An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health


The State of the Evidence about the Family and Community Nurse: A Systematic Review
Federica dellafiore.
1 Section of Hygiene, Experimental and Forensic Medicine, Department of Public Health, University of Pavia, 27100 Pavia, Italy; [email protected] (F.D.); [email protected] (C.A.)
Rosario Caruso
2 Health Professions Research and Development Unit, IRCCS Policlinico San Donato, 20097 Milan, Italy; [email protected] (R.C.); [email protected] (I.B.); [email protected] (G.C.); [email protected] (A.M.)
Michela Cossu
3 Rsa Attanasio, Rsa Limbiate, 20812 Milan, Italy; [email protected]
4 Nursing Degree Course, Section Istituti Clinici di Pavia e Vigevano S.p.A., University of Pavia, 27100 Pavia, Italy
5 Department of Biomedicine and Prevention, University of Rome “Tor Vergata”, 00173 Rome, Italy; [email protected]
Irene Baroni
Serena barello.
6 EngageMinds HUB, Consumer, Food and Health Engagement Research Center, Department of Psychology, Università Cattolica del Sacro Cuore, 20100 Milan, Italy; [email protected] (S.B.); [email protected] (M.A.)
Ida Vangone
7 Department of Oncology and Hematology-Oncology, IEO-European Institute of Oncology, 20100 Milan, Italy
Marta Acampora
Gianluca conte, arianna magon, alessandro stievano.
8 Centre of Excellence for Nursing Scholarship, OPI Rome, 00173 Rome, Italy; [email protected]
Cristina Arrigoni
Associated data.
Not applicable for the methodology of the study.
Introduction. The increase in chronic degenerative diseases poses many challenges to the efficacy and sustainability of healthcare systems, establishing the family and community nurse (FCN) who delivers primary care as a strategic role. FCNs, indeed, can embrace the complexity of the current healthcare demand, sustain the ageing of the population, and focus on illness prevention and health promotion, ensuring a continuous and coordinated integration between hospitals and primary care ser. The literature on FCNs is rich but diverse. This study aimed to critically summarise the literature about the FCN, providing an overall view of the recent evidence. Methods. A state-of-art systematic review was performed on PubMed, CINAHL, and Scopus, employing the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement and checklist to guide the search and reporting. Results. Five interpretative themes emerged from the 90 included articles: clinical practice, core competencies, outcomes, Organisational and educational models, and advanced training program. Conclusions. FCNs can make a major contribution to a population’s health, playing a key role in understanding and responding to patients’ needs. Even if the investment in prevention does not guarantee immediate required strategies and foresight on the part of decisionmakers, it is imperative to invest more political, institutional, and economic resources to support and ensure the FCNs’ competencies and their professional autonomy.
1. Introduction
Population ageing is a global phenomenon [ 1 ], which determines and shapes many societal changes worldwide (at the individual, relational, cultural, and organisational levels), posing novel clinical, psychosocial, and welfare challenges [ 2 ]. In Western countries, the elderly population (i.e., older patients, defined as age > 65 years) has swelled due to the increased life expectancy [ 3 ]. For example, in Italy, the average life expectancy reached its average age peak of 83.22 years in 2019 [ 3 ]. These data represent a great success, but at the same time, a significant societal issue when older citizens cannot survive at optimal levels of their state of health. It is clear, in fact, that after a certain age, people spend about one-third of their life in good health and then develop a chronic disease [ 4 ].
Consequently, a further challenge is determined by an increase in chronic conditions in the population, since due to the more rapid spread of diseases, the demand for treatment has increased [ 5 ]. Moreover, factors such as stressors, which have led the population to suffer from long-term diseases, have grown considerably [ 6 ]. Coping with chronic conditions means dealing with a patient’s long-term management and illness in his or her life context. Chronic patients cannot be hospitalised for a long time to manage their disease; however, they require connection to the health facility through an organisational bridge that fosters communication and exchanges among health professionals and care services [ 7 ].
The COVID-19 pandemic has contributed to a greater focus on this societal phenomenon, accelerating the need for an organisational revolution toward service models aimed at supporting the categories of people defined as vulnerable at home [ 8 ]. Furthermore, the growing expectations and attitudes of health and assistance service users have led to a greater number of health requests, the demand for a higher quality of services, and the skills necessary to deliver them [ 9 ]. Therefore, the health crisis triggered by the COVID-19 pandemic represents the manifestation of the crises of the last decades, which has already highlighted the imbalance between the growth in demand for care and the decline in economic resources [ 10 ].
In this context, the World Health Organisation (WHO) underlined the need to implement models centred on primary healthcare (PHC). The WHO defines PHC as an approach which, as close as possible to people’s everyday environment, ensures the highest level of health. PHC focuses on a community’s needs, from health promotion to disease recognition, from prevention to treatment, and, at least, palliative care [ 11 ]. For these reasons, a bridge between the community and the health system is vital [ 11 , 12 ]. Therefore, further promotion of home-based care is needed to enhance PHC, reduce the length of stay in acute hospitals and the physical burden of the healthcare professionals that staff them, and meet the demands of older people who prefer to remain in their own homes [ 13 ].
In this scenario, the family and community nurse (FCN) is recognised as the key actor for implementing these new models for healthcare delivery, improving PHC and embracing the complexity of the current healthcare demand as it is effectively integrated into a multidisciplinary team [ 14 ]. This role is distinct from the ‘community nurse’, who collaborates closely with other health workers and develops plans for promoting healthcare [ 15 ]. FCNs are able to address the needs of the family throughout the course of life, paying particular attention to the vulnerable groups in society [ 15 , 16 ]. Indeed, FCNs provide care based on evidence and best practice; they have the knowledge, skills, and competencies to tailor care to individual needs [ 17 , 18 , 19 , 20 ], especially for older individuals with chronic diseases. FCNs bolster the transition away from the hospital-centric to the home-centric model for care [ 21 ], improving the care continuity of the healthcare system [ 14 , 21 ]. Many authors have demonstrated that FCNs with advanced competencies and autonomy could improve and assure delivery of PHC [ 22 ], which is crucial for health promotion and disease prevention through screening services and vaccination programs, the adoption of health-related behaviours (e.g., exercise, dietary modification, smoking cessation), and adherence to medical recommendations for managing chronic diseases [ 23 ].
The literature about the FCN is very heterogeneous and diverse, and it has not yet been synthesised; accordingly, a critical summary of the state of the evidence about the FCN represents a current gap in the literature. The lack of an overall view of the evidence available about FCNs undermines identifying aspects that need further improvement or progression, especially in the organisation and implementation of FCN models. The nursing care management to the family and the community could draw support from a general point of view of evidence that highlights an analysis of its current strengths and weaknesses. In addition, the progress of research may falter if researchers fail to recognise the areas that require more empirical investigations to address gaps in knowledge related to the FCNs. Accordingly, this systematic review aimed to critically summarise the state of the evidence of the FCN, providing a big-picture view of the recent evidence.
2.1. Study Design
This systematic review was conducted following the criteria, design, and methods of the state-of-the-art reviews [ 24 , 25 ] to provide an overall view of recent evidence on FCNs. Specifically, state-of-the-art reviews focus on describing what is currently known for a given topic [ 22 ], examining a broad and heterogeneous body of available evidence on a specific topic, and using the rigorous methodology of systematic reviews [ 24 , 26 ]. Systematic reviews adopt a replicable, scientific, and transparent process that minimises bias through exhaustive literature searches of published and unpublished articles and provides an audit trail of the reviewers’ decisions, procedures, and conclusions [ 27 ].
For this study, two independent researchers (MC and SR) systematically sought, appraised, and synthesised research literature evidence between November 2021 and December 2021, adhering to guidelines on the conduct of a systematic review [ 24 , 25 ] and to the ‘Preferred Reporting Items for Systematic Reviews and Meta-Analyses’ (PRISMA) statement and PRISMA flowchart ( Figure 1 ) [ 28 ]. The diagram depicts the flow of information through the different phases of a systematic review, mapping out the number of records identified, included and excluded, and the reasons for exclusions [ 28 ]. The PRISMA 2020 statement provides a checklist to evaluate the introduction, method, results, and discussion section of a systematic review report, ensuring its rigour.

PRISMA 2020 flow diagram for new systematic reviews, including searches of databases, registers, and other sources.
However, the considerable heterogeneities of methods and aims of the included articles did not allow the researchers to perform a meta-analysis. The researchers used a three-stage approach to the interpretative synthesis of available evidence about FCNs, their competencies, and their practical knowledge. First, MC and SR performed free line-by-line coding of the results from the data extraction of the primary articles; then, the authors grouped these codes into representative units of their meanings. This allowed the generation of five descriptive themes. Finally, descriptive themes were discussed among the entire group of authors using an interactive approach and to critically interpret their meanings, generating our themes [ 29 ].
2.2. Literature Search Strategy
The systematic literature search strategy was conducted independently by two researchers (MC and SR) and performed in different phases, and a third researcher (FD) was involved in resolving any doubts or discussions. First, the databases PubMed/Medline, Scopus, and CINAHL were searched using ‘background queries’ to identify the broad literature, including the keywords ‘Community Nurse’ or ‘Family Nurse’ in the title or abstract. In addition, an open search was conducted on Google Scholar to ensure the inclusion of all available literature. After that, specific foreground queries were structured with keywords, Medical Subject Headings (MeSH) terms, and Boolean Operators, and guided by the following questions: ‘What is the current knowledge about FCNs?’; ‘What are FCNs’ specific skills and competencies?’; ‘In which countries and clinical areas are FCNs most developed?’; ‘What is the impact of FCNs’ competencies on patients, families, and communities’ health outcomes?’.
Accordingly, the concepts arising from the background search were operationalised into a framework-based search strategy based on the SPIDER approach for systematic searches (Sample, Phenomenon of Interest, Design, Evaluation, Research type), where: Sample = nurses; Phenomenon of Interest = family and community nursing (FCNs); Design = every study design; Evaluation = experiences, patient-related, nurse-related, and system-related outcomes; Research type = quantitative, qualitative, mixed-method, and ‘other’, such as commentaries. In our study, SPIDER was used instead of PICO (Population/problem, Intervention/exposure, Comparison, and Outcome) because, including different methodologies, PICO was not applicable [ 30 ].
The inclusion criteria for retrieving articles were: (a) a focus on FCNs (i.e., a nurse with specific competencies to address the needs of the family throughout the course of life and with particular attention to the vulnerable groups in society); (b) published from the year 2000 onward; (c) published in English, Italian, or Spanish; and (d) availability of the full text and abstract. Articles that focused on FCNs during the COVID-19 outbreak in paediatric clinical settings or with a low-quality appraisal were excluded. Specifically, the authors decided to exclude articles focused on paediatric FCNs because such nurses have different and more specific competencies, and articles on FCNs during the COVID-19 outbreak described a particular period that could introduce bias into our state-of-the-art revision. Finally, to identify additional articles, backward and forward citation tracking was also carried out by examining the reference lists (citation chasing) of included articles.
Figure 1 shows the flowchart of search strategy: 3098 records were retrieved in the identification phase, and 2858 were removed after screening for duplicates. Accordingly, 235 articles were screened by evaluating the titles and abstracts, 127 articles were removed because their content was not focused on FCNs, and 11 were not available. At the end of the screening phase, three articles were excluded for low-quality appraisals, and three of them were irrelevant for the topic. Then, 97 articles were retrieved in full text and assessed using the critical appraisal checklist ‘Joanna Briggs Institute Qualitative Assessment and Review Instrument’ (JBI-QARI) [ 31 ] and a critical appraisal tool [ 31 , 32 ]. After the quality appraisal, 12 articles were excluded as lower quality ( n = 3) or because their overall content was not focused on FCNs ( n = 9). Therefore, in the third phase (i.e., inclusion), 90 articles were included in our systematic review, 85 from the databases and 5 from other methods.
2.3. Quality Appraisal
The quality appraisal of the 97 eligible articles was performed adopting the JBI-QARI, acknowledging the high heterogeneity of methods [ 31 ]. The JBI-QARI appraisal allows the evaluation of the methodological quality of eligible articles having different methodologies. It assesses full-text articles, determining which should be excluded due to low quality. Specifically, the JBI-QARI assesses the risk of bias in the quantitative published research, which helps to emphasise the rigour of the research and level of transferability for qualitative evidence [ 32 ].
Two authors independently conducted the quality appraisal process (MC and SR), and the final appraisal grading was based on the overall score computed by summing only the items with a positive assessment. The grading was reported as high, medium, or low quality [ 32 ]. Any disagreements between the reviewers were resolved by consensus or referred to a third reviewer (FD). This phase excluded 12 articles as lower quality ( n = 3) or because their overall content was not focused on FCNs ( n = 9). The remaining 90 articles (85 from the databases and 5 from other methods) showed moderate or good quality [ 32 ], and therefore were included ( Figure 1 ).
2.4. Data Abstraction, Analysis, and Synthesis
Supplementary Table S1 synthesises the main characteristics of the 90 articles included by the previous review phases, showing first author and publication year, title, aim, study design, population, country, theme, and results. Then, according to Greenhalgh and colleagues’ recommendations, the articles’ text and results were descriptively synthesised using the thematic aggregation of the line-by-line coding, initially developing a meta-narrative descriptive theme [ 33 ].
Finally, the authors discussed the descriptive themes for interpreting the current knowledge and state of evidence about FCNs, including priorities for future investigation and research. At the end of this process, five descriptive themes emerged: (a) clinical practice, (b) core competencies, (c) outcomes, (d) organisational and educational models, and (e) advanced training program.
The state-of-the-art systematic review allowed the identification of 90 articles that, in line with the inclusion and exclusion criteria previously identified, focused on FCNs. Specifically, most of them were conducted in European countries, including 40 performed in the UK and 8 in Italy; other contexts included Australia (N = 6), North and South America (N = 6), and Asia (N = 6). We identified nine articles using a semi-experimental or experimental design. Eight adopted quantitative observational cross-sectional data, while 12 articles were conducted with a qualitative design and 5 with mixed-method designs. Finally, a project highlighted FCN formation [ 34 ], and numerous discussion papers [ 34 , 35 , 36 , 37 ], case reports [ 17 , 38 , 39 ], and case studies were included [ 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 ].
According to a meta-narrative approach [ 33 ], the results of the 90 included articles were analysed and synthesised into five main interpretative themes: (a) clinical practice, (b) core competencies, (c) outcomes, (d) organisational and educational models, and (e) advanced training program. The articles’ results created more than one theme. Even if there was a dominant theme emerging from each article, the results of many articles fell under multiple themes ( Table 1 ). Supplementary Table S1 shows the main aspects and synthesis of data extraction for each included article.
Aggregation between included studies and interpretative themes arising from the analysis.
- (a) Clinical practice
The theme ‘clinical practice’ emerged from 54 articles included in our state-of-the-art systematic review, describing the main clinical settings where FCN numbers have grown. The recent literature has shown that FCNs utilise their advanced skills and competencies in health promotion, focusing on primary, secondary, and tertiary prevention. To ensure a higher level of professional intervention in healthcare promotion, FCNs must collaborate and become a strategic bridge for linking the competencies of different health care providers, guiding them to answer the healthcare needs of patients, families and communities [ 48 , 49 , 50 , 51 ].
According to the WHO, PHC is a whole-of-society approach that addresses the majority of a person’s health needs throughout their lifetime, focusing on people rather than disease [ 52 ]. The literature shows that PHC is the main area where FCNs feel better represented in their key role. FCNs are mainly engaged in promoting oral care and stopping smoking [ 35 , 44 , 49 , 53 , 54 ], providing education for correct blood pressure measurements, and preventing cerebrovascular events [ 46 , 55 ]. Furthermore, the FCN’s engagement is directed to correct oral intake, especially in the elderly, to prevent diseases related to malnutrition and chronic diseases [ 14 , 53 , 54 ], such as cancer [ 56 ]; to reduce antibiotic resistance [ 45 ] through the FCN as prescriber [ 39 ]; and to reduce elderly abuse [ 57 ]. In addition, in the USA, FCNs are recognised as fundamental to advising women in breast augmentation, supporting them during the path through surgery, and providing appropriate counselling [ 58 ]. However, the PHC needs of the individuals, families, and communities are different from one country to another. For example, in Africa, patients and communities must be educated about tuberculosis infection [ 59 ], unlike in developed countries, which have eradicated the virus. In this regard, Roden and colleagues illustrated how geographical context has an impact on the FCN for promoting health, where the holistic view is different from a rural to an urban context [ 60 ]. Still, educational interventions through their clinical practice are the ones that better determine changes in behaviour [ 61 ].
FCNs have an important role in patients’ education to support secondary healthcare, especially for chronic diseases. FCNs provide care with advanced autonomy, responsibility, and expertise in the whole social setting, especially for supporting the timely recognition of chronic diseases and preventing their spread [ 14 , 62 , 63 ]. The literature affirms that the advanced competencies of FCNs equip them to better understand patients’ needs and know them holistically. For example, different articles have demonstrated a high-level control of FCNs over chronic diseases in communities in Israel [ 64 ].
In addition, FCNs provide tertiary health care, supporting patients, families, and communities in illness management in different clinical settings, such as vascular disease management [ 65 ], psoriasis and eczema [ 18 , 66 ], fibromyalgia [ 67 ], arthritis [ 68 , 69 ], and chronic pain [ 70 , 71 ]. Review results have demonstrated how FCNs face challenges in the entire community in tertiary health care, especially for particular and fragile categories [ 72 , 73 , 74 ]. Chronic diseases, especially diabetes mellitus and chronic heart failure, require a high level of clinical practice and competencies of FCNs [ 37 , 75 , 76 ] to care for complications of these illnesses in the elderly and in oncology patients [ 40 , 77 , 78 , 79 , 80 , 81 , 82 , 83 ]. In psychological and psychiatric diseases, FCNs ensure patient safety and protect their independence [ 43 ]. They ensure patients’ respect and dignity; therefore, communication skills have emerged to be a key characteristic of FCNs [ 84 , 85 ], covering a key role in palliative care [ 85 , 86 , 87 , 88 , 89 ], especially for supporting patients and their families in the end-of-life process.
- (b) Core competencies
The core competencies of FCNs are an important topic. At present, a heated debate surrounding FCN core competencies is active in the scientific community, accounting for 20 articles in the state-of-the-art review. According to the integrated model of nursing competence proposed by Caruso and colleagues (2016), nurse competence is an integrated model based on individual characteristics, composed of motivation, education, and the function or tasks that nurses have in the working organisation and focused on nursing-sensitive outcomes (NSOs), which influence nurses’ performances and clinical patients’ outcomes [ 90 ]. The literature review depicts FCNs’ core competencies, especially based on health education and health promotion, high communication and empathy skills, and advanced clinical knowledge [ 38 , 49 ].
Many authors have agreed on health education as the FCN competency to enhance and promote family and community health [ 17 , 44 , 49 , 91 , 92 , 93 , 94 , 95 , 96 ]. It is very important to involve the caregiver in the health education process [ 97 ]. FCNs must orient their activities toward self-care to achieve the greatest possible autonomy in the health of patients, improving their attitude and knowledge, and helping them develop the skills needed to achieve better control of themselves [ 97 ]. The success of health education depends on FCNs competencies in high communication and empathy skills [ 45 , 58 , 66 , 96 , 98 , 99 ]. FCNs must talk and listen to their patients without judgment, working hard to deliver impartial and individualised care with the utmost compassion and sensitivity [ 97 , 100 ]. FCNs need advanced clinical knowledge to manage, monitor, and evaluate health activities [ 95 , 96 ]; implement strategies that promote continuity and quality of care; evaluate the impact of care by defining process indicators and results; and have sufficient human and materials resources [ 101 ]. In addition, FCNs demonstrate competencies to collaborate and work in multidisciplinary teams. FCNS take the initiative and employ systems thinking to ensure the quality of nursing care [ 14 , 92 , 94 , 99 ], and achieve better outcomes by providing culturally appropriate and safe care [ 95 , 96 , 102 ]. Finally, FCNs must be well prepared and trained to provide care based on evidence and best practice [ 17 , 92 ].
- (c) Outcomes
Twenty-one articles, four of which were randomised controlled studies [ 20 , 61 , 74 , 76 , 103 ], emphasised the positive influence of FCNs on patient-, nurses-, and health system-related outcomes. Regarding patient-related outcomes, we found that the intervention or care delivered by FCNs significantly increased survival [ 42 , 76 , 103 ], improved quality of life and clinical outcomes [ 38 , 104 , 105 ], and reduced the re-hospitalisation rate [ 42 , 103 ]. Furthermore, Ippoliti and Falavigna demonstrated, through socioeconomic planning, how the FCN’s intervention can determine positive patient-related outcomes, such as those involving hip fractures [ 101 , 106 ]. In particular, educational intervention by FCNs allowed a better adherence to correctly measuring blood pressure to prevent cerebrovascular diseases [ 55 ]. Moreover, patients reported being very satisfied with the care provided by FCNs [ 61 ], as they felt their psychological and social needs were considered [ 20 ]. In fact, mental health is one major aspect of sustaining patients’ well-being, particularly in cancer patients [ 107 ], especially to reduce anxiety and stress [ 74 ].
FCNs have a new vision in the nursing profession, allowing positive nurse-related outcomes. In fact, FCNs reported a high level of work satisfaction, which is possible because of the continuity of extended holistic care [ 83 , 108 , 109 ], and patients’ and their families’ full involvement in the educational programs [ 82 , 85 , 110 ]. However, the quality of education provided by FCNs is related to the geographical context; for example, FCNs feel poorly educated and trained in mountain communities [ 60 ]. A higher patient education level by an FCNs’ training program was protective in terms of reducing the risk of using health services and consequently improving system-related outcomes [ 61 , 75 ]. Furthermore, the ‘teach-back’ method, consisting of educational interventions at home, allows reducing public health system interventions and costs [ 61 , 75 ]. The geographical context could impact the delivery of health promotion, specifically for the elderly, who have more difficulty using health services [ 101 ].
- (d) Organisational and educational models
The literature describes different organizational and educational FCNs models, illustrating how caring patients are placed at the centre of all implemented models. The hospital-at-home model was implemented in elderly care, allowing multidisciplinary and holistic care for patients at their homes [ 41 ]. The HADPIPE model was developed to better assist patients, based on a holistic nursing assessment involving psychological, social, and physical aspects [ 111 ]. The social aspect is mainly investigated in the family nursing model, which aims to involve the families and caregivers of patients for optimal care delivery [ 56 ]. A new FCN model, derived from the Dutch Buurtzorg model, was created to better sustain patients in their context, aiming to develop relationships between FCNs and local care services, and promote independence among patients [ 112 ]. Morin and colleagues developed the care management model for patients’ cardiac surgery post-intervention, following patients even after discharge from hospital in highly specialized areas [ 109 ]. In Italy, the CoNSENSo project developed model care, illuminating the necessary conditions for the continued provision of health services, and the crucial role of the FCNs to better support the daily activities of elders and their families [ 101 , 106 , 113 ]. To better understand the importance of FCNs sustaining patients and their families in the educational setting, the FN-AIM model created a map to help nursing students assess patients’ and their families’ knowledge of best practices for maintaining patient health or managing their specific conditions [ 113 , 114 ].
- (e) Advanced training program
An FCN is a clinical nurse specialist with a high ability to introduce depth and innovation in care and nursing through evidence-based clinical specialist knowledge, skills, and competencies, requiring specific and advanced training [ 34 , 84 , 115 , 116 ]. The articles in our analysis showed the importance of such training programs for FCNs, which are heterogeneous and different from one country to another. In Africa, for example, the nursing council and nursing faculty assured courses for the graduate level, and provided FCNs with the didactic and clinical knowledge, skills, and abilities required for successful FCN practice [ 117 ]. Their courses focused on expected learning outcomes, course content, teaching and learning activities, and assessment measures. A graduate course lasts 1 year in China, and allows registered nurses to specialise in family and community nursing [ 118 ]. In the USA and Spain, an FCN training program has been proposed during the bachelor’s degree [ 93 , 114 ], providing possibilities to broaden the students’ perspectives to different social groups [ 119 ]. In the UK, the development of the FCN competencies allows the nurse to become a prescriber through a 10-day training program following 6 months of experience in the field [ 39 ].
Only one article was found describing the training program of FCNs in Italy: a first-level master in a postgraduate course in ‘Family and Community Nursing’ allows nurses to also specialize in telemedicine, which is developing year after year [ 38 ]. The training program also trains FCNs in end-of-life care [ 38 ]. This could help preserve patients’ dignity, whose significance cannot be underestimated, and could enable FCNs to better care for patients and their families at home [ 47 ].
4. Discussion
To the best of our knowledge, this systematic review is the first to provide a synthesis of the current state of the evidence about FCNs. According to a meta-narrative approach [ 33 ], the results of 90 included articles were analysed and synthesised into five main interpretative themes: (a) clinical practice, (b) core competencies, (c) outcomes, (d) organisational and educational models, and (e) advanced training program. These new themes provide an overview of the synthesis on FCNs. Our review identifies current strengths and weaknesses that need further improvement, especially in the organisation or implementation of FCN models, which slows the progression of research.
FCNs are a valuable and strategic resource in many clinical and care settings. The implementation of FCNs continues to develop day by day, with diverse development concerning the context and healthcare needs of the population [ 19 , 64 ]. Accordingly, our state-of-the-art systematic review included 90 articles from which five interpretative themes emerged, underlining that FCNs can contribute to population health, play a key role in understanding and responding to patients’ needs, and positively influence patient-, nurse- and healthcare system-related outcomes. Finally, our results allowed us to draw important conclusions about where to concentrate future resources in the form of economic investments and organisational improvements. Above all, our results indicate necessary areas for future research, such as the organisation or implementation of FCN models.
Increasingly rich and irrefutable evidence recognises that promoting healthy lifestyles improves health outcomes even in the case of diagnosed diseases and palliative care, especially reducing recurrences of cancers [ 120 , 121 ]. Therefore, PHC—acknowledged as the cornerstone of a sustainable health system by the WHO [ 11 ]—presents a golden opportunity for deploying FCNs to apply their advanced competencies and health promotion activities. Considering that scaling PHC interventions across low- and middle-income countries could save 60 million lives and increase the average life expectancy by 3.7 years by 2030 [ 11 ], it is clear that FCNs could have a significant impact on the processes of improvement if economic, organisational, and political supports were implemented to allow FCNs to delivery care and utilise their competencies [ 122 ]. Moreover, our results show the strategic influence of FCNs’ activities on secondary and tertiary health prevention, further strengthening their strategic role in attaining efficient and sustainable healthcare systems. However, FCNs seem to not yet feel fully at ease with this new role and perspective, demonstrating greater mastery and consolidation in the hospital setting and in disease care [ 96 ].
In order to achieve the abovementioned objectives from the salutogenic perspective, FCNs must reach advanced competencies through advanced specialised training [ 123 ]. Moreover, organisational policies must accompany FCNs’ competencies and training to allow the birth and implementation of FCN models to provide quality care, responding to the peculiarities of context and the population’s health needs. Indeed, ‘core competencies’, ‘organisational and educational models’, and ‘advanced training program’ are three themes that emerged from our review. Even if they underline a very heterogeneous result [ 50 , 123 ], they comprise a very powerful triad whose optimal balance seems to benefit health outcomes tremendously. The last theme that emerged from our review describes the positive influence of FCNs on patient-, nurses-, and health system-related outcomes. The empirical evidence on this topic is growing, but it is currently fragmented, highlighting an area where further efforts must be made.
According to Longhini and colleagues [ 122 ], possible NSOs to the family and community nursing care, and the consequent creation of the Nursing Minimum Data Set (NMDS), have not yet been described. NSOs can be defined as changes in an individual’s state, behaviour, or perception that are measured in response to nursing interventions [ 124 ]. The information must be easily registered and systematised in datasets that present specific characteristics to highlight nurses’ contributions to NSOs, in particular, in clinical fields such as family and community settings. For example, the NMDS was created as a minimum set of information that presents standard definitions related to nursing that enable the analysis and comparison of nursing data across different populations, settings, geographic areas, and time [ 125 ]. NMDSs have been developed in many countries to determine resource allocation, stimulate research, and guide health policy decision-making [ 126 ]. Moreover, complex clinical fields such as family and community care—due to their intrinsic characteristics and burdens—could benefit from a system synthesising the tremendous amount of data from the NSOs in a structured dataset. Data-mining algorithms have the potential to discover meaningful pieces of information and tendencies in this vast net of data that could be transferred into direct knowledge in the clinical field [ 127 ].
4.1. Strengths, Limits, and Further Challenges
The research design used is the main strength of our study, as it allowed an overall of view on FCNs, depicting the state of evidence that could serve as a booster for designing in-depth future research [ 24 ]. However, the high methodological heterogeneity of the included articles, which were mainly performed in the UK, represents our study’s principal limit. Indeed, the practice of FCNs varies so significantly between countries that is it is hard to provide a unified, global definition of what an FCN is. This difficulty necessitates additional studies on FCNs in specific countries, solving the problem of high heterogeneity and providing much more detailed and in-depth information. Moreover, the search terms, including “community nurse” and “family nurse”, are not synonymous across countries/regions, and it may lead to a mix of advanced nurses and generalists having different competencies and different practice scopes. Therefore, a meta-analysis for testing the cumulative effects of implementing FCNs on specific outcomes is difficult to realise, and generalizing the results to other contexts requires caution.
4.2. Implications for Clinical Practice
As stated above, our review’s chosen design has allowed us to identify areas where it is necessary to concentrate future resources and experimental research to determine the FCN’s effectiveness on multilevel outcomes. The use of FCNs is progressing in patches; the study of the characteristics of a functional context for FCNs’ implementation could guide policies and organisations in areas where FCNs are not present. Furthermore, assessing the economic savings due to the FCNs’ competencies and skills after their implementation in a specific healthcare system would be very useful. Finally, the nurses’ digital skills are essential for future professional development; however, no study in our FCN review has investigated this aspect.
5. Conclusions
The FCN was introduced in 1998 by the WHO, aiming to extend the care of nurses from the individual to the family and community, and from hospital care to primary care services within each community. Many worldwide healthcare systems have undergone changes to implement and support the birth of this new paradigm of nursing care centred on health promotion and prevention. Increasing empirical evidence demonstrates that FCNs, delivering primary care, could embrace the complexity of the current healthcare demand, sustain the ageing population, and focus on illness prevention and health promotion, ensuring a continuous and coordinated integration between hospitals and primary care services. Thus, FCNs can contribute to population health, play a key role in understanding and responding to patients’ needs, and positively influence patient-, nurse-, and healthcare system-related outcomes. Even if investing in prevention does not guarantee immediate required strategies and foresight on the part of decisionmakers, it is imperative that major political, institutional, and economic investments further support and ensure FCNs’ competencies and their professional autonomy to ensure their efficacy and the sustainability of healthcare systems.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph19074382/s1 , Table S1. Synthesis of the main characteristics of 90 included articles.
Author Contributions
Conceptualization, M.C., I.B., C.A. and F.D.; methodology, F.D., R.C., I.B. and C.A.; data curation, S.R., G.C., M.A., A.M., I.B., M.C. and I.V.; writing—original draft preparation, M.C., I.V., I.B. and S.R.; writing—review and editing, S.R., S.B. and R.C.; visualization, A.S.; supervision, C.A., A.S. and S.B.; project administration, R.C. and F.D.; funding acquisition, C.A. All authors have read and agreed to the published version of the manuscript.
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Data availability statement, conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
📕 Studying HQ
Exploring community health nursing research topics: a comprehensive guide for nursing students, carla johnson.
- August 25, 2023
- Essay Topics and Ideas
Community health nursing is a dynamic and vital field within the nursing profession, focused on providing holistic care to populations within a defined community. This specialized branch of nursing goes beyond individual patient care, extending its reach to families, groups, and entire communities. This article will delve into community health nursing, explore its significance, and provide valuable resources for nursing students to engage in research, evidence-based practice (EBP) projects, capstone projects, research paper topics, research questions, and essay ideas.
What You'll Learn
Understanding Community Health Nursing: A Holistic Approach
Community health nursing emphasizes preventive care , health promotion, and disease prevention within a specific community. This holistic approach involves understanding the community’s unique needs, cultures, and challenges to provide targeted interventions that improve health outcomes. As nursing students, you will find this field to be a gateway to understanding the broader healthcare landscape and the interconnectedness of various factors that influence health.

PICOT Questions on Community Health Nursing
- P: Adult population in psychiatric care ; I: Implementation of daily RS questionnaire; C: Units without the daily survey; O: Reduction in utilization of restraint and seclusion; T: 6 months. Can the implementation of a daily RS (Restraint and Seclusion) questionnaire for adults in psychiatric care lead to a significant decrease in the utilization of restraint and seclusion within a period of 6 months?
- P: Pediatric population in school settings; I: Introduction of daily exercise regimen; C: Schools without daily exercise; O: Improvement in BMI and overall fitness; T: 1 academic year. Does introducing a daily exercise regimen in school settings for pediatric populations result in a noticeable improvement in BMI and overall fitness over the course of 1 academic year?
- P: Elderly population in assisted living facilities; I: Implementation of fall prevention program; C: Facilities without fall prevention program; O: Reduction in fall-related injuries; T: 1 year. Is there a significant reduction in fall-related injuries among the elderly residing in assisted living facilities after the implementation of a comprehensive fall prevention program within 1 year?
- P: Low-income pregnant women; I: Provision of prenatal education classes; C: Those without access to prenatal education; O: Increase in prenatal knowledge and healthier pregnancy outcomes; T: Throughout gestation. Can providing prenatal education classes to low-income pregnant women lead to increased prenatal knowledge and improved pregnancy outcomes when compared to those without access to such education?
- P: Diabetic population within the community; I: Establishment of a mobile diabetic clinic; C: No mobile clinic available; O: Enhanced diabetic management and reduced hospitalizations; T: 2 years. Does the establishment of a mobile diabetic clinic within the community lead to better diabetic management and a decrease in hospitalizations over a span of 2 years?
- P: Adolescent population in schools; I: Implementation of comprehensive sexual education; C: Schools with standard sexual education; O: Reduction in teen pregnancies and sexually transmitted infections (STIs); T: 3 years. Over a period of 3 years, does the implementation of comprehensive sexual education in schools result in a significant decrease in the rates of teen pregnancies and STIs among adolescents compared to schools with standard sexual education?
- P: Homeless population; I: Launch of mobile healthcare unit; C: No access to regular healthcare; O: Improvement in overall health status and decrease in emergency room visits; T: 1 year. Can the introduction of a mobile healthcare unit for the homeless population improve their overall health status and a noticeable reduction in emergency room visits within a year?
- P: Rural elderly population; I: Initiation of telehealth services ; C: Lack of telehealth services; O: Enhanced access to healthcare and better management of chronic conditions; T: 18 months. Does the introduction of telehealth services for the rural elderly population lead to increased access to healthcare services and improved management of chronic conditions over the course of 18 months?
- P: New mothers; I: Implementation of postpartum support groups; C: No postpartum support groups available; O: Reduction in postpartum depression rates and improved maternal well-being; T: 1 year. Can the implementation of postpartum support groups for new mothers lead to a significant reduction in postpartum depression rates and an overall improvement in maternal well-being within a year?
- P: LGBTQ+ youth; I: Creating safe spaces in schools; C: Absence of designated safe spaces; O: Decreased mental health challenges and higher academic achievement; T: Ongoing. Does creating safe spaces within schools for LGBTQ+ youth lead to a noticeable decrease in mental health challenges and a rise in academic achievement over an ongoing period?
Evidence-Based Practice Projects Ideas
- Evaluating the effectiveness of community-wide vaccination drives in reducing vaccine-preventable diseases.
- Assessing the impact of a smoke-free policy in public spaces on community members’ respiratory health.
- Investigating the outcomes of a nutrition education program in improving dietary habits among low-income families.
- Analyzing the effectiveness of a community-based mental health awareness campaign in reducing stigma and increasing help-seeking behavior.
- Exploring the outcomes of a diabetes management intervention using mobile health apps in urban communities.
- Studying the effects of a community gardening initiative on physical activity levels and nutrition awareness.
- Investigating the utilization and impact of telemedicine services in remote rural areas.
- Assessing the benefits of a community fitness program on cardiovascular health and overall well-being.
- Evaluating the effectiveness of a school-based anti-bullying campaign on students’ mental health.
- Analyzing the outcomes of a community-driven initiative to increase access to clean drinking water in underserved areas.
Nursing Capstone Project Ideas
- Developing a comprehensive disaster preparedness plan for a local community.
- Designing and implementing a culturally sensitive prenatal care program for immigrant populations.
- Creating a curriculum for training community health workers in identifying and addressing social determinants of health.
- Establishing a support network for caregivers of elderly individuals living at home.
- Designing a mental health first aid training program for community leaders and volunteers.
- Implementing a community-based program to promote physical activity among children with obesity.
- Creating a resource guide for LGBTQ+ youth to access healthcare services without discrimination.
- Developing a community-wide initiative to combat opioid misuse and overdose.
- Establishing a telehealth platform for remote health consultations in underserved regions.
- Designing a comprehensive sexual education curriculum for high schools to address varying cultural norms.
Nursing Research Paper Topics
- The impact of community health nursing interventions on reducing health disparities .
- Exploring the role of community health nurses in disaster response and recovery.
- Analyzing the effectiveness of school-based health clinics in improving student health outcomes.
- Investigating the barriers and facilitators of healthcare access in underserved rural communities.
- The role of community health nursing in promoting healthy aging and elderly care.
- Addressing mental health stigma through community-based interventions led by nurses.
- Analyzing the outcomes of community health education programs on reducing tobacco use .
- Exploring the relationship between community engagement and positive maternal-child health outcomes.
- The effectiveness of telehealth services in bridging healthcare gaps in remote areas.
- Investigating the impact of community health nursing in preventing and managing chronic diseases.
Community Health Nursing Research Questions
- How does the presence of community health nurses influence health outcomes in underserved urban neighborhoods?
- What are the key components of successful school-based vaccination programs , and how do they impact disease prevention?
- How do cultural competence and sensitivity affect the effectiveness of community health nursing interventions?
- What are the main challenges community health nurses face in addressing social determinants of health ?
- How does community engagement contribute to the sustainability of community health initiatives led by nurses?
- What strategies effectively promote mental health awareness and reduce stigma within communities?
- How do telehealth services improve access to healthcare for individuals in geographically isolated regions?
- What role do community health nurses play in detecting and managing chronic diseases ?
- How do community health interventions impact healthcare utilization patterns and costs?
- What are the outcomes of community health nursing programs focused on improving maternal and child health?
Essay Topic Ideas & Examples
- The Role of Community Health Nursing in Promoting Population Health.
- Addressing Health Disparities: The Impact of Community Health Nursing.
- Community-Based Approaches to Preventing Teenage Pregnancy .
- Telehealth: Bridging Healthcare Gaps in Underserved Communities.
- Cultural Competence in Community Health Nursing: Challenges and Strategies.
- Disaster Preparedness and Response: The Critical Role of Community Health Nurses.
- The Influence of Social Determinants of Health on Community Health Nursing Interventions.
- Community Health Education: Strategies for Promoting Healthy Lifestyles.
- Exploring the Connection Between Mental Health and Community Well-being.
- Innovations in Community Health Nursing: Harnessing Technology for Better Outcomes.
As nursing students, you are poised to become the next generation of community health nurses, armed with the knowledge and skills to impact the health and well-being of diverse populations positively. Community health nursing offers numerous opportunities for research, practice, and advocacy. By delving into PICOT questions, evidence-based practice projects, capstone projects, research paper topics, and research questions, you can deepen your understanding of this vital field and contribute to its growth. Don’t hesitate to seek our writing services if you need assistance with your community health nursing assignments or essays. We understand the demands of nursing education and are here to support you in your academic journey. Your dedication to improving community health is commendable, and together, we can pave the way for healthier, more vibrant communities.
Frequently Asked Questions (FAQs) About Community Health Nursing
- Is community health nursing the same as nursing? Community health nursing is a specialized branch of nursing that focuses on providing holistic care to populations within specific communities. While nursing is a broader field encompassing various specialties, community health nursing is distinct in its emphasis on preventive care and health promotion within communities.
- What are the qualifications of a community health nursing? To practice community health nursing, one typically needs a registered nurse (RN) license. Many community health nurses also hold a Bachelor of Science in Nursing (BSN) degree, and advanced practice may require additional education such as a Master of Science in Nursing (MSN) with a specialization in community health.
- Do community health nurses work in hospitals? While community health nurses primarily work in community settings like public health departments, schools, and clinics, they can also collaborate with hospitals to provide education, preventive care, and continuity of care to patients transitioning from hospital to home.
- Can a community health nurse become a doctor? Community health nurses can certainly pursue further education and career advancement, but the path to becoming a doctor is different. Becoming a doctor requires completing medical school and earning a medical degree (MD) or a doctor of osteopathic medicine (DO) degree, whereas community health nursing involves nursing education and training.
Start by filling this short order form order.studyinghq.com
And then follow the progressive flow.
Having an issue, chat with us here
Cathy, CS.
New Concept ? Let a subject expert write your paper for You
Have a subject expert write for you now, have a subject expert finish your paper for you, edit my paper for me, have an expert write your dissertation's chapter, popular topics.
Business StudyingHq Essay Topics and Ideas How to Guides Samples
- Nursing Solutions
- Study Guides
- Free College Essay Examples
- Privacy Policy
- Writing Service
- Discounts / Offers
Study Hub:
- Studying Blog
- Topic Ideas
- How to Guides
- Business Studying
- Nursing Studying
- Literature and English Studying
Writing Tools
- Citation Generator
- Topic Generator
- Paraphrasing Tool
- Conclusion Maker
- Research Title Generator
- Thesis Statement Generator
- Summarizing Tool
- Terms and Conditions
- Confidentiality Policy
- Cookies Policy
- Refund and Revision Policy
Our samples and other types of content are meant for research and reference purposes only. We are strongly against plagiarism and academic dishonesty.
Contact Us:
📞 +15512677917
2012-2024 © studyinghq.com. All rights reserved
Community Nursing and Global Health
- Living reference work entry
- First Online: 22 December 2022
- Cite this living reference work entry

- Yvonne Parry 2 , 3
64 Accesses
Nursing provides the largest direct care and health intervention workforce and as such is a global health resource. Examinations of the International Classification for Nursing Practice (ICNP) have found that community nursing interventions directly address the identified themes related to gaps in healthcare, services, and system’s coverage and continue to support advancements in understanding the complexities of health for individuals, families, and communities. Additionally, nursing in and of itself addresses some global health goals through the provision of meaningful work for mostly women who are provided with income and career opportunities. Thus, nursing can assist in addressing inequities faced by populations with limited access to health and employment. This chapter outlines the role of community health nursing and how community nursing is used to address the global public health agenda. Community health is a nursing speciality that moves healthcare from the acute setting into the community-based health sector. These appropriate and cost-effective responses place community nursing at the forefront of responses to the global health Sustainable Development Goals. Globally, there is a need for more community nurses as they play a critical role in providing quality healthcare in the community. Community nurses enable the public to access best practice and evidence-based healthcare in their community in easy reach of the population. The research illustrated in this chapter uses community nursing services to directly address the global health agenda. Using examples from the Global North and South, the chapter provides evidence of the impact of community nursing on Global Health. The use of nurses in the community to advance health messaging and health access is foundational in addressing the needs of marginalized and vulnerable populations.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Institutional subscriptions
Similar content being viewed by others

Nurses in expanded roles to strengthen community-based health promotion and chronic care: policy implications from an international perspective; A commentary

Nursing Now
Abu Jaber M (2017) Time to stop ignoring cultural barriers to female employment in the MENA region. Education Plus Development, Monday, September 11, 2017. https://www.brookings.edu/blog/education-plus-development/2017/09/11/time-to-stop-ignoring-cultural-barriers-to-female-employment-in-the-mena-region/
Ahad MA, Parry YK, Willis E (2021) The prevalence and impact of maltreatment of child laborers in the context of four south Asian countries: a scoping review. Child Abuse Negl 117:105052. https://doi.org/10.1016/j.chiabu.2021.105052 . Epub 2021 Apr 5. PMID: 33831788
Article Google Scholar
All-Party Parliamentary Group on Global Health: Triple Impact – how developing nursing will improve health, promote gender equality and support economic growth; London. 17 October 2016.; http://www.appg.globalhealth.org.uk/
Ankers M (2022) How do diverse stakeholder groups perceive the activities of non-government Organisations (NGO) working with disadvantaged children in Siem Reap, Cambodia? Thesis for doctorate of philosophy Flinders University, college of nursing and health sciences. Adelaide, South Australia
Google Scholar
Becqué Y, Rietjens J, van der Heide A, Witkamp E (2021) How nurses support family caregivers in the complex context of end-of-life home care: a qualitative study. BMC Palliat Care 20:162. https://doi.org/10.1186/s12904-021-00854-8
Bell A, Parry Y, Willis E, Kendall S, Marriott R, Sivertsen N, Ankers M (2022) A nurse practitioner reflection on community care for marginalised children – conference presentation, international collaboration for community health nursing research, (ICCHNR). June 21, 2022. Life span health in community nursing (from children to old people) I: ZOMM LINK: https://lnu-se.zoom.us/j/66248317123 . Sweden
Block LJ, Currie LM, Strudwick G (2019) Visibility of community nursing within an administrative health classification system: evaluation of content change. J Med Internet Res 21(60):e12847
Cashin A (2015) The challenge of nurse innovation in the Australian context of universal care. Collegian 22:318–324
Cassiani SHB, Lira Neto JCG (2018) Nursing perspectives and the “nursing now” campaign. Rev Bras Enferm [Internet] 71(5):2351–2352. https://doi.org/10.1590/0034-7167.2018710501
Dhavan P, Reddy S (2017) Public health professionals. In: Quahin S (ed) International encyclopedia of public health, 2nd edn From: International Encyclopedia of Public Health (Second Edition), 2017 , https://www.sciencedirect.com/topics/nursing-and-health-professions/public-health-nursing
Dossey B, William R, Beck D (2019) Nursing and the sustainable development goals: from nightingale to now. Am J Nurs 119(5):44–49. https://doi.org/10.1097/01.NAJ.0000557912.35398.8f
Edmonson C, McCarthy C, Trent-Adams S, McCain C, Marshall J (2017) Global Health issues: a Nurse’s role. Online J Issues Nurs 22
Harvey C, Hegney D, Sobolewska A, Chamberlain D, Wood E, Wirihana L et al (2019) Developing a community-based nursing and midwifery career pathway – a narrative systematic review. PLoS One 14(3):e0211160. https://doi.org/10.1371/journal.pone.0211160
Article CAS Google Scholar
Hunter A, Wilson L, Stanhope M, Hatcher B, Hattar M, Hilfinger Messias DAK, Powell D (2013) Global health diplomacy: an integrative review of the literature and implications for nursing. Nurs Outlook 61(2):85–92. https://doi.org/10.1016/j.outlook.2012.07.013
International Council of Nurses [ICN] (2017) Nurses’ Role In Achieving The Sustainable Development Goals: International Nurses Day Resources And Evidence. Geneva. ISBN: 978–92–95099-41-8
Martin P, Duffy T, Johnston B, Banks P, Harkess-Murphy E, Martin CR (2013) Family health nursing: a response to the global health challenges. J Fam Nurs 19(1):99–118. https://doi.org/10.1177/1074840712471810 . Epub 2013 Jan 3. PMID: 23288887 . https://journals.sagepub.com/doi/abs/10.1177/1074840712471810?journalCode=jfna
MORENO-LACALLE RC, LOCSIN RC (2019) Emancipation through nursing within the context of health disparities. Belitung Nurs J 5(2):65–74. https://belitungraya.org/BRP/index.php/bnj/index
Nicholas P, Breakey S (2015) Chapter 1: Global health and global nursing. In: Breakey S (ed) Global heath nursing in the 21st century, 1st edn. Springer publishing
Parry Y, Button D (2020) Nursing and tensions within the Australian health care system. In: Wilson N, Lewis P, Hunt L, Whitehead L (eds) Nursing in Australia, 1st edn. Routledge. eBook ISBN9781003120698
Parry, Y., & Sivertsen, N. (2021). Social inclusion and the role of nurses. J Handbook Soc Incl, 1–15. https://www.researchgate.net/publication/353527446_Social_Inclusion_and_The_Role_of_Nurses
Parry YK, Hill P, Horsfall S (2018) Assessing levels of student nurse learning in community based health placement with vulnerable families: knowledge development for future clinical practice. Nurse Educ Pract 32:14–20. https://doi.org/10.1016/j.nepr.2018.06.015 . Epub 2018 Jun 30. PMID: 30015302
Parry YK, Willis E, Kendall S, Marriott R, Sivertsen N, Bell A (2020) Addressing the gaps in health for children, innovative health service delivery: enhancing lifelong development and the health and wellbeing of marginalised children 0 to 18 years. Caring Futures Institute, Flinders University. ISBN: 978-1-925562-40-8 https://researchnow.flinders.edu.au/en/publications/addressing-the-gaps-in-health-for-children-innovative-health-serv
Parry Y, Ankers M, Sivertsen N, Willis E (2021a) Where is community during COVID-19? The experiences of families living in housing insecurity. Health Soc Care Community 30(5):e2088–e2096
Parry Y, Willis E, Kendall S, Marriott R, Ankers M (2021b) A nurse practitioner service designed to address the health needs of children living in housing instability: a non-randomised, concurrent mixed methods study protocol. JAN 78(4). https://doi.org/10.1111/jan.15152 . https://onlinelibrary.wiley.com/doi/10.1111/jan.15152
Rosa WE, Kurth AE, Sullivan-Marx E, Shamian J, Shaw HK, Wilson LL, Crisp N (2019) Nursing and midwifery advocacy to lead the United Nations sustainable development agenda. Nurs Outlook 67(6):628–641. https://doi.org/10.1016/j.outlook.2019.06.013
Salvage J, White J (2020) Our future is global: nursing leadership and global health. Rev Lat Am Enfermagem 28:e3339. https://doi.org/10.1590/1518-8345.4542.3339 . Epub 2020 Aug 31. PMID: 32876292; PMCID: PMC7458571. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7458571/
Santos RK, Macedo E, Araujo BR, Lima AAA, Linch GFC, Caregnato RCA (2021) Nursing Now campaign and its impact on nursing education in a federal university. Rev Gaúcha Enferm 42(spe):e20200028. https://doi.org/10.1590/1983-1447.2021.20200028
Teruya N, Sunagawa Y, Sunagawa H, Toyosato T et al (2019) Asia Pac J Oncol Nurs 6(4):389–396. https://doi.org/10.4103/apjon.apjon_18_19 . PMID: 31572759; PMCID: PMC6696802
United Nations, (2015). Transforming our world: the 2030 agenda for sustainable development. [internet]. 2015 [cited Apr 2, 2020]. Available from https://sustainabledevelopment.un.org/post2015/transformingourworld
WHO, T. W. H. O. (2021, 13 April 2021). Noncommunicable diseases. Retrieved 12 Oct 2021 from https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
Wilson L, Mendes IAC, Klopper H, Catrambone C, Al-Maaitah R, Norton ME, Hill M (2016) ‘Global health’ and ‘global nursing’: proposed definitions from the global advisory panel on the future of nursing. J Adv Nurs 72(7):1529–1540. https://doi.org/10.1111/jan.12973
World Health Organization [WHO] (2018) A vision for primary health care in the 21st century: towards universal health coverage and the Sustainable Development Goals. World Health Organization and the United Nations Children’s Fund (UNICEF), Geneva, 2018 (WHO/HIS/SDS/2018.X). Licence: CC BY-NC-SA 3.0 IGO. https://www.who.int/docs/default-source/primary-health/vision.pdf
Download references

Author information
Authors and affiliations.
College of Nursing and Health Sciences, Flinders University, Adelaide, SA, Australia
Yvonne Parry
Research Lead, Better Communities, Caring Futures Institute, Adelaide, SA, Australia
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Yvonne Parry .
Editor information
Editors and affiliations.
School of Health Sciences, Western Sydney University, Camberwell, VIC, Australia
Pranee Liamputtong
Rights and permissions
Reprints and permissions
Copyright information
© 2023 Springer Nature Switzerland AG
About this entry
Cite this entry.
Parry, Y. (2023). Community Nursing and Global Health. In: Liamputtong, P. (eds) Handbook of Social Sciences and Global Public Health. Springer, Cham. https://doi.org/10.1007/978-3-030-96778-9_12-1
Download citation
DOI : https://doi.org/10.1007/978-3-030-96778-9_12-1
Received : 02 October 2022
Accepted : 09 October 2022
Published : 22 December 2022
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-96778-9
Online ISBN : 978-3-030-96778-9
eBook Packages : Springer Reference Social Sciences Reference Module Humanities and Social Sciences Reference Module Business, Economics and Social Sciences
- Publish with us
Policies and ethics
- Find a journal
- Track your research

Home > Graduate Theses, Dissertations, and Capstone Projects > ALL-PROGRAMS > HLTH_COMMUNITY_HEALTH_THESES
Community Health Education Theses
Theses/dissertations from 2023 2023.
Identifying Barriers to Dental Care Among Hispanics in Southwest Minnesota , Lissette Garza
Theses/Dissertations from 2022 2022
The Assessment of Emergency Preparedness Among University Students , Arliah Cox
Stress Coping Responses of Undergraduate University Students Prior to & Since the Onset of the COVID-19 Pandemic , Kaylee Diefenderfer
Perceptions of Well-Being Among College Majors , Baylee Jahraus
Theses/Dissertations from 2021 2021
Assessment of Perceived Levels of Stress and Coping Mechanism Use Among Elementary School Teachers , Lauren Larson
Theses/Dissertations from 2020 2020
An Assessment of Knowledge, Behavior, and Consumption Patterns Surrounding Sugar- Sweetened Beverages Among Young Adults , Anne Harguth
Perceptions, Attitudes, Self-Efficacy, and Behaviors of Mouthguard Use Among Collegiate Athletes , Heather Prosser
Human Papillomavirus (HPV) Infection and Vaccine Knowledge and Attitudes among University Students , McKenzie Schmitz
Theses/Dissertations from 2019 2019
Assessment of Perceived Levels of Stress and Coping Mechanisms Among University Students , Nancy Adomako-Saahene
A Needs Assessment: The Barriers Preventing Students at a Large Midwestern University from Accessing the Dental Clinic on Campus for Preventative Care , Pamela Briese
Incentive-Use in Worksite Wellness Programs in MN Government Agencies , Sandra Bromley
Assessing Knowledge, Attitude and Practices of Hand Hygiene Among University Students , Linda Afia Mbroh
Blood Pressure Screening Practices Among Dental Hygienists , Mariah Sullinger
Theses/Dissertations from 2018 2018
Assessment of Stress Related Issues and Coping Mechanisms among College Students , Emeka Okoro
Assessing the Relationship Between Parenting Styles and Dietary Behaviors Among Young Adults , Breanna Tofteland
Theses/Dissertations from 2017 2017
Workplace Management Knowledge and Support for Employee Breastfeeding Practices , Elizabeth Heimer
Student’s Oral Health Knowledge, Oral Health Practices, and Their Susceptibility to Oral Health Diseases at a Midwestern University , Mouhamed Koubaytari
Avian and Pandemic Influenza Knowledge and Risk Perception in Southern Minnesota , Holly Munch
Preconception Health Knowledge among Undergraduate Women , Ashley Mae Paulsen
Complementary and Alternative Medicine: Current Mind-Body Practices and Perceptions of Undergraduate Students , Julia Ann Marie Putz
Screen Time and Sleep Condition among Selected College Students , Angela Lynn Sargent
Understanding Zoonotic Enteric Disease in Minnesota: A Spatio Temporal Analysis and Causal Theory Approach , Suchismita Swain
The Relationship Between Religiosity and Depression Among Sampled Kenyans In The Twin Cities Metro Area , Dorcas Waite
Theses/Dissertations from 2016 2016
North Minneapolis Residents' Knowledge and Awareness of Indoor Air Quality in Older Residences , Blisse Marie Cajacob
Impact of Stigma on Attitudes towards Seeking Professional Psychological Help for Depression , Anna Marie Dierks
Fruit and Vegetable Availability, Nutrition Education and Access Amongst Food Pantries in California, Maine, Mississippi and South Dakota , Sarah L. Fowler
An Analysis of Western Medicine Mistrust Among Selected African Immigrant Women in Minnesota , Wanjiru Julie Gicheru
Minnesota Collaborative Agreement: Potential for Dental Hygienists to Increase Direct Access for Underserved Populations , Rachel Jane Kashani-Legler
Human Papillomavirus and Human Herpesvirus-8: Knowledge, Perception of Risk and Barriers to Screening and Treatment among Selected Students at Africa University, Zimbabwe , Rujeko Olga Machinga
Young Adults’ Attitudes and Perceptions on Health Insurance and their Health Insurance Literacy Levels , Law Yang
Theses/Dissertations from 2015 2015
Relationship between Nurses' Job Satisfaction and Quality of Healthcare They Deliver , Samuel Aron
Employees' Interests and Preferences Regarding Worksite Exercise Programs , Amber Butcher
Religiosity, Spirituality, and Quality of Life Among Selected University Students , Abby Austin Kreitlow
Health Literacy Proficiency, Sources of Health Information, and Perceived Barriers to Health Literacy Among Selected Members of the Hmong Community in Minnesota , Amanda Vang
Elderly Patient Adherence to Ocular Pharmaceuticals; Impact of Educational and Physical Barriers , Lucky Wagner
Theses/Dissertations from 2014 2014
Physical Environment and Women's Physical Activity Behaviors , Beth Ann Brisky
Plan B Emergency Contraception: Sampled University Students' Knowledge, Attitudes, and Behaviors , Natalie Hazel
Risk Perceptions of Cardiovascular Disease in College Students , Antonia Kolas
Knowledge of HPV, Perception of Risk, and Intent to obtain HPV Vaccination among sampled Male University Students at Minnesota State University, Mankato , Lia Lambert
Sex Education Background of Students at MSU, Mankato Prior to Enrollment at the University , Natalie McConkey
Sampled University Students' Perceived Risk of Diabetes & Self-reported Diabetes Risk Factors , Ajibike R. Shodunke
University Students' Perceptions Of The Severity Of Binge Drinking , Lauren Eleanore Stone
Breastfeeding knowledge, practice, attitudes, and influencing factors: Findings from a selected sample of breastfeeding mothers in Bemidji, Minnesota , Hadeel Adnan Tanash
Recognition of and Attitudes Toward, Intimate Partner Violence Among Sampled University Students , Samantha Maureen Wobschall
Theses/Dissertations from 2013 2013
Health Promotion in the Workplace: Exploring Perspectives of Barriers and Incentives to Employee Participation , Amanda Conlon
The Relationship Between Emotional Intelligence And Alcohol Use Among Students at Minnesota State University - Mankato , Ganisher Davlyatov
The Impact of Telephonic Health Coaching on Physical Activity, Healthy Eating, and Cholesterol Levels , Jill Marie Hansen
Selected College Students' Perceptions, Knowledge and Awareness of Sexual Abuse of Children , Farhiya A. Muse
Access to EMS Services and Training, Knowledge, and Perceptions Related to First Aid and Cardiopulmonary Resuscitation (CPR) Skills Among College Students , Feifei Sun
Theses/Dissertations from 2012 2012
Mothers' Health and Health Behaviors that Influence Childhod Obesity Maternal BMI and Infant Feeding Methods , Mohamed Abdullah Alammari
Assessment of Selected University Students' Knowledge of Blood Donation and the Relationship with Intent to Donate Blood , Jeffrey Allerson
Study of International Students' Definations of, and Perceptions About, Domestic Violence Against Women , Sarbinaz Zamirovna Bekmuratova
Health Care Providers' Intention to Provide Culturally Competent Health Care to Somali Based Upon the Indirect Measures of the Integrated Behavioral Model , Amanda Kaye Ciesinski
The Relationship Between Religiosity & Selected Health Behaviors of African Americans of the Pentecostal Faith , Caprice Jones-Agunbiade
Perceptions of Risk Associated with Unintended Pregnancy and Sexually Transmitted Infections among University Women attending Minnesota State University, Mankato , Jessica Maria Seide
The Relationship Between Disordered Eating Behaviors and Exercise Addiction Among Selected University Students at Minnesota State University, Mankato , Haley Wasko
Theses/Dissertations from 2011 2011
Assessing Students' Risk Factors for Type II Diabetes at a Midwest Public University , Nicole DeCourcy Ferrian
An Investigation on HIV Related Stigma to Improve HIV Prevention Efforts in North Dakota , Krissie Lynn Mayer-Guerard
Use of Social Marketing Promotional Strategies to Create Awareness of Worksite Health Promotion Programs: A Survey of Program Coordinators , Anna Catherine Stahl
Advanced Search
- Notify me via email or RSS
Author Corner
- All Authors
- Submit Research
University Resources
- Digital Exhibits
- ARCH: University Archives Digital Collections
- Library Services
- Minnesota State University, Mankato

Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
- Bibliography
- More Referencing guides Blog Automated transliteration Relevant bibliographies by topics
- Automated transliteration
- Relevant bibliographies by topics
- Referencing guides
Dissertations / Theses on the topic 'Community health nursing – Swaziland'
Create a spot-on reference in apa, mla, chicago, harvard, and other styles.
Consult the top 50 dissertations / theses for your research on the topic 'Community health nursing – Swaziland.'
Next to every source in the list of references, there is an 'Add to bibliography' button. Press on it, and we will generate automatically the bibliographic reference to the chosen work in the citation style you need: APA, MLA, Harvard, Chicago, Vancouver, etc.
You can also download the full text of the academic publication as pdf and read online its abstract whenever available in the metadata.
Browse dissertations / theses on a wide variety of disciplines and organise your bibliography correctly.
Brookbank, Kathleen. "HIV : impact on community health nursing personnel." Virtual Press, 1992. http://liblink.bsu.edu/uhtbin/catkey/834518.
Duah, Maame Akyaa. "Baccalaureate Nursing Students’ Perceptions of Community Health Nursing as a Career." Thesis, Université d'Ottawa / University of Ottawa, 2015. http://hdl.handle.net/10393/33388.
Lidstone, Terri Lynn. "Boundaries and trust in community mental health nursing." Thesis, National Library of Canada = Bibliothèque nationale du Canada, 2000. http://www.collectionscanada.ca/obj/s4/f2/dsk1/tape4/PQDD_0010/MQ60083.pdf.
Mngadi, Patricia Thuli. "Adolescent pregnancy and parenthood in Swaziland : quality of care, community support and health care service needs /." Stockholm, 2007. http://diss.kib.ki.se/2007/978-91-7140-725-2/.
Francis, Karen. "Poverty, chastity and obedience : the foundations of community nursing in New South Wales /." Title page, contents, abstract and introduction only, 1998. http://web4.library.adelaide.edu.au/theses/09PH/09phf8185.pdf.
Duncan, Susan Maxine. "Ethical conflict and response in community health nursing practice." Thesis, University of British Columbia, 1989. http://hdl.handle.net/2429/27333.
Chang, Pei-Jen. "Factors influencing occupational health nursing practice." Thesis, King's College London (University of London), 1994. https://kclpure.kcl.ac.uk/portal/en/theses/factors-influencing-occupational-health-nursing-practice(117dd5b4-81ff-45dd-8966-3ea83809c449).html.
Carter, Nancy Jo Crumpler Thomas P. Spycher Ellen A. "Perceptions of challenges and knowledge and skill for community based nursing practice." Normal, Ill. : Illinois State University, 2007. http://proquest.umi.com/pqdweb?index=0&did=1414124161&SrchMode=1&sid=3&Fmt=2&VInst=PROD&VType=PQD&RQT=309&VName=PQD&TS=1205251510&clientId=43838.
Krassy, Margaret Mary. "As things change : an ethnography of a community health nursing agency /." Access Digital Full Text version, 1995. http://pocketknowledge.tc.columbia.edu/home.php/bybib/12136505.
Weierbach, Florence M. "IGNITES Voices from Our Community." Digital Commons @ East Tennessee State University, 2018. https://dc.etsu.edu/etsu-works/7371.
Bartholomeaux, Frances Marie 1955. "Variables influencing community cardiopulmonary resuscitation course participation." Thesis, The University of Arizona, 1990. http://hdl.handle.net/10150/277318.
Weierbach, Florence M. "Integrating Community Concepts, DNP Essentials & Practice." Digital Commons @ East Tennessee State University, 2012. https://dc.etsu.edu/etsu-works/7402.
Boytell, Darlene M. "Relation of health related hardiness to health perception and psychosocial adaptation in adult hispanics with chronic hepatitis C." FIU Digital Commons, 1996. http://digitalcommons.fiu.edu/etd/1782.
Bjorn, Agnes Marie. "Community health assessment and nursing care needs of the elderly." Thesis, University of Manchester, 1989. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.237239.
Murray, Christopher J. L. "The determinants of health improvement in developing countries : case-studies of St. Lucia, Guyana, Paraguay, Kiribati, Swaziland and Bolivia." Thesis, University of Oxford, 1988. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.304625.
Alcazar, Maria. "Childhood/teen obesity in the Hispanic community." Thesis, California State University, Long Beach, 2015. http://pqdtopen.proquest.com/#viewpdf?dispub=1587255.
Obesity in the United States should be of great concern to all Americans. The rates of obesity among children and adolescents have been on the rise, demonstrating the need for action now. Obesity at a young age can lead to obesity into adulthood, thereby also increasing the risk of health issues such as the development of high blood pressure and diabetes. Many factors go into play when dealing with obesity, yet the factors that will be considered in this study are the effects of decrease activity and the impact of BMI of a child or teen. Another factor that will be consideed in this study is the consumption of sugar sweetened beverages and how this also affects a child or teens BMI.
Teasdale, John Kevin. "Reassurance in nursing." Thesis, Sheffield Hallam University, 1992. http://shura.shu.ac.uk/3162/.
Cheung, Philip L. "Phenomenology of nursing." Thesis, University of Southampton, 1991. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.316012.
Simons, Lucy. "Community mental health nurses' perspectives on the treatment of people with common mental health problems." Thesis, University of Southampton, 2006. https://eprints.soton.ac.uk/57942/.
Dobbins, Elizabeth M. "Non-Language Barriers to Effective Care of the Hispanic Population." Digital Commons @ East Tennessee State University, 2015. https://dc.etsu.edu/honors/274.
Spicer, Judith Evangeline. "District nursing : its focus through a comparative analysis of nursing problems." Thesis, University of Surrey, 1993. http://epubs.surrey.ac.uk/844117/.
Runciman, Phyllis Janet. "Interpreting health promotion with older people in community health nursing : education and practice perspectives." Thesis, Glasgow Caledonian University, 2010. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.547440.
Bennett, Amanda Dawn. "Project GENESIS: Community Assessment of a Rural Southeastern Arizona Border Community." Diss., The University of Arizona, 2009. http://hdl.handle.net/10150/194342.
Al-Darmaki, Salem A. "Assessing the need for community health nursing services in the UAE." Thesis, Durham University, 2004. http://etheses.dur.ac.uk/3173/.
Conrad, Michael Dean, and Anna Kampanartsanyakorn. "Advanced practice nursing health care needs assessment in an underserved community." CSUSB ScholarWorks, 2003. https://scholarworks.lib.csusb.edu/etd-project/2336.
Eastmond, Cheryl. "Implementation of a cardiovascular health-promotion program in a rural Africa-American community." NSUWorks, 2014. https://nsuworks.nova.edu/hpd_con_stuetd/20.
Cuddy, Janet Brooke. "Development of an Evidence-Based Nursing Orientation Program for a Community Health System." ScholarWorks, 2015. https://scholarworks.waldenu.edu/dissertations/748.
Brehm, Jerrilyn S., M. Yasin, and Florence M. Weierbach. "Building Trust with Novice Community Based Preceptors." Digital Commons @ East Tennessee State University, 2018. https://dc.etsu.edu/etsu-works/7397.
Bolton, Mychal. "Perceived Barriers to Obtaining Psychiatric Treatment at Johnson City Community Health Center." Digital Commons @ East Tennessee State University, 2014. https://dc.etsu.edu/honors/223.
Earle, Wendy. "Factors that influence heart failure self-management of community dwelling individuals." Thesis, University of Ottawa (Canada), 2005. http://hdl.handle.net/10393/27195.
Mobley, Deborah. "The Lived Experience of Faith Community Nurses Living the Call to Health Ministry." VCU Scholars Compass, 2010. http://scholarscompass.vcu.edu/etd/101.
Morton, Jea, Florence M. Weierbach, Rebecca Sutter, Kae Livsey, J. Bliss, Jerrilyn S. Brehm, and J. Metcalf. "Transforming Community Health Nursing Education: Lessons Learned from Individual and Cross Grantee Program Evaluations from a Federal Bachelor of Science in Community Practicum Awards." Digital Commons @ East Tennessee State University, 2019. https://dc.etsu.edu/etsu-works/7379.
Schoonover, Heather Diane. "Barriers to research utilization among registered nurses working in a community hospital." Online access for everyone, 2006. http://www.dissertations.wsu.edu/Thesis/Spring2006/H%5FSchoonover%5F033106.pdf.
Meurier, Clency Emmanuel. "Improving the quality of nursing care : a study of nursing errors and their reduction." Thesis, University College London (University of London), 1998. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.287996.
Keith, Rosalind R. "Initiating Nicotine Cessation in a Community Mental Health Center." ScholarWorks, 2016. https://scholarworks.waldenu.edu/dissertations/2128.
Rice, Judy A. "The Johnson City Community Health Center: Treating the Uninsured Mentally Ill." Digital Commons @ East Tennessee State University, 2015. https://dc.etsu.edu/etsu-works/7624.
Boulle, Therese Marie. "Developing an Understanding of the factors related to the effective functioning of Community Health Committees in Nelson Mandela Bay Metropolitan Municipality, Eastern Cape Province, South Africa." Thesis, University of the Western Cape, 2007. http://etd.uwc.ac.za/index.php?module=etd&action=viewtitle&id=gen8Srv25Nme4_4635_1253238212.
This research aimed to investigate the factors related to the functioning of Community Health Committees in Nelston MandelaBay Municipality. It intended to elicit information on factors which promote and inhibit their effective functioning. It used the qualitative research methods of focus group discussions, concluded with a sample of Community Health Committee members, and in depth, individual interviews with key informants. The contents of the transcriptions of all focus group discussions and in-depth individual interviews were analysed so as to identify the recurring themes and key suggestions.The findings indicated that Community Health Committees are not functioning as per their original intention and that relevant policies have not been accurately translated into practice.
Fordham, Maria. "Being and becoming a specialist public health nurse : net weaving in homeless health care." Thesis, University of Bedfordshire, 2012. http://hdl.handle.net/10547/304613.
Greathead, Erica. "Role competencies of first-line nurse managers in community health centres : a delphi study." Master's thesis, University of Cape Town, 2000. http://hdl.handle.net/11427/2951.
Adams, Faiza Kajee. "Violence in nursing : perceived prevalence and impact in community health clinics in Cape Town." Master's thesis, University of Cape Town, 2010. http://hdl.handle.net/11427/12733.
Udjombala, Hilka Tuyenikelao. "Malaria in Namibia : a community study." Thesis, Stellenbosch : Stellenbosch University, 2001. http://hdl.handle.net/10019.1/52329.
Sapsford, Lesley Eliaine. "The professional development of primary health care nurses in integrated self managing teams." Thesis, Bucks New University, 1998. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.270297.
Dudley, Nancy Elizabeth. "Factors Influencing the Uptake of Community-based Palliative Care." Thesis, University of California, San Francisco, 2016. http://pqdtopen.proquest.com/#viewpdf?dispub=10133428.
Over the past ten years, community-based palliative care (CBPC) has rapidly expanded as older adults are living in the community longer with advanced illness and high symptom burden. Yet there are no models of standardized care for this population. It has been suggested that primary and secondary palliative care be delivered in the primary care setting to address palliative care needs in the community. However, a description of older adults in primary care with advanced illness and symptom burden who would benefit from primary and secondary palliative care, and a description of the process to deliver care are lacking. The aim of this dissertation was to explore the facilitators and barriers to providing palliative care in primary care, and to describe the prevalence of advanced illness and symptoms of older adults in primary care to identify who would benefit from palliative care in primary care.
Using a grounded theory methodology, twenty semi-structured interviews were conducted with primary care and palliative care providers in academic and community settings. Four major themes emerged from the data that are facilitators and barriers in care coordination: (i) role clarity; (ii) feedback and communication; (iii) time constraint and workforce; (iv) education.
A secondary analysis was conducted using the National Ambulatory and Hospital Medical Care Surveys 2009-2011 to examine primary care visits. There were more visits by older adults to primary care for advanced illness and symptoms than to non-primary care. More visits were due to advanced COPD, CHF, dementia, pain, depression, anxiety, fatigue, and insomnia compared to non-primary care. This research contributes to our knowledge of the delivery of palliative care in the community and the patient population that could benefit from primary and specialty palliative care. I offer a conceptual model of the process of primary care and specialty palliative care in order to coordinate care for older adults with advanced illness and progressive symptomatology.
Sattler, Victoria. "Understanding the meaning of an international community focused teaching-learning experience in Peru." Pullman, Wash. : Washington State University, 2009. http://www.dissertations.wsu.edu/Thesis/Fall2009/v_sattler_111909.pdf.
Green, Kemble. ""Nursing Contamination: Wearing Scrubs in Public"." Digital Commons @ East Tennessee State University, 2014. https://dc.etsu.edu/honors/238.
Ghaly, Marina Adele. "Client outcomes in a community health setting." Thesis, The University of Arizona, 1990. http://hdl.handle.net/10150/277274.
Morton, Jea, Mary Kay Goldschmidt, Rebecca Sutter, Kae Livsey, D. Martin, Florence M. Weierbach, J. Bliss, and J. Metcalf. "Preparing Graduates for Roles in Community-based Nursing Practice." Digital Commons @ East Tennessee State University, 2018. https://dc.etsu.edu/etsu-works/7381.
McLaughlin, Michael P. "Community college nursing and allied health education programs, and Iowa's healthcare workforce." [Ames, Iowa : Iowa State University], 2009.
Coombs, Maureen A. "Medicine, nursing and policy development in intensive care : an ethnography to explore the contemporary nursing role." Thesis, Oxford Brookes University, 2000. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.323909.
Davis, Kierrynn Miriam Davis. "Cartographies of rural community nursing and primary health care : mapping the in-between spaces /." [Richmond, N.S.W.] : University of Western Sydney, Hawkesbury, 1998. http://library.uws.edu.au/adt-NUWS/public/adt-NUWS20030509.135659/index.html.
Patients with private insurance can face higher health costs at hospitals

People with private health insurance might pay higher prices for procedures or tests at a hospital.
A report published Monday by the research group Rand Corp. found that in 2022, the prices hospitals charged to private and employer-based insurance providers were, on average, 254% higher than what Medicare would have paid for the same services.
“These very high payments ultimately result in higher premiums for health insurance coverage and can result in those needing care having to pay high prices to get it,” said Stacie Dusetzina, a health policy professor at Vanderbilt University in Nashville, Tennessee, who wasn’t involved with the report.
The new findings were based on an analysis of health insurance claims data from more than 4,000 hospitals in 49 states and Washington, D.C., from 2020 through 2022. It included both inpatient and outpatient services. In total, the study analyzed about 6% of what private insurance paid out to hospitals during the time period.
Brian Briscombe, a health care cost analyst at Rand Corp. who led the report, said the high prices charged to private insurers mean patients will also end up paying more, either directly, in the form of higher copays or out-of-pocket payments , or indirectly, in the form of a smaller paycheck.
About 160 million people in the U.S. get their health insurance through their jobs, Briscombe said. “When you think about it in the way of an economist, all of it is paid by the patient. I mean, if it cost my job half as much to have health care, my salary would go up,” he said.
In 2022, hospital services accounted for 42% of health care spending for people with private health insurance, and price hikes from hospitals were a significant contributor to the rise in the average amount spent per person.
The report found wide variation in hospital prices among states.
Hospitals in Arkansas, Iowa, Massachusetts, Michigan and Mississippi charged private insurance prices below 200% of what Medicare would pay.
California, Florida, Georgia, New York, South Carolina, West Virginia and Wisconsin charged private insurance prices that were above 300% of what Medicare would pay.
The report also found that hospitals often charged higher prices for prescription drugs administered by a health care worker, compared to prices charged for the same drugs given in a similar setting, such as a physician’s office.
Briscombe attributed the price discrepancies to the enormous pricing power hospitals wield. If a hospital has limited competition in a given region, for example, it can often charge patients and insurers whatever it wants.
“Obviously, some hospitals cost more because they’re better,” he said. “But as you get more market share, you kind of become the big game in town and it becomes very hard for an employer to say, ‘We won’t use that hospital.’”
Meanwhile, Medicare often pays less in part because it has more negotiating power with hospitals, said Cynthia Cox, a vice president at KFF, a group that researches health policy issues. Most people on Medicare are older adults with underlying health conditions and represent a large portion of hospital revenue.
Molly Smith, group vice president for policy at the American Hospital Association, the hospital industry’s trade group, called the report’s findings “a skewed and incomplete picture of hospital spending.”
An AHA report published in January found that in 2022 Medicare “significantly” underpaid hospitals for the cost of providing care to patients.
For every dollar hospitals spent caring for Medicare patients, they were only reimbursed 82 cents, according to the report. In all, Medicare underpayments totaled $99.2 billion, it said.
“In benchmarking against woefully inadequate Medicare payments, Rand makes an apples-to-oranges comparison that presents an inflated impression of what hospitals are actually getting paid for delivering care while facing continued financial and other operational challenges,” Smith said.
Dusetzina, from Vanderbilt University, said the Rand report’s findings are consistent with earlier studies showing that private insurance often pays higher prices.
“The one benefit for commercially insured individuals is that they do have out-of-pocket limits for in-network care, so even if the prices are very high, as long as the systems where they are getting care are in-network, there is an upper limit on what they would pay,” she noted.
Cox said there has been a push for more pricing transparency from hospitals, which would allow insurers to negotiate for lower rates and patients to shop around for a better deal.
A federal rule from the Centers for Medicare and Medicaid Services requires hospitals to post their prices. However, reports have shown that very few hospitals comply with the rule.
Cox added that pricing transparency can be a bit complicated because it’s not always obvious how much a service will cost and for what reason.
“It’s not always clear from looking at price transparency data exactly how much someone’s being paid,” she said. “For example, you might see that an MRI looks like it costs 20 cents, but really it’s 20% of some other numbers.”
Briscombe said the Rand report is intended to empower and inform employers and patients.
“When you think about the price of anything, whether you’re buying a Lamborghini, you think, ‘Is it overpriced?’” he said. “Well, the only person who can decide that is the person buying it.”
Berkeley Lovelace Jr. is a health and medical reporter for NBC News. He covers the Food and Drug Administration, with a special focus on Covid vaccines, prescription drug pricing and health care. He previously covered the biotech and pharmaceutical industry with CNBC.
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Infection Prevention and Long-term Care Facility Residents
- Nursing Home Infection Preventionist Training
- PPE in Nursing Homes
- Respiratory Virus Toolkit
- Healthcare-Associated Infections (HAIs)
- The resources on this page can keep you and your loved ones safe.
Long-term care facilities provide many services, both medical and personal care, to people who are unable to live without help.
If you live in a nursing home, assisted living facility or other long-term care facility, you have a higher risk of getting an infection. There are steps you can take to reduce your risk:
- Tell your healthcare provider if you think you have an infection or if your infection is getting worse.
- Take antibiotics exactly as prescribed and tell your healthcare provider if you have any side effects, such as diarrhea.
- Keep your hands clean. Remind staff and visitors to keep their hands clean.
- Get vaccinated against flu and other infections to avoid complications.
Resources for staying safe in long-term care facilities

About C. diff
About Carbapenem-resistant Enterobacterales
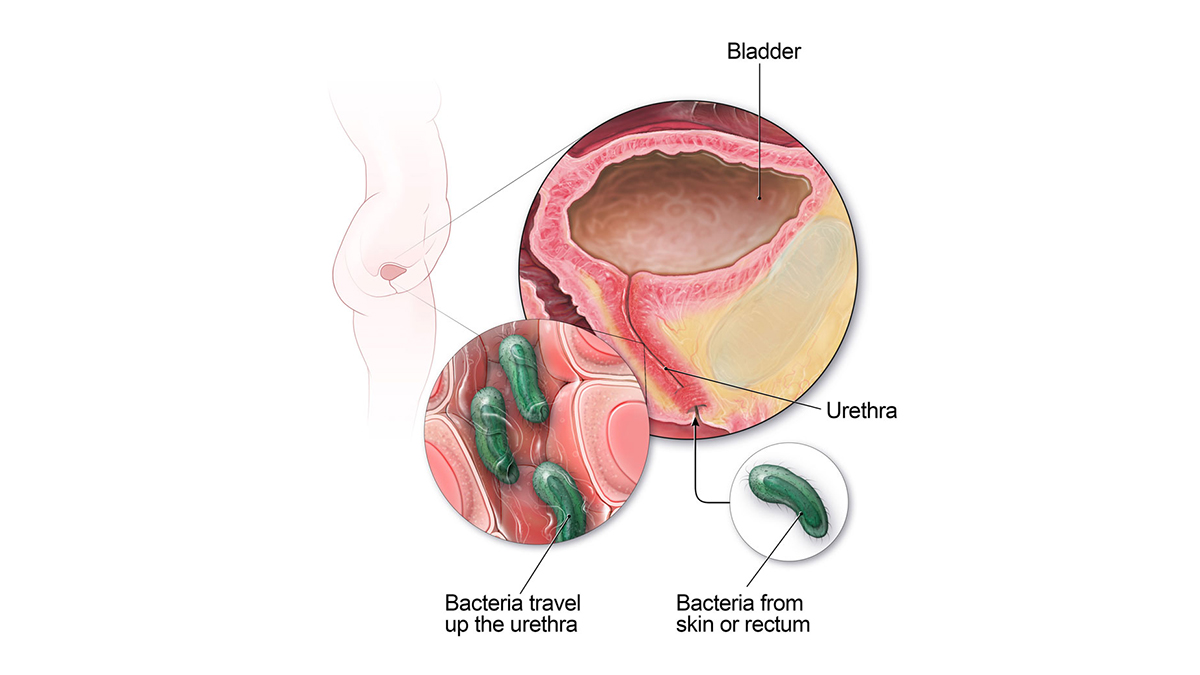
Catheter-associated Urinary Tract Infection Basics
Methicillin-resistant Staphylococcus aureus (MRSA) Basics

Healthy Habits: Antibiotic Do's and Don'ts

About Sepsis

About Norovirus
Resources for family members and caregivers
- Medicare resources for long-term care residents and caregivers.
- Find a nursing home in your area .
This website provides resources for patients, families and caregivers on the prevention of infections in nursing homes and assisted living facilities.
For Everyone
Health care providers.
Nursing Students who will earn while they learn, Father's Day 5K: Seacoast health news
Wentworth-douglass hospital awards $30k for fresh food bus.
DOVER – Wentworth-Douglass Hospital has awarded a $30,000 community benefit grant to support Gather’s Fresh Food Bus, which provides a mobile market of fresh foods for food insecure families.
Portsmouth-based Gather, a non-profit dedicated to food insecurity, introduced the bus last year to make fresh, nutritious food more accessible to underserved families who face transportation barriers. The bus makes about 14 stops per month, including biweekly at Wentworth-Douglass. It serves an average of 40 families per visit to the hospital, most of whom are either patients or part of a hospital-affiliated social service program.
“We are proud to support Gather and their Fresh Food Bus initiative, which exemplifies our commitment to holistic health care,” said Meaghan Heusler, community benefits manager at Wentworth-Douglass. “Gather is one of the oldest social service agencies in the country, but this is a great example of their continued commitment to innovation, and we are extremely grateful for the support they provide our patients and community.”
Food insecurity remains a significant issue for communities in the Greater Seacoast region. New Hampshire Hunger Solutions recently reported that 44% of adults and more than half (52%) of New Hampshire children live in households that reported having insufficient food. Inflated food prices and the rollback of pandemic-area safety net programs are contributing to the crisis.
With the additional funding from Wentworth-Douglass, Gather intends to serve an additional 20 families per bus visit (increasing the total to 60) and provide a balanced selection of fresh produce, meats, dairy, bread, and other essential non-perishable items to program participants.
"We extend our gratitude to Wentworth-Douglass for their generous support of Gather's Fresh Food Bus initiative, which not only helps us address food insecurity, but also underscores their dedication to the health and wellness of the community,” said Gather executive director Anne Hayes. “We are proud that together we are making a tangible difference in the lives of underserved families across the Seacoast.”
Father's Day 5K supports community health
DOVER — Registration is now open for Greater Seacoast Community Health’s annual Father’s Day 5K. This event to be held on Sunday, June 16 at 9 a.m. in Dover. Runners and walkers of all ages and abilities are invited to participate in this family-friendly run/walk. Event proceeds help individuals and families gain access to health care and family support services through Greater Seacoast’s network of community health centers. These include Families First Health & Support Center in Portsmouth and Goodwin Community Health in Somersworth.
The Father’s Day 5K is a part of the Dover Race Series and is run on a USA Track and Field certified course. Anyone who registers before June 1 receives a free race tank or t-shirt. In addition, families are invited to visit the Kids Fun Zone before, after, or during the race. The Kids Fun Zone has age-appropriate games and activities for younger participants.
Registration is open at tinyurl.com/fathers-day-5k . The cost is $25 for teens and adults, $5 for children under 12. Same-day registration is available beginning at 8:00 a.m. and the race will begin at 9 a.m. For more information visit getcommunityhealth.org .
Portsmouth Regional Hospital welcomes New England College Nursing Students who will earn while they learn
PORTSMOUTH Portsmouth Regional Hospital hosted a ribbon-cutting ceremony Monday, May 6, to welcome its first cohort of nursing students from New England College (NEC). The cohort of 20 students is enrolled in NEC’s three-year Bachelor of Science in Nursing program. This program uniquely allows students to earn while they learn by combining traditional classroom learning with paid immersive cooperative clinical experiences at partner hospitals throughout New Hampshire. The partnership between NEC and Portsmouth Regional Hospital, part of the HCA Healthcare family of healthcare services, was announced in January.
During three paid immersive clinical experiences, NEC nursing students work as licensed nursing assistants (LNAs) alongside experienced nurse preceptors and NEC faculty, gaining realworld experience that accelerates their training and enables them to graduate in three years instead of four.
NEC will be part of four additional cohort kickoff events this summer: Cheshire Medical Center in Keene on May 20, Elliot Hospital in Manchester on May 22, Parkland Medical Center in Derry on June 3, and Concord Hospital—Laconia on June 5. Learn more about NEC’s three-year Bachelor of Science in Nursing at www.nec.edu/nursing.
Annual Kites Against Cancer event planned for May 19
EXETER – The community is invited to come fly a kite at Exeter Hospital’s annual Kites Against Cancer event on Sunday, May 19 from 11 a.m. to 2 p.m. at Hampton Beach, near the Oceanfront Pavilion. This uplifting family event invites community members to spend an afternoon at the beach surrounded by family, friends and neighbors in support and in memory of those affected by cancer.
The event is free and open to the public. As in past years, kites will be available to decorate and personalize in memory or in honor of a loved one. Kites will be available to purchase at the event for $10 each, which will support Exeter Hospital’s Beyond the Rainbow Fund, providing financial assistance to cancer patients in need with expenses such as groceries, utilities, gas, and rent/mortgage payments, as well as any other practical needs that may become unmanageable during their treatment.
For additional information about Kites Against Cancer and opportunities to get involved, visit unitedinwellness.org.
Local News | Lowell Community Health Center expands…
Share this:.
- Click to share on Facebook (Opens in new window)
- Click to share on X (Opens in new window)
- Purchase Photos
- Sun Santa Fund
Local News | Lowell Community Health Center expands patient-care model
In-house pharmacy, new walk-in clinic part of $2.4 million upgrade.

The Lowell Community Health Center team working to improve its patient care services to include a new walk-in patient area and a new pharmacy in its first-floor lobby area. Construction started May 1, and is expected to be completed by Sept. 30, 2024. From left, Diane Martin, 340B program compliance manager; Director of Facilities Cynthia Wood; Chief Operating Officer Elizabeth Hale; Dr. Alison Curcio, chief of the Patient Walk-In Center; Senior Director of Pharmacy Services, Amy Sullivan; Director of Security and Public Safety Christopher Maher stand in one of the under-construction patient consult rooms of the new pharmacy space.(Melanie Gilbert/Lowell Sun)

Cynthia Wood, Lowell Community Health Center's director of facilities shows the under-construction space of the new walk-in patient area and a new pharmacy in its first-floor lobby area. Construction started May 1, and is expected to be completed by Sept. 30, 2024. (Melanie Gilbert/Lowell Sun)

Lowell Community Health Center is expanding and improving its patient care services to include a new walk-in patient area and a new pharmacy in its first-floor lobby area. Construction started May 1, and is expected to be completed by Sept. 30, 2024. The construction includes patient kiosks, seen here, for prescription consultation. (Melanie Gilbert/Lowell Sun)

Assistant Superintendent Seth Vogel, right, and Superintendent James Latour, of Green Leaf Construction is doing the work on improving Lowell Community Health Center's patient services by expanding the walk-in patient area and constructing a new pharmacy in its first-floor lobby area. Construction started May 1, and is expected to be complete by Sept. 30, 2024. (Melanie Gilbert/Lowell Sun)

Lowell Community Health Center sign. (Julia Malakie/Lowell Sun)
“We’ve completely outgrown our current pharmacy space,” Chief Operating Officer Elizabeth Hale said during a tour of the under-construction project Friday morning.
Currently, the prescription services of the health center are provided by a 600-square-foot CVS-run pharmacy. Hale said that with the retail drugstore chain getting out of the federally qualified health care business, LCHC saw an opportunity to step in and provide and manage those services in-house.
“Three years ago this July, we started our clinical pharmacy program,” she said. “We brought on Amy [Sullivan] and a team of clinical pharmacists. It demonstrated to us what an important, integral part of the health care team pharmacists are.”
Sullivan, the senior director of pharmacy services, said that expanding the pharmacy space from 1,100 square feet to 1,600 square feet may facilitate prescription compliance by reducing wait times. She noted that of the 1,000 people who come to LCHC every day, between 300-500 of those patients access the current pharmacy services.
“It’s a high-volume pharmacy,” Sullivan said. “We could see a doubling of that. This project will make it easier to access care and reduce barriers to entry, as well as receiving prompt, efficient and culturally competent care.”
The in-house pharmacy will feature the latest high-tech equipment to streamline operations to further improve wait times and efficiencies, said 340B Program Compliance Manager Diane Martin.
“We’re really investing in automation,” she said. “We’ll have a prescription-filling robot that can fill100 prescriptions an hour — sort, count and label.”
The existing Patient Walk-in Center offers a range of immediate care service such as sick visits, joint injuries, stitches, assistance with sprains and back pain, treatment of skin infections, non-severe allergy management and on-the-spot testing for conditions like COVID-19, pregnancy, urinary infections, vaginal infections, sore throats and flu. It can also give same-day vaccines.
But it does so in a crowded, semi-private space that Hale said isn’t user-friendly for staff or patients.
“What we learned from the pandemic is that we had a capacity issue in our walk-in center,” Hale said. “How do we make sure that we have a waiting room where people aren’t top of each other where we can safely take care of them? We need to have quick, easy access where we could service a lot of patients quickly and efficiently – our space wasn’t conducive to that.”
The new space will have a larger waiting area, updated and expanded exam rooms and Americans with Disabilities Act-compliant consult rooms.
The clinical expansion of the pharmacy and walk-in center is one more step in the organization’s model toward providing wrap-around outpatient health care to its clients. The 165,000 square feet of rehabilitated mill space on Jackson Street, just off of Downtown Lowell, already provides a range of medical care including pediatrics, eye and dental care, mental health supports, OB/family planning services and HIV screening and treatment.
The $1.2 million pharmacy project is being funded through board-approved reserves, while the $1.2 million walk-in center construction is funded with American Rescue Plan Act money.
Although 74% of its patients are on MassHealth , which provides health benefits to qualifying children, families, seniors and people with disabilities living in Massachusetts, its clinical and pharmacy services are available to the general public.
More than 37,000 people are registered to receive care through LCHC, which equates to 100,000 visits a year.
LCHC has a reputation of breaking ground on more than just construction projects. It pioneered the Metta Health Center in 2000 , one of the first health centers of its kind in the United States, originally founded to serve the needs of Lowell’s Southeast Asian community.
The center now serves as a healthcare sanctuary for refugees , asylum seekers and all who have been forcibly displaced from their homelands due to war, persecution or human rights abuses. LCHC provides integrated, multidisciplinary care to those survivors.
Threaded throughout LCHC’s mission, clinical work and physical spaces is the commitment to removing barriers to health care, said Dr. Alison Curcio, chief of the Patient Walk-In Center.
“[These projects] will provide seamless front- and back-end services,” she said. “Make it really easy for people to come in the day-of to be seen and get what they need and not have to wait.”
The projects are just the beginning of a reimaging of patient-centered health care, said Christopher Maher, director of security and public safety.
“We’re not resting on our laurels” he said. “What’s next? What else we can do?”
The new pharmacy is scheduled to open September 30, with the walk-in center shortly after. A redesigned lobby greeting area is also part of the renovation. During construction, LCHC’s current walk-in and pharmacy services are “100% operational,” said Cynthia Wood, director of facilities.
More in Local News

SUBSCRIBER ONLY
High school sports | kiley hogan a tremendous talent at plate, in circle for tyngsboro high.

Local News | UML, Mill City Grows celebrate greenhouse expansion

Local News | The Column: Lowell is still segregated by race

Crime and Public Safety | Arrest log

COMMENTS
Introduction. The objective of this literature review is to assess and determine the challenges and safety. issues that remote community health nurses encounter and the impact it may have on the health. equity gap in rural and remote areas. The literature disclosed that there is insufficient amount of.
Nursing theories focus on individual and community care and human relationships in unique contexts. One of these contexts is the community in which a theory-based systematic nursing practice process is warranted. This article describes a theory of Community Caring for Public Health Nursing (CCPHN), which is grounded in four nursing metaparadigms by Fawcett: persons, environment, health, and ...
Mary-Ann Taylor. The core values of community health nursing practice are rooted in the social determinants of health, health equity and social justice. Throughout the COVID-19 pandemic, community ...
Journal overview. The Journal of Community Health Nursing focuses on health care issues relevant to all aspects of community practice. This innovative publication provides well-researched and practical, up-to-date information to aid the nurse and other professionals who frequently make decisions and solve problems that occur in the community ...
Sometimes it does "take a village" to strengthen community resilience. This is the essence of the work of Duva et al. and Austin et al. They provide a blueprint for public health nursing interventions that built community resilience capacity against stress from psychological trauma and substance use during the COVID-19 pandemic.
The COVID-19 pandemic has reset the table for a dialogue about health equity, public health, and the future of nursing. Experts anticipated that payment reforms would lead to a much-needed increase in community and public health nursing. Despite calls for the profession of nursing to take a leadership role in addressing the social determinants of health and health equity, data show that jobs ...
The community needs assessment enables local stakeholders to work together in a collaborative process to analyze the community itself; offer suggestions and examples of change policies, systems and strategies; provide feedback to communities as they institute local changes for healthy living []; ensure resources allocation where there is the greatest health benefit; and adopting the principle ...
Help-Seeking Preferences and Influencing Factors Among Chinese Nurses Exposed to COVID-19: A Person-Centered Approach. Zhihong Wu et al. Article | Published online: 17 Feb 2024. View all latest articles. All journal articles featured in Journal of Community Health Nursing vol 38 issue 4.
community health nursing scholars are dissatisfied with the lack of conceptual frameworks useful in guiding community health nursing practices. Furthermore, Rafael states that Watson's human caring theory [29] is useful for PHNs to provide care in the community. Bent [30] asserted that caring is the key concept in nursing since it relates to ...
showed that community-based nursing provides direct access to health and treatment services through home visits and home care and accurate identication of the patients' needs [7]. Community-based nursing as a new eld in education and a new role of nurses in the community has attracted the attention of many nursing schools in dierent coun-
Methods. An explanatory sequential study was designed to select and study rural hospitals' engagement in community health programmes in a US Midwestern state, where 36% of the population live in a rural area and healthcare access continues to be an issue. 22 23 The study design is suitable for exploring emergent research questions and identifying underlying reasons and motivations for a ...
Community Health Nurse Educators and Disaster Nursing Education. Disasters can destroy lives within a matter of moments, often without warning. The incidence of disasters is on the rise in the United States, with the Federal Emergency. Management Agency (FEMA) reporting an average of 43 disasters declared annually.
There were only. 6 public health nurses, 3 of whom were designated as community health and public health nurses. The mean time working in primary health care was 16 years. Most nurses had been in their current role for 10 years, although some had worked in the same service for the last 30 years.
The FCN was introduced in 1998 by the WHO, aiming to extend the care of nurses from the individual to the family and community, and from hospital care to primary care services within each community. Many worldwide healthcare systems have undergone changes to implement and support the birth of this new paradigm of nursing care centred on health ...
Master the nurse's role in health promotion for Canadian populations and communities! Stanhope and Lancaster's Community Health Nursing in Canada, 4th Edition covers the concepts and skills you ...
Furthermore, community health nursing is facing particular challenges in the education, recruitment, and retention of nurses (Med-Emerg Inc., 2006). Though the demands of community health nursing are growing, the training and preparation to meet this demand is not;
Nursing Research Paper Topics. The impact of community health nursing interventions on reducing health disparities. Exploring the role of community health nurses in disaster response and recovery. Analyzing the effectiveness of school-based health clinics in improving student health outcomes. Investigating the barriers and facilitators of ...
Nursing provides the largest direct care and health intervention workforce and as such is a global health resource. Examinations of the International Classification for Nursing Practice (ICNP) have found that community nursing interventions directly address the identified themes related to gaps in healthcare, services, and system's coverage and continue to support advancements in ...
correction of the thesis with constant motivation and willingness to help all the time for the fruitful outcome of this study. With great pleasure and proud I express gratitude to Selvi.B.Lingeswari, M.Sc(N).,M.B.A.,M.Phil., Reader, Community Health Nursing Department, College of Nursing, Madras Medical
Theses/Dissertations from 2012. Mothers' Health and Health Behaviors that Influence Childhod Obesity Maternal BMI and Infant Feeding Methods, Mohamed Abdullah Alammari. Assessment of Selected University Students' Knowledge of Blood Donation and the Relationship with Intent to Donate Blood, Jeffrey Allerson.
Crafting a thesis on community health nursing is a complex process requiring extensive research, analysis, and clear writing. Students must select a relevant topic, conduct thorough research into academic literature and studies, and synthesize diverse information into a coherent narrative. The methodology and writing aspects present additional challenges, requiring precision in research design ...
Video (online) Consult the lists of relevant articles, books, theses, conference reports, and other scholarly sources on the topic 'Community health nursing.'. Next to every source in the list of references, there is an 'Add to bibliography' button. Press on it, and we will generate automatically the bibliographic reference to the chosen work ...
The underrepresentation of new graduates in community health nursing calls for directed efforts by community health nursing organizations and the university to improve the situation. Conscientious efforts need to be made to provide students with knowledge and information surrounding the roles of community health nurses and the opportunities for ...
2. Comprehensive cross-sector care models can reduce life threatening disparities. Felix Muchomba, Ph.D., M.P.H., assistant professor at Rutgers University School of Social Work, has been looking closely at local policy levers that influence the health of birthing people in New Jersey. Despite having one of the lowest poverty rates and highest ...
The new findings were based on an analysis of health insurance claims data from more than 4,000 hospitals in 49 states and Washington, D.C., from 2020 through 2022. It included both inpatient and ...
Long-term care facilities provide many services, both medical and personal care, to people who are unable to live without help. If you live in a nursing home, assisted living facility or other long-term care facility, you have a higher risk of getting an infection. There are steps you can take to reduce your risk:
Father's Day 5K supports community health DOVER — Registration is now open for Greater Seacoast Community Health's annual Father's Day 5K. This event to be held on Sunday, June 16 at 9 a.m ...
Cynthia Wood, Lowell Community Health Center's director of facilities shows the under-construction space of the new walk-in patient area and a new pharmacy in its first-floor lobby area.
Find out what's new. Find out what's new. More resources. About this tool. Learn more about this tool and what it can do for you. Resources & information ... Home Health Agency Quality Of Patient Care Star Rating See how home health agency quality of patient care star ratings are calculated, based on 8 care measures of process & outcome ...
State of the U.S. Health Care Workforce, 2023 . May 2024 . High-quality health care starts with a well-trained, ... A strong pipeline of new graduates is crucial to ensuring the future of the nursing profession. The ... Community health workers 26,892 24.5% 25.1% 20.5% 17.4% 12.5% :