Home — Essay Samples — Nursing & Health — Mental Health — Thesis Statement For Bipolar Depression

Thesis Statement for Bipolar Depression
- Categories: Mental Health
About this sample

Words: 973 |
Published: Mar 5, 2024
Words: 973 | Pages: 2 | 5 min read

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr. Karlyna PhD
Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
4 pages / 1951 words
4 pages / 1622 words
6 pages / 2752 words
1 pages / 614 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Mental Health
As a college student, I have experienced firsthand the challenges and pressures of navigating higher education while managing mental health issues. According to the American College Health Association, more than 60% of college [...]
Mental health has become an increasingly important topic that deserves attention and awareness. It is a critical aspect of overall health and well-being that affects individuals, communities, and society as a whole. The purpose [...]
It is estimated that one in four people worldwide will be affected by mental or neurological disorders at some point in their lives. The impact of mental health on individuals and society as a whole cannot be overstated. This [...]
In today's society, one of the most pressing social problems is the increasing rate of mental health disorders among college students. According to a study conducted by the American Psychological Association, nearly one in three [...]
Anxiety is a complex and often misunderstood mental health condition that affects millions of people worldwide. It can manifest in a variety of ways, from mild worry to debilitating panic attacks, and can have a significant [...]
A.A Milne’s 1977 show Winnie The Pooh secretly deals with the topic of mental disorders, whether it be the depression of Eeyore, or schizophrenic tendencies of Christopher Robin, many of the characters in this happy, upbeat kids [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Essay Service Examples Health Bipolar Disorder
Thesis Statement for Bipolar Disorder
Part 1. Literature Review and Ethical Considerations
Article one: treatment outcomes of an acute bipolar depressive episode with psychosis (marco antonio caldieraro md, phd1,2, et al., 2018), article two: psychopharmacological treatment of psychotic mania and psychotic bipolar depression compared to non-psychotic mania and non-psychotic bipolar depression (bjørklund et al., 2016. ).
- Proper editing and formatting
- Free revision, title page, and bibliography
- Flexible prices and money-back guarantee
Article 3: Anti-inflammatory agents in the treatments of bipolar depression: a systematic review and meta-analysis (Rosenblat JD et al., 2016).
Article 4: a re-examination of antidepressant treatment-emergent mania in bipolar disorders: evidence of gender differences (scott j. et al., 2017)..
- Bjørklund, L. B., Horsdal, H. T., Mors, O., Gasse, C., & Østergaard, S. D. (2017). Psychopharmacological treatment of psychotic mania and psychotic bipolar depression compared to non-psychotic mania and non-psychotic bipolar depression. Bipolar Disorders,19(6), 505-512. doi:10.1111/bdi.12504
- Caldieraro, M. A., Dufour, S., Sylvia, L. G., Gao, K., Ketter, T. A., Bobo, W. V., . . . Nierenberg, A. A. (2018). Treatment outcomes of the acute bipolar depressive episode with psychosis. Depression and Anxiety,35(5), 402-410. doi:10.1002/da.22716
- Ethical Principles of Psychologists and Code of Conduct. (n.d.). Retrieved June 6, 2019, from https://www.apa.org/ethics/code/
- Friedly, J., Bauer, Z., Comstock, B., Dimango, E., Ferrara, A., Huang, S., . . . Smith-Bindman, R. (2014). Challenges conducting comparative effectiveness research: The Clinical and Health Outcomes Initiative in Comparative Effectiveness (CHOICE) experience. Comparative Effectiveness Research,1. doi:10.2147/cer.s59136
- Lamictal vs. Depakote: Differences & Side Effects. (n.d.). Retrieved June 29, 2019, from https://www.rxlist.com/lamictal_vs_depakote/drugs-condition.htm#what_is_lamictal
- Nestor, P., & Schutt, R. K. (2015). Research methods in psychology: Investigating human behavior. Thousand Oaks, CA: SAGE Publications.
- Rosenblat, J. D., Kakar, R., Berk, M., Kessing, L. V., Vinberg, M., Baune, B. T., . . . Mcintyre, R. S. (2016). Anti-inflammatory agents in the treatment of bipolar depression: A systematic review and meta-analysis. Bipolar Disorders,18(2), 89-101. doi:10.1111/bdi.12373
- Scott, J., Brichant-Petitjean, C., Etain, B., Henry, C., Kahn, J., Azorin, J., . . . Bellivier, F. (2017). A re-examination of antidepressant treatment-emergent mania in bipolar disorders: Evidence of gender differences. Acta Psychiatrica Scandinavica,135(5), 479-488. doi:10.1111/acps.12728
Our writers will provide you with an essay sample written from scratch: any topic, any deadline, any instructions.
Cite this paper
Related essay topics.
Get your paper done in as fast as 3 hours, 24/7.
Related articles
Most popular essays
- Bipolar Disorder
- Human Brain
- Mental Illness
Mental health is a major challenge in the contemporary society. According to the World Health...
- Human Behavior
- Psychological Disorders
Psychology comes from the Greek words “psych” meaning soul and “ology” meaning logic, it...
The track I chose for this project was track two Psychological Influences of Abnormal Behavior....
“No excellent soul is exempt from a mixture of madness.” Aristotle. The link between creativity...
Bipolar disorder is a psychological issue described as a swing between mania and depression....
Bipolar disorder is a debilitating mental illness that causes extreme fluctuation in mood. One...
Approximately 1 in 5 people in the U.S. struggles with a mental illness every year, Hollywood is...
- Post Traumatic Stress Disorder
Bipolar disorder is a condition that has several diagnoses. These are, Bipolar Ⅰ, Bipolar Ⅱ,...
Bipolar disorder, today, can be defined as a brain disorder that causes changes in a person’s mood...
Join our 150k of happy users
- Get original paper written according to your instructions
- Save time for what matters most
Fair Use Policy
EduBirdie considers academic integrity to be the essential part of the learning process and does not support any violation of the academic standards. Should you have any questions regarding our Fair Use Policy or become aware of any violations, please do not hesitate to contact us via [email protected].
We are here 24/7 to write your paper in as fast as 3 hours.
Provide your email, and we'll send you this sample!
By providing your email, you agree to our Terms & Conditions and Privacy Policy .
Say goodbye to copy-pasting!
Get custom-crafted papers for you.
Enter your email, and we'll promptly send you the full essay. No need to copy piece by piece. It's in your inbox!

Understanding Bipolar Disorder: An In-Depth Essay
Imagine living in a world where emotions oscillate between exhilarating highs and crippling lows. Where one moment, you feel invincible, and the next, you are engulfed in a darkness so profound it seems suffocating. Welcome to the complex and enigmatic realm of bipolar disorder.
At some point in our lives, we all experience fluctuations in our moods. However, for individuals with bipolar disorder, these mood swings are extreme, unpredictable, and can have devastating consequences. It is a mental health condition that possesses the power to disrupt lives, strain relationships, and challenge society’s understanding.
In this in-depth essay, we will delve into the intricate facets of bipolar disorder, unraveling its definition, prevalence, and impact. We will explore the different types of the disorder and investigate the causes and risk factors that contribute to its development.
Furthermore, we will examine the symptoms associated with bipolar disorder and the diagnostic criteria used to identify it. We will highlight the challenges faced by individuals with bipolar disorder and the effects this condition can have on personal relationships. Additionally, we will confront the societal stigma and misunderstandings that permeate the public’s perception of bipolar disorder.
Treatment and management play a critical role in the lives of those with bipolar disorder, and we will explore the medication options, therapeutic approaches, and lifestyle changes that can provide support and stability.
To navigate such a vast and complex topic, it is important to understand how to approach writing an essay on bipolar disorder. We will discuss strategies for choosing a focus, structuring your essay, addressing controversial topics, and providing reliable sources.
This essay aims to shed light on the intricacies of bipolar disorder, debunk myths, and promote understanding and empathy. By gaining knowledge and insights into this often-misunderstood condition, we can facilitate a more inclusive and compassionate society. Join us on this journey of discovery as we strive to comprehend the multifaceted nature of bipolar disorder.
Overview of Bipolar Disorder
Bipolar disorder, also known as manic-depressive illness, is a chronic mental health condition that affects a person’s mood, energy levels, and ability to function effectively. It is characterized by extreme shifts in mood, ranging from manic episodes, where individuals experience heightened euphoria and energy, to depressive episodes, where they feel overwhelming sadness, hopelessness, and a lack of interest in activities.
What is Bipolar Disorder?
Bipolar disorder is a complex condition that involves various biological, genetic, and environmental factors. It affects approximately 2.8% of U.S. adults, according to the National Institute of Mental Health. The onset of bipolar disorder usually occurs in late adolescence or early adulthood, although it can manifest at any age.
During manic episodes, individuals may exhibit symptoms such as increased talkativeness, racing thoughts, impulsivity, inflated self-esteem, and a decreased need for sleep. They may engage in risky behaviors, such as excessive spending or substance abuse. On the other hand, depressive episodes are characterized by symptoms like persistent sadness, fatigue, sleep disturbances, difficulty concentrating, and thoughts of death or suicide.
Types of Bipolar Disorder
Bipolar disorder is further categorized into several subtypes:
1. Bipolar I Disorder: This is the most severe form of the illness, involving manic episodes lasting for at least seven days or requiring hospitalization. Depressive episodes lasting for two weeks or more often accompany these manic episodes.
2. Bipolar II Disorder: In this type, individuals experience recurring depressive episodes but have hypomanic episodes that are less severe than full-blown mania. These hypomanic episodes do not usually lead to significant impairment in functioning.
3. Cyclothymic Disorder: Cyclothymic disorder is a milder form of bipolar disorder where individuals have frequent, but less intense, mood swings. They experience hypomanic symptoms and depressive symptoms that persist for at least two years, with brief periods of stability.
Causes and Risk Factors
The exact cause of bipolar disorder is not fully understood. However, research suggests that a combination of genetic, biological, and environmental factors contribute to its development. Individuals with a family history of bipolar disorder or other mood disorders are at a higher risk.
Other factors that may influence the development of bipolar disorder include abnormal brain structure and function, neurotransmitter imbalances, hormonal imbalances, and high levels of stress. Substance abuse or traumatic experiences may also trigger the onset or exacerbation of symptoms.
Understanding the different types of bipolar disorder and the contributing factors can help demystify this complex condition. By recognizing the signs and seeking appropriate diagnosis and treatment, individuals with bipolar disorder can lead fulfilling lives and manage their symptoms effectively.
Symptoms and Diagnosis of Bipolar Disorder
Bipolar disorder is a complex mental health condition characterized by distinct symptoms that significantly impact an individual’s daily life. Accurate diagnosis of bipolar disorder is crucial to ensure appropriate treatment and support. In this section, we will explore common symptoms of bipolar disorder, the diagnostic criteria used for its identification, and how it is distinguished from other mental health conditions.
Common Symptoms of Bipolar Disorder
The symptoms of bipolar disorder can vary depending on the specific episode and its severity. During manic episodes, individuals often experience an intense euphoria, increased energy levels, and a heightened sense of self-esteem. They may engage in risky behavior, such as excessive spending or engaging in dangerous activities. Rapid speech, racing thoughts, and impulsivity are also commonly observed.
Conversely, depressive episodes are characterized by persistent feelings of sadness, hopelessness, and a loss of interest in previously enjoyed activities. Individuals may experience changes in appetite and sleep patterns, difficulties concentrating, and thoughts of self-harm or suicide. Fatigue, a lack of motivation, and a general feeling of emptiness are also common symptoms.
Diagnostic Criteria for Bipolar Disorder
To diagnose bipolar disorder, healthcare professionals refer to the criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). According to the DSM-5, the presence of manic, hypomanic, and depressive episodes is necessary for a bipolar disorder diagnosis.
For a diagnosis of bipolar I disorder, an individual must have experienced at least one manic episode, lasting for a minimum of seven days or requiring immediate hospitalization. Depressive episodes may or may not occur alongside the manic episodes.
In bipolar II disorder, individuals experience at least one major depressive episode and at least one hypomanic episode, which is characterized by milder manic symptoms that do not cause significant impairment in functioning.
Cyclothymic disorder, a milder form of bipolar disorder, is diagnosed when an individual experiences numerous periods of hypomanic symptoms and depressive symptoms over a two-year period.
Distinguishing Bipolar Disorder from other Mental Health Conditions
Differentiating bipolar disorder from other mental health conditions can be challenging due to overlapping symptoms. Depression alone, for example, may resemble the depressive episodes experienced by individuals with bipolar disorder. However, bipolar disorder is distinguished by the presence of manic or hypomanic episodes, which are not present in unipolar depression.
Other conditions such as borderline personality disorder and attention-deficit/hyperactivity disorder (ADHD) may exhibit symptoms similar to bipolar disorder, further complicating the diagnostic process. Thorough evaluation by a mental health professional is essential to accurately differentiate bipolar disorder from other conditions and develop an appropriate treatment plan.
Understanding the symptoms and diagnostic criteria of bipolar disorder helps in early identification and intervention, leading to improved outcomes for individuals living with this complex condition. Seeking professional help and support is crucial for accurate diagnosis and developing an effective management plan to mitigate the impact of bipolar disorder on daily life.
Impact of Bipolar Disorder on Individuals and Society
Bipolar disorder not only affects the lives of individuals diagnosed with the condition but also has a significant impact on their personal relationships, daily functioning, and society as a whole. In this section, we will explore the effects of bipolar disorder on personal relationships, the challenges faced by individuals with the condition, and societal stigma and misunderstandings surrounding bipolar disorder.
Effects of Bipolar Disorder on Personal Relationships
Living with bipolar disorder can strain personal relationships. The extreme mood swings, impulsivity, and erratic behavior exhibited during manic episodes can be confusing and distressing for partners, family members, and friends. Loved ones may struggle to understand the sudden changes in mood and energy levels, leading to strained communication and emotional instability within the relationship.
During depressive episodes, individuals with bipolar disorder may withdraw from social interactions, isolate themselves, and have difficulty expressing their needs and emotions. This can result in feelings of loneliness and isolation, further impacting the dynamics of personal relationships.
Challenges Faced by Individuals with Bipolar Disorder
Individuals with bipolar disorder face numerous challenges that affect their daily lives. The unpredictability of mood swings can make it difficult to maintain stable employment or pursue educational goals. Managing relationships, parenting responsibilities, and financial stability may also become more challenging due to the episodic nature of the condition.
Additionally, the presence of comorbid conditions, such as anxiety disorders or substance abuse, further compounds the difficulties faced by individuals with bipolar disorder. The stigma associated with mental illness may also create barriers in accessing proper treatment and support, exacerbating the challenges they encounter.
Societal Stigma and Misunderstandings
Despite growing awareness and understanding of mental health, societal stigma and misunderstandings surrounding bipolar disorder still persist. Many people hold misconceptions that individuals with bipolar disorder are simply “moody” or “unstable.” Such stigmatization can lead to social exclusion, discrimination, and a reluctance to seek help.
Moreover, the portrayal of bipolar disorder in popular culture and media often exaggerates the extreme behaviors associated with the condition, further perpetuating misconceptions and reinforcing stereotypes. This portrayal not only contributes to societal misunderstandings but also hinders individuals with bipolar disorder from openly discussing their experiences and seeking support.
Reducing stigma and promoting understanding are crucial steps towards creating a compassionate society that supports individuals with bipolar disorder. Educating the public about the true nature of bipolar disorder, highlighting the strengths and resilience of individuals living with the condition, and providing resources for support and education can help combat these misconceptions.
By acknowledging the impact of bipolar disorder on personal relationships, understanding the challenges faced by individuals with the condition, and challenging societal stigma, we can foster an environment that promotes empathy, acceptance, and support for those affected by bipolar disorder.
Treatment and Management of Bipolar Disorder
Effective management of bipolar disorder is essential for individuals to lead stable and fulfilling lives. Treatment typically involves a combination of medication, therapeutic approaches, and lifestyle changes. In this section, we will explore the different options available for treating bipolar disorder.
Medication Options for Bipolar Disorder
Medication plays a crucial role in managing bipolar disorder and stabilizing mood swings. Mood-stabilizing medications are commonly prescribed, such as lithium, which has proven efficacy in reducing the frequency and severity of manic and depressive episodes. Other mood stabilizers, such as valproate or lamotrigine, may also be prescribed.
Antipsychotic medications can be used to manage acute manic or depressive symptoms. They help regulate neurotransmitters in the brain, reducing the intensity of mood episodes. Antidepressant medications may be prescribed cautiously in combination with mood stabilizers to address depressive symptoms, considering the risk of triggering manic episodes.
It is important for individuals to work closely with healthcare professionals to find the most suitable medication regimen, as each individual’s response to medication varies. Regular monitoring and adjustments may be necessary to achieve optimal symptom management.
Therapeutic Approaches for Bipolar Disorder
Therapeutic interventions, such as psychotherapy, play an integral role in the treatment of bipolar disorder. Cognitive-behavioral therapy (CBT) can help individuals identify and modify negative thought patterns and behaviors associated with the disorder. Interpersonal and social rhythm therapy (IPSRT) focuses on stabilizing daily routines and addressing interpersonal issues that may trigger mood episodes.
Family-focused therapy involves educating and involving family members in the treatment process, enhancing communication, and providing support to both the individual with bipolar disorder and their loved ones. For those experiencing difficulties with medication adherence, psychoeducation can be beneficial in promoting understanding about the disorder and the importance of treatment.
Lifestyle Changes to Support Mental Health
In addition to medication and therapy, adopting certain lifestyle changes can be beneficial in managing bipolar disorder. Regular exercise has been shown to improve overall mood, reduce stress, and promote better sleep patterns. A balanced and nutritious diet can also contribute to physical and mental well-being.
Establishing a consistent sleep schedule is crucial, as disrupted sleep patterns can trigger mood episodes. Practicing good sleep hygiene, such as creating a calming bedtime routine and maintaining a comfortable sleep environment, is recommended.
Avoiding or minimizing the use of alcohol and recreational drugs is important, as these substances can negatively interact with medication and exacerbate mood symptoms. Building a strong support system, including seeking support from support groups or engaging in individual counseling, can provide valuable emotional support.
While bipolar disorder presents unique challenges, it is a treatable condition. By finding the right combination of medication, therapeutic approaches, and lifestyle changes, individuals with bipolar disorder can stabilize their moods, reduce the severity and frequency of episodes, and lead fulfilling lives. A comprehensive treatment approach that addresses the complex biological, psychological, and social aspects of the disorder is key to managing and mitigating the impact of bipolar disorder on daily functioning. Collaborating with healthcare professionals and accessing necessary support systems are vital steps towards successful management of this condition.
Writing an Essay on Bipolar Disorder
Writing an essay on bipolar disorder allows for a deeper exploration of this complex topic. However, it is important to approach the subject with sensitivity, accuracy, and a focus on providing valuable information. In this section, we will discuss key considerations when writing an essay on bipolar disorder.
Choosing a Focus for the Essay
Bipolar disorder encompasses a wide range of topics, so it is essential to narrow down your focus based on your interests and the scope of your essay. Consider exploring specific aspects of bipolar disorder, such as its impact on creativity, the relationship between bipolar disorder and substance abuse, or the experiences of individuals living with bipolar disorder.
Structuring the Essay
Organizing your essay in a logical manner is crucial for conveying information effectively. Consider using the introduction to provide an overview of bipolar disorder and set the context for the essay. Each subsequent section can delve deeper into specific aspects, such as symptoms, diagnosis, impact on relationships, treatment options, and societal understanding. Conclude your essay by summarizing key points and highlighting the significance of promoting awareness and support for individuals with bipolar disorder.
Addressing Controversial Topics
Bipolar disorder is a complex and multifaceted subject that may touch upon controversial areas. When discussing topics such as medication use, alternative therapies, or the link between creativity and bipolar disorder, it is important to present balanced viewpoints supported by credible sources. Acknowledge differing perspectives and engage in evidence-based discussions while considering potential biases or limitations in existing research.
Providing Reliable Sources
To ensure the credibility and accuracy of your essay, consult reputable sources that provide evidence-based information on bipolar disorder. Peer-reviewed academic journals, government health websites, and renowned mental health organizations are reliable sources of information. Remember to properly cite your sources using a recognized citation style, such as APA or MLA, to give credit to the original authors and avoid plagiarism.
Writing an essay on bipolar disorder provides an opportunity to educate and inform readers about this complex condition. By selecting a focused topic, structuring your essay logically, addressing controversies with balanced viewpoints, and using reliable sources, you can create an informative and compelling piece that contributes to understanding and promoting empathy for those with bipolar disorder. It is imperative to approach the topic with sensitivity and respect, recognizing the impact it has on individuals, their relationships, and society as a whole.
In conclusion, bipolar disorder is a complex and multifaceted mental health condition that significantly impacts individuals and society as a whole. This in-depth essay has provided a comprehensive understanding of bipolar disorder, covering various aspects such as its definition, prevalence, and impact on personal relationships. We explored the different types of bipolar disorder and the causes and risk factors associated with its development.
Furthermore, we delved into the symptoms and diagnostic criteria used for identifying bipolar disorder while highlighting the importance of distinguishing it from other mental health conditions. The essay also shed light on the challenges faced by individuals with bipolar disorder, including the strain on personal relationships and the societal stigma surrounding the condition.
The treatment and management of bipolar disorder were extensively discussed, emphasizing the significance of medication options, therapeutic approaches, and lifestyle changes to support mental health. By adopting a comprehensive treatment approach, individuals with bipolar disorder can stabilize their moods and lead fulfilling lives.
Moreover, this essay provided insights into writing an essay on bipolar disorder, guiding readers on choosing a focus, structuring the essay effectively, addressing controversial topics, and providing reliable sources. By following these principles, writers can effectively promote awareness and understanding of bipolar disorder.
It is crucial to recognize the impact of bipolar disorder and combat societal misunderstandings and stigmas. By fostering empathy, educating the public, and providing support systems, we can create an inclusive and compassionate society that supports and empowers individuals living with bipolar disorder.
In conclusion, understanding bipolar disorder is integral to promoting mental health and fostering a more informed and accepting society. By spreading knowledge, reducing stigma, and advocating for appropriate support and resources, we can work towards creating a world where individuals with bipolar disorder can lead fulfilling and meaningful lives.
Similar Posts

The Link Between Bipolar Disorder and Messy House: Understanding Manic Cleaning
Messy houses can be a common sight, but have you ever wondered why some individuals seem to have an intense need to clean and organize their homes? Welcome to the intriguing world of manic cleaning and…

Understanding the Relationship between OCD and Bipolar Disorder
Are you familiar with the nagging voice in your head that insists you check if the front door is locked, over and over again? Or the rollercoaster of emotions that seem to have a life of…

Understanding Bipolar Disorder in Nurses: Challenges and Support
Imagine working in an environment that requires constant attention, critical decision-making, and unwavering compassion. Now, add the challenges of managing mood swings, unpredictable behavior, and the overwhelming emotional rollercoaster that comes with bipolar disorder. This is…
Understanding F31.81: Bipolar 2 DSM 5 Code Explained
Imagine experiencing extreme mood swings, from periods of euphoria and energy to deep depression and lethargy. This roller coaster of emotions can disrupt your daily life and relationships. Welcome to the world of Bipolar Disorder Type…

Understanding Lamictal Dreams and Their Connection to Bipolar Disorder
Imagine entering a fantastical realm where the boundaries of reality fade away, where vivid images dance across the canvas of your mind. Dreams have long fascinated humanity, offering a glimpse into the depths of our subconscious…

Can a Therapist Diagnose Bipolar? Exploring the Role of Therapists in Bipolar Disorder Diagnosis
Imagine living with extreme mood swings that are so intense and unpredictable, they disrupt every aspect of your life. One moment you are on top of the world, full of energy and grandiose plans. The next,…
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Bipolar Disord

The challenges of living with bipolar disorder: a qualitative study of the implications for health care and research
Eva f. maassen.
1 Athena Institute, Faculty of Earth and Life Sciences, VU University Amsterdam, Boelelaan 1085, 1081HV Amsterdam, Netherlands
2 Altrecht Institute for Mental Health Care, Nieuwe Houtenseweg 12, 3524 SH Utrecht, Netherlands
Barbara J. Regeer
Eline j. regeer, joske f. g. bunders, ralph w. kupka.
3 Amsterdam Public Health Research Institute, Amsterdam UMC, Vrije Universiteit Amsterdam, Psychiatry, De Boelelaan 1117, Amsterdam, Netherlands
In mental health care, clinical practice is often based on the best available research evidence. However, research findings are difficult to apply to clinical practice, resulting in an implementation gap. To bridge the gap between research and clinical practice, patients’ perspectives should be used in health care and research. This study aimed to understand the challenges people with bipolar disorder (BD) experience and examine what these challenges imply for health care and research needs.
Two qualitative studies were used, one to formulate research needs and another to formulate healthcare needs. In both studies focus group discussions were conducted with patients to explore their challenges in living with BD and associated needs, focusing on the themes diagnosis, treatment and recovery.
Patients’ needs are clustered in ‘disorder-specific’ and ‘generic’ needs. Specific needs concern preventing late or incorrect diagnosis, support in search for individualized treatment and supporting clinical, functional, social and personal recovery. Generic needs concern health professionals, communication and the healthcare system.
Patients with BD address disorder-specific and generic healthcare and research needs. This indicates that disorder-specific treatment guidelines address only in part the needs of patients in everyday clinical practice.
Bipolar disorder (BD) is a major mood disorder characterized by recurrent episodes of depression and (hypo)mania (Goodwin and Jamison 2007 ). According to the Diagnostic and Statistical Manual 5 (DSM-5), the two main subtypes are BD-I (manic episodes, often combined with depression) and BD-II (hypomanic episodes, combined with depression) (APA 2014 ). The estimated lifetime prevalence of BD is 1.3% in the Dutch adult population (de Graaf et al. 2012 ), and BD is associated with high direct (health expenditure) and indirect (e.g. unemployment) costs (Fajutrao et al. 2009 ; Michalak et al. 2012 ), making it an important public health issue. In addition to the economic impact on society, BD has a tremendous impact on patients and their caregivers (Granek et al. 2016 ; Rusner et al. 2009 ). Even between mood episodes, BD is often associated with functional impairment (Van Der Voort et al. 2015 ; Strejilevich et al. 2013 ), such as occupational or psychosocial impairment (Huxley and Baldessarini 2007 ; MacQueen et al. 2001 ; Yasuyama et al. 2017 ). Apart from symptomatic recovery, treatment can help to overcome these impairments and so improve the person’s quality of life (IsHak et al. 2012 ).
Evidence Based Medicine (EBM), introduced in the early 1990s, is a prominent paradigm in modern (mental) health care. It strives to deliver health care based on the best available research evidence, integrated with individual clinical expertise (Sackett et al. 1996 ). EBM was introduced as a new paradigm to ‘de - emphasize intuition’ and ‘ unsystematic clinical experience’ (Guyatt et al. 1992 ) (p. 2420). Despite its popularity in principle (Barratt 2008 ), EBM has also been criticized. One such criticism is the ignorance of patients’ preferences and healthcare needs (Bensing 2000 ). A second criticism relates to the difficulty of adopting evidence-based treatment options in clinical practice (Bensing 2000 ), due to the fact that research outcomes measured in ‘the gold standard’ randomized-controlled trials (RCTs) seldom correspond to the outcomes clinical practice seeks and are not responsive to patients’ needs (Newnham and Page 2010 ). Moreover, EBM provides an overview on population level instead of individual level (Darlenski et al. 2010 ). Thus, adopting research evidence in clinical practice entails difficulties, resulting in an implementation gap.
To bridge the gap between research and clinical practice, it is argued that patients’ perspectives should be used in both health care and research. Patients have experiential knowledge about their illness, living with it in their personal context and their care needs (Tait 2005 ). This is valuable for both clinical practice and research as their knowledge complements that of health professionals and researchers (Tait 2005 ; Broerse et al. 2010 ; Caron-Flinterman et al. 2005 ). This source of knowledge can be used in the process of translating evidence into clinical practice (Schrevel 2015 ). Moreover, patient participation can enhance the clinical relevance of and support for research and the outcomes in practice (Abma and Broerse 2010 ). Hence, it is argued that these perspectives should be explicated and integrated into clinical guidelines, clinical practice, and research (Misak 2010 ; Rycroft-Malone et al. 2004 ).
Given the advantages of including patients’ perspectives, patients are increasingly involved in healthcare services (Bagchus et al. 2014 ; Larsson et al. 2007 ), healthcare quality (e.g. guideline development) (Pittens et al. 2013 ) and health-related research (e.g. agenda setting, research design) (Broerse et al. 2010 ; Boote et al. 2010 ; Elberse et al. 2012 ; Teunissen et al. 2011 ). However, patients’ perspectives on health care and on research are often studied separately. We argue that to be able to provide care focused on the patients and their needs, care and research must closely interact.
We hypothesize that the challenges BD patients experience and the associated care and research needs are interwoven, and that combining them would provide a more comprehensive understanding. We hypothesize that this more comprehensive understanding would help to close the gap between clinical practice and research. For this reason, this study aims to understand the challenges people with BD experience and examine what these challenges imply for healthcare and research needs.
To understand the challenges and needs of people with BD, we undertook two qualitative studies. The first aimed to formulate a research agenda for BD from a patient’s perspective, by gaining insights into their challenges and research needs. A second study yielded an understanding of the care needs from a patient’s perspective. In this article, the results of these two studies are combined in order to investigate the relationship between research needs and care needs. Challenges are defined as ‘difficulties patients face, due to having BD’. Care needs are defined as that what patients ‘desire to receive from healthcare services to improve overall health’ (Asadi-Lari et al. 2004 ) (p. 2). Research needs are defined as that what patients ‘desire to receive from research to improve overall health’.
Study on research needs
In this study, mixed-methods were used to formulate research needs from a patient’s perspective. First six focus group discussions (FGDs) with 35 patients were conducted to formulate challenges in living with BD and hopes for the future, and to formulate research needs arising from these difficulties and aspirations. These research needs were validated in a larger sample (n = 219) by means of a questionnaire. We have reported this study in detail elsewhere (Maassen et al. 2018 ).
Study on care needs
This study was part of a nationwide Dutch project to generate a practical guideline for BD: a translation of the existing clinical guideline to clinical practice, resulting in a standard of care that patients with BD could expect. The practical guideline (Netwerk Kwaliteitsontwikkeling GGZ 2017 ) was written by a taskforce comprising health professionals, patients. In addition to the involvement of three BD patients in the taskforce, a systematic qualitative study was conducted to gain insight into the needs of a broader group of patients.
Participants and data collection
To formulate the care needs of people with BD, seven FGDs were conducted, with a total of 56 participants, including patients (n = 49) and caregivers (n = 9); some participants were both patient and caregiver. The inclusion criteria for patients were having been diagnosed with BD, aged 18 years or older and euthymic at time of the FGDs. Inclusion criteria for caregivers were caring for someone with BD and aged 18 years or older. To recruit participants, a maximum variation sampling strategy was used to collect a broad range of care needs (Kuper et al. 2008 ). First, all outpatient clinics specialized in BD affiliated with the Dutch Foundation for Bipolar Disorder (Dutch: Kenniscentrum Bipolaire Stoornissen) were contacted by means of an announcement at regular meetings and by email if they were interested to participate. From these outpatient clinics, patients were recruited by means of flyers and posters. Second, patients were recruited at a quarterly meeting of the Dutch patient and caregiver association for bipolar disorder. The FGDs were conducted between March and May 2016.
The FGDs were designed to address challenges experienced in BD health care and areas of improvement for health care for people with BD. The FGDs were structured by means of a guide and each session was facilitated by two moderators. The leading moderator was either BJR or EFM, having both extensive experience with FGD’s from previous studies. The first FGD explored a broad range of needs. The subsequent six FGDs aimed to gain a deeper understanding of these care needs, and were structured according to the outline of the practical guideline (Netwerk Kwaliteitsontwikkeling GGZ 2017 ). Three chapters were of particular interest: diagnosis, treatment and recovery. These themes were discussed in the FGDs, two in each session, all themes three times in total. Moreover, questions on specific aspects of care formulated by the members of the workgroup were posed. The sessions took 90–120 min. The FGDs were audiotaped and transcribed verbatim. A summary of the FGDs was sent to the participants for a member check.
Data analysis
To analyze the data on challenges and needs, a framework for thematic analysis to identify, analyze and report patterns (themes) in qualitative data sets by Braun and Clarke ( 2006 ) was used. First, we familiarized ourselves with the data by carefully reading the transcripts. Second, open coding was used to derive initial codes from the data. These codes were provided to quotes that reflected a certain challenge or care need. Third, we searched for patterns within the codes reflecting challenges and within those reflecting needs. For both challenges and needs, similar or overlapping codes were clustered into themes. Subsequently, all needs were categorized as ‘specific’ or ‘generic’. The former are specific to BD and the latter are relevant for a broad range of psychiatric illnesses. Finally, a causal analysis provided a clear understanding of how challenges related to each other and how they related to the described needs.
To analyze the data on needs regarding recovery, four domains were distinguished, namely clinical, functional, social and personal recovery (Lloyd et al. 2008 ; van der Stel 2015 ). Clinical recovery refers to symptomatic remission; functional recovery concerns recovery of functioning that is impaired due to the disorder, particularly in the domain of executive functions; social recovery concerns the improvement of the patient’s position in society; personal recovery concerns the ability of the patient to give meaning to what had happened and to get a grip on their own life. The analyses were discussed between BR and EM. The qualitative software program MAX QDA 11.1.2 was used (MaxQDA).
Ethical considerations
According to the Medical Ethical Committee of VU University Medical Center, the Medical Research Involving Human Subjects Act does not apply to the current study. All participants gave written or verbal informed consent regarding the aim of the study and for audiotaping and its use for analysis and scientific publications. Participation was voluntary and participants could withdraw from the study at any time. Anonymity was ensured.
This section is in three parts. The first presents the participants’ characteristics. The second presents the challenges BD patients face, derived from both studies, and the disorder-specific care and research needs associated with these challenges. The third part describes the generic care needs that patients formulated.
Characteristics of the participants
In the study on care needs, 56 patients and caregivers participated. The mean age of the participants was 52 years (24–75), of whom 67.8% were women. The groups varied from four to sixteen participants, and all groups included men and women. Of all participants 87.5% was diagnosed with BD, of whom 48.9% was diagnosed with BD I. 3.5% was both caregivers and diagnosed with BD. Of 4 patients the age was missing, and from 6 patients the bipolar subtype.
Despite the fact that participants acknowledge the inevitable diagnostic difficulties of a complex disorder like BD, in both studies they describe a range of challenges in different phases of the diagnostic process (Fig. 1 ). Patients explained that the general practitioner (GP) and society in general did not recognize early-warning signs and mood swings were not well interpreted, resulting in late or incorrect diagnosis. Patients formulated a need for more research on what early-warning signs could be and on how to improve GPs’ knowledge about BD. Formulated care needs were associated with GPs using this knowledge to recognize early-warning signs in individual patients. One participant explained that certain symptoms must be noticed and placed in the right context:
I call it, ‘testing overflow of ideas’. [….] When it happens for the first time you yourself do not recognize it. Someone else close to you or the health professional, who is often not involved yet, must signal it. (FG6)

Challenges with diagnosis (squares) including relating research needs (white circles) and care needs (grey circles). (1): mentioned in study on research needs; (2): mentioned in study on care needs. Dotted lines: division of challenges into sub challenges. Arrows: causal relation between challenges
Moreover, these challenges are associated with the need to pay attention to family history and to use a multidisciplinary approach to diagnosis to benefit from multiple perspectives. The untimely recognition of early symptoms also results in another challenge: inadequate referral to the right specialized health professional. After referral, people often face a waiting list, again causing delay in the diagnostic process. These challenges result in the need for research on optimal referral systems and the care need for timely referral. One participant described her process after the GP decided to refer her:
But, yes, at that moment the communication wasn’t good at all. Because the general practitioner said: ‘she urgently has to be seen by someone’. Subsequently, three weeks went by, until I finally arrived at depression [department]. And at that department they said: ‘well, you are in the wrong place, you need to go to bipolar [department ]’. (FG1)
The challenge of being misdiagnosed is associated with the need to be able to ask for a second opinion and to have a timely and thorough diagnosis. On the one hand, it is important for patients that health professionals quickly understand what is going on, on the other hand that health professionals take the time to thoroughly investigate the symptoms by making several appointments.
From both studies, two main challenges related to the treatment of BD were derived (Fig. 2 ). The first is finding appropriate and satisfactory treatment. Participants explained that it is difficult to find the right medication and dosage that is effective and has acceptable side-effects. One participant illustrates:
I think, at one point, we have to choose, either overweight or depressed. (FG1)

Challenges with treatment (squares) including relating research needs (white circles) and care needs (grey circles). (1): mentioned in study on research needs; (2): mentioned in study on care needs. Dotted lines: division of challenges into sub challenges. Arrows: causal relation between challenges
Some participants said that they struggle with having to use medication indefinitely, including the associated medical checks. The difficult search for the right pharmacological treatment results in the need for research on long-term side-effects, on the mechanism of action of medicine and on the development of better targeted medication with fewer adverse side-effects. In care, patients would appreciate all the known information on the side-effects and intended effects. One participant explained the importance of being properly informed about medication:
I don’t read anything [about medication], because then I wouldn’t dare taking it. But I do think, when you explain it well, the advantages, the disadvantages, the treatment, the idea behind it, that would help a lot in compliance. (FG1)
A second aspect is the challenge of finding non-pharmacological therapies that fit patients’ needs. They said they and the health professionals often do not know which non-pharmacological therapies are available and effective:
But we found the carefarm ourselves 1 [….]. You have to search for yourself completely. Yes, I actually hoped that that would be presented to you, like: ‘this would be something for you’. (FG3)
Participants mentioned a variety of non-pharmacological therapies they found useful, namely cognitive behavior therapy (CBT), EMDR, running therapy, social-rhythm training, light therapy, mindfulness, psychotherapy, psychoeducation, and training in living with mood swings. They formulated the care need to receive an overview of all available treatment options in order to find a treatment best suited to their needs. They would appreciate research on the effectiveness of non-pharmacological treatments.
A third aspect within this challenge is finding the right balance between non-pharmacological and pharmacological treatment. Participants differed in their opinion about the need for medication. Whereas some participants stated that they need medication to function, others pointed out that they found non-pharmacological treatments effective, resulting in less or no medication use. They explained that the preferred balance can also change over time, depending on their mood. However, they experience a dominant focus on pharmacological treatment by the health professionals. To address this challenge, patients need support in searching for an appropriate balance.
Next to the challenge of finding appropriate and satisfactory treatment, a second treatment-related challenge is hospitalization. Participants often had a traumatic experience, due to seclusion, the authoritarian attitudes of clinical staff, and not involving their family. Patients therefore found it important to try preventing being hospitalized, for example by means of home treatment, which some participants experienced positively. Despite the challenges relating to hospitalization, participants did acknowledge that in some cases it cannot be avoided, in which case they urged for close family involvement, open communication and being treated by their own psychiatrist. Still, in the study on research needs, hospitalization did not emerge as an important research theme.
In both studies, participants described challenges in all four domains of recovery: clinical, functional, social and personal (Fig. 3 ). In relation to clinical recovery, participants struggled with the symptoms of mood episodes, the psychosis and the fear of a future episode. In contrast, some participants mentioned that they sometimes miss the hypomanic state they had experienced previously due to effective medical treatment. In the domain of functional recovery, participants contended with having to function below their educational level due to residual symptoms, such as cognitive problems, due to the importance of preventing stress in order to reduce the risk of a new episode, and because of low energy levels. This leads to the care need that health professionals should pay attention to the level of functioning of their patients.

Challenges with recovery (squares) including relating research needs (white circles) and care needs (grey circles). (1): mentioned in study on research needs; (2): mentioned in study on care needs. Dotted lines: division of challenges into sub challenges. Arrows: causal relation between challenges
In the domain of social recovery, participants described challenges with maintaining friendships, due to stigma, being unpredictable and with deciding when to disclose the disorder. The latter resulted in the care need for tips on disclosure. Moreover, patients experienced challenges with reintegration to work, due to colleagues’ lack of understanding, problems with functioning during an episode, the complicating policy of the (Dutch) Employee Insurance Agency 2 in relation to the fluctuating course of BD and the negative impact of stress. These challenges are associated with the care need that health professionals should pay attention to work and the need for research on how to improve the Social Security Agency’s policy.
For their personal recovery, participants struggled with acceptance of the disorder, due to shame, stigma, having to live by structured rules and disciplines, and the chronic nature of BD. This results in care needs for grief counselling and attention to acceptance and the need for research on the impact of being diagnosed with BD. Limited understanding within society also causes problems with acceptance, corresponding with the care need for education for caregivers and for research on how to increase social acceptance. Another challenge in personal recovery was discovering what recovery means and what constitute meaningful daily activities. Patients appreciated the support of health professionals in this area. One participant described the difficult search for the meaning of recovery:
I have been looking to recover towards the situation [before diagnosis] for a long time; that I could do what I always did and what I liked. But then I was confronted with the fact that I shouldn’t expect that to happen, or only with a lot of effort. (…) Then you start thinking, now what? A compromise. I don’t want to call that recovery, but it is a recovered, partly accepted, situation. But it is not recovery as I expected it to be. (FG5)
In general, participants considered frequent contact with a nurse or psychiatrist supportive, to help them monitor their mood and help them find (efficient) self-management strategies. Most participants appreciated the involvement of caregivers in the treatment and contact with peers.
Generic care needs
We have described BD-specific needs, but patients mentioned also mentioned several generic care needs. The latter are clustered into three categories. The first concerns the health professionals . Participants stressed the importance of a good health professional, who carefully listens, takes time, and makes them feel understood, resulting in a sense of connection. Furthermore, a good health professional treats beyond the guideline, and focuses on the needs of the individual patient. When there is no sense of connection, it should be possible to change to another health professional. The second category concerns communication between the patient and the health professional . Health professionals should communicate in an open, honest and clear way both in the early diagnostic phase and during treatment. Open communication facilitates individualized care, in which the patient is involved in decision making. In addition, participants wanted to be treated as a person, not as a patient, and according to a strength-based approach. The third category concerns needs at the level of the healthcare system . Participants struggled with the availability of the health professionals and preferred access to good care 24/7 and being able to contact their health professional quickly when necessary. Currently, according to the participants, the care system is not geared to the mood swings of BD, because patients often faced waiting lists before they could see a health professional.
Is adequate treatment also having a number from a mental health institution you can always call when you are in need, that you can go there? And not that you can go in three weeks, but on a really short notice. So at least a phone call. (FG3)
Participants were often frustrated by the limited collaboration between health professionals, within their own team, between departments of the organization, and between different organizations, including complementary health professionals. They would appreciate being able to merge their conventional and complementary treatment, with greater collaboration among the different health professionals. Furthermore, they would like continuity of health professionals as this improves both the diagnostic phase and treatment, and because that health professional gets to know the patient.
We hypothesized that research and care needs of patients are closely intertwined and that understanding these, by explicating patients’ perspectives, could contribute to closing the gap between research and care. Therefore, this study aimed to understand the challenges patients with BD face and examine what these imply for both healthcare and research. In the study on needs for research and in the study on care needs, patients formulated challenges relating to receiving the correct diagnosis, finding the right treatment, including the proper balance between non-pharmacological and pharmacological treatment, and to their individual search for clinical, functional, social and personal recovery. The formulated needs in both studies clearly reflected these challenges, leading to closely corresponding needs. Another important finding of our study is that patients not only formulate disorder-specific needs, but also many generic needs.
The needs found in our study are in line with the current literature on the needs of patients with BD, namely for more non-pharmacological treatment (Malmström et al. 2016 ; Nestsiarovich et al. 2017 ), timely recognition of early-warning signs and self-management strategies to prevent a new episode (Goossens et al. 2014 ), better information on treatment and treatment alternatives (Malmström et al. 2016 ; Neogi et al. 2016 ) and coping with grief (Goossens et al. 2014 ). Moreover, the need for frequent contact with health professionals, being listened to, receiving enough time, shared decision-making on pharmacological treatment, involving caregivers (Malmström et al. 2016 ; Fisher et al. 2017 ; Skelly et al. 2013 ), and the urge for better access to health care and continuity of health professionals (Nestsiarovich et al. 2017 ; Skelly et al. 2013 ) are confirmed by the literature. Our study added to this set of literature by providing insights in patients’ needs in the diagnostic process and illustrating the interrelation between research needs and care needs from a patient’s perspective.
The generic healthcare needs patients addressed in this study are clustered into three categories: the health professional , communication between the patient and the health professional and the health system. These categories all fit in a model of patient-centered care (PCC) by Maassen et al. ( 2016 ) In their review, patients’ perspectives on good care are compared with academic perspectives of PCC and a model of PCC is created comprising four dimensions: patient, health professional, patient – professional interaction and healthcare organization. All the generic needs formulated in this study fit into these four dimensions. The need to be treated as a person with strengths fits the dimension ‘patient’, and the need for a good health professional who carefully listens, takes time and makes them feel understood, resulting in a good connection with the professional, fits the dimension ‘health professional’ of this model. Furthermore, patients in this study stressed the importance of open communication in order to provide individualized care, which fits the dimension of ‘patient–professional interaction’. The urge for better access to health care, geared to patients’ mood swings and the need for better collaboration between health professionals and continuity of health professionals fits the dimension of ‘health care organization’ of the model. This study confirms the findings from the review and contributes to the literature stressing the importance of a patient-centered care approach (Mills et al. 2014 ; Scholl et al. 2014 ).
In the prevailing healthcare paradigm, EBM, the best available evidence should guide treatment of patients (Sackett et al. 1996 ; Darlenski et al. 2010 ). This evidence is translated into clinical and practical guidelines, which thus facilitate EBM and could be used as a decision-making tool in clinical practice (Skelly et al. 2013 ). For many psychiatric disorders, treatment is based on such disorder - specific clinical and practical guidelines. However, this disease-focused healthcare system has contributed to its fragmented nature Stange ( 2009 ) argues that this fragmented care system has expanded without the corresponding ability to integrate and personalize accordingly. We argue that acknowledging that disorder - specific clinical and practical guidelines address only parts of the care needs is of major importance, since otherwise important aspects of the patients’ needs will be ignored. Because there is an increasing acknowledgement that health care should be responsive to the needs of patients and should change from being disease-focused towards being patient-focused (Mead and Bower 2000 ; Sidani and Fox 2014 ), currently in the Netherlands generic practical guidelines are written on specific care themes (e.g. co-morbidity, side-effects, daily activity and participation). These generic practical guidelines address some of the generic needs formulated by the patients in our study. We argue that in addition to disorder-specific guidelines, these generic practical guidelines should increasingly be integrated into clinical practice, while health professionals should continuously be sensitive to other emerging needs. We believe that an integration of a disorder-centered and a patient-centered focus is essential to address all needs a patient.
Strengths, limitations and future research
This study has several strengths. First, it contributes to the literature on the challenges and needs of patients with BD. Second, the study is conducted from a patient’s perspective. Moreover, addressing this aim by conducting two separate studies enabled us to triangulate the data.
This study also has several limitations. First, this study reflects the challenges, care needs and research needs of Dutch patient with BD and caregivers. Despite the fact that a maximum variation sampling strategy was used to derive a broad range of challenges and needs throughout the Netherlands, the Dutch setting of the study may limit the transferability to other countries. To understand the overlap and differences between countries, similar research should be conducted in other contexts. Second, given the design of the study, we could not differentiate between patients and caregivers since they participated together in the FGDs. More patients than caregivers participated in the study. For a more in-depth understanding of the challenges and needs faced by caregivers, in future research separate FGDs should be conducted. Third, due to the fixed outline of the practical guideline used to conduct the FGDs, only the healthcare needs for diagnosis, treatment and recovery of BD are studied. Despite the fact that these themes might cover a broad range of health care, it could have resulted in overlooking certain needs in related areas of well-being. Therefore, future research should focus on needs outside of these themes in order to provide a complete set of healthcare needs.
Patients and their caregivers face many challenges in living with BD. Our study contributes to the literature on care and research needs from a patient perspective. Needs specific for BD are preventing late or incorrect diagnosis, support in search for individualized treatment, and supporting clinical, functional, social and personal recovery. Generic healthcare needs concern health professionals, communication and the healthcare system. This explication of both disorder-specific and generic needs indicates that clinical practice guidelines should address and integrate both in order to be responsive to the needs of patients and their caregivers.
Authors’ contributions
EFM designed the study, contributed to the data collection, managed the analysis and wrote the first draft of the manuscript. BJR designed the study and contributed to the data collection, data analysis, and writing of the manuscript. JFGB contributed to the study design and critical revision of the manuscript. EJR contributed to the study conception and critical revision of the manuscript. RWK contributed to the study design, acquisition of data, and critical revision of the manuscript. All authors contributed to the final manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
The authors received no financial support for the research.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
1 Care farm: farms that combine agriculture and services for people with disabilities (Iancu 2013 ). These farms are used as interventions in mental care throughout Europe and the USA to facilitate recovery (Iancu et al. 2014 ).
2 A government agency involved in the implementation of employee insurance and providing labor market and data services.
Contributor Information
Eva F. Maassen, Phone: +31 (0)6 13861504, Email: [email protected] .
Barbara J. Regeer, Email: [email protected] .
Eline J. Regeer, Email: [email protected] .
Joske F. G. Bunders, Email: [email protected] .
Ralph W. Kupka, Email: [email protected] .
- Abma T, Broerse J. Patient participation as dialogue: setting research agendas. Health Expect. 2010; 13 (2):160–173. doi: 10.1111/j.1369-7625.2009.00549.x. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- APA . Beknopt overzicht van de criteria (DSM-5). Nederlands vertaling van de Desk Reference to the Diagnostic Criteria from DSM-5. Amsterdam: Boom; 2014. [ Google Scholar ]
- Asadi-Lari M, Tamburini M, Gray D. Patients’ needs, satisfaction, and health related quality of life: towards a comprehensive model. Health Qual Life Outcomes. 2004; 2 :1–15. doi: 10.1186/1477-7525-2-32. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bagchus C, Dedding C, Bunders JFG. “I”m happy that I can still walk’—participation of the elderly in home care as a specific group with specific needs and wishes. Health Expect. 2014; 18 (6):1–9. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Barratt A. Evidence based medicine and shared decision making: the challenge of getting both evidence and preferences into health care. Patient Educ Couns. 2008; 73 (3):407–412. doi: 10.1016/j.pec.2008.07.054. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bensing J. Bridging the gap. The separate worlds of evidence-based medicine and patient-centered medicine. Patient Educ Couns. 2000; 39 :17–25. doi: 10.1016/S0738-3991(99)00087-7. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Boote J, Baird W, Beecroft C. Public involvement at the design stage of primary health research: a narrative review of case examples. Health Policy. 2010; 95 (1):10–23. doi: 10.1016/j.healthpol.2009.11.007. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006; 3 (2):77–101. doi: 10.1191/1478088706qp063oa. [ CrossRef ] [ Google Scholar ]
- Broerse J, Zweekhorst M, van Rensen A, de Haan M. Involving burn survivors in agenda setting on burn research: an added value? Burns. 2010; 36 (2):217–231. doi: 10.1016/j.burns.2009.04.004. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Caron-Flinterman JF, Broerse JEW, Bunders JFG. The experiential knowledge of patients: a new resource for biomedical research? Soc Sci Med. 2005; 60 (11):2575–2584. doi: 10.1016/j.socscimed.2004.11.023. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Darlenski RB, Neykov NV, Vlahov VD, Tsankov NK. Evidence-based medicine: facts and controversies. Clin Dermatol. 2010; 28 (5):553–557. doi: 10.1016/j.clindermatol.2010.03.015. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- de Graaf R, ten Have M, van Gool C, van Dorsselaer S. Prevalence of mental disorders and trends from 1996 to 2009. Results from the Netherlands Mental Health Survey and Incidence Study-2. Soc Psychiatry Psychiatr Epidemiol. 2012; 47 (2):203–213. doi: 10.1007/s00127-010-0334-8. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Elberse J, Pittens C, de Cock Buning T, Broerse J. Patient involvement in a scientific advisory process: setting the research agenda for medical products. Health Policy. 2012; 107 (2–3):231–242. doi: 10.1016/j.healthpol.2012.05.014. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fajutrao L, Locklear J, Priaulx J, Heyes A. A systematic review of the evidence of the burden of bipolar disorder in Europe. Clin Pract Epidemiol Ment Health. 2009; 5 (1):3. doi: 10.1186/1745-0179-5-3. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fisher A, Manicavasagar V, Sharpe L, Laidsaar-Powell R, Juraskova I. A qualitative exploration of patient and family views and experiences of treatment decision-making in bipolar II disorder. J Ment Health. 2017; 27 (1):66–79. doi: 10.1080/09638237.2016.1276533. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Goodwin FK, Jamison KR. Manic-depressive illness: bipolar disorder and recurrent depression. 2. New York: Oxford University Press; 2007. [ Google Scholar ]
- Goossens P, Knoopert-van der Klein E, Kroon H, Achterberg T. Self reported care needs of outpatients with a bipolar disorder in the Netherlands: a quantitative study. J Psychiatr Ment Health Nurs. 2014; 14 :549–557. doi: 10.1111/j.1365-2850.2007.01127.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Granek L, Danan D, Bersudsky Y, Osher Y. Living with bipolar disorder: the impact on patients, spouses, and their marital relationship. Bipolar Disord. 2016; 18 (2):192–199. doi: 10.1111/bdi.12370. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Guyatt G, Cairns J, Churchill D, Cook D, Haynes B, Hirsh J, Irvine J, Levine M, Levine M, Nishikawa J, Sackett D, Brill-Edwards P, Gerstein H, Gibson J, Jaeschke R, Kerigan A, Neville A, Panju A, Detsky A, Enkin M, Frid P, Gerrity M, Laupacis A, Lawrence V, Menard J, Moyer V, Mulrow C, Links P, Oxman A, Sinclair J, Tugwell P. Evidence-based medicine: a new approach to teaching the practice of medicine. JAMA. 1992; 268 (17):2420–2425. doi: 10.1001/jama.1992.03490170092032. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Huxley N, Baldessarini R. Disability and its treatment in bipolar disorder patients. Bipolar Disord. 2007; 9 (1–2):183–196. doi: 10.1111/j.1399-5618.2007.00430.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Iancu SC. New dynamics in mental health recovery and rehabilitation. Amsterdam: Vu University; 2013. [ Google Scholar ]
- Iancu SC, Zweekhorst MBM, Veltman DJ, Van Balkom AJLM, Bunders JFG. Mental health recovery on care farms and day centres: a qualitative comparative study of users’ perspectives. Disabil Rehabil. 2014; 36 (7):573–583. doi: 10.3109/09638288.2013.804595. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- IsHak WW, Brown K, Aye SS, Kahloon M, Mobaraki S, Hanna R. Health-related quality of life in bipolar disorder. Bipolar Disord. 2012; 14 (1):6–18. doi: 10.1111/j.1399-5618.2011.00969.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kuper A, Lingard L, Levinson W. Critically appraising qualitative research. BMJ. 2008; 337 (7671):687–689. [ PubMed ] [ Google Scholar ]
- Larsson IE, Sahlsten MJM, Sjöström B, Lindencrona CSC, Plos KAE. Patient participation in nursing care from a patient perspective: a grounded theory study. Scand J Caring Sci. 2007; 21 (3):313–320. doi: 10.1111/j.1471-6712.2007.00471.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lloyd C, Waghorn G, Williams PL. Conceptualising recovery in mental health. Br J Occup Ther. 2008; 71 :321–328. doi: 10.1177/030802260807100804. [ CrossRef ] [ Google Scholar ]
- Maassen EF, Schrevel SJC, Dedding CWM, Broerse JEW, Regeer BJ. Comparing patients’ perspectives of “good care” in Dutch outpatient psychiatric services with academic perspectives of patient-centred care. J Ment Health. 2016; 26 (1):1–11. [ PubMed ] [ Google Scholar ]
- Maassen EF, Regeer BJ, Bunders JGF, Regeer EJ, Kupka RW. A research agenda for bipolar disorder developed from a patient’s perspective. J Affect Disord. 2018; 239 :11–17. doi: 10.1016/j.jad.2018.05.061. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- MacQueen GM, Young LT, Joffe RT. A review of psychosocial outcome in patients with bipolar disorder. Acta Psychiatr Scand. 2001; 103 (3):163–170. doi: 10.1034/j.1600-0447.2001.00059.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Malmström E, Hörberg N, Kouros I, Haglund K, Ramklint M. Young patients’ views about provided psychiatric care. Nord J Psychiatry. 2016; 70 (7):521–527. doi: 10.1080/08039488.2016.1176251. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- MaxQDA [Internet]. Available from: https://www.maxqda.com/ . Accessed 2 Aug 2018.
- Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Soc Sci Med. 2000; 51 (7):1087–1110. doi: 10.1016/S0277-9536(00)00098-8. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Michalak EE, Hole R, Livingston JD, Murray G, Parikh SV, Lapsley S, et al. Improving care and wellness in bipolar disorder: origins, evolution and future directions of a collaborative knowledge exchange network. Int J Ment Health Syst. 2012; 6 :16. doi: 10.1186/1752-4458-6-16. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mills I, Frost J, Cooper C, Moles DR, Kay E. Patient-centred care in general dental practice—a systematic review of the literature. BMC Oral Health. 2014; 14 (1):64. doi: 10.1186/1472-6831-14-64. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Misak CJ. Narrative evidence and evidence-based medicine. J Eval Clin Pract. 2010; 16 (2):392–397. doi: 10.1111/j.1365-2753.2010.01407.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Neogi R, Chakrabarti S, Grover S. Health-care needs of remitted patients with bipolar disorder: a comparison with schizophrenia. World J Psychiatry. 2016; 6 (4):431–441. doi: 10.5498/wjp.v6.i4.431. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nestsiarovich A, Hurwitz NG, Nelson SJ, Crisanti AS, Kerner B, Kuntz MJ, et al. Systemic challenges in bipolar disorder management: a patient-centered approach. Bipolar Disord. 2017; 19 (8):676–688. doi: 10.1111/bdi.12547. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Netwerk Kwaliteitsontwikkeling GGZ. Zorgstandaard Bipolaire stoornissen. 2017;1–54.
- Newnham EA, Page AC. Bridging the gap between best evidence and best practice in mental health. Clin Psychol Rev. 2010; 30 (1):127–142. doi: 10.1016/j.cpr.2009.10.004. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pittens C, Noordegraaf A, van Veen S, Broerse J. The involvement of gynaecological patients in the development of a clinical guideline for resumption of (work) activities in the Netherlands. Health Expect. 2013; 18 :1397–1412. doi: 10.1111/hex.12121. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rusner M, Carlsson G, Brunt D, Nyström M. Extra dimensions in all aspects of life—the meaning of life with bipolar disorder. Int J Qual Stud Health Well-being. 2009; 4 (3):159–169. doi: 10.1080/17482620902864194. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rycroft-Malone J, Seers K, Titchen A, Harvey G, Kitson A, McCormack B. What counts as evidence in evidence-based practice? J Adv Nurs. 2004; 47 (1):81–90. doi: 10.1111/j.1365-2648.2004.03068.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sackett D, Rosenberg W, Gray J, Haynes R, Richardson W. Evidence based medicine: what it is and what it isn’t. Br Med J. 1996; 312 (7023):71–72. doi: 10.1136/bmj.312.7023.71. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Scholl I, Zill JM, Härter M, Dirmaier J. An integrative model of patient-centeredness—a systematic review and concept analysis. PLoS ONE. 2014; 9 (9):e107828. doi: 10.1371/journal.pone.0107828. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schrevel SJC. Surrounded by controversy: perspectives of adults with ADHD and health professionals on mental healthcare. Amsterdam: VU University; 2015. [ Google Scholar ]
- Sidani S, Fox M. Patient-centered care: clarification of its specific elements to facilitate interprofessional care. J Interprof Care. 2014; 28 (2):134–141. doi: 10.3109/13561820.2013.862519. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Skelly N, Schnittger RI, Butterly L, Frorath C, Morgan C, McLoughlin DM, et al. Quality of care in psychosis and bipolar disorder from the service user perspective. Qual Health Res. 2013; 23 (12):1672–1685. doi: 10.1177/1049732313509896. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stange KC. The problem of fragmentation and the need for integrative solutions. Ann Fam Med. 2009; 7 (2):100–103. doi: 10.1370/afm.971. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Strejilevich SA, Martino DJ, Murru A, Teitelbaum J, Fassi G, Marengo E, et al. Mood instability and functional recovery in bipolar disorders. Acta Psychiatr Scand. 2013; 128 (3):194–202. doi: 10.1111/acps.12065. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tait L. Encouraging user involvement in mental health services. Adv Psychiatr Treat. 2005; 11 (3):168–175. doi: 10.1192/apt.11.3.168. [ CrossRef ] [ Google Scholar ]
- Teunissen T, Visse M, De Boer P, Abma TA. Patient issues in health research and quality of care: an inventory and data synthesis. Health Expect. 2011; 16 :308–322. doi: 10.1111/j.1369-7625.2011.00718.x. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- van der Stel. Het begrip herstel in de psychische gezondheidzorg, Leiden; 2015. p. 1–3.
- Van Der Voort TYG, Van Meijel B, Hoogendoorn AW, Goossens PJJ, Beekman ATF, Kupka RW. Collaborative care for patients with bipolar disorder: effects on functioning and quality of life. J Affect Disord. 2015; 179 :14–22. doi: 10.1016/j.jad.2015.03.005. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yasuyama T, Ohi K, Shimada T, Uehara T, Kawasaki Y. Differences in social functioning among patients with major psychiatric disorders: interpersonal communication is impaired in patients with schizophrenia and correlates with an increase in schizotypal traits. Psychiatry Res. 2017; 249 :30–34. doi: 10.1016/j.psychres.2016.12.053. [ PubMed ] [ CrossRef ] [ Google Scholar ]
Bipolar Disorder
1 unmasking bipolar disorder: shedding light on its prevalence.
Introduction How many people do you know that have a mental disorder? Well, 60 million people are affected by this illness. I will be talking about the disorder, symptoms, causes/cures, and the effect it has on the person dealing with this illness. Body Point 1 What is bipolar disorder? Bipolar disorder is an illness that […]
2 Understanding Bipolar Disorder: Symptoms, Impact, and Treatment Approaches
Abstract Bipolar disorder is a chronic mental illness. This is an illness that several Americans have and suffer from each year. Bipolar disorder may be triggered by unfortunate events and stressful experiences. Mood swings usually accompany this disorder. Individuals will oftentimes go from frequent shifts of highs and lows. This reoccurrence and severity may differ […]
3 Exploring Bipolar Disorder: Pathology, Characteristics and Care Strategies
Abstract This paper includes the comparison and contrast of schizophrenia disorder pathology from multiple resources, as well as data obtained from clinical sites at Harris Health Psychiatric Center. The paper will discuss pertinent lab tests and diagnostic studies upon availability and the significance of each; a care plan with three nursing diagnoses, a short-term goal […]
Get Qualified Writing Assistance and an Original Paper.
A qualified writer will create a clear, plagiarism-free essay for you!

4 Differentiating Bipolar Disorder and Schizophrenia: Unraveling Similarities
Introduction Due to related symptoms, mental disorders are often confused with other disorders. Educating yourself about mental disorder differences can increase your chances of distinguishing between the many disorders. “A mental disorder is a behavioral or mental pattern that causes significant personal functioning distress or impairment” (2018. April). Bipolar disorder, also known as manic-depressive disorder […]
5 Exploring Bipolar Disorder through the Lens of Demi Lovato’s Journey
Introduction: Profiling a Famous Person Who is the celebrity you will be diagnosing? The celebrity I will be diagnosing is Demi Lovato. Demi Lovato was born on August 20, 1992, to Patrick Lovato and Dianna De La Garza in Albuquerque, New Mexico. Sadly, her father, Patrick, died of cancer, but she has followed in the […]
Bipolar Disorder - List of Essay Samples And Topic Ideas
Bipolar disorder is a mental health condition characterized by extreme mood swings between emotional highs (mania or hypomania) and lows (depression). Essays on this topic could explore the symptoms, diagnosis, and treatment options for bipolar disorder. Additionally, discussions might extend to the impact of bipolar disorder on individuals’ quality of life, the societal stigmatization of mental health conditions, and the advancements in mental health research and care. A vast selection of complimentary essay illustrations pertaining to Bipolar Disorder you can find in Papersowl database. You can use our samples for inspiration to write your own essay, research paper, or just to explore a new topic for yourself.
Diagnosing Bipolar Disorder
Bipolar Disorder Bipolar disorder is a mental illness that impacts the individual suffers from various mood swings, energy levels, and interest in activities. Bipolar disorder can make everyday activities and life very difficult for the individual. Individuals that suffer from bipolar disorder can have emotional times that can occur at random in their lives. These types of mood swings are manic (mania), hypomanic and depressive. If bipolar disorder is left untreated, the disorder can worsen and become a very serious […]
The Diagnosis of Bipolar Disorder
The diagnosis of Bipolar Disorder is based on the DSM-IV diagnosis criteria, which requires an induvial to meet certain requirements. Bipolar I disorder (manic-depressive disorder), is a mental illness that causes individuals to display mood swings, shifts in their energy or activity levels, and an inhibited ability to carry out simple tasks (Nevid, 2018). It is defined by manic episodes and the individual effected is required to experience at least one. A manic episode is a period of abnormally elevated […]
Substance Abuse and Mental Illnesses
One of the world’s largest and most dangerous epidemics is the raging addiction to illegal drugs and substance abuse. A 2014 study showed that more than 21 million American citizens 12 years of age and older struggle with a substance use disorder. There are many different conceptions of what it means to have an addiction, and while everyone has the right to their own opinion, the true scientific definition of addiction is: “Addiction is a complex disease of the brain […]
We will write an essay sample crafted to your needs.
Bipolar Disorder as a Possibly Treatable Illness
Bipolar disorder is a potentially treatable psychiatric illness that has substantial humanitarian and high social and economic impacts (Swann, A. C., 2006). It is a common, complex, and frequently severe mental health condition, characterized by progressive social and cognitive function disturbances and comorbid medical problems. Exemplifying a regular chronic disorder, it is marked by fluctuations in mood state and energy. It affects more than 1% of the world's population, regardless of nationality, ethnic origin, or socioeconomic status. Notably, bipolar disorder […]
Bipolar Disorder: Tracing Roots and Finding Resilience
Bipolar disorder has two terms that have their own Ancient Greek meaning, melancholy and mania, (Burton, 2017). The greek meaning behind mania is to rage, and the greek meaning behind melancholy comes from the word melas meaning black, (Burton, 2017). Bipolar disorder, (melancholy and mania) traces back to first century AD a greek man named Aretaeus found a number of people were found to be acting happy by dancing and playing at times and down and depressed at other times, […]

Bipolar and Related Disorders
Bipolar Disorder is normally referred to as manic-depressive disorder; this is a mental health disorder that causes mood swing, meaning you experience highs and lows. When people are depressed, they normally feel as though things are hopeless, they lose interest in things that used to be important or things that they do every day on a daily basis before they became depressed. Although bipolar is a lifelong condition, It is a disorder that can be leveled out and controlled to […]
A Mental Health Disorder – Bipolar Disorder
A mental health disorder characterized by extreme highs and lows in mood and energy is known as Bipolar disorder. People naturally experience ups and downs in day to day life however, the severe shifts that happen in bipolar disorder can have a serious impact on life. There are four categories of bipolar disorder. Bipolar one is a person will have experienced one manic event taking place over one week. They may or may not have experienced depressive episodes too. Bipolar […]
Bipolar Disorder as Manic-Depressive Illness
Bipolar disorder, also known as manic-depressive illness, is a brain disorder that causes unusual shifts in mood, energy, activity levels, and the ability to carry out day to day task (The National Institute of Mental Health, n.d.) Bipolar disorder was first recognized by the ancient Greeks. In the mid-1800's, Jules Baillarge described a mental health disorder characterized by recurrent fluctuations between mania and depression. Emil Kraepelin noted that patients with this disorder tended to have symptom-free episodes between their episodes […]
The Reality of Suicide in Children and Young Adolescents
One thing that every human has in common is that we each have our own personal struggles that we work through everyday to overcome. The thing that separates us is our perspective on the life we are given and how we rise above any adversity we are faced with. Life is short and precious and should be valued as such. I do realize that this mentality is much easier said than done. Unfortunately in today’s society, children and young adolescents […]
About Treatment of Bipolar Disorder
The Weird Ways of Bipolar Disorder in Teens Over the decades and since the beginning of life on earth, mental disorders have existed and tormented many different people. The one group of people who tend to be getting more mental disorders than others are teenagers. The teenage years are a time for growth, mistakes, and trying to grow up and be responsible so of course developing a mental disorder at this age is pretty common. But what even is a […]
Bipolar Disorder and its Treatment
Historical and Modern Understandings of Bipolar Disorder and its Treatment This paper will explore Bipolar Disorder, and how it has been viewed within both historical and contemporary contexts. The evolution of the understanding of mental illness has been documented in ancient culture and medicine, including Greek, Indian, and Chinese medicine. How mental illnesses such as Bipolar Disorder are treated has changed throughout the ages; the etiology of mental illness has been documented and researched and has evolved to shape what […]
Bipolar Mood Disorder and Borderline Personality Disorder
Abstract There is a thin line between Bipolar Mood Disorder and Borderline Personality Disorder. It is common to be misdiagnosed as bipolar mood disorder with borderline personality disorder due to some features being similar. Some of the same symptoms run hand in hand with each other. Even some psychiatrist can still misdiagnose one with the wrong disorder if they do not take into consideration using the DSM, factoring in all symptoms current and past, and looking at the symptoms not […]
Bipolar Disorder and Schizophrenia
Bipolar disorder and schizophrenia affect many people. According to Mahoney (2017), over 2.5 million Americans over the age of 18 are believed to be living with bipolar I or bipolar II disorder. This does not include those who have not been diagnosed properly due to misinformation about symptoms. Schizophrenia affects approximately one percent of people worldwide, impacting men and women equally. Schizophrenia can strike anyone and usually occurs between the late teenage years and thirty years of age. Males typically […]
Life with Bipolar Disorder
I have a close friend who lives with bipolar disorder, which is also known as manic-depressive illness. The disease has derailed him several times. After each episode, he brings himself down a notch. Listening to him talk about how he wants to be a better person breaks my heart. He is already an amazing athlete, listener, extremely smart, and thoughtful to those around him. Unfortunately, he doesn't see that all the time. Through his journey with bipolar disorder, I was […]
Childhood Bipolar Disorder
A Closer Examination of Bipolar Disorder in School-Age Children. Professional School Counseling, 9(1), 72-77. In this article Bardick and Bernes states the way children may sometimes get misdiagnosed and their symptoms which can be signs of many other childhood disorders is misunderstood. However, a child may experience symptoms of other disorders such as conduct disorder, attention deficit hyperactivity disorder, oppositional disorder and anxiety disorders. The symptoms can be so much at a time that it can overlap which then gives […]
Navigating the Nuances: Understanding Cyclothymia and Bipolar Disorder
The topic of mental health is one that is often clouded by misunderstandings and oversimplifications, despite the fact that it is both intricate and multidimensional. Cyclothymia and bipolar disorder are two illnesses that are commonly confused with one another because of this common misconception. Understanding the differences between them, despite the fact that they share certain characteristics, is essential for making an accurate diagnosis and providing successful treatment. This article dives further into the complexities of these illnesses in an […]
The Role of Preoccupation with Appearance and Negative Perceptions of Others in Body Dysmorphic Disorder: a Research Paper
Body dysmorphic disorder is generally presented by three separate symptoms: preoccupation with physical appearance, similar to anorexia nervosa and bulimia; frequently looking in mirrors; and the belief that others take special notice of one's appearance in a negative way. Use this sentence as your opening abstract and introduction statement (thesis statement). Research these three distinct elements using at least one recent, scholarly article per factor with populations found in the U.S. Demonstrate how they, separately and ultimately in concert, aid […]
Who Gets Bipolar Disorder?
Abstract Bipolar Disorder is a very serious mental health condition. In this research paper, you will explore what Bipolar Disorder means and the history behind this disorder. Additionally, you review the different stages and compulsions and what role they play in the people of our society. Lastly, you will learn how Bipolar Disorder is diagnosed and come to know the many different treatments and therapy options that help people every day. Bipolar Disorder Bipolar Disorder, also known as Manic Depression […]
The Advantages of Valproate for Bipolar Disorder
Valproate is an antiepileptic drug that has been proven to be effective in acute mania and is often used in the maintenance treatment of bipolar disorder (BPD). Valproate takes a shorter period than lithium before the patient may see benefits. Valproate can be useful as a short-term BPD treatment when rapid mood stabilization is warranted (Nemade & Dombeck, 2018). Valproic acid is thought to be more effective than lithium for treating mania, rapid cycling, or mixed states BPD. However, it […]
The Emotional Appeal and Realistic Animation of Finding Nemo
Premiered in 2003, Finding Nemo depicted the hardships of a parent-child relationship after the loss of a mother. With a simple plot but amazing animation, Pixar, alongside director Andrew Stanton, was able to create a masterpiece that estimated a worldwide gross of $1 billion. How was it possible that a myriad of people were hooked (pun intended) by this movie? Appealing to the ethical and emotional side of human nature, Stanton drew large numbers to the cinema seats. For greater […]
What Can Cause a Mental Illness is Social Problem?
Whenever someone hears the word "mental illness," they automatically assume the worst, and those individuals are seen as different. The term comes with a negative connotation, dating back to the Stone Age. The limited knowledge of mental illnesses was documented in the early 1500s. There might have been studies on mental illnesses, but no tests were conducted for correct treatment. These people have been seen as outsiders instead of ordinary individuals. There are many factors that could cause an individual […]
The Suffering of Vincent Van Gogh with Bipolar II with Rapid Cycling Features
Vincent Van Gogh is regarded as one of the greatest artists of all time. However, it was well documented that he suffered from some type of mental illness. This illness seemed to fuel his creative drive and genius. No formal diagnosis was ever made, but evidence seems to suggest that he was suffering from Bipolar II with Rapid Cycling features. The basic criteria for both a Major Depressive Episode and a Hypomanic Episode are met. When it comes to a […]
Additional Example Essays
- How do Video Games affect the Mental Health of Young Adults
- Social Media: Depression
- House Taken Over by Julio Cortaza
- The Mental Health Stigma
- Psychiatric Nurse Practitioner
- PTSD in Veterans
- Drunk Driving
- A Research Paper on Alzheimer's Disease
- Homeless Veterans
- Mandatory Organ Donation: Ethical or Unethical
- The Effect of Alcohol on College Students
- Leadership and the Army Profession
How To Write An Essay On Bipolar Disorder
Introduction to understanding bipolar disorder.
When writing an essay on bipolar disorder, it's crucial to begin with a clear definition and understanding of the condition. Bipolar disorder is a mental health condition characterized by extreme mood swings that include emotional highs (mania or hypomania) and lows (depression). Your introduction should provide insight into the complexity and seriousness of this disorder, its impact on individuals' lives, and why it's an important topic for discussion. Offer a brief overview of the various aspects of bipolar disorder you intend to explore, whether it's the clinical aspects, treatment options, societal perceptions, or personal accounts.
Examining the Clinical Aspects of Bipolar Disorder
The main body of your essay should delve into the clinical aspects of bipolar disorder. Discuss the symptoms associated with both the manic and depressive phases, and how these can affect a person's behavior, thoughts, and ability to function. Explore the different types of bipolar disorder, such as Bipolar I, Bipolar II, and Cyclothymic Disorder, each having unique patterns of mood swings. It's important to use medically accurate and sensitive language to describe these symptoms and types, relying on reputable sources like psychiatric journals or medical texts. This section should paint a clear clinical picture of bipolar disorder, contributing to a deeper understanding of the condition.
Addressing Treatment and Management
Another critical aspect of your essay should focus on the treatment and management of bipolar disorder. Discuss the various treatment options available, such as medication, psychotherapy, and lifestyle changes, and how these can help manage the symptoms and improve quality of life. Explore the challenges of treating bipolar disorder, including the need for personalized treatment plans, potential side effects of medication, and the importance of long-term management. This part of your essay should also touch upon the support systems, like family, friends, and support groups, which play a crucial role in the lives of those with bipolar disorder.
Concluding with Implications and Personal Reflections
Conclude your essay by summarizing the key points of your analysis and offering a perspective on the broader implications of understanding bipolar disorder. Reflect on the importance of awareness and destigmatization of mental health issues, and how society can better support individuals with bipolar disorder. Consider how advancements in medical research and changes in public perception can impact the treatment and management of the disorder. Your conclusion should not only provide closure to your essay but also encourage further thought and empathy regarding the challenges faced by individuals with bipolar disorder, highlighting the need for ongoing research, support, and understanding.
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers

Bipolar disorder: we’ve pinpointed the brain areas which drive mood bias
Clinical Fellow of Psychology, UCL
Disclosure statement
Hestia Moningka does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
University College London provides funding as a founding partner of The Conversation UK.
View all partners
Moods and emotions play an important role in our day-to-day life. They even influence how we experience things – for instance, whether we start the day feeling hopeful and energised or grumpy and lethargic. This can affect whether we interpret events in a positive or negative light.
In people with bipolar disorder, however, mood can change quickly and unpredictably, so that you get “stuck” in a low or high mood, which can have significant consequences. Yet researchers don’t know exactly what drives such extreme shifts in mood.
Now our new study, published in Biological Psychiatry Global Open Science , has uncovered the brain areas that bias mood and the brain’s response to pleasure in bipolar disorder. It is possible that our findings may one day lead to better treatments.
We all experience shifts in mood throughout the day. When we are in a good mood, we tend to view things more favourably – if we happen to experience a streak of success and are on a roll, our good mood similarly rolls over and gains momentum.
Equally, when we are in a bad mood, we tend to perceive bad outcomes as even worse than they are – this negative mood similarly gains momentum and might make us feel worse.
Such momentum in mood can bias how we perceive events and the decisions we make. Imagine going into a new restaurant for the first time. If you happen to be in a fantastic mood, you are likely to perceive the experience as much better than it actually is. This might set up your expectations that a future visit would give you a similar, positive experience, and leave you feeling disappointed if that is not the case.
The process by which mood biases the perception of pleasurable or rewarding experiences has been thought to be amplified for people with bipolar disorder, who can experience moods that can quickly climb to extremes.
We know from prior research that these extreme mood cycles can be triggered from life experiences involving important goals – such as doing well in exams, buying a property or getting a promotion. This could be either by attaining them or failing to attain them.
Bipolar disorder has been described by those who experience it as a double-edged sword . Alongside periods of fluctuating (hypo)manic or depressive moods, many people with bipolar disorder vigorously pursue goals that are important to them and are often successful as a result.
But what goes on in the brain when our moods shift from one second to the next in response to pleasurable experiences?
Mood bias in the brain
Pleasurable and rewarding experiences activate specific circuits in the brain that involve a neurochemical called dopamine . This helps us learn that the experience was positive and that we should repeat the actions that give rise to this pleasurable experience.
One way to measure the brain’s response to reward is to examine activity in the ventral striatum – the key area of our reward system responsible for the feeling of pleasure.
Our study aimed to find out what goes on in the ventral striatum in 21 participants with bipolar disorder and 21 control participants when momentary shifts in mood occur. We wanted to gauge this down to the order of seconds, in response to monetary rewards.
Our participants were asked to play a computer game, involving gambling to win or lose real sums of money, while in a brain scanner. We used a technique called functional magnetic resonance imaging (fMRI) to measure blood flow in the participants’ brains in order to determine which areas were active.
We also used a mathematical model to calculate participants’ “momentum” in mood – how great they felt as they kept winning.
Across all participants, we observed a heightened brain activity in an area of the brain which is involved in the experience and awareness of transient mood states – the anterior insula .
However, it turns out that during periods of upwards momentum, where participants had won many times, the ventral striatum showed a strong, positive signal only in participants with bipolar disorder. This means that participants with bipolar disorder experienced a heightened feeling of reward.
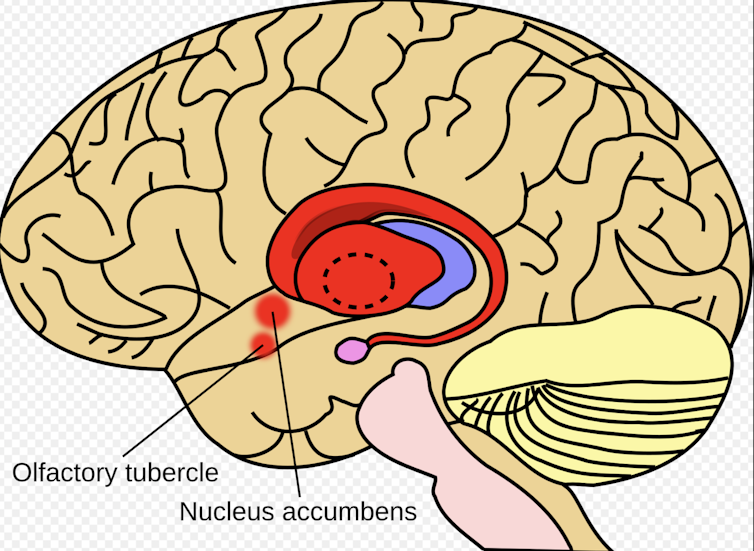
We also found that the amount of communication between the ventral striatum and anterior insula was reduced in participants with bipolar disorder. In the control group, both the ventral striatum and anterior insula were firing up in union.
This suggests that control participants were better able to keep their mood in mind when perceiving rewards in the task. So while participants may find it rewarding to win, we think they were more aware that this put them in a better mood. This might help them adjust quickly to an environment that changes (for the better or worse) and protect them from expectations of getting a future reward becoming very inflated.
However, this was the opposite for participants with bipolar disorder. This means they were less able to set their mood aside from how exciting or pleasurable they found the rewards to be.
These findings may help to explain why people with bipolar disorder can get stuck in a vicious cycle where their mood escalates and sometimes causes them to take bigger risks than usual.
The same mechanism that triggers a positive mood may also trigger a negative mood cycle. If you are on a winning streak and lose unexpectedly, mood may shift towards a negative cycle, with expectations becoming negative and behaviour changing accordingly. However future studies will need to investigate negative mood cycles more specifically.
Our findings may also aid the development of interventions that help people with bipolar disorder to better decouple their mood from their perceptions and decisions, without dampening down exciting experiences. Since dopamine neurons are closely connected to the ventral striatum, it will be interesting to see if dopamine medication could ameliorate this mood bias.
- Neuroscience
- Bipolar disorder

Lecturer in Indigenous Health (Identified)

Social Media Producer

Lecturer in Visual Art

PhD Scholarship

Senior Lecturer, HRM or People Analytics
We use cookies to enhance our website for you. Proceed if you agree to this policy or learn more about it.
- Essay Database >
- Essay Examples >
- Essays Topics >
- Essay on Disorders
Bipolar Disorder Thesis Examples
Type of paper: Thesis
Topic: Disorders , Bipolar Disorder , Suicide , Treatment , Pharmacy , Depression , Nursing , Medicine
Published: 01/31/2020
ORDER PAPER LIKE THIS
Bipolar disorder (manic-depressive disorder) is a severe and highly morbid recurrent mood disorder. The prevalence of the disorder is 1.3% to 1.6% while its mortality rate is 2 to 3 times higher compared to that of the general population. The suicidal rate among bipolar disorder patients is about 10-20%. The disorder has diverse clinical manifestations ranging from mild depression to severe depression and/with psychosis. A severe variant of the disorder, which manifests in rapid cycles and is difficult to treat, is common in women. The disorder has high recurrence and suicidal risks. Bipolar disorder is one of the two main mood disorders. There are two types of the disorder; bipolar disorder I, which is recurrent and features manic, mixed and a major episode of depression; and bipolar disorder II with more than one episode of depression and a hypomanic episode. During the manic episode, a patient experiences an abnormally raised, irritable mood. The changes in mood in hypomanic episodes are not as severe as in manic episodes. A major episode of depression is characterized by depression or loss of interest in almost every activity. This episode lasts for at least two weeks. The disorder mostly begins in people of age between 15 and 24 years. However, treatment is always sought after a time interval of 5-10 years. Other medical conditions such as trauma, Cushing’s disease and AIDS have been attributed to the manifestation of symptoms in people of age 60 years and above. Genetic factors also increase the risk of bipolar disorder in monozygotic twins and other 1st degree relatives. Bipolar disorder is mainly treated to prevent acts of suicides and recurrence. Prophylactic treatment is given to patients who have experienced at least two manic or depressive episodes in 5 years. Lithium salt is used for long-term treatment. It is effective in the prevention of manic or depressive episodes. Anticonvulsants such as carbamazepine are also effective. Valproic acid is used to treat acute mania. Abrupt discontinuation of medication is associated with increased depression and suicides. However, gradual discontinuation of lithium reduces the risks of recurrences of mania. Psychotherapy is used to enhance the patient’s compliance to medication, and accept the illness.
Muller-Oerlinghausen, B., Berghofer, A., & Bauer, M. (2002). Bipolar Disorder. Lancet, 241-7.

Cite this page
Share with friends using:
Removal Request

Finished papers: 319
This paper is created by writer with
ID 274059870
If you want your paper to be:
Well-researched, fact-checked, and accurate
Original, fresh, based on current data
Eloquently written and immaculately formatted
275 words = 1 page double-spaced

Get your papers done by pros!
Other Pages
Recruit select and induct staff essay, religious involvement course work examples, analyze essay examples, family first essay examples, operational considerations for restaurants research paper examples, china and vietnam history course work example, good of mice and men essay example, free essay on post dramatic stress disorder, good example of junk food must be avoided at all costs argumentative essay, classification and functions of lasers essay sample, free rice essay sample, social group being a student athlete creative writings examples, example of is the tragic hero central to the tragic plots of oedipus rex and death of a salesman essay, free research paper about edward snowden a hero or traitor, identity in america essay samples, acquainted with the night by robert frost essay sample, example of leftist politics in latin america essay, free political science essay example, good research paper about environmental scan paper, good the great alaska earthquake of 1964 report example, example of argumentative essay on writing proficiency, sample essay on principles, recommendations essay example, example of essay on one mistake does not have to rule a person 039 s entire life joyce meyer, creative writing on marketing strategy for porsche, arthrology essays, shorewood essays, gale essays, bloody essays, lord henry wotton essays, predictive medicine essays, iowa state university essays, hydrostatic essays, susan glaspell research papers, john marshall research papers, goldwater research papers, chateau research papers, neon research papers, affinity research papers, tent research papers, settler research papers.
Password recovery email has been sent to [email protected]
Use your new password to log in
You are not register!
By clicking Register, you agree to our Terms of Service and that you have read our Privacy Policy .
Now you can download documents directly to your device!
Check your email! An email with your password has already been sent to you! Now you can download documents directly to your device.
or Use the QR code to Save this Paper to Your Phone
The sample is NOT original!
Short on a deadline?
Don't waste time. Get help with 11% off using code - GETWOWED
No, thanks! I'm fine with missing my deadline
- Open access
- Published: 06 November 2018
The challenges of living with bipolar disorder: a qualitative study of the implications for health care and research
- Eva F. Maassen ORCID: orcid.org/0000-0003-0211-0994 1 , 2 ,
- Barbara J. Regeer 1 ,
- Eline J. Regeer 2 ,
- Joske F. G. Bunders 1 &
- Ralph W. Kupka 2 , 3
International Journal of Bipolar Disorders volume 6 , Article number: 23 ( 2018 ) Cite this article
39k Accesses
19 Citations
21 Altmetric
Metrics details
In mental health care, clinical practice is often based on the best available research evidence. However, research findings are difficult to apply to clinical practice, resulting in an implementation gap. To bridge the gap between research and clinical practice, patients’ perspectives should be used in health care and research. This study aimed to understand the challenges people with bipolar disorder (BD) experience and examine what these challenges imply for health care and research needs.
Two qualitative studies were used, one to formulate research needs and another to formulate healthcare needs. In both studies focus group discussions were conducted with patients to explore their challenges in living with BD and associated needs, focusing on the themes diagnosis, treatment and recovery.
Patients’ needs are clustered in ‘disorder-specific’ and ‘generic’ needs. Specific needs concern preventing late or incorrect diagnosis, support in search for individualized treatment and supporting clinical, functional, social and personal recovery. Generic needs concern health professionals, communication and the healthcare system.
Patients with BD address disorder-specific and generic healthcare and research needs. This indicates that disorder-specific treatment guidelines address only in part the needs of patients in everyday clinical practice.
Bipolar disorder (BD) is a major mood disorder characterized by recurrent episodes of depression and (hypo)mania (Goodwin and Jamison 2007 ). According to the Diagnostic and Statistical Manual 5 (DSM-5), the two main subtypes are BD-I (manic episodes, often combined with depression) and BD-II (hypomanic episodes, combined with depression) (APA 2014 ). The estimated lifetime prevalence of BD is 1.3% in the Dutch adult population (de Graaf et al. 2012 ), and BD is associated with high direct (health expenditure) and indirect (e.g. unemployment) costs (Fajutrao et al. 2009 ; Michalak et al. 2012 ), making it an important public health issue. In addition to the economic impact on society, BD has a tremendous impact on patients and their caregivers (Granek et al. 2016 ; Rusner et al. 2009 ). Even between mood episodes, BD is often associated with functional impairment (Van Der Voort et al. 2015 ; Strejilevich et al. 2013 ), such as occupational or psychosocial impairment (Huxley and Baldessarini 2007 ; MacQueen et al. 2001 ; Yasuyama et al. 2017 ). Apart from symptomatic recovery, treatment can help to overcome these impairments and so improve the person’s quality of life (IsHak et al. 2012 ).
Evidence Based Medicine (EBM), introduced in the early 1990s, is a prominent paradigm in modern (mental) health care. It strives to deliver health care based on the best available research evidence, integrated with individual clinical expertise (Sackett et al. 1996 ). EBM was introduced as a new paradigm to ‘de - emphasize intuition’ and ‘ unsystematic clinical experience’ (Guyatt et al. 1992 ) (p. 2420). Despite its popularity in principle (Barratt 2008 ), EBM has also been criticized. One such criticism is the ignorance of patients’ preferences and healthcare needs (Bensing 2000 ). A second criticism relates to the difficulty of adopting evidence-based treatment options in clinical practice (Bensing 2000 ), due to the fact that research outcomes measured in ‘the gold standard’ randomized-controlled trials (RCTs) seldom correspond to the outcomes clinical practice seeks and are not responsive to patients’ needs (Newnham and Page 2010 ). Moreover, EBM provides an overview on population level instead of individual level (Darlenski et al. 2010 ). Thus, adopting research evidence in clinical practice entails difficulties, resulting in an implementation gap.
To bridge the gap between research and clinical practice, it is argued that patients’ perspectives should be used in both health care and research. Patients have experiential knowledge about their illness, living with it in their personal context and their care needs (Tait 2005 ). This is valuable for both clinical practice and research as their knowledge complements that of health professionals and researchers (Tait 2005 ; Broerse et al. 2010 ; Caron-Flinterman et al. 2005 ). This source of knowledge can be used in the process of translating evidence into clinical practice (Schrevel 2015 ). Moreover, patient participation can enhance the clinical relevance of and support for research and the outcomes in practice (Abma and Broerse 2010 ). Hence, it is argued that these perspectives should be explicated and integrated into clinical guidelines, clinical practice, and research (Misak 2010 ; Rycroft-Malone et al. 2004 ).
Given the advantages of including patients’ perspectives, patients are increasingly involved in healthcare services (Bagchus et al. 2014 ; Larsson et al. 2007 ), healthcare quality (e.g. guideline development) (Pittens et al. 2013 ) and health-related research (e.g. agenda setting, research design) (Broerse et al. 2010 ; Boote et al. 2010 ; Elberse et al. 2012 ; Teunissen et al. 2011 ). However, patients’ perspectives on health care and on research are often studied separately. We argue that to be able to provide care focused on the patients and their needs, care and research must closely interact.
We hypothesize that the challenges BD patients experience and the associated care and research needs are interwoven, and that combining them would provide a more comprehensive understanding. We hypothesize that this more comprehensive understanding would help to close the gap between clinical practice and research. For this reason, this study aims to understand the challenges people with BD experience and examine what these challenges imply for healthcare and research needs.
To understand the challenges and needs of people with BD, we undertook two qualitative studies. The first aimed to formulate a research agenda for BD from a patient’s perspective, by gaining insights into their challenges and research needs. A second study yielded an understanding of the care needs from a patient’s perspective. In this article, the results of these two studies are combined in order to investigate the relationship between research needs and care needs. Challenges are defined as ‘difficulties patients face, due to having BD’. Care needs are defined as that what patients ‘desire to receive from healthcare services to improve overall health’ (Asadi-Lari et al. 2004 ) (p. 2). Research needs are defined as that what patients ‘desire to receive from research to improve overall health’.
Study on research needs
In this study, mixed-methods were used to formulate research needs from a patient’s perspective. First six focus group discussions (FGDs) with 35 patients were conducted to formulate challenges in living with BD and hopes for the future, and to formulate research needs arising from these difficulties and aspirations. These research needs were validated in a larger sample (n = 219) by means of a questionnaire. We have reported this study in detail elsewhere (Maassen et al. 2018 ).
Study on care needs
This study was part of a nationwide Dutch project to generate a practical guideline for BD: a translation of the existing clinical guideline to clinical practice, resulting in a standard of care that patients with BD could expect. The practical guideline (Netwerk Kwaliteitsontwikkeling GGZ 2017 ) was written by a taskforce comprising health professionals, patients. In addition to the involvement of three BD patients in the taskforce, a systematic qualitative study was conducted to gain insight into the needs of a broader group of patients.
Participants and data collection
To formulate the care needs of people with BD, seven FGDs were conducted, with a total of 56 participants, including patients (n = 49) and caregivers (n = 9); some participants were both patient and caregiver. The inclusion criteria for patients were having been diagnosed with BD, aged 18 years or older and euthymic at time of the FGDs. Inclusion criteria for caregivers were caring for someone with BD and aged 18 years or older. To recruit participants, a maximum variation sampling strategy was used to collect a broad range of care needs (Kuper et al. 2008 ). First, all outpatient clinics specialized in BD affiliated with the Dutch Foundation for Bipolar Disorder (Dutch: Kenniscentrum Bipolaire Stoornissen) were contacted by means of an announcement at regular meetings and by email if they were interested to participate. From these outpatient clinics, patients were recruited by means of flyers and posters. Second, patients were recruited at a quarterly meeting of the Dutch patient and caregiver association for bipolar disorder. The FGDs were conducted between March and May 2016.
The FGDs were designed to address challenges experienced in BD health care and areas of improvement for health care for people with BD. The FGDs were structured by means of a guide and each session was facilitated by two moderators. The leading moderator was either BJR or EFM, having both extensive experience with FGD’s from previous studies. The first FGD explored a broad range of needs. The subsequent six FGDs aimed to gain a deeper understanding of these care needs, and were structured according to the outline of the practical guideline (Netwerk Kwaliteitsontwikkeling GGZ 2017 ). Three chapters were of particular interest: diagnosis, treatment and recovery. These themes were discussed in the FGDs, two in each session, all themes three times in total. Moreover, questions on specific aspects of care formulated by the members of the workgroup were posed. The sessions took 90–120 min. The FGDs were audiotaped and transcribed verbatim. A summary of the FGDs was sent to the participants for a member check.
Data analysis
To analyze the data on challenges and needs, a framework for thematic analysis to identify, analyze and report patterns (themes) in qualitative data sets by Braun and Clarke ( 2006 ) was used. First, we familiarized ourselves with the data by carefully reading the transcripts. Second, open coding was used to derive initial codes from the data. These codes were provided to quotes that reflected a certain challenge or care need. Third, we searched for patterns within the codes reflecting challenges and within those reflecting needs. For both challenges and needs, similar or overlapping codes were clustered into themes. Subsequently, all needs were categorized as ‘specific’ or ‘generic’. The former are specific to BD and the latter are relevant for a broad range of psychiatric illnesses. Finally, a causal analysis provided a clear understanding of how challenges related to each other and how they related to the described needs.
To analyze the data on needs regarding recovery, four domains were distinguished, namely clinical, functional, social and personal recovery (Lloyd et al. 2008 ; van der Stel 2015 ). Clinical recovery refers to symptomatic remission; functional recovery concerns recovery of functioning that is impaired due to the disorder, particularly in the domain of executive functions; social recovery concerns the improvement of the patient’s position in society; personal recovery concerns the ability of the patient to give meaning to what had happened and to get a grip on their own life. The analyses were discussed between BR and EM. The qualitative software program MAX QDA 11.1.2 was used (MaxQDA).
Ethical considerations
According to the Medical Ethical Committee of VU University Medical Center, the Medical Research Involving Human Subjects Act does not apply to the current study. All participants gave written or verbal informed consent regarding the aim of the study and for audiotaping and its use for analysis and scientific publications. Participation was voluntary and participants could withdraw from the study at any time. Anonymity was ensured.
This section is in three parts. The first presents the participants’ characteristics. The second presents the challenges BD patients face, derived from both studies, and the disorder-specific care and research needs associated with these challenges. The third part describes the generic care needs that patients formulated.
Characteristics of the participants
In the study on care needs, 56 patients and caregivers participated. The mean age of the participants was 52 years (24–75), of whom 67.8% were women. The groups varied from four to sixteen participants, and all groups included men and women. Of all participants 87.5% was diagnosed with BD, of whom 48.9% was diagnosed with BD I. 3.5% was both caregivers and diagnosed with BD. Of 4 patients the age was missing, and from 6 patients the bipolar subtype.
Despite the fact that participants acknowledge the inevitable diagnostic difficulties of a complex disorder like BD, in both studies they describe a range of challenges in different phases of the diagnostic process (Fig. 1 ). Patients explained that the general practitioner (GP) and society in general did not recognize early-warning signs and mood swings were not well interpreted, resulting in late or incorrect diagnosis. Patients formulated a need for more research on what early-warning signs could be and on how to improve GPs’ knowledge about BD. Formulated care needs were associated with GPs using this knowledge to recognize early-warning signs in individual patients. One participant explained that certain symptoms must be noticed and placed in the right context:
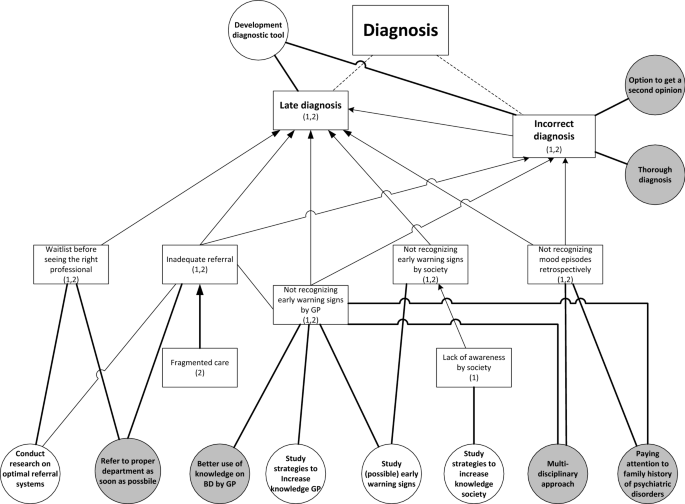
Challenges with diagnosis (squares) including relating research needs (white circles) and care needs (grey circles). (1): mentioned in study on research needs; (2): mentioned in study on care needs. Dotted lines: division of challenges into sub challenges. Arrows: causal relation between challenges
I call it, ‘testing overflow of ideas’. [….] When it happens for the first time you yourself do not recognize it. Someone else close to you or the health professional, who is often not involved yet, must signal it. (FG6)
Moreover, these challenges are associated with the need to pay attention to family history and to use a multidisciplinary approach to diagnosis to benefit from multiple perspectives. The untimely recognition of early symptoms also results in another challenge: inadequate referral to the right specialized health professional. After referral, people often face a waiting list, again causing delay in the diagnostic process. These challenges result in the need for research on optimal referral systems and the care need for timely referral. One participant described her process after the GP decided to refer her:
But, yes, at that moment the communication wasn’t good at all. Because the general practitioner said: ‘she urgently has to be seen by someone’. Subsequently, three weeks went by, until I finally arrived at depression [department]. And at that department they said: ‘well, you are in the wrong place, you need to go to bipolar [department ]’. (FG1)
The challenge of being misdiagnosed is associated with the need to be able to ask for a second opinion and to have a timely and thorough diagnosis. On the one hand, it is important for patients that health professionals quickly understand what is going on, on the other hand that health professionals take the time to thoroughly investigate the symptoms by making several appointments.
From both studies, two main challenges related to the treatment of BD were derived (Fig. 2 ). The first is finding appropriate and satisfactory treatment. Participants explained that it is difficult to find the right medication and dosage that is effective and has acceptable side-effects. One participant illustrates:
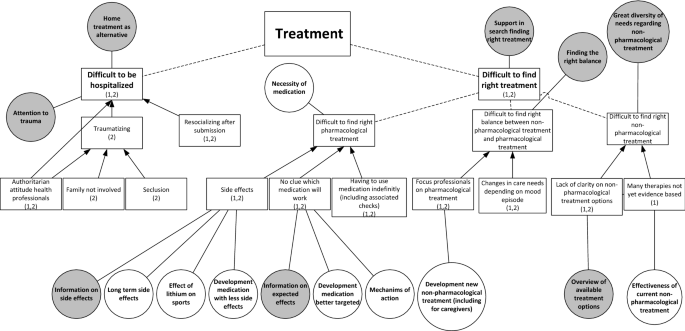
Challenges with treatment (squares) including relating research needs (white circles) and care needs (grey circles). (1): mentioned in study on research needs; (2): mentioned in study on care needs. Dotted lines: division of challenges into sub challenges. Arrows: causal relation between challenges
I think, at one point, we have to choose, either overweight or depressed. (FG1)
Some participants said that they struggle with having to use medication indefinitely, including the associated medical checks. The difficult search for the right pharmacological treatment results in the need for research on long-term side-effects, on the mechanism of action of medicine and on the development of better targeted medication with fewer adverse side-effects. In care, patients would appreciate all the known information on the side-effects and intended effects. One participant explained the importance of being properly informed about medication:
I don’t read anything [about medication], because then I wouldn’t dare taking it. But I do think, when you explain it well, the advantages, the disadvantages, the treatment, the idea behind it, that would help a lot in compliance. (FG1)
A second aspect is the challenge of finding non-pharmacological therapies that fit patients’ needs. They said they and the health professionals often do not know which non-pharmacological therapies are available and effective:
But we found the carefarm ourselves Footnote 1 [….]. You have to search for yourself completely. Yes, I actually hoped that that would be presented to you, like: ‘this would be something for you’. (FG3)
Participants mentioned a variety of non-pharmacological therapies they found useful, namely cognitive behavior therapy (CBT), EMDR, running therapy, social-rhythm training, light therapy, mindfulness, psychotherapy, psychoeducation, and training in living with mood swings. They formulated the care need to receive an overview of all available treatment options in order to find a treatment best suited to their needs. They would appreciate research on the effectiveness of non-pharmacological treatments.
A third aspect within this challenge is finding the right balance between non-pharmacological and pharmacological treatment. Participants differed in their opinion about the need for medication. Whereas some participants stated that they need medication to function, others pointed out that they found non-pharmacological treatments effective, resulting in less or no medication use. They explained that the preferred balance can also change over time, depending on their mood. However, they experience a dominant focus on pharmacological treatment by the health professionals. To address this challenge, patients need support in searching for an appropriate balance.
Next to the challenge of finding appropriate and satisfactory treatment, a second treatment-related challenge is hospitalization. Participants often had a traumatic experience, due to seclusion, the authoritarian attitudes of clinical staff, and not involving their family. Patients therefore found it important to try preventing being hospitalized, for example by means of home treatment, which some participants experienced positively. Despite the challenges relating to hospitalization, participants did acknowledge that in some cases it cannot be avoided, in which case they urged for close family involvement, open communication and being treated by their own psychiatrist. Still, in the study on research needs, hospitalization did not emerge as an important research theme.
In both studies, participants described challenges in all four domains of recovery: clinical, functional, social and personal (Fig. 3 ). In relation to clinical recovery, participants struggled with the symptoms of mood episodes, the psychosis and the fear of a future episode. In contrast, some participants mentioned that they sometimes miss the hypomanic state they had experienced previously due to effective medical treatment. In the domain of functional recovery, participants contended with having to function below their educational level due to residual symptoms, such as cognitive problems, due to the importance of preventing stress in order to reduce the risk of a new episode, and because of low energy levels. This leads to the care need that health professionals should pay attention to the level of functioning of their patients.
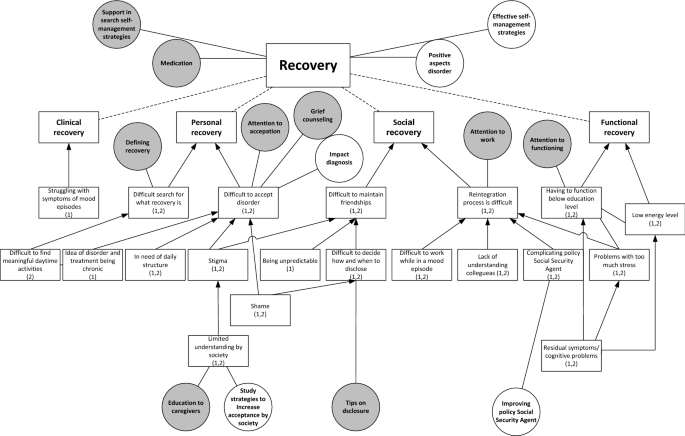
Challenges with recovery (squares) including relating research needs (white circles) and care needs (grey circles). (1): mentioned in study on research needs; (2): mentioned in study on care needs. Dotted lines: division of challenges into sub challenges. Arrows: causal relation between challenges
In the domain of social recovery, participants described challenges with maintaining friendships, due to stigma, being unpredictable and with deciding when to disclose the disorder. The latter resulted in the care need for tips on disclosure. Moreover, patients experienced challenges with reintegration to work, due to colleagues’ lack of understanding, problems with functioning during an episode, the complicating policy of the (Dutch) Employee Insurance Agency Footnote 2 in relation to the fluctuating course of BD and the negative impact of stress. These challenges are associated with the care need that health professionals should pay attention to work and the need for research on how to improve the Social Security Agency’s policy.
For their personal recovery, participants struggled with acceptance of the disorder, due to shame, stigma, having to live by structured rules and disciplines, and the chronic nature of BD. This results in care needs for grief counselling and attention to acceptance and the need for research on the impact of being diagnosed with BD. Limited understanding within society also causes problems with acceptance, corresponding with the care need for education for caregivers and for research on how to increase social acceptance. Another challenge in personal recovery was discovering what recovery means and what constitute meaningful daily activities. Patients appreciated the support of health professionals in this area. One participant described the difficult search for the meaning of recovery:
I have been looking to recover towards the situation [before diagnosis] for a long time; that I could do what I always did and what I liked. But then I was confronted with the fact that I shouldn’t expect that to happen, or only with a lot of effort. (…) Then you start thinking, now what? A compromise. I don’t want to call that recovery, but it is a recovered, partly accepted, situation. But it is not recovery as I expected it to be. (FG5)
In general, participants considered frequent contact with a nurse or psychiatrist supportive, to help them monitor their mood and help them find (efficient) self-management strategies. Most participants appreciated the involvement of caregivers in the treatment and contact with peers.
Generic care needs
We have described BD-specific needs, but patients mentioned also mentioned several generic care needs. The latter are clustered into three categories. The first concerns the health professionals . Participants stressed the importance of a good health professional, who carefully listens, takes time, and makes them feel understood, resulting in a sense of connection. Furthermore, a good health professional treats beyond the guideline, and focuses on the needs of the individual patient. When there is no sense of connection, it should be possible to change to another health professional. The second category concerns communication between the patient and the health professional . Health professionals should communicate in an open, honest and clear way both in the early diagnostic phase and during treatment. Open communication facilitates individualized care, in which the patient is involved in decision making. In addition, participants wanted to be treated as a person, not as a patient, and according to a strength-based approach. The third category concerns needs at the level of the healthcare system . Participants struggled with the availability of the health professionals and preferred access to good care 24/7 and being able to contact their health professional quickly when necessary. Currently, according to the participants, the care system is not geared to the mood swings of BD, because patients often faced waiting lists before they could see a health professional.
Is adequate treatment also having a number from a mental health institution you can always call when you are in need, that you can go there? And not that you can go in three weeks, but on a really short notice. So at least a phone call. (FG3)
Participants were often frustrated by the limited collaboration between health professionals, within their own team, between departments of the organization, and between different organizations, including complementary health professionals. They would appreciate being able to merge their conventional and complementary treatment, with greater collaboration among the different health professionals. Furthermore, they would like continuity of health professionals as this improves both the diagnostic phase and treatment, and because that health professional gets to know the patient.
We hypothesized that research and care needs of patients are closely intertwined and that understanding these, by explicating patients’ perspectives, could contribute to closing the gap between research and care. Therefore, this study aimed to understand the challenges patients with BD face and examine what these imply for both healthcare and research. In the study on needs for research and in the study on care needs, patients formulated challenges relating to receiving the correct diagnosis, finding the right treatment, including the proper balance between non-pharmacological and pharmacological treatment, and to their individual search for clinical, functional, social and personal recovery. The formulated needs in both studies clearly reflected these challenges, leading to closely corresponding needs. Another important finding of our study is that patients not only formulate disorder-specific needs, but also many generic needs.
The needs found in our study are in line with the current literature on the needs of patients with BD, namely for more non-pharmacological treatment (Malmström et al. 2016 ; Nestsiarovich et al. 2017 ), timely recognition of early-warning signs and self-management strategies to prevent a new episode (Goossens et al. 2014 ), better information on treatment and treatment alternatives (Malmström et al. 2016 ; Neogi et al. 2016 ) and coping with grief (Goossens et al. 2014 ). Moreover, the need for frequent contact with health professionals, being listened to, receiving enough time, shared decision-making on pharmacological treatment, involving caregivers (Malmström et al. 2016 ; Fisher et al. 2017 ; Skelly et al. 2013 ), and the urge for better access to health care and continuity of health professionals (Nestsiarovich et al. 2017 ; Skelly et al. 2013 ) are confirmed by the literature. Our study added to this set of literature by providing insights in patients’ needs in the diagnostic process and illustrating the interrelation between research needs and care needs from a patient’s perspective.
The generic healthcare needs patients addressed in this study are clustered into three categories: the health professional , communication between the patient and the health professional and the health system. These categories all fit in a model of patient-centered care (PCC) by Maassen et al. ( 2016 ) In their review, patients’ perspectives on good care are compared with academic perspectives of PCC and a model of PCC is created comprising four dimensions: patient, health professional, patient – professional interaction and healthcare organization. All the generic needs formulated in this study fit into these four dimensions. The need to be treated as a person with strengths fits the dimension ‘patient’, and the need for a good health professional who carefully listens, takes time and makes them feel understood, resulting in a good connection with the professional, fits the dimension ‘health professional’ of this model. Furthermore, patients in this study stressed the importance of open communication in order to provide individualized care, which fits the dimension of ‘patient–professional interaction’. The urge for better access to health care, geared to patients’ mood swings and the need for better collaboration between health professionals and continuity of health professionals fits the dimension of ‘health care organization’ of the model. This study confirms the findings from the review and contributes to the literature stressing the importance of a patient-centered care approach (Mills et al. 2014 ; Scholl et al. 2014 ).
In the prevailing healthcare paradigm, EBM, the best available evidence should guide treatment of patients (Sackett et al. 1996 ; Darlenski et al. 2010 ). This evidence is translated into clinical and practical guidelines, which thus facilitate EBM and could be used as a decision-making tool in clinical practice (Skelly et al. 2013 ). For many psychiatric disorders, treatment is based on such disorder - specific clinical and practical guidelines. However, this disease-focused healthcare system has contributed to its fragmented nature Stange ( 2009 ) argues that this fragmented care system has expanded without the corresponding ability to integrate and personalize accordingly. We argue that acknowledging that disorder - specific clinical and practical guidelines address only parts of the care needs is of major importance, since otherwise important aspects of the patients’ needs will be ignored. Because there is an increasing acknowledgement that health care should be responsive to the needs of patients and should change from being disease-focused towards being patient-focused (Mead and Bower 2000 ; Sidani and Fox 2014 ), currently in the Netherlands generic practical guidelines are written on specific care themes (e.g. co-morbidity, side-effects, daily activity and participation). These generic practical guidelines address some of the generic needs formulated by the patients in our study. We argue that in addition to disorder-specific guidelines, these generic practical guidelines should increasingly be integrated into clinical practice, while health professionals should continuously be sensitive to other emerging needs. We believe that an integration of a disorder-centered and a patient-centered focus is essential to address all needs a patient.
Strengths, limitations and future research
This study has several strengths. First, it contributes to the literature on the challenges and needs of patients with BD. Second, the study is conducted from a patient’s perspective. Moreover, addressing this aim by conducting two separate studies enabled us to triangulate the data.
This study also has several limitations. First, this study reflects the challenges, care needs and research needs of Dutch patient with BD and caregivers. Despite the fact that a maximum variation sampling strategy was used to derive a broad range of challenges and needs throughout the Netherlands, the Dutch setting of the study may limit the transferability to other countries. To understand the overlap and differences between countries, similar research should be conducted in other contexts. Second, given the design of the study, we could not differentiate between patients and caregivers since they participated together in the FGDs. More patients than caregivers participated in the study. For a more in-depth understanding of the challenges and needs faced by caregivers, in future research separate FGDs should be conducted. Third, due to the fixed outline of the practical guideline used to conduct the FGDs, only the healthcare needs for diagnosis, treatment and recovery of BD are studied. Despite the fact that these themes might cover a broad range of health care, it could have resulted in overlooking certain needs in related areas of well-being. Therefore, future research should focus on needs outside of these themes in order to provide a complete set of healthcare needs.
Patients and their caregivers face many challenges in living with BD. Our study contributes to the literature on care and research needs from a patient perspective. Needs specific for BD are preventing late or incorrect diagnosis, support in search for individualized treatment, and supporting clinical, functional, social and personal recovery. Generic healthcare needs concern health professionals, communication and the healthcare system. This explication of both disorder-specific and generic needs indicates that clinical practice guidelines should address and integrate both in order to be responsive to the needs of patients and their caregivers.
Care farm: farms that combine agriculture and services for people with disabilities (Iancu 2013 ). These farms are used as interventions in mental care throughout Europe and the USA to facilitate recovery (Iancu et al. 2014 ).
A government agency involved in the implementation of employee insurance and providing labor market and data services.
Abma T, Broerse J. Patient participation as dialogue: setting research agendas. Health Expect. 2010;13(2):160–73.
Article Google Scholar
APA. Beknopt overzicht van de criteria (DSM-5). Nederlands vertaling van de Desk Reference to the Diagnostic Criteria from DSM-5. Amsterdam: Boom; 2014.
Google Scholar
Asadi-Lari M, Tamburini M, Gray D. Patients’ needs, satisfaction, and health related quality of life: towards a comprehensive model. Health Qual Life Outcomes. 2004;2:1–15.
Bagchus C, Dedding C, Bunders JFG. “I”m happy that I can still walk’—participation of the elderly in home care as a specific group with specific needs and wishes. Health Expect. 2014;18(6):1–9.
Barratt A. Evidence based medicine and shared decision making: the challenge of getting both evidence and preferences into health care. Patient Educ Couns. 2008;73(3):407–12.
Bensing J. Bridging the gap. The separate worlds of evidence-based medicine and patient-centered medicine. Patient Educ Couns. 2000;39:17–25.
Article CAS Google Scholar
Boote J, Baird W, Beecroft C. Public involvement at the design stage of primary health research: a narrative review of case examples. Health Policy. 2010;95(1):10–23.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Broerse J, Zweekhorst M, van Rensen A, de Haan M. Involving burn survivors in agenda setting on burn research: an added value? Burns. 2010;36(2):217–31.
Caron-Flinterman JF, Broerse JEW, Bunders JFG. The experiential knowledge of patients: a new resource for biomedical research? Soc Sci Med. 2005;60(11):2575–84.
Darlenski RB, Neykov NV, Vlahov VD, Tsankov NK. Evidence-based medicine: facts and controversies. Clin Dermatol. 2010;28(5):553–7.
de Graaf R, ten Have M, van Gool C, van Dorsselaer S. Prevalence of mental disorders and trends from 1996 to 2009. Results from the Netherlands Mental Health Survey and Incidence Study-2. Soc Psychiatry Psychiatr Epidemiol. 2012;47(2):203–13.
Elberse J, Pittens C, de Cock Buning T, Broerse J. Patient involvement in a scientific advisory process: setting the research agenda for medical products. Health Policy. 2012;107(2–3):231–42.
Fajutrao L, Locklear J, Priaulx J, Heyes A. A systematic review of the evidence of the burden of bipolar disorder in Europe. Clin Pract Epidemiol Ment Health. 2009;5(1):3.
Fisher A, Manicavasagar V, Sharpe L, Laidsaar-Powell R, Juraskova I. A qualitative exploration of patient and family views and experiences of treatment decision-making in bipolar II disorder. J Ment Health. 2017;27(1):66–79.
Goodwin FK, Jamison KR. Manic-depressive illness: bipolar disorder and recurrent depression. 2nd ed. New York: Oxford University Press; 2007.
Goossens P, Knoopert-van der Klein E, Kroon H, Achterberg T. Self reported care needs of outpatients with a bipolar disorder in the Netherlands: a quantitative study. J Psychiatr Ment Health Nurs. 2014;14:549–57.
Granek L, Danan D, Bersudsky Y, Osher Y. Living with bipolar disorder: the impact on patients, spouses, and their marital relationship. Bipolar Disord. 2016;18(2):192–9.
Guyatt G, Cairns J, Churchill D, Cook D, Haynes B, Hirsh J, Irvine J, Levine M, Levine M, Nishikawa J, Sackett D, Brill-Edwards P, Gerstein H, Gibson J, Jaeschke R, Kerigan A, Neville A, Panju A, Detsky A, Enkin M, Frid P, Gerrity M, Laupacis A, Lawrence V, Menard J, Moyer V, Mulrow C, Links P, Oxman A, Sinclair J, Tugwell P. Evidence-based medicine: a new approach to teaching the practice of medicine. JAMA. 1992;268(17):2420–5.
Huxley N, Baldessarini R. Disability and its treatment in bipolar disorder patients. Bipolar Disord. 2007;9(1–2):183–96.
Iancu SC. New dynamics in mental health recovery and rehabilitation. Amsterdam: Vu University; 2013.
Iancu SC, Zweekhorst MBM, Veltman DJ, Van Balkom AJLM, Bunders JFG. Mental health recovery on care farms and day centres: a qualitative comparative study of users’ perspectives. Disabil Rehabil. 2014;36(7):573–83.
IsHak WW, Brown K, Aye SS, Kahloon M, Mobaraki S, Hanna R. Health-related quality of life in bipolar disorder. Bipolar Disord. 2012;14(1):6–18.
Kuper A, Lingard L, Levinson W. Critically appraising qualitative research. BMJ. 2008;337(7671):687–9.
Larsson IE, Sahlsten MJM, Sjöström B, Lindencrona CSC, Plos KAE. Patient participation in nursing care from a patient perspective: a grounded theory study. Scand J Caring Sci. 2007;21(3):313–20.
Lloyd C, Waghorn G, Williams PL. Conceptualising recovery in mental health. Br J Occup Ther. 2008;71:321–8.
Maassen EF, Schrevel SJC, Dedding CWM, Broerse JEW, Regeer BJ. Comparing patients’ perspectives of “good care” in Dutch outpatient psychiatric services with academic perspectives of patient-centred care. J Ment Health. 2016;26(1):1–11.
Maassen EF, Regeer BJ, Bunders JGF, Regeer EJ, Kupka RW. A research agenda for bipolar disorder developed from a patient’s perspective. J Affect Disord. 2018;239:11–17. https://doi.org/10.1016/j.jad.2018.05.061 .
Article PubMed Google Scholar
MacQueen GM, Young LT, Joffe RT. A review of psychosocial outcome in patients with bipolar disorder. Acta Psychiatr Scand. 2001;103(3):163–70.
Malmström E, Hörberg N, Kouros I, Haglund K, Ramklint M. Young patients’ views about provided psychiatric care. Nord J Psychiatry. 2016;70(7):521–7.
MaxQDA [Internet]. Available from: https://www.maxqda.com/ . Accessed 2 Aug 2018.
Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Soc Sci Med. 2000;51(7):1087–110.
Michalak EE, Hole R, Livingston JD, Murray G, Parikh SV, Lapsley S, et al. Improving care and wellness in bipolar disorder: origins, evolution and future directions of a collaborative knowledge exchange network. Int J Ment Health Syst. 2012;6:16.
Mills I, Frost J, Cooper C, Moles DR, Kay E. Patient-centred care in general dental practice—a systematic review of the literature. BMC Oral Health. 2014;14(1):64.
Misak CJ. Narrative evidence and evidence-based medicine. J Eval Clin Pract. 2010;16(2):392–7.
Neogi R, Chakrabarti S, Grover S. Health-care needs of remitted patients with bipolar disorder: a comparison with schizophrenia. World J Psychiatry. 2016;6(4):431–41.
Nestsiarovich A, Hurwitz NG, Nelson SJ, Crisanti AS, Kerner B, Kuntz MJ, et al. Systemic challenges in bipolar disorder management: a patient-centered approach. Bipolar Disord. 2017;19(8):676–88.
Netwerk Kwaliteitsontwikkeling GGZ. Zorgstandaard Bipolaire stoornissen. 2017;1–54.
Newnham EA, Page AC. Bridging the gap between best evidence and best practice in mental health. Clin Psychol Rev. 2010;30(1):127–42.
Pittens C, Noordegraaf A, van Veen S, Broerse J. The involvement of gynaecological patients in the development of a clinical guideline for resumption of (work) activities in the Netherlands. Health Expect. 2013;18:1397–412.
Rusner M, Carlsson G, Brunt D, Nyström M. Extra dimensions in all aspects of life—the meaning of life with bipolar disorder. Int J Qual Stud Health Well-being. 2009;4(3):159–69.
Rycroft-Malone J, Seers K, Titchen A, Harvey G, Kitson A, McCormack B. What counts as evidence in evidence-based practice? J Adv Nurs. 2004;47(1):81–90.
Sackett D, Rosenberg W, Gray J, Haynes R, Richardson W. Evidence based medicine: what it is and what it isn’t. Br Med J. 1996;312(7023):71–2.
Scholl I, Zill JM, Härter M, Dirmaier J. An integrative model of patient-centeredness—a systematic review and concept analysis. PLoS ONE. 2014;9(9):e107828.
Schrevel SJC. Surrounded by controversy: perspectives of adults with ADHD and health professionals on mental healthcare. Amsterdam: VU University; 2015.
Sidani S, Fox M. Patient-centered care: clarification of its specific elements to facilitate interprofessional care. J Interprof Care. 2014;28(2):134–41.
Skelly N, Schnittger RI, Butterly L, Frorath C, Morgan C, McLoughlin DM, et al. Quality of care in psychosis and bipolar disorder from the service user perspective. Qual Health Res. 2013;23(12):1672–85.
Stange KC. The problem of fragmentation and the need for integrative solutions. Ann Fam Med. 2009;7(2):100–3.
Strejilevich SA, Martino DJ, Murru A, Teitelbaum J, Fassi G, Marengo E, et al. Mood instability and functional recovery in bipolar disorders. Acta Psychiatr Scand. 2013;128(3):194–202.
Tait L. Encouraging user involvement in mental health services. Adv Psychiatr Treat. 2005;11(3):168–75.
Teunissen T, Visse M, De Boer P, Abma TA. Patient issues in health research and quality of care: an inventory and data synthesis. Health Expect. 2011;16:308–22.
van der Stel. Het begrip herstel in de psychische gezondheidzorg, Leiden; 2015. p. 1–3.
Van Der Voort TYG, Van Meijel B, Hoogendoorn AW, Goossens PJJ, Beekman ATF, Kupka RW. Collaborative care for patients with bipolar disorder: effects on functioning and quality of life. J Affect Disord. 2015;179:14–22.
Yasuyama T, Ohi K, Shimada T, Uehara T, Kawasaki Y. Differences in social functioning among patients with major psychiatric disorders: interpersonal communication is impaired in patients with schizophrenia and correlates with an increase in schizotypal traits. Psychiatry Res. 2017;249:30–4.
Download references
Authors’ contributions
EFM designed the study, contributed to the data collection, managed the analysis and wrote the first draft of the manuscript. BJR designed the study and contributed to the data collection, data analysis, and writing of the manuscript. JFGB contributed to the study design and critical revision of the manuscript. EJR contributed to the study conception and critical revision of the manuscript. RWK contributed to the study design, acquisition of data, and critical revision of the manuscript. All authors contributed to the final manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
The authors received no financial support for the research.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and affiliations.
Athena Institute, Faculty of Earth and Life Sciences, VU University Amsterdam, Boelelaan 1085, 1081HV, Amsterdam, Netherlands
Eva F. Maassen, Barbara J. Regeer & Joske F. G. Bunders
Altrecht Institute for Mental Health Care, Nieuwe Houtenseweg 12, 3524 SH, Utrecht, Netherlands
Eva F. Maassen, Eline J. Regeer & Ralph W. Kupka
Amsterdam Public Health Research Institute, Amsterdam UMC, Vrije Universiteit Amsterdam, Psychiatry, De Boelelaan 1117, Amsterdam, Netherlands
Ralph W. Kupka
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Eva F. Maassen .
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Reprints and permissions
About this article
Cite this article.
Maassen, E.F., Regeer, B.J., Regeer, E.J. et al. The challenges of living with bipolar disorder: a qualitative study of the implications for health care and research. Int J Bipolar Disord 6 , 23 (2018). https://doi.org/10.1186/s40345-018-0131-y
Download citation
Received : 06 June 2018
Accepted : 22 August 2018
Published : 06 November 2018
DOI : https://doi.org/10.1186/s40345-018-0131-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- General Healthcare
- Personal Recovery
- Focus Group Discussions
- Professional-patient Interaction
Bipolar Disorder: Causes, Symptoms and Facts Research Paper
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Introduction
Atypical antipsychotic medications, antidepressant medications, works cited.
Bipolar disorder is a medical condition that affects an estimated two million people in the US. It affects both women and men in equal measure. The disorder is associated with many causes some of which are genetic while others result from other factors. However, the exact cause of the disorder has not yet been established.
In its initial stages, the condition has signs and symptoms that are easily identified. It is advisable for individuals to seek medical attention before the mild stages of the disease develop into full-blown bipolar disorder. There are various medications that have been approved as viable treatments for the condition.
Bipolar disorder is defined as a mood disorder where individuals suffering from the disorder show alternate moments of mania and depression. The manic moments are characterized by moods that are better than normal ones. The moods are mild but they may sometimes be extreme to the extent that they interfere with normal life.
It may take hours, weeks or months for the manic moments to disappear after which depression returns (Definition of Bipolar disorder 5). Bipolar disorder is also referred to as manic-depressive disorder. When individuals experience depression, they have feelings of sadness and hopelessness followed by loss of interest in activities they derive pleasure from.
The mood shift to the other direction is characterized by feelings of euphoria and a lot of energy. In some rare instances, symptoms of both mania and depression manifest themselves simultaneously in individuals who suffer from bipolar disorder.
Despite the fact that the disorder causes disruption and often takes long to recover from, individuals can maintain their moods by adhering to certain treatment procedures. Mostly, the disorder is controlled through psychotherapy or psychological counseling and taking prescribed medicines (Treatment for Bipolar Disorder 6).
The cause of bipolar disorder has not been completely established, but it is a common problem in families. Depressive or manic disorders may be manifest for the first time at teenage or early adulthood. The symptoms are usually subtle and confounding. Individuals who suffer from the disorder are usually ignored or misdiagnosed hence compelling them to undergo unjustified suffering. On the other hand, those who receive the right treatment and assistance lead normal and fulfilling lives.
Types of Bipolar Disorders
There are different subtypes of bipolar disorders with each disorder exhibiting its unique pattern of initial symptoms. The different subtypes include the following.
Bipolar I Disorder
The mood fluctuations associated with this type of bipolar disorder lead to significant hardships when performing normal jobs or interference with relationships. The manic periods of this subtype can be extreme to the extent that they lead to harmful outcomes.
Bipolar II Disorder
This subtype of bipolar disorder is not as severe as bipolar I. Individuals who suffer from this type may experience elevation in their moods, a sense of irritation and changes in the way they function, but generally their daily life routines are not affected in any way. Instead of mania showing itself full-blown, individuals experience hypomania which is not as severe as mania. Moments of depression in this bipolar disorder usually take a longer period of time than in bipolar I.
Cyclothymic Disorder
This subtype of bipolar disorder which is also referred to as cyclothymia is mild in nature. With this type of disorder, the moments of depression and hypomania may be disruptive. However, the high and low instances are less severe than the ones experienced in bipolar I and bipolar II.
Myths and Facts about Bipolar Disorder
There are different myths and facts related to bipolar disorder. The first myth associated with the disorder is that individuals who suffer from the condition do not recover or live normal lives. The fact regarding this myth is that many individuals who suffer from the condition succeed in their careers, lead fulfilling family lives and have successful relationships.
To live with the condition is a challenging situation. But in the presence of the right treatment, healthy skills to cope with the condition and appropriate support systems, individuals live and manage bipolar disorder well.
The second myth surrounding bipolar disorder is that individuals who suffer from the condition are always either in depression or in a manic situation. The fact is that moments of depression among individuals who suffer from bipolar disorder are common than moments of mania. It is also possible for manic to be mild such that it is not recognized. Individuals who suffer from bipolar disorder can also stay with the conditions for long periods without portraying any symptoms (Bipolar Disorder 4).
The third myth related to bipolar disorder is that the only thing that is affected by the disorder is the mood. The fact is that the condition also affects other aspects in the lives of individuals who suffer from the condition. For instance, the condition is linked with anxiety, health problems like heart diseases, diabetes and issues that touch on blood pressure.
The fourth myth related to bipolar disorder is that the only remedy for the condition is medication. The fact is that medication forms the basis of attempts to treat bipolar disorder but this does not mean that there are no other methods that are used to treat the disorder.
Self-help strategies and therapy are methods that play a crucial role in dealing with bipolar disorder. Individuals who detect symptoms of bipolar disorder can control the situation through regular exercises, eating well, sleeping enough, checking their moods regularly and staying close to people who can support them. They can also ensure that they avoid anything that causes them stress.
Signs and Symptoms of Bipolar Disorder
Bipolar disorder appears differently in different individuals. The symptoms of the condition vary in frequency, severity and their pattern. Some individuals experience frequent moments of depression or mania, while others have equal alternations between depression and mania.
Some individuals experience disruption of their moods frequently while others do not experience as many mood disruptions throughout their lives. Bipolar disorder is characterized by four different types of mood episodes which include depression, hypomania, mania and mixed episodes.
Signs and Symptoms of Mania
During the manic stage of bipolar disorder, individuals experience increase in their energy, euphoria and a sense of creativity. They are usually very talkative, fail to get sleep and exhibit signs of hyperactivity. They also have feelings of being in possession of great power or headed for great things.
But while individuals who experience mania feel nice at first, they soon become uncontrollable. They often behave in a reckless manner during this phase, engaging in unbecoming behavior such as irresponsible sexual activities, gambling away financial resources, or investing foolishly.
In addition, they are easily angered, become aggressive and irritable which causes them to pick fights with individuals who do not show willingness to cooperate with them. They lay blames on other people once their behavior is questioned. Some even suffer from delusions and begin to respond to imaginary voices (Bipolar Disorder 6)
Symptoms of Hypomania
Hypomania is usually not as severe as mania. Individuals who experience hypomania feel energetic, euphoric and highly productive, but have the capacity to continue with their normal daily activities without losing touch with reality. Some people may look at hypo manic individuals as people who exhibit abnormally good moods.
However, the condition leads to wrong decisions which are detrimental to careers, relationships and reputation of individuals. In addition, the condition grows to complete mania or serious depressive disorder afterwards. Individuals who suffer from hypomania show the following signs and symptoms
The first sign of hypomania is that individuals who suffer from the condition are characterized by rapid talk that other people find difficult to cope with. The second symptom of the condition is that individuals engage in reckless actions with little regard of the consequences.
The third symptom is that victims of hypomania are easily distracted and it is difficult for them to concentrate in what they do. The fourth symptom of hypomania is that the individuals sleep for few hours and feel abnormally energetic. The fifth symptom of the condition is that individuals who suffer from hypomania exhibit impaired judgment. The sixth symptom of the condition is that the individuals have unrealistic beliefs concerning their powers and capabilities.
Signs and Symptoms of Bipolar Depression
Bipolar and regular forms of depression were not in the past considered as different conditions. However, research continuously highlights major differences between the two conditions with emphasis on the treatments recommended to deal with the conditions.
Majority of individuals who suffer from bipolar depression do not get help from the use of antidepressants. Antidepressants are considered risky since they have the potential to make the condition worse. They trigger hypomania or mania, leads to mood swings, or interferes with other drugs that stabilize mood.
Although the two share several similarities, there are certain symptoms that appear more in individuals who suffer from bipolar depression than those with regular depression. For instance, bipolar depression often involves guilt, irritability, random mood changes and restlessness.
Individuals who suffer from the condition are also slow in movement and speech, sleep for many hours and add weight regularly. In addition, their chances of losing touch with reality are high and interference in their works and functioning at the societal level. Some of the common symptoms associated with bipolar depression include lack of pleasure, irritability, changes in weight or appetite, energy loss, hopelessness, memory and concentration challenges, suicidal thoughts and problems in sleeping (Castle 81).
Signs and Symptoms of Mixed Episode
The mixed episode is a combination of symptoms of depression and hypomania or mania. The common symptoms of this disorder include irritability, insomnia, anxiety, racing thoughts and depression that has elements of agitation. This scenario where individuals experience moments of high energy but are lower in moods is a dangerous one since it is characterized by high suicidal thoughts.
Causes of Bipolar Disorder
The causes of bipolar disorder are not yet known. Research shows that certain individuals genetically run high risks of suffering from the condition. Yet not all individuals who have inherited susceptibility actually develop the condition. This implies that there are other causes of the illness apart from genes.
Neurochemical, genetic and environmental factors are believed to play a crucial role that initiates and enables bipolar disorder to progress. The prevailing thoughts on the cause of bipolar disorder are that it is a biological disorder that affects specific brain sections and is caused by inappropriate functioning of neurotransmitters.
The external psychological and environmental factors that aid bipolar disorder development are known as triggers. They can cause new depression and mania episodes or worsen already existing ones. However, most episodes of bipolar disorder do not require an obvious trigger. Although there is no known cause of bipolar disorder, the following clues are believed to be causes of bipolar disorder by researchers.
Genetic Causes
Researchers have found out that bipolar disorder is mostly familial. This means that the condition runs in families. Almost half of individuals who suffer from bipolar disorder come from families with members who exhibit mood disorders like depression. Individuals who have one parent who suffers from bipolar disorder have between 15 and 25 percent likelihood of suffering from the same condition while the risk of non-identical twins suffering from the condition is 25 percent.
The risk of suffering from bipolar disorder for individuals who have identical twins with bipolar disorder in their families is even higher. Researchers who carry out studies on adopted children have been able to gather more information about the environmental versus genetic and events in normal lives that cause bipolar disorder.
Neurochemical Causes
Bipolar disorder is essentially a biological disorder which affects specific brain sections as a result of particular neurotransmitters functioning inappropriately. It may also be as a result of dysfunction of chemical messengers found in the brain. Some of the neurotransmitters involved with the chemicals include serotonin and many others. The condition may remain dormant until it is triggered by external factors.
Environmental Causes
There are certain environmental factors that are not fully understood that are associated with changes in the age that bipolar disorder starts. Occurrence of the disorder at early ages is associated with issues such as misdiagnosis and puts young people at the risk of contracting the illness. In addition, bipolar disorder may be caused by life events that lead to mood episodes. Despite the fact that substance abuse does not primarily cause bipolar disorder, it interferes with the process of recovery.
Medication-triggered Mania
Certain medications like antidepressants have the capacity to stir manic episodes among individuals who are susceptible to bipolar disorder. This calls for exhaustive treatment for depressive disorders among individuals who once experienced manic disorders.
Due to the fact that depressive episodes have the potential of turning into manic ones after antidepressant medications, it is usually advisable to take antimanic drugs to limit the chances of occurrence of manic episodes. Antimanic drugs develop a partial ceiling that makes it difficult for mania induced by antidepressants to develop. There are other medications that are associated with high feelings that are similar to mania.
For example, appetite suppressants may cause an increase in energy levels, lack of sleep and cause individuals to talk a lot. Individuals return to normalcy once they stop the medications. Some of the substances that are associated with manic-like episodes include excessive caffeine, overdoses of certain drugs obtained over the counter and use of illegal drugs like cocaine and designer drugs (Castle 82).
Bipolar disorder can be caused by stressful experiences for individuals whose genetic composition makes them vulnerable to the illness. Stressful events that involve spontaneous or drastic changes either bad or good may trigger bipolar disorder. Some of the events include marriage, job loss, loss of family members or change of location. Individuals who are vulnerable to bipolar disorder should avoid stressful events, stimulants like alcohol and inadequate sleep because these factors trigger bipolar disorder.
Treatment and Medication of Bipolar Disorder
Bipolar disorder is a condition that can be treated contrary to what some individuals believe that the condition cannot be treated. The following are some of the medications available for treating bipolar disorder. Mood Stabilizing Medications
Mood stabilizing medication is usually the first option to treat bipolar disorder. Individuals who suffer from the condition are exposed to the use of mood stabilizers for several years. Most of the medications fall under the category of anticonvulsants with an exception of lithium. Ideally, anticonvulsants are used in the treatment of seizures but control of moods is their other function. There are several mood stabilizing medications used in the treatment of bipolar disorder.
The first mood stabilizer used in treatment of bipolar disorder is lithium which is also referred to as lithobid or eskalith. It was the first medication for mood-stabilizing that FDA approved for use in treatment of mania. It is an effective medication for dealing with mania and prevention of other depressive complications.
The second mood stabilizer used in treatment of bipolar disorder is valproic acid which is used in place of lithium. Just like lithium, it is also an effective method of treating the disorder. In recent years, lamotrigine which is an anticonvulsant has been introduced as a mood stabilizer for treating bipolar disorder.
This is another common medication for bipolar disorder. The medication is combined with other forms of medication. There are atypical and conventional antipsychotics used in treatment of bipolar disorder. The first antipsychotic medication used in treatment of bipolar disorder is Olanzapine which is administered together with antidepressant medication.
It helps in reducing the effects of serious mania. The second antipsychotic used in the treatment of bipolar disorder is Aripiprazole which treats mixed episode of manic disorders. The third antipsychotic used in the treatment of bipolar disorder is Quetiapine. This eliminates the symptoms associated with sudden and severe manic instances (Leay 130).
Antidepressants are occasionally used in the treatment of depression as a form of bipolar disorder. The medications are combined with mood-stabilizers. It is advisable to combine them with mood stabilizers because using them alone may cause individuals to switch into hypomania or mania.
Bipolar disorder is a medical condition that affects both young people and adults. There are different subtypes of bipolar disorder which exhibit different characteristics. Some are characterized by extreme cases of mania such that the normal functioning of individuals is affected while other types are mild and do not affect the normal functioning of individuals.
Bipolar disorder is a condition that is surrounded by myths but for every myth surrounding the condition, there are proven facts. Despite the fact that some individuals argue that the condition cannot be treated and that those who suffer from it cannot functionally normally, it has been proven that bipolar disorder is treatable. Individuals who suffer from the condition can also lead normal lives.
Bipolar Disorder. 2012. Web.
Castle, Lana. Bipolar Disorder Demystified:Mastering the Tightrope of Manic Depression. New York: Da Capo Press, 2003.
Definition of Bipolar disorder 2011. Web.
Leay, Robert. Psychological Treatment of Bipolar Disorder. New York: Guilford Press, 2005.
Treatment for Bipolar Disorder . n.d. Web.
- Bipolar Expeditions: Mania and Depression
- The Psychopathology of Bipolar Disorder
- Bipolar Disorder and Current Treatment Options
- Anorexia as Eating Disorder
- Bipolar Disorder Symptoms and Treatments
- Physical Health and Its Relations to Schizophrenia
- Major Depressive Disorder (MDD)
- Everything You Need to Know About ADHD
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2018, June 21). Bipolar Disorder: Causes, Symptoms and Facts. https://ivypanda.com/essays/bipolar-disorder-2/
"Bipolar Disorder: Causes, Symptoms and Facts." IvyPanda , 21 June 2018, ivypanda.com/essays/bipolar-disorder-2/.
IvyPanda . (2018) 'Bipolar Disorder: Causes, Symptoms and Facts'. 21 June.
IvyPanda . 2018. "Bipolar Disorder: Causes, Symptoms and Facts." June 21, 2018. https://ivypanda.com/essays/bipolar-disorder-2/.
1. IvyPanda . "Bipolar Disorder: Causes, Symptoms and Facts." June 21, 2018. https://ivypanda.com/essays/bipolar-disorder-2/.
Bibliography
IvyPanda . "Bipolar Disorder: Causes, Symptoms and Facts." June 21, 2018. https://ivypanda.com/essays/bipolar-disorder-2/.

IMAGES
VIDEO
COMMENTS
The death of a loved one or an instance of abuse can serve as a trigger for the condition. Implications of Diagnosing and Treating Patients With Bipolar Disorder. The purpose of this essay is to examine a variety of legal, ethical, and cultural implications in treating patients with bipolar disorder.
Thesis Statement for Bipolar Depression. Bipolar depression is a complex mental health condition that affects millions of people worldwide. This disorder is characterized by extreme mood swings, ranging from manic highs to depressive lows, and can have a significant impact on the individual's daily life, relationships, and overall well-being.
Conclusion. Bipolar disorder is a mental disorder that is characterized by extreme mood changes that range from mania to depression. Risk factors include lifestyle, genetics, environment, drug and alcohol abuse, and major life changes such as death or abuse. Symptoms depend on the type of mod.
Purpose Statement: To inform about what is the cause of bipolar depression, and how you can treat it. Thesis: The bipolar disorder is a cause of the depressive moods or lows of mental disorder. Introduction. Attention Getter: Sometimes we all have bad days, and even good days, but these sudden changes in our mind and body is not just a simple ...
Thesis Statement for Bipolar Disorder. Topics: Bipolar Disorder Human Brain Mental Illness. Words: 2233. Pages: 5. This essay sample was donated by a student to help the academic community. Papers provided by EduBirdie writers usually outdo students' samples.
Bipolar disorder is a complex condition that involves various biological, genetic, and environmental factors. It affects approximately 2.8% of U.S. adults, according to the National Institute of Mental Health. The onset of bipolar disorder usually occurs in late adolescence or early adulthood, although it can manifest at any age.
Background. Bipolar disorder (BD) is a major mood disorder characterized by recurrent episodes of depression and (hypo)mania (Goodwin and Jamison 2007).According to the Diagnostic and Statistical Manual 5 (DSM-5), the two main subtypes are BD-I (manic episodes, often combined with depression) and BD-II (hypomanic episodes, combined with depression) (APA 2014).
Bipolar is a mental illness that affects an individual's mood causing fluctuations in energy and activity levels (Chengappa & Gershon, 2013). Bipolar is also known as manic-depressive illness and its effects can abhorrently affect personal relationship with others. Patients suffering from the bipolar disorder exhibit exaggerated mood changes ...
The term 'bipolar disorder' (or 'bipolar affective disorder') is thought to be less stigmatizing than the older term 'manic-depressive illness', and so the former has largely superseded the latter. However, some psychiatrists and some people with bipolar disorder still prefer the term 'manic-depressive illness' because they
2 Understanding Bipolar Disorder: Symptoms, Impact, and Treatment Approaches. Abstract Bipolar disorder is a chronic mental illness. This is an illness that several Americans have and suffer from each year. Bipolar disorder may be triggered by unfortunate events and stressful experiences. Mood swings usually accompany this disorder.
Struggling with crafting a thesis statement on bipolar disorder is challenging due to the topic's complexity, requiring extensive research and synthesis. Bipolar disorder, characterized by alternating periods of mania and depression, has a multifaceted nature that is difficult to capture fully in a thesis statement. Seeking assistance from experienced professionals can help streamline the ...
22 essay samples found. Bipolar disorder is a mental health condition characterized by extreme mood swings between emotional highs (mania or hypomania) and lows (depression). Essays on this topic could explore the symptoms, diagnosis, and treatment options for bipolar disorder. Additionally, discussions might extend to the impact of bipolar ...
Bipolar disorder has been described by those who experience it as a double-edged sword. Alongside periods of fluctuating (hypo)manic or depressive moods, many people with bipolar disorder ...
Bipolar disorder is a complex illness that is difficult to correctly diagnosis and treat. Experts estimate that a correct diagnosis and treatment for bipolar disorder may be delayed for up to 7-10 years after symptoms become problematic. The primary purpose of this study was to identify the complexity of diagnosing bipolar disorder, including
Published: 01/31/2020. Bipolar disorder (manic-depressive disorder) is a severe and highly morbid recurrent mood disorder. The prevalence of the disorder is 1.3% to 1.6% while its mortality rate is 2 to 3 times higher compared to that of the general population. The suicidal rate among bipolar disorder patients is about 10-20%.
Writing a thesis on bipolar disorder presents many challenges due to the complexity of the topic and need for extensive research. Bipolar disorder involves extreme mood swings between mania/hypomania and depression, requiring an understanding of psychology, psychiatry, neuroscience, and sociology. Students struggle with synthesizing the vast research and developing a clear thesis statement ...
between Bipolar Disorder and ... COPYRIGHT STATEMENT I. The author of this thesis (including any appendices and/ or schedules to this thesis) ... provided overall supervision for the thesis which included reading drafts of the manuscript. The author intends to publish the review paper in 'Bipolar Disorders - An International Journal
Thesis Statement Examples for Bipolar Disorder - Free download as PDF File (.pdf), Text File (.txt) or read online for free. Scribd is the world's largest social reading and publishing site.
Bipolar disorder (BD) is a major mood disorder characterized by recurrent episodes of depression and (hypo)mania (Goodwin and Jamison 2007).According to the Diagnostic and Statistical Manual 5 (DSM-5), the two main subtypes are BD-I (manic episodes, often combined with depression) and BD-II (hypomanic episodes, combined with depression) (APA 2014).
Bipolar disorder is defined as a mood disorder where individuals suffering from the disorder show alternate moments of mania and depression. IvyPanda® Free Essays. ... Thesis Statement Generator. Problem Statement Generator. Introduction to Research Generator. Informative Essay Thesis Generator.
Download. Bipolar Disorder, also known as a manic depressive illness, is classified as a brain disorder; that causes unusual shifts in the mood, energy, activity levels, and the ability to carry-out day to day tasks. The majority of bipolar individuals experience alternating episodes of mania such as an elevated or euphoric mood or irritable ...
Thesis Statement for Bipolar Disorder Research Paper - Free download as PDF File (.pdf), Text File (.txt) or read online for free. thesis statement for bipolar disorder research paper
Thesis Statement Bipolar Disorder - Free download as PDF File (.pdf), Text File (.txt) or read online for free.
Bipolar Thesis Statement - Free download as PDF File (.pdf), Text File (.txt) or read online for free.