
Best Nursing Research Topics for Students
What is a nursing research paper.
- What They Include
- Choosing a Topic
- Best Nursing Research Topics
- Research Paper Writing Tips

Writing a research paper is a massive task that involves careful organization, critical analysis, and a lot of time. Some nursing students are natural writers, while others struggle to select a nursing research topic, let alone write about it.
If you're a nursing student who dreads writing research papers, this article may help ease your anxiety. We'll cover everything you need to know about writing nursing school research papers and the top topics for nursing research.
Continue reading to make your paper-writing jitters a thing of the past.
A nursing research paper is a work of academic writing composed by a nurse or nursing student. The paper may present information on a specific topic or answer a question.
During LPN/LVN and RN programs, most papers you write focus on learning to use research databases, evaluate appropriate resources, and format your writing with APA style. You'll then synthesize your research information to answer a question or analyze a topic.
BSN , MSN , Ph.D., and DNP programs also write nursing research papers. Students in these programs may also participate in conducting original research studies.
Writing papers during your academic program improves and develops many skills, including the ability to:
- Select nursing topics for research
- Conduct effective research
- Analyze published academic literature
- Format and cite sources
- Synthesize data
- Organize and articulate findings
About Nursing Research Papers
When do nursing students write research papers.
You may need to write a research paper for any of the nursing courses you take. Research papers help develop critical thinking and communication skills. They allow you to learn how to conduct research and critically review publications.
That said, not every class will require in-depth, 10-20-page papers. The more advanced your degree path, the more you can expect to write and conduct research. If you're in an associate or bachelor's program, you'll probably write a few papers each semester or term.
Do Nursing Students Conduct Original Research?
Most of the time, you won't be designing, conducting, and evaluating new research. Instead, your projects will focus on learning the research process and the scientific method. You'll achieve these objectives by evaluating existing nursing literature and sources and defending a thesis.
However, many nursing faculty members do conduct original research. So, you may get opportunities to participate in, and publish, research articles.
Example Research Project Scenario:
In your maternal child nursing class, the professor assigns the class a research paper regarding developmentally appropriate nursing interventions for the pediatric population. While that may sound specific, you have almost endless opportunities to narrow down the focus of your writing.
You could choose pain intervention measures in toddlers. Conversely, you can research the effects of prolonged hospitalization on adolescents' social-emotional development.
What Does a Nursing Research Paper Include?
Your professor should provide a thorough guideline of the scope of the paper. In general, an undergraduate nursing research paper will consist of:
Introduction : A brief overview of the research question/thesis statement your paper will discuss. You can include why the topic is relevant.
Body : This section presents your research findings and allows you to synthesize the information and data you collected. You'll have a chance to articulate your evaluation and answer your research question. The length of this section depends on your assignment.
Conclusion : A brief review of the information and analysis you presented throughout the body of the paper. This section is a recap of your paper and another chance to reassert your thesis.
The best advice is to follow your instructor's rubric and guidelines. Remember to ask for help whenever needed, and avoid overcomplicating the assignment!
How to Choose a Nursing Research Topic
The sheer volume of prospective nursing research topics can become overwhelming for students. Additionally, you may get the misconception that all the 'good' research ideas are exhausted. However, a personal approach may help you narrow down a research topic and find a unique angle.
Writing your research paper about a topic you value or connect with makes the task easier. Additionally, you should consider the material's breadth. Topics with plenty of existing literature will make developing a research question and thesis smoother.
Finally, feel free to shift gears if necessary, especially if you're still early in the research process. If you start down one path and have trouble finding published information, ask your professor if you can choose another topic.
The Best Research Topics for Nursing Students
You have endless subject choices for nursing research papers. This non-exhaustive list just scratches the surface of some of the best nursing research topics.
1. Clinical Nursing Research Topics
- Analyze the use of telehealth/virtual nursing to reduce inpatient nurse duties.
- Discuss the impact of evidence-based respiratory interventions on patient outcomes in critical care settings.
- Explore the effectiveness of pain management protocols in pediatric patients.
2. Community Health Nursing Research Topics
- Assess the impact of nurse-led diabetes education in Type II Diabetics.
- Analyze the relationship between socioeconomic status and access to healthcare services.
3. Nurse Education Research Topics
- Review the effectiveness of simulation-based learning to improve nursing students' clinical skills.
- Identify methods that best prepare pre-licensure students for clinical practice.
- Investigate factors that influence nurses to pursue advanced degrees.
- Evaluate education methods that enhance cultural competence among nurses.
- Describe the role of mindfulness interventions in reducing stress and burnout among nurses.
4. Mental Health Nursing Research Topics
- Explore patient outcomes related to nurse staffing levels in acute behavioral health settings.
- Assess the effectiveness of mental health education among emergency room nurses .
- Explore de-escalation techniques that result in improved patient outcomes.
- Review the effectiveness of therapeutic communication in improving patient outcomes.
5. Pediatric Nursing Research Topics
- Assess the impact of parental involvement in pediatric asthma treatment adherence.
- Explore challenges related to chronic illness management in pediatric patients.
- Review the role of play therapy and other therapeutic interventions that alleviate anxiety among hospitalized children.
6. The Nursing Profession Research Topics
- Analyze the effects of short staffing on nurse burnout .
- Evaluate factors that facilitate resiliency among nursing professionals.
- Examine predictors of nurse dissatisfaction and burnout.
- Posit how nursing theories influence modern nursing practice.
Tips for Writing a Nursing Research Paper
The best nursing research advice we can provide is to follow your professor's rubric and instructions. However, here are a few study tips for nursing students to make paper writing less painful:
Avoid procrastination: Everyone says it, but few follow this advice. You can significantly lower your stress levels if you avoid procrastinating and start working on your project immediately.
Plan Ahead: Break down the writing process into smaller sections, especially if it seems overwhelming. Give yourself time for each step in the process.
Research: Use your resources and ask for help from the librarian or instructor. The rest should come together quickly once you find high-quality studies to analyze.
Outline: Create an outline to help you organize your thoughts. Then, you can plug in information throughout the research process.
Clear Language: Use plain language as much as possible to get your point across. Jargon is inevitable when writing academic nursing papers, but keep it to a minimum.
Cite Properly: Accurately cite all sources using the appropriate citation style. Nursing research papers will almost always implement APA style. Check out the resources below for some excellent reference management options.
Revise and Edit: Once you finish your first draft, put it away for one to two hours or, preferably, a whole day. Once you've placed some space between you and your paper, read through and edit for clarity, coherence, and grammatical errors. Reading your essay out loud is an excellent way to check for the 'flow' of the paper.
Helpful Nursing Research Writing Resources:
Purdue OWL (Online writing lab) has a robust APA guide covering everything you need about APA style and rules.
Grammarly helps you edit grammar, spelling, and punctuation. Upgrading to a paid plan will get you plagiarism detection, formatting, and engagement suggestions. This tool is excellent to help you simplify complicated sentences.
Mendeley is a free reference management software. It stores, organizes, and cites references. It has a Microsoft plug-in that inserts and correctly formats APA citations.
Don't let nursing research papers scare you away from starting nursing school or furthering your education. Their purpose is to develop skills you'll need to be an effective nurse: critical thinking, communication, and the ability to review published information critically.
Choose a great topic and follow your teacher's instructions; you'll finish that paper in no time.

Joleen Sams is a certified Family Nurse Practitioner based in the Kansas City metro area. During her 10-year RN career, Joleen worked in NICU, inpatient pediatrics, and regulatory compliance. Since graduating with her MSN-FNP in 2019, she has worked in urgent care and nursing administration. Connect with Joleen on LinkedIn or see more of her writing on her website.

Plus, get exclusive access to discounts for nurses, stay informed on the latest nurse news, and learn how to take the next steps in your career.
By clicking “Join Now”, you agree to receive email newsletters and special offers from Nurse.org. We will not sell or distribute your email address to any third party, and you may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.

- Critical Care Medicine
Explore the latest in critical care medicine, including management of respiratory failure, sepsis, HAI prevention, end-of-life care, and more.
Publication
Article type.
This cohort study assesses all interventional and observational research studies that required prospective informed consent from a large academic pediatric intensive care unit (PICU) over 10 years and analyzes disparities in approach and consent by race and ethnicity, religion, spoken language, and socioeconomic status.
This essay describes what the author learned from being in the intensive care unit with her father during multiple cardiac arrests and surgery.
This cohort study compares 90-day mortality in patients with sepsis who received piperacillin-tazobactam vs cefepime for treatment of sepsis.
This cross-sectional study examines whether an increase in pediatric intensive care unit admissions is associated with changes in the use of high-flow nasal cannula and noninvasive ventilation in children with bronchiolitis aged younger than 2 years.
This cohort study assesses the association between social determinants of health and receipt of skilled rehabilitation during intensive care unit (ICU) hospitalizations for older US adults.
This essay describes the author’s experience of improved patient care and collaboration the day the the electronic medical records system went down.
This survey study assesses factors associated with personalizing decision-making regarding fluid and vasopressor administration among patients with sepsis.
This clinical trial examines the effect of an antibiotic stewardship bundle (education, feedback, and real-time multidrug-resistant organism risk-based CPOE prompts) vs routine stewardship on antibiotic selection during the first 3 hospital days in adults with pneumonia.
This cohort study assesses whether use of medications to control blood pressure in patients who have undergone endovascular thrombectomy for acute ischemic stroke is associated with functional outcomes at 3 months.
In this narrative medicine essay, a pediatric critical care physician mulls a discussion about a patient’s status with a male colleague in front of her all-female medical team, a discussion that led her to question herself until she concludes that she can’t be all things to all people at all times.
This cohort study characterizes heterogeneity in cardiac function prior to sepsis and describes associations with hospitalization outcomes and mortality.
This cross-sectional study investigates perioperative oxygen saturation differences in Black and White infants with single ventricles undergoing stage 1 palliation.
This cohort study describes and compares clinical and radiographic features, treatment responses, and outcomes of neuroinvasive West Nile virus infection in individuals with and without immunosuppression.
This cohort study examines whether the use of an artificial intelligence–enabled deterioration model is associated with a decrease in the risk of escalations in care in hospitalized patients.
This cohort study examines whether peripheral oxygenation-saturation targets on mortality would differ by individual patient characteristics among 2 temporally and geographically distinct randomized trials of lower vs higher Sp o 2 targets in critically ill patients receiving mechanical ventilation
This JAMA Guide to Statistics and Methods article explains effect score analyses, an approach for evaluating the heterogeneity of treatment effects, and examines its use in a study of oxygen-saturation targets in critically ill patients.
- Oxygen Supplementation in COVID-19—How Much Is Enough? JAMA Opinion March 19, 2024 Respiratory Failure and Ventilation Pulmonary Medicine Coronavirus (COVID-19) Full Text | pdf link PDF
- Your Mileage May Vary: Toward Personalized Oxygen Supplementation JAMA Opinion March 19, 2024 Respiratory Failure and Ventilation Pulmonary Medicine Full Text | pdf link PDF
This randomized clinical trial assesses the effect of targeting a lower vs higher oxygenation level on 90-day survival without need for life support among intensive care unit patients with COVID-19 and severe hypoxemia.
This cohort study assesses whether severe sepsis during treatment for childhood acute leukemia is associated with increased incidence of long-term organ dysfunction among adult survivors using observational data from the St Jude Lifetime Cohort Study.
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Improving nurses’ readiness for evidence-based practice in critical care units: results of an information literacy training program
Jamileh farokhzadian.
1 Nursing Research Center, Kerman University of Medical Sciences, Kerman, Iran
2 Department of Community Health Nursing, Razi Faculty of Nursing and Midwifery, Kerman University of Medical Sciences, Kerman, Iran
Somayeh Jouparinejad
3 Health in Disasters and Emergencies Research Center, Institute for Futures Studies in Health, Kerman University of Medical Sciences, Kerman, Iran
Farhad Fatehi
4 School of Psychological Sciences, Monash University, Melbourne, Australia
5 Centre for Online Health, The University of Queensland, Brisbane, Australia
Fatemeh Falahati-Marvast
6 Health Information Sciences Department, Faculty of Management and Medical Information Sciences, Kerman University of Medical Sciences, Kerman, Iran
Associated Data
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
One of the most important prerequisites for nurses’ readiness to implement Evidence-Based Practice (EBP) is to improve their information literacy skills. This study aimed to evaluate the impact of a training program on nurses’ information literacy skills for EBP in critical care units.
In this interventional study, 60 nurses working in critical care units of hospitals affiliated to Kerman University of Medical Sciences were randomly assigned into the intervention or control groups. The intervention group was provided with information literacy training in three eight-hour sessions over 3 weeks. Data were collected using demographic and information literacy skills for EBP questionnaires before and 1 month after the intervention.
At baseline, the intervention and control groups were similar in terms of demographic characteristics and information literacy skills for EBP. The training program significantly improved all dimensions of information literacy skills of the nurses in the intervention group, including the use of different information resources (3.43 ± 0.48, p < 0.001), information searching skills and the use of different search features (3.85 ± 0.67, p < 0.001), knowledge about search operators (3.74 ± 0.14, p < 0.001), and selection of more appropriate search statement ( x 2 = 50.63, p = 0.001) compared with the control group.
Conclusions
Nurses can learn EBP skills and apply research findings in their nursing practice in order to provide high-quality, safe nursing care in clinical settings. Practical workshops and regular training courses are effective interventional strategies to equip nurses with information literacy skills so that they can apply these skills to their future nursing practice.
The Institute of Medicine (IOM) has recommended that Evidence-Based Practice (EBP) be used in 90% of clinical decisions by 2020 [ 1 ]. EBP has become a popular buzzword in the healthcare industry [ 1 , 2 ]. This concept is defined as a problem-solving process in clinical decision making, which combines best research evidence with clinical expertise, patient preference, and clinical guidelines. EBP is required to improve quality of care, patient outcomes, and cost effectiveness of care [ 2 , 3 ]. It is a gold standard that provides a framework for delivery of safe and compassionate care. EBP is not only the use of research results but also includes all aspects of nursing knowledge, attitudes, skills and self-efficacy. It is considered as an essential skill for nurses to use the best scientific evidence when designing and implementing healthcare programs as well as when applying the available research evidence in decision-making process [ 2 ].
Critical care nurses are responsible for the assessment of patients and provision of care in critical care units. Critical care nurses need expertise and evidence to recognize clinical changes and prevent complications in patients. EBP should be applied to provide better care for patients in critical care units [ 4 ]. Policymakers expect nurses to make decisions based on the most recent evidence [ 5 ]. Therefore, nurses must be equipped with information literacy skills to obtain research findings and up-to-date information [ 6 , 7 ]. Information literacy is fundamental for successful implementation of EBP, and nurses should learn and improve their search and retrieval skills in order to obtain best evidence and information for providing sympathetic, safe and ethical care [ 7 – 11 ].
Despite the emphasis on EBP being applied in nurses’ daily practice, a significant number of nurses and other clinicians have not get involved in EBP and are not fully aware of the concept of EBP. Nurses are unprepared to implement EBP due to a lack of information literacy skills in information searching and retrieval. Therefore, there is a gap between nurses’ ability and implementation of EBP [ 2 , 3 , 12 – 14 ]. According to the nursing and medical literatures, nurses are facing difficulties with EBP and their most difficult task is to find the best evidence, identify the right sources, use optimal search methods, and critically appraise the evidence in general [ 15 ]. In recent years, health care policymakers have focused on the EBP as a means of improving health services and quality of care [ 16 ].
Several studies have been conducted to determine the significance of information literacy in the implementation of EBP. The New York University Division of Nursing, for example, used components of information literacy in core courses of a master’s program to provide nursing professionals with the skills [ 17 ]. One study addressed the importance of searching for, evaluating, synthesizing and applying documented information and found that more than 80% of the nurses did not receive any training related to EBP [ 10 ]. A number of other studies investigated the importance of information literacy and the need for education programs to enhance nursing search and retrieval skills [ 18 – 20 ]. Moreover, nurses’ readiness for EBP was measured by predictors of EBP, including nurse’s informational needs and skills in using EBP, attitudes, knowledge and workplace culture in order to identify desired interventions to make EBP more practical [ 21 , 22 ]. Concerning the importance of decision-making in critical care units, this study investigated the impact of a training program on nurses’ information literacy skills for EBP in critical care units.
The following hypotheses were tested:
- Hypothesis 1: Intervention group’s mean scores on the use of different information resources would improve after a training program compared with the control group.
- Hypothesis 2: Intervention group’s mean scores of information searching skills and use of different search features would increase after a training program compared with the control group.
- Hypothesis 3: Intervention group’s mean scores of knowledge about search operators would increase after a training program compared with the control group.
- Hypothesis 4: Intervention group’s mean scores of frequency of selecting more appropriate search strategy would increase after a training program compared with the control group.
Study design and settings
This interventional study with pretest-posttest design and two intervention and control groups was conducted from March to April 2019. Nurses working in critical care units (ICUs, CCUs, and Dialysis) were selected from three educational hospitals affiliated with Kerman University of Medical Sciences in the southeast of Iran. All methods were performed in accordance with the relevant guidelines and regulations of this university.
Participants and sampling
All nurses ( N = 330) working in critical care units at the time of data collection were included in the study. A sample size of 27 participants was calculated for each group (54 participants for the two groups) using a previous study and the sample size formula. By taking into account α = 0.05, test power of 80%, and large effect size (Cohen d = 0.7) and 10% dropout probability, 60 nurses were recruited in the study using the stratified random sampling method (30 nurses in each group). Three separate lists were created from nurses working in critical care settings of the three hospitals. Owing to the fact that the number of nurses in the three hospitals was almost equal, the random number table was used to select 20 nurses equally from each hospital (10 nurses for the intervention group and 10 nurses for the control group). Finally, these nurses were divided into the intervention ( n = 30) and control groups ( n = 30).
The inclusion criteria were nurses with a bachelor’s degree or higher, as well as at least 6 months of work experience in critical care units. Participants who missed more than one session and did not complete questionnaires were excluded from the study.
Instruments
Two questionnaires were used in this study. The first one concerned the nurses’ demographic information, including gender, age, work experience, organizational position, type of shift, level of education, marital status, and history of participation in research and information literacy courses (Table 2 ). The second questionnaire assessed information literacy skills for EBP, indicating EBP readiness. This questionnaire was developed by a professional team of faculty members and nurses [ 10 , 23 ]. The information literacy skills for EBP questionnaire comprised two sections. The first section covered the use of different information resources — print, electronic and human with 19 items on a 5-point Likert scale ranging from “never” to “always”. The second section collected data on information searching skills and the use of different search features of online databases and web search engines such as subject headings and search operators, and included 10 items on a 5-point Likert scale ranging from “never” to “always”. Nurses’ knowledge about Boolean/Connectors (‘OR’, ‘AND’, ‘NOT’ or ‘AND NOT’) and Proximity (e.g. W/nn; PRE/nn) operators was assessed using 4 items with yes (one score), no (zero score), and not sure options (zero score). Finally, to assess the nurses’ database searching skills and actual skills in developing an effective search statement, they were given a hypothetical searching topic (Effect of cigarettes on lung Cancer) along with five possible search statements on MEDLINE. They were asked to choose the most appropriate search statement.
Comparison of demographic and professional information of nurses in the intervention and control groups
The cross-cultural adaptation, validity and reliability (α = 0.87) of this questionnaire has been established by Farokhzadian et al. [ 24 ].
Data collection
The self-reported questionnaires were distributed among nurses of the intervention and control groups in the pretest (before workshop) and posttest stages (one month after the workshop). Except for the intervention group that received additional material derived from workshop and the control group that received no educational program during this period, all participants completed questionnaires simultaneously and attended the routine or traditional programs in hospitals. In other words, the two study groups were subjected to the same job descriptions. However, in order to improve internal validity of the study, researchers monitored the study conditions thoroughly to ensure that the intervention and control groups were similar in all aspects, except attendance at the training program. All participants completed the survey.
Intervention procedure
The training workshops were conducted in three eight-hour sessions over 3 weeks. The intervention group was divided into two groups to increase the members’ chances of participating in the workshop. Using lectures, questions and answers, slide presentations, hands-on and online exercises, homework, and educational CDs, one Ph.D. nurse and three experts in the field of medical informatics conducted the educational course. They have entered interactive computer-based search engines with the participants during the training.
Table 1 shows the content presented in this workshop.
Topics presented in the workshop
Statistical analysis
The data were analyzed in SPSS 21 by using descriptive statistics (frequency, percentage, mean and standard deviation) and inferential statistics (independent samples t -test, paired t -test, McNemar-test, chi square, and Fisher’s exact test). The Kolmogorov-Smirnov test showed that the data were normally distributed. The significance level was considered ≤0.05.
Demographic and professional information
All nurses (intervention and control groups) participated in the study and completed questionnaire (response rate = 100%). The nurses were asked to provide their demographic and professional characteristics. No significant difference was found between the intervention and control groups in terms of demographic and professional information (Table (Table2 2 ).
Use of different information resources
No significant difference was found between the intervention (2.66 ± 0.70) and control (2.67 ± 0.66) groups in the pretest mean scores of use of different information resources ( t = 0.10, P = 0.92). However, a significant difference was observed between the intervention (3.43 ± 0.48) and control (2.76 ± 0.60) groups in terms of use of different information resources in the posttest ( t = 4.90, p < 0.001), showing that the training program significantly improved the use of different information resources in the intervention group. In addition, results showed that the training program had the highest impact on the use of different electronic resources (1.11) and the lowest impact on the use of human resources (0.26) (Table 3 ).
Comparison of mean scores of the use of different information resources in intervention and control groups
*Paired t-test
**Independent t-test
As shown in Table Table3, 3 , the use of different information resources in the control group had no significant difference in the pretest and posttest.
Information searching skills and use of different search features
No significant difference was found between the intervention (2.06 ± 0.76) and control (2.19 ± 0.83) groups in the pretest mean scores of the information searching skills and the use of different search features ( t = − 0.59, P = 0.55). However, a significant difference was observed between the intervention (3.85 ± 0.67) and control (1.93 ± 0.70) groups in terms of information searching skills and the use of different search features in posttest ( t = 10.92, p < 0.001), showing that the training program significantly improved information searching skills and the use of different search features in the intervention group. In addition, result showed that the searching skills and use of different search features in the control group had no significant difference at pretest and posttest (Table 4 ).
Comparison of mean scores of the information searching skills and use of different search features
Knowledge about search operators
No significant difference was found between the intervention (0.61 ± 0.23) and control (0.56 ± 0.21) groups in the pretest mean scores of knowledge about search operators ( t = − 0.14, p = 0.88). However, a significant difference was observed between the intervention (3.74 ± 0.14) and control (0.33 ± 0.12) groups in terms of knowledge about search operators in the posttest ( t = 17.37, p < 0.001), showing that the training program improved significantly knowledge about search operators in the intervention group. In addition, result showed that the control group’s knowledge about search operators had no significant difference in the pretest and posttest (Table 5 ).
Comparison of mean scores of knowledge about search operators in intervention and control groups
Assessment of developing search strategy
In the pretest phase, no significant difference was found between the intervention (25.80%, n = 8) and control (3.2%, n = 1) groups in frequency of selecting more appropriate search statement ( x 2 = 6.36, P = 0.01). In addition, frequency of selecting more appropriate search statement increased significantly in the intervention group (93.50%, n = 29) compared with the control (3.2%, n = 1) group in the posttest ( x 2 = 50.63, p = 0.001). In addition, frequency of selecting more appropriate search statement in the control group had no significant difference in the pretest and posttest (Table (Table6 6 ).
Comparison of frequency of selecting more appropriate search statement in intervention and control groups
*McNemar-test
**chi square-test
The present study investigated the impact of a training program on nurse’s information literacy skills for EBP in the critical care units of three hospitals affiliated to an Iranian university. The findings showed that the training program significantly improved the use of different information resources in the intervention group. Furthermore, the nurses in intervention group sought information more from electronic resources than from human and printed resources at posttest. In agreement with our findings, Tannery et al. [ 25 ] designed a pre/post-intervention study and provided access to a collection of online knowledge-based resources. After the intervention, nurses began to use various information resources as well as electronic resources instead of colleagues and print textbooks or journals. In a 4-year longitudinal study, Weng et al. [ 26 ] examined information seeking behaviors for EBP in the physicians and nurses through implementing an EBM multifaceted program that included access to websites, databases, libraries, and workshops. They found that the use of print resources remained unchanged while the use of electronic resources increased. Fiander et al. [ 27 ] in a review study reported that the use of electronic information increased in the intervention groups participating in training programs. The present study finding disagrees with the cross-sectional study conducted by Thiel et al. [ 21 ], which found that the majority of nurses obtained informational needs from peers or colleagues rather than journals, books and electronic databases. According to Patelarou et al. [ 22 ], nurses use electronic databases infrequently, with young nurses and university graduates being more likely to use them. A descriptive study was done by Farokhzadian et al. [ 24 ] who showed that nurses used different information resources, including more human and printed resources than electronic ones to search information. One of the main reasons for nurses’ poor use of electronic resources is their unfamiliarity with online databases and insufficient search skills.
The results showed that our training program improved significantly information searching skills and the use of different search features in intervention group at posttest. Kratochvíl [ 28 ] also showed positive impact of an information literacy course on students in the post-test stage, which improved their knowledge about search skills such as subject heading, defining keywords and wildcards. Carlock and Anderson [ 29 ] assessed information literacy skills of student nurses in two groups after teaching them the instructions and holding sessions. Then, for further investigation, one group was followed up while the other was not. Students in the follow-up group improved their search skills, while students in the non-follow-up group made more mistakes in their searches. Using valid and reliable nurse’s readiness tool for EBP with four specific domains including “EBP-attitude”, “EBP-knowledge”, “informational needs” and “workplace culture” [ 30 ], Patelarou et al. [ 22 ]reported an average level of nurse’s skill to conduct a search in CINAHL or MEDLINE databases based on informational needs domain. They also found “EBP knowledge” domain was positively correlated with both “informational needs” and “workplace culture” domains, implying that a nurse can learn EBP knowledge by developing necessary skills in an EBP-friendly workplace.
The findings indicated that the educational program improved significantly knowledge about search operators and frequency of selecting more appropriate search statement in the intervention group at the posttest. Therefore, the educational program improved significantly the database searching skills and actual skills in developing an effective search statement in nurses of the intervention group.
Thiel and Ghosh [ 21 ] discovered that the perceived nurse’s EBP knowledge was at a moderate level and significantly correlated with the nurse’s education level and years of nursing experiences. They described perceived EBP knowledge as different from actual knowledge and suggested that providing various resources for EBP teaching–learning plans was a helpful tool to evaluate actual knowledge of EBP over time. In addition, Kratochvíl [ 28 ] showed that students’ knowledge about search statement and Boolean operators increased after educational intervention. In a randomized controlled trial, Brettle et al. [ 31 ] evaluated the effectiveness of an online information literacy tutorial and a face-to-face session for teaching information literacy skills to nurses. The searching skills, including developing search strategy and using search operators, improved after intervention and remained unchanged in both methods 1 month later, but no improvement in any of the methods was observed after one month. El-sayed et al. [ 32 ] showed improvement in the search of information resources and search strategy among master nursing students through a training program. Ruzafa-Martínez et al. [ 33 ] conducted a 15-week educational course on EBP for the undergraduate nursing students, covering topics such as search strategies, Boolean operators, and limit function, and showed that knowledge and skill for EBP improved in the interventional group. In their pretest-posttest research, Hsieh et al. [ 34 ] employed an EBP program for search strategy and electronic literature search and evaluated learning outcomes before, immediately after, and 3 months after the intervention. They found that knowledge and skill increased immediately after the intervention, but then decreased in the final follow-up. Therefore, continuous training is essential for the stability and durability of the learned skills through follow-up courses in the previous studies. In contrast, Farokhzadian et al. [ 24 ] reported in a descriptive study that most of the nurses knew nothing or very little about information literacy skills like advanced searching techniques, Boolean and proximity operators, search features such as truncations, wildcards, MeSH terms, and search limits. Majid et al. [ 23 ]investigated nurses’ literature searching skills and discovered that they used basic search features and that less than one-quarter were familiar with Boolean and proximity operators. They also reported that nurses who had previously attended EBP training programs had more knowledge than those who had not. Hirt et al. [ 35 ] conducted a review study of educational interventions on health-related literature searching skills. They indicated that participants in the included studies were students and physicians from various health professions. The study findings were divided into two categories: search strategy development and database searching skills. Some interventional studies included in this review reported significant improvements in the development of search strategies and database searching skills, while others showed no changes in these two categories. Therefore, nurses must have sufficient knowledge to improve their information literacy skills in order to retrieve information related to clinical practice, improve the quality of care and make better decisions.
Diverse and efficient methods are recommended to empower nurses in information literacy, including integrating computer and search skills training program into the nursing curriculum in different semesters, ongoing education through holding practical workshops and sessions, following seeking behaviors among nurses and presenting feedback to them, easy access to online databases in clinical wards, updating nurses’ information about changes in search features and user interfaces of online database such as launch of the “new PubMed”, continuous encouragement to turn EBP into a routine activity, development of an information center and educational spaces equipped with IT facilities, and provision of 24/7 online trainings. Further research on the efficacy of these interventions is also suggested by using controlled study designs and long-term follow-up. According to the findings of a review study [ 35 ], few educational interventional studies on search skills have been conducted in the last 10 years. Therefore, more emphasis must be placed on nurses' education.
Limitations
We did not evaluate the effectiveness of follow-up courses in this study because nurses working in the critical care units did not have enough time and motivation to participate in these courses due to heavy shift works. This study investigated the effect of training program on nurses in critical care units and similar interventions could be performed on nurses in other wards to ensure the results are generalizable.
The results of this study show that the training program can effectively improve nurses’ information literacy skills. Information literacy is one of the key components of EBP for identifying and evaluating available scientific evidence. Nurses need search skills in order to find and use evidence in their nursing practice and provide positive patient outcomes. Therefore, it is critical to develop educational programs to help nurses improve their information literacy skills. Our findings provide health planners and policymakers with the opportunity to design an educational model that is effective, practical, and continuous in order to strengthen the nurses’ skills and make EBP more practical in the clinical setting. Extensive developments in EBP will eventually lead to improvement in healthcare and health services quality.
Acknowledgements
The researchers appreciate all nurses who spent their time so generously to participate in this study.
Abbreviations
Authors’ contributions.
JF, SJ and FFM contributed to conceiving and designing the research. The data were collected, analyzed, and interpreted by JF, SJ, FF and FFM. JF, SJ, FF and FFM contributed equally to writing and revising the manuscript and approved the final manuscript.
This research received no financial support from any funding agency in the public, commercial, or not-for-profit sectors.
Availability of data and materials
Declarations.
This study was approved by the Ethics Committee of Kerman University of Medical Science with the code of ethics No. IR.KMU.REC.1397.373. At the request of the Ethical committee, the study was conducted in accordance with the Declaration of Helsinki and Ethics Publication on Committee (COPE). There was no ethical issue during the study and data collection. Furthermore, the participants were informed that they could withdraw from the study at any time. Moreover, they were ensured about confidentiality of information. Informed consent was obtained from all nurses. For the participations’ information confidentiality to be ensured special codes were allocated to each questionnaire and the data were analyzed using these codes. Following the completion of the intervention and collection of the second phase data, participants of the control group were provided with an educational package consisting of a CD and a handbook.
Not applicable.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Critical Care Nursing Research Paper Topics

Critical care nursing research paper topics are an essential part of the academic journey of nursing students. This abstract aims to provide a brief overview of the comprehensive list of research paper topics related to critical care nursing. It encompasses a wide range of categories, including Acute Respiratory Failure, Sepsis and Septic Shock, Cardiogenic Shock, and many more. Moreover, it highlights the importance of critical care nursing in healthcare and encourages students to explore the diverse range of topics provided. Additionally, it introduces iResearchNet’s writing services, which offers students the opportunity to order a custom critical care nursing research paper on any topic, ensuring success in their academic pursuits.
100 Critical Care Nursing Research Paper Topics
Introductory Paragraph: Critical care nursing is a crucial and intricate part of the healthcare system. This specialized field of nursing caters to patients with life-threatening illnesses and injuries, necessitating a deep understanding and specialized knowledge in various aspects of critical care. The keyphrase ‘critical care nursing research paper topics’ underlines the wide array of subjects that nursing students can delve into, to not only enrich their knowledge but also contribute to this vital field.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% off with 24start discount code.
- Pathophysiology of Acute Respiratory Failure
- Non-invasive Ventilation in Acute Respiratory Failure
- Oxygen Therapy in Acute Respiratory Failure
- Risk Factors for Acute Respiratory Failure
- Complications of Acute Respiratory Failure
- Nursing Management of Acute Respiratory Failure
- Pharmacological Management of Acute Respiratory Failure
- Role of Physiotherapy in Acute Respiratory Failure
- Prognosis of Acute Respiratory Failure
- Preventive Measures for Acute Respiratory Failure
- Pathophysiology of Sepsis and Septic Shock
- Early Goal-Directed Therapy in Sepsis
- Biomarkers in Sepsis and Septic Shock
- Nursing Interventions for Sepsis and Septic Shock
- Antibiotic Therapy in Sepsis and Septic Shock
- Vasopressor Therapy in Septic Shock
- Fluid Resuscitation in Sepsis and Septic Shock
- Organ Dysfunction in Sepsis and Septic Shock
- Prognostic Factors in Sepsis and Septic Shock
- Preventing Sepsis and Septic Shock
- Pathophysiology of Cardiogenic Shock
- Management of Cardiogenic Shock
- Intra-aortic Balloon Pump in Cardiogenic Shock
- Vasopressor and Inotropes in Cardiogenic Shock
- Nursing Management of Cardiogenic Shock
- Complications of Cardiogenic Shock
- Mechanical Circulatory Support in Cardiogenic Shock
- Prognosis of Cardiogenic Shock
- Preventing Cardiogenic Shock
- Case Studies on Cardiogenic Shock
- Principles of Hemodynamic Monitoring
- Invasive vs Non-Invasive Hemodynamic Monitoring
- Role of Echocardiography in Hemodynamic Monitoring
- Nursing Considerations in Hemodynamic Monitoring
- Complications of Hemodynamic Monitoring
- Accuracy and Limitations of Hemodynamic Monitoring
- Hemodynamic Monitoring in Specific Conditions (e.g., ARDS, Sepsis)
- Future Trends in Hemodynamic Monitoring
- Clinical Case Studies on Hemodynamic Monitoring
- Best Practices in Hemodynamic Monitoring
- Principles of Mechanical Ventilation
- Modes of Mechanical Ventilation
- Setting and Adjusting Ventilator Parameters
- Nursing Care of Patients on Mechanical Ventilation
- Weaning from Mechanical Ventilation
- Complications of Mechanical Ventilation
- Mechanical Ventilation in Specific Conditions (e.g., COPD, ARDS)
- High-Frequency Oscillatory Ventilation
- Non-Invasive Ventilation
- Ethical Considerations in Mechanical Ventilation
- Assessment of Pain in Critical Care
- Pharmacological Management of Pain
- Non-Pharmacological Management of Pain
- Sedation in Critical Care: Principles and Practice
- Assessment of Sedation Levels
- Complications of Sedation
- Special Considerations in Pain and Sedation Management (e.g., Renal Failure)
- Pain and Sedation in Specific Populations (e.g., Elderly, Pediatric)
- Role of Family in Pain and Sedation Management
- Guidelines and Protocols for Pain and Sedation Management
- Pathophysiology of Delirium
- Assessment Tools for Delirium
- Risk Factors for Delirium
- Preventive Strategies for Delirium
- Pharmacological Management of Delirium
- Non-Pharmacological Management of Delirium
- Impact of Delirium on Patient Outcomes
- Role of Family in Managing Delirium
- Delirium in Specific Populations (e.g., Elderly, Postoperative)
- Future Directions in Delirium Research and Management
- Pathophysiology of Acute Kidney Injury
- Risk Factors for Acute Kidney Injury
- Diagnosis and Staging of Acute Kidney Injury
- Prevention of Acute Kidney Injury
- Management of Acute Kidney Injury
- Role of Renal Replacement Therapy in Acute Kidney Injury
- Complications of Acute Kidney Injury
- Prognosis of Acute Kidney Injury
- Acute Kidney Injury in Specific Conditions (e.g., Sepsis, Surgery)
- Nursing Care of Patients with Acute Kidney Injury
- Nutritional Assessment in Critical Care
- Enteral vs Parenteral Nutrition
- Nutritional Requirements in Specific Conditions (e.g., Sepsis, ARDS)
- Complications of Nutritional Support
- Monitoring and Adjustment of Nutritional Support
- Role of Micronutrients in Critical Care
- Ethical Considerations in Nutritional Support
- Impact of Nutritional Support on Patient Outcomes
- Guidelines and Protocols for Nutritional Support
- Future Directions in Critical Care Nutrition
- Principles of End of Life Care in ICU
- Communication Strategies in End of Life Care
- Ethical Considerations in End of Life Care
- Role of Palliative Care in ICU
- Management of Symptoms at End of Life
- Decision Making in End of Life Care
- Role of Family in End of Life Care
- Cultural Considerations in End of Life Care
- Bereavement Support for Families
- Organ Donation and End of Life Care
In conclusion, the breadth of critical care nursing research paper topics available for exploration is vast and diverse. This list provides a comprehensive overview of potential topics that nursing students can choose from, thereby helping them delve deeply into specific areas of interest. It is crucial for aspiring nurses and researchers to explore these topics in depth, as it will not only enhance their knowledge but also contribute to the advancements in the critical care nursing field.
The Range of Critical Care Nursing Research Paper Topics
Critical care nursing is a specialized area of nursing that is dedicated to meeting the needs of patients and families facing life-threatening illnesses or injuries. This involves not only managing acute and often complex health issues but also addressing the psychosocial and communication challenges that arise in these high-stress environments. Due to the nature of the work, critical care nurses need to be highly skilled in assessment, problem-solving, and decision-making. This article delves into the significance of critical care nursing and the wide range of critical care nursing research paper topics it offers, such as acute respiratory failure, sepsis and septic shock, and mechanical ventilation.
The Significance of Critical Care Nursing
Critical care nursing is pivotal in the healthcare system as it deals with life and death situations. Nurses in this field play a crucial role in the management of critically ill patients. They provide specialized care, monitor the patients’ condition, and use advanced technology and medications to optimize outcomes. These nurses also support the patients’ families, helping them to understand the situation and to cope with the stress and anxiety associated with critical illnesses or injuries.
A critical care nurse’s role includes assessing the patient’s condition, planning and implementing care, and evaluating the patient’s response to the treatment. They collaborate with a multidisciplinary team of healthcare professionals, including physicians, pharmacists, respiratory therapists, and dietitians, to provide comprehensive care to the critically ill. This collaborative approach ensures that all aspects of the patient’s well-being are addressed, from physiological to psychological needs.
One of the most crucial skills of a critical care nurse is the ability to make quick and accurate decisions. The condition of critically ill patients can change rapidly, and timely interventions can be the difference between life and death. Therefore, critical care nurses must have a deep understanding of the pathophysiology of critical illnesses and the pharmacology of medications used in critical care settings.
Additionally, critical care nurses play a significant role in end-of-life care. They provide compassionate care to patients who are at the end of their lives and support their families during this difficult time. This includes managing symptoms, providing emotional support, and facilitating communication between the patient, family, and healthcare team.
Acute Respiratory Failure
Acute respiratory failure is a common condition encountered in critical care settings. It occurs when the lungs cannot adequately exchange oxygen and carbon dioxide, leading to hypoxemia (low levels of oxygen in the blood) or hypercapnia (high levels of carbon dioxide in the blood). Acute respiratory failure can be caused by various factors, including pneumonia, acute respiratory distress syndrome (ARDS), chronic obstructive pulmonary disease (COPD), and neuromuscular disorders.
Management of acute respiratory failure involves addressing the underlying cause, supporting oxygenation and ventilation, and preventing complications. This may include administering supplemental oxygen, medications to treat the underlying cause (e.g., antibiotics for pneumonia), and mechanical ventilation in severe cases. Critical care nurses play a vital role in the management of patients with acute respiratory failure by monitoring their respiratory status, administering medications, managing mechanical ventilation, and providing supportive care.
Sepsis and Septic Shock
Sepsis is a life-threatening response to an infection that can lead to tissue damage, organ failure, and death. Septic shock is a subset of sepsis characterized by profound circulatory, cellular, and metabolic abnormalities, leading to a higher risk of mortality. Early recognition and management of sepsis and septic shock are crucial for improving outcomes.
The management of sepsis and septic shock involves administering antibiotics, fluids, and vasopressors (medications that constrict blood vessels and increase blood pressure) as needed. Other treatments may include mechanical ventilation, renal replacement therapy, and surgical interventions to remove the source of infection. Critical care nurses play a crucial role in the early recognition and management of sepsis and septic shock by monitoring the patient’s vital signs, administering medications and fluids, and providing supportive care.
Mechanical Ventilation
Mechanical ventilation is a life-saving intervention used in critical care settings to support or replace the patient’s spontaneous breathing. It is commonly used in patients with acute respiratory failure, ARDS, and during surgical procedures requiring general anesthesia. Mechanical ventilation can be invasive (via an endotracheal tube or tracheostomy) or non-invasive (via a mask or helmet).
Managing a patient on mechanical ventilation requires specialized knowledge and skills. It involves selecting the appropriate mode of ventilation, setting and adjusting the ventilator parameters, monitoring the patient’s response to ventilation, and preventing and managing complications. Critical care nurses play a pivotal role in the management of patients on mechanical ventilation by monitoring their respiratory status, adjusting ventilator settings as needed, and providing supportive care.
Critical care nursing is a vital and specialized field in healthcare that focuses on managing patients with life-threatening illnesses or injuries. This includes addressing various aspects such as acute respiratory failure, sepsis and septic shock, and mechanical ventilation. Critical care nurses play a pivotal role in assessing, planning, implementing, and evaluating the care of critically ill patients. They collaborate with a multidisciplinary team of healthcare professionals to provide comprehensive and compassionate care. Research in critical care nursing is essential for developing evidence-based practices, improving patient outcomes, and advancing the profession. The range of critical care nursing research paper topics is diverse and offers numerous opportunities for in-depth exploration and contribution to this crucial field.
iResearchNet’s Custom Writing Services
iResearchNet is a leading provider of academic writing services, dedicated to helping students succeed in their academic pursuits. We understand the challenges that students face when it comes to writing research papers, particularly in specialized fields such as critical care nursing. Our commitment is to provide high-quality, customized solutions that meet your specific needs and requirements.
- Expert Degree-Holding Writers: Our team comprises writers who hold advanced degrees in nursing and other related fields. They have extensive experience in academic writing and are well-versed in the latest research and trends in critical care nursing.
- Custom Written Works: We provide custom written research papers tailored to your specific requirements. Our writers will create a unique and original paper that meets your instructions and academic standards.
- In-Depth Research: Our writers conduct comprehensive research using reliable and up-to-date sources. They critically evaluate the literature and incorporate relevant evidence into your paper.
- Custom Formatting: We format your paper according to your preferred citation style, whether it is APA, MLA, Chicago/Turabian, or Harvard.
- Top Quality: We ensure top quality by thoroughly reviewing and editing the paper before delivery. Our quality assurance team checks the paper for coherence, consistency, and adherence to your instructions.
- Customized Solutions: We understand that each student has unique needs and requirements. Therefore, we offer customized solutions that cater to your specific needs.
- Flexible Pricing: We offer flexible pricing options that fit your budget. Our pricing is transparent, and there are no hidden charges.
- Short Deadlines up to 3 hours: We can work within tight deadlines and deliver your paper in as little as three hours. However, the quality of our work is never compromised, even with short deadlines.
- Timely Delivery: We always deliver your paper on time. You can rely on us to meet your deadlines, no matter how tight they are.
- 24/7 Support: Our customer support team is available 24/7 to assist you with any questions or concerns. You can contact us via email, phone, or live chat.
- Absolute Privacy: We respect your privacy and ensure that your personal information is kept confidential. We never share your information with third parties.
- Easy Order Tracking: You can easily track your order status and communicate with your writer through our user-friendly customer portal.
- Money-Back Guarantee: We are confident in the quality of our services. However, if you are not satisfied with the final product, we offer a money-back guarantee.
At iResearchNet, we are committed to helping you succeed in your academic pursuits. We understand the importance of developing high-quality research papers in specialized fields such as critical care nursing. Our team of expert writers, comprehensive research approach, and commitment to quality make us the ideal choice for your academic writing needs. Order a custom critical care nursing research paper today and experience the benefits of our professional writing services.

Unlock Success with iResearchNet
Embarking on a journey through the world of critical care nursing research can be daunting. The path is riddled with intricate details, complex concepts, and a need for a profound understanding of both theory and practice. However, you are not alone on this journey. iResearchNet is here to guide you through each step, ensuring your success.
Our expert degree-holding writers are well-versed in the intricacies of critical care nursing and are equipped to provide you with a top-quality, custom-written research paper tailored to your specific needs. With our commitment to in-depth research, custom formatting, and timely delivery, you can rest assured that your academic pursuits are in capable hands.
Take the next step towards academic excellence. Trust iResearchNet with your critical care nursing research paper and unlock the doors to success. Our comprehensive range of services, coupled with a dedicated team of experts, ensures that you receive the highest quality work, tailored to your specific needs.
Order your custom critical care nursing research paper today and embark on a journey towards academic excellence with iResearchNet as your trusted companion. Your success is our priority, and we are committed to helping you achieve it. Don’t miss out on the opportunity to elevate your academic performance. Place your order now!
ORDER HIGH QUALITY CUSTOM PAPER

- 44-207-097-1871
Dissertation Writing Tools
- 1. Complete Dissertation Writing Guide - eBook
- 2. Dissertation Templates Pack
- 3. Research Methodology Handbook
- 4. Academic Writing Checklist
- 5. Citation Style Guide
- 6. Time Management for Dissertation Writing
- 7. Literature Review Toolkit
- 8. Grammar and Style Guide
- 9. Dissertation Proposal Template
- 10.Five Pre-written Full Dissertation Papers

56 Best Critical Care Nursing Research Topics ideas with examples
Are you searching Critical Care Nursing Research Topics? Critical care nursing is an evolving field. If you are looking for research proposal topics in critical care, we’ve got you. We have a great list of the latest nursing dissertation topics in critical care. You can use these for your undergrad and master’s programs. Similarly, if […]

Are you searching Critical Care Nursing Research Topics? Critical care nursing is an evolving field. If you are looking for research proposal topics in critical care, we’ve got you. We have a great list of the latest nursing dissertation topics in critical care. You can use these for your undergrad and master’s programs. Similarly, if you want, we also have a list of nursing , dementia , marketing , and human resource management topics. We can also help you in completing your research according to the standards and requirements.
Best Critical Care Nursing Dissertation topics or research topics for masters and undergraduate students
Here is the list of Critical Care Nursing Research Topics and titles for college students.
- Analyzing the importance of timings in the critical care nursing areas.
- Probing the essential role of nursing – a literature review.
- Literature review on critical nursing analysis in the past 10 years.
- Examining the strategies of management of acute patients of dementia.
- To maintain professional habits in the intensive care system – a case analysis of the US.
- Brief examination and plans for critical care patients above the age of 50.
- Do you think visitation should be allowed in the critical care unit?
- An analysis of the nurse’s perspective on essential visitors of the patient.
- Necessary care education is very important among critical nurses – a cross-country analysis.
- Risk and caring factors of pressure injuries among ICU patients.
- The difference between planned and emergency surgeries – a case scenario analysis
- The study on Ventilator-associated ill patients and their need for health care facilities.
- What are the challenges faced by the critical care nursing system?
- Do nurses face problems with visitors? How do they cause disturbance?
- Review on critical decision making by nurses in cardiac patients in the UK.
- What key challenges do nurses face in ICU? – a critical analysis
- Study on care in a technologically intense environment.
- Study on the situation of patients with heart failure in the primary health care unit.
- Equipment training for the nurses in the critical care unit.
- Nurses study the importance of urgent and intensive care in the nursing field in the UK.
- The nurse also provides telephonic consultation in the primary care of patients in the UK.
- Discussion is related to why Should nurses are allowed to prescribe medicines to critical patients in the UK.
- Emphasizing the status of psychological aid in ICU patients – a case analysis
- Critically stating the miscommunication between the Physician and nurses in the intensive care unit.
- A study on low income in essential nurses and how it affects their motivation and work commitment.
- How do caregivers communicate with critical patients in ICU?
- How do nurses manage covid’19 acute patients?
- What issues were faced by nurses during the covid’19 pandemic period?
- Did the covid situation also affect the personal life of critical care nurses?
- What was the actual condition of the care department during this pandemic?
- Is job satisfaction important in a nursing career?
- Do nurses get demotivated due to low pay like offices?
- What problem do nurses face while decision-making for the patients?
- How do nurses take the end of life decisions? A survey analysis.
- The study states that nursing scores got high in this pandemic period.
- Spiritual well-being survey unit.
- Does good critical thinking equal effectiveness in decision-making among critical nurses care?
- Study on psychological stress among health care professionals.
- Case study on post-traumatic stress system for the nurses after a patient’s death.
- How does the relationship between nurse and patient impact the intensive care unit?
- Study on doing critical care nurses accomplish resilience.
- What is burnout syndrome, and how does it affect the quality of care offered by nurses?
- Study on nutritional care to acute care patients and the role of nurses.
- Connection in the middle of blood shortage and the patient outcome after transfusion.
- Managing the open wound in urgent care – what measures must be taken instantly by nurses?
- Study on the patients with aid and how nurses play their role.
- Case study on causes of burnout patients in critical care.
- Do nurses get affected by essential patients of care conditions?
- Does a nurse’s private life get affected by the patient’s outcome?
- Do Male and females get different types of critical care?
Above is the best Critical Care Nursing Research Topics, choose any topic of your choice and start dissertation writing in nursing or hire our expert services to customize the Critical Care Nursing Research Topics brief.
Paid Topic Mini Proposal (500 Words)
You will get the topics first and then the mini proposal which includes:
- An explanation why we choose this topic.
- 2-3 research questions.
- Key literature resources identification.
- Suitable methodology including raw sample size and data collection method
- View a Sample of Service
Note: After submiting your order please must check your email [inbox/spam] folders for order confirmation and login details.If email goes in spam please mark not as spam to avoid any communication gap between us.
Get An Expert Dissertation Writing Help To Achieve Good Grades
By placing an order with us, you can get;
- Writer consultation before payment to ensure your work is in safe hands.
- Free topic if you don't have one
- Draft submissions to check the quality of the work as per supervisor's feedback
- Free revisions
- Complete privacy
- Plagiarism Free work
- Guaranteed 2:1 (With help of your supervisor's feedback)
- 2 Instalments plan
- Special discounts
Other Related Posts
- Dissertation Topics in International Relations February 20, 2024 -->
- Unlock Your Academic Potential with the Right Topics for Dissertation October 12, 2023 -->
- 89+ Best Unique and Informative Speech Topics for Students January 6, 2023 -->
- Employment Law Dissertation Topics January 4, 2023 -->
- 59 Best Environmental Law Dissertation Topics & Examples January 4, 2023 -->
- 37 Monetary economics dissertation topics ideas March 20, 2022 -->
- 39 Economic geography dissertation topics examples March 19, 2022 -->
- 37 Public economics dissertation topics Ideas March 18, 2022 -->
- 39 Financial Economics Dissertation Topics Ideas March 17, 2022 -->
- 39 Experimental economics dissertation topics Ideas March 16, 2022 -->
- 39 Environmental Economics Dissertation Topics Ideas and Samples March 15, 2022 -->
- 39 Health economics dissertation topics Ideas and Examples March 14, 2022 -->
- 39 Business economics dissertation topics Ideas and Examples March 13, 2022 -->
- 39 Behavioral Economics Dissertation Topics Examples March 12, 2022 -->
- 39 Agricultural Economics Dissertation Topics Examples March 11, 2022 -->
WhatsApp and Get 35% off promo code now!
Critical care nursing research: opportunities and resources
Affiliation.
- 1 Rutgers-State University of New Jersey, Newark, NJ.
- PMID: 8167774
Background: As patient needs become more complex in the critical care setting, nurses with increased clinical expertise are needed to expand the research knowledge base and apply existing knowledge in practice settings.
Purpose: To review opportunities and resources that are available to facilitate nurses' involvement in critical care research: opportunities for participation in research, sources of ideas, human and financial resources, and ideas for the dissemination of research findings.
Conclusions: Opportunities and resources available for critical care research are numerous, varied, and widely available. They should be used to advance the scientific bases for critical care practice.
Publication types
- Clinical Nursing Research* / economics
- Clinical Nursing Research* / methods
- Critical Care*
- Information Services
- Research Support as Topic
Jump to navigation

Bookmark/Search this post

Mayo Clinic School of Continuous Professional Development
You are here, foundations of critical care nursing online cne course: connecting patient diagnosis to medication therapy.
- Accreditation

Caring for the critical care patient includes understanding common medication therapies for complex diagnosis. This course will review common medications and nursing considerations for administration. Concept review and case scenarios include patients with heart failure, acute coronary syndrome and frequently seen therapies including anticoagulation.
Course Director Denise Rismeyer, DNP, MSN, RN, NPD-BC Director of Continuing Nursing Education Mayo Clinic
Target Audience
This CNE course is designed for RNs, LPNs, and healthcare professionals providing care for progressive and critical care patients.
Learning Objectives
Upon completion of this activity, participants should be able to:
- Identify common drug classes of medications administered in the inpatient setting
- Describe side effects of common medications
- Discuss nursing considerations related to medication administration for complex patient diagnoses
- Apply knowledge of medications to patient scenarios that may be encountered in the critical care setting
Attendance at any Mayo Clinic course does not indicate or guarantee competence or proficiency in the skills, knowledge or performance of any care or procedure(s) which may be discussed or taught in this course.
- 1.50 Attendance
This course will be presented via a self-guided online interactive module.
Faculty Tiffany Schoenfelder, MSN, RN Nursing Education Specialist – Interventional Cardiovascular Instructor in Nursing – Mayo Clinic College of Medicine and Science Nursing Professional Development Division Department of Nursing Mayo Clinic, Rochester, MN
Course Director Denise Rismeyer, MSN, RN, NPD-BC Director Continuing Nursing Education Program Assistant Professor of Nursing, Mayo Clinic College of Medicine and Science Department of Nursing Mayo Clinic, Rochester, MN
Credit Statements ANCC Mayo Clinic College of Medicine and Science designates this enduring activity for a maximum of 1.50 ANCC contact hours.

Other Healthcare Professionals A record of attendance will be provided to all registrants for requesting credits in accordance with state nursing boards, specialty societies or other professional associations.
Available Credit
Commitment to Equity, Diversity and Inclusion
Mayo Clinic School of Continuous Professional Development (MCSCPD) strives to foster a learning environment in which individual differences are valued, allowing all to achieve their fullest potential.
Cancellation and Refund Policy
Request for cancellations must be submitted in writing to [email protected]. If the cancellation is made prior to the start of the activity, a refund less an administration fee of $25 will be issued. If the cancellation is made after the start of the activity, no refund will be issued. All refunds will be made using the same method as the original payment.
Any use of this site constitutes your agreement to the Terms and Conditions of Online Registration.
- Career Center
- Member Login
From the Bedside to Research: Navigating Change in Nursing
As we celebrate National Nurses Week, the AcademyHealth Interdisciplinary Research Group on Nursing Issues shines a spotlight on the indispensable contributions of nurses to the health care sector. Amid evolving challenges, these frontline professionals continue to lead with resilience and innovation, driving significant changes across the industry.

National Nurses Week is a time to celebrate and reflect on the evolving role of nurses and their significant impact on the health care system. As frontline caregivers, nurses face a myriad of challenges, yet they continue to lead and innovate, shaping the future of health care with their resilience and pioneering spirit.
Addressing Nurse Compensation
The establishment of the Commission for Nurse Reimbursement in 2023 marks a significant shift in the financial recognition of nurses within the health care system. Historically, nursing services have been bundled into the general costs of health care, much like hospital supplies, leading to undervaluation and lack of visibility in the billing process. This commission, led by co-chairs Rebecca Love, RN, BS, MSN, FIEL, and Sharon Pearce, DNP, CRNA, FAANA, FAAN, was formed in response to a critical staffing shortage and aims to transform nursing care into a billable service. By advocating for changes in how Medicare and other entities reimburse for nursing services, the commission seeks to elevate the financial stature of nursing, enhancing job satisfaction, and retention, and ultimately stabilizing health care services. This initiative not only acknowledges the indispensable role of nurses but also strives to create a sustainable work environment that attracts and retains skilled professionals
Combating Workplace Violence
Workplace safety is another critical issue in the nursing sector, particularly the rising incidents of violence that nurses face. On average, two nurses per hour are assaulted in acute care settings, underscoring the urgent need for better protection. Strategies to combat this include training staff in de-escalation techniques, implementing stricter security protocols, and establishing support systems for those affected by violence. Ensuring the safety of nurses is crucial for allowing them to provide the best possible care to their patients.
Policy Engagement: Amplifying Nurses' Voices
Nurses play a vital role in health care policymaking, given their direct patient care experience and patient-centered perspectives. Their active participation in legislative discussions helps ensure that health policies are practical and effectively implemented. Nurses advocate for policies that reflect the realities of patient care, steering the health care system toward more effective and humane outcomes.
Nurse Researchers: Pioneers of Innovation
Nurse researchers are at the forefront of refining nursing practices and introducing innovations that improve patient outcomes. Their work in 2024 is particularly vital as they research staffing models, patient care techniques, and the integration of new technologies such as digital health records and predictive analytics tools. These innovations are transforming everyday nursing practices, making health care more effective and responsive.
Embracing Technological Innovations
The integration of Artificial Intelligence (AI) and Telehealth has been a game-changer in health care delivery, spearheaded by nurses . AI enhances diagnostic accuracy and treatment protocols by analyzing vast amounts of patient data. Telehealth, on the other hand, expands access to medical services, especially in remote or underserved areas, ensuring timely and efficient care. These technologies provide nurses with tools that augment their clinical skills and allow for better care across various settings.
As we observe National Nurses Week, it is essential to acknowledge the adaptability and innovative spirit of nurses globally. Despite numerous challenges, they continue to lead in the health care sector. With initiatives like the Commission for Nurse Reimbursement and the adoption of new technologies like AI, nurses are setting new standards in health care delivery. This week, and every week, we reaffirm our commitment to supporting and empowering the nursing profession as it continues to navigate these transformative times. From bedside care to research labs, nurses play an indispensable role in enhancing our health care system.
- Open access
- Published: 14 May 2024
Developing a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in Medical Assistance in Dying (MAiD): a mixed method modified e-Delphi study
- Jocelyn Schroeder 1 ,
- Barbara Pesut 1 , 2 ,
- Lise Olsen 2 ,
- Nelly D. Oelke 2 &
- Helen Sharp 2
BMC Nursing volume 23 , Article number: 326 ( 2024 ) Cite this article
31 Accesses
Metrics details
Medical Assistance in Dying (MAiD) was legalized in Canada in 2016. Canada’s legislation is the first to permit Nurse Practitioners (NP) to serve as independent MAiD assessors and providers. Registered Nurses’ (RN) also have important roles in MAiD that include MAiD care coordination; client and family teaching and support, MAiD procedural quality; healthcare provider and public education; and bereavement care for family. Nurses have a right under the law to conscientious objection to participating in MAiD. Therefore, it is essential to prepare nurses in their entry-level education for the practice implications and moral complexities inherent in this practice. Knowing what nursing students think about MAiD is a critical first step. Therefore, the purpose of this study was to develop a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in MAiD in the Canadian context.
The design was a mixed-method, modified e-Delphi method that entailed item generation from the literature, item refinement through a 2 round survey of an expert faculty panel, and item validation through a cognitive focus group interview with nursing students. The settings were a University located in an urban area and a College located in a rural area in Western Canada.
During phase 1, a 56-item survey was developed from existing literature that included demographic items and items designed to measure experience with death and dying (including MAiD), education and preparation, attitudes and beliefs, influences on those beliefs, and anticipated future involvement. During phase 2, an expert faculty panel reviewed, modified, and prioritized the items yielding 51 items. During phase 3, a sample of nursing students further evaluated and modified the language in the survey to aid readability and comprehension. The final survey consists of 45 items including 4 case studies.
Systematic evaluation of knowledge-to-date coupled with stakeholder perspectives supports robust survey design. This study yielded a survey to assess nursing students’ attitudes toward MAiD in a Canadian context.
The survey is appropriate for use in education and research to measure knowledge and attitudes about MAiD among nurse trainees and can be a helpful step in preparing nursing students for entry-level practice.
Peer Review reports
Medical Assistance in Dying (MAiD) is permitted under an amendment to Canada’s Criminal Code which was passed in 2016 [ 1 ]. MAiD is defined in the legislation as both self-administered and clinician-administered medication for the purpose of causing death. In the 2016 Bill C-14 legislation one of the eligibility criteria was that an applicant for MAiD must have a reasonably foreseeable natural death although this term was not defined. It was left to the clinical judgement of MAiD assessors and providers to determine the time frame that constitutes reasonably foreseeable [ 2 ]. However, in 2021 under Bill C-7, the eligibility criteria for MAiD were changed to allow individuals with irreversible medical conditions, declining health, and suffering, but whose natural death was not reasonably foreseeable, to receive MAiD [ 3 ]. This population of MAiD applicants are referred to as Track 2 MAiD (those whose natural death is foreseeable are referred to as Track 1). Track 2 applicants are subject to additional safeguards under the 2021 C-7 legislation.
Three additional proposed changes to the legislation have been extensively studied by Canadian Expert Panels (Council of Canadian Academics [CCA]) [ 4 , 5 , 6 ] First, under the legislation that defines Track 2, individuals with mental disease as their sole underlying medical condition may apply for MAiD, but implementation of this practice is embargoed until March 2027 [ 4 ]. Second, there is consideration of allowing MAiD to be implemented through advanced consent. This would make it possible for persons living with dementia to receive MAID after they have lost the capacity to consent to the procedure [ 5 ]. Third, there is consideration of extending MAiD to mature minors. A mature minor is defined as “a person under the age of majority…and who has the capacity to understand and appreciate the nature and consequences of a decision” ([ 6 ] p. 5). In summary, since the legalization of MAiD in 2016 the eligibility criteria and safeguards have evolved significantly with consequent implications for nurses and nursing care. Further, the number of Canadians who access MAiD shows steady increases since 2016 [ 7 ] and it is expected that these increases will continue in the foreseeable future.
Nurses have been integral to MAiD care in the Canadian context. While other countries such as Belgium and the Netherlands also permit euthanasia, Canada is the first country to allow Nurse Practitioners (Registered Nurses with additional preparation typically achieved at the graduate level) to act independently as assessors and providers of MAiD [ 1 ]. Although the role of Registered Nurses (RNs) in MAiD is not defined in federal legislation, it has been addressed at the provincial/territorial-level with variability in scope of practice by region [ 8 , 9 ]. For example, there are differences with respect to the obligation of the nurse to provide information to patients about MAiD, and to the degree that nurses are expected to ensure that patient eligibility criteria and safeguards are met prior to their participation [ 10 ]. Studies conducted in the Canadian context indicate that RNs perform essential roles in MAiD care coordination; client and family teaching and support; MAiD procedural quality; healthcare provider and public education; and bereavement care for family [ 9 , 11 ]. Nurse practitioners and RNs are integral to a robust MAiD care system in Canada and hence need to be well-prepared for their role [ 12 ].
Previous studies have found that end of life care, and MAiD specifically, raise complex moral and ethical issues for nurses [ 13 , 14 , 15 , 16 ]. The knowledge, attitudes, and beliefs of nurses are important across practice settings because nurses have consistent, ongoing, and direct contact with patients who experience chronic or life-limiting health conditions. Canadian studies exploring nurses’ moral and ethical decision-making in relation to MAiD reveal that although some nurses are clear in their support for, or opposition to, MAiD, others are unclear on what they believe to be good and right [ 14 ]. Empirical findings suggest that nurses go through a period of moral sense-making that is often informed by their family, peers, and initial experiences with MAID [ 17 , 18 ]. Canadian legislation and policy specifies that nurses are not required to participate in MAiD and may recuse themselves as conscientious objectors with appropriate steps to ensure ongoing and safe care of patients [ 1 , 19 ]. However, with so many nurses having to reflect on and make sense of their moral position, it is essential that they are given adequate time and preparation to make an informed and thoughtful decision before they participate in a MAID death [ 20 , 21 ].
It is well established that nursing students receive inconsistent exposure to end of life care issues [ 22 ] and little or no training related to MAiD [ 23 ]. Without such education and reflection time in pre-entry nursing preparation, nurses are at significant risk for moral harm. An important first step in providing this preparation is to be able to assess the knowledge, values, and beliefs of nursing students regarding MAID and end of life care. As demand for MAiD increases along with the complexities of MAiD, it is critical to understand the knowledge, attitudes, and likelihood of engagement with MAiD among nursing students as a baseline upon which to build curriculum and as a means to track these variables over time.
Aim, design, and setting
The aim of this study was to develop a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in MAiD in the Canadian context. We sought to explore both their willingness to be involved in the registered nursing role and in the nurse practitioner role should they chose to prepare themselves to that level of education. The design was a mixed-method, modified e-Delphi method that entailed item generation, item refinement through an expert faculty panel [ 24 , 25 , 26 ], and initial item validation through a cognitive focus group interview with nursing students [ 27 ]. The settings were a University located in an urban area and a College located in a rural area in Western Canada.
Participants
A panel of 10 faculty from the two nursing education programs were recruited for Phase 2 of the e-Delphi. To be included, faculty were required to have a minimum of three years of experience in nurse education, be employed as nursing faculty, and self-identify as having experience with MAiD. A convenience sample of 5 fourth-year nursing students were recruited to participate in Phase 3. Students had to be in good standing in the nursing program and be willing to share their experiences of the survey in an online group interview format.
The modified e-Delphi was conducted in 3 phases: Phase 1 entailed item generation through literature and existing survey review. Phase 2 entailed item refinement through a faculty expert panel review with focus on content validity, prioritization, and revision of item wording [ 25 ]. Phase 3 entailed an assessment of face validity through focus group-based cognitive interview with nursing students.
Phase I. Item generation through literature review
The goal of phase 1 was to develop a bank of survey items that would represent the variables of interest and which could be provided to expert faculty in Phase 2. Initial survey items were generated through a literature review of similar surveys designed to assess knowledge and attitudes toward MAiD/euthanasia in healthcare providers; Canadian empirical studies on nurses’ roles and/or experiences with MAiD; and legislative and expert panel documents that outlined proposed changes to the legislative eligibility criteria and safeguards. The literature review was conducted in three online databases: CINAHL, PsycINFO, and Medline. Key words for the search included nurses , nursing students , medical students , NPs, MAiD , euthanasia , assisted death , and end-of-life care . Only articles written in English were reviewed. The legalization and legislation of MAiD is new in many countries; therefore, studies that were greater than twenty years old were excluded, no further exclusion criteria set for country.
Items from surveys designed to measure similar variables in other health care providers and geographic contexts were placed in a table and similar items were collated and revised into a single item. Then key variables were identified from the empirical literature on nurses and MAiD in Canada and checked against the items derived from the surveys to ensure that each of the key variables were represented. For example, conscientious objection has figured prominently in the Canadian literature, but there were few items that assessed knowledge of conscientious objection in other surveys and so items were added [ 15 , 21 , 28 , 29 ]. Finally, four case studies were added to the survey to address the anticipated changes to the Canadian legislation. The case studies were based upon the inclusion of mature minors, advanced consent, and mental disorder as the sole underlying medical condition. The intention was to assess nurses’ beliefs and comfort with these potential legislative changes.
Phase 2. Item refinement through expert panel review
The goal of phase 2 was to refine and prioritize the proposed survey items identified in phase 1 using a modified e-Delphi approach to achieve consensus among an expert panel [ 26 ]. Items from phase 1 were presented to an expert faculty panel using a Qualtrics (Provo, UT) online survey. Panel members were asked to review each item to determine if it should be: included, excluded or adapted for the survey. When adapted was selected faculty experts were asked to provide rationale and suggestions for adaptation through the use of an open text box. Items that reached a level of 75% consensus for either inclusion or adaptation were retained [ 25 , 26 ]. New items were categorized and added, and a revised survey was presented to the panel of experts in round 2. Panel members were again asked to review items, including new items, to determine if it should be: included, excluded, or adapted for the survey. Round 2 of the modified e-Delphi approach also included an item prioritization activity, where participants were then asked to rate the importance of each item, based on a 5-point Likert scale (low to high importance), which De Vaus [ 30 ] states is helpful for increasing the reliability of responses. Items that reached a 75% consensus on inclusion were then considered in relation to the importance it was given by the expert panel. Quantitative data were managed using SPSS (IBM Corp).
Phase 3. Face validity through cognitive interviews with nursing students
The goal of phase 3 was to obtain initial face validity of the proposed survey using a sample of nursing student informants. More specifically, student participants were asked to discuss how items were interpreted, to identify confusing wording or other problematic construction of items, and to provide feedback about the survey as a whole including readability and organization [ 31 , 32 , 33 ]. The focus group was held online and audio recorded. A semi-structured interview guide was developed for this study that focused on clarity, meaning, order and wording of questions; emotions evoked by the questions; and overall survey cohesion and length was used to obtain data (see Supplementary Material 2 for the interview guide). A prompt to “think aloud” was used to limit interviewer-imposed bias and encourage participants to describe their thoughts and response to a given item as they reviewed survey items [ 27 ]. Where needed, verbal probes such as “could you expand on that” were used to encourage participants to expand on their responses [ 27 ]. Student participants’ feedback was collated verbatim and presented to the research team where potential survey modifications were negotiated and finalized among team members. Conventional content analysis [ 34 ] of focus group data was conducted to identify key themes that emerged through discussion with students. Themes were derived from the data by grouping common responses and then using those common responses to modify survey items.
Ten nursing faculty participated in the expert panel. Eight of the 10 faculty self-identified as female. No faculty panel members reported conscientious objector status and ninety percent reported general agreement with MAiD with one respondent who indicated their view as “unsure.” Six of the 10 faculty experts had 16 years of experience or more working as a nurse educator.
Five nursing students participated in the cognitive interview focus group. The duration of the focus group was 2.5 h. All participants identified that they were born in Canada, self-identified as female (one preferred not to say) and reported having received some instruction about MAiD as part of their nursing curriculum. See Tables 1 and 2 for the demographic descriptors of the study sample. Study results will be reported in accordance with the study phases. See Fig. 1 for an overview of the results from each phase.
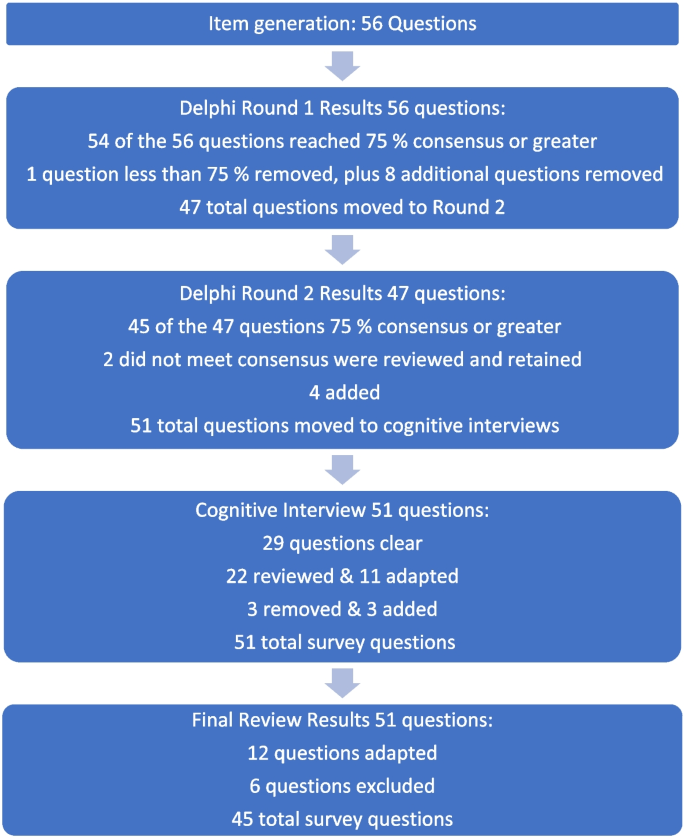
Fig. 1 Overview of survey development findings
Phase 1: survey item generation
Review of the literature identified that no existing survey was available for use with nursing students in the Canadian context. However, an analysis of themes across qualitative and quantitative studies of physicians, medical students, nurses, and nursing students provided sufficient data to develop a preliminary set of items suitable for adaptation to a population of nursing students.
Four major themes and factors that influence knowledge, attitudes, and beliefs about MAiD were evident from the literature: (i) endogenous or individual factors such as age, gender, personally held values, religion, religiosity, and/or spirituality [ 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ], (ii) experience with death and dying in personal and/or professional life [ 35 , 40 , 41 , 43 , 44 , 45 ], (iii) training including curricular instruction about clinical role, scope of practice, or the law [ 23 , 36 , 39 ], and (iv) exogenous or social factors such as the influence of key leaders, colleagues, friends and/or family, professional and licensure organizations, support within professional settings, and/or engagement in MAiD in an interdisciplinary team context [ 9 , 35 , 46 ].
Studies of nursing students also suggest overlap across these categories. For example, value for patient autonomy [ 23 ] and the moral complexity of decision-making [ 37 ] are important factors that contribute to attitudes about MAiD and may stem from a blend of personally held values coupled with curricular content, professional training and norms, and clinical exposure. For example, students report that participation in end of life care allows for personal growth, shifts in perception, and opportunities to build therapeutic relationships with their clients [ 44 , 47 , 48 ].
Preliminary items generated from the literature resulted in 56 questions from 11 published sources (See Table 3 ). These items were constructed across four main categories: (i) socio-demographic questions; (ii) end of life care questions; (iii) knowledge about MAiD; or (iv) comfort and willingness to participate in MAiD. Knowledge questions were refined to reflect current MAiD legislation, policies, and regulatory frameworks. Falconer [ 39 ] and Freeman [ 45 ] studies were foundational sources for item selection. Additionally, four case studies were written to reflect the most recent anticipated changes to MAiD legislation and all used the same open-ended core questions to address respondents’ perspectives about the patient’s right to make the decision, comfort in assisting a physician or NP to administer MAiD in that scenario, and hypothesized comfort about serving as a primary provider if qualified as an NP in future. Response options for the survey were also constructed during this stage and included: open text, categorical, yes/no , and Likert scales.
Phase 2: faculty expert panel review
Of the 56 items presented to the faculty panel, 54 questions reached 75% consensus. However, based upon the qualitative responses 9 items were removed largely because they were felt to be repetitive. Items that generated the most controversy were related to measuring religion and spirituality in the Canadian context, defining end of life care when there is no agreed upon time frames (e.g., last days, months, or years), and predicting willingness to be involved in a future events – thus predicting their future selves. Phase 2, round 1 resulted in an initial set of 47 items which were then presented back to the faculty panel in round 2.
Of the 47 initial questions presented to the panel in round 2, 45 reached a level of consensus of 75% or greater, and 34 of these questions reached a level of 100% consensus [ 27 ] of which all participants chose to include without any adaptations) For each question, level of importance was determined based on a 5-point Likert scale (1 = very unimportant, 2 = somewhat unimportant, 3 = neutral, 4 = somewhat important, and 5 = very important). Figure 2 provides an overview of the level of importance assigned to each item.
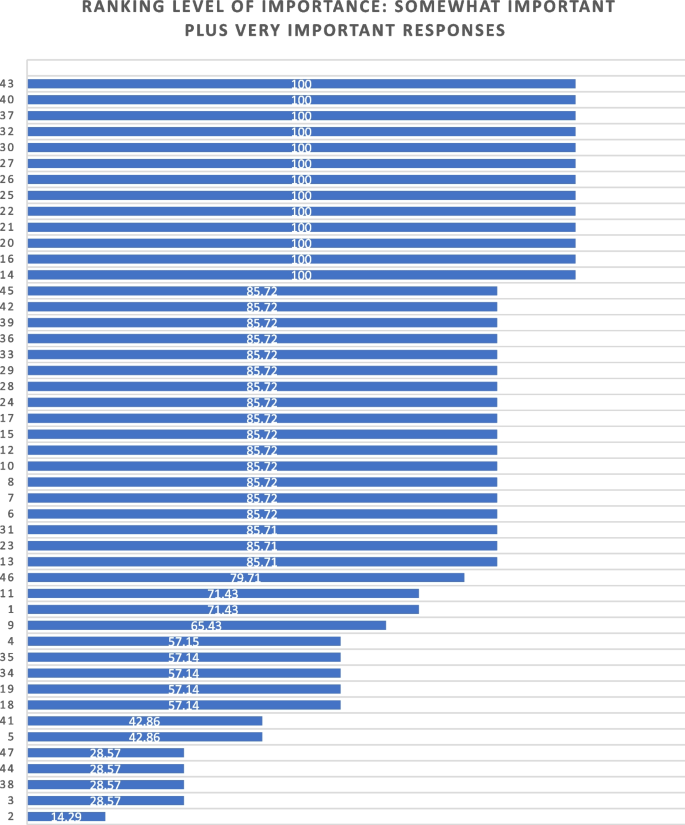
Ranking level of importance for survey items
After round 2, a careful analysis of participant comments and level of importance was completed by the research team. While the main method of survey item development came from participants’ response to the first round of Delphi consensus ratings, level of importance was used to assist in the decision of whether to keep or modify questions that created controversy, or that rated lower in the include/exclude/adapt portion of the Delphi. Survey items that rated low in level of importance included questions about future roles, sex and gender, and religion/spirituality. After deliberation by the research committee, these questions were retained in the survey based upon the importance of these variables in the scientific literature.
Of the 47 questions remaining from Phase 2, round 2, four were revised. In addition, the two questions that did not meet the 75% cut off level for consensus were reviewed by the research team. The first question reviewed was What is your comfort level with providing a MAiD death in the future if you were a qualified NP ? Based on a review of participant comments, it was decided to retain this question for the cognitive interviews with students in the final phase of testing. The second question asked about impacts on respondents’ views of MAiD and was changed from one item with 4 subcategories into 4 separate items, resulting in a final total of 51 items for phase 3. The revised survey was then brought forward to the cognitive interviews with student participants in Phase 3. (see Supplementary Material 1 for a complete description of item modification during round 2).
Phase 3. Outcomes of cognitive interview focus group
Of the 51 items reviewed by student participants, 29 were identified as clear with little or no discussion. Participant comments for the remaining 22 questions were noted and verified against the audio recording. Following content analysis of the comments, four key themes emerged through the student discussion: unclear or ambiguous wording; difficult to answer questions; need for additional response options; and emotional response evoked by questions. An example of unclear or ambiguous wording was a request for clarity in the use of the word “sufficient” in the context of assessing an item that read “My nursing education has provided sufficient content about the nursing role in MAiD.” “Sufficient” was viewed as subjective and “laden with…complexity that distracted me from the question.” The group recommended rewording the item to read “My nursing education has provided enough content for me to care for a patient considering or requesting MAiD.”
An example of having difficulty answering questions related to limited knowledge related to terms used in the legislation such as such as safeguards , mature minor , eligibility criteria , and conscientious objection. Students were unclear about what these words meant relative to the legislation and indicated that this lack of clarity would hamper appropriate responses to the survey. To ensure that respondents are able to answer relevant questions, student participants recommended that the final survey include explanation of key terms such as mature minor and conscientious objection and an overview of current legislation.
Response options were also a point of discussion. Participants noted a lack of distinction between response options of unsure and unable to say . Additionally, scaling of attitudes was noted as important since perspectives about MAiD are dynamic and not dichotomous “agree or disagree” responses. Although the faculty expert panel recommended the integration of the demographic variables of religious and/or spiritual remain as a single item, the student group stated a preference to have religion and spirituality appear as separate items. The student focus group also took issue with separate items for the variables of sex and gender, specifically that non-binary respondents might feel othered or “outed” particularly when asked to identify their sex. These variables had been created based upon best practices in health research but students did not feel they were appropriate in this context [ 49 ]. Finally, students agreed with the faculty expert panel in terms of the complexity of projecting their future involvement as a Nurse Practitioner. One participant stated: “I certainly had to like, whoa, whoa, whoa. Now let me finish this degree first, please.” Another stated, “I'm still imagining myself, my future career as an RN.”
Finally, student participants acknowledged the array of emotions that some of the items produced for them. For example, one student described positive feelings when interacting with the survey. “Brought me a little bit of feeling of joy. Like it reminded me that this is the last piece of independence that people grab on to.” Another participant, described the freedom that the idea of an advance request gave her. “The advance request gives the most comfort for me, just with early onset Alzheimer’s and knowing what it can do.” But other participants described less positive feelings. For example, the mature minor case study yielded a comment: “This whole scenario just made my heart hurt with the idea of a child requesting that.”
Based on the data gathered from the cognitive interview focus group of nursing students, revisions were made to 11 closed-ended questions (see Table 4 ) and 3 items were excluded. In the four case studies, the open-ended question related to a respondents’ hypothesized actions in a future role as NP were removed. The final survey consists of 45 items including 4 case studies (see Supplementary Material 3 ).
The aim of this study was to develop and validate a survey that can be used to track the growth of knowledge about MAiD among nursing students over time, inform training programs about curricular needs, and evaluate attitudes and willingness to participate in MAiD at time-points during training or across nursing programs over time.
The faculty expert panel and student participants in the cognitive interview focus group identified a need to establish core knowledge of the terminology and legislative rules related to MAiD. For example, within the cognitive interview group of student participants, several acknowledged lack of clear understanding of specific terms such as “conscientious objector” and “safeguards.” Participants acknowledged discomfort with the uncertainty of not knowing and their inclination to look up these terms to assist with answering the questions. This survey can be administered to nursing or pre-nursing students at any phase of their training within a program or across training programs. However, in doing so it is important to acknowledge that their baseline knowledge of MAiD will vary. A response option of “not sure” is important and provides a means for respondents to convey uncertainty. If this survey is used to inform curricular needs, respondents should be given explicit instructions not to conduct online searches to inform their responses, but rather to provide an honest appraisal of their current knowledge and these instructions are included in the survey (see Supplementary Material 3 ).
Some provincial regulatory bodies have established core competencies for entry-level nurses that include MAiD. For example, the BC College of Nurses and Midwives (BCCNM) requires “knowledge about ethical, legal, and regulatory implications of medical assistance in dying (MAiD) when providing nursing care.” (10 p. 6) However, across Canada curricular content and coverage related to end of life care and MAiD is variable [ 23 ]. Given the dynamic nature of the legislation that includes portions of the law that are embargoed until 2024, it is important to ensure that respondents are guided by current and accurate information. As the law changes, nursing curricula, and public attitudes continue to evolve, inclusion of core knowledge and content is essential and relevant for investigators to be able to interpret the portions of the survey focused on attitudes and beliefs about MAiD. Content knowledge portions of the survey may need to be modified over time as legislation and training change and to meet the specific purposes of the investigator.
Given the sensitive nature of the topic, it is strongly recommended that surveys be conducted anonymously and that students be provided with an opportunity to discuss their responses to the survey. A majority of feedback from both the expert panel of faculty and from student participants related to the wording and inclusion of demographic variables, in particular religion, religiosity, gender identity, and sex assigned at birth. These and other demographic variables have the potential to be highly identifying in small samples. In any instance in which the survey could be expected to yield demographic group sizes less than 5, users should eliminate the demographic variables from the survey. For example, the profession of nursing is highly dominated by females with over 90% of nurses who identify as female [ 50 ]. Thus, a survey within a single class of students or even across classes in a single institution is likely to yield a small number of male respondents and/or respondents who report a difference between sex assigned at birth and gender identity. When variables that serve to identify respondents are included, respondents are less likely to complete or submit the survey, to obscure their responses so as not to be identifiable, or to be influenced by social desirability bias in their responses rather than to convey their attitudes accurately [ 51 ]. Further, small samples do not allow for conclusive analyses or interpretation of apparent group differences. Although these variables are often included in surveys, such demographics should be included only when anonymity can be sustained. In small and/or known samples, highly identifying variables should be omitted.
There are several limitations associated with the development of this survey. The expert panel was comprised of faculty who teach nursing students and are knowledgeable about MAiD and curricular content, however none identified as a conscientious objector to MAiD. Ideally, our expert panel would have included one or more conscientious objectors to MAiD to provide a broader perspective. Review by practitioners who participate in MAiD, those who are neutral or undecided, and practitioners who are conscientious objectors would ensure broad applicability of the survey. This study included one student cognitive interview focus group with 5 self-selected participants. All student participants had held discussions about end of life care with at least one patient, 4 of 5 participants had worked with a patient who requested MAiD, and one had been present for a MAiD death. It is not clear that these participants are representative of nursing students demographically or by experience with end of life care. It is possible that the students who elected to participate hold perspectives and reflections on patient care and MAiD that differ from students with little or no exposure to end of life care and/or MAiD. However, previous studies find that most nursing students have been involved with end of life care including meaningful discussions about patients’ preferences and care needs during their education [ 40 , 44 , 47 , 48 , 52 ]. Data collection with additional student focus groups with students early in their training and drawn from other training contexts would contribute to further validation of survey items.
Future studies should incorporate pilot testing with small sample of nursing students followed by a larger cross-program sample to allow evaluation of the psychometric properties of specific items and further refinement of the survey tool. Consistent with literature about the importance of leadership in the context of MAiD [ 12 , 53 , 54 ], a study of faculty knowledge, beliefs, and attitudes toward MAiD would provide context for understanding student perspectives within and across programs. Additional research is also needed to understand the timing and content coverage of MAiD across Canadian nurse training programs’ curricula.
The implementation of MAiD is complex and requires understanding of the perspectives of multiple stakeholders. Within the field of nursing this includes clinical providers, educators, and students who will deliver clinical care. A survey to assess nursing students’ attitudes toward and willingness to participate in MAiD in the Canadian context is timely, due to the legislation enacted in 2016 and subsequent modifications to the law in 2021 with portions of the law to be enacted in 2027. Further development of this survey could be undertaken to allow for use in settings with practicing nurses or to allow longitudinal follow up with students as they enter practice. As the Canadian landscape changes, ongoing assessment of the perspectives and needs of health professionals and students in the health professions is needed to inform policy makers, leaders in practice, curricular needs, and to monitor changes in attitudes and practice patterns over time.
Availability of data and materials
The datasets used and/or analysed during the current study are not publicly available due to small sample sizes, but are available from the corresponding author on reasonable request.
Abbreviations
British Columbia College of Nurses and Midwives
Medical assistance in dying
Nurse practitioner
Registered nurse
University of British Columbia Okanagan
Nicol J, Tiedemann M. Legislative Summary: Bill C-14: An Act to amend the Criminal Code and to make related amendments to other Acts (medical assistance in dying). Available from: https://lop.parl.ca/staticfiles/PublicWebsite/Home/ResearchPublications/LegislativeSummaries/PDF/42-1/c14-e.pdf .
Downie J, Scallion K. Foreseeably unclear. The meaning of the “reasonably foreseeable” criterion for access to medical assistance in dying in Canada. Dalhousie Law J. 2018;41(1):23–57.
Nicol J, Tiedeman M. Legislative summary of Bill C-7: an act to amend the criminal code (medical assistance in dying). Ottawa: Government of Canada; 2021.
Google Scholar
Council of Canadian Academies. The state of knowledge on medical assistance in dying where a mental disorder is the sole underlying medical condition. Ottawa; 2018. Available from: https://cca-reports.ca/wp-content/uploads/2018/12/The-State-of-Knowledge-on-Medical-Assistance-in-Dying-Where-a-Mental-Disorder-is-the-Sole-Underlying-Medical-Condition.pdf .
Council of Canadian Academies. The state of knowledge on advance requests for medical assistance in dying. Ottawa; 2018. Available from: https://cca-reports.ca/wp-content/uploads/2019/02/The-State-of-Knowledge-on-Advance-Requests-for-Medical-Assistance-in-Dying.pdf .
Council of Canadian Academies. The state of knowledge on medical assistance in dying for mature minors. Ottawa; 2018. Available from: https://cca-reports.ca/wp-content/uploads/2018/12/The-State-of-Knowledge-on-Medical-Assistance-in-Dying-for-Mature-Minors.pdf .
Health Canada. Third annual report on medical assistance in dying in Canada 2021. Ottawa; 2022. [cited 2023 Oct 23]. Available from: https://www.canada.ca/en/health-canada/services/medical-assistance-dying/annual-report-2021.html .
Banner D, Schiller CJ, Freeman S. Medical assistance in dying: a political issue for nurses and nursing in Canada. Nurs Philos. 2019;20(4): e12281.
Article PubMed Google Scholar
Pesut B, Thorne S, Stager ML, Schiller CJ, Penney C, Hoffman C, et al. Medical assistance in dying: a review of Canadian nursing regulatory documents. Policy Polit Nurs Pract. 2019;20(3):113–30.
Article PubMed PubMed Central Google Scholar
College of Registered Nurses of British Columbia. Scope of practice for registered nurses [Internet]. Vancouver; 2018. Available from: https://www.bccnm.ca/Documents/standards_practice/rn/RN_ScopeofPractice.pdf .
Pesut B, Thorne S, Schiller C, Greig M, Roussel J, Tishelman C. Constructing good nursing practice for medical assistance in dying in Canada: an interpretive descriptive study. Global Qual Nurs Res. 2020;7:2333393620938686. https://doi.org/10.1177/2333393620938686 .
Article Google Scholar
Pesut B, Thorne S, Schiller CJ, Greig M, Roussel J. The rocks and hard places of MAiD: a qualitative study of nursing practice in the context of legislated assisted death. BMC Nurs. 2020;19:12. https://doi.org/10.1186/s12912-020-0404-5 .
Pesut B, Greig M, Thorne S, Burgess M, Storch JL, Tishelman C, et al. Nursing and euthanasia: a narrative review of the nursing ethics literature. Nurs Ethics. 2020;27(1):152–67.
Pesut B, Thorne S, Storch J, Chambaere K, Greig M, Burgess M. Riding an elephant: a qualitative study of nurses’ moral journeys in the context of Medical Assistance in Dying (MAiD). Journal Clin Nurs. 2020;29(19–20):3870–81.
Lamb C, Babenko-Mould Y, Evans M, Wong CA, Kirkwood KW. Conscientious objection and nurses: results of an interpretive phenomenological study. Nurs Ethics. 2018;26(5):1337–49.
Wright DK, Chan LS, Fishman JR, Macdonald ME. “Reflection and soul searching:” Negotiating nursing identity at the fault lines of palliative care and medical assistance in dying. Social Sci & Med. 2021;289: 114366.
Beuthin R, Bruce A, Scaia M. Medical assistance in dying (MAiD): Canadian nurses’ experiences. Nurs Forum. 2018;54(4):511–20.
Bruce A, Beuthin R. Medically assisted dying in Canada: "Beautiful Death" is transforming nurses' experiences of suffering. The Canadian J Nurs Res | Revue Canadienne de Recherche en Sci Infirmieres. 2020;52(4):268–77. https://doi.org/10.1177/0844562119856234 .
Canadian Nurses Association. Code of ethics for registered nurses. Ottawa; 2017. Available from: https://www.cna-aiic.ca/en/nursing/regulated-nursing-in-canada/nursing-ethics .
Canadian Nurses Association. National nursing framework on Medical Assistance in Dying in Canada. Ottawa: 2017. Available from: https://www.virtualhospice.ca/Assets/cna-national-nursing-framework-on-maidEng_20170216155827.pdf .
Pesut B, Thorne S, Greig M. Shades of gray: conscientious objection in medical assistance in dying. Nursing Inq. 2020;27(1): e12308.
Durojaiye A, Ryan R, Doody O. Student nurse education and preparation for palliative care: a scoping review. PLoS ONE. 2023. https://doi.org/10.1371/journal.pone.0286678 .
McMechan C, Bruce A, Beuthin R. Canadian nursing students’ experiences with medical assistance in dying | Les expériences d’étudiantes en sciences infirmières au regard de l’aide médicale à mourir. Qual Adv Nurs Educ - Avancées en Formation Infirmière. 2019;5(1). https://doi.org/10.17483/2368-6669.1179 .
Adler M, Ziglio E. Gazing into the oracle. The Delphi method and its application to social policy and public health. London: Jessica Kingsley Publishers; 1996
Keeney S, Hasson F, McKenna H. Consulting the oracle: ten lessons from using the Delphi technique in nursing research. J Adv Nurs. 2006;53(2):205–12.
Keeney S, Hasson F, McKenna H. The Delphi technique in nursing and health research. 1st ed. City: Wiley; 2011.
Willis GB. Cognitive interviewing: a tool for improving questionnaire design. 1st ed. Thousand Oaks, Calif: Sage; 2005. ISBN: 9780761928041
Lamb C, Evans M, Babenko-Mould Y, Wong CA, Kirkwood EW. Conscience, conscientious objection, and nursing: a concept analysis. Nurs Ethics. 2017;26(1):37–49.
Lamb C, Evans M, Babenko-Mould Y, Wong CA, Kirkwood K. Nurses’ use of conscientious objection and the implications of conscience. J Adv Nurs. 2018;75(3):594–602.
de Vaus D. Surveys in social research. 6th ed. Abingdon, Oxon: Routledge; 2014.
Boateng GO, Neilands TB, Frongillo EA, Melgar-Quiñonez HR, Young SL. Best practices for developing and validating scales for health, social, and behavioral research: A primer. Front Public Health. 2018;6:149. https://doi.org/10.3389/fpubh.2018.00149 .
Puchta C, Potter J. Focus group practice. 1st ed. London: Sage; 2004.
Book Google Scholar
Streiner DL, Norman GR, Cairney J. Health measurement scales: a practical guide to their development and use. 5th ed. Oxford: Oxford University Press; 2015.
Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Adesina O, DeBellis A, Zannettino L. Third-year Australian nursing students’ attitudes, experiences, knowledge, and education concerning end-of-life care. Int J of Palliative Nurs. 2014;20(8):395–401.
Bator EX, Philpott B, Costa AP. This moral coil: a cross-sectional survey of Canadian medical student attitudes toward medical assistance in dying. BMC Med Ethics. 2017;18(1):58.
Beuthin R, Bruce A, Scaia M. Medical assistance in dying (MAiD): Canadian nurses’ experiences. Nurs Forum. 2018;53(4):511–20.
Brown J, Goodridge D, Thorpe L, Crizzle A. What is right for me, is not necessarily right for you: the endogenous factors influencing nonparticipation in medical assistance in dying. Qual Health Res. 2021;31(10):1786–1800.
Falconer J, Couture F, Demir KK, Lang M, Shefman Z, Woo M. Perceptions and intentions toward medical assistance in dying among Canadian medical students. BMC Med Ethics. 2019;20(1):22.
Green G, Reicher S, Herman M, Raspaolo A, Spero T, Blau A. Attitudes toward euthanasia—dual view: Nursing students and nurses. Death Stud. 2022;46(1):124–31.
Hosseinzadeh K, Rafiei H. Nursing student attitudes toward euthanasia: a cross-sectional study. Nurs Ethics. 2019;26(2):496–503.
Ozcelik H, Tekir O, Samancioglu S, Fadiloglu C, Ozkara E. Nursing students’ approaches toward euthanasia. Omega (Westport). 2014;69(1):93–103.
Canning SE, Drew C. Canadian nursing students’ understanding, and comfort levels related to medical assistance in dying. Qual Adv Nurs Educ - Avancées en Formation Infirmière. 2022;8(2). https://doi.org/10.17483/2368-6669.1326 .
Edo-Gual M, Tomás-Sábado J, Bardallo-Porras D, Monforte-Royo C. The impact of death and dying on nursing students: an explanatory model. J Clin Nurs. 2014;23(23–24):3501–12.
Freeman LA, Pfaff KA, Kopchek L, Liebman J. Investigating palliative care nurse attitudes towards medical assistance in dying: an exploratory cross-sectional study. J Adv Nurs. 2020;76(2):535–45.
Brown J, Goodridge D, Thorpe L, Crizzle A. “I am okay with it, but I am not going to do it:” the exogenous factors influencing non-participation in medical assistance in dying. Qual Health Res. 2021;31(12):2274–89.
Dimoula M, Kotronoulas G, Katsaragakis S, Christou M, Sgourou S, Patiraki E. Undergraduate nursing students’ knowledge about palliative care and attitudes towards end-of-life care: A three-cohort, cross-sectional survey. Nurs Educ Today. 2019;74:7–14.
Matchim Y, Raetong P. Thai nursing students’ experiences of caring for patients at the end of life: a phenomenological study. Int J Palliative Nurs. 2018;24(5):220–9.
Canadian Institute for Health Research. Sex and gender in health research [Internet]. Ottawa: CIHR; 2021 [cited 2023 Oct 23]. Available from: https://cihr-irsc.gc.ca/e/50833.html .
Canadian Nurses’ Association. Nursing statistics. Ottawa: CNA; 2023 [cited 2023 Oct 23]. Available from: https://www.cna-aiic.ca/en/nursing/regulated-nursing-in-canada/nursing-statistics .
Krumpal I. Determinants of social desirability bias in sensitive surveys: a literature review. Qual Quant. 2013;47(4):2025–47. https://doi.org/10.1007/s11135-011-9640-9 .
Ferri P, Di Lorenzo R, Stifani S, Morotti E, Vagnini M, Jiménez Herrera MF, et al. Nursing student attitudes toward dying patient care: a European multicenter cross-sectional study. Acta Bio Medica Atenei Parmensis. 2021;92(S2): e2021018.
PubMed PubMed Central Google Scholar
Beuthin R, Bruce A. Medical assistance in dying (MAiD): Ten things leaders need to know. Nurs Leadership. 2018;31(4):74–81.
Thiele T, Dunsford J. Nurse leaders’ role in medical assistance in dying: a relational ethics approach. Nurs Ethics. 2019;26(4):993–9.
Download references
Acknowledgements
We would like to acknowledge the faculty and students who generously contributed their time to this work.
JS received a student traineeship through the Principal Research Chairs program at the University of British Columbia Okanagan.
Author information
Authors and affiliations.
School of Health and Human Services, Selkirk College, Castlegar, BC, Canada
Jocelyn Schroeder & Barbara Pesut
School of Nursing, University of British Columbia Okanagan, Kelowna, BC, Canada
Barbara Pesut, Lise Olsen, Nelly D. Oelke & Helen Sharp
You can also search for this author in PubMed Google Scholar
Contributions
JS made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and drafting and substantively revising the work. JS has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. BP made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and drafting and substantively revising the work. BP has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. LO made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and substantively revising the work. LO has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. NDO made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and substantively revising the work. NDO has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. HS made substantial contributions to drafting and substantively revising the work. HS has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Authors’ information
JS conducted this study as part of their graduate requirements in the School of Nursing, University of British Columbia Okanagan.
Corresponding author
Correspondence to Barbara Pesut .
Ethics declarations
Ethics approval and consent to participate.
The research was approved by the Selkirk College Research Ethics Board (REB) ID # 2021–011 and the University of British Columbia Behavioral Research Ethics Board ID # H21-01181.
All participants provided written and informed consent through approved consent processes. Research was conducted in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Schroeder, J., Pesut, B., Olsen, L. et al. Developing a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in Medical Assistance in Dying (MAiD): a mixed method modified e-Delphi study. BMC Nurs 23 , 326 (2024). https://doi.org/10.1186/s12912-024-01984-z
Download citation
Received : 24 October 2023
Accepted : 28 April 2024
Published : 14 May 2024
DOI : https://doi.org/10.1186/s12912-024-01984-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical assistance in dying (MAiD)
- End of life care
- Student nurses
- Nursing education
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Minority Nurse
- Springer Publishing Company
- Springer Publishing Connect
- Faculty Nurse
- Nursing Diversity
- Neonatal Network

What, Why, How of Clinical Judgment
May 16, 2024 | Blog , Clinical Nurse Leader , News , Nurse educators , Nursing Students

Clinical judgment is a hot topic in nurse education right now! The NCSBN’s NCSBN’s Next-Gen Clinical Judgment Measurement Model (CJMM) is the new standard for safe clinical practice. The NCSBN research found that nursing students and newly licensed nurses may lack clinical judgment, a true cornerstone of safe practice.
According to Hoffman, “The two most common reasons that new graduate nurses are disciplined are (1) failure to notice changes in patient status and (2) failure to act when a patient is deteriorating” (2024, 3). This is a sobering report. How can the CJMM help students and newly licensed nurses enter with steady intention into their careers with confidence and competence? The answer is curiosity.
There are five components of clinical judgment in the CJMM: recognize cues, analyze cues, prioritize hypotheses, take actions, and evaluate outcomes (NCSBN, 2019). When addressed in an orderly fashion, these elements can help the nurse make better clinical decisions. Let’s ask ourselves three simple questions to guide us through this model: What? Why? How?
As a nurse educator , I ask students, “Why?” more frequently than they wish, I’m sure. The more they answer that question, the more they make connections between the what, or subject matter, and the how or the actions that may address those findings. This vital principle of connection allows decisions based on understanding and leaves little room for assumption. I have created a graphic using the five domains of the CJMM to help us ask some critical questions and lead us toward good clinical decisions.

Curiosity Invites Connection
A seasoned nurse knows through experience the cues of a deteriorating patient, but unfortunately, we cannot transfer our knowledge to our students, peers, or mentees. We can, however, thoughtfully unravel the process by which we understand that a patient has had a status change. For a novice nurse , this process may take more time and require confirmation by another. For a well-experienced nurse, this could take mere seconds. What happened? Why did it happen? How do I address it?
Curiosity Keeps Us Cautious
Using these three simple words to begin each series of questions can be a guide to any nurse who needs to gain confidence and competence in clinical decision-making . At their most simplistic, these questions can keep us moving forward in decision-making rather than being stuck in indecision. We notice systematically that the what leads to the why, and the why guides us to the how. We cannot forsake any step in this process lest our patients receive incorrect treatment or unsafe nursing actions.
Curiosity Helps Us Care
Identifying the gap in clinical judgment offers an opportunity for students, educators, and all nurses to examine our processes and practices of inquiry. Learning this process, like any other, requires repetition and intention. You can make better choices when you ask better questions. Whether you are a student, a staff nurse, or an educator, I hope that the What? Why? How? of clinical judgment will help you as you continue forward in your nursing career. Keep learning.
Stay curious!
Hoffman, Janice J., and Nancy J. Sullivan. “Foundations for Medical-Surgical Nursing.” Essay. In Davis Advantage for Medical-Surgical Nursing: Making Connections to Practice , 3rd ed. Philadelphia: F.A. Davis Company, 2024.
NCSBN. Clinical Judgment Measurement Model. Accessed January 23, 2024. https://nclex.com/clinical-judgment-measurement-model.page .
- Recent Posts
- What, Why, How of Clinical Judgment - May 16, 2024
- facebook.com/nurseloop
- https://www.linkedin.com/company/83002777

IMAGES
VIDEO
COMMENTS
Between January 2022 (Volume 31, Issue 1) and the current May 2023 journal issue (Volume 32, Issue 3), AJCC published 71 reports of original research. These recent papers addressed a wide range of research topics, including bedside patient care, palliative and end-of-life care, intensive care unit (ICU) survivorship, measurement and prediction of patient problems, family concerns ...
1. Clinical Nursing Research Topics. Analyze the use of telehealth/virtual nursing to reduce inpatient nurse duties. Discuss the impact of evidence-based respiratory interventions on patient outcomes in critical care settings. Explore the effectiveness of pain management protocols in pediatric patients. 2.
Explore the latest full-text research PDFs, articles, conference papers, preprints and more on CRITICAL CARE NURSING. Find methods information, sources, references or conduct a literature review ...
Critical Care Medicine. Explore the latest in critical care medicine, including management of respiratory failure, sepsis, HAI prevention, end-of-life care, and more. This cohort study compares 90-day mortality in patients with sepsis who received piperacillin-tazobactam vs cefepime for treatment of sepsis. This cross-sectional study examines ...
There are increasing examples of critical care nurses leading large multicentre trials, 17, 18 and even running their own clinical nursing research laboratory, 19 who have contributed to the evidence base and successfully changed practice. However, these numbers need to increase substantially to keep up with the increasingly diverse and dynamic ...
Nursing in Critical Care publishes articles on all aspects of critical care nursing practice, research, education and management. The journal is concerned with the whole spectrum of skills, knowledge and attitudes utilised by practitioners in any setting where adults or children and their families are experiencing critical illness.
The aims of Intensive and Critical Care Nursing are to promote excellence of care of critically ill patients by specialist nurses and their professional colleagues; to provide an international and interdisciplinary forum for the publication, dissemination and exchange of research findings, experience and ideas; to develop and enhance the knowledge, skills, attitudes and creative thinking ...
The research was planned as a quasi-experimental to increase the compliance and feasibility of nurses in the implementation of the preoperative evidence-based care. 2.2 Place and period. This research was carried out with the participation of patients who underwent cardiovascular surgery at a Balikesir University Health Practice and Research ...
Potentiate critical care research both through research funding portfolios and by enhancing knowledge dissemination: Develop real-time updates to clinical practice guidelines: Advocate for equitable and inclusive critical care, particularly in underresourced care settings: Expand and support a global network of critical care professionals
She is dean and professor, School of Nursing and Health Studies, University of Miami, Coral Gables, Florida. 2 Aluko A. Hope is coeditor in chief of the American Journal of Critical Care. He is an associate professor and physician scientist at Oregon Health and Science University in Portland, Oregon. PMID: 37121892. DOI: 10.4037/ajcc2023943.
In standard ICU care, limited communication options for critically ill patients and a lack of integrated family engagement into routine critical care practice contribute to feelings of isolation. 3 During the current COVID-19 crises, nurses and physicians have needed to use technology ad hoc to allow family to see or interact remotely with ...
Background. The Institute of Medicine (IOM) has recommended that Evidence-Based Practice (EBP) be used in 90% of clinical decisions by 2020 [].EBP has become a popular buzzword in the healthcare industry [1, 2].This concept is defined as a problem-solving process in clinical decision making, which combines best research evidence with clinical expertise, patient preference, and clinical guidelines.
The need for nursing research on assessing and improving patient-family communication, advocacy, and engagement in critical care setting (e.g., during mechanical ventilation) was recognized previously as a nursing research priority (3, 17).
HOT TOPICS IN CRITICAL CARE MEDICINE. Home > ATS Conferences > ATS 2018. American Journal of Respiratory and Critical Care Medicine 2018, Volume 197 Conference Abstracts ... Potential Mechanisms of Physician-Attributable Variation in Critical Care. J. Hart, K.N. Yadav, M. Josephs, ...
The AACN is the largest specialty organization in the world, representing over 125,000 progressive and critical care nurses. The AACN offers resources, education, and support to enhance its members' careers. It is also a leader in advancing evidence-based guidelines that allow nurses to deliver optimal patient care.
S. Ehrmann and OthersN Engl J Med 2023;389:2052-2062. In a randomized trial involving critically ill patients who had undergone mechanical ventilation for 3 days, a 3-day course of inhaled ...
Purpose: To examine the status of critical care nursing internationally, assess the impact of the COVID-19 pandemic, and identify research priorities by surveying professional critical care nursing organizations (CCNOs) worldwide. Design: A descriptive survey methodology was used. This study is the sixth worldwide quadrennial review to assess international critical care nursing needs and ...
The Range of Critical Care Nursing Research Paper Topics. Critical care nursing is a specialized area of nursing that is dedicated to meeting the needs of patients and families facing life-threatening illnesses or injuries. This involves not only managing acute and often complex health issues but also addressing the psychosocial and ...
Dear Colleagues, The main purpose of this Special Issue is to present scientific evidence regarding multidimensional nursing care provided in Intensive Care Units (ICUs). Intensive and critical care nurses play a vital role in the whole process of treatment and care for patients in different critical health conditions.
Critical Care Topics. Antibiotic Resistance. Clostridium difficile Infection. Coronavirus (COVID-19) Critical Care Nursing. Ebola. Hospital Medicine. Mechanical Ventilation. Methicillin-Resistant ...
Here is the list of Critical Care Nursing Research Topics and titles for college students. Analyzing the importance of timings in the critical care nursing areas. Probing the essential role of nursing - a literature review. Literature review on critical nursing analysis in the past 10 years. Examining the strategies of management of acute ...
LWW
Background: As patient needs become more complex in the critical care setting, nurses with increased clinical expertise are needed to expand the research knowledge base and apply existing knowledge in practice settings. Purpose: To review opportunities and resources that are available to facilitate nurses' involvement in critical care research: opportunities for participation in research ...
1. Introduction. In intensive care units (ICU), communication between nurses and patients is crucial to facilitate each individual`s understanding of the other`s thoughts, feelings and opinions, and to humanize care in the ICU, which may be experienced as an unfriendly environment (Kvande et al., Citation 2022).For the intensive care nurse (ICN), communication with the patient is important to ...
Caring for the critical care patient includes understanding common medication therapies for complex diagnosis. This course will review common medications and nursing considerations for administration. Concept review and case scenarios include patients with heart failure, acute coronary syndrome and frequently seen therapies including anticoagulation.
Historically, nursing services have been bundled into the general costs of health care, much like hospital supplies, leading to undervaluation and lack of visibility in the billing process. This commission, led by co-chairs Rebecca Love, RN, BS, MSN, FIEL, and Sharon Pearce, DNP, CRNA, FAANA, FAAN, was formed in response to a critical staffing ...
As nursing education also continues to evolve to meet the demands of the health care system, all levels of nurses are being exposed to research through their education programs and work environments. We often hear potential students talk about having an interest in research as a nurse, but are hesitant because they don't have a specific ...
Background Medical Assistance in Dying (MAiD) was legalized in Canada in 2016. Canada's legislation is the first to permit Nurse Practitioners (NP) to serve as independent MAiD assessors and providers. Registered Nurses' (RN) also have important roles in MAiD that include MAiD care coordination; client and family teaching and support, MAiD procedural quality; healthcare provider and public ...
Clinical judgment is a hot topic in nurse education right now! The NCSBN's NCSBN's Next-Gen Clinical Judgment Measurement Model (CJMM) is the new standard for safe clinical practice. The NCSBN research found that nursing students and newly licensed nurses may lack clinical judgment, a true cornerstone of safe practice. According to Hoffman, "The two most