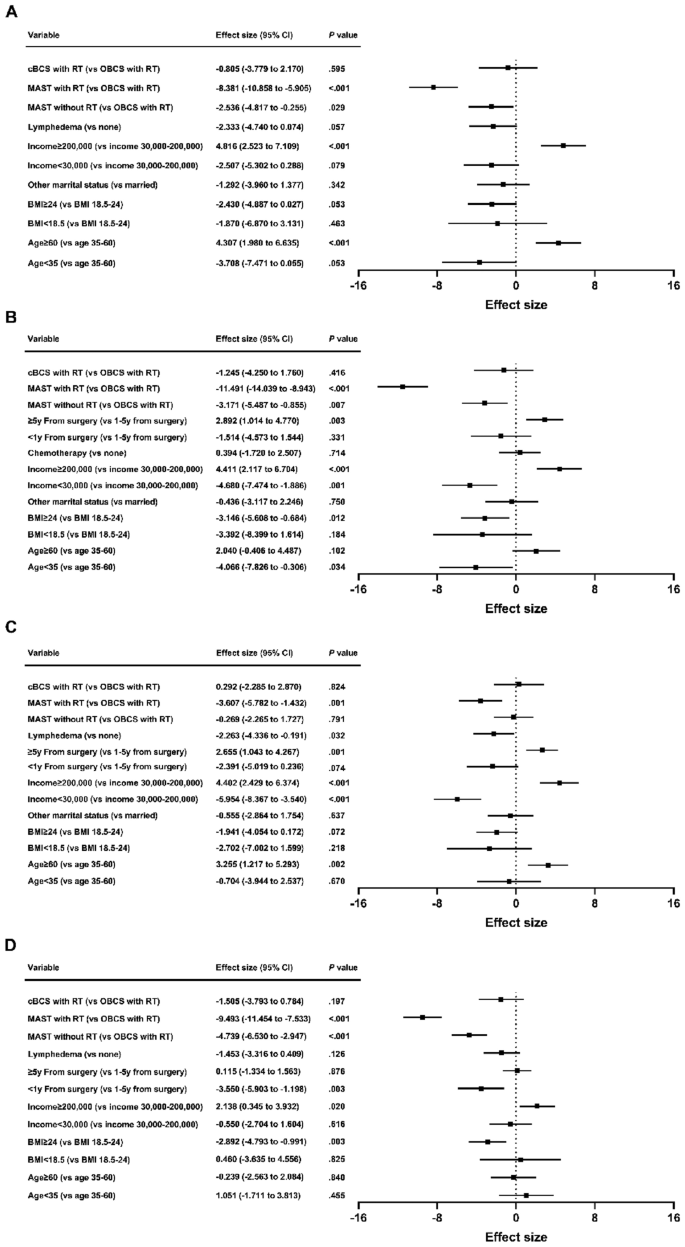
Patient and treatment factors associated with breast satisfaction ( A ), psychosocial well-being ( B ), physical well-being ( C ) and sexual well-being ( D ) scores by local therapy strategy. cBCS: conventional breast-conserving surgery; OBCS: oncoplastic breast-conserving surgery; MAST: mastectomy; RT: radiotherapy; BMI: body mass index; CI: confidence interval.
The rates of BCS and breast reconstruction after mastectomy are significantly lower in China than in Western countries 15 . One contributing factor is that Chinese women typically have smaller breast sizes than women in Western countries, while presenting with larger breast tumor volumes at the time of initial diagnosis, making BCS challenging. Additionally, some Chinese patients adhere to outdated beliefs and have concerns about potential impacts on treatment outcomes or cancer recurrence associated with BCS. OBCS provides acceptable long-term oncological outcomes and has extended treatment options for patients who would traditionally be candidates for mastectomies 6 . In recent years, there has been a clear change in the emphasis of surgical oncology in China, with a growing emphasis on utilizing modern oncoplastic surgical techniques to perform more breast conserving surgeries. Given the increasing prevalence of OBCS, it is essential to examine its impact on quality of life.
In this single-center prospective study, discernible disparities in quality of life surfaced among patients with breast cancer undergoing various local treatment strategies within ten years of surgery. Patients opting for more extensive surgery, particularly when combined with RT, experienced diminished quality of life; satisfaction with breasts; and psychosocial, physical, and sexual well-being. This aligns with findings from prior studies. Engel et al.’s study 16 has shown that patients undergoing BCS reports a higher quality of life compared to those opting for mastectomy. This improvement is often linked to the conservation of the breast and the associated psychological advantages. BCS enables breast conservation, leading to enhanced body image and self-esteem. Patients undergoing BCS may experience less psychological distress and enjoy better psychosocial well-being due to breast conservation. Additionally, BCS has a lesser impact on sexual well-being in comparison to mastectomy, as it retains natural breast tissue.
This study’s findings concur with those of Otsuka et al.’s study 17 in that oncoplastic surgery improved satisfaction with breasts. However, in Otsuka et al.’s study, the quality of life score was not elevated by OBCS (major breast surgery: 154.5 ± 24.6; minor breast surgery: 159.0 ± 20.8; OBCS: 158.7 ± 14.0). Although differences exist between major breast surgery and OBCS, the difference is not pronounced. In the present study, psychosocial and sexual well-being scores were elevated compared to MAST. Additionally, patients who underwent OBCS had better physical well-being scores than those who underwent MAST with RT and equal physical well-being scores than those who underwent MAST without RT. This may be attributable to the omission of RT, reduced chemotherapy and lymphedema in the MAST without RT group. Previous studies 18 , 19 have highlighted RT, chemotherapy, and lymphedema as adverse determinants of quality of life.
Rose et al. 20 suggested that patients who underwent OBCS showed significant improvement in the “psychosocial well-being” module compared to cBCS, while no significant differences were observed between the two groups in the “physical health,” “breast satisfaction,” and “sexual health” modules. Furthermore, a meta-analysis 21 indicated improved quality of life with OBCS compared with cBCS in patients with early-stage breast cancer, with better physical and psychological well-being, higher self-esteem, and a more stable body image, leading to improved social and emotional functioning. However, the clinical studies included in the meta-analysis were predominantly small- sample studies from single centers, and the surgical approaches varied. This study identified no significant differences in any of the quality of life modules between the patients who underwent OBCS and those who underwent cBCS, which is consistent with the findings of de Oliveira-Junior et al 22 . This may be because the present study’s follow-up time was longer, and several aspects of OBCS will decline over time 23 . In our study, the tumor lesion on imaging before surgery averaged 2.11 ± 0.67 cm in OBCS subgroup, and 1.62 ± 0.52 cm in cBCS subgroup. Smaller lesions are more likely to undergo cBCS, resulting in comparable cosmetic outcomes between the two surgical groups. Moreover, the limited number of BCS patients in our study is a significant factor that limits the ability to detect differences in quality of life between OBCS and cBCS subgroups.
In addition to the type of surgery, other clinical factors such as BMI (≥ 24), income (< 30,000), < 1y from surgery, axillary dissection, and lymphedema were negatively correlated with quality of life. Identifying these risk factors can facilitate early postoperative intervention and ultimately improve the postoperative quality of life of patients with breast cancer. Age (≥ 60) and ≥ 5y from surgery were associated with enhanced quality of life. Breast cancer patients can experience significant effects from the disease itself and the ongoing adjuvant therapies, both after diagnosis and during the treatment process 24 . These are all factors that lead to decreased quality of life within 5 years, especially within 1 year, rather than ≥ 5y after surgery. Moreover, good economic status was associated with better satisfaction with breasts, and psychosocial, physical, and sexual well-being. Patients with improved financial circumstances can access higher-quality healthcare services, opt for more expensive treatment options that may improve aesthetic outcomes. The financial advantage also affords patients more opportunities for supportive care, counseling, and resources to manage the challenges of breast cancer treatment and recovery, resulting in a decrease in stress, anxiety, and depression. These enhancements can have a positive impact on patients’ self-perception, confidence, and overall satisfaction with their breast appearance, all of which are closely connected to sexual health and intimacy. Notably, other studies 25 , 26 found an association between economic status and quality of life.
This study has some limitations. It was a cross-sectional, single-time, survey-based prospective study; therefore, the baseline quality of life of patients before surgery was not recorded, which may have influenced their choice of surgical approach and postoperative quality of life. Additionally, this study did not identify patients who chose MAST due to refusal of BCS; patients who selected MAST based on personal preferences may have different quality-of-life scores. Furthermore, this study did not include patients with postmastectomy breast reconstructions, which may improve quality of life of postmastectomy patients. Finally, given that this was a single-center small-sample study, studies with larger sample sizes are required to further confirm the findings of this study. Nevertheless, patient-reported questionnaires can provide basic information on quality of life and assist in identifying potential areas requiring intervention during the patient’s survival period.
OBCS is an acceptable option for patients with larger tumors who are not suitable for cBCS because it allows them to conserve their breasts 6 . This study demonstrated that patients who had their breast conserved reported a higher quality of life compared to mastectomy patients. Despite extensive incisions, additional tissue manipulation, and potential flap reconstruction, patients who underwent OBCS did not report a lower quality of life than those who underwent cBCS. Furthermore, they experienced significantly enhanced quality of life compared with patients who underwent MAST, particularly in the domains of satisfaction with breasts, psychosocial well-being, and sexual well-being. Quality of life data should be incorporated into decision support tools to assist patients with breast cancer in selecting the surgical approach, and discussions with patients should include information regarding quality of life to ensure that they understand the long-term impacts of different surgical approaches. This is particularly crucial because most patients with breast cancer have an extended postoperative survival period. Our data can support further improvements in Chinese breast surgical care for better survival and quality of life.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to Chinese law but are available from the corresponding author on reasonable request.
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71 (3), 209–249 (2021).
Article PubMed Google Scholar
Fisher, B. et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N. Engl. J. Med. 347 (16), 1233–1241 (2002).
Veronesi, U. et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N. Engl. J. Med. 347 (16), 1227–1232 (2002).
Clough, K. B., Cuminet, J., Fitoussi, A., Nos, C. & Mosseri, V. Cosmetic sequelae after conservative treatment for breast cancer: Classification and results of surgical correction. Ann. Plast. Surg. 41 (5), 471–481 (1998).
Article CAS PubMed Google Scholar
Audretsch, W. et al. Oncoplatic surgery in breast conserving therapy and flap supported operability. In Proceedings of the Annual Symposium on Breast Surgery and Body Contouring. Santa Fe, New Mexico (1993).
Calabrese, C. et al. Oncoplastic conservative surgery for breast cancer: Long-term outcomes of our first ten years experience. Eur. Rev. Med. Pharmacol. Sci. 22 (21), 7333–7342 (2018).
CAS PubMed Google Scholar
Mohamedahmed, A. Y. Y. et al. Comparison of surgical and oncological outcomes between oncoplastic breast-conserving surgery versus conventional breast-conserving surgery for treatment of breast cancer: A systematic review and meta-analysis of 31 studies. Surg. Oncol. 42 , 101779 (2022).
Knowles, S. et al. An alternative to standard lumpectomy: A 5-year case series review of oncoplastic breast surgery outcomes in a Canadian setting. Can. J. Surg. 63 (1), E46–E51 (2020).
Article PubMed PubMed Central Google Scholar
Bonci, E. A., Anacleto, J. C. & Cardoso, M. J. Sometimes it is better to just make it simple. De-escalation of oncoplastic and reconstructive procedures. Breast. 69 , 265–273 (2023).
Ohsumi, S. et al. Factors associated with health-related quality-of-life in breast cancer survivors: Influence of the type of surgery. Jpn. J. Clin. Oncol. 39 (8), 491–496 (2009).
Luini, A. et al. The evolution of the conservative approach to breast cancer. Breast. 16 (2), 120–129 (2007).
Pusic, A. L. et al. Development of a new patient-reported outcome measure for breast surgery: The BREAST-Q. Plast. Reconstr. Surg. 124 (2), 345–353 (2009).
Voineskos, S. H., Klassen, A. F., Cano, S. J., Pusic, A. L. & Gibbons, C. J. Giving meaning to differences in BREAST-Q scores: Minimal important difference for breast reconstruction patients. Plast. Reconstr. Surg. 145 (1), 11e–20e (2020).
American Joint Committee on Cancer. AJCC Cancer Staging Manual 8th edn, 589–628 (Springer, 2017).
Google Scholar
Chen, Y. et al. Current trends of breast reconstruction after mastectomy for breast cancer patients in China: A survey report. Zhonghua Zhong Liu Za Zhi. 36 (11), 851–857 (2014).
PubMed Google Scholar
Engel, J., Kerr, J., Schlesinger-Raab, A., Sauer, H. & Hölzel, D. Quality of life following breast-conserving therapy or mastectomy: Results of a 5-year prospective study. Breast J. 10 (3), 223–231 (2004).
Otsuka, S., Watanabe, N., Sasaki, Y. & Shimojima, R. Postoperative courses of breast reconstruction using inferior adipofascial tissue repair. Breast Cancer. 22 (6), 570–577 (2015).
Chu, C. N., Hu, K. C., Wu, R. S. & Bau, D. T. Radiation-irritated skin and hyperpigmentation may impact the quality of life of breast cancer patients after whole breast radiotherapy. BMC Cancer. 21 (1), 330 (2021).
Article CAS PubMed PubMed Central Google Scholar
Mokhtari-Hessari, P. & Montazeri, A. Health-related quality of life in breast cancer patients: Review of reviews from 2008 to 2018. Health Qual. Life Outcomes. 18 (1), 338 (2020).
Rose, M. et al. Patient-reported outcome after oncoplastic breast surgery compared with conventional breast-conserving surgery in breast cancer. Breast Cancer Res. Treat. 180 (1), 247–256 (2020).
Aristokleous, I. & Saddiq, M. Quality of life after oncoplastic breast-conserving surgery: A systematic review. ANZ J. Surg. 89 (6), 639–646 (2019).
de Oliveira-Junior, I. et al. Oncoplastic surgery in breast-conserving treatment: Patient profile and impact on quality of life. Breast Care 16 (3), 243–253 (2021).
Maguire, P. D., Adams, A. & Nichols, M. A. Oncoplastic surgery and radiation therapy for breast conservation: Early outcomes. Am. J. Clin. Oncol. 38 (4), 353–357 (2015).
Ohsumi, S., Shimozuma, K., Kuroi, K., Ono, M. & Imai, H. Quality of life of breast cancer patients and types of surgery for breast cancer—current status and unresolved issues. Breast Cancer. 14 (1), 66–73 (2007).
Bowen, D. J. et al. Possible socioeconomic and ethnic disparities in quality of life in a cohort of breast cancer survivors. Breast Cancer Res. Treat. 106 (1), 85–95 (2007).
Lathan, C. S. et al. Association of financial strain with symptom burden and quality of life for patients with lung or colorectal cancer. J. Clin. Oncol. 34 (15), 1732–1740 (2016).
Download references
Disclaimers
The interpretation and reporting of these data are the sole responsibility of the authors, and no endorsement by the Hangzhou Cancer Hospital is intended nor should be inferred.
This research was financed by the Medical and Health Research Project of Zhejiang Province, China (No. 2023KY964).
Author information
Authors and affiliations.
Division of Breast Surgery, Department of Surgical Oncology, Hangzhou Cancer Hospital, Zhejiang, China
Yi Wang, Yibo He, Shiyan Wu & Shangnao Xie
You can also search for this author in PubMed Google Scholar
Contributions
YW and SX contributed to the conception, design, wrote the manuscript and analyzed the data; YH was responsible for the execution and for data collection; and SW supervised the study. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Shangnao Xie .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Wang, Y., He, Y., Wu, S. et al. Disparities in quality of life among patients with breast cancer based on surgical methods: a cross-sectional prospective study. Sci Rep 14 , 11364 (2024). https://doi.org/10.1038/s41598-024-62105-z
Download citation
Received : 05 October 2023
Accepted : 14 May 2024
Published : 18 May 2024
DOI : https://doi.org/10.1038/s41598-024-62105-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Operable breast cancer
- Oncoplastic surgery
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Cancer newsletter — what matters in cancer research, free to your inbox weekly.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 54, Issue 11
- Breast cancer hypothesis: a single cause for the majority of cases
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Richard A Wiseman
- Department of Epidemiology and Population Health, London School of Hygiene and Tropical Medicine, Keppel Street, London WC1E 7HT
- Dr Wiseman ( richard.wiseman{at}lshtm.ac.uk )
STUDY OBJECTIVE The main cause of breast cancer remains unknown. Numerous causal factors or predisposing conditions have been proposed, but account for only a small percentage of the total disease. The current search for multiple causes is unavailing. This report explores whether any single aetiological agent may be responsible for the majority of cases, and attempts to define its properties.
METHODS Examination of all relevant epidemiological and biological evidence.
MAIN RESULTS Genetic inheritance is not the main cause of breast cancer because most cases are sporadic, there is a low prevalence of family history, and genetically similar women have differing rates after migration. Environmental exposure, such as pollution by industrialisation, is not a major cause, as deduced from a spectrum of epidemiological data. The possibility of infection as cause is not persuasive as there is no direct biological evidence and no epidemiological support. Oestrogen status is closely related to breast cancer risk, but there are numerous inconsistencies and paradoxes. It is suggested that oestrogens are not the proximate agent but are promoters acting in concert with the causal agent. Dietary factors, and especially fat, are associated with the aetiology of breast cancer as shown by intervention and ecological correlation studies, but the evidence from case-control and cohort studies is inconsistent and contradictory.
CONCLUSIONS The hypothesis that best fits the epidemiological data is that dietary fat is not itself the causal agent, but produces depletion of an essential factor that is normally protective against the development of breast cancer. Many of the observed inconsistencies in the epidemiology are explainable if deficiency of this agent is permissive for breast cancer to develop. Some properties of the putative agent are outlined, and research investigations proposed.
- breast cancer
https://doi.org/10.1136/jech.54.11.851
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
The main cause of breast cancer remains unexplained by the known epidemiology. 1-3 Most women who develop breast cancer are ostensibly at low risk. Various factors or predisposing conditions have been identified—the American Public Health Association list obesity, age over 30 years at first child, nulliparity and radiation—but they account for only 26% of the incidence at most 4 and even these are characteristics of secondary risk factors merely associated with factors that determine risk. An alternative hypothesis to multifactorial aetiology is that a single main entity is responsible for the majority of cases (of similar pathology), as with many other cancers.
This report examines the epidemiological evidence and, where appropriate, relevant biological data relating to breast cancer including genetic, external environmental and internal environmental factors. The hypothesis that best fits the data is that there is a single causal agent for the majority of cases, and that it is a deficiency of this agent that is responsible. An attempt is made to deduce what such an aetiological agent may be, how it interacts with other factors, and to define its properties.
A systematic search was made through Medline and BIDS (Bath Information and Data Service) for all epidemiological studies related to breast cancer and causation, particularly to the incidence of breast cancer susceptibility genes, to familial history, to breast cancer and diet, to breast cancer and infection, to oestrogen status, and to mammary tumours in animals. National and International Cancer Registration Statistics were searched. Further data and relevant biological evidence were supplemented from textbooks, other searches and references in publications.
The main cause of breast cancer remains unexplained by the known epidemiology. The search for multiple causes has been unsuccesful. This report explores whether a single causal agent may be responsible for the majority of cases.
Published epidemiology indicates that genetic predisposition is not the main cause, nor are environmental exposures, nor infection; oestrogens are promoters but not the main agent.
Dietary factors and especially fat consumption are associated with breast cancer. However, the hypothesis that best fits the data is that dietary fat is not itself the causal agent but instead causes depletion of an essential agent that is normally protective against breast cancer.
Deficiency of this agent, by limited intake combined with the depletive effect of high fat diet interacting with age and oestrogen status, explains many of the inconsistencies in the epidemiology.
Genetic inheritance is an infrequent but not the main cause of breast cancer. The consensus is that breast cancer susceptibility or cancer predisposition genes are associated with only 4%–8% of breast cancer cases. 5-7 It is apparent therefore that 92%–96% of cases are sporadic.
The risk of developing disease for carriers of germline mutations has been estimated at 54% by age 60 years 8 or 92% lifetime risk. 9 Thus 46% of carriers do not develop the disease by 60 years and 8% never develop the disease. That leaves unanswered the question of what agent is responsible for progression from genetic predisposition to cancer state in women who develop the disease, and why other carriers do not progress, but it is apparent that genetic predisposition cannot be the sole agent. Therefore even for carriers of strong cancer susceptibility genes an environmental trigger is necessary for the disease to become manifest.
Secondly, there is a low incidence of family history in breast cancer patients; typically, 11% of breast cancer patients have a first degree relative, compared with 5% of controls; less than 1% of patients have both a mother and sister with the disease. 9 10
Thirdly, ethnic groups who share the same close gene pool have dissimilar rates after migration to different locations. Breast cancer rates among the Chinese, 93% of whom are of the Han race, 11 vary twofold and threefold on migration, as do those of the genetically close Japanese 12 (see table 1 ). Thus environmental conditions powerfully modify breast cancer rates.
- View inline
Breast cancer rates for Chinese and Japanese women, per 100 000 woman years age adjusted to world standard for 1978–1982 in different locations
ENVIRONMENTAL EXPOSURE
Environmental exposure, such as pollution by industrialisation, is not the main cause of breast cancer.
Location and ethnicity
Singapore is a city state in which a number of ethnic groups have resided for some generations; it is a small island without diverse environments. Relative risk (95% CI) of breast cancer, age adjusted, by Singapore born ethnic group for 1968–82 was: Chinese 1.00 (reference group), Malays 0.78 (0.66, 0.93) Indians 1.26 (0.93, 1.70). 13
Such dissimilar rates between ethnic groups living under the same environmental conditions are unlikely to be attributable to the external environment. A more plausible explanation is that different ethnic groups on migrating overseas caried with them their cultural and dietary habits.
Rural versus urban
Cancer rates in England and Wales reveal rural areas with higher rates than metropolitan/ urban, and vice versa. 14 For women under 45 years, the incidence rates were similar in metropolitan, urban and rural areas but for over 45 years there was “a slight gradient of higher risks in rural than urban and metropolitan areas”.
It thus seems that breast cancer distribution in English or Welsh 15 counties is not associated with industrialision but is simply random with respect to urbanisation.
Social class
(1) England and Wales
The OPCS reported 16 breast cancer proportional registration ratios (PPRs) for 1984 in women for each social class: Class I = 121; Class II = 109; Class IIIN = 109; Class IIIM = 89; Class IV = 80; Class V = 78.
Industrialisation throughout Britain in this time period, or regional variations in industrialisation, could not account for these social class differences.
Standard mortality ratios in Japan, from a prospective study involving 142 857 women, were 17 : high strata (professional, managers) 23.6; middle strata (clerks, sales, service, factory workers) 13.7; low strata (agriculture, fishery, miners) 8.9.
Such differences in SMRs are unlikely to be attributable to industrialisation—which, if responsible for differences in breast cancer risk, are more likely to affect workers in the specific manufacture or industry rather than professional classes and managers.
Thus the social class differences reported from Britain and Japan strongly suggest that industrialisation is unlikely to be responsible for breast cancer.
Industrialisation in different countries
There are (see table 2 ) higher rates in many agricultural/non-industrialised countries as compared with heavily industrialised areas, as well as vice versa. 12 Conversely, in a study of 65 counties in China, 18 all of which were rural and relatively homogeneous with respect to industrialisation, breast cancer mortality rates varied fivefold (from 6.6 to 34.7 per 100 000).
Age standardised breast cancer incidence rates in selected industrialised and non-industrialised locations
Therefore the level of general industrialisation in a country or area is unrelated to the incidence of breast cancer.
INFECTION AND BREAST CANCER
Indirect data concerning retroviruses.
Antibodies to murine mammary tumour virus (MuMTV)—a retrovirus causally associated with the development of mammary tumors in mice 19 —and antigens immunologically related to it, and MuMTV-like particles, have been identifed in human breast cancer cells. 19-24 A retrovirus-like agent has been detected in monocytes of breast cancer patients 25 as have RNA and DNA sequences identical to MuMTV. 26-28 However, against this, MuMTV antibodies were also found in healthy controls 20 29 and MuMTV-like antigens detected in lactating women without breast cancer. 30
The indirect evidence may be attributable to the presence of endogenous retroviral sequences identical to sequences in MuMTV 28 31-33 or other factors. 28 34
Other agents—such as cytomegalovirus—have been proposed, with speculation that late exposure to a common virus increases risk, 35 but there is no experimental evidence and an absence of epidemiological support.
Absence of direct evidence
There is no direct evidence—such as isolation of the retrovirus from cancerous tissue or ductal aspirates, or passage to breast cells. It is possible that the normal human breast contains retroviral sequences, identical to those in MuMTV, thus accounting for the presence of both antigens and antibodies.
Epidemiology of an infecting agent
The geographical and ethnic epidemiology is consistent with an infective theory. An infecting agent is likely to be transmitted by breast feeding, but (a) relative risk for mother-daughter incidence compared with controls in the large CASH Study was only 2.1 (95% CI 1.7, 2.6) 36 ; (b) breast fed infants as compared with bottle fed were shown to have a decreased risk in some studies, 37 38 while others showed no association 39 ; and (c) no increased risk was found in daughters breast fed by mothers who later developed breast cancer. 38 None of these findings are consistent with vertical transmission. There is no evidence either of horizontal transmission—that is, by direct person to person contact.
Thus the possibility of an infection being the causal agent of human breast cancer is not persuasive although an infective cause cannot be disregarded.
THE INTERNAL ENVIRONMENT
Cumulative exposure to oestrogens is associated with most known risk factors, 1 40-42 but the theory that oestrogens are a necessary part of risk has numerous inconsistencies and paradoxes:
pregnant women: there are no reliable statistical data regarding the incidence of breast cancer during pregnancy, but all reports indicate that it is either rare or no more frequent than in non-pregnant women 43 44 despite the surge of oestrogens during pregnancy 45 46
postmenopausal women normally have oestradiol levels at approximately one third that of the lowest premenopausal level, 41 yet the majority of breast cancers occur paradoxically in postmenopausal women;
postmenopausal women taking HRT have raised oestrogen levels. Some studies reported raised breast cancer rates, 5 47-49 others observed no increase in risk, 50-53 and one reported a decreased risk compared with controls. 54 A re-analysis in 1997 of the worldwide data, based on 51 studies and 53 865 postmenopausal women, 55 showed an increased risk comparable to delaying the menopause; the risk increased with increased duration of use. A comprehensive review noted that since 1941 there have been 71 epidemiological studies of the oestrogen-breast cancer link, of which 27 showed a slight increase in risk, 32 showed no difference, and 10 a slight decrease, and concluded that the excess risk is exceedingly small or non-existent. 56
long term administration of oestrogens to premenopausal women, as with oral contraceptives, has not caused a large increase in incidence—one early study found a trend to decreased risk, 57 while most studies agree there is no excess risk 58-61 or at most a small one in recently exposed women only 61 or associated with long term use 62 or in other subgroups related to age or timing of use. 63-66
although higher serum concentrations of oestradiol—a meta-analysis calculated 15% higher 67 —have been reported in breast cancer cases as compared with controls, 68 other studies found no differences. 69 70
men develop breast cancer—the majority are normal men, 71 with normal high level of androgens, proven male fertility, 72 73 and normal oestradiol levels. 71
breast cancer is rarely reported in men having oestrogen treatment for prostatic cancer. 74 75
Accordingly, it seems that oestrogens are not the proximate cause of breast cancer, but are permissive, acting as promoters in concert with a causative agent.
Animal experiments
Animal experiments have repeatedly shown that mice or rats consuming a high fat diet have a higher mammary tumour incidence than those on a basic or restricted fat diet. 76-80 The higher incidence is age dependent, the high fat diet causes a significant shortening of time to tumour appearance 76 and the longer the duration the greater the development of mammary tumours. 81 82 Energy intake affects tumour incidence but is a separate and not a confounding factor. 83-85
Ecological correlation studies
Many studies reported highly significant correlations between consumption of fats and mortality from breast cancer, 86-88 including reports from the UK, 89 90 the USA, 91 92 China, 18 and Japan. 17 The correlation is maximal for diet mortality intervals of 10 years 91 or 12 years. 90 There were highly negative associations for cereal consumption. 17 89 90
Other national and cross national ecological correlation studies have confirmed the positive associations of breast cancer mortality and/or incidence with fat intake, and usually negative correlations with cereals and pulses. 93-96 Reviews of the data have come to the same conclusion. 97-101
Ecological correlation studies in cancer have been justifiably criticised 102 on various grounds, but for breast cancer they show strength, direction, consistency and predictability.
Intervention studies
(i) The Women's Health Trial in the USA
To investigate the effects of a low fat diet on breast cancer, women at increased risk were randomised into a dietary intervention group—a reduction of total daily fat intake by 60%—or control. 103 Results from the Seattle participants 3.5 years after randomisation showed a 15% reduction in breast cancer incidence.
(ii) Fat and DNA damage
Twenty one women with at least one first degree relative diagnosed with breast cancer were randomised to a non-intervention group who had their usual diets or to a group taking a low fat diet developed by the American Health Foundation. 104 Decreased fat intake significantly decreased systematic oxidative stress as shown by DNA damage to leucocytes.
(iii) Wartime in Norway
Breast cancer incidence in Norwegian women who were pubescent or post-pubescent before, during or just after the second world war were compared 105 and fitted to an age cohort model (fig 1 ). There was a definite break in cancer incidence during and after the war, being lower among women who experienced puberty during the war. The incidence rose again after the war.
- Download figure
- Open in new tab
- Download powerpoint
Wartime in Norway. Birth cohort—estimated exposure variable for breast cancer by calender year (year 1916 = 100). From: Tretli S and Gaard H. Lifestyle changes during adolescence and risk of breast cancer: an ecologic study of the effect of World War II in Norway. Cancer Causes Control 1996;7:509 (fig 3). Reproduced by kind permission of Klewer Academic Publishers.
(iv) Wartime in United Kingdom
Trend data showed that breast cancer mortality fell (by over 12%) at the start of the second world war and stayed at the lower level until 1956. It was highly significantly and positively correlated with consumption of meat, fat and sugar, and highly negatively correlated with consumption of cereals. 90
The conclusions from intervention studies are that diet plays an essential part in breast cancer incidence, and that changes in diet do not need decades for the effect to become manifest, but can act within a short time span.
Case-control and cohort studies
(i) Weight and obesity
For premenopausal women studies of risk and weight are inconsistent, while for postmenopausal women there is fairly consistent evidence of weight being associated with an increased risk of breast cancer, 55 106-109 particularly weight gain in adulthood 106 and central obesity. 70 110-113 There is a strong trend of increasing risk with increasing adiposity, recent adiposity influencing breast cancer risk more than early adiposity. 114 This reinforces the point that changes in diet do not need decades for the effect on breast cancer incidence to become manifest.
(ii) Dietary fat
Reviews of case-control studies were varied, but concluded that they did not provide strong support for an association, 101 that the published reports were inconsistent, 115 and that, there was at most a weak and inconsistent association with breast cancer incidence.
Prospective studies of fat intake, many of which were large with substantial statistical power to detect an effect if there was one, were reviewed comprehensively by the COMA Working Group 106 and other reviewers, 97 102 116 117 who concluded that the evidence was moderately consistent that no association exists between fat intake and breast cancer, but that, if an association does exist, the effect is likely to be small.
(iii) Meat consumption
The COMA review 106 observed greater risks with higher meat intake in 17 of 20 case-control studies (despite possible recall bias 118 ) and significantly higher risks (RRs 1.8–2.4) in some prospective studies. 119-123 but others found no association. 124 125 The consensus was that cohort studies are moderately consistent that meat consumption is associated with higher risk.
REASONS FOR DISCREPANT RESULTS
Ecological correlation and intervention studies show a beneficial effect from reduction of total daily fat intake (as do animal experiments) whereas the case-control and cohort studies are inconsistent, although the larger prospective studies show little or no effect on risk of dietary fat but probably some increased risk associated with high meat consumption. There may be methodological reasons for these differences, for example, selection bias or recall bias in case-control studies, confounding in cohort and case-control studies—but such discrepancies could be more reliably explained if we posit the existence of an additional factor, a causal agent of breast cancer acting in conjunction with dietary fat, which has not as yet been taken into account.
FATS AND OESTROGENS ARE NOT SUFFICIENT
If fat—whether dietary fat, or obesity, or increased hip-waist ratio—is the sole dietary cause of breast cancer, it is difficult to explain the discrepancies between the ecological correlation plus intervention studies as contrasted with studies in individuals. Small increases in relative risk, even if statistically significant, could also not account for the large differences in breast cancer incidence in different locations or between different ethnic groups.
Thus the epidemiology indicates that fat is often associated with risk, but as it is neither necessary in all cases, nor sufficient on its own, it is probably a vehicle for another factor, which may or may not be present.
Oestrogens are also involved, but the numerous contradictions and paradoxes show that they are neither necessary (witness men with breast cancer) nor sufficient in themselves (for example, ethnic risk differences in women with normal levels) and thus are probably simply “permissive”, acting, when present, as promoters.
The effect of fat and oestrogens in conjunction is the simplest and most parsimonious model for breast cancer causation, which model would be viable if fats contained a stimulating agent carcinogenic for breast tissue. However, fat and oestrogens together are not sufficient; if they were:
no “thin” women with low dietary fat intake and normal oestrogen levels would develop breast cancer.
a dose response relation should be present—increasing dietary fat in women with normal oestrogen levels should be paralleled by an increasing incidence of breast cancer.
similar levels of fat intake between populations would result in similar rates of breast cancer—but there is evidence directly contradicting this. 18
fat men with increased oestrogen or low androgen levels should develop breast cancer; but thin men with normal male hormonal balance would not.
Therefore some factor additonal to the fat/oestrogen interaction is involved in the initiation or promotion of breast cancer.
DEPLETION OF PROTECTIVE AGENT
The hypothesis that best fits the epidemiological data is that dietary fat is associated with breast cancer risk but is itself not the causal agent; instead high fat intake produces depletion of an essential factor, this factor or agent normally being protective against the development of breast cancer. Deficiency of this agent, perhaps after some latent interval, and probably with a threshold level, permits breast cancer to develop. Increased fat intake, as in a Western diet, causes systemic depletion or depletion in breast tissue of this factor. Increased intake of the agent, or foodstuffs containing it, prevent depletion.
This hypothesis explains a number of inconsistencies in the descriptive epidemiology, as follows:

(i) Deficiency gradient
Women with genetic predisposition need only minor degrees of the deficiency; women with sporadic cancer require a moderate deficiency; women with bilateral cancer will have severe deficiency; and men with breast cancer will have extreme depletion. Oestrogens are promoters making it easier for a carcinoma to develop, or to progress, but they are not necessary if the depletion is sufficiently severe.
(ii) Age gradient
An age related decrease of the protective agent would result in (a) the observed increased incidence of breast cancer with increasing age, and (b) the relation between weight and breast cancer incidence—the absence of excess risk in women under 50 years 109 being attributable to high levels of the agent despite excess fat consumption, whereas natural decline after 50 years combined with depletion caused by high fat intake increases breast cancer incidence.
(iii) Geographical variations
High concentrations in the soil or plants, and consequently in the foodstuffs, in some countries accounts for areas where breast cancer incidence is traditionally low; conversely, low concentrations of the agent combined with a fatty diet accounts for traditionally high areas. High concentrations of this agent in Japanese foodstuffs, and low concentrations in Western foodstuffs, explain why overweight Japanese women have a lower incidence than Dutch women who are actually lighter. 109
(iv) Ethnic and social class variations
The spread of a Western fatty diet has caused depletion of the agent in various populations, accounting for example for rate differences in Asians who migrated to the USA, and low rates in Chinese and Japanese (low fat diet, natural high levels of the agent in foodstuffs).
Previous social class differences in the United Kingdom occurred because foods that cause depletion (meat, milk) were consumed to a greater extent by the higher social groups. This dietary habit has now been reversed, explaining the change in observed incidence between the social classes.
(v) Oestrogen interaction
Oestrogens are tumour promoters, stimulating oestrogen dependent breast tissue when levels of the agent fall below a specific threshold. In areas or populations where tissue levels of the agent are low, hormonally mediated events that cause high oestrogen concentrations will be associated with increased risk, but where women are protected by high levels of the agent no excess risk will be found despite oestrogenic stimulation.
PROPERTIES OF THE AGENT
The agent is a micro-nutrient or trace element present in soils, found in varying amounts in different localities, taken up by plants, grains, fruits, to enter the food chain, present at high levels in, and readily available from, cereals and pulses, but present at only low levels in, or not available from, fat, red meat, or dairy products.
FUTURE RESEARCH
If the hypothesis is correct, then animals given high doses of the agent will have lower rates of induced mammary tumours than control groups not given the agent, or groups with agent depletion; and in humans, concentrations of the agent will vary according to the genetic and gender deficiency gradient, age gradient, and geographical, ethnic and social class differences described above.
Research into the properties and concentrations of a spectrum of micro-nutrients, trace elements, antibodies to infective agents, and vitamins, should reveal if any fits the above criteria. If such an agent is detected, then intervention studies with supplementation should lead to a decline in the incidence of breast cancer.
Acknowledgments
The author is most grateful to Professor Klim McPherson, Cancer and Public Health Unit, London School of Hygiene and Tropical Medicine, for numerous suggestions and revisions, and to Professor Elizabeth Barrett-Connor, Chief Division of Epidemiology, University of California San Diego, for critical but helpful comments on the manuscript.
- Harris JR ,
- Lippman ME ,
- Brinton LA ,
- McLachlan J ,
- Brownson RC ,
- Alavanja MCR
- Colditz GA ,
- Willett WC ,
- Hunter DJ ,
- Lancaster JM ,
- Easton DF ,
- Bishop DT ,
- the Breast Cancer Linkage Consortium
- Thompson WD
- Sattin RW ,
- Webster LA ,
- ↵ ( 1988 ) New Encyclopaedia Brittanica 15th ed. China. ( Encyclop Britt Inc, University of Chicago , Chicago ), 3 : 229 .
- Waterhouse J ,
- Shanmugaratnam K
- Swerdlow A ,
- dos Santos Silva I
- Welsh Office
- Office of Population Censuses and Surveys
- Marshall JR ,
- Yinsheng Q ,
- Charney J ,
- Kramarsky B ,
- Witkin SS ,
- Sarkar NH ,
- Mesa-Tejada R ,
- Ramanarayanan M ,
- Al-Sumidaie AM ,
- Leinster SJ ,
- Spiegelman S
- Spiegleman S ,
- Zotter ST ,
- Kemmer CHR ,
- Lossnitzer A ,
- Yasunaga T ,
- Murray AB ,
- Schmidt J ,
- Bernard D ,
- Bignon YJ ,
- Hareuven M ,
- Richardson A
- Freudenheim JL ,
- Titus-Ernstoff L ,
- Newcomb PA ,
- Hsieh C-C ,
- Trichopoulos D ,
- Wynder EL ,
- Spicer DV ,
- Dahmoush L ,
- Bradlow HL ,
- Fishman J ,
- Axelrod D ,
- Osborne M ,
- Hoover HC , Jr
- Whitfield CR
- Shearman RP
- Speroff L ,
- McPherson K ,
- Fraser GE ,
- Paganini-Hill A ,
- Armstrong BK
- Stanford JL ,
- Collaborative Group on Hormonal Factors in Breast Cancer
- Vessey MP ,
- Hankinson SE ,
- Manson JE ,
- Longnecker MP ,
- Storer BE ,
- Stavraky K ,
- Adami H-O ,
- Henderson BE ,
- Casagrande JT ,
- Rookus MA ,
- van Leeuwen FE
- Malone KE ,
- Daling JR ,
- Thomas HV ,
- Reeves GK ,
- Garland CF ,
- Friedlander NJ ,
- Barrett-Connor E ,
- Bruning PF ,
- Bonfrer JMG ,
- Hanisch R ,
- Thomas DB ,
- Jimenez LM ,
- McTiernan A ,
- Mabuchi K ,
- McClure JA ,
- Schlappack OK ,
- Tannenbaum A
- Setevenson GT ,
- Carroll KK ,
- Aylsworth CF ,
- Trosko JE ,
- Kritchevsky D ,
- Klurfeld DM
- Welsch CW ,
- Freedman LS ,
- Clifford C ,
- Gammal EB ,
- Plunkett ER
- Armstrong B ,
- Gaskill SP ,
- McGuire WL ,
- Osborne CK ,
- Tominaga S ,
- Schatzkin A ,
- Piantadosi S ,
- Miccozzi M ,
- Nicolosi A ,
- McMichael AJ ,
- Goodwin PJ ,
- Greenwald P ,
- Gorbach SL ,
- Morrill-LaBrode A ,
- Martino S ,
- Heilbrun LK ,
- Committee on Medical Aspects of Food and Nutrition Policy (COMA)
- Sherwood K ,
- McDonald SS
- Waard de F ,
- Cornelis JP ,
- Schapira DV ,
- Ballard-Barbash R ,
- Sellers TA ,
- Potter JD ,
- Ziegler RG ,
- Hoover RN ,
- Nomura AMY ,
- Martin LJ ,
- Spiegelman D ,
- Giovannucci E ,
- Stampfer MJ ,
- Toniolo P ,
- Pasternack BS
- Vatten LJ ,
- Kvinnsland S
- Steineck G ,
- Jarvinen R ,
- Phillips RL ,
Funding: none.
Conflicts of interest: none.
Read the full text or download the PDF:
DigitalCommons@UNMC
Home > Eppley Institute > Theses & Dissertations
Theses & Dissertations: Cancer Research
Theses/dissertations from 2024 2024.
Novel Spirocyclic Dimer (SpiD3) Displays Potent Preclinical Effects in Hematological Malignancies , Alexandria Eiken
Therapeutic Effects of BET Protein Inhibition in B-cell Malignancies and Beyond , Audrey L. Smith
Identifying the Molecular Determinants of Lung Metastatic Adaptation in Prostate Cancer , Grace M. Waldron
Identification of Mitotic Phosphatases and Cyclin K as Novel Molecular Targets in Pancreatic Cancer , Yi Xiao
Theses/Dissertations from 2023 2023
Development of Combination Therapy Strategies to Treat Cancer Using Dihydroorotate Dehydrogenase Inhibitors , Nicholas Mullen
Overcoming Resistance Mechanisms to CDK4/6 Inhibitor Treatment Using CDK6-Selective PROTAC , Sarah Truong
Theses/Dissertations from 2022 2022
Omics Analysis in Cancer and Development , Emalie J. Clement
Investigating the Role of Splenic Macrophages in Pancreatic Cancer , Daisy V. Gonzalez
Polymeric Chloroquine in Metastatic Pancreatic Cancer Therapy , Rubayat Islam Khan
Evaluating Targets and Therapeutics for the Treatment of Pancreatic Cancer , Shelby M. Knoche
Characterization of 1,1-Diarylethylene FOXM1 Inhibitors Against High-Grade Serous Ovarian Carcinoma Cells , Cassie Liu
Novel Mechanisms of Protein Kinase C α Regulation and Function , Xinyue Li
SOX2 Dosage Governs Tumor Cell Identity and Proliferation , Ethan P. Metz
Post-Transcriptional Control of the Epithelial-to-Mesenchymal Transition (EMT) in Ras-Driven Colorectal Cancers , Chaitra Rao
Use of Machine Learning Algorithms and Highly Multiplexed Immunohistochemistry to Perform In-Depth Characterization of Primary Pancreatic Tumors and Metastatic Sites , Krysten Vance
Characterization of Metastatic Cutaneous Squamous Cell Carcinoma in the Immunosuppressed Patient , Megan E. Wackel
Visceral adipose tissue remodeling in pancreatic ductal adenocarcinoma cachexia: the role of activin A signaling , Pauline Xu
Phos-Tag-Based Screens Identify Novel Therapeutic Targets in Ovarian Cancer and Pancreatic Cancer , Renya Zeng
Theses/Dissertations from 2021 2021
Functional Characterization of Cancer-Associated DNA Polymerase ε Variants , Stephanie R. Barbari
Pancreatic Cancer: Novel Therapy, Research Tools, and Educational Outreach , Ayrianne J. Crawford
Apixaban to Prevent Thrombosis in Adult Patients Treated With Asparaginase , Krishna Gundabolu
Molecular Investigation into the Biologic and Prognostic Elements of Peripheral T-cell Lymphoma with Regulators of Tumor Microenvironment Signaling Explored in Model Systems , Tyler Herek
Utilizing Proteolysis-Targeting Chimeras to Target the Transcriptional Cyclin-Dependent Kinases 9 and 12 , Hannah King
Insights into Cutaneous Squamous Cell Carcinoma Pathogenesis and Metastasis Using a Bedside-to-Bench Approach , Marissa Lobl
Development of a MUC16-Targeted Near-Infrared Antibody Probe for Fluorescence-Guided Surgery of Pancreatic Cancer , Madeline T. Olson
FGFR4 glycosylation and processing in cholangiocarcinoma promote cancer signaling , Andrew J. Phillips
Theses/Dissertations from 2020 2020
Cooperativity of CCNE1 and FOXM1 in High-Grade Serous Ovarian Cancer , Lucy Elge
Characterizing the critical role of metabolic and redox homeostasis in colorectal cancer , Danielle Frodyma
Genomic and Transcriptomic Alterations in Metabolic Regulators and Implications for Anti-tumoral Immune Response , Ryan J. King
Dimers of Isatin Derived Spirocyclic NF-κB Inhibitor Exhibit Potent Anticancer Activity by Inducing UPR Mediated Apoptosis , Smit Kour
From Development to Therapy: A Panoramic Approach to Further Our Understanding of Cancer , Brittany Poelaert
The Cellular Origin and Molecular Drivers of Claudin-Low Mammary Cancer , Patrick D. Raedler
Mitochondrial Metabolism as a Therapeutic Target for Pancreatic Cancer , Simon Shin
Development of Fluorescent Hyaluronic Acid Nanoparticles for Intraoperative Tumor Detection , Nicholas E. Wojtynek
Theses/Dissertations from 2019 2019
The role of E3 ubiquitin ligase FBXO9 in normal and malignant hematopoiesis , R. Willow Hynes-Smith
BRCA1 & CTDP1 BRCT Domainomics in the DNA Damage Response , Kimiko L. Krieger
Targeted Inhibition of Histone Deacetyltransferases for Pancreatic Cancer Therapy , Richard Laschanzky
Human Leukocyte Antigen (HLA) Class I Molecule Components and Amyloid Precursor-Like Protein 2 (APLP2): Roles in Pancreatic Cancer Cell Migration , Bailee Sliker
Theses/Dissertations from 2018 2018
FOXM1 Expression and Contribution to Genomic Instability and Chemoresistance in High-Grade Serous Ovarian Cancer , Carter J. Barger
Overcoming TCF4-Driven BCR Signaling in Diffuse Large B-Cell Lymphoma , Keenan Hartert
Functional Role of Protein Kinase C Alpha in Endometrial Carcinogenesis , Alice Hsu
Functional Signature Ontology-Based Identification and Validation of Novel Therapeutic Targets and Natural Products for the Treatment of Cancer , Beth Neilsen
Elucidating the Roles of Lunatic Fringe in Pancreatic Ductal Adenocarcinoma , Prathamesh Patil
Theses/Dissertations from 2017 2017
Metabolic Reprogramming of Pancreatic Ductal Adenocarcinoma Cells in Response to Chronic Low pH Stress , Jaime Abrego
Understanding the Relationship between TGF-Beta and IGF-1R Signaling in Colorectal Cancer , Katie L. Bailey
The Role of EHD2 in Triple-Negative Breast Cancer Tumorigenesis and Progression , Timothy A. Bielecki
Perturbing anti-apoptotic proteins to develop novel cancer therapies , Jacob Contreras
Role of Ezrin in Colorectal Cancer Cell Survival Regulation , Premila Leiphrakpam
Evaluation of Aminopyrazole Analogs as Cyclin-Dependent Kinase Inhibitors for Colorectal Cancer Therapy , Caroline Robb
Identifying the Role of Janus Kinase 1 in Mammary Gland Development and Breast Cancer , Barbara Swenson
DNMT3A Haploinsufficiency Provokes Hematologic Malignancy of B-Lymphoid, T-Lymphoid, and Myeloid Lineage in Mice , Garland Michael Upchurch
Theses/Dissertations from 2016 2016
EHD1 As a Positive Regulator of Macrophage Colony-Stimulating Factor-1 Receptor , Luke R. Cypher
Inflammation- and Cancer-Associated Neurolymphatic Remodeling and Cachexia in Pancreatic Ductal Adenocarcinoma , Darci M. Fink
Role of CBL-family Ubiquitin Ligases as Critical Negative Regulators of T Cell Activation and Functions , Benjamin Goetz
Exploration into the Functional Impact of MUC1 on the Formation and Regulation of Transcriptional Complexes Containing AP-1 and p53 , Ryan L. Hanson
DNA Polymerase Zeta-Dependent Mutagenesis: Molecular Specificity, Extent of Error-Prone Synthesis, and the Role of dNTP Pools , Olga V. Kochenova
Defining the Role of Phosphorylation and Dephosphorylation in the Regulation of Gap Junction Proteins , Hanjun Li
Molecular Mechanisms Regulating MYC and PGC1β Expression in Colon Cancer , Jamie L. McCall
Pancreatic Cancer Invasion of the Lymphatic Vasculature and Contributions of the Tumor Microenvironment: Roles for E-selectin and CXCR4 , Maria M. Steele
Altered Levels of SOX2, and Its Associated Protein Musashi2, Disrupt Critical Cell Functions in Cancer and Embryonic Stem Cells , Erin L. Wuebben
Theses/Dissertations from 2015 2015
Characterization and target identification of non-toxic IKKβ inhibitors for anticancer therapy , Elizabeth Blowers
Effectors of Ras and KSR1 dependent colon tumorigenesis , Binita Das
Characterization of cancer-associated DNA polymerase delta variants , Tony M. Mertz
A Role for EHD Family Endocytic Regulators in Endothelial Biology , Alexandra E. J. Moffitt
Biochemical pathways regulating mammary epithelial cell homeostasis and differentiation , Chandrani Mukhopadhyay
EPACs: epigenetic regulators that affect cell survival in cancer. , Catherine Murari
Role of the C-terminus of the Catalytic Subunit of Translesion Synthesis Polymerase ζ (Zeta) in UV-induced Mutagensis , Hollie M. Siebler
LGR5 Activates TGFbeta Signaling and Suppresses Metastasis in Colon Cancer , Xiaolin Zhou
LGR5 Activates TGFβ Signaling and Suppresses Metastasis in Colon Cancer , Xiaolin Zhou
Theses/Dissertations from 2014 2014
Genetic dissection of the role of CBL-family ubiquitin ligases and their associated adapters in epidermal growth factor receptor endocytosis , Gulzar Ahmad
Strategies for the identification of chemical probes to study signaling pathways , Jamie Leigh Arnst
Defining the mechanism of signaling through the C-terminus of MUC1 , Roger B. Brown
Targeting telomerase in human pancreatic cancer cells , Katrina Burchett
The identification of KSR1-like molecules in ras-addicted colorectal cancer cells , Drew Gehring
Mechanisms of regulation of AID APOBEC deaminases activity and protection of the genome from promiscuous deamination , Artem Georgievich Lada
Characterization of the DNA-biding properties of human telomeric proteins , Amanda Lakamp-Hawley
Studies on MUC1, p120-catenin, Kaiso: coordinate role of mucins, cell adhesion molecules and cell cycle players in pancreatic cancer , Xiang Liu
Epac interaction with the TGFbeta PKA pathway to regulate cell survival in colon cancer , Meghan Lynn Mendick
Theses/Dissertations from 2013 2013
Deconvolution of the phosphorylation patterns of replication protein A by the DNA damage response to breaks , Kerry D. Brader
Modeling malignant breast cancer occurrence and survival in black and white women , Michael Gleason
The role of dna methyltransferases in myc-induced lymphomagenesis , Ryan A. Hlady
Design and development of inhibitors of CBL (TKB)-protein interactions , Eric A. Kumar
Pancreatic cancer-associated miRNAs : expression, regulation and function , Ashley M. Mohr
Mechanistic studies of mitochondrial outer membrane permeabilization (MOMP) , Xiaming Pang
Novel roles for JAK2/STAT5 signaling in mammary gland development, cancer, and immune dysregulation , Jeffrey Wayne Schmidt
Optimization of therapeutics against lethal pancreatic cancer , Joshua J. Souchek
Theses/Dissertations from 2012 2012
Immune-based novel diagnostic mechanisms for pancreatic cancer , Michael J. Baine
Sox2 associated proteins are essential for cell fate , Jesse Lee Cox
KSR2 regulates cellular proliferation, transformation, and metabolism , Mario R. Fernandez
Discovery of a novel signaling cross-talk between TPX2 and the aurora kinases during mitosis , Jyoti Iyer
Regulation of metabolism by KSR proteins , Paula Jean Klutho
The role of ERK 1/2 signaling in the dna damage-induced G2 , Ryan Kolb
Regulation of the Bcl-2 family network during apoptosis induced by different stimuli , Hernando Lopez
Studies on the role of cullin3 in mitosis , Saili Moghe
Characteristics of amyloid precursor-like protein 2 (APLP2) in pancreatic cancer and Ewing's sarcoma , Haley Louise Capek Peters
Structural and biophysical analysis of a human inosine triphosphate pyrophosphatase polymorphism , Peter David Simone
Functions and regulation of Ron receptor tyrosine kinase in human pancreatic cancer and its therapeutic applications , Yi Zou
Theses/Dissertations from 2011 2011
Coordinate detection of new targets and small molecules for cancer therapy , Kurt Fisher
The role of c-Myc in pancreatic cancer initiation and progression , Wan-Chi Lin
The role of inosine triphosphate pyrophosphatase (ITPA) in maintanence [sic] of genomic stability in human cells , Miriam-Rose Menezes
- Eppley Institute Website
- McGoogan Library
Advanced Search
- Notify me via email or RSS
- Collections
- Disciplines
Author Corner
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
- Open access
- Published: 15 May 2024
Dietary supplement intake in women with breast cancer before and after diagnosis: results from the SUCCESS C trial
- Dagmar Hauner 1 ,
- Anna Mang 1 ,
- Lara Donik 1 ,
- Florian Schederecker 1 , 2 ,
- Dorothy Meyer 1 ,
- Brigitte Rack 3 ,
- Wolfgang Janni 3 &
- Hans Hauner 1
BMC Cancer volume 24 , Article number: 591 ( 2024 ) Cite this article
148 Accesses
Metrics details
There is little evidence that dietary supplements are beneficial for patients with breast cancer; therefore, they are usually not recommended by treatment guidelines. The aim of the present analysis was to assess the prevalence of dietary supplement (DS) intake among women before and after a breast cancer diagnosis.
Participants in the SUCCESS C lifestyle intervention study, a randomized controlled trial in women with newly diagnosed intermediate- to high-risk breast cancer, completed two questionnaires on dietary supplement intake 24 months (QS1) and 48 months (QS2) after beginning the lifestyle intervention. The study was registered on 12.17.2008 under the EU Clinical Trials Register https://www.clinicaltrialsregister.eu/ , trial registration number: 2008-005453-38. The questionnaires collected data on DS intake during the 5-year period prediagnosis (QS1) and in the period postdiagnosis (QS2). Multivariate logistic regression models were fitted to examine differences in DS intake between the two intervention groups. The groups were then pooled to examine differences in DS use between the prediagnostic and postdiagnostic period.
A total of 320 questionnaires from 58.5% of intervention group completers and 416 questionnaires from 46.6% of low-level intervention group completers were included in the analysis. Overall, 20.2% of all respondents reported taking DS prior to their diagnosis. After a cancer diagnosis, the percentage of women taking DS significantly increased to 56.4% (p for time effect < 0.0001). No differences in DS intake between the intervention groups were observed. Single or combined preparations of vitamins and minerals/trace elements were the most frequently reported supplements. Notably, a 9-fold increase in vitamin D intake was reported postdiagnosis, where the proportion of women increased from 3.8 to 34.5%.
A 3-fold increase in the reported intake of dietary supplements was seen in women after a breast cancer diagnosis. These observations underscore the need to incorporate patient education surrounding the use of dietary supplements in a treatment care plan, particularly addressing the negligible benefits as well as the potential risks and treatment interactions.
Peer Review reports
Dietary supplement (DS) intake has gained popularity among patients with a wide range of diseases and can be obtained without a prescription in most countries. DS are subject to European law in the European Union [ 1 ] and complemented by national regulations. In Germany, DS are defined as food products that supplement general nutrition and consist of a “concentrate of nutrients or other substances with a nutrition-specific or physiological effect, alone or in composition” [ 2 ]. Importantly, DS do not require approval before they are marketed, and in Germany, in contrast to other countries such as Denmark and France, there is no defined upper intake level [ 3 ]. Only the amounts of the individual ingredients, per serving, must be indicated with reference to the recommended daily intake and an accompanying warning not to exceed the recommended daily amount [ 2 ]. National consumer surveys show that over one-quarter (27.6%) of adults in Germany report taking DS [ 4 , 5 ].
The use of DS is also rather common among cancer patients [ 6 , 7 ], and is particularly high in women with breast cancer, with reported rates ranging between 45 and 87% of patients [ 6 , 8 , 9 , 10 , 11 , 12 , 13 , 14 ]. This behavior is in clear contrast to recommendations from expert panels, which universally discourage the use of supplements for both cancer survivors in general and breast cancer patients [ 15 , 16 ]. Because of this discrepancy, we were interested in examining the prevalence of DS intake among participants in the lifestyle modification part of the German SUCCESS C trial before and after a breast cancer diagnosis.
The SUCCESS C trial
Data was obtained from the SUCCESS C trial, an open-label, multicenter, randomized controlled study that examined the effect of two different chemotherapy regimens ( n = 3642) as well as the effect of a comprehensive lifestyle intervention program on disease-free survival in women with newly diagnosed HER2/neu-negative intermediate-risk to high-risk breast cancer [ 17 , 18 , 19 ]. The study and all experimental protocols were approved by the Heinrich Heine University Düsseldorf Ethics Committee and was registered on 12.17,2008 under the EU Clinical Trials Register https://www.clinicaltrialsregister.eu/ , identifier: 2008-005453-38. All participants provided written informed consent.
The focus of the 2-year lifestyle intervention was on moderate weight loss in breast cancer patients with a BMI between 24 and 40 kg/m² ( n = 2292). Not later than six weeks after surgery, 2292 women were randomized to either the lifestyle intervention group (IG) or the low-level intervention group (LLIG). The lifestyle intervention started either 3 or 6 months after the completion of chemotherapy. Women in the IG received an individualized, telephone-based program promoting an energy-reduced, healthy diet and regular physical activity, whereas the LLIG received general recommendations for a healthy lifestyle [ 18 ]. Figure 1 shows a participation flowchart. From the 776 women (IG) and 1009 women (LLIG) who began the lifestyle program, at total of 547 in the IG (70.5%) and 893 in the LLIG (88.5%) completed the 2-year intervention. Specific information or advice on dietary supplements was not delivered to either group.
Assessment of dietary supplement intake
Participants in both groups were requested to record their food intake, using 7-day dietary records, as well as their physical activity. These data were collected at five time points (i.e., baseline, 6, 12, 24 and 48 months after starting the lifestyle intervention). All participants were also requested to fill in two additional questionnaires on DS intake, developed by our research team and added to the dietary record forms, at 24 months (i.e. the end of the lifestyle intervention, QS1) and 48 months (i.e. 24 months later, QS2). The questionnaires collected data on DS intake for the following periods: (1) within 5 years prior to a breast cancer diagnosis (T0), and (2) postdiagnosis at 24 months (T1) and 48 months (T2) after starting the lifestyle intervention (Table S1 ).
Participants were asked whether they used DS, and if so, to report the dosage, frequency (i.e. how often in a day), and product name of any vitamins, minerals/trace elements, and/or any combinations of vitamins and minerals and/or any other dietary supplements.
Statistical methods
This secondary analysis used data from 736 women who completed questionnaires on DS intake. Descriptive data were derived from QS1 and reported as mean values ± standard deviation (SD).
The components and dosages of DS were calculated from questionnaires, when available. Any drugs that were misclassified as DS by participants were excluded from analysis.
Analyses were performed with IBM SPSS Statistics version 26 (IBM, Armonk, NJ, USA) and R software version 4.0.3 (RStudio Inc, Boston MA, USA). The proportion of women taking DS were compared between the two intervention groups using binary logistic regression models. The primary aim of this analysis was to investigate any differences in DS prevalence before (T0) and after a breast cancer diagnosis (T1) for the entire cohort by fitting binary logistic regression models. We further investigated the change in DS intake in the period postdiagnosis (i.e. the change between T1 and T2). Only women who filled out questionnaires at both time points were included in the descriptive data presentation.
Subgroups were determined a priori and analyses were performed to compare the following groups: participants with a BMI < 30 kg/m² vs. BMI ≥ 30 kg/m², and participants with positive vs. negative hormone receptor status. Participants were also subcategorized into three age groups: < 51 years, 51–64 years and ≥ 65 years to observe any differences in DS use. The SUCCESS C study was not powered to detect differences between subgroups; hence mainly descriptive reporting of between-group differences was considered the most appropriate choice rather than using interaction tests to assess subgroup effects. This approach was chosen to reduce the risk of Type 1 errors [ 20 ]. All models were adjusted for age at baseline, weight at baseline and chemotherapy arm. A two-tailed p value of ≤ 0.05 was considered statistically significant.
In total, 342 women in the IG and 434 women in the LLIG filled out the QS1, of which 320 (from 58.5% of the IG completers) and 416 (46.6% of the LLIG completers) could be included in the analyses. For QS2, we obtained 276 (IG) and 368 (LLIG) questionnaires, of which 216 (IG) and 288 (LLIG) provided complete questionnaires at both time points to assess the change in DS use over time (Fig. 1 ). The discrepancy in the number of collected questionnaires versus those included in the analyses was due to several questionnaires containing either insufficient or implausible responses. Comparing women whose QS1 were missing or incomplete ( n = 712) to those who were included in this study ( n = 736), we found that the non-included women were younger (55.5 vs. 57.4 years), had a higher BMI (29.4 vs. 28.6 kg/m 2 ) and an increased waist circumference (94.6 vs. 92.9 cm). Moreover, a larger proportion of these women were premenopausal (37.4% vs. 27.6%), smokers (17.1% vs. 11.0%) and underwent an anthracyclin-based chemotherapy regimen (52.5% vs. 47.0%) (all p-values < 0.05).
The baseline participant characteristics on dietary supplement intake are presented in Table 1 and stratified by intervention group. Findings were generally comparable in both groups. The mean age was 57.4 years (both groups) and mean BMI was 28.8 kg/m² (IG) and 28.5 kg/m² (LLIG). Baseline weight was comparable in both groups (IG 78.1 kg and LLIG 77.3 kg). Most participants had tumor staging T1 or T2, N0 or N1 status, and G2 or G3 grading. The majority of women were hormone receptor positive (IG 83.7% and LLIG 79.3%). Most women, 77.2% (IG) and 79.6% (LLIG), underwent breast-conserving surgery, whereas 18.8% (IG) and 17.5% (LLIG) had mastectomies. All participants received adjuvant chemotherapy and most underwent radiation therapy (IG 90.9% and LLIG 89.9%). Hypertension was noted in 40.0% (IG) and 39.2% (LLIG) of the participants, diabetes mellitus in 4.7% (IG) and 4.8% (LLIG), and coronary heart disease in 0% (IG) and 1.0% (LLIG) (Table 1 ).
Total intake and intake of specific groups of dietary supplements
Prediagnostic DS use was reported by 20.2% and postdiagnostic use by 56.4% of all women. Results were similar when groups were split into IG and LLIG, with no significant between-group differences at either time point (Table 2 ). After a breast cancer diagnosis, a significant 2.8-fold increase (p-value for time effect < 0.0001) in DS use was found in all participants, which was also similar when observing the behavior of each group separately (2.6-fold in IG and 2.9-fold in LLIG, with no significant group difference) (Table 2 ).
We found that 13.9% of women reported taking any mineral/trace mineral, 11.1% any vitamin, and 8.3% any combination of vitamins and/or minerals before diagnosis. Postdiagnosis, the use of DS increased significantly by 4.1-fold for any vitamin (45.9% of women), 3.2-fold for any mineral/trace element (44.7% of women), and 3.9-fold for any combination of vitamins and/or minerals (31.9% of women) (p for time effect < 0.0001 for all three). Similar results were found for the IG and the LLIG separately, with no significant between-group differences for either time point. The consumption of herbal supplements (T0 4.5% vs. T1 11.8%), omega-3 fatty acid supplements (T0 1.5% vs. T1 2.9%) and other supplements (T0 1.6% vs. T1 8.0%) was less frequently reported (Table 2 ).
Intake of specific micronutrients
We found that prediagnosis, women most frequently took magnesium (9.9%), followed by zinc (5.4%), vitamin C (5.2%), B vitamins (4.6%) and vitamin D (3.8%). Fewer women reported taking vitamin E (2.2%), calcium (2.3%), selenium (1.6%), beta-carotene (1.2%) and vitamin A (1.1%). After a breast cancer diagnosis, 1 out of 3 women (34.5%) reported taking vitamin D. A considerable increase in intake was also reported for B vitamins (21.6%), magnesium (21.2%), zinc (19.6%), selenium (17.4%), vitamin C (13.6%) and calcium (12.8%). Fewer women reported taking vitamin E (8.8%), vitamin A (6.5%), and beta-carotene (5.2%). The increase in DS use postdiagnosis was particularly notable for selenium, vitamin D and calcium (p for time effect < 0.0001). No significant between-group differences were found when comparing DS use in the IG vs. LLIG (Table 3 ).
Dosage of specific micronutrients
The dosage of selected micronutrients that were taken postdiagnosis is shown in Table S2 . The median daily dosage values were 310.0 mg/d for vitamin C, 22.0 µg/d for vitamin D, 38.0 mg/d for vitamin E, 600.0 mg/d for calcium, 300.0 mg/d for magnesium, 100.0 mg/d for selenium, and 10.0 mg/d for zinc. A high percentage of women who reported using selected micronutrients took dosages that exceeded the reference values for daily intake (Table S3 ), such as vitamin C (85.5%), vitamin E (80.0%), zinc (78.6%), selenium (66.4%), and vitamin D (50.7%), followed by magnesium (31.3%), and calcium (14.6%) (Table S2 ). Women taking dosages exceeding the tolerable upper intake level (UL) (Table S3 ) were reported for magnesium (53.1%), zinc (20.0%) vitamin E (13.3%), selenium (8.4%), vitamin C (4.4%), vitamin D (3.0%), and calcium (2.3%) (Table S2 ).
Subgroup analyses
A similar significant increase in the intake of total DS was found for women with a BMI < 30 kg/m² and women with a BMI ≥ 30 kg/m² (p for time effect < 0.0001) as well as for women with and without anti-hormonal therapy (data not shown). Similar increases in postdiagnosis DS use were seen when participants were classified into three age-range categories (T0 vs. T1 in women < 51 years old: from 22.1 to 58.4%; 51–64 years old: from 19.2 to 56.4% and in women ≥ 65 years old: from 20.3 to 54.2%).
Temporal changes of postdiagnosis DS intake
No significant differences were observed when analysis was restricted to participants who filled out both QS1 and QS2 at the end of active lifestyle intervention (T1) and at a follow-up two years later (T2). Overall, DS intake was reported by 58.3% ( n = 294) of women at T1 and 57.9% ( n = 292) at T2; 48.0% reported taking any vitamin supplement at T1 and 46.6% at T2, 46.6% took any mineral/trace mineral at T1 and 43.1% at T2 and 42.3% took any combination of vitamins/minerals and/or other dietary supplements at T1 and 41.5% at T2 (Table S4 ).
The main finding of this secondary analysis was that women increased their use of DS almost 3-fold, from 20.2 to 56.4%, after receiving a breast cancer diagnosis. The proportion of participants taking DS was similar when the cohort was split into their respective study intervention groups (i.e., IG and LLIG). Confounders, such as age, BMI or type of cancer treatment did not substantively change the outcomes.
Data from a nationally representative sample showed that 28.0% of women in Germany report taking DS, with even higher rates observed among older women (e.g. 43.2% of women aged 65–80 years) [ 4 ]. Our findings show that the percentage of SUCCESS C participants who took DS was clearly higher than those who were part of the national sample, irrespective of age. The prevalence we report is comparable to findings from a recent German survey that found that 59.8% of women with breast cancer took DS after their diagnosis [ 14 ]. Notably, another German study in women with breast cancer observed that almost twice as many women compared to our cohort (36%) took DS prediagnosis and observed only a moderate increase in prevalence after diagnosis (45%) [ 13 ].
Our observations of a postdiagnostic increase in DS intake is in line with other cross-sectional and prospective studies. European studies have reported postdiagnostic DS intake rates of 62.8% in women with cancer [ 10 ] and 68.3% in individuals with breast cancer [ 21 ]. It is noteworthy that US-American studies show higher prevalence rates in both the prediagnostic (i.e. 54 − 84%) [ 9 , 10 , 12 ] and postdiagnostic periods (i.e. 60.6% and 87.0%) [ 6 , 7 , 9 , 11 , 12 , 22 ], reflecting a generally higher DS intake compared to European studies. Of interest, some of these studies showed that adult cancer survivors with a healthier lifestyle, lower BMI, higher diet quality, and higher physical activity were more likely to use DS [ 7 , 21 , 23 ].
Single or combined preparations of vitamins and minerals/trace minerals were the most frequently reported DS in the SUCCESS-C trial, with a significant 3- to 4-fold increase postdiagnosis, a finding that is in line with data from another European study [ 10 ]. The widespread use of DS, reported in these studies, is in striking contrast to current recommendations for breast cancer survivors. The Continuous Update Expert Report from 2018 [ 15 ] as well as national expert statements [ 24 ] explicitly do not recommend the use of DS in this population. In addition, the US Preventive Services Task Force recently released an updated report on the evidence for the efficacy and safety of DS for the prevention of cancer and cardiovascular diseases. In this report, a clear recommendation against beta carotene and vitamin E supplements for cancer patients was given [ 16 ]. The authors also noted that only insufficient evidence was found to evaluate the benefits and potential harms of multivitamins, vitamins B3, B6, C and D, calcium, selenium, and folic acid (both with and without vitamin B12) on cancer outcomes [ 16 ]. In accordance with this report, literature confirms that there is not only no proven benefit for DS, but also the potential for negative effects which must be considered when taking any DS [ 16 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 ].
Given compelling evidence indicating the absence of benefits from dietary supplements, their widespread use by a majority of breast cancer patients is concerning. One reason for this discrepancy is the inadequate translation of established scientific knowledge and research findings into clinical practice to inform patient care and improve health literacy. In the SUCCESS C trial, no specific information on the use of DS was delivered to either group. Therefore, the marked increase in DS intake following a cancer diagnosis, found in this analysis, likely did not result from medical recommendations provided by their oncologists. A large breast cancer trial observed that one-third of participants were advised to take DS by their clinicians and 10% were asked to discontinue DS intake, while 51% of the patients did not receive any advice [ 32 ]. These findings suggest that the widespread use of DS is not medically supervised. Other research indicates that the majority of physicians are unaware of DS use among their cancer patients [ 6 ]. A web-based survey conducted as part of the NutriNet Sante Cohort study noted potentially adverse DS intake patterns among a significant number of cancer patients. Examples include concurrently taking vitamin E and anticoagulants or smokers taking beta-carotene supplements [ 21 ].
The general lack of awareness among clinicians on their cancer patients’ use of DS aligns with a growing trend toward self-medication and a heightened interest in complementary and alternative medicine [ 33 ]. At the same time, predatory marketing campaigns targeting cancer patients and offering deceptive or unsupported health claims are common. Patients are vulnerable to such messages and frequently believe that DS can prevent nutritional deficiencies and thereby support their immune system. Furthermore, many patients hope or expect that DS can mitigate the side effects of conventional cancer therapies and improve their quality of life [ 34 ].
Vitamin D supplementation showed the most dramatic increase postdiagnosis in the present study: from 3.8 to 34.5% of participants. Similarly, in a French study, vitamin D was clearly preferred among all single-ingredient DS, where 47.7% of women with breast cancer reported regular intake [ 21 ]. The reasons for these high intake rates are unclear. According to current recommendations by the World Cancer Research Fund there is insufficient evidence for general vitamin D use for this population [ 15 , 24 ], although some guidelines recommend routine measurement of serum 25(OH)D in oncology patients and supplementation if a deficiency is detected [ 35 ]. For osteoporosis prevention in postmenopausal women, consuming the recommended daily amounts of calcium and vitamin D should be ensured through a balanced diet. If the recommended levels cannot be achieved through food then supplements should be given to fill nutrient gaps [ 36 ]. Vitamin D supplements are principally recommended when clinical osteoporosis is diagnosed [ 36 ]. In breast cancer patients, prevention of therapy-associated bone loss is advised. However, vitamin D and calcium supplementation should be medically indicated and tailored to the individual patient [ 24 ]. Therefore, the increase in vitamin D supplementation we observed in this cohort is plausible and at least partially justified.
A high-quality diet is associated with a better breast cancer prognosis [ 37 ] and routine monitoring for nutritional imbalances and weight change is important for all cancer patients [ 38 , 39 ]. During chemotherapy and radiotherapy, an adequate intake of micronutrients should be ensured according to physiological requirements [ 24 ]. However, possible drug interactions must be considered. While some antioxidants might reduce side effects, antagonistic effects of antioxidants and other nutrients may compromise the therapeutic efficiency of chemotherapy and radiotherapy, thereby affecting prognostic outcomes [ 24 , 25 , 27 , 30 , 40 , 41 ]. Hence, unnecessary and unmonitored consumption of dietary supplements should be avoided, particularly in excessive doses.
Finally, there is also a financial burden on patients arising from out-of-pocket costs for DS that cannot be ignored. Many cancer patients suffer from financial hardship as a consequence of their illness due to diverse additional costs [ 42 ], a reduction in working hours [ 43 ], a loss of revenue and an increased likelihood of unemployment [ 43 ]. Around 20–30% of cancer survivors do not return to the workplace [ 42 ]. Financial challenges could potentially exacerbate the disease burden and hinder the adoption of a healthy lifestyle. For these reasons, clinicians bear the responsibility of addressing costs associated with DS use within the patient treatment plan to prevent avoidable additional expenses [ 15 , 39 ].
Our manuscript presents several strengths that contribute to the robustness of our findings. Firstly, our study was able to analyze data on DS intake from a sizable cohort of 736 participants. Additionally, we collected data from DS use in both the pre- and postdiagnostic periods, providing a nuanced understanding of changes in DS intake behavior. Furthermore, detailed baseline characteristics of participating women were documented, enhancing the reliability and applicability of our results. The nationwide recruitment of women from over 200 gynecological practices across Germany underscores the potential generalizability of our findings to adult German women with overweight or obesity and Her2/neu-negative breast cancer.
However, several weaknesses also merit consideration. Notably, data on DS use was available from only around one-third of the initially randomized participants and around 40% of those who commenced the lifestyle intervention. This may have resulted in an overall discrepancy between the DS use we report in this study and behavior from the entire cohort, although other studies have reported similar findings. Additionally, we lacked information regarding the reasons for DS intake among participants and relied solely on retrospective self-reporting. Lastly, the study was limited to women with a BMI between 24 and 40 kg/m² and Her2/neu-negative breast cancer who received chemotherapy, potentially restricting the generalizability of our findings to a broader population. These weaknesses highlight areas for further investigation and consideration in future research endeavors.
In conclusion, results from this study show that the proportion of women taking DS markedly increased after a diagnosis of breast cancer. Given the inadequate scientific evidence supporting the general benefit and safety of additional DS intake, patients with breast cancer should receive fundamental guidance from their treating physicians regarding DS. Consideration of DS use should be a recurring and consistently addressed aspect of comprehensive cancer care.
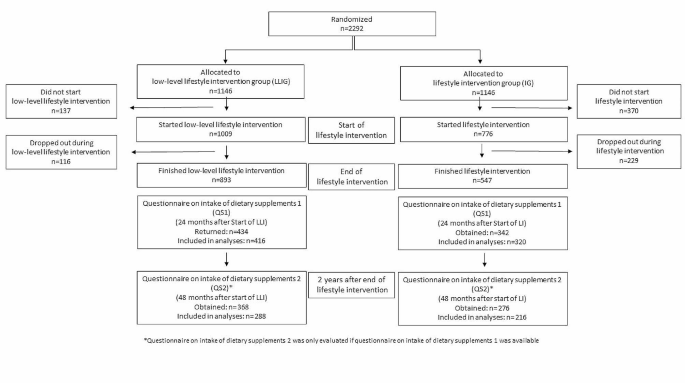
Flow diagram of the lifestyle intervention part of SUCCESS C Trial and the analysis of the intake of dietary supplements
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Dietary supplements
Intervention group
Low-level intervention group
Dietary supplement questionnaire
GUIDELINE 2002/46/EG OF THE EUROPEAN PARLIAMENT AND COUNCIL of June 10. 2002 on the adaptation of laws of the legal regulation of member states relating to supplements. Official Journal of European Communities: The European Parliament and the Council of the European Union 2021 [ https://eur-lex.europa.eu/legal-content/DE/TXT/PDF/?uri=CELEX:02002L0046-20170726&qid=1545903950901&from=DE
Verordnung über Nahrungsergänzungsmittel. (Nahrungsergänzungsmittelverordnung - NemV): Bundesministerium der Justiz und für Verbraucherschutz; [updated 2017; cited October 26, 2022. https://www.gesetze-im-internet.de/nemv/NemV.pdf .
Weißenborn A, Bakhiya N, Demuth I, Ehlers A, Ewald M, Niemann B, et al. Höchstmengen für Vitamine Und Mineralstoffe in Nahrungsergänzungsmitteln. J Consumer Prot Food Saf. 2018;13(1):25–39.
Article Google Scholar
Bundesministerium für Ernährung LuV. Ergebnisbericht Teil 1: Nationale Verzehrsstudie II, die bundesweite Befragung Zur Ernährung Von Jugendlichen Und Erwachsenen. Volume 5. Contract No.: Max Rubner-Institut; 2008.
Google Scholar
Bundesministerium für Ernährung LuV. Ergebnisbericht Teil 2: Nationale Verzehrsstudie II, Die bundesweite Befragung zur Ernährung von Jugendlichen und Erwachsenen: Max Rubner-Institut. 2008.
Velicer CM, Ulrich CM. Vitamin and mineral supplement use among US adults after cancer diagnosis: a systematic review. J Clin Oncol. 2008;26(4):665–73.
Article CAS PubMed Google Scholar
Miller PE, Vasey JJ, Short PF, Hartman TJ. Dietary supplement use in adult cancer survivors. Oncol Nurs Forum. 2009;36(1):61–8.
Article PubMed PubMed Central Google Scholar
Newman V, Rock CL, Faerber S, Flatt SW, Wright FA, Pierce JP. Dietary supplement use by women at risk for breast cancer recurrence. The women’s healthy eating and living Study Group. J Am Diet Assoc. 1998;98(3):285–92.
Kwan ML, Greenlee H, Lee VS, Castillo A, Gunderson EP, Habel LA, et al. Multivitamin use and breast cancer outcomes in women with early-stage breast cancer: the Life after Cancer Epidemiology study. Breast Cancer Res Treat. 2011;130(1):195–205.
Velentzis LS, Keshtgar MR, Woodside JV, Leathem AJ, Titcomb A, Perkins KA, et al. Significant changes in dietary intake and supplement use after breast cancer diagnosis in a UK multicentre study. Breast Cancer Res Treat. 2011;128(2):473–82.
Greenlee H, Kwan ML, Kushi LH, Song J, Castillo A, Weltzien E, et al. Antioxidant supplement use after breast cancer diagnosis and mortality in the Life after Cancer Epidemiology (LACE) cohort. Cancer. 2012;118(8):2048–58.
Greenlee H, Kwan ML, Ergas IJ, Strizich G, Roh JM, Wilson AT, et al. Changes in vitamin and mineral supplement use after breast cancer diagnosis in the pathways Study: a prospective cohort study. BMC Cancer. 2014;14:382.
Jung AY, Cai X, Thoene K, Obi N, Jaskulski S, Behrens S, et al. Antioxidant supplementation and breast cancer prognosis in postmenopausal women undergoing chemotherapy and radiation therapy. Am J Clin Nutr. 2019;109(1):69–78.
Article PubMed Google Scholar
Holzapfel C, Kocsis A, Jaeckel B, Martignoni M, Hauner D, Hauner H. Dietary habits and intake of nutritional supplements in patients of outpatient cancer clinics. Ernährungs Umschau. 2020;67(3):60–8.
Research WCRFIAIfC. Continuous Update Project Expert Report. 2018. Survivors of breast and other cancers [ https://www.wcrf.org/wp-content/uploads/2021/02/Cancer-Survivors.pdf .
Mangione CM, Barry MJ, Nicholson WK, Cabana M, Chelmow D, Coker TR, et al. Vitamin, Mineral, and Multivitamin supplementation to prevent Cardiovascular Disease and Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2022;327(23):2326–33.
Rack B, Andergassen U, Neugebauer J, Salmen J, Hepp P, Sommer H, et al. The German SUCCESS C study - the first European lifestyle study on breast Cancer. Breast Care (Basel). 2010;5(6):395–400.
Hauner D, Rack B, Friedl T, Hepp P, Janni W, Hauner H. Rationale and description of a lifestyle intervention programme to achieve moderate weight loss in women with non-metastatic breast cancer: the lifestyle intervention part of the SUCCESS C study. BMJ Nutr Prev Health. 2020;3(2):213–9.
de Gregorio A, Janni W, Friedl TWP, Nitz U, Rack B, Schneeweiss A, et al. The impact of anthracyclines in intermediate and high-risk HER2-negative early breast cancer-a pooled analysis of the randomised clinical trials PlanB and SUCCESS C. Br J Cancer. 2022;126(12):1715–24.
Wang X, Piantadosi S, Le-Rademacher J, Mandrekar SJ. Statistical considerations for subgroup analyses. J Thorac Oncol. 2021;16(3):375–80.
Pouchieu C, Fassier P, Druesne-Pecollo N, Zelek L, Bachmann P, Touillaud M, et al. Dietary supplement use among cancer survivors of the NutriNet-Santé cohort study. Br J Nutr. 2015;113(8):1319–29.
Poole EM, Shu X, Caan BJ, Flatt SW, Holmes MD, Lu W, et al. Postdiagnosis supplement use and breast cancer prognosis in the after breast Cancer Pooling Project. Breast Cancer Res Treat. 2013;139(2):529–37.
Article CAS PubMed PubMed Central Google Scholar
Li K, Kaaks R, Linseisen J, Rohrmann S. Consistency of vitamin and/or mineral supplement use and demographic, lifestyle and health-status predictors: findings from the European prospective investigation into Cancer and Nutrition (EPIC)-Heidelberg cohort. Br J Nutr. 2010;104(7):1058–64.
S3-Leitlinie Früherkennung, Diagnose, Therapie und Nachsorge des Mammakarzinoms, Langversion 4.4 [Internet]. AWMF Registernummer: 032-045OL. 2021a. https://register.awmf.org/assets/guidelines/032-045OLl_S3_Mammakarzinom_2021-07.pdf .
D’Andrea GM. Use of antioxidants during chemotherapy and radiotherapy should be avoided. CA Cancer J Clin. 2005;55(5):319–21.
Bjelakovic G, Nikolova D, Gluud LL, Simonetti RG, Gluud C. Antioxidant supplements for prevention of mortality in healthy participants and patients with various diseases. Cochrane Database Syst Rev. 2012;2012(3):Cd007176.
PubMed PubMed Central Google Scholar
Harvie M. Nutritional supplements and cancer: potential benefits and proven harms. Am Soc Clin Oncol Educ Book. 2014:e478–86.
Navarro VJ, Barnhart H, Bonkovsky HL, Davern T, Fontana RJ, Grant L, et al. Liver injury from herbals and dietary supplements in the U.S. Drug-Induced Liver Injury Network. Hepatology. 2014;60(4):1399–408.
Rayman MP, Winther KH, Pastor-Barriuso R, Cold F, Thvilum M, Stranges S, et al. Effect of long-term selenium supplementation on mortality: results from a multiple-dose, randomised controlled trial. Free Radic Biol Med. 2018;127:46–54.
Vernieri C, Nichetti F, Raimondi A, Pusceddu S, Platania M, Berrino F, et al. Diet and supplements in cancer prevention and treatment: clinical evidences and future perspectives. Crit Rev Oncol Hematol. 2018;123:57–73.
Chen F, Du M, Blumberg JB, Ho Chui KK, Ruan M, Rogers G, et al. Association among Dietary Supplement Use, Nutrient Intake, and Mortality among U.S. adults: a Cohort Study. Ann Intern Med. 2019;170(9):604–13.
Zirpoli GR, Brennan PM, Hong CC, McCann SE, Ciupak G, Davis W, et al. Supplement use during an intergroup clinical trial for breast cancer (S0221). Breast Cancer Res Treat. 2013;137(3):903–13.
Micke O, Bruns F, Glatzel M, Schönekaes K, Micke P, Mücke R, et al. Predictive factors for the use of complementary and alternative medicine (CAM) in radiation oncology. Eur J Integr Med. 2009;1(1):19–25.
Tank M, Franz K, Cereda E, Norman K. Dietary supplement use in ambulatory cancer patients: a survey on prevalence, motivation and attitudes. J Cancer Res Clin Oncol. 2021;147(7):1917–25.
S3-Leitlinie Komplementärmedizin in der Behandlung von onkologischen PatientInnen, Kurzversion 1.1 [Internet]. Deutsche Krebshilfe, AWMF. 2021b. https://register.awmf.org/assets/guidelines/032-055OLk_Komplementaermedizin-in-der-Behandlung-von-onkologischen-PatientInnen-2021-11.pdf .
Prophylaxe eVDO. Diagnostik und Therapie der Osteoporose bei postmenopausalen Frauen und bei Männern, Langfassung. 2017. Contract No.: AWMF-Register-Nr.: 183/001.
Weigl J, Hauner H, Hauner D. Can Nutrition Lower the risk of recurrence in breast Cancer? Breast Care (Basel). 2018;13(2):86–91.
Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, Bozzetti F, et al. ESPEN guidelines on nutrition in cancer patients. Clin Nutr. 2017;36(1):11–48.
Muscaritoli M, Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, et al. ESPEN practical guideline: Clinical Nutrition in cancer. Clin Nutr. 2021;40(5):2898–913.
Lawenda BD, Kelly KM, Ladas EJ, Sagar SM, Vickers A, Blumberg JB. Should supplemental antioxidant administration be avoided during chemotherapy and radiation therapy? J Natl Cancer Inst. 2008;100(11):773–83.
Ambrosone CB, Zirpoli GR, Hutson AD, McCann WE, McCann SE, Barlow WE, et al. Dietary supplement use during chemotherapy and survival outcomes of patients with breast Cancer enrolled in a Cooperative Group Clinical Trial (SWOG S0221). J Clin Oncol. 2020;38(8):804–14.
Arbeitsgemeinschaft Soziale Arbeit in der Onkologie (ASO). [ https://www.krebsgesellschaft.de/onko-internetportal/basis-informationen-krebs/leben-mit-krebs/beratung-und-hilfe/armutsrisiko-krebs.html .
Hernandez D, Schlander M. Income loss after a cancer diagnosis in Germany: an analysis based on the socio-economic panel survey. Cancer Med. 2021;10(11):3726–40.
Download references
Acknowledgements
The study was initially funded by unrestricted grants given to WJ from Pfizer, Sanofi-Aventis, Chugai and Veridex. We wish to thank Dr. Lynne Stecher for initial statistical advice. We also appreciate the excellent contribution by the almeda GmbH Munich lifestyle coaches, led by Mrs. Rose, for performing the telephone-based lifestyle intervention. We thank Mrs. Heidrun-Lorsbach, CEO of the CRO Alcedis, Giessen, for support with data collection. Finally, we would like to thank all the study centers, their contributing staff members and all participating women.
HH received funding for the analysis of dietary supplement intake by the Else Kröner Fresenius Foundation, Bad Homburg, Germany (grant no. 2016_A31), the Bavarian State Ministry of Health (project no. 89397) and the Technical University of Munich, Germany. The study design, data collection and analysis, decision to publish, and preparation of the manuscript were independent from the funder.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
Institute of Nutritional Medicine, Else Kröner Fresenius Center for Nutritional Medicine, TUM School of Medicine and Health, Technical University of Munich, Munich, Germany
Dagmar Hauner, Anna Mang, Lara Donik, Florian Schederecker, Dorothy Meyer & Hans Hauner
Chair of Epidemiology, TUM School of Medicine and Health, Technical University of Munich, Munich, Germany
Florian Schederecker
Department of Gynecology and Obstetrics, University Hospital Ulm, Ulm, Germany
Brigitte Rack & Wolfgang Janni
You can also search for this author in PubMed Google Scholar
Contributions
HH, DH and BR designed the lifestyle intervention arm of the SUCCESS C trial. WJ was responsible for the design of the complete SUCCESS C trial. BR and WJ were responsible for supervision and support of the study centers. DH supervised the lifestyle program conducted by lifestyle coaches of almeda, a health care provider in Munich. DH and the almeda team were responsible for data collection and management. AM supported the analysis of DS intake, LD and FS performed the final statistical analyses. DH, DM and HH wrote the manuscript. All authors reviewed and commented on the manuscript.
Corresponding author
Correspondence to Hans Hauner .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the Heinrich Heine University Düsseldorf Ethics Committee. The protocol was registered under the EU Clinical Trials Register https://www.clinicaltrialsregister.eu/ , identifier: 2008-005453-38. All women gave written informed consent to participate in the trial.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hauner, D., Mang, A., Donik, L. et al. Dietary supplement intake in women with breast cancer before and after diagnosis: results from the SUCCESS C trial. BMC Cancer 24 , 591 (2024). https://doi.org/10.1186/s12885-024-12341-3
Download citation
Received : 01 February 2024
Accepted : 06 May 2024
Published : 15 May 2024
DOI : https://doi.org/10.1186/s12885-024-12341-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Dietary supplement use
- Inadequate intake
- Excess intake
- Breast cancer
- Micronutrients
ISSN: 1471-2407
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Today's news
- Reviews and deals
- Climate change
- 2024 election
- Fall allergies
- Health news
- Mental health
- Sexual health
- Family health
- So mini ways
- Unapologetically
- Buying guides
Entertainment
- How to Watch
- My Portfolio
- Latest News
- Stock Market
- Premium News
- Biden Economy
- EV Deep Dive
- Stocks: Most Actives
- Stocks: Gainers
- Stocks: Losers
- Trending Tickers
- World Indices
- US Treasury Bonds
- Top Mutual Funds
- Highest Open Interest
- Highest Implied Volatility
- Stock Comparison
- Advanced Charts
- Currency Converter
- Basic Materials
- Communication Services
- Consumer Cyclical
- Consumer Defensive
- Financial Services
- Industrials
- Real Estate
- Mutual Funds
- Credit cards
- Balance Transfer Cards
- Cash-back Cards
- Rewards Cards
- Travel Cards
- Personal Loans
- Student Loans
- Car Insurance
- Morning Brief
- Market Domination
- Market Domination Overtime
- Opening Bid
- Stocks in Translation
- Lead This Way
- Good Buy or Goodbye?
- Fantasy football
- Pro Pick 'Em
- College Pick 'Em
- Fantasy baseball
- Fantasy hockey
- Fantasy basketball
- Download the app
- Daily fantasy
- Scores and schedules
- GameChannel
- World Baseball Classic
- Premier League
- CONCACAF League
- Champions League
- Motorsports
- Horse racing
- Newsletters
New on Yahoo
- Privacy Dashboard
Yahoo Finance
Olema oncology announces promising new data for palazestrant in combination with ribociclib presented at the 2024 esmo breast cancer congress.
Across 50 treated patients, palazestrant (OP-1250) in combination with ribociclib was well tolerated with no new safety signals or increased toxicity and no clinically meaningful impact on drug exposure of either therapy
85% clinical benefit rate (CBR) observed to date across all CBR-eligible patients supports promising preliminary efficacy profile of the palazestrant-ribociclib combination
Olema will host an investor conference call today at 8:00 a.m. ET
SAN FRANCISCO, May 15, 2024 (GLOBE NEWSWIRE) -- Olema Pharmaceuticals, Inc. ( “Olema” or “Olema Oncology,” Nasdaq: OLMA), a clinical-stage biopharmaceutical company focused on the discovery, development and commercialization of targeted therapies for women’s cancers, today announced interim results from an ongoing Phase 1b/2 clinical study of palazestrant (OP-1250) in combination with CDK4/6 inhibitor ribociclib for the treatment of ER+/HER2- metastatic breast cancer. These results, as of the data cut-off of March 13, 2024, will be presented on May 16, 2024, in a poster session at the 2024 ESMO Breast Cancer Annual Congress in Berlin, Germany (ESMO Breast).
The poster, titled “A Phase 1b/2 Study of Palazestrant (OP-1250) in Combination with Ribociclib in Patients with Estrogen Receptor-Positive, Human Epidermal Growth Factor Receptor 2-Negative, Advanced and/or Metastatic Breast Cancer”, highlighted that:
Across 50 treated patients, the combination of up to 120 mg of palazestrant with the full and approved dose of 600 mg of ribociclib daily was well tolerated, with no new safety signals or enhancement of toxicity and an overall safety profile consistent with the established safety profile of ribociclib plus an endocrine therapy.
Palazestrant did not affect ribociclib drug exposure and ribociclib had no clinically meaningful effect on palazestrant drug exposure.
Promising preliminary efficacy was observed to date with a clinical benefit rate (CBR) of 85% across all CBR-eligible patients (11/13), 83% in ESR1 -mutant patients (5/6), 86% in ESR1 -wild-type patients (6/7), and 83% in prior CDK4/6 inhibitor patients (10/12).
Partial responses were observed in five patients through the data cut-off (2 confirmed, 3 unconfirmed) among 23 response-evaluable patients.
Findings from this study support the continued clinical development of palazestrant in combination with ribociclib for the first-line treatment of ER+/HER2- advanced or metastatic breast cancer.
“The data we are presenting at the ESMO Breast Cancer Annual Congress in Berlin add further support to our thesis that palazestrant possesses key characteristics that make it a potential backbone endocrine therapy of preference for ER+/HER2- breast cancer, both as a monotherapy and in combination with other targeted agents,” said Sean P. Bohen, M.D., Ph.D., President and Chief Executive Officer of Olema Oncology. “We are grateful to the approximately 300 women to date that have participated across our clinical trials. We are excited with the progress we are making, and we look forward to advancing toward our goal of transforming the endocrine therapy standard of care for breast cancer.”
Phase 1b/2 Clinical Study Results
As of the data cut-off of March 13, 2024, 50 patients with recurrent, locally advanced or metastatic ER+/HER2- breast cancer with at least four weeks of follow-up were treated with palazestrant (3 patients each at 30 mg once daily and 60 mg once daily, 44 patients at the palazestrant recommended Phase 2 dose (RP2D) of 120 mg once daily) plus ribociclib 600 mg once daily (three weeks followed by one week off treatment). The majority of patients (37 or 74%) were 2 nd /3 rd line+, with 37 (74%) patients having received prior endocrine therapy for metastatic breast cancer, 35 (70%) patients having received prior CDK4/6 inhibitors (11 or 22% having received two prior lines of CDK4/6 inhibitors), and nine (18%) patients having received chemotherapy for metastatic breast cancer. Of 48 patients whose circulating tumor DNA (ctDNA) was assessed as of the data cut-off, 27% had activating mutations in ESR1 at baseline. The study is now fully enrolled with 60 patients.
Pharmacokinetics
Palazestrant demonstrated favorable pharmacokinetics characterized by high oral bioavailability, dose proportional exposure and a half-life of eight days as a single agent, with steady-state plasma levels showing minimal peak-to-trough variability enabling consistent inhibition of ER for the full dosing interval. Palazestrant did not affect ribociclib 600 mg drug exposure when compared with published exposure data for single-agent ribociclib. Steady-state trough values showed no clinically significant difference between the combination and single-agent palazestrant.
Safety and Tolerability
Treatment with palazestrant up to the RP2D of 120 mg was well tolerated with no dose-limiting toxicities, and the maximum tolerated dose (MTD) was not reached. The majority of treatment-emergent adverse events (TEAEs) were Grade 1 or 2, and the severity and incidence of adverse events were consistent with the expected safety profile of ribociclib plus endocrine therapy. Ten patients had dose reduction of ribociclib only, due to QTcF prolongation (n=4), neutropenia (n=4), or fatigue (n=2). No patients discontinued palazestrant due to a treatment-related adverse event, and two patients discontinued ribociclib for neutropenia without discontinuation of palazestrant in the 120 mg cohort. Neutropenia was reversible in all patients and the timing was consistent with ribociclib-related neutropenia.
In a maturing dataset, palazestrant showed anti-tumor activity and prolonged disease stabilization in patients both with ESR1 wild-type and ESR1 activating mutations at baseline, and in those previously treated with one or two lines of CDK4/6 inhibitors. Partial responses were observed in five patients (two confirmed, three unconfirmed as of data cut-off) out of 23 response-evaluable patients. Across patients who were CBR-eligible, the CBR was 85% (11/13) for all patients, 83% (5/6) for patients with ESR1 mutations, 86% (6/7) for patients that were ESR1 wild-type, and for CDK4/6i-pretreated patients the CBR was 83% (10/12). The longest duration on treatment is 44 weeks through the data cut-off, and 66% (33/50) of patients in this data set remain on treatment as of the data cut-off date.
A copy of the poster will be available on Olema’s website under the Science section.
Company Investor Webcast and Conference Call
Olema will host a webcast and conference call for analysts and investors to review the data being presented at ESMO Breast Cancer Annual Congress 2024 today, Wednesday, May 15, 2024, at 8:00 a.m. ET (2:00 p.m. CEST). Please register for the webcast by visiting the Investors & Media section of Olema’s website at olema.com .
About Palazestrant (OP-1250)
Palazestrant (OP-1250) is a novel, orally-available small molecule with dual activity as both a complete estrogen receptor (ER) antagonist (CERAN) and selective ER degrader (SERD). It is currently being investigated in patients with recurrent, locally advanced or metastatic ER-positive (ER+), human epidermal growth factor receptor 2-negative (HER2-) breast cancer. In clinical studies, palazestrant completely blocks ER-driven transcriptional activity in both wild-type and mutant forms of metastatic ER+ breast cancer and has demonstrated anti-tumor efficacy along with attractive pharmacokinetics and exposure, favorable tolerability, CNS penetration, and combinability with CDK4/6 inhibitors. Palazestrant has been granted U.S. Food and Drug Administration (FDA) Fast Track designation for the treatment of ER+/HER2- metastatic breast cancer that has progressed following one or more lines of endocrine therapy with at least one line given in combination with a CDK4/6 inhibitor. It is being evaluated both as a single agent in an ongoing Phase 3 clinical trial, OPERA-01, and in Phase 1/2 combination studies with CDK4/6 inhibitors (palbociclib and ribociclib), a PI3Ka inhibitor (alpelisib), and an mTOR inhibitor (everolimus). For more information, please visit www.opera01study.com .
About Olema Oncology
Olema Oncology is a clinical-stage biopharmaceutical company committed to transforming the standard of care and improving outcomes for women living with cancer. Olema is advancing a pipeline of novel therapies by leveraging our deep understanding of endocrine-driven cancers, nuclear receptors, and mechanisms of acquired resistance. In addition to our lead product candidate, palazestrant (OP-1250), a proprietary, orally-available complete estrogen receptor (ER) antagonist (CERAN) and a selective ER degrader (SERD), Olema is developing a potent KAT6 inhibitor (OP-3136). Olema is headquartered in San Francisco and has operations in Cambridge, Massachusetts. For more information, please visit us at www.olema.com .
Forward Looking Statements
Statements contained in this press release regarding matters that are not historical facts are “forward-looking statements” within the meaning of Section 27A of the Securities Act of 1933 and Section 21E of the Securities Exchange Act of 1934. Words such as “anticipate,” “expect,” “will,” “may,” “goal,” “potential” and similar expressions (as well as other words or expressions referencing future events, conditions or circumstances) are intended to identify forward-looking statements. These statements include those related to the potential beneficial characteristics, safety, tolerability, efficacy, and therapeutic effects of palazestrant, the development of palazestrant, the initiation and timing of clinical trials, palazestrant’s combinability with other drugs, the potential of palazestrant to become a backbone endocrine therapy in the treatment of ER+/HER2- metastatic breast cancer, and Olema’s potential to transform the endocrine therapy standard of care treatments for women living with ER+/HER2- metastatic breast cancer. Because such statements deal with future events and are based on Olema’s current expectations, they are subject to various risks and uncertainties, and actual results, performance or achievements of Olema could differ materially from those described in or implied by the statements in this press release. These forward-looking statements are subject to risks and uncertainties, including, without limitation, those discussed in the section titled “Risk Factors” in Olema’s Quarterly Report on Form 10-Q for the quarter ended March 31, 2024, and other filings and reports that Olema makes from time to time with the U.S. Securities and Exchange Commission. Except as required by law, Olema assumes no obligation to update these forward-looking statements, including in the event that actual results differ materially from those anticipated in the forward-looking statements.
Contact : Geoffrey Mogilner, Vice President, Investor Relations and Communications [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.38(1); 2015

Knowledge, attitudes and practices toward breast cancer screening in a rural South African community
Dorah u. ramathuba.
1 Department of Advanced Nursing, University of Venda, South Africa
Confidence T. Ratshirumbi
2 Department of Psychology, University of Venda, South Africa
Tshilidzi M. Mashamba
The study assessed the knowledge, attitudes and breast cancer screening practices amongst women aged 30–65 years residing in a rural South African community.
A quantitative, descriptive cross-sectional design was used and a systematic sampling technique was employed to select 150 participants. The questionnaire was pretested for validity and consistency. Ethical considerations were adhered to in protecting the rights of participants. Thereafter, data were collected and analysed descriptively using the Predictive Analytics Software program.
Findings revealed that the level of knowledge about breast cancer of women in Makwarani Community was relatively low. The attitude toward breast cancer was negative whereas the majority of women had never performed breast cancer diagnostic methods.
Health education on breast cancer screening practices is lacking and the knowledge deficit can contribute negatively to early detection of breast cancer and compound late detection. Based on the findings, community-based intervention was recommended in order to bridge the knowledge gap.
Introduction
Breast cancer is a global health problem and the most common cancer amongst women, comprising 23% of the female cancers (Parkins & Fernández 2006 :S71). It is also the leading cause of cancer-related deaths in low-resourced countries. Women in any age range are at risk of breast cancer and the risks increases with advanced age (Omotara et al . 2012 :1). Despite the development of advanced technology in the detection of breast cancer, the mortality rate remains high. Breast cancer is the main cause of cancer mortality in women aged 40–44 years old (Alwan et al . 2012 :338; Khanjani, Noor & Rostami 2012 :177). Although substantial improvement in survival has been reported in high-income countries, the risk continues to increase. The survival rates in middle- and low-income countries remain low (Alwan et al . 2012 :338).
Data from South Africa's National Cancer Registry (NCR) show breast cancer as the leading cancer amongst women. South African women have a one in 29 lifetime risk of developing breast cancer, with an age-standardised incidence rate of 30.6 per 100 000 population (Lemlem et al . 2013 :2). In a study done in Turkey amongst female health workers, it was found that breast self-examination (BSE) was not a regular behaviour; doctors made up 31.3% of those who performed BSE and midwives, 21.8% (Akpinar et al . 2011 :3065). This indicates that health personnel do perform BSE, but the rate of those who practise BSE on a regular basis is low. The level of knowledge and attitude of health professionals are important determinants for the use of screening programmes and creation of an environment supportive of screening behaviours by offering positive role models. Empowering nurses with information about early detection methods and their related benefits could help advance their skills in performing BSE and expand their roles as client educators (Akpinar et al . 2011 :3065; Lemlem 2013 :3). It is important that health personnel are aware of the risk factors for breast cancer, in order to guide their patients for necessary screening.
Lack of basic knowledge and an effective information delivery system for breast cancer further threatens the life and well-being of women. Breast cancer is silently killing women – mainly those who have no knowledge and continue to be ignorant about breast cancer and breast diagnostic screening methods for early detection (Shepherd & McInerney 2006 :71). Knowledge is a necessary component but it is insufficient unless the cultural relevance is assured by the health professional providing direct healthcare (Dow Meneses & Yarbro 2007 :111). Omotara et al . ( 2012 :1) also reported lack of information regarding breast cancer to the rural and urban populace of Nigeria, saying that it is responsible for the negative perception of the curability of a cancer detected early and the efficacy of screening tests. In addition, silence and lack of understanding of the concept of risk factors associated with breast cancer discourage people from seeking early intervention or even admitting that the symptoms that they are experiencing are related to breast cancer. Level of awareness regarding how to perform simple life-saving diagnostic breast checks such as BSE further compounds the problem of late detection. Empowerment of women with information on BSE is of paramount importance, especially in countries without modern technologies for breast cancer screening (Shepherd & McInerney 2007 :38). South African rural communities have limited technological resources, but BSE can contribute greatly if women are informed about this technique and regular practice would reduce late presentation.
Akhigbe and Akhigbe ( 2012 :74) also suggest that health beliefs differs from culture to culture, that cancer fatalism may be a deterrent to participation in health-promoting behaviours. This is because some people believe that illnesses or catastrophic events happen because of a higher power (such as God), or they are meant to happen and cannot be avoided; as a result, fatalism becomes part of the person's worldview. Black African communities usually associate chronic conditions with witchcraft and evil spirits. Cultural values and ethnic diversity have an impact on health beliefs, which may influence how rural women interact with the western medication, especially conditions such as breast cancer. Some women delay seeking treatment because of fear of stigma concerning their daughters as it is believed that they also might be affected by breast cancer and might not be considered for a good marriage. Furthermore, it is believed that cancer is a death sentence from God (Dow Meneses & Yarbro 2007 :108).
Problem statement
Breast cancer is the most common cancer in South Africa and it is increasing in incidence, with large numbers of women with breast cancer being found in rural areas. The reason for this could be that access to information is limited as many women miss out on early detection because of their lack of knowledge and practice of BSE and other screening practices (Khokhar 2009 :249). The researcher observed a pattern of women presenting with symptoms of late stage of the disease, such as a red, swollen, tender breast, but confusing it with an inflammatory condition. This is despite the fact that breast cancer is a preventable disease, which indicates a knowledge deficit. When a woman notices skin changes on the breast, she should immediately seek medical help for early diagnosis and treatment. In Thulamela Municipality, for the year spanning 2011–2012, there were 85 women being treated for gynaecological cancers at the Provincial hospital, according to the gynaecological register in two hospitals within the district for the financial year 2011 and 2012 (District Health Statistics-2011/2012). There are different methods for early diagnosis of breast cancer: BSE, physical examination by a medical doctor and mammography. Unfortunately, most breast cancers are diagnosed when they are in the advanced stages. Breast cancer mortality in Vhembe District may be compounded by limited resources, inadequate preventative screening programmes and lack of access to advanced technology in rural health facilities, leading to late presentation or not coming forth because of their health-belief system.
The purpose of the study was to determine the knowledge, attitudes and breast cancer screening practices amongst women in a rural South Africa community.
To assess knowledge regarding breast cancer amongst women in a rural South African community.
To describe the attitudes and practices regarding breast cancer screening amongst women in a rural South African community.
Research methods and design
Research setting.
Vhembe District is one of the districts in Limpopo Province, situated in the northern part of the province and sharing borders with the Capricorn and Mopani districts in the eastern and western parts, respectively. The sharing of borders extends to Zimbabwe and Botswana in the northwest and Mozambique in the southeast, through the Kruger National Park. Vhembe District comprises three municipalities, namely, Thulamela, Makhado and Mutale. The study was undertaken in Makwarani, a rural village in the outskirts of Thohoyandou town, which is a low-resourced Venda community in Thulamela Municipality.
Research design
This study employed a descriptive cross-sectional survey, which is a non-experimental design examining data from a specific group, at one point in time (LoBiondo-Wood & Haber 2006 :244), designed to assess knowledge, attitudes and practices toward breast cancer screening in a rural South African community.
Burns and Grove ( 2007 :40) state that a population comprises all elements (individuals, objects or substances) that meet the criteria for inclusion in a study. In this survey, the study population comprised 150 women. The target population was all Tshivenda-speaking women aged between 30–65 years.
Systematic sampling was used for this study. Polit and Beck ( 2008 :347) state that the process of systematic sampling involves selecting every k th individual on the list after having selected a starting point at random. Makwarani village has 300 households; these were written on a list and 150 households were selected randomly using the lottery method, with a random start of two and then the researcher selected one woman from every second household, which comprised 150 women. This type of sampling was used because probability sampling reduces sampling errors and bias, whilst enhancing representation and the confidence of the sample.
Data collection method
The researcher used a closed-ended questionnaire comprising three sections, namely, demographic information, knowledge about breast cancer and breast cancer screening practices. A Likert scale was used to gather information on attitudes toward breast cancer. The questionnaire was translated into the local African language (Venda) for easier comprehension by the participants. This was done by Venda educator in the Department of African Languages at the University. There was a back translation by another language educator in order to ensure English and Tshivenda equivalence. One hundred and fifty questionnaires were self-administered and were collected after three days from the respective households, with a response rate of 100%.
Data analysis
Statistical analysis was used to summarise the results of the study and to reduce, organise and give meaning to the data (Burns & Grove 2005 :43) obtained from the 150 completed questionnaires. A statistician analysed the data by using the Predictive Analytics Software (PASW) version 18.0 (SPSS Inc., Chicago 2009) and Microsoft ® Excel was used to draw some charts. Descriptive statistics were used to describe the data and the Chi-square test was used to describe relationships amongst variables, with a significance level of p < 0.00.
Ethical considerations
Ethical clearance was obtained from the University of Venda Ethics Committee (project SHS/11/PH/004). Authorisation and approval for conducting the study were requested from Makwarani Royal Committee. The researchers ensured protection of the rights of the participants by informing the participants that their participation was voluntary, they would remain anonymous, they were free to withdraw from the study at any time without penalty and that all information would be kept confidential. Each participant signed a written consent; even those with no formal education were able to write down their names.
Trustworthiness
Validity and reliability.
Content validity concerns the degree to which the instrument has an appropriate sample of items for the construct being measured (Polit & Beck 2008 :458). The questionnaire was scrutinised for relevance by peers in the field of oncology nursing; construct validity was ensured by aligning the content of the instrument based on literature related to oncology and reproductive health. Reliability refers to the consistency and stability with which the instrument measures a target attribute, if administered to different individuals at different times (Polit & Beck 2008 :455). Reliability of the research instrument evaluated by use of a pre-test. Fifteen questionnaires were distributed to women who were not part of the study in order to test the stability of the instrument, including clarity of the questions. The questionnaire addressed the respondents in their own language so as to improve understanding.
Socio-demographic characteristics
The score for the participants’ mean age was 1.6, with a range of 30 years to 65 years. Forty (26.7%) of the participants had no formal education, whilst only 26 (17.3%) had a tertiary level of education, 47 (31.3%) had a secondary education and 37 (24.7%) had obtained a primary-level education. Twenty-six (17.3%) were professional workers whilst 50 (29.3%) were casual labourers and pensioners.
Knowledge on breast cancer and source of information
One hundred and four (69%) of the women had never heard of breast cancer, whilst only 46 (31%) had heard of breast cancer, with their source of information being mainly from the media ( n = 26; 56%) as opposed to coming from a health facility ( n = 6; 14%).
Symptoms of breast cancer
Swelling of the breast or lump was cited by the majority of participants ( n = 90; 60%), followed by abscess ( n = 25; 17%) and accumulation of fluid in the breast ( n = 15; 10%). Nipple changes ( n = 10; 7%), skin changes ( n = 5; 3.3%) and swelling of the breast or armpit ( n = 5; 3%) were least known.
Risk factors for breast cancer
The responses to the list of risk factors for breast cancer were as follows: high fat intake ( n = 32; 21.3%), lack of exercise ( n = 30; 20.0%) and overweight ( n = 22; 14.7%). Others, in order of percentage, were: hormonal changes ( n = 19; 12.8%), heredity and radiation (both n = 14; 9.3%), drinking alcohol ( n = 13; 8.7%) and smoking ( n = 6; 4.0%).
Knowledge of breast cancer diagnostic methods
Eight (5.3%) of the participants had heard about breast diagnostic methods, whereas the majority ( n = 142; 95.0%) of the participants never heard about breast diagnostic methods. Amongst the eight (5.3%) participants who said they had heard about breast cancer diagnostic methods, four (2.6%) knew of clinical breast examination, three (2%) knew of BSE and one (0.6%) mammography. Furthermore, 94 (62.5%) of the participants did not know the appropriate time to perform BSE, whereas 56 (37.5%) knew that BSE should be performed seven days after menstruation.
Attitudes toward treatment and early detection
Almost half of the women ( n = 75; 50%) disagreed and 35 (23.3%) strongly disagreed that breast cancer treatment worsens the condition, whereas 33 (22.0%) agreed and 7 (4.7%) strongly agreed that the treatment worsens the condition. Seventy (46.7%) of the women agreed that the possibility of a cure for breast cancer is determined by early detection and 38 (25.3%) strongly agreed with this statement, whereas 30 (20.0%) disagreed and 12 (8%) strongly disagreed that the possibility of a cure is not determined by early detection.
Practices of breast cancer screening and behaviour
One hundred and forty-two (94.7%) of the women said that they had never performed breast cancer diagnostic checks and only eight (6.3%) had practised one of the methods during their lifetime. Regarding health-seeking behaviour, 124 (82.7%) reported that if they noticed any change in their breast, they would consult the medical doctor, 21 (14.0%) said that they would consult the traditional doctor and only five (3.3%) would consult a prophet.
Table 1 provides the demographic profile for the study ( N = 150) and describes the age distribution, level of education and occupational status. The items in this section attempted to obtain personal information about the participants in order to contextualise the responses concerning their knowledge, attitudes and practices regarding breast cancer.
Demographic characteristics.
The strongest risk factor for breast cancer is age. A woman's risk of developing this disease increases as she gets older, however those who are at risk should be made aware of personal risk factors of developing breast cancer. Similarly, the participants in the older age group displayed low levels of knowledge regarding screening practices. Allam and Abd Elaziz ( 2012 :196) concur with the findings that younger subjects in Egypt had a higher level of knowledge about breast cancer compared with older subjects. When older women demonstrate poor knowledge of breast cancer, it is of great concern as the risk of cancer increases with age. It is at this age that women should be more proactive in their health promotion behaviours. Women in the menopausal stage are at risk as a result of the high levels of hormones associated with breast cancer.
Employment status determines one's ability to access healthcare, as well as determining other factors in terms of cost, proximity and acceptance of medical services. Occupation and education show a positive association with breast cancer screening methods; women of intermediate and high occupational class are more likely to use screening methods as compared with those in the lowest class (Damiani et al . 2012 :2). Socioeconomic status may determine the variety of life styles and dietary practices that might affect breast cancer risk, as well as possibly influencing the health-seeking behaviour of the participants. The majority of women in the study were of low socioeconomic status which is linked to decreased rates of breast cancer screening, greater probability for late-stage diagnosis, receipt of inadequate and disparate treatment and higher mortality from breast cancer. Poverty is associated with poorer breast cancer outcomes worldwide and only 26 (17.3%) of the participants were working professionally. The possibilities of these women going for screening is limited if the information is not available or services are limited. This might also increase their mortality rate as they might also present late for screening, resulting in poor health outcomes.
Education is also a marker for specific traits such as intelligence, acquisition of adaptive skills, or awareness of risky health behaviours; it improves our understanding of the causes and natural history of some diseases. The Chi-square test was carried out to determine the relationship between level of education and breast cancer screening practices. The mean score for the level of education was 1.4, with a p -value of < 0.00, which suggests that those who are educated were likely to use breast-screening methods, unlike the uneducated. Education might influence the participants’ knowledge of breast cancer as well as the methods of breast cancer early detection. Alwan et al . ( 2012 :343) report that breast-screening practices appear to be correlated with the higher level of education and healthcare services offered in those regions as compared with the developing world. However, Reyes-Ortiz et al . ( 2007 :392), surprisingly, reported that a few college women were aware of the procedures but did not practise them. Similar findings were reported by Khokhar ( 2009 :248), where teachers in Nigeria were aware of breast-screening practices but none of them knew that clinical breast examination (CBE) and mammography should be done annually from the age of 40 years; BSE was not performed regularly by the participants in the study. In this study, women lacked adequate information on breast cancer, symptoms and breast-screening practices. Education plays a vital part in modifying lifestyle behaviour, however health education and promotion are important in reinforcing breast cancer screening practices through community awareness campaigns so as to empower women to take a proactive approach to their health.
Knowledge is equally important as it could influence health-seeking behaviour and change attitudes toward breast cancer. McMullin et al . ( 2008 :33), in their study conducted in United States amongst a Togan population sample, reported that 35 of the 48 participants lacked knowledge of exactly what cancer is, although they knew that the disease was linked to death. Some compared it with HIV, saying it is a disease for which there is no cure. This understanding of cancer as a death sentence is often informed by cancer experiences on the part of family and friends. Another study conducted in South Nigeria reported that the mean knowledge score was about 42.3% and only 21.4% of the participants were aware of breast cancer (Omotara et al . 2012 :2). This might be attributed to ineffective awareness campaigns by health workers, as they should be helping women to develop healthy lifestyle practices and promote breast-screening practices. The main source of information to the participants was the media (56%), whilst clinics and/or hospitals provided 14%. This suggests that hospitals and clinics are not doing enough to make information readily accessible to the communities and, as such, women rely on media such as radio and television which do not address health issues in a constant manner. The media coverage is sporadic and health promotion issues are only highlighted during awareness days or weeks, which is not effective. Thus, health education should be intensified so as to enlighten women of all age groups on the particular risks of breast cancer. Omatara et al . ( 2012 :2) are also of the opinion that health workers should endeavour to educate women on breast awareness during regular clinic visits for other health issues in order to increase the level of awareness of breast cancer in the community. Most women either lack knowledge or are ignorant about breast cancer; they usually not perceive themselves as being susceptible or at risk of breast cancer, especially amongst black communities. They see cancers as being diseases that affect other racial groups.
Black women historically have had fewer incidences of breast cancer as compared with white women and there are still those who are unaware that, as a result of lifestyle changes, they are at risk of developing breast cancer. They need to understand how to detect the disease early – when they feel the lump they should not ignore it. Figure 1 depicts the low levels of knowledge regarding symptoms, such as accumulation of fluid in the breast, nipple changes, skin changes and swelling of the breast or armpit. The findings of this study contrast with studies in Botswana and Brazil. Tieng'O et al . ( 2011 :3524) and Marinho et al . ( 2008 :25) reported that 54.1% and 42.4% of participants, respectively, could identify that nipple discharge and skin changes are symptoms of breast cancer. Insufficient knowledge about the signs and symptoms of breast cancer might lead to poor performances of breast diagnostic checks. Knowledge about the symptoms of breast cancer appears to influence the participants’ screening behaviour. It can thus be concluded that knowledge is a basic component that may help the participants to perform breast cancer diagnostic checks for early breast cancer detection. Poorer knowledge regarding the identification of symptoms of breast cancer is associated with late detection and poor survival.

Responses regarding symptoms of breast cancer.
Most women do not perceive themselves as being at risk for breast cancer as the information regarding risk factors is not readily available in rural areas. Figure 2 indicates that risk factors such as smoking, genetics, hormones and obesity were not known, although obesity is common amongst black women. The findings are consistent with those of Al-Dubai et al . ( 2011 :2536) who also reported poor understanding of risk factors and unsatisfactory responses amongst Malaysian women, where nulliparity, delivery at older than 30 years, big breasts, contraceptive pills and menarche before age were not known to be risk factors. Yan ( 2009 :100) also found that breastfeeding, age of menopause and menarche were not recognised as risk factors; these findings may lead to underestimation of the importance of regular screening by older women if they believe that it is the younger age group that is most at risk. The results of the survey suggest the need for educational programmes to improve current knowledge of cancer. Knowing the risk factors for breast cancer might help the participants to adopt a healthy lifestyle of proper nutrition and exercise, avoidance of unnecessary exposure to radiation and going for genetic testing if at risk, as well as avoiding such practices such as smoking and drinking in order to reduce the incidence of breast cancer morbidity and mortality (Hadi et al . 2010 :33). Poor knowledge of risk factors and knowledge of their relative risk of developing breast cancer also explains why they do not engage in health-promotion behaviour or breast-screening practices.

Risk factors for breast cancer.
Poor knowledge regarding breast cancer screening methods is responsible for late detection of the disease. Eight (5.3%) of the participants had heard about breast diagnostic methods, whereas the majority ( n = 142; 95.0%) of the participants had never heard about breast diagnostic methods. Knowledge about diagnostic methods is highly beneficial to the participants as it assists women regarding when and how to perform breast cancer screening for early detection in order to reduce late presentation of the disease that might complicate treatment of breast cancer. Furthermore, 62.5% of the participants did not know the appropriate time to perform BSE, whereas 37.5% knew that BSE should be performed seven days after menstruation. Kanaga et al . ( 2011 :1967) concur that the low rates of BSE, CBE and mammography were also of concern amongst Malaysian women and suggested that increased awareness and subsidised mammography be given to the general population. The Minister of Health in South Africa also intends to adopt the National Health Insurance so as to increase accessibility of such diagnostic screening tests. Lack of social support can influence the choice of screening amongst women.
One hundred and thirty-one (88%) of the participants in this study had never had a mammogram, whilst one (0.6%) had experienced a mammogram in the past and knew that it should be performed once every two years. This is attributable to the fact that mammography is not available in public hospitals in the region of Vhembe and there are no large-scale awareness campaigns regarding its existence as the majority cannot afford it. Khokhar ( 2009 :249) also indicated, in a study amongst Indian teachers, that mammography is not performed as a routine screening procedure, but is mostly used for those with symptoms or who are at high risk for the disease. Lack of information and knowledge about breast cancer screening practices influences women to miss early detection and treatment opportunities. Screening for early detection and diagnosis of diseases is an important public health principle (Tieng'O et al . 2011 :3517). Early detection of breast cancer plays the leading role in reducing mortality rates; health education programmes should make women aware of these screening tests, so that they can present themselves early for diagnosis and treatment in order to overcome the burden of the disease. Nurses should emphasise the potential benefits when raising awareness.
Table 2 shows that the participants’ attitudes toward treatment and early detection was positive, however a minority (4.7%) strongly agreed that the treatment worsens the condition and there are still some beliefs that the possibility of a cure is not determined by early detection. Khanjani et al . ( 2012 :181) also reported relatively poor knowledge and behaviour amongst female healthcare workers in Tehran. The main reasons given for not performing screening methods were: not feeling a problem; not believing it is necessary; and lack of knowledge. According to the results of the study, being knowledgeable about breast cancer screening methods and when to perform breast cancer diagnostic methods might promote positive health outcomes. Participants who have adequate knowledge regarding how to perform simple life-saving techniques such as BSE, CBE and mammography might be more likely to present at the early stages of breast cancer.
Attitudes of the women toward breast cancer.
The participants’ attitudes toward treatment and early detection might be influenced by knowledge of breast diagnostic methods and by the participants’ choices on when to seek medical help. Religion, education, occupation and culture might influence the attitudes of the participants regarding who should examine their breast during CBE.
The majority of the women (82.7%) reported that if they noticed any change in their breast, they would consult the medical doctor, whilst 14.0% said that they would consult the traditional doctor and 3.3% would consult the prophet. The issue of religious and cultural belief might play a significant role in the health-seeking behaviour of the participants in this study. McMullin et al . ( 2008 :35) reported that native Hawaiians were ‘often offended and resisted participating in research because of the primacy given to the scientific medical model as opposed to lay knowledge and cultural protocols’. This denigration took the form of classifying lay knowledge as myths and misconceptions instead of learning the cultural meaning of cancer in populations. Ethnicity, cultural factors, enabling factors such as having a regular physician to visit, health insurance covering the screening, family and social/family support factors are attributed to health-seeking behaviour. Culture plays a pivotal role in breast cancer screening; amongst black women it can be a barrier as most may not engage in screening programmes because of fear, anxiety and worry as compared to white women, which would prevent them from disclosing the illness or seeking therapy. Social support is important in increasing help-seeking behaviours because having a family or friend can increase the likelihood of being screened.
One hundred and forty-two (94.7%) of the women said that they had never performed breast cancer diagnostic checks before. The results showed no breast cancer screening programme campaigns had ever been conducted in Makwarani Community and participants did not even know how often screening be done. Similar findings were reported by Ojikutu and Adetifa ( 2009 :183), who indicated that the majority (93.3%) of study participants preferred reporting at the hospital or any other health facility within their neighbourhood, whilst only 5.9% preferred to seek the intervention of traditional medical services. This is supported by Mugivhi, Maree and Wright ( 2009 :43), who asserted that most women prefer biomedical treatment. Religious beliefs are particularly dominant amongst black women with a passionate confidence in God, but their mindsets are somehow stuck in attitudes and beliefs such as fatalism, magic, witchcraft and demons. Although Christianity and Islam have replaced traditional religions, the thoughts of the people about life and their attitude to it are still shaped by the old worldview (Akhigbe & Akhigbe 2012 :74). Cultural norms and beliefs can act as a barrier to breast cancer treatment. It is therefore important to incorporate culture into interventions designed to increase cancer screening. If we are to develop materials for educational intervention, they should be culturally sensitive as the goal of such a drive would be to increase breast cancer knowledge, decrease cancer fatalism and improve participation in breast cancer screening amongst women.
Limitations
The research was conducted in one municipality, so the results can therefore not be generalised to others. The results of this research may also not be generalised to larger groups, as they apply only to the rural women of Makwarani who participated in the study.
Recommendations
There is a need for educational intervention to enhance knowledge about breast cancer, its risk factors and symptoms as well as breast diagnostic examination. The health awareness campaigns should be initiated at primary health level and community home-based carers within communities should be included in these campaigns so as to disseminate information.
Breast cancer information should be accessible to everyone, particularly from the health information centres, through a visible display of posters, information leaflets and health education video clips or recorded health talks whilst clients are awaiting consultations in reception areas.
Additional research is required to change the attitudes of women toward breast cancer and to investigate the various health belief models, as there are still women who believe in the traditional and spiritual dimensions of health and delay seeking help by going to a ‘special doctor’ as they do not understand the concept of speciality in the field of medicine.
Women must be encouraged to practise breast cancer diagnostic examinations regularly. BSE is an economical, simple and basic procedure that can be integrated into all programmes of reproductive health such as adolescent health, pregnancy, post-partum and menopausal women.
The participants’ level of knowledge about breast cancer was relatively low since the majority (69%) of the participants had never even heard of breast cancer before. This then would make them miss out on the practice of breast cancer screening methods and might also increase their chance of being diagnosed with breast cancer only at the later stages. A negative attitude was found amongst the participants as others still preferred going to traditional and spiritual healers for treatment and did not think that they have personal risk factors.
Poor breast cancer screening was reported in the community since all the participants reported that no screening had ever been conducted in the community, which indicates that dissemination of health information is not working effectively since much information is acquired from the media rather than clinics and/or hospitals. The participants’ practices of breast cancer diagnostic methods were relatively low because only 5.3% had ever practised BSE or CBE or had a mammogram. Education about the importance of early detection in decreasing mortality rates might be of value in raising awareness about the various methods of early detection of breast cancer.
Acknowledgements
The authors are grateful to the University Research and Innovation Department for funding of this project.
Competing interests
The authors declare that they have no financial or personal relationship(s) that may have inappropriately influenced them in writing this article.
Authors’ contributions
D.U.R. (University of Venda) is the author of the article. C.T.R. (University of Venda) assisted in the literature review and T.M.M. (University of Venda) provided the methodology.
- Akhigbe A & Akhigbe K., 2012, Effects of health belief and cancer fatalism on the practice of breast cancer screening among Nigerian Women , viewed January 2013, from www.intechopen.co/books/mammography-recent-advances/effects-of-health-belief-and-cancer-fatalism-on-the-practice-of-breast-cancer-screening-among-nigeri
- Akpinar Y.Y., Baykan Z., Naçar M., Gün I. & Çetinkaya F., 2011, ‘ Knowledge, attitude about breast cancer and practice among female health care professionals: A study from Turkey ’, Asian Pacific Journal of Cancer Prevention 12 ( 11 ), 3063–3068. [ PubMed ] [ Google Scholar ]
- Al-Dubai S.A., Qureshi A.M., Saif-Ali R., Ganasegeran K, Alwan M.R. & Hadi J.I., 2011, ‘ Awareness and knowledge of breast cancer and mammography among a group of Malaysian women in Shah Alam ’, Asian Pacific Journal of Cancer Prevention 12 ( 10 ), 2531–2538. [ PubMed ] [ Google Scholar ]
- Allam M.F. & Abd Elaziz K.M., 2012, ‘ Evaluation of the level of knowledge of Egyptian women of breast cancer and its risk factors: A cross sectional study ’, Journal of Preventive Medicine and Hygiene 53 ( 4 ), 195–198. [ PubMed ] [ Google Scholar ]
- Alwan N.A., Al-Attar W.M., Eliessa R.A., Madfaie Z.A. & Tawfeeq F.N., 2012, ‘ Knowledge, attitude and practice regarding breast cancer and breast self-examination among sample of the educated population in Iraq ’, Eastern Mediterranean Health Journal 18 ( 4 ), 337–345. [ PubMed ] [ Google Scholar ]
- Burns N. & Grove S.K., 2005, The practice of nursing research: Conduct, critique and utilization , 5th edn, Saunders, Philadelphia. [ Google Scholar ]
- Burns N. & Grove S.K., 2007, Understanding nursing research: Building an evidence based practice , 4th edn, Saunders Elsevier, St Louis. [ Google Scholar ]
- Damiani G., Federico B., Basso D., Ronconi A., Bianchi C.B., Anzelotti G.M.. et al , 2012, ‘ Socioeconomic disparities in the uptake of breast and cervical cancer screening in Italy: A cross sectional study ’, BMC Public Health 2012, 12 , 99 10.1186/1471-2458-12-99 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dow Meneses K. & Yarbro C.H., 2007, ‘ Cultural perspectives of international breast health and breast cancer education ’, Journal of Nursing Scholarship 39 ( 2 ), 105–112. 10.1111/j.1547-5069.2007.00154.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hadi M.A., Hassali M.A., Shafie A.A. & Awaisu A., 2010, ‘ Evaluation of breast cancer awareness among female university students in Malaysia ’, Pharmacy Practice 8 ( 1 ), 29–34. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kanaga K.C., Nithiya J. & Noor Shatirah M.F., 2011, ‘ Awareness of breast cancer and screening procedures among Malaysian women ’, Asian Pacific Journal of Cancer Prevention 12 ( 8 ), 1965–1967. [ PubMed ] [ Google Scholar ]
- Khanjani N., Noori A. & Rostami F., 2012, ‘ The knowledge and practice of breast cancer screening among women in Kerman, Iran ’, Al Ameen Journal of Medical Science 5 ( 2 ), 177–182. [ Google Scholar ]
- Khokhar A., 2009, ‘ Level of awareness regarding breast cancer and its screening amongst Indian teachers ’, Asian Pacific Journal of Cancer Prevention 10 ( 2 ), 247–250. [ PubMed ] [ Google Scholar ]
- Lemlem S.B., Sinishaw W., Hailu M., Abebe M. & Aregay A., 2013, ‘ Assessment of knowledge of breast cancer and screening methods among nurses in University Hospital in Addis Ababa, Ethiopia, 2011 ’, International Scholarly Research Notices 2013(2013), Article ID 470981, 8 pages.
- LoBiondo-Wood G. & Haber J., 2006, Nursing research: Methods and critical appraisal for evidence based practice , 6th edn, Mosby, St Louis. [ Google Scholar ]
- Marinho L.A.B., Cecatti J.G., Osis M.J.D. & Gurgel M.S.C., 2008, ‘ Knowledge, attitude and practice of mammography among women users of public health services ’, Revista de Saúde Pública 42 ( 2 ), 21–31. 10.1590/S0034-89102008005000006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McMullin J.M., Taumoepeau L., Talakai M., Kivalu F. & Hubbell M.D., 2008, ‘ Tongan perceptions of cancer ’, Cancer Detection and Prevention 32 ( Suppl 1 ), 29–36. 10.1016/j.cdp.2007.12.004 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mugivhi N.H., Maree J.E. & Wright S.C.D., 2009, ‘ Rural women's knowledge of prevention and care related to breast cancer ’, Curationis 32 ( 2 ), 38–45. 10.4102/curationis.v32i2.928 [ CrossRef ] [ Google Scholar ]
- Ojikutu R.K. & Adetifa F.A., 2009, Psycho-social analysis of breast cancer awareness in Lagos state, Nigeria , International Journal of Academic Research 1 ( 2 ), 181–187. [ Google Scholar ]
- Omotara B., Yahya S., Amodu M. & Bimba J., 2012, ‘ Awareness, attitude and practice of rural women regarding breast cancer in Northeast Nigeria ’, Journal of Community Medicine & Health Education 2 ( 5 ), 4 pages. [ Google Scholar ]
- Parkins D.M. & Fernández L.M., 2006, ‘ Use of statistics to assess the global burden of breast cancer ’, The Breast Journa 12 ( Suppl 1 ), S70–S80. 10.1111/j.1075-122X.2006.00205.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Polit D.F. & Beck C.T., 2008, Nursing research: generating and assessing evidence for nursing practice , 8th edn, Lippincott Williams & Wilkins, Philadelphia, PA. [ Google Scholar ]
- Reyes-Ortiz C.A., Camacho M.E., Amador L.F., Velez L.F., Ottenbacher K.J. & Markides K.S., 2007, ‘ The impact of education and literacy levels on cancer screening among older Latin American and Caribbean adults ’, Cancer Control 14 ( 4 ), 388–395. [ PubMed ] [ Google Scholar ]
- Shepherd J.H. & Mclnerney P.A., 2006, ‘ Knowledge of breast cancer in women in Sierra Leone ’, Curationis 29 ( 3 ), 70–77. 10.4102/curationis.v29i3.1105 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shepherd J.H. & Mclnerney P.A., 2007, ‘ Knowledge of breast-self examination in women in Sierra Leone ’, Curationis 30 ( 4 ), 38–44. 10.4102/curationis.v30i4.1115 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tieng'O J.G., Pengpid S., Skaal L. & Peltzer K., 2011, ‘ Knowledge, attitude and practice of breast cancer examination among women attending a health facility in Gaborone, Botswana ’, Gender and Behaviour 9 ( 1 ), 3513–3527. 10.4314/gab.v9i1.67455 [ CrossRef ] [ Google Scholar ]
- Yan Y.Y., 2009, ‘ Breast cancer: Knowledge and perceptions of Chinese women in Hong Kong ’, Global Journal of Health Science 1 ( 2 ), 97–105. 10.5539/gjhs.v1n2p97 [ CrossRef ] [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
new case diagnosed every 18 seconds; additionally, 626,679 women with breast cancer died. The global. incidence of breast cancer has been rising wi th annual. increases of 3.1%, beginning with ...
Introduction. Breast cancer is the most common cancer affecting 25.2% of women and is also the second leading cause of cancer-related deaths among women [].Almost half of breast cancer cases and 60% of breast cancer-related deaths are estimated to occur in middle-and-low-income countries [].Globally, the devastating effects on women diagnosed with breast cancer are appalling [].
Breast cancer (BC) is the most frequently diagnosed cancer in women worldwide with more than 2 million new cases in 2020. Its incidence and death rates have increased over the last three decades due to the change in risk factor profiles, better cancer registration, and cancer detection. The number of risk factors of BC is significant and ...
Introduction. Breast cancer (BC) was allocated 11.7% of all kinds of cancers in 2020.[] To date, the new cases of the disease were beyond two million, forecasted to reach more than 3 million cases with more than one million deaths by 2040.[2,3]BC was imposed a considerable economic burden on countries as well as public health problems[4,5] while it can be prevented by early detection ...
Breast cancer is a complex topic encompassing risk factors, treatment options, survivorship, and advocacy. Crafting an effective thesis statement on breast cancer requires thorough research and understanding of the subject. Seeking expert assistance can help those struggling to write a breast cancer thesis statement craft a well-researched, compelling thesis that meets academic standards.
In the United States, 13% of women are diagnosed with invasive breast cancer in their lifetime. and 6% of breast cancer patients have metastatic disease at initial diagnosis [1]. Moreover, nearly. 30% of women with early stage breast cancer will develop metastatic disease [2]. About 42,000.
1.2.1 Definition. Breast cancer is a malignant tumor arising from epithelial cells of glandular milk ducts or lobules of the breast [16]. Breast carcinoma is classified as either non-invasive (carcinoma in situ) or invasive, depending on whether or not the tumor has started to grow outside the basal membrane.
Breast cancer is the second most common cancer in women, surpassed only by skin cancer (National Institute of Health, 2019). In 2019, approximately 268,000 women were diagnosed with breast cancer (National Cancer Institute, 2020). Approximately seven out of a hundred women will develop breast cancer before the age of seventy (Centers for Disease
Breast Cancer Outline for Research Paper. Now that your topic and thesis are in hand, you can begin the process of creating an outline. Think of this as a foundation for your completed paper. It will help you decide on the structure of your paper, and choose the most important points to support your research paper.
This thesis provides a report on a study of four women's experience of breast cancer, asking them to tell me their stories of cancer and reflect upon their experiences. Over the course of this thesis, I will hope to develop a theoretical framework from which to answer the following questions:
17 essay samples found. Breast cancer is a type of cancer that develops from breast tissue. Essays on this topic could explore the causes, diagnosis, treatment, and prevention of breast cancer. Additionally, discussions might delve into the psychological and social impact of breast cancer on patients and their families, the ongoing research ...
3.3 Breast Cancer worldwide. Breast cancer is the most common type of cancer in women around the globe. It affects women from low, middle and high-income countries (Rohani, Abedi, Omranipour, & Langius-Eklöf, 2015, 2). Breast cancer prevalence has increased within the last few years in middle- and low-income countries.
Western countries breast cancer represents of 25% to 30% of the total incidence of cancers in women and is responsible for 15% to 18 % of mortality (Emaus, 2009). Worldwide, 1.301.867 of new cases of breast cancer is registered and deaths were 464.454 fallowed by other types of cancer (WHO, 2008).
new and more effective treatments for breast cancer have been found. In lots of cases, breast cancer is curable and the most important factor for a full recovery is an early detection. Information collected in this thesis will help women to understand how to prevent and treat breast cancer at young age.
Collectively, this work contributes novel findings about the breast cancer immune microenvironment that may aid in precision medicine approaches for breast cancer prevention and intervention, and highlights the importance of diversity in impactful and equitable clinical research. Date of publication. 2022; Keyword. Pathology; breast cancer ...
breast[Porter, 1998] ridding the body of this excess of black bile involved venesection, purgation, cupping, leaching, enemas and bizarre diets (many "alternative" treatments of breast cancer to this day are in fact a form of neo-galenism). In the mid 19th Century the humoral theory of breast cancer was overturned by a mechanistic model which
Defining breast cancer in men and women 1. The difference in men awareness 2. The difference in women and its awareness 3. How breast cancer is formed B. Dealing with a chronic illness and its awareness 1. Challenges for men 2. Challenges for women 3. The differences in men and women III. Historical Background: Where the lack of Awareness and ...
A positive family history of breast cancer in a first-degree relative is the most commonly known risk factor for the disease . Women with a family history of breast cancer in a mother or sister have up to a 3-fold increase in the risk of developing breast cancer . In this present study, about 14% of the participants had a positive family ...
To determine the impact of breast conservation on quality of life and identify treatment-related and other demographic factors associated with post-breast cancer treatment quality of life. A ...
GENETICS. Genetic inheritance is an infrequent but not the main cause of breast cancer. The consensus is that breast cancer susceptibility or cancer predisposition genes are associated with only 4%-8% of breast cancer cases.5-7 It is apparent therefore that 92%-96% of cases are sporadic. The risk of developing disease for carriers of germline mutations has been estimated at 54% by age 60 ...
Functions and regulation of Ron receptor tyrosine kinase in human pancreatic cancer and its therapeutic applications, Yi Zou. Theses/Dissertations from 2011 PDF. Coordinate detection of new targets and small molecules for cancer therapy, Kurt Fisher. PDF. The role of c-Myc in pancreatic cancer initiation and progression, Wan-Chi Lin. PDF
Obesity status, adjusted for MetS score, was significantly associated with more good prognosis, ER-positive, PR-positive cancers (p < .001), more total breast cancers (p < .001), and more deaths after breast cancer (p < .001), with higher breast cancer mortality only in women with severe obesity (BMI, ≥35 kg/m 2; p < .001). Conclusions
Introduction. Breast cancer is considered a multifactorial disease and the most common cancer in women worldwide [ 1, 2] with approximately 30% of all female cancers [ 3, 4] (i.e. 1.5 million women are diagnosed with breast cancer each year, and 500,000 women die from this disease in the world).Over the past 30 years, this disease has increased, while the death rate has decreased.
The SUCCESS C trial. Data was obtained from the SUCCESS C trial, an open-label, multicenter, randomized controlled study that examined the effect of two different chemotherapy regimens (n = 3642) as well as the effect of a comprehensive lifestyle intervention program on disease-free survival in women with newly diagnosed HER2/neu-negative intermediate-risk to high-risk breast cancer [17,18,19].
Cancer-related fatigue (CRF) has been increasingly recognized as an important symptom during and after treatment of cancer, impacting physical, mental, and emotional functions. 1 CRF is a prevalent symptom among survivors of the most common types of cancer, including breast, lung, and colon cancer. 2,3 It is a distressing symptom 3 and one of ...
Phase 1b/2 Clinical Study Results. Enrollment. As of the data cut-off of March 13, 2024, 50 patients with recurrent, locally advanced or metastatic ER+/HER2- breast cancer with at least four weeks ...
Problem statement. Breast cancer is the most common cancer in South Africa and it is increasing in incidence, with large numbers of women with breast cancer being found in rural areas. ... Akhigbe A & Akhigbe K., 2012, Effects of health belief and cancer fatalism on the practice of breast cancer screening among Nigerian Women, viewed January ...