Follow us on social media
- See us on facebook
- See us on twitter
- See us on youtube
- See us on instagram
- See us on linkedin

Stanford Comprehensive Epilepsy Program Research

While each member of our team is involved in various clinical or basic science research projects, there are four active laboratories in the Stanford Comprehensive Epilepsy Program where investigators conduct systematic research. These laboratories are led by four of the faculty members in our program and funded by the National Institute of Health.
Buckmaster, Paul, DVM, PhD
Temporal lobe epilepsy is common, frequently refractory to treatment, and devastating to those affected. Our long-term goal is to better understand the pathophysiological mechanisms of this disease so that rational and effective therapies can be developed. We use electrophysiological, molecular, and anatomical techniques to evaluate neuronal circuitry in normal and in epileptic brains.
Huguenard, John, PhD
We are interested in the neuronal mechanisms that underlie synchronous oscillatory activity in the thalamus, cortex and the massively interconnected thalamocortical system. Such oscillations are related to cognitive processes, normal sleep activities and certain forms of epilepsy.
Our approach is an analysis of the discrete components that make up thalamic and cortical circuits, and reconstitution of components into both in vitro biological and in silico computational networks. Accordingly, we have been able to identify genes whose products, mainly ion channels, play key roles in the regulation of thalamocortical network responses.
Nuyujukian, Paul, MD, PhD (Brain Interfacing Laboratory)
The Brain Interfacing Laboratory is interested in the applicability of brain-machine interfaces as a platform technology for a variety of brain-related medical conditions, particularly stroke and epilepsy. This research spans both preclinical models and human clinical studies.
With respect to epilepsy, we are looking to better characterize and model seizures from patients with refractory epilepsy so that we may provide better treatments. In particular, we are seeking to develop statistical techniques to predict seizures.
Parvizi, Josef, MD, PhD (Laboratory of Behavioral and Cognitive Neuroscience)
The general theme of our research is the study of the human brain from clinical and system neuroscience perspective using the tools of intracranial electrocorticography (ECoG), electrical brain stimulation (EBS), and functional imaging (fMRI). The main impetus for our research is to understand the anatomical and physiological signatures of behavioral expression and cognitive experience in humans and how these might be broken in patients with epilepsy. Using our sophisticated research tools, our goal is to help patients with uncontrolled epilepsy to gain seizure freedom without cognitive deficits.
Prince, David, MD
Work in the Prince lab has focused on normal and abnormal regulation of excitability in neurons of mammalian cerebral cortex and thalamus and mechanisms underlying development and prophylaxis of epilepsy in animal models. Long-term goals are to understand how cortical injury and other pathological processes induce changes in structure and function of neurons and neuronal networks that lead to hyperexcitability and epileptogenesis. With this information, it will be possible to devise experimental strategies to prevent the occurrence of epilepsy after cortical injury and eventually apply them to individuals with significant brain trauma. We have already provided a proof in principal that prophylaxis of posttraumatic epilepsy is possible, using a rat model.
Ivan Soltesz, PhD
Dr. Soltesz's laboratory employs a combination of closely integrated experimental and theoretical techniques, including closed-loop in vivo optogenetics, paired patch clamp recordings, in vivo electrophysiological recordings from identified interneurons in awake mice, 2-photon imaging, machine learning-aided 3D video analysis of behavior, video-EEG recordings, behavioral approaches, and large-scale computational modeling methods using supercomputers. He is the author of a book on GABAergic microcircuits (Diversity in the Neuronal Machine, Oxford University Press), and editor of a book on Computational Neuroscience in Epilepsy (Academic Press/Elsevier). He co-founded the first Gordon Research Conference on the Mechanisms of neuronal synchronization and epilepsy, and taught for five years in the Ion Channels Course at Cold Springs Harbor. He has over 30 years of research experience, with over 20 years as a faculty involved in the training of graduate students (total of 16, 6 of them MD/PhDs) and postdoctoral fellows (20), many of whom received fellowship awards, K99 grants, joined prestigious residency programs and became independent faculty.
The University of Chicago neuroscience community is host to a diverse group of researchers investigating epilepsy and seizure disorders. The faculty of Department of Neurology play a key role in this research, conducting critical clinical and neurophysiological studies, and providing valuable collaborations with the neuroscience researchers in other departments.
John Ebersole MD directs a research program aimed at:
- Clarifying the relationships between cerebral electrical activity and the resultant scalp EEG; and
- Developing and validating computational techniques of functional imaging and seizure localization using scalp, intracranial EEG, and magnetoencephalography (MEG).
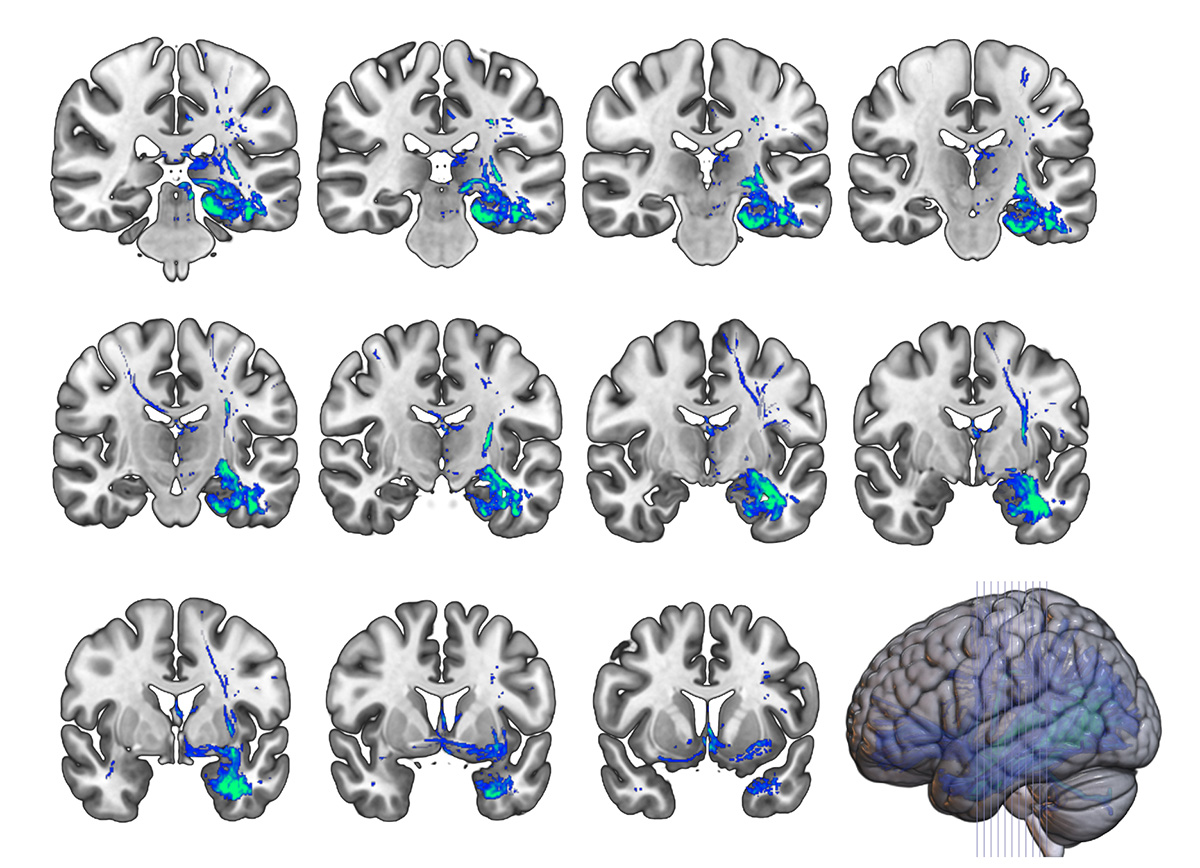
Over the past fifteen years research from his laboratory has established the usefulness of spike and seizure dipole modeling with both EEG and MEG in order to localize non-invasively epileptogenic foci in epilepsy surgery candidates. He is a foremost proponent of and authority on the use of source models in the evaluation of epilepsy. Ongoing projects include studies of the accuracy of dipole and other extended source models of epileptic foci using simultaneously recorded scalp and intracranial EEG, comparisons of real-time EEG imaging with other functional imaging techniques using three-dimensional co-registrations, and the development of a new spatio-temporal analysis technique for intracranial EEG utilizing field and source display on the patient’s reconstructed cortex. These direct applications of neurocomputational, neuroimaging, and electrical engineering developments to the evaluation of epileptic foci in the human brain are an example of translational research at its best.
James Tao MD PhD is interested in determining the cerebral substrates of scalp EEG epileptiform patterns, in order to improve the accuracy of non-invasive seizure localization during epilepsy surgery. His long-term interests include investigations of the mechanisms of epileptogenesis and of new modalities of epilepsy therapy. Current projects include:
- The impact of cerebral source area and synchrony on recording scalp EEG ictal patterns; and
- The pathophysiology of interictal temporal delta activity (ITDA) and its value in localizing epileptogenic zone.
His long term goals are to investigate the electrophysiological behavior of cerebral epileptogenic networks and the mechanism of epileptogenesis at the neural network level in order to identify new preventive and therapeutic modalities.
Wim Van Drongelen PhD (Department of Pediatrics) has focussed his research on the long-range goal of optimizing therapeutic intervention in pediatric epilepsy by improved spatial and temporal localization of seizure activity and examining the underlying mechanisms in the pathogenesis of seizures. His research focuses on:
- Underlying neuronal mechanisms in epilepsy (synchrony, recruitment, oscillation, weak coupling);
- Relationships between neuronal activity at different scales (neuron, network, brain);
- Detection and prediction of brain electrical activity during seizures using various signal processing techniques (correlation dimension, Kolmogorov entropy, wavelet analysis);
- Localization of sources from surface recordings (dipole analysis, MUSIC, LORETA, spatial filtering); and
- Monitoring of the nervous system in the intensive care environment (EEG, evoked potential
James Tao, MD, PhD.
Sandra Rose, MD
Shasha Wu, MD, PhD.
Naoum P. Issa, MD, PhD.
Peter Warnke, MD, FRCS
David Frim, MD, PhD.
Maureen Lacy, PhD.
Vernon L. Towle, PhD.
Shadrach Castillo, RN
Diane Suarez, REEGT
The Comprehensive Epilepsy Center at the University of Chicago Medicine is at the forefront of epilepsy care. Many of our patients come to us after trying a number of different medications and therapies with little success.
Leading Advancements in Epilepsy Care
Backed by the development of groundbreaking diagnostic techniques and a long history of research, our expert team has the experience to manage nearly all epilepsy-related problems from new onset seizures to rare and difficult-to-treat epileptic syndromes. With non-invasive technology and contemporary diagnostic techniques, we can pinpoint the origin of most seizures with precision. Having this advantage can significantly increase diagnostic accuracy and improve patient outcomes.
Epilepsy is a chronic, non-communicable neurologic disorder defined by two or more unprovoked seizures. Provoked seizures result from some immediately recognizable stimulus (for example, low blood sugar in people with diabetes), while unprovoked seizures have no immediately recognizable cause. Provoked seizures are unlikely to recur if the provocations can be avoided; however, unprovoked seizures have the tendency to recur and are the hallmark of epilepsy. When someone has two or more seizures, doctors diagnose epilepsy.
Types of Epilepsy
There are many types of epilepsy. Some types of epilepsy and epilepsy syndromes include:
- Benign rolandic epilepsy
- Childhood absence epilepsy
- Doose syndrome (myoclonic astatic epilepsy of childhood)
- Frontal lobe epilepsy
- Infantile spasms
- Juvenile myoclonic epilepsy
- Landau-Kleffner syndrome
- Lennox-Gastaut syndrome
- Occipital lobe epilepsy
- Parietal lobe epilepsy
- Rasmussen's syndrome
- Sturge-Weber syndrome
- Temporal lobe epilepsy
- West syndrome
A seizure is a sudden surge of abnormal electrical activity in the brain. Electrical activity in the brain is normal. It’s how our brain works. Seizures occur when there is significant disruption of that normal electrical activity in the brain. The general symptoms of seizures may include changes in consciousness, sensation, movement or behavior.
Is a Seizure the Same Thing as Epilepsy?
No. Not all seizures are caused by epilepsy. Approximately 10 percent of the general population may experience a seizure during their lifetime, but only 1 percent of the population has epilepsy. A single seizure may or may not progress to a chronic and recurrent condition or epilepsy.
Although there are many types of seizures, those that people with epilepsy experience commonly fall into generalized and partial (or focal) seizures.
Generalized Seizures
Generalized seizures are characterized by widespread electrical discharges in both sides of the brain. You might think of it as a lightning storm in which the lightning seems to be coming from all areas of the sky at the same time.
There are six types of generalized seizures:
- Absence seizures are also known as petit mal seizures. When people experience an absence seizure, they may seem to disconnect from the world, blank out or stare into space for at least a few seconds. Their eyes may roll as well. People who have absence seizures usually lose awareness for a short time and have no memory of the seizure afterward. This type of seizure usually begins between the ages of 4 and 14, and it can resemble daydreaming. Subtle body movement may accompany the seizure, but it’s not the jerking movements that occur with tonic-clonic or clonic seizures.
- Atonic seizures , also known as drop attacks, drop seizures or akinetic epileptic drop attacks, may involve a sudden loss of muscle tone, a head drop or leg weakening. People suffering an atonic seizure may suddenly collapse. This type of seizure may also cause the person suffering it to drop objects.
- Clonic seizures include jerking muscle movements that are more rhythmic than chaotic. The muscle spasms typically affect the face, neck and arms. They may last for several minutes.
- Myoclonic seizures are typically short and involve uncontrollable jerking, usually of the arms and/or legs, and last for only a second or two
- Tonic-clonic seizures , also known as grand mal seizures, are what most people think of when they imagine a seizure. They involve a loss of consciousness, stiffening of the body and shaking or jerking, sometimes followed by loss of bladder or bowel control
- Tonic seizures include body stiffening, but do not include the clonic phase of uncontrolled jerking or spasms. Back, arm and leg muscles are affected most often. The seizure may cause a patient to fall or collapse.
Partial Seizures
Partial seizures, also known as focal seizures, begin in one side of the brain. They fall into one of two groups:
- Simple partial seizures (also known as simple focal seizures) may only include the aura stage (see below). During this type of seizure, awareness, memory and consciousness remain intact. This type of seizure may alter emotions or change the way things look, smell, feel, taste or sound. It may also result in involuntary jerking of a body part, such as an arm or leg, or spontaneous sensory symptoms, such as tingling, dizziness and flashing lights.
- Complex partial seizures (also known as psychomotor seizures) alter consciousness or responsiveness. The person having the seizure may appear to be staring into space or moving without purpose. Some common movements include hand rubbing, chewing, swallowing, and repetitive motion, such as bicycling leg movements or walking in a circle.
For some types of seizures, an aura happens before a seizure and may alert a person that a seizure may occur. Auras typically begin seconds before the seizure.
The symptoms that accompany an aura can vary depending on the type of seizure and the area of the brain affected. Some symptoms of aura include:
- Abnormal sensations
- Deja vu (familiar feelings) or jamais vu (unfamiliar feelings)
Distorted emotions, such as panic or fear
Forced thinking
Perceived sounds, tastes, or smells (some people report smelling burning rubber, for example)
Physical sensations, like dizziness, headache, numbness, and lightheadedness
- Unusual feelings
At UChicago Medicine, we offer an advanced treatment designed to prevent seizures before they start and often before a patient feels the aura. The NeuroPace Responsive Neurostimulation System (RNS) is a tiny device that detects abnormal brain activity and responds in real time to deliver short bursts of electrical stimulation designed to reduce how often seizures happen.
Similarly, deep brain stimulation (DBS) prevents seizures to spread throughout the brain and stops them from becoming clinically relevant. Neuromodulation is just one of the several treatment options we provide, from the latest anti-epileptic drugs to Visualase MRI-guided laser thermal ablation.
Ictus Stage
Ictus is another word for the seizure itself — the part of the seizure that outsiders can witness. It can be convulsive, commonly called “grand mal,” or non-convulsive, such as staring and inability to respond normally.
Postictal Stage
The postictal stage occurs after the ictus or active stage of the seizure. During the postictal stage, the body begins to relax and aftereffects may set in. The type and length of aftereffects will vary from person to person and may include:
- Confusion and agitation
- Fatigue and drowsiness
- Loss of bowel or bladder control
- Loss of consciousness or unresponsiveness
- Partial paralysis
The official website for the neurology fellowship programs at University of Pennsylvania in Philadelphia.
Epilepsy Fellowship Program

- Epilepsy Surgery (>80 procedures last year, including phase II monitoring with stereo EEG and subdural electrodes, implantable devices, resections and laser ablations )
- Outpatient epilepsy, including specialty clinics for epilepsy genetics, neuromodulation, transitioning care from pediatrics to adult, tuberous sclerosis and others
- Clinical trials - medications and devices
- Implantable devices, including RNS, DBS and VNS
- International medicine
- Quality of care in collaboration with the Wharton School of Business
Fellowship Curriculum
Clinical fellows in our program evaluate and care for epilepsy patients in both inpatient and outpatient settings. Our Epilepsy Monitoring Unit (currently 8 beds) and our active epilepsy surgical program provide a means for fellows to learn how to evaluate and refer patients for epilepsy surgery and device implantation. This includes very active intracranial EEG program, including functional brain mapping. In addition, there is an active long-term monitoring/ICU EEG program which covers 4 hospitals in downtown Philadelphia, including advanced techniques such as quantitative EEG and intracranial depth electrodes for traumatic brain injury. Fellows also participate in the outpatient management of patients with epilepsy (or concern for epilepsy) by co-managing patients in attending clinics as well as their own longitudinal clinic. The outpatient EEG laboratory is very active and offers routine, prolonged and ambulatory EEG studies at multiple locations.
In addition to the above, fellows rotate at the Children’s Hospital of Philadelphia for pediatric epilepsy and at the Philadelphia Veterans Affairs Medical Center.
A critical aspect of our program is the active integration of clinical, translational and basic research with the clinical programs. This includes active research projects related to intracranial EEG, neuromodulation, neuroimaging, genetics and others. Fellows have the opportunity to participate in these projects based on their interests. Dedicated didactic sessions include core lectures on epilepsy and EEG followed by weekly conferences on EEG/Neurophysiology and Clinical Epilepsy. Active participation by fellows is encouraged including case presentations, journal clubs and presentation of projects. There is also a weekly Epilepsy Surgery conference where the fellows present the vast majority of patients for discussion, with active participation by neuroradiology and neuropsychology. Joint conferences include the NeuroICU and pediatric epilepsy programs.

“Penn provided an ideal environment for diverse training in clinical epileptology, leading the cutting edge on many aspects of EEG and patient care. In addition, there were tremendous opportunities for funded translational research, which were instrumental in establishing my own academic career.”
Application Process
- November 15, 2023 Applicants may begin submitting applications on ERAS.
- December 6, 2023 Programs may begin reviewing applications on ERAS.
- January - April 2024 Penn Epilepsy Fellowship Interviews.
- May 1, 2024 Deadline for submitting Rank Order List.
- May 15, 2024 Match Day.
- July 1, 2025 First Day of Fellowship.
- Personal Statement explaining your interests in Epilepsy
- USMLE Transcript
- Professional photo
- Three Letters of Recommendation.
Thank you for your interest in our program!
Epilepsy faculty.

Kathryn Davis, MD, MTR
Epilepsy division chief medical director, epilepsy monitoring unit medical director, epilepsy surgical program interests: epilepsy anti-epileptic medications, electroencephalogram, seizures faculty profile.

Erin Conrad, MD
Assistant professor of neurology faculty profile.

Ramon Diaz-Arrastia, MD, PhD

Colin Ellis, MD
Taneeta ganguly, md, faculty profile , michael gelfand, md, phd.

Ramya Raghupathi, MD
- Age Span Fellowship in Multiple Sclerosis and related Neuroinflammatory Disorders
- Headache and Facial Pain
- Movement Disorders
- Neurocritical Care
- Neurohospitalist Medicine
- Neuro-Ophthalmology
- Neuromuscular Medicine
- Neuro-Oncology
- Sleep Medicine
- Vascular Neurology
Contact Information
Popular posts.

Copyright 2015 Penn Neurology Fellowship Programs
Sora Templates

Biomedical Graduate Studies
Neuroscience graduate group.
- Focused Areas
By Traditional Areas of Neuroscience Research
- Behavioral and Cognitive
- Cellular and Molecular
- Computational Neuroscience
- Developmental
- Neurobiology of Disease
By Focused Areas of Neuroscience Research
- Affective Disorders
- Autism and Other Neurodevelopmental Disorders
- Axon Guidance
- Behavioral Neuroscience
- Cognitive Neuroscience
- Decision Neuroscience
- Genetics and Epigenetics
- Imaging Approaches
- Ion Channels and Receptors
- Learning and Memory
- Motor Systems
- Neural Injury, Regeneration, Repair, and Stem Cells
- Neurobiology of Obesity
- Neurobiology of Sleep and Circadian Rhythms
- Neurobiology of Stress
- Neurodegeneration
- Neuroendocrinology
- Neuroengineering
- Neuroinflammation and Neurovirology
- Neuron-Glia Interactions
- Schizophrenia
- Sensory Systems and Perception
- Synaptic Plasticity
- Synaptogenesis and Circuit Formation
Current Members
Click the faculty member's name to see more detailed information.
© The Trustees of the University of Pennsylvania | Site best viewed in a supported browser . | Report Accessibility Issues and Get Help | Privacy Policy | Site Design: PMACS Web Team.
Emory Epilepsy Center section navigation
Emory epilepsy center.
The Emory Epilepsy Center is a multidisciplinary specialized team from the Departments of Neurology and Neurosurgery. The Emory Epilepsy Center is part of the Emory Brain Health Center.

The Emory University Epilepsy Program is a multi-specialty group of physicians, neuropsychologists, and nurses from the departments of Neurology, Neurosurgery, Pediatrics, Physical Medicine and Rehabilitation and Radiology. The Epilepsy Program provides specialized clinical care in the diagnosis and treatment of seizures, epilepsy and conditions that may mimic epilepsy.
Learn more about the Emory Epilepsy Center.
Research Highlights
Emory University is a major research center. The faculty of the Emory Epilepsy Program are national leaders in research and in the forefront of medical discoveries related to epilepsy. Our group is involved in several NIH and foundation supported research projects, as well as innovative partnerships with industry.
Advanced fellowship training opportunities are available in the Epilepsy Program, and include clinical and research fellowships .

Patient Care
Emory Epilepsy Center is one of the only Level-4 epilepsy centers in the southeastern United States, which means patients can count on us for providing them with the most comprehensive and innovative care available.

Our Epilepsy and Seizures Team
A team of epilepsy experts.
Our multidisciplinary team of doctors at the University of Chicago Medicine includes specialists who are board-certified in neurology, neurosurgery, neurophysiology, neuropsychology, neuropsychiatry, neurogenetics, radiology and rehabilitation. We collaborate to offer the most effective, individualized treatments to every patient we see.
Schedule an Appointment with an Epilepsy Expert
Meet Our Epilepsy and Seizures Team
Neuro-Oncology (Brain & Spinal Tumors)
Epilepsy Nurse
Shadrach Castillo, RN
Registered Electroencephalographic Technologist
Diane Suarez, REEGT
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.

Editor: Stanislaw J. Czuczwar , MD, PhD.
Affiliations
- Copyright and Permissions
Epilepsy is a neurological disorder that affects about 65 million people worldwide. Although antiepileptic drugs provide sufficient control of seizures in approximately 70% of patients with epilepsy, the remaining 30% are resistant to monotherapy. This means around 20 million people worldwide face significant adverse life-long consequences such as sudden unexpected death from epileptic seizures, increased risk of injuries, and learning and developmental disabilities at school age. That is why, a continuous search for drugs targeting novel antiseizure mechanisms and alternative ways of epilepsy management is going on. This book covers a number of valid issues aimed at understanding the etiology and pathophysiology of epilepsy, epilepsy genetics, current therapeutic challenges, and possible novel therapeutic targets. The authors point to a number of etiologic factors, which incorporate anatomic, acquired, genetic, metabolic, and immunologic aspects. The overlap between neurodevelopmental disorders and epilepsy, and the involvement of hippocampal sclerosis in the process of epileptogenesis are also elegantly described. The readers will also find a very detailed description of the contemporary management of status epilepticus. There are also clues on how to inhibit a very dangerous super refractory status epilepticus. Regarding precision medicine-based management of epilepsy, recent data on GABAA receptor variants and canonical transient receptor potential channels are provided, which can help develop novel strategies for epilepsy treatment. Ketogenic diet may be considered as a non-pharmacological option for children and adolescents suffering from drug-resistant epilepsy. The book, covering various aspects of epilepsy from receptor and genetic studies to therapeutic clues, will be of particular value to scientists and clinicians.
- Collapse All
- List of Contributors
- INTRODUCTION
- ETIOLOGY OF EPILEPSY AND PATHOPHYSIOLOGICAL MECHANISMS
- CURRENT EPILEPSY TREATMENT
- FUTURE DIRECTIONS
- THE HIPPOCAMPUS AND EPILEPSY
- THE TEMPORAL LOBE, THALAMUS, AMYGDALA AND EPILEPSY
- OLFACTORY CORTEX AND EPILEPSY
- FRONTAL CORTEX AND EPILEPSY
- CEREBELLUM AND EPILEPSY
- DENDRITIC PATHOLOGY AND EPILEPSY
- EPIDEMIOLOGY
- METHODS AND TECHNOLOGY PROGRESS – FROM BENCH TO BEDSIDE
- PARADIGM SHIFT IN THE FIELD
- IMPLICATIONS AND IMPACT ON PATIENT CARE
- EVALUATION PATHWAY
- CHALLENGES IN GENETIC EVALUATIONS AND TEST INTERPRETATION
- SUGGESTED CLINICAL PRACTICE MODEL
- THE GENETIC BACKGROUNDS OF NEURODEVELOPMENTAL DISORDERS AND EPILEPSY
- MODELS OF OVERLAP BETWEEN EPILEPSY AND NEURODEVELOPMENTAL DISORDERS
- EARLY-STAGE STATUS EPILEPTICUS
- ESTABLISHED STATUS EPILEPTICUS
- REFRACTORY STATUS EPILEPTICUS
- SUPER-REFRACTORY STATUS EPILEPTICUS
- NON-ANTISEIZURE MEDICATIONS USED IN THE TREATMENT OF STATUS EPILEPTICUS
- OTHER TREATMENT OPTIONS
- TRPC: SUBUNIT COMPOSITION, STRUCTURE, AND GATING
- STRUCTURE OF GABA A RECEPTORS
- EPILEPSY-ASSOCIATED VARIANTS IN THE α1 SUBUNIT
- EPILEPSY-ASSOCIATED VARIANTS IN THE β2/β3 SUBUNIT
- EPILEPSY-ASSOCIATED VARIANTS IN THE γ2 SUBUNIT
- VARIANTS WITH MODERATE SEVERITY OF EPILEPSY SYNDROMES
- VARIANTS WITH SEVERE EPILEPSY SYNDROMES
- THE GUT-BRAIN AXIS IN CHILDHOOD EPILEPSY DISORDER
- THE ROLE OF KETOGENIC DIET IN EPILEPSY TREATMENT
- COW’S MILK ALLERGY AND EPILEPTIC EVENTS
Professor Stanislaw J. Czuczwar, MD, PhD, graduated from the Medical Faculty of Lublin Medical University, Poland, in 1975. Currently, he is the Head of Department of Pathophysiology at the Lublin Medical University. His area of research is mainly focused on experimental epilepsy and antiepileptic drugs. With his research team, he characterized, using isobolographic analysis, several synergistic combinations of antiepileptic drugs, which may be of importance for the management of drug-resistant epilepsy. During his time in the Department of Experimental Neurology, University of London, UK, he tested newly synthesized antagonists of N-methyl-D-aspartate receptors as potential anticonvulsant agents. His research continued at the Free University of West Berlin, Germany, where he evaluated ligands of various receptors in the search of anticonvulsants. In the 1990s of the former century, he stayed as a visiting professor at the Department of Neurology of Vanderbilt University (Nashville, TN, USA). He has published more than 450 papers, mainly devoted to interactions of antiepileptic drugs with drugs affecting various receptors or channels, delineating promising combined treatments from the preclinical point of view.
ISBN: 978-0-6453320-4-9
DOI: https://doi.org/10.36255/exon-publications-epilepsy
Stanislaw J. Czuczwar, MD, PHD, Department of Pathophysiology, Medical University of Lublin, Lublin, Poland
Published by
Exon Publications, Brisbane, Australia
Copyright© 2022 Exon Publications
Copyright of individual chapters belongs to the respective authors. The authors grant unrestricted publishing and distribution rights to the publisher. The electronic versions of the chapters are published under Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0). https://creativecommons.org/licenses/by-nc/4.0/ . Users are allowed to share and adapt the chapters for any non-commercial purposes as long as the authors and the publisher are explicitly identified and properly acknowledged as the original source. The book in its entirety is subject to copyright by the publisher. The reproduction, modification, replication and display of the book in its entirety, in any form, by anyone, for commercial purposes are strictly prohibited without the written consent of the publisher.
Notice to the user
The views and opinions expressed in this book are believed to be accurate at the time of publication. The publisher, editors or authors cannot be held responsible or liable for any errors, omissions or consequences arising from the use of the information contained in this book. The publisher makes no warranty, implicit or explicit, with respect to the contents of this book, or its use.
First Published in April 2022
Printed in Australia
- Cite this Page Czuczwar SJ, editor. Epilepsy [Internet]. Brisbane (AU): Exon Publications; 2022 Apr 2. doi: 10.36255/exon-publications-epilepsy
- PDF version of this title (22M)
Related Items in Bookshelf
- All Reference Works
- All Textbooks
Related information
- NLM Catalog Related NLM Catalog Entries
Similar articles in PubMed
- Review Febrile Infection-Related Epilepsy Syndrome (FIRES): An Overview of Treatment and Recent Patents. [Recent Pat Inflamm Allergy Dru...] Review Febrile Infection-Related Epilepsy Syndrome (FIRES): An Overview of Treatment and Recent Patents. Hon KL, Leung AKC, Torres AR. Recent Pat Inflamm Allergy Drug Discov. 2018; 12(2):128-135.
- Review TRPC channels as emerging targets for seizure disorders. [Trends Pharmacol Sci. 2022] Review TRPC channels as emerging targets for seizure disorders. Yu Y, Li W, Jiang J. Trends Pharmacol Sci. 2022 Sep; 43(9):787-798. Epub 2022 Jul 12.
- Review [Contemporary opinions on classification, pathogenesis and treatment of drug-resistant epilepsy]. [Wiad Lek. 2007] Review [Contemporary opinions on classification, pathogenesis and treatment of drug-resistant epilepsy]. Jóźwiak S. Wiad Lek. 2007; 60(5-6):258-64.
- Clinical predictors of drug-resistant epilepsy in children. [Turk J Med Sci. 2021] Clinical predictors of drug-resistant epilepsy in children. Karaoğlu P, Yaş U, Polat Aİ, Ayanoğlu M, Hız S. Turk J Med Sci. 2021 Jun 28; 51(3):1249-1252. Epub 2021 Jun 28.
- Review The changing face of dietary therapy for epilepsy. [Eur J Pediatr. 2016] Review The changing face of dietary therapy for epilepsy. Pasca L, De Giorgis V, Macasaet JA, Trentani C, Tagliabue A, Veggiotti P. Eur J Pediatr. 2016 Oct; 175(10):1267-76. Epub 2016 Sep 1.
Recent Activity
- Epilepsy Epilepsy
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

UCL Queen Square Institute of Neurology

The following are PhD theses from the UCL Epilepsy Imaging Group with links to the full text in UCL Discovery where available:
- Vakharia, Vejay Niranjan; (2020) Computer-Assisted Planning and Robotics in Epilepsy Surgery .
- De Blasi, Bianca; (2020) Multi-parametric Imaging Using Hybrid PET/MR to Investigate the Epileptogenic Brain
- Lorenzo Caciagli - Neuroimaging of epilepsy: disease severity, cognitive comorbidities and endophenotypes
- Mark Nowell - Novel multimodality imaging in the planning and surgical treatment of epilepsy
- Christian Vollmar - Neuroimaging of functional and structural alterations in juvenile myoclonic epilepsy and frontal lobe epilepsy
- Britta Wandschneider - The effects of genes, antiepileptic drugs and risk of death on functional anatomy and cognitive networks in epilepsy
- Maria Feldmann - Imaging p-glycoprotein function: prediction of treatment response in mesial temporal lobe epilepsy
- Meneka Sidhu - Episodic memory in temporal lobe epilepsy
- Silvia Bonelli-Nauer - Cognitive functional MRI in temporal lobe epilepsy
- Helmut Laufs - EEG-fMRI signatures of spontaneous brain activity in healthy volunteers and epilepsy patients
- Rachel Thornton - Imaging brain networks in focal epilepsy : a prospective study of the clinical application of simultaneous EEG-fMRI in pre-surgical evaluation
- Gavin Winston - Translation of novel imaging techniques into clinical use for patients with epilepsy
- Mahinda Yogarajah - Imaging structural connections of the brain in epilepsy
- Umair Chaudhary - Haemodynamic correlates of interictal and ictal epileptic discharges and ictal semiology using simultaneous scalp video-EEG-fMRI and intracranial EEG-fMRI
- Robert Simister - Magnetic Resonance Spectroscopy as applied to epilepsy
- Serge Vulliemoz - Imaging functional and structural networks in the human epileptic brain
- Beate Diehl - Imaging correlates of the epileptogenic zone and functional deficit zone using diffusion tensor imaging (DTI)
- Khalid Hamandi - Functional MRI of focal and generalised interictal epileptiform discharges
- Afraim Salek-Haddadi - EEG-correlated functional MRI in epilepsy
- Rebecca Samson - Optimisation of quantitative magnetisation transfer (qMT) MRI to study restricted protons in the living human brain
- Robert Powell - Investigating brain structure and function in temporal lobe epilepsy
- Karsten Krakow - Imaging of epileptic activity using EEG-correlated functional MRI
- Rebecca Liu - Investigation of secondary cerebral damage in epilepsy
- Tejal Mitchell - Quantitative MRI in cerebral development disorders and epilepsy
- Fergus Rugg-Gunn - Imaging the neocortex in epilepsy with advanced MRI techniques
- Alex Everitt - The structural basis of the epilepsies: MRI and epidemiological studies
- Alexander Hammers - PET investigations in focal epilepsy
- Udo Wieshmann - New MR imaging techniques in epilepsy
- Matthias Koepp - Central benzodiazepine receptors in hippocampal sclerosis and idiopathic generalised epilepsies and opioid receptors in reading epilepsy
- Mark Richardson - Positron emission tomography investigation of cortical malformations causing epilepsy
- Wim van Paesschen - Quantitative MRI and hippocampal neuropathology of temporal lobe epilepsy
- Sanjay Sisodiya - Qualitative and quantitative analysis of MRI data from patients with epilepsy
BRET Career Development ASPIRE Program
Epilepsy foundation / american epilepsy society – predoctoral fellowship.
Posted by hagansa2 on Wednesday, May 8, 2024 in Announcements .
Deadline: January 18, 2025
URL: Predoctoral Research Fellowships (aesnet.org)
Description:
Fellowships support predoctoral students pursuing dissertation research with an epilepsy-relevant theme, and who are working under the supervision of a mentor with expertise to supervise in the area of epilepsy investigation. The fellowship offers one year of support.
Eligibility: Applicants must:
- Be matriculating in a full-time doctoral (PhD) program in a field relevant to epilepsy research with an academic career focus.
- Have a defined research plan and access to institutional resources to conduct the proposed project.
- Have a qualified mentor(s) with expertise to supervise and provide guidance on epilepsy-related research.
- Have not previously been awarded an American Epilepsy Society or an Epilepsy Foundation Predoctoral Fellowship.
- U.S. citizenship is not required; however, all research must be conducted in the U.S.
Award amount:
- $29,000 stipend.
- $1,000 to support attendance at the AES annual meeting.
- Complimentary registration for the AES annual meeting.
- One year of complimentary AES membership.
If this information is out of date, please email [email protected] to let us know.
Share this post:
Tags: Predoctoral Funding Opportunity
Comments are closed
VIEW MORE EVENTS >
Beyond the Lab: Data Science

Epilepsy and Seizures
What are epilepsy and seizures.
Epilepsy is a chronic brain disorder in which groups of nerve cells, or neurons, in the brain sometimes send the wrong signals and cause seizures. Neurons normally generate electrical and chemical signals that act on other neurons, organs, and muscles to produce human thoughts, feelings, and actions.
During a seizure, many neurons send signals at the same time, much faster than normal. This surge of excessive electrical activity may cause involuntary movements, sensations, emotions, and/or behaviors. The disturbance of normal nerve cell activity may cause a loss of awareness. Some people recover immediately after a seizure, while others may take minutes to hours to feel like themselves again. During this time, they may feel tired, sleepy, weak, or confused.
Epilepsy (sometimes referred to as a seizure disorder) can have many different causes and seizure types. Epilepsy varies in severity and impact from person to person and can be accompanied by a range of co-existing conditions. Epilepsy is sometimes called “the epilepsies” because of the diversity of types and causes. Some people may have convulsions (muscles contract repeatedly) and lose consciousness. Others may simply stop what they are doing, have a brief lapse of awareness, and stare into space for a short period. Some people have seizures very infrequently, while other people may experience hundreds of seizures each day.
While any seizure is cause for concern, having a seizure does not by itself mean a person has epilepsy. First seizures, febrile seizures, nonepileptic events, and eclampsia (a life-threatening condition that can occur during pregnancy) are examples of conditions involving seizures that may not be associated with epilepsy. Regardless of the type of seizure, it's important to inform your doctor when you have a seizure.
Who is more likely to have epilepsy and seizures?
Anyone can develop epilepsy. It affects both men and women of all races, ethnic backgrounds, and ages.
Epilepsy has many possible causes, but about half of people living with epilepsy do not know the cause. In some cases, epilepsy is clearly linked to genetic factors, developmental brain abnormalities, infection, traumatic brain injury (TBI) , stroke , brain tumors , or other identifiable problems. Anything that disturbs the normal pattern of nerve cell activity—from illness to brain damage to brain development problems—can lead to seizures.
Epilepsy may develop because of problems in the brain’s wiring, an imbalance of nerve signaling in the brain (in which some cells are unusually active or stop other brain cells from sending messages), or some combination of these factors. Sometimes, when the brain tries to repair itself after a head injury, stroke, or other problem, it can unintentionally create nerve connection issues that lead to seizures.
The role of genes in epilepsy
Genetic changes may play a key role in the development of certain types of epilepsy. Many types affect multiple members of a family, pointing to an inherited gene or genes. In other cases, gene variations may occur spontaneously and contribute to the development of epilepsy in people with no family history of the disorder (called “de novo” mutations). Overall, researchers estimate that hundreds of genes could play a role.
Several types of epilepsy (called channelopathy-associated epilepsy) have been linked to variations in genes that provide instructions for ion channels, the "gates" that control the flow of ions (charged molecules) in and out of cells and help regulate neuronal signaling. Other genetic changes that may play a role in epilepsy include variations in genes that control how neurons move through the brain during development (neuronal migration) and genes that help break down carbohydrates in the brain.
Other genetic changes may not cause epilepsy but may influence the disorder in other ways, for example, some genes may affect a person's susceptibility to seizures and responsiveness to anti-seizure medications.
Conditions that can lead to epilepsy
Epilepsy may develop as a result of many types of conditions that disrupt normal brain activity, known as “co-occurring conditions”. Once these conditions are treated, individuals may no longer have seizures. However, whether the seizures stop varies based on the type of disorder, the brain region that is affected, and how much brain damage occurred prior to treatment. Examples of conditions that can lead to epilepsy include:
- Brain tumors
- Head trauma
- Alcoholism or alcohol withdrawal
- Alzheimer's disease
- Strokes, heart attacks, and other conditions that deprive the brain of oxygen
- Abnormal blood vessel formation (called arteriovenous malformations) or bleeding in the brain
- Brain inflammation or swelling
- Infections such as meningitis, HIV-related infections, and viral encephalitis
Cerebral palsy and other developmental disorders also may be associated with epilepsy. Epilepsy is often seen in people with other brain development disorders, for example, among individuals with autism spectrum disorder or intellectual disabilities.

What can trigger seizures?
Seizure triggers do not cause epilepsy but can provoke seizures in those who are susceptible. For those who are already diagnosed with epilepsy and taking medication, triggers can spark a seizure. Triggers include:
- Drinking alcohol, or alcohol withdrawal
- Dehydration or missing meals
- Exposure to toxins or poisons, including lead, carbon monoxide, illicit drugs, and very large doses of prescription medications
- Hormonal changes associated with the menstrual cycle
- Sleep deprivation
- Visual stimulation such as flashing lights or moving patterns
In surveys of people with epilepsy, stress is the most commonly reported seizure trigger.
Types of seizures
Seizures are divided into two broad categories: focal seizures and generalized seizures. There are many different types of seizures within each of these categories.
Focal seizures
Focal seizures come from just one part of the brain. About 60% of people with epilepsy have focal seizures. These seizures are frequently described by the area of the brain in which they originate. For example, many people are diagnosed with focal frontal lobe or medial temporal lobe seizures.
Symptoms of focal seizures
In some focal seizures, the person remains conscious during the seizure but may experience motor, sensory, or psychic feelings (for example, intense dejà vu or memories) or sensations. The person may experience sudden and unexplainable feelings of joy, anger, sadness, or nausea. He or she also may hear, smell, taste, see, or feel things that are not real and may have movements of just one part of the body, for example, just one hand.
In other focal seizures, the person has a change in consciousness, which can produce a dreamlike experience. The person may display unusual, repetitive behaviors such as blinks, twitches, mouth movements, or even walking in a circle. These repetitive movements are called automatisms. A person may perform more complicated actions, which may seem purposeful, involuntarily. Individuals may also continue activities they started before the seizure began, such as washing dishes in a repetitive, unproductive fashion. These seizures usually last no more than a minute or two.
Some people with focal seizures may experience auras—unusual sensations that warn of an impending seizure. An individual's symptoms, and how they progress, tend to be similar every time. Some people report experiencing a prodrome, a feeling that a seizure is imminent lasting hours or days.
Following focal seizures, a person may experience symptoms in areas controlled by the area of the brain where their seizure originated. This can help doctors locate the brain region where the seizure started. After a seizure, some people may experience a headache or pain in the muscles that contracted during the seizure.
The symptoms of focal seizures can be easily confused with other disorders. The strange behavior and sensations caused by focal seizures also can be mistaken for symptoms of narcolepsy, fainting, or even mental illness. Several tests and careful monitoring may be needed to make the distinction between epilepsy and these other disorders.
Generalized seizures
Generalized seizures are a result of abnormal neuronal activity that rapidly emerges on both sides of the brain. These seizures may cause loss of consciousness, falls, or massive muscle contractions. Types of generalized seizures and their effects include:
- Absence seizures may cause the person to appear to be staring into space, with or without slight twitching of the muscles
- Tonic seizures cause a stiffening of muscles of the body, generally in the back, legs, and arms
- Clonic seizures cause repeated jerking movements of muscles on both sides of the body
- Myoclonic seizures cause jerks or twitches of the upper body, arms, or legs
- Atonic seizures cause a loss of normal muscle tone, which can cause the person to fall or drop the head involuntarily
- Tonic-clonic seizures cause a combination of symptoms, including stiffening of the body and repeated jerks of the arms and/or legs as well as loss of consciousness
- Secondary generalized seizures begins in one part of the brain, then spreads to both halves of the brain (basically, a focal seizure followed by a generalized seizure)
Other types of seizures
Not all seizures can be easily defined as either focal or generalized. Some people have both types of seizures but with no clear pattern.
Febrile seizures are seizures that happen when a child has an illness that causes a high fever. Children who have febrile seizures are typically not prescribed antiseizure medications unless they have a family history of epilepsy, signs of nervous system impairment before the seizure, or have a relatively long or complicated seizure or more than one febrile seizure. The risk of subsequent non-febrile seizures is low unless one of these factors is present.
First seizures affect many people who have a single seizure at some point in their lives. It can be provoked or unprovoked, meaning that they can occur with or without any obvious triggering factors. Unless the person has suffered brain damage or there is a family history of epilepsy or other neurological abnormalities, most single seizures usually are not followed by additional seizures. Medical disorders which can provoke a seizure include:
- Low or very high blood sugar
- Changes in chemical levels in the blood (sodium, calcium, magnesium)
- Eclampsia during or after pregnancy
- Impaired function of the kidneys or liver
In some cases where additional epilepsy risk factors are present, drug treatment after the first seizure may help prevent future seizures. Evidence suggests that it may be beneficial to begin antiseizure medication once a person has had a second unprovoked seizure, as the chance of future seizures increases significantly after this occurs. A person with a pre-existing brain problem, for example, a prior stroke or traumatic brain injury, will have a higher risk of experiencing a second seizure. In general, the decision to start antiseizure medication is based on the health care provider’s assessment of many factors that influence how likely it is that another seizure will occur in that person.
Types of epilepsy
Just as there are many different kinds of seizures, there are many different kinds of epilepsy. Hundreds of different epilepsy syndromes—disorders that include seizures as a prominent symptom—have been identified. Some of these syndromes appear to be either hereditary or caused by de novo gene changes. For other syndromes, the cause is unknown. Epilepsy syndromes are frequently described by their symptoms or by where in the brain they originate.
- Absence epilepsy is characterized by repeated seizures that cause momentary lapses of consciousness. The seizures almost always begin in childhood or adolescence and tend to run in families, suggesting that they may at least be partially due to genetic factors. Individuals may show purposeless movements during their seizures, such as a jerking arm or rapidly blinking eyes, while others may have no noticeable symptoms except for brief times when they appear to be staring off into space. Immediately after a seizure, the person can resume whatever he or she was doing. However, these seizures may occur so frequently (in some cases up to 100 or more a day) that the person cannot concentrate in school or other situations.
- Frontal lobe epilepsy is a common epilepsy syndrome that features brief focal seizures that may occur in clusters. It can affect the part of the brain that controls movement and its seizures can cause muscle weakness or unusual, uncontrolled movement such as twisting, waving the arms or legs, eyes drifting to one side, or grimacing, and are usually associated with some loss of awareness. Seizures usually occur during sleep but may also occur while awake.
- Temporal lobe epilepsy (TLE) is the most common epilepsy syndrome in people who get focal seizures. These seizures are often associated with auras of nausea, emotions (such as déjà vu or fear), or unusual smell or taste. The seizure itself is a brief period of impaired consciousness which may appear as a staring spell, dream-like state, or repeated automatisms. TLE often begins in childhood or teenage years. Research has shown that repeated temporal lobe seizures are often associated with shrinkage and scarring (sclerosis) of the hippocampus. The hippocampus is a brain region that is important for memory and learning.
- Neocortical epilepsy is characterized by seizures that originate from the cerebral cortex, or outer layer. The seizures can be either focal or generalized. Symptoms may include unusual sensations, visual hallucinations, emotional changes, muscle contractions, convulsions, and a variety of other symptoms, depending on where in the brain the seizures originate.
Types of childhood epilepsy
There are many other types of epilepsy that begin in infancy or childhood. Some childhood epilepsy syndromes tend to go into remission or stop entirely during adolescence. Other syndromes, such as juvenile myoclonic epilepsy (which features jerk-like motions upon waking) and Lennox-Gastaut syndrome are usually present for life.
For example:
- Infantile spasms are clusters of seizures that usually begin before the age of 6 months. During these seizures the infant may drop their head, bend at the waist, jerk their arms up toward their head, and/or cry out.
- Childhood absence epilepsy usually stops when the child reaches puberty. However, some children will continue to have absence seizures into adulthood and/or go on to develop other seizure types.
- Children with Lennox-Gastaut syndrome have several different types of seizures, including atonic seizures, which cause sudden falls and are also called drop attacks. Children with this condition usually begin having seizures before age four. This severe form of epilepsy can be very difficult to treat.
- Rasmussen's encephalitis is a progressive form of epilepsy in which half the brain shows chronic inflammation.
- Children with Dravet syndrome and Tuberous Sclerosis Complex typically have seizures that start before age one.
- Hypothalamic hamartoma is a rare form of epilepsy that first occurs during childhood and is associated with malformations of the hypothalamus at the base of the brain. People with this disorder have seizures that resemble laughing or crying. Such seizures frequently go unrecognized and are difficult to diagnose.
- Developmental and Epileptic Encephalopathy (DEE) refers to a group of severe epilepsies that are characterized both by seizures, which are often drug-resistant, as well as encephalopathy, which is a term used to describe significant developmental delay or even loss of developmental skills.
Nonepileptic seizures
Non-epileptic seizures outwardly resemble epileptic seizures but are not associated with electrical discharge in the brain. Non-epileptic events may be referred to as psychogenic non-epileptic seizures (PNES). PNES do not respond to antiseizure drugs; instead, they are often treated by cognitive behavioral therapy to decrease stress and improve mindfulness.
A history of traumatic events is among the known risk factors for PNES. People with PNES should be evaluated for underlying psychiatric disorders and treated appropriately. Some people with epilepsy have psychogenic seizures in addition to their epileptic seizures.
Other nonepileptic events may be caused by:
- Tourette syndrome
- Cardiac arrhythmia (irregular heartbeat)
- Other medical conditions with symptoms that resemble seizures
Because symptoms of these disorders can look very much like epileptic seizures, they are often mistaken for epilepsy.
How are epilepsy and seizures diagnosed and treated?
Diagnosing epilepsy and seizures.
Accurate diagnosis of epilepsy is crucial for finding an effective treatment. Several tests are used to determine whether a person has epilepsy and, if so, what kind of seizures the person has. Generally, epilepsy is diagnosed after a person has had two or more unprovoked seizures separated by at least 24 hours.
Medical history
Taking a detailed medical history, including symptoms and duration of the seizures, is still one of the best methods available to determine what kind of seizures a person has had and to help determine what type of epilepsy the person has. The medical history should include details about any past illnesses or other symptoms a person may have had, as well as any family history of seizures.
Since people who have a seizure often do not remember what happened, accounts from people who have witnessed the seizures are very important. The person who experienced the seizure is asked about whether they felt anything unique (warning experiences) before the seizure started. The observers will be asked to provide a detailed description and timeline for the seizure.
Imaging and monitoring epilepsy
There are several scans and imaging techniques that can help diagnose and monitor a person's epilepsy. These include:
- An electroencephalogram (EEG) , a test that measures electrical activity in the brain, can look for abnormalities in the person's brain waves and may help to determine if antiseizure drugs would help. Video monitoring may be used in conjunction with EEG to determine the nature of a person's seizures and to rule out other disorders that may look like epilepsy.
- SEEG (stereoelectoencephalograpy) is the surgical implantation of electrodes into the brain in order to better find where the seizures are located. SEEG can help determine if an individual is a candidate for epilepsy surgery. A magnetoencephalogram (MEG) measures the magnetic signals generated by neurons to help find unusual brain activity. MEG can help surgeons plan any appropriate surgeries to remove focal areas involved in seizures while minimizing interference with normal brain function.
- CT (computerized tomography) and MRI (magnetic resonance imaging) scans reveal structural abnormalities of the brain such as tumors and cysts, which may cause seizures. A type of MRI called functional MRI (fMRI) can be used to localize normal brain activity and detect abnormalities in brain function.
- PET (positron emission tomography) scans take pictures of the brain and show regions of the brain with normal and abnormal chemical activity. PET scans can be used to identify brain regions with lower-than-normal metabolism, which can indicate the focus of the seizure after it has stopped.
- Single photon emission computed tomography (SPECT) is sometimes used to find the location of focal seizures in the brain. In a person admitted to the hospital for epilepsy monitoring, the SPECT blood flow tracer is injected within 30 seconds of a seizure. The images of brain blood flow at the time of the seizure are compared with blood flow images taken in between seizures. The seizure onset area shows a high blood flow region on the scan.
Blood tests
Blood tests can screen for metabolic or genetic disorders that may contribute to the seizures. They also may be used to check for underlying health conditions such as infections, lead poisoning, anemia, and diabetes that may be causing or triggering the seizures.
Developmental, neurological, and behavioral tests
Tests to measure motor abilities, behavior, and intellectual ability often are used to determine how epilepsy is affecting an individual. These tests also can provide clues about what kind of epilepsy the person has.
Treating epilepsy and seizures
Once epilepsy is diagnosed, it is important to begin treatment as soon as possible. There are many different ways to successfully control seizures. There are several treatment approaches that can be used, depending on the individual and the type of epilepsy.
Medications to treat seizures in epilepsy
The most common approach to treating epilepsy is to prescribe antiseizure medications. . More than 40 different antiseizure medications are available today, all with different benefits and side effects. Most seizures can be controlled with one drug. Combining medications may amplify side effects such as fatigue and dizziness, so doctors usually prescribe just one drug whenever possible. Combinations of drugs, however, are still sometimes necessary for some forms of epilepsy that do not respond to a single drug.
Which drug a person should be prescribed depends on many different factors, including:
- Seizure type
- Lifestyle and age
- Seizure frequency
- Drug side effects
- Medicines for other conditions
It may take several months to determine the best drug and dosage. If one treatment is unsuccessful, another may work better.
When starting any new antiseizure medication, a doctor will begin with a low dose and increase the dose as needed depending on how effective the drug is. Sometimes doctors monitor the level of the drug in a person’s blood to help determine when the optimal dosage has been reached. It may take time to find a dose that gives the best seizure control while minimizing side effects.
Side effects are often worse when first starting a new medicine and get better over time. Talk with your doctor about any side effects you experience while on medications and make sure they are aware of any other prescription or over-the-counter medications you are taking, including any herbs or supplements. Some antiseizure medications can affect how and whether other drugs work and can interact in harmful ways with other medications. Some may make hormonal birth control less effective in women. Some medications are harmful to the fetus, so women who plan to get pregnant should consult with their physician to be sure that they are using medications that are safe during pregnancy.
Discontinuing medication should always be done with supervision of a health care professional. It is very important to continue taking antiseizure medication for as long as it is prescribed. Discontinuing medication too early is one of the major reasons people who have been seizure-free start having new seizures and can lead to status epilepticus, which is potentially life threatening. Some people with epilepsy may be advised to discontinue their antiseizure drugs after two to three years have passed without a seizure. Others may be advised to wait for four to five years depending on the cause of the seizures.
While antiseizure medications are effective for many people with epilepsy, some do not respond to or are not able to take medications. Those individuals may be candidates for surgery, dietary changes, or devices to stop their seizures.
Diet and lifestyle changes in epilepsy
Some types of epilepsy may respond to changes in diet. A high-fat, high-protein, very low carbohydrate ketogenic diet is sometimes used to treat medication-resistant epilepsies. The diet induces a state known as ketosis, which means that the body shifts to breaking down fats instead of carbohydrates to survive. A ketogenic diet effectively reduces seizures for some people, especially children, with certain forms of epilepsy.
The ketogenic diet can be difficult to maintain since it requires that a person only eat certain foods and avoid many common foods that contain sugars and carbohydrates. Individuals using this diet to manage their seizures should be monitored to make sure they are getting enough nutrients. One side effect of a ketogenic diet is a buildup of uric acid in the blood, which can lead to kidney stones. A doctor or nutritionist can help people on this diet make sure they are getting the nutrients they need, and in the right amounts.
Sleep disorders are common among people with epilepsy and sleep deprivation is a powerful trigger of seizures. Treating sleep problems can help reduce seizures. People with epilepsy should practice good sleep hygiene: going to bed and getting up at the same time each day, reducing distractions in the bedroom, and avoiding big meals and exercise within a few hours of bedtime.
Surgery for epilepsy
Surgery is typically only considered after a person with epilepsy has unsuccessfully tried at least two medications to prevent seizures, or when doctors have found a brain lesion (an area of abnormal brain tissue) believed to be causing the seizures. When someone is found to be a good candidate, the surgery should be performed as soon as possible.
In considering a person’s candidacy for surgery to prevent seizures, doctors will review:
- Brain region involved
- Effect of the brain region on everyday function and behavior
Surgeons usually avoid operating in areas of the brain that are necessary for speech, movement, sensation, memory and thinking, or other important abilities.
While surgery can significantly reduce or even halt seizures for many people, any kind of surgery involves risk. Surgery for epilepsy does not always successfully reduce seizures and it can result in cognitive or personality changes as well as physical disability, even in people who are excellent candidates for it. Nonetheless, when medications fail, several studies have shown that surgery is much more likely to make someone seizure-free compared to attempts to use other medications. Anyone thinking about surgery for epilepsy should be assessed at an epilepsy center experienced in surgical techniques and should discuss the surgery’s risks and benefits with their healthcare team.
Even when surgery completely ends a person's seizures, it is important to continue taking antiseizure medication for some time, as prescribed by your health care provider. It is generally recommended that individuals continue medication for at least two years after a successful operation to avoid recurrence of seizures.
Surgical procedures for treating epilepsy disorders include:
- Surgery to remove a seizure focus involves removing the defined area of the brain where seizures originate. It is the most common type of surgery for epilepsy, which doctors may refer to as a lobectomy or lesionectomy and is appropriate only for focal seizures that originate in just one area of the brain.
- Multiple subpial transection may be performed when seizures originate in part of the brain that cannot be removed. It involves making a series of cuts that are designed to prevent seizures from spreading into other parts of the brain while leaving the person's normal abilities intact.
- Corpus callosotomy or severing the network of neural connections between the right and left halves (hemispheres) of the brain, is done primarily in children with severe seizures that start in one half of the brain and spread to the other side. Corpus callosotomy can end drop attacks and other generalized seizures. However, the procedure does not stop seizures in the side of the brain where they originate, and these focal seizures may get worse after surgery.
- Hemispherectomy and hemispherotomy involve removing half of the brain's cortex, or outer layer. These procedures are used predominantly in children who have seizures that do not respond to medication because of damage that involves only half the brain, as in Rasmussen's encephalitis.
- Thermal ablation for epilepsy , also known as laser interstitial thermal therapy, directs energy to a specific, targeted brain region causing the seizures (the seizure focus). The energy, which is changed to thermal energy, destroys the brain cells causing the seizures. Laser ablation is less invasive than open brain surgery for treating epilepsy.
Some people may use neurostimulation devices to treat their epilepsy. These d evices deliver electrical stimulation to the brain to reduce seizure frequency:
- Vagus nerve stimulation involves surgically implanting a device under the skin of the chest. The device, which is attached by wire to the vagus nerve in the lower neck, delivers short bursts of electrical energy to the brain.
- Responsive stimulation uses an implanted device that analyzes brain activity patterns to detect a forthcoming seizure. Once detected, the device administers an intervention, such as electrical stimulation or a fast-acting drug to prevent the seizure from occurring.
- Deep brain stimulation involves surgically implanting an electrode connected to a pulse generator (similar to a pacemaker) to deliver electrical stimulation to specific areas in the brain to regulate electrical signals in neural circuits.
How can I or my loved one live with epilepsy and seizures?
Many people with epilepsy can do the same things as people without the disorder and have successful and productive lives. One-third or more of people with epilepsy, however, may have cognitive or neuropsychiatric symptoms that can negatively impact their quality of life. Many people with epilepsy who respond to treatment may go months or years without having a seizure.
People with treatment-resistant epilepsy may have as many as hundreds of seizures a day or they may have one seizure a year with sometimes disabling consequences. Having treatment-resistant epilepsy is associated with an increased risk of cognitive impairment, particularly if the seizures developed in early childhood. These impairments may be related to the underlying conditions associated with the epilepsy rather than to the epilepsy itself.
Special risks associated with epilepsy Although many people with epilepsy lead full, active lives, there is an increased risk of death or serious disability associated with epilepsy. There may be an increased risk of suicidal thoughts or actions related to some antiseizure medications that are also used to treat mania and bipolar disorder. Two life-threatening conditions associated with epilepsy are status epilepticus and sudden unexpected death in epilepsy (SUDEP). Status epilepticus is a potentially life-threatening condition in which a person either has an abnormally prolonged seizure (over five minutes) or does not fully regain consciousness between recurring seizures. Status epilepticus can be convulsive (where signs of a seizure are seen) or nonconvulsive (which cannot be seen and is diagnosed by an abnormal electroencephalogram or EEG). Nonconvulsive status epilepticus may look like a long episode of confusion, agitation, loss of consciousness, or even coma. Evidence has shown that five minutes is sufficient to damage neurons and that seizures are unlikely to end on their own, making it necessary to seek medical care immediately. SUDEP (Sudden Unexplained Death in Epilepsy ) refers to deaths in people with epilepsy that are not from injury, drowning, or other known causes . Most, but not all, cases of SUDEP happen during or right after a seizure. Current research on SUDEP points to abnormal brain activity that impacts heart and respiratory function. This may be due to variations in a person’s genes, particularly genes that cause epilepsy and also affect heart function. SUDEP can occur at any age and people with seizures that are difficult to control tend to have a higher incidence of SUDEP. People with epilepsy may be able to reduce their risk of SUDEP by carefully taking all antiseizure medication as prescribed and making sure they are receiving the best possible care for their epilepsy. Not taking the prescribed dosage of medication or not taking the most appropriate medication on a regular basis may increase the risk of SUDEP, especially in people who are taking more than one medication.
Mental health and stigmatization
Depression is common among people with epilepsy. In adults with epilepsy, depression and anxiety are the two most frequent mental health diagnoses. Depression or anxiety in people with epilepsy can be treated with counseling or most of the same medications used in people who do not have epilepsy. People with epilepsy should discuss their symptoms of mental health issues with their healthcare professionals so they can receive the appropriate treatments and care.
Children with epilepsy have a higher risk of developing depression and/or attention deficit hyperactivity disorder (ADHD) compared with their peers. Behavioral problems and/or mental health issues may precede the onset of seizures in some children. Counseling and support groups can help families cope with epilepsy in a positive manner.
Driving and recreation
Some states may not issue a driver’s license to a person with epilepsy. Individuals with epilepsy may be able to get an exception if they can demonstrate a period of being seizure-free, or if their seizures only happen during sleep.
The risk of seizures may also limit a person’s ability to participate in sports, exercise, or other recreational activities, including climbing, sailing, swimming, or working on ladders. There is some evidence that regular exercise may improve seizure control in some people, but this should be done under a doctor's supervision. The benefits of sports participation may outweigh the risks. Coaches and activity leaders can take appropriate safety precautions. Individuals with epilepsy should avoid dehydration, overexertion, and low blood sugar, as these problems can increase the risk of seizures.
Education and employment
By law, people with epilepsy in the U.S. cannot be denied employment or access to any educational, recreational, or other activity because of their epilepsy. However, significant barriers still exist for people with epilepsy in school and work. Antiseizure medications may cause side effects that interfere with concentration and memory. Children with epilepsy may need extra time to complete schoolwork, and they may need to have instructions or other information repeated for them. Some children with epilepsy will need special educational plans to help address their learning challenges. Teachers should be given instructions on what to do if a child in their classroom has a seizure, and parents should work with the school system to find reasonable ways to accommodate any special needs their child may have.
Pregnancy and parenthood
Epilepsy itself does not interfere with the ability to become pregnant and women who have epilepsy and take appropriate precautions have similar odds of having a healthy pregnancy and a healthy child to women without a chronic medical condition. With the appropriate selection of safe antiseizure medications during pregnancy, use of supplemental folic acid, and ideally, with pre-pregnancy planning, most people with epilepsy can have a healthy pregnancy with good outcomes for themselves and their developing child.
Women with epilepsy should be advised that some antiseizure medications carry an increased risk of birth defects. It is important to work with a team of providers that includes a neurologist and an obstetrician to learn about any special risks associated with epilepsy and antiseizure medications.
Children of parents with epilepsy have about five percent risk of developing the condition at some point, compared to roughly one percent in a child in the general population. However, the risk of developing epilepsy increases if a parent has a hereditary form of the disorder. Parents who are concerned that their epilepsy may be hereditary may wish to consult a genetics health care provider to determine their risk of passing on the disorder.
What are the latest updates on epilepsy and seizures?
NINDS conducts and supports research to better understand and diagnose epilepsy, develop new treatments, and ultimately, to prevent epilepsy. NINDS epilepsy research efforts include:
The Epilepsy Therapy Screening Program (previously called the Anticonvulsant Screening Program) was created in 1975 to facilitate the discovery of new antiseizure drugs and has contributed to the development of nearly a dozen approved medications.
NINDS Centers Without Walls (CWoW) for Collaborative Research in the Epilepsies are multicenter, multidisciplinary groups that address research challenges to advance prevention, diagnosis, and/or treatment of the epilepsies and related co-occurring conditions. NINDS’s epilepsy CWoW projects include:
- Epilepsy 4000 (Epi4K) was an international effort to analyze DNA from 4,000 people with epilepsy and their relatives to identify disease-causing genes. Epi4K has now expanded into the worldwide effort called the Epi25 Collaborative with support from the National Human Genome Research Institute .
- The Center for SUDEP Research (CSR) brought together a collaboration of researchers with diverse expertise from multiple academic institutions in the United States and England to study and understand Sudden Unexpected Death in Epilepsy (SUDEP).
- The Epilepsy Bioinformatics Study for Antiepileptogenic Therapy (EpiBioS4Rx) uses human and animal studies to investigate epilepsy that develops following traumatic brain injury (TBI) with the goal of identifying biomarkers (biological signs of disease) that could be used to predict who is most likely to develop epilepsy following TBI.
- The Channelopathy-Associated Epilepsy Research Center combines high-throughput technologies and high-content data modeling systems to investigate the functional consequences of genetic variants in channelopathy-associated epilepsy including Dravet Syndrome.
- The Epilepsy Multiplatform Variant Prediction (EpiMVP) aims to advance knowledge of genetic variants of uncertain significance in non-ion-channel epilepsy genes.
NINDS investigators on the NIH campus and NINDS-funded investigators around the country are conducting clinical studies aimed at finding better ways to safely detect, treat, or prevent epilepsy.
Several projects relevant to epilepsy are funded through the Brain Research through Advancing Innovative Neurotechnologies (BRAIN) Initiative®. These efforts aim to better understand, measure, and monitor how the brain generates neural activity and are working to develop new technologies and devices to measure brain activity, predict seizure onset, and deliver therapeutic stimulation to limit seizure activity.
Other areas of epilepsy research include:
- Advancing gene sequencing tools and technologies to identify genetic mutations that cause various forms of epilepsy.
- Understanding the underlying biology that contributes to epilepsy, including how brain cells communicate with one another and the role that various brain chemicals play in the disease.
- Developing new animal models to learn about the causes of epilepsy, ways to prevent the disease, and test promising therapies.
- Studying brain tissue obtained from epilepsy surgery or at the time of death to increase knowledge into causes of epilepsy and how they affect the brain.
- Identifying the genes and their function(s) relevant to rare epilepsy syndromes so that targeted treatments can be developed for children and adults with these causes of epilepsy.
- Developing new therapies through preclinical studies utilizing the NINDS Translational research programs as well as the Blueprint Neurotherapeutics programs.
- Studying the impact of early in life seizures on cognitive and behavioral outcomes in children with epilepsy.
- Using artificial intelligence (AI) and machine learning (ML) to help to identify the specific area of the brain where the seizures begin.
How can I or my loved one help improve care for people with epilepsy and seizures?
Consider participating in a clinical trial so clinicians and scientists can learn more about epilepsy, seizures, and related disorders. Clinical research uses human study participants to help researchers learn more about a disorder and perhaps find better ways to safely detect, treat, or prevent disease.
All types of study participants are needed— those who are healthy or may have an illness or disease— of all different ages, sexes, races, and ethnicities to ensure that study results apply to as many people as possible, and that treatments will be safe and effective for everyone who will use them.
For information about participating in clinical research visit NIH Clinical Research Trials and You . Learn about clinical trials currently looking for people with epilepsy and seizures at Clinicaltrials.gov .
There are additional ways for people with epilepsy and their families can help advance research. Pregnant people who are taking antiseizure drugs can help researchers learn how these drugs affect unborn children by participating in the The North American Antiepileptic Drug (AED) Pregnancy Registry . Registry participants are given educational materials on pre-conception planning and perinatal care and are asked to provide information about the health of their children, which is kept confidential and only used in an anonymized fashion by researchers.
People with epilepsy can help research efforts by making arrangements to donate tissue either at the time of surgery for epilepsy or at the time of death. Researchers can then use the tissue to study epilepsy and other disorders to better understand what causes seizures. For example, The NIH NeuroBioBank is an effort to coordinate a network of brain banks it supports in the U.S. where brain tissue and data are collected, evaluated, stored, and made available to researchers in a standardized way for the study of neurological, psychiatric and developmental disorders, including epilepsy. A l ist of participating NIH NeuroBioBank repositories and additional brain banks are maintained on the NIH NeuroBioBank website. Each brain bank may have different protocols for registering a potential donor. Individuals are strongly encouraged to contact the brain bank directly to learn more.
Where can I find more information about epilepsy and seizures? Information about epilepsy and seizures may be available from the following organizations and resources: American Epilepsy Society Phone: 312-883-3800 BeMedWise Program at NeedyMeds Phone: 978-281-6666 Caregiver Action Network Phone: 202-454-3970 or Caregiver Help Desk: 855-227-3640 Child Neurology Foundation Phone: 888-417-3435 CURE Epilepsy Phone: 312-255-1801 or 844-231-2873 Dravet Syndrome Foundation Phone: 203-392-1950 Epilepsy Alliance of America Phone: 800-642-0500 Epilepsy Leadership Council Phone: 312-883-3800 Epilepsy Foundation Phone: 800-332-1000 Family Caregiver Alliance Phone: 415-434-3388 or 800-445-8106 International League Against Epilepsy Phone: +860-586-7547 Lennox-Gastaut Syndrome (LGS) Foundation Phone: 718-374-3800 National Organization for Rare Disorders (NORD) Phone: 203-744-0100 or 800-999-6673 Partners Against Mortality in Epilepsy (PAME) The Charlie Foundation for Ketogenic Therapies Phone: 310-393-2347 The North American Antiepileptic Drug (AED) Pregnancy Registry Phone: 888-233-2334 Tuberous Sclerosis Complex Alliance Phone: 800-225-6872 or 301-562-9890 SLC6A1 Connect Phone: 303-907-8038
Learn about related topics
- Dravet Syndrome
- Febrile Seizures
- Lennox-Gastaut Syndrome
Fellow of the American Epilepsy Society
Accepting 2024 Applications This Summer
AES offers a Fellow of the American Epilepsy Society (FAES) designation to recognize long-term, committed members who have shared their time and talents to advance both the AES mission and the field of epilepsy.
Selection as a Fellow of the American Epilepsy Society is an honor that recognizes professional accomplishment and dedication in the field of epilepsy. It is a way that AES recognizes members who have made especially meaningful contributions over time through research, clinical or academic achievement, volunteerism, and/or leadership.
Fellows are recognized at the AES Annual Meeting and on the AES website. In professional communications, Fellows may use the FAES designation along with other credentials after their name.
Criteria and Required Materials
You may be eligible to earn the FAES designation if:
- You are a current AES member in good standing and have been an Active, Professional, or International member for at least the last seven consecutive years . To qualify, your continuous membership with AES must have begun on or before December 31, 2016. Fellows are expected to maintain their memberships and remain in good standing with AES.
- Or, you are currently a Senior or Associate member and have previously been an Active, Professional, or International member for at least seven consecutive years.
- You have attended (in person or digitally) a minimum of five out of the last ten AES Annual Meetings.
- You have significantly contributed to advancing the AES mission through volunteerism or leadership, epilepsy research, and/or clinical care.
To apply you will need the following:
- Completed online application form
- Two letters of recommendation from peers. One letter must be from a FAES member. Below you can find a list of current AES members who have earned the FAES designation.
- Your Curriculum Vitae.
- One-time, non-refundable application fee of $100
The AES Membership Committee reviews all applications, and the AES Board of Directors approves them. Applicants will be notified of their application status during the fall of 2024.
Members who may be eligible based on years of membership and attendance at Annual Meetings are notified and invited to apply via email.
Questions? Please contact the member services team at [email protected] .
Shan Abbas, MD, FAES Ahmed Abdelmoity, MD, FAES Taylor Abel, MD, FAES Nicholas Abend, MD, FAES Karine Abou Khaled, MD, FAES Bassel Abou-Khalil, MD, FAES Daniel Abrams, MD, FAES Abuhuziefa Abubakr MD, FRCP, FAES Vinita Acharya, MD, FAES Jayant Acharya MD, DM, FAES Seema Adhami, PhD, FAES Pegah Afra, MD, FAES Satish Agadi, MD, FAES Nitin Agarwal, MD, FAES Naoki Akamatsu, MD, PhD, FAES Raidah Al-Baradie, MD, FAES Dara Albert, DO, MEd, FAES Amza Ali, MD, FRCP, FAES Imran Ali, MD, FAAN, FAES Sasha Alick-Lindstrom, MD, FAES Jane Allendorfer, PhD, FAES Mario Alonso-Vanegas, MD, FAES Hamada Altalib, DO, MPH, FAES Gail Anderson, PhD, FAES Chinekwu Anyanwu, MD, FAES Juan Appendino, MD, FAES Amir Arain, MD, FAES John Archer, MBBS, PhD, FAES Nikesh Ardeshna, MD, FAES Daniel Arndt, MD, FAES Susan Arnold, MD, FAES Ravindra Arya, MD, FAES Eishi Asano, MD, PhD, MS, FAES Gewalin Aungaroon, MD, FAE Joan Austin, PhD, RN, FAES Stephane Auvin, MD, PhD, FAES Reda Badry, MD, FAAN, FAES Anto Bagic, MD, PhD, FAES Jacquelyn Bainbridge, PharmD, FCCP, MSCS, FAES Antoaneta Balabanov, MD, FAES Susanta Bandyopadhyay, MD, PhD, FAES Luca Bartolini, MD, FAES Maysaa Basha, MD, FAES Gaston Baslet, MD, FAES Robert Beach, MD, PhD, FAES Joshua Bear, MD, MA, FAES Elizabeth Bebin, MD, MPA, FAES Mark Bej, MD, FAES Nicholas Beimer, MD, FAES Luis Bello-Espinosa, MD, FAES Selim Benbadis, MD, FAES Elinor Ben-Menachem, MD, PhD, FAES Meriem Bensalem-Owen, MD, FAES Eduard Bercovici, MD, MS, MSc, R.EEGT, FRCP, FAES Michel Berg, MD, FAES Bryan Berger, MD, MHA, FAES Gregory Bergey, MD, FAES Peter Bergin, MBChB, MD, FAES Madison Berl, PhD, FAES Adriana Bermeo-Ovalle, MD, FAES Angela Birnbaum, PhD, FAES Jason Bisping, MD, FAES Victor Biton, MD, FAES Thomas Bleck, MD, FAES Jeffrey Blount, MD, FAES Andrew Blum, MD, PhD, FAAN, FAES Michael Boffa, MD, FAES Jane Boggs, MD, FAES Deana Bonno, MD, FAES Robert Bonwetsch, MD, FAES Kirsten Bracht, MD, FAES Jeffrey Britton, MD, FAES Amy Brooks-Kayal, MD, FAES Donna Broshek, PhD, FAES James Bruno, MD, FAES Ellen Bubrick, MD, FAES Jeffrey Buchhalter, MD, PhD, FAES Marjorie Bunch, MD, FAES Richard Burgess, MD, PhD, FACNS, FAES David Burkholder, MD, FAES Jorge Burneo, MD, MSPH, FAES Robyn Busch, PhD, FAES Paul Carney, MD, FAES Gregory Cascino, MD, FAES Jose E. Cavazos, MD, PhD, FAES Fernando Cendes, MD, PhD, FAES James Cereghino, MD, FAES Kevin Chapman, MD, FAES Sirichai Chayasirisobhon, MD, FAAN, FAES David Chen, MD, FAES Hai Chen, MD, PhD, FAES Stephanie Chen, MD, FAES Jocelyn Cheng, MD, FAES Raymond Cheng, MD, FAES Michael Chez, MD, FAES Yotin Chinvarun, MD, PhD, FAES Bilal Choudry, MD, FAES Nitish Chourasia, MD, FAES Jakob Christensen, MD, PhD, Dr. Med. Sci., FAES Steve Chung, MD, FAES Jeffrey Chung, MD, FAES Jean Cibula, MD, FAES Michael Cilliberto, MD, FAES Dave Clarke, MBBS, FAES Mary Connolly, MD, FRCPC, FAES Jeannine Conway, PharmD, FAES Paul Cooper, DM, MA, FRCP, FAES Louis Dang, MD, PhD, FAES Rohit Das, MD, MPH, FAES Kathryn Davis, MD, FAES Ronald Davis, MD, MPH, FAES William DeBassio, PhD, MD, FAES Sunita Dergalust, PharmD, BCPS, FAES Laxmikant Deshpande, PhD, FAES Kamil Detyniecki, MD, FAES Orrin Devinsky, MD, FAES Sandra Dewar, PhD, APRN, FAES Jennifer DeWolfe, DO, FAES Monica Dhakar, MD, FAES Ashish Dhir, PhD, FAES Marc Dichter, MD, PhD, FAES Dennis Dlugos, MD, FAES Michael Doherty, MD, FAES Elizabeth Donner, MD, MSc, FRCPC, FAES Julia Doss, PsyD, FAES Victor Dostrow, MD, FAES Michelle Dougherty, MD, FAES Kendra Drake, MD, FAES Daniel Drane, PhD, FAES Joseph Drazkowski, MD, FAES Cornelia Drees, MD, FAES Susan Duberstein, MD, FAES F. Edward Dudek, PhD, FAES Barbara Dworetzky, MD, FAES Yaman Eksioglu, MD, PhD, FAES Ro Elgavish, MD, PhD, FAES Dawn Eliashiv, MD, FAES Jerome Engel, MD, PhD, FAES Kathy England, FNP-BC, FAES Dario Englot, MD, PhD, FAES Lia Ernst, MD, FAES Krista Eschbach, MD, FAES Mill Etienne, MD, MPH, FAES Alan Ettinger, MD, MBA, FAES Sara Eyal, MD, FAES Stephen Falchek, MD, FAES Jessica Falco-Walter, MD, FAES Pue Farooque, DO, FAES Philip Fastenau, PhD, FAES R. Edward Faught, MD, FAES Lauren Feldman, DO, FAES Elizabeth Felton, MD, PhD, FAES Hua-Jun Feng, PhD, FAES Enrique Feoli, MD, FAES Victor Ferastraoaru, MD, FAES James Ferrendelli, MD, FAES Evan Fertig, MD, FAES Anteneh Feyissa, MD, MS, MSc, FAES David Ficker, MD, FAES Robert Fisher, MD, PhD, FAES Robert Flamini, MD, FAES Nancy Foldvary-Schaefer, DO, MS, FAES Perry Foreman, MD, PhD, FAES Nathan Fountain, MD, FAES Birgit Frauscher, MD, FAES Jacqueline French, MD, FAES Lauren Frey, MD, FAES Daniel Friedman, MD, FAES Alfred Frontera, MD, FAES Michael Frost, MD, FAES Michael Frucht, MD, FAES Aradia Fu, MD, FAES Denson Fujikawa, MD, FAES Marcio Furtado, PhD, FAES William Gaillard, MD, FAES Aristea Galanopoulou, MD, PhD, FAES Jay Gavvala, MD, MS, MSc, FAES Eduardo Garcia, MD, FAES Nina Garga, MD, FAES Satya Gedela, MD, MRCPI, FAES Eric Geller, MD, FAES James Geyer, MD, FAES Barry Gidal, PharmD, FAES Tatyana Gitlevich, MD, FAES Chaitali Ghosh, PhD, FAHA, FAES Bruce Gluckman, PhD, FAES Joseph Glykys, MD, PhD, FAES Cristina Go, MD, FAES Daniel Goldenholz, MD, PhD Alan Goldin, MD, PhD, FAES Alica Goldman, MD, PhD, FAES Victor Gonzalez Montoya, MD, FAES Howard Goodkin, MD, PhD, FAES Michael Goodman, MD, MMM, FAES Jill Gotoff, MD, FAES Heidi Grabenstatter, PhD, FAES Arthur Grant, MD, PhD, FAES L. John Greenfield, MD, PhD, FAES Zachary Grinspan, MD, FAES Shanna Guilfoyle, PhD, FAES Ajay Gupta, MD, FAES Suresh Gurbani, MD, PhD, FAES
Ahsan Moosa Naduvil Valappil, MD, FAES Hiroki Nariai, MD, PhD, MS, FAES Dean Naritoku, MD, FAES Marcus Ng, MD, FRCPC, FACNS, FAES Yu-Tze Ng, MD, FAES Dang Nguyen, MD, FAES Colin Nguyen, MD, FAES Lorraine Newborn-Palmer, DNP, APRN, RN, FAES Katherine Nickels, MD, FAES Conrad Nievera, MD, FAES Katherine Noe, MD, PhD, FAES Jeffrey Noebels, MD, PhD, FAES Edward Novotny, MD, FAES Lilia Nunez-Orozco, MD, FAES Marc Nuwer, MD, PhD, FAES Terence O'Brien, MD, FRACP, FAES Juan Ochoa, MD, FAES Jeffrey Ojemann, MD, FAES Piotr Olejniczak, MD, PhD, FAES Chima Oluigbo, MD, FAES Tomonori Ono, MD, PhD, FAES Kalarickal Oommen, MD, FAES Melissa Osborn, BSN, RN, FAES Joel Oster, MD, FAES Daniel Orta, MD, FAES Temitayo Oyegbile-Chidi, MD, PhD, FAES A. LeBron Paige, MD, FAES Jayoung Pak, MD, FAES Juliann Paolicchi, MD, MA, FAES Kimberly Pargeon, MD, FAES Yong Duck Park, MD, FAES Jun Park, MD, FAES Karen Parko, MD, FAES Jaime Parra Gomez, MD, PhD, FAES Erasmo Passaro, MD, FAES Hema Patel, MD, FAES Anup Patel, MD, FAES Sima Patel, MD, FAES Jay Pathmanathan, MD, PhD, FAES Phillip Pearl, MD, FAES Nigel Pedersen, MD, FANA, FAES Timothy Pedley, MD, FAES Page Pennell, MD, FAES Patricia Penovich, MD, FAES Freedom Perkins, MD, FAES M. Scott Perry, MD, FAES Elia Pestana Knight, MD, FAES Jurriaan Peters, MD, PhD, FACNS, FAES Ognen Petroff, MD, FAES Sandra Petty, MBBS, FRACP, PhD, FAES Donald Phillips, MD, MPH, FAES Jyoti Pillai, MD, FAES Neelan Pillay, MBChB, FCP (SA), FRCP (London) , FRCPC, FAES Jesus Pina Garza, MD, FAES Alberto Pinzon-Ardila, MD, PhD, FAES Ignacio Pita, MD, FAES Madona Plueger, APRN, ACNS-BC, FAES Annapurna Poduri, MD, MPH, FAES John Pollard, MD, FAES Brenda Porter, MD, PhD, FAES Roger Porter, MD, FAES Asuri Prasad, MD, FRCPC, FRCPE, FAES David Prince, MD, FAES Michael Privitera, MD, FAES Mary Jo Pugh, PhD, RN, FAES Mark Quigg, MD, MSc, FAES Imran Quraishi, MD, PhD, FAES Raj Rajaraman, MD, MS, FAES Vijayalakshmi Rajasekaran, MD, FAES Rajesh Ramachandran Nair, MD; FRCPC, FAES Patsy Ramey, MSN, RN, FAES R. Ramsay, MD, FAES Lekha Rao, MD, FAES Vikram Rao, MD, PhD, FAES Jaivir Rathore, MD, FAES Samba Reddy, PhD, RPh, FAES Ronald Reed, BS Pharm, PharmD, FAES Claus Reinsberger, MD, PhD, FAES Jong Rho, MD, FAES Awais Riaz, MD, PhD, FAES George Richerson, MD, PhD, FAES Anthony Ritaccio, MD, FAES James Riviello, MD, FACNS, FNCS, FAES Colin Roberts, MD, FAES Andres Rodriguez, MD, FAES Ildefonso Rodriguez-Leyva, MD, PhD, FAES Michael Rogawski, MD, FAES Joanne Rogin, MD, FAES John Rolston, MD, PhD, FAES Judith Roman, MD, FAES Steven Roper, MD, FAES William Rosenfeld, MD, FAES Andrea Rossetti, MD, FAES Marvin Rossi, MD, PhD, FAES Stephan Rueegg, MD, FAES Dragos Sabau, MD, FAES Kinshuk Sahaya, MD, FAES Martha Sajatovic, MD, FAES Vicenta Salanova, MD, FAES Jay Salpekar, MD, FAES Maria Sam, MD, FAES Debopam Samanta, MD, FAES Evan Sandok, MD, FAES Tristan Sands, MD, PhD, FAES Raman Sankar, MD, PhD, FAES Ram Sankaraneni, MD, FAES Rani Sarkis, MD, M.Sc., FAES Shifteh Sattar, MD, FAES Mona Sazgar, MD, FAES Morris Scantlebury, MBBS, FAES Steven Schachter, MD, FAES Ingrid Scheffer, MBBS, PhD, FRACP, FAES Steven Schiff, MD, PhD, FAES Sarah Schmitt, MD, FAES Janel Schneider, MD, FAES Mike Schoenberg, PhD, FAES Lara Schrader, MD, MSCR, FAES Stephan Schuele, MD, MPH, FAES Rebecca Schultz, PhD, RN, CPNP, FAES Jason Schwalb, MD, FAANS, FACS Lawrence Seiden, MD, FAES Syndi Seinfeld, DO, FAES Anbesaw Selassie, PhD, FAES Olga Selioutski, DO, FAES Linda Selwa, MD, FAES Udaya Seneviratne, FRACP, FAES Demitre Serletis, MD, PhD, FRCSC, FAANS, FACS, FAES Masud Seyal, MD, PhD, FAES Patricia Shafer, MN, RN, FAES Sona Shah, MD, FAES Visal Shah, MBBS, FAES Asim Shahid, MD, FAES Minoo Shams, MD, FAES Susan Shaw, MD, FAES Renee Shellhaas, MD, MS, FAES Anumeha Sheth, MD, FAES Raj Sheth, MD, FAES Jerry Shih, MD, FAES Shlomo Shinnar, MD, PhD, FAES Daniel Shrey, MD, FAES Hillary Shurtleff, PhD, FAES Sameena Siddiqui, MD, FAES Diosely Silveira, MD, PhD, FAES Anuradha Singh, MD, FAES Baldev Singh, MD, FAES Rajdeep Singh, MD, FACNS, FAES Vikas Singh, MD, MHSA, FAES Saurabh Sinha, MD, PhD, FACNS, FAES Deepa Sirsi, MD, FAES Joseph Sirven, MD, FAES Bilal Sitwat, MD, FAES Karen Skjei, MD, FAES Jeremy Slater, MD, FAAN, FAES Brien Smith, MD, FAES Georgette Smith, PhD, RN, CPNP-PC, FAES Lacey Smith, MS, FAES Michael Smith, MD, FAES Steven Smith, MD, FAES Elson So, MD, FAES Julie Socha, APRN, FAES Kenneth Sommerville, MD, FAES Marianna Spanaki, MD, PhD, MBA, FAES Kathy Speechley, PhD, FAES David Spencer, MD, FAES Dennis Spencer, MD, FAES Michael Sperling, MD, FAES Rebecca Spiegel, MD, FAES Mark Spitz, MD, FAES William Stacey, MD, PhD, FAES Erik St. Louis, MD, FAES Carl Stafstrom, MD, PhD, FAES Kevin Staley, MD, FAES Alan Stein, MD, FAES John Stern, MD, FAES David Steven, MD, FRCSC, FAES Laura Strom, MD, FAES Kenji Sugai, MD, PhD, FAES Joseph Sullivan, MD, FAES Thomas Sutula, MD, PhD, FAES Barbara Swartz, MD, PhD, FAAN, FANA, FAES Thomas Swanson, MD, FAES Charles Szabo, MD, FAES Jerzy Szaflarski, MD, PhD, FAES Masanori Takeoka, MD, FAES Nitin Tandon, MD, FAES Richard Tang-Wai, MDCM, DM, FRCPC, FAES Adriana Tanner, MD, FAES Olga Taraschenko, MD, PhD William Tatum, DO, FAES Jose Tellez-Zenteno, MD, PhD, FRCP (C), CSCN (EEG), FAES * Francine Testa, MD, FAES William Theodore, MD, FAES Thimmasettappa Thippeswamy, PhD, FAES Ashley Thomas, MD, FAES Azreena Thomas, MD, FAES Tricia Ting, MD, FAES Francis Tirol, MD, FAES Jeffrey Titus, PhD, FAES Benjamin Tolchin, MD, MS Alan Towne, MD, MPH, FAES Lily Tran, MD, FAES David Treiman, MD, FAES Dorothee Trenite, MD, PhD, MPH Noriko Tsuru, MD, FAES Carol Ulloa, MD, FAES Alexandra Urban, MD, FAES Ignacio Valencia, MD, FAES Anne Van Cott, MD, FAES Paul Van Ness, MD, FAES Kevan VanLandingham, MD, PhD, FAES Naymee Velez-Ruiz, MD, FAES Libor Velisek, PhD, FAES Anu Venkat, MD, FAES Akila Venkataraman, MD, FAES Jorge Vidaurre, MD, FAES David Vossler, MD, FAES Angela Wabulya, MBChB, FAES Janelle Wagner, PhD, FAES Sonya Wang, MD, FAES Braxton Wannamaker, MD, FAES Sandran Waran, MD, FAES Meghan Ward, MD, FAES Vibhangini Wasade, MD, FAES Claude Wasterlain, MD, FAES Elizabeth Waterhouse, MD, FAES Robert Wechsler, MD, PhD, FAES Sarah Weckhuysen, MD, PhD, FAES Howard Weiner, MD, FAES Mindl Weingarten, PharmD, BCPPS, FAES Arie Weinstock, MD, FAES Shennan Weiss, MD, PhD, FAES Timothy Welty, PharmD, FAES David Wheeler, MD, PhD, FAES James Wheless, BSPharm, MD, FAES Robyn Whitney, MD, FRCPC< FAES Peter Widdess-Walsh, MD, FAES Angus Wilfong, MD, FAES Korwyn Williams, MD, PhD, FAES L. James Willmore, MD, FAES Jennifer Wong, PhD, FAES Michael Wong, MD, PhD, FAES Victoria Wong, MD, FAES Lily Wong-Kisiel, MD, FAES Courtney Wusthoff, MD, FAES Thomas Wychowski, MD, FAES Elaine Wyllie, MD, FAES Michael Xu, MD, PhD, FAES Qi Helen Xu, MD, FAES Takamichi Yamamoto, MD, MS, DMSc, FAES Ji Yeoun (Jenna) Yoo, MD, FAES Elissa Yozawitz, MD, FAES Wenbo Zhang, MD, PhD, FAES Xiangping Zhou, MD, PhD, FAES Andrew Zillgitt, DO, FAES Deepti Zutshi, MD, FAES *Deceased

- Find a Doctor
- Transfer a Patient
- Patient Portal

2024 Acquired Brain Injury and Spinal Cord Injury Symposium
Course description.
This interdisciplinary symposium will focus on the current evidenced-based practice and research for the treatment of those with acquired brain injury and spinal cord injury. The symposium will provide an educational opportunity for rehabilitation professionals focusing on the medical management and rehabilitative treatment interventions.
Course Learning Objectives
- The participant will be able to describe how medical interventions affect functional recovery.
- The participant will describe current research in acquired brain injury and spinal cord injury.
- The participant will be able to identify challenges associated with living with a disability.
- The participant will be able to list therapeutic interventions utilized post acquired brain injury and spinal cord injury.
Registration Information
Cme information.

*CEUs will be awarded to participants after they have successfully completed the post-symposium assessment and learning outcomes assessment.
Hybrid Event October 12-13, 2024
Early Bird Prices: Register Today
Vendor Registration Coming Soon

Date, Time, and Location
In-Person Goldman Auditorium & Virtual Availability Saturday and Sunday, October 12-13, 2024
Target Audience
This program is designed for allied health professionals who treat people with acquired brain injury and spinal cord injury.
Speaker Information
All times refer to Arizona time (Pacific Daylight Time).
Course Directors

Disclosures
- Disclosures pending
To give you the best possible experience, this site uses cookies. By continuing to use the site, you agree that we can save them on your device.
Tools & Resources
- Find Your Local Chapter
- Use my current location

- Our Editors
Sloka Iyengar, PhD

Basic Science Editor
Sloka Iyengar PhD, PMP, grew up in India, where she had the amazing opportunity of working as an administrator at a shelter for stray animals. This is where she started wondering how animals (and humans) regulate temperature, feel hunger, and what might kick off maternal behavior.
These ideas led her to pursue her doctoral work in neuroscience. At the University of South Carolina, she used a technique called electrophysiology to better understand epilepsy circuits. As a postdoctoral fellow in New York, she studied the role of postnatal neurogenesis (the birth of neurons in the adult brain) in the hippocampus. After this, she worked as a clinical researcher at the Northeast Regional Epilepsy Group, where she facilitated clinical trials for adults and children with epilepsy and set up projects to understand the mechanisms involved in brain tumor-related epilepsy. She has advocated for increased funding for epilepsy research in Washington, D.C., and is involved in epilepsy-related projects in India.
Dr. Iyengar currently works as an associate medical director at a medical communication agency in New York, where she works with pharmaceutical companies to develop content for education and stakeholder engagement. In her non-science time, she is a professional dancer and an avid swimmer. Her goal as the basic science editor for epilepsy.com is to bring cutting-edge research in the field of epilepsy to you.
Reach out to Dr. Iyengar at www.slokaiyengar.com if there is a topic that interests you and you want to know more about it.
Authored By: Epilepsy Foundation Marketing & Communications
Selim Benbadis, MD
Stephan U Schuele, MD, MPH
Epilepsy Centers
Epilepsy centers provide you with a team of specialists to help you diagnose your epilepsy and explore treatment options.
Epilepsy Medication
Find in-depth information on anti-seizure medications so you know what to ask your doctor.
Epilepsy and Seizures 24/7 Helpline
Call our Epilepsy and Seizures 24/7 Helpline and talk with an epilepsy information specialist or submit a question online.
Get information, tips, and more to help you manage your epilepsy.
Related Stories

People & Community
Debunking Epilepsy Misconceptions
Press Releases
Patient Organizations Applaud Release of Affordable Care Act Rule to Protect All Patients from Discrimination When Accessing Health Care

What is the Epilepsy Foundation’s Multicultural Outreach Program?
Sign Up for Emails
Stay up to date with the latest epilepsy news, stories from the community, and more.

IMAGES
VIDEO
COMMENTS
The breakdown of neurovascular coupling in the diseased state specifically Epilepsy and Alzheimer's disease. University of Sheffield Department of Psychology. Epilepsy is the most common neurological condition in the UK, affecting 1 - 2 % of the population. Epilepsies often involve only a small area of the brain - the epileptic focus ...
The University of Manchester Faculty of Biology, Medicine and Health. Epilepsy is a chronic neurological disease characterised by recurrent spontaneous seizures and cognitive co-morbidities. Current small molecule approaches to treating epilepsy are ineffective in a significant portion of cases, and are associated with substantial adverse effects.
Roger Chang, MD, PhD Adult Epilepsy Fellow. Roger earned his undergraduate degree in Biomedical Engineering at Washington University in St. Louis. He completed his doctorate work in the lab of Dr. Robert Edwards at UCSF, determining the unique, dual role of chloride in synaptic vesicular glutamate transport. He subsequently received his MD at UCSF.
Nuyujukian, Paul, MD, PhD (Brain Interfacing Laboratory) The Brain Interfacing Laboratory is interested in the applicability of brain-machine interfaces as a platform technology for a variety of brain-related medical conditions, particularly stroke and epilepsy. This research spans both preclinical models and human clinical studies.
James Tao MD PhD is interested in determining the cerebral substrates of scalp EEG epileptiform patterns, in order to improve the accuracy of non-invasive seizure localization during epilepsy surgery. His long-term interests include investigations of the mechanisms of epileptogenesis and of new modalities of epilepsy therapy.
Epilepsy. Jerome Engel Jr., MD, PhD. The UCLA Adult Epilepsy Program has been engaged in both clinical and basic research for over 54 years, funded by the National Institutes of Health, as well as by other sources. Clinical investigations involve the development of new diagnostic and therapeutic procedures and the evaluation of the beneficial ...
The Penn Epilepsy fellowship is now recruiting fellows starting training on July 1, 2025. The fellowship is participating in the Epilepsy and Clinical Neurophysiology Fellowship Match The New Epilepsy and Clinical Neurophysiology Fellowship Match with applications accepted through ERAS . November 15, 2023 Applicants may begin submitting ...
The NGG is a collaborative and interdisciplinary PhD program that provides training for careers in neuroscience research, teaching and more. Our training program is designed to provide a strong foundation of neuroscience knowledge while at the same time taking into account each student's strengths, needs and career goals.
Claude Steriade, MD. Assistant Professor, Department of Neurology Expertise: epilepsy, neuroinflammation, and autoimmune neurology Methodological skills: neuroimaging, clinical trials, microbiome, and predictive modeling. NYU Langone's Comprehensive Epilepsy Center comprises faculty who are leaders in the field of epilepsy research.
Our Research Mission. Since 2003, we've funded nearly half of the therapies in the epilepsy clinical pipeline. We are developing an epilepsy research ecosystem that covers all parts of therapy, from idea to market. Our research initiatives include: Innovation programs that test new ideas and follow new research leads.
2021 AES/NINDS Epilepsy Research Benchmarks. Area I: Understand the causes of the epilepsies and their relationship to epilepsy-associated neurologic, psychiatric, and somatic conditions. A. Identify the many genes and molecular pathways associated with the epilepsies and epilepsy-related conditions.
Focus On Epilepsy Research. The epilepsies are a set of disorders characterized by recurring seizures, or disturbances in the electrical activity of the brain. Epilepsy affects people of all ages, from infants to the aged, and can result from many causes, including genetic variations, illness, head injury, or abnormal brain development.
The Emory Epilepsy Center is part of the Emory Brain Health Center. The Emory University Epilepsy Program is a multi-specialty group of physicians, neuropsychologists, and nurses from the departments of Neurology, Neurosurgery, Pediatrics, Physical Medicine and Rehabilitation and Radiology. The Epilepsy Program provides specialized clinical ...
Maureen Lacy, PhD. Psychology. Epilepsy Nurse. Shadrach Castillo, RN. Registered Electroencephalographic Technologist. Diane Suarez, REEGT. Meet our dedicated epilepsy team at UChicago Medicine. With expertise in cutting-edge treatments and personalized care, our specialists are committed to guiding you through every step of your epilepsy journey.
Epilepsy is a neurological disorder that affects about 65 million people worldwide. Although antiepileptic drugs provide sufficient control of seizures in approximately 70% of patients with epilepsy, the remaining 30% are resistant to monotherapy. This means around 20 million people worldwide face significant adverse life-long consequences such as sudden unexpected death from epileptic ...
2016. Mark Nowell - Novel multimodality imaging in the planning and surgical treatment of epilepsy. Christian Vollmar - Neuroimaging of functional and structural alterations in juvenile myoclonic epilepsy and frontal lobe epilepsy. Britta Wandschneider - The effects of genes, antiepileptic drugs and risk of death on functional anatomy and ...
Building New Technologies to Aid Epilepsy Patients. Brian Litt, MD, a professor of Neurology and Bioengineering. The new epilepsy unit will be a place where tons of systems neuroscience research converges — everything from basic science research to the stuff I do to develop and build devices for people with neurologic disease and epilepsy.
Call 310-794-1195 to request an appointment with an epilepsy specialist at UCLA Health. To schedule an appointment with the Seizure Disorder Center, please call 424-260-8836. Our epilepsy specialists are experts in diagnosing and treating seizure disorders. Learn more about epilepsy medicine at UCLA Health, or find a doctor today.
Be matriculating in a full-time doctoral (PhD) program in a field relevant to epilepsy research with an academic career focus. Have a defined research plan and access to institutional resources to conduct the proposed project. Have a qualified mentor(s) with expertise to supervise and provide guidance on epilepsy-related research. ...
Please call the Epilepsy & Seizures 24/7 Helpline at 1-800-332-1000 or submit a question online. Getting control of your seizures takes specialized care. Find a doctor who can help you diagnose and treat your seizures effectively.
Epilepsy is a chronic brain disorder in which groups of nerve cells, or neurons, in the brain sometimes send the wrong signals and cause seizures. Epilepsy (sometimes referred to as a seizure disorder) can have many different causes and seizure types. Epilepsy varies in severity and impact from person to person and can be accompanied by a range of co-existing conditions.
AES offers a Fellow of the American Epilepsy Society (FAES) designation to recognize long-term, committed members who have shared their time and talents to advance both the AES mission and the field of epilepsy. Selection as a Fellow of the American Epilepsy Society is an honor that recognizes professional accomplishment and dedication in the ...
Please call the Epilepsy & Seizures 24/7 Helpline at 1-800-332-1000 or submit a question online. If you have trouble controlling your seizures, find an epilepsy center to get specialized care. Epilepsy centers have experts in the diagnosis, evaluation, and treatment of epilepsy.
A shift toward this new realm of thought can be traced back to two Children's Colorado patients, Vina and Lena Gozeh, who suffered from near-constant seizures — almost 100 per day. Dr. Demarest and his team knew that the sisters, who experienced the same symptoms, had a genetic condition. Lena and Vina, born in 2008 and 2011, respectively ...
Course Description. This interdisciplinary symposium will focus on the current evidenced-based practice and research for the treatment of those with acquired brain injury and spinal cord injury. The symposium will provide an educational opportunity for rehabilitation professionals focusing on the medical management and rehabilitative treatment ...
Sloka Iyengar PhD, PMP, grew up in India, where she had the amazing opportunity of working as an administrator at a shelter for stray animals. This is where she started wondering how animals (and humans) regulate temperature, feel hunger, and what might kick off maternal behavior. These ideas led her to pursue her doctoral work in neuroscience.
Some 30% to 40% of patients do not respond to medications for depression and obsessive-compulsive disorder (OCD), but half of them could be helped by a noninvasive in-office procedure. To mark National Mental Health Awareness Month in May, we talk to psychiatrist Katherine Scangos, MD, PhD, co-director of the Transcranial Magnetic Stimulation ...