Volume 27, Number 6—June 2021

Perspective
Reflections on 40 years of aids.
Cite This Article
June 2021 marks the 40th anniversary of the first description of AIDS. On the 30th anniversary, we defined priorities as improving use of existing interventions, clarifying optimal use of HIV testing and antiretroviral therapy for prevention and treatment, continuing research, and ensuring sustainability of the response. Despite scientific and programmatic progress, the end of AIDS is not in sight. Other major epidemics over the past decade have included Ebola, arbovirus infections, and coronavirus disease (COVID-19). A benchmark against which to compare other global interventions is the HIV/AIDS response in terms of funding, coordination, and solidarity. Lessons from Ebola and HIV/AIDS are pertinent to the COVID-19 response. The fifth decade of AIDS will have to position HIV/AIDS in the context of enhanced preparedness and capacity to respond to other potential pandemics and transnational health threats.
“When the history of AIDS and the global response is written, our most precious contribution may well be that, at a time of plague, we did not flee, we did not hide, we did not separate ourselves.”
—Jonathan Mann, Founding Director of Project SIDA and the World Health Organization Global Programme on AIDS, 1998
Forty years ago, on June 5, 1981, the Centers for Disease Control’s Morbidity and Mortality Weekly Report described 5 cases of Pneumocystis pneumonia in gay men ( 1 ). That report heralded the HIV/AIDS pandemic, which has resulted in over 75 million HIV infections and 32 million deaths. In 2011, we reviewed 30 years of AIDS and commented that the HIV/AIDS response would be a benchmark against which responses to other health threats would be compared ( 2 ). After 40 years of AIDS, we present our personal reflections on scientific and global health evolution over the fourth decade of AIDS in a world that has recently suffered other major epidemics. We focus on biomedical advances because these have had the greatest effect on HIV transmission and disease; advances in structural and behavioral interventions are reviewed in the CDC Compendium of Evidence-Based Interventions and Best Practices for HIV Prevention ( 3 ).
After the initial MMWR report was published, it took 2–3 years for the cause of AIDS, the novel retrovirus designated HIV, to be identified ( 4 , 5 ), and many more years to uncover its simian origin ( 6 ). Because of the asymptomatic spread of HIV, the long incubation period before disease, and transmission through sex and blood, millions of persons around the world, including several hundred thousand in the United States, were infected by the time the first AIDS cases were reported. The epidemiology and natural history of HIV infection, combining elements of acute and chronic diseases, ensured a diverse and long-lasting pandemic.
The history of HIV/AIDS and the struggle to contain it have seen the best and worst of human nature. Frequent examples of discrimination and exclusion are contrasted by leadership, illustrated by community activists ( 7 ), Jonathan Mann molding the first global response ( 8 ), Kofi Annan rallying the United Nations behind the search for a global fund ( 9 ), and President George W. Bush committing United States generosity to a war on HIV/AIDS of uncertain duration ( 10 ). Despite continued instances of injustice, the story has overall been a positive one, providing lessons for how to respond to other epidemic and pandemic threats.
Evolving Epidemiology
The Joint United Nations Programme on HIV/AIDS (UNAIDS) estimates that in 2019, 38 million persons worldwide were living with HIV, 1.7 million became newly infected, and 690,000 died with HIV disease ( 11 ). Compared with 2010 estimates, overall HIV incidence in 2019 decreased by 23% and mortality by 37%. However, age stratification shows that new infections have decreased by 52% among children but by only 13% among adults. With reduced mortality rates yet continued HIV incidence and population growth, the overall number of persons living with HIV was 24% greater in 2019 than in 2010.
Global summaries hide regional differences. The epicenter of the pandemic remains in East and southern Africa, which account for 54% of all HIV-infected persons and 43% of incident HIV infections and deaths ( 11 ). High prevalence of HIV-infected persons with unsuppressed viremia predicts high incidence and maintenance of community infection, an observation that applies to regions and countries, as well as specific populations such as men who have sex with men (MSM).
The next greatest HIV burden is in the Asia and Pacific region, where the population is vastly greater than that of East and southern Africa but there are 3.5 times fewer HIV-infected persons ( 11 ). Despite overall prevention progress, HIV incidence has not declined equally everywhere; little success has been seen in eastern Europe, the Middle East, and Central Asia.
Ever clearer is the global burden of HIV in key populations: MSM, transgender persons, people who inject drugs, sex workers and their clients, and incarcerated persons. In 2019, an estimated 62% of all new HIV infections were in members of those key populations ( 11 ). In 7 of the 8 UNAIDS regions, key populations accounted for 60%–99% of incident HIV infections; only in East and southern Africa, where the proportion was 28%, were new infections predominant in general populations ( 11 ).
Among high-income nations, the most heavily affected country is still the United States. In 2018, a total of 37,881 HIV infections were newly reported, with regional differences ( 12 ). In the South, the rate of new infections was more than twice that for the Midwest, where the rate was the lowest. Major disparities by race/ethnicity persist; the rate among Black/African American persons is 2 times that among Hispanic and 8 times that among White persons. Also associated with higher rates are factors indicating social deprivation and poverty, even allowing for racial and ethnic disparities. Among new HIV infections, 70% resulted from male-to-male sex. A cause for concern is potential overlap between the HIV/AIDS and opioid epidemics through increased drug injection and needle sharing, which has resulted in explosive HIV outbreaks ( 13 ).
Evolving Science and Program
In our 2011 commentary ( 2 ), we considered the following as priorities: improving use of existing interventions, defining how best to use HIV testing and antiretroviral therapy (ART) for prevention as well as treatment, continuing the quest for new knowledge and interventions, and ensuring sustainability of the global response. By and large, progress has been made on all fronts.
After the CAPRISA 004 trial of precoital and postcoital use of tenofovir gel was published in 2010 ( 14 ), the Ring ( 15 ) and Aspire ( 16 ) studies (randomized, placebo-controlled trials in South Africa) examined the protective efficacy of a self-inserted vaginal ring impregnated with slow-release dapivirine, a nonnucleoside reverse transcription inhibitor. The overall efficacy rates for reducing HIV incidence were 31% (Ring) and 27% (Aspire); many questions about overall efficacy, adherence, and differences by age remained. This collective experience provided proof of concept for woman-controlled prevention but did not provide the definitive public health solution to high HIV incidence among young women in Africa.
Four pivotal randomized trials ( 17 – 20 ) of oral preexposure prophylaxis (PrEP) with Truvada (combination of tenofovir and emtricitabine) were pivotal for international licensing of the compound. The relevant trials studied MSM, transgender women having sex with men, and at-risk heterosexual persons. A review of evidence considered another 9 studies, some of tenofovir alone, in different populations including people who inject drugs ( 21 ). The pivotal trials showed reduced HIV incidence (44%–86%) with Truvada use. However, a consistent observation has been a strong association between efficacy and adherence; PrEP is effective, but the drugs need to be taken.
Subsequent research focused on differential tissue penetration of drugs to relevant anatomic sites in men and women and on modes of drug delivery. HIV Prevention Trials Network (HPTN) studies compared the prevention efficacy of the long-acting injectable drug cabotegravir with Truvada in men and transgender women who have sex with men (study 083 [ 22 ]) and in heterosexual women (study 084 [ 23 ]). Interim results showed that cabotegravir, delivered every 8 weeks by injection, was associated with 66% lower incidence than oral Truvada in study 083 and 89% less in study 084. The long half-life of cabotegravir enables intermittent dosing, but waning drug levels over time may become subtherapeutic, thus requiring additional interventions to prevent infection and preclude development of drug resistance.
In its 2016 guidelines, the World Health Organization (WHO) recommended public health use of PrEP, as have other national and international regulatory or advisory bodies. However, the enthusiasm engendered by PreP science needs to be tempered by consideration of cost, need for rigorous adherence, rising rates of other sexually transmitted infections and thus need for continued condom use, and contraception for women. Long-acting injectables could be a major advance, but accessibility and logistics for their delivery need to be considered.
Mathematical modeling and ecologic studies suggested that greatly increased delivery of ART could reduce HIV transmission at the community level. The definitive study showing that ART provided prevention benefits was the landmark HPTN 052 study ( 24 ), published in interim form in 2011. This trial among discordant couples found a 96% reduction in HIV transmission among those who started ART early versus those for whom it was deferred. Combined with an influential modeling study ( 25 ) that suggested that regular HIV testing and immediate use of ART could suppress and perhaps ultimately eliminate HIV transmission, the results of HPTN 052 led to studies in East and southern Africa of the so-called test and treat intervention ( 26 – 29 ). These studies were community randomized evaluations of widespread HIV testing and immediate ART compared with standard care; the primary endpoint was HIV incidence. These large, expensive implementation science studies yielded rich information but did not lead to local HIV elimination. Of the 4 studies, 2 showed no significant incidence reduction and the other 2 showed 20%–30% reduction.
One of the reasons for the unexpectedly modest differences in HIV incidence between intervention and control communities in the test and treat study was changing global practice with regard to when to start ART. In 2015, results of the START ( 30 ) and TEMPRANO ( 31 ) trials showed unequivocally that immediate ART, irrespective of CD4+ lymphocyte count, resulted in reduced HIV-associated disease and death, ending more than 2 decades of argument about when to start treatment. WHO rapidly changed global recommendations to immediately start ART, one result of which was erosion of differences between intervention and control communities in the test and treat trials.
Although test and treat did not reduce HIV incidence to the extent hoped for, the accumulated evidence supports the notion of early, universal ART for extending the lives of HIV-positive persons as well as reducing the prevalence of unsuppressed viremia, the driver of HIV transmission. Large observational studies ( 32 ) showed that persons with suppressed viremia do not transmit the virus sexually, leading to the slogan “U = U”—undetectable equals untransmittable. This experience provides a much more compelling argument for active HIV case finding through increased HIV testing and partner notification, to enhance individual and public health through early treatment.
Although none of the approaches described provides a unique solution, the combination of widespread HIV testing, early ART for those infected, and PrEP for those at risk offers opportunity for substantially limiting the epidemic. Such approaches have been associated with reductions in new HIV infections among MSM in London, UK ( 33 ), and in New South Wales, Australia ( 34 ). In the United States, these advances—testing, case finding including through partner notification, universal treatment, PrEP, and rapid molecular investigation of clusters for service provision—have been incorporated into a revised national strategy for HIV elimination ( 35 ).
Progress toward an HIV vaccine remains discouraging. The only report of protective efficacy, published in 2009, has been the RV-144 study in Thailand ( 36 ), which investigated use of a recombinant canarypox vector vaccine (ALVAC-HIV) delivered in 4 monthly priming injections followed by a recombinant glycoprotein 120 subunit vaccine (AIDSVAX B/E) given in 2 additional injections. Reported efficacy was 26%–31%, but statistical and technical interpretation of these results was controversial ( 37 ). In 2016, the HVTN 702 study was launched in South Africa and used the same product as in the Thailand trial but modified for the dominant subtype C. After interim analysis, the study was halted for futility in early 2020 ( 38 ). Other efficacy studies of vaccines based on so-called mosaic immunogens from diverse HIV subtypes are in progress.
There has been great interest in broadly neutralizing antibodies to HIV, which some infected persons produce naturally and which might protect against a wide variety of strains. Two international trials of infusions with a broadly neutralizing antibody, VRC01, every 8 weeks showed relative protection against sensitive strains but no significantly reduced HIV incidence overall ( 39 ).
In 2014, UNAIDS launched its 90:90:90 initiative, aiming for 90% of persons with HIV infection to be diagnosed, 90% of those with an HIV diagnosis to receive ART, and 90% of those receiving treatment to show viral suppression by 2020. Globally, the respective proportions in 2019 were 81%, 82%, and 88%, so that an estimated 59% of persons living with HIV were showing viral suppression. Initially, 90:90:90 (with a goal of these numbers being 95s by 2030) was an advocacy proposal rather than an evidence-based initiative, but these targets have become adopted as policy promising “epidemic control,” itself a concept requiring precise definition ( 40 ).
ART scale-up, increased male circumcision, and prevention of mother-to-child transmission have all contributed to encouraging advances in the most heavily affected regions of Africa ( 11 , 41 , 42 ). Successful program implementation and declines in new HIV infections and deaths, combined with scientific progress, have led to a certain complacency that “AIDS is over.” Former US Secretary of State Hillary Clinton and staff promoted the idea that current tools could abruptly halt the epidemic. We largely agree with the 2018 judgment of the International AIDS Society–Lancet Commission on AIDS: “The HIV/AIDS community made a serious error by pursuing ‘the end of AIDS’ message” ( 43 ). Key populations, hiding in obscurity as well as in plain sight, will probably remain as reservoirs, even with highly performing programs. Experience in East and southern Africa has highlighted the challenge of adequate service provision to youth and men. Stigma and discrimination remain barriers in many parts of the world, and lack of an HIV cure (a priority research area) and vaccine remain scientific obstacles ( 44 ).
Evolving Global Health
The HIV/AIDS pandemic has evolved in parallel with other global health events that necessarily influence how HIV/AIDS is perceived and prioritized. In a 2012 paper, author K.D.C. suggested that global health trends could best be analyzed through the lenses of development, public health, and health security ( 45 ). The fourth decade of AIDS started in the aftermath of the global financial crisis and the influenza (H1N1) pandemic and is finishing amid the coronavirus disease (COVID-19) pandemic. Although substantial progress has been made toward reducing maternal deaths, improving child survival rates, and scaling up programs for HIV/AIDS, malaria, and tuberculosis, the past decade has seen major disease outbreaks and a consequent focus on health security. Because of its sociodemographic effects, AIDS was portrayed as a security issue in United Nations discussions early in this century. With massive scale-up of treatment and prevention, HIV/AIDS is now perceived as another public health priority rather than a security emergency.
In 2014, Ebola was reported in Guinea, Liberia, and Sierra Leone, far west of previously recognized outbreaks. The epidemic lasted until mid-2016 and ultimately resulted in 28,646 reported cases and 11,323 deaths ( 46 ). Infections were exported to 3 other countries in Africa, several countries in Europe, and the United States. This health crisis resulted in widespread fear of possible global spread, unparalleled global mobilization of emergency health assistance including use of armed forces of the different high-income countries, and political involvement at the highest levels of governments and the United Nations. Subsequent outbreaks of Ebola have occurred in Uganda and the Democratic Republic of the Congo (DRC), including a large epidemic in conflict-ridden eastern DRC in 2018–2020 that resulted in 3,481 reported cases and 2,299 deaths ( 47 ). Underemphasized aspects of these Ebola epidemics were that cases over the past 6 years represent more than 90% of all cases reported cumulatively since recognition of Ebola in 1976; that vast geographic distances were involved; and that these outbreaks were largely urban, sometimes involving capital and other major cities. Ebola epidemiology has changed from that of an exotic, remote infection in Africa to one capable of causing extensive urban outbreaks threatening global health ( 48 ). Also of note was that field research conducted during the outbreaks under the most difficult conditions showed efficacy of a vaccine and therapeutics, both now considered the standard of care for Ebola ( 49 , 50 ).
Over the past decade, arboviral epidemic activity has been diverse. The epidemics of yellow fever in Angola and the DRC in 2015–2016 were the world’s largest over the past 30 years. A total of 965 cases and 400 deaths were reported, but true numbers were far greater. Over 30 million persons were vaccinated, and shortage of yellow fever vaccine required healthcare providers to resort to the untested practice of fractionating vaccine doses ( 51 ). Huge epidemics of chikungunya and dengue occurred internationally; virus was transmitted to areas previously considered at low risk, such as Europe ( 52 ). In 2015, the Zika epidemic raised global concern when infection with this virus was shown to be associated with microcephaly in infants and with Guillain-Barré syndrome and to be sexually transmissible. The outbreak resulted in at least 3,700 cases of birth defects in the Americas ( 53 ).
In 2005, after the outbreak of severe acute respiratory syndrome (SARS), WHO revised its International Health Regulations ( 54 ). A key change was authority to declare a Public Health Emergency of International Concern, a health emergency that could result in international spread or required coordinated action. WHO has implemented this authority only 6 times, 5 of them during the fourth decade of AIDS: for polio (2014), Ebola (2014 and 2019), Zika (2015), and COVID-19 (2019).
Related to health security are the interrelated challenges of global warming, demographic change, and migration. Climate change affects social and environmental determinants of health, such as access to clean air, water, shelter, and arable lands, but also exerts direct health effects. The United Nations High Commissioner for Refugees characterized 2010–2019 as “a decade of displacement,” during which 100 million persons were forced to flee their homes, many because of conflict such as that in the Middle East. During 2014–2020, some 20,000 migrants crossing the Mediterranean Sea to Europe drowned, and another 12,000 or more were unaccounted for.
Broad themes that have dominated global health discourse include the transition from the era of the Millennium Development Goals (MDGs; 2000–2015) to that of the broader Sustainable Development Goals (SDGs; 2015–2030) ( 55 ) and the issue of universal health coverage. Other disease-specific programs require continued support, such as the unfinished efforts to eradicate polio and Guinea worm disease. The MDGs had 3 specific health goals relating to child survival; maternal health; and HIV/AIDS, tuberculosis, and malaria. Only 1 of the 17 SDGs is devoted to health, SDG3, which has 13 targets and 28 indicators. Specifically, SDG3 calls for: “By 2030, end the epidemics of AIDS, tuberculosis, malaria and neglected tropical diseases and combat hepatitis, water-borne diseases and other communicable diseases.” Another target and WHO priority is provision of universal health coverage, global access to decent healthcare, and protection against penury from out-of-pocket health expenditures. HIV/AIDS exists in a crowded and complex global health space.
Preparing for the Fifth Decade of AIDS
As the world emerged from the financial crisis a decade ago, there was concern that HIV/AIDS funding might be constrained. Development assistance for health reached $40.6 billion in 2019, an increase of 15% over the amount in 2010 ( 56 ). Approximately half of this assistance goes to HIV/AIDS, especially for treatment, and to newborn, maternal, and child health. Thus, although health security has eclipsed health development and global public health in this fourth decade of AIDS, financial commitments have been largely maintained.
The overall annual spending on HIV/AIDS by low- and middle-income countries is ≈$20.2 billion, of which ≈$9.5 billion represents donor funding. UNAIDS consistently communicates that to meet SDG targets, overall spending on HIV/AIDS needs to increase by ≈40%. Nonetheless, this HIV-specific spending is privileged compared with funding for other high-impact diseases in low-income settings, such as malaria and tuberculosis. AIDS is no longer among the 10 leading causes of death globally and is now widely viewed as a medically manageable disease. HIV/AIDS prioritization and funding may be justified by the youthful groups affected and its lifelong nature, but this view may be increasingly challenged. Expecting the United States to pay indefinitely for most of the world’s HIV/AIDS response is unrealistic. The end of the SDG era in 2030 will probably come with reappraisal of global commitments, including those for global health funding, disease-specific focus, and maintenance of single-disease organizations such as UNAIDS. Over the coming years, HIV/AIDS programs need to show good fiscal management and epidemiologic results, and affected countries need to shoulder an increased share of their disease burdens.
Lessons from HIV/AIDS and Other Epidemics
The most dramatic epidemics in recent time (COVID-19 [ 57 ], Ebola, and HIV/AIDS) involve quite different biological agents and challenges yet also raise common themes and questions. Especially needed are global responses to challenges that transcend national borders. Pathogen emergence is enhanced by globalization, but globalized systems are needed to address an interconnected worldwide emergency. The slogan “no one is safe until everyone is safe” has been heard in relation to COVID-19, but it was said years ago about HIV. And global health needs global funding.
Individual leaders and organizations have performed valiant work on COVID-19, yet countries have isolated themselves in all senses, resulting in global fragmentation. Major powers look inward yet are reluctant to cede space, and the influence of multilateral agencies is limited. WHO was heavily criticized after the Ebola epidemic in West Africa but is constrained by restricted authority, inadequate funding, and unrealistic expectations from member states. Repeated calls for WHO reform are unclear about what is really wanted.
Honesty is required concerning preparedness and surveillance. The Ebola epidemic in West Africa became as severe as it did because the 3 affected countries had been neglected for years and had no functioning surveillance and public health infrastructure. We cannot say that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was completely unexpected; the literature on pandemic threats is voluminous. SARS in 2002–2003 was severe but not widespread; the 2009 influenza (H1N1) pandemic was widespread but not severe. It is hubristic to assume that pathogen severity and spread would always segregate, yet we were not prepared. Preparedness metrics can give false reassurance, witnessed by the lamentable response to COVID-19 in the United States in 2020. “Never again” was the mood after the Ebola epidemic in West Africa, but preparedness just seems too hard and costly. Perhaps true preparedness exists only in the military, where personnel train continuously for wars they hope will never happen.
As a result of technologic advances such as whole-genome sequencing, scientific progress on COVID-19 has been breathtakingly rapid compared with early laboratory research on HIV. We hope to not see a replay of the early history of ART, with scientific advances relating to COVID-19, and specifically vaccines, not being rapidly or equitably accessible everywhere. “Vaccine nationalism” is a new term raising the specter of lower risk groups in high-income countries receiving vaccine before, for example, frontline healthcare workers in low-income settings. Healthcare workers have been disproportionately affected by Ebola and COVID-19, highlighting the need for much greater investment in infection prevention and control in healthcare settings worldwide. Attention and innovation are required to ensure maintenance of HIV and other essential public health services amid other outbreaks such as COVID-19.
Although initially slow, the HIV/AIDS response over the years has been a beacon in global health for respect for individuals and their rights and for health equity. More reflection is required with regard to what the responses to HIV and Ebola have taught us and how they might be relevant to COVID-19 and other future epidemics.
Conclusions
Although great need remains, the past decade has seen scientific and programmatic successes with regard to the HIV/AIDS priorities we defined after 30 years of AIDS. Existing interventions have been scaled up, and new tools such as PrEP and long-lasting drug preparations have been introduced. The roles of HIV testing and ART for treatment and prevention have been clarified, and the need for immediate ART for all HIV-infected persons has been proven. The global HIV/AIDS response has been sustained, financing has been maintained, and the world has kept focus on the SDGs. Mann’s judgment that “we did not separate ourselves” remains justified. We must also accept that political promises of “the end of AIDS” were hyperbole that current epidemiology does not support.
The COVID-19 pandemic has exploited the fault lines of global systems and existing inequalities in a way that HIV did early on. Regrettably, the solidarity that HIV/AIDS engendered has not yet been carried over. In retrospect, the recent epidemics of Ebola in West Africa and DRC were preparation for the COVID-19 pandemic, but follow-through was lacking. The fifth decade of AIDS will take us to the SDG target date and reassessment of global health and development priorities. HIV/AIDS may not be central to global health discourse as it was earlier, but it will remain a yardstick by which to judge commitment and efforts, including, and especially in relation to, health security.
On February 7, 2021, the Ministry of Health of DRC reported a laboratory-confirmed case of Ebola in North Kivu Province, the most heavily affected province during the 2018–2020 outbreak in eastern Congo. The case-patient experienced symptom onset on January 25, 2021, and died in Butembo, a city of ≈1 million persons, on February 4, 2021. She was reportedly linked epidemiologically to an Ebola survivor, and genetic sequencing reportedly showed phylogenetic association with the earlier outbreak rather than a new spillover event. As of February 8, 2021, a total of 118 contacts were being investigated ( https://www.who.int/emergencies/diseases/ebola/ebola-2021-north-kivu , https://www.who.int/csr/don/10-february-2021-ebola-drc/en ).
Separately, on February 14, 2021, the Ministry of Health of the Republic of Guinea reported an outbreak of Ebola in the subprefecture of Gouécké, Nzérékoré Region, the first report of Ebola in Guinea since the 2014–2016 epidemic. The index case-patient, a nurse, experienced symptoms on January 18, 2021, and died on January 28, 2021. A total of 6 secondary Ebola cases were reported, 1 in a traditional practitioner who cared for the index case-patient and 5 in family members attending her subsequent funeral. Of the 7 case-patients, 5 died. As of February 15, 2021, a total of 192 contacts were being investigated, including in the capital city, Conakry ( https://www.who.int/emergencies/diseases/ebola/ebola-2021-nzerekore-guinea , https://www.who.int/csr/don/17-february-2021-ebola-gin/en ).
Dr. De Cock retired from CDC in December 2020. He had previously served as founding director of Projet RETRO-CI, Abidjan, Côte d’Ivoire; director of the CDC Division of HIV/AIDS Prevention, Surveillance and Epidemiology; director of the WHO Department of HIV/AIDS; founding director of the CDC Center for Global Health; and director, CDC Kenya.
- Centers for Disease Control (CDC) . Pneumocystis pneumonia—Los Angeles. MMWR Morb Mortal Wkly Rep . 1981 ; 30 : 250 – 2 . PubMed Google Scholar
- De Cock KM , Jaffe HW , Curran JW . Reflections on 30 years of AIDS. Emerg Infect Dis . 2011 ; 17 : 1044 – 8 . DOI PubMed Google Scholar
- Centers for Disease Control and Prevention . Compendium of evidence-based interventions and best practices for HIV prevention [ cited 2021 Apr 18 ]. https://www.cdc.gov/hiv/research/interventionresearch/compendium/index.html
- Barré-Sinoussi F , Chermann J-C , Rey F , Nugeyre MT , Chamaret S , Gruest J , et al. Isolation of a T-lymphotropic retrovirus from a patient at risk for acquired immune deficiency syndrome (AIDS). Science . 1983 ; 220 : 868 – 71 . DOI PubMed Google Scholar
- Popovic M , Sarngadharan MG , Read E , Gallo RC . Detection, isolation, and continuous production of cytopathic retroviruses (HTLV-III) from patients with AIDS and pre-AIDS. Science . 1984 ; 224 : 497 – 500 . DOI PubMed Google Scholar
- Hahn BH , Shaw GM , De Cock KM , Sharp PM . AIDS as a zoonosis: scientific and public health implications. Science . 2000 ; 287 : 607 – 14 . DOI PubMed Google Scholar
- France D . How to survive a plague: the inside story of how citizens and science tamed AIDS. New York: Alfred Knopf; 2016 .
- Merson M , Inrig S . The AIDS pandemic. Searching for a global response. 2018 . Cham (Switzerland); Springer International Publishing; 2018. p. 25–113.
- Piot P . No time to lose. A life in pursuit of deadly viruses. New York: W.W. Norton & Co.; 2012 . p. 316–34.
- Fauci AS , Eisinger RW . PEPFAR—15 years and counting the lives saved. N Engl J Med . 2018 ; 378 : 314 – 6 . DOI PubMed Google Scholar
- Joint United Nations Programme on HIV/AIDS . UNAIDS data 2020 [ cited 2021 Apr 18 ]. https://www.unaids.org/sites/default/files/media_asset/2020_aids-data-book_en.pdf
- Centers for Disease Control and Prevention . HIV surveillance report, 2018 (Preliminary); vol. 30 [ cited 2021 Mar 14 ]. https://www.cdc.gov/hiv/library/reports/hiv-surveillance.html
- Peters PJ , Pontones P , Hoover KW , Patel MR , Galang RR , Shields J , et al. ; Indiana HIV Outbreak Investigation Team . HIV infection linked to injection use of oxymorphone in Indiana, 2014–2015. N Engl J Med . 2016 ; 375 : 229 – 39 . DOI PubMed Google Scholar
- Abdool Karim Q , Abdool Karim SS , Frohlich JA , Grobler AC , Baxter C , Mansoor LE , et al. ; CAPRISA 004 Trial Group . Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science . 2010 ; 329 : 1168 – 74 . DOI PubMed Google Scholar
- Nel A , van Niekerk N , Kapiga S , Bekker L-G , Gama C , Gill K , et al. ; Ring Study Team . Safety and efficacy of a dapivirine vaginal ring for HIV prevention in women. N Engl J Med . 2016 ; 375 : 2133 – 43 . DOI PubMed Google Scholar
- Baeten JM , Palanee-Phillips T , Brown ER , Schwartz K , Soto-Torres LE , Govender V , et al. ; MTN-020–ASPIRE Study Team . Use of a vaginal ring containing dapivirine for HIV-1 prevention in women. N Engl J Med . 2016 ; 375 : 2121 – 32 . DOI PubMed Google Scholar
- Grant RM , Lama JR , Anderson PL , McMahan V , Liu AY , Vargas L , et al. ; iPrEx Study Team . Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med . 2010 ; 363 : 2587 – 99 . DOI PubMed Google Scholar
- Baeten JM , Donnell D , Ndase P , Mugo NR , Campbell JD , Wangisi J , et al. ; Partners PrEP Study Team . Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med . 2012 ; 367 : 399 – 410 . DOI PubMed Google Scholar
- McCormack S , Dunn DT , Desai M , Dolling DI , Gafos M , Gilson R , et al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet . 2016 ; 387 : 53 – 60 . DOI PubMed Google Scholar
- Molina J-M , Capitant C , Spire B , Pialoux G , Cotte L , Charreau I , et al. ; ANRS IPERGAY Study Group . On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med . 2015 ; 373 : 2237 – 46 . DOI PubMed Google Scholar
- National Institute for Health and Care Excellence . Pre-exposure prophylaxis of HIV in adults at high risk: Truvada (emtricitabine/tenofovir disoproxil). Evidence summary. [ESNM78] [ cited 2021 Mar 14 ]. https://www.nice.org.uk/advice/esnm78/chapter/full-evidence-summary
- National Institutes of Health . Long-acting injectable form of HIV prevention outperforms daily pill in NIH study [ cited 2021 Apr 18 ]. https://www.nih.gov/news-events/news-releases/long-acting-injectable-form-hiv-prevention-outperforms-daily-pill-nih-study
- National Institutes of Health . NIH study finds long-acting injectable drug prevents HIV acquisition in cisgender women [ cited 2021 Apr 18 ]. https://www.nih.gov/news-events/news-releases/nih-study-finds-long-acting-injectable-drug-prevents-hiv-acquisition-cisgender-women
- Cohen MS , Chen YQ , McCauley M , Gamble T , Hosseinipour MC , Kumarasamy N , et al. ; HPTN 052 Study Team . Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med . 2011 ; 365 : 493 – 505 . DOI PubMed Google Scholar
- Granich RM , Gilks CF , Dye C , De Cock KM , Williams BG . Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet . 2009 ; 373 : 48 – 57 . DOI PubMed Google Scholar
- Iwuji CC , Orne-Gliemann J , Larmarange J , Balestre E , Thiebaut R , Tanser F , et al. ; ANRS 12249 TasP Study Group . Universal test and treat and the HIV epidemic in rural South Africa: a phase 4, open-label, community cluster randomised trial. Lancet HIV . 2018 ; 5 : e116 – 25 . DOI PubMed Google Scholar
- Havlir DV , Balzer LB , Charlebois ED , Clark TD , Kwarisiima D , Ayieko J , et al. HIV testing and treatment with the use of a community health approach in rural Africa. N Engl J Med . 2019 ; 381 : 219 – 29 . DOI PubMed Google Scholar
- Makhema J , Wirth KE , Pretorius Holme M , Gaolathe T , Mmalane M , Kadima E , et al. Universal testing, expanded treatment, and incidence of HIV infection in Botswana. N Engl J Med . 2019 ; 381 : 230 – 42 . DOI PubMed Google Scholar
- Hayes RJ , Donnell D , Floyd S , Mandla N , Bwalya J , Sabapathy K , et al. ; HPTN 071 (PopART) Study Team . HPTN 071 (PopART) Study Team. Effect of universal testing and treatment on HIV incidence—HPTN 071 (PopART). N Engl J Med . 2019 ; 381 : 207 – 18 . DOI PubMed Google Scholar
- Lundgren JD , Babiker AG , Gordin F , Emery S , Grund B , Sharma S , et al. ; INSIGHT START Study Group . Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med . 2015 ; 373 : 795 – 807 . DOI PubMed Google Scholar
- Danel C , Moh R , Gabillard D , Badje A , Le Carrou J , Ouassa T , et al. ; TEMPRANO ANRS 12136 Study Group . TEMPRANO ANRS 12136 Study Group. A trial of early antiretrovirals and isoniazid preventive therapy in Africa. N Engl J Med . 2015 ; 373 : 808 – 22 . DOI PubMed Google Scholar
- Rodger AJ , Cambiano V , Bruun T , Vernazza P , Collins S , van Lunzen J , et al. ; PARTNER Study Group . Sexual activity without condoms and risk of HIV transmission in serodifferent couples when the HIV-positive partner is using suppressive antiretroviral therapy. JAMA . 2016 ; 316 : 171 – 81 . DOI PubMed Google Scholar
- Nwokolo N , Hill A , McOwan A , Pozniak A . Rapidly declining HIV infection in MSM in central London. Lancet HIV . 2017 ; 4 : e482 – 3 . DOI PubMed Google Scholar
- Grulich AE , Guy R , Amin J , Jin F , Selvey C , Holden J , et al. ; Expanded PrEP Implementation in Communities New South Wales (EPIC-NSW) research group . Population-level effectiveness of rapid, targeted, high-coverage roll-out of HIV pre-exposure prophylaxis in men who have sex with men: the EPIC-NSW prospective cohort study. Lancet HIV . 2018 ; 5 : e629 – 37 . DOI PubMed Google Scholar
- Fauci AS , Redfield RR , Sigounas G , Weahkee MD , Giroir BP . Ending the HIV epidemic: a plan for the United States. JAMA . 2019 ; 321 : 844 – 5 . DOI PubMed Google Scholar
- Rerks-Ngarm S , Pitisuttithum P , Nitayaphan S , Kaewkungwal J , Chiu J , Paris R , et al. ; MOPH-TAVEG Investigators . Vaccination with ALVAC and AIDSVAX to prevent HIV-1 infection in Thailand. N Engl J Med . 2009 ; 361 : 2209 – 20 . DOI PubMed Google Scholar
- Desrosiers RC . Protection against HIV acquisition in the RV144 trial. J Virol . 2017 ; 91 : e00905 – 17 . DOI PubMed Google Scholar
- National Institutes of Health . Experimental HIV vaccine regimen ineffective in preventing HIV [ cited 2021 Apr 18 ]. https://www.niaid.nih.gov/news-events/experimental-hiv-vaccine-regimen-ineffective-preventing-hiv
- National Institutes of Health . Antibody infusions prevent acquisition of some HIV strains, NIH studies find [ cited 2021 Apr 18 ]. https://www.niaid.nih.gov/news-events/antibody-infusions-prevent-acquisition-some-hiv-strains-nih-studies-find
- Ghys PD , Williams BG , Over M , Hallett TB , Godfrey-Faussett P . Epidemiological metrics and benchmarks for a transition in the HIV epidemic. PLoS Med . 2018 ; 15 : e1002678 . DOI PubMed Google Scholar
- Grabowski MK , Serwadda DM , Gray RH , Nakigozi G , Kigozi G , Kagaayi J , et al. ; Rakai Health Sciences Program . HIV prevention efforts and incidence of HIV in Uganda. N Engl J Med . 2017 ; 377 : 2154 – 66 . DOI PubMed Google Scholar
- Borgdorff MW , Kwaro D , Obor D , Otieno G , Kamire V , Odongo F , et al. HIV incidence in western Kenya during scale-up of antiretroviral therapy and voluntary medical male circumcision: a population-based cohort analysis. Lancet HIV . 2018 ; 5 : e241 – 9 . DOI PubMed Google Scholar
- Das P , Horton R . Beyond the silos: integrating HIV and global health. Lancet . 2018 ; 392 : 260 – 1 . DOI PubMed Google Scholar
- Eisinger RW , Fauci AS . Ending the HIV/AIDS Pandemic. Emerg Infect Dis . 2018 ; 24 : 413 – 6 . DOI PubMed Google Scholar
- De Cock KM , Simone PM , Davison V , Slutsker L . The new global health. Emerg Infect Dis . 2013 ; 19 : 1192 – 7 . DOI PubMed Google Scholar
- Lo TQ , Marston BJ , Dahl BA , De Cock KM . Ebola: Anatomy of an Epidemic. Annu Rev Med . 2017 ; 68 : 359 – 70 . DOI PubMed Google Scholar
- World Health Organization . Ending an Ebola outbreak in a conflict zone [ cited 2021 Apr 18 ]. https://storymaps.arcgis.com/stories/813561c780d44af38c57730418cd96cd
- Arwady MA , Bawo L , Hunter JC , Massaquoi M , Matanock A , Dahn B , et al. Evolution of ebola virus disease from exotic infection to global health priority, Liberia, mid-2014. Emerg Infect Dis . 2015 ; 21 : 578 – 84 . DOI PubMed Google Scholar
- Mulangu S , Dodd LE , Davey RT Jr , Tshiani Mbaya O , Proschan M , Mukadi D , et al. ; PALM Writing Group ; PALM Consortium Study Team . PALM Consortium Study Team. A randomized, controlled trial of Ebola virus disease therapeutics. N Engl J Med . 2019 ; 381 : 2293 – 303 . DOI PubMed Google Scholar
- Henao-Restrepo AM , Camacho A , Longini IM , Watson CH , Edmunds WJ , Egger M , et al. Efficacy and effectiveness of an rVSV-vectored vaccine in preventing Ebola virus disease: final results from the Guinea ring vaccination, open-label, cluster-randomised trial (Ebola Ça Suffit!). Lancet . 2017 ; 389 : 505 – 18 . DOI PubMed Google Scholar
- World Health Organization . Yellow fever outbreak Angola, Democratic Republic of the Congo and Uganda 2016–2017 [ cited 2021 Mar 14 ]. https://www.who.int/emergencies/yellow-fever/en
- Paixão ES , Teixeira MG , Rodrigues LC . Zika, chikungunya and dengue: the causes and threats of new and re-emerging arboviral diseases. BMJ Glob Health . 2018 ; 3 ( Suppl 1 ): e000530 . DOI PubMed Google Scholar
- Musso D , Ko AI , Baud D . Zika virus infection—after the pandemic. N Engl J Med . 2019 ; 381 : 1444 – 57 . DOI PubMed Google Scholar
- World Health Organization . International Health Regulations (2005). 2nd ed. Geneva: The Organization; 2008 .
- United Nations . The 17 goals [ cited 2021 Apr 18 ]. https://sdgs.un.org/goals
- Institute for Health Metrics and Evaluation . Financing global health 2019 . Tracking health spending in a time of crisis [ cited 2021 Mar 14 ]. http://www.healthdata.org/policy-report/financing-global-health-2019-tracking-health-spending-time-crisis
- World Health Organization . Weekly epidemiological update on COVID-19—13 April 2021 [ cited 2021 Apr 27 ]. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---13-april-2021
DOI: 10.3201/eid2706.210284
Original Publication Date: April 29, 2021
Table of Contents – Volume 27, Number 6—June 2021
Please use the form below to submit correspondence to the authors or contact them at the following address:
Kevin M. De Cock, c/o Miriam McNally, 669 Palmetto Ave, Suites H–I, Chico, CA 95926, USA, and PO Box 25705-00603, Lavington, Nairobi, Kenya
Comment submitted successfully, thank you for your feedback.
There was an unexpected error. Message not sent.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Article Citations
Highlight and copy the desired format.
Metric Details
Article views: 9100.
Data is collected weekly and does not include downloads and attachments. View data is from .
What is the Altmetric Attention Score?
The Altmetric Attention Score for a research output provides an indicator of the amount of attention that it has received. The score is derived from an automated algorithm, and represents a weighted count of the amount of attention Altmetric picked up for a research output.

- About Degrees
- A Deeper Look
- Research Blog
Living with HIV: A reflection on the past 25 years
A version of this post originally appeared on Interagency Youth Working Group’s Blog, "Half the World". Reposted with permission.
Greg Louganis is a gold-medal-winning Olympic diver and author. He tested positive for HIV in 1988 and has become a prominent and inspirational activist.

It has been almost 25 years since I was diagnosed with HIV. At the time the only drug we had available for treatment was AZT. The prescription for AZT was two pills every four hours around the clock. It’s a bit of an understatement to say this was not conducive to a good night’s rest while I was in training for a challenge of a lifetime, the Olympics.
Dealing with HIV was, on a daily basis, a physical and emotional challenge. The fear, the shame, the pain were, at times, almost more than I could bear. But then, it’s not really in my makeup to give up.
Ten years after I was diagnosed, I thought I would have to say good-bye to my friends and family. I was wasting away to almost nothing. Alone, I boarded a plane and flew thousands of miles from my home, where I checked into a hospital under an assumed name. To my good fortune, my doctors found the treatment to address the fungal infection in my colon and I recovered! But the next issue to face was how the heck to pay those enormous bills?! I didn’t claim it on my insurance as I was afraid of anyone finding out about my diagnoses.
I also survived the Protease Inhibitors treatment — not an easy ride! But it gave hope to many who were failing on other medications.
Now today, holy moly. I can’t believe I’m here. And the longer I live the more exciting my life becomes. So many new adventures before me and I am looking ahead fearlessly!
While it is comforting to know HIV is no longer necessarily a death sentence, I would be negligent if I did not address prevention. I wouldn’t wish my drug regimen on anyone … the side effects, not to mention the cost. Thankfully, the treatments are MUCH more tolerable and there are choices now.
I have spoken with quite a number of young, newly diagnosed men, and the first questions they are plagued by are “Why?” and “How?” Accidents happen. In the long run, does it really help to let yourself go there? It just “is.”
On a practical note, the one thing my HIV has taught me is the importance of exercise to help me tolerate my meds. I think my workouts are as important as the meds themselves. Also, I alleviate stress in my life; stress kills! I also spend time trying to tweak my thinking, looking at — and accepting — what I can change and what I cannot. It’s simple enough, and it becomes easier the more I practice it!
The fact is I live with a virus called HIV; it is a part of me, like an old friend. At times we challenge each other. But it’s clear to me now that those questions “How?” and “Why?” are irrelevant. They do not support my constitution; they inhibit my growth as a human being.
Though it may be cliché, I actually am thankful to my HIV; it has given me perspective and pushed me to pursue my passions because I don’t know how much time I have left on this earth. I have truly learned to appreciate every day. While I was expecting to be gone within 5 years of my diagnoses, it has now been 25 years and the light of my life has never been brighter. I have someone with whom to share my adventures and amazing opportunities for the future!
I have been incredibly blessed to have had such strong support and understanding as I’ve told the world about my HIV. Yes, I have my haters, but I give as little energy to those people as I possibly can. And I practice choosing words that are supportive to myself and others. I do my best not to participate in gossip and trash talk because I am sure it affects my T-cells. It’s easy to spin in other people’s stories, but it’s also pointless. And, it’s exhausting!
That’s not to say all stress is bad …. I am a bit of an adrenaline junky. Now in my 50s, I’ve taken up trapeze, and next year, I’m looking forward to an incredible scuba diving trip and a sky dive! Awareness is my path. Do the people around me make me feel good? They can stay! Those who seem like a black hole and bring me down, I let them go. It’s been a long road to get here, but now that I’m here, I’ve chosen a joyous and happy life!
No one knows how long we have, so all we can do is be at peace with ourselves and make the most of our opportunities. I never thought I would have such a wonderful impact … to be able to try to make everywhere I go better because I was there … to have a purpose! Actually, don’t ask what my purpose is, because it shifts as events present themselves. But right now, it has to do with living outside of myself and being in service to others.
It’s been 25 long years filled with trials, adventures, lessons and ultimately — at last — love. I love my life so in turn, I love my HIV; it is a part of me but doesn’t define me.
No Responses
More from this series, youth: our best sexual health investment.
Ward Cates, MD, MPH, president emeritus and distinguished scientist at FHI 360, makes a clear case for prioritizing investments in the sexual and reproductive health of the world’s youth.
Moving USAID’s Youth in Development Policy Forward: What’s Next for Sexual and Reproductive Health?
Joy Cunningham, a senior technical officer at FHI 360, explains why a 2012 U.S. Agency for International Development policy is critical to young people’s sexual and reproductive health.
Our use of cookies
Privacy overview.
- Open access
- Published: 20 October 2006
A reflection on HIV/AIDS research after 25 years
- Robert C Gallo 1
Retrovirology volume 3 , Article number: 72 ( 2006 ) Cite this article
57k Accesses
63 Citations
32 Altmetric
Metrics details
Dr. Robert C. Gallo provides a personal reflection on the 25 year history of AIDS.
A reflection on the 25 year history of AIDS can begin with no better outline than that provided by the late Jonathan Mann of WHO. A slide he gave to me in the late 1980's divides the history of AIDS into four periods: (see fig. 1 ). Jonathan could not know that the period of silent spread (part 1 of this saga) of HIV actually began years earlier. We now know that, by 1971, the virus had moved to several different regions of the world, but exactly when it came out of Africa is conjectural.
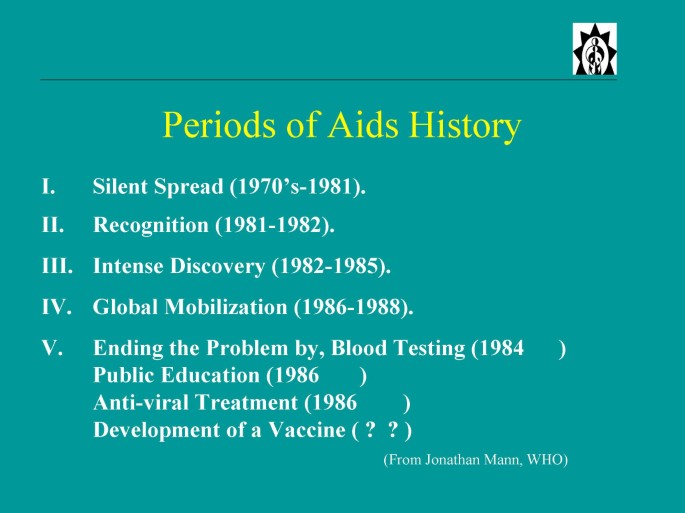
A summary of the five periods of AIDS history as modified after Jonathan Mann.
There has been considerable attention (no less than three papers in Science and Nature over the past few years from B. Hahn and her colleagues) that the natural reservoir for HIV-1 is a particular subspecies of chimp [ 1 – 3 ]. The primate-to-man origin of HIV was suspected almost from the beginning, albeit without knowing which primate. The reasons were three fold: 1) the early evidence that HIV was widespread in central Africa; 2) the evidence that HIV was more variable in Africa (hence longer presence); and 3) prior experience with HTLV-1 and HTLV-2 and their related retroviruses in African and Asian primates (STLV strains), especially the evidence suggesting a chimp origin of HTLV-1, coupled with the discovery of SIV by scientists in Boston, and later of many other strains identified in various African but not Asian monkeys. Human sera reacted better with some of these SIV strains from West Africa than they did with HIV-1, giving impetus to the work that led to the finding of HIV-2, and the obvious conclusion that HIV-2 came into man from these monkeys (sooty mangabey) [ 4 ].
But, how did the original infection of people in rainforests become an epidemic? Here we must rely on history. I presume people in rainforests (especially hunters) were occasionally infected for a long time, but died with their disease. Migration to cities may have been associated with increased prostitution. The movement of the rainforests to the world can be seen as the consequence of post World War II societal changes: increased travel with increased promiscuity, advancing intravenous drug addiction, and blood and blood products moving from one nation to another for medical purposes.
Part 2 (Fig. 1 ) is the identification of the disease by U.S. clinicians (1981) [ 5 – 7 ], and defining it as an immune disorder characterized by a decline of immune function and of T cells, and notably CD4 T cells, and by 1982 the identification of risk groups then called the "4 H's" (hemophiliacs, heroin addicts, homosexuals and Haitians). It is in the period (1982) when my colleagues and I began to think about this problem, and we initiated our first experiments in May 1982.
Along with Max Essex in Boston, I speculated in early 1982 that AIDS would be caused by a retrovirus. This was based on information that some retroviruses, like feline leukemia virus (FeLV), caused not only leukemia, but blood cell deficiencies including those of T cells [ 8 ]. This was apparently associated with genetic changes in the FeLV envelope. More importantly, I was influenced by our experiences with human retroviruses (HTLV-1 and HTLV-2), which we had only recently discovered [ 9 – 11 ]. The reasons were six fold: 1) HTLV-1 and HTLV-2 mainly targeted CD4 T cells; 2) we knew they were transmitted by blood, sex, and mother to infant especially by breast feeding. These were precisely the suggested modes of transmission of the putative microbial cause of AIDS suggested by James Curran of the U.S. Centers for Disease Control (CDC); 3) HTLV's were endemic in parts of Africa and in Haiti, and CDC had announced these were hot-beds for AIDS; 4) we knew that, even in the absence of leukemia, HTLV-1 could cause minor immune impairment; 5) we had just discovered HTLV-1 and HTLV-2, so why not a 3 rd human retrovirus, and one with the capacity to cause a profound immune disorder? 6) finally, as we began this work somewhat tentatively, I was encouraged by David Baltimore, who independently wondered aloud to me that a retrovirus was probably the origin of AIDS.
The idea, however, has sometimes been misunderstood and misrepresented as our hypothesizing that HTLV-1 itself was the cause of AIDS. That is clearly not the case. Our idea was that AIDS would be caused by a new retrovirus , but one in the HTLV family. At the time, there were at least a dozen theories as to the cause of AIDS, including non-infectious causes. Our hypothesis was the one that bore fruit. As we soon learned to our astonishment, HIV would be in a separate family of retroviruses.
J. Mann's Part 3 of AIDS history are the years 1983–85. He called this the period of intense discovery. It begins with the isolation of HIV. Our approach to find the virus of AIDS was to follow our successful pattern with the HTLV's, namely, the culture of blood cells from patients, activation of the T cells in these samples, growth of the T cells with IL-2, and search for reverse transcriptase actively in the supernatant. If positive, we would look for some cross reactivity with HTLV-1 or HTLV-2 with antibodies to proteins of these viruses. Concomitantly, we probed DNA and RNA of some primary tissues of AIDS patients using cDNA from HTLV-1 under rather relaxed conditions in order to detect sequences that might be related to HTLV-1 and 2. In 1982 and in early 1983, these experiments gave variable results that were sometimes highly positive, other times borderline or even negative. In retrospect, the highly positive samples (with sequences related to HTLV) were due to patients being doubly infected with HTLV-1 or HTLV-2 plus HIV, which occurred in close to 10% of our samples. Negative or borderline RT positive samples were due to our performing the RT assays later than the optimal peak of virus production, which occurs days earlier with HIV than with HTLV. Luc Montagnier was stimulated in part by our ideas brought to France by the French clinician Jacques Leibowitch and, in early 1983, I sent Montagnier IL-2 and antibodies against the HTLV's. He and his co-workers had found evidence of a retrovirus in a patient with lymphadenopathy, and they could distinguish it from the HTLV-1 and with those antibodies [ 12 ]. This was the first "clean" finding of HIV. Our samples at that time always had HTLV-1 as the dominant virus. However, by mid 1983, we were able to obtain many isolates of HIV, and by the time we published our papers (May 4, 1984) we described isolates from 48 patients [ 13 ]. Importantly, we were able to put six of these isolates into continuously growing T cell lines [ 14 ].
This was the necessary breakthrough, because for the first time there would be sufficient virus for detailed characterization and the development of a workable HIV blood test. The blood test (for serum antibodies to HIV), along with the large number of isolates from AIDS patients, were the major convincing results that HIV (which at the time we called HTLV-III and the French group called LAV) was the causative agent of AIDS [ 15 ].
Demonstrating that HIV was the cause of AIDS provided some special challenges – unlike most viral infections. The first was the long period between infection and the signs of AIDS (5 to 15 years). Physicians and public health officials do not ask a patient what they did a decade earlier, but rather think in terms of days or weeks. The second was the numerous infections a patient develops as they present with AIDS. Which one, if any, was the cause? The third was our concerns about verification. For rapid progress, it was essential to have rapid verification, and there were at least two factors that could greatly prolong achieving this goal. (1) Samples from AIDS patients were not only limited, but some institutions had forbade even their entry due to fears of infection. (2) T-cell culture technology, though available in immunology laboratories, was not widely available in virology laboratories. Both of these restrictions made it unlikely that there would be sufficiently rapid and conclusive confirmation by HIV isolation. Consequently, the blood test seemed to us to be particularly urgent for three reasons: 1) it allowed prevention of HIV transmission from contaminated blood; 2) it opened the door to our ability to follow the epidemic from the early period of infection, and 3) it provided for verification of HIV's causative role in AIDS. The test for serum antibodies was simple, inexpensive, safe, rapid, sensitive and accurate. Consequently, verification came rapidly and globally.
A problem then occurred that enormously hindered our work over the coming years. One of our culture samples became contaminated with virus sent to us by Luc Montagnier. At first we stubbornly refused to believe that this was possible, because the strain of HIV from Paris had different characteristics in cell culture. However, this has now been clarified [ 16 , 17 ]. Montagnier had unknowingly sent us a very different strain of HIV that grows well in cell lines. This strain contaminated his culture of LAV before it contaminated one of ours.
Then, from all sides and in big doses, came patent suits over royalties to the blood test, lawyers, media, politics and just plain pressure. Meanwhile, there were other odd problems such as people who denied the existence of AIDS, others who believed HIV did not exist, groups who believed HIV existed, but didn't cause AIDS, and those who believed HIV existed, caused AIDS, and was developed in a U.S. laboratory to kill African Americans and gay men. Suffice it to say, no scientist is prepared for things like this. Despite these distractions, science progressed with great speed. Mann called it the fastest pace of discovery in medical history from the time of inception of a new disease.
To briefly revisit that period, some of the noteworthy advances are listed here. They include discovery of HIV (1983–84) [ 12 – 14 ]; convincing evidence that it was the cause of AIDS ('84) [ 15 , 18 , 19 ]; modes of transmission understood ('84–'85); genome sequenced ('85) [ 20 – 22 ]; most genes and proteins defined ('84–'85) though not all their functions[ 23 – 25 ]; main target cells CD4 T cells, macrophages, and brain microglial cells – elucidated [ 26 , 27 ]; key reagents produced and made available for involved scientists all over the world ('84–'85); genomic heterogeneity of HIV ('84) – including the innumerable microvariants within a single patient ('86–'88) [ 28 , 29 ], first practical life saving advance ('85); the blood test ('84)[ 30 ]; close monitoring of the epidemic for the first time, because of the wide availability of the blood test ('85); the SIV-monkey model ('85) [ 31 , 32 ]; the beginning of therapy – AZT ('85)[ 33 ]; and the beginning understanding of pathogenesis ('85)[ 34 ].
These rapid advances led to expectations that AIDS might be quickly solved. However, those scientists with experience in retrovirology knew differently: Unless a successful vaccine was soon available, this would be a long road – an infection that might be permanent in the population as retroviruses are in many species. Furthermore, we knew by mid-1984 that the infection was becoming global. We had tested sera from many countries, and we could follow the evidence for HIV coming into a region (a positive HIV blood test) with subsequent AIDS. However, we could never anticipate the HIV African tragedy.
Despite the rapid advances in those years, I think it is still appropriate to ask whether we could have done better. For example, were we as medical scientists, health officials, doctors or simply as members of society prepared? The answer is an interesting mix of opposites! On the one hand, if AIDS had to come, we were lucky that (scientifically speaking) it came at a very good time. The 1970's saw the revelation of the replication cycle of animal retroviruses (so we had a framework to work by once HIV was established as the cause). We had most modern tools of molecular biology (mainly developed in the 1970's). We had monoclonal antibodies also developed in the 1970's. We had access to technology to grow human T-cells with IL-2 which my colleagues and I developed in the mid-1970's, and we had found other human retroviruses in the 1980's-82 giving the first credence to their presence in humans. However, if AIDS had to come, we could also say it came at the worst of times. It seems that people have a memory span not longer than 25–30 years. Here are three examples of what I mean: First, was the surprise and lack of preparation in 1918–1919 for the great influenza epidemic – forgetting lessons of the late 19 th century [ 35 ]. Secondly, there was surprise and lack of preparation at the onset of the polio epidemic in the late 1940's and early 1950's [ 36 ]. It is eerie to read accounts of that period showing that medical science in particular and society as a whole, were focused on chronic degenerative diseases, believing serious infectious diseases to be "conquered". Eerie also because, thirdly that was precisely the attitude once again by the late 1970's evidenced by the closure of some microbiology departments, and threats of increasing reductions to CDC. The microbe would be simply the playground of the molecular biologist. Some even felt humans could not be infected by retroviruses.
No group was really responsible for unraveling the cause of the new epidemic, except the CDC, but in my view the CDC cannot and does not have expertise in every class of microbes, let alone for all types of viruses, and indeed they had no expertise in animal or human retroviruses. Our group became involved only after I listened to a lecture by the CDC's James Curran, who called for help from virologists. I have suggested that the government provide base support for 10 or more virus centers, covering all types of viruses among the centers. These centers would be responsible for providing needed expertise to the CDC for the etiological agent, diagnostics and possibly therapy and prevention. In accordance with the kind of virus suspected, the center(s) would be activated. Each center might also be required to have close collaborations with at least two groups from developing nations.
Though the HIV blood test was brought forward rapidly (early 1985) to large companies that could make the test available on an industrialized scale, I believe we could have still done better. For instance, we could have tested the pooled plasma used for hemophiliacs in 1984 without a large industrial scale production of the test. I don't think anyone was thinking of this. We were advised to return to basic laboratory research and assumed someone would be doing these tests. The lesson here for me is to take more control of things that come from your own work.
Where did things go since this early period of 1982–85? Jonathan Mann describes Part 4 ('86) as the time of global mobilization. This means education leading to prevention of infection, and no doubt this was the second major practical advance and it continues today with results that vary in place and even in time. There is proven success in some places, but not all, and sometimes there is only temporary success. It is noteworthy that appropriate education also depends upon the blood test, hence on basic science.
There were many other major advances over these next 20 years ('86-06), but none were more important than therapy. This is listed as Part 5 of Mann's summary, but it was added by me as the "period" era of practical advances, but the time lines for these advances are actually from 1984–1995. AZT showed for the first time that a viral disease could be objectively treated (decline in virus levels and lessened signs of AIDS), and there is no need to embellish here on the great advances made with the triple drug therapy in the mid 1990's. This was from contributions of a great number of scientists: those who contributed to our basic understanding of HIV replication, and as a result to targets for therapy, and those who developed the culture systems to grow HIV that could also be used in drug testing, and of course to the pharmaceutical industry, especially those like E. Emini who helped design and develop the protease inhibitors.
The other major practical advances in the last two decades have mainly been an extension of the earlier ones: more widespread use of the blood test as well as educational programs; refining therapies; learning about HIV drug resistance and how best to avoid it; better care of patients; and learning about serious co-infections especially of tuberculosis and HCV. A selection of the most important basic science advances will be debatable. In my view, the most important include the following: clarification of the two HIV strain functional extremes – the pure CCR5 tropic viruses and the CXCR4 tropic viruses [ 37 – 42 ], for review, see [ 43 , 44 ]; the discovery of the first endogenous inhibitors of HIV (β-chemokines) [ 44 ]; elucidation of the mechanisms involved in the action of some the HIV non-structural proteins [ 45 , 46 ]; an appreciation of the role of abnormal immune activation in pathogenesis, which impacts not only HIV infected cells, but is also detrimental to uninfected immune cells for review, see [ 44 , 47 ]; major advances in our understanding of the various types of HIV in different regions of the world and new recombinant forms; evolving knowledge of the envelope structure [ 48 , 49 ]; the details of HIV entry into cells [ 50 ]; and various genetic and some environmental mechanisms for resisting infection and slowing progression to AIDS in infected persons, as well others fostering infection and progression [ 51 , 52 ]. These latter basic advances have already had their practical impact, including for example several new approaches for drugs that target HIV entry.
We have reached the end of the first 25 years of AIDS, and we can safely say that we know as much about HIV as we do of any pathogen and about AIDS as we do any human disease. The remaining problems and needs are evident: bringing therapy and better health infrastructure to poor nations; continuing to develop new treatments because of the need for life-long therapy and the associated drug side effects and HIV resistance; continuing and advancing education; global monitoring of the different strains of HIV for changes in their virulence, transmissibility and drug resistance; and development of a preventive vaccine which provides sterilizing immunity (or close to it) [ 53 ]. For a successful vaccine, I believe we need neutralizing antibodies that are sustained (do not need rapid recall), and I think this is a reachable objective. Parenthetically, it has often been erroneously said (most recently in the New York Times reporting of the Toronto International AIDS Conference) that, at the April 1984 press conference, Secretary of Health, Margaret Heckler stated that a successful vaccine would be available within two years. Transcripts of comments are still available and show that no such claim was made. Rather, it was said that the virus could be continuously produced in large amounts, thereby making trials possible within two years. Indeed, this proved true, because in 1986, Daniel Zagury carried out some phase 1 trials in Africa and in Paris.
Several encouraging developments provide some optimism for the future, such as the ability of some nations to diminish rates of infection by education, and major new funding sources aimed at practical achievements. One laudable example is President Bush's Emergency Plan for AIDS Relief, which is providing $15 billion for therapy for HIV positive patients in needy nations. We have been impressed that this effort carries out its mission with leadership by university clinical scientists who work with groups with long experience in the specific country. In contrast to alternative plans that simply and rapidly provide funds for the drugs, these programs add to local infrastructure and training, thereby reducing the prospects for creating more multi-drug resistant HIV mutants. Private foundations have also been a new forceful addition; International AIDS Vaccine Initiative (IAVI) for developing vaccine candidates and the Bill and Melinda Gates Foundation for fulfilling many needs.
There are also major concerns for the future. We know science is essential for solving the HIV problem and, as noted before, science has been responsible for all the major practical advances in fighting this disease. However, there is a growing distance between scientists and the larger public. John Moore of Cornell Weill Medical School reminded me that C.P. Snow wrote about this in the 1950's, but I think the gap has continued to widen as technology becomes more and more specialized. Sometimes, it leads to tension and even hostility by the larger public toward scientists. This is sometimes evident in AIDS, seemingly so in recent years. Consider a recent CNN program that was a positive educational force, but advertised as one composed of AIDS experts. However, not one scientist was among the experts, and the program ended with a movie actor stating that to solve the problem, we all "had to be together." It was togetherness rather than science that he informed us would solve AIDS.
To return to and end on a positive note: it is interesting and useful to remember that there has been some silver lining on the dark AIDS clouds. Consider the many positive spin-offs to science in immunology, cancer biology, basic virology, and even molecular biology along with the leadership and focus AIDS research has provided to therapy of viral infections and to vaccine development. Positive spin-offs have not been limited to science. Consider how AIDS has inspired far greater tolerance (at least in the West) of differences in sexuality and much greater scientific and humanitarian collaborations between developed and less developed nations. Certainly, this is the case for relations between the U.S. and Africa. Let us hope these advances in understanding and in conscience will continue to evolve and grow so that there will be no need for anyone to reflect on AIDS in its 50 th birthday year.
Gao F, Bailes E, Robertson DL, Chen Y, Rodenburg CM, Michael SF, Cummins LB, Arthur LO, Peeters M, Shaw GM, Sharp PM, Hahn BH: Origin of HIV-1 in the chimpanzee Pan troglodytes troglodytes. Nature. 1999, 397: 436-441. 10.1038/17130.
Article CAS PubMed Google Scholar
Keele BF, Van HF, Li Y, Bailes E, Takehisa J, Santiago ML, Bibollet-Ruche F, Chen Y, Wain LV, Liegeois F, Loul S, Ngole EM, Bienvenue Y, Delaporte E, Brookfield JF, Sharp PM, Shaw GM, Peeters M, Hahn BH: Chimpanzee reservoirs of pandemic and nonpandemic HIV-1. Science. 2006, 313: 523-526. 10.1126/science.1126531.
Article PubMed Central CAS PubMed Google Scholar
Santiago ML, Rodenburg CM, Kamenya S, Bibollet-Ruche F, Gao F, Bailes E, Meleth S, Soong SJ, Kilby JM, Moldoveanu Z, Fahey B, Muller MN, Ayouba A, Nerrienet E, McClure HM, Heeney JL, Pusey AE, Collins DA, Boesch C, Wrangham RW, Goodall J, Sharp PM, Shaw GM, Hahn BH: SIVcpz in wild chimpanzees. Science. 2002, 295: 465-10.1126/science.295.5554.465.
Sharp PM, Bailes E, Chaudhuri RR, Rodenburg CM, Santiago MO, Hahn BH: The origins of acquired immune deficiency syndrome viruses: where and when?. Philos Trans R Soc Lond B Biol Sci. 2001, 356: 867-876. 10.1098/rstb.2001.0863.
Siegal FP, Lopez C, Hammer GS, Brown AE, Kornfeld SJ, Gold J, Hassett J, Hirschman SZ, Cunningham-Rundles C, Adelsberg BR: Severe acquired immunodeficiency in male homosexuals, manifested by chronic perianal ulcerative herpes simplex lesions. N Engl J Med. 1981, 305: 1439-1444.
Gottlieb MS, Schroff R, Schanker HM, Weisman JD, Fan PT, Wolf RA, Saxon A: Pneumocystis carinii pneumonia and mucosal candidiasis in previously healthy homosexual men: evidence of a new acquired cellular immunodeficiency. N Engl J Med. 1981, 305: 1425-1431.
Friedman-Kien AE: Disseminated Kaposi's sarcoma syndrome in young homosexual men. J Am Acad Dermatol. 1981, 5: 468-471.
Wernicke D, Trainin Z, Ungar-Waron H, Essex M: Humoral immune response of asymptomatic cats naturally infected with feline leukemia virus. J Virol. 1986, 60: 669-673.
PubMed Central CAS PubMed Google Scholar
Kalyanaraman VS, Sarngadharan MG, Robert-Guroff M, Miyoshi I, Golde D, Gallo RC: A new subtype of human T-cell leukemia virus (HTLV-II) associated with a T-cell variant of hairy cell leukemia. Science. 1982, 218: 571-573. 10.1126/science.6981847.
Poiesz BJ, Ruscetti FW, Gazdar AF, Bunn PA, Minna JD, Gallo RC: Detection and isolation of type C retrovirus particles from fresh and cultured lymphocytes of a patient with cutaneous T-cell lymphoma. Proc Natl Acad Sci U S A. 1980, 77: 7415-7419. 10.1073/pnas.77.12.7415.
Poiesz BJ, Ruscetti FW, Reitz MS, Kalyanaraman VS, Gallo RC: Isolation of a new type C retrovirus (HTLV) in primary uncultured cells of a patient with Sezary T-cell leukaemia. Nature. 1981, 294: 268-271. 10.1038/294268a0.
Barre-Sinoussi F, Chermann JC, Rey F, Nugeyre MT, Chamaret S, Gruest J, Dauguet C, Axler-Blin C, Vezinet-Brun F, Rouzioux C, Rozenbaum W, Montagnier L: Isolation of a T-lymphotropic retrovirus from a patient at risk for acquired immune deficiency syndrome (AIDS). Science. 1983, 220: 868-871. 10.1126/science.6189183.
Gallo RC, Salahuddin SZ, Popovic M, Shearer GM, Kaplan M, Haynes BF, Palker TJ, Redfield R, Oleske J, Safai B: Frequent detection and isolation of cytopathic retroviruses (HTLV-III) from patients with AIDS and at risk for AIDS. Science. 1984, 224: 500-503. 10.1126/science.6200936.
Popovic M, Sarngadharan MG, Read E, Gallo RC: Detection, isolation, and continuous production of cytopathic retroviruses (HTLV-III) from patients with AIDS and pre-AIDS. Science. 1984, 224: 497-500. 10.1126/science.6200935.
Sarngadharan MG, Popovic M, Bruch L, Schupbach J, Gallo RC: Antibodies reactive with human T-lymphotropic retroviruses (HTLV-III) in the serum of patients with AIDS. Science. 1984, 224: 506-508. 10.1126/science.6324345.
Wain-Hobson S, Vartanian JP, Henry M, Chenciner N, Cheynier R, Delassus S, Martins LP, Sala M, Nugeyre MT, Guetard D: LAV revisited: origins of the early HIV-1 isolates from Institut Pasteur. Science. 1991, 252: 961-965. 10.1126/science.2035026.
Guo HG, Chermann JC, Waters D, Hall L, Louie A, Gallo RC, Streicher H, Reitz MS, Popovic M, Blattner W: Sequence analysis of original HIV-1. Nature. 1991, 349: 745-746. 10.1038/349745a0.
Schupbach J, Popovic M, Gilden RV, Gonda MA, Sarngadharan MG, Gallo RC: Serological analysis of a subgroup of human T-lymphotropic retroviruses (HTLV-III) associated with AIDS. Science. 1984, 224: 503-505. 10.1126/science.6200937.
Safai B, Sarngadharan MG, Groopman JE, Arnett K, Popovic M, Sliski A, Schupbach J, Gallo RC: Seroepidemiological studies of human T-lymphotropic retrovirus type III in acquired immunodeficiency syndrome. Lancet. 1984, 1: 1438-1440. 10.1016/S0140-6736(84)91933-0.
Sanchez-Pescador R, Power MD, Barr PJ, Steimer KS, Stempien MM, Brown-Shimer SL, Gee WW, Renard A, Randolph A, Levy JA: Nucleotide sequence and expression of an AIDS-associated retrovirus (ARV-2). Science. 1985, 227: 484-492. 10.1126/science.2578227.
Ratner L, Haseltine W, Patarca R, Livak KJ, Starcich B, Josephs SF, Doran ER, Rafalski JA, Whitehorn EA, Baumeister K: Complete nucleotide sequence of the AIDS virus, HTLV-III. Nature. 1985, 313: 277-284. 10.1038/313277a0.
Wain-Hobson S, Sonigo P, Danos O, Cole S, Alizon M: Nucleotide sequence of the AIDS virus, LAV. Cell. 1985, 40: 9-17. 10.1016/0092-8674(85)90303-4.
Arya SK, Gallo RC, Hahn BH, Shaw GM, Popovic M, Salahuddin SZ, Wong-Staal F: Homology of genome of AIDS-associated virus with genomes of human T-cell leukemia viruses. Science. 1984, 225: 927-930. 10.1126/science.6089333.
Muesing MA, Smith DH, Cabradilla CD, Benton CV, Lasky LA, Capon DJ: Nucleic acid structure and expression of the human AIDS/lymphadenopathy retrovirus. Nature. 1985, 313: 450-458. 10.1038/313450a0.
Robey WG, Safai B, Oroszlan S, Arthur LO, Gonda MA, Gallo RC, Fischinger PJ: Characterization of envelope and core structural gene products of HTLV-III with sera from AIDS patients. Science. 1985, 228: 593-595. 10.1126/science.2984774.
Harper ME, Marselle LM, Gallo RC, Wong-Staal F: Detection of lymphocytes expressing human T-lymphotropic virus type III in lymph nodes and peripheral blood from infected individuals by in situ hybridization. Proc Natl Acad Sci U S A. 1986, 83: 772-776. 10.1073/pnas.83.3.772.
Shaw GM, Hahn BH, Arya SK, Groopman JE, Gallo RC, Wong-Staal F: Molecular characterization of human T-cell leukemia (lymphotropic) virus type III in the acquired immune deficiency syndrome. Science. 1984, 226: 1165-1171. 10.1126/science.6095449.
Saag MS, Hahn BH, Gibbons J, Li Y, Parks ES, Parks WP, Shaw GM: Extensive variation of human immunodeficiency virus type-1 in vivo. Nature. 1988, 334: 440-444. 10.1038/334440a0.
Hahn BH, Shaw GM, Taylor ME, Redfield RR, Markham PD, Salahuddin SZ, Wong-Staal F, Gallo RC, Parks ES, Parks WP: Genetic variation in HTLV-III/LAV over time in patients with AIDS or at risk for AIDS. Science. 1986, 232: 1548-1553. 10.1126/science.3012778.
Joyce C, Anderson I: US licenses blood test for AIDS. New Sci. 1985, 105: 3-4.
PubMed Google Scholar
Chakrabarti L, Guyader M, Alizon M, Daniel MD, Desrosiers RC, Tiollais P, Sonigo P: Sequence of simian immunodeficiency virus from macaque and its relationship to other human and simian retroviruses. Nature. 1987, 328: 543-547. 10.1038/328543a0.
Chalifoux LV, Ringler DJ, King NW, Sehgal PK, Desrosiers RC, Daniel MD, Letvin NL: Lymphadenopathy in macaques experimentally infected with the simian immunodeficiency virus (SIV). Am J Pathol. 1987, 128: 104-110.
Mitsuya H, Weinhold KJ, Furman PA, St Clair MH, Lehrman SN, Gallo RC, Bolognesi D, Barry DW, Broder S: 3'-Azido-3'-deoxythymidine (BW A509U): an antiviral agent that inhibits the infectivity and cytopathic effect of human T-lymphotropic virus type III/lymphadenopathy-associated virus in vitro. Proc Natl Acad Sci U S A. 1985, 82: 7096-7100. 10.1073/pnas.82.20.7096.
Lane HC, Fauci AS: Immunologic abnormalities in the acquired immunodeficiency syndrome. Annu Rev Immunol. 1985, 3: 477-500. 10.1146/annurev.iy.03.040185.002401.
Barry JM: The Great Influenza: The Epic Story of the Deadliest Plague in History. 2004, New York, NY, Viking
Google Scholar
Oshinsky DM: Polio: An American Story. 2005, New York, NY, Oxford University Press
Dragic T, Litwin V, Allaway GP, Martin SR, Huang Y, Nagashima KA, Cayanan C, Maddon PJ, Koup RA, Moore JP, Paxton WA: HIV-1 entry into CD4+ cells is mediated by the chemokine receptor CC-CKR-5. Nature. 1996, 381: 667-673. 10.1038/381667a0.
Doranz BJ, Rucker J, Yi Y, Smyth RJ, Samson M, Peiper SC, Parmentier M, Collman RG, Doms RW: A dual-tropic primary HIV-1 isolate that uses fusin and the beta- chemokine receptors CKR-5, CKR-3, and CKR-2b as fusion cofactors. Cell. 1996, 85: 1149-1158. 10.1016/S0092-8674(00)81314-8.
Deng H, Liu R, Ellmeier W, Choe S, Unutmaz D, Burkhart M, Di Marzio P, Marmon S, Sutton RE, Hill CM, Davis CB, Peiper SC, Schall TJ, Littman DR, Landau NR: Identification of a major co-receptor for primary isolates of HIV-1. Nature. 1996, 381: 661-666. 10.1038/381661a0.
Choe H, Farzan M, Sun Y, Sullivan N, Rollins B, Ponath PD, Wu L, Mackay CR, LaRosa G, Newman W, Gerard N, Gerard C, Sodroski J: The beta-chemokine receptors CCR3 and CCR5 facilitate infection by primary HIV-1 isolates. Cell. 1996, 85: 1135-1148. 10.1016/S0092-8674(00)81313-6.
Alkhatib G, Combadiere C, Broder CC, Feng Y, Kennedy PE, Murphy PM, Berger EA: CC CKR5: a RANTES, MIP-1alpha, MIP-1beta receptor as a fusion cofactor for macrophage-tropic HIV-1. Science. 1996, 272: 1955-1958.
Feng Y, Broder CC, Kennedy PE, Berger EA: HIV-1 entry cofactor: functional cDNA cloning of a seven- transmembrane, G protein-coupled receptor. Science. 1996, 272: 872-877.
Lusso P: HIV and the chemokine system: 10 years later. EMBO J. 2006, 25: 447-456. 10.1038/sj.emboj.7600947.
Cocchi F, DeVico AL, Garzino-Demo A, Arya SK, Gallo RC, Lusso P: Identification of RANTES, MIP-1 alpha, and MIP-1 beta as the major HIV-suppressive factors produced by CD8+ T cells. Science. 1995, 270: 1811-1815.
Feinberg MB, Jarrett RF, Aldovini A, Gallo RC, Wong-Staal F: HTLV-III expression and production involve complex regulation at the levels of splicing and translation of viral RNA. Cell. 1986, 46: 807-817. 10.1016/0092-8674(86)90062-0.
Sodroski J, Rosen C, Wong-Staal F, Salahuddin SZ, Popovic M, Arya S, Gallo RC, Haseltine WA: Trans-acting transcriptional regulation of human T-cell leukemia virus type III long terminal repeat. Science. 1985, 227: 171-173. 10.1126/science.2981427.
Ascher MS, Sheppard HW: AIDS as immune system activation: a model for pathogenesis. Clin Exp Immunol. 1988, 73: 165-167.
Chan DC, Fass D, Berger JM, Kim PS: Core structure of gp41 from the HIV envelope glycoprotein. Cell. 1997, 89: 263-273. 10.1016/S0092-8674(00)80205-6.
Kwong PD, Wyatt R, Robinson J, Sweet RW, Sodroski J, Hendrickson WA: Structure of an HIV gp120 envelope glycoprotein in complex with the CD4 receptor and a neutralizing human antibody. Nature. 1998, 393: 648-659. 10.1038/31405.
Dalgleish AG, Beverley PC, Clapham PR, Crawford DH, Greaves MF, Weiss RA: The CD4 (T4) antigen is an essential component of the receptor for the AIDS retrovirus. Nature. 1984, 312: 763-767. 10.1038/312763a0.
Dean M, Jacobson LP, McFarlane G, Margolick JB, Jenkins FJ, Howard OM, Dong HF, Goedert JJ, Buchbinder S, Gomperts E, Vlahov D, Oppenheim JJ, O'Brien SJ, Carrington M: Reduced risk of AIDS lymphoma in individuals heterozygous for the CCR5- delta32 mutation. Cancer Res. 1999, 59: 3561-3564.
CAS PubMed Google Scholar
Martin MP, Dean M, Smith MW, Winkler C, Gerrard B, Michael NL, Lee B, Doms RW, Margolick J, Buchbinder S, Goedert JJ, O'Brien TR, Hilgartner MW, Vlahov D, O'Brien SJ, Carrington M: Genetic acceleration of AIDS progression by a promoter variant of CCR5. Science. 1998, 282: 1907-1911. 10.1126/science.282.5395.1907.
Gallo RC: The end or the beginning of the drive to an HIV-preventive vaccine: a view from over 20 years. Lancet. 2005, 366: 1894-1898. 10.1016/S0140-6736(05)67395-3.
Article PubMed Google Scholar
Download references
Acknowledgements
I am deeply grateful to my long time colleague, Dr. Marvin Reitz, for his reading of this manuscript and help with references. I thank Ms. Risa Davis for her editorial assistance.
Author information
Authors and affiliations.
Institute of Human Virology, University of Maryland Biotechnology Institute and Department of Microbiology and Immunology, University of Maryland School of Medicine, Baltimore, Maryland, 21201, USA
Robert C Gallo
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Robert C Gallo .
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Gallo, R.C. A reflection on HIV/AIDS research after 25 years. Retrovirology 3 , 72 (2006). https://doi.org/10.1186/1742-4690-3-72
Download citation
Received : 04 October 2006
Accepted : 20 October 2006
Published : 20 October 2006
DOI : https://doi.org/10.1186/1742-4690-3-72
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Melinda Gate Foundation
- Triple Drug Therapy
- Feline Leukemia Virus
- Large Industrial Scale Production
- Successful Vaccine
View archived comments (1)
Retrovirology
ISSN: 1742-4690
- Submission enquiries: [email protected]

Reflection on World AIDS Day: HIV/AIDS still matters

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Emerg Infect Dis
- v.17(6); 2011 Jun
Reflections on 30 Years of AIDS
TOC summary: Although the end of the epidemic is not yet in sight, the remarkable response has improved health around the world.
June 2011 marks the 30th anniversary of the first description of what became known as HIV/AIDS, now one of history’s worst pandemics. The basic public health tools of surveillance and epidemiologic investigation helped define the epidemic and led to initial prevention recommendations. Features of the epidemic, including the zoonotic origin of HIV and its spread through global travel, are central to the concept of emerging infectious diseases. As the epidemic expanded into developing countries, new models of global health and new global partnerships developed. Advocacy groups played a major role in mobilizing the response to the epidemic, having human rights as a central theme. Through the commitments of governments and private donors, modern HIV treatment has become available throughout the developing world. Although the end of the epidemic is not yet in sight and many challenges remain, the response has been remarkable and global health has changed for the better.
We seem to think, with health problems as with other things, that science and technology will always save us, even though in the realm of human endeavor, it always comes (down) to people and our relationships—James Curran One of the saddest days of my life was when my mother told me Superman did not exist…. “’cause you just thought… he always shows up and he saves all the good people… and I was crying because there was no one… coming with enough power to save us.”—Geoffrey Canada
On June 5, 1981, the Morbidity and Mortality Weekly Report (MMWR), published by the Centers for Disease Control and Prevention (CDC), described Pneumocystis carinii (now P. jiroveci ) pneumonia in 5 homosexual men in Los Angeles, California, USA, documenting for the first time what became known as acquired immunodeficiency syndrome (AIDS). The accompanying editorial suggested that the illness might be related to the men’s sexual behavior. A month later, the MMWR reported additional diagnoses of P. carinii pneumonia, other opportunistic infections (OIs), and Kaposi sarcoma (KS) in homosexual men from New York City and California. These articles were sentinels for what became one of history’s worst pandemics, with >60 million infections, 30 million deaths, and no end in sight.
This 30th anniversary year of the first description of AIDS is also the 15th anniversary of the introduction of highly active antiretroviral therapy (ART). Henceforth, AIDS will have been a treatable condition longer than it was the inevitably fatal disease first recognized. We offer highlights and reflections from a predominantly global perspective on 3 decades of collective experience with AIDS.
Early AIDS Surveillance and Epidemiology
To investigate this apparent outbreak, CDC investigators developed a simple surveillance case definition for what was first called KS/OI. The definition focused on certain OIs or KS in otherwise healthy persons and was used to establish a national reporting system. In light of new knowledge concerning AIDS and its underlying cause, the case definition was modified over time, but early surveillance indicated that an epidemic was under way and, in retrospect, had begun several years before the first reports. Retrospective testing of stored serum specimens from hepatitis patients in Los Angeles documented human immunodeficiency virus (HIV) infection as early as 1979.
The initial risk groups identified were men who have sex with men (MSM) and injection drug users (IDU). Field investigations and surveillance activities demonstrated sexually linked cases in MSM and in persons with hemophilia and transfusion recipients, implicating transmission by male-to-male sexual contact as well as through blood and blood products. Cases in heterosexual persons and infants indicated that transmission could also occur through heterosexual contact and from mother to child.
Within <2 years, the essential epidemiology of AIDS—groups at risk and modes of transmission—was established, although debate about transmission through blood and blood products continued for several months after CDC believed the evidence was clear. In March 1983, the US Public Health Service published the first recommendations for AIDS prevention, including a recommendation that members of risk groups limit their numbers of sex partners and not donate blood or plasma. Although these recommendations were made before the etiologic agent, HIV, had been identified, they initiated AIDS prevention efforts and have largely stood the test of time, as has promotion of condom use.
As evidence accumulated that AIDS would not be confined to MSM and IDU, media interest grew and fears of contagion increased. Fear about transmission through casual contact led to discrimination against persons with AIDS, including barring HIV-infected children from school. During this time, CDC was recognized as a source of trustworthy information, and the agency gained respect by placing science above political considerations. Having devoted 71 articles to AIDS during 1981–1985, MMWR played a central role in dissemination of health information for rational policy decisions.
CDC regularly consulted with the World Health Organization (WHO), which published global data in its Weekly Epidemiological Record. While cases of AIDS in MSM and IDU began to be reported from other countries, several European countries reported cases in black Africans with no history of drug use or male-to-male sex. In the United States, cases also occurred in recent migrants from Haiti, subsequently designated as a risk group. Although this designation was useful for public health purposes, it resulted in discrimination against Haitian Americans. The subsequent explanation for AIDS in Africans and Haitians without other risk factors was heterosexual transmission of the causative agent.
In 1983, HIV was discovered, an accomplishment for which French scientists received the Nobel Prize for Medicine in 2008. In 1985, a serologic test for HIV became commercially available. Agreement on HIV as the causative agent and the availability of a diagnostic test were closing features of these early years. Despite the potential for hysteria and some examples of irrational responses, science and reason prevailed; epidemiology and surveillance served as the foundation of society’s understanding and early response, as they would have to do repeatedly in future infectious disease epidemics.

AIDS as a Metaphor for Emerging Infections and the New Global Health
Social and environmental change, increased public health awareness, and improved diagnostic tools led to the emergence and recognition of several new pathogens in the last third of the 20th century. After a prolonged period of complacency with regard to infectious diseases, in 1992 the Institute of Medicine published an influential report on emerging infectious diseases. This term referred to conditions that were increasing in incidence in human populations or threatening to do so, were newly introduced or detected, or were recognized as being linked to a chronic disease or syndrome. No agent and disease better exemplify this concept than HIV and AIDS.
HIV type 1, group M (HIV-1), the predominant cause of the AIDS epidemic, evolved from a virus that crossed the species barrier from chimpanzees to humans. The earliest retrospective diagnosis of HIV-1 infection was made from a serum specimen collected in 1959 in Kinshasa, capital of what is now the Democratic Republic of Congo. Two additional but rare groups of HIV-1 (N and O) cause related zoonotic infections that are essentially restricted to central Africa. HIV-2, a second type of HIV rarely found outside western Africa, originated in sooty mangabeys.
Phylogenetic analysis of HIV-1 and SIVcpz (the simian immunodeficiency virus of chimpanzees closely related to HIV-1), combined with knowledge about the geographic range of the chimpanzee host, Pan troglodytes troglodytes , suggest that this cross-species transmission took place in central Africa early in the 20th century. The exact circumstances of cross-species transmission in central Africa are uncertain, but opportunities for human exposure to simian viruses through hunting and related activities are abundant. Over time, the virus presumably adapted to the human host and began to spread from person to person. At some unknown point, it was introduced into the Western Hemisphere, including Haiti and the United States.
Although the epidemic appears to have begun in central Africa, HIV prevalence is now highest in southern Africa; the Republic of South Africa alone is home to about one sixth of the world’s HIV-infected persons. The reasons for this geographic distribution are not entirely clear, but biological factors, such as lack of male circumcision and rates of other genital (especially ulcerative) infections that facilitate HIV transmission, and social factors (some of which may have been influenced by the end of apartheid), such as frequent partner change and concurrent sexual partnerships, migration, and commercial sex, likely play a role. Whether infectiousness varies by virus subtype (subtype C is dominant in southern Africa) remains debated. Under the South African presidency of Thabo Mbeki, AIDS denialism (the view that HIV is not the cause of AIDS) led to delayed implementation of ART and resulted in thousands of deaths.
Understanding the emergence and origins of HIV/AIDS will provide insight into global vulnerability to new infectious diseases. Without globalization and its central characteristic of increased movement of people, HIV might have remained in central Africa and the AIDS pandemic might have been delayed or might not have occurred. Although commerce and trade are as old as civilization, international air travel increased greatly in the latter half of the 20th century and enabled people to arrive at their destinations in greater numbers and within the incubation periods of many infectious diseases. The prolonged period between HIV infection and symptomatic AIDS, ≈11 years in adults, allowed widespread HIV transmission before recognition of the epidemic and any prevention attempts.
The response to HIV/AIDS epitomizes a new concept of global health. Essentials of global health today are its integration of core public health attributes (data and surveillance-based approaches, emphasis on populations, goals of social justice and equity, and prioritization of prevention), expansion into new areas such as treatment and health systems, and focus on emerging challenges beyond traditional priorities. New areas of emphasis include health security, chronic diseases (e.g., diabetes), and road traffic injuries. Global health is now about how the world deals with health rather than how a particular country addresses health problems in other countries.
AIDS and the Globalization of Science, Research, and Practice
A positive development in the response to AIDS has been its effect on science and the globalization of research and practice. Retrovirology and immunology became well-supported disciplines whose practitioners interacted productively with workers in other subjects such as epidemiology. Cohorts of physicians and scientists built their careers in basic as well as applied and clinical research. The frequency with which tuberculosis occurs in HIV-infected persons has led to a resurgence of interest in the diagnosis and treatment of this ancient disease, especially in Africa. Advances in the treatment of HIV-associated OIs have benefited other immunosuppressed persons. In addition, sexual and reproductive health gained renewed prominence.
Scientific advances resulted in the development of lifesaving, albeit not curative, treatment for HIV. Beginning with the approval of AZT (azidothymidine or zidovudine) in 1987, the development of antiretroviral drugs and the design of simple and standardized approaches for therapy in the developing world constituted a public health triumph. By the end of 2009, >5 million persons in low- and middle-income countries were accessing ART, unimaginable just a few years before and made possible through the use of generic drugs, price reductions for brand-name drugs, and efforts of international donors through initiatives such as the President’s Emergency Plan for AIDS Relief and the Global Fund.
Research on the prevention of mother-to-child transmission of HIV has led to interventions with the potential to virtually eliminate HIV disease in children. Screening of donated blood and plasma for HIV and heat treatment of blood products have virtually eliminated transfusion-related HIV in high-income countries and vastly reduced its occurrence throughout low- and middle-income settings. Research has identified viable options for HIV prevention in IDU, such as needle and syringe exchange and opioid substitution therapy. Hospital hygiene and safe injection practices, previously neglected in much of the developing world, have become topics of global concern.
The earliest international collaborative field investigations on HIV/AIDS were in 1983 in Rwanda and the former Zaire, now the Democratic Republic of Congo. In 1984, Projet SIDA (French for AIDS Project) was established. This project, a joint venture between CDC, the National Institutes of Health, the Belgian Institute of Tropical Medicine, Mama Yemo Hospital (Kinshasa), and the then Zairian Department of Public Health, conducted landmark epidemiologic studies in central Africa. At one time Zaire had the highest citation index for AIDS research in the world. Subsequently, a second CDC-sponsored field station, Projet Retro-CI, contributed to the body of research from in western Africa, documenting lower pathogenicity and transmission rates for HIV-2, which indicated that although HIV-2 was a cause of AIDS, it was unlikely to result in a pandemic.
Numerous other international collaborations on HIV/AIDS had influence far beyond research publications. Investigators from low- and middle-income countries were trained, university exchanges arranged, and numerous careers influenced and internationalized with incalculable effects. Many US and European universities established HIV training and research collaborations with their counterparts in developing countries. These relationships have built platforms upon which new initiatives, in areas such as maternal and child health, could be built. One of the lasting contributions of international HIV/AIDS work may be the training and empowering of professionals in low- and middle-income countries to influence health in their own countries.
Despite the advances in HIV prevention and treatment, the challenges remain daunting. In 1984, the US Secretary of Health and Human Services famously predicted the availability of an HIV vaccine within 2 years. Now, >25 years later, an effective vaccine remains elusive. Although billions of dollars have been expended on prevention research, an estimated 2.6 million persons acquire HIV annually. Only about a third of patients who qualify for treatment under the relatively conservative WHO guidelines actually receive it, and neither the optimal time for treatment initiation nor the optimal use of antiretroviral drugs to interrupt transmission have been determined. Tuberculosis remains a major killer of HIV-infected persons in Africa, our tools for combating it are outdated, and coordination between tuberculosis programs and HIV/AIDS programs remains less than optimal.
The AIDS Response, Nothing for Us without Us
Activism and advocacy profoundly influenced the response to HIV/AIDS. Outside the gay community, initial concern about HIV/AIDS was largely limited to scientists tracking the epidemic or searching for a cause. In the face of stigma, discrimination, and indifference to their friends dying, affected communities organized to provide prevention advice, care, and support. Community groups like Gay Men’s Health Crisis sprung up, delivering services and engaging in political activities. Organizations such as ACT UP undertook acts of civil disobedience to influence the research agenda, improve access to HIV drugs, and lower the cost of treatment.
Although early activists were predominantly American MSM, their work influenced other affected communities. When the magnitude of the epidemic in Africa became apparent, activists from the Northern Hemisphere contributed to demands for treatment access in the Southern Hemisphere. Vulnerable groups, including sex workers and IDU, made themselves heard internationally in an unprecedented way. “Nothing for us without us” captures the insistence of affected communities that they participate in the design of programs and interventions.
A key figure in the global response was Jonathan Mann, an epidemiologist from CDC who served as the founding director of Projet SIDA and was appointed in 1986 as the first director of WHO’s HIV/AIDS program. Mann recognized that the global spread of HIV/AIDS represented unequal vulnerability more than it did individual behavior, and he defined human rights as central to health and an effective HIV/AIDS response. He clashed with WHO leadership and bureaucracy and resigned in 1990. Tragically, Mann died in a plane crash in 1998.
Much has been written about the different ways that HIV/AIDS has been addressed, compared with other sexually transmitted infections, and the term AIDS exceptionalism has been coined. For example, specific consent forms and counseling were required before HIV testing, and limits were placed on sharing patient names between health jurisdictions for HIV surveillance purposes. These practices responded to concerns of affected communities that infected persons would be subject to discrimination such as termination of insurance or employment. Mandatory HIV testing, unhelpful and discriminatory, was largely prevented, but exceptionalist views may also have delayed expansion of HIV testing in clinical settings and thus access to care, including in the Southern Hemisphere. As HIV became treatable and surveillance practices successfully protected confidentiality, much of the exceptional approach to HIV gradually diminished.
Major human rights challenges persist, however. IDU and MSM suffer intense discrimination in many countries; their prevention needs are neglected and their very lives are sometimes in danger. Gender inequalities remain a driver of ill health. Increased attempts at criminalizing HIV transmission and continued travel restrictions for HIV-infected persons illustrate the enduring relevance of Jonathan Mann’s message.
AIDS and the Architecture of Global Health
HIV/AIDS played a major role in shaping current global health architecture. The threat posed by HIV led WHO to establish a dedicated program in 1986. In 1996, the Joint United Nations Programme on HIV/AIDS was established to coordinate the multisectoral response. In 2001, the United Nations General Assembly Special Session on HIV/AIDS, the first high-level summit ever devoted to a disease, committed the world to specific targets. In 2002, the Global Fund to Fight AIDS, Tuberculosis and Malaria was created, and a year later, US President G.W. Bush announced the President’s Emergency Plan for AIDS Relief, the largest bilateral health program ever undertaken. The scale-up of HIV/AIDS services has highlighted the need to focus on strengthening health systems and on other health-related Millennium Development Goals relating to maternal and child health.
The increase in actors in global health, including philanthropic organizations such as the Bill and Melinda Gates Foundation and the William J. Clinton Foundation, in part resulted from, but also coincided with, development of the global AIDS response. A result of the altered landscape is a diminution of the World Health Assembly’s influence on global decision making and WHO’s role in technical assistance. At the same time, HIV/AIDS demonstrated WHO’s unrivaled convening authority and the influence of its normative guidelines for global practice, such as for HIV/AIDS treatment. Major contributions from the Joint United Nations Programme on HIV/AIDS include global prioritization of HIV/AIDS and resource mobilization, epidemiologic monitoring, advocacy for treatment in low-income settings, and promotion of sound policies.
A problem with the early response in the United States as well as globally was an overemphasis on universal vulnerability, the concept that everyone is at risk. Predictions of widespread, generalized HIV/AIDS epidemics among heterosexual persons outside Africa, especially in Asia, were not borne out. The concept of “know your epidemic,” highlighting the need to focus interventions where HIV transmission is most intense, came surprisingly late, along with acknowledgment of the fundamentally different nature of the epidemic in sub-Saharan Africa compared with elsewhere.
Many countries with concentrated epidemics have had difficulty accepting that communities of MSM and IDU existed in their midst, let alone mounting targeted responses. Vigilance is required to ensure that resources are deployed to the right places in a timely fashion, rather than to general population groups that are politically safer but at lower risk. Characteristically, it has taken AIDS to bring the existence of marginalized groups such as sexual minorities to attention in low- and middle-income countries and to highlight their vulnerability and needs.
AIDS and the Future
We should not expect a single leader or intervention to deliver an abrupt end to the HIV/AIDS pandemic, yet the tide can be turned with principled pragmatism, adequate resources, trust in communities, and science as our guide. At times the process is slow. For example, US government support for needle and syringe exchange to prevent HIV in IDU did not happen until Barack Obama became US President (2009), and scale-up of male circumcision has been inadequate. But a middle way has to be found between arguments for the magic bullet of the moment and calls for unrealistic social and behavioral change with regard to sex and drug use.
We (the authors) have 4 priorities: 1) defining the best ways to use existing interventions to interrupt HIV transmission, 2) continuing the focused search for new knowledge and interventions, 3) resolving how best to use HIV testing and antiretroviral drugs for prevention as well as treatment, and 4) ensuring sustainability and commitment for the global response. Aspirations for social justice, human rights, and decency must motivate the response while epidemiology and surveillance provide technical direction as well as evaluation. True country and community ownership of the response is essential because solutions wanted more by donors or governments than by affected communities themselves almost never succeed.
Further success in HIV/AIDS prevention and treatment is challenged by numerous threats including fatigue and shifting priorities on the part of donors, the global financial downturn, and diversion of attention to other health problems plaguing the developing world. Better integration of HIV/AIDS efforts and interventions with those addressing maternal and child health are needed, and the global health infrastructure supported by HIV/AIDS scale-up will have to face the looming pandemic of noncommunicable diseases. Regardless how global health evolves, the unfinished agenda of HIV/AIDS must remain central.
Conclusions
Although we continue to face many challenges while responding to HIV/AIDS, we must also acknowledge the enormous scientific, social, and human achievements of the past 3 decades. The epidemic has severely tested many countries, especially those with the most limited resources, yet these countries have generally responded with decency, compassion, and good judgment. Despite the human and financial costs, millions of infections have been prevented and millions of life-years saved. The response to AIDS will be a benchmark against which responses to future health threats will be compared.
Many themes of the HIV/AIDS epidemic were captured by Albert Camus in his classic novel The Plague , and the expectations expressed therein largely apply. Inevitably, the story of HIV/AIDS “could not be one of final victory. It could be only the record of what had to be done, and what assuredly would have to be done again in the never-ending fight against terror and its relentless onslaughts.” An enduring frustration is that we will not know how the story of AIDS will finally end because the epidemic will outlast us. A perpetual challenge will be living up to the commitment and courage of those who went before—health workers, scientists, and affected persons—who faced the unknown and took risks. In general, 30 years of AIDS confirm that there is indeed “more to admire in men than to despise.” And while the epidemic continues, the world of global health has changed for the better.
Kevin M. De Cock is director of the Center for Global Health at CDC in Atlanta.
Suggested citation for this article : De Cock KM, Jaffe HW, Curran JW. Reflections on 30 years of AIDS. Emerg Infect Dis [serial on the Internet]. 2011 Jun [ date cited ]. http://dx.doi.org/10.3201/eid1706.100184
- What Are HIV and AIDS?
- How Is HIV Transmitted?
- Who Is at Risk for HIV?
- Symptoms of HIV
- U.S. Statistics
- Impact on Racial and Ethnic Minorities
- Global Statistics
- HIV and AIDS Timeline
- In Memoriam
- Supporting Someone Living with HIV
- Standing Up to Stigma
- Getting Involved
- HIV Treatment as Prevention
- Pre-exposure Prophylaxis (PrEP)
- Post-exposure Prophylaxis (PEP)
- Preventing Sexual Transmission of HIV
- Alcohol and HIV Risk
- Substance Use and HIV Risk
- Preventing Perinatal Transmission of HIV
- HIV Vaccines
- Long-acting HIV Prevention Tools
- Microbicides
- Who Should Get Tested?
- HIV Testing Locations
- HIV Testing Overview
- Understanding Your HIV Test Results
- Living with HIV
- Talking About Your HIV Status
- Locate an HIV Care Provider
- Types of Providers
- Take Charge of Your Care
- What to Expect at Your First HIV Care Visit
- Making Care Work for You
- Seeing Your Health Care Provider
- HIV Lab Tests and Results
- Returning to Care
- HIV Treatment Overview
- Viral Suppression and Undetectable Viral Load
- Taking Your HIV Medicine as Prescribed
- Tips on Taking Your HIV Medication Every Day
- Paying for HIV Care and Treatment
- Other Health Issues of Special Concern for People Living with HIV
- Alcohol and Drug Use
- Coronavirus (COVID-19) and People with HIV
- Hepatitis B & C
- Vaccines and People with HIV
- Flu and People with HIV
- Mental Health
- Mpox and People with HIV
- Opportunistic Infections
- Sexually Transmitted Infections
- Syphilis and People with HIV
- HIV and Women's Health Issues
- Aging with HIV
- Emergencies and Disasters and HIV
- Employment and Health
- Exercise and Physical Activity
- Food Safety and Nutrition
- Housing and Health
- Traveling Outside the U.S.
- Civil Rights
- Workplace Rights
- Limits on Confidentiality
- National HIV/AIDS Strategy (2022-2025)
- Implementing the National HIV/AIDS Strategy
- Prior National HIV/AIDS Strategies (2010-2021)
- Key Strategies
- Priority Jurisdictions
- HHS Agencies Involved
- Learn More About EHE
- Ready, Set, PrEP
- Ready, Set, PrEP Pharmacies
- Ready, Set, PrEP Resources
- AHEAD: America’s HIV Epidemic Analysis Dashboard
- HIV Prevention Activities
- HIV Testing Activities
- HIV Care and Treatment Activities
- HIV Research Activities
- Activities Combating HIV Stigma and Discrimination
- The Affordable Care Act and HIV/AIDS
- HIV Care Continuum
- Syringe Services Programs
- Finding Federal Funding for HIV Programs
- Fund Activities
- The Fund in Action
- About PACHA
- Members & Staff
- Subcommittees
- Prior PACHA Meetings and Recommendations
- I Am a Work of Art Campaign
- Awareness Campaigns
- Global HIV/AIDS Overview
- U.S. Government Global HIV/AIDS Activities
- U.S. Government Global-Domestic Bidirectional HIV Work
- Global HIV/AIDS Organizations
- National Black HIV/AIDS Awareness Day February 7
- HIV Is Not A Crime Awareness Day February 28
- National Women and Girls HIV/AIDS Awareness Day March 10
- National Native HIV/AIDS Awareness Day March 20
- National Youth HIV & AIDS Awareness Day April 10
- HIV Vaccine Awareness Day May 18
- National Asian & Pacific Islander HIV/AIDS Awareness Day May 19
- HIV Long-Term Survivors Awareness Day June 5
- National HIV Testing Day June 27
- Zero HIV Stigma July 21
- Southern HIV/AIDS Awareness Day August 20
- National Faith HIV/AIDS Awareness Day August 27
- National African Immigrants and Refugee HIV/AIDS and Hepatitis Awareness Day September 9
- National HIV/AIDS and Aging Awareness Day September 18
- National Gay Men's HIV/AIDS Awareness Day September 27
- National Latinx AIDS Awareness Day October 15
- World AIDS Day December 1
- Event Planning Guide
- U.S. Conference on HIV/AIDS (USCHA)
- National Ryan White Conference on HIV Care & Treatment
- AIDS 2020 (23rd International AIDS Conference Virtual)
Want to stay abreast of changes in prevention, care, treatment or research or other public health arenas that affect our collective response to the HIV epidemic? Or are you new to this field?
HIV.gov curates learning opportunities for you, and the people you serve and collaborate with.
Stay up to date with the webinars, Twitter chats, conferences and more in this section.
Reflection on 40 Years of HIV/AIDS Research
- Share on Facebook
- Share on Twitter
- Share on LinkedIn
- Share on Email
Cross-posted from NIH Office of AIDS Research

On June 5, 1981, the U.S. Centers for Disease Control and Prevention released a Morbidity and Mortality Weekly Report that first recognized the syndrome of diseases later named AIDS. June 5th also marks HIV Long-term Survivors Awareness Day.
Over the past 40 years, HIV/AIDS has evolved from a fatal disease to a manageable chronic illness with treatment. This progress is attributable in large part to the nation’s longstanding HIV leadership and contributions at home and abroad through the National Institutes of Health (NIH), the Office of AIDS Research (OAR), the President’s Emergency Plan for AIDS Relief (PEPFAR) at the U.S. Department of State Office of the Global AIDS Coordinator, the Ending the HIV Epidemic in the U.S. initiative (EHE) at the U.S. Department of Health and Human Services . It is important to recognize the U.S. Department of State, the Department of Defense, the U.S. Agency for International Development (USAID), U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID), the Centers for Disease Control and Prevention (CDC), and the U.S. Health Resources and Services Administration . The NIH, through its HIV Research Agenda, has contributions from the National Institute of Allergy and Infectious Diseases plus most of the Institutes, Centers, and Offices that receive HIV funding. The U.S. HIV/AIDS efforts continue as whole of government approach with international partners to overcome barriers to end the pandemic.
The NIH remains committed to supporting basic, clinical, and translational research to develop cutting-edge solutions for the ongoing challenges of the HIV epidemic. The scientific community has achieved groundbreaking advances in the understanding of basic virology, human immunology, and HIV pathogenesis, and have led the development of safe, effective antiretroviral medications and effective interventions to prevent HIV acquisition and transmission. Nevertheless, HIV remains a serious public health issue.
The OAR was established in 1988 to ensure that NIH HIV/AIDS research funding is directed at the highest priority research areas and to facilitate maximum return on the investment. OAR’s mission is accomplished in partnership within the NIH through the Institutes, Centers, and Offices (ICOs) that plan and implement specific HIV programs or projects, coordinated by the NIH HIV/AIDS Executive Committee. As I reflect on our advancements over the years (see the Progress Against HIV/AIDS Timeline on the OAR website), I would like to note the collaboration, cooperation, innovation, and other activities across the NIH ICOs in accelerating HIV/AIDS research.
Key scientific advances using novel methods and technologies have emerged in the priority areas of the NIH HIV research portfolio. Many of these advances derive from NIH-funded efforts, and all point to important directions for the NIH HIV research agenda in the coming years, particularly in the areas of new formulations of current drugs, new delivery systems, dual use of drugs for treatment and prevention, and new classes of drugs with novel strategies to treat viruses with resistance to current drug regimens.
Further development of long-lasting HIV prevention measures and treatments remains at the forefront of the NIH research portfolio on HIV/AIDS research. NIH-funded investigators continue to uncover new details about the virus life cycle, which is crucial for the development of next generation HIV treatment approaches. Additionally, the NIH is focused on developing novel diagnostics to detect the virus as early as possible after infection.
Results in the next two years from ongoing NIH-supported HIV clinical trials will have vital implications for HIV prevention, treatment, and cure strategies going forward. For example, two NIH-funded clinical trials for HIV vaccines, Imbokodo Exit Disclaimer and Mosaico Exit Disclaimer , are evaluating an experimental HIV vaccine regimen designed to protect against a wide variety of global HIV strains. These studies comprise a crucial component of the NIH’s efforts to end the HIV/AIDS epidemic.
As we close on four decades of research, I look forward to the new advances aimed at prevention and treatment in the years to come. To learn more about the OAR and how it catalyzes the NIH HIV/AIDS research investment, please visit the OAR website . In addition, you can find the statement here .
Maureen M. Goodenow, Ph.D. Associate Director for AIDS Research and Director, Office of AIDS Research National Institutes of Health
Related HIV.gov Blogs
- Anniversary Anniversary of first AIDS reports
- NIH National Institutes of Health
- OAR NIH Office of AIDS Research
- Subscribe Now
[Ilonggo Notes] Reflections on AIDS, 40 years since it was first reported
Already have Rappler+? Sign in to listen to groundbreaking journalism.
This is AI generated summarization, which may have errors. For context, always refer to the full article.
![hiv reflection essay [Ilonggo Notes] Reflections on AIDS, 40 years since it was first reported](https://www.rappler.com/tachyon/2021/11/tl-aids-40-ls.jpg)
In June 1981, cases of a rare lung infection, Pneumocystis carinii pneumonia (PCP), were reported in five young, previously healthy gay men in Los Angeles, followed by reports of an unusually aggressive cancer, Kaposi’s Sarcoma, in a group of men in New York and California. Cases suggested that the cause of the immune deficiency was sexual. In 1983, a new retrovirus, initially named HLTV-III, was identified as a possible cause. An antibody test was developed; major modes of transmission were identified, and blood supplies screening started. The US Centers for Disease Control (CDC) first used the term “AIDS,” describing it as “a disease with a defect in cell mediated immunity, occurring in a person with no known cause for diminished resistance.” In 2014, scientists at Oxford University concluded that HIV likely originated in or around Kinshasa in the Democratic Republic of Congo decades before it became a pandemic. It is believed that a hybrid form of the simian immunodeficiency virus (SIV) “jumped” from the Pan troglodytes chimpanzee to humans as a result of either blood exposure or ingesting bush meat.
I first heard about this strange illness in 1981, just after medical school. Little did I know that most of my work since then would be related to something so incurable and stigmatizing, that brought with it connotations of immorality, deviant behavior, divine punishment, and death.
In the early years, when this disease was without a name and of unknown cause, it was an “interesting topic” for medical conferences. A few years later, while doing medicals on refugees and migrants in Vietnam, the HIV antibody test became part of the screening procedures, but there were practically none who tested positive. I recall the first few cases detected in Vietnam – around 1990 – in several Thai fishermen who had been caught fishing illegally in Vietnamese waters, subsequently detained and then tested for HIV. Though they were well and had no symptoms, the discovery came as a shock to Vietnamese health authorities.
In 1992, while in the US for graduate studies, more was known about AIDS, its consequences so devastating; people were thrown out of their homes, and many ended up in hospices especially set up for them. I volunteered at one such place near the School of Public Health, run by the Missionaries of Charity, to help care and feed for people, who were merely wasting away waiting for the end. These years were rife with protests by groups like the AIDS Coalition to Unleash Power (ACT UP), against the government, religious authorities, and big pharma companies, with their famed slogan, “Silence=Death.” The LGBTQ+ rights movement was then gathering momentum. One of the most affecting events I have ever attended was the 1993 March on Washington, and the display of thousands of panels of AIDS quilts on the grounds of the National Mall, the only time in history that all the panels were shown together.
[Ilonggo Notes] A community-based approach to HIV in Western Visayas
![hiv reflection essay [Ilonggo Notes] A community-based approach to HIV in Western Visayas](https://www.rappler.com/tachyon/2021/04/tl-hiv-self-test-kit.jpg?fit=449%2C449)
In 1994, I attended one of the weekend HIV workshops of the Library Foundation and did consultancy work with HAIN (Health Action Information Network), visiting projects funded by the American Foundation for AIDS Research in four countries. There followed three pivotal AIDS-focused jobs between 1994 and 2007 – the Philippine HIV & AIDS NGO Support Program, UNDP, and the International AIDS Alliance. I also served on the Board of NGOs working on AIDS. From 2007 until the pandemic onset I was based in Cambodia as a freelance consultant; by 2020 I had worked in 25 countries – writing national strategic and operations plans for HIV, evaluating numerous UN, INGO, and local NGO programs, doing research, training and advising organizations on NGO governance, sexual health, TB, leprosy, LGBTQ+ rights and SOGIE (Sexual Orientation, Gender Identity and Expression), among other topics.
Meanwhile between 1995 and 2015 major steps towards AIDS prevention and control were achieved: AZT monotherapy gave way to HAART (Highly Active Anti-Retroviral Therapy) in 1996, but this reached the Philippines only years later. No country remained untouched; Africa became a hotbed and AIDS the main cause of death, setting back development gains by decades and decreasing life expectancies. By 1999, AIDS was the number four cause of death worldwide. New drugs and modalities of testing were developed and scaled up, condoms and needle exchange programs proven effective. The Joint UN Program on AIDS, UNAIDS, came into being in 1996, and the Global Fund for AIDS, TB, and Malaria started in 2002. AIDS became the first disease to have its own special session with the UN General Assembly. The UN included HIV in the MDGs in 2015 and in the SDGs for 2030. The French discoverers of the virus won a Nobel prize. Today, millions of people are on ART. Great progress has been made in many countries, new combination drugs have been developed, and the participation of PLHIV and affected communities is acknowledged. Vaccine development has not been successful. Of approximately 75 million cases worldwide, over 30 million have died.
HIV is a topic that no longer has the aura of death. People can safely have children, and and can think more about the future and getting older. Treatment and pre-exposure prophylaxis (PrEP) is available. I was a godparent to an HIV-positive couple in the mid-1990s, and “Liza,” as she was then known, went on to have a daughter. Yet, tragically, many in the Philippines still live in fear and stigma, not just because of their HIV status but because of the stigma surrounding being gay or transgender. 90-95% of all cases in the Philippines since 2008 have been in gay or bisexual males, and people are getting infected at a younger age. In 2015, HIV surveillance studies showed that in some cities 8.9% (or up to 1 in 11 men who have sex with men) above the age of 25 is HIV-positive.
It is 2021 but in the Philippines, one in six persons is in the late stage by the time they are diagnosed, indicating they have had HIV for several years prior to getting a test. There are low rates of HIV testing and condom use in the most vulnerable and high risk populations, there is still opposition to comprehensive sexuality education, sexual debut is getting younger, and children are having children. Many deaths still go unreported or are labeled as pneumonia, generalized infections, or TB. The Philippine epidemic is still expanding, while in other countries rates are declining. Since 2017 the country has the dubious title of having the greatest rate of rise of HIV worldwide. If things don’t improve radically, in the next few years, the country will fail to meet the Sustainable Development Goals in 2030, an echo of its failure to reach the 2015 MDGs.
UNAIDS to PH: Don’t ‘drop the ball’ on fight against HIV

The Philippine timeline
1984 Two cases of suspected AIDS in Filipino-Americans at a military base outside Manila, results only confirmed in 1986.
1985 The first known case of AIDS in a Filipino reported. In December, seven sero-positives in female sex workers working in the vicinity of the US bases are detected
1986 DOH declares AIDS a notifiable disease.
1987 The National AIDS Program is organized. The AIDS Study Group at RITM Is formed.
1988 The Philippines reports its 100 th case. The AIDS Registry is set up. The First Medium Term Plan for AIDS is developed.
1989 DOH issues 12 policy thrusts for AIDS. RITM and Kabalikat, an NGO, start working with female sex workers in the Ermita and Malate areas.
1990 Initial mass media campaigns on AIDS Organized in Metro Manila. Remedios AIDS Information Center starts the first AIDS hotline services. Condom social marketing starts.
1991 Several Philippine NGOs start working on HIV awareness and education, with USAID funding.
1992 Among Asian/Pacific Islanders, Filipinos post the highest number of cases of AIDS in San Francisco, Hawaii, New York, and Los Angeles. Dolzura Cortez is the first person to reveal she has AIDS. Her story becomes a film, Dahil Mahal Kita (Because I Love You: The Dolzura Cortez Story) . The Philippine National AIDS Council (PNAC) is convened, with government agencies and NGOs as members. First support group for People with HIV formed.
1993 The HIV/AIDS NGO Network Philippines is established . First International AIDS Video and Poster festival is held. National HIV surveillance started by DOH, supported by USAID.
1994 Sarah Jane Salazar goes public with her diagnosis; a film, Secrets of Sarah Jane , released. Pinoy Plus, a PLHIV group, is organized. Reach Out’s “Condom Café” in Makati City is shut down by authorities a day after it opened amid protests by religious groups, and the local government calls it “obscene.”
1995 Construction of Bahay Lingap, a halfway and treatment home for PLHIV opens.
1996 The family of Fil-Canadian singer and actor Rodel Naval confirms he had AIDS when he passed away in 1995. Presidential proclamation 888 declares 1997 as National AIDS Prevention year.
1997 The Philippines hosts the 4 th International Congress on AIDS in Asia and the Pacific, with the AIDS Society of the Philippines as the organizer . Policies and strategies for STD & HIV prevention launched by DOLE, DECS, DFA, and DILG.
1998 Positive Action Pilipinas Foundation, Inc.(PAFPI) is organized. The AIDS Law, RA 8504, is passed and hailed as “good practice” for AIDS legislation.
2000 A “buyers club” is organized to purchase generic ARVs in bulk through an agreement with a pharmaceutical company; 16 people start treatment . Sarah Jane dies of AIDS complications at the age of 25.
2001 Local AIDS Councils organized.
2003 Molecular studies of HIV in the Philippines show predominant subtype to be subtype B, virtually unchanged since the 1990s. Actress Kris Aquino accuses her live-in partner of giving her an STD and physical abuse, raising much awareness on STIs, domestic violence, and gender relations.
2006 ART is supported through the Global Fund, with 170 people started on treatment at RITM and San Lazaro Hospitals.
2007 The PH epidemic, said to be “low and slow” from the past 20 years, now seems to be “hidden and growing,” as one case a day is reported, double that of 2005.
2008 DOH announces that there are now more reported cases of sexual transmission from homosexual and bisexual males. Wanggo Gallaga, son of film director Peque Gallaga, goes public. This signals a shift in the face of HIV in the country. Reported cases of HIV increase by 65% over the previous year. Six treatment hubs are funded.
2009 The Philippine epidemic is said to be transitioning from “hidden and growing” to “fast and furious.” Number of cases reported in 2009 has more than doubled compared to 2007.
2010 147 PWID are found to be HIV-positive in Cebu City, a gigantic leap from the eight cases from 1985-2009. This is 9% of all new HIV cases recorded for the year. For the first time over 1,000 cases a year are reported.
2011 “Red Whistle” founded by Niccolo Cosme and friends after they noticed people around them were contracting the virus at an alarming rate.
2012 Reproductive Health Bill signed into law on December 21, 2012 (RA 10354). 16 ART sites are operational in the Philippines, 3,643 under treatment
2013 Sero surveillance of PWID in Cebu shows 44.9% positive; HIV prevalence nationwide in FSW remains low at <1%.
2014 There are now 19 ART sites, treating 8219 people.
2015 Philippines records 7809 new cases (21/day) and fails to reach the MDG targets for reducing HIV. 5% of gay and MSM nationwide are positive, with 8.9% prevalence among those above 25 years.
2016 H airdresser Ricky Reyes is found guilty of AIDS-related discrimination against an employee and pays damages. 9,238 new cases for the year, the highest ever, equivalent to 25.3 new cases a day, or roughly one new case every 57 minutes.
2017 The President signs an executive order calling for universal access to modern family planning methods and the accelerated implementation of the country’s RH law. Research shows that the molecular epidemiology of HIV in the country has shifted since the 1990s-2009, with the “more aggressive” subtype ORF O1-AE more predominant. 11,101 cases for the year (30/day), a record. The country gains the dubious distinction of having the highest rates of rise of HIV worldwide. Philippine domestic funding for HIV now makes up 80% of overall funding for the response.
2018 AIDS Registry starts to differentiate transgender women in its reporting. They comprise 2-3% of all cases recorded since. Homosexual and bisexual males now make up 90-95% of all cases. Republic Act 11166 becomes law. It defines HIV and AIDS education as a right, provides for HIV testing without the need for parental consent for those between 15 to 17; ensures free treatment is provided. 88 ART sites operating, with 33,479 on treatment.
2019 12,728 new cases of HIV in a year (35 new cases each day, one every 41 minutes, another record). A pilot program providing PrEP to 250 gay and other MSM is started. 126 treatment sites in the country with 47,977 on treatment. Despite the big increase, this is merely 42% of all PLHIV in the country.
2020 COVID-19 hits, resulting in lockdowns and large scale disruptions of health services. Fewer testing, diagnoses, and treatment, a reversal of the trends for the past decade. The % of people in later stages of HIV at the time of diagnosis climbs up to 20%, compared to 12% from 2009-2019. Health authorities and NGOs devise innovative ways to counsel, test, and get ART to clients. It is estimated that 68% of PLHIV know status, 42% are on treatment. Only 26% of pregnant women with HIV are on PMTCT.
2021 40 years since the first reports of the disease. By end-September, registered cases hit 90,960, with 54,022 on treatment. There are 33 new infections a day, a 50% increase from 2020, only slightly lower than 35 cases/day in 2019. UNAIDS estimates that the number of HIV cases is 133,000. The “treatment gap” is widening, as the country cannot keep up with getting people on treatment as fast as they should be. – Rappler.com
Vic Salas is a physician and public health specialist by training, and now retired from international consulting work. He is back in Iloilo City, where he spent his first quarter century.
Add a comment
Please abide by Rappler's commenting guidelines .
There are no comments yet. Add your comment to start the conversation.
How does this make you feel?
Related Topics
Recommended stories, {{ item.sitename }}, {{ item.title }}, nfl distances itself from player’s controversial speech on women, lgbtq issues.

Peru protesters slam new insurance law that deems transgender people mentally ill

Marina Summers has no regrets over ‘Drag Race: UK vs. the World’ run
How fashion designer Jude Macasinag uses haute couture for queer visibility
Refusing to be invisible: Intersex Filipinos struggle to be seen, understood

public health
Philippine heat has always been a problem – and it’s going to get worse.

Sodex Mobile Clinic to give free family-planning services in Luzon

DOH raises concern over increasing HIV/AIDS cases in Bicol

Boys should be included in HPV vaccination drive – specialist

The Green Report: It’s getting hotter – now what?

Checking your Rappler+ subscription...
Upgrade to Rappler+ for exclusive content and unlimited access.
Why is it important to subscribe? Learn more
You are subscribed to Rappler+

- WORLD Herstory
- WORLD Staff
- Outreach & Linkage
- Peer Advocacy
- PrEP Navigation
- WORLD Retreats
- WORLD Leadership Institute
- SUN Project
- 30th Anniversary Celebration
- Get the Vax
- Get Involved
Reflections on Women and Girls HIV/AIDS Awareness Day
We have all heard the facts about HIV and AIDS. The statistics are broken down by race, gender, age, nation, and every conceivable data driven segmentation.
-Epidemiological data tells us that over 35 million people are living with HIV worldwide and approximately 18 million, over half, are women.
-HIV is the world’s leading infectious killer.
-An estimated 39 million people have died since the first cases were reported in 1981.
-More than 1.5 million people died of AIDS-related causes in 2013.
These are the commonly cited facts we are all too familiar with. And they represent nothing less then a human tragedy of cataclysmic proportions. But numbers and statistics cannot fully represent what this means for the everyday lived experiences of individuals, families and communities.
Women are often the primary caregivers for their families; the custodians for the health of their children, partners, aging parents and extended families. Their own health priorities often fade into the background, even if they are living with HIV. This means women who are living with the virus are often juggling earning a living, family care-giving, and managing their own life-saving health regimen.
Too often, they must accomplish all this while being careful not to disclose their HIV status for fear of violence or harassment that could affect the quality of life for themselves or their family, even being at personal risk of death.
Women’s stories tell us it is about more than just statistics. Statistics have a margin of error—a margin that often negatively affects those who live on the margins of social, economic, and political injustice; the vast majority of whom are women and children.
How many of us know that AIDS related illnesses are the leading cause of death among women of child bearing age globally? We have conquered mother to child transmission, but women are still dying.
Every minute one young woman becomes HIV-positive, with young women aged 15-24 in sub-Saharan Africa are twice as likely to be living with HIV than young men. Black women are 16 times more likely than white women to acquire HIV.
This must change!! In too many rooms, at too many tables, women who are fighting these health disparities and advocating for health equity are asked, “What do women want?” as if these facts do not exist and women’s lives and issues are secondary to that of men.
It is not a complicated answer for women and those who love them. It is embodied in the WORLD mission.
We envision a world where women, girls, and families affected by HIV and AIDS have the tools, support and knowledge to live healthy and productive lives with dignity. Our vision is rooted in a commitment to human rights and wellness with the understanding that this includes freedom from violence; access to housing; quality healthcare; food security; physical, spiritual and emotional wellbeing; education and economic justice.
Nothing more, nothing less.
In sisterhood and solidarity,
Cynthia Carey-Grant, Executive Director
Following are WAGHAAD reflections from WORLD staff and members of the community:
“While most people know that March is Women’s History Month, many people do not know about the many important holidays recognizing women that make up Women’s History Month. Two days that WORLD wants to acknowledge are International Women’s Day (March 8th) and National Women and Girls’ HIV/AIDS Awareness Day (March 10th). These two important days ring especially important to WORLD as one acknowledges the rights of women as important and contributing members of society while the other recognizes the importance of supporting women’s health and well-being. We live in a time where funding for HIV education and prevention dwindles, and the number of women living with HIV rises. WORLD is calling on women and those who love women to do two things. First of all, update your status! Today is an excellent day to show your girlfriend, daughter, sister, or friend some love by going together to get an HIV test and to talk with each other or with your provider about safer sex options. Secondly, today and everyday, demand that your representatives support funding for HIV education, prevention, and treatment services. While treatment as prevention is an excellent tool in the fight against HIV, it is shameful to deplete funding from other tools at our disposal! Our communities deserve the educational support to prevent HIV and all health disparities! In recognition of National Women and Girl’s HIV/AIDS Awareness Day, International Women’s Day, and every day that women act as caregivers, leaders, movers and shakers, WORLD honors all women and girls living with HIV and affected by HIV. And today especially, WORLD honors all girls who deserve the education and support to help us get to an AIDS Free Generation.” – Ashley Fairburn, Outreach and Linkage Specialist
“Women and Girls HIV Awareness Day should be every day. Because every day we laugh, we communicate, we share, we love, we are girls and we are women…” -Nikia Harris, Outreach and Linkage Specialist
“National Women and Girls HIV Awareness Day is not only an opportunity for us to recognize the extraordinary strength, perseverance, and vibrancy of all women who are living with the virus, but also an occasion for us to share our stories. If we want to curb and eventually end the transmission of HIV among women, we have to be able to have conversations about what sex and prevention look like in the real world. In a month where so much focus is placed on how far women have advanced throughout history, I believe it is vitally important to share our knowledge about our bodies and ourselves so that from granny to grandchild, we are empowered to take charge of our own health!” -Dietz, Outreach and Linkage Specialist
“Women and Girls HIV Awareness Day this year is very important to me because we’re including young girls ages 12-24 at our event and I think that’s the age group when it really matters about HIV and STDs. I feel if I had somebody to talk me around this age, it could have made a difference in my life. I think Women and Girls HIV Awareness Day should be more then once a year.” -Felecia Greenly, Peer Advocate
“Women and Girls HIV/AIDS Awareness Day is the perfect opportunity to take a look at where we are with the HIV/AIDS epidemic among women and where we want to be. Through a commitment to keeping an open dialogue about HIV/AIDS, we can reduce stigma and ensure that all women and girls have access to information about HIV/AIDS and know how to protect themselves.” -Stephanie Cornwell, Program Services Director
“As I recall, there were specific subjects and conversations that were taboo in our Catholic Black home between my mother and I. We did not discuss molestation, trauma, same sex relationships or STDs. It wasn’t until my late 30s after Dad had died, my girlfriend and I moved in together and Magic Johnson disclosed his status that a real dialogue between my mother and I began. It was amazing to hear how much my mom didn’t know about her own body. I’m not waiting more than half my life to start the conversation with my daughters.” -unknown
“When I was 12, I found Banana Flavored candies in my Grandmother’s purse. When I was 22 my Grandmother finally shared her Banana Pudding Recipe. When I was 32 I found a Banana Flavored condom in my Grandmother’s top drawer. I don’t like Bananas anymore.” -Anonymous
“On this special day, I reflect on the impact of HIV/AIDS in the lives of women around the world. With so many tools to prevent HIV transmission and to control the virus replication in HIV+ women today, there are more reasons to be optimistic that we will conquer this virus and end the global pandemic.
But there is no room for complacency. Women and men of color remain at disproportionate risk for contracting HIV. During the last recession, funding for HIV prevention and education was all but eliminated. In place of education we are left with the bio-medical prevention model, which relies on testing and linking HIV+ individuals to high quality healthcare. The obvious weakness of this model is that it leaves the people most at risk for contracting HIV with little or no education about how the disease is transmitted or how to protect oneself.
No one today would dispute the unethical and dangerous ‘science’ practices used to experiment on African Americans in Tuskegee. Why are we left with a nearly non-existent public education effort when people of color overwhelmingly constitute the number of new cases of HIV infection?
Today, in all of the highest risk categories-men who have sex with men, women and youth-people of color are disproportionately impacted by HIV. Yet no public education campaigns are directed to these populations. None.
The outcome of this continued neglect is quite foreseeable. Entire populations will become dependent upon pharmaceutical and insurance companies for their health.
In the early days of the epidemic, ACT-UP declared that “Silence equals death.” Now we are in danger that continued silence will equal perpetual dependence. Let’s find our voices again and raise them to demand that funding for public education about HIV prevention is restored in our communities.” -Kabir Hypolite, WORLD Board Member
Essay on AIDS for Students and Children
500+ words essay on aids.
Acquired Immune Deficiency Syndrome or better known as AIDS is a life-threatening disease. It is one of the most dreaded diseases of the 20 th century. AIDS is caused by HIV or Human Immunodeficiency Virus, which attacks the immune system of the human body. It has, so far, ended more than twenty-nine million lives all over the world. Since its discovery, AIDS has spread around the world like a wildfire. It is due to the continuous efforts of the Government and non-government organizations; AIDS awareness has been spread to the masses.

AIDS – Causes and Spread
The cause of AIDS is primarily HIV or the Human Immunodeficiency Virus. This virus replicates itself into the human body by inserting a copy of its DNA into the human host cells. Due to such property and capability of the virus, it is also known as a retrovirus. The host cells in which the HIV resides are the WBCs (White Blood Cells) that are the part of the Human Immune system.
HIV destroys the WBCs and weakens the human immune system. The weakening of the immune system affects an individual’s ability to fight diseases in time. For example, a cut or a wound takes much more time to heal or the blood to clot. In some cases, the wound never heals.
HIV majorly transmits in one of the three ways – Blood, Pre-natal and Sexual transmission. Transfusion of HIV through blood has been very common during the initial time of its spread. But nowadays all the developed and developing countries have stringent measures to check the blood for infection before transfusing. Usage of shared needles also transmits HIV from an infected person to a healthy individual.
As part of sexual transmission, HIV transfers through body fluids while performing sexual activity. HIV can easily be spread from an infected person to a healthy person if they perform unprotective sexual intercourse through oral, genital or rectal parts.
Pre-natal transmission implies that an HIV infected mother can easily pass the virus to her child during pregnancy, breastfeeding or even during delivery of the baby.
AIDS – Symptoms
Since HIV attacks and infects the WBCs of the human body, it lowers the overall immune system of the human body and resulting in the infected individual, vulnerable to any other disease or minor infection. The incubation period for AIDS is much longer as compared to other diseases. It takes around 0-12 years for the symptoms to appear promptly.
Few of the common symptoms of AIDS include fever , fatigue, loss of weight, dysentery, swollen nodes, yeast infection, and herpes zoster. Due to weakened immunity, the infectious person falls prey to some of the uncommon infections namely persistent fever, night sweating, skin rashes, lesions in mouth and more.
Get the huge list of more than 500 Essay Topics and Ideas
AIDS – Treatment, and Prevention
Till date, no treatment or cure is available for curing AIDS, and as a result, it is a life-threatening disease. As a practice by medical practitioners, the best way to curb its spread is antiretroviral therapy or ART. It is a drug therapy which prevents HIV from replicating and hence slows down its progress. It is always advisable to start the treatment at the earliest to minimize the damage to the immune system. But again, it is just a measure and doesn’t guarantee the cure of AIDS.
AIDS prevention lies in the process of curbing its spread. One should regularly and routinely get tested for HIV. It is important for an individual to know his/her own and partner’s HIV status, before performing any sexual intercourse activity. One should always practice safe sex. Use of condoms by males during sexual intercourse is a must and also one should restrict oneself on the number of partners he/she is having sex with.
One should not addict himself/herself to banned substances and drugs. One should keep away from the non-sterilized needles or razors. Multiple awareness drives by the UN, local government bodies and various nonprofit organizations have reduced the risk of spread by making the people aware of the AIDS – spread and prevention.
Life for an individual becomes hell after being tested positive for AIDS. It is not only the disease but also the social stigma and discrimination, felling of being not loved and being hated acts as a slow poison. We need to instill the belief among them, through our love and care, that the HIV positive patients can still lead a long and healthy life.
Though AIDS is a disease, which cannot be cured or eradicated from society, the only solution to AIDS lies in its prevention and awareness. We must have our regular and periodical health checkup so that we don’t fall prey to such deadly diseases. We must also encourage and educate others to do the same. With the widespread awareness about the disease, much fewer adults and children are dying of AIDS. The only way to fight the AIDS disease is through creating awareness.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App

Reflection: HIV Testing in Africa Essay (Critical Writing)
Introduction, feelings on scenario, ethical theories.
Africa is a continent constantly plagued by drought, disease, and military conflicts. The standards of living here are very low, and the average life expectancy in countries like Zimbabwe does not exceed 33 years (De Wet, 2019). HIV contributes greatly to the death statistic and affects around 9% of the population in Sub-Saharan Africa (De Wet, 2019). Two opposing views on what must be done are presented by Dr. Meadows and Dr. Williams. Dr. Meadows believes that the key lies in eliminating barriers to condom distribution and greater engagement with suppliers. Dr. Williams claims that it would not be enough, and mandatory HIV testing is necessary for preventing HIV/AIDS from spreading. The point of contention lies in the ethics of forcing individuals to undergo tests versus the allegedly less effective method of condom distribution.
I think that the option presented by Dr. Williams is the most ethical because it does not explicitly violate an individual’s right to privacy while offering great improvements. Dr. Meadows’ stance is understandable, but it relies on too many factors to be effective. No amount of advocacy will change the minds of religious fundamentalists. In addition, restraint is the best form of defense against HIV/AIDS. Therefore, I strongly support mandatory testing for the disease in Africa.
The ethical theory of utilitarianism relies on the balance of positive and negative factors in comparison to one another. If an action benefits most people without severely disenfranchising minorities, then it can be considered good (Pence, 2017). Mandatory testing will infringe on the right to choose, but at the same time will save numerous lives. If anonymity is preserved and everyone is made to submit to the test, then there are virtually no downsides. Thus, from a utilitarian point of view, Dr. Williams’s stance is ethical.
HIV/AIDS is an incurable disease that is very widespread in Africa. Cultural and logistical barriers prevent widespread condom distribution in the area. Mandatory testing will allow everyone to know whether they are infected or not. It will enable them to make conscious choices about sex. The negative sides of the practice can be mitigated by following proper patient anonymity protocols. I believe Dr. Williams is right in this situation.
De Wet, K. (2019). The normalization of the HIV and AIDS epidemic in South Africa . Routledge.
Pence, G. (2017). Medical ethics: Accounts of ground-breaking cases (8th ed.). McGraw-Hill.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, March 22). Reflection: HIV Testing in Africa. https://ivypanda.com/essays/reflection-hiv-testing-in-africa/
"Reflection: HIV Testing in Africa." IvyPanda , 22 Mar. 2024, ivypanda.com/essays/reflection-hiv-testing-in-africa/.
IvyPanda . (2024) 'Reflection: HIV Testing in Africa'. 22 March.
IvyPanda . 2024. "Reflection: HIV Testing in Africa." March 22, 2024. https://ivypanda.com/essays/reflection-hiv-testing-in-africa/.
1. IvyPanda . "Reflection: HIV Testing in Africa." March 22, 2024. https://ivypanda.com/essays/reflection-hiv-testing-in-africa/.
Bibliography
IvyPanda . "Reflection: HIV Testing in Africa." March 22, 2024. https://ivypanda.com/essays/reflection-hiv-testing-in-africa/.
- Drivers of HIV and AIDS in Sub-Saharan Africa and San Francisco
- Great Zimbabwe History Overview: The Ancient Mystery in Southern Africa
- Madonna of the Meadows and Madonna of the Long Neck
- Discharge Process Improvement in Acute Care
- Effects of Racism on Mental Health Article by Kwate and Goodman
- Key Players in US Healthcare: USPSTF, MedPAC, and CDC
- Education Material for a Dialysis Patient
- Danger of Female Circumcision

IMAGES
VIDEO
COMMENTS
Essay about HIV-AIDS reflection instructions: use the guide questions in writing your reflection, minimum of 200 words. guide questions: how are you going to. ... (PTSD ) reflection essay; Importance of having fire and earthquake drills yearly in school; Legalizing the use of marijuana in the country essay; Pain - essay; Related Studylists nurs205.
Objectives. Approximately 32.7% of people living with HIV/AIDS (PLWHA) in the U.S. are now over the age of 50. Women comprise a significant percentage of the U.S. HIV epidemic and the percentage of women diagnosed with HIV continues to grow; however, little is known about women's experiences living and coping with HIV over time.
The HIV/AIDS pandemic has evolved in parallel with other global health events that necessarily influence how HIV/AIDS is perceived and prioritized. In a 2012 paper, author K.D.C. suggested that global health trends could best be analyzed through the lenses of development, public health, and health security . The fourth decade of AIDS started in ...
Greg Louganis is a gold-medal-winning Olympic diver and author. He tested positive for HIV in 1988 and has become a prominent and inspirational activist. It has been almost 25 years since I was diagnosed with HIV. At the time the only drug we had available for treatment was AZT. The prescription for AZT was two pills every four hours around the ...
A reflection on the 25 year history of AIDS can begin with no better outline than that provided by the late Jonathan Mann of WHO. A slide he gave to me in the late 1980's divides the history of AIDS into four periods: (see fig. 1 ). Jonathan could not know that the period of silent spread (part 1 of this saga) of HIV actually began years earlier.
Despite this scientific progress, HIV remains incurable and no vaccine has been proven effective. Meanwhile, HIV has progressed to infect over 60 million, now becoming the world's fourth leading cause of death. The global impact of AIDS has yet to peak with estimates of new infections still exceeding deaths by millions per year.
By Mabor Chadhuol. World AIDS Day marks a special day of reflection, compassion and unity in the fight against HIV/AIDS around the World. The first ever-global health day has been celebrated on December 1 for more than two decades. The day enables people to show support and passion for HIV positive people and commemorate loved ones who have died from AIDS-related illnesses.
HIV/AIDS played a major role in shaping current global health architecture. The threat posed by HIV led WHO to establish a dedicated program in 1986. In 1996, the Joint United Nations Programme on HIV/AIDS was established to coordinate the multisectoral response. In 2001, the United Nations General Assembly Special Session on HIV/AIDS, the ...
The. HIV/AIDS catastrophe has been one of the defining features of the past quarter of a century. Although it is short-lived in the scheme of public-health crises, the pandemic ranks among the ...
As the 2013-16 director of APA's HIV/AIDS Programs, David J. Martin revamped the office's efforts to reflect developing realities about HIV/AIDS and to advocate for social science solutions to HIV-related problems. Below is his reflection on the early challenges of HIV/AIDS prevention and treatment. I saw my first AIDS patient in 1983, a ...
June 5th also marks HIV Long-term Survivors Awareness Day. Over the past 40 years, HIV/AIDS has evolved from a fatal disease to a manageable chronic illness with treatment. This progress is attributable in large part to the nation's longstanding HIV leadership and contributions at home and abroad through the National Institutes of Health (NIH ...
The ten essays in this volume look at the many and complex relationships between HIV/AIDS and education. It is clear that education in an AIDS-infected world cannot be the same as that in an AIDS-free world. It is imperative to adapt educational planning and management principles, curriculum-development goals, and the provision of education itself, in order to take into account this pandemic ...
Let him call for the elders of the church, and let them pray over him, anointing him with oil in the name of the Lord. And the prayer of faith will save the one who is sick, and the Lord will raise him up. And if he has committed sins, he will be forgiven. Personal reflection. HIV is an issue I was interested in doing because personally I was ...
Only 26% of pregnant women with HIV are on PMTCT. 2021 40 years since the first reports of the disease. By end-September, registered cases hit 90,960, with 54,022 on treatment. There are 33 new ...
Reflection Paper on Hiv/Aisd. The first cases of acquired immunodeficiency syndrome (AIDS) were reported in the United States in the spring of 1981. By 1983 the human immunodeficiency virus (HIV), the virus that causes AIDS, had been isolated. Early in the U.S. HIV/AIDS pandemic, the role of substance abuse in the spread of AIDS was clearly ...
The statistics are broken down by race, gender, age, nation, and every conceivable data driven segmentation. -Epidemiological data tells us that over 35 million people are living with HIV worldwide and approximately 18 million, over half, are women. -HIV is the world's leading infectious killer. -An estimated 39 million people have died since ...
500+ Words Essay on AIDS. Acquired Immune Deficiency Syndrome or better known as AIDS is a life-threatening disease. It is one of the most dreaded diseases of the 20 th century. AIDS is caused by HIV or Human Immunodeficiency Virus, which attacks the immune system of the human body. It has, so far, ended more than twenty-nine million lives all ...
Williams claims that it would not be enough, and mandatory HIV testing is necessary for preventing HIV/AIDS from spreading. The point of contention lies in the ethics of forcing individuals to undergo tests versus the allegedly less effective method of condom distribution.
703. Pages: 2. This essay sample was donated by a student to help the academic community. Papers provided by EduBirdie writers usually outdo students' samples. Cite this essay. Download. The Philippines belong to most countries who experiencing the continually epidemic HIV, human immune deficiency virus that can destroy your immunity ...
REFLECTION PAPER HIV/AIDS AWARENESS. Honestly before the webinar started I only had a little knowledge about HIV/AIDS, I didn't even know the meaning of those two terms. This webinar is entitled HIV/AIDS AWARENESS WEBINAR by Mr. Mark Benedict. This is very important to me. It is not only for compliance but this will help me to gain more ...