- Open access
- Published: 08 May 2024

Advances and challenges of the cell-based therapies among diabetic patients
- Ramin Raoufinia 1 , 2 ,
- Hamid Reza Rahimi 2 ,
- Ehsan Saburi 2 &
- Meysam Moghbeli ORCID: orcid.org/0000-0001-9680-0309 2
Journal of Translational Medicine volume 22 , Article number: 435 ( 2024 ) Cite this article
407 Accesses
Metrics details
Diabetes mellitus is a significant global public health challenge, with a rising prevalence and associated morbidity and mortality. Cell therapy has evolved over time and holds great potential in diabetes treatment. In the present review, we discussed the recent progresses in cell-based therapies for diabetes that provides an overview of islet and stem cell transplantation technologies used in clinical settings, highlighting their strengths and limitations. We also discussed immunomodulatory strategies employed in cell therapies. Therefore, this review highlights key progresses that pave the way to design transformative treatments to improve the life quality among diabetic patients.
Diabetes mellitus poses a formidable global public health challenge due to its rapid growing prevalence and associated morbidity, disability, and mortality [ 1 ]. According to the International Diabetes Federation, over 537 million adults aged 20–79 had diabetes worldwide in 2021 that is expected to rise to around 783 million cases by 2045 [ 2 ]. Obesity, unhealthy diets, physical inactivity as well as genetic and epigenetic predispositions are important risk factors of diabetes [ 3 , 4 , 5 ]. Diabetes is typically classified into type 1 diabetes mellitus (T1DM), gestational diabetes mellitus (GDM), and type 2 diabetes mellitus (T2DM) [ 2 ]. T1DM primarily arises from autoimmune-related damage of insulin-secreting beta cells, resulting in severe hyperglycemia and ketoacidosis [ 6 ]. In contrast, T2DM generally has a more gradual onset characterized by insulin resistance along with diminished compensatory insulin secretion from pancreatic beta cell dysfunction [ 7 ]. Diabetes is associated with macrovascular complications such as heart disease and stroke, as well as microvascular issues in eyes, kidneys, and nervous system [ 8 ]. Cancer is also a leading cause of diabetes-related death, and dementia-associated mortality has risen in recent decades [ 9 , 10 , 11 , 12 ]. Cell therapy involves transferring autologous or allogenic cellular material into patients [ 13 ]. The global market size of cell therapy is estimated to grow from $9.5 billion in 2021 to $23 billion by 2028 [ 14 ]. It combines stem and non-stem cell therapies consisting of unicellular or multicellular preparations. Cell therapies typically use autologous or allogenic cells via injection and infusion [ 15 ]. In the present review, we discussed the recent advances in cell-based therapy of diabetes, from foundational islet transplantation to regenerative strategies to highlight key developments that improve the effective treatments for diabetic patients.
Cell replacement therapy for diabetes
Pancreatic transplantation was firstly used in 1966 to treat type 1 diabetes using whole organ transplants. During the 1970s–80s, segmental pancreatic grafts were combined with techniques to divert digestive secretions away from transplanted cells. Three main techniques emerged; simultaneous pancreas-kidney transplants, pancreas transplants following kidney transplants, and pancreatic transplants. International collaboration on tracking outcomes began in 1980 with the formation of several pancreatic transplant registries and associations. However, whole organ transplantation was faced with several challenges including organ rejection, vascular complications, limited organ availability, and the effects of lifelong immunosuppression [ 16 , 17 ]. Islet cell transplantation was explored as an alternative, however isolating and transplanting pancreatic islets proved difficult due to donor availability, rejection, and immunosuppression side effects. Recent research has focused on stem cell sources that could reconstitute immune tolerance and preserve beta cell function such as mesenchymal stem cells, bone marrow cells, and embryonic stem cells [ 18 ]. A novel stem cell therapy called VX-880 was developed using proprietary technology to grow insulin-producing beta cells from allogeneic stem cells. Clinical trials began in 2021 after FDA approval to deliver the cells intrahepatically under immune suppression. A second approach called VX-264 encapsulates the same cells, avoiding immunosuppression but requiring surgical implantation [ 17 ]. In 2023, FDA approved the first allogeneic pancreatic islet cell therapy called Lantidra for adults with type 1 diabetes experiencing severe hypoglycemia. Approval was based on two studies where 21–30% of participants no longer required insulin one year post-treatment, with benefits lasting over five years in some cases. However, this treatment have mild and serious adverse events that are associated with treatment dose and the methods of islet cell infusion [ 19 , 20 ].
Emerging strategies for cell delivery via microencapsulation and biological devices in clinical trials
Alginate capsules as cell delivery systems.
A seminal investigation conducted in 1994 demonstrated the successful transplantation of alginate-encapsulated islets into the peritoneum of kidney transplant patients who were receiving immunosuppression therapy. Remarkably, these patients achieved insulin independence for up to nine months [ 21 ]. However, subsequent trials conducted without immunosuppression yielded inconsistent outcomes. In a study conducted in 2006, islets were encapsulated in triple-layer alginate capsules and implanted intraperitoneally in type 1 diabetes (T1D) patients. There was a positive correlation between the encapsulation and insulin production that reduced exogenous insulin requirements during one year. Despite this progress, the entry of cytokines remained a potential concern [ 22 ]. Another study employed the single-layer barium-alginate capsules that sustained insulin production for up to 2.5 years [ 23 ]. It has been reported that the microneedle, comprising a calcium alginate frame with polydopamine-coated poly-lactic-co-glycolic acid microspheres encapsulating insulin, enables light-triggered insulin release. Microneedle provided a suitable insulin dose to maintain blood glucose levels in line with daily fluctuations. These results established the efficacy and safety of the developed microneedle for diabetes treatment [ 24 ]. Another therapeutic approach explored the encapsulation of pancreatic islets with mesenchymal stem cells (MSCs) and decellularized pancreatic extracellular matrix (ECM). ECM derived from the pancreas supported islet cell growth and maintenance to enhance insulin expression [ 25 ]. Sodium alginate and hyaluronic acid were incorporated due to their roles in collagen production, wound healing, and physical crosslinking. The 3D porous membranes allowed optimal water and oxygen transfer while diverting excess exudate from diabetic wounds. Hydrogel accelerated re-epithelization, while decreased inflammation, indicating potential as the diabetic wound dressings [ 26 ]. Additionally, the incorporation of specific ECM components, such as collagen IV and RGD, into alginate-based microcapsules significantly improved the survival, insulin secretion, and longevity of microencapsulated islets [ 27 ].
Encaptra® device from ViaCyte
In contrast to microencapsulation techniques, ViaCyte developed a semipermeable pouch method named Encaptra, which contains pancreatic precursor cells derived from the embryonic stem cells [ 28 ]. In the initial trial conducted in 2014, the “VC-01” device was implanted in T1D individuals without the use of immunosuppression [ 29 ]. The trial confirmed the safety of the device; however, the occurrence of hypoxia induced cellular necrosis [ 30 ]. The device was modified as “VC-02” with larger pores, and two trials (NCT03162926, NCT03163511) demonstrated promising outcomes, including increased fasting C-peptide levels and a 20% reduction in insulin requirements during one year in the majority of participants [ 31 ]. In order to eliminate the necessity for immunosuppressants, ViaCyte collaborated with Gore to develop an expanded polytetrafluoroethylene (ePTFE) device with both immuno-isolating and pro-angiogenic properties [ 32 ]. This device (NCT04678557) aimed to prevent immune cell attachment and T-cell activation [ 33 ]. Additionally, ViaCyte is exploring the integration of CRISPR technology to modify stem cells, specifically by eliminating β2-microglobulin expression and PD-L1 up regulation. It is hypothesized that these genetic modifications will further hinder immune cell attachment and T-cell activation [ 30 , 34 ].
Semipermeable device from Semma therapeutics
Semma Therapeutics, which has been acquired by Vertex, pioneered the utilization of differentiated stem cell-derived islet cell clusters in clinical trials. Semma houses these cells between two semipermeable polyvinylidene fluoride membranes and is designed for subcutaneous implantation (NCT04786262) [ 31 , 35 ]. Vertex reported a significant breakthrough by infusing differentiated beta cells via the portal vein in a participant who was receiving immunosuppressants. This approach led to substantial C-peptide production and improved glycemic control during 90 days [ 36 ].
βAir device from Beta O2
Beta O2’s innovative βAir device utilizes an alginate-PTFE membrane complex to encapsulate islets, providing partial immunoisolation while ensuring a continuous supply of oxygen, which is crucial for optimal islet function [ 37 , 38 ]. The βAir device that was seeded with human islets was subcutaneously implanted in T1D individuals (NCT02064309). Although, low insulin levels were produced for up to eight weeks, there was not any reduction in the required exogenous insulin [ 37 ]. While, increasing the number of islets could potentially enhance their function, it is important to note that the continuous reliance on oxygen poses a risk of infection, despite efforts to optimize the survival of encapsulated islets [ 39 , 40 ].
Cell pouch™ device from Sernova
Sernova has developed the Cell Pouch device, which offers pre-vascularized polypropylene chambers for islet transplantation without the need for immunoprotection. The device consists of multiple cylindrical chambers that are prefilled with PTFE plugs, which are then removed after implantation to create the empty space [ 41 ]. In a 2012 trial (NCT01652911), islets were placed in the vascularized pouches of three recipients who were also receiving immunosuppression that resulted in a transient increase in C-peptide levels [ 41 ]. In a 2018 trial (NCT03513939), immunosuppression was administered after implantation and islet introduction. This trial reported sustained C-peptide production for up to nine months in two recipients, along with improved glycemic control [ 42 ]. Regarding the limitations of immunosuppression, Sernova is exploring the possibility of encapsulating islets in hydrogel as an alternative approach [ 43 ].
Shielded living therapeutics™ from Sigilon Therapeutics
Sigilon has developed the Shielded Living Therapeutics sphere, which consists of cell clusters enclosed within an alginate-TMTD coating [ 44 ]. Preclinical studies demonstrated that murine islet transplants encapsulated within these spheres maintained normoglycemia for a period of six months [ 45 ]. In a 2020 trial conducted for hemophilia (NCT04541628), the spheres were evaluated for their ability to express Factor VIII [ 46 ]. However, the trial was paused due to the development of antibodies in the third recipient receiving the highest cell doses. While, preclinical studies have shown promising efficacy, there are safety concerns regarding the TMTD coating that need to be addressed before these spheres can be used for human islet transplantation as a treatment for diabetes [ 31 ]. Emerging technologies have been investigated in clinical trials for delivering insulin-producing islets or stem cell-derived beta cells via microencapsulation or use of implantable biological devices (Table 1). Optimizing encapsulation and developing alternative implantable devices moves the field toward delivering safe and effective islet replacement without chronic immunosuppression dependency that represented an important new frontier for the cell-based treatment of diabetes. However, continued refining will be required to fully realize this promising vision and using these preclinical concepts in clinic.
Immunoengineering strategies: biomaterials for modulating immune responses
Islet encapsulation aims to prevent immune responses toward transplant antigens. However, foreign body response (FBR) against biomaterials induces inflammation around encapsulated islets that obstructs oxygen/nutrient access and causes graft failure [ 31 ]. Extensive research revealed biomaterial properties profoundly influence FBR severity, with high purity/biocompatibility moderating inflammation [ 47 ]. Deeper understanding of biomaterial immunobiology enabled developing immune-modulating constructs to steer host interactions. By altering topology/chemistry to hinder nonspecific binding and cell adhesion, these “immune-evasive biomaterials” intended to attenuate xenograft rejection at inception [ 44 ]. Both innate and adaptive immune responses have crucial roles in the context of pancreatic islet transplantation. These responses encompass the activation of tissue macrophages and neutrophils following injury, leading to the release of inflammatory cytokines that subsequently activate antigen-presenting cells (APCs), CD8 + T cells, CD4 + T cells, and cytotoxic T lymphocytes (Fig. 1 ). Zwitterionic polymers conferred anti-fouling attributes but crosslinking limitations constrained their application [ 48 ]. Novel mild zwitterionization introduced alginate modifications that prolonged prevention of fibrotic overgrowth by mitigating initial responses [ 49 , 50 , 51 ]. The prevention of graft rejection following islet cell transplantation necessitates the systemic administration of immunosuppressive agents. While, these agents effectively suppress immune responses, their continuous use exposes patients to an increased risk of infection and cancer. To mitigate these concerns, an alternative approach involving the localized delivery of immunosuppressants at the transplantation site has emerged. This localized delivery system offers several advantages, including targeted drug delivery, reduced systemic exposure, and potentially reduces the immunosuppressants doses [ 52 ]. Polymeric carriers dispersed cyclosporine A continuously at the graft site to dynamically tamp down proinflammatory cascades and T-cell activation [ 53 , 54 ]. TGF-β/IL-10 co-delivery at the microencapsulation interface hindered innate antigen presentation, obstructing adaptive response priming [ 55 , 56 ]. Regulatory T-cells emerged as the potent immunomodulators when coated on islets to improve insulin production in vitro [ 57 ]. Similarly, recombinant Jagged-1 surface patterning increased regulatory lymphocytes in vitro while enhancing glycemic oversight in vivo [ 58 ]. Targeting proinflammatory effector T-cells or presenting their Fas ligand death receptor improved long-term viability when combined with rapamycin prophylaxis [ 52 , 59 ]. Immobilizing thrombomodulin or urokinase mitigated local inflammation, with the latter conferring lifelong xenotransplant survival [ 60 ]. Peptides recognizing IL-1 receptors provided robust protection from destabilizing proinflammatory cytokines [ 61 ]. Leukemia inhibiting factor improved islet performance over polyethylene glycol encapsulation alone by inducing regulatory T-cell lineages [ 62 ]. Silk scaffolds facilitated IL-4/dexamethasone emancipation that meaningfully decreased immune reactions to grafts [ 63 ]. Therefore, the localized delivery of immunosuppressants at the transplantation site represents a promising strategy for islet cell transplantation. Compared to systemic administration, local delivery can achieve targeted immune modulation only at the graft location while reducing drug exposure throughout the body. This localized approach aims to sufficiently suppress the immune response to prevent rejection, while limiting negative side effects that may occur from systemic immunosuppression. A variety of biomaterials and surface modification strategies have been developed and investigated for the local delivery of immunosuppressive agents and immunomodulatory cytokines [ 64 , 65 , 66 ]. Understanding how biomaterial properties influence the immune response is critical to design biomaterials that can modulate inflammation and improve islet graft survival through localized immunomodulation.
Cell-based therapy through the integration of additive manufacturing techniques
Additive manufacturing utilizes computer modeling to fabricate complex 3D structures on-site with minimal post-processing. Common methods for the biomedical application are fused filament fabrication (FFF), stereolithography (SLA), and bioprinting [ 67 ]. FFF is a layer-by-layer technique that extrudes heated thermoplastics [ 68 ]. Commonly used feedstocks include acrylonitrile butadiene styrene (ABS) and polylactic acid (PLA). Other thermoplastics that have been utilized with FDM include thermoplastic polyurethane (TPU), polycarbonate (PC), polystyrene (PS), polyetherimide (PEI), polycaprolactone (PCL), polyaryletherketone (PAEK), and polyetheretherketone (PEEK), with the latter demonstrating high strength and heat tolerance. A major advantage of FDM is its ability to fabricate multi-material objects through continuous printing and alteration of the build material. In addition to typical polymers like PC and polystyrene (PS), FDM can print composites reinforced with glass, metals, ceramics, and bioresorbable polymers via integration of the constituent powders with a binding matrix. This enables enhanced control over the experimental component fabrication. While, ceramic and metal filaments traditionally contain the corresponding powder mixed with a binder, FDM provides versatility in the functional prototype construction from a wide range of thermoplastic feedstocks using precise and additive layer manufacture [ 68 , 69 , 70 , 71 , 72 ]. It provides geometric reproducibility and reduced variability compared to traditional techniques. FFF prints served as scaffolds for the transplanted cells [ 67 ]. However, minimum feature size is limited to ? ∼ 250 μm by nozzle diameter [ 68 ]. SLA employs light-curable liquid resins and achieves higher 50–150 μm resolution than FFF but with restricted material choices. Bone grafts and surgical guides are common applications [ 67 ]. Incorporating biomaterials like hydroxyapatite has expanded utility, though processing is required to mitigate cytotoxicity. Additive manufacturing can address limitations in oxygen transport, cell/material placement control and vasculature formation, and clinically translatable insulin-secreting implants [ 67 ]. Therefore, additive manufacturing technologies have the potential to enhance various aspects of the cell-based transplant design, from improving nutrient transport through optimized implant geometry to achieving precision integration of therapeutic agents (Table 2).
Enhancing nutrient transport through optimization of implant geometry
Tissue engineering for the islet transplantation requires maximizing nutrient transport [ 73 , 74 ]. Traditional scaffold fabrication introduces macroporosity but lacks precision that results in inflammation [ 67 ]. Cell encapsulation provides immunoprotection by limiting interactions between transplanted cells and the host immune system. However, this protective barrier also poses challenges for the efficient transport of essential nutrients, including oxygen, to the encapsulated cells. Modifying the geometries of encapsulation devices using conventional methods to enhance oxygen delivery has proven to be inconsistently challenging [ 67 ], so that novel approaches are required to address these challenges. Additive manufacturing allows customizing biomaterial scaffolds with defined geometries and micropore sizes to improve transport [ 75 , 76 , 77 , 78 , 79 ]. The 3D printed PLA scaffolds with islets have successful vascularization and cellular survival after subcutaneous transplantation [ 80 , 81 ]. Interlocking toroidal hydrogel-elastomer constructs also increased surface area and cell viability [ 82 , 83 , 84 ].
Enhancing vascularization and engraftment
Rich host vascularization of transplant devices is essential to support long-term islet survival through efficient nutrient delivery and insulin kinetics. Early platforms modified bulk material properties to promote vessel infiltration and anastomoses [ 85 , 86 , 87 , 88 , 89 ]. Additive manufacturing can further optimize microscale geometry to both accelerate host vessel connections and control intra-device vasculature homogeneity beyond traditional fabrication. Initial work reproduced macroscale vessels but scales were diverged from cell-based therapies [ 73 , 90 , 91 , 92 ]. Leveraging Additive manufacturing designed structures guided vessel formation in vitro and in vivo [ 80 , 89 , 93 ]. Shifting to bioprinting complex branching conduits in supportive hydrogels facilitated clinical translation for diverse cell therapies [ 94 , 95 , 96 , 97 , 98 ]. Researchers focused on developing a 3D scaffold platform to improve the transplantation outcomes of islet cells in T1D. The scaffold featured a heparinized surface and immobilized vascular endothelial growth factor (VEGF) to enhance vascularization. Scaffold effectively promoted angiogenesis and facilitated the growth of new blood vessels. Additionally, encapsulated islets within the scaffold had functional responses to glucose stimuli. These findings suggested that the developed scaffold platform holds potential for successful extra-hepatic islet transplantation, offering new possibilities for T1D treatment [ 99 ]. Research on vascularization of islets via additive manufacturing techniques has primarily focused on the fundamental discoveries. In one study, engineered pseudo islets (EPIs) were created by combining the mouse insulin-secreting beta cells with rat heart microvascular endothelial cells. EPIs demonstrated extensive outgrowth of capillaries into the surrounding matrix. Although, EPIs containing both cell types that underwent capillarization maintained viability and function over time in culture, non-vascularized EPIs lacking endothelial cells could not sustain viability or functionality long-term. This supported the potential for inducing angiogenesis within bioengineered islet constructs. Future work may combine patient-specific stem cell-derived human beta cells with endothelial cells using this approach to promote long-term graft survival for treating type 1 diabetes [ 98 ]. While, large-scale 3D printed vascularized structures are currently limited for the islet transplantation, advancements in leveraging additive manufacturing for the optimization vascularization conditions through the pore sizes and material choices, may facilitate translation to β-cell therapy in type 1 diabetes.
Precision placement of cells and matrix for enhanced control
Beyond distributing biomaterials, additive manufacturing enables micro-level cell and protein control. For islet transplantation, optimal cellular distribution and supportive extracellular matrix niche reduce rapid dysfunction and apoptosis [ 100 , 101 , 102 ]. Traditional techniques heterogeneously load cells after fabrication or struggle with incomplete encapsulation [ 103 , 104 ]. Bioprinting allows in situ encapsulation and printing of multiple cell types and matrix components while dictating 3D placement and dimensions [ 105 , 106 ]. Islet transplant research prints hydrogel-encapsulated clusters surrounded by supportive cells and doped with immune modulators to improve the transplant environment [ 107 ]. Progress in bioprinting offers consistency and defines physical/chemical graft properties beyond traditional fabrication.
Achieving controlled integration of therapeutic agents for enhanced efficacy
In addition to the cell and matrix placement, additive manufacturing enables precision therapeutic integration. Incorporating therapeutics aims to recapitulate the in vivo environment through angiogenesis, islet health promotion, and immunomodulation [ 67 , 108 ]. Growth factors promote vessel formation and insulin secretion while decrease apoptosis [ 108 , 109 , 110 , 111 ]. Local immunomodulators regulate the immune system in a specific site of the body. They decrease inflammation and promote the successful integration of transplanted cells or tissues by minimizing the need for widespread immune suppression in whole body [ 67 ]. Traditional homogeneous delivery methods restrict the ability to customize the spatial distribution of substances and pose a risk of harmful effects on transplants or hosts [ 112 ]. The use of discreet gradients in bioprinting can offer precise physiological signals. By combining traditional drug release methods with AM, it becomes possible to create tissues that exhibit distinct therapeutic localization. Bioprinted composites have the ability to release factors with gradients throughout the entire construct that enables a more comprehensive and targeted approach in tissue engineering [ 112 , 113 , 114 ].
Cell based gene therapy
Gene therapy holds great promise for diabetes management, offering innovative approaches to deliver and manipulate the insulin gene in various tissues. Viral methods, such as lentivirus, adenovirus, and adeno-associated virus (AAV), along with non-viral techniques like liposomes and naked DNA, have been utilized to deliver the insulin gene to target tissues [ 115 ]. This section aims to provide an overview of important studies in the field of gene therapy for diabetes management, emphasizing advancements in insulin gene delivery and manipulation (Table 3).
Enteroendocrine K-cells and pancreatic β-cells
Enteroendocrine K-cells in the intestines and pancreatic β-cells share similarities in their production of glucose-dependent insulinotropic polypeptide (GIP) and their regulatory mechanisms. Understanding these similarities offers insights into T2D management and improving glucose homeostasis. However, attempts to reverse diabetes effectively through K-cell transplantation have been unsuccessful. Nevertheless, research on gene editing techniques has shown promising results in management of the diabetes mellitus [ 116 , 117 ]. AAV vectors have been employed to co-express insulin and glucokinase genes in skeletal muscles, demonstrating long-term effectiveness in achieving normo-glycemia without exogenous insulin [ 118 , 119 ].
Gene editing techniques
Gene editing techniques using AAV vectors effectively improved normo-glycemia in animal models. Co-expression of insulin and glucokinase in transgenic mice increased glucose absorption and regulated insulin production. Duodenal homeobox 1 (PDX1) gene transfer via AAV2 in a humanized liver mouse model also led to insulin secretion and glycemic control [ 120 ]. Adenovirus-mediated transfection of hepatic cells with neurogenin 3 (NGN3) resulted in insulin production and trans-differentiation of oval cell populations [ 121 , 122 ]. Targeting specific promoters in liver cells such as phosphoenolpyruvate carboxykinase (PEPCK), glucose 6-phosphatase (G6Pase), albumin, and insulin-like growth factor binding protein-1 (IGFBP-1) enhanced hepatic insulin gene therapy [ 123 , 124 ]. AAV-mediated overexpression of SIRT1 reduced inflammation, hypoxia, apoptosis and improved neural function in the retina of diabetic db/db mice [ 125 ]. Another study developed a plasmid expressing a single-strand insulin analogue for intramuscular injection using a specialized gene delivery technique. A single administration provided sustained insulin expression for 1.5 months and effectively regulated blood glucose levels without immune responses or tissue damage in diabetic mice.
Non-viral gene delivery methods
Non-viral approaches have also key roles in achieving glycemic control. The combination of insulin fragments with DNA plasmid, administered via intravenous injection improved normo-glycemia for extended periods. DNA transposon facilitated gene integration into the host chromosome that addressed the short-term liver expression. Additionally, the co-injection of DNA plasmid containing insulin with furin significantly enhanced insulin production within muscles [ 126 ]. Non-viral plasmids were engineered to carry proinsulin and pancreatic regenerating genes to ameliorate streptozotocin-induced T1DM [ 127 ]. The pVAX plasmid vectors prolonged therapeutic effects in achieving normo-glycemia without the need for further treatment [ 127 ]. Bioreducible cationic polymers, such as poly-(cystamine bisacrylamide-diamino hexane) (p(CBA-DAH)), have been employed to deliver RAE-1 to pancreatic islets, resulting in improved insulin levels [ 128 ]. Furthermore, ex vivo gene transfer and autologous grafts have shown promising outcomes in animal models. The introduction of the human insulin gene into pancreatic or liver cells followed by autologous grafts improved insulin secretion, glycemic control, and alleviated the diabetic complications in pigs. However, gene silencing eventually occurred, necessitating a deeper understanding of the underlying mechanisms [ 128 , 129 ].
Stem cell based therapy in diabetes
Efforts are ongoing to develop standardized processes for donor and recipient selection/allocation to increase pancreas utilization [ 130 , 131 , 132 , 133 ]. Techniques for isolating pancreatic islets are being optimized to become more standardized and consistent. Noninvasive imaging technologies allow the monitoring of the transplanted islets without surgery [ 134 , 135 ]. Biomarkers could also evaluate how immunomodulation strategies are working [ 136 , 137 , 138 ]. Researchers are also exploring alternative transplant sites in the body beyond just the liver, to see if the other locations may better support islet graft survival and function. Together, these areas of refinement aim to improve the safety and reliability of islet transplantation procedures as a potential therapy for diabetes [ 139 ]. Bioengineering approaches are being developed to optimize the islet transplantation microenvironment using biomaterials which enhance islet engraftment and function through engineered extracellular niches [ 140 , 141 ]. For example, encapsulation techniques aim to protect pancreatic islets against immune reponse by enclosing them within semipermeable hydrogel polymer capsules [ 142 , 143 ]. This localized immunoisolation strategy utilizes biomaterials like alginate to create a physical barrier preventing immune cell contact while still allowing nutrient and oxygen diffusion. Researchers concurrently seek alternative unlimited cellular sources to address limited islet availability. Mesenchymal stem cells possess immunomodulatory properties and their adjuvant delivery, either early in disease onset or simultaneously with islet transplantation, has shown promising signs of improving outcomes in preclinical investigations. By dampening inflammatory responses and favoring regenerative processes, stem cells may help to establish a more tolerogenic transplant environment. These bioengineering and cell therapy approaches offer potential pathways towards eliminating the exogenous insulin requirement [ 144 , 145 ]. A variety of stem cell types have therapeutic potential for diabetes (Fig. 2 ). Pluripotent stem cells possess immense promise for overcoming the limitations of islet transplantation. Human embryonic stem cells and induced pluripotent stem cells are especially attractive candidates due to their unique ability to both self-renew indefinitely and differentiate into any cell type. This makes them an ideal source of replacement pancreatic beta cells. Significant research effort across academic and industrial laboratories has led to advancement in differentiation protocols that can convert pluripotent stem cells into functional beta-like cells in vitro. However, establishing consistent, well-characterized cellular production methods that comply with stringent safety and efficacy standards remains a priority for clinical translation. Ongoing work aims to generate therapeutic stem cell-derived beta cell replacements exhibiting stable, glucose-responsive insulin secretion comparable to primary islets. Although, technological and regulatory hurdles still must be cleared, pluripotent stem cells have the greatest potential to finally solve the problem of limited cell availability and provide an unlimited source of transplantable tissue suitable for widespread treatment of diabetes [ 145 , 146 , 147 , 148 ]. There are currently six registered clinical trials evaluating the use of human pluripotent stem cells for the T1D treatment. All trials except one use PEC-01 cells, which consist of a mixture of pancreatic endoderm and polyhormonal cell population derived from CyT49 stem cells that are fully committed to endocrine differentiation upon implantation [ 149 ]. The initial trial implanted PEC-01 cells within an encapsulation device, hypothesizing no need for immunosuppression. While, well-tolerated with minor adverse effects, insufficient engraftment occurred due to foreign body responses that eliminated the cells [ 150 ]. The trial transitioned in 2017 to use an open encapsulation device that required immunosuppression. Subcutaneous engraftment, differentiation of cells into islet-like clusters, and glucose-responsive insulin production provided the first evidence that pancreatic progenitor cells can survive, mature, and function as the endocrine cells in humans. Potential benefits on stimulated C-peptide levels and glycemic control were observed in one patient [ 151 , 152 ]. Two reports in late 2021 described results in 17 patients receiving PEC-01 cells in an open device. Engraftment and insulin expression occurred in the majority, glucose-responsive secretion in over one-third, and various glycemic improvements were observed at six months. Explanted tissues contained heterogeneous pancreatic compositions including mature beta cells, with no teratoma formation and mild adverse effects related to surgery/immunosuppression. VX-880 uses fully differentiated insulin-producing stem cell-derived islet cells in phase 1/2 trial evaluating portal infusion and different doses requiring immunosuppression. Preliminary results suggest early engraftment and insulin secretion. The manin challenge was controlling immune rejection without systemic immunosuppression [ 149 ]. Several strategies are being explored to address the challenges of immune rejection in stem cell therapies for diabetes. They include generating stem cell lines that are universally compatible through HLA silencing, developing milder regimens of immunosuppression, and refining encapsulation and containment approaches to protect transplanted cells toward immune response. Establishing standardized stem cell banks is also an area of investigation [ 153 , 154 ]. Xenotransplantation using gene-edited porcine islets remains an exciting avenue of research given advances to improve engraftment and reduce immunogenicity in preclinical studies [ 155 ]. Novel approaches continue to emerge as well, such as decellularization techniques, 3D bioprinting of tissue constructs, and creating interspecies chimeras. Rapid evolution of cell-based therapies across both academic and commercial sectors is promising to restore normoglycemic control in diabetic cases. Refinement of existing methods and development of new strategies hold potential to perform a safe and effective cell replacement without reliance on systemic immunosuppression. Stem cell and regenerative therapies may ultimately manage diabetes through restored endogenous insulin production [ 156 ]. Recently a meta analysis evaluated the safety and efficacy of MSC-based therapy for diabetes in humans. This comprehensive analysis was conducted on 262 patients across six trials that met the inclusion criteria within the last five years. The results reveal that treatment with MSCs significantly reduced the dosage of anti-diabetic drugs over a 12-months. Following treatment, HbAc1 levels decreased by an average of 32%, fasting blood glucose levels decreased by an average of 45%, and C-peptide levels showed a decrease of 38% in two trials and an increase of 36% in four trials. Notably, no severe adverse events were reported across all trials. Therefore, it can be concluded that MSC therapy for type 2 diabetes is safe and effective [ 157 ].
Advances in islet transplantation and stem cell-derived Beta cells
Limited number of the islet transplantation donors highlights the importance of cell therapy in diabetes. Although, higher islet numbers from multiple donors increase the success, limited pancreas availability restricts widespread use [ 158 ]. Using multiple donors also increases rejection risk, while isolation of the islets can cause tissue damage [ 159 ]. To overcome these challenges, researchers have explored the differentiation of stem cells into beta cells in vitro to generate an unlimited supply of insulin-producing cells with standardized and characterized products. Genetic engineering techniques have also been investigated to confer advantages such as stress resistance or immune evasion [ 158 ]. ViaCyte has developed a stem cell-derived pancreatic progenitor called PEC-01, which has the ability to mature into endocrine cells in rodent models. To protect the transplanted cells from immune response, retrieval encapsulation devices were also created [ 160 , 161 , 162 ]. In an initial human clinical trial conducted in 2014 (NCT02239354), the Encaptra device was utilized with the aim of providing complete immunoprotection of transplanted cells through the use of a cell-impermeable membrane. Although, the PEC-Encap product showed reliable tolerance and minimal adverse effects, the trial was stopped due to the inadequate engraftment of functional products. While, a few endocrine cells were observed, fibrosis around the capsule led to graft loss and supression of the insulin secretion. To address this challenge, a more recent development called the PEC-Direct device was introduced, which featured openings in the membrane to facilitate vascularization, thereby improving nutrient exchange and supporting cell viability. However, since host cells could infiltrate the device, immunosuppression was necessary following the transplantation [ 163 , 164 , 165 ]. Protocols were developed to generate clusters of stem cell-derived beta cells that secreted glucose-responsive insulin. These clusters, referred to SC-islets, also contained other endocrine cells, including glucagon-producing cells. SC-islets improved glycemic control in diabetic mice and nonhuman primates [ 146 , 166 , 167 , 168 ]. In a trial conducted in 2017 (NCT03163511), the transplantation of progenitor cells resulted in the maturation of endocrine cells, and glucose-responsive C-peptide secretion was observed 6–9 months post-transplantation. Notably, the majority of these mature endocrine cells exhibited glucagon-positive characteristics. The porous regions housing the endocrine cells allowed for the infiltration of host vessels to facilitate vascularization. However, non-cellular regions were isolated by the presence of fibrosis [ 164 , 165 ]. Although, there was not a sufficient levels of circulating C-peptide in these trials, the findings underscored the significance of promoting vascularization and minimizing fibrotic reactions [ 164 , 169 ]. Vertex conducted a human trial in 2021 (NCT04786262) involving the transplantation of half-dose VX-880 cells (SC-islets) without a device to avoid previous problems, which necessitated immunosuppression. Preliminary results reported improved glycemic control, although it took longer to achieve the same outcome compared to rodent models [ 158 ]. Overall, progresses in islet transplantation and stem cell-derived beta cells pave the way for overcoming the limitations of traditional approaches. Further research and refinements are also required to achieve consistent and clinically significant outcomes in the treatment of diabetes.
Chalenges and limitations
Cell-based therapies have been significantly progressed for diabetes; however, there are still several challenges that need to be overcome. Clinical trials investigating encapsulation devices and islet transplantation techniques have provided valuable insights but face several obstacles including oxygenation, host immune responses, and insufficient long-term engraftment success. Immunoengineering of biomaterials and additive manufacturing for the development of 3D islet structures aim to modulate inflammation and promote graft revascularization. Nevertheless, achieving consistent normalization of blood glucose levels without exogenous insulin remains a challenge in human studies. In the field of gene therapy and stem cell differentiation, research focuses on genetically-modified or progenitor-derived insulin-secreting β-like cells to optimize protocols that ensure safety and functionality. The main challenge is to establish stable and functional cells capable of permanently restoring normoglycemia without the need for external intervention. One major barrier is the immune response, which targets allogeneic and xenogeneic islet grafts. Although, local immunotherapy minimizes the systemic effects, evading graft destruction through biomaterials without the requirement of immune suppression remains a significant challenge. The translation of precision 3D islet constructs and genetically reprogrammed cells also necessitates scalable manufacturing processes to ensure consistent function and long-term safety across batches. When critically appraising progress in the field of cell-based diabetes treatments, it is imperative to consider the regulatory, ethical, economic, and safety factors that shape translational applications. At the regulatory level, oversight bodies play a pivotal role in establishing standards to ensure patient welfare while enabling therapeutic innovation. FDA oversees clinical trials and product approvals in the United States (US), while in Europe the EMA provides parallel regulatory guidance. Within the US, organizations like the United Network for Organ Sharing (UNOS) and Organ Procurement and Transplantation Network (OPTN) govern organ and cell allocation protocols [ 17 , 170 ]. However, as regenerative approaches diverge from traditional organ transplantation, regulatory pathways require ongoing harmonization between the agencies and jurisdictions. Continual dialogue between researchers, oversight boards, and policymakers will be crucial to streamline guidelines in a patient-centric manner that balances safety, efficacy, and timely access to cutting-edge therapies. For instance, as stem cell-derived beta cells and 3D bioprinted tissue constructs emerge, traditional drug and device frameworks may not adequately address product characterization and manufacturing complexities for these advanced therapeutic products [ 67 ]. Within clinics, maintaining compliance with evolving regulations impacts research directives and ultimately patients’ access to the novel treatments. Addressing informed consent, clinical trial design, and privacy protections for sensitive health data are also paramount from an ethical perspective [ 128 , 129 ]. Autonomy and agency of research participants in decision-making related to experimental therapies demand prudency. Equitable accessibility of new treatment options also warrants attention to avoid certain populations facing undue barriers. Cell sourcing presents ethical issues depending on derivation from embryonic, fetal or adult tissues. Logistical matters like shipping and processing stem cell-derived islets prior to transplantation necessitate scrutiny. Tumorigenic potential of the undifferentiated pluripotent stem cells should be optimized through rigorous preclinical testing. Transitioning therapies between animal and early human investigations necessitates well-characterized cellular products showing consistent safety and glucose-responsive insulin secretion profiles comparable to pancreatic islets. Long-term animal model data substantiating lack of malignant transformation following transplantation aids allaying ethical safety concerns as the therapies progress clinically. Researchers carefully screen new concepts to prevent side effects in participants while pursuing curative goals. In terms of economic costs, islet and stem cell transplant procedures remain prohibitively expensive for broad applicability despite promising clinical signals. The field requires sustained study to validate techniques, track long-term outcomes, assess healthcare costs offsets from mitigating diabetes’ debilitating complications, and establish cost-benefit ratios for national reimbursement paradigms. Public-private partnerships may accelerate large, interventional trials and longitudinal research to precisely quantify the cellular therapies’ safety profiles and real-world efficacies compared to intensive management versus costs of intensive diabetes care. Ongoing developments like 3D bioprinting offer catalytic manufacturing potential fundamentally recalibrating economics by enhancing yields, standardizing procedures, and reducing costs through scale. By thoroughly and sensitively examining regulatory frameworks, informed consent processes, risks and benefits, as well as financial considerations at both micro and macro levels, researchers, oversight boards and broader stakeholder networks can advance cell-based therapies towards delivering life-changing benefits for all communities. A multidisciplinary, conscientious approach balances progress against patient welfare. A combination of multiple strategies may help to overcome these limitations. For instance, gene-modified islets integrated within vascularized biomaterial implants or sequenced therapies have promising results to prime grafts in pro-regenerative environments before transplantation. Collaboration across disciplines offers hope that refined individualized therapies may eventually achieve durable insulin independence through functional pancreatic cell or tissue engraftment, not only for diabetes but also for chronic pancreatitis. Regarding, ongoing progresses in unraveling these barriers, cell replacement approaches have the potential to improve diabetes management.
Conclusions
This review provides a comprehensive overview of the advances, challenges, and future directions in various cell-based therapeutic approaches for the treatment of diabetes. Significant progresses have been achieved in microencapsulation design, immunomodulation, tissue constructs, genetic and cellular reprogramming techniques, as well as initial clinical translation. However, the complete restoration of normoglycemia without the need for lifelong immunosuppression is still considered as a significant therapeutic challenge. Therefore, addressing the transplant environment of the hostile nature, developing minimally invasive delivery methods, and overcoming limitations in engraftment efficiency and longevity are crucial issues for the future researches. Through the sustained multidisciplinary efforts for the improvement of existing strategies and establishing novel paradigms, achieving durable insulin independence can be a realistic goal for all diabetic cases through the personalized cell replacement or regeneration.
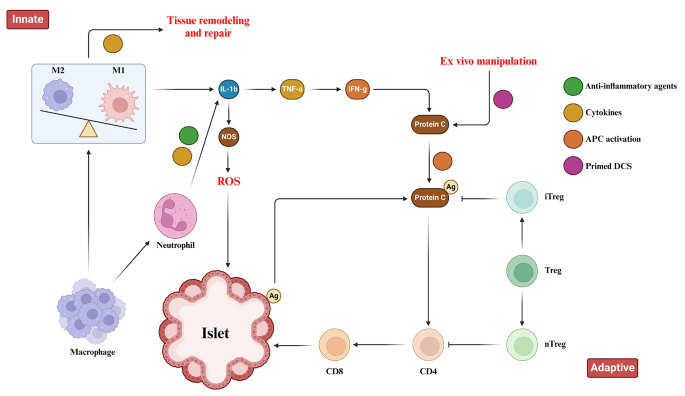
Immune Responses toward pancreatic islets following transplantation. This figure illustrates the immune responses, including the innate and adaptive immunity that are triggered upon pancreatic islet transplantation. Immune response begins with the activation of tissue macrophages and neutrophils in response to injury. Subsequent, release of inflammatory cytokines stimulates antigen-presenting cells (APCs), CD4 + T cells, CD8 + T cells, and cytotoxic T lymphocytes to orchestrate the immune response
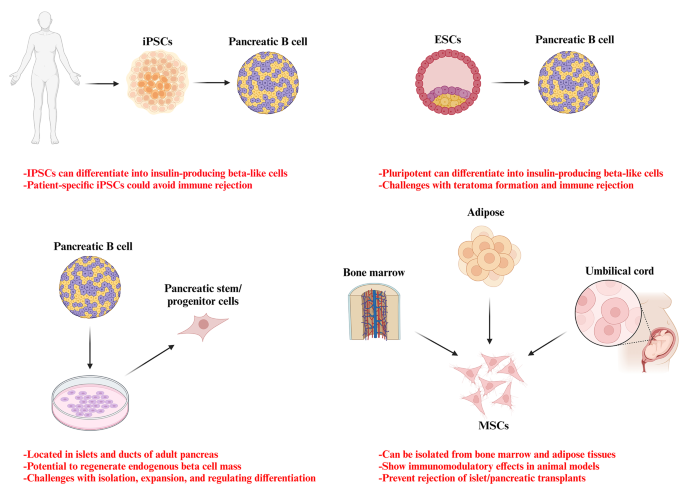
Potential stem cell sources for the treatment of diabetes
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Acrylonitrile butadiene styrene
Activate antigen-presenting cells
Adeno-associated virus
Duodenal homeobox 1
Engineered pseudo islets
Expanded polytetrafluoroethylene
Extracellular matrix
Foreign body response
Fused filament fabrication
Gestational diabetes mellitus
Glucose 6-phosphatase
Insulin-like growth factor binding protein-1
Mesenchymal stem cells
Neurogenin 3
Organ Procurement and Transplantation Network
Phosphoenolpyruvate carboxykinase
Polyaryletherketone
Polycaprolactone
Polycarbonate
Polyetheretherketone
Polyetherimide
Poly-lactic acid
Polystyrene
Stereolithography
Thermoplastic polyurethane
Type 1 diabetes
Type 1 diabetes mellitus
Type 2 diabetes mellitus
United Network for Organ Sharing
United States
Vascular endothelial growth factor
Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22.
Article Google Scholar
Cho NH, Shaw J, Karuranga S, Huang Y, da Rocha Fernandes J, Ohlrogge A, et al. IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–81.
Article CAS PubMed Google Scholar
Moghbeli M, Naghibzadeh B, Ghahraman M, Fatemi S, Taghavi M, Vakili R, et al. Mutations in HNF1A gene are not a Common cause of familial young-onset diabetes in Iran. Indian J Clin Biochem. 2018;33(1):91–5.
Akhlaghipour I, Bina AR, Mogharrabi MR, Fanoodi A, Ebrahimian AR, Khojasteh Kaffash S, et al. Single-nucleotide polymorphisms as important risk factors of diabetes among Middle East population. Hum Genomics. 2022;16(1):11.
Article CAS PubMed PubMed Central Google Scholar
Moghbeli M, Khedmatgozar H, Yadegari M, Avan A, Ferns GA, Ghayour Mobarhan M. Cytokines and the immune response in obesity-related disorders. Adv Clin Chem. 2021;101:135–68.
Eizirik DL, Pasquali L, Cnop M. Pancreatic β-cells in type 1 and type 2 diabetes mellitus: different pathways to failure. Nat Reviews Endocrinol. 2020;16(7):349–62.
Article CAS Google Scholar
Siqueira ISLd, Alves Guimarães R, Mamed SN, Santos TAP, Rocha SD, Pagotto V, et al. Prevalence and risk factors for self-report diabetes mellitus: a population-based study. Int J Environ Res Public Health. 2020;17(18):6497.
Free radical research.
Zhu B, Qu S. The relationship between diabetes mellitus and cancers and its underlying mechanisms. Front Endocrinol. 2022;13:800995.
Mojarrad M, Moghbeli M. Genetic and molecular biology of bladder cancer among Iranian patients. Mol Genet Genomic Med. 2020;8(6):e1233.
Article PubMed PubMed Central Google Scholar
Moghbeli M. Genetic and molecular biology of breast cancer among Iranian patients. J Transl Med. 2019;17(1):218.
Abbaszadegan MR, Moghbeli M. Genetic and molecular origins of colorectal Cancer among the iranians: an update. Diagn Pathol. 2018;13(1):97.
Kim I. A brief overview of cell therapy and its product. J Korean Association Oral Maxillofacial Surg. 2013;39(5):201.
Mount NM, Ward SJ, Kefalas P, Hyllner J. Cell-based therapy technology classifications and translational challenges. Philosophical Trans Royal Soc B: Biol Sci. 2015;370(1680):20150017.
El-Kadiry AE-H, Rafei M, Shammaa R. Cell therapy: types, regulation, and clinical benefits. Front Med. 2021;8:756029.
Squifflet J-P, Gruessner R, Sutherland D. The history of pancreas transplantation: past, present and future. Acta Chir Belg. 2008;108(3):367–78.
Article PubMed Google Scholar
Parums DV. First Regulatory approval for allogeneic pancreatic islet Beta cell infusion for adult patients with type 1 diabetes Mellitus. Med Sci Monitor: Int Med J Experimental Clin Res. 2023;29:e941918–1.
Yang L, Hu Z-M, Jiang F-X, Wang W. Stem cell therapy for insulin-dependent diabetes: are we still on the road? World J Stem Cells. 2022;14(7):503.
Affan M, Dar MS. Donislecel-the first approved pancreatic islet cell therapy medication for type 1 diabetes: a letter to the editor. Ir J Med Sci (1971-). 2023:1–2.
Harris E. FDA greenlights first cell therapy for adults with type 1 diabetes. JAMA. 2023.
Soon-Shiong P, Heintz R, Merideth N, Yao Q, Yao Z, Zheng T, et al. Insulin independence in a type 1 diabetic patient after encapsulated islet transplantation. Lancet (London England). 1994;343(8903):950–1.
Calafiore R, Basta G, Luca G, Lemmi A, Montanucci MP, Calabrese G, et al. Microencapsulated pancreatic islet allografts into nonimmunosuppressed patients with type 1 diabetes: first two cases. Diabetes Care. 2006;29(1):137–8.
Tuch BE, Keogh GW, Williams LJ, Wu W, Foster JL, Vaithilingam V, et al. Safety and viability of microencapsulated human islets transplanted into diabetic humans. Diabetes Care. 2009;32(10):1887–9.
Weng L, Wang X, Liu H, Yu Z, Liu S. Light-responsive microneedle array with tunable insulin release function for painless and on-demand anti-diabetic therapy. Mater Lett. 2023:135684.
Okcu A, Yazir Y, Şimşek T, Mert S, Duruksu G, Öztürk A, et al. Investigation of the effect of pancreatic decellularized matrix on encapsulated islets of Langerhans with mesenchymal stem cells. Tissue Cell. 2023;82:102110.
Khaliq T, Sohail M, Minhas MU, Mahmood A, Munir A, Qalawlus AHM, et al. Hyaluronic acid/alginate-based biomimetic hydrogel membranes for accelerated diabetic wound repair. Int J Pharm. 2023;643:123244.
Kuwabara R, Qin T, Llacua LA, Hu S, Boekschoten MV, de Haan BJ, et al. Extracellular matrix inclusion in immunoisolating alginate-based microcapsules promotes longevity, reduces fibrosis, and supports function of islet allografts in vivo. Acta Biomater. 2023;158:151–62.
Kirk K, Hao E, Lahmy R, Itkin-Ansari P. Human embryonic stem cell derived islet progenitors mature inside an encapsulation device without evidence of increased biomass or cell escape. Stem cell Res. 2014;12(3):807–14.
Dufrane D, van Steenberghe M, Goebbels R-M, Saliez A, Guiot Y, Gianello P. The influence of implantation site on the biocompatibility and survival of alginate encapsulated pig islets in rats. Biomaterials. 2006;27(17):3201–8.
Pullen LC. Stem cell–derived pancreatic progenitor cells have now been transplanted into patients: report from IPITA 2018. Wiley Online Library; 2018. pp. 1581–2.
Dang HP, Chen H, Dargaville TR, Tuch BE. Cell delivery systems: toward the next generation of cell therapies for type 1 diabetes. J Cell Mol Med. 2022;26(18):4756–67.
Viacyte. ViaCyte and gore enter clinical phase agreement based on novel membrane technology for PEC-encap product candidate. 2020.
Viacyte. viacyte announces initiation of phase 2 study of encapsulated cell therapy for type 1 diabetes patients 2021 2021. https://viacyte.com/press-releases/viacyte‐announces‐initiation‐of‐phase‐2‐study‐of‐encapsulated‐cell‐ther‐apy‐for‐type‐1‐diabetes‐patients/ .
Hodgson J. Drug pipeline 3Q23—ERT, bispecifics and CRISPR in sickle cell disease. Nat Biotechnol. 2023;41(11):1498–500.
Pagliuca F. Pre-clinical proof-of-Concept in two lead programs in type 1 diabetes. International Socety for Stem Cell Research; 2019.
Jones PM, Persaud SJ. β-cell replacement therapy for type 1 diabetes: closer and closer. Diabet Med. 2022;39(6).
Carlsson P-O, Espes D, Sedigh A, Rotem A, Zimerman B, Grinberg H, et al. Transplantation of macroencapsulated human islets within the bioartificial pancreas βAir to patients with type 1 diabetes mellitus. Am J Transplant. 2018;18(7):1735–44.
Ludwig B, Zimerman B, Steffen A, Yavriants K, Azarov D, Reichel A, et al. A novel device for islet transplantation providing immune protection and oxygen supply. Horm Metab Res. 2010;42(13):918–22.
Evron Y, Colton CK, Ludwig B, Weir GC, Zimermann B, Maimon S, et al. Long-term viability and function of transplanted islets macroencapsulated at high density are achieved by enhanced oxygen supply. Sci Rep. 2018;8(1):6508.
Cao R, Avgoustiniatos E, Papas K, de Vos P, Lakey JR. Mathematical predictions of oxygen availability in micro-and macro‐encapsulated human and porcine pancreatic islets. J Biomedical Mater Res Part B: Appl Biomaterials. 2020;108(2):343–52.
Gala-Lopez B, Pepper A, Dinyari P, Malcolm A, Kin T, Pawlick L, et al. Subcutaneous clinical islet transplantation in a prevascularized subcutaneous pouch–preliminary experience. CellR4. 2016;4(5):e2132.
Google Scholar
Sernova Corp Presents Positive Preliminary. Safety and Efficacy Data in its Phase I/II Clinical Trial for Type-1 Diabetes: Biospace. https://www.biospace.com/article/sernova‐corp‐presents‐positive‐preliminary‐safety‐and‐efficacy‐data‐in‐its‐phase‐i‐ii‐clinical‐trial‐for‐type‐1‐diabetes/ .
Bachul PJ, Perez-Gutierrez A, Juengel B, Golab K, Basto L, Perea L et al. 306-OR: modified approach for improved isllotransplantation into prevascularized sernova cell pouch device: preliminary results of the phase i/ii clinical trial at University of Chicago. Diabetes. 2022;71(Supplement_1).
Vegas AJ, Veiseh O, Doloff JC, Ma M, Tam HH, Bratlie K, et al. Combinatorial hydrogel library enables identification of materials that mitigate the foreign body response in primates. Nat Biotechnol. 2016;34(3):345–52.
Vegas AJ, Veiseh O, Gürtler M, Millman JR, Pagliuca FW, Bader AR, et al. Long-term glycemic control using polymer-encapsulated human stem cell–derived beta cells in immune-competent mice. Nat Med. 2016;22(3):306–11.
Shapiro AD, Konkle BA, Croteau SE, Miesbach WA, Hay CRM, Kazmi R, et al. First-in-human phase 1/2 clinical trial of SIG-001, an innovative shielded cell therapy platform, for hemophilia Α. Blood. 2020;136:8.
Taraballi F, Sushnitha M, Tsao C, Bauza G, Liverani C, Shi A, et al. Biomimetic tissue engineering: tuning the immune and inflammatory response to implantable biomaterials. Adv Healthc Mater. 2018;7(17):1800490.
Yesilyurt V, Veiseh O, Doloff JC, Li J, Bose S, Xie X, et al. A facile and versatile method to endow biomaterial devices with zwitterionic surface coatings. Adv Healthc Mater. 2017;6(4):1601091.
Liu Q, Chiu A, Wang L-H, An D, Zhong M, Smink AM, et al. Zwitterionically modified alginates mitigate cellular overgrowth for cell encapsulation. Nat Commun. 2019;10(1):5262.
Noverraz F, Montanari E, Pimenta J, Szabó L, Ortiz D, Gonelle-Gispert C, et al. Antifibrotic effect of ketoprofen-grafted alginate microcapsules in the transplantation of insulin producing cells. Bioconjug Chem. 2018;29(6):1932–41.
Jeon SI, Jeong J-H, Kim JE, Haque MR, Kim J, Byun Y, et al. Synthesis of PEG-dendron for surface modification of pancreatic islets and suppression of the immune response. J Mater Chem B. 2021;9(11):2631–40.
Derakhshankhah H, Sajadimajd S, Jahanshahi F, Samsonchi Z, Karimi H, Hajizadeh-Saffar E, et al. Immunoengineering Biomaterials in Cell-based therapy for type 1 diabetes. Tissue Eng Part B: Reviews. 2022;28(5):1053–66.
Piemonti L, Maffi P, Nano R, Bertuzzi F, Melzi R, Mercalli A, et al. Treating diabetes with islet transplantation: lessons from the Milan experience. Transplantation, Bioengineering, and regeneration of the endocrine pancreas. Elsevier; 2020. pp. 645–58.
Azzi J, Tang L, Moore R, Tong R, El Haddad N, Akiyoshi T, et al. Polylactide-cyclosporin A nanoparticles for targeted immunosuppression. FASEB J. 2010;24(10):3927.
Chen X, Liu H, Li H, Cheng Y, Yang L, Liu Y. In vitro expansion and differentiation of rat pancreatic duct-derived stem cells into insulin secreting cells using a dynamic three-dimensional cell culture system. Genet Mol Res. 2016;15(2).
Becker MW, Simonovich JA, Phelps EA. Engineered microenvironments and microdevices for modeling the pathophysiology of type 1 diabetes. Biomaterials. 2019;198:49–62.
Graham JG, Zhang X, Goodman A, Pothoven K, Houlihan J, Wang S, et al. PLG scaffold delivered antigen-specific regulatory T cells induce systemic tolerance in autoimmune diabetes. Tissue Eng Part A. 2013;19(11–12):1465–75.
Izadi Z, Hajizadeh-Saffar E, Hadjati J, Habibi-Anbouhi M, Ghanian MH, Sadeghi-Abandansari H, et al. Tolerance induction by surface immobilization of Jagged-1 for immunoprotection of pancreatic islets. Biomaterials. 2018;182:191–201.
McHugh MD, Park J, Uhrich R, Gao W, Horwitz DA, Fahmy TM. Paracrine co-delivery of TGF-β and IL-2 using CD4-targeted nanoparticles for induction and maintenance of regulatory T cells. Biomaterials. 2015;59:172–81.
Chen H, Teramura Y, Iwata H. Co-immobilization of urokinase and thrombomodulin on islet surfaces by poly (ethylene glycol)-conjugated phospholipid. J Controlled Release. 2011;150(2):229–34.
Su J, Hu B-H, Lowe WL Jr, Kaufman DB, Messersmith PB. Anti-inflammatory peptide-functionalized hydrogels for insulin-secreting cell encapsulation. Biomaterials. 2010;31(2):308–14.
Dong H, Fahmy TM, Metcalfe SM, Morton SL, Dong X, Inverardi L, et al. Immuno-isolation of pancreatic islet allografts using pegylated nanotherapy leads to long-term normoglycemia in full MHC mismatch recipient mice. PLoS ONE. 2012;7(12):e50265.
Kumar M, Nandi SK, Kaplan DL, Mandal BB. Localized immunomodulatory silk macrocapsules for islet-like spheroid formation and sustained insulin production. ACS Biomaterials Sci Eng. 2017;3(10):2443–56.
Hotaling NA, Tang L, Irvine DJ, Babensee JE. Biomaterial Strategies for Immunomodulation. Annu Rev Biomed Eng. 2015;17:317–49.
Shi Y, Zhao YZ, Jiang Z, Wang Z, Wang Q, Kou L, et al. Immune-Protective formulations and process strategies for improved survival and function of transplanted islets. Front Immunol. 2022;13:923241.
Zhang S, Yang H, Wang M, Mantovani D, Yang K, Witte F, et al. Immunomodulatory biomaterials against bacterial infections: Progress, challenges, and future perspectives. Innovation. 2023;4(6):100503.
CAS PubMed PubMed Central Google Scholar
Accolla RP, Simmons AM, Stabler CL. Integrating Additive Manufacturing techniques to improve cell-based implants for the treatment of type 1 diabetes. Adv Healthc Mater. 2022;11(13):e2200243.
Gross BC, Erkal JL, Lockwood SY, Chen C, Spence DM. Evaluation of 3D printing and its potential impact on biotechnology and the chemical sciences. ACS; 2014.
Bol RJ, Šavija B. Micromechanical models for FDM 3D-Printed polymers: a review. Polymers. 2023;15(23):4497.
Paul S. Finite element analysis in fused deposition modeling research: a literature review. Measurement. 2021;178:109320.
Monaldo E, Ricci M, Marfia S. Mechanical properties of 3D printed polylactic acid elements: experimental and numerical insights. Mech Mater. 2023;177:104551.
Anoop M, Senthil P. Microscale representative volume element based numerical analysis on mechanical properties of fused deposition modelling components. Materials Today: Proceedings. 2021;39:563 – 71.
McGuigan AP, Sefton MV. Vascularized organoid engineered by modular assembly enables blood perfusion. Proceedings of the National Academy of Sciences. 2006;103(31):11461-6.
Pedraza E, Coronel MM, Fraker CA, Ricordi C, Stabler CL. Preventing hypoxia-induced cell death in beta cells and islets via hydrolytically activated, oxygen-generating biomaterials. Proceedings of the National Academy of Sciences. 2012;109(11):4245-50.
Espona-Noguera A, Ciriza J, Cañibano-Hernández A, Orive G, Hernández RM, del Saenz L, et al. Review of advanced hydrogel-based cell encapsulation systems for insulin delivery in type 1 diabetes mellitus. Pharmaceutics. 2019;11(11):597.
Dimitrioglou N, Kanelli M, Papageorgiou E, Karatzas T, Hatziavramidis D. Paving the way for successful islet encapsulation. Drug Discovery Today. 2019;24(3):737–48.
Omer A, Duvivier-Kali V, Fernandes J, Tchipashvili V, Colton CK, Weir GC. Long-term normoglycemia in rats receiving transplants with encapsulated islets. Transplantation. 2005;79(1):52–8.
Song S, Roy S. Progress and challenges in macroencapsulation approaches for type 1 diabetes (T1D) treatment: cells, biomaterials, and devices. Biotechnol Bioeng. 2016;113(7):1381–402.
Zhi ZL, Kerby A, King AJF, Jones PM, Pickup JC. Nano-scale encapsulation enhances allograft survival and function of islets transplanted in a mouse model of diabetes. Diabetologia. 2012;55(4):1081–90.
Farina M, Chua CYX, Ballerini A, Thekkedath U, Alexander JF, Rhudy JR, et al. Transcutaneously refillable, 3D-printed biopolymeric encapsulation system for the transplantation of endocrine cells. Biomaterials. 2018;177:125–38.
Farina M, Ballerini A, Fraga DW, Nicolov E, Hogan M, Demarchi D et al. 3D printed vascularized device for Subcutaneous Transplantation of Human islets. Biotechnol J. 2017;12(9).
Lei D, Yang Y, Liu Z, Yang B, Gong W, Chen S, et al. 3D printing of biomimetic vasculature for tissue regeneration. Mater Horiz. 2019;6(6):1197–206.
Melchels FP, Domingos MA, Klein TJ, Malda J, Bartolo PJ, Hutmacher DW. Additive manufacturing of tissues and organs. Prog Polym Sci. 2012;37(8):1079–104.
Ernst AU, Wang LH, Ma M. Interconnected toroidal hydrogels for islet encapsulation. Adv Healthc Mater. 2019;8(12):1900423.
Liang J-P, Accolla RP, Jiang K, Li Y, Stabler CL. Controlled release of anti-inflammatory and proangiogenic factors from macroporous scaffolds. Tissue Eng Part A. 2021;27(19–20):1275–89.
Pedraza E, Brady A-C, Fraker CA, Molano RD, Sukert S, Berman DM, et al. Macroporous three-dimensional PDMS scaffolds for extrahepatic islet transplantation. Cell Transplant. 2013;22(7):1123–35.
Chiu Y-C, Cheng M-H, Engel H, Kao S-W, Larson JC, Gupta S, et al. The role of pore size on vascularization and tissue remodeling in PEG hydrogels. Biomaterials. 2011;32(26):6045–51.
Kuss MA, Wu S, Wang Y, Untrauer JB, Li W, Lim JY, et al. Prevascularization of 3D printed bone scaffolds by bioactive hydrogels and cell co-culture. J Biomedical Mater Res Part B: Appl Biomaterials. 2018;106(5):1788–98.
Liu X, Jakus AE, Kural M, Qian H, Engler A, Ghaedi M, et al. Vascularization of natural and synthetic bone scaffolds. Cell Transplant. 2018;27(8):1269–80.
Costa-Almeida R, Gomez-Lazaro M, Ramalho C, Granja PL, Soares R, Guerreiro SG. Fibroblast-endothelial partners for vascularization strategies in tissue engineering. Tissue Eng Part A. 2015;21(5–6):1055–65.
Newman AC, Nakatsu MN, Chou W, Gershon PD, Hughes CC. The requirement for fibroblasts in angiogenesis: fibroblast-derived matrix proteins are essential for endothelial cell lumen formation. Mol Biol Cell. 2011;22(20):3791–800.
Vlahos AE, Cober N, Sefton MV. Modular tissue engineering for the vascularization of subcutaneously transplanted pancreatic islets. Proceedings of the National Academy of Sciences. 2017;114(35):9337-42.
Farina M, Ballerini A, Fraga DW, Nicolov E, Hogan M, Demarchi D, et al. 3D printed vascularized device for subcutaneous transplantation of human islets. Biotechnol J. 2017;12(9):1700169.
Bertassoni LE, Cecconi M, Manoharan V, Nikkhah M, Hjortnaes J, Cristino AL, et al. Hydrogel bioprinted microchannel networks for vascularization of tissue engineering constructs. Lab Chip. 2014;14(13):2202–11.
Jia W, Gungor-Ozkerim PS, Zhang YS, Yue K, Zhu K, Liu W, et al. Direct 3D bioprinting of perfusable vascular constructs using a blend bioink. Biomaterials. 2016;106:58–68.
Gao Q, Liu Z, Lin Z, Qiu J, Liu Y, Liu A, et al. 3D bioprinting of vessel-like structures with multilevel fluidic channels. ACS Biomaterials Sci Eng. 2017;3(3):399–408.
Noor N, Shapira A, Edri R, Gal I, Wertheim L, Dvir T. 3D printing of personalized thick and perfusable cardiac patches and hearts. Adv Sci. 2019;6(11):1900344.
Hospodiuk M, Dey M, Ayan B, Sosnoski D, Moncal KK, Wu Y, et al. Sprouting angiogenesis in engineered pseudo islets. Biofabrication. 2018;10(3):035003.
Marchioli G, Luca AD, de Koning E, Engelse M, Van Blitterswijk CA, Karperien M, et al. Hybrid polycaprolactone/alginate scaffolds functionalized with VEGF to promote de novo vessel formation for the transplantation of islets of Langerhans. Adv Healthc Mater. 2016;5(13):1606–16.
Dionne KE, Colton CK, Lyarmush M. Effect of hypoxia on insulin secretion by isolated rat and canine islets of Langerhans. Diabetes. 1993;42(1):12–21.
de Groot M, Schuurs TA, Keizer PP, Fekken S, Leuvenink HG, Van Schilfgaarde R. Response of encapsulated rat pancreatic islets to hypoxia. Cell Transplant. 2003;12(8):867–75.
Thomas F, Wu J, Contreras JL, Smyth C, Bilbao G, He J, et al. A tripartite anoikis-like mechanism causes early isolated islet apoptosis. Surgery. 2001;130(2):333–8.
Barkai U, Rotem A, de Vos P. Survival of encapsulated islets: more than a membrane story. World J Transplantation. 2016;6(1):69.
Jiang K, Chaimov D, Patel SN, Liang JP, Wiggins SC, Samojlik MM, et al. 3-D physiomimetic extracellular matrix hydrogels provide a supportive microenvironment for rodent and human islet culture. Biomaterials. 2019;198:37–48.
Pati F, Jang J, Ha D, Won Kim S, Rhie J, Shim J, et al. Printing three-dimensional tissue analogues with decellularized extracellular matrix bioink. Nat Commun. 2014;5:3935.
Kim BS, Kwon YW, Kong J-S, Park GT, Gao G, Han W, et al. 3D cell printing of in vitro stabilized skin model and in vivo pre-vascularized skin patch using tissue-specific extracellular matrix bioink: a step towards advanced skin tissue engineering. Biomaterials. 2018;168:38–53.
Hu S, Martinez-Garcia FD, Moeun BN, Burgess JK, Harmsen MC, Hoesli C, et al. An immune regulatory 3D-printed alginate-pectin construct for immunoisolation of insulin producing β-cells. Mater Sci Engineering: C. 2021;123:112009.
Phelps EA, Templeman KL, Thulé PM, García AJ. Engineered VEGF-releasing PEG–MAL hydrogel for pancreatic islet vascularization. Drug Delivery Translational Res. 2015;5:125–36.
Kooptiwut S, Kaewin S, Semprasert N, Sujjitjoon J, Junking M, Suksri K, et al. Estradiol prevents high glucose-induced β-cell apoptosis by decreased BTG2 expression. Sci Rep. 2018;8(1):12256.
Dang TT, Thai AV, Cohen J, Slosberg JE, Siniakowicz K, Doloff JC, et al. Enhanced function of immuno-isolated islets in diabetes therapy by co-encapsulation with an anti-inflammatory drug. Biomaterials. 2013;34(23):5792–801.
Wang Y, He D, Ni C, Zhou H, Wu S, Xue Z, et al. Vitamin D induces autophagy of pancreatic β-cells and enhances insulin secretion. Mol Med Rep. 2016;14(3):2644–50.
Tarafder S, Koch A, Jun Y, Chou C, Awadallah MR, Lee CH. Micro-precise spatiotemporal delivery system embedded in 3D printing for complex tissue regeneration. Biofabrication. 2016;8(2):025003.
Liu YY, Yu HC, Liu Y, Liang G, Zhang T, Hu QX. Dual drug spatiotemporal release from functional gradient scaffolds prepared using 3 D bioprinting and electrospinning. Polym Eng Sci. 2016;56(2):170–7.
Freeman FE, Pitacco P, van Dommelen LH, Nulty J, Browe DC, Shin J-Y, et al. 3D bioprinting spatiotemporally defined patterns of growth factors to tightly control tissue regeneration. Sci Adv. 2020;6(33):eabb5093.
Wong MS, Hawthorne WJ, Manolios N. Gene therapy in diabetes. Self Nonself. 2010;1(3):165.
Ahmad Z, Rasouli M, Azman AZF, Omar AR. Evaluation of insulin expression and secretion in genetically engineered gut K and L-cells. BMC Biotechnol. 2012;12:1–9.
Tudurí E, Bruin JE, Kieffer TJ. Restoring insulin production for type 1 diabetes. J Diabetes. 2012;4(4):319–31.
Romer AI, Sussel L. Pancreatic islet cell development and regeneration. Current opinion in endocrinology, diabetes, and obesity. 2015;22(4):255.
Jaén ML, Vilà L, Elias I, Jimenez V, Rodó J, Maggioni L, et al. Long-term efficacy and safety of insulin and glucokinase gene therapy for diabetes: 8-year follow-up in dogs. Mol therapy-methods Clin Dev. 2017;6:1–7.
Li H, Li X, Lam KS, Tam S, Xiao W, Xu R. Adeno-associated virus-mediated pancreatic and duodenal homeobox gene-1 expression enhanced differentiation of hepatic oval stem cells to insulin-producing cells in diabetic rats. J Biomed Sci. 2008;15:487–97.
Schwitzgebel VM, Scheel DW, Conners JR, Kalamaras J, Lee JE, Anderson DJ, et al. Expression of neurogenin3 reveals an islet cell precursor population in the pancreas. Development. 2000;127(16):3533–42.
Abed A, Critchlow C, Flatt PR, McClenaghan NH, Kelly C. Directed differentiation of progenitor cells towards an islet-cell phenotype. Am J Stem Cells. 2012;1(3):196.
PubMed PubMed Central Google Scholar
Zhao M, Amiel SA, Ajami S, Jiang J, Rela M, Heaton N, et al. Amelioration of streptozotocin-induced diabetes in mice with cells derived from human marrow stromal cells. PLoS ONE. 2008;3(7):e2666.
Handorf AM, Sollinger HW, Alam T. Genetic engineering of surrogate β cells for treatment of type 1 diabetes mellitus. J Diabetes Mellitus. 2015;5(04):295–312.
Grant MB, Adu-Agyeiwaah Y, Vieira CP, Asare-Bediako B, Hammer SS, Calzi SL, et al. Intravitreal administration of AAV2-SIRT1 reverses diabetic retinopathy (DR) in a murine model of type 2 diabetes (T2D). Investig Ophthalmol Vis Sci. 2022;63(7):2310.
Yoon J-W, Jun H-S. Recent advances in insulin gene therapy for type 1 diabetes. Trends Mol Med. 2002;8(2):62–8.
Hou W-R, Xie S-N, Wang H-J, Su Y-Y, Lu J-L, Li L-L, et al. Intramuscular delivery of a naked DNA plasmid encoding proinsulin and pancreatic regenerating III protein ameliorates type 1 diabetes mellitus. Pharmacol Res. 2011;63(4):320–7.
Joo WS, Jeong JH, Nam K, Blevins KS, Salama ME, Kim SW. Polymeric delivery of therapeutic RAE-1 plasmid to the pancreatic islets for the prevention of type 1 diabetes. J Controlled Release. 2012;162(3):606–11.
Dezashibi HM, Shabani A. A Mini-review of Current Treatment approaches and Gene Therapy as potential interventions for diabetes Mellitus types 1. Adv Biomed Res. 2023;12:219.
Vantyghem M-C, de Koning EJ, Pattou F, Rickels MR. Advances in β-cell replacement therapy for the treatment of type 1 diabetes. Lancet. 2019;394(10205):1274–85.
Hudson A, Bradbury L, Johnson R, Fuggle S, Shaw J, Casey J, et al. The UK pancreas allocation scheme for whole organ and islet transplantation. Am J Transplant. 2015;15(9):2443–55.
Cornateanu SM, O’Neill S, Dholakia S, Counter CJ, Sherif AE, Casey JJ, et al. Pancreas utilization rates in the UK–an 11-year analysis. Transpl Int. 2021;34(7):1306–18.
Nordheim E, Lindahl JP, Carlsen RK, Åsberg A, Birkeland KI, Horneland R, et al. Patient selection for islet or solid organ pancreas transplantation: experiences from a multidisciplinary outpatient-clinic approach. Endocr Connections. 2021;10(2):230–9.
Arifin DR, Bulte JW. In vivo imaging of pancreatic islet grafts in diabetes treatment. Front Endocrinol. 2021;12:640117.
Murakami T, Fujimoto H, Inagaki N. Non-invasive beta-cell imaging: visualization, quantification, and beyond. Front Endocrinol. 2021;12:714348.
Piemonti L, Everly MJ, Maffi P, Scavini M, Poli F, Nano R, et al. Alloantibody and autoantibody monitoring predicts islet transplantation outcome in human type 1 diabetes. Diabetes. 2013;62(5):1656–64.
Anteby R, Lucander A, Bachul PJ, Pyda J, Grybowski D, Basto L, et al. Evaluating the prognostic value of islet autoantibody monitoring in islet transplant recipients with long-standing type 1 diabetes mellitus. J Clin Med. 2021;10(12):2708.
Buron F, Reffet S, Badet L, Morelon E, Thaunat O. Immunological monitoring in beta cell replacement: towards a pathophysiology-guided implementation of biomarkers. Curr Diab Rep. 2021;21:1–11.
Cantarelli E, Piemonti L. Alternative transplantation sites for pancreatic islet grafts. Curr Diab Rep. 2011;11:364–74.
Tremmel DM, Odorico JS. Rebuilding a better home for transplanted islets. Organogenesis. 2018;14(4):163–8.
Citro A, Moser PT, Dugnani E, Rajab TK, Ren X, Evangelista-Leite D, et al. Biofabrication of a vascularized islet organ for type 1 diabetes. Biomaterials. 2019;199:40–51.
Basta G, Montanucci P, Calafiore R. Microencapsulation of cells and molecular therapy of type 1 diabetes mellitus: the actual state and future perspectives between promise and progress. J Diabetes Invest. 2021;12(3):301–9.
Samojlik MM, Stabler CL. Designing biomaterials for the modulation of allogeneic and autoimmune responses to cellular implants in type 1 diabetes. Acta Biomater. 2021;133:87–101.
Carlsson P-O, Schwarcz E, Korsgren O, Le Blanc K. Preserved β-cell function in type 1 diabetes by mesenchymal stromal cells. Diabetes. 2015;64(2):587–92.
Madani S, Setudeh A, Aghayan HR, Alavi-Moghadam S, Rouhifard M, Rezaei N, et al. Placenta derived mesenchymal stem cells transplantation in type 1 diabetes: preliminary report of phase 1 clinical trial. J Diabetes Metabolic Disorders. 2021;20:1179–89.
Pagliuca FW, Millman JR, Gürtler M, Segel M, Van Dervort A, Ryu JH, et al. Generation of functional human pancreatic β cells in vitro. Cell. 2014;159(2):428–39.
Russ HA, Parent AV, Ringler JJ, Hennings TG, Nair GG, Shveygert M, et al. Controlled induction of human pancreatic progenitors produces functional beta-like cells in vitro. EMBO J. 2015;34(13):1759–72.
Sambathkumar R, Migliorini A, Nostro MC. Pluripotent stem cell-derived pancreatic progenitors and β-like cells for type 1 diabetes treatment. Physiology. 2018;33(6):394–402.
Sordi V, Monaco L, Piemonti L. Cell therapy for type 1 diabetes: from islet transplantation to stem cells. Hormone Res Paediatrics. 2022;96(6):658–69.
Henry RR, Pettus J, Wilensky J, SHAPIRO AJ, Senior PA, Roep B et al. Initial clinical evaluation of VC-01TM combination product—a stem cell–derived islet replacement for type 1 diabetes (T1D). Diabetes. 2018;67(Supplement_1).
Shapiro A, Thompson D, Donner TW, Bellin MD, Hsueh W, Pettus JH et al. Insulin expression and glucose-responsive circulating C-peptide in type 1 diabetes patients implanted subcutaneously with pluripotent stem cell-derived pancreatic endoderm cells in a macro-device. David and Donner, Thomas W and Bellin, Melena D and Hsueh, Willa and Pettus, Jeremy H and Wilensky, Jon S and Daniels, Mark and Wang, Richard M and Kroon, Evert J and Brandon, Eugene Paul and D’Amour, Kevin A and Foyt, Howard, Insulin Expression and Glucose-Responsive Circulating C-Peptide in Type. 2019;1.
Keymeulen B, Jacobs-Tulleneers-Thevissen D, Kroon EJ, Jaiman MS, Daniels M, Wang R et al. 196-LB: stem cell–derived islet replacement therapy (VC-02) demonstrates production of C-peptide in patients with type 1 diabetes (T1D) and hypoglycemia unawareness. Diabetes. 2021;70(Supplement_1).
Piemonti L. Felix dies natalis, insulin… ceterum autem censeo beta is better. Acta Diabetol. 2021;58(10):1287–306.
Sordi V, Pellegrini S, Piemonti L. Immunological issues after stem cell-based β cell replacement. Curr Diab Rep. 2017;17:1–8.
Coe TM, Markmann JF, Rickert CG. Current status of porcine islet xenotransplantation. Curr Opin Organ Transpl. 2020;25(5):449–56.
Edgar L, Pu T, Porter B, Aziz J, La Pointe C, Asthana A, et al. Regenerative medicine, organ bioengineering and transplantation. J Br Surg. 2020;107(7):793–800.
Mathur A, Taurin S, Alshammary S. The safety and efficacy of mesenchymal stem cells in the treatment of type 2 Diabetes- A literature review. Diabetes Metab Syndr Obes. 2023;16:769–77.
Hogrebe NJ, Ishahak M, Millman JR. Developments in stem cell-derived islet replacement therapy for treating type 1 diabetes. Cell Stem Cell. 2023;30(5):530–48.
Paraskevas S, Maysinger D, Wang R, Duguid WP, Rosenberg L. Cell loss in isolated human islets occurs by apoptosis. Pancreas. 2000;20(3):270–6.
Kelly OG, Chan MY, Martinson LA, Kadoya K, Ostertag TM, Ross KG, et al. Cell-surface markers for the isolation of pancreatic cell types derived from human embryonic stem cells. Nat Biotechnol. 2011;29(8):750–6.
Rezania A, Bruin JE, Riedel MJ, Mojibian M, Asadi A, Xu J, et al. Maturation of human embryonic stem cell–derived pancreatic progenitors into functional islets capable of treating pre-existing diabetes in mice. Diabetes. 2012;61(8):2016–29.
Kroon E, Martinson LA, Kadoya K, Bang AG, Kelly OG, Eliazer S, et al. Pancreatic endoderm derived from human embryonic stem cells generates glucose-responsive insulin-secreting cells in vivo. Nat Biotechnol. 2008;26(4):443–52.
Agulnick AD, Ambruzs DM, Moorman MA, Bhoumik A, Cesario RM, Payne JK, et al. Insulin-producing endocrine cells differentiated in vitro from human embryonic stem cells function in macroencapsulation devices in vivo. Stem Cells Translational Med. 2015;4(10):1214–22.
Ramzy A, Thompson DM, Ward-Hartstonge KA, Ivison S, Cook L, Garcia RV, et al. Implanted pluripotent stem-cell-derived pancreatic endoderm cells secrete glucose-responsive C-peptide in patients with type 1 diabetes. Cell Stem Cell. 2021;28(12):2047–61. e5.
Dolgin E, Diabetes. Encapsulating the problem. Nature. 2016;540(7632):S60–2.
Rezania A, Bruin JE, Arora P, Rubin A, Batushansky I, Asadi A, et al. Reversal of diabetes with insulin-producing cells derived in vitro from human pluripotent stem cells. Nat Biotechnol. 2014;32(11):1121–33.
Hogrebe NJ, Augsornworawat P, Maxwell KG, Velazco-Cruz L, Millman JR. Targeting the cytoskeleton to direct pancreatic differentiation of human pluripotent stem cells. Nat Biotechnol. 2020;38(4):460–70.
Nair GG, Liu JS, Russ HA, Tran S, Saxton MS, Chen R, et al. Recapitulating endocrine cell clustering in culture promotes maturation of human stem-cell-derived β cells. Nat Cell Biol. 2019;21(2):263–74.
Shapiro AJ, Thompson D, Donner TW, Bellin MD, Hsueh W, Pettus J et al. Insulin expression and C-peptide in type 1 diabetes subjects implanted with stem cell-derived pancreatic endoderm cells in an encapsulation device. Cell Rep Med. 2021;2(12).
Witkowski P, Anteby R, Olaitan OK, Forbes RC, Niederhaus S, Ricordi C, et al. Pancreatic islets Quality and Potency cannot be verified as required for drugs: reflection on the FDA Review of a biological license application for human islets. Transplantation. 2021;105(12):e409–10.
Download references
Acknowledgements
Author information, authors and affiliations.
Noncommunicable Diseases Research Center, Neyshabur University of Medical Sciences, Neyshabur, Iran
Ramin Raoufinia
Department of Medical Genetics and Molecular Medicine, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
Ramin Raoufinia, Hamid Reza Rahimi, Ehsan Saburi & Meysam Moghbeli
You can also search for this author in PubMed Google Scholar
Contributions
RR, HRR, and ES were involved in search strategy and drafting. MM revised, designed, and supervised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Meysam Moghbeli .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Raoufinia, R., Rahimi, H.R., Saburi, E. et al. Advances and challenges of the cell-based therapies among diabetic patients. J Transl Med 22 , 435 (2024). https://doi.org/10.1186/s12967-024-05226-3
Download citation
Received : 14 February 2024
Accepted : 22 April 2024
Published : 08 May 2024
DOI : https://doi.org/10.1186/s12967-024-05226-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cell therapy
- Translplantation
- Immunosuppression
Journal of Translational Medicine
ISSN: 1479-5876
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
A bibliometric perspective to the most cited diabetes articles
- Research article
- Published: 26 February 2023
- Volume 22 , pages 763–773, ( 2023 )
Cite this article

- Gulru Ulugerger Avci ORCID: orcid.org/0000-0002-5661-1738 1
297 Accesses
Explore all metrics
This bibliometric analysis aims to evaluate the characteristics and impact of the top 100 cited articles published under the title of diabetes mellitus.
We performed to define the most cited articles in diabetes research by using the Web of Science. The papers were analyzed in terms of their year of publication, journal of publication, authors, impact factor (IF), total citations number, the average number of citations per year, studies topic, and type.
The number of citations ranged from 1519 to 17.298. They were published from 1987 to 2018. The most cited articles were published in the New England Journal of Medicine (n = 26), followed by Diabetes Care (n = 17) and Lancet (n = 9). The original scientific paper was the most popular article type (46%), followed by review article (36%). The generality studies’ subject was about treatment (n = 22), followed by pathogenesis (n = 19), etiology and risk factors (n = 16), diagnosis, screening, classification (n = 15), epidemiology (n = 11), prevention (n = 11) and complications (n = 6). There was a correlation between the average number of citations per year (ACpY) and IF (p = < 0.010, r = 0.259), citations and ACpY (p = < 0.001, r = 0.646), citations and time (p = 0.008, r = 0.266).
This study showed that original scientific papers were the most-cited and more articles were published in influential journals. Articles on diabetes treatment and pathogenesis were popular topics. Future interventions should focus on the management and prevention of diabetes.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
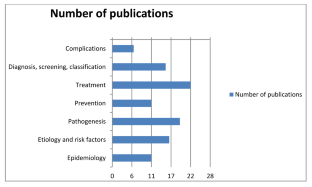
Similar content being viewed by others
The top 100 most cited scientific reports focused on diabetes research.
Type 1 diabetes in children: a scientometric assessment of Indian research output from 1990 to 2019
Bibliometric overview of the Tehran Lipid and Glucose Study (TLGS) publications from 2000 to 2022
International Diabetes Federation. (2021) IDF Diabetes atlas. 10th edn. http://www.idf.org/diabetesatlas .
Bellary S, Kyrou I, Brown JE, Bailey CJ. Type 2 diabetes mellitus in older adults: clinical considerations and management. Nat Rev Endocrinol. 2021;17(9):534–48. https://doi.org/10.1038/s41574-021-00512-2 .
Article PubMed Google Scholar
Okaiyeto K, Oguntibeju OO. Trends in diabetes research outputs in South Africa over 30 years from 2010 to 2019: a bibliometric analysis. Saudi J Biol Sci. 2021;28(5):2914–24. https://doi.org/10.1016/j.sjbs.2021.02.025 .
Article PubMed PubMed Central Google Scholar
Cole JB, Florez JC. Genetics of diabetes mellitus and diabetes complications. Nat Rev Nephrol. 2020;16(7):377–90. https://doi.org/10.1038/s41581-020-0278-5 .
Shuaib W, Costa JL. Anatomy of success: 100 most cited articles in diabetes research. Therapeutic Adv Endocrinol Metabolism. 2015;6(4):163–73. https://doi.org/10.1177/2042018815580254 .
Article CAS Google Scholar
Yang Y, Ma Y, Chen L, Liu Y, Zhang Y. The 100 Top-Cited Systematic Reviews/Meta-Analyses on Diabetic Research. J Diabetes Res . 2020;2020:5767582. Published 2020 Sep 11. doi: https://doi.org/10.1155/2020/5767582
Bektan Kanat B, Yavuzer H. Top 100 articles on vitamin D: bibliometric versus altmetric analysis. Bratisl Lek Listy. 2022;123(3):160–71. https://doi.org/10.4149/BLL_2022_027 .
Diagnostic criteria and classification. Of hyperglycaemia first detected in pregnancy: a World Health Organization Guideline. Diabetes Res Clin Pract. 2014;103(3):341–63. https://doi.org/10.1016/j.diabres.2013.10.012 .
Article Google Scholar
Stout NL, Alfano CM, Belter CW, Nitkin R, Cernich A, Lohmann SK, et al. A bibliometric analysis of the landscape of cancer rehabilitation research (1992–2016. J Natl Cancer Inst. 2018;110(8):815–24. https://doi.org/10.1093/jnci/djy108 .
Chen X, Chen J, Cheng G, Gong T. Topics and trends in artificial intelligence assisted human brain research. PLoS One. 2020;15(4):e231192.
Coverage analysis of Scopus: a journal metric approach. de Moya-Anegón, Chinchilla-Rodríguez F, Vargas-Quesada Z. B, Corera-Álvarez E, Muñoz-Fernández F, González-Molina A. Scientometrics 2007;73 (1):53–78.
Garfield E. 100 citation classics from the Journal of the American Medical Association. JAMA. 1987;257(1):52–9.
Article CAS PubMed Google Scholar
Diabetes Control and Complications Trial Research Group, Nathan DM, Genuth S, et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–86. https://doi.org/10.1056/NEJM199309303291401 .
Shuaib W, Costa JL. Anatomy of success: 100 most cited articles in diabetes research. Ther Adv Endocrinol Metab. 2015;6(4):163–73. https://doi.org/10.1177/2042018815580254 .
Article CAS PubMed PubMed Central Google Scholar
Rosas S, Schouten J, Cope M, Kagan J. Modeling the dissemination and uptake of clinical trials results. Res Eval. 2013;22:179–86.
Aksnes DW, Langfeldt L. Wouters. Citations, citation indicators, and research quality: an overview of basic concepts and theories. SAGE Open. 2019;9. https://doi.org/10.1177/2158244019829575 .
Song Y, Ma P, Gao Y, Xiao P, Xu L, Liu H. A Bibliometrics Analysis of Metformin Development from 1980 to 2019. Front Pharmacol. 2021;12:645810. https://doi.org/10.3389/fphar.2021.645810 . Published 2021 Apr 28.
Rena G, Hardie DG, Pearson ER. The Mechanisms of Action of Metformin. Diabetologia. 2017;60(9):1577–85. https://doi.org/10.1007/s00125-017-4342-z .
Forslund K, Hildebrand F, Hildebrand F, Nielsen T, Falony G, Le Chatelier E, et al. Disentangling type 2 diabetes and Metformin Treatment Signatures in the human gut microbiota. Nature. 2015;528(7581):262–6. https://doi.org/10.1038/nature15766 .
Moghetti P, Castello R, Negri C, Tosi F, Perrone F, Caputo M, et al. Metformin Effects on clinical features, endocrine and metabolic profiles, and insulin sensitivity in polycystic ovary syndrome: a Randomized, Double-Blind, placebo-controlled 6-Month Trial, followed by Open, Long-Term Clinical Evaluation1. J Clin Endocrinol Metab. 2000;85(1):139–46. https://doi.org/10.1210/jcem.85.1.6293 .
Palmer SC, Tendal B, Mustafa RA et al. Sodium-glucose cotransporter protein-2 (SGLT-2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists for type 2 diabetes: systematic review and network meta-analysis of randomised controlled trials [published correction appears in BMJ. 2022 Jan 18;376:o109]. BMJ . 2021;372:m4573. Published 2021 Jan 13. doi: https://doi.org/10.1136/bmj.m4573
Liu H, Guo L, Xing J, et al. The protective role of DPP4 inhibitors in atherosclerosis. Eur J Pharmacol. 2020;875:173037. https://doi.org/10.1016/j.ejphar.2020.173037 .
Deacon CF. Dipeptidyl peptidase 4 inhibitors in the treatment of type 2 diabetes mellitus. Nat Rev Endocrinol. 2020;16(11):642–53. https://doi.org/10.1038/s41574-020-0399-8 .
Naderpoor N, Shorakae S, Joham A, Boyle J, De Courten B, Teede HJ. Obesity and polycystic ovary syndrome. Minerva Endocrinol. 2015;40(1):37–51.
CAS PubMed Google Scholar
Brown AE, Walker M. Genetics of insulin resistance and the metabolic syndrome. Curr Cardiol Rep. 2016;18(8):75. https://doi.org/10.1007/s11886-016-0755-4 .
Kautzky-Willer A, Harreiter J, Pacini G. Sex and gender differences in risk, pathophysiology and complications of type 2 diabetes Mellitus. Endocr Rev. 2016 Jun;37(3):278–316. https://doi.org/10.1210/er.2015-1137 . Epub 2016 May 9. PMID: 27159875; PMCID: PMC4890267.
Alberti KG, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the study of obesity. Circulation. 2009;120(16):1640–5.
Zou L, Sun L. Global diabetic kidney disease research from 2000 to 2017. Medicine. 2019;98(6):e14394. https://doi.org/10.1097/MD.0000000000014394 .
Jaiswal M, Schinske A, Pop-Busui R. Lipids and lipid management in diabetes. Best Pract Res Clin Endocrinol Metab. 2014;28(3):325–38. https://doi.org/10.1016/j.beem.2013.12.001 .
Iftikhar PM, Ali F, Faisaluddin M, Khayyat A, De Gouvia De Sa M, Rao T. A bibliometric analysis of the top 30 most-cited Articles in Gestational Diabetes Mellitus Literature (1946–2019). Cureus. 2019;11(2):e4131. https://doi.org/10.7759/cureus.413 . Published 2019 Feb 25.
Download references
The authors declare this study to have received no financial support.
Author information
Authors and affiliations.
Division of Geriatric Medicine, Department of Internal Medicine, Cerrahpasa Medical Faculty, Istanbul University-Cerrahpasa, Istanbul, Turkey
Gulru Ulugerger Avci
You can also search for this author in PubMed Google Scholar
Contributions
G UA: concept and design, interpretation of data, analyzed, wrote, reviewed, edited and approved the manuscript.
Corresponding author
Correspondence to Gulru Ulugerger Avci .
Ethics declarations
Conflict of interest.
The authors report no conflict of interest and no competing interests.
Ethical statement
All authors declare that the research has been conducted according to the principles of the World Medical Association Declaration of Helsinki “Ethical Principles for Medical Research Involving Human Subjects.” This study does not require approval from an ethics committee, because it performs a bibliometric analysis/citation analysis of the existing published classical studies.
Informed consent
Informed consent is not required as our work is a retrospective international data study.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Ulugerger Avci, G. A bibliometric perspective to the most cited diabetes articles. J Diabetes Metab Disord 22 , 763–773 (2023). https://doi.org/10.1007/s40200-023-01199-0
Download citation
Received : 27 May 2022
Accepted : 13 February 2023
Published : 26 February 2023
Issue Date : June 2023
DOI : https://doi.org/10.1007/s40200-023-01199-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Bibliometrics
- Top 100 citations
- Impact factors
- Find a journal
- Publish with us
- Track your research

- Previous Article
- Next Article
Article Information
Summary and conclusion.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Thomas W. Gardner; Summary and Conclusion. ADA Clinical Compendia 1 May 2019; 2019 (1): 21. https://doi.org/10.2337/db20191-21
Download citation file:
- Ris (Zotero)
- Reference Manager
The worldwide diabetes epidemic has created an unsustainable financial and personal crisis for health care systems and for patients and their families. At the same time, the ability of patients to maintain useful vision has never been greater. Screening of people who are at risk and timely institution of treatment, combined with coordination of systematic and ophthalmic care, provides the best outlook for people with diabetes.
The opinions expressed are those of the authors and do not necessarily reflect those of Genentech or the American Diabetes Association. The content was developed by the authors and does not represent the policy or position of the American Diabetes Association, any of its boards or committees, or any of its journals or their editors or editorial boards.
To request permission to reuse or reproduce any portion of this publication, please contact [email protected] .
Dualities of Interest
T.W.G. has received research support from Zebra Biologics and consulting fees from Novo Nordisk.
C.C.W. has received research support from Adverum, Allergan, Apellis, Clearside, Genentech, Roche, Neurotech, Novartis, Opthea, Regeneron, Regenxbio, Samsung, and Santen; is a consultant for Adverum, Alimera Sciences, Allegro, Allergan, Apellis, Bayer, Clearside, EyePoint, Genentech, Kodiak, Novartis, Regeneron, Regenxbio, and Roche; and is a speaker for Regeneron.
B.A.C. has been a speaker for Novo Nordisk and served on an advisory board for Regeneron.
No other potential conflicts of interest relevant to this compendium were reported.
Acknowledgments
Editorial and project management services were provided by Debbie Kendall of Kendall Editorial in Richmond, VA.
Author Contributions
All authors researched and wrote their respective sections. Lead author T.W.G. reviewed all content and is the guarantor of this work.
Email alerts
- Online ISSN 2771-6880
- Print ISSN 2771-6872
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
357 Diabetes Essay Topics & Examples
When you write about the science behind nutrition, heart diseases, and alternative medicine, checking titles for diabetes research papers can be quite beneficial. Below, our experts have gathered original ideas and examples for the task.
🏆 Best Diabetes Essay Examples & Topics
⭐ most interesting diabetes research paper topics, ✅ simple & easy diabetes essay topics, 🎓 good research topics about diabetes, 💡 interesting topics to write about diabetes, 👍 good essay topics on diabetes, ❓ diabetes research question examples.
- Type 2 Diabetes The two major types of diabetes are type 1 diabetes and type 2 diabetes. Doctor: The first step in the treatment of type 2 diabetes is consumption of healthy diet.
- Adult-Onset Type 2 Diabetes: Patient’s Profile Any immediate care as well as post-discharge treatment should be explained in the best manner possible that is accessible and understandable to the patient.
- Living With a Chronic Disease: Diabetes and Asthma This paper will look at the main effects of chronic diseases in the lifestyle of the individuals and analyze the causes and the preventive measures of diabetes as a chronic disease.
- Leadership in Diabetes Management Nurses can collaborate and apply evidence-based strategies to empower their diabetic patients. The involvement of all key stakeholders is also necessary.
- Diabetes in Adults in Oxfordshire On a national level, Diabetes Research and Wellness Foundation aims to prevent the spread of the decease through research of the causes and effective treatment of diabetes 2 type.
- Case Study of Patient with DKA and Diabetes Mellitus It is manifested by a sharp increase in glucose levels and the concentration of ketone bodies in the blood, their appearance in the urine, regardless of the degree of violation of the patient’s consciousness.
- Intervention Methods for Type 2 Diabetes Mellitus An individual should maintain a regulated glycemic control using the tenets of self-management to reduce the possibility of complications related to diabetes.
- Relation Between Diabetes And Nutrition Any efforts to lessen and eliminate the risk of developing diabetes must involve the dietary habit of limiting the consumption of carbohydrates, sugar, and fats. According to Belfort-DeAguiar and Dongju, the three factors of obesity, […]
- Diabetes Mellitus: Symptoms, Types, Effects Insulin is the hormone that controls the levels of glucose in the blood, and when the pancreas releases it, immediately the high levels are controlled, like after a meal.
- Health Promotion: Diabetes Mellitus and Comorbidities This offers a unique challenge in the management of diabetes and other chronic diseases; the fragmented healthcare system that is geared towards management of short-term medical emergencies often is not well prepared for the patient […]
- Type 2 Diabetes as a Public Health Issue In recent years, a steady increase in the incidence and prevalence of diabetes is observed in almost all countries of the world.
- Diabetes Management: Case Study Type 1 and Type 2 diabetes contrast based on their definitions, the causes, and the management of the conditions. Since the CDC promotes the avoidance of saturated fat and the increase of fiber intake for […]
- Diabetes Mellitus Management in the Elderly Diabetes mellitus is a health complication involving an increase in the concentration in the concentration of blood sugar either due to a failure by cells to effectively respond to the production of insulin in the […]
- A Study of Juvenile Type 1 Diabetes in the Northwest of England The total number of children under seventeen years living with type 1 diabetes in North West England by 2009 was 2,630.
- Diabetes Prevention: The Sanofi-Aventis Leaflet Review Using the Flesh formula, it can be concluded that the leaflet has a good level of readability, but it can be improved in case it is shorter because a few sections of it are better […]
- Gestational Diabetes in a 38-Year-Old Woman The concept map, created to meet B.’s needs, considers her educational requirements and cultural and racial hurdles to recognize her risk factors and interventions to increase her adherence to the recommended course of treatment.B.said in […]
- Type 2 Diabetes Mellitus and Its Implications You call an ambulance and she is taken in to the ED. Background: Jean is still very active and works on the farm 3 days a week.
- Development of Comprehensive Inpatient and Outpatient Programs for Diabetes Overcoming the fiscal and resource utilization issues in the development of a comprehensive diabetes program is essential for the improvement of health and the reduction of treatment costs.
- Healthcare Cost Depending on Chronic Disease Management of Diabetes and Hypertension A sufficient level of process optimization and the presence of a professional treating staff in the necessary number will be able to help improve the indicators.
- Improving Glycemic Control in Black Patients with Type 2 Diabetes Information in them is critical for answering the question and supporting them with the data that might help to acquire an enhanced understanding of the issue under research. Finally, answering the PICOT question, it is […]
- Shared Decision-Making That Affects the Management of Diabetes The article by Peek et al.is a qualitative study investigating the phenomenon of shared decision-making that affects the management of diabetes. The researchers demonstrate the racial disparity that can arise in the choice of approaches […]
- Managing Obesity as a Strategy for Addressing Type 2 Diabetes When a patient, as in the case of Amanda, requires a quick solution to the existing problem, it is necessary to effectively evaluate all options in the shortest possible time.
- Tests and Screenings: Diabetes and Chronic Kidney Disease The test is offered to patients regardless of gender, while the age category is usually above 45 years. CDC1 recommends doing the test regardless of gender and is conducted once or twice to check the […]
- Obesity Management for the Treatment of Type 2 Diabetes American Diabetes Association states that for overweight and obese individuals with type 2 diabetes who are ready to lose weight, a 5% weight reduction diet, physical exercise, and behavioral counseling should be provided.
- COVID-19 and Diabetes Mellitus Lim et al, in their article, “COVID-19 and diabetes mellitus: from pathophysiology to clinical management”, explored how COVID-19 can worsen the symptoms of diabetes mellitus.
- The Importance of Physical Exercise in Diabetes II Patients The various activities help to improve blood sugar levels, reduce cardiovascular cases and promote the overall immunity of the patient. Subsequently, the aerobic part will help to promote muscle development and strengthen the bones.
- Diabetes Education Workflow Process Mapping DSN also introduces the patient to the roles of specialists involved in managing the condition, describes the patient’s actions, and offers the necessary educational materials.
- Diabetes: Treatment Complications and Adjustments One of the doctor’s main priorities is to check the compatibility of a patient’s medications. The prescriptions of other doctors need to be thoroughly checked and, if necessary, replaced with more appropriate medication.
- The Type 2 Diabetes Mellitus PICOT (Evidence-Based) Project Blood glucose levels, A1C, weight, and stress management are the parameters to indicate the adequacy of physical exercise in managing T2DM.
- Chronic Disease Cost Calculator (Diabetes) This paper aims at a thorough, detailed, and exhaustive explanation of such a chronic disease as diabetes in terms of the prevalence and cost of treatment in the United States and Maryland.
- Diabetes Mellitus Epidemiology Statistics This study entails a standard established observation order from the established starting time to an endpoint, in this case, the onset of disease, death, or the study’s end. It is crucial to state this value […]
- Epidemiology: Type II Diabetes in Hispanic Americans The prevalence of type II diabetes in Hispanic Americans is well-established, and the search for inexpensive prevention methods is in the limelight.
- Diabetes: Risk Factors and Effects Trends in improved medical care and the development of technology and medicine are certainly contributing to the reduction of the problem. All of the above indicates the seriousness of the problem of diabetes and insufficient […]
- Barriers to Engagement in Collaborative Care Treatment of Uncontrolled Diabetes The primary role of physicians, nurses, and other healthcare team members is to provide patients with medical treatment and coordinate that care while also working to keep costs down and expand access.
- Hereditary Diabetes Prevention With Lifestyle Modification Yeast infections between the fingers and toes, beneath the breast, and in or around the genital organs are the common symptoms of type 2 diabetes.
- Health Equity Regarding Type 2 Diabetes According to Tajkarimi, the number of research reports focusing on T2D’s prevalence and characteristics in underserved minorities in the U. Adapting the program’s toolkits to rural Americans’ eating and self-management habits could also be instrumental […]
- Diabetes Mellitus: Treatment Methods Moreover, according to the multiple findings conducted by Park et al, Billeter et al, and Tsilingiris et al, bariatric surgeries have a positive rate of sending diabetes into remission.
- Diagnosing Patient with Insulin-Dependent Diabetes The possible outcomes of the issues that can be achieved are discussing the violations with the patient’s family and convincing them to follow the medical regulations; convincing the girl’s family to leave her at the […]
- Human Service for Diabetes in Late Adulthood The mission of the Georgia Diabetic Foot Care Program is to make a positive difference in the health of persons living with diabetes.
- Diabetes: Symptoms and Risk Factors In terms of the problem, according to estimates, 415 million individuals worldwide had diabetes mellitus in 2015, and it is expected to rise to 642 million by the year 2040.
- Diabetes: Types and Management Diabetes is one of the most prevalent diseases in the United States caused when the body fails to optimally metabolize food into energy.
- Type 2 Diabetes’ Impact on Australian Society Consequently, the most significant impact of the disease is the increased number of deaths among the population which puts their lives in jeopardy. Further, other opportunistic diseases are on the rise lowering the quality of […]
- Epidemiology of Diabetes and Forecasted Trends The authors note that urbanization and the rapid development of economies of different countries are the main causes of diabetes. The authors warn that current diabetes strategies are not effective since the rate of the […]
- The Aboriginal Diabetes Initiative in Canada The ADI’s goal in the CDS was to raise type 2 diabetes awareness and lower the incidence of associated consequences among Aboriginal people.
- Communicating the Issue of Diabetes The example with a CGM sensor is meant to show that doctors should focus on educating people with diabetes on how to manage their condition and what to do in extreme situations.
- Obesity and Diabetes Mellitus Type 2 The goal is to define the features of patient information to provide data on the general course of the illness and its manifestations following the criteria of age, sex, BMI, and experimental data.
- The Prevention of Diabetes and Its Consequences on the Population At the same time, these findings can also be included in educational programs for people living with diabetes to warn them of the risks of fractures and prevent them.
- Uncontrolled Type 2 Diabetes and Depression Treatment The data synthesis demonstrates that carefully chosen depression and anxiety treatment is likely to result in better A1C outcomes for the patient on the condition that the treatment is regular and convenient for the patients.
- Type 2 Diabetes: Prevention and Education Schillinger et al.came to the same conclusion; thus, their findings on the study of the Bigger Picture campaign effectiveness among youth of color are necessary to explore diabetes prevention.
- A Diabetes Quantitative Article Analysis The article “Correlates of accelerometer-assessed physical activity and sedentary time among adults with type 2 diabetes” by Mathe et al.refers to the global issue of the prevention of diabetes and its complications.
- A Type 2 Diabetes Quantitative Article Critique Therefore, the main issue is the prevention of type 2 diabetes and its consequences, and this paper will examine one of the scientific studies that will be used for its exploration.
- The Diabetes Prevention Articles by Ford and Mathe The main goal of the researchers was to measure the baseline MVPA of participants and increase their activity to the recommended 150 minutes per week through their participation in the Diabetes Community Lifestyle Improvement Program.
- Type 2 Diabetes in Hispanic Americans The HP2020 objectives and the “who, where, and when” of the problem highlight the significance of developing new, focused, culturally sensitive T2D prevention programs for Hispanic Americans.
- Diabetes Mellitus as Problem in US Healthcare Simultaneously, insurance companies are interested in decreasing the incidence of diabetes to reduce the costs of testing, treatment, and provision of medicines.
- Diabetes Prevention as a Change Project All of these queries are relevant and demonstrate the importance of including people at high risk of acquiring diabetes in the intervention.
- Evidence Synthesis Assignment: Prevention of Diabetes and Its Complications The purpose of this research is to analyze and synthesize evidence of good quality from three quantitative research and three non-research sources to present the problem of diabetes and justify the intervention to address it.
- Diabetes Mellitus: Causes and Health Challenges Second, the nature of this problem is a clear indication of other medical concerns in this country, such as poor health objectives and strategies and absence of resources.
- Diabetes Mellitus (DM) Disorder Case Study Analysis Thus, informing the patient about the importance of regular medication intake, physical activity, and adherence to diet in maintaining diabetes can solve the problem.
- Diabetes Mellitus in Young Adults Thus, programs for young adults should predominantly focus on the features of the transition from adolescence to adulthood. As a consequence, educational programs on diabetes improve the physical and psychological health of young adults.
- A Healthcare Issue of Diabetes Mellitus Diabetes mellitus is seen as a primary healthcare issue that affects populations across the globe and necessitates the combination of a healthy lifestyle and medication to improve the quality of life of people who suffer […]
- Control of LDL Cholesterol Levels in Patients, Gestational Diabetes Mellitus In addition, some patients with hypercholesterolemia may have statin intolerance, which reduces adherence to therapy, limits treatment efficacy, and increases the risk of CVD.
- Exploring Glucose Tolerance and Gestational Diabetes Mellitus In the case of a glucose tolerance test for the purpose of diagnosing GDM type, the interpretation of the test results is carried out according to the norms for the overall population.
- Type 2 Diabetes Health Issue and Exercise This approach will motivate the patient to engage in exercise and achieve better results while reducing the risk of diabetes-related complications.
- Diabetes Interventions in Children The study aims to answer the PICOT Question: In children with obesity, how does the use of m-Health applications for controlling their dieting choices compare to the supervision of their parents affect children’s understanding of […]
- Diabetes Tracker Device and Its Advantages The proposed diabetes tracker is a device that combines the functionality of an electronic BGL tester and a personal assistant to help patients stick to their diet plan.
- Disease Management for Diabetes Mellitus The selection of the appropriate philosophical and theoretical basis for the lesson is essential as it allows for the use of an evidence-based method for learning about a particular disease.
- Latino People and Type 2 Diabetes The primary aim of the study is to determine the facilitators and barriers to investigating the decision-making process in the Latin population and their values associated with type 2 diabetes.
- Diabetes Self-Management Education and Support Program The choice of this topic and question is based on the fact that despite the high prevalence of diabetes among adolescents in the United States, the use of DSMES among DM patients is relatively low, […]
- Diabetes Mellitus Care Coordination The aim is to establish what medical technologies, care coordination and community resources, and standards of nursing practice contribute to the quality of care and safety of patients with diabetes.
- Healthy Lifestyle Interventions in Comorbid Asthma and Diabetes In most research, the weight loss in cases of comorbid asthma and obesity is reached through a combination of dietary interventions and physical exercise programs.
- PDSA in Diabetes Prevention The second step in the “Do” phase would be to isolate a few members of the community who are affected by diabetes voluntarily.
- Diabetes: Statistics, Disparities, Therapies The inability to produce adequate insulin or the body’s resistance to the hormone is the primary cause of diabetes. Diabetes is a serious health condition in the U.S.and the world.
- Type 2 Diabetes Prescriptions and Interventions The disadvantage is the difficulty of obtaining a universal model due to the complexity of many factors that can affect the implementation of recommendations: from the variety of demographic data to the patient’s medical history.
- Health Education for Female African Americans With Diabetes In order to address and inform the public about the challenges, nurses are required to intervene by educating the population on the issues to enhance their understanding of the risks associated with the conditions they […]
- Diabetes Risk Assessment and Prevention It is one of the factors predisposing patients suffering from diabetes to various cardiovascular diseases. With diabetes, it is important to learn how to determine the presence of carbohydrates in foods.
- Diabetes Mellitus: Preventive Measures In addition to addressing the medical specialists who will be of service in disease prevention, it will emphasize the intervention programs required to help control the spread of the illness.
- “The Diabetes Online Community” by Litchman et al. The researchers applied the method of telephone interviews to determine the results and effectiveness of the program. The study described the value of DOC in providing support and knowledge to older diabetes patients.
- Mobile App for Improved Self-Management of Type 2 Diabetes The central focus of the study was to assess the effectiveness of the BlueStar app in controlling glucose levels among the participants.
- Type 2 Diabetes in Minorities from Cultural Perspective The purpose of this paper is to examine the ethical and cultural perspectives on the issue of T2DM in minorities. Level 2: What are the ethical obstacles to treating T2DM in ethnic and cultural minorities?
- Ethics of Type 2 Diabetes Prevalence in Minorities The purpose of this article analysis is to dwell on scholarly evidence that raises the question of ethical and cultural aspects of T2DM prevalence in minorities.
- Type 2 Diabetes in Minorities: Research Questions The Level 2 research questions are: What are the pathophysiological implications of T2DM in minorities? What are the statistical implications of T2DM in minorities?
- Improving Adherence to Diabetes Treatment in Primary Care Settings Additionally, the patients from the intervention group will receive a detailed explanation of the negative consequences of low adherence to diabetes treatment.
- An Advocacy Tool for Diabetes Care in the US To ensure the implementation and consideration of my plea, I sent a copy of the letter to the government officials so it could reach the president.
- Diabetes and Allergies: A Statistical Check The current dataset allowed us to test the OR for the relationship between family history of diabetes and the presence of diabetes in a particular patient: all variables were dichotomous and discrete and could take […]
- Type 2 Diabetes in Adolescents According to a National Diabetes Statistics Report released by the Centers for Disease Control and Prevention, the estimated prevalence of the disease was 25 cases per 10,000 adolescents in 2017. A proper understanding of T2D […]
- Analysis of Diabetes and Its Huge Effects In the US, diabetes is costly to treat and has caused much physical, emotional and mental harm to the people and the families of those who have been affected by the disease.
- Nursing: Self-Management of Type II Diabetes Sandra Fernandes and Shobha Naidu’s journal illustrates the authors’ understanding of a significant topic in the nursing profession.”Promoting Participation in self-care management among patients with diabetes mellitus” article exposes readers to Peplau’s theory to understand […]
- The Impact of Vegan and Vegetarian Diets on Diabetes Vegetarian diets are popular for a variety of reasons; according to the National Health Interview Survey in the United States, about 2% of the population reported following a vegetarian dietary pattern for health reasons in […]
- “Diabetes Prevention in U.S. Hispanic Adults” by McCurley et al. This information allows for supposing that face-to-face interventions can be suitable to my practicum project that considers measures to improve access to care among African Americans with heart failure diseases. Finally, it is possible to […]
- Diabetes Disease of the First and Second Types It is a decrease in the biological response of cells to one or more effects of insulin at its average concentration in the blood. During the first type of diabetes, insulin Degludec is required together […]
- The Trend of the Higher Prevalence of Diabetes According to the CDC, while new cases of diabetes have steadily decreased over the decades, the prevalence of the disease among people aged below twenty has not.
- Person-Centered Strategy of Diabetes and Dementia Care The population of focus for this study will be Afro-American women aged between sixty and ninety who have diabetes of the second type and dementia or are likely to develop dementia in the future.
- Video Consultations Between Patients and Clinicians in Diabetes, Cancer, and Heart Failure Services For example, during one of my interactions with the patient, I was asked whether the hospital had the policy to avoid face-to-face interaction during the pandemic with the help of video examinations.
- Diets to Prevent Heart Disease, Cancer, and Diabetes In order to prevent heart disease, cancer, and diabetes, people are required to adhere to strict routines, including in terms of diet. Additionally, people wanting to prevent heart disease, cancer, and diabetes also need to […]
- The Centers for Diabetes’ Risks Assessment In general, the business case for the Centers for Diabetes appears to be positive since the project is closely aligned with the needs of the community and the targets set by the Affordable Care Act.
- Diabetes Mellitus as Leading Cause of Disability The researchers used data from the Centers for Disease Control and Prevention, where more than 12% of older people in the US live with the condition.
- Depression in Diabetes Patients The presence of depression concomitant to diabetes mellitus prevents the adaptation of the patient and negatively affects the course of the underlying disease.
- The Relationship Between Diabetes and COVID-19 After completing the research and analyzing the articles, it is possible to suggest a best practice that may be helpful and effective in defining the relationship between diabetes and COVID-19 and providing a way to […]
- Pre-diabetes and Urinary Incontinence Most recent reports indicate that a physiotherapy procedure gives a positive result in up to 80% of patients with stage I or SUI and mixed form and 50% of patients with stage II SUI.
- Type 1 Diabetes: Recommendations for Alternative Drug Treatments Then, they have to assess the existing levels of literacy and numeracy a patient has. Tailoring educational initiatives to a person’s unique ethnic and cultural background is the basis of cultural competence in patient education.
- Type 2 Diabetes: A Pharmacologic Update Diabetes presents one of the most common diagnoses in causes of ED visits among adults and one of the leading causes of death in the United States.
- Type 2 Diabetes and Its Treatment The main difference in type 2 diabetes is the insensitivity of the body’s cells to the action of the hormone insulin and their insulin resistance.
- Diabetes: Vulnerability, Resilience, and Care In nursing care, resilience is a critical concept that shows the possibility of a person to continue functioning and meeting objectives despite the existing challenges.
- Diabetes Prevention in the United States The analysis of these policies and the other strategies provides the opportunity to understand what role they might play in the improvement of human health. NDPP policy, on the other hand, emphasizes the role of […]
- Teaching Experience: Diabetes Prevention The primary objective of the seminar is to reduce the annual number of diabetes cases and familiarize the audience with the very first signs of this disease.
- Summary of Type 2 Diabetes: A Pharmacologic Update The authors first emphasize that T2D is one of the most widespread diseases in the United States and the seventh leading cause of death.
- Insulin Effects in a Diabetes Person I will use this source to support my research because the perception of diabetes patients on insulin therapy is essential for understanding the impact they cause on the person.
- Diabetes and Medical Intervention In the research conducted by Moin et al, the authors attempted to define the scope of efficiency of such a tool as an online diabetes prevention program in the prevention of diabetes among obese/overweight population […]
- Diabetes Mellitus Type 2 and a Healthy Lifestyle Relationship The advantage of this study over the first is that the method uses a medical approach to determining the level of fasting glucose, while the dependences in the study of Ugandans were found using a […]
- Diabetes and Its Economic Effect on Healthcare For many years, there has been an active increase in the number of cases of diabetes of all types among the global population, which further aggravates the situation.
- Diabetes: Epidemiological Analysis I would like to pose the following question: how can epidemiology principles be applied to these statistics for further improvements of policies that aim to reduce the impact of diabetes on the U.S.population? The limited […]
- Pathogenesis and Prevention of Diabetes Mellitus and Hypertension The hormone is produced by the cells of the islets of Langerhans found in the pancreas. It is attributed to the variation in the lifestyle of these individuals in these two geographical zones.
- Parental Intervention on Self-Management of an Adolescent With Diabetes Diabetes development and exposure are strongly tied to lifestyle, and the increasing incidents rate emphasizes the severity of the population’s health problem.
- Addressing the Needs of Hispanic Patients With Diabetes Similarly, in the program at hand, the needs of Hispanic patients with diabetes will be considered through the prism of the key specifics of the community, as well as the cultural background of the patients.
- Diabetes Issues: Insulin Price and Unaffordability According to the forecast of researchers from Stanford University, the number of people with type 2 diabetes who need insulin-containing drugs in the world will increase by about 79 million people by 2030, which will […]
- Diabetes: Epidemiologic Study Design For instance, the range of their parents’ involvement in the self-management practices can be a crucial factor in treatment and control.
- What to Know About Diabetes? Type 1 diabetes is caused by autoimmune reaction that prevent realization of insulin in a body. Estimated 5-10% of people who have diabetes have type 1.
- Diabetes in Saudi Arabia It is expected that should this underlying factor be discovered, whether it is cultural, societal, or genetic in nature, this should help policymakers within Saudi Arabia create new governmental initiatives to address the problem of […]
- “Medical Nutrition Therapy: A Key to Diabetes Management and Prevention” Article Analysis In the process of MNT application, the dietitian keeps a record of the changes in the main components of food and other components of the blood such as blood sugars to determine the trend to […]
- Nutrition and Physical Activity for Children With a Diabetes When a child understands that the family supports him or her, this is a great way to bring enthusiasm in dealing with the disease.
- Global and Societal Implications of the Diabetes Epidemic The main aim of the authors of this article seems to be alerting the reader on the consequences of diabetes to the society and to the whole world.
- Diabetes and Hypertension Avoiding Recommendations Thus, the promotion of a healthy lifestyle should entail the encouragement of the population to cease smoking and monitor for cholesterol levels.
- Pregnant Women With Type I Diabetes: COVID-19 Disease Management The grounded theory was selected for the given topic, and there are benefits and drawbacks of utilizing it to study the experiences of pregnant women with type I diabetes and COVID-19.
- Current Recommendations for the Glycemic Control in Diabetes Management of blood glucose is one of the critical issues in the care of people with diabetes. Therefore, the interval of the A1C testing should also depend on the condition of the patient, the physician’s […]
- Diabetes Mellitus: Types, Causes, Presentation, Treatment, and Examination Diabetes mellitus is a chronic endocrinologic disease, which is characterized by increased blood glucose concentration.
- Diabetes Problem at Country Walk Community: Intervention and Evaluation This presentation develops a community health nursing intervention and evaluation tool for the diabetes problem affecting Country Walk community.
- The Minority Diabetes Initiative Act’s Analysis The bill provides the right to the Department of Health and Human Services to generate grants to public and nonprofit private health care institutions with the aim of providing treatment for diabetes in minority communities.
- Communication Challenges Between Nurses and Patients With Type 2 Diabetes According to Pung and Goh, one of the limitations of communication in a multicultural environment is the language barrier that manifests itself in the direct interaction of nurses with patients and in the engagement work […]
- Diabetes Type 2 from Management Viewpoint Demonstrate the effects of type 2 diabetes and provide background information on the disease; Discuss the management plans of diabetes centers and critically analyze the frameworks implemented in the hospitals; Examine the existing methodology models […]
- Nursing Plan for the Patient with Diabetes Type 2, HTN, and CAD The health of the population is the most valuable achievement of society, so the preservation and strengthening of it is an essential task in which everyone should participate without exception.
- Diagnosis and Classification of Diabetes Mellitus Diabetes is a serious public health concern that introduces a group of metabolic disorders caused by changes in the sugar blood level.
- Diabetes Mellitus Type II: A Case of a Female Adult Patient In this presentation, we are going to develop a care plan for a 47-year-old woman with a 3-year-old history of Diabetes Mellitus Type 2 (also known as Type II DM).
- Diabetes Insipidus: Disease Process With Implications for Healthcare Professionals This presentation will consider the topic of Diabetes Insipidus (DI) with a focus on its etiology and progress.
- The Nature of Type 1 Diabetes Mellitus Type 1 diabetes mellitus is a chronic autoimmune disease that has an active genetic component, which is identified by increased blood glucose levels, also known as hyperglycemia.
- Imperial Diabetes Center Field Study The purpose is to examine the leadership’s practices used to maintain and improve the quality and safety standards of the facility and, using the observations and scholarly research, offer recommendations for improvement.
- Diabetes Risk Assessment After completing the questionnaire, I learned that my risk for the development of diabetes is above average. Modern risk assessment tools allow identifying the current state of health and possibilities of developing the disease.
- The Role of Telenursing in the Management of Diabetes Type 1 Telemedicine is the solution that could potentially increase the coverage and improve the situation for many t1DM patients in the world.
- Health Issues of Heart Failure and Pediatric Diabetes As for the population, which is intended to participate in the research, I am convinced that there is the need to specify the patients who should be examined and monitored.
- Juvenile Diabetes: Demographics, Statistics and Risk Factors Juvenile diabetes, also referred to as Type 2 diabetes or insulin-dependent diabetes, describes a health condition associated with the pancreas’s limited insulin production. The condition is characterized by the destruction of the cells that make […]
- Diabetes Mellitus: Pathophysiologic Processes The main function of insulin produced by cells within the pancreas in response to food intake is to lower blood sugar levels by the facilitation of glucose uptake in the cells of the liver, fat, […]
- Type 2 Diabetes Management in Gulf Countries One such study is the systematic review on the quality of type 2 diabetes management in the countries of the cooperation council for the Arab states of the Gulf, prepared by Alhyas, McKay, Balasanthiran, and […]
- Patient with Ataxia and Diabetes Mellitus Therefore, the therapist prioritizes using the cushion to the client and persuades the patient to accept the product by discussing the merits of the infinity cushion with a low profile in enabling the customer to […]
- Diabetes Evidence-Based Project: Disseminating Results In this presentation, the involvement of mentors and collaboration with administration and other stakeholders are the preferred steps, and the idea to use social networking and web pages has to be removed.
- The Problem of Diabetes Among African Americans Taking into consideration the results of the research and the information found in the articles, the problem of diabetes among African Americans has to be identified and discussed at different levels.
- Childhood Obesity, Diabetes and Heart Problems Based on the data given in the introduction it can be seen that childhood obesity is a real problem within the country and as such it is believed that through proper education children will be […]
- Hypertension and Antihypertensive Therapy and Type 2 Diabetes Mellitus In particular, Acebutolol impairs the functions of epinephrine and norepinephrine, which are neurotransmitters that mediate the functioning of the heart and the sympathetic nervous system.
- Diabetes: Diagnosis and Treatment The disease is characterized by the pancreas almost not producing its own insulin, which leads to an increase in glucose levels in the blood.
- How to Manage Type 2 Diabetes The article is significant to the current research problem as the researchers concluded that the assessment of metabolic processes in diabetic patients was imperative for adjusting in the management of the condition.
- Type 2 Diabetes Analysis Thus, type 2 diabetes has medical costs, or the difficulties of coping up with the illness, economic ones, which are the financial costs of managing it, and the organizational ones for the healthcare systems.
- Clinical Trial of Diabetes Mellitus On the other hand, type II diabetes mellitus is caused by the failure of the liver and muscle cells to recognize the insulin produced by the pancreatic cells.
- Diabetes: Diagnosis and Related Prevention & Treatment Measures The information presented on the articles offers an insight in the diagnosis of diabetes among various groups of persons and the related preventive and treatment measures. The study identified 3666 cases of initial stages of […]
- Reinforcing Nutrition in Schools to Reduce Diabetes and Childhood Obesity For example, the 2010 report says that the rates of childhood obesity have peaked greatly compared to the previous decades: “Obesity has doubled in Maryland over the past 20 years, and nearly one-third of youth […]
- The Connection Between Diabetes and Consuming Red Meat In light of reporting the findings of this research, the Times Healthland gave a detailed report on the various aspects of this research.
- Synthesizing the Data From Relative Risk Factors of Type 2 Diabetes Speaking of such demographic factors as race, the white population suffers from it in the majority of cases, unlike the rest of the races, the remaining 0.
- Using Exenatide as Treatment of Type 2 Diabetes Mellitus in Adults Kendal et al.analyzed the effects of exenatide as an adjunct to a combination of metformin and sulfonylurea against the combination of the same drugs without the adjunct.
- Enhancing Health Literacy for People With Type 2 Diabetes Two professionals, Andrew Long, a professor in the school of heath care in the University of Leeds, and Tina Gambling, senior lecturer in the school of health care studies from the University of Cardiff, conducted […]
- The Scientific Method of Understanding if Coffee Can Impact Diabetes The hypothesis of the experiment ought to be straightforward and understandable. The control group and the experiment group for the test are then identified.
- Gestational Diabetes Mellitus: Review This is because of the current patterns that show an increase in the prevalence of diabetes in offspring born to mothers with GDM.
- Health Service Management of Diabetes During the task, Fay makes a countless number of short calls and often takes water irrespective of the time of the day or the prevailing weather conditions.
- Necrotizing Fasciitis: Pathophysiology, Role of Diabetes In the event of such an infection, the body becomes desperate to get rid of the intruders. For WBC, zero is given if the count is below 15cells/mm3, one is given if the count lies […]
- The Benefits of Sharing Knowledge About Diabetes With Physicians
- Gestational Diabetes Mellitus – NSW, Australia
- Health and Wellness: Stress, Diabetes and Tobacco Related Problems
- 52-Year-Old Female Patient With Type II Diabetes
- Healthy People Project: Personal Review About Diabetes
- Nursing Diagnosis: Type 1 Diabetes & Hypertension
- Nursing Care For the Patient With Diabetes
- Nursing Care Development Plan for Diabetes and Hypertension
- Coronary Heart Disease Aggravated by Type 2 Diabetes and Age
- Diabetes as the Scourge of the 21st Century: Locating the Solution
- Psychosocial Implications of Diabetes Management
- Gestational Diabetes in a Pregnant Woman
- Diabetes Mellitus: Prominent Metabolic Disorder
- Holistic Approach to Man’s Health: Diabetes Prevention
- Holistic Image in Prevention of Diabetes
- Educational Strategies for Diabetes to Patients
- Diabetes and Obesity in the United Arab Emirates
- Epidemiological Problem: Diabetes in Illinois
- Diabetes as a Chronic Condition
- Managing Diabetes Through Genetic Engineering
- Diabetes, Functions of Insulin, and Preventive Practices
- Treating of Diabetes in Adults
- Counseling and Education Session in Type II Diabetes
- Diabetes II: Reduction in the Incidence
- Community Health Advocacy Project: Diabetes Among Hispanics
- Community Health Advocacy Project: Hispanics With Diabetes
- Hispanics Are More Susceptible to Diabetes That Non-Hispanics
- Rates Diabetes Between Hispanics Males and Females
- Diabetes Mellitus and HFSON Conceptual Framework
- Prince Georges County Community Health Concern: Diabetes
- Fats and Proteins in Relation to Type 2 Diabetes
- Alcohol Interaction With Medication: Type 2 Diabetes
- Diabetes Management and Evidence-Based Practice
- Critical Analysis of Policy for Type 2 Diabetes Mellitus in Australia
- The Treatment and Management of Diabetes
- Obesity and Diabetes: The Enemies Within
- Impact of Diabetes on the United Arab Emirates’ Economy
- Childhood Obesity and Type 2 Diabetes
- Health Nursing and Managing Diabetes
- Diabetes Management: How Lifestyle, Daily Routine Affect Blood Sugar
- Diabetes Management: Diagnostics and Treatment
- Diabetes Mellitus Type 2: The Family Genetic History
- Diabetes Type II: Hormonal Mechanism and Intracellular Effects of Insulin
- Social, Behavioral, and Psychosocial Causes of Diseases: Type 2 Diabetes
- Supportive Intervention in the Control of Diabetes Mellitus
- Enhancing Foot Care Practices in Patients With Diabetes
- Community Health Promotion: The Fight Against Diabetes in a Community Setting
- Diabetes in Australia and Saudi Arabia
- Diabetes: The Advantages and Disadvantages of Point of Care Testing
- Diabetes Mellitus Type 2 or Non-Insulin-Dependent Diabetes Mellitus
- Qualitative Research in Diabetes Management in Elderly Patient
- Diabetes Prevention Measures in the Republic of the Marshall Islands
- Impact of Diabetes on Healthcare
- Gestational Diabetes: American Diabetes Association Publishers
- Gestational Diabetes: Child Bearing Experience
- Diabetes Mellitus Effects on Periodontal Disease
- Diabetes Type II Disease in the Community
- The Relationship of Type 2 Diabetes and Depression
- Glycemic Control in Individuals With Type 2 Diabetes
- The Diagnosis of Diabetes in Older Adults and Adolescents
- Physical Activity in Managing Type-2 Diabetes
- High Risk of Developing Type 1 and Type 2 Diabetes Mellitus
- Children With Type 1 Diabetes in Clinical Practice
- Type 2 Diabetes Treatment Analysis
- Type 2 Diabetes Mellitus: Revealing the Diagnosis
- The Type 2 Diabetes Prevention: Lifestyle Choices
- Indigenous and Torres Strait Population and Diabetes
- Interpretation of the Diabetes Interview Transcript
- Type 1 Diabetes: Using Glucose Monitoring in Treatment
- Managing Type 2 Diabetes Patients’ Blood Sugar Prior to and After Surgical Procedures
- Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes: Medical Terminology Definition
- Modern Diabetes Treatment Tools
- Diabetes: Encapsulation to Treat a Disease
- Current Dietary for the Treatment of Diabetes
- Diabetes: Discussion of the Disease
- Stranahan on Diabetes Impairs Hippocampal Function
- A Clinical-Based Study of Young Adults Who Have Diabetes
- Panax Ginseng for Diabetes Treatment
- Depression and Diabetes Association in Adults
- Is There Anu Cure For Diabetes?
- Diabetes Self-Management: Evidence-Based Nursing
- Diabetes Type 2 in Children: Causes and Effects
- Type 1 Diabetes Mellitus Case
- Health, Culture, and Identity as Diabetes Treatment Factors
- Diabetes Prevention in Chinese Elderly in Hunan
- “Experiences of Patients With Type 2 Diabetes Starting Insulin Therapy” by Phillips
- Type 2 Diabetes: Nursing Change Project
- Diabetes and Health Promotion Concepts
- Type 2 Diabetes Project Results Dissemination
- Type 2 Diabetes in Geriatric Patients
- Type 2 Diabetes and Geriatric Evidence-Based Care
- Cultural Empowerment. Diabetes in Afro-Americans
- Diabetes Self-Management: Relationships & Expectations
- Diagnosis and Classification of Diabetes Mellitus
- Improving Comprehensive Care for Patients With Diabetes
- Diabetes Impact on Cardiovascular and Nervous Systems
- Side Effects of Metformin in Diabetes Treatment
- Type 2 Diabetes and Drug Treatments
- Diabetes Mellitus and Health Determinants
- Nursing Leadership in Diabetes Management
- Diabetes Education for African American Women
- Latent Autoimmune Adult Diabetes
- Obesity: Epidemiology and Health Consequences
- Diabetes in Urban Cities of United States
- Diabetes in Australia: Analysis
- Type 2 Diabetes in the Afro-American Bronx Community
- Type 2 Diabetes From Cultural and Genetic Aspects
- Type 2 Diabetes in Bronx: Evidence-Based Practice
- Type 2 Diabetes in Bronx Project for Social Change
- Cardiovascular Care in Type 2 Diabetes Patients
- Ambition Diabetes and Diet on Macbeths’ Example
- Diabetes as Community Health Issue in the Bronx
- Diabetes Management Plan: Diagnosis and Development
- Diabetes Treatment and Care
- Transition from Pediatric to Adult Diabetes Care
- Diabetes Awareness Program and Strategic Planning
- Diabetes: Disease Control and Investigation
- Diabetes Pain Questionnaire and Patient Feedback
- Perception of Diabetes in the Hispanic Population
- Clinical Studies of Diabetes Mellitus
- Diabetes Mellitus and Problems at Work
- Diabetes in the US: Cost Effectiveness Analysis
- Diabetes Investigation in Space Flight Research
- Diabetes Care Advice by Food and Drug Administration
- Artificial Intelligence for Diabetes: Project Experiences
- Diabetes Patients’ Long-Term Care and Life Quality
- Chronic Care Model for Diabetes Patients in the UAE
- Diabetes Among British Adults and Children
- Endocrine Disorders: Diabetes and Fibromyalgia
- Future Technologies: Diabetes Treatment and Care
- Epidemiology of Type 1 Diabetes
- Diabetes: Treatment Technology and Billing
- Pathophysiology of Mellitus and Insipidus Diabetes
- Cure for Diabetes: The Impossible Takes a Little Longer
- Stem Cell Therapy as a Potential Cure for Diabetes
- Stem Cell Therapy and Diabetes Medical Research
- Type II Diabetes Susceptibility and Socioeconomic Status
- Diabetes Mellitus Type 2: Pathophysiology and Treatment
- Obesity and Hypertension in Type 2 Diabetes Patients
- Strongyloides Stercoralis Infection and Type 2 Diabetes
- Socioeconomic Status and Susceptibility to Type II Diabetes
- Diabetes Mellitus: Differential Diagnosis
- Diabetes Disease in the USA Adults
- Education for African Americans With Type 2 Diabetes
- Diabetes Treatment and Funding in Fulton County
- Diabetes Care: Leadership and Strategy Plan
- Diabetes Mellitus’ New Treatment: Principles and Process
- Diet and Nutrition: European Diabetes
- Preventing the Proliferation Diabetes
- Diabetes: Symptoms, Treatment, and Prevention
- Diabetes and Cardiovascular Diseases in Medicine
- Ecological Models to Deal with Diabetes in Medicine
- Different Types of Diabetes Found in Different Countries
- Analysis of Program “Prevent Diabetes Live Life Well”
- The Effect of Physical, Social, and Health Variables on Diabetes
- Micro and Macro-Cosmos in Medicine and Care Models for Prevention of Diabetes
- Why Qualitative Method Was Chosen for Diabetes Program Evaluation
- Humanistic Image of Managing Diabetes
- Diabetes mellitus Education and hemoglobin A1C level
- Obesity, Diabetes and Heart Disease
- Illuminate Diabetes Event Design
- Cause and Diagnosis of Type 2 diabetes
- Patient Voices: Type 2 Diabetes. Podcast Review
- Type I Diabetes: Pathogenesis and Treatment
- Human Body Organ Systems Disorders: Diabetes
- Age Influence on Physical Activity: Exercise and Diabetes
- Hemoglobin A1C Test for Diabetes
- Why Injury and Diabetes Have Been Identified as National Health Priority?
- What Factors Are Involved in the Increasing Prevalence of Type II Diabetes in Adolescents?
- Does the Socioeconomic Position Determine the Incidence of Diabetes?
- What Are the Four Types of Diabetes?
- How Fat and Obesity Cause Diabetes?
- How Exercise Affects Type 2 Diabetes?
- How Does the Treatment With Insulin Affect Type 2 Diabetes?
- How Diabetes Does Cause Depression?
- Does Diabetes Prevention Pay For Itself?
- How Does Snap Participation Affect Rates of Diabetes?
- Does Overeating Sugar Cause Diabetes, Cavities, Acne, Hyperactivity and Make You Fat?
- Why Diabetes Mellitus and How It Affects the United States?
- Does Alcohol Decrease the Risk of Diabetes?
- How Does a Person With Diabetes Feel?
- Does Periodontal Inflammation Affect Type 1 Diabetes in Childhood and Adolescence?
- How Can the Paleolithic Diet Control Type 2 Diabetes?
- How Does Insulin Help Diabetes Be Controlled?
- Does Economic Status Matter for the Regional Variation of Malnutrition-Related Diabetes?
- How Can Artificial Intelligence Technology Be Used to Treat Diabetes?
- What Are the Main Causes and Treatments of Diabetes?
- What Evidence Exists for Treatments Depression With Comorbid Diabetes Using Traditional Chinese Medicine and Natural Products?
- Why Was Qualitative Method Chosen for Diabetes Program Evaluation?
- What Are the Three Types of Diabetes?
- How Does Poverty Affect Diabetes?
- What Is the Leading Cause of Diabetes?
- How Is Diabetes Diagnosed?
- What Are the Main Symptoms of Diabetes?
- How Diabetes Adversely Affects Your Body?
- What Are the Most Common Symptoms of Undiagnosed Diabetes?
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, February 25). 357 Diabetes Essay Topics & Examples. https://ivypanda.com/essays/topic/diabetes-essay-examples/
"357 Diabetes Essay Topics & Examples." IvyPanda , 25 Feb. 2024, ivypanda.com/essays/topic/diabetes-essay-examples/.
IvyPanda . (2024) '357 Diabetes Essay Topics & Examples'. 25 February.
IvyPanda . 2024. "357 Diabetes Essay Topics & Examples." February 25, 2024. https://ivypanda.com/essays/topic/diabetes-essay-examples/.
1. IvyPanda . "357 Diabetes Essay Topics & Examples." February 25, 2024. https://ivypanda.com/essays/topic/diabetes-essay-examples/.
Bibliography
IvyPanda . "357 Diabetes Essay Topics & Examples." February 25, 2024. https://ivypanda.com/essays/topic/diabetes-essay-examples/.
- Epigenetics Essay Titles
- Alcohol Abuse Paper Topics
- Pathogenesis Research Ideas
- Therapeutics Research Ideas
- Hypertension Topics
- Osteoarthritis Ideas
- Cardiomyopathy Titles
- Malnutrition Titles
- Open supplemental data
- Reference Manager
- Simple TEXT file
People also looked at
Original research article, the effect of multimorbidity patterns on physical and cognitive function in diabetes patients: a longitudinal cohort of middle-aged and older adults in china.

- School of Nursing, Department of Geriatric, Zhongnan Hospital of Wuhan University, Wuhan, China
Background: The prevalence of diabetes has increased rapidly, and comorbid chronic conditions are common among diabetes patients. However, little is known about the pattern of multimorbidity in diabetes patients and the effect on physical and cognitive function. This study aimed to assess the disease clusters and patterns of multimorbidity in diabetes patients using a novel latent class analysis (LCA) approach in middle-aged and older adults and explore the association between different clusters of multimorbidity in diabetes and the effect on physical and cognitive function.
Methods: This national observational study included 1,985 diabetes patients from the four waves of the China Health and Retirement Longitudinal Study (CHARLS) in 2011 to 2018. Thirteen chronic diseases were used in latent class analysis to identify the patterns of multimorbidity in diabetes, which span the cardiovascular, physical, psychological, and metabolic systems. Cognitive function is assessed via a structured questionnaire in three domains: memory, executive function, and orientation. We combined activities of daily living (ADL) with instrumental activities of daily living (IADL) to measure physical function. Linear mixed models and negative binomial regression models were used to analyze the association between patterns of multimorbidity in diabetes and the effect on cognitive function and disability, respectively.
Results: A sample of 1,985 diabetic patients was identified, of which 1,889 (95.2%) had multimorbidity; their average age was 60.6 years (standard deviation (SD) = 9.5), and 53.1% were women. Three clusters were identified: “cardio-metabolic” ( n = 972, 51.5%), “mental-dyslipidemia-arthritis” ( n = 584, 30.9%), and “multisystem morbidity” ( n = 333, 17.6%). Compared with diabetes alone, the “multisystem morbidity” class had an increased association with global cognitive decline. All patterns of multimorbidity were associated with an increased risk of memory decline and disability; however, the “multisystem morbidity” group also had the strongest association and presented a higher ADL-IADL disability (ratio = 4.22, 95% CI = 2.52, 7.08) and decline in memory Z scores ( β = −0.322, 95% CI = −0.550, −0.095, p = 0.0058).
Conclusion: Significant longitudinal associations between different patterns of multimorbidity in diabetes patients and memory decline and disability were observed in this study. Future studies are needed to understand the underlying mechanisms and common risk factors for multimorbidity in diabetes patients and to propose treatments that are more effective.
Introduction
Diabetes is one of the major challenges for healthcare systems worldwide. In 2021, approximately 537 million adults were found to live with diabetes worldwide and 6.7 million people died from diabetes ( International Diabetes Federation, 2021 ). According to previous research, approximately 97.5% of adults with diabetes have at least one chronic condition, and as many as 88.5% have two or more concurrent chronic conditions. Multimorbidity is defined as the co-occurrence of at least two chronic conditions in the same individual ( Xu et al., 2017 ; Skou et al., 2022 ), including hypertension and coronary heart disease, as well as diseases affecting the mental system, the nervous system, chronic kidney disease, and chronic lung disease. Having a multimorbidity further increases the complexity of treatment for diabetes patients and is associated with reduced quality of life, impaired functional status, and increased burden on limited healthcare resources ( Glynn et al., 2011 ; Marcel, 2013 ; Fu et al., 2022 ).
Compared with non-diabetic patients, diabetes patients are more likely to develop multiple conditions ( Piette and Kerr, 2006 ). This greater risk reflects the fundamental impact of extended exposure to elevated glucose and insulin resistance on multiple organ systems. Evidence suggests that multimorbidity is likely to impair physical and mental health outcomes ( Chen et al., 2011 ; Koyanagi et al., 2018 ; Makovski et al., 2019 ; Pati et al., 2020 ). A US cross-sectional study showed that patients with comorbid depression and diabetes are at an increased risk for activities of daily living (ADL) disability compared to those with either depression or diabetes alone ( Egede, 2004 ). A 40-month cohort study found that depression was associated with accelerated cognitive decline in diabetes patients in comparison to non-depressed patients with diabetes ( Sullivan et al., 2013 ). However, these studies have focused on single specific comorbidities (such as depression), rather than patterns of comorbidities. A prospective study found that varying clusters of comorbidities led to different results than some specific disease groups ( Aarts et al., 2011 ). Previous studies examining patterns of multimorbidity in diabetes patients have focused on a count of numbers of conditions related to diabetes and independent conditions ( Halanych et al., 2007 ; Kerr et al., 2007 ; An et al., 2019 ). These findings suggested that the single-disease orientation of diabetes management programs and guidelines is unlikely to address the healthcare needs of patients with diabetes. A systematic review on the effectiveness of interventions for the management of multimorbidity concluded that interventions targeted at specific risk factors or at specific problems, such as with functional ability or the management of medicines, are more likely to be effective ( Smith et al., 2012 ). Therefore, it is important to recognize patterns of multimorbidity in diabetes, along with how they associate with health outcomes.
Using data of the China Health and Retirement Longitudinal Study (CHARLS), including middle-aged participants and older adults, we explored the disease clusters and patterns of multimorbidity in diabetes patients. In particular, the present study aimed (a) to test whether multimorbidity in diabetes patients increases the risk of disability and (b) to determine whether specific cognitive domains are differentially affected by multimorbidity in diabetes patients.
The China Health and Retirement Longitudinal Study (CHARLS) is an ongoing nationally representative survey that investigates the social, economic, and health statuses of middle-aged and older people aged 45 years and above in China ( Zhao et al., 2014 ). The baseline survey was conducted in 2011 with 17,708 participants and is followed-up every 2 years. Four follow-up visits are available: 2011 (wave 1), 2013 (wave 2), 2015 (wave 3), and 2018 (wave 4). The CHARLS datasets can be downloaded at the CHARLS home page at http://charls.pku.edu.cn/en . The CHARLS survey project was approved by the Biomedical Ethics Committee of Peking University, and all participants were required to sign informed consent.
Of the 17,707 participants surveyed in 2011 and 2012, 2,336 (13.2%) participants with diabetes were included. A total of 351 participants with missing data about chronic diseases were excluded. For the cognitive function study, we excluded 1,197 participants based on the following criteria: (1) failure to complete the cognitive function examination at baseline; (2) presence of health problems affecting cognitive function, including brain damage, vision problem, hearing problem, speech problem, and memory-related diseases; (3) presence of mild cognitive impairment (MCI) at baseline; and (4) absence of follow-up cognitive function scores. The final sample included 788 participants with baseline data and at least one reassessment of cognitive function (wave 1 to wave 4). For the physical function study, participants with a disability at baseline or those who could not complete functionality questionnaires at the 2011 and 2018 waves were excluded. The final sample included 895 participants. The detailed flow chart of participant selection is shown in Figure 1 .
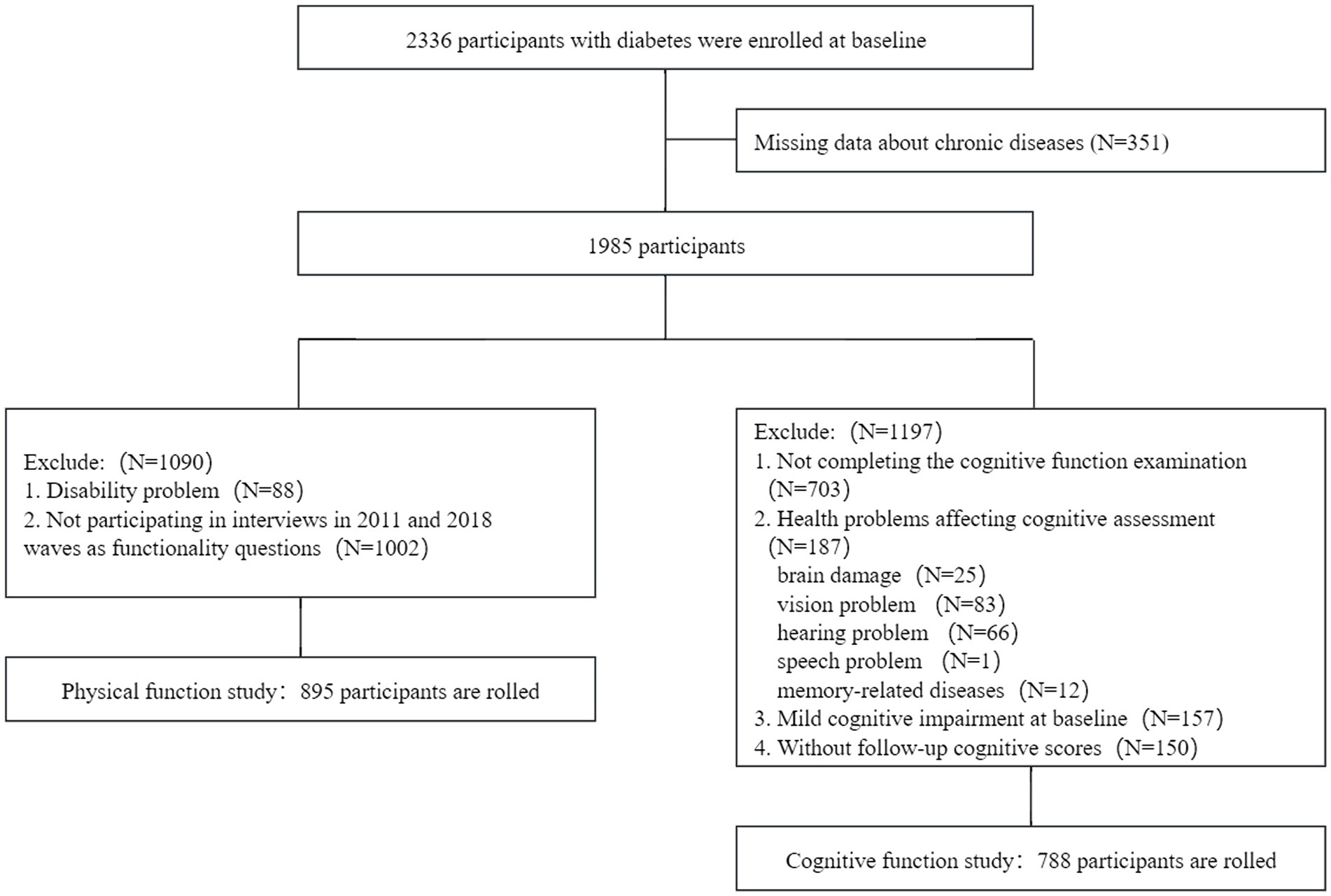
Figure 1 . Flowchart of participant selection for the present study.
Chronic diseases and multimorbidity
Thirteen chronic diseases were modeled in this study, namely, hypertension, dyslipidemia, cancer, chronic lung disease, liver disease, heart disease, stroke, kidney disease, stomach or other digestive disease, psychiatric problems, arthritis, asthma, and depressive symptoms. Each participant’s disease status (yes or no) for a total of 13 non-communicable chronic diseases was confirmed by the patient’s self-report of a physician’s diagnosis “Have you been diagnosed with [conditions listed below, read one by one] by a doctor?” or in combination with medication data “Are you now taking any of the following treatments to treat […] or its complications (Check all that apply)? Taking Chinese traditional medicine, taking Western modern medicine, or other treatments?” in the 2011 CHARLS survey.
Diabetes is defined as fasting plasma glucose ≥126 mg/dL or HbA1c ≥ 6.5%, or current use of any treatment to control blood sugar, or any self-reported history of physician-diagnosed diabetes ( American Diabetes Association Professional Practice Committee, 2021 ). Hypertension is defined as mean systolic blood pressure of ≥140 mmHg or mean diastolic blood pressure of ≥90 mmHg, or current use of antihypertensive drugs, or any self-reported history of physician-diagnosed hypertension ( Chobanian et al., 2003 ). Dyslipidemia is defined as TC ≥ 240 mg/dL, or TG ≥ 200 mg/dL, or LDL-C ≥ 160 mg/dL, or HDL-C < 40 mg/dL, or taking any treatment to lower blood lipid levels, or having any self-reported history of physician-diagnosed dyslipidemia ( Zhu et al., 2018 ). Multimorbidity is defined as the co-occurrence of at least two chronic conditions in the same individual.
Depressive symptoms
The Center for Epidemiologic Studies Depressive Scale (CESD-10), a 10-item questionnaire, was used to measure depressive symptoms, which was highly validated for use in the general population ( Chen and Mui, 2014 ). The respondents were asked to rate “how often you felt this way during the past week,” including their depressive behaviors and feelings such as depressive, loneliness, or fear. A four-scale metric was used to rate the CESD-10 answers, with the total score ranging from 0 to 30 points. Previous research studies have confirmed that a cutoff point of 10 is valid in identifying clinically depressive symptoms ( Boey, 1999 ).
Cognitive function
Cognitive function assessments, consisting of three domains, namely, memory, executive function, and orientation, were conducted in waves 1 to 4 in the CHARLS, using questionnaires that were adapted from the Telephone Interview for Cognitive Status ( Fong et al., 2009 ; Ma et al., 2021 ). Memory was evaluated by immediate and delayed recall of 10 unrelated words. One point was given for each word recalled either immediately or delayed (0 to 10 points). The score of memory ranged from 0 to 20 points. Orientation was assessed by asking four questions based on the year, the month, the date of the month, and the day of the week (0 to 4 points). Executive function was evaluated by the Serial Sevens Test (0 to 5 points) and drawing the picture of two overlapping pentagons (0 or 3 points). The higher the cognitive scores, the better the cognitive function.
To evaluate the global cognitive function, Z scores were generated in each cohort, which has been widely accepted ( Dregan et al., 2013 ; Zheng et al., 2018 ; Xie et al., 2019 ). First, the domain Z scores were generated by standardizing to the baseline. Each domain test score was subtracted by the mean and then divided by the standard deviation (SD) of the baseline domain scores. Second, the global Z scores of an individual at each wave were calculated from the mean score of the three domains by re-standardizing to the baseline.
Mild cognitive impairment (MCI) was defined according to aging-associated cognitive decline (AACD), namely, at least 1 standard deviation (SD) below the age standard in three domains, namely, memory, executive function, and orientation ( Richards et al., 1999 ; Hu et al., 2022 ).
Physical function
Participants were asked all ADL/IADL questions and were defined as having a specific ADL/IADL disability if they answered as follows: (1) I have difficulty but can still do it, (2) I have difficulty and need help, or (3) I cannot do it. The ADL index, which includes dressing, bathing, eating, going to bed, and using the toilet or controlling incontinence, represents the count of ADL disabilities for each participant (range 0–6; a higher number indicates higher ADL disability) ( Katz, 1963 ). The IADL index, which includes doing housework, preparing meals, shopping, managing money, or taking medications, represents the count of IADL disabilities for each participant (range 0–5; a higher number indicates higher IADL disability) ( Lawton and Brody, 1969 ). The ADL–IADL index was generated by summing the ADL and IADL index scores (range 0–11), which might capture a greater range of functional disability prevalence and has been previously validated ( Spector and Fleishman, 1998 ; Thomas et al., 1998 ; Liang et al., 2008 ).
Sociodemographic characteristics and health-related factors, which were shown by previous studies to be associated with diabetes and cognitive function, were selected for our analyses. Sociodemographic characteristics included age (years), gender (male or female), education (illiterate, primary school, middle school, high school/vocational high school, and junior college or above), and marital status (married, cohabitating, separated/divorced/ widowed, and never married). Health-related factors included ever smoking (yes or no), ever drinking (yes or no), and body mass index (BMI), which is defined as the weight (kg) divided by the square of height (m). Blood data were also selected, including blood urea nitrogen (BUN), glucose, creatinine, glycated hemoglobin, total cholesterol, HDL-cholesterol, LDL-cholesterol, triacylglycerol, C-reactive protein (CRP), uric acid, and cystatin C.
Statistical analysis
The results are presented as the mean ± SD or the median with the interquartile range (IQR) for continuous variables and numbers (percentage) for categorical variables.
Latent class analysis (LCA) was conducted to identify patterns of multimorbidity in the 1,889 diabetes participants who were defined with a multimorbidity at baseline. Thirteen chronic diseases (hypertension, dyslipidemia, cancer, chronic lung disease, liver disease, heart disease, stroke, kidney disease, stomach or other digestive disease, psychiatric problems, arthritis, asthma, and depressive symptoms) were used as observed indicators. We first tested increasingly complex models, beginning with two classes and ending with five classes. The best-fit model was determined using the Bayesian information criterion (BIC), the Akaike information criterion (AIC), and the Entropy Index ( Seol and Chun, 2022 ). Lower values of BIC and AIC indicate better fit, whereas Entropy Index (0 to 1) represented the precision of the classification degree. The closer the value is to 1, the more accurate the classification is ( Lubke and Muthén, 2007 ). The Lo–Mendell–Rubin likelihood ratio (LMR LR) test confirmed that the number of classified layers was the optimal value. We finally presented clusters ordered by descending prevalence and named each latent class (“cardio-metabolic” class, “mental-dyslipidemia-arthritis” class, and “multisystem morbidity” class) according to the most prevalent diseases ( Bayes-Marin et al., 2020 ).
Missing data in the covariates were handled using multiple imputation by chained equations. The imputation model included all the variables used in the regression models. All analyses were conducted with R, version 4.2.2. LCAs were performed using Mplus.
Linear mixed models were used to evaluate longitudinal associations between different patterns of multimorbidity in diabetes patients and decline in cognitive Z scores. In the two models that we constructed, the intercept was fitted as random effects to account for interindividual differences at the baseline and the change in cognitive function over the follow-up period. The first model included the diabetes–multimorbidity group as the fixed-effect component. The second model was adjusted for age, gender, time (wave 1 to wave 4), education, marital status, ever smoking, ever drinking, BMI, and biomarkers.
Given the overdispersion of the outcome variable, we used negative binomial regression models to investigate the incremental burden of disability associated with patterns of multimorbidity in diabetes patients. The following models were tested: (1) unadjusted, (2) minimally adjusted (age, gender, education, and BMI), and (3) fully adjusted. The dependent variable was the ADL–IADL index. We compared the ADL–IADL indices of each pattern of multimorbidity in diabetes patients only. Exponentiated coefficients, interpreted as the incident rate ratio for patterns of multimorbidity in diabetes patients compared to the diabetes-only group, were estimated for each model.
Sensitivity analyses were conducted to assess the robustness of the result. First, we adjusted for covariates other than CRP. Second, the raw cognitive function score was used for analysis.
Baseline characteristics and sample size
The mean age of the 1,985 participants was 60.6 ± 9.5 years; 53.1% of participants were women. Within the sample, 96 participants (4.8%) were classified as having diabetes only and 1,889 (95.2%) were classified as having multimorbidity. The distribution of baseline covariates is shown in Table 1 . The most notable difference in demographics between the two groups was the higher proportion of men in the diabetes-only group. The mean age and BMI were higher in the multimorbidity group, while the educational level was lower. Nearly 81.6% of adults with diabetes have at least two other chronic conditions, and as many as 56.1% have three or more concurrent chronic conditions. The most common chronic diseases in patients with diabetes were dyslipidemia (59.4%), hypertension (54.8%), and depressive symptoms (49.8%).
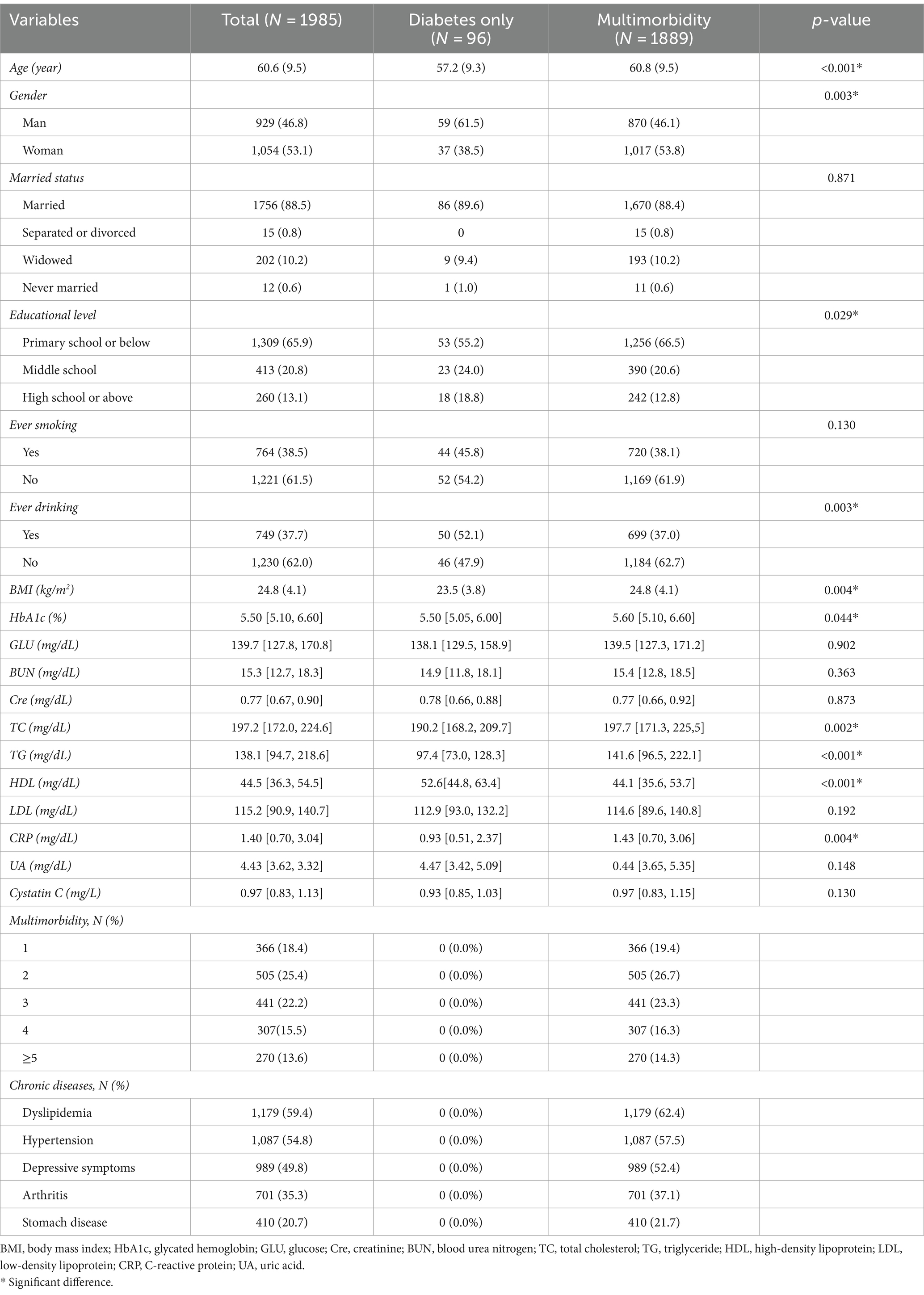
Table 1 . Characteristics of the study participants at baseline (wave 1).
Multimorbidity patterns
Table 2 displays the BIC, AIC, LMR, entropy values, and proportions of each latent class for a two-class to five-class model. The model finally selected was the three-class model. We presented clusters ordered by descending prevalence and named each latent class according to the most prevalent diseases within each latent class. As shown in Figure 2 , class 1 presented excess prevalence of hypertension and dyslipidemia, comprising 51.5% of the total sample, which we named the “cardio-metabolic” class. Class 2 comprised 30.9% of each sample and showed high prevalence of depressive symptoms, dyslipidemia, and arthritis, which we named the “mental-dyslipidemia-arthritis” class. Finally, class 3 presented a higher prevalence of hypertension, dyslipidemia, arthritis, depressive symptoms, and function damage of various organs (chronic lung diseases, heart disease, and stomach or other digestive disease), comprising 17.6% of the sample, which we named the “multisystem morbidity” class.
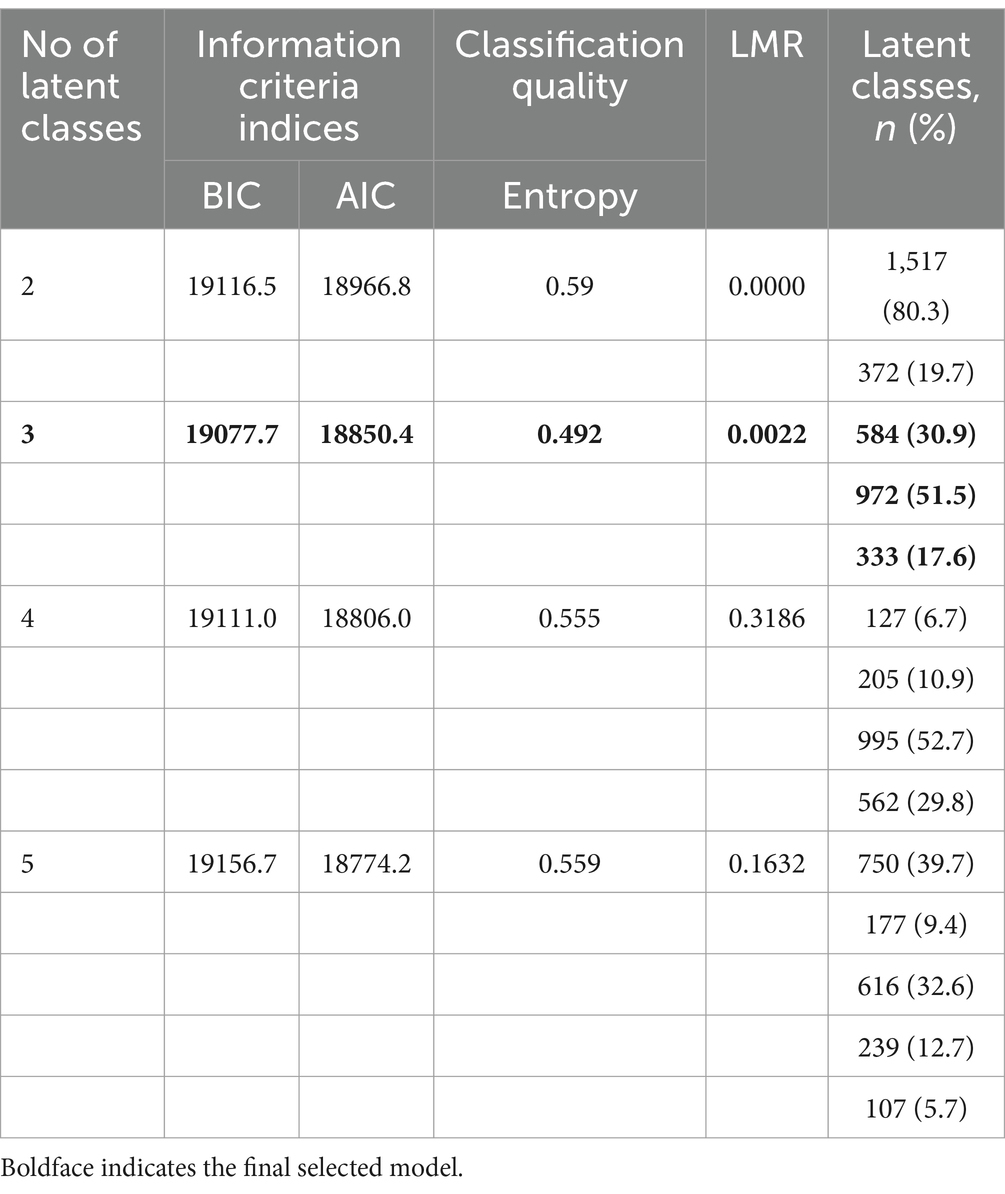
Table 2 . Latent class model fit comparison ( n = 1889).
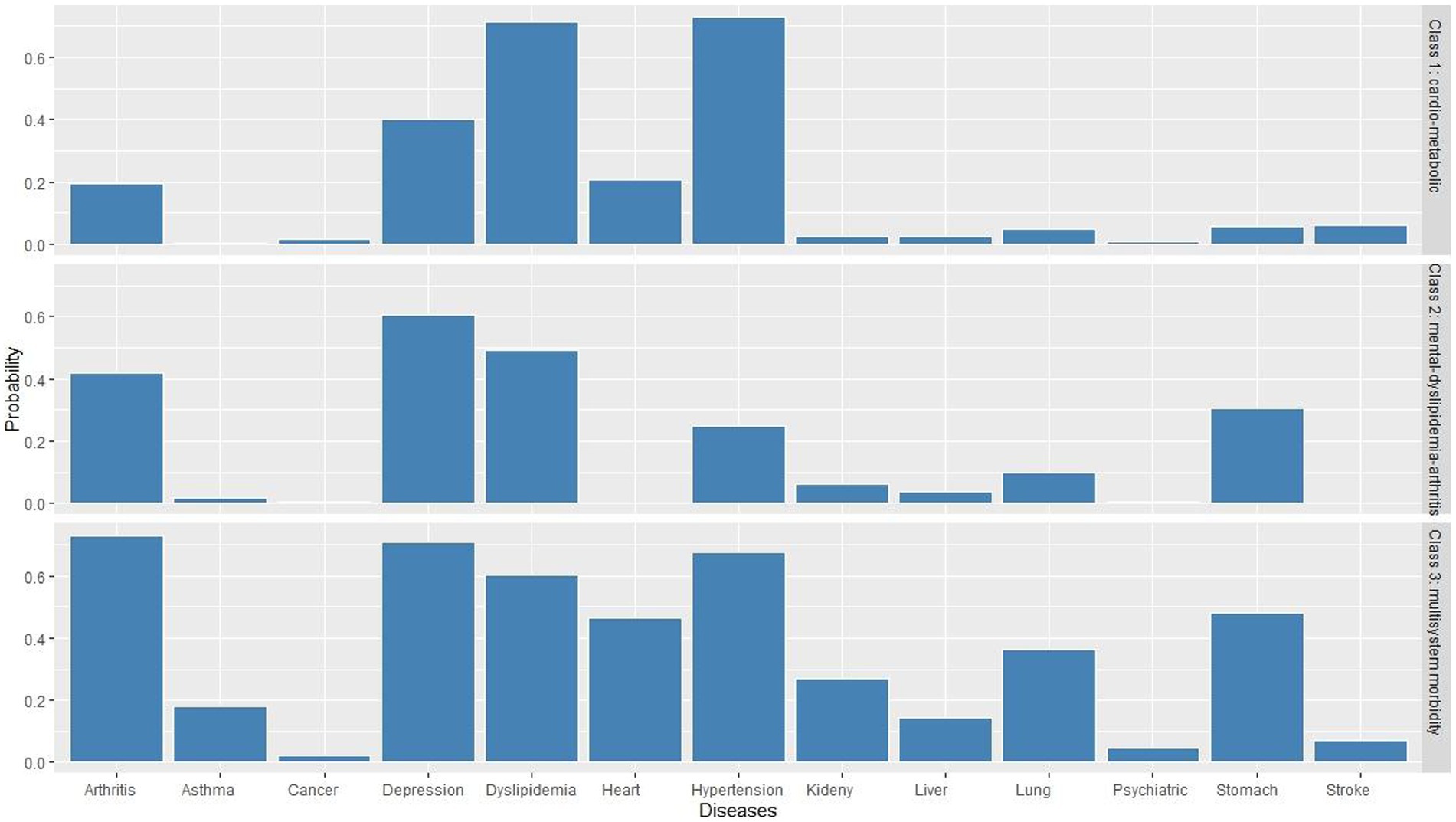
Figure 2 . Three-class model of multimorbidity patterns in diabetes patients.
In the “cardio-metabolic” class, the incidence of hypertension was as high as 73.1%, and the incidence of dyslipidemia was as high as 71.2%. In the “mental-dyslipidemia- arthritis” class, depression (60.4%), dyslipidemia (49.3%), and arthritis (42.0%) had the highest incidence. In the “multisystem morbidity” class, arthritis (72.7%), depression (70.9%), hypertension (67.5), dyslipidemia (60.1%), digestive diseases (48.1%), heart disease (46.5%), and chronic lung diseases (36.4%) had the highest incidence.
Association between multimorbidity patterns and cognitive function
Figure 3 shows the longitudinal associations between different patterns of multimorbidity in diabetes patients and decline in cognitive Z scores. In unadjusted model 1, none of the cognitive domain Z scores were significantly associated with baseline patterns of multimorbidity in diabetes patients, while the “multisystem morbidity” class had a marginally significant association with decline in global cognitive Z scores ( β = −0.169, 95% CI = −0.326, −0.012, p = 0.0483). In fully adjusted model 2, the “cardio-metabolic” ( β = −0.233, 95% CI = −0.431, −0.035, p = 0.0220), “mental-dyslipidemia-arthritis” ( β = −0.249, 95% CI = −0.451, −0.047, p = 0.0162), and “multisystem morbidity” ( β = −0.322, 95% CI = −0.550, −0.095, p = 0.0058) patterns were significantly associated with decline in memory Z scores. In addition, there was a slight increase in association between “multisystem morbidity” class and decline in global cognitive Z scores ( β = −0.160, 95%CI = −0.316, −0.004, p = 0.0464). We found consistent results in sensitivity analyses (as shown in Supplementary material ).
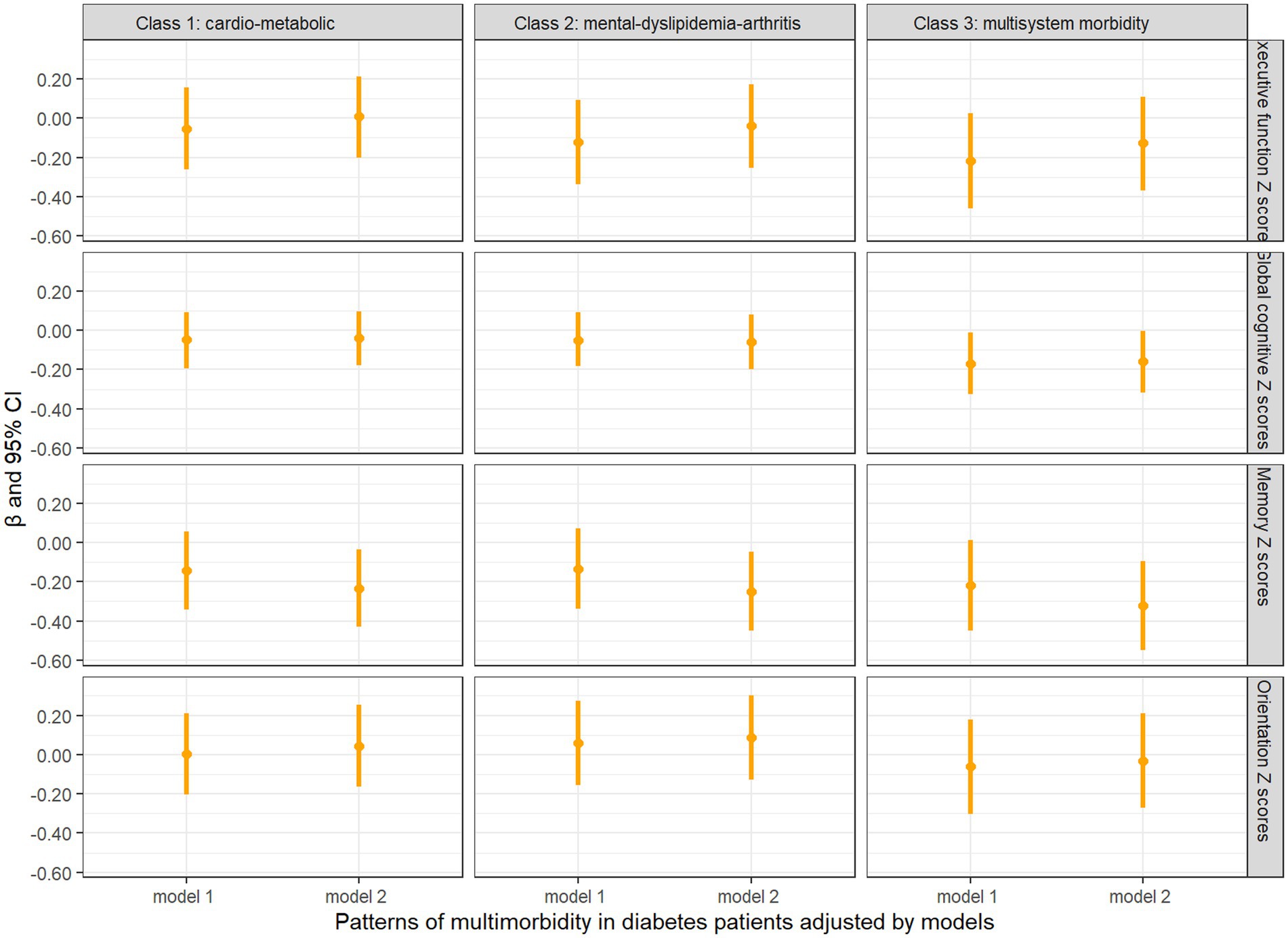
Figure 3 . Longitudinal analysis of cognitive z scores comparing baseline diabetes only with multimorbidity patterns in diabetes patients. Model 1: unadjusted covariates. Model 2: adjusted covariates for age, gender, education, marital status, time, smoking, drinking, BMI, BUN, Glu, Cre, HbA1c, TC, HDL, LDL, TG, CRP, UA, and cystatin C.
Association between multimorbidity patterns and physical function
Figure 4 presents comparisons between the ADL–IADL indices of different multimorbidity patterns in diabetes patients and those with diabetes only. All the patterns of multimorbidity in diabetes patients had an association with disability in the unadjusted model and the partially adjusted model that controlled for age, sex, education, and BMI. In fully adjusted models, it was indicated that the “cardio-metabolic” (ratio = 2.88, 95% CI = 1.72, 4.82), “mental-dyslipidemia-arthritis” (ratio = 3.29, 95% CI = 1.97, 5.50), and “multisystem morbidity” (ratio = 4.22, 95% CI = 2.52, 7.08) patterns were still associated with significantly higher ADL–IADL disability compared with patients with diabetes only, and the “multisystem morbidity” class had the highest prospective ADL–IADL index.
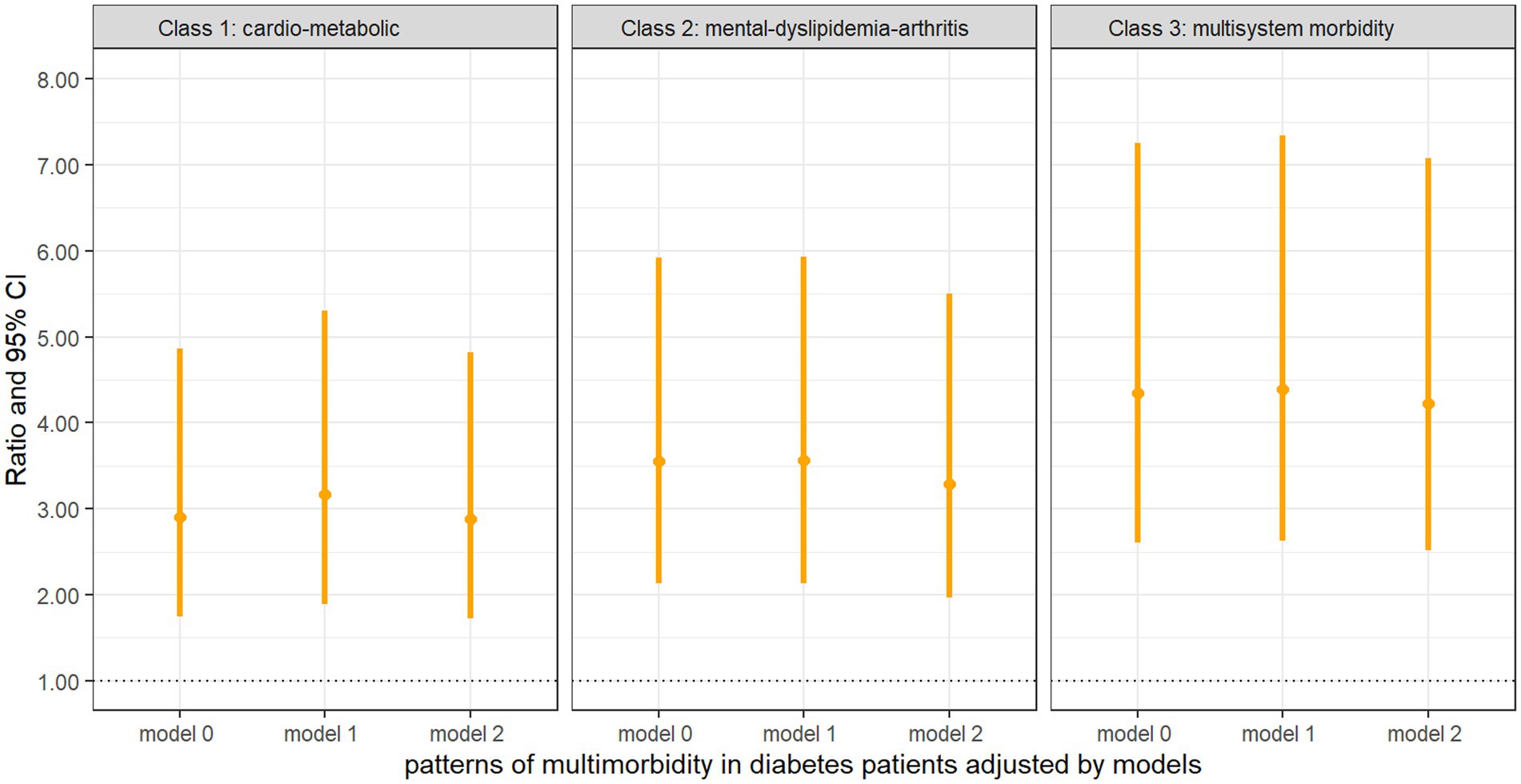
Figure 4 . Negative binomial regression of the ADL–IADL index on multimorbidity patterns with diabetes compared with diabetes only Model 0: unadjusted covariates. Model 1: adjusted covariates for age, gender, education, and BMI. Model 2: Model 1 + marital status, smoking, drinking, BUN, Glu, Cre, HbA1c, TC, HDL, LDL, TG, CRP, UA, and cystatin C.
Using a large national data set from China, we found the prevalence of multimorbidity in diabetes patients to be 95% and more than half of the adults with diabetes having at least three concurrent chronic conditions. The most observed comorbidities were hypertension, dyslipidemia, and depressive symptoms. We identified three clusters using LCA based on the presence of 13 chronic diseases: the “cardio-metabolic,” “mental-dyslipidemia-arthritis,” and the “multisystem morbidity.” These findings suggested an association between clusters of multimorbidity that span several cardiovascular, physical, psychological, and metabolic systems and memory decline and disability in middle-aged and older adults with diabetes. The difference in populations, definitions, and patterns of multimorbidity makes it difficult to compare the result of the present study. Using a similar definition of multimorbidity, a previous study in the United States found the prevalence of multimorbidity in diabetes patients to be 92% ( Kerr et al., 2007 ), which is similar to the present findings. We also found the prevalence of multimorbidity in diabetes patients to be slightly higher in women than in men, which is consistent with a previous finding ( Bing et al., 2023 ). A potential explanation for the higher prevalence in women is the structural placement of women in society ( Arber and Cooper, 1999 ).
A systematic review of 12 studies on multimorbidity among patients with diabetes found similarities for three types of condition clusters, namely, cardiometabolic precursor conditions, vascular conditions, and mental health conditions ( Cicek et al., 2021 ). In contrast, the present study found three main clusters: the first containing hypertension and dyslipidemia, with a higher prevalence; the second dominated by depressive symptoms, dyslipidemia and arthritis; the third consisting of functional impairment of organs, in addition to hypertension, dyslipidemia, depressive symptoms, and arthritis, with a lower prevalence. The cluster of mental health, arthritis, and dyslipidemia had not been observed in previous studies. There are several possible explanations. First, individuals with diabetes reported higher levels of depressive symptoms ( Anderson et al., 2001 ). The risks of comorbid arthritis were significantly higher in the presence of concomitant depressive symptoms, among both diabetic and non-diabetic individuals ( Black, 1999 ). Second, arthritis leads to limited joint movement, impaired mobility ( Rodriguez et al., 2022 ), loss of control over the original life, and being prone to depressive symptoms ( Mammen and Faulkner, 2013 ; Schuch et al., 2018 ). Third, arthritis is a chronic inflammation, and some inflammatory factors may be involved in the body’s normal lipid metabolism. The tumor necrosis factor (TNF) increases the fat decomposition, resulting in the increase of the level of the cyclic free fatty acid, which stimulates the production of triglycerides of the liver, which causes TNF-induced hyperlipemia ( Feingold et al., 1992 ).
When we examined the association of multimorbidity patterns in diabetes patients with cognitive function, we found a “multisystem morbidity” class that consists of several chronic conditions, particularly depressive symptoms, is associated with declines in global cognitive function, which aligns with previous results ( de Araujo et al., 2022 ). In addition, we found that all patterns of multimorbidity in diabetes patients were associated with memory decline. Similar to this result, a longitudinal cohort study in the United Kingdom showed that individuals with certain combinations of health conditions are more likely to have lower levels of memory compared to those with no multimorbidity, and their memory scores tend to differ between combinations ( Bendayan et al., 2021 ). Several mechanisms may explain the link between multimorbidity in diabetes patients and impaired memory. First, multimorbidity can affect the ability of diabetes patients to engage in self-management activities, resulting in suboptimal diabetes control, which in turn can impact memory function ( Ryan et al., 2006 ; Kielstein, 2013 ). Second, diabetes patients often experience vascular changes, such as arteriosclerosis, that can affect blood flow to the brain. These changes in blood supply can lead to alterations in brain structure and function, ultimately affecting memory ( Cukierman et al., 2005 ; Biessels and Reijmer, 2014 ). Third, inflammatory mediators associated with multimorbidity can progressively affect both microvascular and macrovascular structures, leading to structural changes that impair the ability to retain long-term memory. Finally, the presence of multiple comorbidities can have a negative impact on the patient’s mental well-being, including increased levels of anxiety and depression, which can interfere with cognitive processes, including memory function.
With regard to physical function, we found that multimorbidity was significantly associated with an increased risk of disability, which was consistent with previous research studies ( Quiñones et al., 2016 , 2018 ; Wei et al., 2018 ; Pengpid et al., 2022 ). We also found that the “cardio-metabolic” and “multisystem morbidity” classes were associated with a higher risk of disability, which is consistent with previous studies showing a positive association of metabolic multimorbidity with a higher risk of disability ( Zhao et al., 2021 ). Additionally, the present study included patients with diabetes, whereas most included all patients with multimorbidity. A similar cohort study was conducted among US participants, though the magnitude of this association differed from this study (i.e., exponential coefficients ranging from 3.99 to 18.15, in comparison to our 2.88 to 4.22) ( Quiñones et al., 2019 ). However, our findings do correspond with evidence found in Mexican older adults ( McClellan et al., 2021 ). We speculate that the difference might be interpreted by the following reasons. First, multimorbidity with diabetes is classified in different ways, one is a specific comorbidity, and the other is an overall disease group. Second, there are differences in demographic characteristics, socioeconomic status, and lifestyle factors. Previous studies have shown that age, sex, material status, income, education, smoking, and alcohol consumption are associated with morbidity and disability ( Jindai et al., 2016 ; Berlinski et al., 2021 ).

Strengths and limitations
To our knowledge, this is the first study using data from a nationally representative sample among Chinese middle-aged and older adults to identify patterns of multimorbidity in diabetes by a list of 13 chronic conditions and to explore the effect on physical and cognitive function. However, some limitations need to be acknowledged. First, our study could not capture all of chronic conditions, and different chronic diseases may generate different numbers of clusters and constituents within the clusters. Future studies should use datasets that cover various chronic conditions to better explain the multimorbidity patterns in diabetes patients. Second, these chronic diseases were diagnosed based on self-reported information, which may be under- or over-reported, and can thus be subject to measurement errors or lack of accuracy. Third, although we have adjusted some potential confounders based on previous research studies, some extra confounders were not considered, such as physical activity. Fourth, our study did not take into account the effect of self-management level, which results in suboptimal diabetes control on cognitive function and physical function in diabetes patients. Finally, the assessment of cognitive function used in the present study may not be the most commonly used approach, although the items in CHARLS similar to those used in the US Health and Retirement Study.
Our findings indicated that most patients with diabetes have a multimorbidity, and multimorbidity patterns were associated with increased risk of memory decline and disability. These findings suggest health practitioners should pay special attention to early detection of physical and mental health among middle-aged and older adults with diabetes. Moreover, advocating for public awareness of the potentially increased risk of memory decline and disability among diabetes patients with multimorbidity is necessary as a preventive approach for their physical and mental health.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found at: http://charls.pku.edu.cn/en .
Ethics statement
The studies involving humans were approved by the Biomedical Ethics Committee of Peking University. The studies were conducted in accordance with the local legislation and institutional requirements. The human samples used in this study were acquired from China Health and Retirement Longitudinal Study (CHARLS) is an ongoing nationally representative survey to investigate the social, economic and health status of middle-aged and elderly people aged 45 years and above in China. All participants were required to sign informed consent.
Author contributions
XZ: Data curation, Formal analysis, Software, Writing – original draft, Writing – review & editing. JQ: Conceptualization, Data curation, Methodology, Writing – review & editing, Writing – original draft. HL: Data curation, Investigation, Writing – original draft. JC: Investigation, Writing – original draft. QZ: Supervision, Writing – review & editing. XY: Supervision, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to thank the China Health and Retirement Longitudinal Study participants and researchers for their contributions to this important study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnagi.2024.1388656/full#supplementary-material
Abbreviations
LCA, Latent class analysis; MCI, Mild cognitive impairment; BMI, Body mass index; HbA1c, Glycated hemoglobin; GLU, Glucose; Cre, Creatinine; BUN, Blood urea nitrogen; TC, Total cholesterol; TG, Triglyceride; HDL, High-density lipoprotein; LDL, Low-density lipoprotein; CRP, C-reactive protein; UA, Uric acid.
Aarts, S., van den Akker, M., Tan, F. E. S., Verhey, F. R. J., Metsemakers, J. F. M., and van Boxtel, M. P. J. (2011). Influence of multimorbidity on cognition in a normal aging population: a 12-year follow-up in the Maastricht aging study. Int. J. Geriatr. Psychiatry 26, 1046–1053. doi: 10.1002/gps.2642
PubMed Abstract | Crossref Full Text | Google Scholar
American Diabetes Association Professional Practice Committee (2021). 2. Classification and diagnosis of diabetes: standards of medical Care in Diabetes—2022. Diabetes Care 45, S17–S38. doi: 10.2337/dc22-S002
Crossref Full Text | Google Scholar
An, J., Le, Q. A., and Dang, T. (2019). Association between different types of comorbidity and disease burden in patients with diabetes. J. Diabetes 11, 65–74. doi: 10.1111/1753-0407.12818
Anderson, R. J., Freedland, K. E., Clouse, R. E., and Lustman, P. J. (2001). The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care 24, 1069–1078. doi: 10.2337/diacare.24.6.1069
Arber, S., and Cooper, H. (1999). Gender differences in health in later life: the new paradox? Soc. Sci. Med. 48, 61–76. doi: 10.1016/s0277-9536(98)00289-5
Bayes-Marin, I., Sanchez-Niubo, A., Egea-Cortés, L., Nguyen, H., Prina, M., Fernández, D., et al. (2020). Multimorbidity patterns in low-middle and high income regions: a multiregion latent class analysis using ATHLOS harmonised cohorts. BMJ Open 10:e034441. doi: 10.1136/bmjopen-2019-034441
Bendayan, R., Zhu, Y., Federman, A. D., and Dobson, R. J. B. (2021). Multimorbidity patterns and memory trajectories in older adults: evidence from the English longitudinal study of aging. J. Gerontol. Ser. A Biol. Med. Sci. 76, 867–875. doi: 10.1093/gerona/glab009
Berlinski, S., Duryea, S., and Perez-Vincent, S. M. (2021). Prevalence and correlates of disability in Latin America and the Caribbean: evidence from 8 national censuses. PLoS One 16:e0258825. doi: 10.1371/journal.pone.0258825
Biessels, G. J., and Reijmer, Y. D. (2014). Brain changes underlying cognitive dysfunction in diabetes: what can we learn from MRI? Diabetes 63, 2244–2252. doi: 10.2337/db14-0348
Bing, Y., Yuan, L., Liu, J., Wang, Z., Chen, L., Sun, J., et al. (2023). Cluster analysis for the overall health status of elderly, multimorbid patients with diabetes. Front. Public Health 11:1031457. doi: 10.3389/fpubh.2023.1031457
Black, S. A. (1999). Increased health burden associated with comorbid depression in older diabetic Mexican Americans. Results from the Hispanic established population for the epidemiologic study of the elderly survey. Diabetes Care 22, 56–64. doi: 10.2337/diacare.22.1.56
Boey, K. W. (1999). Cross-validation of a short form of the CES-D in Chinese elderly. Int. J. Geriatr. Psychiatry 14, 608–617. doi: 10.1002/(SICI)1099-1166(199908)14:8<608::AID-GPS991>3.0.CO;2-Z
Chen, H.-Y., Baumgardner, D. J., and Rice, J. P. (2011). Health-related quality of life among adults with multiple chronic conditions in the United States, behavioral risk factor surveillance system, 2007. Prev. Chronic Dis. 8:A09.
PubMed Abstract | Google Scholar
Chen, H., and Mui, A. C. (2014). Factorial validity of the Center for Epidemiologic Studies Depression Scale short form in older population in China. Int. Psychogeriatr. 26, 49–57. doi: 10.1017/S1041610213001701
Chobanian, A. V., Bakris, G. L., Black, H. R., Cushman, W. C., Green, L. A., Izzo, J. L., et al. (2003). Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 42, 1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2
Cicek, M., Buckley, J., Pearson-Stuttard, J., and Gregg, E. W. (2021). Characterizing multimorbidity from type 2 diabetes. Endocrinol. Metab. Clin. N. Am. 50, 531–558. doi: 10.1016/j.ecl.2021.05.012
Cukierman, T., Gerstein, H. C., and Williamson, J. D. (2005). Cognitive decline and dementia in diabetes—systematic overview of prospective observational studies. Diabetologia 48, 2460–2469. doi: 10.1007/s00125-005-0023-4
de Araujo, J. A. P., Xavier, É. F. M., Rodrigues, E. D. S., Machado, D. B., Barreto, M. E., Kanaan, R. A., et al. (2022). Main and moderated effects of multimorbidity and depressive symptoms on cognition. Brazilian J. Psychiatry 44, 644–649. doi: 10.47626/1516-4446-2022-2601
Dregan, A., Stewart, R., and Gulliford, M. C. (2013). Cardiovascular risk factors and cognitive decline in adults aged 50 and over: a population-based cohort study. Age Ageing 42, 338–345. doi: 10.1093/ageing/afs166
Egede, L. E. (2004). Diabetes, major depression, and functional disability among U.S. adults. Diabetes Care 27, 421–428. doi: 10.2337/diacare.27.2.421
Feingold, K. R., Doerrler, W., Dinarello, C. A., Fiers, W., and Grunfeld, C. (1992). Stimulation of lipolysis in cultured fat cells by tumor necrosis factor, interleukin-1, and the interferons is blocked by inhibition of prostaglandin synthesis. Endocrinology 130, 10–16. doi: 10.1210/endo.130.1.1370149
Fong, T. G., Fearing, M. A., Jones, R. N., Shi, P., Marcantonio, E. R., Rudolph, J. L., et al. (2009). Telephone interview for cognitive status: creating a crosswalk with the Mini-mental state examination. Alzheimers Dement. 5, 492–497. doi: 10.1016/j.jalz.2009.02.007
Fu, Y., Chen, M., and Si, L. (2022). Multimorbidity and catastrophic health expenditure among patients with diabetes in China: a nationwide population-based study. BMJ Glob. Health 7:e007714. doi: 10.1136/bmjgh-2021-007714
Glynn, L. G., Valderas, J. M., Healy, P., Burke, E., Newell, J., Gillespie, P., et al. (2011). The prevalence of multimorbidity in primary care and its effect on health care utilization and cost. Fam. Pract. 28, 516–523. doi: 10.1093/fampra/cmr013
Halanych, J. H., Safford, M. M., Keys, W. C., Person, S. D., Shikany, J. M., Kim, Y.-I., et al. (2007). Burden of comorbid medical conditions and quality of diabetes care. Diabetes Care 30, 2999–3004. doi: 10.2337/dc06-1836
Hu, Y., Peng, W., Ren, R., Wang, Y., and Wang, G. (2022). Sarcopenia and mild cognitive impairment among elderly adults: the first longitudinal evidence from CHARLS. J. Cachexia. Sarcopenia Muscle 13, 2944–2952. doi: 10.1002/jcsm.13081
International Diabetes Federation (2021). IDF Diabetes Atlas. Available at: http://www.diabetesatlas.org/resources/2021-atlas.html
Google Scholar
Jindai, K., Nielson, C. M., Vorderstrasse, B. A., and Quiñones, A. R. (2016). Multimorbidity and functional limitations among adults 65 or older, NHANES 2005-2012. Prev. Chronic Dis. 13:E151. doi: 10.5888/pcd13.160174
Katz, S. (1963). The index of ADL: a standardized measure of biological and psychosocial function. JAMA 185:914. doi: 10.1001/jama.1963.03060120024016
Kerr, E. A., Heisler, M., Krein, S. L., Kabeto, M., Langa, K. M., Weir, D., et al. (2007). Beyond comorbidity counts: how do comorbidity type and severity influence diabetes patients’ treatment priorities and self-management? J. Gen. Intern. Med. 22, 1635–1640. doi: 10.1007/s11606-007-0313-2
Kielstein, J. T. (2013). Glucose levels and risk of dementia. N. Engl. J. Med. 369, 1863–1864. doi: 10.1056/NEJMc1311765
Koyanagi, A., Lara, E., Stubbs, B., Carvalho, A. F., Oh, H., Stickley, A., et al. (2018). Chronic physical conditions, multimorbidity, and mild cognitive impairment in low- and middle-income countries. J. Am. Geriatr. Soc. 66, 721–727. doi: 10.1111/jgs.15288
Lawton, M. P., and Brody, E. M. (1969). Assessment of older people: self-maintaining and instrumental activities of daily living. The Gerontologist 9, 179–186. doi: 10.1093/geront/9.3_Part_1.179
Liang, J., Bennett, J. M., Shaw, B. A., Quiñones, A. R., Ye, W., Xu, X., et al. (2008). Gender differences in functional status in middle and older age: are there any age variations? J. Gerontol. B Psychol. Sci. Soc. Sci. 63, S282–S292. doi: 10.1093/geronb/63.5.s282
Lubke, G., and Muthén, B. O. (2007). Performance of factor mixture models as a function of model size, covariate effects, and class-specific parameters. Struct. Equ. Model. Multidiscip. J. 14, 26–47. doi: 10.1080/10705510709336735
Ma, Y., Hua, R., Yang, Z., Zhong, B., Yan, L., and Xie, W. (2021). Different hypertension thresholds and cognitive decline: a pooled analysis of three ageing cohorts. BMC Med. 19:287. doi: 10.1186/s12916-021-02165-4
Makovski, T. T., Schmitz, S., Zeegers, M. P., Stranges, S., and Van Den Akker, M. (2019). Multimorbidity and quality of life: systematic literature review and meta-analysis. Ageing Res. Rev. 53:100903. doi: 10.1016/j.arr.2019.04.005
Mammen, G., and Faulkner, G. (2013). Physical activity and the prevention of depression: a systematic review of prospective studies. Am. J. Prev. Med. 45, 649–657. doi: 10.1016/j.amepre.2013.08.001
Marcel, E. S. (2013). Multimorbidity in older adults. Epidemiol. Rev. 35, 75–83. doi: 10.1093/epirev/mxs009
McClellan, S. P., Haque, K., and García-Peña, C. (2021). Diabetes multimorbidity combinations and disability in the Mexican health and aging study, 2012-2015. Arch. Gerontol. Geriatr. 93:104292. doi: 10.1016/j.archger.2020.104292
Pati, S., Pati, S., van den Akker, M., Schellevis, F., Jena, S., and Burgers, J. S. (2020). Impact of comorbidity on health-related quality of life among type 2 diabetic patients in primary care. Prim. Health Care Res. Dev. 21:e9. doi: 10.1017/S1463423620000055
Pengpid, S., Peltzer, K., and Anantanasuwong, D. (2022). Bidirectional association between functional disability and multimorbidity among middle-aged and older adults in Thailand. Front. Public Health 10:1055699. doi: 10.3389/fpubh.2022.1055699
Piette, J. D., and Kerr, E. A. (2006). The impact of comorbid chronic conditions on diabetes care. Diabetes Care 29, 725–731. doi: 10.2337/diacare.29.03.06.dc05-2078
Quiñones, A. R., Markwardt, S., and Botoseneanu, A. (2016). Multimorbidity combinations and disability in older adults. J. Gerontol. Ser. A Biol. Med. Sci. 71, 823–830. doi: 10.1093/gerona/glw035
Quiñones, A. R., Markwardt, S., and Botoseneanu, A. (2019). Diabetes-multimorbidity combinations and disability among middle-aged and older adults. J. Gen. Intern. Med. 34, 944–951. doi: 10.1007/s11606-019-04896-w
Quiñones, A. R., Markwardt, S., Thielke, S., Rostant, O., Vásquez, E., and Botoseneanu, A. (2018). Prospective disability in different combinations of somatic and mental multimorbidity. J. Gerontol. A Biol. Sci. Med. Sci. 73, 204–210. doi: 10.1093/gerona/glx100
Richards, M., Touchon, J., Ledesert, B., and Richie, K. (1999). Cognitive decline in ageing: are AAMI and AACD distinct entities? Int. J. Geriatr. Psychiatry 14, 534–540. doi: 10.1002/(SICI)1099-1166(199907)14:7<534::AID-GPS963>3.0.CO;2-B
Rodriguez, M. A., Chou, L.-N., Sodhi, J. K., Markides, K. S., Ottenbacher, K. J., and Snih, S. A. (2022). Arthritis, physical function, and disability among older Mexican Americans over 23 years of follow-up. Ethn. Health 27, 1915–1931. doi: 10.1080/13557858.2021.2002271
Ryan, C. M., Freed, M. I., Rood, J. A., Cobitz, A. R., Waterhouse, B. R., and Strachan, M. W. J. (2006). Improving metabolic control leads to better working memory in adults with type 2 diabetes. Diabetes Care 29, 345–351. doi: 10.2337/diacare.29.02.06.dc05-1626
Schuch, F. B., Vancampfort, D., Firth, J., Rosenbaum, S., Ward, P. B., Silva, E. S., et al. (2018). Physical activity and incident depression: a Meta-analysis of prospective cohort studies. Am. J. Psychiatry 175, 631–648. doi: 10.1176/appi.ajp.2018.17111194
Seol, R., and Chun, J.-H. (2022). Classification of type 2 diabetes incidence risk and the health behavior of the 30-50-year-old Korean adults: latent class analysis. Int. J. Environ. Res. Public Health 19:16600. doi: 10.3390/ijerph192416600
Skou, S. T., Mair, F. S., Fortin, M., Guthrie, B., Nunes, B. P., Miranda, J. J., et al. (2022). Multimorbidity. Nat. Rev. Dis. Primers 8:48. doi: 10.1038/s41572-022-00376-4
Smith, S. M., Soubhi, H., Fortin, M., Hudon, C., and O’Dowd, T. (2012). Managing patients with multimorbidity: systematic review of interventions in primary care and community settings. BMJ (Clinical Research Ed.) 345:e5205. doi: 10.1136/bmj.e5205
Spector, W. D., and Fleishman, J. A. (1998). Combining activities of daily living with instrumental activities of daily living to measure functional disability. J. Gerontol. B Psychol. Sci. Soc. Sci. 53B, S46–S57. doi: 10.1093/geronb/53b.1.s46
Sullivan, M. D., Katon, W. J., Lovato, L. C., Miller, M. E., Murray, A. M., Horowitz, K. R., et al. (2013). Association of depression with accelerated cognitive decline among patients with type 2 diabetes in the ACCORD-MIND trial. JAMA Psychiatry 70, 1041–1047. doi: 10.1001/jamapsychiatry.2013.1965
Thomas, V. S., Rockwood, K., and McDowell, I. (1998). Multidimensionality in instrumental and basic activities of daily living. J. Clin. Epidemiol. 51, 315–321. doi: 10.1016/s0895-4356(97)00292-8
Wei, M. Y., Kabeto, M. U., Langa, K. M., and Mukamal, K. J. (2018). Multimorbidity and physical and cognitive function: performance of a new multimorbidity-weighted index. J. Gerontol. Ser. A Biol. Med. Sci. 73, 225–232. doi: 10.1093/gerona/glx114
Xie, W., Zheng, F., Yan, L., and Zhong, B. (2019). Cognitive decline before and after incident coronary events. J. Am. Coll. Cardiol. 73, 3041–3050. doi: 10.1016/j.jacc.2019.04.019
Xu, X., Mishra, G. D., and Jones, M. (2017). Evidence on multimorbidity from definition to intervention: An overview of systematic reviews. Ageing Res. Rev. 37, 53–68. doi: 10.1016/j.arr.2017.05.003
Zhao, Y., Hu, Y., Smith, J. P., Strauss, J., and Yang, G. (2014). Cohort profile: the China health and retirement longitudinal study (CHARLS). Int. J. Epidemiol. 43, 61–68. doi: 10.1093/ije/dys203
Zhao, Y., Zhang, P., Lee, J. T., Oldenburg, B., Heusden, A., Haregu, T. N., et al. (2021). The prevalence of metabolic disease multimorbidity and its associations with spending and health outcomes in middle-aged and elderly Chinese adults. Front. Public Health 9:658706. doi: 10.3389/fpubh.2021.658706
Zheng, F., Yan, L., Yang, Z., Zhong, B., and Xie, W. (2018). HbA1c, diabetes and cognitive decline: the English longitudinal study of ageing. Diabetologia 61, 839–848. doi: 10.1007/s00125-017-4541-7
Zhu, J.-R., Gao, R.-L., Zhao, S.-P., Lu, G.-P., Zhao, D., and Li, J.-J. (2018). 2016 Chinese guidelines for the management of dyslipidemia in adults. J. Geriatr. Cardiol. 15, 1–29. doi: 10.11909/j.issn.1671-5411.2018.01.011
Keywords: diabetes, multimorbidity, cognitive function, disability, physical function
Citation: Zhou X, Qin J-J, Li H, Chen J, Zhang Q and Ye X (2024) The effect of multimorbidity patterns on physical and cognitive function in diabetes patients: a longitudinal cohort of middle-aged and older adults in China. Front. Aging Neurosci . 16:1388656. doi: 10.3389/fnagi.2024.1388656
Received: 20 February 2024; Accepted: 22 April 2024; Published: 14 May 2024.
Reviewed by:
Copyright © 2024 Zhou, Qin, Li, Chen, Zhang and Ye. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qing Zhang, [email protected] ; Xujun Ye, [email protected]
† These authors have contributed equally to this work and share first authorship
This article is part of the Research Topic
Mental, Sensory, Physical and Life Style Parameters Related to Cognitive Decline in Aging
- Open access
- Published: 15 May 2024
The association between ultra-processed food and common pregnancy adverse outcomes: a dose-response systematic review and meta-analysis
- Sepide Talebi 1 , 2 ,
- Sanaz Mehrabani 3 ,
- Seyed Mojtaba Ghoreishy 4 , 5 ,
- Alexei Wong 6 ,
- Aliasghar Moghaddam 7 ,
- Peyman Rahimi Feyli 7 ,
- Parsa Amirian 8 ,
- Mahsa Zarpoosh 8 ,
- Mohammad Ali Hojjati Kermani 9 &
- Sajjad Moradi 10
BMC Pregnancy and Childbirth volume 24 , Article number: 369 ( 2024 ) Cite this article
Metrics details
Given the increasing incidence of negative outcomes during pregnancy, our research team conducted a dose-response systematic review and meta-analysis to investigate the relationship between ultra-processed foods (UPFs) consumption and common adverse pregnancy outcomes including gestational diabetes mellitus (GDM), preeclampsia (PE), preterm birth (PTB), low birth weight (LBW), and small for gestational age (SGA) infants. UPFs are described as formulations of food substances often modified by chemical processes and then assembled into ready-to-consume hyper-palatable food and drink products using flavors, colors, emulsifiers, and other cosmetic additives. Examples include savory snacks, reconstituted meat products, frozen meals that have already been made, and soft drinks.
A comprehensive search was performed using the Scopus, PubMed, and Web of Science databases up to December 2023. We pooled relative risk (RR) and 95% confidence intervals (CI) using a random-effects model.
Our analysis (encompassing 54 studies with 552,686 individuals) revealed a significant association between UPFs intake and increased risks of GDM (RR = 1.19; 95% CI: 1.10, 1.27; I 2 = 77.5%; p < 0.001; studies = 44; number of participants = 180,824), PE (RR = 1.28; 95% CI: 1.03, 1.59; I 2 = 80.0%; p = 0.025; studies = 12; number of participants = 54,955), while no significant relationships were found for PTB, LBW and SGA infants. Importantly, a 100 g increment in UPFs intake was related to a 27% increase in GDM risk (RR = 1.27; 95% CI: 1.07, 1.51; I 2 = 81.0%; p = 0.007; studies = 9; number of participants = 39,812). The non-linear dose-response analysis further indicated a positive, non-linear relationship between UPFs intake and GDM risk P nonlinearity = 0.034, P dose-response = 0.034), although no such relationship was observed for PE (P nonlinearity = 0.696, P dose-response = 0.812).
In summary, both prior to and during pregnancy, chronic and excessive intake of UPFs is associated with an increased risk of GDM and PE. However, further observational studies, particularly among diverse ethnic groups with precise UPFs consumption measurement tools, are imperative for a more comprehensive understanding.
Peer Review reports
Introduction
The Centers for Disease Control and Prevention’s (CDC’s) 2022 National Center for Health Statistics report alarmingly indicates a persistent rise in pregnancy-related mortality in the US across three decades, highlighting significant disparities in “race” and maternal age [ 1 ]. This trend underscores the pivotal role of addressing common pregnancy adverse outcomes as a critical component of maternal morbidity and mortality prevention strategies [ 2 ].
Promoting healthy dietary habits during pregnancy is imperative to meet the increased physiological needs of expectant mothers. The phenomenon of “nutritional transition”, characterized by a shift towards high-calorie, low-micronutrient foods, culminates in malnutrition and obesity [ 3 ]. The significance of maternal nutrition in prenatal care is heavily emphasized by researchers as a preventive measure against adverse pregnancy outcomes [ 4 ]. The consumption of diets rich in refined carbohydrates, fats, and sweets is linked to an increased risk of gestational diabetes mellitus (GDM) and preterm birth (PTB) [ 5 ]. Moreover, such dietary patterns adversely affect women’s health by exacerbating hypertensive disorders and contributing to conditions like preeclampsia (PE), low birth weight (LBW), and small-for-gestational-age (SGA) infants [ 6 ]. Recognizing the detrimental impact of these unhealthy dietary patterns, it becomes crucial to consider the role of food processing in the maternal diet.
The NOVA classification, a framework for grouping edible substances, categorizes foods into four groups based on the extent and purpose of food processing applied, ranging from unprocessed or minimally processed foods to ultra-processed foods (UPFs) [ 7 , 8 ]. UPFs are characterized by their high content of additives such as preservatives, artificial flavors, colors, and sweeteners, and are typically devoid of whole or minimally processed ingredients [ 9 ]. The consumption of UPFs has been associated with higher risks of obesity, hypertension, cancer, and other chronic diseases [ 8 , 10 , 11 , 12 ]. These foods are implicated in disrupting insulin signaling, promoting excessive energy intake, weight gain, and increased urinary concentrations of phthalate metabolites, which act as endocrine disruptors [ 13 , 14 ]. In the context of adverse pregnancy outcomes, recent meta-analytic work highlighted a heightened risk of GDM (odds ratio (OR): 1.48; 95% confidence interval (CI): 1.17, 1.87) and PE (OR: 1.28; 95% CI: 1.15, 1.42) among high UPFs consumers, with no significant associations observed in LBW, PTB, and Large for Gestational Age (LGA) [ 15 ]. However, the previous meta-analysis did not encompass a comprehensive set of extant studies for each adverse outcome (as evidenced by the inclusion of only 10 studies for GDM in contrast to the 44 studies incorporated in our current investigation), thereby underscoring the challenge posed by the unutilized data in previous analyses. Additionally, recent studies of relevance have emerged [ 16 , 17 , 18 ] and the preceding meta-analytic work did not include a dose-response analysis [ 15 ]. The integration of dose-response analysis offers benefits such as facilitating the formulation of public health directives, augmenting precision, and quantifying the dose-response relationship. Consequently, we decided to conduct an updated dose-response systematic review and meta-analysis to rigorously evaluate the association between UPFs consumption and common adverse pregnancy outcomes, including GDM, SGA, LBW, PTB, and PE.
This systematic review and meta-analysis was conducted according to the guidelines specified in the 2020 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [ 19 ]. The study protocol was registered with the International Prospective Register of Systematic Reviews Database (PROSPERO) under the registration number CRD42023486135.
Literature search and selection
A systematic literature search was done employing PubMed/MEDLINE, ISI Web of Science and Scopus, with no date restrictions, up to December 6, 2023. The search keywords and strategy are reported in Supplementary Table 1 . Data from grey literature sources such as notes, conference abstracts, reviews, case reports, letters, short surveys, and reports were obtained from a manual search of references mentioned in original research articles published in one of these databases. To augment the breadth of research identified, references within reviews and pertinent studies that met eligibility criteria were further subjected to manual examination.
Inclusion and exclusion criteria
Inclusion criteria were defined as follows: a) observational studies (cohort, case-control, or cross-sectional,) in adult subjects (≥18 years) reporting data on the association between UPFs intake and the risk of adverse pregnancy outcomes (including GDM PE, PTB, LBW, and SGA infants), and reporting effect estimates in the form of hazard ratio (HR), relative risk (RR), or odds ratios (OR), each with at least 95% confidence interval (95% CI). Exclusion criteria included: a) studies done in children and adolescents (< 18 years), b) studies without sufficient data (for instance, those failing to report effect sizes or 95% CIs, instead reporting beta coefficients), and c) those with no relevant exposure. Study titles and abstracts, as well as full-text reviews from database searches meeting the inclusion criteria, were assessed by two reviewers (ST and SM). Any disagreements regarding study inclusion/exclusion criteria were resolved by consensus following discussion. The PICOS tool for each article was reported in Supplementary Table 2 .
Data extraction
Two investigators (FJ and SM) extracted the following data, based on a standardized extraction form, from the studies that met the inclusion criteria: a) first author’s name, year of publication, and country of origin; b) study characteristics (design, follow-up period, and source of data on health status); c) participant characteristics (number of participants/cases, age and sex); d) methods of evaluating UPFs intake; e) the risk of adverse pregnancy outcomes; f) main study results (outcomes), and g) covariates utilized for adjustments in multivariate analyses. Any disagreement regarding data extraction characteristics was decided by consensus following the discussion.
Quality assessment
Applying the Newcastle-Ottawa Scale (NOS) [ 20 ], two investigators assessed the quality of each shortlisted study. The NOS was specifically chosen due to its comprehensive framework designed to evaluate the quality of non-randomized studies. This scale excels in its design, content, and user-friendliness, making it particularly suitable for integrating quality assessments into the interpretation of meta-analytic results. The NOS scale for systematic reviews or meta-analyses, allocating up to 9 points across three domains: study group selection (four points), study group comparability (two points), and exposure and outcomes ascertainment for case-control or cohort studies (three points). Studies scoring 7–9 are deemed high quality/low risk of bias, whereas a score of 0–3 indicates a high risk of bias. Table 1 shows the consensus from this assessment.
Statistical analyses and data synthesis
Statistical analyses were performed applying STATA version 14.0 (StataCorp, College Station, TX, USA) and SPSS version 25.0 (IBM, Armonk, NY, USA). The RR and 95% CI were established as overall effect sizes in this work, similar to effect estimates reported in observational articles meeting the inclusion criteria for this meta-analysis [ 21 ]. The synthesized effect estimates were reported as pooled RR with 95% CI. Due to anticipated heterogeneity between studies, effect estimates were calculated using the DerSimonian-Laird weighted random-effects model [ 22 ]. A pairwise meta-analysis combined the effect size results for the highest and lowest categories of UPFs intake. Heterogeneity among the articles was examined by the Cochran Q and I-squared (I 2 ) statistics, with the I 2 value estimated from [(Q-df)/Q × 100%]; where Q is the χ 2 value and df the corresponding degrees of freedom. Between-study heterogeneity was considered significant when the Cochran Q statistic was significant ( p < 0.05) or if I 2 > 50%; specifically, low, moderate, high, and extreme heterogeneity was defined based on the I 2 statistics cut-offs of < 25%, 25–50%, 50–75%, and >75%, respectively.
Furthermore, subgroup analyses were conducted to evaluate any potential effects due to the study design (cross-sectional, case-control, or cohort), UPFs classification method (NOVA food classification, Western-type diet pattern, fast-food, or sweets consumption), the study region of origin (North America, South America, Asia, Europe, and Australia), pre-pregnancy body mass index (< 25 kg/m 2 and ≥ 25 kg/m 2 ) [ 23 , 24 ], age (< 30 years and ≥ 30 years) [ 24 ], number of cases (< 100 or ≥ 100), number of participants (< 1000 or ≥ 1000), dietary assessment method (food frequency questionnaires [FFQ], 24 h recall, or food records), dietary assessment period (pre-pregnancy, early pregnancy, mid-pregnancy), and other covariate adjustments. Sensitivity analysis was conducted by omitting each study and evaluating the remaining pooled effect estimates. Publication bias was evaluated by visual inspection of funnel plots, and formal testing using Egger’s regression asymmetry and Begg’s rank correlation tests [ 25 , 26 ], with outcomes considered as significant at p < 0.05.
A dose-response meta-analysis was completed to estimate the RRs per 100 g increment in UPFs intake, based on the method introduced by Greenland and colleagues [ 27 , 28 ]. For this process, studies needed to report the number of cases (i.e., participants with incidence) and non-cases (i.e., participants without incidence) or person-years (i.e., the number of people in the study and the duration of their participation) as well as the median point of UPFs intake across more than three categories of intake. Ultimately, a one-stage linear mixed-effects meta-analysis was undertaken to model the dose-response associations, estimating and combining study-specific slope lines to obtain an average slope in a single stage. This linear mixed-effects meta-analysis includes studies with two categories of exposures (at least two effect sizes) in the dose-response analysis.
Quality of evidence
The quality of evidence across articles was ranked employing the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) working group guidelines. The GRADE criteria categorize evidence quality into high, moderate, low, or very low levels [ 29 ].
Study characteristics
Our systematic search and examination of reference lists yielded a total of 3433 records. After omitting duplicates, 2787 articles remained for assessment (Fig. 1 ). A title and abstract review led to the removal of 2707 articles. Subsequent full-text assessment of the 80 remaining studies resulted in the exclusion of a further 26 articles for the following reasons: five articles reported outcomes not relevant to our research scope, six lacked sufficient data, and 15 did not focus on relevant exposure (Supplemental Table 3 ). Consequently, 54 studies met our inclusion criteria and were selected in the present meta-analysis [ 16 , 17 , 18 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 ].
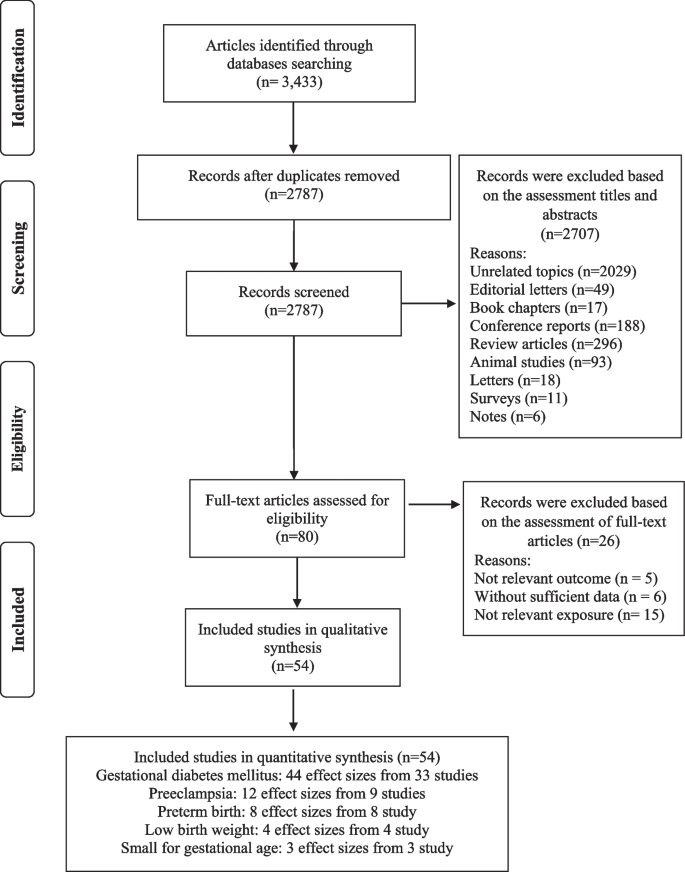
Flow chart of the process of the study selection
The selected studies (detailed in Supplemental Table 4 ) encompass 38 cohort studies [ 16 , 31 , 33 , 34 , 35 , 36 , 37 , 39 , 40 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 51 , 52 , 54 , 55 , 57 , 58 , 59 , 60 , 61 , 62 , 65 , 66 , 67 , 69 , 70 , 71 , 73 , 74 , 75 , 78 ], 11 case-control studies [ 17 , 18 , 30 , 32 , 34 , 50 , 63 , 66 , 68 , 72 , 77 ], and five cross-sectional studies [ 38 , 46 , 64 , 76 , 79 ]. These articles, conducted between 1988 and 2023, originated from different countries including the USA [ 33 , 36 , 53 , 58 , 60 , 62 , 69 , 74 , 78 ], the UK [ 16 ], China [ 43 , 49 , 51 , 71 , 73 ], Brazil [ 31 , 59 , 63 , 64 , 68 , 79 ], Spain [ 39 , 40 , 42 , 55 , 57 ], Iran [ 17 , 18 , 30 , 32 , 48 , 54 , 66 , 76 , 77 ], Malaysia [ 75 ], Palestine [ 72 ], Australia [ 45 , 46 , 65 ], Singapore [ 37 , 38 ], Norway [ 35 , 44 , 47 ], Japan [ 41 , 67 ], Czech Republic [ 34 ], Iceland [ 70 ] and Denmark [ 61 ]. The study-specific, maximally adjusted RR was reported for 552,686 individuals across the included articles and was pooled for meta-analysis to assess the association between UPFs and the risk GDM [ 16 , 32 , 33 , 34 , 36 , 38 , 39 , 40 , 41 , 43 , 48 , 49 , 50 , 51 , 53 , 54 , 55 , 56 , 59 , 60 , 64 , 65 , 66 , 70 , 71 , 72 , 73 , 74 , 75 , 77 , 78 , 79 ], PE [ 17 , 18 , 30 , 35 , 48 , 52 , 62 , 69 , 74 , 76 ], PTB [ 31 , 37 , 44 , 45 , 46 , 48 , 52 , 58 , 61 , 67 ], LBW [ 45 , 63 , 67 ] and SGA infants [ 46 , 67 , 68 ]. The Newcastle-Ottawa grade (used for quality assessment) categorized 27 studies as high quality [ 17 , 33 , 35 , 36 , 37 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 47 , 51 , 53 , 55 , 57 , 58 , 60 , 62 , 65 , 67 , 69 , 74 , 75 , 78 ] and 27 as medium quality [ 16 , 18 , 30 , 31 , 32 , 34 , 38 , 46 , 48 , 49 , 50 , 52 , 54 , 56 , 59 , 61 , 63 , 64 , 66 , 68 , 70 , 71 , 72 , 73 , 76 , 77 , 79 ]. Moreover, the outcomes revealed that the level of agreement between investigators for data collection as well as for quality assessment was appropriate (Kappa = 0.897).
Ultra-processed food and common adverse pregnancy outcomes
Our results suggested a significant relationship between higher UPF intake and an increased risk of GDM (RR = 1.19; 95% CI: 1.10, 1.27; I 2 = 77.5%; p < 0.001; n = 44), PE (RR = 1.28; 95% CI: 1.03, 1.59; I 2 = 80.0%; p = 0.025; n = 12), but not PTB (RR = 1.06; 95% CI: 0.97, 1.17; I 2 = 34.2%; p = 0.231; n = 8), LBW (RR = 1.01; 95% CI: 0.91, 1.12; I 2 = 52.2%; p = 0.905; n = 4) and SGA infants (RR = 1.11; 95% CI: 0.81, 1.52; I 2 = 66.3%; p = 0.532; n = 3), (Refer to Table 1 , Supplementary Fig. 1 ).
In the context of GDM, subgroup analysis showed that a greater UPFs intake was significantly associated with an enhanced risk in cohort studies (vs. cross-sectional) (RR = 1.18; 95% CI: 1.09, 1.27; I 2 = 79.3%; p < 0.001; n = 31) and case-control studies (RR = 2.06; 95% CI: 1.31, 3.35; I 2 = 77.7%; p = 0.002; n = 10), particularly in studies assessed western dietary pattern (RR = 1.34; 95% CI: 1.01, 1.76; I 2 = 43.0%; p = 0.040; n = 7) or fast-foods (RR = 1.32; 95% CI: 1.15, 1.51; I 2 = 79.3%; p < 0.001; n = 22), (vs. NOVA classification or sweets consumption), in North America (vs. Europe, South America, Asia and Australia) (RR = 1.43; 95% CI: 1.27, 1.53; I 2 = 45.4%; p < 0.001; n = 10), and across studies with > 100 number of case (RR = 1.38; 95% CI: 1.21, 1.58; I 2 = 74.8%; p < 0.001; n = 12)(vs. < 100 number of case), in studies with > 1000 number of participants (RR = 1.33; 95% CI: 1.15, 1.54; I 2 = 76.9%; p < 0.001; n = 21)(vs. < 1000 number of participants), in studies used FFQ for dietary assessment (RR = 1.27; 95% CI: 1.14, 1.43; I 2 = 78.6%; p < 0.001; n = 34) (vs. 24 h recall or food record), particularly in studies where the period of dietary assessment was at early pregnancy (RR = 1.26; 95% CI: 1.09, 1.46; I 2 = 80.5%; p = 0.002; n = 19) (vs. pre-pregnancy or mid-pregnancy). Moreover, subgroup analysis for covariates adjustment showed that BMI and physical activity may influence the association between UPF intake and the risk of GDM (Table 2 ).
For PE, the subgroup analysis also highlighted that greater UPFs intake was significantly associated with an enhanced risk in studies assessed western dietary pattern (RR = 2.51; 95% CI: 1.13, 5.57; I 2 = 91.1%; p = 0.023; n = 3) or NOVA classification (RR = 1.22; 95% CI: 1.04, 1.42; I 2 = 0.0%; p = 0.013; n = 3), (vs. sweets consumption), in Asia (vs. Europe or US areas) (RR = 1.65; 95% CI: 1.07, 2.55; I 2 = 86.1%; p < 0.001; n = 6), and across studies with > 100 number of case (RR = 1.57; 95% CI: 1.03, 2.40; I 2 = 93.2%; p < 0.001; n = 4)(vs. < 100 number of case), in studies with number of < 1000 participants (RR = 1.65; 95% CI: 1.07, 2.55; I 2 = 86.1%; p = 0.023; n = 6)(vs. > 1000 number of participants), in participants aged ≥30 years (RR = 1.28; 95% CI: 1.07, 1.54; I 2 = 50.4%; p = 0.089; n = 5)(vs. participants aged < 30 years), in participants with pre-pregnancy-BMI > 25 (RR = 1.52; 95% CI: 1.07, 2.15; I 2 = 84.7%; p = 0.021; n = 1)(vs. participants with pre-pregnancy-BMI ≤ 25), in studies used FFQ for dietary assessment (RR = 1.38; 95% CI: 1.10, 1.72; I 2 = 82.6%; p = 0.005; n = 10) (vs. questions), and particularly in studies where the period of dietary assessment was at mid-pregnancy (RR = 1.23; 95% CI: 1.05, 1.43; I 2 = 38.8%; p = 0.009; n = 3) (vs. early pregnancy). Furthermore, subgroup analysis for covariates adjustment showed that BMI and physical activity may influence the association between UPF intake and the risk of PE (Table 3 ).
Linear and non-linear dose-response analysis
The linear dose-response analysis (refer to Table 1 and Fig. 2 ) indicates a 27% increase in GDM risk per 100 g increment in UPF intake RR = 1.27; 95% CI: 1.07, 1.51; I 2 = 81.0%; p = 0.007; n = 9). However, the linear dose-response analysis for other outcomes was not undertaken due to the limited number of studies available.
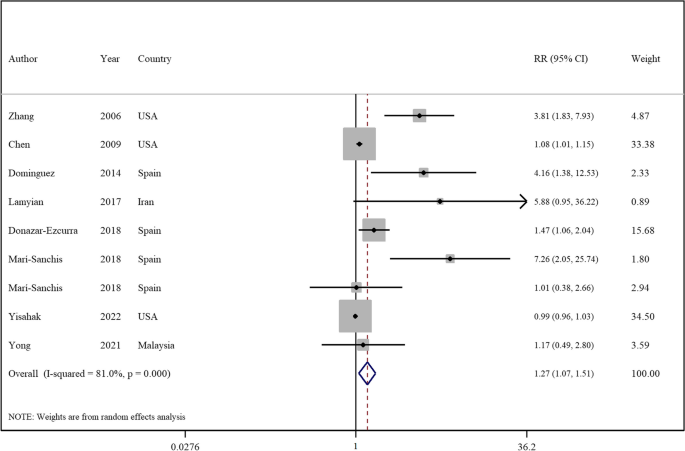
Forest plots showing the linear dose-response meta-analysis of mortality risk for 100 g change in ultra-processed food consumption in daily intake and risk of gestational diabetes mellitus
The non-linear dose-response analysis revealed a positive non-linear relationship between UPFs intake and GDM risk (P nonlinearity = 0.034, P dose-response = 0.034, Fig. 3 ), but not for PE (P nonlinearity = 0.696, P dose-response = 0.812, Fig. 4 ). The non-linear dose-response analysis was not conducted for other outcomes due to insufficient studies.
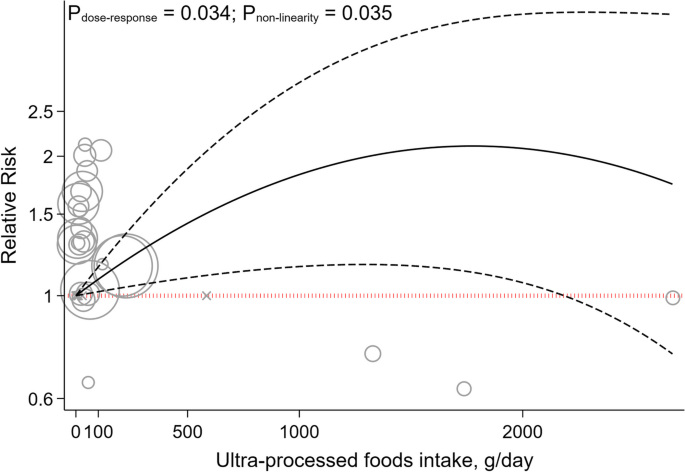
Non-linear dose-response indicated associations between UPF intake and the risk of gestational diabetes mellitus
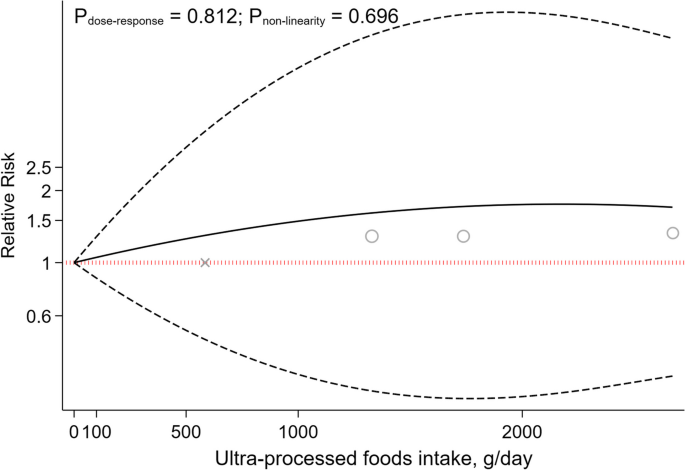
Non-linear dose-response indicated associations between UPF intake and the risk of preeclampsia
Sensitivity analyses and publication bias
Sensitivity analysis across the highest to the lowest meta-analysis for GDM, PE, PTB, LBW and SGA infants showed no significant influence of any single study (Supplemental Fig. 2 ).
No evidence of publication bias was found in articles related to the association with an increased risk of PE ( p = 0.529, Egger’s test; p = 0.891, Begg’s), PTB ( p = 0.458, Egger’s test; p = 0.473, Begg’s), LBW ( p = 0.905, Egger’s test; p = 1.00, Begg’s test), and SGA infants ( p = 0.348, Egger’s test; p = 1.00, Begg’s test). Although, for GDM, Egger’s test indicated potential publication bias ( p < 0.001), not corroborated by Begg’s test ( p = 0.241). As illustrated in Supplemental Fig. 3 , the funnel plot was symmetrical for the association between the UPFs intake and all outcomes, except for studies that reported the risk of GDM disease.
Utilizing the GRADE scale for quality evaluation, we detected the evidence for associations between UPFs intake and risk of GDM, PE, PTB, LBW and SGA infants was classified as moderate (Refer to Table 1 ).
In the realm of maternal and fetal health, the quality of dietary intake during pregnancy is of paramount significance. Accumulating evidence suggests a correlation between the consumption of UPFs and the deterioration of diet quality, potentially elevating the risk of various health complications [ 80 , 81 , 82 ]. This systematic review and meta-analysis aimed to elucidate the relationship between UPFs intake and adverse pregnancy outcomes including GDM, SGA, LBW, PTB, and PE, through an integrative analysis of existing studies. Our outcomes indicate a significant association between UPFs consumption and increased risks of PE, and GDM either prior to or during pregnancy. However, no significant association was found between UPFs intake and the risks of LBW, SGA, and PTB. Importantly, a 27% increment in the incidence of GDM was linked to a 100 g increase in UPF intake. Furthermore, a positive, non-linear relationship between UPF intake and GDM risk was identified through non-linear dose-response analysis, albeit no analogous association was found for PE.
The results of the current work showed a positive association between UPFs consumption and the risk of PE. In addition, subgroup analysis revealed this relationship to be more pronounced in studies using the NOVA-food classification and a Western dietary pattern for UPFs intake assessment, compared to those focusing on sweet intake. The NOVA classification categorizes foods based on the extent of processing, encompassing various UPFs. Moreover, the association between UPFs consumption and the risk of PE was significant in studies conducted in Asia (vs other regions). Prevalence of PE varies globally, ranging from 0.2–6.7% in Asia, 2.8–9.2% in Oceania, 2.8–5.2% in Europe, 2.6–4.0% in North America, and 1.8–7.7% in South America and the Caribbean [ 83 ]. However, the high heterogeneity in Asian studies should be noted when interpreting this result. Furthermore, a significant association was observed in studies involving women aged 30 years or older, aligning with the increased PE risk associated with advanced maternal age [ 84 ]. Additionally, a significant association was identified between PE risk and UPFs intake in women with pre-pregnancy BMI higher than 25 kg/m 2 (vs BMI ≤25). This aligns with previous findings linking excessive weight gain in expectant mothers to an elevated PE risk, with overweight and obese mothers facing substantially higher risks [ 85 ].
The association between UPFs intake and PE can be elucidated through several mechanisms. The risk factors for PE, including GDM, maternal obesity, and advanced maternal age, are extensively documented in the literature [ 84 , 85 , 86 ]. It has been established that adopting healthy lifestyle habits (including dietary patterns) can mitigate these risk factors [ 87 ]. A higher intake of UPFs is associated with a diminished dietary quality, marked by an increased consumption of sugars and fats, alongside a decrease in fiber, protein, vitamins, and minerals [ 88 , 89 ]. UPFs are known to contain elevated levels of pro-inflammatory agents such as refined sugars, salt, and trans fats. The ingestion of these inflammatory components can precipitate oxidative stress and systemic inflammation [ 90 , 91 , 92 ], which are implicated in the pathogenesis of preeclampsia [ 93 , 94 ]. Additionally, the presence of trans fatty acids, added phosphates, and a high salt content in UPFs may impair endothelial function [ 95 , 96 , 97 ], a critical factor in the pathophysiology of hypertension observed in preeclampsia [ 98 ]. Furthermore, the intake of UPFs can alter the composition and diversity of the gut microbiota [ 99 ]. Studies have shown that food additives commonly found in UPFs, such as emulsifiers, sweeteners, and colorants, adversely affect the gut flora [ 100 ]. The interplay between the gut microbiota and the placenta, referred to as the “gut–placenta” axis, is crucial for understanding the etiology of PE. Dysbiosis of the gut microbiota and bacterial products like lipopolysaccharide (LPS) have been identified as promotive of PE [ 101 , 102 ]. According to Kell et al., microbial infection, particularly through bacterial products such as LPS (also known as endotoxin), which is highly inflammatory, can initiate an innate immune response that exacerbates inflammation [ 103 ]. Hence, it is hypothesized that dysbiosis induced by UPFs consumption may play a significant role in the promotion of preeclampsia. Moreover, UPFs intake is positively associated with a risk of obesity [ 104 ], a condition marked by insulin resistance and hyperinsulinemia, crucial factors in PE development [ 105 ]. Pregnant women with obesity and PE exhibit higher leptin levels, correlating with increased Tumor Necrosis Factor-Alfa (TNF-α), Interleukin 6 (IL-6), and C-reactive protein concentrations [ 106 , 107 ]. Additionally, excessive adipose tissue near the reproductive tract is the source of increased complement components and fragments in preeclamptic pregnancies. These complement proteins may promote an imbalance in angiogenic factors (characterized by increased production of antiangiogenic factors and a decrease in proangiogenic factors). This imbalance leads to placental injury, resulting in decreased blood flow to the tissue, and is accompanied by changes in cytokines levels (decreased IL-10 and increased TNF-α) before the onset of PE [ 108 ].
Our pooled analysis also revealed that higher UPFs intake was related to an increased risk of GDM. This association was significant in studies employing cohort and case-control designs (as opposed to those with cross-sectional methodologies). The inherent recall bias in cross-sectional studies that rely on self-reporting, is a notable limitation affecting the reliability of outcomes [ 109 ]. Moreover, this association was more pronounced in studies that used Western dietary patterns and fast-food consumption for the assessment of UPFs intake (vs those employing NOVA food classification and sweet consumption metrics). The concept of a dietary pattern, which represents the aggregate of eating and drinking habits, is critical as it exerts a greater impact on health and chronic diseases than any individual food item [ 110 ]. Additionally, the application of the NOVA food classification in existing studies is less frequent, suggesting the need for further research utilizing this methodology to derive more meaningful results. Geographical variations were also evident, with significant associations observed in studies conducted in America, compared to those in Asia and Europe. This is in context with the differing regional prevalences of GDM: 7.1% in North America and the Caribbean, 7.8% in Europe and 20.8% in South-East Asia [ 111 ]. Despite the higher prevalence of GDM in Asian populations, the greater intake of UPFs in American and European cohorts may have influenced the study outcomes [ 112 , 113 , 114 , 115 ]. Additionally, a positive association between UPFs intake and GDM risk was observed in studies focusing on women with a pre-pregnancy BMI > 25. Previous research indicates that being overweight or obese before and during pregnancy is a significant risk factor for GDM [ 116 , 117 , 118 ]. However, the scarcity of studies in women with pre-pregnancy BMI > 25 kg/m 2 kg/m suggests the need for more research in this demographic for robust conclusions.
Our outcomes also indicated that a 100 g increase in UPF intake was associated with a 27% increase in the risk of GDM. Moreover, the non-linear dose-response analysis similarly showed a positive, non-linear association between the consumption of UPFs and the risk of GDM. These findings underscore the significant impact that UPF consumption can have on GDM risk. The evidence points towards a robust and worrying correlation where even moderate increases in UPF intake can precipitate a marked rise in GDM risk, highlighting the critical need for dietary awareness and intervention among pregnant women. This aligns with broader nutritional science, emphasizing the importance of minimizing UPF consumption to mitigate not only GDM risk but potentially other metabolic disorders as well, given the multitude of adverse mechanisms through which UPFs affect glucose metabolism and insulin sensitivity.
Pathophysiologically, UPFs intake may increase GDM risk through several mechanisms. In pregnant women with GDM, pre-pregnancy reduced insulin sensitivity and β-cell dysfunction lead to hyperglycemia [ 119 , 120 ]. The hypothesis that excessive sugar intake may augment body mass, thereby indirectly precipitating insulin resistance and subsequent diabetes, is widely recognized. Moreover, the liver’s capacity to assimilate and metabolize refined sugars prevalent in UPFs (such as fructose and sucrose) may be compromised, leading to augmented fat deposition and deteriorated insulin sensitivity [ 121 ]. Furthermore, insulin resistance may be induced by cosmetic ingredients present in UPFs. For example, dietary additives like carrageenan, employed as a thickening and stabilizing agent, may interfere with insulin signaling and thus foster insulin resistance [ 122 ]. Additionally, UPFs intake correlates with increased production of reactive oxygen species and inflammatory biomarkers [ 123 ], inducing insulin resistance through molecular pathways such as β-cell and mitochondrial dysfunction, decreased GLUT4 expression, impaired insulin signaling and heightened inflammatory responses [ 124 ]. Furthermore, UPFs often contain packaging materials like phthalates and bisphenol A, known to have endocrine disruption properties that may contribute to insulin resistance and diabetes development [ 125 , 126 ]. The ingestion of substantial quantities of UPFs also elevates inflammation, a pivotal factor in the genesis of insulin resistance, culminating in hyperglycemia and the development of GDM [ 127 ]. A diet replete with saturated fats, trans fats, sugars, and salt, characteristic of high UPFs consumption, may contribute to chronic inflammation [ 128 ]. Furthermore, excessive UPFs consumption may supplant essential components of a balanced and nutritious diet. For instance, fruits and vegetables are associated with an anti-inflammatory effect [ 129 ]. In addition, the leaching of chemicals from food packaging into UPFs could introduce non-nutritional elements such as phthalates or bisphenol A, potentially eliciting an inflammatory response [ 130 ].
The present study did not establish a significant association between UPFs consumption and the risk of LBW. This result may be attributable to several factors. Firstly, a limited number of studies have evaluated the association between UPFs intake and LBW risk. Additionally, the intake of high-sugar foods (such as sugar-sweetened beverages) has been correlated with an increased risk of LBW in non-GDM subjects [ 34 , 40 ]. This could be attributed to impaired fetal nutrition due to reduced vascular function, potentially induced by oxidative stress, inflammation, and endothelial dysfunction associated with high sugar consumption [ 131 ]. However, in GDM subjects this association may not be found due to the higher glucose loads in the fetus [ 47 ]. Therefore, additional research is warranted in both GDM and non-GDM populations to elucidate these relationships comprehensively.
Moreover, SGA was not associated with the intake of UPFs according to the pooled analysis of conducted studies. Although additional studies are necessary to explore this relationship further, existing evidence suggests that a fast-food dietary pattern may lead to increased fat intake and a reduced intake of essential micronutrients crucial for fetal development [ 132 ]. Maternal UPFs intake is linked to lower protein intake, reduced overall nutrition quality, and higher intake of trans fats, carbohydrates and saturated fats, which may increase the risk of neonatal adiposity [ 133 , 134 , 135 ]. Furthermore, higher fast-food intake during pregnancy has been linked with an elevated risk of maternal obesity, which in turn, may increase the likelihood of LGA babies [ 132 , 136 ].
Regarding PTB, the current study found no association with UPFs consumption. Previous research has indicated that dietary patterns rich in fruits and vegetables are associated with a lower risk of PTB [ 37 , 45 ]. Inadequate nutrition before and during pregnancy can lead to health issues for both the mother and fetus, increasing the risk of preterm delivery and intrauterine growth retardation [ 137 ]. The absence of an association between UPFs consumption and preterm delivery in this study could be due to various factors, including the need for a higher UPFs consumption threshold during pregnancy to manifest negative impacts on preterm birth. Additionally, the varied diet of pregnant women, typically including beneficial foods such as fruits, vegetables and nuts, may mitigate the adverse effects of UPFs.
The current investigation has several crucial strengths that make its findings highly significant. Firstly, by pooling all available observational data on the topic, the study provides a comprehensive and robust analysis of the relationship between UPFs intake and adverse pregnancy outcomes. Secondly, the study’s use of a dose-response analysis adds further weight to its conclusions and bolsters our understanding of the link between these two factors. However, there are limitations to consider. These include potential information and recall biases due to the self-reported nature of dietary intake assessments (such as the FFQ) and the absence of specific dietary tools for assessing UPFs consumption. Additionally, this meta-analysis included studies that did not use NOVA’s specialized dietary assessments. Moreover, dietary changes following pregnancy discovery could affect results, and the observational nature of the included studies precludes causal inference. Despite the inclusion of numerous confounding variables, several factors must be cautiously considered in the interpretation of the research findings. For instance, the socio-economic status of participants influences their dietary habits, while race and ethnicity may affect pregnancy outcomes. Furthermore, disparities in access to healthcare services can impact dietary choices and pregnancy outcomes. Other health statuses, such as mental health conditions among pregnant subjects, also influence dietary selections and pregnancy results [ 138 , 139 ]. Finally, the availability of data on broader categories such as diabetes in pregnancy and hypertensive disorders was limited, hindering our ability to conduct a comprehensive analysis on these broader categories.
Our outcomes indicate that prior to or during pregnancy, UPFs intake is associated with a higher risk of GDM and PE. However, no significant link tying UPFs intake to SGA, LWB and PTB was established. Importantly, a 100 g increment in UPFs intake was related to a 27% increase in GDM risk. This study aligns with global trends, where a rise in adverse pregnancy outcomes seems to align with the escalation of industrialization and the corresponding surge in UPFs production and consumption. Investigating the potential linkage between UPFs intake and the rise of adverse pregnancy outcomes may help in the development of nutrition-centric policies for expecting mothers and promote more health-conscious decision-making. To further substantiate these findings, extensive empirical research is required. Future studies should encompass observational research across diverse ethnic groups. Moreover, the adoption of more precise tools for measuring UPFs consumption is imperative. In observational research, it may be challenging to ascertain whether the consumption of UPFs directly contributes to adverse pregnancy outcomes or if it serves as an indicator of other underlying factors. Components of UPFs may escalate the risk of negative pregnancy outcomes. Moreover, UPF consumption could be part of a complex interplay affecting other variables that directly result in adverse outcomes. For instance, UPF intake could influence gestational weight gain, potentially leading to insulin resistance, which is known to correlate with unfavorable pregnancy outcomes, including GDM. Additionally, the consumption of UPFs may not only diminish dietary quality but also be linked with various lifestyle and dietary factors, such as poor diet quality, thereby increasing the risk of adverse pregnancy outcomes [ 140 ]. The bidirectional correlation between UPF consumption and unfavorable pregnancy outcomes also merits consideration. For example, individuals experiencing depression or other health conditions might alter their dietary patterns to include a higher intake of UPFs [ 138 ]. Evaluating changes in UPF consumption over time, utilizing precise questionnaires that assess food items classified as UPFs according to the NOVA food classification system, and their association with other health outcomes affecting pregnancy, such as obesity, could offer insights into this relationship. Considering these approaches is essential to enhance the depth and accuracy of investigations into the potential association between UPFs intake and the incidence of adverse pregnancy outcomes.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due but are available from the corresponding author on reasonable request.
Hoyert DL, Miniño AM. Maternal Mortality in the United States: Changes in Coding, Publication, and Data Release, 2018. Natl Vital Stat Rep. 2020;69(2):1–18.
PubMed Google Scholar
Parikh NI, Gonzalez JM, Anderson CA, Judd SE, Rexrode KM, Hlatky MA, et al. Adverse pregnancy outcomes and cardiovascular disease risk: unique opportunities for cardiovascular disease prevention in women: a scientific statement from the American Heart Association. Circulation. 2021;143(18):e902–e16.
Article CAS PubMed Google Scholar
Hashmi AH, Solomon N, Lee SJ, Min AM, Gilder ME, Wiladphaingern J, et al. Nutrition in transition: historical cohort analysis summarising trends in under-and over-nutrition among pregnant women in a marginalised population along the Thailand–Myanmar border from 1986 to 2016. Br J Nutr. 2019;121(12):1413–23.
Lind JM, Hennessy A, McLean M. Cardiovascular disease in women: the significance of hypertension and gestational diabetes during pregnancy. Curr Opin Cardiol. 2014;29(5):447–53.
Article PubMed Google Scholar
Englund-Ögge L, Birgisdottir BE, Sengpiel V, Brantsæter AL, Haugen M, Myhre R, et al. Meal frequency patterns and glycemic properties of maternal diet in relation to preterm delivery: results from a large prospective cohort study. PLoS One. 2017;12(3):e0172896.
Article PubMed PubMed Central Google Scholar
Mekie M, Mekonnen W, Assegid M. Cohabitation duration, obstetric, behavioral and nutritional factors predict preeclampsia among nulliparous women in West Amhara zones of Ethiopia: age matched case control study. PLoS One. 2020;15(1):e0228127.
Article CAS PubMed PubMed Central Google Scholar
Monteiro CA, Cannon G, Levy R, Moubarac J-C, Jaime P, Martins AP, et al. NOVA The star shines bright. World Nutrition. 2016;7(1–3):28–38.
Google Scholar
da Costa Louzada ML, Baraldi LG, Steele EM, Martins APB, Canella DS, Moubarac J-C, et al. Consumption of ultra-processed foods and obesity in Brazilian adolescents and adults. Prev Med. 2015;81:9–15.
Article Google Scholar
Monteiro CA, Levy RB, Claro RM, Castro IRR, Cannon G. A new classification of foods based on the extent and purpose of their processing. Cadernos de saude publica. 2010;26:2039–49.
Mendonça RD, Pimenta AM, Gea A, de la Fuente-Arrillaga C, Martinez-Gonzalez MA, Lopes ACS, et al. Ultraprocessed food consumption and risk of overweight and obesity: the University of Navarra Follow-up (SUN) cohort study. Am J Clin Nutr. 2016;104(5):1433–40.
Mendonça RD, Lopes ACS, Pimenta AM, Gea A, Martinez-Gonzalez MA, Bes-Rastrollo M. Ultra-processed food consumption and the incidence of hypertension in a Mediterranean cohort: the Seguimiento Universidad de Navarra project. Am J Hypertens. 2017;30(4):358–66.
Fiolet T, Srour B, Sellem L, Kesse-Guyot E, Allès B, Méjean C, Deschasaux M, Fassier P, Latino-Martel P, Beslay M, Hercberg S, Lavalette C, Monteiro CA, Julia C, Touvier M. Consumption of ultra-processed foods and cancer risk: results from NutriNet-Santé prospective cohort. BMJ. 2018;360:k322. https://doi.org/10.1136/bmj.k322 .
Bhattacharyya S, Feferman L, Tobacman JK. Carrageenan inhibits insulin signaling through GRB10-mediated decrease in Tyr (P)-IRS1 and through inflammation-induced increase in Ser (P) 307-IRS1. J Biol Chem. 2015;290(17):10764–74.
Buckley JP, Kim H, Wong E, Rebholz CM. Ultra-processed food consumption and exposure to phthalates and bisphenols in the US National Health and nutrition examination survey, 2013–2014. Environ Int. 2019;131:105057.
Paula WO, Patriota ES, Gonçalves VS, Pizato N. Maternal consumption of ultra-processed foods-rich diet and perinatal outcomes: a systematic review and meta-analysis. Nutrients. 2022;14(15):3242.
Mahendra A, Kehoe SH, Kumaran K, Krishnaveni GV, Arun N, Pidaparthy P, et al. Periconceptional diet and the risk of gestational diabetes in south Indian women: findings from the BAngalore nutrition gestational diabetes LiFEstyle study (BANGLES). Lancet Glob Health. 2023;11:S4.
Kooshki A, Sovizi B, Mahmoudi R, Ghezi S, Foroumandi E. The association between food groups and preeclampsia: a case-control study. Hyperten Pregnancy. 2022;41(1):64–9.
Article CAS Google Scholar
Moradi M, Niazi A, Selajgeh F, Mazloumi E. Comparing dietary patterns during pregnancy in women with preeclampsia and healthy women: a case-control study. J Midwife Reproduct Health. 2022;10(1)
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Oxford: Ottawa Hospital Research Institute; 2000.
Symons M, Moore D. Hazard rate ratio and prospective epidemiological studies. J Clin Epidemiol. 2002;55(9):893–9.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Jayedi A, Soltani S, Zargar MS, Khan TA, Shab-Bidar SJB. Central fatness and risk of all cause mortality: systematic review and dose-response meta-analysis of 72 prospective cohort studies. 2020;370.
Song C, Lyu Y, Li C, Liu P, Li J, Ma R, et al. Long-term risk of diabetes in women at varying durations after gestational diabetes: a systematic review and meta-analysis with more than 2 million women 2018;19(3):421–9.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–101.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ (Clin res ed). 1997;315(7109):629–34.
Berlin JA, Longnecker MP, Greenland S. Meta-analysis of epidemiologic dose-response data. Epidemiology. 1993;4(3):218–28. https://doi.org/10.1097/00001648-199305000-00005 .
Orsini N, Bellocco R, Greenland SJTsj. Generalized least squares for trend estimation of summarized dose–response data 2006;6(1):40–57.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. Bmj. 2008;336(7650):924–6.
Abbasi R, Bakhshimoghaddam F, Alizadeh M. Major dietary patterns in relation to preeclampsia among Iranian pregnant women: a case–control study. J Matern Fetal Neonatal Med. 2021;34(21):3529–36.
Alves-Santos NH, Cocate PG, Benaim C, Farias DR, Emmett PM, Kac G. Prepregnancy dietary patterns and their association with perinatal outcomes: a prospective cohort study. J Acad Nutr Diet. 2019;119(9):1439–51.
Asadi M, Shahzeidi M, Nadjarzadeh A, Hashemi Yusefabad H, Mansoori A. The relationship between pre-pregnancy dietary patterns adherence and risk of gestational diabetes mellitus in Iran: a case–control study. Nutr Diet. 2019;76(5):597–603.
Bao W, Tobias DK, Olsen SF, Zhang C. Pre-pregnancy fried food consumption and the risk of gestational diabetes mellitus: a prospective cohort study. Diabetol. 2014;57(12):2485–91.
Bartáková V, Kuricová K, Zlámal F, Bělobrádková J, Kaňková K. Differences in food intake and genetic variability in taste receptors between Czech pregnant women with and without gestational diabetes mellitus. Eur J Nutr. 2018;57(2):513–21.
Brantsæter AL, Haugen M, Samuelsen SO, Torjusen H, Trogstad L, Alexander J, et al. A dietary pattern characterized by high intake of vegetables, fruits, and vegetable oils is associated with reduced risk of preeclampsia in nulliparous pregnant Norwegian women. J Nutr. 2009;139(6):1162–8.
Chen LW, Hu FB, Yeung E, Willett W, Zhang CL. Prospective study of pre-gravid sugar-sweetened beverage consumption and the risk of gestational diabetes mellitus. Diabetes Care. 2009;32(12):2236–41.
Chia AR, de Seymour JV, Colega M, Chen LW, Chan YH, Aris IM, et al. A vegetable, fruit, and white rice dietary pattern during pregnancy is associated with a lower risk of preterm birth and larger birth size in a multiethnic Asian cohort: the growing up in Singapore towards healthy outcomes (GUSTO) cohort study. Am J Clin Nutr. 2016;104(5):1416–23.
de Seymour J, Chia AR, Colega M, Jones B, McKenzie E, Cai SR, et al. Maternal dietary patterns and gestational diabetes mellitus in a multi-ethnic Asian cohort: the GUSTO study. Nutrients. 2016;8(9)
Dominguez LJ, Martinez-Gonzalez MA, Basterra-Gortari FJ, Gea A, Barbagallo M, Bes-Rastrollo M. Fast food consumption and gestational diabetes incidence in the SUN project. PLoS One. 2014;9(9):e106627.
Donazar-Ezcurra M, Lopez-del Burgo C, Martinez-Gonzalez MA, Basterra-Gortari FJ, de Irala J, Bes-Rastrollo M. Soft drink consumption and gestational diabetes risk in the SUN project. Clin Nutr. 2018;37(2):638–45.
Dong JY, Kimura T, Ikehara S, Cui M, Kawanishi Y, Yamagishi K, et al. Chocolate consumption and risk of gestational diabetes mellitus: the Japan environment and Children's study. Br J Nutr. 2019;122(8):936–41.
Drozd-Dąbrowska M, Trusewicz R, Ganczak M. Selected risk factors of developmental delay in polish infants: a case-control study. Int J Environ Res Public Health. 2018;15(12)
Du HY, Jiang H, Karmin O, Bo C, Xu LJ, Liu SP, et al. Association of dietary pattern during pregnancy and gestational diabetes mellitus: a prospective cohort study in northern China. Biomed Environ Sci. 2017;30(12):887–97.
CAS PubMed Google Scholar
Englund-Ögge L, Brantsæter AL, Sengpiel V, Haugen M, Birgisdottir BE, Myhre R, et al. Maternal dietary patterns and preterm delivery: Results from large prospective cohort study. BMJ (Online). 2014;348
Gete DG, Waller M, Mishra GD. Prepregnancy dietary patterns and risk of preterm birth and low birth weight: findings from the Australian longitudinal study on Women's health. Am J Clin Nutr. 2020;111(5):1048–58.
Grieger JA, Grzeskowiak LE, Clifton VL. Preconception dietary patterns in human pregnancies are associated with preterm delivery. J Nutr. 2014;144(7):1075–80.
Grundt JH, Eide GE, Brantsæter AL, Haugen M, Markestad T. Is consumption of sugar-sweetened soft drinks during pregnancy associated with birth weight? Mater Child Nutrit. 2017;13(4):e12405.
Hajianfar H, Esmaillzadeh A, Feizi A, Shahshahan Z, Azadbakht L. The association between major dietary patterns and pregnancy-related complications. Archiv Iran Med. 2018;21(10):443–51.
Hehua Z, Yang X, Qing C, Shanyan G, Yuhong Z. Dietary patterns and associations between air pollution and gestational diabetes mellitus. Environ Int. 2021;147
Hezaveh ZS, Feizy Z, Dehghani F, Sarbakhsh P, Moini A, Vafa M. The association between maternal dietary protein intake and risk of gestational diabetes mellitus. International journal of. Prev Med. 2019;10(1)
Hu JJ, Oken E, Aris IM, Lin PID, Ma YA, Ding N, et al. Dietary patterns during pregnancy are associated with the risk of gestational diabetes mellitus: evidence from a Chinese prospective birth cohort study. Nutrients. 2019;11(2)
Ikem E, Halldorsson TI, Birgisdóttir BE, Rasmussen MA, Olsen SF, Maslova E. Dietary patterns and the risk of pregnancy-associated hypertension in the Danish National Birth Cohort: a prospective longitudinal study. BJOG: An Int J Obstetr Gynaecol. 2019;126(5):663–73.
Kahr MK, Suter MA, Ballas J, Ramin SM, Monga M, Lee W, et al. Geospatial analysis of food environment demonstrates associations with gestational diabetes. Am J Obstet Gynecol. 2016;214(1):110.e1-.e9.
Lamyian M, Hosseinpour-Niazi S, Mirmiran P, Banaem LM, Goshtasebi A, Azizi F. Pre-pregnancy fast food consumption is associated with gestational diabetes mellitus among tehranian women. Nutrients. 2017;9(3)
Leone A, Martínez-González M, Craig W, Fresán U, Gómez-Donoso C, Bes-Rastrollo M. Pre-gestational consumption of ultra-processed foods and risk of gestational diabetes in a Mediterranean cohort. The SUN project. Nutrients. 2021;13(7)
Lotfi MH, Fallahzadeh H, Rahmanian M, Hosseinzadeh M, Lashkardoost H, Doaei S, et al. Association of food groups intake and physical activity with gestational diabetes mellitus in Iranian women. J Mater -Fetal Neonatal Med. 2020;33(21):3559–64.
Marí-Sanchis A, Díaz-Jurado G, Basterra-Gortari FJ, de la Fuente-Arrillaga C, Martínez-González MA, Bes-Rastrollo M. Association between pre-pregnancy consumption of meat, iron intake, and the risk of gestational diabetes: the SUN project. Eur J Nutr. 2018;57(3):939–49.
Martin CL, Sotres-Alvarez D, Siega-Riz AM. Maternal dietary patterns during the second trimester are associated with preterm birth. J Nutr. 2015;145(8):1857–64.
Nascimento GR, Alves LV, Fonseca CL, Figueiroa JN, Alves JG. Dietary patterns and gestational diabetes mellitus in a low income pregnant women population in Brazil - a cohort study. Archivos Latinoamericanos de Nutricion. 2016;66(4):301–8.
Osorio-Yáñez C, Gelaye B, Qiu C, Bao W, Cardenas A, Enquobahrie DA, et al. Maternal intake of fried foods and risk of gestational diabetes mellitus. Ann Epidemiol. 2017;27(6):384–90.e1.
Rasmussen MA, Maslova E, Halldorsson TI, Olsen SF. Characterization of dietary patterns in the Danish National Birth Cohort in relation to preterm birth. PLoS One. 2014;9(4)
Saftlas AF, Triche EW, Beydoun H, Bracken MB. Does chocolate intake during pregnancy reduce the risks of preeclampsia and gestational hypertension? Ann Epidemiol. 2010;20(8):584–91.
Santos IS, Victora CG, Huttly S, Carvalhal JB. Caffeine intake and low birth weight: a population-based case-control study. Am J Epidemiol. 1998;147(7):620–7.
Sartorelli DS, Crivellenti LC, Zuccolotto DCC, Franco LJ. Relationship between minimally and ultra-processed food intake during pregnancy with obesity and gestational diabetes mellitus. Cadernos de Saude Publica. 2019;35(4)
Schoenaker DA, Soedamah-Muthu SS, Callaway LK, Mishra GD. Pre-pregnancy dietary patterns and risk of gestational diabetes mellitus: results from an Australian population-based prospective cohort study. Diabetol. 2015;58(12):2726–35. https://doi.org/10.1007/s00125-015-3742-1 . Epub 2015 Sep 10.
Sedaghat F, Akhoondan M, Ehteshami M, Aghamohammadi V, Ghanei N, Mirmiran P, Rashidkhani B. Maternal Dietary Patterns and Gestational Diabetes Risk: A Case-Control Study. J Diabetes Res. 2017;2017:5173926. https://doi.org/10.1155/2017/5173926 . Epub 2017 Dec 6.
Tamada H, Ebara T, Matsuki T, Kato S, Sato H, Ito Y, et al. Ready-meal consumption during pregnancy is a risk factor for stillbirth: the Japan environment and Children’s study (JECS). Japan environment and Children’s study, Ready-Meal Consumption During Pregnancy is a Risk Factor for Stillbirth: The Japan Environment and Children’s Study (JECS).
Teixeira JA, Hoffman DJ, Castro TG, Saldiva S, Francisco RPV, Vieira SE, et al. Pre-pregnancy dietary pattern is associated with newborn size: results from ProcriAr study. Br J Nutr. 2021;126(6):903–12.
Triche EW, Grosso LM, Belanger K, Darefsky AS, Benowitz NL, Bracken MB. Chocolate consumption in pregnancy and reduced likelihood of preeclampsia. Epidemiol. 2008;19(3):459–64.
Tryggvadottir EA, Medek H, Birgisdottir BE, Geirsson RT, Gunnarsdottir I. Association between healthy maternal dietary pattern and risk for gestational diabetes mellitus. Eur J Clin Nutr. 2016;70(2):237–42.
Tsoi KY, Chan RSM, Tam CH, Li LS, Tam WH, Ma RCW. Dietary patterns of Chinese pregnant women in Hong Kong. Asia Pac J Clin Nutr. 2022;31(3):378–93.
Wahedy K, El Bilbeisi AHH, Bakry MJ. DIETARY PATTERNS and THEIR ASSOCIATION with GLYCEMIC CONTROL and RISK of GESTATIONAL DIABETES MELLITUS in GAZA STRIP, PALESTINE: a CASE-CONTROL STUDY. Bullet Pharmaceut Sci Assiut. 2021;44(2):537–49.
Wen L, Ge H, Qiao J, Zhang L, Chen X, Kilby MD, et al. Maternal dietary patterns and risk of gestational diabetes mellitus in twin pregnancies: a longitudinal twin pregnancies birth cohort study. Nutr J. 2020;19(1)
Yisahak SF, Hinkle SN, Mumford SL, Gleason JL, Grantz KL, Zhang C, et al. Periconceptional and first trimester Ultraprocessed food intake and maternal Cardiometabolic outcomes. Diabetes Care. 2022;45(9):2028–36.
Yong HY, Mohd Shariff Z, Mohd Yusof BN, Rejali Z, Tee YYS, Bindels J, van der Beek EM. Beverage Intake and the Risk of Gestational Diabetes Mellitus: The SECOST. Nutrients. 2021;13(7):2208. https://doi.org/10.3390/nu13072208 .
Zareei S, Homayounfar R, Naghizadeh MM, Ehrampoush E, Amiri Z, Rahimi M, et al. Dietary pattern in patients with preeclampsia in Fasa. Iran Shiraz E Med J. 2019;20(11)
Zareei S, Homayounfar R, Naghizadeh MM, Ehrampoush E, Rahimi M. Dietary pattern in pregnancy and risk of gestational diabetes mellitus (GDM). Diabet Metabol Syndrome: Clin Res Rev. 2018;12(3):399–404.
Zhang C, Schulze MB, Solomon CG, Hu FB. A prospective study of dietary patterns, meat intake and the risk of gestational diabetes mellitus. Diabetologia. 2006;49(11):2604-13. https://doi.org/10.1007/s00125-006-0422-1 . Epub 2006 Sep 7.
Zuccolotto DCC, Crivellenti LC, Franco LJ, Sarotelli DS. Dietary patterns of pregnant women, maternal excessive body weight and gestational diabetes. Revista de Saude Publica. 2019;53.
Moradi S, Hojjati Kermani MA, Bagheri R, Mohammadi H, Jayedi A, Lane MM, et al. Ultra-processed food consumption and adult diabetes risk: a systematic review and dose-response Meta-analysis. Nutrients. 2021;13(12)
Suksatan W, Moradi S, Naeini F, Bagheri R, Mohammadi H, Talebi S, Mehrabani S, Hojjati Kermani MA, Suzuki K. Ultra-Processed Food Consumption and Adult Mortality Risk: A Systematic Review and Dose-Response Meta-Analysis of 207,291 Participants. Nutrients. 2021;14(1):174. https://doi.org/10.3390/nu14010174 .
Babaei A, Pourmotabbed A, Talebi S, Mehrabani S, Bagheri R, Ghoreishy SM, et al. The association of ultra-processed food consumption with adult inflammatory bowel disease risk: a systematic review and dose-response meta-analysis of 4 035 694 participants. Nutr Rev. 2023;
Umesawa M, Kobashi G. Epidemiology of hypertensive disorders in pregnancy: prevalence, risk factors, predictors and prognosis. Hyperten res: official j Japan Soc Hypert. 2017;40(3):213–20.
Sutan R, Aminuddin NA, Mahdy ZA. Prevalence, maternal characteristics, and birth outcomes of preeclampsia: a cross-sectional study in a single tertiary healthcare center in greater Kuala Lumpur Malaysia. Front Public Health. 2022;10:973271.
Bodnar LM, Ness RB, Markovic N, Roberts JM. The risk of preeclampsia rises with increasing prepregnancy body mass index. Ann Epidemiol. 2005;15(7):475–82.
Catalano PM, McIntyre HD, Cruickshank JK, McCance DR, Dyer AR, Metzger BE, et al. The hyperglycemia and adverse pregnancy outcome study: associations of GDM and obesity with pregnancy outcomes. Diabetes Care. 2012;35(4):780–6.
Perry A, Stephanou A, Rayman MP. Dietary factors that affect the risk of pre-eclampsia. BMJ nutrit prevent health. 2022;5(1):118–33.
Martini D, Godos J, Bonaccio M, Vitaglione P, Grosso G. Ultra-processed foods and nutritional dietary profile: a Meta-analysis of nationally representative samples. Nutrients. 2021;13(10)
Maldonado-Pereira L, Barnaba C, de Los CG, Medina-Meza IG. Evaluation of the nutritional quality of ultra-processed foods (ready to eat + fast food): fatty acids, sugar, and sodium. J Food Sci. 2022;87(8):3659–76.
Monguchi T, Hara T, Hasokawa M, Nakajima H, Mori K, Toh R, et al. Excessive intake of trans fatty acid accelerates atherosclerosis through promoting inflammation and oxidative stress in a mouse model of hyperlipidemia. J Cardiol. 2017;70(2):121–7.
Ma X, Nan F, Liang H, Shu P, Fan X, Song X, et al. Excessive intake of sugar: an accomplice of inflammation. Front Immunol. 2022;13:988481.
Wojcik M, Krawczyk M, Zieleniak A, Mac Marcjanek K, Wozniak LA. Chapter 14 - associations of high blood sugar with oxidative stress and inflammation in patients with type 2 diabetes. In: Preuss HG, Bagchi D, editors. Dietary Sugar Salt and Fat in Human Health. Academic Press; 2020. p. 305–23.
Chapter Google Scholar
Chiarello DI, Abad C, Rojas D, Toledo F, Vázquez CM, Mate A, et al. Oxidative stress: Normal pregnancy versus preeclampsia. Biochim Biophys Acta (BBA)-Mol Basis Dis. 2020;1866(2):165354.
Harmon AC, Cornelius DC, Amaral LM, Faulkner JL, Cunningham MW, Jr., Wallace K, et al. The role of inflammation in the pathology of preeclampsia. Clinical science (London, England : 1979). 2016;130(6):409–19.
Patik JC, Lennon SL, Farquhar WB, Edwards DG. Mechanisms of dietary sodium-induced impairments in Endothelial function and potential countermeasures. Nutrients. 2021;13(1)
Shuto E, Taketani Y, Tanaka R, Harada N, Isshiki M, Sato M, et al. Dietary phosphorus acutely impairs endothelial function. J Am Soc Nephrol: JASN. 2009;20(7):1504–12.
Lopez-Garcia E, Schulze MB, Meigs JB, Manson JE, Rifai N, Stampfer MJ, et al. Consumption of trans fatty acids is related to plasma biomarkers of inflammation and Endothelial Dysfunction1. J Nutr. 2005;135(3):562–6.
Lamarca B. Endothelial dysfunction. An important mediator in the pathophysiology of hypertension during pre-eclampsia. Minerva Ginecol 2012;64(4):309–20.
Fernandes AE, Rosa PWL, Melo ME, Martins RCR, Santin FGO, Moura AMSH, et al. Differences in the gut microbiota of women according to ultra-processed food consumption. Nutr Metab Cardiovasc Dis. 2023;33(1):84–9. https://doi.org/10.1016/j.numecd.2022.09.025 . Epub 2022 Oct 11.
Whelan K, Bancil AS, Lindsay JO, Chassaing B. Ultra-processed foods and food additives in gut health and disease. Nat Rev Gastroenterol Hepatol. 2024;22:1–22.
Fan M, Li X, Gao X, Dong L, Xin G, Chen L, et al. LPS induces preeclampsia-like phenotype in rats and HTR8/SVneo cells dysfunction through TLR4/p38 MAPK pathway. Front Physiol. 2019;10:1030.
Jin J, Gao L, Zou X, Zhang Y, Zheng Z, Zhang X, et al. Gut Dysbiosis promotes preeclampsia by regulating macrophages and trophoblasts. Circ Res. 2022;131(6):492–506.
Kell DB, Kenny LC. A dormant microbial component in the development of preeclampsia. Front Med. 2016;3:60.
Rauber F, Chang K, Vamos EP, da Costa Louzada ML, Monteiro CA, Millett C, et al. Ultra-processed food consumption and risk of obesity: a prospective cohort study of UK biobank. Eur J Nutr. 2021;60(4):2169–80.
Wondmkun YT. Obesity, insulin resistance, and type 2 diabetes: associations and therapeutic implications. Diabet metab syndrome obes: targets therapy. 2020;13:3611–6.
Teran E, Escudero C, Moya W, Flores M, Vallance P, Lopez-Jaramillo P. Elevated C-reactive protein and pro-inflammatory cytokines in Andean women with pre-eclampsia. Int J Gynecol Obstet. 2001;75(3):243–9.
Palei AC, Spradley FT, Granger JP. Chronic hyperleptinemia results in the development of hypertension in pregnant rats. Am J Phys Regul Integr Comp Phys. 2015;308(10):R855–R61.
CAS Google Scholar
Olson KN, Redman LM, Sones JL. Obesity "complements" preeclampsia. Physiol Genom. 2019;51(3):73–6.
Wang X, Cheng Z. Cross-sectional studies: strengths, weaknesses, and recommendations. Chest. 2020;158(1 Supplement):S65–71.
Mozaffarian D, Ludwig DS. Dietary guidelines in the 21st century—a time for food. Jama. 2010;304(6):681–2.
Wang H, Li N, Chivese T, Werfalli M, Sun H, Yuen L, et al. IDF diabetes atlas: estimation of global and regional gestational diabetes mellitus prevalence for 2021 by International Association of Diabetes in pregnancy study Group's criteria. Diabetes Res Clin Pract. 2022;183:109050.
Kityo A, Lee SA. The intake of ultra-processed foods and prevalence of chronic kidney disease: the health examinees study. Nutrients. 2022;14(17)
Nardocci M, Leclerc B-S, Louzada M-L, Monteiro CA, Batal M, Moubarac J-C. Consumption of ultra-processed foods and obesity in Canada. Can J Public Health. 2019;110:4–14.
Rauber F, Louzada MLC, Steele EM, Millett C, Monteiro CA, Levy RB. Ultra-processed food consumption and chronic non-communicable diseases-related dietary nutrient profile in the UK (2008–2014). Nutrients. 2018;10(5):587.
Lavigne-Robichaud M, Moubarac J-C, Lantagne-Lopez S, Johnson-Down L, Batal M, Sidi EAL, et al. Diet quality indices in relation to metabolic syndrome in an indigenous Cree (Eeyouch) population in northern Québec. Canada Pub health nutrit. 2018;21(1):172–80.
Sun Y, Shen Z, Zhan Y, Wang Y, Ma S, Zhang S, et al. Effects of pre-pregnancy body mass index and gestational weight gain on maternal and infant complications. BMC pregnan childbirth. 2020;20(1):1–13.
Linder T, Eder A, Monod C, Rosicky I, Eppel D, Redling K, et al. Impact of prepregnancy overweight and obesity on treatment modality and pregnancy outcome in women with gestational diabetes mellitus. Front Endocrinol. 2022;13:799625.
Najafi F, Hasani J, Izadi N, Hashemi-Nazari S-S, Namvar Z, Shamsi H, et al. Risk of gestational diabetes mellitus by pre-pregnancy body mass index: a systematic review and meta-analysis. Diabet Metab Syndrome: Clin Res Rev. 2021;15(4):102181.
McIntyre HD, Catalano P, Zhang C, Desoye G, Mathiesen ER, Damm P. Gestational diabetes mellitus. Nat Rev Dis Primers. 2019;5(1):47.
Plows JF, Stanley JL, Baker PN, Reynolds CM, Vickers MH. The pathophysiology of gestational diabetes mellitus. Int J Mol Sci. 2018;19(11):3342.
Stanhope KL. Sugar consumption, metabolic disease and obesity: the state of the controversy. Crit Rev Clin Lab Sci. 2016;53(1):52–67.
Bhattacharyya S, I OS, Katyal S, Unterman T, Tobacman JK. Exposure to the common food additive carrageenan leads to glucose intolerance, insulin resistance and inhibition of insulin signalling in HepG2 cells and C57BL/6J mice. Diabetologia. 2012;55(1):194–203.
Quetglas-Llabrés MM, Monserrat-Mesquida M, Bouzas C, Mateos D, Ugarriza L, Gómez C, et al. Oxidative stress and inflammatory biomarkers are related to high intake of ultra-processed food in old adults with metabolic syndrome. Antioxidants (Basel, Switzerland). 2023;12(8).
Yaribeygi H, Sathyapalan T, Atkin SL, Sahebkar A. Molecular mechanisms linking oxidative stress and diabetes mellitus. Oxidative Med Cell Longev. 2020;2020:8609213.
Bertoli S, Leone A, Battezzati A. Human bisphenol a exposure and the “diabesity phenotype”. Dose-Response. 2015;13(3):1559325815599173.
Rolfo A, Nuzzo AM, De Amicis R, Moretti L, Bertoli S, Leone A. Fetal–maternal exposure to endocrine disruptors: correlation with diet intake and pregnancy outcomes. Nutrients. 2020;12(6):1744.
Lorenzo PI, Martín-Montalvo A, Cobo Vuilleumier N, Gauthier BR. Molecular modelling of islet β-cell adaptation to inflammation in pregnancy and gestational diabetes mellitus. Int J Mol Sci. 2019;20(24)
Christ A, Lauterbach M, Latz E. Western diet and the immune system: an inflammatory connection. Immunity. 2019;51(5):794–811.
Neale E, Batterham M, Tapsell LC. Consumption of a healthy dietary pattern results in significant reductions in C-reactive protein levels in adults: a meta-analysis. Nutr Res. 2016;36(5):391–401.
Liu Z, Lu Y, Zhong K, Wang C, Xu X. The associations between endocrine disrupting chemicals and markers of inflammation and immune responses: a systematic review and meta-analysis. Ecotoxicol Environ Saf. 2022;234:113382.
Node K, Inoue T. Postprandial hyperglycemia as an etiological factor in vascular failure. Cardiovasc Diabetol. 2009;8:23.
Hu Z, Tylavsky FA, Kocak M, Fowke JH, Han JC, Davis RL, et al. Effects of maternal dietary patterns during pregnancy on early childhood growth trajectories and obesity risk: the CANDLE study. Nutrients. 2020;12(2)
Wang Y, Wang K, Du M, Khandpur N, Rossato SL, Lo C-H, et al. Maternal consumption of ultra-processed foods and subsequent risk of offspring overweight or obesity: results from three prospective cohort studies. Bmj. 2022:379.
Paula WO, Gonçalves VSS, Patriota ESO, Franceschini SCC, Pizato N. Impact of ultra-processed food consumption on quality of diet among Brazilian pregnant women assisted in primary health care. Int J Environ Res Public Health. 2023;20(2)
Crume TL, Brinton JT, Shapiro A, Kaar J, Glueck DH, Siega-Riz AM, et al. Maternal dietary intake during pregnancy and offspring body composition: the healthy start study. Am J Obstet Gynecol. 2016;215(5):609–e1-e8.
Article PubMed Central Google Scholar
Wan Y, Chen Y, Wu X, Yin A, Tian F, Zhang H, et al. Mediation effect of maternal triglyceride and fasting glucose level on the relationship between maternal overweight/ obesity and fetal growth: a prospective cohort study. BMC Pregnancy and Childbirth. 2023;23(1):449.
Akbari Z, Mansourian M, Kelishadi R. Relationship of the intake of different food groups by pregnant mothers with the birth weight and gestational age: need for public and individual educational programs. J educ health promot. 2015;4:23.
Fischer S, Morales-Suárez-Varela M. The bidirectional relationship between gestational diabetes and depression in pregnant women: a systematic search and review. Healthcare (Basel, Switzerland). 2023;11(3).
Khan R, Waqas A, Bilal A, Mustehsan ZH, Omar J, Rahman A. Association of Maternal depression with diet: a systematic review. Asian J Psychiatr. 2020;52:102098.
Ancira-Moreno M, O'Neill MS, Rivera-Dommarco J, Batis C, Rodríguez Ramírez S, Sánchez BN, et al. Dietary patterns and diet quality during pregnancy and low birthweight: the PRINCESA cohort. Matern Child Nutr. 2020;16(3):e12972.
Download references
Acknowledgments
Author information, authors and affiliations.
Students’ Scientific Research Center (SSRC), Tehran University of Medical Sciences, Tehran, Iran
Sepide Talebi
Department of Clinical Nutrition, School of Nutritional Sciences and Dietetics, Tehran University of Medical Sciences, Tehran, Iran
Food Security Research Center, Isfahan University of Medical Sciences, Isfahan, Iran
Sanaz Mehrabani
Department of Nutrition, School of Public Health, Iran University of Medical Sciences, Tehran, Iran
Seyed Mojtaba Ghoreishy
Student research committee, School of Public Health, Iran University of Medical Sciences, Tehran, Iran
Department of Health and Human Performance, Marymount University, Arlington, VA, USA
Alexei Wong
Department of Clinical Sciences, Faculty of Veterinary Medicine, Razi University, Kermanshah, Iran
Aliasghar Moghaddam & Peyman Rahimi Feyli
General Practitioner, Kermanshah University of Medical Sciences (KUMS), Kermanshah, Iran
Parsa Amirian & Mahsa Zarpoosh
Clinical Tuberculosis and Epidemiology Research Center, National Research Institute of Tuberculosis and Lung Diseases (NRITLD), Masih Daneshvari Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Mohammad Ali Hojjati Kermani
Department of Nutrition and Food Sciences, Research Center for Evidence-Based Health Management, Maragheh University of Medical Sciences, Maragheh, Iran
Sajjad Moradi
You can also search for this author in PubMed Google Scholar
Contributions
SM and ST designed this study. SM, MZ and PA contributed to the conduct of the search. SM and ST performed the statistical analysis and interpreted the results. SM, SM-GH, Sanaz Merabani, and MA-HK wrote the initial manuscript. AW, AM and PR_F critically revised the manuscript and contributed to the subsequent drafts of the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Correspondence to Sajjad Moradi .
Ethics declarations
Ethics approval and consent to participate.
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., supplementary material 4., supplementary material 5., supplementary material 6., supplementary material 7., supplementary material 8., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Talebi, S., Mehrabani, S., Ghoreishy, S.M. et al. The association between ultra-processed food and common pregnancy adverse outcomes: a dose-response systematic review and meta-analysis. BMC Pregnancy Childbirth 24 , 369 (2024). https://doi.org/10.1186/s12884-024-06489-w
Download citation
Received : 18 January 2024
Accepted : 07 April 2024
Published : 15 May 2024
DOI : https://doi.org/10.1186/s12884-024-06489-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Ultra-processed foods
- Gestational diabetes mellitus
- Preeclampsia
- Preterm birth
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Risk Factors
- Providing Care
- Living with Diabetes
- Clinical Guidance
- DSMES for Health Care Providers
- Prevent Type 2 Diabetes: Talking to Your Patients About Lifestyle Change
- Employers and Insurers
- Community-based Organizations (CBOs)
- Toolkits for Diabetes Educators and Community Health Workers
- National Diabetes Statistics Report
- Reports and Publications
- Current Research Projects
- National Diabetes Prevention Program
- State, Local, and National Partner Diabetes Programs for Public Health
- Diabetes Self-Management Education and Support (DSMES) Toolkit
Diabetes Articles
Explore this collection of articles created for people with diabetes or who are at risk for diabetes, and their families and friends. You'll learn about the basics of self-care, when education makes a big difference, and signs and symptoms to watch out for.
Diabetes is a chronic disease that affects how your body turns food into energy. About 1 in 10 Americans has diabetes.
For Everyone
Health care providers, public health.

Apple Cider Vinegar For Diabetes, Benefits, Risk and Uses
Table of Contents
Have you ever wondered is apple cider vinegar good for diabetes? Is apple vinegar the magical weapon that will help you win the war against this chronic condition? It is not a surprise to see apple cider vinegar for diabetes being recommended for many years because of its unique health properties and recent studies show that it may aid in the management of diabetes. The fermented potion, made from crunched apples, has gained acceptance for its ability to regulate blood sugar levels, improve insulin sensitivity and promote weight loss, all vital issues to manage diabetes.

With the growing number of people suffering from diabetes worldwide, it is vital to look into natural and inexpensive remedies. Apple Cider Vinegar is paving the way for research, presenting an exciting option, showing that it can impede glucose absorption, cut off blood sugar highs after meals, and also assist in controlling both type 1 and type 2 diabetes.
In this article, we will discover the possible advantages of apple cider vinegar to manage diabetes such as regulating blood sugar levels, improving insulin sensitivity and aiding in weight loss. It will also talk about the risks and side effects and will give you some practical tips on how to include apple cider vinegar in your diabetes management plan.
What is Apple Cider Vinegar?
Apple cider vinegar is a vinegar made from the fermentation of apple juice. It is produced through a two-step fermentation process: first, the apple juice is turned to alcohol and then acetic acid bacteria convert the alcohol into acetic acid. This process is responsible for producing the distinctive sour taste and pungent smell of the vinegar.
Also Read: Smart Eating with Diabetes: Benefits Of Chickpeas
What does the Research Say?
Although the research on Apple Cider Vinegar For Diabetes is still scarce, some studies have already shown encouraging results. A small study published in the Journal of Functional Foods showed that drinking apple cider vinegar before bed can regulate blood sugar levels in the morning. A recent study in the journal Diabetes Care showed that an intake of 20 mL of apple cider vinegar diluted in water and sweetened with saccharin may lower blood sugar after meals. Here are the benefits of ACV based on research:
Benefits of Apple Cider Vinegar for Diabetes
1. Helps to Manage Blood Sugar Levels
Blood sugar management is an important factor for people with diabetes. Apple cider vinegar is believed to be useful for the management of diabetes through its role of inhibiting the rate at which the body absorbs glucose from food. Among the array of health benefits, a research article published in the Journal of Functional Foods found apple cider vinegar mixed with a high-carbohydrate meal might decrease blood sugar levels remarkably compared to if one just takes the meal alone.
2. Helps Manage Type 1 Diabetes
Type 1 diabetes is an autoimmune disease where the body’s immune system specifically targets and destroys cells in the pancreas which produce insulin. Insulin therapy is lifesaving for people who have type 2 diabetes, but the ACV may provide some extra advantages. Research published in the journal Diabetes Care showed that consuming two tablespoons of apple cider vinegar was able to lower hyperglycemia (high blood sugar levels) after meals in individuals with type 1 diabetes.
Also Read: Discover the Amazing Fenugreek Seeds Benefits
3. Helps to Manage Obesity
Obesity is considered a major determinant of type 2 diabetes. Apple Cider Vinegar For Diabetes could help in weight management by making you feel full, increasing the metabolism, and maybe even reducing the amount of fat that is stored in your body. A research paper in the Journal of Functional Foods indicated that taking apple cider vinegar as a supplement may result in slight weight loss and better body composition.
4. Improves Insulin Sensitivity
Insulin resistance is the main issue that leads to the type 2 diabetes disease. Apple cider vinegar, likely to improve insulin sensitivity, might help the body to use insulin more efficiently to regulate blood sugar levels. Research published in the journal Diabetes Care showed that the combination of apple cider vinegar with a high-carbohydrate meal could increase insulin sensitivity in people with insulin resistance or type 2 diabetes.
5. Supports Heart Health
Individuals with diabetes develop cardiovascular diseases more often. Apple cider vinegar could be a boon for cardiovascular health as it is also known to improve levels of cholesterol and reduce inflammation. A paper that was published in the Journal of Functional Foods showed that consuming apple cider vinegar could help lower triglyceride levels and increase HDL (good) cholesterol levels.
Also Read: 10 Amazing Avocado (Butter Fruit) Benefits For Good Health
Potential Risks and Side Effects of Consuming ACV for Diabetic Patients
While Apple Cider Vinegar For Diabetes is generally considered safe when consumed in moderation, there are a few potential risks and side effects to be aware of:
1. Tooth Enamel Erosion
Apple cider vinegar is an acid, and taking it in undiluted or large quantities form might gradually destroy the tooth enamel.
2. Throat Irritation
The acidity of apple cider vinegar may lead to throat irritation or discomfort, especially when it is consumed undiluted.
3. Interaction with Medications
Apple cider vinegar can cause drug interactions with some types of medications, including insulin, diuretics, or potassium-lowering drugs. It is crucial to have a doctor’s advice before making apple cider vinegar part of your diabetes treatment plan.
4. Low Potassium Levels
The consumption of a lot of apple cider vinegar can lead to the lowering of potassium levels, which can be dangerous for diabetics who are already at risk of potassium deficiency.
How to Use Apple Cider Vinegar for Diabetes?
Consumption of Apple Cider Vinegar for Diabetes Methods:
1. Dilute It
For the sake of minimizing the risks and side effects, dilute the apple cider vinegar by mixing it with water or any other non-acidic liquid. One of the most common advice is to blend 1-2 tablespoons of apple cider vinegar with 8 ounces of water.
2. Time It Right
It is better to take apple cider vinegar before or after meals for the best results. This could lead to slow down the absorption of glucose and thus reduce blood sugar spikes following the meal.
3. Start Small
Initially, start with small doses (for example, a teaspoon) of apple cider vinegar if you are new to its consumption and gradually increase as tolerated.
Also Read: Benefits Of Coconut Water That You Need To Know
Recipes and Ideas
Apple cider vinegar can be incorporated into different recipes and drinks to make it more acceptable. Here are a few ideas:
1. Apple Cider Vinegar Tonic
Blend 1-2 tablespoons of apple cider vinegar with 8 oz of lukewarm water and 1 tsp of honey or stevia (optional) to make a soothing drink.
2. Salad Dressing
Stir apple cider vinegar, olive oil, Dijon mustard, and your favourite herbs and spices together to make a tangy salad dressing.
3. Marinades and Sauces
Include apple cider vinegar in every marinade for meats, vegetables, or sauces for extra flavour and the possible regulating benefits of blood sugar.
4. Beverages
In a small amount add apple cider vinegar to iced tea, lemonade, or sparkling water for a flavorful and fresh drink.
Also Read: 10 Amazing Spinach Benefits For A Healthy Heart And Eyes
In conclusion, while more research is required to completely understand the potential of using Apple Cider Vinegar For Diabetes, the available findings indicate that it is beneficial for diabetes management even at an early stage. Incorporating unmodified apple cider vinegar into your diet is recommended but you must consult with a health care provider before use. This may help with your diabetes management.
Nevertheless, it is essential to note that apple cider vinegar must not be used as a replacement for prescribed medications or a healthy lifestyle. Incorporating apple cider vinegar into your diet should also be supplemented with a doctor’s advice just like in the case of any dietary supplement or natural remedy, especially if you have some ongoing health condition or are taking any drugs.
Disclaimer: The content of this article is compiled information from generic and public sources. It is in no way a substitute, suggestion, or advice for a qualified medical opinion. Always consult a specialist or your own doctor for more information. BeatoApp does not claim responsibility for this information.
Throw out your non-verified glucometer and try the BeatO clinically approved smart glucometer kit. Check your blood sugar level instantly. Try out the BeatO diabetes care program for a more organized healthcare routine.
How useful was this post?
Click on a star to rate it!
Average rating 5 / 5. Vote count: 1
No votes so far! Be the first to rate this post.
We are sorry that this post was not useful for you!
Let us improve this post!
Tell us how we can improve this post?

Mohd Aasif Ahmad
15 lemon juice benefits for your health you should know now, height weight chart for male and female according to age, leave a reply cancel reply.
Save my name, email, and website in this browser for the next time I comment.
Are Markups Driving the Ups and Downs of Inflation?

Download PDF (158 KB)
FRBSF Economic Letter 2024-12 | May 13, 2024
How much impact have price markups for goods and services had on the recent surge and the subsequent decline of inflation? Since 2021, markups have risen substantially in a few industries such as motor vehicles and petroleum. However, aggregate markups—which are more relevant for overall inflation—have generally remained flat, in line with previous economic recoveries over the past three decades. These patterns suggest that markup fluctuations have not been a main driver of the ups and downs of inflation during the post-pandemic recovery.
In the recovery from the pandemic, U.S. inflation surged to a peak of over 7% in June 2022 and has since declined to 2.7% in March 2024, as measured by the 12-month change in the personal consumption expenditures (PCE) price index. What factors have been driving the ups and downs of inflation? Production costs are traditionally considered a main contributor, particularly costs stemming from fluctuations in demand for and supply of goods and services. As demand for their products rises, companies need to hire more workers and buy more intermediate goods, pushing up production costs. Supply chain disruptions can also push up the cost of production. Firms may pass on all or part of the cost increases to consumers by raising prices. Thus, an important theoretical linkage runs from cost increases to inflation. Likewise, decreases in costs should lead to disinflation.
Labor costs are an important factor of production costs and are often useful for gauging inflationary pressures. However, during the post-pandemic surge in inflation, nominal wages rose more slowly than prices, such that real labor costs were falling until early 2023. By contrast, disruptions to global supply chains pushed up intermediate goods costs, contributing to the surge in inflation (see, for example, Liu and Nguyen 2023). However, supply chains have more direct impacts on goods inflation than on services inflation, which also rose substantially.
In this Economic Letter , we consider another factor that might drive inflation fluctuations: changes in firms’ pricing power and markups. An increase in pricing power would be reflected in price-cost markups, leading to higher inflation; likewise, a decline in pricing power and markups could alleviate inflation pressures. We use industry-level measures of markups to trace their evolving impact on inflation during the current expansion. We find that markups rose substantially in some sectors, such as the motor vehicles industry. However, the aggregate markup across all sectors of the economy, which is more relevant for inflation, has stayed essentially flat during the post-pandemic recovery. This is broadly in line with patterns during previous business cycle recoveries. Overall, our analysis suggests that fluctuations in markups were not a main driver of the post-pandemic surge in inflation, nor of the recent disinflation that started in mid-2022.
Potential drivers of inflation: Production costs and markups
To support households and businesses during the pandemic, the Federal Reserve lowered the federal funds rate target to essentially zero, and the federal government provided large fiscal transfers and increased unemployment benefits. These policies boosted demand for goods and services, especially as the economy recovered from the depth of the pandemic.
The increase in overall demand, combined with supply shortages, boosted the costs of production, contributing to the surge in inflation during the post-pandemic recovery. Although labor costs account for a large part of firms’ total production costs, real labor costs were falling between early 2021 and mid-2022 such that the increases in prices outpaced those in nominal wages. This makes it unlikely that labor costs were driving the surge in inflation.
Instead, we focus on another potential alternative driver of inflation that resulted from firms’ ability to adjust prices, known as pricing power. As demand for goods surged early in the post-pandemic recovery, companies may have had a greater ability to raise their prices above their production costs, a gap known as markups. Following a sharp drop in spending at the height of the pandemic, people may have become eager to resume normal spending patterns and hence more tolerant to price increases than in the past. In fact, growth of nonfinancial corporate profits accelerated in the early part of the recovery (see Figure 1), suggesting that companies had increased pricing power. Some studies have pointed to the strong growth in nonfinancial corporate profits in 2021 as evidence that increased markups have contributed to inflation (see, for example, Weber and Wasmer 2023). However, the figure also shows that growth in corporate profits is typically volatile. Corporate profits tend to rise in the early stages of economic recoveries. Data for the current recovery show that the increase in corporate profits is not particularly pronounced compared with previous recoveries.
Figure 1 Profit growth for nonfinancial businesses
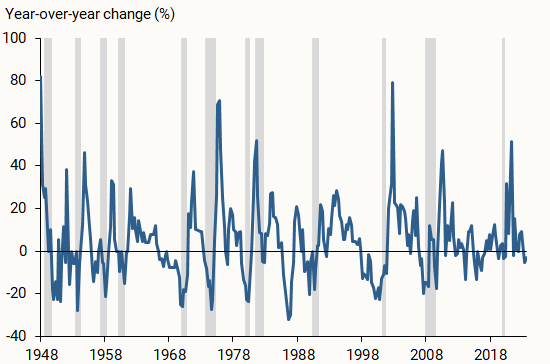
More importantly, corporate profits are an imperfect measure of a firm’s pricing power because several other factors can drive changes in profitability. For instance, much of the recent rise in corporate profits can be attributed to lower business taxes and higher subsidies from pandemic-related government support, as well as lower net interest payments due to monetary policy accommodation (Pallazzo 2023).
Instead of relying on profits as a measure of pricing power, we construct direct measures of markups based on standard economic models. Theory suggests that companies set prices as a markup over variable production costs, and that markup can be inferred from the share of a firm’s revenue spent on a given variable production factor, such as labor or intermediate goods. Over the period of data we use, we assume that the specific proportion of a company’s production costs going toward inputs does not change. If the share of a firm’s revenue used for inputs falls, it would imply a rise in the firm’s price-cost margin or markup. In our main analysis, we use industry-level data from the Bureau of Economic Analysis (BEA) to compute markups based on the share of revenue spent on intermediate inputs. Our results are similar if we instead use the share of revenue going toward labor costs.
We compare the evolution of markups to that of prices, as measured by the PCE price index, since the recovery from the pandemic. In constructing this price index, the BEA takes into account changes in product characteristics (for instance, size) that could otherwise bias the inflation measure by comparing the prices of inherently different products over time. Similarly, based upon standard economic theory, our markup measure implicitly captures changes in those characteristics (see, for example, Aghion et al. 2023).
The post-pandemic evolution of markups
We examine the evolution of markups in each industry since the third quarter of 2020, the start of the post-pandemic recovery. Figure 2 shows that some sectors, such as the motor vehicles and petroleum industries, experienced large cumulative increases in markups during the recovery. Markups also rose substantially in general merchandise, such as department stores, and for other services, such as repair and maintenance, personal care, and laundry services. Since the start of the expansion, markups in those industries rose by over 10%—comparable in size to the cumulative increases over the same period in the core PCE price index, which excludes volatile food and energy components. However, the surge in inflation through June 2022 was broad based, with prices also rising substantially outside of these sectors. Thus, understanding the importance of markups for driving inflation requires a macroeconomic perspective that examines the evolution of aggregate markups across all sectors of the economy.
Figure 2 Cumulative changes in markups for salient industries
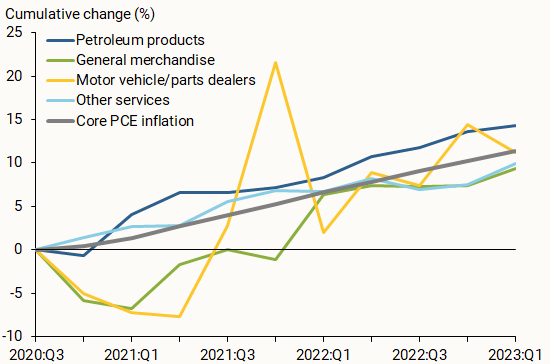
The role of aggregate markups in the economy
To assess how much markup changes contribute to movements in inflation more broadly, we use our industry-level measurements to calculate an aggregate markup at the macroeconomic level. We aggregate the cumulative changes in industry markups, applying two different weighting methods, as displayed in Figure 3. In the first method (green line), we match our industry categories to the spending categories in the core PCE price index for ease of comparison; we then use the PCE weights for each category to compute the aggregate markup. Alternatively, we use each industry’s cost weights to compute the aggregate markup (blue line). Regardless of the weighting method, Figure 3 shows that aggregate markups have stayed essentially flat since the start of the recovery, while the core PCE price index (gray line) rose by more than 10%. Thus, changes in markups are not likely to be the main driver of inflation during the recovery, which aligns with results from Glover, Mustre-del-Río, and von Ende-Becker (2023) and Hornstein (2023) using different methodologies or data. Markups also have not played much of a role in the slowing of inflation since the summer of 2022.
Figure 3 Cumulative changes in aggregate markups and prices
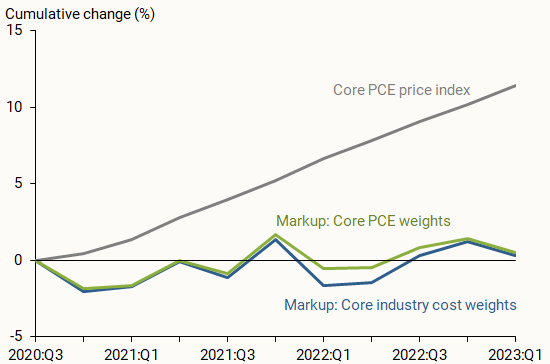
Moreover, the path of aggregate markups over the past three years is not unusual compared with previous recoveries. Figure 4 shows the cumulative changes in aggregate markups since the start of the current recovery (dark blue line), alongside aggregate markups following the 1991 (green line), 2001 (yellow line), and 2008 (light blue line) recessions. Aggregate markups have stayed roughly constant throughout all four recoveries.
Figure 4 Cumulative changes of aggregate markups in recoveries
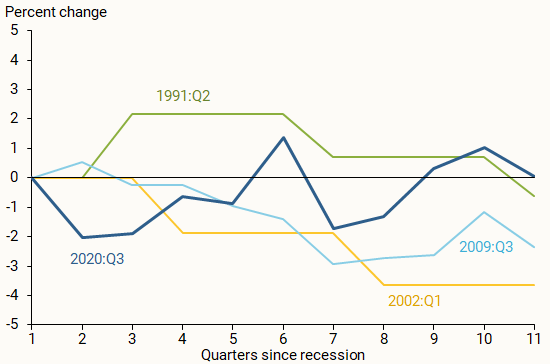
Firms’ pricing power may change over time, resulting in markup fluctuations. In this Letter , we examine whether increases in markups played an important role during the inflation surge between early 2021 and mid-2022 and if declines in markups have contributed to disinflation since then. Using industry-level data, we show that markups did rise substantially in a few important sectors, such as motor vehicles and petroleum products. However, aggregate markups—the more relevant measure for overall inflation—have stayed essentially flat since the start of the recovery. As such, rising markups have not been a main driver of the recent surge and subsequent decline in inflation during the current recovery.
Aghion, Philippe, Antonin Bergeaud, Timo Boppart, Peter J. Klenow, and Huiyu Li. 2023. “A Theory of Falling Growth and Rising Rents.” Review of Economic Studies 90(6), pp.2,675-2,702.
Glover, Andrew, José Mustre-del-Río, and Alice von Ende-Becker. 2023. “ How Much Have Record Corporate Profits Contributed to Recent Inflation? ” FRB Kansas City Economic Review 108(1).
Hornstein, Andreas. 2023. “ Profits and Inflation in the Time of Covid .” FRB Richmond Economic Brief 23-38 (November).
Liu, Zheng, and Thuy Lan Nguyen. 2023. “ Global Supply Chain Pressures and U.S. Inflation .” FRBSF Economic Letter 2023-14 (June 20).
Palazzo, Berardino. 2023. “ Corporate Profits in the Aftermath of COVID-19 .” FEDS Notes , Federal Reserve Board of Governors, September 8.
Weber, Isabella M. and Evan Wasner. 2023. “Sellers’ Inflation, Profits and Conflict: Why Can Large Firms Hike Prices in an Emergency?” Review of Keynesian Economics 11(2), pp. 183-213.
Opinions expressed in FRBSF Economic Letter do not necessarily reflect the views of the management of the Federal Reserve Bank of San Francisco or of the Board of Governors of the Federal Reserve System. This publication is edited by Anita Todd and Karen Barnes. Permission to reprint portions of articles or whole articles must be obtained in writing. Please send editorial comments and requests for reprint permission to [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.15(4); 2023 Apr
- PMC10230119

Knowledge and Awareness About Diabetes Mellitus Among Urban and Rural Population Attending a Tertiary Care Hospital in Haryana
Dr.lalit kumar.
1 Internal Medicine, Adesh Medical College and Hospital, Shahbad, Kurukshetra, IND
Rahul Mittal
Akhil bhalla.
2 Pain Medicine, Adesh Medical College and Hospital, Shahbad, Kurukshetra, IND
Ashwani Kumar
Hritik madan, kushagra pandhi.
3 Pharmacy, Adesh Institute of Pharmacy and Biomedical Sciences, Adesh University, Bathinda, IND
Kamaldeep Singh
4 Internal Medicine, Jawaharlal Nehru Medical College, Chandigarh, IND
5 Emergency Medicine, All India Institute of Medical Sciences, New Delhi, New Delhi, IND
Background: Diabetes mellitus (DM) is one of the fastest-growing public health problems in the twenty-first century. The ignorance among people about their disease may be related to their low socioeconomic status and lack of quality education available to them about the disease. It is a serious condition leading to several complications if the individual does not follow up regularly for check-ups and blood sugar monitoring. Lifestyle modifications such as a healthy diet, regular exercise, reducing weight, stress management, and smoking cessation can play a critical role in managing diabetes and improving the health and well-being of diabetic patients. Thus, through this study, we want to assess and create awareness among diabetic patients.
Methodology: It is a hospital-based cross-sectional study conducted at a tertiary care hospital on diagnosed cases of DM. The patients aged 18 years or above of either gender who had already been diagnosed with DM type 1 and type 2 were included, and patients with gestational DM were excluded from the study. Informed consent was taken from the patients, and all the required details were obtained using a well-structured questionnaire. After obtaining all the answers, the level of knowledge and awareness was analyzed, and the data was entered into an MS Excel sheet (Microsoft, Redmond, Washington) and analyzed by Statistical Package for the Social Sciences (SPSS) version 22.0 (IBM Corp., Armonk, NY).
Results: In our study, the maximum prevalence of diabetes was seen in males (55.5%) than females (44.5%), and the mean age of our study population was 53.3 ± 16.4 years. In our study, participants from rural areas made up the majority (59%) compared to those from urban areas (41%), and the majority of participants had a high school education. Among 211 diabetics, about 84%, 79%, and 41% of the patients knew about diabetes, symptoms of diabetes, and complication of diabetes. Only 18% of the patients were aware of the symptoms of hypoglycemia, and 38% of the patients possess their own glucometers and monitor their blood sugar levels on a regular basis. Merely 38% of the diabetics were aware of the various DM treatment choices. About 52% of patients had some awareness of insulin therapy. Out of 211 patients, about half skipped their antidiabetic prescriptions, and of those, 22% took a double dose the next day. A total of 121 patients (57%) combined the use of alternative and allopathic medications, and among these, 22% of patients had replaced the allopathic with alternative medicines. Almost 53% of patients had a positive family history of diabetes; 54% of patients believe that obesity is unrelated to diabetes, and 79% of diabetics are aware of the lifestyle changes that must be done for diabetes. Almost 67% of the patients believed that diabetes could be permanently treated, and 84% of patients believed that eating too much sugar caused their diabetes.
Conclusion: In our study, a significant number of patients suffering from diabetes had less knowledge and awareness about it. The prevalence of myths about the onset of diabetes was noticeably higher among diabetic patients. It was observed that a greater number of patients were shifting to alternative medications instead of allopathic ones, and in the long run, it can lead to various complications. Therefore, there is an immediate need to promote awareness about diabetes among the general population.
Introduction
Diabetes mellitus (DM) is one of the fastest-growing public health problems in the twenty-first century. According to the International Diabetes Federation (IDF) 10th edition, the prevalence of diabetes is 537 million in 2021, and it will exponentially rise to 643 million by 2030 and 783 million by 2045, out of which 50% of cases (i.e., one in two adults with diabetes) remain undiagnosed [ 1 ]. It was seen in a study that India ranks second, while China ranks first in the global diabetes epidemic [ 2 ]. India will have a prevalence of about 79.4 million diabetic cases by the year 2030 [ 3 ]. Many people (around 45%) remain undiagnosed for years and are later diagnosed as a case of type 2 DM [ 1 ].
The ignorance among people about their disease process may be related to their low socioeconomic status and lack of quality education available to them about the disease. Some people come to know about their disease once it has led to various complications like retinopathy, nephropathy, and neuropathy. Therefore, increasing awareness and education of people about the disease may help people to control their blood sugar levels and prevent its complications [ 4 ].
Diabetes is a serious condition leading to several complications if the individual does not follow up regularly for check-ups and blood sugar monitoring [ 5 ]. There are various treatment options available for diabetes such as insulin injections or insulin pumps in conjunction with continuous glucose monitoring technology for type 1 diabetes and oral hypoglycemic drugs for type 2 diabetes [ 6 ]. Lifestyle modifications such as a healthy diet, regular exercise, reducing weight, stress management, and smoking cessation can play a critical role in managing diabetes and improving the health and well-being of diabetic patients [ 7 ].
The aim of this study is to create awareness and knowledge about DM and its complications. The objectives of this study are to assess the awareness and knowledge about the disease, its complications, treatment preferences, lifestyle modifications, and self-monitoring of glucose among diabetic patients.
The rationale of this study was that most people in Haryana lack literacy and that diabetes is a significant non-communicable disease that affects a large number of people. It is the need of the hour to raise awareness about diabetes as the incidence of diabetes is increasing nowadays even in the younger age group.
Materials and methods
It was a hospital-based cross-sectional study on already diagnosed cases of DM. The study was conducted in Adesh Medical College and Hospital, Shahbad, over a period of two months from August 15, 2022, to October 15, 2022, with a sample size of 211 (duration based). The study was conducted after due approval from Institutional Ethics Committee for Biomedical and Health Research (IEC-BHR), Adesh Medical College and Hospital, Shahabad, Haryana, vide reference number AMCH/IEC-BHR/2022/08/01. The patients, aged 18 years or above of either gender, who had already been diagnosed with DM type 1 and type 2 were included, and the patients with gestational DM were excluded from the study.
Patients were included in the study after obtaining informed consent from them. A structured questionnaire was provided to the patients for obtaining demographic details like name, age, sex, occupation, education, and area of residence. It also had basic questions regarding knowledge and awareness of DM. Questions were interpreted by the interviewer to the patients, and forms were filled out according to the answers given by those patients. The form was in English language and interpreted by the interviewer in the local language (Hindi) to those who could not understand or read English. After obtaining all the answers, the level of knowledge and awareness was analyzed. All the data collected were kept confidential. The data were entered into an MS Excel sheet (Microsoft, Redmond, Washington) and analyzed by the Statistical Package for the Social Sciences (SPSS®) version 22.0 (IBM Corp., Armonk, NY). Categorical data were represented as percentages and frequencies. The mean age of diabetes was calculated in terms of mean ± standard deviation.
Demographic characteristics
The majority of our study sample, 51 patients (24%) who have an average age of 53.3 ± 16.4 years, falls within the age range of 51-60 years as shown in Table Table1, 1 , while patients above 60 years of age made up 37.4% of the population and patients under 50 years of age made up 38.4%.
In our study, the maximum prevalence of diabetes was seen in males (55.5%) than in females (44.5%) as shown in underlying Table Table2. 2 . As a result, males are more susceptible to disease than females.
In our study, participants from rural areas made up the majority (59%) compared to those from urban areas (41%) as shown in Table Table3. 3 . Therefore, the rural population has more inclination toward DM than the urban population.
About 32% of patients, or the majority, had high school education; 27% of the patients completed middle school, whereas one-fourth (25%) of our study population was illiterate as shown in Table Table4. 4 . Only 16% were educated to the graduation level.
About 84% of the 211 diabetic individuals were aware that having diabetes indicated having higher blood sugar levels as shown in Table Table5, 5 , and 79% of patients were aware of the symptoms of DM, including frequent urination, increased thirst, persistent hunger, and unexpected weight loss. About 41% of patients were aware of diabetes-related complications, which include blurred vision, nerve damage, renal damage, and various issues with foot and oral health. Only 18% of the patients were aware of the symptoms of hypoglycemia.
DM: Diabetes mellitus.
Only 38% of the 211 patients possess their own glucometers and monitor their blood sugar levels on a regular basis, yet Table Table6 6 reveals that 57% of those patients are unaware of typical fasting and postprandial blood sugar levels.
Merely 38% of the 211 diabetics were aware of the various DM treatment choices and duration of treatment as indicated in Table Table7. About 7 . About 52% of the patients knew something about the insulin injections available for the treatment of diabetes.
Out of 211 patients, approximately half (49%) skipped their antidiabetic prescriptions, and of those, approximately half (22%) took a double dose the next day. About 121 patients (57%) combined the use of alternative medications along with allopathic medications, and of these 121 patients, 26 patients (22%) had replaced the allopathic medications with alternative medicines as indicated in Table Table8 8 .
As shown in Table Table9, 9 , almost 53% of patients had a positive family history of diabetes. About 54% of patients think that obesity and diabetes are unrelated, and although 79% of diabetics are aware of the lifestyle adjustments required to control their illness, they have not been able to incorporate these changes into their daily routines.
The majority of patients, nearly 67%, thought that diabetes could be cured permanently. Table Table10 10 shows that 84% of patients thought that having diabetes was due to eating too much sugar.
DM, simply called diabetes, is a serious, long-term (or “chronic”) condition that is characterized by raised blood glucose levels because the body cannot produce any or enough of the hormone insulin or cannot effectively use the insulin it produces [ 1 ]. The typical symptoms are excessive thirst, frequent urination, lack of energy or fatigue, constant hunger, sudden weight loss, and blurred vision [ 1 ]. In our study, around 79% of the patients knew these symptoms of diabetes, and about 84% of patients answered that diabetes means raised blood glucose levels. The mean age of our study population was 53 ± 16 years, and the maximum number of patients in the age interval of 51-60 years is 24%. Age is one of the risk factors for the development of diabetes, and age ≥ 60 years is an independent risk factor for diabetes-related complications despite good control of cardiovascular risk factors [ 8 ]. In our study, 79 patients (37%) were aged above 60 years. Therefore, diabetes is more prevalent among the elderly, and similar data is seen in previous studies [ 9 , 10 ]. Another key risk factor for DM is a positive family history of diabetes. It is crucial to understand that people with a family history of diabetes are more knowledgeable about the signs and symptoms of the disease as well as the organs impacted by it than people without such a history. In a study conducted in 2017, it was found that in contrast to persons with negative family histories of DM, they experienced early-onset diabetes and were more likely to experience complications [ 11 ]. In our study, 53% of individuals were found to have a positive family history of DM out of which 26.4% of patients had knowledge and awareness about diabetes.
Obesity, particularly central obesity, is significantly linked to the onset and progression of type 2 diabetes. In a prior study, patients with type 2 DM had rates of overall obesity, abdominal obesity, and central obesity of 58.68%, 81.84%, and 53.42%, respectively [ 12 ]. About 46% of participants in our study were aware of the link between diabetes and obesity. As insulin sensitivity declines in fatty tissues, regulation of beta cell function also declines [ 13 , 14 ]. Increased levels of nonesterified fatty acids (NEFA), glycerol, hormones, cytokines, and pro-inflammatory chemicals in an obese person cause the development of insulin resistance [ 13 ].
The diagnosis of DM is made according to the criteria given by the American Diabetes Association (ADA) [ 15 ]. A 2020 meta-analysis by Dessie et al. found that a glucometer is significantly associated with higher medication adherence [ 16 ]. In our study, only 38% of the patients own a glucometer of their own and keep a check on their blood glucose levels on a regular basis, and 57% of patients do not even know about normal fasting and postprandial blood sugar levels.
In order to treat type 1 diabetes, the traditional method involves checking blood glucose levels manually, followed by daily subcutaneous insulin injections [ 17 ]. It has been demonstrated that using insulin pumps in conjunction with continuous glucose monitoring (CGM) technology lowers the long-term risks of diabetic complications [ 6 ]. Gene therapy is a novel approach to treating the disease, which offers a promising substitute for insulin injections since it tries to repair defective genes responsible for disease progression and thus prevents or reverses the development of the disease [ 17 , 18 ]. Particularly for type 1 DM, stem cell-based therapy has been viewed as a promising possible therapeutic approach for the management of diabetes [ 17 , 19 ]. For the treatment of type 2 DM, a variety of non-insulin-based oral treatments are available, including biguanides, insulin secretagogues, SGLT2 inhibitors, insulin sensitizers, etc. [ 20 ]. In our study, among 211 diabetics, only 38% of the patients were aware of the various treatment options for DM and duration of treatment, whereas about 52% of the patients had some awareness and knowledge about insulin therapy.
A study conducted by Benil et al. in 2003 showed that if a patient forgets to take the prior dose, almost 10% of patients had taken a double dose the next day. However, in our study, about half of the patients missed their antidiabetic medications out of which about 22% of them had taken a double dose on the next day. Also, 57% of patients used alternative medications along with allopathic medications, and 22% of them had replaced allopathic medications completely with alternative medications [ 21 ].
Human pluripotent stem cells are an appealing alternative beta cell source for transplantation. Beta cell replacement through islet of Langerhans transplantation is a potential treatment for DM, but the lack of donors prevents its widespread use [ 22 , 23 ]. The benefit upon transplantation is sometimes insufficient, and the transcript causes the functional ability to fall to 60% at 12 months [ 23 , 24 ]. Another suitable limitation that restricts its use is its pocket-draining expenses. After transplantation, the persistence of autoimmunity leads to a lifelong need for immunosuppression, which is a major drawback.
The most significant risk factors for the development of diabetes complications appear to be poor glycemic control and a protracted illness [ 25 ]. Diabetes complications affect almost every organ system. Diabetes complications fall into two categories, namely, microvascular and macrovascular. Microvascular issues include diabetic nephropathy, neuropathy, and retinopathy, whereas macrovascular complications include coronary artery disease, stroke, and peripheral vascular disease (PVD) leading to bruises and injuries which do not heal leading to gangrene and ultimately amputation [ 5 ]. One of the main barriers to restoring adequate metabolic control of the disease is hypoglycemia, which is the most prevalent acute complication in type 1 diabetes patients. In our study, about 41% of the patients were aware of the complications of DM. Only 18% of the patients were aware of the symptoms of hypoglycemia, i.e., fainting, tremors, convulsions, excessive hunger, etc.
A total of 3,200 participants in the National Diabetes Prevention Program (NDPP) of the United States were randomized to receive standard medical care, metformin therapy, or comprehensive lifestyle intervention. In order to attain a mean objective of 7% weight loss, the lifestyle intervention concentrated on reducing caloric intake by reducing fat calories and increasing physical activity to a goal of at least 150 min/per week [ 26 ]. The incidence of type 2 diabetes was shown to have decreased by 58% in the lifestyle intervention group, 31% in the metformin group, and 17% in the routine care group after an average of 2.8 years; thus, lifestyle modifications, i.e., exercise, dietary modifications, and smoking and alcohol cessation, play a major preventable therapy to reduce the disease burden [ 27 ]. In our study, around 22% of patients were still unaware of the beneficial and preventive effects of lifestyle modifications.
The majority of the patients believed the misconception that eating more sugar caused diabetes. In our study, 67% of people believe that diabetes can be cured permanently. Other beliefs about diabetes include the notions that it only develops in old age, that bathing your feet in water will help you manage your blood sugar, and that it is caused by your previous misdeeds and can only be treated spiritually [ 28 ]. Our study did not ask for any such specific beliefs; hence, there is no data for the same.
There could be several limitations of this study, which could have affected the final outcome. First, the study had highly heterogenous data in regard to the literacy, economic standards, and level of education of the participants involved. The fact that both type I and type II DM were included in the selection process could have a certain effect on the results. There is a possibility of reporting bias as this study was more focused on the knowledge and awareness among participants and not involved in an intervention-based approach. Although these limitations might have some indirect effect on the results, albeit having an insignificant effect on the objectives and final outcome of this study.
Conclusions
In our study, a significant number of patients suffering from diabetes had less knowledge and awareness about diabetes. The prevalence of myths like diabetes will be permanently cured after taking medications for some time and eating too much sugar causes diabetes was noticeably higher among diabetic patients. It was observed that a greater number of patients were shifting to alternative medications instead of allopathic ones, and in the long run, it can lead to more severe microvascular and macrovascular complications. There is an immediate need to promote awareness about diabetes among the general population with the help of community-based campaigns, collaborations with local media outlets, partnerships with healthcare providers, and optimal use of social media platforms. The stress should be made on early diagnosis and proper management, which are keys to preventing or delaying complications and improving the quality of life for patients with diabetes.
Questionnaire
Name: Age/Sex:
Education: Occupation:
Area of Residence: Rural/Urban
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study. Institutional Ethics Committee for Biomedical and Health Research (IEC-BHR), Adesh Medical College and Hospital issued approval AMCH/IEC-BHR/2022/08/01. The plan was approved for carrying out the study.
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.

IMAGES
VIDEO
COMMENTS
Summary and Conclusion. Diabetes is a multifactorial disease process, and its long-term management requires the active involvement of people with diabetes and their families, as well as a large multidisciplinary care team to ensure optimal health, quality of life, and productivity. Keeping up with new medications, emerging technology, and ...
Biomedical research continues to provide new insights in our understanding of the mechanism of diabetes development that is reviewed here. Recent studies may provide tools for the use of several genes as targets for risk assessment, therapeutic strategies and prediction of complications. ... CONCLUSION. Diabetes mellitus is the epidemic of the ...
Type-2 diabetes is a major, non-communicable disease with increasing prevalence at a global level. ... In conclusion, effective lifestyle modifications including counseling on weight loss, adoption of a healthy dietary pattern like the Mediterranean diet, together with physical activity are the cornerstone in the prevention of type-2 diabetes ...
I. Introduction. Diabetes mellitus, a metabolic disease defined by elevated fasting blood glucose levels due to insufficient insulin production, has reached epidemic proportions worldwide (World Health Organization, 2020).Type 1 and type 2 diabetes (T1D and T2D, respectively) make up the majority of diabetes cases with T1D characterized by autoimmune destruction of the insulin-producing ...
The research articles from 1990 onwards, a total of 111 studies were reviewed for the present study, a deep illustration about the inclusion and exclusion of studies is given in Fig. 1. Download : Download high-res image ... will be improved and can be used as used to predict cumulative risk associated with diabetes. 19. Conclusion ...
Conclusion. The rising pattern of sedentary lifestyle and the higher incidence of obesity has contributed to an ever-increasing number of patients with diabetes, generating a massive demand for anti-diabetic medication and prompting companies to invest more on research and development for developing targeted formulations.
A similar conclusion can be reached about whether there is a core tissue defect at the organismal level ... As articulated in a classic essay by McGarry , ... Accili D. Insulin action research and the future of diabetes treatment: The 2017 Banting Medal for Scientific Achievement lecture. Diabetes. 2018;67:1701-9.
Diabetes mellitus (DM) is commonest endocrine disorder that affects more than 100 million people. worldwide (6% po pulation). It is caused b y deficiency or ineffective production of insulin by ...
A systematic examination of scholarly literature found 42 papers on diabetes and its worldwide costs of illness (COI). Asia paid 50% of sickness publication costs, while Europe and the US spent 25% apiece. ... In conclusion, this systematic review has significantly advanced our understanding of the global economic impact of type 2 diabetes ...
requires insulin injections for survival) and type 2 diabetes (where the body cannot properly use the insulin it produces), separate global estimates of diabetes prevalence for type 1 and type 2 do not exist. The majority of people with diabetes are affected by type 2 diabetes. This used to occur nearly entirely among adults, but
diabetes research and clinical practice 143 (2018) 101 - 112 105 modulate caloric intake or loss (GLP-1RAs, SGLT2b' s) [31,40] . Successful outcomes of some GLP-1RA and SGLT2b CVO Ts
Diabetes mellitus is a significant global public health challenge, with a rising prevalence and associated morbidity and mortality. Cell therapy has evolved over time and holds great potential in diabetes treatment. In the present review, we discussed the recent progresses in cell-based therapies for diabetes that provides an overview of islet and stem cell transplantation technologies used in ...
The research could lead to a better availability of beta cells for future research purposes. Type 1 and type 2 diabetes results when beta cells in the pancreas fail to produce enough insulin, the ...
Introduction. Diabetes mellitus (DM) is probably one of the oldest diseases known to man. It was first reported in Egyptian manuscript about 3000 years ago. 1 In 1936, the distinction between type 1 and type 2 DM was clearly made. 2 Type 2 DM was first described as a component of metabolic syndrome in 1988. 3 Type 2 DM (formerly known as non-insulin dependent DM) is the most common form of DM ...
Aim This bibliometric analysis aims to evaluate the characteristics and impact of the top 100 cited articles published under the title of diabetes mellitus. Metods We performed to define the most cited articles in diabetes research by using the Web of Science. The papers were analyzed in terms of their year of publication, journal of publication, authors, impact factor (IF), total citations ...
Summary and Conclusion. The worldwide diabetes epidemic has created an unsustainable financial and personal crisis for health care systems and for patients and their families. At the same time, the ability of patients to maintain useful vision has never been greater. Screening of people who are at risk and timely institution of treatment ...
Diabetes"5 and "Conquer Diabetes".6 One of the main goals of USDHHS's report, Healthy People 2010, is to improve the quality of life for persons with diabetes.7 Taking control of diabetes to improve quality of life has put the spotlight on the need for additional support and education for patients with type 2 diabetes.
357 Diabetes Essay Topics & Examples. Updated: Feb 25th, 2024. 25 min. When you write about the science behind nutrition, heart diseases, and alternative medicine, checking titles for diabetes research papers can be quite beneficial. Below, our experts have gathered original ideas and examples for the task.
Introduction. Diabetes is one of the major challenges for healthcare systems worldwide. In 2021, approximately 537 million adults were found to live with diabetes worldwide and 6.7 million people died from diabetes (International Diabetes Federation, 2021).According to previous research, approximately 97.5% of adults with diabetes have at least one chronic condition, and as many as 88.5% have ...
Given the increasing incidence of negative outcomes during pregnancy, our research team conducted a dose-response systematic review and meta-analysis to investigate the relationship between ultra-processed foods (UPFs) consumption and common adverse pregnancy outcomes including gestational diabetes mellitus (GDM), preeclampsia (PE), preterm birth (PTB), low birth weight (LBW), and small for ...
The Indian Council of Medical Research (ICMR) - India DIABetes (ICMR-INDIAB) study has reported diabetes prevalence in 15 of the 31 states/union territories of India completed and published to date. ... For example, one review paper identified Short Form -12 and Appraisal of Diabetes Scale as ideal and feasible tools for QoL assessment in busy ...
Overview. Explore this collection of articles created for people with diabetes or who are at risk for diabetes, and their families and friends. You'll learn about the basics of self-care, when education makes a big difference, and signs and symptoms to watch out for. Series of articles about diabetes - how to manage, complications, and how to ...
According to the Public Health Agency of Canada, between. 2003 -2004 and 2013-2014, there was a relative increase of 37.3% of diagnosed. diabetes cases, from 5.6% to 7.8% in Canada. The prime ...
A research paper in the Journal of Functional Foods indicated that taking apple cider vinegar as a supplement may result in slight weight loss and better body composition. 4. Improves Insulin Sensitivity. Insulin resistance is the main issue that leads to the type 2 diabetes disease.
Conclusion. Firms' pricing power may change over time, resulting in markup fluctuations. In this Letter, we examine whether increases in markups played an important role during the inflation surge between early 2021 and mid-2022 and if declines in markups have contributed to disinflation since then. Using industry-level data, we show that ...
as 592 million. Diabetes is a disease caused due to the increase level of blood. glucose. This h igh blood glucose produces the symptoms of frequent urination, increased thirst, and increased ...
Introduction. Diabetes mellitus (DM) is one of the fastest-growing public health problems in the twenty-first century. According to the International Diabetes Federation (IDF) 10th edition, the prevalence of diabetes is 537 million in 2021, and it will exponentially rise to 643 million by 2030 and 783 million by 2045, out of which 50% of cases (i.e., one in two adults with diabetes) remain ...