- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
October 30, 2023
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source

FDA approves mirikizumab, a promising induction and maintenance therapy for ulcerative colitis
by The Mount Sinai Hospital
The U.S. Food and Drug Administration (FDA) approved mirikizumab, on October 26, 2023, a highly effective new treatment for ulcerative colitis (UC), offering a new option to patients battling this chronic and debilitating inflammatory bowel disease.
This therapy offers a safe and effective treatment option for patients with moderate-to-severely active UC who have yet to achieve rapid and lasting improvements on currently available therapies. Unlike existing treatments for UC, mirikizumab also offers relief from a key symptom—bowel urgency—that greatly impacts patients' quality of life.
Ulcerative colitis affects millions of people worldwide. The induction and maintenance of remission are critical goals in the management of UC. However, existing therapies may not provide sufficient efficacy or patients may have trouble tolerating them.
"Mirikizumab is the first antibody targeting p19/interleukin-23 to be approved for the treatment of ulcerative colitis . Its performance in both induction and maintenance phases of the clinical trials is truly impressive," said Bruce Sands, MD, MS, senior author of the clinical trial study published in the New England Journal of Medicine ( NEJM ). Dr. Sands is Chief, Dr. Henry D. Janowitz Division of Gastroenterology, Mount Sinai Health System, and the Dr. Burrill B. Crohn Professor of Medicine, Icahn School of Medicine at Mount Sinai. Dr. Sands is also a paid consultant for Lilly U.S., LLC.
"The Lucent program was the first clinical trial program that addressed bowel urgency in a meaningful way," said Marla C. Dubinsky, MD, co-author of the NEJM study, Co- director, Susan and Leonard Feinstein Inflammatory Bowel Disease Clinical Center, and Professor of Pediatrics, and Medicine, Icahn Mount Sinai. "It is one of the most burdensome patient-reported symptoms, and a drug that achieves bowel urgency remission is an outcome of great importance to our patients with UC."
As published in NEJM , mirikizumab demonstrated exceptional results in both the induction and maintenance arms of the phase 3, randomized, double-blind, placebo-controlled trials in adults with moderately-to-severely active UC.
Induction Phase (LUCENT-1 Trial)
During the induction phase, the LUCENT-1 trial evaluated the efficacy of mirikizumab in inducing clinical remission at week 12 in patients with moderate to severely active UC.
The study enrolled 1,281 patients who were randomized 3:1 to receive intravenous 330mg mirikizumab or placebo every four weeks for 12 weeks. A significantly greater proportion of mirikizumab-treated patients achieved clinical remission at week 12 (mirikizumab: 24.2%; placebo: 13.3%; p<0.001).
Maintenance Phase (LUCENT-2 Trial)
In the maintenance phase, the LUCENT-2 trial assessed the potential of mirikizumab to maintain clinical remission in patients who had achieved a clinical response in the induction phase. This phase enrolled 544 patients who were re-randomized 2:1 to receive mirikizumab 200 mg or placebo subcutaneously every four weeks for 40 weeks (mirikizumab: 49.9%; placebo: 25.1%; p<0.001).
All major secondary endpoints were achieved in both trials, including clinical response, endoscopic remission, and bowel urgency. Bowel urgency, in particular, was tremendously improved in patients who responded to the treatment, an important achievement because relief from this symptom is a major unmet patient need.
Mirikizumab demonstrated a favorable safety profile in both trials, with adverse events consistent with those expected in this patient population. These safety findings further support the potential of mirikizumab as a well-tolerated therapy for long-term use. The data showed not only rapid relief of symptoms but also the potential to maintain remission over the long term.
Explore further
Feedback to editors

Study finds jaboticaba peel reduces inflammation and controls blood sugar in people with metabolic syndrome
45 minutes ago

Study reveals how extremely rare immune cells predict how well treatments work for recurrent hives
2 hours ago

Researchers find connection between PFAS exposure in men and the health of their offspring

Researchers develop new tool for better classification of inherited disease-causing variants

Specialized weight navigation program shows higher use of evidence-based treatments, more weight lost than usual care

Exercise bouts could improve efficacy of cancer drug

Drug-like inhibitor shows promise in preventing flu

Scientists discover a novel way of activating muscle cells' natural defenses against cancer using magnetic pulses
3 hours ago

Cancer drug shows powerful anti-tumor activity in animal models of several different tumor types
4 hours ago

Ultra-processed foods increase cardiometabolic risk in children, study finds
Related stories.

New drug application doubles rates of remission in patients with ulcerative colitis
Jun 28, 2023

Two new studies evaluate agents for treating ulcerative colitis
Sep 27, 2019

FDA approves Skyrizi for moderately to severely active Crohn disease
Jun 20, 2022

Ozanimod beats placebo for ulcerative colitis
Sep 30, 2021

FDA approves velsipity for moderate-to-severe ulcerative colitis in adults
Oct 18, 2023

Upadacitinib superior to placebo in moderate-to-severe Crohn disease
May 31, 2023
Recommended for you

Second Phase 3 clinical trial again shows dupilumab lessens disease in COPD patients with type 2 inflammation
May 20, 2024

Low-dose iron supplementation has no benefit for breastfed infants, shows study

Acetaminophen shows promise in warding off acute respiratory distress syndrome, organ injury in patients with sepsis
May 19, 2024

Better medical record-keeping needed to fight antibiotic overuse, studies suggest
May 18, 2024

Researcher discovers drug that may delay onset of Alzheimer's, Parkinson's disease and treat hydrocephalus
May 17, 2024
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Ulcerative colitis articles within Nature Reviews Gastroenterology & Hepatology
Review Article | 25 April 2024
Pouchitis: pathophysiology and management
Pouchitis is a common condition that can occur after intestinal surgery. In this Review, Shen discusses our current understanding of the multifactorial pathophysiology, diagnosis and management of pouchitis, primarily in patients with underlying ulcerative colitis.
Year in Review | 07 December 2023
Upgrading therapeutic ambitions and treatment outcomes
Important studies published in 2023 outlined new agents and strategies for the management of inflammatory bowel disease. Therapeutic ambitions for the management of inflammatory bowel disease were raised by the success of combinations of biologic agents in ulcerative colitis and early surgical resection in Crohn’s disease.
- Paulo Gustavo Kotze
- & Severine Vermeire
Review Article | 10 November 2023
Deciphering the different phases of preclinical inflammatory bowel disease
Inflammatory bowel disease (IBD) is an immune-mediated inflammatory disease (IMID). Here, the authors review evidence on the preclinical phase of IBD, outlining and describing the proposed at-risk, initiation and expansion phases. Overlap with other IMIDs is discussed alongside the possible future directions for research into preclinical IBD.
- Jonas J. Rudbaek
- , Manasi Agrawal
- & Tine Jess
In Brief | 08 August 2023
Mirikizumab for inducing and maintaining clinical remission in ulcerative colitis
- Jordan Hindson
Perspective | 20 April 2023
The appendix and ulcerative colitis — an unsolved connection
The appendix is thought to have a role in the pathogenesis of ulcerative colitis but the association remains unclear. In this Perspective, the authors consider the biology of the appendix with respect to its immunological function and the microbiome, and how this relates to its possible involvement in ulcerative colitis.
- Manasi Agrawal
- , Kristine H. Allin
- & Jean-Frederic Colombel
In Brief | 07 March 2023
Two therapeutic antibodies better than one
Clinical Outlook | 27 January 2023
Positioning therapies for the management of inflammatory bowel disease
A careful integration of the effectiveness and safety of the therapies for inflammatory bowel disease, considering patients’ disease risks, treatment complications and preferences, is warranted to inform the positioning of therapies in clinical practice. Precision medicine might help choose the best option for an individual patient.
- Siddharth Singh
Comment | 19 December 2022
Risk minimization of JAK inhibitors in ulcerative colitis following regulatory guidance
The European Medicines Agency safety committee has revisited the label and recommended the use of Janus kinase inhibitors in patients with certain risk factors only if no suitable treatment alternatives are available. Although regulatory decisions are key to place therapeutic options based on safety, broad restrictions might lead to unintended consequences without an individualized benefit–risk evaluation.
- Silvio Danese
- , Virginia Solitano
- & Laurent Peyrin-Biroulet
Clinical Outlook | 16 September 2022
Medical therapy of paediatric inflammatory bowel disease
Antibodies targeting tumour necrosis factor have substantially advanced the treatment of paediatric inflammatory bowel disease. Understanding pharmacokinetics and therapeutic drug monitoring has led to increased efficacy and durability of response. Primary non-response is more common in ulcerative colitis than in Crohn’s disease, highlighting the need for alternative biologic agents and oral small molecules.
- Luca Scarallo
- & Anne M. Griffiths
Review Article | 07 December 2021
Revisiting fibrosis in inflammatory bowel disease: the gut thickens
Intestinal fibrosis is an important feature of inflammatory bowel disease (IBD) that remains poorly understood. Here, D’Alessio and Ungaro et al. review the cellular and molecular mechanisms contributing to intestinal fibrosis and discuss future therapeutic strategies for IBD-related fibrosis.
- Silvia D’Alessio
- , Federica Ungaro
- & Silvio Danese
In Brief | 01 October 2021
Ozanimod is efficacious in ulcerative colitis
- Katrina Ray
Journal Club | 20 September 2021
Inflammatory bowel disease and corticosteroids: the first RCT
- Fernando Gomollón
In Brief | 22 June 2021
Filgotinib for ulcerative colitis
Research Highlight | 04 May 2021
Intercrypt goblet cells — the key to colonic mucus barrier function
News & Views | 05 February 2021
IBD risk prediction using multi-ethnic polygenic risk scores
Inflammatory bowel disease (IBD) has emerged as a global disease, yet identifying those at higher risk of developing IBD remains challenging. A new study highlights the use of a multi-ethnic polygenic risk score to determine risk of inflammatory bowel disease in a large primary care population.
- Ashwin N. Ananthakrishnan
Comment | 20 January 2021
SARS-CoV-2 vaccination in IBD: more pros than cons
Data on the efficacy and safety of SARS-CoV-2 vaccines are now available, but evidence for these vaccines in those who are immunocompromised (including patients with inflammatory bowel diseases) are lacking. As vaccination begins, questions on advantages and disadvantages can be partially addressed using the experience from other vaccines or immune-mediated inflammatory disorders.
- Ferdinando D’Amico
- , Christian Rabaud
News & Views | 01 October 2020
Environmental stimuli and gut inflammation via dysbiosis in mouse and man
A new study sheds further light on the interplay between environmental stimuli, the gut microbiota and intestinal inflammation. Identification of modifiable environmental triggers and the mechanisms by which they act has implications for the prevention and treatment of inflammatory bowel disease.
- Charlie W. Lees
Research Highlight | 03 September 2020
Deciphering the role of CD8 + T cells in IBD: from single-cell analysis to biomarkers
Research Highlight | 21 January 2020
Shining a spotlight on somatic mutations in ulcerative colitis
Research Highlight | 15 October 2019
New trials in ulcerative colitis therapies
- Iain Dickson
Comment | 13 September 2019
Evolving therapeutic goals in ulcerative colitis: towards disease clearance
In ulcerative colitis, treating beyond endoscopic healing has shown a reduction of relapse and hospitalization, pushing for histological remission to be embraced in clinical practice and clinical trials. Here, we propose the concept of disease clearance (symptomatic, endoscopic and histological remission) as the ultimate goal in the treatment of ulcerative colitis.
- , Giulia Roda
In Brief | 29 March 2019
Gut mucosal virome altered in ulcerative colitis
News & Views | 08 March 2019
FMT for ulcerative colitis: closer to the turning point
A new study shows that a sustainable faecal microbiota transplantation (FMT) treatment protocol, including anaerobic sample preparation, induces remission of active ulcerative colitis. The promising results are another piece in the puzzle, but it is not yet possible to draw conclusions and implement the procedure in clinical practice.
- Giovanni Cammarota
- & Gianluca Ianiro
In Brief | 06 April 2018
Autofluorescence inferior for dysplasia surveillance
In Brief | 02 November 2017
The changing epidemiology of IBD
Review Article | 11 October 2017
Environmental triggers in IBD: a review of progress and evidence
A wide variety of environmental triggers have been associated with IBD pathogenesis, including the gut microbiota, diet, pollution and early-life factors. This Review discusses the latest evidence and progress towards better understanding the environmental factors associated with IBD.
- , Charles N. Bernstein
- & Claudio Fiocchi
Review Article | 19 July 2017
Gut microbiota and IBD: causation or correlation?
Changes in the composition and metabolic function of the gut microbiota have been linked to IBD, but a direct causal association has yet to be established in humans. This Review discusses the evidence supporting dysbiosis in the gut microbiota in Crohn's disease and ulcerative colitis, exploring evidence from animal models and the translation to human disease.
- Josephine Ni
- , Gary D. Wu
- & Vesselin T. Tomov
In Brief | 14 June 2017
Phase II trial success for anti-MADCAM1 antibody
Research Highlight | 17 May 2017
Tofacitinib effective in ulcerative colitis
- Conor A. Bradley
Research Highlight | 01 March 2017
FMT induces clinical remission in ulcerative colitis
- Hugh Thomas
News & Views | 07 December 2016
Mucosal healing in ulcerative colitis: what constitutes remission?
Patients with ulcerative colitis in clinical remission are increasingly undergoing colonoscopies to determine endoscopic remission. However, the histological evaluation of biopsy samples provides additional criteria to predict which patients are most likely to undergo relapse, so what is the ideal therapeutic end point for patients with ulcerative colitis?
- Robert H. Riddell
Research Highlight | 05 October 2016
A role for GATA3 in ulcerative colitis
Review Article | 01 September 2016
Acute severe ulcerative colitis: from pathophysiology to clinical management
Acute severe ulcerative colitis (ASUC) is a potentially life-threatening condition that occurs in ∼20% of patients with ulcerative colitis. Here, the authors provide an overview of ASUC from pathophysiology to clinical management (including drug therapy and surgery).
- Pieter Hindryckx
- , Vipul Jairath
- & Geert D'Haens
In Brief | 13 July 2016
Treatment for acute severe ulcerative colitis
- Isobel Leake
News & Views | 05 May 2016
Vitamin D and IBD: moving towards clinical trials
A new study reports that low vitamin D levels are associated with increased morbidity and severity of IBD. A number of issues must now be addressed to enable the optimal design of interventional studies to test whether vitamin D supplementation can improve outcomes in this disease.
- Margherita T. Cantorna
In Brief | 17 February 2016
CT-P13: a safe and effective treatment for IBD
Research Highlight | 24 December 2015
Maintaining the mucosal barrier in intestinal inflammation
In Brief | 18 November 2015
Who benefits the most from etrolizumab in ulcerative colitis?
In Brief | 08 September 2015
Gel-based drug delivery for IBD hits the target
In Brief | 21 April 2015
Faecal transplant from donors no more effective than autologous transplant for treating ulcerative colitis
News & Views | 15 July 2014

Sequential rescue therapy in steroid-refractory ulcerative colitis
Treatment of patients with steroid-refractory ulcerative colitis is still a challenge for physicians. A recent study has evaluated the effectiveness and safety of sequential rescue therapies in this subgroup of patients.
- Paolo Gionchetti
- & Fernando Rizzello
Research Highlight | 24 June 2014
T H 9 cells might have a role in the pathogenesis of ulcerative colitis
In Brief | 17 June 2014
Phase II study reveals potential of etrolizumab as induction therapy for ulcerative colitis
Research Highlight | 22 April 2014
Mouse model reveals how appendicitis protects against ulcerative colitis
- Claire Greenhill
Research Highlight | 18 March 2014
EUS can differentiate Crohn's disease from ulcerative colitis
- Natalie J. Wood
News & Views | 04 March 2014
Which makes patients happier, surgery or anti-TNF therapy?
Quality of life and disability have been compared in patients with ulcerative colitis who were undergoing one of the two current major treatments of choice, proctocolectomy or anti-TNF therapy. The only significant differences between the two groups were increased use of antidiarrhoeal medication and stool frequency in those who underwent surgery.
- Taku Kobayashi
- & Toshifumi Hibi
Review Article | 07 January 2014
Tailoring anti-TNF therapy in IBD: drug levels and disease activity
Despite the proven and often clinically marked efficacy of anti-TNF drugs for IBD, these biologic agents are not immune to treatment failures. Tailoring anti-TNF treatment in IBD mandates considerations of the different clinical scenarios in which therapy failure might occur while bearing in mind an opposite group of patients in whom intensive therapy might be unnecessary.
- Shomron Ben-Horin
- & Yehuda Chowers
In Brief | 17 September 2013
Induction and maintenance therapy for ulcerative colitis—vedolizumab more effective than placebo
News & Views | 13 August 2013
Activity of IBD during pregnancy
Women worry that their IBD will flare during pregnancy. A prospective multicentre study from Europe has now demonstrated that although women with Crohn's disease do not have an increased risk of relapse during pregnancy, women with ulcerative colitis are at increased risk of relapse, both during pregnancy and postpartum.
- Sunanda Kane
News & Views | 30 July 2013
Golimumab in ulcerative colitis: a 'ménage à trois' of drugs
Golimumab, a human anti-TNF antibody, is effective in patients with ulcerative colitis, according to new findings from an international phase III double-blind trial. The addition of this drug makes a ménage à trois of available drugs—comprising infliximab, adalimumab and golimumab—for the treatment of ulcerative colitis.
Browse broader subjects
- Inflammatory diseases
- Inflammatory bowel disease
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Switch language:

J&J’s Tremfya meets endpoints in Phase III ulcerative colitis trial
The company’s monoclonal antibody met primary and secondary endpoints as a maintenance therapy for ulcerative colitis in a Phase III trial.
- Share on Linkedin
- Share on Facebook

Johnson and Johnson (J&J) has announced positive data from the Phase III QUASAR maintenance trial for Tremfya (guselkumab) as a maintenance therapy in patients with moderate to severe active ulcerative colitis.
Tremfya is an interleukin (IL)-23 and CD64-inhibiting monoclonal antibody. It was first approved as a treatment for moderate to severe plaque psoriasis by the US Food and Drug Administration (FDA), in 2017. Tremfya has since been approved to treat psoriatic arthritis.
Go deeper with GlobalData

LOA and PTSR Model - JNJ-4703 in Ulcerative Colitis
Loa and ptsr model - jnj-4804 in ulcerative colitis, premium insights.
The gold standard of business intelligence.
Find out more
Related Company Profiles
Johnson & johnson.
The therapy achieved the primary and nine major secondary endpoints in the placebo-controlled Phase III QUASAR maintenance study (NCT04033445). The participants in the trial were randomised to receive either placebo or one of the two doses of subcutaneous Tremfya – 200mg every four weeks (q4w) or 100mg every eight weeks (q8w).
The trial met its primary endpoint by inducing remission in 50% and 45.2% of the participants in the q4w and q8w treatment groups respectively at 44 weeks, compared to the placebo. Of the participants who were in clinical remission, 67% and 71% of the participants in the q4w and q8w treatment groups respectively also achieved endoscopic remission at 44 weeks.
Clinical response was seen in 74.7% and 77.7% of the participants in the q4w and q8w treatment groups respectively at 44 weeks, compared to 43.2% of participants in the placebo group. Endoscopic improvement was seen in 51.6% and 49.5% of the participants in the q4w and q8w treatment groups respectively at 44 weeks, compared to 18.9% of participants in the placebo group.
The data from the trial was presented at the Digestive Disease Week 2024 taking place in Washington DC from 19 to 21 May.
How well do you really know your competitors?
Access the most comprehensive Company Profiles on the market, powered by GlobalData. Save hours of research. Gain competitive edge.

Your download email will arrive shortly
Not ready to buy yet? Download a free sample
We are confident about the unique quality of our Company Profiles. However, we want you to make the most beneficial decision for your business, so we offer a free sample that you can download by submitting the below form
J&J’s Tremfya is expected to be the successor to the company’s IL-12/IL-23 inhibitor Stelara (ustekinumab). Stelara is an approved treatment for severe plaque psoriasis, active psoriatic arthritis, and ulcerative colitis. As per J&J’s annual report, the therapy generated $10.8bn in global sales last year, but its future sales are expected to decline with multiple biosimilars entering the market .
J&J is also evaluating Tremfya as a treatment for Crohn’s disease in a Phase II GALAXI trial (NCT03466411). The therapy maintained efficacy for three years, with 54.1% of the participants demonstrating clinical remission.
Sign up for our daily news round-up!
Give your business an edge with our leading industry insights.
More Relevant
Faron Pharmaceuticals reports positive data from MDS trial
Gsk boasts win for depemokimab in asthma trials, rila therapeutics doses first cohort in phase i ckd treatment trial, gigagen doses first subject in phase i advanced solid tumour trial, sign up to the newsletter: in brief, your corporate email address, i would also like to subscribe to:.
I consent to Verdict Media Limited collecting my details provided via this form in accordance with Privacy Policy
Thank you for subscribing
View all newsletters from across the GlobalData Media network.
- See us on facebook
- See us on twitter
- See us on youtube
- See us on linkedin
- See us on instagram
Stanford scientists link ulcerative colitis to missing gut microbes
Bacteria normally inhabiting healthy people’s intestines — and the anti-inflammatory metabolites these bacteria produce — are depleted in ulcerative colitis patients, a Stanford study shows.
February 25, 2020 - By Bruce Goldman
Aida Habtezion is the senior author of a study that describes how people with ulcerative colitis have insufficient amounts of a metabolite produced by a family of gut-dwelling bacteria. Steve Castillo
About 1 million people in the United States have ulcerative colitis, a serious disease of the colon that has no cure and whose cause is obscure. Now, a study by Stanford University School of Medicine investigators has tied the condition to a missing microbe.
The microbe makes metabolites that help keep the gut healthy.
“This study helps us to better understand the disease,” said Aida Habtezion , MD, associate professor of gastroenterology and hepatology. “We hope it also leads to our being able to treat it with a naturally produced metabolite that’s already present in high amounts in a healthy gut.”
When the researchers compared two groups of patients — one group with ulcerative colitis, the other group with a rare noninflammatory condition — who had undergone an identical corrective surgical procedure, they discovered that a particular family of bacteria was depleted in patients with ulcerative colitis. These patients also were deficient in a set of anti-inflammatory substances that the bacteria make, the scientists report.
A paper describing the research findings was published online Feb. 25 in Cell Host & Microbe . Habtezion is the senior author. Lead authorship is shared by Sidhartha Sinha , MD, assistant professor of gastroenterology and hepatology, and postdoctoral scholar Yeneneh Haileselassie, PhD.
The discoveries raise the prospect that supplementing ulcerative colitis patients with those missing metabolites — or perhaps someday restoring the gut-dwelling bacteria that produce them — could effectively treat intestinal inflammation in these patients and perhaps those with a related condition called Crohn’s disease, Habtezion said.
A clinical trial to determine whether those metabolites, called secondary bile acids, are effective in treating the disease is now underway at Stanford. Sinha is the trial’s principal investigator, and Habtezion is the co-principal investigator.
Surgery often required
Ulcerative colitis is an inflammatory condition in which the immune system attacks tissue in the rectum or colon. Patients can suffer from heavy bleeding, diarrhea, weight loss and, if the colon becomes sufficiently perforated, life-threatening sepsis.
There is no known cure. While immunosuppressant drugs can keep ulcerative colitis at bay, they put patients at increased risk for cancer and infection. Moreover, not all patients respond, and even when an immunosuppressant drug works initially, its effectiveness can fade with time. About one in five ulcerative colitis patients progress to the point where they require total colectomy, the surgical removal of the colon and rectum, followed by the repositioning of the lower end of the small intestine to form a J-shaped pouch that serves as a rectum.
These “pouch patients” can lead quite normal lives. However, as many as half will develop pouchitis, a return of the inflammation and symptoms they experienced in their initial condition.
The new study began with a clinical observation. “Patients with a rare genetic condition called familial adenomatous polyposis, or FAP, are at extremely high risk for colon cancer,” Habtezion said. “To prevent this, they undergo the exact same surgical procedure patients with refractory ulcerative colitis do.” Yet FAP pouch patients rarely if ever experience the inflammatory attacks on their remaining lower digestive tract that ulcerative-colitis patients with a pouch do, she said.
The Stanford scientists decided to find out why. Their first clue lay in a large difference in levels of a group of substances called secondary bile acids in the intestines of seven FAP patients compared with 17 patients with ulcerative colitis who had undergone the pouch surgery. The investigators measured these metabolite levels by examining the participants’ stool samples.
Primary bile acids are produced in the liver, stored in the gallbladder and released into the digestive tract to help emulsify fats. The vast majority of secreted primary bile acids are taken up in the intestine, where resident bacteria perform a series of enzymatic operations to convert them to secondary bile acids.
Prior research has suggested, without much elaboration or follow-up, that secondary bile acids are depleted in ulcerative colitis patients and in those with a related condition, Crohn’s disease, in which tissue-destroying inflammation can occur in both the colon and the small intestine.
The researchers confirmed that levels of the two most prominent secondary bile acids, deoxycholic acid and lithocholic acid, were much lower in stool specimens taken from the ulcerative colitis pouch patients than from FAP pouch patients. Clearly, the surgical procedure hadn’t caused the depletion.
Diminished microbial diversity
These findings were mirrored by the scientists’ observation that microbial diversity in the specimens from ulcerative colitis pouch patients was diminished. Moreover, the investigators showed that a single bacterial family — Ruminococcaceae — was markedly underrepresented in ulcerative colitis pouch patients compared with FAP pouch patients. A genomic analysis of all the gut bacteria in the participants showed that the genes for making enzymes that convert primary bile acids to secondary bile acids were underrepresented, too. Ruminococcaceae, but few other gut bacteria, carry those genes.
“All healthy people have Ruminococcaceae in their intestines,” Habtezion said. “But in the UC pouch patients, members of this family were significantly depleted.”
Incubating primary bile acids with stool samples from FAP pouch patients, but not from ulcerative colitis pouch patients, resulted in those substances’ effective conversion to secondary bile acids.
In three different mouse models of colitis, supplementation with lithocholic acid and deoxycholic acid reduced infiltration by inflammatory immune cells and levels of several inflammatory signaling proteins and chemicals in the mice’s intestines, the researchers showed. The supplements also mitigated the classic symptoms of colitis in the mice, such as weight loss or signs of colon pathology.
All three mouse models are considered representative of not just ulcerative colitis but inflammatory bowel disease in general, a category that also includes Crohn’s disease. So the findings may apply to Crohn’s disease patients, as well, Habtezion said.
In an ongoing Phase 2 trial at Stanford, Sinha, Habtezion and their colleagues are investigating the anti-inflammatory effects, in 18- to 70-year-old ulcerative colitis pouch patients, of oral supplementation with ursodeoxycholic acid, a naturally occurring secondary bile acid approved by the Food and Drug Administration for treatment of primary biliary sclerosis and for management of gall stones. Information about the trial, which is still recruiting people, is available at https://clinicaltrials.gov/ct2/show/NCT03724175 .
Habtezion is associate dean for academic affairs in the School of Medicine, a faculty fellow of Stanford ChEM-H and a member of Stanford Bio-X , the Stanford Cancer Institute , the Stanford Pancreas Cancer Research Group and the Wu Tsai Neurosciences Institute at Stanford .
Other Stanford co-authors of the study are postdoctoral scholars Min Wang, PhD, Estelle Spear, PhD, Gulshan Singh, PhD, and Hong Namkoong, PhD; former research scientist Linh Nguyen, PhD; former postdoctoral scholar Carolina Tropini, PhD; former gastroenterology medical fellow Davis Sim, MD; research assistant Karolin Jarr; Laren Becker , MD, instructor of gastroenterology and hepatology; Michael Fischbach, PhD, associate professor of bioengineering; and Justin Sonnenburg , PhD, associate professor of microbiology and immunology.
Researchers from the Children’s Hospital of Philadelphia also contributed to the work.
The work was funded by the National Institutes of Health (grants R01DK101119, KL2TR001083 and UL1TR001085), the Ann and Bill Swindells Charitable Trust, the Kenneth Rainin Foundation, and Leslie and Douglas Ballinger.
Stanford’s Department of Medicine also supported the work.

About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu .
Hope amid crisis
Psychiatry’s new frontiers

A comprehensive review and update on ulcerative colitis
Affiliations.
- 1 Department of Internal Medicine, Texas Tech University Health Science Center El Paso, 2000B Transmountain Road, El Paso, TX 79911, USA; Paul L. Foster School of Medicine (PLFSOM), Texas Tech University Health Science Center El Paso, 5001 El Paso Dr, El Paso, TX 79905, USA. Electronic address: [email protected].
- 2 Department of Internal Medicine, Texas Tech University Health Sciences Center, 4800 Alberta Avenue, El Paso, TX 79905, USA.
- 3 Paul L. Foster School of Medicine (PLFSOM), Texas Tech University Health Science Center El Paso, 5001 El Paso Dr, El Paso, TX 79905, USA.
- 4 Department of Family Medicine, Texas Tech University Health Science Center El Paso, 2000B Transmountain Road, El Paso, TX 79911, USA.
- 5 Department of Surgery, Texas Tech University Health Science Center El Paso, 2000B Transmountain Road, El Paso, TX 79911, USA.
- 6 Department of Gastroenterology & Hepatology, University of California San Francisco (UCSF), Fresno, CA, USA.
- 7 Division of Gastroenterology, American University of Beirut, Beirut, Lebanon.
- 8 Division of Gastroenterology, American University of Beirut, Beirut, Lebanon; Division of Gastroenterology, Hepatology and Nutrition, University of Pittsburgh, M2, C Wing, 200 Lothrop Street, Pittsburgh, PA 15213, USA.
- PMID: 30837080
- DOI: 10.1016/j.disamonth.2019.02.004
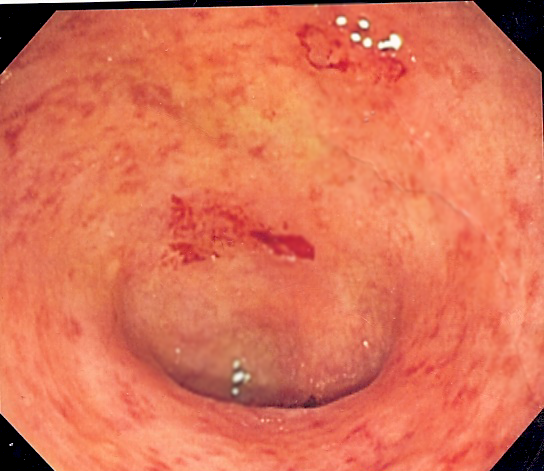
Ulcerative colitis (UC) is a chronic idiopathic inflammatory bowel disorder of the colon that causes continuous mucosal inflammation extending from the rectum to the more proximal colon, with variable extents. UC is characterized by a relapsing and remitting course. UC was first described by Samuel Wilks in 1859 and it is more common than Crohn's disease worldwide. The overall incidence and prevalence of UC is reported to be 1.2-20.3 and 7.6-245 cases per 100,000 persons/year respectively. UC has a bimodal age distribution with an incidence peak in the 2nd or 3rd decades and followed by second peak between 50 and 80 years of age. The key risk factors for UC include genetics, environmental factors, autoimmunity and gut microbiota. The classic presentation of UC include bloody diarrhea with or without mucus, rectal urgency, tenesmus, and variable degrees of abdominal pain that is often relieved by defecation. UC is diagnosed based on the combination of clinical presentation, endoscopic findings, histology, and the absence of alternative diagnoses. In addition to confirming the diagnosis of UC, it is also important to define the extent and severity of inflammation, which aids in the selection of appropriate treatment and for predicting the patient's prognosis. Ileocolonoscopy with biopsy is the only way to make a definitive diagnosis of UC. A pathognomonic finding of UC is the presence of continuous colonic inflammation characterized by erythema, loss of normal vascular pattern, granularity, erosions, friability, bleeding, and ulcerations, with distinct demarcation between inflamed and non-inflamed bowel. Histopathology is the definitive tool in diagnosing UC, assessing the disease severity and identifying intraepithelial neoplasia (dysplasia) or cancer. The classical histological changes in UC include decreased crypt density, crypt architectural distortion, irregular mucosal surface and heavy diffuse transmucosal inflammation, in the absence of genuine granulomas. Abdominal computed tomographic (CT) scanning is the preferred initial radiographic imaging study in UC patients with acute abdominal symptoms. The hallmark CT finding of UC is mural thickening with a mean wall thickness of 8 mm, as opposed to a 2-3 mm mean wall thickness of the normal colon. The Mayo scoring system is a commonly used index to assess disease severity and monitor patients during therapy. The goals of treatment in UC are three fold-improve quality of life, achieve steroid free remission and minimize the risk of cancer. The choice of treatment depends on disease extent, severity and the course of the disease. For proctitis, topical 5-aminosalicylic acid (5-ASA) drugs are used as the first line agents. UC patients with more extensive or severe disease should be treated with a combination of oral and topical 5-ASA drugs +/- corticosteroids to induce remission. Patients with severe UC need to be hospitalized for treatment. The options in these patients include intravenous steroids and if refractory, calcineurin inhibitors (cyclosporine, tacrolimus) or tumor necrosis factor-α antibodies (infliximab) are utilized. Once remission is induced, patients are then continued on appropriate medications to maintain remission. Indications for emergency surgery include refractory toxic megacolon, colonic perforation, or severe colorectal bleeding.
Copyright © 2019 Elsevier Inc. All rights reserved.
Publication types
- Anti-Inflammatory Agents / therapeutic use
- Colitis, Ulcerative / complications
- Colitis, Ulcerative / diagnosis
- Colitis, Ulcerative / pathology
- Colitis, Ulcerative / therapy*
- Colon / pathology
- Inflammation / diagnosis
- Inflammation / therapy
- Intestinal Mucosa / pathology*
- Quality of Life
- Rectum / pathology
- Severity of Illness Index
- Anti-Inflammatory Agents
- Search Menu
- Advance articles
- Open Access
- Editor's Choice
- Supplements
- ECCO Guideline/Consensus Papers
- ECCO Topical Reviews
- ECCO Scientific Workshop Papers
- ECCO Position Statements
- Why Publish with JCC
- Author Guidelines
- Submission Site
- Order Offprints
- Advertising and Corporate Services
- Advertising
- Reprints and ePrints
- Sponsored Supplements
- Branded Books
- Journals Career Network
- About Journal of Crohn's and Colitis
- About the European Crohn's and Colitis Organisation
- Editorial Board
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic
Article Contents
Mri features indicative of permanent colon damage in ulcerative colitis: an exploratory study.
- Article contents
- Figures & tables
- Supplementary Data
Jordi Rimola, Jesús Castro-Poceiro, Víctor Sapena, Marta Aduna, Juan Arevalo, Isabel Vera, Miguel Ángel Pastrana, Marta Gallego, Maria Carme Masamunt, Agnès Fernández-Clotet, Ingrid Ordás, Elena Ricart, Julian Panés, MRI features indicative of permanent colon damage in ulcerative colitis: an exploratory study, Journal of Crohn's and Colitis , 2024;, jjae075, https://doi.org/10.1093/ecco-jcc/jjae075
- Permissions Icon Permissions
It is uncertain whether ulcerative colitis leads to accumulated bowel damage on cross sectional image. We aimed to characterize bowel damage in patients with ulcerative colitis using magnetic resonance imaging and determine its relation with duration of disease and the impact on patients’ quality of life.
In this prospective study, subjects with ulcerative colitis in endoscopic remission underwent MRI without bowel cleansing and completed quality-of-life questionnaires. Subjects’ magnetic resonance findings were analyzed considering normal values and thresholds determined in controls with no history of inflammatory bowel disease (n=40) and in patients with Crohn’s disease with no history of colonic involvement (n=12). Subjects with UC were stratified according to disease duration (<7 years vs. 7‒14 years vs. >14 years).
We analyzed 41 subjects with ulcerative colitis [20 women; Mayo endoscopic subscore 0 in 38 (92.7%) and 1 in 3 (7.3%)]. Paired segment-by-segment comparison of magnetic resonance findings in colonic segments documented of being affected by ulcerative colitis versus controls showed subjects with ulcerative colitis had decreased cross-sectional area (p≤0.0034) and perimeter (p≤0.0005), and increased wall thickness (p=0.026) in all segments. Colon damage, defined as wall thickness ≥3 mm, was seen in 22 (53.7%) subjects. Colon damage was not associated with disease duration or quality of life.
Morphologic abnormalities in the colon were highly prevalent in patients with ulcerative colitis in the absence of inflammation. Structural bowel damage was not associated with disease duration or quality of life.
- nuclear magnetic resonance
- magnetic resonance imaging
- ulcerative colitis
- quality of life
- illness length
Supplementary data
Email alerts, citing articles via.
- About Journal of Crohn's and Colitis
- Recommend to your Library
Affiliations
- Online ISSN 1876-4479
- Print ISSN 1873-9946
- Copyright © 2024 European Crohn's and Colitis Organisation (ECCO) Published by Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Open access
- Published: 14 May 2024
The development of probiotics and prebiotics therapy to ulcerative colitis: a therapy that has gained considerable momentum
- Jing Guo 1 ,
- Liping Li 1 ,
- Yue Cai 2 &
- Yongbo Kang 1
Cell Communication and Signaling volume 22 , Article number: 268 ( 2024 ) Cite this article
344 Accesses
1 Altmetric
Metrics details
Ulcerative colitis (UC) is increasingly common, and it is gradually become a kind of global epidemic. UC is a type of inflammatory bowel disease (IBD), and it is a lifetime recurrent disease. UC as a common disease has become a financial burden for many people and has the potential to develop into cancer if not prevented or treated. There are multiple factors such as genetic factors, host immune system disorders, and environmental factors to cause UC. A growing body of research have suggested that intestinal microbiota as an environmental factor play an important role in the occurrence and development of UC. Meanwhile, evidence to date suggests that manipulating the gut microbiome may represent effective treatment for the prevention or management of UC. In addition, the main clinical drugs to treat UC are amino salicylate and corticosteroid. These clinical drugs always have some side effects and low success rate when treating patients with UC. Therefore, there is an urgent need for safe and efficient methods to treat UC. Based on this, probiotics and prebiotics may be a valuable treatment for UC. In order to promote the wide clinical application of probiotics and prebiotics in the treatment of UC. This review aims to summarize the recent literature as an aid to better understanding how the probiotics and prebiotics contributes to UC while evaluating and prospecting the therapeutic effect of the probiotics and prebiotics in the treatment of UC based on previous publications.
Introduction
Ulcerative colitis (UC) is a chronic non-specific intestinal inflammatory disease [ 1 ]. UC becomes an important health problem, because it’s high morbidity. Especially in newly industrialized countries [ 2 ]. Research shows that the incidence of UC is 10 to 20 patients per 100,000 people every year [ 3 ]. UC often presents with recurrent attacks. And the inflammatory of UC will become a factor of colon cancer in the long run [ 4 ]. The pathogenic factors of UC are sophisticated, it is related to intestinal microbiota, immune function of the body (For example, UC is closely related with Th2 cells) [ 5 ], genetic factor and environment factor (e.g. life-style, dietary habits) and so on [ 6 ]. wherein, intestinal microbiota is one of the most important factor that arise UC [ 7 ]. Therefore, we can use probiotics to regulate the intestinal flora in the treatment of UC [ 8 , 9 ]. A growing body of research has shown that probiotics and prebiotics can bring about remission the symptoms of UC improving intestinal mucosal homeostasis, ameliorating the intestinal microbiota environment, regulating the body’s immune function. Therefore, probiotics and prebiotics may be a very safe and efficient treatment for UC. At the same time, it can greatly reduce the financial burden of patients. Furthermore, New techniques have made it possible to attempt systematic studies of probiotics prebiotics, which can provide more specific information about their functions and pathological variations. This review summarizes cutting-edge research on probiotics and prebiotics treatment for UC, existing issues in probiotics treatment and prebiotics therapy, the future of probiotics and prebiotics, and microbial therapeutics.
Pathogenesis of UC
Ulcerative colitis is a chronic inflammatory disorder of the gastrointestinal tract. It is characterized by a progressive decline in health. UC is marked by inflammation of the mucosal lining, usually confined to the colon and rectum [ 10 ]. The pathogenesis of UC is closely related to a variety of factors, such as genetics and environment [ 11 ]. Statistically, genetics can only explain 7.5% of the variation in disease and has little predictive power for phenotype. Therefore, it has limited clinical application. Examples of loci associated with increased susceptibility to UC including genes associated with barrier function and human leukocyte antigen, such as HNF4A and CDH1 [ 12 , 13 ]. Environment plays an important role in the development of UC. Such as, living condition, hygiene, diet, etc. While UC is mainly due to immune dysfunction and intestinal barrier dysfunction. Colonic epithelial cells (colonocytes), as the first line of defense of the gut immune system, are closely related to the pathogenesis of the UC. Research findings, the expression of peroxisome proliferator-activated receptor γ (PPAR γ) is reduced in the colonocytes in patients with UC. And the reduced expression of PPAR γ, which is a nuclear receptor that downregulates inflammation, will stimulate an inflammatory cascade responses through a series of immune responses, leading to the production of large quantities of inflammatory factors [ 14 ]. Also, when certain genes in the intestinal epithelium are functionally deficient, it may lead to disruption of the intestinal barrier function [ 10 ]. The deficiency or malfunction of various immune cells and the abnormal expression of cytokines, which play an important signaling function, can also lead to inflammation, which, if prolonged, can lead to the development of UC. The intestinal immune system also involves the intrinsic and adaptive immunity [ 15 ], involving a variety of immune cells and molecules and others. If dendritic cells abundantly express Toll-like receptors (TLR) which can recognize pathogen pattern receptors, this will leads to the activation of several inflammatory signaling pathway, such as NF-κB [ 16 ] and MAPK pathway, triggering an inflammatory response. The production of large amounts of pro-inflammatory factors affects the differentiation of immune cells such as T cell differentiation towards subpopulation. For example, massive activation of Th2 cells leads to high expression of IL-13, which induces apoptosis of epithelial cells and disrupts the integrity of mucosal barrier [ 17 , 18 ]. Other T helper cells also play an important role in UC. And some research suggest that Breg deficiency may also associated with UC [ 19 ]. The damage of the intestinal mucosal barrier is also an important causative factor in UC. Intestinal secretory dysfunction such as decreased secretion of antimicrobial peptides and mucus layer, or structural defects of intestinal barrier including occludin, ZO-1, ZO-2 and so on. It has been found that the disruption of human gut microbiota, the largest collection of microbes within the body [ 20 ], is critical in the progression of UC, but the specific mechanism is not yet clear.
The role of gut microflora in UC
Gut microflora lives on intestinal mucosal and forms bacterial layer. Thus, there is a strong and complex relationship between gut microbiota and gut. Intestinal dysbacteriosis can leads to a decrease in intestinal defense function and immune regulatory function. Furthermore, the decrease of the body immune function and an increase in associated pathogenic factors leading to the intestinal mucosal invasion or exacerbates the gastrointestinal diseases [ 6 ]. Recently, a large number of studies have shown that alterations of intestinal microbiota can play an important role in the occurrence and development of UC. Meanwhile, some studies have shed light on UC subjects exhibiting alterations in the relative abundance of “beneficial” and potentially “harmful” bacteria compared to healthy subjects. The existence of a link between UC and the gut microbiota was indicated based on studies in animals and patients with UC. Changes of gut microbiota together with their-derived products and metabolites account for the important factors to promote UC occurrence. Here, the possible mechanisms of microbiome-gut action in promoting UC occurrence are discussed as well as outlined in Fig. 1 .
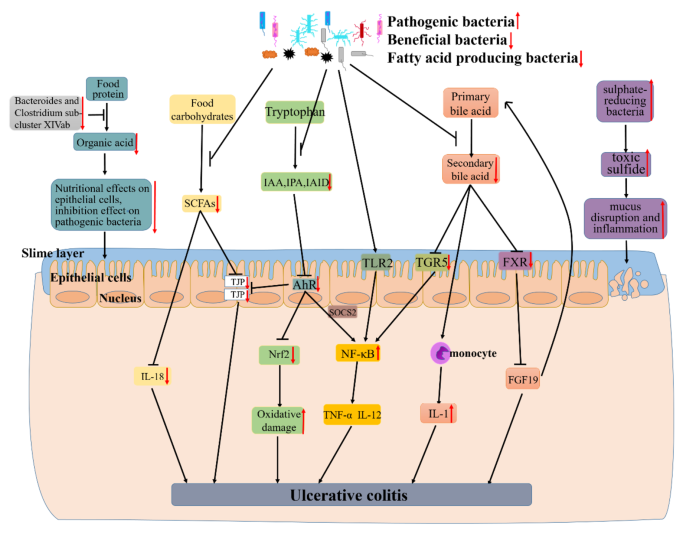
The mechanism of UC caused by dysbiosis of gut microbiota. Research findings, the decline of certain beneficial bacteria inhibits the conversion of food protein into organic acid which can nourish epithelial cells and inhibit pathogenic bacteria. Firmicutes as a major producer of butyrate (a kind of SCFAs), its decline leads to lower intestinal SCFAs. Leading the decreased secretion of epithelial repair cytokine interleukin-18, reduced the integrity of epithelial cells, and inhibited goblet cells secrete mucin and modification of tight junctions. And the decline of some gut microbiota also can lead to a decrease of indoles and their derivatives (e.g., IAA, IPA and IAID) which is produced by tryptophan. Thereby reducing the activation of AhR, a member of the activation of PER-ARNT-SIM (PAS) superfamily of transcription factors. The activation of AhR can inhibited the expression of NF-κB in a manner dependent on suppressor of cytokine signaling 2 (SOCS2). And AhR can also maintains the integrity of intestinal barrier activation by increasing the expressions of intestinal tight junction protein (TJPs) or activating the AhR-Nrf2 pathway. All of these effects were reversed due to the decrease of IAA, IPA or IAID. Thus lead to the increase of inflammatory factors (e.g., TNF-α and IL-17) and oxidative damage. Other researchers found that certain pathogenic bacteria such as Bacteroides (B.) fragilis and capsular lipopolysaccharide A can activate NF-κB signaling pathway and promote the secretion of inflammatory factors. The gut microbiota dysbiosis can also lead to the decreased synthesis of secondary bile acid. And secondary acid act as high-affinity ligands for TGR5 and FXR, its decline can promote NF-κB activation to synthesize inflammatory and the expression of proinflammatory cytokines secreted by monocyte and downregulate the expression of FGF19 and promote the synthesis of bile acids thus increasing its toxicity effect on tissues. As an intestinal pathogen, the increase of sulphate-reducing bacteria leads to cell disintegration and inflammatory via toxic sulfide. All of these can lead to the occurrence and development of UC.
A large number of studies have shown that patients with UC have a decrease in the bacterial diversity of gut microbiota [ 21 ]. Animal study results indicate a close association between gut microbiota and UC. Li et al. found that Firmicutes and Proteobacteria increased, whereas Bacteroidetes decreased in UC rats. And Lactobacillus , Lachnospiraceae_NK4A136_group , Prevotella_9 and Bacteroides were dominant genera in the model group [ 22 ]. Consistent with animal studies, the existence of a link between UC and the gut microbiota was indicated based on studies in patients with UC. Guo et al. also found that the abundance of Bacteroides and Clostridium sub-cluster XIVab as well as the concentration of organic acids significantly decrease by comparing with healthy individuals [ 23 ]. Similarly, Mizoguchi et al. shown that UC patients harbored relatively more abundant Actinobacteria, Proteobacteria and Tenericutes [ 24 ]. A comparison between UC and healthy individuals differed in the composition and diversity of the microbiota, with an upward trend in the Clostridium cluster IX and a decreased Clostridium cluster XIVa in patients with UC [ 25 ]. Consistent with the above results, there is a reduced amounts of bacterial groups from the Clostridium cluster XIVa , and the levels of Bacteroidetes was increased [ 26 ].
In addition, Kotlowski et al. found that the numbers of Escherichia coli were high in the rectal tissue of patients with UC [ 27 ]. By comparing with healthy controls, Xu et al. showed that the inflamed mucosa had more Proteobacteria (e.g. Escherichia–Shigella ) and fewer Firmicutes (e.g., Enterococcus ) [ 28 ]. As demonstrated by Schwiertz et al., Patients with active UC have lower cell counts of Bifidobacterium than healthy controls [ 29 ]. Another study found that the sulfate-reducing bacteria which is the dominant microflora in UC, it may proliferate with the release of toxic sulfide [ 30 ].
Recently, Verma et al. shown that during the active and remission stages of UC cases, the proportions of Bacteroides , Eubacterium , and Lactobacillus spp. are decrease [ 31 ]. Similarly, in another analysis of mucosa-associated flora in UC patients, it was learned that UC patients contained proportionally less Firmicutes , and correspondingly more Bacteroidetes [ 32 ]. Tahara et al. demonstrated that Fusobacterium nucleatum is common which is isolate from human intestinal biopsy from UC, compared to healthy controls [ 33 ].
In keeping with these results, Machiels et al. found that there is a decrease of the Roseburia hominis and Faecalibacterium prausnitzii in patients with UC [ 34 ]. Lepage et al. demonstrated that patients with UC are characterized by more Actinobacteria and Proteobacteria and less bacteria from the Lachnospiraceae and Ruminococcaceae families [ 35 ]. Likewise, a significant reduction was found on the UC mucosa compared with the non-IBD controls, that is levels of Clostridium clostridioforme , the Eubacterium rectale group, Faecalibacterium prausnitzii , Bifidobacteria , Lactobacilli , and Clostridium butyricum [ 36 ]. Consistent with the above results of this study, patients with UC in remission compared to that of controls, there is a loss of Bacteroides , Escherichia , Eubacterium , Lactobacillus , and Ruminococcus spp [ 37 ].
Recently, Hu et al. [ 38 ] found that the decreased of the dominant bacteria that digest food carbohydrates to short chain fatty acid (SCFA) lead to the reduce of intestinal barrier integrity (for example, the decrease of TJPs in colon). Guo et al. [ 23 ] also found that SCFAs can affect the secretion of the epithelial repair cytokine interleukin-18. And they found that the decreased of Bacteroides and Clostridium sub-cluster XIVab leading to the decrease of organic acid, which reduces the trophic effect of organic acid to epithelial cells and the inhibitory effect on pathogenic bacteria [ 39 ]. Agus et al. [ 40 ] found that the reduced of certain intestinal flora inhibited the conversion of tryptophan to indole and its derivatives, and AhR as a receptor of indole and its derivatives, its activation will reduced, thereby inhibiting the intestinal TJP and AhR-Nrf2 pathway, leading to the reduced of intestinal barrier integrity and increased oxidative stress [ 41 ]. Rothhammer et al. [ 42 ] demonstrated that the reduce of AhR can promote the activation of NF-κB pathway in a manner dependent on suppressor of cytokine signaling 2 (SOCS2), then increase the expression of a number of inflammatory factors, including TNF-α and IL-12 et al. It is reported that some bacteria regulate the secretion of TNF-α and IL-12 by activating the NF-κB pathway through TLR2 receptor [ 43 ]. Iracheta et al. [ 44 ] found that primary bile acid are converted to secondary bile acid by gut microorganisms after being secreted into gut through a series of reactions, and that a decline of these gut microorganisms leads to a decrease of secondary bile acid. The decrease of secondary bile acid, which act as high-affinity ligands for TGR5 and FXR, leads to a decreased activation of TGF5 and FXR. The inhibitory effect of TGR5 on NF-κB is reduced, thereby promoting the activation of NF-κB. Reduced activation of FXR down-regulates the expression of FGF19, then its inhibitory effect to hepatic bile acid is declined, leading to a further increase of bile acid and exacerbating the development of inflammation [ 45 ]. And the decrease of secondary bile acids promote the secretion of pro-inflammatory factors by monocytes [ 46 ]. Figliuolo et al. [ 47 ] found that the increase of sulphate-reducing bacteria lead to an increase of toxic sulfide, which cause the disruption of gut epithelial cell and increase intestinal inflammatory.
Taken together, these results provide further insights into a role for gut microbiota in the pathogenesis of UC and might potentially serve as guidance for the interventions of UC by manipulating gut microbiota.
Research advances existing challenges IBD treatment
At present, there are many various treatment methods for IBD. Conventional treatment is the use of pharmacotherapy, including aminosalicylates, corticosteroids (CSs), immunomodulators (e.g., thiopurines (TPs), methotrexate (MTX), and calcineurin inhibitors), and biologics (e.g., pro-inflammatory cytokine inhibitors and integrin antagonists). Surgical resection and other methods including apheresis therapy, antibiotics, probiotics and prebiotics can also be used for treatment [ 48 ]. However, the side effects and high reccurence rate of these substances and methods limit there application. For example, research found, although aminosalicylates have been used in the treatment of IBD for the past 80 years, its efficacy remains controversial. And its mild side effects include diarrhea, nausea, abdominal pain, flatulence and others [ 49 ]. Severe cases can lead to infertility and anemia. CSs inhibits the transcription of certain inflammatory factors [ 50 ] and regulate the expression of certain anti-inflammatory genes [ 51 ] through certain signaling pathways. And it has many side effects, including diabetes mellitus, hypertension, venous thromboembolism (VTE), etc [ 52 ].. Some patients may also have dependence on this medication [ 53 ]. TPs inhibits intestinal inflammatory response by regulating T cell proliferation and activation. But TPs can cause side effects such as liver damage [ 54 ] and gastrointestinal intolerance [ 55 ]. MTS excerts its effects also by downregulating inflammatory factors. But it can cause adverse reactions such as fatigue, diarrhea, pneumonia and rash [ 51 ]. Calcineurin inhibitors also supresses inflammatory responses by interfering with signaling pathways. The incidence of side effects of calcineurin inhibitors is high, including renal function damage, hyperkalemia and infectious diseases and so on [ 56 ]. Anti-TNF therapy will inhibit the secretion of pro-inflammatory factor TNF-α. Anti-IL-12/23 therapy works by inhibiting the production of pro-inflammatory factor IL-12 and IL-23 by antigen-presenting cells. Anti-integrin therapy inhibits the accumulation of white blood cells in intestinal and alleviates intestinal inflammatory. But these biological agents are expensive and many patients may experience unresponsive and intolerant states. Therefore, it is urgent to study effective and safe methods to treat UC.
In the recent years, regulating gut microbiota has become a hot topic in the treatment of UC. Therefore, as a promising method for treating IBD, probiotics act as live microorganisms have therapeutic effects on IBD which is caused by intestinal ecological disorders and other reasons. The treatment of IBD can be achieved through its antioxidant effects [ 57 ], the regulatory effect on gut microbiota [ 58 ], anti-inflammatory effect [ 59 ], the promotion effect to intestinal barrier integrity [ 60 ] and so on. As an indigestible food ingredient, prebiotics can also be used to treat or alleviate UC by regulating the redox system, immune system, etc. It can also selectively regulate colon microbiota, for example, enhancement of beneficial intestinal bacteria and inhibition of the growth of pathogenic microorganisms. All of these suggests that probiotics and prebiotics have a lot of room to develop as new form of treatment.
Effect and mechanism of probiotics and prebiotics in treating UC
Probiotics are nonpathogenic living microorganisms which, when administered in adequate amounts, have been shown to confer health benefits to the host and regulate intestinal microecological balance. Probiotics are widely used in medical application to prevent or treat many diseases, such as obesity [ 61 ], hepatocellular Carcinoma [ 62 ], autoimmune hepatitis [ 63 ], diabetic retinopathy [ 64 ], and alcoholic liver disease [ 65 ] and so on. The therapeutic effects of probiotics on UC have also been confirmed in animals and humans (Tables 1 and 2 ). Thus, therapeutic interventions with probiotics may offer new treatment for UC. Here, the possible effects and mechanisms of probiotics in the treatment of UC are summarized in Fig. 2 .

The potential mechanism of probiotics in alleviating Ulcerative Colitis (UC). Probiotics that enter the gut can bind with corresponding receptors (e.g. PTK) which are on the intestinal epithelial cells, then inhibit its stimulation to MAPKKK (e.g. TNK1, ASK1, MEKK1, MLK3), further suppress the activation of MAPKK (e.g. MKK3/6, MKK4/7) which are activated by MAPKKK, thereby inhibiting the activation of MAPK (e.g. p38, JNK1,2,3). Blocking the transcription factor transcribe of relevant genes (e.g. Cyclin D1, Raf). Finally, inhibition the inflammatory, apoptosis, and differentiation activated by this pathway. Meanwhile, probiotics protect the intestinal barrier by increasing the levels of tight junction proteins of ZO-1 and Occludin between intestinal epithelial cells, preventing the invasion of pathogenic microorganisms. In addition, probiotics can bind with its receptors (e.g. TLR) on the intestinal epithelial cells, inhibiting the activation of adaptor protein (e.g. RIP1) and suppressing the recruitment of TAB/TAK complex, thereby inhibiting the ubiquitination degradation of IκB by ubiquitinatingNEMO. Prevents the release of NF-κB proteins (RelA/p50) to nucleus. Ultimately inhibits the transcription of proinflammatory factors (e.g. TNF-β) and reduces the promotion effect of TNFα releasing by macrophages to this pathway. Meanwhile, probiotics act on intestinal epithelial cells-associated receptors (e.g. TLR), then phosphorylate AKT, and inhibit the degradation of Nrf2. Nrf2 enters the nucleus and promotes the expression of a range of cytoprotective genes (e.g. SOD, CAT, GSH).
Probiotics therapy
Experimental studies.
Convincing evidence from animal studies indicate that probiotics treatment can relieve UC (Table 1 ). Wu et al. [ 66 ] found that the use of Bifidobacterium longum CCFM1206 to treat Dextran-Sulfate-Sodium (DSS) induced Colitis mice will promotes the conversion of Glucoraphanin (GRP) to sulforaphane (SFN). SFN help to upregulate the Nrf2 signaling pathway and inhibit the NF-κB activity, which can ameliorate DSS-induced colitis. The result also indicated that the intervention of B.longum CCFM1206 could relieve the dysbiosis of intestinal microbiota. That is, promoted the proportion of Alistipes , Bifidobacterium , Blautia and Lachnospiraceae NK4A136 group and inhibited the proportion of Acinetobacter , and Lachnospiraceae A2 in the gut. Similar study, Han et al. [ 67 ] demonstrated that Bifidobacterium infantis enhances genetic stability by maintaining the balance of gut flora to increase anaphase-promoting complex subunit 7 (APC7) expression in colonic tissues, changing gut flora such as an increase in B.infantis . Then reducing DSS-induced colonic inflammation. Consistent with the above results, Fu et al. [ 68 ] found that Bacteroides xylanisolvens AY11-1 regulate the intestinal microbiota through the efficient degradation of alginate, improving the dysbiosis of intestinal ecology and promoting the growth of beneficial bacteria, for example, the increase of Blautia spp and Prevotellaceae UCG-001. Then ameliorated the symptoms of DSS-induced UC in mice. Wang et al. [ 69 ] revealed that the administration of probiotic Companilactobacillus crustorum MN047 in DSS-induced UC mice resulted in the expression of tight junctions, and down-regulation of pro-inflammatory and chemokine expression. It was also found that an increase of goblet cells, MUCs, TFF3, and TJs in the probiotic group, which demonstrated that the treat with CCMN could enhance the gut barrier function. And confirmed by fecal microbiota transplantation (FMT), the mechanisms of CCMN alleviating UC were partly due to its modulation to gut microbiota. The result showed that an increase in Bacteroidaceae and Burkholderiaceae and a decrease in Akkermansiaceae and Eggerthellaceae . Hu et al. [ 70 ] also found that Selenium-enriched Bifidobacterium longum DD98 administration alleviated the symptoms caused by DSS, inhibited the expression of the pro-inflammatory cytokines, decreased the level of oxidative stress, promoted the expression of tight junction proteins, inhibited the activation of toll-like receptor 4 (TLR4), and regulated the gut flora. They found that after the treatment of Se-B. longum DD98, the phylum of Bacteroidetes decreased and the phylum of Firmicutes increased. All of the above can be effective attenuated DSS-induced colitis in mice. In another study, the results of Han et al.’s [ 71 ] study of Lacticaseibacillus rhamnosus Hao9 in DSS-induced UC mice showed that the use of Hao9 attenuated weight loss which is caused by DSS, lowered DAI scores, attenuated colonic damage and inflammatory infiltrates and promoted the growth of Faecalibaculum and Romboutsia in the gut. The researcher attributed the observed effects of Hao9 on UC to its ability to inhibit lipopolysaccharide-induced intestinal IκB activation of mice. Consistent with the above results, Huang et al. [ 72 ] also showed that Lactobacillus paracasei R3 supplementation improved the general symptoms of murine colitis, attenuated inflammatory cell infiltration and more. And it was showed that the imbalance of Treg/Th17 cell in the intestinal inflammation caused by DSS was restored after treatment with L.p R3. Similarly, Xu et al. [ 73 ] investigated the effect of Saccharomyces boulardii and its postbiotics on DSS-induced UC in mice, showing that both S. boulardii elements and its postbiotics could significantly alleviate weight loss, reduce colonic tissue damage, regulate the balance of pro/anti-inflammatory cytokines in serum and colon, promote the expression of colonic tight junction proteins, and regulate the stability of intestinal microecology in mice. Changing in the bacterial flora were characterized by a significant increase in Turcibacter at the genus level, which collectively attenuate DSS-induced colitis. Komaki et al. [ 74 ] administered Lactococcus lactis subsp.lactis JCM5850 to mices with colitis induced by DSS and found that moderate amounts of L. lactis had a mitigating effect on colitis. In keeping with these results, Hizay et al. [ 75 ] also found that Lactobacillus acidophilus reduces abnormally high levels of serotonin in colon tissue in acetic acid-induced UC and relieves inflammation in intestinal tissue. As with the results above, Gao et al. [ 76 ] made Saccharomyces boulardii into suspension, observing its effect on DSS induced colitis in mice. The results suggested that S. boulardii can alleviate the clinical symotoms of colitis in mice exposed to DSS and the histological lesions. And it was found that the mechanism of S. boulardii to treat UC is inhibite nuclear transcription factor kappa B (NF-κB) and activate nuclear factor erythroid 2-related factor 2 (Nrf2) signaling pathway. As demonstrated by He [ 77 ] et al., Enterococcus faecium administration prevented DSS-induced intestinal inflammation and intestinal flora dysbiosis and particially repaired the damage to intestinal mucosal barrier and tight junctions. The modulatory effect on intestinal flora was characterized by an increase in Butyricicoccus sp., Lactobacillus sp., and Bifidobacterium sp. and a decrease in Ochrobactrum sp. and Acinetobacter sp. .
By studying the effects of tetrapeptide from maize (TPM) and probiotic (5 Lactobacillus strains: L.animalis- BA12, L.bulgaricus- LB42, L.paracasei- LC86, L.casei- LC89 and L.plantarum- LP90) in mice with DSS-induced UC, Li et al. [ 78 ] found that it could reduce the level of oxidative stress, attenuate the loss of kidney and colon, and regulate the intestinal flora to alleviate the inflammatory effects of UC. Wherein, the modulation effect to gut microbiota in manifested as an increase in Muribaculaceae, Alistipes, Ligilactobacillus and Lactobacillus . Recently, Shang et al. [ 79 ] reported that Bifidobacterium bifidum H3-R2 can effectively alleviate of pathogenesis by inhibiting inflammatory signaling, maintaining intestinal ecological homeostasis, and protecting colonic integrity. B.bifidum H3-R2 administration similarly affected the composition of gut microbiota, showing that B.bifidum H3-R2 caused a significant increase in the abundance of Bifidobacterium and Lactobacillus and a decrease in Enterobacter , Enterococcus and Streptococcus . Chen et al. [ 80 ] also discovered Lactobacillus fermentum ZS40 could inhibit DSS-induced mice colon shortening, colon damage, and intestinal wall thickening. It does so by inhibiting the activation of NF-κB and MAPK signaling pathways, and ultimately relieved inflammation.
To sum up, these results provide important clues for the design and use of more effective probiotic agents to treat UC and may provide new insights into the mechanisms by which host-microbe interactions confer the protective effect. And probiotics as additionally supplemented active micro-organisms, may have better value in clinical applications as drugs in the future [ 81 ].
Clinical studies
There are many contributing factors to UC, but much evidence suggests a strong link between host gut microbes and the treatment of UC pathogenesis, and suggests that mediation of gut microbes is the key to treating UC. Probiotics have been shown to alleviate UC by altering the composition of the gut microbiota and many other ways. A growing number of clinical trials have also demonstrated the therapeutic effects of probiotics in UC (Table 2 ). As early as 2010, Hegazy et al.’s [ 82 ] study showed that administration of probiotics ( Lactobacillus delbruekii and L. fermentum ) not only decreased the NF-κB DNA binding activity, but also reduced the accumulation of leukocytes, and down-regulated levels of pro-inflammatory factors, and thereby ameliorated the severity of the colitis. Similarly, in order to study the long-term effect of probiotics on UC, Palumbo et al. [ 83 ] conducted a clinical study and the results of the study showed that patients in the probiotics ( L. salivarius , L.acidophilus and B.bifidus strain BGN4) treatment group had better outcomes which is reflected through MMDAI. Thus, the use of probiotics may enhance the anti-inflammatory effect. Similar results, Bjarnason et al. [ 84 ] tried to prove the impact of the probiotic Symprove (including Lactobacillus rhamnosus NCIMB 30,174, Lactobacillus plantarum NCIMB 30,173, Lactobacillus acidophilus NCIMB 30,175 and Enterococcus faecium NCIMB 30,176) which contains four naturally occurring bacterial strain for this experiment. Research showed that Symprove are associated with reduced intestinal inflammation in UC patients. In line with these results, Tsuda et al. [ 85 ] gave patients with moderate to severe UC treated with BIO-THREE (containing Streptococcus faecalisa T-110, Clostridium butyricum TO-A and Bacillus mesentericus TO-A). Researchers found that the treated with BIO-THREE were able to improve clinical and endoscopic examinations in about half of UC patients who were intolerant to conventional therapy. And its intake improved intestinal microflora, the main change may be an increase in bifidobacteria. After a six-week study, Agraib et al. [ 86 ] found that patients in the probiotic (containing nine Lactobacillus and five Bifidobacterium species) group had higher levels of anti-inflammatoty and better clinical symptoms compared with the placebo group. Groeger et al. [ 87 ] demonstrated that Bifidobacterium infantis 35,624 achieved palliate effect to UC primarily by reducing intestinal inflammatory biomarkers (e.g. CRP, TNF-α, IL-6). In 2021, the study conducted by Gu et al. [ 88 ] revealed that Akkermansia muciniphila activate aryl hydrocarbon receptor (AhR) signaling, inhibite Kyn pathway (KP) activation, and restore the down-regulation of anti-inflammatory factors through increasing the levels of indoleacetic acid (IAA) and indole acrylic acid (IA) in the tryptophan (Trp) metabolic pathway. Similarly, the mitigation effect of probiotics (containing L.casei Zhang, L.plantarum P-8 and B.animalis subsp. lactis V9) was demonstrated in a trail by Chen et al. [ 89 ] in the treatment of UC. And the researchers found that the probiotic group had more beneficial bacteria, such as Eubacterium ramulus , Pediococcus pentosaceus , Bacteroides fragilis and Weissella cibaria .
All in all, these clinical studies have shown that the effectiveness of treating UC patients with probiotics is increasingly being proven. Above all, probiotics intervention might be a potentially effective approach in the treatment of UC by restoration of gut microbiota. Meanwhile, therapies that may most efficiently bring the disease under control are still being sought.
Prebiotics therapy
Prebiotics are selectively fermentable, non-digestible oligosaccharides, or ingredients. They function to accelerate beneficial bacterial growth and suppress harmful bacterial growth, thus adjusting the balance of gut microbiota. In addition, they can lead to the production of SCFAs, regulate immune response, control gene expression in bacterial cells, and improve absorption of micronutrients. And prebiotics are used to treat a wide variety of disease, such as obesity [ 90 ], chronic enteritis [ 91 ], skin disease [ 92 ] and autism spectrum disorder [ 93 ]. The therapeutic effects of prebiotics on UC have also been confirmed in animal and humans (Tables 3 and 4 ). Thus, Prebiotics can be used as a novel dietary management approach for UC. Here, the possible effects and mechanisms of prebiotics in the treatment of UC are summarized in Fig. 3 .
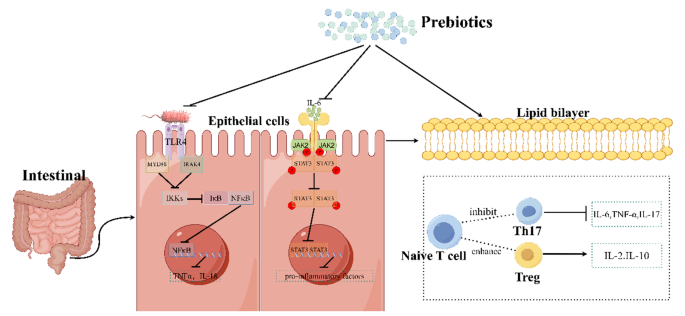
The mechanism of prebiotics in alleviating Ulcerative Colitis in Mice. It was found that the mechanism of prebiotics alleviate UC is probably through inhibiting of the TLR4/NF-κB signaling pathway, the JAK2/STAT3 signaling pathway, and regulating the ratio of T cell subsets. Firstly, prebiotics inhibit the activation effect of lipopolysaccharides from Gram-positive bacteria on TLR4 receptors, thereby inhibiting NF-κB from being released into nucleus and thus reducing the transcription of pro-inflammatory factors. Secondly, prebiotics can inhibit the activation of cytokine receptors by IL-6, thus suppress the entry of STAT3 into the nucleus and likewise inhibit its production of pro-inflammatory factors. Thirdly, prebiotics can inhibit of the conversion of naive T cells into Th17 cells and promote of their conversion into Treg cells, causing an increase of the expression of anti-inflammatory. (This mechanism diagram was drawn by Figdraw ( https://www.figdraw.com ))
Convincing evidence from animal studies indicate that prebiotics treatment can relieve UC. Koleva et al. [ 94 ] showed that fructo-oligosaccharides (FOS) promoted Bifidobacterium spp. and inulin and FOS can all decrease Clostridium cluster XI in rats, while Bifidobacterium spp. and Clostridium cluster XI correlated negatively and positively, respectively, to chronic intestinal inflammation. That is, both this two fructans inhibited intestinal inflammation. Hoentjen et al. [ 95 ] also orally administered a prebiotic combination of chicory-derived long-chain inulin-type fructans and short-chain inulin fraction oligofructose to HLA-B27 transgenic rats and found that this prebiotic can significantly reduce colitis and demonstrated that this effect was not only related to the gut microbiota, but also to immunomodulatory effects. They found that the prebiotic can promote the increase of bifidobacteria and endogenous lactobacilli. In immunomodulation, for example, it is possible to increase TGF-β in cecum. Wang et al. [ 96 ] allowed C57BL/6 mice with UC to receive oral administration of stachyose which is a prebiotic that traditionally extracted from plants for a period of time, and demonstrated the effect of stachyose on the recovery of body weight and found that it can reduced colonic tissue damage, lowered the level of pro-inflammatory cytokines, and restored the dysbiosis of the intestinal microbiota imblance (reduce the abundance of Escherichia_Shigella , Parabacteroides , Romboutsia and Turicibacter and raise the abundance of Alistipes and Roseburia ). In the study of Lunken et al. [ 97 ], they used an adoptive T-cell transfer mice model of colitis to examine the effects of enriching exclusive enteral nutrition (EEN) with inulin-type fructans (IN) (ENN IN) on colitis and found that a less deterioration of the mucus layer, increased butyrate production, and the expansion of anti-inflammatory T-cell subsets, including IL-10 producing Foxp3 + Tregs. And they also found an increased relative abundance of beneficial microbes ( Bifidobacterium spp. and Anaerostipes caccae ) and an reduced relative abundance of potentially pathogenic microbes ( Escherichia Shigella spp.). All of these results continue to prove the benefits of prebiotics in UC. Li et al. [ 98 ] established the DSS-induced mice model of colitis by evaluating the therapeutic effects of prebiotics high-substituted hydroxypropyl cellulose (HHPC) and low-substituted hydroxypropyl cellulose (LHPC) on UC, and the results confirmed that these two prebiotics dose-dependently ameliorated the inflammation in colitis mice, inhibited pro-inflammatory cytokine and regulated the balance of intestinal flora, including increased the relative abundance of Bacteroides and Alloprevotella genus and reduced the relative abundance of Firmicutes. Kanauchi et al. [ 99 ] investigated the effect of Germinated barley foodstuff (GBF), a prebiotic product, on the gut environment and found that it can inhibited the expression of STAT3 and NF-κB, thereby reducing the inflammatory response of the epithelium.
In summary, these animal experiments have showed the good effect of prebiotic therapy alone or in combination to UC. This provides a new direction in the clinical treatment of UC.
Many clinical studies have demonstrated the benefits of prebiotics for people with UC. Oligofructose and Inulin as the oligosaccharide fraction of Raftilose and the oligosaccharide fraction of Raftiline, which was obtained by the extraction of chicory roots, Gibson et al. [ 100 ] have demonstrated the stimulatory effect of these two substances on intestinal bifibacteria, which is a bacterium thought to be beneficial to health through clinical experiment and reduced some pathogenic bacteria that can produce toxins or hydrolyzed proteins, including bacteroides, clostridia, and fusobacteria. Vulevic et al. [ 101 ] found that Galactooligosaccharides (GOSs) promoted the population of beneficial bacteria, especially bifidobacteria and lactobacilli, and reduced numbers of less beneficial bacteria (bacteroides, the C. histolyticum group, E. coli , and Desulfovibrio spp.), and also enhanced the immune response and reduced the production of pro-inflammatory factors. Similarly. Casellas et al. [ 102 ] demonstrated that oligofructose-enriched inulin reduced intestinal inflammation by measuring fecal calprotectin levels in patients. Faghfoori et al. [ 103 ] administrated germinated barley foodstuff (GBF) to patients with UC and showed that GBF were able to reduce serum levels of pro-inflammatory including IL-6, IL-8,TNF-α. As demonstrated by Mitsuyama et al. [ 104 ], by determining the changes of microorganisms in the feces of patients with UC after four weeks of oral administration of GBF, the results proved that prebiotics can increase the concentration of fecal Bifidobacterium and Eubacterium limosum and increase the concentration of colonic butyrate, which is a source of energy for epithelium. And decreased the presence of Bacteroides .
Ryan et al. [ 105 ] conducted in vitro and in vivo experiments and demonstrated the promoting effect of \( {2}^{{\prime }}\) -fucosyllactose ( \( {2}^{{\prime }}\) -FL) which is a prebiotic human milk oligosaccharide on butyric acid producers, including Bifidobacterium , Clostridium cluster XIVa and Roseburia spp. Butyric acid, on the other hand, as a kind of SCFA, can inhibit the inflammatory response. In this study, they also found a significant increase in fecal Faecalibacterium prausnitzii , Anaerotruncus colihominis , and Pseudoflavonifractor species. Consistent with the above results, Suzuki et al. [ 106 ] tested the effectiveness of Bifidogenic growth stimulator (BGS) which is a prebiotic preparation produced by Propionibacterium freudenreichii isolated from Swiss cheese in patients with UC and found that it can selectively stimulated the activation of Bifidobacteria , which not only produced butyrate to nourish colonocytes and inhibited cytokine production and activation of NF-κB pathway, but also improved the balance of the intestinal microflora to maintain intestinal mucosal integrity and prevented intestinal damage. In the clinical study by Li et al. [ 107 ], they demonstrated the potential of Xylo-oligosaccharide (XOS) to alleviate microecological dysbiosis in patients with UC by measuring the effect of XOS on the intestinal flora. They found that XOS promotes the proliferation of Bifidobacteria , which produces a variety of organic acids and inhibits the growth of harmful bacteria by altering their metabolites.
In conclusion, these clinical studies demonstrated the palliative effects of prebiotics on UC, showing that prebiotics hold promise as primary or adjunctive maintenance therapy for UC.
Concluding remarks
UC as a common disease has become a financial burden for many people and has the potential to develop into cancer if not prevented or treated. Therefore, it is important to identify and intervene in a timely manner. The pathogenesis of UC is complex, that’s why it’s important to find a reliable treatment. There is a strong and complex relationship between gut microbiota and gut. Crucially, growing evidence strongly suggests that the gut microbiota plays a pivotal role in intestinal defense function, immune regulatory function, inflammatory responses, as a result, the development and progression of UC. Meanwhile, mechanistic studies have demonstrated these particular species of intestinal commensal bacteria capable of playing either a protective or pathogenic role in UC development. Traditional treatment methods come with a lot of side effects. And probiotics and prebiotics emerge as a new therapeutic modality to modulate the gut microbiota. Based on these, numerous animal and clinical studies have shown that regulating gut microbiota may be an effective strategy to treat UC.
Probiotics being able to confer notable health benefits by modulating the composition of gut microbiota and restoring the physiological bacterial flora. However, while an increasing number of studies have pointed to the therapeutic effects of probiotics on UC, the available data in this field remain limited and the relevant scientific work is still in its early stages. Thus, further research is still necessary. Firstly, due to the complex relationship between gut microbiota and UC, in order to better use probiotics to treat UC, it is necessary to further study the mechanism of intestinal flora affecting the occurrence and development of UC through more animal and clinical experiments. Secondly, we need to know how these probiotics regulate gut microbiota or how they function in the intestinal and what factors contribute to their long-run stability in both health and disease. Changes in certain pathway molecules can be probed to determine the specific mechanism of probiotic treats UC. Meanwhile, in the study of probiotics in the treatment of UC, we should pay more attention to the etiology and pathogenesis. Based on this, the composition and metabolites of probiotics should be of great concern. In particularly, it should be thoroughly studied for their antioxidant effects, anti-inflammatory properties, maintenance of the intestinal homeostasis, regulation of mucosal immune homeostasis, and so on. Some key probiotic components and metabolites may be highly effective postbiotic in the treatment of UC. Thirdly, most medications for the treatment of UC have many adverse effects. Meanwhile, probiotics have great potential as drugs to treat UC. Therefore, it may be more cost-efficient to invest more effort in probiotics than in developing new anti-inflammatory drugs. Fourth, in order to provide more effective probiotics to clinical, we can study the beneficial gut microbiota of healthy humans to dig out more and better probiotics. At the same time, it is necessary to search for the most effective probiotic compositions for the treatment of UC. Fifth, more clinical rationalized trials should be carried out to determine whether probiotics is safe and effective in the treatment of UC. Furthermore, because the composition of the gut microbiota is related to region, ethnicity, and diet, it is necessary to study large samples of people in different regions. Sixth, we must figure out the route of administration of the probiotics as well as the dosage, to ensure the probiotics will maximize the benefits in patient’s body under safe administration. Seventh, in order to make it easier and more convenient for patients to use probiotics, such as how to keep probiotics maintain highly active in some way and make it easier for patients to take, we should further explore the production and preservation of probiotics. Last but not least, to accepted by patients as a reliable treatment, it should be clarified for which patients a particular probiotic is effective, or which is preferable for a single probiotic or a blend of strains. So, there are still many problems it faces. In the future, probiotic therapy may be a potentially useful approach for UC, but research in this area has just started.
Prebiotics offer an exciting new approach to dietary management of gastrointestinal disorders including UC. It has been accepted as a dietary food ingredient that helps to nourish gut microbes, which can improve health and prevent UC. But while many studies to date have demonstrated the beneficial effects of prebiotics in UC, it still faces numerous challenges. Now many studies have the limitation of too small a sample size or lack of a control group, so the evidence for a significant effect of prebiotics is still lacking. The dosage of prebiotics is also a question to be confirmed, if too high a dosage will lead to tolerance, or if a higher dosage of prebiotics will produce better results when well tolerated. With so many types of prebiotics available, it is also deserving of further study as to which prebiotics have better results for which type of UC patients. Although a large number of in vitro and in vivo experiments have confirmed the positive effects of prebiotics, there is still a need for more clinical trials or animal experiments to further evaluate their specific effects.The specific mechanism by which we found that prebiotics alleviate UC remains unclear. It’s worth exploring further. In-depth experiments are needed to further elucidate the role of prebiotics in patients with UC, whether it is their own structure or their metabolites that play a role. And to meet the needs of consumers, new strategies for cost-effective and efficient prebiotics can be developed. Prebiotics, as a food-sourced ingredient for the treatment of UC, offer a new clinical direction, and it is important to study its good effects and side effects as clearly as possible. Therefore, in any case, the prospect of the application of prebiotics in UC is worthy of attention and expectation.
Certainly, in order to gain wider acceptance and recognition for probiotics and prebiotics to treat UC, further research is urgently required.
Data availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Hijova E, Soltesova A. Effects of probiotics and prebiotics in ulcerative colitis. Bratislava Med J. 2013;114(09):540–3.
Article CAS Google Scholar
Ng SC, Shi HY, Hamidi N, Underwood FE, Tang W, Benchimol EI, et al. The Worldwide Incidence and Prevalence of Inflammatory Bowel Disease in the 21 St Century: a systematic review of Population-Based studies. Gastroenterology. 2017;152(5):S970–1.
Article Google Scholar
Iheozor-Ejiofor Z, Kaur L, Gordon M, Baines PA, Sinopoulou V, Akobeng AK. Probiotics for maintenance of remission in ulcerative colitis. Cochrane Database of Systematic Reviews. 2020;3(3):CD007443.
Mladenova D, Kohonen-Corish MRJ. Mouse models of inflammatory bowel disease - insights into the mechanisms of inflammation-associated Colorectal Cancer. Vivo. 2012;26(4):627–46.
CAS Google Scholar
Li J, Ueno A, Fort Gasia M, Luider J, Wang T, Hirota C, et al. Profiles of Lamina Propria T Helper Cell subsets discriminate between Ulcerative Colitis and Crohnʼs Disease. Inflamm Bowel Dis. 2016;22(8):1779–92.
Article PubMed Google Scholar
Shen Z-H, Zhu C-X, Quan Y-S, Yang Z-Y, Wu S, Luo W-W, et al. Relationship between intestinal microbiota and ulcerative colitis: mechanisms and clinical application of probiotics and fecal microbiota transplantation. World J Gastroenterol. 2018;24(1):5–14.
Article CAS PubMed PubMed Central Google Scholar
Yao SY, Zhao ZX, Wang WJ, Liu XL. Bifidobacterium Longum: Protection against Inflammatory Bowel Disease. Journal of Immunology Research. 2021:8030297.
Zou JF, Shen YM, Chen MJ, Zhang ZM, Xiao SW, Liu C, et al. Lizhong decoction ameliorates ulcerative colitis in mice via modulating gut microbiota and its metabolites. Appl Microbiol Biotechnol. 2020;104(13):5999–6012.
Article CAS PubMed Google Scholar
Rather IA, Majumder R, Alshammari FH, Park JG, Bajpai VK. Ulcerative colitis and probiotics: an overview. Pak J Pharm Sci. 2016;29(5):1877–80.
CAS PubMed Google Scholar
Peyrin-Biroulet L, Sandborn W, Sands BE, Reinisch W, Bemelman W, Bryant RV, et al. Selecting therapeutic targets in inflammatory bowel disease (STRIDE): determining therapeutic goals for treat-to-target. Am J Gastroenterol. 2015;110(9):1324–38.
Kushkevych I, Martinkova K, Vitezova M, Rittmann SKR. Intestinal microbiota and perspectives of the Use of Meta-Analysis for comparison of Ulcerative Colitis studies. J Clin Med. 2021;10(3):462.
Jostins L, Ripke S, Weersma RK, Duerr RH, McGovern DP, Hui KY, et al. Host-microbe interactions have shaped the genetic architecture of inflammatory bowel disease. Nature. 2012;491(7422):119–24.
Barrett JC, Lee JC, Lees CW, Prescott NJ, Anderson CA, Phillips A, et al. Genome-wide association study of ulcerative colitis identifies three new susceptibility loci, including the < i > HNF4A region. Nat Genet. 2009;41(12):1330–U99.
Ordas I, Eckmann L, Talamini M, Baumgart DC, Sandborn WJ. Ulcerative colitis. Lancet. 2012;380(9853):1606–19.
Sands BE, Kaplan GG. therapeutic review the role of tnfα α in ulcerative colitis.2007;47(8):930-41.
Zhang FX, Kirschning CJ, Mancinelli R, Xu XP, Jin Y, Faure E, et al. Bacterial lipopolysaccharide activates nuclear factor-kappab through interleukin-1 signaling mediators in cultured human dermal endothelial cells and mononuclear phagocytes. J Biol Chem. 1999;274(12):7611–4.
Selin KA, Hedin CRH, Villablanca EJ. Immunological networks defining the heterogeneity of Inflammatory Bowel diseases. J Crohns Colitis. 2021;15(11):1959–73.
Article PubMed PubMed Central Google Scholar
Heller F, Florian P, Bojarski C, Richter J, Christ M, Hillenbrand B, et al. Interleukin-13 is the Key Effector Th2 Cytokine in Ulcerative Colitis that affects epithelial tight junctions, apoptosis, and cell restitution. Gastroenterology. 2005;129(2):550–64.
Zhu QG, Rui K, Wang SJ, Tian J. Advances of Regulatory B cells in Autoimmune diseases. Front Immunol. 2021;12:12:592914.
Dave M, Higgins PD, Middha S, Rioux KP. The human gut microbioma current knowledge, challenges, and future directions. Translational Res. 2012;160(4):246–57.
He XL, Gao J, Peng L, Hu TT, Wan Y, Zhou MJ, et al. Bacterial O-GlcNAcase genes abundance decreases in ulcerative colitis patients and its administration ameliorates colitis in mice. Gut. 2021;70(10):1872–83.
Li BL, Du PL, Du Y, Zhao DY, Cai YR, Yang Q et al. Luteolin alleviates inflammation and modulates gut microbiota in ulcerative colitis rats. Life Sci. 2021;269:269:119008.
Guo XY, Liu XJ, Hao JY. Gut microbiota in ulcerative colitis: insights on pathogenesis and treatment. J Dig Dis. 2020;21(3):147–59.
Mizoguchi E, Tong M, Li X, Wegener Parfrey L, Roth B, Ippoliti A et al. A Modular Organization of the Human Intestinal Mucosal Microbiota and its Association with Inflammatory Bowel Disease. PLoS ONE. 2013;8(11):e80702.
Andoh A, Ida S, Tsujikawa T, Benno Y, Fujiyama Y. Terminal restriction fragment polymorphism analyses of fecal microbiota in five siblings including two with ulcerative colitis. Clin J Gastroenterol. 2009;2(5):343–5.
Fuentes S, Rossen NG, van der Spek MJ, Hartman JHA, Huuskonen L, Korpela K, et al. Microbial shifts and signatures of long-term remission in ulcerative colitis after faecal microbiota transplantation. ISME J. 2017;11(8):1877–89.
Kotlowski R, Bernstein CN, Sepehri S, Krause DO. High prevalence of Escherichia coli belonging to the B2 + D phylogenetic group in inflammatory bowel disease. Gut. 2007;56(5):669–75.
Xu J, Chen N, Wu Z, Song Y, Zhang Y, Wu N et al. 5-Aminosalicylic acid alters the gut bacterial microbiota in patients with Ulcerative Colitis. Front Microbiol. 2018;9:1274.
Schwiertz A, Jacobi M, Frick J-S, Richter M, Rusch K, Köhler H. Microbiota in Pediatric Inflammatory Bowel Disease. J Pediatr. 2010;157(2):240–e41.
Khalil NA, Walton GE, Gibson GR, Tuohy KM, Andrews SC. In vitrobatch cultures of gut microbiota from healthy and ulcerative colitis (UC) subjects suggest that sulphate-reducing bacteria levels are raised in UC and by a protein-rich diet. Int J Food Sci Nutr. 2013;65(1):79–88.
Verma R, Verma AK, Ahuja V, Paul J. Real-Time Analysis of Mucosal Flora in patients with inflammatory bowel disease in India. J Clin Microbiol. 2010;48(11):4279–82.
Walker AW, Sanderson JD, Churcher C, Parkes GC, Hudspith BN, Rayment N et al. High-throughput clone library analysis of the mucosa-associated microbiota reveals dysbiosis and differences between inflamed and non-inflamed regions of the intestine in inflammatory bowel disease. BMC Microbiol. 2011;11:7.
Tahara T, Shibata T, Kawamura T, Okubo M, Ichikawa Y, Sumi K, et al. Fusobacterium detected in Colonic Biopsy and Clinicopathological features of Ulcerative Colitis in Japan. Dig Dis Sci. 2014;60(1):205–10.
Machiels K, Joossens M, Sabino J, De Preter V, Arijs I, Eeckhaut V, et al. A decrease of the butyrate-producing speciesRoseburia hominisandFaecalibacterium prausnitziidefines dysbiosis in patients with ulcerative colitis. Gut. 2014;63(8):1275–83.
Lepage P, Häsler R, Spehlmann ME, Rehman A, Zvirbliene A, Begun A, et al. Twin study indicates loss of Interaction between Microbiota and Mucosa of patients with Ulcerative Colitis. Gastroenterology. 2011;141(1):227–36.
Fite A, Macfarlane S, Furrie E, Bahrami B, Cummings JH, Steinke DT, et al. Longitudinal analyses of gut mucosal microbiotas in Ulcerative Colitis in Relation to Patient Age and Disease Severity and Duration. J Clin Microbiol. 2013;51(3):849–56.
Ott SJ, Plamondon S, Hart A, Begun A, Rehman A, Kamm MA, et al. Dynamics of the Mucosa-Associated Flora in Ulcerative Colitis patients during remission and clinical relapse. J Clin Microbiol. 2008;46(10):3510–3.
Hu Y, Chen Z, Xu C, Kan S, Chen D. Disturbances of the gut microbiota and microbiota-derived metabolites in Inflammatory Bowel Disease. Nutrients. 2022;14(23):5140.
Andreopoulou M, Tsiouris V, Georgopoulou I. Effects of organic acids on the gut ecosystem and on the performance of broiler chickens. J Hellenic Veterinary Med Soc. 2017;65(4):289.
Agus A, Planchais J, Sokol H. Gut microbiota regulation of Tryptophan Metabolism in Health and Disease. Cell Host Microbe. 2018;23(6):716–24.
Singh R, Chandrashekharappa S, Bodduluri SR, Baby BV, Hegde B, Kotla NG et al. Enhancement of the gut barrier integrity by a microbial metabolite through the Nrf2 pathway. Nat Commun. 2019;10(1):89.
Rothhammer V, Mascanfroni ID, Bunse L, Takenaka MC, Kenison JE, Mayo L, et al. Type I interferons and microbial metabolites of tryptophan modulate astrocyte activity and central nervous system inflammation via the aryl hydrocarbon receptor. Nat Med. 2016;22(6):586–97.
Q W, RM M, BA C, M C-D, KJ Z. D G, - A bacterial carbohydrate links innate and adaptive responses through Toll-like. D– 2985109r. (– 0022-1007 (Print)):- 2853-63.
A I-V CDC, K JPAA. K, L A, - FXR and TGR5 Agonists Ameliorate Liver Injury, Steatosis, and Inflammation After. D– 101695860. (– 2471-254X (Electronic)):- 1379-91.
Agus A, Clément K, Sokol H. Gut microbiota-derived metabolites as central regulators in metabolic disorders. Gut: J Br Soc Gastroenterol. 2021;70(6):1174–82.
Wahlstrom A, Kovatcheva-Datchary P, Stahlman M, Backhed F, Marschall H-U. Crosstalk between bile acids and gut microbiota and its impact on farnesoid receptor signalling. Dig Dis. 2017;35(3):246–50.
Figliuolo VR, Coutinho-Silva R, Lara Melo Coutinho CM. Contribution of sulfate-reducing bacteria to homeostasis disruption during intestinal inflammation. Life Sci. 2018;215:145–51.
Cai Z, Wang S, Li J. Treatment of inflammatory bowel disease: a Comprehensive Review. Front Med (Lausanne). 2021;8:765474.
Tremblay L, Pineton de Chambrun G, De Vroey B, Lavogiez C, Delaporte E, Colombel JF, et al. Stevens-Johnson syndrome with sulfasalazine treatment: report of two cases. J Crohns Colitis. 2011;5(5):457–60.
Hayashi R, Wada H, Ito K, Adcock IM. Effects of glucocorticoids on gene transcription. Eur J Pharmacol. 2004;500(1–3):51–62.
Lichtenstein GR, Abreu MT, Cohen R, Tremaine W, American Gastroenterological A. American Gastroenterological Association Institute technical review on corticosteroids, immunomodulators, and infliximab in inflammatory bowel disease. Gastroenterology. 2006;130(3):940–87.
Curkovic I, Egbring M, Kullak-Ublick GA. Risks of inflammatory bowel disease treatment with glucocorticosteroids and aminosalicylates. Dig Dis. 2013;31(3–4):368–73.
Chhaya V, Saxena S, Cecil E, Subramanian V, Curcin V, Majeed A, et al. Steroid dependency and trends in prescribing for inflammatory bowel disease - a 20-year national population-based study. Aliment Pharmacol Ther. 2016;44(5):482–94.
D’Haens G. Systematic review: second-generation vs. conventional corticosteroids for induction of remission in ulcerative colitis. Aliment Pharmacol Ther. 2016;44(10):1018–29.
Jharap B, Seinen ML, de Boer NK, van Ginkel JR, Linskens RK, Kneppelhout JC, et al. Thiopurine therapy in inflammatory bowel disease patients: analyses of two 8-year intercept cohorts. Inflamm Bowel Dis. 2010;16(9):1541–9.
Herrlinger KR, Barthel DN, Schmidt KJ, Buning J, Barthel CS, Wehkamp J, et al. Infliximab as rescue medication for patients with severe ulcerative/indeterminate colitis refractory to tacrolimus. Aliment Pharmacol Ther. 2010;31(9):1036–41.
Moura FA, de Andrade KQ, Dos Santos JCF, Araujo ORP, Goulart MOF. Antioxidant therapy for treatment of inflammatory bowel disease: does it work? Redox Biol. 2015;6:617–39.
Hui L, Wei-Hsien L, Hanying Z, Haotian F, Wen Z, Wei-Lian H et al. Bifidobacterium lactis BL-99 protects mice with osteoporosis caused by colitis via gut inflammation and gut microbiota regulation. Food & Function. 2022;13(3):1482-1494.
Aghamohammad S, Sepehr A, Miri ST, Najafi S, Pourshafie MR, Rohani M. The role of combining Probiotics in Preventing and Controlling inflammation: a focus on the anti-inflammatory and Immunomodulatory effects of Probiotics in an in vitro model of IBD. Can J Gastroenterol Hepatol. 2022:2045572.
White R, Atherly T, Guard B, Rossi G, Wang C, Mosher C, et al. Randomized, controlled trial evaluating the effect of multi-strain probiotic on the mucosal microbiota in canine idiopathic inflammatory bowel disease. Gut Microbes. 2017;8(5):451–66.
Kang Y, Cai Y. The development of probiotics therapy to obesity: a therapy that has gained considerable momentum. Hormones. 2018;17(2):141–51.
Kang Y, Cai Y, Yang Y. The gut Microbiome and Hepatocellular Carcinoma: implications for early diagnostic biomarkers and Novel therapies. Liver Cancer. 2022;11(2):113–25.
Li LP, Kang YB. The gut Microbiome and Autoimmune Hepatitis: implications for early diagnostic biomarkers and Novel therapies. Molecular Nutrition & Food Research; 2023;67(24):e2300043.
Cai Y, Kang YB. Gut microbiota and metabolites in diabetic retinopathy: insights into pathogenesis for novel therapeutic strategies. Biomed Pharmacother. 2023;164:114994.
Liu HX, Kang X, Yang XD, Yang H, Kuang XY, Ren P, et al. Compound Probiotic ameliorates Acute Alcoholic Liver Disease in mice by modulating gut microbiota and maintaining intestinal barrier. Probiotics Antimicrob Proteins. 2023;15(1):185–201.
Wu J, Cui S, Tang X, Zhang Q, Jin Y, Zhao J, et al. Bifidobacterium longum CCFM1206 promotes the Biotransformation of Glucoraphanin to Sulforaphane that contributes to amelioration of Dextran-Sulfate-Sodium-Induced Colitis in mice. J Agric Food Chem. 2023;71(2):1100–12.
Han T, Hu X, Li K, Zhang D, Zhang Y, Li J. Bifidobacterium infantis maintains Genome Stability in Ulcerative Colitis via regulating anaphase-promoting Complex Subunit 7. Front Microbiol. 2021;12:761113.
Fu T, Wang Y, Ma M, Dai W, Pan L, Shang Q et al. Isolation of Alginate-degrading Bacteria from the human gut microbiota and Discovery of Bacteroides xylanisolvens AY11-1 as a Novel Anti-colitis Probiotic Bacterium. Nutrients. 2023;15(6):1352.
Wang T, Shi C, Wang S, Zhang Y, Wang S, Ismael M, et al. Protective effects of Companilactobacillus Crustorum MN047 against Dextran Sulfate Sodium-Induced Ulcerative Colitis: a fecal microbiota transplantation study. J Agric Food Chem. 2022;70(5):1547–61.
Hu Y, Jin X, Gao F, Lin T, Zhu H, Hou X et al. Selenium-enriched Bifidobacterium longum DD98 effectively ameliorates dextran sulfate sodium-induced ulcerative colitis in mice. Front Microbiol. 2022;13:955112.
Han M, Liao W, Si X, Bai C, Gai Z. Protective effects of lacticaseibacillus rhamnosus Hao9 on dextran sulphate sodium-induced ulcerative colitis in mice. J Appl Microbiol. 2022;133(3):2039–49.
Huang J, Yang Z, Li Y, Chai X, Liang Y, Lin B et al. Lactobacillus paracasei R3 protects against dextran sulfate sodium (DSS)-induced colitis in mice via regulating Th17/Treg cell balance. J Translational Med. 2021;19(1):356.
Xu X, Wu J, Jin Y, Huang K, Zhang Y, Liang Z. Both Saccharomyces boulardii and its postbiotics alleviate Dextran Sulfate Sodium-Induced Colitis in mice, Association with modulating inflammation and intestinal microbiota. Nutrients. 2023;15(6):1484.
Komaki S, Haque A, Miyazaki H, Matsumoto T, Nakamura S. Unexpected effect of probiotics by Lactococcus lactis subsp. lactis against colitis induced by dextran sulfate sodium in mice. J Infect Chemother. 2020;26(6):549–53.
Hizay A, Dag K, Oz N, Comak-Gocer EM, Ozbey-Unlu O, Ucak M et al. Lactobacillus acidophilus regulates abnormal serotonin availability in experimental ulcerative colitis. Anaerobe. 2023;80:102710.
Gao H, Li Y, Sun J, Xu H, Wang M, Zuo X, et al. Saccharomyces Boulardii ameliorates Dextran Sulfate Sodium-Induced Ulcerative Colitis in mice by regulating NF-κB and Nrf2 signaling pathways. Oxidative Med Cell Longev. 2021;2021:1–14.
Google Scholar
He W, Ni W, Zhao J, M’Koma A. Enterococcus faecium alleviates Gut Barrier Injury in C57BL/6 mice with Dextran Sulfate Sodium-Induced Ulcerative Colitis. Gastroenterol Res Pract. 2021;2021:1–9.
Li ZG, Zhang S, Xu L, Fang XX, Wan YZ, Yu DH, et al. A tetrapeptide from maize combined with probiotics exerted strong anti-inflammatory effects and modulated gut microbiota in DSS-induced colitis mice. Food Funct. 2022;13(24):12602–18.
Shang JC, Yang S, Tang ZX, Chen YH, Duan BF, Meng XC. Bifidobacterium bifidum H3-R2 and its Molecular Communication within the context of Ulcerative Colitis. J Agric Food Chem. 2022;70(37):11678–88.
Chen ZX, Yi L, Pan YN, Long XY, Mu JF, Yi RK et al. Lactobacillus fermentum ZS40 ameliorates inflammation in mice with Ulcerative Colitis Induced by Dextran Sulfate Sodium. Front Pharmacol. 2021;12:700217.
Ren Z, Hong Y, Huo Y, Peng L, Lv H, Chen J et al. Prospects of probiotic adjuvant drugs in clinical treatment. Nutrients. 2022;14(22):4723.
Hegazy SK. Effect of probiotics on pro-inflammatory cytokines and NF-κB activation in ulcerative colitis. World J Gastroenterol. 2010;16(33):4145-51.
Palumbo VD, Romeo M, Gammazza AM, Carini F, Damiani P, Damiano G, et al. The long-term effects of probiotics in the therapy of ulcerative colitis: a clinical study. Biomedical Papers-Olomouc. 2016;160(3):372–7.
Bjarnason I, Sission G, Hayee B. A randomised, double-blind, placebo-controlled trial of a multi-strain probiotic in patients with asymptomatic ulcerative colitis and Crohn’s disease. Inflammopharmacology. 2019;27(3):465–73.
Tsuda Y, Yoshimatsu Y, Aoki H, Nakamura K, Irie M, Fukuda K, et al. Clinical effectiveness of probiotics therapy (BIO-THREE) in patients with ulcerative colitis refractory to conventional therapy. Scand J Gastroenterol. 2009;42(11):1306–11.
Agraib LM, Yamani MI, Tayyem R, Abu-Sneineh AT, Rayyan YM. Probiotic supplementation induces remission and changes in the immunoglobulins and inflammatory response in active ulcerative colitis patients: a pilot, randomized, double-blind, placebo-controlled study. Clin Nutr ESPEN. 2022;51:83–91.
Groeger D, O’Mahony L, Murphy EF, Bourke JF, Dinan TG, Kiely B, et al. Bifidobacterium infantis35624 modulates host inflammatory processes beyond the gut. Gut Microbes. 2014;4(4):325–39.
Gu ZY, Pei WL, Shen YH, Wang LJ, Zhu J, Zhang Y, et al. Akkermansia muciniphila and its outer protein Amuc_1100 regulates tryptophan metabolism in colitis. Food Funct. 2021;12(20):10184–95.
Chen P, Xu HY, Tang H, Zhao FY, Yang CC, Kwok LY, et al. Modulation of gut mucosal microbiota as a mechanism of probiotics-based adjunctive therapy for ulcerative colitis. Microb Biotechnol. 2020;13(6):2032–43.
Carnahan S, Balzer A, Panchal SK, Brown L. Prebiotics in obesity. Panminerva Med. 2014;56(2):165–75.
Looijer-van Langen MA, Dieleman LA. Prebiotics in chronic intestinal inflammation. Inflamm Bowel Dis. 2009;15(3):454–62.
Baquerizo Nole KL, Yim E, Keri JE. Probiotics and prebiotics in dermatology. J Am Acad Dermatol. 2014;71(4):814–21.
Sanlier N, Kocabas S. The effect of probiotic, prebiotic and gut microbiota on ASD: a review and future perspectives. Crit Rev Food Sci Nutr. 2023;63(15):2319–30.
Koleva PT, Valcheva RS, Sun X, Ganzle MG, Dieleman LA. Inulin and fructo-oligosaccharides have divergent effects on colitis and commensal microbiota in HLA-B27 transgenic rats. Br J Nutr. 2012;108(9):1633–43.
Hoentjen F, Welling GW, Harmsen HJM, Zhang X, Snart J, Tannock GW, et al. Reduction of colitis by prebiotics in HLA-B27 transgenic rats is associated with microflora changes and immunomodulation. Inflamm Bowel Dis. 2005;11(11):977–85.
Wang C, Bai J, Wang B, Yu L, Tian F, Zhao J, et al. Stachyose modulates gut microbiota and alleviates DSS-induced ulcerative colitis in mice. Food Sci Hum Wellness. 2023;12(6):2211–20.
Lunken GR, Tsai K, Schick A, Lisko DJ, Cook L, Vallance BA, et al. Prebiotic enriched exclusive Enteral Nutrition suppresses colitis via gut microbiome modulation and expansion of anti-inflammatory T cells in a mouse model of colitis. Cell Mol Gastroenterol Hepatol. 2021;12(4):1251–66.
Li X, Lv H, Shi F, Song J, Zhang Z. The potential therapeutic effects of hydroxypropyl cellulose on acute murine colitis induced by DSS. Carbohydr Polym. 2022;289:119430.
Kanauchi O, Serizawa I, Araki Y, Suzuki A, Andoh A, Fujiyama Y, et al. Germinated barley foodstuff, a prebiotic product, ameliorates inflammation of colitis through modulation of the enteric environment. J Gastroenterol. 2003;38(2):134.
Gibson GR, Beatty ER, Wang X, Cummings JH, Gibson GR, Beatty ER, Wang X, Cummings JH. Selective stimulation of Bifidobacteria in the human colon by oligofructose and inulin. Gastroenterology. 1995;108(4):975– 82.
Vulevic J, Drakoularakou A, Yaqoob P, Tzortzis G, Gibson GR. Modulation of the fecal microflora profile and immune function by a novel trans-galactooligosaccharide mixture (B-GOS) in healthy elderly volunteers. Am J Clin Nutr. 2008;88(5):1438–46.
Casellas F, Borruel N, Torrejon A, Varela E, Antolin M, Guarner F, et al. Oral oligofructose-enriched inulin supplementation in acute ulcerative colitis is well tolerated and associated with lowered faecal calprotectin. Aliment Pharmacol Ther. 2007;25(9):1061–7.
Faghfoori Z, Navai L, Shakerhosseini R, Somi MH, Nikniaz Z, Norouzi MF. Effects of an oral supplementation of germinated barley foodstuff on serum tumour necrosis factor-alpha, interleukin-6 and– 8 in patients with ulcerative colitis. Ann Clin Biochem. 2011;48(Pt 3):233–7.
Mitsuyama K, Saiki T, Kanauchi O, Iwanaga T, Sata M. Treatment of ulcerative colitis with germinated barley foodstuff feeding: a pilot study. Aliment Pharmacol Ther. 1998;12(12):1225–30.
Ryan JJ, Monteagudo-Mera A, Contractor N, Gibson GR. Impact of 2’-Fucosyllactose on Gut Microbiota Composition in Adults with Chronic Gastrointestinal Conditions: Batch Culture Fermentation Model and Pilot Clinical Trial Findings. Nutrients. 2021;13(3):938.
Suzuki A, Mitsuyama K, Koga H, Tomiyasu N, Masuda J, Takaki K, et al. Bifidogenic growth stimulator for the treatment of active ulcerative colitis: a pilot study. Nutrition. 2006;22(1):76–81.
Li Z, Li Z, Zhu L, Dai N, Sun G, Peng L, et al. Effects of Xylo-Oligosaccharide on the gut microbiota of patients with Ulcerative Colitis in Clinical Remission. Front Nutr. 2021;8:778542.
Download references
Acknowledgements
Not applicable.
This work was supported by Shanxi Province Natural Science Foundation (Grant No. 202203021221182), Science Research Start-up Fund for Doctor of Shanxi Medical University (Grant No. XD1807), Science Research Start-up Fund for Doctor of Shanxi Province (Grant No.SD1807), Scientific and Technological Innovation Programs of Higher Education Institutions in Shanxi (Grant No. 2019L0425), and Shanxi Province Science Foundation for Youths (Grant No. 201901D211314).
Author information
Authors and affiliations.
Department of microbiology and immunology, School of Basic Medical Sciences, Shanxi Medical University, Taiyuan, Shanxi, China
Jing Guo, Liping Li & Yongbo Kang
Faculty of Life science and Technology, Kunming University of Science and Technology, Kunming, Yunnan, China
You can also search for this author in PubMed Google Scholar
Contributions
Jing Guo wrote the main manuscript text with the help of Liping Li, Xinwei Huang and Yongbo Kang. All authors reviewed the manuscript.
Corresponding author
Correspondence to Yongbo Kang .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Guo, J., Li, L., Cai, Y. et al. The development of probiotics and prebiotics therapy to ulcerative colitis: a therapy that has gained considerable momentum. Cell Commun Signal 22 , 268 (2024). https://doi.org/10.1186/s12964-024-01611-z
Download citation
Received : 10 October 2023
Accepted : 10 April 2024
Published : 14 May 2024
DOI : https://doi.org/10.1186/s12964-024-01611-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Ulcerative colitis
- Gut microflora
- Inflammation
Cell Communication and Signaling
ISSN: 1478-811X
- General enquiries: [email protected]
- Patient Care & Health Information
- Diseases & Conditions
- Ulcerative colitis
- What is ulcerative colitis? A Mayo Clinic expert explains
Listen to gastroenterologist William Faubion, M.D., walk through ulcerative colitis basics.
[Music playing]
William A. Faubion, Jr., M.D., Gastroenterology, Mayo Clinic I'm Dr. Bill Faubion, a gastroenterologist at Mayo Clinic. In this video, we'll cover the basics of ulcerative colitis. What is it? Who gets it? The symptoms, diagnosis, and treatment. Whether you're looking for answers for yourself or someone you love, we're here to give you the best information available.
Ulcerative colitis is an inflammatory bowel disease that causes chronic inflammation and ulcers in the superficial lining of the large intestine, also called the colon. And that includes the rectum. It's estimated that about a million Americans are living with ulcerative colitis, making it the most common form of inflammatory bowel disease. It can be painful and debilitating, occasionally leading to severe complications. It can also be emotionally stressful. And while there is no cure, once you've been diagnosed, treatment can help you get back to a much more normal and comfortable life.
Who gets it?
The exact cause of ulcerative colitis is unknown, but there are things that appear to trigger or aggravate it. It may involve an abnormal immune response against some microorganism in which your tissues are also attacked. Genetics might also play a role. You are at higher risk if a first-degree relative has it. There's also a correlation with age. Although it can show up at any stage of life, most people are diagnosed before the age of 30. And ethnicity is a risk factor. Whites have the highest risk, especially among people of Ashkenazi Jewish descent. While diet and stress don't cause ulcerative colitis, they are known to exacerbate symptoms.
What are the symptoms?
Most people have mild to moderate cases of ulcerative colitis. Although it can be more severe, you may also experience periods of remission when you have no issues at all. A person's symptoms depend on the severity of the case in the area of the colon that's involved. They usually develop over time, and they can include diarrhea, often with blood or pus, fever, fatigue, anemia, loss of appetite and weight loss, abdominal pain and cramping, rectal pain and bleeding, the need for a bowel movement, yet the inability to do so despite the urgency. And in children, delayed growth and development. Over time, ulcerative colitis can lead to other complications, such as severe dehydration, a perforated colon, bone loss, inflammation of your skin, joints and eyes. It can also increase your risk for blood clots and colon cancer. These symptoms don't automatically mean that you have ulcerative colitis. But if you're experiencing anything that concerns you, it's a good idea to make an appointment with your doctor.
How is it diagnosed?
The only way to definitively diagnose ulcerative colitis is with a biopsy after taking a tissue sample through an endoscopic procedure. But first, less invasive things can be done to rule out other causes. First, your doctor will consider your medical history. They may want to run a variety of tests or procedures. And at some point, your general practitioner may refer you to a specialist called a gastroenterologist like myself. A blood test can check for anemia and check for signs of infection. A stool study can test for white blood cells and other specific proteins that point to ulcerative colitis, as well as rule out certain pathogens. A colonoscopy may be needed. This allows your doctor to view the entirety of the large intestine using an endoscope, a small camera mounted on a thin flexible tube. They can take tissue samples for a biopsy at the same time. Or if your colon is extremely inflamed, they may do a flexible sigmoidoscopy, which only goes as far as the rectum and lower or sigmoid colon. If your symptoms are more severe, your doctor may want some imaging done. An abdominal x-ray can rule out serious complications, like a perforated colon. An MRI or CT scan can also be performed for a more detailed view of the bowel, as well as to reveal the extent of the inflammation.
How is it treated?
Although there is no cure for ulcerative colitis there are widely effective treatments, usually involving either drug therapy or surgery. Your doctor can work with you to find things that alleviate your symptoms and in some cases, even bring about long-term remission. Treatments may include anti-inflammatory drugs like corticosteroids and immune system suppressants. Certain targeted therapies directed against the immune system called biologics can help. Antidiarrheals, pain relievers, antispasmodics and iron supplements can help counter other symptoms. And surgery may be required to remove the damaged tissue. In extreme cases, the whole colon may be removed. Which sounds drastic, but this can sometimes be the best option for eliminating the pain and struggle of ulcerative colitis once and for all. Some of these therapies may have side effects themselves. So be sure to review the risks and benefits with your doctor.
Ulcerative colitis can be physically and emotionally challenging, but there are things that can help. Although there's no firm evidence that any foods cause ulcerative colitis, certain things seem to aggravate flare-ups. So a food diary can help you identify personal triggers. Beyond that, limit dairy products, eat small meals, stay hydrated, try to avoid caffeine and alcohol and carbonation. If you're concerned about weight loss or if your diet has become too limited, talk to a registered dietitian. It's important to take care of your mental health, too. Find ways to manage stress, like exercise, breathing and relaxation techniques or biofeedback. Some symptoms like abdominal pain, gas, and diarrhea can cause anxiety and frustration. That can make it difficult to be out in public for any amount of time. It can feel limiting and isolating and lead to depression. So learn as much as you can about ulcerative colitis. Staying informed can help a lot in feeling like you're in control of your condition. Talk to a therapist, especially one familiar with inflammatory bowel disease. Your doctor should be able to give you some recommendations. And you might want to find a support group for people going through the same thing that you are. Ulcerative colitis is a complex disease, but having expert medical care and developing a treatment strategy can make it more manageable and even help patients get back to the freedom of a normal life. Meanwhile, significant advances continue to be made in understanding and treating the disease and getting us closer to curing it or preventing it entirely. If you'd like to learn even more about ulcerative colitis, watch our other related videos or visit mayoclinic.org. We wish you well.
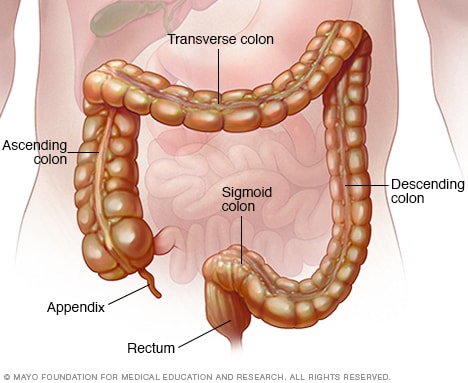
Colon and rectum
The colon is a long tube-like organ in the abdomen. It's the largest part of the large intestine. The colon carries waste to be expelled from the body. The rectum makes up the last several inches of the colon.
Gastroenterology & GI Surgery Blog
Ulcerative colitis (UL-sur-uh-tiv koe-LIE-tis) is an inflammatory bowel disease (IBD) that causes inflammation and ulcers (sores) in your digestive tract. Ulcerative colitis affects the innermost lining of your large intestine, also called the colon, and rectum. In most people, symptoms usually develop over time, rather than suddenly.
Ulcerative colitis can be draining and can sometimes lead to life-threatening complications. While it has no known cure, there are several new treatments that can greatly reduce signs and symptoms of the disease and bring about long-term remission.
Products & Services
- A Book: Mayo Clinic on Crohn’s Disease and Ulcerative Colitis
- A Book: Mayo Clinic on Digestive Health
- Available Digestive Health Products at Mayo Clinic Store
Ulcerative colitis symptoms can vary, depending on the severity of inflammation and where it occurs. Signs and symptoms may include:
- Diarrhea, often with blood or pus
- Rectal bleeding — passing small amount of blood with stool
- Abdominal pain and cramping
- Rectal pain
- Urgency to defecate
- Inability to defecate despite urgency
- Weight loss
- In children, failure to grow
Most people with ulcerative colitis have mild to moderate symptoms. The course of ulcerative colitis may vary, with some people having long periods when it goes away. This is called remission.
Health care providers often classify ulcerative colitis according to its location. Symptoms of each type often overlap. Types of ulcerative colitis include:
- Ulcerative proctitis. Inflammation is confined to the area closest to the anus, also called the rectum. Rectal bleeding may be the only sign of the disease.
- Proctosigmoiditis. Inflammation involves the rectum and sigmoid colon — the lower end of the colon. Symptoms include bloody diarrhea, abdominal cramps and pain, and an inability to move the bowels despite the urge to do so. This is called tenesmus.
- Left-sided colitis. Inflammation extends from the rectum up through the sigmoid and descending portions of the colon. Symptoms include bloody diarrhea, abdominal cramping and pain on the left side, and urgency to defecate.
- Pancolitis. This type often affects the entire colon and causes bouts of bloody diarrhea that may be severe, abdominal cramps and pain, fatigue, and significant weight loss.
When to see a doctor
See your health care provider if you experience a persistent change in your bowel habits or if you have signs and symptoms such as:
- Abdominal pain
- Blood in your stool
- Ongoing diarrhea that doesn't respond to nonprescription medications
- Diarrhea that awakens you from sleep
- An unexplained fever lasting more than a day or two
Although ulcerative colitis usually isn't fatal, it's a serious disease. In some cases, ulcerative colitis may cause life-threatening complications.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
Get the latest health information from Mayo Clinic delivered to your inbox.
Subscribe for free and receive your in-depth guide to digestive health, plus the latest on health innovations and news. You can unsubscribe at any time. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing
Your in-depth digestive health guide will be in your inbox shortly. You will also receive emails from Mayo Clinic on the latest health news, research, and care.
If you don’t receive our email within 5 minutes, check your SPAM folder, then contact us at [email protected] .
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
The exact cause of ulcerative colitis remains unknown. Previously, diet and stress were suspected. However, researchers now know that these factors may aggravate but don't cause ulcerative colitis.
One possible cause is an immune system malfunction. When your immune system tries to fight off an invading virus or bacterium, an irregular immune response causes the immune system to attack the cells in the digestive tract, too.
Heredity also seems to play a role in that ulcerative colitis is more common in people who have family members with the disease. However, most people with ulcerative colitis don't have this family history.
Risk factors
Ulcerative colitis affects about the same number of women and men. Risk factors may include:
- Age. Ulcerative colitis usually begins before the age of 30, but it can occur at any age. Some people may not develop the disease until after age 60.
- Race or ethnicity. Although white people have the highest risk of the disease, it can occur in any race. If you're of Ashkenazi Jewish descent, your risk is even higher.
- Family history. You're at higher risk if you have a close relative, such as a parent, sibling or child, with the disease.
Complications
Possible complications of ulcerative colitis include:
- Severe bleeding
- Severe dehydration
- A rapidly swelling colon, also called a toxic megacolon
- A hole in the colon, also called a perforated colon
- Increased risk of blood clots in veins and arteries
- Inflammation of the skin, joints and eyes
- An increased risk of colon cancer
- Bone loss, also called osteoporosis
Ulcerative colitis care at Mayo Clinic
- Feldman M, et al, eds. Epidemiology, pathogenesis, and diagnosis of inflammatory bowel diseases. In: Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. 11th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed July 22, 2020.
- Goldman L, et al., eds. Inflammatory bowel disease. In: Goldman-Cecil Medicine. 26th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed July 22, 2020.
- The facts about inflammatory bowel diseases. Crohn's and Colitis Foundation. https://www.crohnscolitisfoundation.org/. Accessed Sept. 6, 2022.
- Ulcerative colitis. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/ulcerative-colitis. Accessed Sept. 6, 2022.
- What is ulcerative colitis? Crohn's and Colitis Foundation. https://www.crohnscolitisfoundation.org/what-is-ulcerative-colitis. Accessed Sept. 6, 2022.
- Kliegman RM, et al. Inflammatory bowel diseases. In: Nelson Textbook of Pediatrics. 21st ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed July 22, 2020.
- AskMayoExpert. Chronic ulcerative colitis. Mayo Clinic; 2019.
- Abraham B, et al. Antibiotics and probiotics in inflammatory bowel disease: When to use them? Frontline Gastroenterology. 2020; doi:10.1136/flgastro-2018-101057.
- What should I eat? Crohn's and Colitis Foundation. https://www.crohnscolitisfoundation.org/diet-and-nutrition/what-should-i-eat. Accessed Sept. 6, 2022.
- Mind-body therapies. Crohn's and Colitis Foundation. https://www.crohnscolitisfoundation.org/complementary-medicine/mind-body-therapies. Accessed Sept. 6, 2022.
- Nguyen H. Allscripts EPSi. Mayo Clinic. April 1, 2022.
- Special IBD diets. Crohn's and Colitis Foundation. https://www.crohnscolitisfoundation.org/diet-and-nutrition/special-ibd-diets. Accessed Sept. 6, 2022.
- Shergill A, et al. Surveillance and management of dysplasia in patients with inflammatory bowel disease. https://www.uptodate.com/contents/search. Accessed Sept. 6, 2022.
- Kashyap PC (expert opinion). Mayo Clinic. Aug. 13, 2020.
- Kane SV (expert opinion). Mayo Clinic. Sept. 12, 2020.
- Xeljanz, Xeljanz XR (tofacitinib): Drug safety communication — Initial safety trial results find increased risk of serious heart-related problems and cancer with arthritis and ulcerative colitis medicine. U.S. Food and Drug Administration. https://www.fda.gov/safety/medical-product-safety-information/xeljanz-xeljanz-xr-tofacitinib-drug-safety-communication-initial-safety-trial-results-find-increased?utm_medium=email&utm_source=govdelivery. Accessed Sept. 6, 2022.
- Khanna S (expert opinion). Mayo Clinic. Aug. 20, 2022.
- Cohen RD, et al. Management of moderate to severe ulcerative colitis in adults. https://www.uptodate.com/contents/search. Accessed Aug. 1, 2022.
- Ulcerative colitis flare-ups: 5 tips to manage them
Associated Procedures
- Acupuncture
- Barium enema
- Colonoscopy
- Flexible sigmoidoscopy
- Ileoanal anastomosis (J-pouch) surgery
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Ulcerative colitis.
Whitney D. Lynch ; Ronald Hsu .
Affiliations
Last Update: June 5, 2023 .
- Continuing Education Activity
Ulcerative colitis is an idiopathic inflammatory condition of the colon that results in diffuse friability and superficial erosions on the colonic wall and associated bleeding. It is the most common form of inflammatory bowel disease worldwide. Characteristically, it involves inflammation restricted to the mucosa and submucosa of the colon. Typically, the disease starts in the rectum and extends proximally in a continuous manner. In the United States, the disease accounts for a quarter-million provider visits annually. This activity reviews the evaluation and management of ulcerative colitis and highlights the role of the interprofessional team in evaluating and improving care for patients with this condition.
- Explain the history and physical examination of patients with ulcerative colitis.
- Outline evaluation of patients with ulcerative colitis.
- Describe treatment considerations for patients with ulcerative colitis.
- Identify interprofessional team strategies for improving care coordination and outcomes in patients with ulcerative colitis.
- Introduction
Ulcerative colitis is an idiopathic inflammatory condition of the colon that results in diffuse friability and superficial erosions on the colonic wall associated with bleeding. It is the most common form of inflammatory bowel disease worldwide. It characteristically involves inflammation restricted to the mucosa and submucosa of the colon. Typically, the disease starts in the rectum and extends proximally in a continuous manner. In the United States, the disease accounts for a quarter-million provider visits annually, and medical costs directly related to the disease are estimated to exceed four billion dollars annually. [1] [2] [3] Ulcerative has no cure and is a lifelong disorder with a significant impact on both physical and mental health.
The specific cause of inflammatory bowel disease is not known. There seems to be a primary genetic component since the most important independent risk factor is a family history of the disease (8% to 14% of patients). A first-degree relative of a patient with ulcerative colitis has a four times higher risk of developing the disease. Additionally, ulcerative colitis has a higher incidence in Jewish populations than other ethnicities.
Although there is little evidence to support this, it has been postulated that alterations in the composition of the gut microbiota and defects in mucosal immunity could lead to ulcerative colitis. Autoimmunity may also play an important role in the etiology of ulcerative colitis. [4] [5]
Some evidence suggests that smoking may be protective, but so far, no one has been able to confirm a direct relationship between the two.
- Epidemiology
Worldwide, the highest incidence and prevalence of inflammatory bowel diseases are seen in Northern Europe and North America. Inflammatory bowel disease is closely linked to a Westernized environment and lifestyle. Ulcerative colitis has an incidence of 9 to 20 cases per 100,000 persons per year. Its prevalence is 156 to 291 cases per 100,000 persons per year. Compared to Crohn disease, ulcerative colitis has a greater prevalence in adults. When considering the pediatric population, however, ulcerative colitis is less prevalent than Crohn disease.
Ulcerative colitis has a bimodal pattern of incidence. The main onset peaks between the age of 15 and 30 years. A second, and the smaller peak of incidence occurs between the age of 50 and 70 years. Though some studies show a slight predilection for men, most studies note no preference regarding sex. There is an increased prevalence of ulcerative colitis in nonsmokers or those who recently quit smoking. Additionally, smokers diagnosed with ulcerative colitis tend to have milder disease, fewer hospitalizations and need for less medication. There is evidence, though weak, that non-steroidal anti-inflammatory drug use is associated with the onset or relapse of ulcerative colitis.
There is also an association of inflammatory bowel disease with the removal of an inflamed appendix. Appendectomy before the age of twenty is associated with a decreased incidence of ulcerative colitis, whereas the opposite is true for Crohn disease. In fact, appendectomy has been shown to reduce the risk of developing ulcerative colitis by 69%. [6] [7]
- Pathophysiology
The pathophysiology of ulcerative colitis involves defects in the epithelial barrier, immune response, leukocyte recruitment, and microflora of the colon. [8] [9]
The epithelial barrier has a defect in colonic mucin and possibly tight junctions, leading to increased uptake of luminal antigens. The lamina propria of the mucosa also has an increased number of activated and mature dendritic cells, which include a large number of toll-like receptors (TLR), specifically TLR2 and TLR4. There also seems to be an atypical T-helper (Th) cell response in patients with ulcerative colitis, specifically Th2, which exerts a cytotoxic response against epithelial cells. Other immune-related factors that play a role in the pathophysiology of ulcerative colitis include tumor necrosis factor-alpha (TNF-alpha), interleukin 13, and natural killer T-cells. Levels of IgM, IgA, and IgG are elevated in inflammatory bowel disease; however, a disproportionate increase in IgG1 antibodies is found in patients diagnosed with ulcerative colitis.
Leukocyte recruitment is affected on two fronts. There is an upregulated release of the chemoattractant CXCL8 in ulcerative colitis so that leukocytes are recruited to the mucosa from systemic circulation. Additionally, there is an upregulation of mucosal cellular adhesion molecule-1 (Mad-CAM1) on the endothelium of mucosal blood vessels, which promotes leukocyte adhesion and extravasation into mucosal tissue.
Studies have shown that enteric microflora is important in the pathogenesis and severity of inflammation and disease phenotype. Ulcerative colitis seems also to result, in part, from a homeostatic imbalance between enteric microflora and the host's mucosal immunity. This results in an aberrant response to non-pathogenic bacteria.
- Histopathology
Histologically, the mucosal layer of the colon in a patient with ulcerative colitis includes infiltrates of varying density and composition, depending on the stage of the disease. These infiltrates primarily consist of lymphocytes, plasma cells, and granulocytes, with the latter being more prominent during acute flares of the disease. Additionally, goblet cell depletion, ulcerations, and alterations in mucosal crypts are sometimes apparent. These findings might also be present on histological evaluation of the distal ileum, even though ulcerative colitis is a disease confined to the colon. This is backwash ileitis.
- History and Physical
The main symptom of ulcerative colitis is bloody diarrhea, with or without mucus. Associated symptoms also include urgency or tenesmus, abdominal pain, malaise, weight loss, and fever, depending on the extent and severity of the disease. The onset of the disease is typically gradual, and patients will likely experience periods of spontaneous remission and subsequent relapses. Factors that typically exacerbate ulcerative colitis include smoking cessation and nonsteroidal anti-inflammatory drug use.
There are some extraintestinal manifestations (EIMs) that are also present in 10% to 30% of patients with ulcerative colitis. Extraintestinal manifestations associated with disease activity include episcleritis, scleritis, uveitis, peripheral arthropathies, erythema nodosum, and pyoderma gangrenosum. Extraintestinal manifestations independent of colitis activity include axial arthropathies, sacroiliitis, and ankylosing spondylitis. A significant hepatic extraintestinal manifestation of ulcerative colitis includes primary sclerosing cholangitis and is associated with a greater risk of colorectal cancer.
Diagnosis of ulcerative colitis is made clinically with supportive findings on endoscopy, biopsy, and by negative stool examination for infectious causes. Because colonic infection can produce clinical findings indistinguishable from idiopathic ulcerative colitis, microbiologic studies for bacterial infection and parasitic infestation should be included in the initial evaluation. [10] [11]
Radiologic examinations are not critical for the diagnosis but may be useful. Patients with longstanding ulcerative colitis may show a "stove-pipe" sign on double-contrast barium enema (DCBE).
Colonoscopy or proctosigmoidoscopy might reveal loss of typical vascular pattern, granularity, friability, and ulceration, which involve the distal rectum and proceed proximally in a symmetric, continuous, and circumferential pattern. The disease can range from isolated to the rectum and sigmoid colon (proctitis) to disease of the entire colon (pancolitis). Population-based studies show that, upon presentation, proctitis is found in 30% to 60% of patients, left-sided colitis is found in 16% to 45%, and pancolitis is found in 14% to 35%.
Laboratory evaluation will usually reveal an increase in inflammatory factors (ESR, CRP, leukocytosis), especially during an acute flare. Regardless of disease stage, 60% to 70% of ulcerative colitis patients are positive for perinuclear antineutrophil cytoplasmic antibodies (P-ANCA). P-ANCA is also found in a small number of patients with Crohn disease. In addition to P-ANCA, anti-saccharomyces cerevisiae antibodies (ASCA) are found in both Crohn disease and ulcerative colitis but are more prevalent in Crohn disease; therefore, testing for both P-ANCA and ASCA has some utility in distinguishing types. Testing for carcinoembryonic antigen (CEA) can also be helpful in ulcerative colitis, as higher levels can indicate a flare.
Testing for fecal calprotectin also has some utility in the diagnosis of ulcerative colitis, though it is nonspecific. Fecal calprotectin correlates with increased neutrophils in the intestine and, therefore, can be helpful in ruling out inflammatory bowel disease. Studies show that less than 1% of patients with low fecal calprotectin are likely to suffer from inflammatory bowel disease.
An endoscopy (colonoscopy) must be done at some point which will reveal:
- Fragile mucosa
- Granular mucosa
- Loss of vascular pattern
- Presence of erosions and pseudopolyposis
Multiple biopsies should be obtained to confirm the diagnosis.
When a diagnosis of ulcerative colitis is made, the most common classification system used to determine the extent and severity of the disease is the Montreal classification system. Extent (E) is determined by endoscopic evaluation and includes E1 (Proctitis), E2 (left-sided or distal colitis), and E3 (pancolitis). Symptoms and systemic findings determine severity (S). It ranges from S0 (remission) to S3 (severe).
- Treatment / Management
Treatment choice for patients with ulcerative colitis is based on both the extent of the disease and the severity. The prognosis during the first decade after diagnosis is often generally good, and most patients go into remission. Rectal application of medical therapy, via suppository or enema, is usually appropriate for isolated distal disease (proctitis); however, a rectal application is usually used in combination with systemic therapy to help target the distal colon and, therefore, decrease tenesmus. [6] [12] [13]
First-line treatment is sulfasalazine and 5-aminosalicylates, given orally or rectally, which have a remission rate of about 50%. Glucocorticoids, orally or rectally, can be added for those who fail to achieve remission within two weeks. Except for glucocorticoids, all of these medications can be used in the maintenance of remission. Additionally, there is some evidence that probiotics are helpful in attaining remission. Fecal microbiota transplantation also shows promise in the treatment of ulcerative colitis to help establish healthy gut microbiota.
If patients are refractory to glucocorticoids, thiopurines or biological drugs can be added to therapy. Thiopurines are immunosuppressants such as azathioprine or 6-mercaptopurine. Biological drugs include anti-TNF-alpha drugs, such as infliximab, adalimumab, and golimumab. Infliximab is the most widely used for ulcerative colitis and can be used in severe cases during hospital admissions. The newest class of biological drugs are anti-adhesion molecule inhibitors, such as vedolizumab, which blocks alpha-4-beta-7 integrin.
Since patients with ulcerative colitis have reduced expression of peroxisome proliferator-activated receptor-gamma (PPAR-gamma) in their colonocytes, future treatment may include (PPAR-gamma) agonistic activity. PPAR-gamma is a negative regulator of NF-KB-dependent inflammation. Novel 5-aminosalicylic acid (5-ASA) analogs are being developed that have greater PPAR-gamma activity. Cardiotoxicity and metabolic toxicity restrict the use of existing PPAR-gamma agonists.
Colectomy is curative in patients with ulcerative colitis since the disease is restricted to the colon. Indications for surgery are a failure of medical therapy, intractable fulminant colitis, toxic megacolon, perforation, uncontrollable bleeding, intolerable side effects of medications, strictures, unresectable high-grade or multifocal dysplasia, cancer, or growth retardation in children. The procedure of choice is proctocolectomy with ileal pouch-anal anastomosis (IPAA); however, in patients who are ineligible for IPAA, proctocolectomy with ileostomy is a viable alternative.
Because of the risk of colon cancer, colonoscopy is recommended at regular intervals.
All patients need maintenance therapy to prevent relapse. Oral aminosalicylates are the drugs of choice, but others may respond to azathioprine and 6-mercaptopurine.
There is no specific diet for patients with ulcerative colitis, but many develop lactose intolerance. Unlike Crohn disease, there is no role for elemental or parenteral nutrition.
- Differential Diagnosis
In patients presenting with lower abdominal pain and bloody diarrhea, the following differentials should be considered:
- Crohn disease
- Parasitic colitis
- Tuberculosis
- Radiation colitis
- Colon cancer
- Toxic megacolon
- Bacterial/viral gastroenteritis
The severity of ulcerative colitis is graded from mild to severe depending upon rectal bleeding:
- Mild: Fewer than four rectal bleeding episodes per day
- Moderate: More than four rectal bleeding episodes per day
- Severe: More than four rectal bleeding episodes per day, and the patient has systemic features of an illness combined with hypoalbuminemia
Ulcerative colitis is a lifelong illness, but the overall mortality is not greater than in the general population. However, mortality is increased in patients who develop shock and surgical complications. When the muscularis propria is involved, it may damage the nerves resulting in dilatation, aperistalsis, and ischemia (toxic megacolon). Today, toxic megacolon is the most common cause of death in ulcerative colitis. At least 5% of patients develop colon cancer, and this risk increases with the duration of the disease. Unlike Crohn disease, stricture formation is rare.
- Complications
Ulcerative colitis is a lifelong disease with periods of remission and relapse. Following complications can occur in patients suffering from ulcerative colitis:
- Leak from anastomosis
- Pelvic abscess
- Enterocutaneous fistulas
- Pouch prolapse,
- Pouchitis, acute is less than 4 weeks, chronic is more than 4 weeks
- Incontinence
- Sexual dysfunction
- Toxic megacolon
- Colon/rectal cancer
- Deterrence and Patient Education
American College of Gastroenterology has made guidelines on preventive care in patients with ulcerative colitis. These recommendations include:
- Screening for skin malignancies, irrespective of the use of biological agents
- Assessing bone mineral density
- Be vaccinated against Herpes zoster
- Vaccinated against Pneumococcus, H. influenzae , and the flu virus
- Should not travel to areas of yellow fever without first consulting with an infectious disease expert
- Be screened for depression and anxiety
- Women with ulcerative colitis should get annual cervical cancer screening
- Pearls and Other Issues
There is an increased risk of colorectal cancer in patients with ulcerative colitis. The risk is cumulative, with a 2% chance of colorectal cancer after ten years of diagnosis, 8% after 20 years, and 20% to 30% after 30 years. Two factors associated with increased risk of colorectal cancer are the duration and extent of the disease.
- Enhancing Healthcare Team Outcomes
Ulcerative colitis is a systemic disorder with no cure. The disorder has numerous extraintestinal involvement in addition to the colon. Thus, it is best managed by an interprofessional team. All patients with the disorder need lifelong monitoring. Because of the risk of colorectal cancer, surveillance colonoscopy should occur every 1-2 years. Further, since patients are often treated with biological agents, they need to undergo screening for melanoma and nonmelanoma skin cancer.
The pharmacists should assist the team by educating the patient on the importance of medication compliance to avoid relapse. The nurse should encourage regular vaccinations, hand washing, and cancer screening. A dietary consult should be obtained to educate the patient on foods to eat and what not to eat, especially if they have a stoma. In addition, a stoma nurse should be involved in the teaching of stoma care.
An infectious disease nurse should monitor the patient in the outpatient setting to ensure that they are not immunocompromised. Social workers should be involved to ensure that the patient has ample support and finances so that the treatments are not missed. Patients with risk factors for osteoporosis need screening for bone mineral density periodically. Patients should be encouraged to undergo annual vaccination against influenza and pneumococcus. Finally, many patients with ulcerative colitis develop depression and anxiety and should be referred to a mental health counselor. [14] [15]
Ulcerative colitis has no cure, and despite treatment, many continue to have increased bouts of stool frequency. An increase in mortality is usually seen in older patients, those with complications like infection, shock, and anemia, and those who require repeated surgical interventions. Data show that when the disease involves the muscularis propria, it can lead to bowel dysmotility, necrosis, and gangrene. A certain number of patients also develop toxic megacolon with poor outcomes. It is estimated that about 5% of patients will develop colorectal cancer over time. The risk of colon cancer is higher in patients with pancolitis and in patients whose disease started before the age of 15. Overall, the quality of life in patients with ulcerative colitis is poor. [16] [17] [Level 5]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Whitney Lynch declares no relevant financial relationships with ineligible companies.
Disclosure: Ronald Hsu declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Lynch WD, Hsu R. Ulcerative Colitis. [Updated 2023 Jun 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review A comprehensive review and update on ulcerative colitis(). [Dis Mon. 2019] Review A comprehensive review and update on ulcerative colitis(). Gajendran M, Loganathan P, Jimenez G, Catinella AP, Ng N, Umapathy C, Ziade N, Hashash JG. Dis Mon. 2019 Dec; 65(12):100851. Epub 2019 Mar 2.
- Myositis as an Extraintestinal Manifestation of Ulcerative Colitis: A Case Report and Literature Review. [Cureus. 2023] Myositis as an Extraintestinal Manifestation of Ulcerative Colitis: A Case Report and Literature Review. Nagi TK, Gheit Y, Hernandez OL, Suarez ZK, Vallejo C, Haider MA, Zahra T. Cureus. 2023 Jul; 15(7):e42336. Epub 2023 Jul 23.
- Review Ulcerative colitis. [Lancet. 2012] Review Ulcerative colitis. Ordás I, Eckmann L, Talamini M, Baumgart DC, Sandborn WJ. Lancet. 2012 Nov 3; 380(9853):1606-19. Epub 2012 Aug 20.
- Review Inflammatory disease of the colon: ulcerative colitis and Crohn's colitis. [J Pediatr. 1975] Review Inflammatory disease of the colon: ulcerative colitis and Crohn's colitis. Ament ME. J Pediatr. 1975 Mar; 86(3):322-34.
- The Impact of Inflammatory Bowel Disease in Canada 2018: Indirect Costs of IBD Care. [J Can Assoc Gastroenterol. 2019] The Impact of Inflammatory Bowel Disease in Canada 2018: Indirect Costs of IBD Care. Kuenzig ME, Lee L, El-Matary W, Weizman AV, Benchimol EI, Kaplan GG, Nguyen GC, Bernstein CN, Bitton A, Lee K, et al. J Can Assoc Gastroenterol. 2019 Feb; 2(Suppl 1):S34-S41. Epub 2018 Nov 2.
Recent Activity
- Ulcerative Colitis - StatPearls Ulcerative Colitis - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
"Mirikizumab is the first antibody targeting p19/interleukin-23 to be approved for the treatment of ulcerative colitis. Its performance in both induction and maintenance phases of the clinical trials is truly impressive," said Bruce Sands, MD, MS, senior author of the clinical trial study published in The New England Journal of Medicine (NEJM). Dr.
AltruBio raises $225 million to develop ulcerative colitis drug and other immune checkpoint enhancers. By Jonathan Wosen May 21, 2024. ... At a flashy new research hub, AstraZeneca lays out…
Together, Dr. Wang said, these findings suggest that the combination injections could be a viable new way of treating ulcerative colitis. A similar approach may also be used to treat other autoimmune diseases. ... of more than 3,100 is responsible for groundbreaking medical advances and is committed to translating science-driven research ...
Ulcerative colitis is an inflammatory bowel disease that is characterized by chronic inflammation of the colon. ... Important studies published in 2023 outlined new agents and strategies for the ...
May 27, 2021. LA JOLLA, CA— Ozanimod, the drug invented at Scripps Research that won FDA approval last year for relapsing forms of multiple sclerosis, has been approved in the United States for a second high-need medical condition, ulcerative colitis. The once-daily oral drug, sold by Bristol Myers Squibb under the name Zeposia, can now be ...
A new aspect of the LUCENT trial program was the inclusion of end points relating to bowel urgency. 21,22 Many patients with ulcerative colitis consider control of bowel movements to be more ...
The U.S. Food and Drug Administration (FDA) approved mirikizumab, on October 26, 2023, a highly effective new treatment for ulcerative colitis (UC), offering a new option to patients battling this ...
Ulcerative colitis (UC) is a chronic inflammatory bowel disease of unknown aetiology affecting the colon and rectum. ... Thus, narrowing the gaps between basic, clinical and translational research ...
Ulcerative colitis is a lifelong inflammatory disease affecting the rectum and colon to a variable extent. In 2023, the prevalence of ulcerative colitis was estimated to be 5 million cases around the world, and the incidence is increasing worldwide. Ulcerative colitis is thought to occur in people with a genetic predisposition following ...
A new study shows that a sustainable faecal microbiota transplantation (FMT) treatment protocol, including anaerobic sample preparation, induces remission of active ulcerative colitis.
AltruBio, after tweaking checkpoint drug, raises $225M for midphase ulcerative colitis program. AltruBio put ALTB-268 through a phase 1 study in healthy volunteers in 2023. (Nuthawut Somsuk/iStock ...
Ulcerative colitis is a lifelong inflammatory disease affecting the rectum and colon to a variable extent. In 2023, the prevalence of ulcerative colitis was estimated to be 5 million cases around the world, and the incidence is increasing worldwide. Ulcerative colitis is thought to occur in people with a genetic predisposition following environmental exposures; gut epithelial barrier defects ...
Scientists are developing new treatments for ulcerative colitis (UC). There is ongoing scientific research into stem cell therapy for UC. Despite such developments, it remains an incurable condition.
San Francisco-based biotech AltruBio has raised $225 million in an oversubscribed Series B round, the company announced Tuesday. The financing will help the company advance its ulcerative colitis candidate into mid-stage clinical trials. AltruBio's candidate ALTB-268 is a first-in-class immune checkpoint enhancer (ICE) PSGL agonist antibody ...
Biotechnology startup AltruBio on Tuesday raised a Series B round that could hand it up to $225 million, cashing in again on a decision four years ago to change its development strategy. Originally known as AbGenomics Holdings, the startup had aimed to develop cancer drugs. But in 2020, it shifted course, swapped out its leadership and ...
Image Credit: josefkubes / Shutterstock. Johnson and Johnson (J&J) has announced positive data from the Phase III QUASAR maintenance trial for Tremfya (guselkumab) as a maintenance therapy in patients with moderate to severe active ulcerative colitis. Tremfya is an interleukin (IL)-23 and CD64-inhibiting monoclonal antibody.
In the past decade or so, the number of medications approved to treat ulcerative colitis (UC) has increased. But because the drugs haven't been around long, we don't have many details about the people taking them, how people respond to treatments in the real world, or how newer therapies compare with older ones. Clinical trial data is limited, and it doesn't really capture the impact of ...
Introduction. Ulcerative colitis (UC) was first described in mid-1800s.1 It is an idiopathic, chronic inflammatory disorder of the colonic mucosa that commonly involves the rectum and may extend in a proximal and continuous fashion to involve other parts of the colon.2 The disease typically affects individuals in the second or third decade of life with hallmark clinical symptoms of bloody ...
Ulcerative colitis (UC) is a chronic inflammatory disorder defined by mucosal inflammation that involves the colon and rectum in a continuous pattern [ 1, 2, 3 ]. The peak age of onset is 30-40 years old, and men and women are affected equally [ 4 ]. While still not yet fully defined, the pathogenesis of UC is multifactorial and implicates ...
Introduction. The Inflammatory Bowel Diseases (IBDs), namely Ulcerative Colitis (UC) and Crohn's disease (CD) ( Table 1), are chronic immune-mediated conditions with a high prevalence in developed countries (>0.3%) and rapidly increasing incidence in newly industrialised countries (annual percentage change +14.9%) 1, 2.Global prevalence is projected to affect up to 30 million individuals by ...
The new study began with a clinical observation. "Patients with a rare genetic condition called familial adenomatous polyposis, or FAP, are at extremely high risk for colon cancer," Habtezion said. "To prevent this, they undergo the exact same surgical procedure patients with refractory ulcerative colitis do."
The Stanford research team has an ongoing clinical trial to learn whether taking SBA supplements can reduce inflammation after surgery in people with ulcerative colitis. The estimated primary ...
Abstract. Ulcerative colitis (UC) is a chronic idiopathic inflammatory bowel disorder of the colon that causes continuous mucosal inflammation extending from the rectum to the more proximal colon, with variable extents. UC is characterized by a relapsing and remitting course. UC was first described by Samuel Wilks in 1859 and it is more common ...
We analyzed 41 subjects with ulcerative colitis [20 women; Mayo endoscopic subscore 0 in 38 (92.7%) and 1 in 3 (7.3%)]. Paired segment-by-segment comparison of magnetic resonance findings in colonic segments documented of being affected by ulcerative colitis versus controls showed subjects with ulcerative colitis had decreased cross-sectional area (p≤0.0034) and perimeter (p≤0.0005), and ...
When inflammatory bowel disease is identified in a new population, ulcerative colitis invariably precedes Crohn's disease and has a higher incidence. ... Lerner Research Institute, Department of ...
Ulcerative colitis (UC) is increasingly common, and it is gradually become a kind of global epidemic. UC is a type of inflammatory bowel disease (IBD), and it is a lifetime recurrent disease. UC as a common disease has become a financial burden for many people and has the potential to develop into cancer if not prevented or treated. There are multiple factors such as genetic factors, host ...
Ulcerative colitis is a complex disease, but having expert medical care and developing a treatment strategy can make it more manageable and even help patients get back to the freedom of a normal life. ... You will also receive emails from Mayo Clinic on the latest health news, research, and care. If you don't receive our email within 5 ...
In a retroactive, 24-month study, researchers compared key drivers of medical costs in a SonarMD engaged population of 495 patients with IBD from three New Jersey-based medical practices against a ...
Ulcerative colitis is an idiopathic inflammatory condition of the colon that results in diffuse friability and superficial erosions on the colonic wall associated with bleeding. It is the most common form of inflammatory bowel disease worldwide. It characteristically involves inflammation restricted to the mucosa and submucosa of the colon. Typically, the disease starts in the rectum and ...
Ulcerative colitis is a relapsing and remitting condition, meaning symptoms can die down for long periods but then flare-up from time to time. These flare-ups can be sudden and severe. During a ...